WHY OUTCOME-BASED EDUCATION (OBE) IS AN IMPORTANT DEVELOPMENT IN MEDICAL EDUCATION
A key development in medical education in the past decade has been the move to outcome-based or competency-based education.
The importance of outcome-based education
It has been argued, and for good reasons, that outcome-based education (OBE) represents the most important development in education in the past two decades. A clear specification of the end product of training and the associated learning outcomes is essential for effective curriculum planning. We would not commission an architect to build a new house until we had approved the plans. The seeds we plant in our garden and how we cultivate them, including the growing conditions we create and the fertilisers we use, will depend on the plants we expect to grow. In the same way, in OBE recognition is given to the importance of the end product of the training programme and the competencies expected of the doctor trained. Who could disagree with that? In this OBE backward or reverse-planning model, the course content and the teaching, learning and assessment methods are derived from the expected learning outcomes.
Curriculum development in medical education traditionally is associated with a forward-planning approach, with course content and teaching methods determined first. This approach, however, has failed to meet the needs of the population and systems of healthcare (Frenk et al. 2010) and there is compelling evidence and an overall global consensus that it is no longer appropriate for the training of a 21st-century doctor.
As described in Chapter 9, OBE is an important element in the move away from the perception of the curriculum as a syllabus comprising a body of knowledge and skills to be transmitted to the student. Set out in OBE are the expected learning outcomes and the competences or abilities required in healthcare professionals if they are to move on to the next stage of their training programme or be accredited to practice independently as healthcare professionals. The rapid development of an outcome-based approach to education was recognised in the March 2002 issue of Medical Teacher, which had OBE as a theme with international developments in the field highlighted. A subsequent issue of the journal in 2010 featured a series of papers on competency-based education (CBE) authored by the International Competency-Based Medical Educators (ICBME) collaborative. In this chapter we will not distinguish between the concepts of OBE and CBE and for practical purposes will treat them as the same.
Despite critics, OBE has become part of mainstream education through initiatives such as the Tuning Project and has been recognised by regulating bodies in medicine such as the General Medical Council in the UK, the Accrediting Committee on Graduate Medical Education (ACGME) in the USA, the Royal College of Physicians and Surgeons of Canada (RCPSC: the CanMEDS initiative) and other bodies internationally. The Geneva case study illustrates how a curriculum was constructed around the CanMEDS competency framework.
Case study 3.1 An integrated and community-oriented curriculum at the University of Geneva Faculty of Medicine, Switzerland
The 6-year Geneva curriculum was constructed to prepare students for medical roles, as defined in the CanMEDS competency framework:
• Medical expert – To develop clinical competence, students acquire basic knowledge in the first year, then integrate basic, clinical and psychosocial knowledge to explain the mechanisms underlying clinical cases (problem-based learning (PBL)), together with an early practice of clinical skills among students and with simulated patients in the second and third years, and finally progressively shift to clinical reasoning by solving clinical cases during the fourth year, and practising in an integrated clinical environment until the end of the sixth year.
• Communicator – To develop their doctor–patient communication skills, students are trained in communication skills while practising history taking and clinical examination with simulated patients in the second and third years, then with real patients in the fourth, fifth and sixth years.
• Collaborator – To develop students’ ability to work with other healthcare professionals, we are currently developing interprofessional training in the fourth and fifth years. Some students collaborate with nutritionists and physiotherapists during practicum in the community (third year). In addition, small-group working, inherent to the PBL practice, trains students to work with peers during the second and third years. This is also true on the wards, where they regularly collaborate with nurses, midwives and other allied health professions during the fourth, fifth and sixth years.
• Health advocate – The central choice of our medical school is to train students for primary care. They are introduced to the links existing between patients, society and illness during the first year, then to public health issues such as the Swiss healthcare system, and preventive and social medicine during the second and third years. They practise with patients in private primary care settings and public institutions during the second and third years.
• Scholar – To develop an autonomous and lifelong learning, students get self-readings complementary to the lectures during the first year and regularly practise self-directed learning with PBL from the second to the fourth years. Moreover, they are initiated to scientific research through a master’s thesis during the fourth and fifth years and an optional research programme for medical students during the second and third years.
• Professional – The importance of developing professional values is present throughout the curriculum and students are assessed in a summative way by validated criteria. The Medical Humanities programme includes biomedical ethics and medicolegal teaching during the first 3 years.
• Manager – Although this dimension is little developed in our pregraduate curriculum, students are introduced to organisation and challenges of healthcare systems during the first 3 years.
Our present curriculum, implemented in 1995 and refined over the years, responds to many dimensions of the 21st-century physician. It has been accredited twice (2006, 2012) and is supported by alumni.
