

This chapter looks at procedures and problems that are particular to women’s organs and the female body. It covers some of the conditions that affect large numbers of women—conditions for which it is sometimes difficult to get reliable women-centered information. Much is still unknown about many of these conditions, though new research findings emerge regularly.
These conditions are organized by anatomy. Some problems, of course, will involve more than one area of the body. The chapter focuses on benign (noncancerous) diseases or problems and on cancer prevention and diagnosis. It deals less with cancer treatments, since they tend to change quickly.
Other chapters in this book cover many topics related to medical concerns. In particular, see Chapter 2, “Intro to Sexual Health” for information on preventive care for sexual and reproductive health and what to expect in a gynecological exam, and Chapter 23, “Navigating the Health Care System” for information on how to find good care, how to work collaboratively with a health care provider, and where to find trustworthy and up-to-date health information.
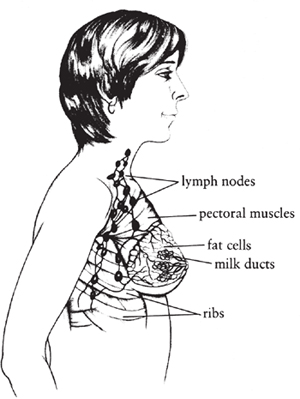
© Christine Bondante
A breast, showing the structure of milk ducts, lymph nodes, and fat cells.
Our breasts are dynamic organs. They change considerably during our lifetime in response to aging and to variations in our body’s hormone production. Understanding these changes can help reassure us when we think something is going wrong.
The breasts respond to estrogen and progesterone during each menstrual cycle, with growth and fluid retention that may be barely noticeable for some women but painful for others. The individual differences in breasts, along with the changes caused by age and menstrual cycles, can produce needless anxiety. We may worry that every change or pain is a symptom of cancer, when in fact most conditions causing change, lumps, or pain are benign.
Small cysts (a lobule or duct with fluid inside) may form, but they are usually smaller than a pea. Benign (noncancerous) tumors, such as fibroadenomas, may form during the teens and twenties and grow large enough to feel like smooth, mostly round, rubbery marbles that can be moved back and forth in place.
As we mature, small cysts may fill up further with fluid, sometimes causing tenderness and growing to sizes that can be felt with the fingers. By our fifties, dense glandular tissue and stroma begin to decrease (a process called involution), and fatty tissue increases. During perimenopause, hormone levels begin to fluctuate, and our usual cycles may become irregular. Effects of hormone changes on the breasts may include increased pain and lumpiness, which might be worrisome if we are looking for signs of breast cancer. Cancer rarely forms within cysts, but we may feel anxious while awaiting proof that a cyst is not cancer.
Some women’s breasts remain lumpy after menopause. Most benign lumps are caused by hormone stimulation, so if you are taking hormones after menopause, the breasts will continue to feel as they used to. Cysts rarely form after menopause, so if a new lump does form, it’s a good idea to have your health care provider examine it. Breast pain in the postmenopausal years may be coming from the chest wall, arthritis of the spine, or, only rarely, cancer.
There are several kinds of breast lumps. Cysts are fluid-filled sacs that develop from dilated lobules or ducts, most commonly during our forties or fifties. They can be identified by ultrasound or by removing the fluid and making sure no lump remains. Simple cysts—those that are just fluid, for example—don’t have to be removed unless they are causing pain or are so big that you can’t feel the surrounding breast tissue. A breast ultrasound is the best way to be sure a cyst is simple.
Treatment involves numbing the skin with a local anesthetic, inserting a thin needle into the cyst, and drawing the fluid into a syringe—a process called aspiration. The fluid may look gray and cloudy, dark and oily, or clear yellow or green. If a lump remains after aspiration, or if the fluid looks dark and bloody, you’ll need to have the area biopsied (tissue will be removed and examined under a microscope for further diagnosis). Cysts may refill with fluid after aspiration. If the same cyst continues to refill, removal may be recommended.
Fibroadenomas are benign growths that form mostly during our teens and twenties; some that form early may last throughout life. They may develop in one or both breasts. A fibroadenoma that’s getting larger is usually removed surgically. These growths sometimes shrink at menopause, as hormone levels decrease. Fibroadenomas are rarely associated with cancer, although some breast cancers can feel like fibroadenomas. The younger you are, the more likely it is that you have a fibroadenoma and not a cancer. Often a mammogram can confirm that the lump is a fibroadenoma, but the only way to be certain is by doing a biopsy and looking at the tissue under a microscope.
Pseudolumps are areas of dense normal breast tissue. They develop in many women during the premenopausal years. To make sure there is no cancer, these areas should be evaluated with good breast imaging and follow-up breast exams.
Cancer in the breast usually feels firm and hard. It often does not have clear edges but blends into the surrounding breast tissue. Breast cancers are usually about 1 centimeter (half an inch) in size before you can feel them; in women with firmer, lumpier breasts, they must be even larger to be felt.
First of all, don’t panic! More than 80 percent of all breast lumps are not cancer, especially in women under forty. Lumps in our breasts big enough to feel may be cysts, benign tumors such as fibroadenomas, pseudolumps, or cancers. It is impossible to tell the difference with physical examination alone. A lump that gets smaller over time is unlikely to be cancer. A lump that remains the same size or gets bigger could be cancer, so it should be medically evaluated.
Many women feel anxiety and fear upon finding a lump and immediately think it’s cancer. Our reactions may vary from wanting to go to the doctor immediately to being immobilized by fear. Finding a lump requires taking some decisive actions for yourself and your health. Tell someone you love about your concerns, so you can get some support and not have to go through the next steps alone. Then, contact your health care provider. Tell the appointment person or nurse that you have found a new breast lump and ask to be seen promptly.
Your clinician will do a physical examination of your breasts and determine whether further evaluation is necessary. She or he may suggest following the lump for one or two months, schedule you for diagnostic breast imaging (mammogram or ultrasound), and/or refer you to a breast specialist (usually a surgeon). If more information is needed, a biopsy may be recommended, since only a tissue sample determines for sure whether a lump is cancerous or benign.
This can be a very stressful time. Even though it’s likely that a breast lump is benign, statistics don’t always calm our fears. It helps to speak frankly with your health care provider about your concerns and to have the support of friends and/or family. It is also important to have confidence in your health care provider. If you are not comfortable with his or her recommendations, particularly a “wait and see” approach, be sure to say so. Getting a second opinion may be a good idea in this situation.
Breast discharge, itching on the areola, breast pain, and a breast infection are some of the other benign conditions of the breast that women experience. Nipple discharge, especially if it is bloody or coming from just one breast, should always be evaluated because it can be associated with cancer. Consult your health care provider for any persistent and troubling symptoms.
Mammography is the primary means of screening women at average risk for breast cancer. It utilizes a low dose of radiation to identify malignant tumors, especially those not easily felt by hand. A mammogram can also further investigate breast lumps that have already been identified, as well as other symptoms. Mammography involves X-ray radiation passing through the breast, producing an image on film or on a digital recording plate.
From 1975 to about 1990, the age-adjusted mortality rates from invasive breast cancer increased. In about 1990, they began to fall. By 2007, mortality had fallen by about one-third compared with its peak in 1989 and by 28 percent compared with 1975.1 It is not clear how much of the decline in mortality is due to screening mammography. (For a discussion of routine mammogram screening for all women over age forty).
Digital images can be enlarged and the contrast adjusted, enabling radiologists to concentrate on suspicious areas. This improves their ability to detect tumors in dense breast tissue. Digital images can also be stored and transmitted electronically, making it easier to consult with experts at a distance. For women under age fifty, women who are pre -or perimenopausal, and women who have dense breasts, digital mammography may work better, but for most women over age fifty, the use of digital mammography does not seem to catch cancers earlier or improve outcomes.
Ultrasound imaging—also called sonography—may be used to evaluate abnormalities that appear on regular mammograms. This technique excels in distinguishing solids from liquids, so it’s useful for differentiating solid tumors from fluid-filled cysts, which are benign. Ultrasound can also be used to guide needle biopsies. Ultrasound works by creating an image from reflected high-frequency sound waves emitted by a device called a transducer, a microphone that helps magnify the sound. Ultrasound is not useful as a screening tool by itself.
Recently, two medical devices have been developed to address the problem of missed tumors following mammography in women with dense breasts, a condition present in about one-third of women having mammograms today. One of these automated whole-breast ultrasound devices has been shown in a large, well-designed study to significantly improve cancer detection compared with mammography alone.2 This technique is not yet widely available.
