Your body has an extraordinary capacity to adapt. With endurance training, your heart’s chambers enlarge and your blood volume increases, allowing more nutrients and oxygen to be circulated during maximal aerobic exercise. Inside your muscles, the enzymes that speed up certain metabolic pathways increase in quantity, allowing you to produce ATP more rapidly or efficiently. With resistance training, your skeletal muscle fibers enlarge and are able to generate extra force. And as recent research in older adults has demonstrated, even certain regions of the brain adapt to exercise training by enlarging.1, 2
To achieve these adaptations, most athletes spend the bulk of their training time slogging away on the pavement, hitting the practice field, or pumping iron in the weight room. All this training stimulates muscle growth, builds muscular strength and endurance, and is the basis for long-term athletic development. There’s one type of athlete, however, who focuses less on developing their muscles and heart and more on training their gut. These are the competitive eaters of the world, and as I mentioned in Chapter 1, the world record in hot dog eating is 74 frankfurters and buns in 10 minutes, held by none other than Joey Chestnut. Although genetics likely play a role in determining one’s potential to become a high-caliber speed eater, Chestnut and his fellow competitors certainly weren’t born entirely capable of choking down dozens of hot dogs in just 10 minutes. No, these athletes train just like any other athlete, except their idea of “keeping fit” involves repeatedly stretching their stomachs by eating masses of food and fluid.
The other giant of the competitive eating world is Takeru Kobayashi, who holds numerous records and dominated Nathan’s Fourth of July contest before Chestnut’s first victory there in 2007. In a 2015 interview with the online magazine Vice, Kobayashi detailed some of the training methods that make him such a prolific devourer of foodstuffs, one example being that he prepares months in advance by drinking slightly more water every day.3 On the afternoon he was interviewed, Kobayashi planned to drink 3 gallons of water in 90 seconds. (Warning: Chugging water like this can be dangerous because it can lead to hyponatremia.) Other competitive eaters conduct two or three practice eating sessions each week, where they gorge on huge quantities of food.
In contrast to competitive eaters, the performance of cyclists, runners, triathletes, footballers, basketballers, and various other athletes isn’t dependent on eating piles of food during competition. Even so, being able to tolerate modestly larger intakes during exercise could be advantageous for athletes looking to push the boundaries of their incompetition nutrition plans. Thus, it’s worth pondering how you might be able to train your gut to optimize the digestion, absorption, and delivery of nutrients during exercise.
Amazingly, science tells us that your gut has the capacity to adapt to not only physical training but also to the diet you eat over days and weeks. What’s also remarkable is that many of these adaptations are nutrient specific. Just as adaptations to exercise training follow the principle of specificity, so do many of the adaptations of gut training. If your objective is to get stronger, it works best to lift heavy weights. In a similar way, if your objective is to absorb and burn more carbohydrate during exercise, it works best to eat a high-carbohydrate diet. In this chapter, we cover these nutrient-specific adaptations in the gut as well as how they might impact exercise performance and the development of digestive symptoms.
THE GUT’S ADAPTATION TO EXERCISE TRAINING
By now, you should be aware that the redistribution of blood flow during exercise is a way for your body to prioritize the delivery of oxygen and nutrients to your muscles. This additional blood also serves to remove by-products of metabolism that, if left to accumulate, induce fatigue. Blood flow to your skin increases too, particularly in hot/humid environments, which facilitates heat loss and prevents a rapid rise in body temperature. In nonathletes, cardiac output is equivalent to about 5 liters of blood per minute at rest, of which the gut and liver receive about 20 percent.4 During maximal aerobic exercise, cardiac output swells roughly fivefold to 25 liters per minute in an average man, with the skeletal muscle receiving the lion’s share (roughly 80 percent). While the absolute amount of blood flowing to your gut may not decline much during heavy exercise, the relative percentage of your cardiac output reaching your gut drops to just a few percent. With fluid losses from sweating, gut blood flow can become even further compromised.5, 6 Undoubtedly, reductions in gut blood flow help explain the greater occurrence of digestive symptoms reported during endurance events.