Our future challenges consist of continuing our efforts to promote primary care medicine, reinforcing interprofessional training and valuing test-enhanced learning, based on the best available evidence. This approach must remain an important preventive remedy against the danger of ‘curriculum sclerosis’.
OBE and new approaches to medical education
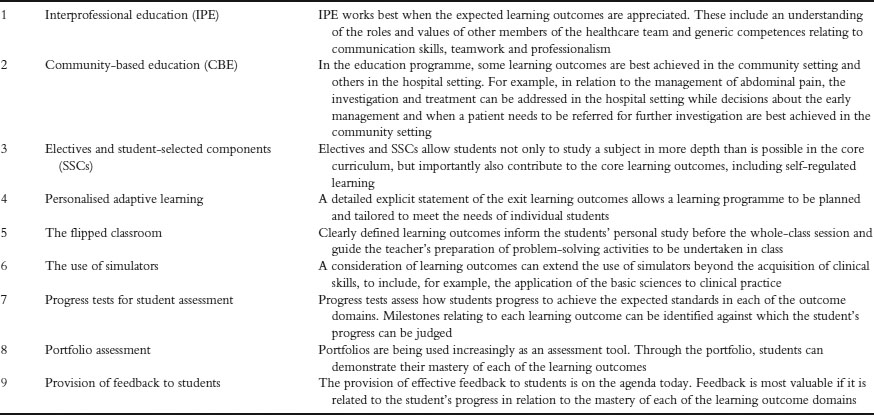
This has been a time of change in medical education, with the introduction of curriculum strategies such as PBL, vertical and horizontal integration and interprofessional learning; new teaching methods, including e-learning and simulation; and new approaches to assessment, including a greater emphasis on performance and work-based assessment. Many of these approaches are described in this book. Embedded in these developments is the need for the recognition of clearly defined learning outcomes and competences to be achieved by the end of the training programme. Table 3.1 lists examples of changes in education in the health professions and highlights the relevance of OBE to each trend.
Learning outcomes describe what is expected of the student and provide a vocabulary to support the use of the different curriculum approaches. OBE empowers students to take more responsibility for their own learning and supports the move to greater student engagement with the curriculum and to student-centred approaches. The teacher works with the student in planning a course of study to meet his or her personal needs – a move in the direction of an adaptive curriculum which is likely to be a feature of education in the future.
Benefits of OBE
OBE offers important benefits to all of the stakeholders – teachers, curriculum developers, students, healthcare professionals and the public. Some of the benefits are described below.
Quality control of the curriculum
The learning outcomes define the end product of training and are a statement as to the relevance of the curriculum and how the doctor entering practice meets the needs of the community which he or she is to serve. The learning outcomes are at the heart of quality assurance and accreditation of a school or an education programme. They can be used to support curriculum renewal and to support the revision of professional accreditation standards.
Table 3.1 Examples of trends in medical education and the relevance of learning outcomes
Case study 3.2 Implementing an outcome- or competency-based approach in practice in Indonesia
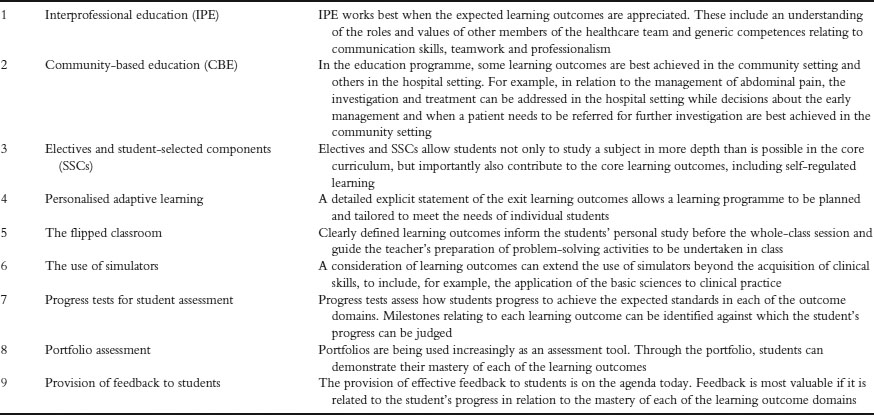
In 2006, based upon a study of society and health needs in Indonesia, a task force on primary healthcare set out the minimum competencies to be achieved by graduates. Seven areas of competence were identified: professionalism; self-awareness and self-development; effective communication; information management; scientific foundation of medicine; clinical skills; and health problem management (Figure 3.1). This was the starting point for Indonesia to implement a National Standard for Medical Education and National Standard Competency in medicine. With a subsequent revision, the standards were approved in 2012 by the Indonesian Medical Council. The curriculum model was competency-based and implemented through a SPICES approach to curriculum planning. The SPICES model is based on six educational strategies that can be implemented within a curriculum along a spectrum from innovative to traditional (further discussion can be found in Chapter 9 of this Handbook).