MRI is quite effective in detecting invasive breast cancer, but it also can falsely identify benign lesions as malignant. It is not a substitute for regular mammography, nor is it for screening of the general population. Some recommend it for screening women at very high risk for breast cancer. MRI uses a powerful magnetic field and radio frequency pulses that are processed by a computer to create images of organs and tissues. It does not use ionizing radiation (X-rays) but does require an intravenous contrast injection.
PEM is used in addition to mammography to identify small invasive cancers and ductal carcinoma in situ (DCIS)—cancer that is confined to the milk ducts. PEM is not yet widely available and may not be covered by insurance. It uses gamma rays to detect “hot spots” of rapidly growing cells, and a computer analyzes the image to determine the size, shape, and location of the mass. The efficacy of PEM is still under study.
Like PEM, BSGI is used along with mammography. It is not widely available and needs more research to determine how well it works. It may not be covered by insurance. BSGI employs a radioactive tracer to identify cancer cells.
Thermography is used to assist in the diagnosis of breast cancer, but it produces too many false-positive and false-negative results to be used alone as a screening tool. It records the temperature of different areas of the body by measuring infrared radiation. Malignant tissue generally has a higher temperature than normal tissue because of its richer blood supply and higher metabolic rate.
In the future, as less invasive and more effective approaches are sought for early diagnosis and treatment of breast cancer, newer imaging technologies that look at breast cancer at the cellular level may become more widely used if there is clear evidence of their effectiveness as screening tools. Currently, BSGI and PEM involve fairly high doses of radiation and are therefore not appropriate for routine breast cancer screening.
All experts agree that mammograms can find breast cancers when they are small, are more curable, and need less treatment. But there is disagreement among experts over how many are found or missed, how many are successfully treated when found, how many don’t need treatment at all, when to begin a regular mammogram schedule, and when to end it.
For women between age forty and forty-nine, there is wide disagreement about screening mammograms.
The United States Preventive Services Task Force (USPSTF), a highly respected expert group, issued new guidelines in November 2009 recommending that women in this age group discuss with their clinicians when to start screening and whether to begin screening at age forty after considering the benefits and risks and discussing personal preferences.
In doing so, the USPSTF retracted its previous guideline for this age group, which recommended routine (that is, automatic) screening every one to two years starting at age forty.
The American Cancer Society (ACS) and the American College of Radiology (ACR), however, both continue to recommend routine screening every year starting at age forty for all women.
There is agreement that mammography reduces death from breast cancer, even in women between the ages of forty and forty-nine. The USPSTF agreed that screening in this age group was responsible for at least a 15 percent decrease in mortality. So why the different recommendations?
The USPSTF used a rigorous method of evaluating mammography studies. It relied almost exclusively on prospective randomized trials comparing death rates from breast cancer in those randomized for screening against those randomized for observation only. Since the benefits of screening mammography have been widely acknowledged, only one randomized trial started during the last twenty years (because randomizing would have to assign some women to “no mammography,” which most researchers would consider unethical). Critics of the USPSTF position assert that the weight of the USPSTF review is based on radiology studies that are out of date, but other experts dismiss this criticism.
In addition, different expert groups give different weight to the factors against and for routinely screening forty- to forty-nine-year-old women.
Factors against routine screening starting at age forty: Breast cancer is much less common in this group than in older women; the number of false-positive tests (in which the mammogram suggests a woman has cancer, but a biopsy shows no cancer) is higher for younger women; and starting mammograms at forty would mean having exams every two years for an average of thirty-four years. Over a lifetime, a woman’s chances of needing a biopsy to prove she didn’t have breast cancer might be as high as 50 percent.
Factors for routine screening in women starting at age forty: Cancers that are found in this age group tend to be more aggressive than those found in older women, and screening done every year, instead of every two years, may catch more of these aggressive cancers. While women may have to endure more biopsies, or anxiety with false-positive diagnoses, not getting screened can also produce anxiety.
It may be helpful to consider the comment of Dr. Ned Calogne, who chaired the USPSTF: “If I take 1,000 women age 40, over their lifetimes, 30 of them will die from breast cancer if we do no screening. If I screen every one of those women beginning at age 50 until she’s 74, we reduce the deaths from 30 to 23. And if I reach down and screen them in their forties, I can increase that by one additional life saved—at best.”3
Most experts agree that if a woman between the ages of forty and forty-nine is identified as being at high risk, she should be regularly screened (see “What Are the Risk Factors Associated with Getting Breast Cancer?”
All experts agree that women age fifty to seventy-four should be screened regularly.
Some experts say women in this group should be screened every year; others say every one or two years.
The USPSTF proposes screening every two years. It argues that the additional lives saved by screening yearly are not enough to justify an annual procedure. Screening at two-year intervals would preserve 81 percent of breast cancer mortality reduction seen with screening at one-year intervals.
The American Cancer Society and the American College of Radiology recommend screening every year. They argue that the 19 percent increase in breast cancer deaths that comes with screening only every two years is not acceptable.
For women over seventy-four, there is disagreement.
The USPSTF makes no recommendations, because there are no randomized studies for this age group. The ACS and the ACR recommend annual screening as long as a woman has a life expectancy of five to seven years (most experts believe that the benefits of mammography compared with no mammography show up only after five years). They also note that it is easier to find breast cancer in older breasts and breast cancer risk increases with age. They also believe that the risks of screening are small.
The decision to screen or not screen in this age group, all agree, should rest on a discussion with one’s clinician/primary care provider. Whether it’s better to be screened every year or every two years is disputed. The incidence of breast cancer continues to increase into one’s eighties, although most of these breast cancers are not as aggressive as those found in younger women.
Clearly, mammography can find curable breast cancers, even though there are disagreements about when to start routine screening. Weighing your personal preferences and concerns along with the recommendations of experts can be confusing and very stressful, especially if you have personal risk factors or friends or relatives who have faced breast cancer. Nevertheless, informed deliberation will help you make the best decision for you.
A woman living in the United States has a one in nine lifetime risk of developing breast cancer. While any woman can develop breast cancer, the chances increase with age. Breast cancer in men is extremely rare but does occur (about 1 in 100 individuals diagnosed with the disease will be male). Most breast cancer occurs in women with no family history or known genetic risk. In fact, 70 to 80 percent of women with breast cancer have none of the known risk factors besides age. Only 5 to 10 percent of cases are in women with high-risk mutations of the BRCA1 and BRCA2 genes. About 255,000 women per year are diagnosed with breast cancer, both noninvasive ductal carcinoma in situ (approximately 62,000) and invasive breast cancers (approximately 192,000). The National Cancer Institute estimates that there are more than 2.5 million women living with breast cancer in the United States.
Breast cancer incidence is highest in the United States and in western and northern Europe. The lowest rates are in Asia and Africa, although incidence rates have been rising in areas such as Japan, Singapore, and urban China. These regions are moving toward more Western economies and patterns of reproductive behavior. Although the influence of dietary patterns is complicated, higher caloric intake at younger ages can lead to earlier onset of menstruation, which is a risk for breast cancer.
PROBABILITY OF DEVELOPING INVASIVE BREAST CANCER AMONG WOMEN5* |
||||||||
CURRENT AGE IN YEARS** |
|
RISK PER 1,000 WOMEN *** |
||||||
|
|
in 10 years |
|
in 20 years |
|
in 30 years |
|
Lifetime |
30 |
|
4 |
|
17 |
|
41 |
|
123 |
40 |
|
14 |
|
37 |
|
68 |
|
120 |
50 |
|
24 |
|
56 |
|
86 |
|
109 |
60 |
|
34 |
|
67 |
|
86 |
|
91 |
70 |
|
37 |
|
58 |
|
— |
|
65 |
* Based on an analysis of data from the Surveillance, Epidemiology and End Results registry for 2005–2007. | ||||||||
** Women who are free from invasive breast cancer at their current age. | ||||||||
*** Number of women in 1,000 who would develop invasive breast cancer in the next period of time. |
||||||||
The established risk factors for breast cancer do not account for all of the breast cancer cases. Despite the billions of dollars spent on breast cancer research, we have much to learn about why some women develop breast cancer and others don’t.
