
This chapter is all about keeping your toddler well and safe, with information on how to find good health care for your child, including how to choose a care provider, identifying and treating common childhood illnesses, learning about medical procedures, and more.
You’ll also find information about children’s accident prevention, how to childproof your home, and instructions on family fire safety, vehicle safety, and drowning prevention. There are practical hints on how to treat minor injuries, such as removing a splinter and tending to minor cuts, and how to deal with sprains, strains, and fractures.
A special section discusses autism and finding professional and intervention services for toddlers with autism or other childhood disabilities.
Special Note
This section has been written for educational purposes only. It does not cover ALL toddler illnesses—only the most common ones (and diseases that children are vaccinated against)—as well as toddler injuries. It is not intended to serve as a substitute for medical advice from a healthcare provider. Do not use this information to diagnose or treat any health problems, illnesses, or accidents your toddler has without first consulting your pediatrician or family doctor. Your toddler’s health-care provider is the best person to answer any questions or concerns you may have regarding your toddler’s health and safety.
CHOOSING A HEALTH-CARE PROVIDER
If you’re not happy with the healthcare provider you currently have, or you’re searching for a doctor during your child’s toddler years, this section will help you figure out where to go to ensure that your child gets the health care he needs.
Most communities offer a variety of resources you can tap for recommendations about healthcare providers. Ask your friends with children if they’re happy with the care they get from their medical professionals. Your own physician may have suggestions for pediatricians.
If you have health insurance, your insurer may require that you use only those physicians who are part of its network of providers. If you can’t afford health insurance, all states offer some form of medical services for children whose families have moderate or low incomes.
When choosing a health-care provider for your toddler and family, it’s important to think ahead about how that arrangement will work over the years to come, and not just what’s convenient right now.
Family physicians are trained to work with an entire family, parents and children alike, which can provide a welcome sense of familiarity and continuity, and they can be more convenient, too. They’re a good choice if everyone in your family is generally healthy. (Should serious problems arise, you will be referred to a specialist, depending on the situation.)
Pediatricians and pediatric nurse-practitioners have specialized training in caring just for babies and children. Pediatricians are medical doctors who diagnose, treat, examine, and prevent diseases and injuries in children. A pediatrician must hold a four-year undergraduate college degree, a four-year doctor of medicine (MD) or doctor of osteopathy (DO) degree, plus at least three years of residency training. A license and board certification from the American Board of Pediatrics (ABP) are also required to practice as a pediatrician in the United States.
Nurse-practitioners (NPs) are registered nurses who have completed specific advanced nursing education, such as a master’s degree, and some specialize in pediatrics. They have training in the diagnosis and management of common as well as some complex medical conditions. Depending upon the state in which they are licensed, they can perform medical exams, order tests and therapy for patients, and write prescriptions. Unlike physician’s assistants, who can only practice under the license of a medical doctor, nurse-practitioners practice under their own license, and they may practice independently, or they can be affiliated with physicians’ practices.
Since no two health-care providers are the same, it makes sense to interview several providers before choosing the one that best suits your lifestyle and needs. When you meet a prospective provider, ask about nurse-practitioners, physician assistants, and other staff support, billing practices and charges, weekend and nighttime coverage, hospital affiliation, after-hours visits, home visits, and telephone consultations. Find out, too, how emergencies are handled, whether the doctor has privileges at any nearby hospitals, and how promptly you can expect a callback when there’s a problem.
When you go to meet with a prospective pediatrician or other provider, pay attention not only to your comfort level with him or her, but also the way the receptionist and the rest of the staff act toward you, your child, and other patients/ parents in the practice. (Once your child has been accepted as a patient, you’ll probably discover that you are spending as much time interacting with the staff as you do with the doctor.)
Of course, some providers may be very popular and have very busy practices. That translates into shorter visits and less time for talking with you and answering your questions. One solution is to try to get your child’s non-urgent health concerns, such as rashes, colds, cuts, and scrapes, answered by a nurse-practitioner or other professional on the staff.
To minimize long wait times in a waiting room after you’ve made an appointment, call ahead before you leave home to find out if the doctor is on schedule, and/or try to schedule appointments during the least busy times.
Since you’re going to be relying on your doctor’s support and advice for many years, pick one that not only relates well to you, but to your child, too. A child-friendly doctor will take some time to warm up to your child by smiling and talking to win his trust, rather than talking down to him. He’ll take special care not to upset your toddler if possible.
If You Can’t Afford Medical Care
Health departments in most cities offer well care and immunizations at low or no cost, and federal Medicaid programs administered through states provide medical care for low-income families who meet certain eligibility requirements.
• Working families who are ineligible for Medicaid could still qualify for their state’s Children’s Health Insurance Program (CHIP) administered by the federal Centers for Medicare and Medicaid Services.
• In some states, a family of four that earns up to about $36,200 a year may still be eligible for CHIP, but requirements vary by state. The program pays for doctor visits, immunizations, and hospitalizations.
• To apply for either Medicaid or CHIP, contact your local department of social services, often listed under the name of your county. To find out more about what programs your state offers, check out www.insurekidsnow.gov/state/index.html online.
MEDICAL EXAMS
Checkups for toddlers usually are at 12, 15, 18, 24, and 36 months. When your child reaches 18 months, most likely he will have received all of his immunizations until his “kindergarten shots,” which are usually administered between 4 years and 6 years of age.
Before going to your first appointment, use a small notebook to write down all the questions that have been nagging you. Take the notebook and a pen along to the appointment, so that you can log all the doctor’s recommendations.
Here’s how a good exam is likely to go: A nurse will take your child’s vital signs: temperature, heart rate (pulse), speed of breathing (respiration), weight, and height. (A child’s pulse is faster than a grownup’s and is usually around 110.)
Typically blood pressure won’t be measured until age 3, although doctors and health-care providers are becoming increasingly more concerned about the rising levels of chronic diseases affecting children, particularly obesity, so they are administering tests and ordering preventive care earlier than they used to.
Blood pressure is measured by inflating and deflating a small, child-size cuff around the upper arm while counting heartbeats with a stethoscope. Blood pressure (BP) measurements will show possible kidney, hormone, and circulation problems related to the heart. BP gradually increases throughout infancy and childhood, so your toddler’s blood pressure may seem lower than yours is as an adult.
A practitioner skilled in treating children will be careful about how he (or she) approaches your toddler. He will wash his own hands, both to make sure they’re clean and to warm them up. Then he will greet you and your child, and probably suggest that the exam take place with your toddler sitting on your lap or right beside you. A toy or doll may be used to make the procedure seem more playful. He will likely start his exam with the least-threatening body parts, your child’s hands, and end it with the ears and throat.
While taking a close look at your child, he will also be conversing with you to see if you have any questions or concerns. Take your time and don’t feel rushed about raising issues that are important to you, even if they could seem minor.
Even though your child’s physical exam may seem cursory and fast, in fact, your child’s health-care provider will be carefully evaluating a whole host of physical signs. Your toddler may stay dressed for part of the exam, but then might be asked to undress down to his diaper or underpants for the rest of the exam.
Your child’s general physical appearance will be noted, as well as his activity level, how he interacts in his surroundings, and whether or not he seems to be in distress (as many toddlers are when they’re in doctor’s offices).
His skull shape and circumference will be noted. His skin and scalp will be examined for birthmarks, moles, or other growths and for rashes, head lice, or ringworm. The shape and position of his eyes and any abnormal eye movements or an inability to focus will be noted.
The practitioner will want to know that the inside of your toddler’s nose is healthy and that his breathing passages are working well and aren’t inflamed or have unusual mucus or tenderness. He’ll be looking for inappropriate items in the nostrils, too.
Your care provider may ask if you suspect your toddler of having any hearing problems, will examine the shape and position of the ears, and may suggest a hearing test if your child isn’t acquiring words or speaking as expected. Peering into your child’s ear canal, he will be looking to see if the eardrum looks inflamed or is stiff from infection. And he’ll want to make sure that there isn’t something in the ear canals that shouldn’t be there.
Your child will be asked to stick out his tongue, and a flat, wooden stick (tongue depressor) may be used to inspect the tongue, teeth, gums, tonsils, and palate in the back for signs of problems. Your toddler may gag, but that’s on purpose so that the doctor can catch a quick glimpse deeper in his throat.
Your toddler’s chest and abdomen will be examined and listened to with a stethoscope for how his heart and breathing sound.
The practitioner will also be checking his belly to see that there are no lumps or hard places. He’ll want to check your toddler’s muscle tone and if your child’s arms and legs move okay, and that joints are not warm or swollen. He will check how responsive your child’s reflexes are by gently tapping certain places on his knees, ankles, and elbows using a small rubber hammer that will make these parts of limbs automatically jump.
While some practitioners prefer to check a child’s abdomen while he’s lying down, others have found that a toddler might cooperate if he is sitting in your lap. While your child is cooperative, the doctor will also check the belly and other places with you helping. He will be listening for bowel sounds or unusual gurgles and growls, since the belly makes five to thirty-four sounds per minute.
A swollen or enlarged belly could mean there is a blockage, infection, or mass that’s in the way.
He’ll also be checking for tender spots that make your toddler wince or yelp. He will also take a quick look at your toddler’s genitals by pushing the diaper to the side to ensure that everything is as expected.
IMMUNIZATIONS
Modern vaccines provide protection from major, and sometimes life-threatening, illnesses. If your toddler requires immunizations, they could be first-time vaccines or, more likely, continuations of immunizations (booster shots) that were begun in your child’s first year.
Some parents have serious concerns about the safety of vaccines, and they worry about the rumors they have heard about shots causing autism. Talk frankly with your child’s health-care provider about your immunization concerns and seek his or her reasoned, educated opinion about it. Also, make sure to ask about the reactions you can expect and the signs of serious side effects that could potentially result from a vaccination.
It’s helpful to also do your own research about vaccines from trusted medical sources, but remember that immunizing is a hotly debated topic among parents, and they may provide highly biased views that aren’t always well informed or based on research.
Some injections may cause mild side effects such as redness, swelling, and a slight fever, but serious side effects are extremely rare. Once you’ve got all of the information available on immunizations, you’re in a better position to make an informed decision.
Getting Through Shots
Nobody likes to get shots, but they’re a necessary part of preventive care. Here are a few ideas for how you can help your toddler through the process of getting injections.
• Trust. Have confidence that your child’s health-care provider and nurse know how to administer shots quickly and correctly. Let the provider handle him. (The shot is more likely to be given in the thigh because the fat there makes it less uncomfortable than in the arm.)
• Be calm and lighthearted. The way you relax and act will help him to feel less anxious. Trying to prepare a toddler beforehand won’t do much good.
Make a fun little noise to distract him so he’s looking at you instead of the injection shot, or place some colorful stickers on his opposite arm to peel off for a distraction.
• Bring adhesive bandages. Most health-care providers supply child-friendly bandages, such as those with superheroes or Elmo pictured on them, but you can also bring your own, just in case. Keep some extras at home in case he wants a fresh one later.
• Praise. Instead of commiserating about how “awful” the shot was, let him know how proud you are for how he acted through it. Offer a sticker or some other small reward, if desired.
Questions to Ask About Immunizations
• How serious and prevalent is the illness that this shot will help to prevent?
• How effective is this immunization?
• Will a booster be needed? How often?
• Should my child be well (fever-free and without other symptoms) to have it?
• What’s the best way to prepare my toddler for the injection?
• Will there be any side effects? What are they and how should they be treated? How long do they typically last? What are the signs of a more serious side effect?
• If I am pregnant, could my toddler infect me with the vaccination virus and endanger the unborn child?
Immunization Guide


FEVERS AND THEIR TREATMENT
Fevers are quite common in toddlers, so it’s important to have at least one type of thermometer in your first aid kit. Knowing what your toddler’s temperature is can help your health-care provider decide how serious your child’s fever is and how best to treat it.
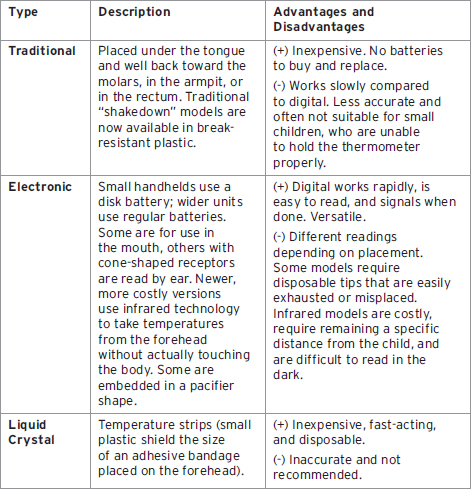
Types of Thermometers
Temperature can be measured by mouth, in the ear, under the arm, or rectally. It is measured in tenths. The average temperature for children and adults is 98.6°F. If you contact your health-care provider about your toddler’s temperature, you will need to tell him where it was measured—oral (mouth), aural (ear), axillary (armpit), or rectal (anus).
Over-the-Counter Fever-Reducing Medications
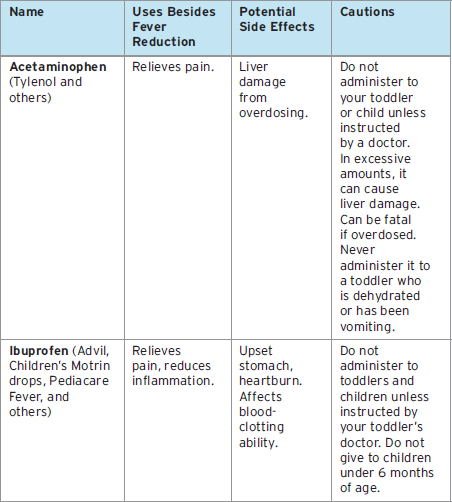
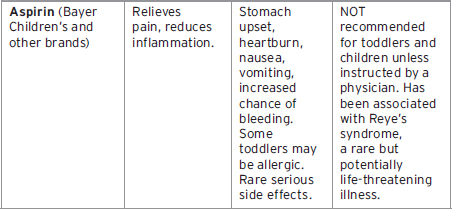
When a toddler has a fever, his health-care provider may recommend an over-the-counter medication to help bring his temperature down. Your child’s exact weight is important for determining how much medication to give him. Always consult your child’s health-care provider first before giving any medications and follow instructions very, very precisely.
If you have ever wondered what the difference is between medications such as Motrin, Tylenol, and aspirin, here’s a chart to help explain it.
Febrile Seizures
Sometimes a rapid rise in temperature to a high fever can trigger a seizure in a toddler. These episodes can be terrifying, but they’re usually harmless. They don’t lead to epilepsy, nor do they cause brain damage, nervous system problems, paralysis, mental retardation, or death.
• If your toddler has a fever-related seizure, he will start to look strange, then he will stiffen, twitch, and his eyes may roll back in his head. He may be momentarily unresponsive, and have uneven breathing, and his skin may appear darker than usual. He may shake on both sides of the body, or twitching may only appear in an arm or leg on only the right or the left side of the body.
• While it’s happening, quickly move your toddler away from anything he could hit if he is thrashing. Turn his head to the side so his mouth can drain, and don’t try to put anything into his mouth or try to feed him until he has recovered.
• Seizures typically happen in the first few hours after the onset of fever and last less than a minute. More rarely, they may go on for up to 15 minutes. After the seizure, your toddler may be sluggish for a couple of hours but will then return to normal. It’s rare that a toddler will have more than one febrile seizure in a 24-hour period. Children older than 1 year of age at the time of their first seizure have only a 30 percent chance of having a second febrile seizure.
To be on the safe side, contact your toddler’s pediatrician after the seizure has ended, particularly if your child seems to be seriously ill. In rare cases, a seizure accompanied by drowsiness, a stiff neck, vomiting, or other symptoms could signal a deadly attack of meningitis that needs rapid, life-saving intervention.