All medical schools in Indonesia are required to base their education programme and curriculum on these standards. Twenty per cent of the curriculum is allocated to take into account local needs and areas of excellence. Faculty of Medicine, University of Airlangga (FMUA) decided to include in the curriculum tropical medicine, mass disaster training and research that related to these topics. Tropical diseases are still a problem for Indonesia and mass disaster training was chosen as Java is in the ring-of-fire pathway of natural disaster.
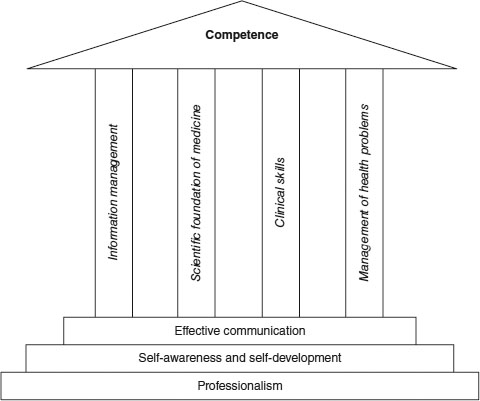
Figure 3.1 Standard competence of Indonesian doctor, 2012.
Changing from content-based to competency-based was not a smooth process as, although it was believed the outcome would be better as the competences identified related to health needs in the country, at that time the concept of competence-based curriculum was not clearly understood by most teachers. Many teachers were concerned that the word ‘standard’ would mean a limitation of the competence to be achieved and that the revised curriculum with fewer lectures would be associated with a decrease in the graduate quality compared to the graduates of the previous content-based curriculum. Over time the problems associated with the approach diminished, the educational climate became more supportive and more teachers became willing to become involved.
An example of the difficulties faced can be seen in the implementation of an integrated module. In delivering an integrated lecture, teachers were confused about the goal of the lecture, lacked training in working as an interprofessional team and found it difficult to align the lecture with learning outcomes and identify appropriate achievement to test the specified outcomes.
National Board examinations for medical students began in 2006 and since 2012 all the graduates of medical school in Indonesia have to pass the national exit examination based on the national standard of competence. The test consists of a computer-based test for knowledge and an Objective Structured Clinical Examination (OSCE) for skills.
In 2012, FMUA conducted a study of customer’s opinions regarding the achievement by graduates of the specified competences. This provided valuable feedback and indicated where further efforts are needed to improve the students’ learning and the curriculum. There is no doubt regarding the advantages of the competence-based curriculum, but the transition needs time. For a traditional medical institution like FMUA, it is necessary to change the mindset of the stakeholders.
As shown in the case study from Indonesia, the determination of a set of learning outcomes can be the starting point for the specification of national standards for medical education. Clearly defined learning outcomes, as shown in the Australian case study, can lead to harmonisation of professional accreditation and quality assurance processes across a range of healthcare professions.
The case study from Canada relates learning outcomes and the curriculum to the school’s mission to train physicians with the necessary competences, including a humanistic view and the ability to respond as necessary to change.
Case study 3.3 Sharing learning outcomes across health disciplines in Australia
Australian higher education operates within a quality and regulatory environment with legislated higher-education standards (Australian Government Tertiary Education Quality and Standards Agency 2012). In preparation for this new era of academic quality assurance, the Australian Learning and Teaching Council in 2010 undertook a national learning and teaching academic standards project. Health was included as a single discipline group and, as project leaders in health, the authors were tasked with developing four to six learning outcome statements. These learning outcome statements (or threshold learning outcomes) would then represent the capabilities and competencies to be expected of every Australian health graduate (O’Keefe et al. 2011).
Twenty-six individual disciplines were included in the work: inter alia medicine, dentistry, nursing, veterinary science, osteopathy and Western Chinese medicine. The professional accreditation standards/competencies for each of these individual health disciplines were then compared using qualitative thematic analysis techniques to identify common content domains. As a result, six threshold learning outcomes were developed and refined.
Discipline engagement was a critical factor in the acceptance of the emerging threshold learning outcomes as a true representation of disciplinary expectations for student learning. Considerable reliance was placed on deans and chairs of individual professional and accreditation councils (of which there were over 70) to disseminate information and provide feedback to the project leaders at various stages of the thematic analysis. Nationally, 37 meetings and workshops were conducted to explain the purpose and value of the project and to refine the emerging threshold learning outcome statements. A project email database of key academic contacts grew to over 1,000 in just months.