Starting in the 1970s, the incidence of breast cancer rose at alarming rates. Much of this long-term increase is believed to be due to delayed childbearing and having few children. Obesity is also a factor. And as more women have screening mammograms, more cases are found; that accounts for some of the increase.
Between 2002 and 2003 there was a decrease in the incidence of breast cancer, particularly among women ages fifty to sixty-nine. This drop in the number of breast cancer cases coincides with the release of research findings from the Women’s Health Initiative study (nhlbi.nih.gov/whi), which prompted many women to discontinue their use of hormone therapy.
Many people believe that the industrial processes and environmental damage that began during or after World War II play a major role in rising rates of breast cancer in Western countries. Research into environmental connections to breast cancer is the focus of organizations and foundations such as Silent Spring Institute (silent spring.org). Such research is difficult and frustrating because it entails identifying geographic breast cancer patterns in a population that is very mobile and hard to track.
Reproductive hormones play a role in the development of breast cancer because they can affect cell growth as well as promote the growth of an existing cancer. As women age, the effect of estrogen on breast tissue decreases. As we go through perimenopause and become postmenopausal, breast tissue changes to fat.
On mammograms, young normal breast tissue appears thick and white, but as the breast ages and turns to fat, it shows up dark on breast imaging. In part, this accounts for why breast cancers, which appear white on a mammogram, are more easily detectible in women after fifty, who are usually approaching completion of perimenopause. As Dr. Susan Love has commented, “Looking for cancer on a young woman’s mammogram [is] like looking for a polar bear in the snow.”6 Having denser breasts—with more glandular tissue in relation to fatty tissue—is a risk factor for the development of breast cancer. More research is being done to try to figure out why dense breast tissue is a risk factor and what, if anything, can be done for women with dense breasts.
The Women’s Health Initiative (WHI) was the first randomized controlled study looking at women and hormone therapy (HT, formerly called hormone replacement therapy or HRT). It began in 1991 with the first results released in 2002 (see nhlbi.nih.gov/whi for more information). The major objectives of the WHI were to study cancer, osteoporosis, and heart disease among older women. The trial was stopped early in 2002 when researchers found that women who had taken a particular estrogen and progestin had a greater incidence of several diseases compared with women receiving a placebo.
For healthy women who took estrogen plus progestin, the research demonstrated an increased risk of heart attack, stroke, blood clots, and breast cancer. This same group also had a decreased risk of colorectal cancer and fewer fractures. After 2002, hormone therapy use declined in the United States and around the world. Many believe that this decline explains in large part the decline in incidence of breast cancer shortly afterward.
In 2006, the National Cancer Institute reported on the Women’s Intervention Nutrition Study (WINS), which included women who had undergone hysterectomy and were given estrogen without progestin. (Women with a uterus who take hormones usually include a form of progesterone along with the estrogen, to reduce the chances that estrogen “unopposed” will lead to endometrial cancer.) Results from this study comparing women receiving estrogen with women receiving a placebo found that there was no difference in the risk of heart attack, but there was an increased risk of stroke and blood clots among the estrogen group. The effect on the risk of developing breast cancer was uncertain. (Estrogen made no difference in risk for colorectal cancer, but there was a reduced risk of bone fractures in women who took it.) The Million Women Study conducted in the United Kingdom7 did show a clear increase in breast cancer among women on estrogen alone.
Follow-up studies have shown that the increased risk for breast cancer with hormone therapy—including both estrogen and progestin—diminishes within five years of discontinuing hormones. Recent studies report that the breast cancers developing in women taking both estrogen and progestin are more aggressive and more lethal than doctors previously thought.
What all of this means for women is that long-term use of hormones (greater than five years) increases breast cancer risk.8 Each woman needs to discuss hormone use with her health care provider to determine what makes the most sense for her own situation. Some women consider using bioidentical hormones as an alternative to conventional hormones. Bioidentical hormones are chemically identical to the hormones produced by your body; there are many FDA-approved hormones that fit the definition of bioidentical, and their long-term safety has yet to be established. (See Chapter 20, “Perimenopause and Menopause,” for more discussion.)
Breast cancer develops when changes occur in genes in breast cells. In that sense, all breast cancer has a genetic element. But genetic does not mean inherited. Only an estimated 5 to 10 percent of breast cancer cases result from an inherited genetic predisposition. In other words, more than 90 percent of all breast cancer cases result from factors that are not inherited and, in many cases, are unknown.
We all inherit half our genes from our mother and half from our father. There are some genes that dramatically increase the risk of breast cancer. Two of them are called BRCA1 and BRCA2 gene mutations. Blood tests have been developed—and are now aggressively marketed commercially—that can identify these mutations. A positive test result (having one of these mutations) does not mean that an individual will definitely develop breast cancer. Nor does a negative test mean that a woman won’t develop breast cancer; it means only that her lifetime risk is the same as that of most other women in the industrialized world. But for those individuals who have an inherited BRCA1 or BRCA2 mutation, there is a significantly increased lifetime risk of developing breast, pancreatic, and ovarian cancers. BRCA1 carriers have an average cumulative breast cancer risk (up to age seventy) of 65 percent, compared with 45 percent for BRCA2 carriers.
It’s important to consider the family history of breast and ovarian cancer from both your mother’s and your father’s sides of the family. Genetic testing should be considered only in limited circumstances.10 It is usually recommended that individuals with breast and/or ovarian cancer undergo testing for BRCA mutations because if the results are negative, their children would not need to be tested. Individuals without breast and/or ovarian cancer who are most likely to benefit from genetic testing are those of us who believe—because of a family history of two or more first-degree relatives (such as a mother or sister) with breast and/or ovarian cancer—that we may be mutation carriers and, if so, who want to take some action to try to reduce our cancer risk.
All genetic testing should be accompanied by written, informed consent; complete information about benefits and risks; and professional counseling about options. This is best done through one of the many cancer risk assessment programs located throughout the country. A comprehensive list of programs can be found on the websites of the National Society of Genetic Counselors (nsgc.org) and American Board of Genetic Counseling (abgc.net).
If you have BRCA gene mutations, several possible strategies can reduce your risk of breast and ovarian cancer. These include taking drugs such as tamoxifen or raloxifene; prophylactic—that is, preventive—mastectomy; and having the fallopian tubes and ovaries removed. Because the science behind these strategies is changing so rapidly, and because these are major decisions with important risks to consider, it’s best to consult experts, pursue the latest information about these options, and consider their possible effects on your life.
When you find out you have cancer, it’s normal to feel shock, disbelief, fear, and anger. This psychological trauma comes exactly when you need to focus all your energy on learning about your treatment options. The most important thing to remember is that a diagnosis of breast cancer is usually not a medical emergency. This means that you have time to seek out opinions about the best way to proceed and to choose physicians with whom you feel comfortable. You have the right to have all of your questions answered and to understand your treatment options fully before deciding what to do.
Doing whatever your doctor suggests may be appealing at a time when you need to be taken care of, but it does not always result in the best care. Although most doctors have good intentions, they tend to offer only the treatment they know best. It’s wise to get a second opinion before committing yourself to a plan, even if you feel confident with your first doctor. This is especially true if your physician has not fully explained your surgical treatment options.
Lumpectomy and radiation therapy (also called breast-conserving therapy) when compared with mastectomy (removal of the entire breast) has the same survival rates; that is, the same percentage of women who don’t die of breast cancer. If your surgeon is not explaining this to you, then you should definitely seek a second opinion. While in some circumstances a mastectomy may be recommended and be better for keeping the cancer from spreading, you should fully understand why your doctor is recommending it. Some physicians may be slow to accept new therapies until there’s more experience with them; some may be unwilling or unable to discuss all available treatments. Some states, including Massachusetts, California, and Minnesota, have laws that require patients to be informed of all medical options.
Even though you may have a good relationship with your health care provider, if you live in a small town you should strongly consider going to the nearest large city with a research-oriented or university hospital. These institutions generally keep up with ongoing studies, use a team approach, and may be more flexible about treatment. A local women’s health center, the National Cancer Institute (cancer.gov), or the American College of Surgeons (facs.org) can help you find appropriate cancer centers and specialists. Cancer centers usually have special breast cancer centers. The advantage of getting a second opinion or of being treated at a breast cancer center is that a team of specialists—medical, surgical, and radiation oncologists—will be involved with your care from the beginning. Private oncologists may not practice in teams, making coordination of your care more difficult. Certain breast cancer centers offer more treatment choices, including clinical trials testing new therapies.