Cough Medicine Warning
In 2008, the U.S. Food and Drug Administration issued a Public Health Advisory for parents and caregivers, recommending that over-the-counter (OTC) cough and cold medications not be used to treat infants and children younger than 2 years of age because of serious adverse events such as rapid heart rates, convulsions, decreased levels of consciousness, and death.
Administering Medications
Accurately measuring your toddler’s medicine doses is very important. There are a variety of devices and tactics for getting medicine into your toddler. Most toddler medications come in liquid form and have a dropper inside with tiny lines for measuring doses. (Use a bright light or flashlight, if needed, to ensure you get the right amount.)
There are also medicine spoons and tiny medicine cups with dose markings. The most accurate way to measure toddler medicine and make sure it doesn’t get spit out is to use a medicine syringe, which resembles a medical syringe, but without the needle. Draw the medicine up to the correct marking, and then squeeze out the medication at the back of your toddler’s tongue. Many pharmacies can add appealing flavorings to children’s liquid medicines. Over-the-counter flavor additives are also available, including some that are sugar-free.
Speak with your pharmacist about pill crushers that enable you to mix your child’s pill with his favorite foods, such as applesauce, pudding, or soft ice cream, to make taking pills more palatable. Also ask your pharmacist about which medicines shouldn’t be mixed with certain foods. Time-release medications cannot be crushed, as your child will not get the full effects of the medication.
A cold ice pop can help to numb your toddler’s taste buds, making bad-tasting medicine easier to take, and if swallowing a pill is required, a product called Swallow Aid is a gel that can be placed on a spoon to coat the pill, making it go down easier.
Sniffing a strong aroma, such as lemon zest or peppermint flavoring, while taking medication can help reduce your toddler’s awareness of bad-smelling liquids.
There are also suppository medications for fever or vomiting that you painlessly insert into your toddler’s anus.
A Note About Antibiotics
Antibiotics are used to fight bacterial infections, such as those that affect the ears, the throat, and the lungs, including tonsillitis (swollen inflamed glands in the throat) and bronchitis (infection in your toddler’s lungs).
More than sixty antibiotics are approved for use in pediatrics, and if your toddler has an infection you may well walk out of the hospital or doctor’s office with a prescription for something you’ve never heard of.
Antibiotics for toddlers are usually in liquid form, so make sure you have a good, easy-to-clean medicine dropper. Amoxicillin is the oldest and most prescribed for ear infections or strep throat, and is commonly used to treat acute middle-ear infections, but there are also other names and brands.
Whatever the prescription, it’s important to limit the use of antibiotics only to a diagnosed bacterial infection, because antibiotics can increase your toddler’s risk of developing asthma. Excessive antibiotic use can also contribute to the rise of antibiotic-resistant strains of bacteria. But, if your toddler does have a serious bacterial infection, antibiotics can be a (literal) lifesaver. It’s important that you follow your health-care provider’s instructions to a tee.
TIP
Never give your toddler any drug without your doctor’s prior approval and directions, including those available in drugstores or labeled “for children.”
TIP
The National Poison Center has poison experts (including for accidental medication overdose) on call 24 hours a day: 800-222-1212.
TIP
Antibiotics fight only bacteria, not viruses.
TYPICAL TODDLER ILLNESSES
Having your child come down with an illness can be distressing. Often toddlers are cranky and out of sorts before the symptoms of an illness actually show up. Your child may refuse to eat, or he may look different, too, perhaps more pale or red-faced, or with dark circles under his eyes, and he may be more whiney than usual.
As luck would have it, most parents don’t discover that their kids are really sick until the middle of the night, the day before a critical meeting or job interview, or on weekends when doctors (and babysitters) are hard to find.
There’s no need to panic or fear for the worst, though. Most children run a whole gamut of garden-variety illnesses before their immune systems become strong enough to help them ward off encroaching bacteria and viruses. Once their bodies get used to handling the bugs, most toddlers sail through weeks and even months without coming down with something.
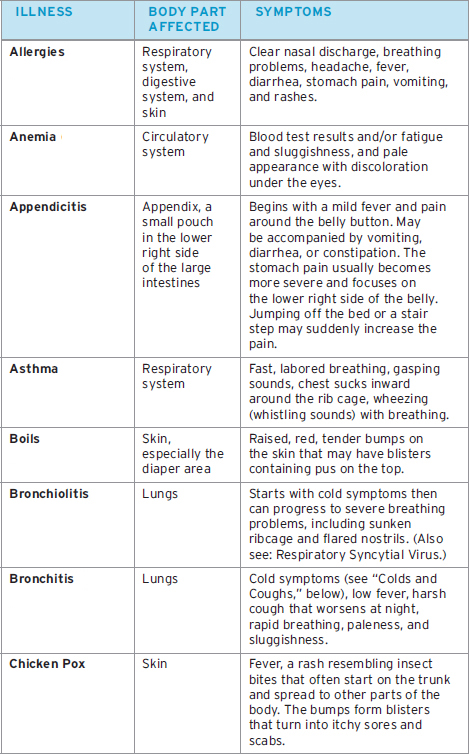
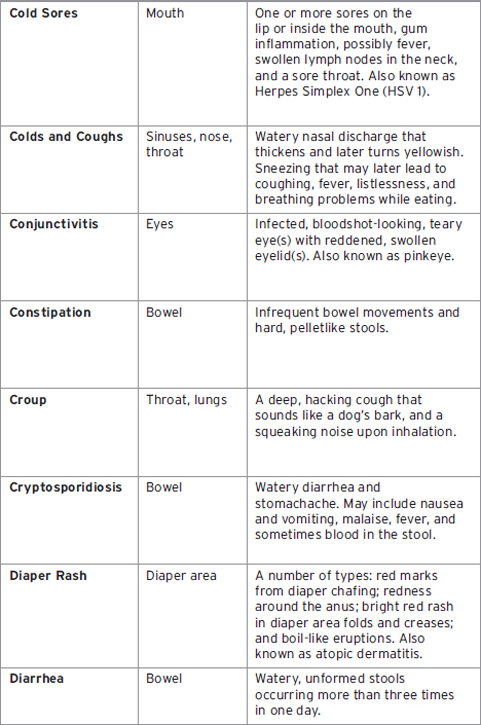
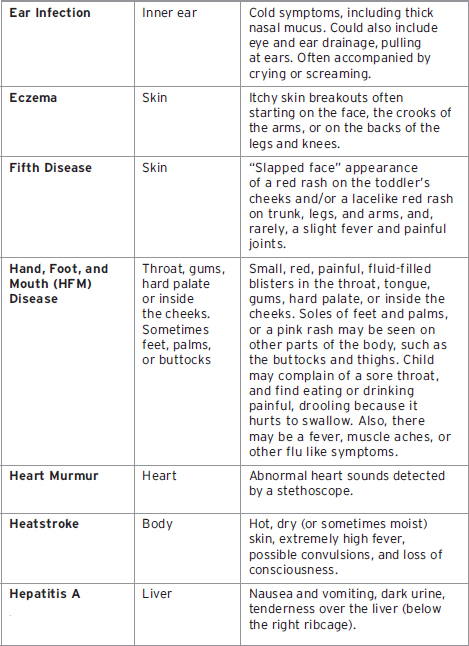
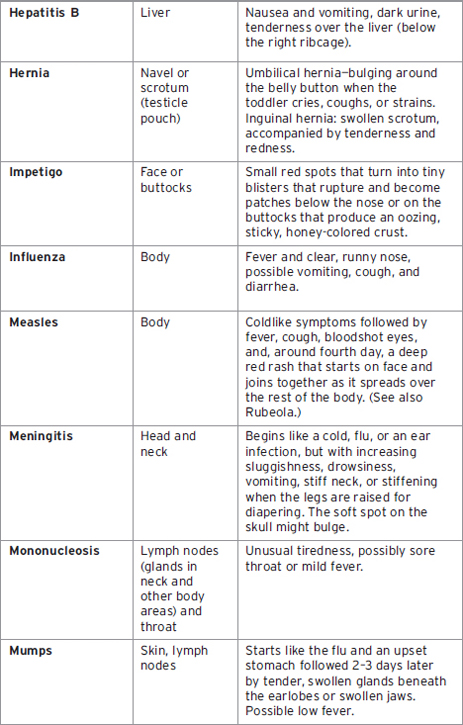
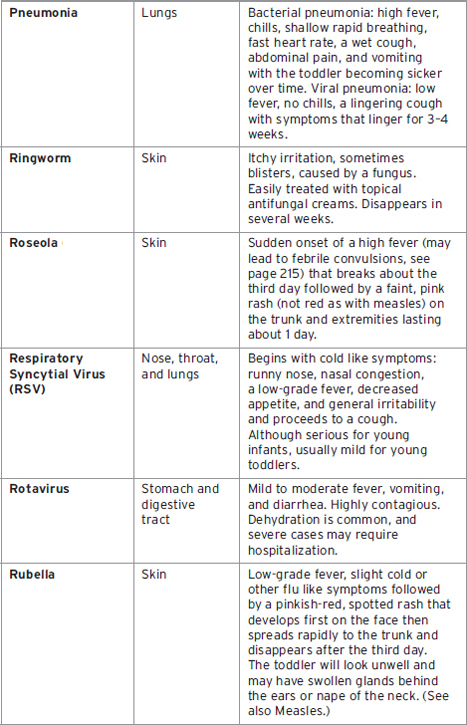
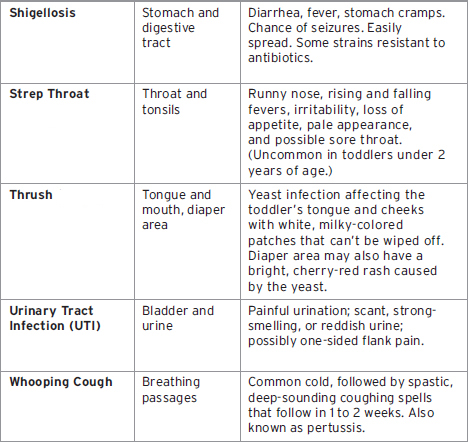
Below is a quick-reference guide to common toddler illnesses and physical problems you may encounter. The chart lists symptoms and gives you page numbers for where to find more detailed descriptions in this section or in other parts of the book.
TIP
Place a humidifier far enough away from the crib and other furniture to prevent moisture damage to wood surfaces.
TODDLER ILLNESSES A TO Z
Allergies
Sometimes the toddler’s body reacts to contact with substances and the immune system releases histamines and other chemicals to fight what the body believes to be an invader.
Symptoms of an allergic reaction may include any of these: a stuffy or runny nose (usually with clear discharge); sneezing or wheezing; red, itchy skin or rashes; and red, watery eyes. While some allergic reactions happen almost immediately, others may take days to happen, making it harder to find the cause.
Your toddler will be more likely to have allergic reactions if he is exposed to cigarette smoke, if you have a family history of allergies, including rashes, sneezing, asthma, or eczema, or if your toddler has been given antibiotics.
Sometimes toddlers will have allergic reactions to plant pollens and animal fur, foods, medications, or plastics found in disposable diapers.
Allergic rhinitis is the swelling and inflammation of the lining of the nose that lingers, rather than disappearing in a week to 10 days as a cold would. In addition to displaying some of the symptoms listed above, toddlers may have dark circles under their eyes, called “allergic shiners,” and a puffy-looking face.
Your doctor may recommend tests to help determine the cause of your toddler’s reaction, and a special elimination diet may be recommended to test for food reactivity. Medications may also be suggested.
A pediatric allergist/immunologist may be needed to help ferret out the cause of your toddler’s reactions. This is a medical doctor trained to treat babies and children who have allergies.
TIP
A severe allergic reaction may be indicated by anaphylactic shock (red, itchy whelps [hives], difficulty breathing). Call 911; every second counts.
TIP
Ana-Kit and EpiPen are brand names of epinephrine emergency kits designed to help reduce the effects of severe, life-threatening body reactions (anaphylactic shock).
Anemia
Iron is important in your child’s diet, particularly during the toddler years of rapid brain growth. The body uses iron to carry oxygen through the blood to the tissues. Iron deficiency can cause serious damage during these formative years.
Anemia is very common during toddlerhood due to toddlers’ dietary changes, such as switching from breastmilk or iron-fortified formula to regular cow’s milk or changing from iron-fortified baby cereals to regular cereals, appetite changes, or drinking juices that don’t supply iron.
Several studies have shown that being iron deficient can also increase a toddler’s vulnerability to lead poisoning, which can cause serious neurological damage.
If your toddler looks pale and seems tired a lot, anemia could be the cause. Other symptoms include a rapid heartbeat, irritability, loss of appetite, brittle nails, and a sore or swollen tongue.
Ask your toddler’s healthcare provider about iron supplementation. Typically, 10 milligrams of elemental iron from iron-fortified drops are suitable for children ages 1 to 6.
Appendicitis
Appendicitis is one of the most common causes for having an operation in childhood. It happens to about 4 out of every 1,000 children. It is an infection in a small, fingerlike pouch in the lower right-hand side of the large bowel.
The most common symptom is pain starting around the belly button that migrates to the lower right side of his abdomen, a tenderness that he doesn’t want touched, and sometimes nausea and vomiting. Your toddler may have trouble eating, or seem unusually sleepy, and in young children, diarrhea may be an early symptom. If your child has appendicitis and is horrified at having his belly touched, you can help your doctor examine him by offering to push on your child’s belly as directed or by putting your child over your shoulder so he’s facing away from the doctor and having the doctor slip his hand between you and your child to feel his abdomen.
Stomach pain is a familiar complaint of toddlers, and that makes it hard to tell if appendicitis or something else is the problem. Only about 3 percent of the time is appendicitis the source of stomach pain. For example, constipation is a much more common cause of severe stomach pain.
If your doctor suspects appendicitis and has your child hospitalized, the chances are 82 percent that he’s right. Perforation is when the swollen appendix balloons and becomes so large that it bursts, sending infectious material into the abdomen, which can be life threatening. The perforation rates for appendicitis are much higher for children than adults (about 30 to 65 percent of the time).
The cure for appendicitis is abdominal surgery, called an appendectomy, to remove it, hopefully before it can rupture, which could lead to lead to a life-threatening inflammation of the abdomen and other organs.
An open appendectomy involves making an incision over the appendix to remove it. A laparoscopic appendectomy uses a special tubular instrument inserted into a tiny incision that allows the surgeon both to view the appendix and to remove it.
Asthma
Asthma is a recurrent inflammatory condition of the bronchial airways. In layman’s terms, it’s difficulty breathing, but it’s also known as bronchial asthma, asthmatic bronchitis, reactive airway disease, bronchitis, and wheezy bronchitis. It affects nearly five million children in the United States.
It has become so widespread that it is now considered one of the most common childhood illnesses. Toddlers and children are more likely to develop asthma if they have allergies or a family history of allergies and asthma, were exposed to tobacco smoke in utero or after birth, were born with low birthweight, or have frequent respiratory infections.
A baby’s or toddler’s first asthma attack can be triggered by a number of things: a chest cold, cold air, exercise, some types of viral infections, changes in air quality (such as cigarette smoke in the air), and allergens such as dust mites, mold, pollen, or animal dander.
During an attack, the lining of your toddler’s lungs will become inflamed, and his airways will spasm and produce mucus. Symptoms will include: coughing, tightness in the chest, shortness of breath, and an unusual wheezing or whistling sound when your toddler exhales.
There are many different kinds of asthma. Your child’s health-care provider is the best person to help you decide if your child has asthma and what treatments should be used. Your child may be prescribed an inhaler (bronchodilator) with a breathing mask for use during attacks without the need for daily medications. If your child develops moderate, persistent asthma, then an inhaled anti-inflammatory steroid and a long-acting bronchodilator may be recommended.