What effect, if any, does physical training have on these blood-flow impairments of the gut? Well, both animal and human studies demonstrate that long-term exercise training blunts the reduction in gut blood flow that typically occurs with acute exercise.7 The primary explanation for this adaptation is a reduction in sympathetic nervous system output. As a reminder, the sympathetic nervous system is the fight-or-flight division of your nervous system that readies your body for physical action, and one way that it accomplishes this is by constricting blood vessels in your gut. (Historically, blood flow to the gut wasn’t a priority when one was being chased by a lion, was it?) In essence, as you increase your fitness over time, your autonomic nervous system becomes less “fight-or-flight” and more “rest-and-digest” at a given exercise workload. The long-term effects of exercise training on gut blood flow may help explain why several gut symptoms are less common in experienced athletes;8, 9 these athletes may have trained their guts—through hundreds or thousands of hours of training time—to better maintain blood flow during exercise.
ADAPTATION TO INCREASED CARBOHYDRATE INTAKE
Carbohydrate ingestion—and its subsequent digestion, absorption, and delivery to skeletal muscle—is imperative for maintaining carbohydrate burning during intense exercise that lasts longer than 60–90 minutes. As carbohydrate stores in your body dwindle, rates of energy production and muscular contraction decline because slower-burning fatty acids become an increasingly dominant fuel source. Consequently, ingesting carbohydrate helps maintain higher absolute workloads during intense, prolonged exercise.
There is a natural limit, though, to the amount of carbohydrate you can digest and absorb over any given period. The SGLT1 and GLUT5 transporters located in the intestinal brush border have upper limits as to how quickly they let carbohydrate into your body. If you consume too much carbohydrate, abdominal cramping, diarrhea, and flatulence may develop. To combat this problem of limited absorptive capacity, ingesting a mix of carbohydrate types (fructose and glucose), as opposed to a single source, is recommended—at least when you plan to consume more than 50 grams per hour.
One intriguing question is whether it’s possible to train your gut to increase the capacity of these transporters, which would allow you to increase the amount of carbohydrate you absorb and burn during exercise. As discussed in an eloquently written paper by sports scientist Asker Jeukendrup, an abundance of data from animal studies makes it clear that the activity and/or concentration of these transporters can change based on the carbohydrate content of the diet.10 Simply put, more carbohydrate in the diet equals more of these transporters in the intestinal brush border.
Data directly confirming that this also happens in humans are lacking, in large part because isolating these transporters requires excising a sample of intestine. Even so, there’s some indirect evidence that this adaptation also happens in the intestines of humans. Take a study from the Australian Institute of Sport that tested whether feeding a four-week high-carbohydrate diet would increase athletes’ capacities to burn carbohydrate eaten during exercise.11 Athletes assigned to a high-carbohydrate group consumed glucose drinks before and during training sessions while athletes allocated to a moderate-carbohydrate group consumed fat-rich foods (macadamia nuts or a cream drink) after training sessions. Importantly, both diets provided the same total energy. At the start and near the end of the four-week dietary period, the athletes completed a 100-minute cycling test while consuming a beverage containing a special form of glucose that can be traced in the body. The experiment ultimately revealed that the high-carbohydrate diet increased the oxidation of traced glucose by 16 percent, with no apparent change on the moderate-carbohydrate diet. The researchers concluded that enhanced intestinal absorption of glucose was the most likely explanation for this finding. In terms of practical guidelines, studies—albeit using animals—have found that just a few days on a high-carbohydrate diet can upregulate intestinal transporter expression,10 meaning you probably don’t need to crush carbohydrate for weeks straight to see these changes.

figure 9.1TRAINING THE GUT FOR GREATER CARBOHYDRATE INGESTION

Additional carbohydrate added to the diet over several days to weeks promotes the expression of intestinal carbohydrate transporters, which can enhance carbohydrate absorption, reduce gut distress, and perhaps improve performance when an athlete ingests 50-plus grams per hour of carbohydrate during exercise.
While mounting evidence supports the notion that eating a high-carbohydrate diet boosts the quantity and/or activity of intestinal carbohydrate transporters like SGLT1, these adaptations’ implications on performance are less clear. In fact, that same study from the Australian Institute of Sport also measured performance and failed to find any differences.11 One potential reason for this is that the moderate-carbohydrate diet still contained an ample amount of carbohydrate; if the comparison diet had been low carbohydrate, it’s possible that even larger differences in carbohydrate burning would have been observed, which could have led to meaningful changes in performance. That said, one recent study conducted by researchers at Monash University in Australia did find improvements in running performance after two weeks of a carbohydrate-based gut-training protocol, and these improvements were likely mediated through reductions in digestive symptoms.12 Overall, these studies tell us that training your gut to tolerate more carbohydrate during exercise could translate to improvements in not only carbohydrate burning and digestive symptoms, but also possibly performance (see Figure 9.1). An important caveat to this statement is that it applies to athletes who are planning to push the envelope of carbohydrate ingestion during competition (i.e., more than 50 grams per hour). If you plan to consume 30–45 grams of carbohydrate per hour, there’s little reason to do this sort of aggressive gut-training protocol.