If you meet income guidelines and were diagnosed under a federally funded screening program for uninsured or underinsured women, Medicaid will cover treatment for breast cancer. Some communities have local support groups for women with cancer, where you may be able to get help with transportation to medical appointments and with child care, as well as encouragement from other women who have had or are having similar experiences.
Surgery is usually recommended within six to eight weeks of the biopsy, so it’s okay to take time to adjust, ask questions, and find out about your options. In some cases, chemotherapy is used over several weeks or months to reduce the size of the tumor prior to surgery (this is called neoadjuvant chemotherapy).
When you are trying to decide about treatment, the most pressing question is likely to be “How can I maximize my chances of disease-free survival?” But you will also want to understand the long-term effects of cancer therapy. To decide on the best treatment, you also need to know the size of the tumor, whether or not there is cancer in the lymph nodes, the hormone status of your tumor (called ER/PR), and what the HER-2/neu* status of your tumor is. These are specific for each woman’s cancer, and these tumor markers can help individualize and optimize your therapy. Most of this information is available after the biopsy, and it is used to recommend systemic therapies (endocrine/hormone therapy or chemotherapy) and/or radiation. Usually the medical oncologist is the one who discusses appropriate treatment options based on the biopsy or surgery results.
It is important to learn about all the available options. The entire field of breast cancer medicine is changing rapidly. Old, established theories and treatments are being questioned, while newer techniques have not been used long enough to be completely evaluated. The 2010 edition of Dr. Susan Love’s Breast Book and her website (dslrf.org) contain up-to-date and credible information on breast cancer treatment as well as important current research. The National Breast Cancer Coalition website (breastcancer deadline2020.org) takes an activist approach. Getting balanced information on the pros and cons of various treatment options will help with knowing what questions to ask and how best to proceed with your care.
Cancers are classified in stages. These stages provide some information about prognosis for an individual, as well as a mechanism for comparison of treatments and outcomes in different populations. Staging for breast cancer is based on three elements: tumor size or extent (T); which lymph nodes, if any, contain cancerous cells (N); and metastases—cancer detected by X-rays or scans in other parts of the body (M).
When cancer is first diagnosed, the clinical stage is identified by physical exam and some testing for metastatic spread. After surgery, lab analysis of the breast tissue and lymph nodes removed will determine the pathologic stage. The stage is important because doctors usually base their recommendations for treatment on how well other women with cancer at the same stage and similar history have responded to various treatments. The TNM stage is then grouped into five categories or overall stages.
BREAST CANCER STAGES* |
|||
STAGE |
SIZE |
AXILLARY LYMPH NODES |
COMMENT |
0 |
DCIS |
Negative |
Noninvasive |
I |
Less than 2 cm |
Negative |
|
IIA |
2–5 cm Less than 5 cm |
Negative Positive |
|
IIB |
More than 5 cm |
Negative |
|
IIIA |
Less than 5 cm More than 5 cm |
Positive and matted Positive |
|
IIIB |
Any size and spread to chest wall, skin |
Negative or positive |
|
IIIC |
Any size |
Spread to other nodes |
|
IV |
Any size |
|
Spread beyond breast and nodes to other organs of the body |
* For more information on breast cancer stages, see cancer.gov/cancertopics/wyntk/breast/page 7. |
|||
Breast cancers are classified by whether they are noninvasive (or in situ) or invasive breast cancer. In situ tumors are made up of cells that when seen under a microscope look like but do not behave like cancer. They remain encapsulated within their usual environment—inside the duct or the lobule. There are no blood vessels or lymphatic vessels there, so these cells have no access to other parts of the body. In contrast, invasive (also known as infiltrating) breast cancer goes through the walls of the ducts and lobules, invading the surrounding fatty/fibrous portion of the breast tissue where blood vessels and lymphatic vessels lie.
LCIS is not cancer now—it’s considered a risk factor for the development of breast cancer someday. Because LCIS is not preinvasive, there’s no need to remove it unless it is found on a core biopsy. Because a core biopsy is a limited sample, the recommendation in this case is to have more tissue removed and examined to be sure there is no neighboring in situ or invasive cancer.
In studies of women with LCIS, 20 to 40 percent developed cancer (mostly invasive ductal carcinomas) over twenty years or more. Such cancers may occur anywhere within either breast, not only in the area where the biopsy was done.
DCIS is a noninvasive cancer. Many scientists believe DCIS will become invasive cancer if enough time passes. But it may never become an invasive cancer in your lifetime. More women get this diagnosis now because improvements in technology have made it possible to find more and more DCIS with screening mammograms. Because DCIS can become an invasive cancer, treatment is usually recommended. There is unfortunately no way yet to tell which women really need treatment.
If you receive this diagnosis, get a second pathology opinion—preferably with a breast pathologist—before agreeing to any treatment. If possible get an opinion from a breast cancer center where you could meet with a multidisciplinary team of breast specialists.
Women diagnosed with DCIS have approximately a 1 percent risk of developing metastatic disease and 96 to 98 percent are alive ten years after diagnosis.12 Treatment aims to remove the area of DCIS and reduce the chance of a local recurrence within the breast. For years the customary treatment for DCIS was mastectomy. Early studies comparing a more breast-conserving approach with lumpectomy combined with radiation therapy showed similar rates for local recurrence of disease and no difference in survival. Now women have a choice regarding treatment options. For breast-conserving therapy, a procedure similar to lumpectomy, called wide excision or partial mastectomy, is performed with the goal of clearing the margins of DCIS (meaning no DCIS is found at the edges of the tissue removed). For some women, even after several excisions, DCIS remains at the margins and mastectomy is recommended.
There is a lack of consensus in the medical community regarding whether radiation therapy is needed for all women diagnosed with DCIS. Studies have not yet provided strong evidence suggesting that adding radiation therapy is more or less effective than wide excision alone.
In invasive or infiltrating breast cancer, the breast cancer cells have moved outside the ducts or lobules into the surrounding tissue. Because the tumor cells can spread to other parts of the body, through either the blood or the lymph system, treatment usually requires both local surgical and possibly radiation therapy, along with systemic treatments, such as hormone-locking medicines and/or chemotherapy.
An unusual but very aggressive form of breast cancer is known as inflammatory breast cancer (IBC). The first symptom is usually redness of the skin, along with an orange peel appearance of the skin called peau d’orange (which is why it is called inflammatory). Usually an antibiotic is prescribed to see if the redness is caused by an infection. If it doesn’t get better, a biopsy of the breast and the skin will diagnose the cancer. The usual treatment is chemotherapy first, followed by mastectomy and radiation.
As researchers discover more about the biology of breast cancer, treatment theories change. Breast cancer, in general, grows slowly. Most breast cancers have been growing for six to ten years before they are large enough to be seen on a mammogram or felt during an exam. During this time, cancer cells could be spreading (metastasizing), through blood vessels and the lymphatic system, to other places within the body. This doesn’t always happen—not all breast cancer cells survive outside the breast. Also, the size of the cancer doesn’t always correspond to how aggressive it is; the type of cells in it will affect what happens, too. However, there is no sure cure. A classic saying among breast cancer survivors is that you don’t know you’re cured until you die from something else. Women who have been successfully treated “so far” refer to being NED, or having No Evidence of Disease.
Current treatments for breast cancer are either local (therapy to the breast) or systemic (therapy to the whole body). Surgery and radiation are local therapies; chemotherapy, endocrine/hormone therapy, and biologic/targeted therapy are systemic therapies because they reach other parts of the body beyond the breast.
Almost all women with breast cancer get some kind of local therapy, typically a combination of surgery with or without radiation therapy. The two usual surgical treatment options are (1) lumpectomy (breast-conserving therapy) followed by localized radiation to the affected area or (2) mastectomy. Some sort of lymph node testing is done for invasive cancers or noninvasive cancers that are more than 5 centimeters in size. A sentinel node procedure can be done when there are no palpable nodes (nodes that can be felt) under the arm. This involves removing only the nodes closest to the cancer, called the sentinel nodes. If those nodes do not show a spread of the cancer from the breast, then the more extensive operation removing more axillary nodes, which used to be standard, is not needed.
Overall survival depends on whether cancer cells have already spread beyond the breast to other parts of the body, and if so, on the effectiveness of systemic therapy. Local therapy may make a difference in the risk of local recurrence within the breast or how likely the cancer is to come back within the breast/chest area. In general, deciding whether it’s a good idea to have systemic therapy (such as hormone/endocrine therapy) depends on what testing suggests about whether the cancer might spread and on how you feel about the risks and side effects.