A 2002 study published in the American Journal of Respiratory and Critical Care Medicine found that wheezing or coughing in babies and toddlers 2 years or younger was not necessarily a sign of developing lifelong asthma. But, after age 2, these symptoms could signal that the child might be vulnerable to asthma later. The largest majority of children who developed chronic asthma were found to have a history of asthma in the family. But, the study showed, even with a strong family history of asthma, more than 60 percent of children in asthma-vulnerable families did not go on to have lifelong asthma.
Reducing Asthma Attacks
Take these steps to help to reduce the severity of your toddler’s asthma attacks:
• Eliminate triggers. Keep your home as free as possible of dust and animal hair and dander, eliminate carpeting, and vacuum the floor and stuffed furniture frequently using a vacuum with powerful filters. Change linens frequently, and use allergen-proof casings on all bedding.
• Clean the air. Stop smoking and don’t allow others to smoke in your home. (Even if you smoke outdoors, your lungs will exhale smoke for days, and smoke will also cling to your hair, skin, and clothing when you are indoors.) Constantly run a fan-style air cleaner that contains high-density filtration layers in your child’s bedroom.
• Lower exposure. If pollen is a trigger, you may need to reduce outdoor activities in spring and fall, and be vigilant during sudden or extremely cold temperatures in winter.
Boils
Boils are raised, red bumps on the skin that may develop into infected white-topped blisters. They can erupt anywhere on the skin, but for toddlers who are still in diapers, they most often appear in the diaper area. It’s best to let a boil heal on its own.
Don’t try to pick or squeeze the bumps, as this could cause the infection to spread and could also lead to scarring. If the bump seems seriously infected, your toddler’s doctor may decide to open the boil, and may recommend antibiotic ointment to help with healing.
Bronchiolitis
Bronchiolitis is a viral infection of the tiny bronchioles deep in the lungs of babies and toddlers who are usually less than 2 years of age. In many cases RSV (Respiratory Syncytial Virus) is the culprit. The illness begins with typical cold symptoms, including nasal congestion, a fever of 100 degrees or higher, and mild coughing. It then can progress to become more severe and life-threatening when the lungs’ smallest air passages become inflamed. Signs of severe bronchiolitis include: sucking in of the skin around the ribs and the base of the throat when the child tries to breathe (retractions), flaring nostrils, and grunting. A baby or young child can become exhausted from the effort required to breathe, and in some cases breathing may completely stop. In those cases, emergency care is required. (See also Respiratory Syncytial Virus).
Bronchitis
When the large breathing airways become swollen, bronchitis results. There are two types: acute and chronic. Symptoms of acute bronchitis include fever; a painful cough; a sore throat; thick, yellow mucus; and shortness of breath.
Acute bronchitis is usually the result of a cold or flu, and while this kind of bronchitis is not dangerous in itself, it may lead to pneumonia. If your toddler shows any signs of breathing problems accompanied by a fever, you should call your health-care provider right away. In children, bronchitis is nearly always caused by a virus.
Your doctor will recommend a cough suppressant and/or other methods of treating the individual symptoms. The best ways to prevent bronchitis are to keep your child away from people who are ill, and away from pollution and secondhand smoke.
Chronic bronchitis is bronchitis that lasts for three months or longer. Pollutants, such as secondhand smoke or dust, can make it worse.
Chicken Pox
Chicken pox is a highly contagious childhood disease caused by the varicella zoster virus (VZV), a member of the herpes family. It can be very serious for young toddlers. If you are an adult and haven’t had chicken pox, you may catch it, too. Your toddler may be contagious 1 to 2 days before symptoms show.
Chicken pox is spread by other children, so keep your toddler away from children who have been exposed to chicken pox at school or from siblings. The varicella vaccine is available, and is recommended between 12 to 18 months of age. (And it is also recommended for you if you’re not pregnant and for your toddler’s siblings if any of you have not had the disease.)
The symptoms of chicken pox are sluggishness, frequent crying, and loss of appetite. Several days after exposure, a rash of flat, red, splotchy dots will erupt. It usually starts on the chest or stomach and back, then spreads to the face and scalp a day or so later. The red dots of the rash then join together to form clusters of tiny pimples, which then progress to small, delicate, clear blisters with new rash areas developing each day. The blisters form into extremely itchy scabs. Recovery can take as long as two weeks.
Oatmeal baths can be very soothing to dry, itchy skin. Tie a handful of raw oatmeal in a washcloth and swish it around in your child’s bathwater. Your toddler’s health-care provider may prescribe creams to put on the itchy spots, or over-the-counter lotions, such as calamine lotion, to help relieve the intense itching.
Cold Sores
Cold sores, also known as fever blisters, are small, fluid-filled blisters that crop up on or near the lips, and are very common during childhood. They can appear individually or in clusters. Despite their name, they have nothing to do with colds, but are caused by the herpes simplex virus type 1 (not herpes simplex virus type 2 that causes genital herpes, though either can cause sores in the facial or genital area).
Your toddler can catch the virus by sharing a cup, utensil, or slobbery toy with another person who has the infection or carried in his saliva through mouth-to-mouth kissing. During the first bout, called primary herpes, there may be mouth soreness, gum inflammation, possibly fever, swollen lymph nodes in the neck, and a sore throat, but symptoms could be very mild.
Recovery is in about 7 to 10 days, but the virus will stay in his body for life. For some children, the virus lies dormant; for others, it will periodically show up again. These flare-ups are called secondary herpes and can erupt from stress, fever, and sun exposure. Secondary flare-ups may be milder without swelling of his gums or lymph nodes or a fever or sore throat, but he will have the telltale blistering on or near his lips.
If your toddler develops a sore on his eyelid or the surface of his eye, call your health-care provider right away. Your child may need antiviral drugs to keep the infection from scarring his cornea. (In rare cases, ocular herpes can weaken vision and even cause blindness.)
Most treatments reduce the pain of the sore, but the virus has to run its course.
Colds and Coughs
It’s likely that your toddler will have more colds and other upper respiratory infections than any other illnesses throughout his childhood. On average, children catch nine colds during their first 2 years. Your toddler will be more vulnerable to these infections with more public contact, because viruses and bacteria are spread by contact and his body hasn’t yet learned how to fight them.
If your toddler has a cold, it will usually begin with clear fluid running from the nose, sneezing, and possibly a low fever. Though exposing your toddler to cold air doesn’t cause a cold, exposure to cold weather changes the way our bodies fight off viruses. The protective mucus and cilia in the respiratory tract do not function as efficiently, so if you get exposed to a virus in those conditions, you’re more likely to catch it.
If your toddler has a difficult time blowing his nose, treat his nasal congestion by using a ball-shaped, rubber suction bulb. Squeeze the bulb part of the syringe first, carefully place the tip into one nostril, and then gently release the bulb to create suction. Only a slight suction is needed. If secretions are particularly thick, your pediatrician may recommend mild saline nose drops. Using a dropper that has been cleaned with soap and water and rinsed well with plain water, place two drops in each nostril, and then immediately suction with the bulb. However, don’t suction too often as this can cause irritation. You might also try placing saline in the nose several times during the day.
When your child has a cold or an upper respiratory infection, place a cool-mist humidifier in his room to keep the air moist and make him more comfortable, being sure to clean and dry the humidifier thoroughly each day to prevent bacterial or mold contamination. (Hot-water vaporizers are not recommended because they can cause serious scalds or burns at their spouts.)
TIP
Nose drops that contain medication may be harmful to toddlers.
Conjunctivitis
Sometimes toddlers’ eyes get swollen or crusty, either because one or both tear ducts are plugged, or due to an infection, such as conjunctivitis (pinkeye). One or both eyes will appear red and swollen, crusty, or sticky with mucus. The infection can be caused by bacteria, a virus, or plugged tear ducts.
The home remedy is to dip a clean, soft washcloth or cotton ball in mildly warm water, squeeze out the excess moisture, and then gently massage the affected area every 2 to 4 hours. If symptoms persist after a day of lukewarm compresses, call your toddler’s health-care provider. Special eye drops or an ointment are likely to be prescribed. Most cases clear up in 3 to 5 days.
The viral and bacterial forms of pinkeye are highly contagious and can be spread very easily from one person to another, usually through hand-to-eye contact. Make sure everyone in the family keeps their hands clean when there’s an outbreak, and don’t allow anyone to share washcloths or towels.
Constipation
(See Chapter 9.)
Croup
Croup is not a single problem, but a symptom that occurs when a child’s upper airway swells and becomes narrowed by an illness or an allergic reaction. It causes a cough that sounds like a dog’s bark, and a squeaking noise when the child inhales. Croup is most common in babies and children between 3 months and 5 years.
Croup is usually not serious and can be helped with a cool-mist humidifier or by holding your toddler in the bathroom while a hot shower fills the room with steam. However, if your child shows signs of having difficulty breathing and/ or swallowing or is breathing rapidly, or the skin between his ribs pulls in with each breath, and/or he has a fever, call your pediatrician immediately.
In some toddlers and children, croup is a recurring problem, and those who are vulnerable to it may have three to four bouts of croup per flu season. Usually, croup doesn’t present a serious problem, but you should always seek your doctor’s advice. In most cases, children outgrow croup when their air passages mature and increase in size.
Cryptosporidiosis
Cryptosporidiosis, called crypto for short, is an infectious diarrheal disease caused by the Cryptosporidium parasite. It’s common among children in child-care settings, but it can also be transmitted at swimming pools, especially kiddie pools.
Cryptosporidiosis is spread through fecal-oral transmission by feces of an infected person or an object that has been contaminated with the infected person’s feces. Infection can also occur if contaminated food or water is ingested. Outbreaks in child-care settings are most common in August and September.
Symptoms can take a week to develop and usually include watery diarrhea and stomachache, but can also include nausea and vomiting, general ill feeling, and fever, and sometimes there may be blood in the stool. The most severe part lasts from 4 to 7 days, but symptoms may come and go for up to 30 days.
The spread of cryptosporidiosis is highest among children who are not toilet-trained, and higher among toddlers than infants, because of their increased movement and interaction with other children. Child-care providers can get it from diaper changing.
The parasite is hard to detect, as few laboratories run tests for it, and there is no effective treatment for it. It simply runs its course.
Diaper Rash
Diaper rash is a red, sore patch of skin on your child’s bottom, genital area, or between the creases inside his thighs. It’s common for diaper users between 5 and 15 months of age. There are a variety of causes, but usually the red patches last for only a few days and then disappear.
Skin infections break out in the diaper area when moisture has broken down the skin’s naturally protective, oily barrier. Sometimes the breakdown is worsened by harsh chemicals produced when urine and feces mix together in the diaper and stay there for a while. That’s why it’s important to change your toddler’s diaper frequently and to keep the area rinsed off with clear water after a bowel movement.
Frequent airing out of the diaper area, preferably with some sunlight, can also help to improve the rash by letting the skin dry out. Baby powder and cornstarch don’t help diaper rash; in fact, they can make it worse, as can alcohol-based wipes. A thick layer of a zinc-based diaper cream can help to protect the skin long enough so that the rash can heal.
A cherry-red, oozing diaper rash may signal a yeast infection that may need special treatment. Your toddler’s health-care provider may recommend an anti-fungal cream, ointment, or a mild topical steroid. But don’t apply any over-the-counter products yourself unless they’ve gotten your health-care provider’s approval.
Contact your health-care provider if the rash doesn’t go away, or if it worsens, such as spreading to other body parts, there’s a fever involved, or it turns into pimples, blisters, ulcers, acne-like bumps or pus-filled sores.
Diarrhea
Diarrhea is loose, watery stools occurring more than three times per day. It is not the occasional loose stool or the frequent passing of barely formed stools. There are many possible causes of diarrhea in toddlers, such as bacterial infections, viruses, and parasites, and sometimes it can be caused by medical conditions, or allergic reactions to foods or milk products. One of the most common causes of toddler diarrhea is a stomach flu (viral gastroenteritis). Although many different viruses can cause stomach flu in toddlers, the most common one is called rotavirus.
Toddlers with diarrhea are a special concern because of their small body size, which puts them at greater risk for dehydration, particularly if the diarrhea is accompanied by vomiting. Your health-care provider will want to treat against dehydration by replacing lost fluid and electrolytes (sodium and potassium).
Giving special fluids by mouth (oral rehydration therapy) may be recommended using rehydration drinks such as Pedialyte, which can be found in bottles or as a powder to be added to water in most pharmacies and supermarkets and purchased without a prescription. (Note: Rehydration fluids have a brief shelf life. Once a bottle has been opened or a mix prepared, it must be used or thrown out within 24 hours. Bacteria rapidly grow in the solution, and a toddler could easily drink three or four bottles of the fluid during an illness.)
Do not try to treat diarrhea without first consulting with your toddler’s health-care provider. For home treatment, allow your toddler’s system to settle for a few hours after a diarrhea attack before encouraging him to eat again. If vomiting is involved, offer him small sips of water, or clear liquids, such as chicken or beef broth, or let him suck on ice chips. After several hours, gradually reintroduce food, starting with bland, easy-to-digest foods, such as applesauce, strained bananas, strained carrots, rice, or mashed potatoes.
Intestines that have been damaged by severe diarrhea may have trouble digesting whole cow’s milk, and your toddler’s health-care provider can suggest alternative liquids.
Diarrhea can cause your toddler’s diaper area to become red and sore. Use a thick layer of zinc-based diaper cream, to provide a shield for the skin. Change diapers frequently, rinsing his bottom with water and air-drying it, and cut down on the use of baby wipes, which can be irritating to toddlers’ irritated skin.
Ear Infection
Next to colds, middle-ear infection (otitis media) is the most common cause for trips to the pediatrician. As many as three out of four children have some form of ear infections by age 3.
There are two different kinds of infections: otitis media with effusion (OME), which means there is fluid in the middle ear, and acute otitis media (AOM), which refers to fluid in the middle ear that also comes with pain, redness, and a bulging eardrum.
Children with OME will seem completely fine, and you won’t know anything is wrong unless your pediatrician discovers the infection during a well-toddler visit. But toddlers with AOM will be fussy, especially at night, and may have a fever and other coldlike symptoms.
After a case of AOM, your toddler will probably have a case of OME for several weeks afterward. Typically, an acute infection will set in a few days after a cold has started. You can’t see that the toddler has the infection, but your health-care provider will be able to detect it by looking for swelling in your toddler’s ear with an otoscope and by blowing air on the eardrum to see if it’s swollen (the toddler will hate this, so be prepared for screaming).
If your toddler has an ear infection, a painkiller such as acetaminophen may be recommended along with a course of antibiotics that will usually come in liquid form. (If your toddler rejects the liquid, try mixing it in applesauce or yogurt.) In the meantime, your toddler may be more comfortable upright than lying down. Applying a warm, moist towel to your toddler’s cheek near the ears could help soothe the pain.
Usually ear infections get better after several days of treatment. If ear infections are recurrent (more than three episodes in 6 months), and your pediatrician believes the infections interfere with your toddler’s hearing and language development, minor surgery may be recommended that involves placing tiny tubes in the ear for draining fluid.
Eczema
Eczema (or atopic dermatitis) produces thickened, red, dry, flaky skin patches that itch. Sometimes the patches can become infected and look weepy with crusts, especially if your toddler scratches them. While eczema usually shows up on babies’ faces, toddlers get the rash around their knees, elbows, and ankles.
Eczema is thought to run in families who have other allergies, too, such as asthma and hay fever. It is not a direct allergic reaction itself, but certain things can trigger it, such as something your toddler eats or comes in contact with, such as wool or chemicals in detergents, soaps, lotions, and fabric softeners. Too much sun can also set off an attack.