At national meetings and workshops, representatives from different institutions and healthcare disciplines came together to focus on commonalities in healthcare education. One of many positive outcomes of the workshops and meetings was the attendant fostering of interdisciplinary dialogue and sharing of good educational practice. At one meeting, for example, seven different institutions and health disciplines were represented at a round-table discussion of common student learning outcomes. Academics from veterinary science, medicine and exercise physiology affirmed the centrality of good communication skills, while colleagues from nursing, osteopathy and dentistry confirmed the importance of delivering safe, collaborative healthcare. For the project leaders this experience, repeated multiple times around the country, was one of the truly rewarding aspects of the project.
The utility of project outcomes has extended beyond the original intent of the project. A framework of common health graduate learning outcomes has contributed to government health workforce planning and harmonisation of professional accreditation and higher-education quality assurance processes. It has also been of use as an organising framework for revisions of professional accreditation standards and curriculum renewal, and has provided a robust platform to support interprofessional education initiatives.
Focus and simplicity in capturing key learning outcomes proved a critical factor in relation to ensuring relevance and resonance across disciplines. Anchoring the threshold learning outcomes to existing accreditation standards/competencies gave weight and credibility to the project outcomes. The project also underlined the complex and interrelated nature of health disciplines.
Case study 3.4 Towards a competency-based curriculum – the focus of undergraduate medical education curriculum renewal at the Université de Sherbrooke, Canada
The Faculty of Medicine and Health Sciences, Université de Sherbrooke greeted its first students in 1966 with an organ system-based curriculum. The 4-year undergraduate medical programme underwent an initial PBL reform in 1987, followed by a ‘reform of the reform’ in 1997, with tutors becoming more active and students receiving problem objectives. A clerkship reform was implemented in 2007 featuring an integrated competency-based framework. Ninety-eight key clinical situations and related tasks focusing on four types of competencies – diagnosis, investigation, treatment and education – were identified. Students were required to maintain a log book of the tasks with which they engaged across the different clerkships in a transdisciplinary fashion. Formative and summative assessments removed from specific disciplinary contexts, including OSCEs, were developed to evaluate clerks. They were designed to reflect various professional roles – clinical reasoning, communicator, collaborator, manager, health advocate and lifelong learner.
Due to organisational limitations the clerkship reform was carried out in relative isolation from the pre-clinical curriculum, where disciplinary teaching remained predominant and evaluation methods unchanged. The impetus for the present pre-clerkship renewal process in 2010 stemmed not only from current literature regarding medical education reform and evolving national standards, but also from a local situational portrait based on multiple consultations with different stakeholders. Through this process it became clear that there was a widening gap between the curriculum as planned by designers, the enacted curriculum by teachers and the curriculum experienced by students (Bédard and Béchard 2009).
Inspired by Stufflebeam’s context, input, process and product (CIPP) evaluation model (2003), needs, opportunities and threats were defined, general orientations and actions selected and implementation scenarios drafted. Six broad orientations to shape the curriculum and student assessment were identified: (1) acting with competency; (2) generalism/global approach to health; (3) transdisciplinary perspective; (4) interprofessional collaboration; (5) flexibility; and (6) comprehensive and coherent management. Significant modifications were proposed, including the integration of competency assessment into authentic clinical practice throughout the curriculum; provision of a roadmap for physician cognitive and professional development; and the establishment of milestones to situate better the gradual acquisition of professional competencies. Clerkship competencies will be used as the basis for this development. Regular communications with key stakeholders maximise buy-in as the process unfolds.
Pre-clinical curricular changes since 1987 have had a primarily methodological focus on the enacted curriculum. The current changes are focusing rather on the planned curriculum. The curriculum experienced by students will serve to inform the latter (rather than the former) such that fundamental principles of competency will not be lost and remain congruent with our mission (to train competent physicians with a humanistic view, dedicated to lifelong learning and committed to responding to evolving community needs) and values (professionalism, quality, dynamism, humanism, autonomy, collaboration).
Although previous curricular changes shared similar positive intentions, a drift occurred over time. In implementing any sort of change, we need to be mindful of the gap that can develop between what was initially planned and what is experienced by students in the end. Regular ‘product’ evaluations by those in charge of curricular planning are essential to ensure that things remain on track by monitoring outcomes (both intentional and unintentional).