Questions to ask your health care team so that you can be as well informed as possible include the following.
At initial diagnosis:
• Please explain to me the type of breast cancer that I have. Is it noninvasive DCIS or invasive cancer?
• How can I get an appointment with a breast surgeon? Are there hospitals near where I live that have multidisciplinary breast cancer programs with a team of breast specialists I can meet in one visit?
• What information do I need to bring with me to my visit?
• Do you have a breast pathologist who can review my slides? How would we get a second opinion on the pathology?
• Can we review my pathology report? What is meant by “grade”?
• What is staging and what is my stage of disease?
• Do I need any additional testing and if so, why?
• What support services are available for me and whom can I talk with?
• Is there someone who can follow me through treatment and be available to answer questions?
When discussing local surgical treatment options:
• Can I have a breast-sparing lumpectomy and radiation therapy?
• If not, why not?
• Can you walk me through the surgical procedure?
• Will there be a lymph node procedure, and if so, what kind?
• Explain your technique for a sentinel node biopsy (used to determine if cancer has spread into the lymphatic system). What does it mean when a sentinel “lights up”? How many of these procedures have you done? How many false-negative cases are there?
• What is the risk of a local recurrence in my breast or chest wall if I have a mastectomy?
• What is my risk of developing breast cancer in my other breast?
• If mastectomy is recommended or if I choose to have a mastectomy, can breast reconstruction be done? What types of reconstruction would be available?
• If I have a lumpectomy (also called partial mastectomy and wide excision), what are the chances you will not get clear margins?
• How many breast surgeries do you do in one month?
• How will the pathology results of my surgery influence my overall treatment?
• Walk me through the recovery process. What will I be able to do and not be able to do?
• What restrictions will there be on my activity? Can I exercise?
• How long do I need to miss work?
• If I have a mastectomy, how long will I be in the hospital? Will I need help at home afterward?
• What are possible short-term and long-term complications of the surgery?
Questions for the radiation oncologist:
• What happens during the radiation treatments?
• What will the side effects be?
• Will I be tired from my treatments? Can I work during my radiation therapy?
• How many treatments will I need?
• I hear there is a shorter course of radiation therapy that takes less than six weeks. Can I have the shorter treatment? If not, why not?
Questions for the medical oncologist:
• Please explain to me what ER and PR and HER-2/neu mean.
• How are these markers used in planning my treatment?
• When would chemotherapy begin?
• What are the immediate (short-term) and long-term side effects of the drugs I’m supposed to take?
• What happens to my veins? What is a port, and will I need a port during treatment?
• Is there a clinical trial appropriate for me?
• If I need chemotherapy, can someone give me a tour of the treatment area?
• Are there integrative therapies such as Reiki, acupuncture, and massage that I might use to help manage the side effects?
Lifestyle questions:
• What exercise can I do during my treatment?
• Can I dye my hair during treatment? Will I lose my hair during treatment?
• Can I travel during treatment?
• Will I gain weight or lose weight during treatment?
• Are there special foods that I should eat or avoid during my treatment?
Some women who have had a mastectomy feel comfortable doing nothing to “fill in” the place where a breast is missing, choosing not to get an external prosthesis or have breast reconstruction surgery:
I refuse to have my scars hidden or trivialized behind lambswool or silicone gel. . . . I refuse to hide my body simply because it might make a woman-phobic world more comfortable. . . . I am personally affronted by the message that I am only acceptable if I look “right” or “normal.”
Others of us don’t want a visible scar, and some worry that other people may be repelled by it. Some decide to use a prosthesis inside a bra, to fill in the area and “match” the other side under clothing. Some prefer to have breast reconstruction done by a plastic surgeon; this is done by using your own tissue and/or an implant.
With an external prosthesis, you may look as if nothing has changed, as long as you wear your bra, which holds the prosthesis in place. It may shift under your clothes or feel heavy; it may be hot in the summer and cold in the winter. However, the feel, fit, and comfort of prostheses are continually improving. Stores and online companies that specialize in prosthesis fitting can custom-make one to fit your anatomy. You can get a temporary prosthesis after surgery; once your scar has healed, you can be fitted for a permanent one. Many health plans cover all or part of the cost of a prosthesis. Medicare will pay for one every year or two if you get a prescription from your doctor. If you have health care insurance, ask your insurance company what costs it will cover.
Breast reconstruction is a surgical option either at the time of the mastectomy or later. Some physicians pressure women to start reconstruction at the same time that they undergo a mastectomy. Although this may provide a psychological boost and slightly reduce the number of surgeries, it’s also okay to wait and see how you feel. If it seems that you have too many decisions to make all at once—sorting out your cancer therapy as well as whether to have reconstruction and what kind—then don’t rush into it. You will also want to learn about important safety considerations, especially regarding silicone breast implants.
Surgical reconstruction involves using either an implant under the chest muscle or your own tissues, with blood vessels, moved from your back, abdomen, or buttocks to your chest area (called a flap reconstruction). Sometimes an implant is used to supplement the tissue transfer operation. Reconstruction is not without risks, both during surgery (risk of blood loss or infection) and later on, but it also may have physical and emotional benefits.
An implant is a flexible synthetic envelope made of silicone and filled with salt water (saline) or silicone gel. The implant is placed behind the pectoral muscle or a flap of your own tissue and then the skin is sewn together. If there’s not enough space for the implant, a flexible expander is put in first to stretch the overlying tissues with saline injections over three to six months. Once the space is the right size, the expander is removed and replaced with a permanent implant.
Many women have developed debilitating conditions after breast implant surgery. The two major breast implant manufacturers have both reported a very high rate of complications after reconstruction with their implants. Here are the statistics from one company, for women two or three years after surgery: 46 percent needed additional surgery; 25 percent had their implants removed; 6 percent had substantial breast pain; 6 percent had necrosis (death of tissue); and 6 percent had ruptured implants, often with “silent” and prolonged leakage of silicone into their bodies.13 These complications were expected to increase over the following years.
Both manufacturers also reported a significant increase of symptoms associated with autoimmune diseases, including joint pain, fatigue, hair loss, and muscle pain. This increase happened within two years of getting implants.14 Unfortunately, the companies never published those findings in medical journals.
We need more research on women who have had breast implants for at least ten to twelve years, since most leakage or rupture occurs after that period of time. Some research has found an increase in fibromyalgia and some autoimmune diseases among women with leaking silicone gel breast implants. We need better research to determine how often women with leaking silicone implants suffer from autoimmune symptoms, not just autoimmune diseases.
Make sure you consult a board-certified plastic surgeon to find out what type of reconstruction is best for you. If the reconstruction uses muscle from somewhere else on your body (such as a TRAM flap), you will lose strength at the spot it came from. This is less likely if you have a tissue transfer that does not use muscle, such as the DIEP flap, which instead uses fat and skin tissue from the abdomen. If you want to consider a TRAM flap or DIEP flap, it’s especially important to find a plastic surgeon who is very experienced at that type of procedure, because experience increases the chances of success in these more complicated surgeries.
For any reconstruction, ask how long the recovery period is for the operation being recommended. If you smoke or have diabetes, complications may be more likely, as your blood vessels may be narrower or damaged, and healing can be more difficult. If you are active, especially in a particular sport, ask your surgeon to try to make it possible for you to return to this activity eventually. Once you get a recommendation, ask to speak with other women who have had the same procedure, both with this surgeon and with others. You can find other women to talk to through oncology social workers as well as through breast cancer support groups and other organizations. Breast Cancer Action (bcaction.org) is a great place to start.
If you have one breast removed, the plastic surgeon will probably try to make your two breasts look as similar as possible. This is difficult with implants, which tend to make the new breast much higher and rounder than the remaining breast. Some plastic surgeons recommend a breast lift and/or an implant in the remaining breast, so that the two breasts will be more symmetrical.
Consider the possible problems that can result from additional surgery and its risks. Further recovery time and side effects, such as loss of nipple sensation, should be taken into account. It is also important to know that an implant in the remaining (healthy) breast is likely to interfere with the accuracy of mammography, since the implant shows up as a solid white shape on the mammogram, hiding any cancer above or below it. To try to improve the accuracy, whenever you go for a mammogram, the technician should take additional mammography views (called displacement views). These views are important to detect cancer, but they expose you to more radiation and could thus increase your risk of breast cancer in the future. In addition, the pressure from a mammogram can cause an implant to break or leak. For those reasons, women who undergo reconstruction should seriously consider whether they want the additional risk of an implant in the remaining breast.