Practical treatments can help to soothe the skin during an attack. Daily baths in lukewarm (not hot) water using bath oil and a soap substitute can help, but be careful to not rub the skin when drying off. Moisturizers are soothing. They may need to be applied repeatedly throughout the day, and sometimes moist wraps also can help to soothe the skin. Sunscreen can help to protect the skin from burning. Keeping fingernails trimmed and clean will help to reduce inflammation. (Mittens or socks over your toddler’s hands may help keep him from scratching himself during the night).
A recent study found that soaking a child for 5 to 10 minutes twice a week in a highly diluted bleach bath was five times more effective in treating eczema than plain water. The researchers’ treatment instructions were to stir a scant 2 teaspoons of bleach per gallon into bathwater (or ½ cup per full tub) before your child enters the tub with the caution that your child not be allowed to drink the water. Ask your health-care provider first before trying it.
Fifth Disease
A fine, lacy pink rash starts on the cheeks, giving the toddler a “slapped cheek” look, and it may then move to the backs of the arms and legs. It may show up and disappear over the process of 1 to 2 weeks, especially in response to a toddler bath or irritation. Rarely, the rash is accompanied by a slight fever and achy joints. The rash on the face will usually disappear within 4 days after it shows up, while the rash on the rest of the body will take 3 to 7 days to go away. Usually, the only symptom is the rash, and it will disappear on its own.
German Measles
(See Rubella.)
Hand, Foot, and Mouth Disease
Hand, Foot, and Mouth Disease (HFMD) (coxsackie virus) is common among toddlers, especially children in child care. It is caused by a highly contagious virus, which is mostly spread through coughing and sneezing. The incubation stage is about 3 to 6 days, and, unfortunately, a child is most contagious before he shows any symptoms.
When they do appear, the symptoms include a blistery rash on the hands, feet, and mouth. There may also be an accompanying sore throat, fever, and a general sense of feeling unwell.
If a toddler refuses to eat or drink because his mouth and throat are too sore, it can lead to dehydration, a serious condition that can be detected by decreased urination. If his fever rises above 103°F, see his health-care provider.
Like most viruses, HFMD has no cure, and it simply has to run its course, which takes about 7 to 10 days.
Heart Murmur
Heart murmurs are common in children, and they’re often harmless. “Innocent” or “harmless” heart murmurs, as health-care providers call them, are simply the sound the blood makes as it moves through the chambers of the heart. They may get louder when a child’s heart beats faster, and softer when he’s calm.
More serious murmurs are caused by something wrong with a child’s heart, such as a hole in it, or a leaky or narrow heart valve. If your health-care provider is concerned about what is being heard with the stethoscope, your child may be refered to a pediatric cardiologist (children’s heart doctor). Your child will have an exam, and he may be given tests, such as a chest X-ray, an electrocardiogram (EKG, or ECG), or an echocardiogram (“echo”) to find out what is making the unusual sound. Depending upon the severity of the heart problem, medication or surgery may be options.
Heatstroke
Heat stroke occurs in toddlers when their bodies are unable to cool themselves down because of high temperatures, humidity or becoming dehydrated from insufficient fluids. Young children’s bodies don’t adapt as quickly to heat changes as adults’ do. They don’t sweat very well and can overdo their activities without realizing that they are too hot or thirsty. Fevers and medications can also make toddlers more susceptible to overheating, as can wrapping them up during a cold or flu in an attempt to cure it. (Never, ever leave your toddler in a hot car!)
Heat stroke at this age can be deadly and result in serious organ damage. If your toddler is in trouble, he may spike a high temperature (103°F and above), he may appear red-faced and feel hot and dry, he will have dark urine or none at all, and he may either not sweat at all or have profuse sweating. If he is dehydrated, his mouth will appear dry and parched, his eyes may appear sunken, and his hands and feet may feel cold or look splotchy. He may act sluggish, dizzy, or confused, see things that aren’t there, or even lose consciousness.
If you suspect heat stroke, notify 9-1-1 immediately, and meanwhile, get your child into the shade or inside a cool building. Offer him tepid water to drink. Apply cool or tepid water to the skin and seek out a vent or fan his wet body to help cool him down. Ice packs wrapped in towels and placed under the arms or at his crotch may help. Your child will likely be given fluids containing electrolytes to drink or through a vein.
Hepatitis
There are many types of hepatitis. All are infections of the liver. Some may be silent and hard to detect, while others may result in jaundice—a yellowing of the skin and whites of the eyes—combined with nausea and weakness. Other symptoms could seem similar to the flu, such as loss of appetite, nausea, vomiting, diarrhea, and itchiness. Most children recover from hepatitis, but some go on to have chronic liver problems.
Hepatitis A is a liver inflammation. The virus can be passed through contaminated food, water, or contact with small amounts of an infected person’s bowel movements. It is usually short lived and may not lead to the serious consequences of hepatitis B.
Hepatitis B is a serious infection of the liver transmitted by exposure to an infected person’s blood. It can be transmitted from mother to baby during delivery. Hepatitis B infects more than 200,000 people each year in the United States and 4,000 to 5,000 die as a result of chronic problems relating to it. Since 1991, the Centers for Disease Control and Prevention have recommended that toddlers be vaccinated against hepatitis B through a series of shots given during the first 6 months after birth.
Hernia
A hernia is the protrusion of an organ through the structure that normally surrounds or contains it. With an umbilical hernia, a bit of intestine or fatty tissue near the navel breaks through the muscular wall of the abdomen. The hernia will bulge out around the belly button when the toddler cries, coughs, or strains.
Umbilical hernias are much more common in African-American toddlers than other races, and they usually resolve on their own by age 4. (Note: Having a permanent “innie” or “outie” belly button is not a hernia).
An inguinal hernia occurs when a small portion of the toddler’s intestine becomes captured in the scrotal sac (that holds his testicles) and causes swelling, tenderness, and redness. It may first happen after a bout of vigorous crying. Since it may cause severe problems with blockage in the intestine, medical intervention may be necessary.
Impetigo
Impetigo is a bacterial skin infection caused by a staph or strep bacterium. It begins as tiny blisters. The blisters burst and leave brown or red wet patches of skin that may weep fluid that forms a yellowish, honeycomblike crust, usually around the nose and mouth or the buttocks, and sometimes the hands and forearms.
Your toddler’s health-care provider may recommend applying an over-the-counter antibiotic ointment or prescribe an oral antibiotic to prevent its spreading. Also be sure to cut your toddler’s nails short to prevent scratching and a spread of the infection.
If applying antibiotic ointment doesn’t make the rash noticeably better in a few days, contact your pediatrician. In rare cases, impetigo may lead to a kidney problem known as glomerulonephritis, which causes the urine to turn dark (cola) brown. In most cases, impetigo is short lived and usually heals completely in children.
Influenza
Typically, flu starts with a fever, fatigue, and chills, followed by a runny nose with clear mucus and a cough. Your toddler may also be irritable and have swollen glands, arch his back with abdominal pain, have smelly, explosive diarrhea, and projectile vomiting.
In other words, if your toddler gets the flu, it’s going to be a long, long night. Your health-care provider may want to examine your toddler to be sure that there are no other causes, and she might tell you that the most you can do is keep the toddler fed and hydrated, and be on the lookout for a high fever or signs of dehydration (sunken eyes and decreased urination).
Your health-care provider may prescribe an antiviral medication that can lessen the symptoms and shorten the length of the flu by a day or two. The trick is in making the diagnosis as soon as possible, because the medication must be given in the first 48 hours. Once that 48-hour window closes, the antiviral medications are no longer effective.
Also, you may be able to prevent your toddler from catching the flu in the first place by asking your health-care provider to give your toddler a flu shot at the beginning of flu season (usually in late fall).
Measles
Measles is a highly contagious viral illness characterized by coldlike symptoms, fever, cough, conjunctivitis (pinkeye), and a deep red rash that starts on the face. Around the fourth day, the toddler will seem more ill as the rash spreads over the rest of the body.
Over the last few decades, measles cases have decimated in the United States and Canada because of widespread immunization. Before widespread immunization, measles was so common during childhood that the majority of the population had been infected by age 20. Rarely, measles can develop into pneumonia, encephalitis (brain swelling), and ear infections. (See also Rubella, below.)
Meningitis
Meningitis is a rare but sometimes deadly infection of the tissues that cover the brain, and it can be deadly within a matter of hours. The beginning signs of meningitis are subtle and not very different from coming down with a bad cold. There may be fever, vomiting, and a general feeling of unwell. Your child may complain that his head or neck area hurts and he seems to dislike bright lights.
As meningitis progresses, your toddler may have seizures or become extremely sluggish, sleepy, and difficult to wake, which calls for racing to the emergency room. Sometimes a rash may be involved (be sure to tell your child’s healthcare provider about that).
A blood test to check for a bacterial infection may be called for, and possibly a spinal tap to see if the spinal fluid is infected. If meningitis is treated aggressively and quickly with antibiotics, the crippling and long-lasting effects of the disease can be minimized.
Mononucleosis
Mononucleosis (“mono,” or glandular fever) is caused by Epstein-Barr virus (EBV). Although it is more common among teenagers, it can also affect young children. In younger children there may be only a mild fever, and the child may not appear ill, but other symptoms may include being more tired than usual and having swollen lymph nodes (small, round infection-fighting lymph glands in different places on the body), and a mild fever.
A specific blood test for mono is available. It is transmitted by fluids from the nose and throat and sharing of utensils or cups. There is no current treatment for mono except plenty of rest. Once a child gets over the active phase, it will remain active in his body throughout his life and it may occasionally reactivate.
Mumps
Mumps is a highly contagious viral infection that spreads from child to child through saliva. It can be caught by sharing eating utensils or drinks, or even breathing the air immediately after someone has sneezed or coughed.
The first symptoms are usually mild: a fever and loss of appetite. Then, within a week, the area in front of your toddler’s ears, the parotid glands, will noticeably swell, giving your child a chipmunk appearance. Other symptoms could also include a stiff neck (see also meningitis), sluggishness and weakness, and painful chewing and swallowing. Sometimes mumps will affect the salivary glands under the tongue or chin or in the chest area.
Since it is caused by a virus, antibiotics don’t help, but having your child innoculated with the MMR vaccine before he is exposed to it can help to protect him from it. Generally, having mumps conveys lifelong immunity to catching it again. (See immunization table.)
Pneumonia
Pneumonia is an inflammation or infection of the lungs, when the air sacs fill with pus, mucus, and other liquid that interferes with their functioning. There are multiple causes and types of pneumonia. The symptoms of bacterial pneumonia are a fever, chills, rapid breathing, fast heart rate, a wet cough, abdominal pain, and vomiting, with the toddler becoming sicker over time.
Viral pneumonia is marked by a low fever, no chills, and a lingering cough, but with the toddler seeming almost normal and with symptoms persisting for 3 to 4 weeks. Lobar pneumonia refers to pneumonia in a section (lobe) of a lung, while bronchial pneumonia (or bronchopneumonia) refers to pneumonia that affects patches throughout both lungs.
In serious cases of pneumonia oxygen can’t reach the blood, and when there is insufficient oxygen in the blood, body cells can’t function properly and may die. Prompt treatment with antibiotics and oxygen almost always cures bacterial pneumonia, but treating it aggressively and early is important.
Ringworm
Ringworm is a harmless and sometimes itchy skin inflammation that often appears as a round ring of tiny blisters with a sharp border between the skin and the dime- to quarter-sized lesions, often with clear skin inside the ring. It is not caused by a worm, but by one or two types of fungus, Trichophyton and Microsporum, and it often shows up on the face, trunk, or limbs.
It is easily treated by topical, over-the-counter antifungal creams that contain clotrimazole (brand name Lotrimin or Mycelex) and are applied twice a day to the reddened area and surrounding skin. Your health-care provider will be able to recommend the most effective treatment.
The fungi in the rash are contagious by direct contact with the rash or from the hands of an infected person who has been scratching the rash. Your child can also catch it from infected pets, especially dogs and cats.
It will disappear with treatment after several weeks.
Roseola
Roseola infantum is a very common viral illness found in children all over the world. In the United States, about one in three children have some kind of roseola, and 86 percent of children have acquired the virus’ antibodies by 1 year of age.
Your toddler could be a carrier for the virus and neither show symptoms nor appear ill, or he could suddenly develop a fever between 102°F and 104°F that lasts for 3 to 5 days. In some cases, the sudden rise in the fever may lead to febrile seizures (see Febrile Seizures).
Your toddler will have decreased appetite, mild diarrhea, a slight cough, and a runny nose, and seem more irritable and sleepy than usual. His eyelids may seem swollen and droopy.
The fever will likely break on about the third day and be followed by a faint, pink rash (not red as with measles) on the toddler’s trunk, arms, and legs that will last about a day. After the fever subsides, a faint, pink rash develops on the body, spreads to the upper arms and neck, and then disappears in a day or so. Your toddler’s health-care provider may prescribe medications to increase comfort.
Rotavirus
Rotavirus is responsible for approximately 5 to 10 percent of all cases of diarrhea among children under 5 years of age. It accounts for more than 500,000 physician visits and approximately 55,000 to 70,000 hospitalizations each year among children under 5 years of age, and, sadly, an estimated 1 in 200,000 toddlers worldwide with rotavirus diarrhea die from the complications of the infection.
Symptoms can be mild to severe. It begins with few or no symptoms, or a mild to moderate fever followed by severe vomiting followed by diarrhea. The incubation period is about 2 days before symptoms appear, starting with vomiting followed by 4 to 8 days of profuse diarrhea. It is highly contagious and usually spread when children touch or place in their mouths small, usually invisible amounts of fecal matter found on surfaces such as toys, books, and clothing, or on the hands of caregivers. It can also be transmitted through contaminated water or food, and possibly by respiratory droplets in a sneeze, cough, or exhalation.
Dehydration is the most dangerous side effect of the virus. Your health-care provider will guide you in how to provide hydration, such as electrolyte solutions (Pedialyte), to keep your toddler well hydrated. Severe cases may require hospitalization with intravenous fluids.
Rotavirus can be prevented with a vaccination that usually is administered in 2 doses during infancy. Once a child has it, later infections are apt to be less severe as his immune system may provide some protection.
RSV
RSV stands for respiratory syncytial (pronounced “sin- SHISH-al”) virus. It infects most children sooner or later (usually by the age of 2), but during toddlerhood, it is rarely more troublesome for a child than the common cold. (It is more serious in babies and can cause serious respiratory infections such as bronchiolitis and pneumonia.)
RSV begins with coldlike symptoms, such as a runny or stuffy nose, a minor cough, and fever, with the cough becoming more pronounced after a few days. In severe cases, your toddler may have labored breathing (faster than 40 breaths per minute), flared nostrils, rib cage expanding more than usual, wheezing or grunting when breathing, bluish lips or fingernails, and a fever that rises to over 103°F—all of which are signs to contact your health-care provider.
Because RSV is a virus, antibiotics and other medications aren’t effective. Milder symptoms usually last 5 to 7 days and go away on their own, but the cough may linger for weeks longer. Severe forms may call for hospitalization for oxygen treatments, intravenous fluids, and drugs to help open your toddler’s airways.
A vaccination is available called Synagis, but the protection is only temporary and monthly shots may need to be given during RSV season, between October and April.
Rubella
Sometimes called “3-day measles” or German measles, this virus starts with mild symptoms of illness, such as a low-grade fever, a slight cold, or flulike indications. Then, a pinkish red, spotted rash develops, first on the toddler’s face and rapidly spreads to the trunk. It disappears after the third day. The toddler will look unwell and may have swollen glands behind the ears or nape of the neck but will recover within a few days. Contact your toddler’s health-care provider, although no medical treatment is usually needed.
More rarely, rubella can lead to brain swelling or a problem with bleeding. It is the most dangerous when mothers without immunity catch it and transmit it to their babies in utero during certain months of pregnancy. It can cause a fetus to be stillborn, or to be born blind or deaf or with learning disabilities. Rubella immunization is part of MMR shots (see immunization chart).