Assessment of the competencies of students, trainees and doctors
The learning outcomes provide a framework for the assessment of the competence and abilities of the learner during and at the end of the medical school programme, of the trainee at the end of specialist training and of the doctor in practice. In a spiral curriculum (Harden and Stamper 1999: 141), students demonstrate that they have achieved the specified milestone and appropriate level of mastery at each phase of the curriculum. Related to this is the concept of the ‘entrustable professional activity (EPA)’, a task that an individual can be trusted to perform unsupervised in a given healthcare context, once sufficient competence has been acquired (ten Cate 2005).
The case study from Indonesia describes the development of a national examination for medical students based on agreed competencies. The USA case study describes how the assessment of paediatric residents at the University of Colorado School of Medicine was based on the ACGME competencies.
Case study 3.5 Assessment of paediatric residents based on ACGME competencies in the USA
A system of assessing residents in the Department of Pediatrics, University of Colorado School of Medicine Pediatric Residency programme has been introduced based on the ACGME Pediatric Milestones. The Milestones provide detailed descriptions of components of clinical work sequenced in a quasi-developmental progression from novice to master. They are nested under each of the six ACGME competencies – patient care; medical knowledge; interpersonal and communication skills; professionalism; systems-based practice; and practice-based learning and improvement.
Difficulties had been experienced in implementing a numerical rating scale based on the six ACGME competencies, with descriptive anchors of each element of the competencies aligned with a number rating scale. Faculty found it difficult to relate ratings to the capabilities of residents in the workplace, and found it challenging to analyse and deconstruct what they observed in order to match observations to one of the six ACGME competencies. In addition, it was impossible to develop a shared understanding of the context of work and expectations for performance among over 600 faculty evaluating almost 90 residents. Number ratings conveyed nothing meaningful about performance other than to identify who was at the top and who was at the bottom and provided little information that residents could use to set goals for learning.
A revised assessment system was introduced which focused on performance. We developed a framework for assessment based on the reporter, interpreter, manager, educator (RIME) model while continuing to incorporate language reflecting the six ACGME competencies and the new Pediatric Milestones introduced by ACGME.
Our new framework relies on tasks that faculty routinely observe and make sense in the clinical practice workplace. The new assessment form has no numbers and asks for descriptions of observed work and up to three feedback points. We use qualitative data analysis software to code and link each comment/description to the appropriate milestone or milestones. Teachers are able to go online and complete a descriptive comments form from any computer in our institution, and residents are able to send forms electronically to their teachers requesting descriptive comments. When a descriptive comments form has been completed, the resident is notified and can review the information immediately instead of waiting for a meeting in the indefinite future.
We undertook intensive faculty development about the new approach to assessment prior to launch. Faculty development is ongoing. Since implementation, the number of useful descriptions of resident performance has increased fourfold. Comments are electronically assembled for review by residency programme leadership and individual residents. Residents, in consultation with faculty, set individual learning goals based on the descriptive data.
The assessment system introduced provides richer evidence of capability to facilitate judgements about progression to competence and independent practice. Residents appreciate receiving timely information about their performance that they can use to create learning goals and improve their practice.
There is a move to change from the current time-based system of training, where what is fixed is the time or duration of training with standards that are variable, to a standard-based approach where what is fixed is the standards or outcomes achieved and what varies is the time for training. This may apply to an element within a training programme such as the acquisition of skills using a simulator or to a shortening (or lengthening, where necessary) of the time required for mastery of the overall training programme.
Empowering the student and the teacher
A statement of the expected learning outcomes empowers both students and teacher –students to take more responsibility for their own learning and the teacher or trainer to innovate and select the most appropriate content and teaching methods from the rich menu of choices now available.
A curriculum blueprint helps to ensure that both the learning experiences provided and the student assessment instruments are matched to the learning outcomes. The curriculum map and the learning outcomes provide the learner with information about his or her progress and what further or remedial study is required. The case study from the University of Colorado School of Medicine illustrates how, based on a competency framework, paediatric residents were assessed and given feedback as to their performances. The residents working with faculty were able to set their individual learning goals.
Priorities and information overload
A major challenge facing educators is how to respond to curriculum demands associated with the ‘information explosion’ and the doubling of knowledge in the biomedical sciences every 2 years, along with the recognition of new topics such as patient safety and personalised medicine. A consideration of the expected learning outcomes assists the teacher and curriculum designer in assigning priorities as to what is to be included in the curriculum and to ensure that no important aspects are ignored or left out.
Support for collaboration
The value of collaboration in the development and delivery of education programmes in the healthcare professions has become increasingly appreciated and will feature increasingly in health professions education. Collaboration may be between the different disciplines within a medical school, between the different phases of education – undergraduate, postgraduate and continuing education – and between the different healthcare professions. Learning outcomes provide a vocabulary which facilitates discussion among the stakeholders.
