Adverse drug reactions are among the most frequent problems encountered clinically and represent a common cause for hospitalization. They occur most frequently in pts receiving multiple drugs and are caused by:
• Errors in self-administration of prescribed drugs (quite common in the elderly);
• Exaggeration of intended pharmacologic effect (e.g., hypotension in a pt given antihypertensive drugs);
• Concomitant administration of drugs with synergistic effects (e.g., aspirin and warfarin);
• Cytotoxic reactions (e.g., hepatic necrosis due to acetaminophen);
• Immunologic mechanisms (e.g., quinidine-induced thrombocytopenia, hydralazine-induced SLE);
• Genetically determined enzymatic defects (e.g., primaquine-induced hemolytic anemia in G6PD deficiency); or
• Idiosyncratic reactions (e.g., chloramphenicol-induced aplastic anemia).
History is of prime importance. Consider the following:
• Nonprescription drugs and topical agents as potential offenders
• Previous reaction to identical drugs
• Temporal association between drug administration and development of clinical manifestations
• Subsidence of manifestations when the agent is discontinued or reduced in dose
• Recurrence of manifestations with cautious readministration (for less hazardous reactions)
• Rare: (1) biochemical abnormalities, e.g., red cell G6PD deficiency as cause of drug-induced hemolytic anemia; (2) abnormal serum antibody in pts with agranulocytosis, thrombocytopenia, or hemolytic anemia.
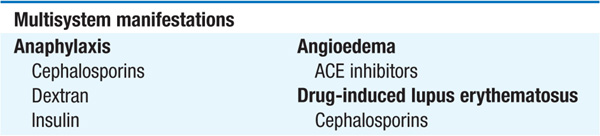
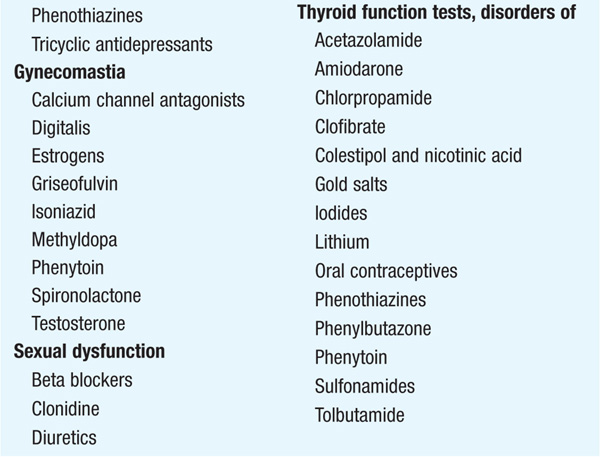
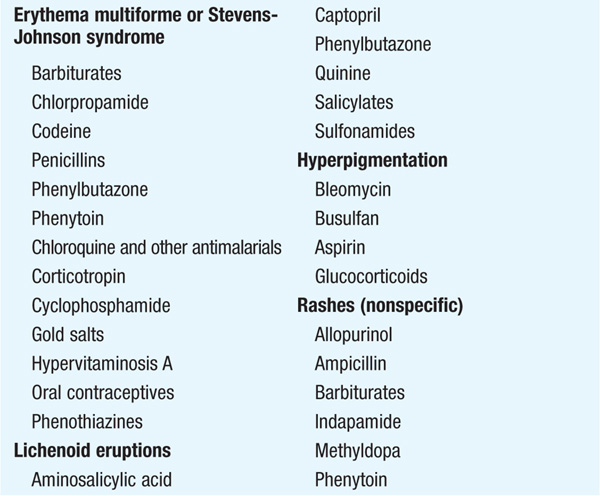
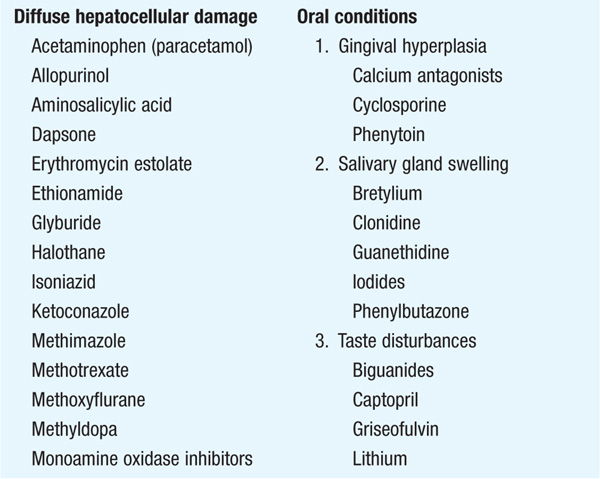
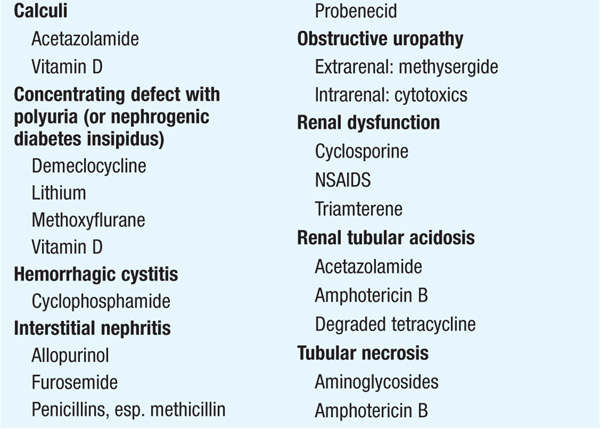
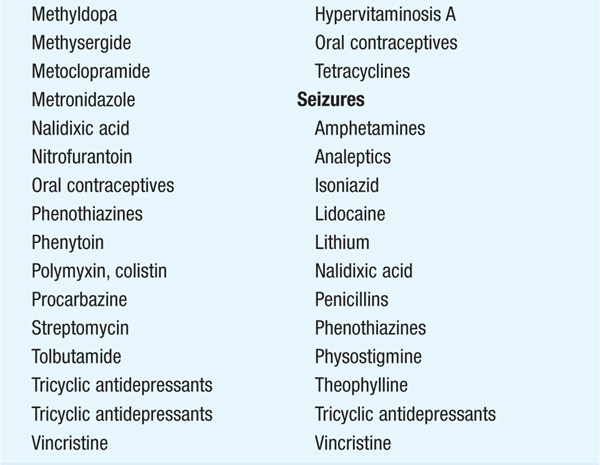
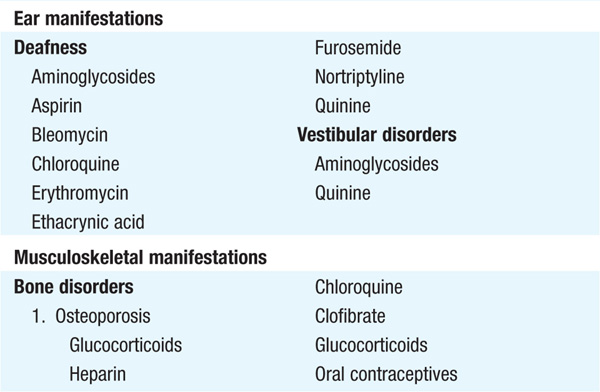
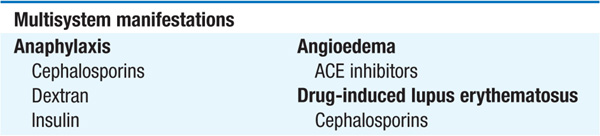
Table 219-1 lists a number of clinical manifestations of adverse effects of drugs. It is not designed to be complete or exhaustive.
TABLE 219-1 CLINICAL MANIFESTATIONS OF ADVERSE REACTIONS TO DRUGS