Shigellosis
Shigellosis is an infectious disease caused by a group of bacteria called Shigella. Toddlers who are infected with Shigella develop diarrhea, fever, and stomach cramps 1 or 2 days after being exposed to the bacterium, and diarrhea is often bloody.
The bacteria are present in the diarrheal stools of infected person while they are sick and for a week or two afterward, and it can be passed by soiled fingers from one person to another by mouth, particularly between children who are still wearing diapers. It also can be caught by swimming in contaminated water or eating vegetables that have been grown in fields contaminated by sewage.
It is more common during the summer months and in toddlers from 2 to 4 years of age. In some young children, the diarrhea can be so severe and the risks of dehydration so severe that hospitalization may be recommended. A high fever may also be associated with seizures in children younger than 2 years of age. Some persons who are infected may have no symptoms at all, but may still pass the Shigella bacteria to others.
Children with mild infections will usually recover quickly without antibiotic treatment, but it may take several months until their bowel habits return to normal. Some forms can later lead to Reiter’s syndrome, which causes joint pain, eye irritation, and painful urination that can last for months or years, and possibly lead to chronic arthritis.
Effective treatment depends on which germ is causing the diarrhea. Usually it is treated with antibiotics to kill it and shorten the illness. Unfortunately, some Shigella bacteria have become resistant to antibiotics and using antibiotics to treat shigellosis can actually make the germs more resistant in the future.
TIP
Avoid antidiarrheal medicines to treat shigellosis, as they are likely to make the illness worse.
Strep Throat
Officially called streptococcal pharyngitis, strep throat is caused by streptococcal bacteria. In children, the infection can cause red, swollen tonsils covered in a white, smelly material, red patches on the roof of the mouth, a white tongue, a high fever, swollen glands, abdominal pain, vomiting, and trouble swallowing. Neck glands may also be swollen.
In toddlers the symptoms are usually milder, and include a runny nose, rising and falling fevers, irritability, loss of appetite, and a pale appearance. The infection usually lasts about a week, but some toddlers can have chronic strep infections that last longer.
Your health-care provider will collect a culture from your toddler’s nose or throat to confirm that the infection is strep. Then it will be decided whether antibiotics will be needed to prevent more serious complications such as ear and sinus infections, or involvement of other organs such as the lungs, brain, or kidneys, or rheumatic fever. (Note: Strep throat is very rare in children under 2 years of age.)
Thrush
If your toddler’s tongue and cheeks stay coated in white patches that won’t wipe away, he may have thrush, a fungal problem. This yeast infection grows in moist places on the inside and on the skin, and it may also appear as red, irritated patches in the folds of your toddler’s skin, such as the neck, the armpits, and the thighs. Sometimes a cherry red diaper rash that doesn’t clear up easily can also be caused by yeast. Your health-care provider will suggest medication to treat it.
Urinary Tract Infection (UTI)
A urinary tract infection causes irritation of the lining of the bladder, urethra, ureters, or kidneys, just like the inside of the nose or the throat becomes irritated with a cold. The signs of a UTI may not be clear, since a toddler may not be able to describe how he is feeling. Sometimes symptoms include a high fever, irritability, and loss of appetite. And some children have a low-grade fever, nausea, and vomiting.
Urine may have an unusual smell, and your toddler may urinate more than usual. If he has a high temperature and appears sick for more than a day without signs of a runny nose or other obvious cause for discomfort, he or she may need to be checked for a bladder infection. If the kidney is infected, a child may complain of pain under the side of the rib cage, called the flank, or low back pain.
Crying or complaining that it hurts to urinate and producing only a few drops of urine at a time are other signs of urinary tract infection, or a child may have difficulty controlling the urine and may leak urine into clothing or bed sheets, and it could smell unusual or look cloudy or red.
If a urinary tract infection is suspected, your child’s urine will be collected. Toddlers who are not yet toilet trained may be fitted with a plastic collection bag over the genital area that is sealed with an adhesive strip. An older child may be asked to urinate into a container, or a small tube may be directly fed into the urethra to directly drain into a container, or a needle may be placed directly into the bladder through the skin of the lower abdomen.
Urinary tract infections are treated with antibiotics.
Whooping Cough (Pertussis)
Also known as pertussis, whooping cough is a highly contagious respiratory illness that used to kill thousands of people every year. But now, thanks to the DTaP vaccine, there are only a handful of deaths from the disease every year. Still, cases of pertussis seem to be on the rise, particularly among infants younger than 6 months who are not yet protected by immunizations, and in young adults whose childhood vaccines have begun to wear off.
If your toddler develops a spastic, honking cough, and possibly vomits after coughing, contact his health-care provider, who will probably prescribe antibiotics. Your toddler will be contagious until the course of the medication has been completed, which is about 5 days.
ACCIDENT-PROOFING YOUR TODDLER
Protecting your exploring toddler from his own curiosity is a full-time job! Your ever-moving child is driven by a powerful, innate urge to explore the world: to see, taste, and experience everything that attracts him.
Emergency Medical Restraint
If your child has been injured and needs treatment but isn’t able to cooperate, you may need to help medical personnel in restraining him so he can be examined or treated. Here’s how to hold your tot with your body to keep him still so he can be helped:
• Get into a sitting position. Sit in a chair or on the floor with your back against a wall.
• Place your child in your lap. Sit your child on your lap with his back to you.
• Hold his legs between yours. Cross your legs so that his legs are held still in between yours.
• Use one hand on his forehead. Gently press your child’s head toward your chest so you can talk softly to him in his ear.
• Hold him across his chest. Cross his chest with your other arm so that both of his arms are held in place.
• Unwind. Once your child has calmed down or the procedure has ended, start by slowly letting his legs go, followed by his arms and then his head.
When Your Toddler Should Stay Home from Child Care
Most child-care centers have their own rules about when kids have to stay home and when they can come back after illnesses, but here’s a quick reference guide to help you make the decision.
• Fever. Your toddler has a temperature according to the definition given by your toddler’s child-care provider.
• Breathing problems. Difficulty breathing, wheezing, or coughing.
• Diarrhea. Blood in stools not explainable by dietary change or medication.
• Vomiting. Two or more episodes in the previous 24 hours.
• Persistent abdominal pain. Complains of unusual belly pain that continues for more than 2 hours.
• Mouth sores. Outbreak on the lips, inside the mouth, or in the throat.
• Rash. Combined with a fever or overall sense of illness.
• Eye infection. Purulent conjunctivitis (“pinkeye”) with thick discharge from the eye, until after treatment has started.
Unfortunately, a toddler isn’t very discerning. He’ll try to open the bleach bottle, perch precariously on a second-story window ledge, and race unknowingly into traffic. He’ll pull any dog’s tail, drag down kitchen pots, and tug on electrical cords.
Many toddlers are raced to emergency rooms every year with serious injuries sustained from accidents in and around their homes and even from playgrounds designed for children. Most often, these accidents arise from toddlers just acting like toddlers.
What seems like simple exploration and play can turn tragic in only a matter of minutes when an adult is momentarily distracted by something else.
Hazards Inside Your Home
If you have a toddler, you’ve probably already discovered that all the decorative touches in the home, like figurines, ceramics, and glass objects, need to be put out of reach.
Pathways need to be as safe as possible to help reduce tripping. Electrical cords, throw rugs, and other “loose” things that could trip your toddler should be kept out of the way.
The truth is, during the toddler years, the most innocuous things can be potential dangers for a fearless and curious toddler. Low shelves can be climbed, appliance or floor-lamp cords could be pulled, and coffee tables can become stages of disaster.
Here’s a list of some potential hazards around the home and some easy solutions:
• Bureaus and shelves. Simple chests with drawers and open shelves don’t look dangerous, but when tots try to use them as steps for getting to the top, they can be downright deadly. Drawers can also drop out, crashing on small heads, hands, or feet. Too often television sets tumble from the tops of dressers, too.
Prevention: Fasten the chest and shelves in your child’s room to the wall using a special safety strap, or an L-shaped bracket found in hardware stores. Install stops at the backs of drawers so they can’t be pulled out. Move the television off the dresser and out of reach.
Protecting Your Toddler from Accidents
• Burns. Set the water heater’s temperature control to 120°F or less, and always check the water temperature carefully before allowing your toddler near the bath.
• Choking. Don’t let your toddler play with small objects, particularly coins, buttons, latex balloons, and marbles—anything with a diameter of less than an inch and a half. Avoid hot dogs, nuts, cheese cubes, and grapes—that could get caught in his throat.
• Drowning. Never leave your toddler alone near the bathtub, a bucket of water, a child’s wading pool, a swimming pool, or an open body of water, even for a short time. Never use a suctioned toddler bath seat.
• Falls. Use safety gates on all stairs. Keep your toddler from climbing on tables, sinks, and other high surfaces.
• Fires and Suffocation. Install smoke detectors, and test them periodically. Install a carbon monoxide detector if you have a flame-burning furnace, fireplace, or woodstove.
• Heatstroke. Protect your toddler from getting overheated in unshaded places and never leave him unattended in a car. Don’t bundle him up to help him “sweat out” a fever.
• Strangulation. Tie up cords from curtains, wall hangings, and blinds to keep them out of your toddler’s reach. Never suspend toys from a string tied across a crib or playpen. Use fitted sheets and tuck blankets below your toddler’s underarms.
• Vehicle accidents. Install and use an approved car seat appropriate for your toddler’s weight.
• Cribs and bunk beds. More babies and toddlers die from crib-and bunk bed–related accidents than from any other children’s product-related accidents. Hand-me-down cribs can be lethal when their slats are too wide and capture children’s heads and necks. Children fall from bunk beds or their heads get captured in bunk bed ladders or side railings.
Prevention: Don’t accept an old crib; instead, purchase a new, certified model. (You’ll spot the sticker on the frame.) Don’t buy a bunk bed, but if your children are already using one, keep your toddler on the bottom bed, carefully inspect for capturing gaps in head and foot boards and ladders, and don’t allow your kids to play on the beds.
• Detergents and cleaners. Toddlers aren’t discerning about what’s safe to put in their mouths and what’s not. Bleach, cleaners, and detergents—the types of bottles and boxes you store under your sink are dangerous! Dishwashing detergents can cause severe, disfiguring mouth and throat burns—most often when a tot scoops some out of the cup on the dishwasher door before the door is closed.
Prevention: Store toxic detergents and chemicals high out of toddler’s reach. Don’t have the dishwasher door open when your tot’s in the kitchen. Wipe down detergent spills and residues with paper towels and discard them immediately.
• Fires. Children from birth to 4 years old account for 65 percent of deaths in house fires. Things ignite on the stove, and faulty electrical wiring and appliances start fires. More commonly, smokers fall asleep with cigarettes in their hands, or children start fires when they play with lighters and matches.
Prevention: Install smoke alarms on all floors of your home. Have a fire evacuation plan in place, and rehearse it regularly, including teaching your young children how to call 911. Store a fold-up window ladder in your children’s closets, and mark your children’s rooms using stickers on their bedroom windows (ask your fire department). Make sure your address is easy to see from the street.
• Stairs. Crawling and newly walking toddlers are fascinated by staircases.
Prevention: Protect your toddler from falling by installing safety gates, which are usually constructed of wood, metal, molded plastic, or combinations of these materials. There are three basic types: those that attach to the wall with screws (hardware-mounted gates), those that cling to the wall using the suction of rubber gaskets (pressure-mounted gates), and expandable corrals. Hardware-mounted gates are considered the safest. Specialty gates help shield wide and unusual openings in homes, such as dining room entries or open stairs with iron railings on the side. Taller-than-normal gates are also available for pets that may work for toddlers who are climbers.
• Toys and toy chests. Toys send thousands of kids to emergency rooms every year. Most of the injured children are under 2 years old. Toy chests have figured in numerous deaths when they’ve fallen on children’s necks, cutting off their air supply.
Prevention: Buy quality age-appropriate toys and inspect them for sturdiness. Make sure there are no sharp corners and edges that could hurt if your child falls on them and check for pinch points. Look for small parts that could come loose, choke, or be swallowed, particularly for children under age 3.
Safety Gate Checklist
Here’s what to look for when you shop for a safety gate:
• Latches that are impossible for toddlers to work, but easy for older children and adults
• No finger-pinching hardware.
• Slats or narrow plastic mesh to make it hard for your toddler to get a foothold for climbing.
• Easy opening and closing that can be done with one hand.
• No tripping hazards, such as bars that go across the floor.
Once you get your safety gate installed, don’t allow anyone to step over it instead of opening and closing it properly.
• Vitamins and medications. “Childproof caps” on medicines aren’t childPROOF! They simply serve to slow children down several minutes before they get inside. Children can overdose on chewable vitamin pills if they manage to get into them. Ingesting too much iron is particularly dangerous. Acetaminophen (Tylenol, for example) can cause organ damage if a child accidentally eats the pills. Heart medicines, antidepressants—the types of medications that a child can easily access in purses and bedside tables—can be harmful and possibly fatal.
Prevention: Put medications and vitamin products in a box somewhere out of reach. (Store toothbrushing supplies—toothpaste, mouthwash—similarly.) If you keep medicines in your purse, store it out of reach. Measure liquid medications with extreme care under a bright light, and administer them only under your physician’s advice. And keep the national poison control center’s number handy (800-222-1222).
• Hair dryers, radios, and other electronics. People can be electrocuted, especially in older homes without circuit breakers, when hair dryers and radios fall into sinks and bathtubs. Kids love experimenting with electrical outlets because they’re usually at child’s-eye level. They get their small, damp fingers wedged between a plug and the outlet, or they stick pins, keys, or other metal objects in the outlet and get shocked.
Prevention: Unplug and store hair dryers and radios out of reach until you’re ready to use them. Install circuit breakers for bathroom outlets. Cover electrical outlets in the rest of the house with screw-on cases that snap shut to protect plugs from small hands. Find these at hardware and retail stores.
TIP
Small, plastic plug covers can be pried loose by a child and can choke.
Garage Hazards
The garage or basement may be a domain best forbidden to toddlers. Consider the following hazards, though, if your child follows you into the garage:
• Garage door. Children have been killed when they were captured and crushed after automatic garage doors slammed down on them.
Prevention: Test your automatic garage door to make certain it springs back open when it encounters any resistance, such as a brick or a carton. If your garage door doesn’t stop immediately and reverse, have the safety reverse repaired or replace the door.
• Paint thinners, gasoline, antifreeze, and other chemicals. Tots will play with caustic chemicals and even drink them.
Prevention: Keep chemicals in a locked cabinet and store them in their original containers (so you know accurately what is in each container). Post the number of the nearest poison control center near the kitchen phone. If your child does ingest a toxic chemical, don’t try to make him vomit unless you’re instructed to do so.
• Garage ladders and shelves. Toddlers love to climb and don’t understand that shelves and ladders will fall forward if they pull on them.
Prevention: Hang ladders up on hooks and bolt shelves to the wall.
• Tools. Toddlers like to imitate what their moms and dads do. They will pull down and handle drills, saws, and other dangerous tools, and may even succeed in turning them on.
Prevention: Put a safety gate on the door to your work area. Shorten electrical cords so they are out of reach, and unplug tools and store them safely out of reach when not in use. Keep tots away or restrained while you’re working.
Outdoor Hazards
• Vehicles. Children are at risk of being rolled over by vehicles backing out of the garage or driveway.
Prevention: Always check around your car before backing out, and have an alert installed in your car that sounds when the car is in reverse. Create a secure, fenced-in area for your child to play, rather than using the garage or driveway as a play area.
• Pools, tubs, and buckets. Small children can drown in only a couple of inches of water within a few minutes. Toddlers drown in bathtubs, wading pools, and water buckets.