Examination of the expected learning outcomes across the different healthcare professions may demonstrate, as illustrated in the case study from Australia, the commonalities in healthcare education and encourage interprofessional dialogue and the sharing of good educational practice. An agreement about common core outcomes also facilitates mobility of doctors and students, an increasingly important aspect due to the globalisation of the medical profession.
The challenges of OBE
OBE has featured prominently on the education agenda over the past two decades. Alongside a sometimes extravagant enthusiasm for the subject, one finds rants and raves against an OBE approach. Both extreme positions risk distorting the picture, as in a hall of mirrors in some circus show, confusing or hiding the real power of OBE. This conflict was highlighted by Harris et al. (1995) and by Bowden (1995).
Those occupying both sides of the argument – the strong protagonists or champions for the cause and the highly vocal critics or opponents – in general agree that there needs to be some sort of direction in an education programme with clarity about the nature of the end product. No one wants to return to the situation when what was covered in the education programme depended entirely on the whims of a teacher or trainer. So if there is a measure of agreement about OBE, where then does the problem or confusion lie? Why is it that what seems to be an attractive idea is not universally accepted? The answer lies in a misunderstanding or misinterpretation of the concept.
The big picture and fragmentation of learning
Problems have arisen where the specification of learning outcomes has been confused with behavioural instructional objectives (Harden 2002). Grant (1999) has argued that:
behavioural objectives, or competencies, can never describe complex human behaviour. The sum of what professionals do is far greater than any of the parts that can be described in competence terms. They are making judgements, managing cases in the absence of definitive information.
(Grant 1999: 273)
OBE, however, if correctly implemented, is about the larger picture. Indeed, one of the strong arguments for an OBE approach is that the broad frameworks of competencies specified identify and represent what is expected today of the doctor, including metacompetencies such as decision making, attitudes and professionalism (Harden et al. 1999).
The expected learning outcomes provide a holistic perspective on the curriculum. Each discipline is challenged to consider not only what is expected of the student in relation to the discipline, whether it is a clinical subject such as obstetrics or a basic medical science subject such as physiology, but also how the discipline contributes to the generic competencies as set out in the school’s exit learning outcomes.
Concern has been expressed that OBE leads to teachers being told what they must teach with no freedom for them to use their personal experience and intuition. At an extreme of this view, the teacher is turned into some sort of automaton, programmed to follow automatically and mechanically a predetermined course. One reason that the move to OBE more generally attracted fierce opposition was that it was believed that education should be open ended, not constrained by outcomes. While this liberal notion of education may be appropriate in the arts and humanities, the difficulty in the healthcare professions is that we do not have the luxury of being vague about the product of the training.
An agreement as to the expected learning outcomes, rather than disempowering the teacher, gives the teacher the freedom to determine and implement a programme that will result in students achieving the required level of mastery. Teachers have the freedom to devise and create appropriate learning opportunities and experiences and to introduce their own individuality and perspective to this. The case study from Indonesia shows how local needs can be accommodated within a national statement of learning outcomes with 20 per cent of the curriculum specified locally.
A challenge, however, is to provide the necessary staff development, as for many teachers OBE will be a new concept and assistance will be required as to how learning outcomes can best be embedded in the curriculum. The case study from Indonesia shows how over time a competency-based approach is accepted by teachers.
Level of competence
A criticism of OBE is that minimum levels of competence are promoted. This need not be so. Learning outcomes can be specified at different levels, as demonstrated at Brown University (Smith and Dollase 1999). Competence was defined in nine domains at three levels – beginner level, intermediate level and advanced level. Students were required to attain a beginner- and intermediate-level competence in all nine abilities. An advanced level of competence in problem solving and three other abilities of the student’s choice were also required. The model of progression described by Harden (2007) is easily translated into the specification of learning outcomes at different levels of competence. The idea of progression in terms of learning outcomes can be seen in the Australian case study, where the ‘threshold learning outcomes’ indicate a baseline of competence.
Implementation of OBE
How OBE is best implemented will depend on the local context. Almost certainly, however, steps in the process will include those described below, although the order or attention to detail will vary in different situations. All of the stakeholders should be involved in the process, as described in the Australian case study. The introduction of an outcome-based approach is most easily achieved as part of a curriculum review, as illustrated in the Canadian case study. There are major benefits, as demonstrated in the Indonesian and other case studies, relating the learning outcomes to national accreditation standards and in so doing give credibility to the outcomes specified.