If you are considering reconstruction, make sure the surgeon understands what you want; she or he may have something different in mind. It’s important to mention what size you would like to be and make sure the surgeon agrees. If you are planning a TRAM flap or DIEP flap, talk to your surgeon about how you feel about having a second scar where your own tissue will be taken for the operation. Your body size and how much flesh you can spare may be a factor in whether these procedures work for you. Some plastic surgeons suggest a tissue flap with an implant, but that means you have the longer recovery time of the flap surgery and all the long-term complications of the breast implant. Ask about newer procedures that may be less damaging. Take time to become as well informed about reconstruction as you are about treatment.
Whatever type of reconstruction you choose, the surgeon can create a nipple and areola using darker, grafted skin or a tattoo. This is usually done several months after the reconstruction surgery.
More than 200,000 new cases of breast cancer are diagnosed every year in the United States; more than 44,000 women in the United States die of breast cancer each year. Currently, about three-quarters of women who get breast cancer are still alive ten years later, and almost two-thirds are still alive fifteen years later. Many women live long, healthy lives after a breast cancer diagnosis. But even with all the indicators available, it is difficult to make predictions for any specific woman. An individual’s immune system and general health are part of the picture, but there are still many unknown factors.
Current research is focusing on identifying biomarkers—proteins in the blood that indicate the presence of cancers and how they will behave. Research is also looking at ways to keep cancer cells from reproducing, such as cutting off the blood supply to tumors and changing the genetic instructions that make them grow out of control; and developing drugs that can target cancer cells without killing healthy ones. In the foreseeable future, further work in these areas should result in more individualized and effective treatments—and perhaps even a cure. Participating in research such as comparative studies or clinical trials of new treatments is an opportunity to contribute to progress in breast cancer research and can be meaningful for some women.
The uterus (womb) is a pear-sized organ made up of muscle that sits in the lower abdomen. It is lined with endometrium, hormonally sensitive tissue designed to nourish a developing embryo. Each month that a woman doesn’t conceive, this lining is shed through a menstrual period. The uterus can stretch to accommodate a growing fetus, then push the baby out and return almost to its former state. The cervix is the opening to the uterus. It protects the inside of the uterus from the outside world and then opens during labor to let a baby out.
This section covers some of the major conditions and problems we may experience with these parts of our body. For more information on the anatomy and function of the uterus and cervix, see Chapter 1, “Our Female Bodies.”
Fibroids are solid benign smooth-muscle tumors* that appear, often in groups, on the outside, inside, or within the wall of the uterus, possibly changing the size and shape of it. Many fibroids cause no problems at all, and many woman do not even know that they are present. Most women with fibroids can conceive and carry a pregnancy to term without any special treatment.
© Casserine Toussaint
A uterus without fibroids, left, and a uterus with fibroids (benign growths), right
Some fibroids, depending on size and location, can cause heavy vaginal bleeding, abdominal or back pain, urinary problems, and constipation. Sometimes they may make a woman’s belly look bigger. Fibroids that bulge into the uterine cavity (submucous fibroids) may make it difficult to conceive or to sustain a full-term pregnancy. There are several way to remove fibroids—which one is best depends on the size and location of the fibroids, as well as the skills of your surgeon. In at least 10 to 50 percent of cases in which fibroids are removed, new fibroids grow. However, only about 20 percent of women will require more treatment.
About 30 percent of all women get fibroids by age thirty-five and almost 80 percent of women will have fibroids by age fifty. Black women are more likely to have them, and to get them at a younger age. The cause of fibroids is unknown. About 40 percent of fibroids will grow during pregnancy, usually within the first three months. Some researchers used to think that using oral contraceptives made fibroids grow, but this is not as clear with low-dose pills. Very rarely, taking estrogen after menopause might affect fibroids.
Fibroids may be discovered during a routine pelvic exam. Because fibroids can grow, they should be monitored. If they haven’t grown any more by the time you have your next monitoring exam several months later, a yearly checkup will be enough. Ultrasound can give more definite information about the number and size of fibroids, but this is not always necessary.
If you have fibroids and abnormal bleeding, be sure to get carefully checked for other possible causes of the bleeding (see “Abnormal Uterine Bleeding”).
In many cases, no treatment is necessary for fibroids; this is called watchful waiting. If you are nearing menopause, the natural decline in estrogen levels at that time usually shrinks fibroids. Although many physicians recommend hysterectomy—removal of the uterus— as a treatment for fibroids, this is usually not necessary.
Myomectomy. If you have excessive bleeding, pain, urinary difficulties, or problems with pregnancy, you may want to have an operation called a myomectomy to remove the fibroids. Done by a skilled practitioner, myomectomy avoids some of the problems associated with hysterectomy and poses no greater risks. Even large, multiple fibroids can be removed with a myomectomy. There are several approaches, depending on the size and location of the fibroids.
Embolization of the uterine arteries. This procedure, performed by an interventional radiologist, cuts off blood supply to the fibroids, making them shrink. It reduces bleeding and tumor or uterus size in most women who have it done. The recovery time is typically shorter than for surgical removal of fibroids, if the procedure goes smoothly. Complications may include severe pain and fever that might require an emergency hysterectomy, damage to the uterus or other organs, and loss of ovarian function due to a constricted blood supply (this leads to premature menopause). For these reasons, this may be a risky approach for a woman who still wants to get pregnant.
Focused ultrasound surgery. Also called focused ultrasound ablation, this is another less-invasive option, but it can be used only for smaller fibroids and is not widely available.
Other treatments. Sometimes the drug leuprolide acetate (Lupron) is recommended to help shrink fibroids in women approaching menopause or planning to have surgery. However, Lupron has many negative effects, some of which may last many months beyond use of the drug. These include hot flashes, vaginal dryness, trouble with memory and concentration, and bone thinning. Also, after the Lupron is stopped, the fibroids can grow back.
The newest treatment, a medicated intrauterine device (IUD) called Mirena put into the uterus, can reduce bleeding and possibly enable you to avoid surgery.
Some women try to prevent or reduce fibroids by avoiding processed foods and the hormones usually found in commercial meat, dairy, and egg products, but there is no evidence that this will work. If your fibroids cause heavy bleeding, see the self-help treatments. Yoga exercises may ease the feelings of heaviness and pressure; some women find visualization techniques helpful, too.
Polyps are a focal buildup of the uterine lining. Sometime benign polyps can grow in the uterine lining and cause a woman to have heavy periods or bleeding between periods. Once they are diagnosed—usually by ultrasound, and sometimes by a procedure with a thin fiberoptic instrument called a hysteroscope—they are typically easy to remove. Removal is usually recommended because of the small risk (fewer than 3 out of 100 polyps) that they may be precancerous, and to treat abnormal bleeding.
The endometrium can also become hyperplastic owing to abnormal growth of the endometrial cells. This condition can cause abnormal uterine bleeding, especially in women who are not ovulating regularly or who are taking estrogen without progesterone (or a progesterone-like substance like a progestin). While endometrial hyperplasia is benign, another condition called atypical endometrial hyperplasia can be a precursor of cancer of the lining of the uterus (endometrial cancer). In this circumstance, a hysterectomy is sometimes recommended to prevent the development of uterine cancer. Benign endometrial hyperplasia may be treated with high-dose progesterone, depending on the woman’s age or intention to become pregnant, or with the Mirena IUD, which contains a progestin.
Endometrial cancer is the most common pelvic cancer, affecting fourteen out of every ten thousand women yearly. Most women with this cancer are over fifty and past menopause; 10 percent are still menstruating. If you are heavy for your size, take synthetic estrogen without a progestogen, or have diabetes, high blood pressure, or a hormone imbalance that combines high estrogen levels with infrequent ovulation, your risk of uterine cancer is increased.
During the early 1970s, there was a sharp rise in the incidence of uterine cancer because of estrogens prescribed for menopausal women without any additional progestogen (progestin or progesterone) to reduce the chances of endometrial hyperplasia. Taking progestogens usually prevents the development of this condition in women taking estrogen.