Prevention: Protect an outdoor pool of any size with a fence and a gate that locks, preferably one that locks automatically. Drain all containers and store them upside down. If there’s an unprotected pool or body of water nearby, teach your tot about the dangers of water and have him wear a life vest outdoors.
• Lawnmowers. Toddlers have been horribly injured from falls and being run over by mowers, or hurt when the mowers threw up sticks and rocks. Curious tots have lost fingers and hands from reaching under the mower deck while it was idling and a parent’s back was turned.
Prevention: Remember that lawnmowers are not big, friendly ride-on toys. Keep your toddler safely inside while the lawn is being mowed.
• Dogs. More than 800,000 people visit emergency rooms each year for dog bites. Most victims are children, and the children usually know the dog that bites them.
Prevention: Teach your child proper “animal manners,” even with familiar animals, and warn him not to approach unfamiliar animals or to try to corner them. Get rid of a pet that snaps at your child, and insist that local fence and leash laws are enforced in your neighborhood.
• Plants. Many household plants and blossoming spring flowers can be toxic. Though most are not fatal if swallowed, they can burn the mouth as well as cause stomach pain.
Prevention: For an extensive list of poisonous plants, the Children’s Safety Association of Canada (www.safekid.org/plants.htm) offers a list of common plant dangers.
• Playgrounds. Although they appear to be great for meeting children’s play needs, most playgrounds have serious hazards, too. For example, children have sustained severe head injuries from falling from playground equipment onto non-cushioned, hard surfaces, such as asphalt and compacted earth. Even a headfirst fall from just 2 feet can cause a serious head injury. Children’s monkey bars and climbers result in falls and broken bones. Sliding boards strangle children when the hood strings from coats entangle in hardware. Toddlers are routinely struck by swings. Sandboxes are breeding grounds for parasites thriving in animal feces.
Prevention: Always supervise your kids at play. If the surface beneath climbing structures isn’t adequately cushioned, don’t allow your children to use the equipment. Avoid public sandboxes, and keep home sandboxes covered when not in use.
• Walkers and ride-on toys. Often parents make the mistake of buying a ride-on toy, tricycle, or beginner’s bicycle that’s too large in hopes that their child will grow into it. Toddlers’ ride-on toys don’t have brakes. They fall over when the front wheel is turned too far to one side, which only makes them more difficult to control. Children sustain injuries when bikes fall over or go out into the street.
Prevention: Before you buy a wheeled toy, make sure you have access to a safe riding place that isn’t near a driveway or road. Postpone buying a ride-on toy or trike until your toddler is at least 3 years old, and then be sure to teach him how to steer and stop. Always stay right with your child when he’s on a ride-on vehicle.
The Toddler-Safe Home
One study of childproofing products found that they were far from fail-safe. Cunning toddlers could figure out safety locks and other devices within a few minutes. Those findings underscore the fact that nothing can protect your toddler better than your own constant supervision.
Here’s a checklist of toddlerproofing items to consider:
• Safety gates (at top and bottom of staircases)
• Electrical outlet covers (on all electrical outlets)
• Stove knob covers (on front of stove)
• Fireplace guard (in front of fireplace)
• Corner guards (on coffee or end table corners)
• Double-sided rug tape (on throw rug)
• Cord shorteners (on kitchen appliances and drapery cords)
• Skid-proof tub mat (in bathtub)
• Lid lock (on toilet seat)
• Medicine cabinet lock (on medicine cabinet)
• Drawer and cabinet locks (on kitchen drawers, and on TV stand doors)
• Lowered mattress support (on crib)
• Shelf fasteners (L-shaped bracket on back of shelf)
TREATING COMMON TODDLER INJURIES
It’s almost inevitable that, at some point during your child’s toddler years, you’ll have a moment of total terror when he chokes, swallows or stuffs an object in his ear or nose, or falls and gets a nosebleed, cut, or worse.
Accidents, including falls and poisonings, are really common. Nearly one-fourth of all children suffer an injury severe enough to require medical attention. In fact, accidents are the leading cause of death of all people ages 1 to 21. And no matter how watchful and careful you are, your toddler can get hurt before you can intervene—even if you’re only a few feet away.
Abrasions
Prevention: Restrict unstable toddlers from playing on concrete, asphalt, or hard dirt surfaces.
Treatment: Rinse the area to remove all dirt, gravel, or sand; wash with soap and running water without rubbing. Dry thoroughly and apply an antibiotic ointment. Cover with an adhesive bandage or gauze pad on elbows and knees. Change dressing frequently until the wound begins to heal.
Get Help: If the wound covers a large surface, such as the back or abdomen, or if it is on the face, especially near the eye. When it’s embedded with dirt, stones, or gravel that are not easily removed (they may cause scarring). When there are signs of infection, such as warmth, redness, swelling, or puslike drainage.
Airway Obstruction
Prevention: Keep your toddler safe from ingesting small objects such as small toys (deflated balloons) or chunks of food (carrot coins, cheese chunks, hot dogs, meat sticks), and getting entangled in window treatment cords or hood ties. Have every adult in the family learn CPR.
Treatment: Try to clear the obstruction. Perform CPR (see www.heart.org) while someone calls 911.
Get Help: Call 911 and/or go to the emergency room for any kind of breathing problem.
Animal Bites
Prevention: Keep your curious toddler away from animals, and especially guard him when he is in others’ homes and yards.
Treatment: If the skin is broken, wash thoroughly with soap and running water and dab hydrogen peroxide in the wound. Cover the wound with sterile gauze or a bandage. Infection is a danger. Try to have the animal confined for rabies testing. A rabies vaccination may be needed.
Get Help: Any child with a bite wound should have medical treatment.
Cuts or Scrapes
Prevention: Remove square-cornered coffee tables and other sharp-edged or glass-topped tables from your living area. Don’t allow a newly walking toddler to play on gravel or asphalt surfaces.
Treatment: Wash your hands with soap and water, and then gently wash the toddler’s wound. Pat the area dry with a sterile gauze pad, using pressure to help stop the bleeding, if needed. Apply antibacterial ointment. Wash your hands again to get the grease from the ointment off your fingers, then cover the wound with a bandage. Newer, waterproof bandages work best. Change the bandage daily, inspecting for redness or pus, signs of infection.
Get Help: If your toddler’s wound is jagged, deep, or longer than 1 inch, or if it keeps bleeding for longer than 5 minutes. If your toddler has been bitten by an animal (or human); if the sore is contaminated with gravel or dirt; or if it’s a puncture wound from a nail or other rusty object, such as barbed wire.
Head Injuries or Concussion
Prevention: Don’t let your toddler climb on furniture. Use screw-mounted safety gates at the tops of staircases. Never leave your toddler to nap or allow rough play in an adult bed. Pad concrete surfaces at the bottom of staircases. Exercise caution with children’s climbing equipment, especially if the surface underneath isn’t well padded.
Treatment: Soothe the toddler, examine the injury for cuts. Monitor for signs of concussion (loss of consciousness, headache, dizziness, confusion, nausea, or vomiting).
Get Help: If the toddler loses consciousness at any time, has more than one bout of vomiting, or is unusually sluggish.
Insect Bites and Stings
Prevention: Avoid areas where bees, wasps, hornets, or yellow jackets congregate, or when you are doing yardwork or digging in the earth. (Don’t count on insect repellants, which can be toxic to toddlers and young children. Read the label.)
Treatment: Try to identify the insect. Most bite reactions are temporary and heal on their own. Remove the stinger from a bee with a scrape of your fingernail or a charge card. Aloe vera gel from the plant can be soothing for minor bites.
Get Help: Seek immediate medical attention if your child develops breathing problems or shows signs of anaphylactic shock (see Tip).
Mild Burns
Prevention: Set your water heater to 120°F or cooler. Don’t drink hot beverages near your toddler. Keep cups and bowls containing hot liquids and pots and appliances (irons, hair wands, coffee makers) and cords away from counter and table edges. When there is a hot oven, keep toddler out of the kitchen with a gate or play yard. Shield heaters, wood stoves, and fireplace openings.
Treatment: Run cool water over the burn as quickly as possible to cool down the area. Apply aloe vera gel or cream, but don’t put butter, ice, or other home remedies on the burn. They can actually make it worse. Your toddler’s health-care provider may recommend an antibiotic ointment applied several times a day to keep mild burns from becoming infected.
Get Help: For all serious burns, such as an electrical burn, a large burn over his body, or if he stops breathing after being burned. If the burn begins to blister, looks chalky, covers a large area of skin, or is on the toddler’s face, hands, feet, or genitals.
Snake Bites
Prevention: Keep your toddler away from wood and mulch piles, rocks or boulders, tall grasses, the edges of streams, and other areas where snakes have been reported.
Treatment: Try to identify the snake, but do not pursue it or try to capture it. Your child’s reaction, whether mild or severe, depends upon the snake and the amount of venom. Symptoms may include swelling at the wound site, shortness of breath, and shock. Don’t try to suck the venom, apply a tourniquet, or cut the wound, which may only cause more tissue damage or introduce infection.
Get Help: Always seek immediate medical attention for snake bites.
Splinters and Embedded Shards
Prevention: Keep shoes on your toddler’s feet if he is walking on rough wooden flooring or is outdoors. Don’t let him climb on woodpiles; keep wood furniture and windowsills sanded and stained. Clean up all glass splinters and safely dispose in a thick paper bag. Keep cacti well out of reach.
Treatment: Wash your hands and the splinter area with warm, soapy water. Use tweezers and pull out the splinter at the same angle it went in. Apply antibiotic ointment and bandage the area.
Get Help: If your child is in pain; you’re having trouble removing the splinter; for a deep puncture from a needle or toothpick; if the injury was caused by rusty metal, such as a nail or a fish hook with a barb; if it’s a pellet from a BB gun; if it’s clear plastic or glass that’s hard to remove; or if it’s an imbedded pencil lead that could cause a permanent mark under the skin. (Note: pencil lead is graphite, not lead, so it’s not toxic.)
Sunburn
Prevention: Stay out of the sun from midmorning until midafternoon, when the sun’s rays are the strongest. Stay in the shade or use an umbrella at the beach and swimming pool. Apply toddler-safe sunscreens (30 SPF and above) on exposed skin when you’re going to be outdoors for more than a few minutes.
Treatment: Apply aloe vera and/ or cool compresses of water and baking soda. Give plenty of fluids.
Get Help: Call your pediatrician if your toddler has a fever and/or blistered skin.
Ticks
Prevention: Inspect pets that go outdoors daily for ticks, and give them tick-repellent medications. Look for ticks on your child after walks, and dress him in long pants tucked into socks to help prevent ticks from jumping on his skin.
Treatment: Ticks usually burrow next to the scalp or in other warm places. Do not try to pull the tick off with your fingers. Grasp as close to the head as possible with a pair of tweezers. Pull slowly and firmly. Once the tick is removed, wash the wound with soap and water, then wipe it down with rubbing alcohol or hydrogen peroxide to disinfect it. Apply an antibiotic ointment and cover with an adhesive bandage.
Get Help: If the bite site becomes infected or develops a rash or red ring around it, which could signal Lyme disease.
EMERGENCY PLANNING
Tens of thousands of children are rushed to emergency rooms in the United States each year as the result of accidents and severe illnesses. Emergency rooms can be chaotic, crowded, and sometimes unhealthy places. They can also be downright frightening to vulnerable, highly emotional toddlers.
Here are some strategies for anticipating the unexpected:
• Research hospital options in advance. Investigate local hospitals and walk-in centers to weigh your options before your toddler ever needs emergency care. First, find out which hospitals are covered by your insurance and where your toddler’s doctor has admitting privileges, since that hospital will have the quickest access to your toddler’s medical records, which could expedite his care. Also ask your doctor for the names of preferred emergency rooms. (Some emergency rooms are better equipped than others for handing pediatric emergencies, such as burns, falls, and fractures.)
Contact the hospitals to ask questions about the emergency services offered and how admissions work. (When emergency rooms are crowded, toddlers who show the symptoms of the flu or who are deemed to have less-than-life-threatening injuries may be diverted to a different treatment area in the hospital to make room for more serious cases.) Consider checking on your hospital’s score from the Joint Commission on Accreditation of Healthcare Organizations (www.jcaho.org).
• Keep a “loaded” cell phone in the car. Keep a cell phone and car charger in the car at all times so you will always have a device for summoning help. Load the phone with your pediatrician’s number, the numbers of key relatives, customer service for your health insurance, and the hospital’s emergency number so you’ll have rapid access to whomever you need. Phone your toddler’s pediatrician, who can give the hospital the heads up that you’re on the way and any details about your toddler’s condition, and possibly meet you there. Knowing that your doctor is on the way may improve the efficiency of your care and your state of mind.
• Notarize a “consent to treat” form. Make sure that whoever has responsibility for your child’s care has a signed form from you that allows your toddler to be treated in an emergency. You can find a printable version for treating children by doing an Internet search for a “consent to treat form for minors.”
• Create an emergency information packet. Each person in your family should have a packet. Your toddler’s packet should includes his full name, sex, a photocopy of the front and back of his health insurance card, a recent picture, address, telephone number, date of birth, weight, height, blood type, doctor name and contact info, a short list of relatives to contact, a list of any medications he is taking (including vitamins), and a detailed description of any preexisting conditions he has.
Fold the information into a self-sealing, transparent sandwich bag, mark it with “IN CASE OF EMERGENCY” and the child’s name, and duct tape it onto the inside of your refrigerator door where you (or emergency personnel) can grab it in a hurry. That will save you having to divert your attention from your toddler when rescue squad members require critical information before they transport your toddler to the hospital.
• Plan backup support. Rehearse with your partner, your next of kin, and your neighbor(s) about what you will do if you have a family emergency and you need someone to be with you at the hospital, or someone to care for your child(ren) should something unexpected happen.
• Get insurance pre-approval. If there’s time, contact your health insurance company on the way to the hospital or shortly after you arrive, or ask one of your support people to do that for you. Health insurance companies may require notification when a patient is receiving emergency medical care. Informing them may help to smooth out problems with billing and paperwork later.
• Expect to call 911. When your toddler’s emergency is serious, call for help rather than trying to drive your toddler to the hospital yourself. He will have professional care and attention all the way to the hospital, and he will also get a more rapid response once he arrives there. Ambulance services are expensive, but the few minutes that it takes the rescue squad to arrive may make a huge difference in the speed and quality of intervention your toddler receives.
• Be assertive. You are your toddler’s primary source for security, safety, and protection, so it’s important to be firm and insistent when it comes to going along with your toddler, rather than allowing the emergency staff to whisk him away without you. Explain that you will remain quiet, but as your toddler’s guardian, you must insist that you stay with him.
• Maintain records. Keep a record of the staff members who treat your child in the emergency room in case your insurer needs further proof that your toddler’s visit was warranted. Calling the insurer may help to reverse denied coverage.
When your toddler is discharged, ask for a copy of his X-rays and lab results. It’s much easier to take them at the time than it is to ask the hospital for them weeks later. Having them in hand will help when you go for a follow-up appointment with your toddler’s doctor.
TIP
If any toy can fit through a cardboard toilet paper tube, it can pose a choking hazard.
TIP
Among children of all ages, balloons are the most common cause of toy-related choking death.
Life-Threatening Emergencies
These are the leading causes of children’s deaths from trauma (in order of frequency):
• Motor-vehicle accidents
• Drowning
• Fires/burns
• Suffocation and choking
• Firearms
• Falls
• Poisonings
An emergency is termed “life-threatening” when a toddler’s critical body functions, such as breathing or circulation, start to fail. When this happens, your toddler might be in danger of dying, which requires an immediate response, even before you summon help. Some life-threatening accidents include: poisoning, drowning, electric shock, an obstructed airway, serious burns, and heavy bleeding from a wound.