Beyond affecting the intestine’s capacity for absorption, the carbohydrate content of a diet also influences emptying from the stomach. Specifically, studies supplementing the diet with either glucose or fructose for just a few days have shown the emptying of these sugars to be accelerated.13–15 The reasons for this adaptation are still being elucidated but almost certainly involve less feedback inhibition from receptors in your small intestine that detect the presence of carbohydrate. This feedback inhibition—originally discussed in Chapter 1—is a way for your body to regulate the amount of sugar being dumped into your small intestine. Interestingly, fasting for several days also slows the emptying of carbohydrate from the stomach,16 and it’s long been known that the dietary restriction typical of anorexia nervosa induces similar delays and that these effects are quickly reversed if adequate nutrition is provided.17 Slowed stomach emptying might also explain why athletes who heavily restrict energy intake experience more gut problems than their well-fed counterparts.18
Again, the practical implication of this research is that if you plan to consume large amounts of carbohydrate during competition, make sure you don’t heavily restrict energy intake during the days leading up to competition, particularly from carbohydrate-rich foods and beverages. If you do, emptying of carbohydrate from your stomach might be slowed and could increase the likelihood of symptoms like fullness, reflux, and nausea.
ADAPTATION TO INCREASED FAT INTAKE
Unlike ingesting carbohydrate, eating fat during exercise doesn’t improve performance, primarily because most of said fat isn’t burned for energy. The major exception to this rule of thumb is for athletes partaking in relatively low-intensity, ultraendurance-type activities that last many hours to days. There’s enough time for more of the ingested fat to be digested, absorbed, and utilized during these events, and as an added bonus, relying more on dietary fat in these situations requires carrying less food because fat is such an energy-dense nutrient.
Even though eating significant quantities of fat during high-intensity exercise doesn’t make sense from a performance perspective, can the same be said for high-fat diets eaten over the weeks or months leading up to competition? As covered in Chapter 5, long-term high-fat diets may not hinder performance in all sports, especially in ultraendurance competitions that rely heavily on fat oxidation to sustain muscular contraction.19 In addition, an increasing number of athletes are trying high-fat diets. What, then, can these athletes expect to happen to gut function if they adhere to a diet that’s filled with bacon-wrapped avocado fries and almond-butter milkshakes?
Just as eating a high-carbohydrate diet speeds emptying of carbohydrate from your stomach, eating a fat-rich diet seems to do the same for fat emptying. In one study, men ate a high-fat diet (55 percent of total energy) for two weeks, and before and after they were fed a high-carbohydrate meal as well as a high-fat meal in order to assess how the fatty diet affected stomach emptying.20 Compared to before the diet, emptying of a fatty meal was accelerated after the high-fat diet, while no change was observed for emptying of the high-carbohydrate meal. In another study, eating a fat-rich diet for four days didn’t quicken how fast a fatty meal left the stomach, but fat emptying sped up after two weeks.21 Finally, a third study showed accelerated emptying after just three days on a diet supplemented with 90 grams of sunflower oil, which ended up supplying almost 50 percent of total dietary energy as fat.22
One major limitation of these studies needs to be acknowledged before we definitely declare that eating a fat-rich diet accelerates fat emptying from the stomach. While they often included a control diet (usually a low-fat diet), these experiments typically failed to ensure that total energy and food volume were equal between the diets, so it isn’t 100 percent clear if the faster emptying was due to the extra fat, specifically, or just a by-product of the additional food and energy. Still, from the thirty-thousand-foot view, it is true that eating a high-fat diet as a part of a high-energy diet accelerates the emptying of fatty meals from the stomach.