Bleeding (including light staining) after menopause is the most common symptom of uterine cancer. However, most women who bleed do not have cancer. For women who are still menstruating, increased menstrual flow and bleeding between periods may be the only symptoms. Unfortunately, the Pap test, while effective at detecting cervical cancer, is not reliable for detecting uterine cancer. If you have the above symptoms, your medical practitioner will probably recommend an aspiration or endometrial biopsy to sample the uterine lining—this is a simple office procedure. In some cases, a dilation and curettage (D&C) is preferred (performed with intravenous sedation or general anesthesia). Make sure that you have discussed the risks and benefits of these alternatives before making a decision.
Because endometrial cancer appears to be influenced by factors such as obesity, hypertension, and diabetes, controlling these conditions with self-help methods may prevent this type of cancer from developing. Exercise and a healthy diet with plenty of fruits and vegetables is the best strategy.
When uterine cancer is found early, the success rate of conventional treatments is very high. Medical treatment for uterine cancer includes surgery, radiation, and chemotherapy. There is wide disagreement about which is best. Outside the United States, radiation is used frequently with good results. Hysterectomy is the most common treatment in the United States. Follow-up radiation after surgery is possible if the tumor was large, if it is found or suspected to have spread to the lymph nodes, or if cellular changes suggest a fast-growing tumor. Hysterectomy can often be done laparoscopically. If the cancer comes back after one of these treatments, progestogen treatment may help slow it down.
Heavy menstrual bleeding (which may include clots of blood) or bleeding happening outside the normal cyclic menstruation is referred to as abnormal uterine bleeding (AUB). AUB is a common gynecological problem, but its causes can be tricky to diagnose. The most likely cause of AUB for any woman depends on whether she is premenopausal, perimenopausal (near menopause), or postmenopausal.
Some causes of AUB include hormonal imbalances, pregnancy, the use of hormonal contraceptives (birth control pills or Depo-Provera, for instance), fibroids, endometrial polyps, infection, and, more rarely, precancerous or cancerous growths. Infrequently, bleeding that seems to be coming from the vagina may actually come from the urinary tract or gastrointestinal tract. For severe bleeding without an obvious explanation, ask to be screened for von Willebrand disease, especially if you have a history of other bleeding problems.
Fibroids can cause heavy, longer periods, sometimes with cramping and clots. More commonly, this occurs when the fibroids are submucosal and impinge on the uterine lining. Such periods are usually not irregular.
In addition to being a sign of a possible physical problem, heavy and/or irregular bleeding is a nuisance. It can also result in anemia from low iron and thus cause fatigue. Sometimes, heavy and prolonged bleeding may be part of the normal transition to menopause.
During perimenopause (the transition to menopause), new and different bleeding patterns are common. That makes it hard to decide when the menstrual cycle is normal and when there is a problem. The amount of blood flow may vary from month to month. Women sometimes skip their period for a few months, and then have regular periods again. However, if you are experiencing many episodes of irregular bleeding as described in the box above, it could be a sign of a medical problem that should be addressed.
Women who take hormone therapy may experience normal or abnormal uterine bleeding. You should understand what pattern is expected with your hormone prescription and contact your health care provider if your bleeding is different from what you’ve been told to expect.
Vaginal bleeding is abnormal in any woman who is postmenopausal (has gone a full year without any menstrual periods), unless she is taking hormones.
Clinicians will review a woman’s medical history. For premenopausal women who are missing periods, the bleeding pattern may suggest pregnancy or ovulation (producing an egg). A pregnancy test can find out whether an abnormal pregnancy is causing AUB. Blood tests can check for anemia, thyroid function, and female hormone levels. Other symptoms, such as pelvic pain or hair growth, can suggest other particular causes of AUB.
A clinician may be able to detect uterine abnormalities such as fibroids through a pelvic exam. Women with AUB should get a Pap test if one has not been performed recently.
Adenomyosis (endometriosis in the wall of the uterus, a condition affecting about 10 percent of women) is another cause of heavy and painful periods. It can be diagnosed only with an expensive MRI or a surgical specimen during a hysterectomy.
Four special tests are often used to evaluate AUB, as follows.
Endometrial biopsy: This is a quick office procedure involving the removal of tissue from the uterine lining (endometrium) to check for precancerous and cancerous cells. A thin tube, which is a suction device, is inserted into the uterus through the vagina and the cervical opening. It withdraws samples of uterine tissue for analysis. This may cause cramping, and some women will need pain medication, including anesthesia.
Transvaginal ultrasound: In this test, a wand placed in the vagina produces sound waves that create an image of the pelvic organs. The test can identify uterine fibroids. It measures the endometrial lining and may indicate abnormalities in the endometrium.
Sonohysterogram, or saline infusion sonography: This special kind of transvaginal ultrasound involves putting saline (salt water) into the uterus through a thin tube, to improve the image and detection of abnormalities.
Hysteroscopy: Diagnostic hysteroscopy involves threading a thin flexible scope into the uterus to view the contents of the uterine cavity. It can be done in the office or at a surgical procedure unit. Operative hysteroscopy is done at the hospital with anesthesia. A slightly larger scope is used to look at the uterine cavity and remove abnormal tissue such as fibroids or polyps.
The treatment for abnormal bleeding depends on what is thought to be its cause. A woman’s age and plans for childbearing, as well as her preference, are important in planning the treatment. Treatments range from observation (and taking iron, if a woman is anemic) to hysterectomy, or removing the uterus.
Various medications can reduce or regulate abnormal bleeding and relieve pain. Nonsteroidal anti-inflammatory drugs (such as ibuprofen) taken for pain may also reduce bleeding. Tranexamic acid is a medication that significantly decreases menstrual bleeding. Only recently introduced in the United States, it has been available in other countries for many years. Birth control pills make the cycle more regular and reduce bleeding, but there is some controversy about using them during perimenopause (See the Centre for Menstrual Cycle and Ovulation Research for more information: cemcor.org).
An IUD (intrauterine device) treated with a progestin, such as the levonorgestrel-releasing Mirena, can be a nonestrogen hormonal option for controlling bleeding. Some other drugs, such as danazol and Lupron, reduce bleeding even more but also have serious negative side effects (see above); they are typically used for only a short time, to postpone or prepare you for surgery.
Noninvasive outpatient surgery (endometrial ablation) may be done with several techniques that cauterize, freeze, or remove the lining of the uterus to reduce bleeding. These include operative hysteroscopy (where the uterine lining is surgically removed) or the use of specially designed instruments such as the thermal balloon (ThermaChoice) or NovaSure to cauterize or even freeze the uterine lining. Endometrial ablation is an option after more serious causes of abnormal bleeding are ruled out. It may be less effective in the presence of fibroids. Hysterectomy is the only known effective treatment for adenomyosis.
Always discuss the particulars of your situation and your choices with your clinician. If you are uncomfortable with the options offered, try to get a second opinion.
If you are premenopausal, you may be able to stabilize your menstrual flow by reducing stress and changing your diet. Cutting down on animal fat and adding fiber helps to restore normal hormonal balance by lowering cholesterol, which is converted to estrogen in your body.
There is controversy about whether soy products—and which types—are beneficial for AUB or may help to regulate periods. Supplements of vitamins A, E, and C with bioflavonoids may help if your diet does not include enough of these vitamins. (Take no more than 10,000 IU of a vitamin A supplement twice a day, since larger doses can be toxic. One carrot contains 8,000 IU, and dark green leafy vegetables contain a lot, too, so you can get enough vitamin A from food.) If you are bleeding heavily, increase your iron intake to prevent anemia.
Some women find that Chinese medicine, including acupuncture and Chinese herbs, helps to restore hormonal balance. If you are approaching menopause, the bleeding may stop by itself as your hormone levels get lower.
The underlying cause of very heavy periods may be von Willebrand disease (VWD), the world’s most common inherited bleeding disorder. It’s a deficiency in the amount or quality of a protein that is required for blood to clot. VWD affects about 1 percent of people of all racial and ethnic backgrounds. Both men and women can inherit it from either parent. Because of our monthly periods, VWD affects females more frequently than males, but health care providers don’t always realize that is what’s wrong. The bleeding can range from being simply annoying to interfering with school, work, sleep, and mood.