An accident is “life-endangering” when a toddler is unconscious and his body is going into shock. The term shock refers to the way a body reacts when the blood supply to vital organs, including the brain, heart, liver, and kidneys, has been threatened. It can be caused by significant loss of blood or bodily fluids, but it can also be the result of an allergic reaction to drugs or insect bites.
A toddler in shock will have rapidly falling blood pressure, and will seem to get progressively worse. Hypovolemic shock occurs when there is a rapid loss of blood or other body fluids. It can happen after any serious injury, and a burn, or result from a bleeding wound. It can also be caused by severe dehydration when a toddler isn’t getting enough fluids or is ill and vomits a lot, has prolonged diarrhea, or is suffering from heat exhaustion.
If your toddler is going into shock, he will appear pale, have cold and clammy skin, a rapid but weak pulse, and shallow breathing, and will seem extremely irritable and uncomfortable. Alternatively, he could be extremely sluggish and hard to wake up. Your toddler may also have nausea and vomiting and appear extremely thirsty.
Emergency CPR
Basic life support is designed to keep your child alive and breathing until help comes. It is very rare for a toddler to need emergency resuscitation, but it’s important to take a course in life support or CPR (cardiopulmonary resuscitation) through your local American Red Cross chapter or the American Heart Association.
In the meantime, here are some basic instructions to rehearse:
1. Ascertain whether your toddler is breathing or moving. Mucus, blood, vomit, a solid piece of food or candy, or the tongue can easily obstruct a toddler’s small airways, causing him to become unconscious.
2. Shout for help.
3. Have a second person call 911.
4. If there’s been an accident, try to see how seriously your toddler is injured and whether he is unconscious. He might not respond to gentle motions or to tapping his feet.
5. If you suspect that your toddler has a head or neck injury, take special care not to move his body, which could make the spinal cord vulnerable.
6. Look, listen, and feel your toddler’s chest. If there is no one to help you, and your toddler is obviously not breathing or turning blue, perform CPR (see www.heart.org) for 1 minute before calling for help. Remember, a toddler’s lungs are tiny, and so are his air passages.
Severe Bleeding
A 25-pound toddler’s body holds only about a quart of blood. In a serious bleeding situation, your toddler’s body and brain can be seriously compromised unless immediate action is taken.
Here are the steps to take if your toddler has been seriously injured and is bleeding:
• Enlist help. Get someone else to make the emergency call while you stay with your toddler. If emergency help is delayed, have someone else drive you to the ER while you stay close to the toddler.
• Stop the bleeding. Use a piece of cloth or a shirt to apply steady pressure to the wound to stop the flow of blood. Put more cloth over the old pad when it becomes soaked, rather than changing dressings, since that might dislodge early clotting.
• Raise the wounded limb. If you’re sure that your toddler’s spine has not been injured, raise the arm or leg above the heart to help slow down the loss of blood. (Your toddler’s limbs may be limp and numb if there has been a spinal injury.)
• Await instruction. Once your child arrives at the hospital, he may require stitches (sutures) or surgery to repair the wound. You will be given instructions about what to do for your child once the bleeding has been stemmed and the wound dressed.
Product Recalls
Federal agencies have the power to recall toddler products that pose dangers, and literally millions of toddler products have been banned, pulled off shelves, or undergone “corrective actions” that retrofit the unsafe parts of a product.
• In spite of federal actions, product-related accidents and injuries continue to happen, killing hundreds of babies and toddlers every year, and rushing over 10,000 children to emergency rooms for treatment. New products introduce new dangers into the marketplace; old and worn out products fail; and greedy importers ignore federal regulations by selling shoddy goods that fail federal standards.
• Keep on top of recalls and report toddler product problems by frequently accessing these federal sites:
U.S. Consumer Product Safety Commission (CPSC)
Bethesda, MD 20814
800-638-2772
Regulates the safety of most children’s products, clothing, bedding, and toys. (Car seat recalls generally come from the National Highway Traffic Safety Commission.)
National Highway Traffic Safety Administration (NHTSA)
Washington, DC 20590
888-327-4236
Regulates and recalls children’s car seats and rates their installation instructions.
Food and Drug Administration (FDA)
Silver Spring, MD 20993
888-INFO-FDA (888-463-6332)
Regulates formula and baby food, medicines, and cosmetics, such as bathing products and diaper rash creams.
TIP
Safety gates send thousands of children and adults to emergency rooms when they fall in attempts to step over closed gates.
SPECIAL SECTION: Autism and Other Disabilities
A lot of parents of toddlers are concerned about autism, and rightfully so. According to the Centers for Disease Control, autism rates have spiked in recent years, with 1 out of every 150 children currently being diagnosed with it, with numbers expected to continue rising. As yet, no one knows for sure yet why so many more toddlers and children are being diagnosed with it, but there are suggestions that it might be genetic.
Autism is sometimes called Pervasive Developmental Disorder (PDD), which is an umbrella term used when a more specific diagnosis is unknown, such as Asperger’s syndrome, Childhood Disintegrative Disorder, or Rett syndrome. How autism presents itself in a child is as unique as every child is, although some tendencies are more common than others, such as having difficulties with communication and social interaction, and the appearance of repetitive behaviors.
It is now believed that some children have a strong genetic predisposition to autism that may be set off by something that happens in their environment, but researchers don’t know yet what the triggers are. One early warning signal for autism that is now being studied is an unusual head growth pattern.
Researchers have observed that babies who were later diagnosed as having autism may be born with smaller-than-average head circumferences, but the great majority of those children experienced a period of unusually rapid head growth between ages 1 and 14 months. It’s important to note, though, that this head growth pattern was also found in 6 percent of normally developing children. It is thought that identifying these growth patterns early in life could be useful in getting an earlier diagnosis, when interventions can have the most impact.
What causes autism in children simply isn’t clear yet. There are a number of theories for its causes, from mercury (thimerosal) exposure in vaccines or exposure to other environmental toxins, genetic mutations, or an interaction between inborn vulnerability and environmental factors.
In 1998, British researchers raised a furor with a controversial report suggesting a link between the rising number of children being diagnosed with autism and preservatives in the measles, mumps, and rubella (MMR) vaccine. But early in 2004, ten of the thirteen original authors of the study retracted the statements in the paper, saying that their data was not strong enough to support that conclusion. Before-and-after studies have compared the rates of autism and appear to refute the idea that thimerosal is implicated in autism. Not only did cases of autism not go down after the removal of this preservative from vaccines, but they actually rose substantially.1
Meanwhile geneticists are getting closer to pinning down certain gene anomalies that may be associated with autism. Late in 2009, Dutch geneticists have reported specific genetic anomalies that appeared to be connected to a set of physical characteristics associated with autism. Autistic children with the genetic disorder were found to have prominent foreheads, large ears, a smooth philtrum (between the nose and lips), a pointed chin, wide mouth, different degrees of mental impairment, and brain structure abnormalities.2
Since 2004, the National Institutes of Health has been helping underwrite the Autism Cohort Study in Denmark. The study is closely following 110,000 children from pregnancy onward in an attempt to identify factors related to autism, such as diet, vaccinations, birth weight, and head circumference, and exposure to toxins, including mercury.
Meanwhile, developmental experts are working hard to identify signs of autism earlier to help improve children’s long-term outcomes. Since 2007, the American Academy of Pediatrics has recommended that all patients between the ages of 18 months and 24 months be screened for autism.
SOME EARLY SYMPTOMS OF AUTISM
No two children with autism are alike. One child may have no language but be very affectionate. Another with Asperger’s syndrome, a high-functioning autism spectrum disorder, might have a large vocabulary but not be able to use it appropriately. He may be able to label a flamingo, but not be able to answer simple questions, such as, “What did you eat for breakfast?”
Child development experts are beginning to develop a clearer understanding of the early signs of autism spectrum disorders that appear during the first year of life. Most normally developing babies enjoy sharing an object or event with another person by glancing back and forth between the two. An older baby will use gestures and speech to try to engage another person as he learns about the enjoyment of sharing experiences. He will smile in recognition and give other responses to the smiles and voices of his parents or other familiar caregivers.
At about 8 months of age, a neurotypical baby will follow his parent’s gaze and look in the same direction, but a baby with autism may fail to engage in that way. Between 10 months and 12 months of age, babies showing symptoms of autism may fail to follow a parent’s finger, no matter how hard the parent tries to engage his attention.
By 12 months to 14 months, a non-autistic child will begin pointing at things himself, first to ask for something he wants that’s out of his reach, and later to draw his parents’ attention to something he sees that he wants to share. Pointing may be accompanied by expressive sounds, such as “uh” or actual words. A child with autism may try rudimentary pointing by opening and closing his hand while raising it to request an object, or try to lead his parent to the object, but without the back-and-forth glancing that’s part of nonverbal communication.
A child with autism may hear well but could appear to have selective hearing. He may be acutely aware of certain sounds but be unresponsive to human voices. He may also obsess on small details, and he may repetitively rock himself, or mouth, twirl, bang, and manipulate objects in unusual or ritualistic ways. Some toddlers may also have mild speech delays and an inability to articulate themselves. Others might not exhibit these behaviors.
Approximately 25 percent to 30 percent of children with autism have age-appropriate language skills but then stop speaking, usually between the ages of 15 months and 24 months, or they gain other skills only to lose them. They may suddenly or gradually stop gesturing, waving, pointing, seeking eye contact, or responding to praise, and they may show unusual development patterns or an unusually intense interest in objects or other nonsocial things.
Not all mainstream doctors and health-care professionals know how to properly diagnose early signs of autism. If you believe your child may have early signs of autism, First Signs (www.firstsigns.org) has a large collection of videos comparing neurotypical toddlers with those who have autism that can help you figure out where your tot stands. If you see warning signs, it’s important to seek diagnosis and intervention while his behavior patterns can still be helped.
Startling Autism Facts
• At some point in their lives, 1 in 63 U.S. children (160 per 10,000) will receive an autism-related diagnosis.
• Out of every 160 children diagnosed with autism, 60 of them (37.5 percent) will somehow go on to lose that diagnosis.
• With boys, 34.6 percent originally diagnosed with an autism spectrum disorder may not continue to have the diagnosis later, while 44.5 percent of girls lose their diagnosis.3
HELP FOR TODDLERS
“Disability” is a big umbrella term covering anything that keeps your child from being able to interact with the world in the same ways most kids of the same age do. When it comes to intervening with toddlers who have problems, sooner is a lot better than later. And getting an accurate diagnosis of a problem early on will help you get hooked up with programs and resources that can help.
Having an accurate diagnosis will also help to protect your toddler from being labeled with negative and wrong pseudo-diagnoses for problems, such as being “aggressive,” “difficult,” “lazy,” “clumsy,” “poorly socialized,” “a behavior problem,” “zoned out,” or “not really trying” by misinformed child-care workers and teachers. Those hurtful labels tend to stick from year to year and may delay your child getting the skilled and productive interventions he deserves (and is legally entitled to) to help him live to his full potential.
Federal Early Intervention
The federal Individuals with Disabilities Education Act of 2004 (IDEA) is a law that requires that children under the age of 6 who have or are at risk of developing school-related problems be screened for potential disabilities. Part C of IDEA provides a federal mandate for services for young children from birth through age 3 who are at risk of developmental delays or disabilities. (Part B of IDEA provides the federal mandate for students with special needs, age 3 years to 21 years.)
Early Intervention (EI) is a term used to describe specific agencies, programs, services, and resources provided for children birth to 5 and their families. Each state provides its own Early Intervention system of services under IDEA, usually run by the state Department of Education or the state Department of Health. A baby, toddler, or child can be referred for screening by his parents, physicians, educators, or others who are concerned about the child.
The National Early Childhood Technical Assistance Center (NECTAC) can help you navigate the maze of Early Intervention services. The National Dissemination Center for Children with Disabilities (www.nichcy.org/states.htm) offers state-by-state directories for the agencies offering services to children (and adults), and the Centers for Disease Control and Prevention has links to information for families for children with disabilities (www.cdc.gov/actearly).
The EI program for babies and toddlers provides access to therapeutic services designed to help each unique child reach his full potential. Getting your toddler evaluated is free of charge to you, and in most states, rather easy to arrange. Everything usually gets started with a simple telephone call.
Each state has different rules and regulations about which children qualify for special services. The National Dissemination Center for Children with Disabilities (www.nichcy.org) is a good place to start your information search for IDEA, since it can help you find the lead agency in charge of Early Intervention in your particular state.
How Early Intervention Works
State services are typically offered by county, and your journey may differ, depending upon what state you live in. It usually begins with a telephone intake interview with your state’s Early Intervention office. An Initial Service Coordinator (ISC) will talk with you about your family history, your child’s milestones, and your concerns about your toddler. You will be asked about your toddler’s typical behaviors and will have a chance to fully air your concerns.
Your toddler’s assessments and other appointments are likely to be carried out in your own home. Team members will bring along props, including age-appropriate toys, that will help the team assess how your child navigates his home, how he responds to others, and how he responds to new situations. You will also be informally interviewed about his behavior.
Even though the EI representatives assigned to work with you and your child are not doctors and cannot make official medical diagnoses, they are well trained in evaluating babies and toddlers, having worked with hundreds of them. What they can do is tell you if your child’s challenges qualify him for special services.
The goal of each EI agency is to pull together a “dream team” for your child to ensure that he receives the services that he needs to reach his maximum potential to function in the world and at school.
If you are only concerned about a speech delay, then a speech evaluation will be set up for you. If you have concerns about multiple areas of your child’s functioning, such as social abilities, communication, and physical development, then the evaluation will be with a physical therapist, occupational therapist, and/or a special education therapist.
Once your EI team has a clearer idea of your child’s situation and needs, an Individualized Family Service Plan (IFSP) will be created. Your input will be included in the plan tailored to your toddler’s unique needs. The team may also offer you feedback about your family dynamics as it affects your toddler, and team members work with you to set up realistic goals for your child over time.
Formal Disability Definitions
If your toddler has been diagnosed with autism or another disability, he may be eligible for special education and related services under IDEA if he meets very specific criteria that show his educational performance could be adversely affected due to his disability. There are fourteen specific terms used to define a child with a disability, which will determine whether a child can receive special care at no charge.
Here are the formal definitions of disabilities that will open the gate for your toddler getting special intervention:
Autism. A developmental disability significantly affecting verbal and nonverbal communication and social interaction, generally evident before age 3 that adversely affects a child’s educational performance. Other characteristics often associated with autism are engaging in repetitive activities and stereotyped movements, resistance to environmental change or change in daily routines, and unusual responses to sensory experiences. (The term autism does not apply if the child’s educational performance is adversely affected primarily because the child has an emotional disturbance.)
Deaf-Blindness. A child has both hearing and visual impairments together that cause such severe communication and other developmental and educational needs that he cannot be accommodated in special education programs solely for children with deafness or children with blindness.
Deafness. A hearing impairment so severe that a child is impaired in processing linguistic information through hearing, with or without amplification, that adversely affects a child’s educational performance.
Developmental Delay. Children from birth to age 3 (under IDEA Part C) and children from ages 3 through 9 (under IDEA Part B), as defined by each state, means a delay in one or more of the following areas: physical development; cognitive development; communication; social or emotional development; or adaptive (behavioral) development.
Emotional Disturbance. Children who exhibit one or more of the following characteristics over a long period of time and to a marked degree that adversely affects a child’s educational performance: (a) An inability to learn that cannot be explained by intellectual, sensory, or health factors. (b) An inability to build or maintain satisfactory interpersonal relationships with peers and teachers. (c) Inappropriate types of behavior or feelings under normal circumstances. (d) A general pervasive mood of unhappiness or depression. (e) A tendency to develop physical symptoms or fears associated with personal or school problems.