Decide on an overall framework
Key to the success of OBE is a user-friendly, intuitive framework which covers the key domains to be addressed. One option is to choose an existing framework such as the Scottish Doctor, CanMEDS or ACGME frameworks. This approach has been adopted successfully in many institutions. Amendments can be made and each domain expanded to meet local needs. An alternative is to start ab ignitio and develop a framework designed to meet local needs. The Saudi Arabia case study describes how the national framework of Saudi Arabia was used along with recommendations from the UK General Medical Council as a basis for the identified learning outcomes.
Case study 3.6 Basic science integration into the whole curriculum at the Faculty of Medicine, King Abdulaziz University, Saudi Arabia
The new curriculum in the Faculty of Medicine, King Abdulaziz University started in the academic year 2006–2007. The curriculum follows an outcome-based approach to curriculum design and development, where significant outcomes or attributes of students at graduation were well defined at the start. The programme attributes take into account Saudi MED and the General Medical Council’s Tomorrow’s Doctors (2009). The programme clearly defines the graduate attributes, which include: practice and maintenance of good standards of clinical care and professional communication; establishment of good relationships with patients, colleagues and senior and junior staff; acquisition of teaching and training skills; lifelong learning attitude; and humbleness, punctuality and honesty. Graduates’ attributes are compatible with community needs and employability skills required for the medical field practice as well as the National Qualifications Framework set by the National Commission for Academic Accreditation and Assessment.
The specific learning outcomes informed the phase 1 curriculum, which appeared over 2 years – a system-based course including the basic medical sciences and the clinical clerkships and electives in phase 2. A feature of the curriculum has been the introduction of problem-based learning (PBL) through constructed cases, which become the focus for 2 weeks of study. The cases were designed in such a way that students must draw on knowledge, ideas and concepts from across the discipline, integrating basic and clinical sciences in order to generate and pursue learning goals. PBL, in particular, emphasises elaboration of learning goals and their discussion in small groups, calling on all relevant knowledge across the disciplines.
Populate the framework with the agreed learning outcomes
The desired outcomes should be established for each of the framework domains. For example, in relation to practical procedures, a decision has to be taken as to which procedures should be included and, in relation to communication skills, which aspects of communication and the level of mastery required at the completion of the education programme.
Prepare a grid or preferably a curriculum map relating the learning outcomes to the phases and courses in the curriculum
It is important to recognise that OBE does not stop with the specification of the learning outcomes. The content of the curriculum and the aspects addressed in each stage of the curriculum must be determined by the expected learning outcomes (Figure 3.2). How each course contributes to the exit learning outcomes should be specified and the milestones or what is expected of a student at each phase of the curriculum should be determined.
Prepare a grid or curriculum map identifying for each learning experience the expected learning outcomes
Learning outcomes should be specified for all learning experiences, including lectures, tutorials, PBL sessions, practical classes, clinical experiences and work in a simulation laboratory. The work may be completed over a period of time, with responsibility given to the individual in charge of the session.
Relate the assessment to the learning outcomes
Prepare a grid or curriculum map identifying how each learning outcome is assessed at the different stages in the curriculum, e.g. through a written assessment, an OSCE or as part of a portfolio assessment. As discussed in Chapters 17–19, important advances have been made in the assessment of outcomes such as professionalism, attitudes and team working. The case study from the University of Colorado illustrates how the assessment of trainees was built round the ACGME competencies for paediatrics residents and the milestones in the move from novice to master.
Arrange a faculty development programme
It is essential to engage the faculty in the specification of learning outcomes and in the implementation of an OBE approach. The concept of OBE will be new to many faculty and faculty must be involved and made familiar with the approach, with the learning outcome framework and how the course for which they are responsible contributes to this.
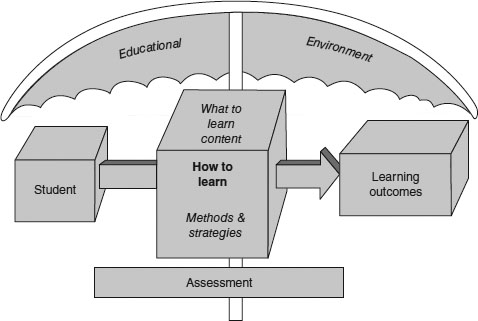
Figure 3.2 Learning outcomes as a focus for curriculum development.
• The principal focus for medical education should be on the product and the desired learning outcomes rather than on the programme structure and education process. Quite simply, outcome-based and competency-based education mean clearly focusing and organising the educational programme around what are deemed to be the essential competencies and abilities for the learner at the end of the educational programme.
• OBE is a powerful education strategy that should be used as a focus for curriculum planning, as a means of making informed discussions about the approaches to teaching and learning be adopted, and as a basis for the assessment of students/trainees and of the education programme itself. This means starting with a clear picture of what it is important for the healthcare professional to be able to do and then organising the curriculum, learning opportunities and assessment to make sure that this learning happens.