The impact on your gut of eating an energy-rich, high-fat diet goes beyond stomach emptying. These diets may also shorten the amount of time it takes for fatty foods to travel from your mouth to your large intestine. In one of the same studies that evaluated stomach emptying, eating a high-fat diet for three days shortened the mouth-to-cecum transit time of a fatty meal from 280 minutes to 226 minutes.22 (The cecum is a pouch that’s considered the beginning of your large intestine.) These findings were replicated over a four-week period as well, with transit time dropping from 318 minutes before a high-fat diet to 248 minutes post-diet.23
Whether the effects of high-fat diets on stomach emptying and small intestine transit time ultimately impact athletic performance and gut symptoms is unresolved. An obvious downside of consuming a high-fat diet would be a reduction in the absorptive capacity of carbohydrate during exercise. To counter this potential problem, an athlete adhering to a high-fat diet who also plans to consume a substantial amount of carbohydrate during competition may want to temporarily increase carbohydrate intake for at least a couple days before the event.
ADAPTATION TO INCREASED PROTEIN INTAKE
Research examining how the gut adapts to protein-rich diets is scarce, which is probably because extremely high-protein diets aren’t that popular among the public. While several popular diets promote elevating protein intake as a way to preserve muscle mass and blunt hunger, it’s still pretty uncommon for protein to make up any more than 35–40 percent of energy in these diets. Thus, the possible range of intakes as a percentage of dietary energy is narrower for protein (10–40 percent) than it is for carbohydrate and fat. In comparison, the carbohydrate content of diets can vary wildly from less than 10 percent to more than 70 percent, and the same is true for fat. So there just aren’t many situations in which a truly “very high” quantity of protein is consumed.
Logically, this relative lack of variability makes it less likely that changing protein intake (at least within normal dietary patterns) will dramatically impact gut function. Nonetheless, a couple of rodent studies do suggest that eating a high-protein diet quickens stomach emptying of protein.24, 25 Obviously, rats aren’t humans, so we shouldn’t assume these results translate across species. As far as I’m aware, no studies in humans have assessed whether long-term high-protein diets influence how quickly protein empties from the stomach. Moreover, even if high-protein diets do accelerate gastric emptying of protein, that doesn’t mean you would reap performance gains from it. As with high-fat diets, it’s hard to think of a performance benefit that would arise from protein leaving from your stomach with haste. Remember, you typically burn small amounts of protein during exercise, so it isn’t a fuel that limits energy production. Finally, if you eat a relatively large percentage of your diet as protein (say, 30 percent), one or both of the other macronutrients (fat and carbohydrate) will probably end up being restricted. On most high-protein diets, carbohydrates are restricted more heavily than fat, and in the end, the carbohydrate restriction that often accompanies high-protein diets could reduce your intestine’s capacity to absorb carbohydrate.
ADAPTATION TO INCREASED FLUID INTAKE
Maintaining blood volume during prolonged exercise—especially in the heat—is critical to fighting off fatigue. The American College of Sports Medicine recommends attempting to drink enough fluid to prevent body mass losses of greater than 2 percent (if possible),26 but a major obstacle to meeting this recommendation is that drinking large volumes of fluid during exercise raises gut discomfort to levels severe enough to slow down athletes.27, 28 This may be precisely why some research shows drinking to thirst is a superior hydration strategy.
Given these facts, you might be asking yourself if it’s possible for your gut to adapt to—as is seen with other dietary components—increased fluid intakes. In the first decade of the 2000s, G. Patrick Lambert, a professor at Creighton University, designed a study to figure out if repeatedly drinking large volumes of fluid during 90-minute runs affects stomach emptying and gut comfort.29 Participants performed six runs at 65 percent of VO2max, with each run separated by 7–11 days, and from the second to sixth run they drank a 4 percent carbohydrate beverage at volumes that matched their sweat rates. The average volume consumed was nearly 42 ounces, or slightly over 28 ounces per hour. Although the five trials of drinking large fluid volumes didn’t speed stomach emptying over time, the participants’ perceptions of stomach discomfort were improved. Specifically, stomach discomfort—which was rated on a 1-to-4 scale (1 = very comfortable, 4 = very uncomfortable)—decreased from about 2.3 during run two to 1.7 by runs five and six.
These findings imply that any athlete who’s planning to consume more than 15–20 ounces of fluid per hour during competition should repeatedly practice drinking at those higher rates during training. If you decide to try this, it’s important that you don’t overconsume fluids, which is a risk factor for developing the potentially serious condition hyponatremia. As a general rule, you shouldn’t gain weight over the course of an exercise session; if you do, that’s a clear sign you’re replacing fluid at a rate that’s higher than your sweat losses.