The term includes schizophrenia. The term does not apply to children who are socially maladjusted, unless it is determined that they have an emotional disturbance.
Hearing Impairment. An impairment in hearing, whether permanent or fluctuating, that adversely affects a child’s educational performance but is not included under the definition of deafness.
Mental Retardation (Intellectual Disability). Significantly below average general intellectual functioning, existing at the same time with deficits in adaptive behavior and manifested during the developmental period, that adversely affects a child’s educational performance.
Multiple Disabilities. Combined, multiple impairments (such as mental retardation–blindness, mental retardation–orthopedic impairment, etc.), which cause such severe educational needs that they cannot be accommodated in a special education program solely for one of the impairments. (Does not include deaf-blindness, which is in a different category.)
Orthopedic Impairment. A severe orthopedic impairment that adversely affects a child’s educational performance. The term includes impairments caused by a congenital anomaly, those caused by disease (e.g., poliomyelitis, bone tuberculosis), and those from other causes (e.g., cerebral palsy, amputations, and fractures or burns that cause contractures).
Other Health Impairment. Having limited strength, vitality, or alertness, including a heightened alertness to environmental stimuli, that affects the educational environment, which: (a) is due to chronic or acute health problems such as asthma, attention deficit disorder or attention deficit hyperactivity disorder, diabetes, epilepsy, a heart condition, hemophilia, lead poisoning, leukemia, nephritis, rheumatic fever, sickle cell anemia, or Tourette’s syndrome; and (b) adversely affects a child’s educational performance.
Specific Learning Disability. A disorder in one or more of the basic psychological processes involved in understanding or in using language, spoken or written, that may manifest itself in the imperfect ability to listen, think, speak, read, write, spell, or to do mathematical calculations. The term includes such conditions as perceptual disabilities, brain injury, minimal brain dysfunction, dyslexia, and developmental aphasia. The term does not include learning problems that are primarily the result of visual, hearing, or motor disabilities; of mental retardation; of emotional disturbance; or of environmental, cultural, or economic disadvantage.
Speech or Language Impairment. A communication disorder such as stuttering, impaired articulation, a language impairment, or a voice impairment that adversely affects a child’s educational performance.
Traumatic Brain Injury. An acquired injury to the brain caused by an external physical force, resulting in total or partial functional disability or psychosocial impairment, or both, that adversely affects a child’s educational performance. The term applies to open or closed head injuries resulting in impairments in one or more areas, such as cognition; language; memory; attention; reasoning; abstract thinking; judgment; problem-solving; sensory, perceptual, and motor abilities; psychosocial behavior; physical functions; information processing; and speech. (The term does not apply to brain injuries that are congenital or degenerative, or to brain injuries induced by birth trauma.)
Visual Impairment Including Blindness. An impairment in vision that, even with correction, adversely affects a child’s educational performance. The term includes both partial sight and blindness.
Medicaid Disability Waiver Program
The Medicaid Disability Waiver program is another federal program that provides services to children with intellectual and developmental disabilities. It is designed to provide services in homes and neighborhoods of children who might otherwise require care in a Medicaid-funded facility. It may also supply respite for caregivers of these children. Other state programs may help to provide comprehensive health care for families who make too much to be eligible for Medicaid, but not enough to afford health insurance. Programs may provide for physician or clinic services, surgery, drugs, dental care, occupational and physical therapy, and additional services for children with mental or physical conditions.
Gaining access to these services is not a quick process by any means, but once you are in, you can be eligible for respite care, which enables you to have a qualified and trained person come to your house and watch your child to give you time off, or you may be eligible to receive respite reimbursement, which means you can get reimbursed for part of what you pay your babysitter or qualified person to help you with your child.
NEXT STEPS
You will be given guidance about a variety of activities you can pursue with your child; you may also receive parenting resources that you can access in your community.
EI specialists will guide you about what to do next. If your child’s problems are thought to be serious enough to warrant formal interventions, it will likely be recommended that you make an appointment for more evaluation by a developmental specialist, such as developmental pediatrician, a pediatric neurologist, or other specialist (see descriptions of these professions). Of course, your toddler’s pediatrician is another health-care provider who can supply you with formal referrals to experts.
As you begin your services, you will be assigned a Family Service Coordinator who will help guide you through EI and help you address any issues that may surface. You will get the green light for services for 6 months, and then another meeting will be held to see how your toddler is doing and what services should be continued or discontinued.
Ask your EI Family Service Coordinator about special preschool groups or developmental play groups in your area. These groups can include toddlers who are on the autism spectrum or have other special needs, and benefit from being in a specialized toddler class where more aides are available to provide one-on-one assistance in encouraging peer interaction (circle time, play time, snack time). Whether the class is a “mommy and me” type class or not, you are sure to meet other moms and dads who are going through what you are going through.
Getting the Diagnosis Confirmed
Some parents feel that EI doesn’t afford them the amount of hours of professional help that their toddlers need. For example, if your toddler is a preemie with a speech delay, but shows no other signs of a speech disorder or any symptoms for autism, he may not qualify for speech therapy, or he may qualify for only an hour of speech therapy per week. To you, an hour per week barely touches the surface, while 5 hours per week would be phenomenal and make definite changes in your child’s maladaptive speech patterns.
It’s in your child’s benefit to get a second opinion from a developmental pediatrician or pediatric neurologist, both of whom are experts in children’s development. The findings may help your child access a higher level of services than in the original plan.
The American Academy of Pediatrics has information on developmental pediatricians, pediatric neurologists, and dozens of other subspecialties. Visit www.aap.org and click on the “Find a Pediatrician” link on the homepage for the Pediatric Referral Service.
Your pediatrician can give you a referral, but you may have to pay for the appointment out of your own pocket. Fortunately, many health insurance policies will cover a visit to a specialist if your child’s pediatrician deems it necessary. Since these specialists are rare and in high demand, it may take months to get the first appointment. If you’re not covered by insurance, your Family Service Coordinator may be able to offer suggestions on which specialist to choose.
We suggest making the appointment almost as soon as you receive your child’s first diagnosis and that you ask to be called if there is a cancellation when a family can’t make an appointment. If you have the opportunity to get in, give a spontaneous “Yes!”
Meeting Your Team
The speed with which you receive EI services varies from state to state, but typically programs start at least 30 days after your initial EI evaluation. If your services have started by the time you meet a specialist, your toddler could benefit from additional hours after receiving an official diagnosis.
If you are able stay home with your toddler or schedule home lessons around your work schedule, it will take both you and your toddler time to get used to the routine of having visitors come. After the first month, your family and your child will get accustomed to it, and you’ll look forward to seeing your child’s progress and breakthroughs, and you won’t even worry if your house isn’t “visitor ready.” Don’t worry about how clean your floor is or if your child is still wearing his pajamas when they knock on your door at 11 a.m.
Your toddler’s therapists, his therapist task force, will always arrive equipped with a bagful of preferred toys.
Depending on how your toddler responds to therapy, you may sit in on lessons or step away or out of the room if your presence is distracting to him. Over time, your child’s therapists may start to feel like family.
If you feel that your toddler’s service provider is falling short of your expectations, you have the right to request a different therapist in your area. Keep an open dialogue with your Family Service Coordinator about your likes and dislikes.
Experts and Their Specialties
If you can afford it, you may want to consider hiring your own specialists and therapists in addition to what EI can offer. Specialists often can work together to apply their expertise to deciding what your toddler needs. Here is a brief description of what different service providers do:
Profession |
Specialization |
Pediatrician |
Diagnoses physical and developmental problems, diseases, structural defects, refers to specialists. |
|
Family Physician |
Diagnoses physical and developmental problems, diseases, structural defects, refers to specialists. |
Psychiatrist |
Diagnoses psychological problems, chemical imbalances, attention deficit disorder (ADD) or attention deficit hyperactivity disorder (ADHD), autism, pervasive developmental disorders. Performs intelligence assessments. |
Pediatric Neurologist |
Deals with seizure activity, abnormal brain activity, brain injury. |
|
Optometrist/ Opthalmologist |
Diagnoses vision problems, cross eyes, nearsightedness, farsightedness, astigmatism, binocular, and other vision problems. |
Audiologist |
Assesses hearing loss, auditory processing, receptive language problems. |
Speech Language Pathologist (SLP) or Speech Therapist (ST) |
Assesses and treats speaking problems, language delay, and swallowing problems. |
|
Pediatric Occupational Therapist (OT) |
Assesses and treats sensory processing disorders, problems with spatial relationships, visual discrimination, coordination, and social skills. |
|
Pediatric Physical Therapist (PT) |
Assesses and rehabilitates children with fine and gross motor impairments due to developmental delays or physical problems, such as cerebral palsy, spina bifida, and torticollis. |
Developmental Psychologist |
Assesses and provides therapy for children with emotional and behavioral disorders. Evaluates the extent of developmental disabilities, such as language delays. |
Developmental Pediatrician |
A board-certified pediatrician with special training in diagnosing and treating of children with developmental and behavioral disorders, such as autism spectrum disorders. Provides recommendations and referrals to other treatment options. |
Special Education Instructor |
Provides one-on-one play therapy and learning experiences to enhance children’s cognitive skills. |
Your Toddler’s First Appointment
Your toddler’s appointment with a specialist, such as one of those described above, is likely to run anywhere from 1 to 3 hours. Typically, the specialist will want to observe your toddler being his natural self. He will carefully observe how your toddler plays with toys, how he interacts with and responds to others, and how your toddler reacts to being in a strange setting.
You will also be given time to discuss your concerns and to solicit the pediatrician’s opinion about what kind of therapies would work best for your toddler. Typical questions that parents ask have to do with what comes next, such as: “Which schools/programs in our area would be the right fit for our child?” “What are your opinions on specific treatments?”
The specialist will prepare a formal report, and may even scribble his findings and his proposal about what to next on a prescription pad and hand them over to you. With this tiny piece of paper you’ll have proof to give your EI official or school district that shows that your child needs help now, and that he needs to be assigned a slot for a special education class or other toddler programs available in your area.
You wouldn’t be human or a real parent if your heart didn’t ache or grieve if your worst fears are confirmed. But the good news is that a child who has an “official” diagnosis for developmental delays has an opportunity to receive Early Intervention therapies, which are key to helping your toddler reach his full potential.
STRATEGIES FOR PARENTS OF DISABLED TODDLERS
If your toddler is diagnosed with any of these impairments, and you would like to seek special intervention to help him, here’s how to proceed:
• Research. Learn all you can about your child’s condition and what kinds of doctors, therapists, medicine, support, and supplies he’s likely to need.
• Keep a journal with dates. Write down the names and contact information for all referrals, appointment dates, notes on what you’ve been told, immunizations and questions after appointments to research or ask the next time around. Don’t forget to also jot down your feelings and reactions. That will help you keep perspective and may be useful for helping other parents who seek your advice.
• Find another “go-to” parent. Raising a toddler with special needs can be a roller-coaster ride on some days. One way to make it through is by having a go-to mom to share advice, to give you the inside scoop on a doctor, or just to share a good laugh.
• Make parent-to-parent connections. Nonprofit organizations, informal parenting groups, societies, associations, or even online parenting groups can provide much needed social and comic relief. Contact charities in your area that support your toddler’s disability for volunteer opportunities or that sponsor charity walks you can participate in.
• Scope out good places. Get to know which restaurants and other public places are the most accommodating to your toddler’s needs, and which inspire meltdowns. Get to know your toddler’s preferences: Maybe he is more comfortable at fast-food joints or he seems calmer in rowdy sports-themed restaurants or diners, and go with what works for the two of you.
Emotional Effects of Your Child’s Diagnosis
Even though you may have waited for months for that fateful appointment with a specialist, finally being given your toddler’s diagnosis can come as a relief (now you know what’s wrong), but also a devastation, and perhaps information overload, which can lead to panic or depression.
Keep in mind that no matter how expert or prominent a specialist is, he or she doesn’t have a crystal ball. No human can truly predict what a child will be doing when he is 16, or when he grows into an adult, especially considering all the new research and treatments that are still emerging and could make a big difference down the road.
Once you find the best interventions for your child, things will start to feel less threatening and more balanced. You will be able to access support from specialists, your family, other parents, or your faith, and eventually you will come to realize that your love for your child hasn’t changed.
Sharing “the News” with Others
There’s no need to feel pressured to let your inner circle know the official news until you’ve had a chance to get used to it yourself. True friends will understand that you have a lot on your mind, and they will accept your promise to reconnect again once you’ve had time to wrap your mind around everything that’s going on.
Once you decide to break “the news” to loved ones, you’re likely to be bombarded with lots of questions. People will want to know what all that means and what you’re doing about it. There will always be people—even friends and family—who say the wrong things to try to cheer you up, or who try to offer their own suggestions, things you have already tried or wouldn’t want to try.
Sometimes people are prompted to share their war stories about their own children or others they’ve heard about. Then again, they may also deliver stories that bring a glint of hope: “My friend’s son was diagnosed with autism as a toddler, and now he is doing great!” or “They said our daughter would have motor problems, but now she dances and plays tennis!” Probably, both super downs and super ups delivered by others need to be taken with a big grain of salt.
It can be a lonely feeling to realize that most advice givers can’t fully grasp what it’s like to be in your shoes or to shoulder the responsibility you do for caring for your toddler, unless they have gone through that experience themselves. It bears repeating that the people who love you and your child the most will still be there for you, no matter what, and their feelings won’t change simply because your child has a diagnosis.
If you get sincere offers of support from family and friends, by all means accept their help. If they truly want to be helpful, hand them a to-do list. Here are some examples: Check out books from the library; do research on the Internet; take a sibling out for play date; babysit. Don’t think you’re selfish to ask family and friends to give you some time off simply to rest and restore yourself after the all the stress you’ve been through. Your toddler will survive, and you’ll return better able to cope with everything on your platter.
The Importance of Keeping Records
There will be lots of paper trails to keep up with when it comes to having your child diagnosed and treated. To begin with, keep photocopies of all applications for services.
You have a legal right to all of your child’s medical records, including doctors’ and therapists’ notes and findings. Sometimes you have to press for these, but insist that all lab and evaluators’ written reports be sent in duplicate to you and your child’s primary care physician.
Sometimes offices are hesitant or negligent about releasing them, and they will probably require you to sign a formal release form with the names and addresses where records are to be sent. Then, it may require more than one telephone call or by direct visit to get all of the paperwork in hand.
This documentation will be invaluable for your research into your child’s problems, for seeking second opinions, and for asking advice from your child’s physician. Create a file (or a designate a file drawer or special box) to store all of your child’s records, including immunizations and treatments, brochures and information sheets, and printouts from your Internet searches and other research you’ve uncovered that could apply to your child’s diagnosis.
Helping Siblings Understand
It may be natural for siblings to wonder out loud about their baby sibling. Teach them that he’ll be able to love them and share in the family fun no matter what his capabilities and skills. Many times, older siblings will enjoy taking part in Early Intervention lessons, and take pride in being the assistant teacher.
Look into extracurricular programs at special needs schools in your area, or connect with a society. Sometimes schools will have special groups set up where other siblings of children with special needs can socialize and discuss things they are going through. There may be things they may feel more comfortable talking about with other kids.
Siblings can become little brother or sister’s best advocate, but they can also secretly or not-so-secretly want more attention. They may also start asking you questions about their sibling with special needs. “Will Johnny ever get married?” “Why can’t he walk yet like I can?” “Why can’t he speak to me?” “Why does he act like that?” “Why can’t we go to the circus just because Johnny doesn’t want to go?” These are familiar questions from older siblings. It’s important to talk with siblings about how life is different right now for their brother or sister, and it’s also important to keep reassuring them of your equal love for them.
By communicating honestly and openly with siblings, you may find yourself becoming more open to discussing your child’s diagnosis with others and sharing with them what you are learning as you go along.