• OBE is at the cutting edge of curriculum development and an understanding of the expected learning outcomes can contribute to our appreciation and success of newer approaches to medical education, such as team-based learning and interprofessional education.
• OBE is not a magic bullet that on its own can address the problems facing medical education. As with all developments or tools and as illustrated in the case studies, how it is implemented and how staff are engaged with the process matter.
• OBE requires a regular revision of the curriculum to ensure that competencies outlined continue to meet the needs of the student, profession and wider community.
Bibliography
ACGME Paediatric Milestones. Online. Available HTTP: http://www.acgme.org/acgmeweb/Portals/0/PDFs/Milestones/320_PedsMilestonesProject.pdf (accessed 10 April 2014).
Australian Government Tertiary Education Quality and Standards Agency (2012) Online. Available HTTP: http://www.teqsa.gov.au/ (accessed 28 March 2013).
Bédard, D. and Béchard, J.P. (2009) ‘Quelques conditions pour un curriculum en développement au supérieur’. In D. Bédard and J.P. Béchard (eds) Innover dans l’enseignement supérieur, Paris: Presses Universitaires de France.
Bowden, J.A. (1995) Competency-based education: Neither a panacea nor a pariah. Paper presented to TEND 97, Abu Dhabi, 6–8 April. Online. Available HTTP: http://crm.hct.ac.ae/events/archive/tend/018bowden.html (accessed 10 April 2014).
Faculty of Medicine, University of Airlangga (2012) Summary of tracer study. Unpublished.
Frenk, J., Chen, L., Bhutta, Z.A., Cohen, J., Crisp, N., Evans, T., Fineberg, H., Garcia, P., Ke, Y., Kelley, P., Kistnasamy, B., Meleis, A., Naylor, D., Pablos-Mendez, A., Reddy, S., Scrimshaw, S., Sepulveda, J., Serwadda, D. and Zurayk, H. (2010) ‘Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world’, Lancet, 376(9756): 1923–58.
General Medical Council (2009) Tomorrow’s doctors: Outcomes and standards for undergraduate medical education, London: GMC. Online. Available HTTP: http://www.gmc-uk.org/education/undergraduate/tomorrows_doctors_2009_foreword.asp (accessed 29 April 2014).
Grant, J. (1999) ‘The incapacitating effects of competence: a critique’, Advances in Health Sciences Education: Theory and Practice, 4(3): 271–7.
Harden, R.M. (2002) ‘Learning outcomes and instructional objectives: Is there a difference?’, Medical Teacher, 24(2): 151–5.
Harden, R.M. (2007) ‘Learning outcomes as a tool to assess progression’, Medical Teacher, 29(7): 678–82.
Harden, R.M. and Stamper, N. (1999) ‘What is a spiral curriculum?’, Medical Teacher, 21(2), 141–3.
Harden, R.M., Crosby, J.R. and Davis, M.H. (1999) ‘From competency to meta-competency: A model for the specification of learning outcomes’, Medical Teacher, 21(6): 546–52.
Harris, R., Guthrie, H., Hobart, B. and Lundberg, D. (1995) Competency-based education and training: Between a rock and a whirlpool, Melbourne, Australia: Macmillan Education.
Indonesian Medical Council (2006) The National Standards competencies of Indonesian medical doctors, Jakarta: Indonesian Medical Council.
Indonesian Medical Council (2012) Standard for Indonesian medical education, Jakarta: Indonesian Medical Council.
O’Keefe, M., Henderson, A. and Pitt, R. (2011) Learning and teaching academic standards: Statement for health medicine and veterinary science, Australian Learning and Teaching Council. Online. Available HTTP: http://www.olt.gov.au/resources (accessed 28 March 2013).
Smith, S.R. and Dollase, R. (1999) ‘Planning, implementing and evaluating a competency-based curriculum. AMEE education guide no. 14 part 2’, Medical Teacher, 21(1): 15–22.
Stufflebeam, D.L. (2003) ‘The CIPP model for evaluation’. In T. Kellaghan and D.L. Stufflebeam (eds) International handbook of educational evaluation, Boston, MA: Kluwer.
ten Cate, O. (2005) ‘Entrustability of professional activities and competency-based training’, Medical Education, 39(12): 1176–7.
Zaini, R.G., Bin Abdulrahman, K.A., Al-Khotani, A.A., Al-Hayani, A.M.A., Al-Alwan, I.A. and Jastaniah, S.D. (2011) ‘Saudi meds: A competence specification for Saudi medical graduates’, Medical Teacher, 33(7): 582–4.