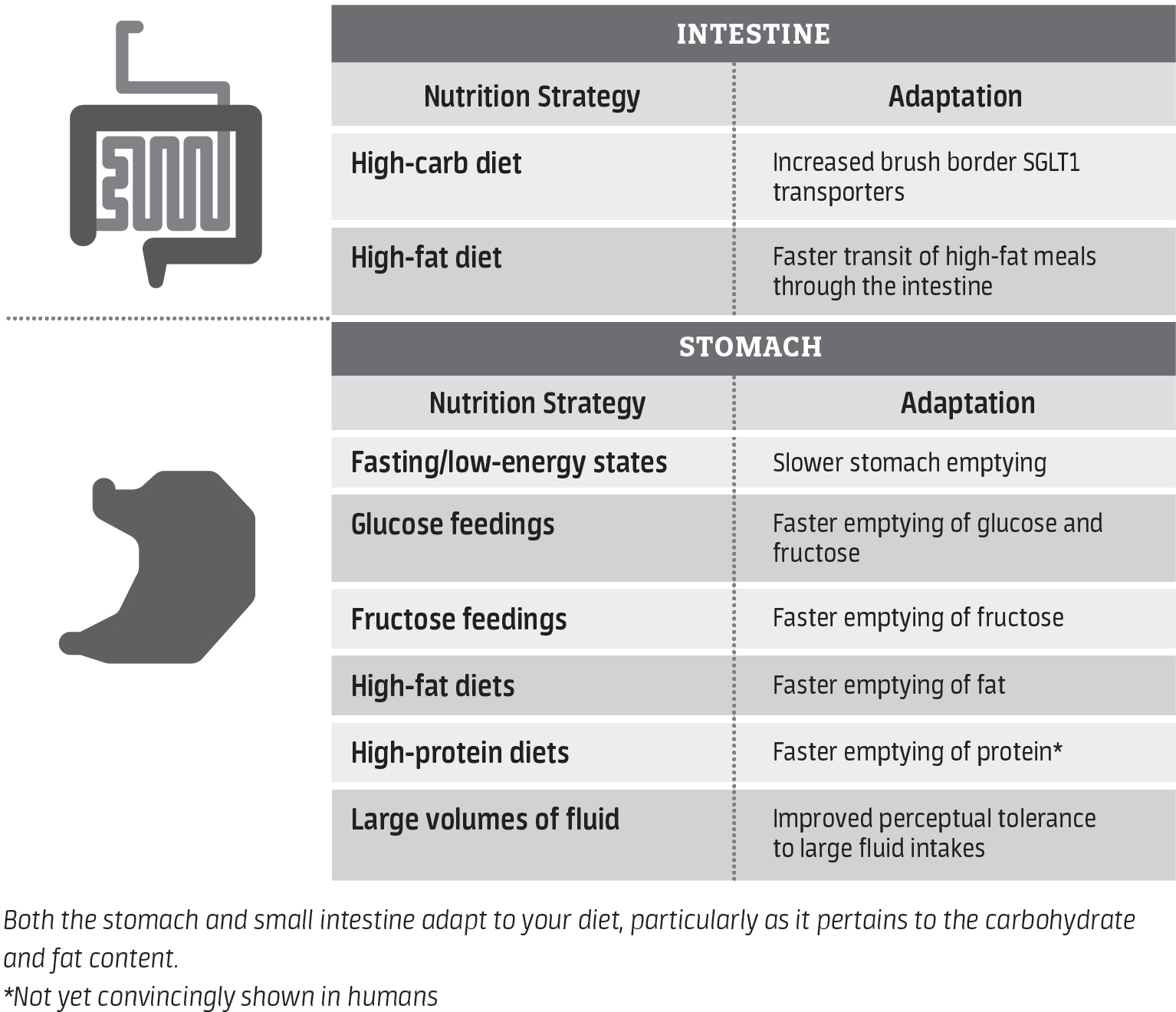
Table 9.1 provides an overview of the major nutrition-related adaptations that have been documented in the scientific literature.
table 9.1.OVERVIEW OF THE GUT’S ADAPTATIONS TO VARIOUS NUTRITIONAL STRATEGIES