VWD bleeding can be described as “oozing and bruising.” Bleeding typically occurs in the mucous membranes (for example, in the mouth after dental work, or in the rest of the gastrointestinal system). The most common symptoms are heavy or prolonged periods, easy bruising, prolonged nosebleeds, and prolonged bleeding following surgery, injury, dentistry, and childbirth. Other signs can be bleeding into the joints and urine. VWD may result in miscarriage and unnecessary surgery, including D&C, uterine ablations, and hysterectomy at a young age. Affected family members can have different bleeding patterns, as can people with the same type of VWD. Absence of bleeding does not rule out the disease. People with severe VWD have the same level of joint damage as do those with moderate hemophilia.
The American Congress of Obstetricians and Gynecologists (ACOG) recommends screening all women with severe uterine bleeding for VWD. A federally supported U.S. hemophilia treatment center, if near you, may be a good place to seek help.
There is no cure for VWD, but there are effective treatments. Treatment varies according to how severe your condition is, and may include hormones, a synthetic nasal spray, or medication that is injected under the skin or infused into a vein. You may need to see a hematologist (blood specialist) familiar with VWD for accurate diagnosis and appropriate treatment.
Cervicitis is a general term for inflammation of the cervix. A Pap test report or cervical biopsy may mention it, but it’s not always a real disease or disorder. Cervicitis may accompany vaginal infections, pelvic inflammatory disease, and sexually transmitted infections.
Cervical eversion (also called ectropion) occurs when the kind of tissue that lines the cervical canal grows on the outer vaginal part of the cervix, making it red, with a bumpy-looking texture that is smooth to the touch. If the inside (columnar epithelium) puckers out, that is referred to as eversion. This is a common physical variation. Most women do not have any symptoms, although eversion can cause bleeding during a Pap test. Eversion requires no treatment unless it is accompanied by infection. Those of us whose mothers took diethylstilbestrol (DES) during pregnancy are more likely to have this condition.
Cervical erosion is a pinkish-red sore on the cervix, next to the cervical opening. This rare condition causes little discomfort. Most cases referred to as erosion in the past were really eversion.
Cervical polyps consist of excess cervical cells that “pile up” within the cervical canal. They appear as bright red tubelike protrusions from the cervical opening, either alone or in clusters. Polyps are very common and usually benign. Most polyps contain many blood vessels with a fragile outer wall, so bleeding may occur after intercourse or other vaginal penetration, douching, or self-exam. Polyps may also bleed during pregnancy, when hormonal changes stimulate growth of blood vessels in all cervical, vaginal, and uterine tissue.
Cells from the polyps will be collected as part of a Pap test. Cervical polyps are almost never cancerous.
Polyps do not necessarily require treatment. When they are small and there is little or no contact bleeding, you or your clinician can usually just keep track of them with regular exams. Removing cervical polyps is often recommended as a preventive measure but is not required. You may want to have them removed if the polyps begin to grow. This is a simple office procedure where your practitioner twists the polyp off and scrapes or cauterizes the base. If your polyp is very large (this is rare), or if you have several of them, you may have to go to the hospital for removal. Sometimes polyps grow back after removal.
Cancer of the cervix is responsible for the deaths of half a million women around the world every year. In some countries, it is the leading cause of cancer death in women. Cervical cancer deaths are on the decline in the United States, probably as a result of Pap tests (which can catch cervical cancer early) and the treatment of precancerous cervical problems called dysplasia. Most cervical cancer results from human papillomavirus (HPV) infections that are transmitted through sexual contact (In Chapter 11, “Sexually Transmitted Infections). The Pap test, often done as part of a routine gynecologic exam (see “Pap Tests”), is a screening test for precancerous or cancerous changes in cervical cells. Most of the cellular abnormalities we call dysplasia are now thought to be caused by HPV, but only some types of HPV are associated with cervical cancer. Tests that can identify the presence of these “high-risk” HPV types are now available.
The results of the Pap test are classified according to what kinds and degrees of cell changes you have, if any. Many systems have been used over the years. At one end of all the scales is normal, and at the other end is cancer. In between are grades of dysplasia. Sometimes it can be difficult to distinguish one stage or grade of dysplasia from the next, and different laboratories or practitioners may interpret a given cell sample differently. Since the addition of the HPV DNA test in 2003, many clinicians interpret results of the Pap test in conjunction with this newer test.
As many as 40 percent of all tested women will have an abnormal Pap test at some time during their life. We often feel anxious when we hear our results are “abnormal,” because we fear cancer, but there is no need to panic. Most cervical cell changes are very slow. Dysplasia is not cancer, and in about 80 percent of cases, dysplasia does not develop into cancer. The cells of most women diagnosed with mild dysplasia will return to normal. But all cases of diagnosed dysplasia should be watched closely—with repeated Pap tests and other recommended procedures. If abnormal cells are found, many women get tested again after six months to see if the abnormalities are still present. Dysplasia should be treated if it is severe or if it progresses.
Clinicians sometimes recommend a colposcopy after an abnormal Pap test. This is an office procedure during which the cervix is swabbed with an acetic acid (dilute vinegar) solution to make the abnormal areas stand out. Selected biopsies of the most abnormal areas are then examined under a microscope by a pathologist to better define the extent and severity of the abnormalities.
Treatments for cervical dysplasia are based on age, severity of the dysplasia, and each woman’s personal history.
Treatments for dysplasia (precancer) of the cervix vary widely. Different practitioners may have varying preferred treatments for each diagnosis, making it difficult sometimes to get appropriate treatment for your condition and avoid unnecessary or pointless diagnostic tests, treatments, and surgery. That’s why second and even third opinions may be important. Procedures such as colposcopy, punch biopsy, and cone biopsy should be done only by medical practitioners who have special training, skills, and sufficient experience.
Minimal abnormalities often require no treatment. Mild (low-grade) abnormalities are usually managed with watchful waiting. Moderate or severe (high-grade) abnormalities require treatment or further evaluation. Treatments include:
Cryotherapy, which destroys abnormal tissue by freezing, can be done in the clinician’s office. Laser, which uses a high-intensity light beam to evaporate abnormal tissue, is most often performed in an outpatient procedure center or occasionally in a hospital on an outpatient basis. Often, local anesthesia is given to numb the cervix.
Loop electrical excision procedure (LEEP), which uses a wire loop charged with a small electrical current, is usually performed in an office or outpatient procedure center with local anesthesia. Clinicians use LEEP to remove abnormal tissue. The sample can also be sent to a pathology lab for evaluation. Sometimes this procedure is also called a LLETZ (large loop excision of the transformation zone).
Cone biopsy, which removes a cone-shaped portion of the cervix, can be done in an outpatient procedure center, or in the hospital on an outpatient basis, with local or general anesthesia. Clinicians may use a scalpel, laser, or electrical loop as used in LEEP to remove the tissue. Because cone biopsy does not destroy tissue, the sample will be sent to the pathologist for evaluation.
Hysterectomy is not appropriate for cervical dysplasia, but it is recommended as the appropriate treatment for invasive cancer (see “Uterine Cancer,”). This is major surgery, with serious risks and other health consequences.
Long-term negative effects of laser and LEEP on the cervix are uncommon. Tissue damage may, on rare occasions, weaken the cervix, so it can be harder to carry a pregnancy to term. (This is more common with a cone biopsy, which also can produce scarring that might later interfere with dilation of the cervix during labor and birth, sometimes leading to a cesarean section.)
Since the 1940s, the U.S. cervical cancer mortality has decreased by 75 percent. Currently, between 10,000 and 11,000 cervical cancer cases occur yearly, resulting in 3,000 to 4,000 deaths. (In comparison, about 40,000 women die yearly from breast cancer.)
In its early stages, cervical cancer is almost always curable, depending on the severity of the lesions and the treatment used.
If severely abnormal cells have spread beyond the upper tissue layer (surface epithelium) of your cervix into the underlying connective tissues, you have invasive cervical cancer. A Pap test followed by a biopsy can determine whether that has happened. At first the spread is very shallow and may not involve the lymph or blood circulation systems.
For invasive cervical cancer, most physicians recommend a hysterectomy with removal of lymph nodes in the pelvis. If the cancer has spread into the lymph or blood vessels, doctors usually suggest radiation or hysterectomy plus removal of the ovaries. Sometimes a combination of the two is used (chemotherapy is not as effective as local radiation). Recently, there have been efforts to find fertility-sparing surgeries for cervical cancer.
You should be involved in your treatment and have the final say in all decisions. If you have any doubts about treatments recommended by your health care provider, try to get second and third opinions.
Ovarian cysts are relatively common and may result from normal ovulation. They develop when a follicle (the fluid-filled sac that nurtures a developing egg) has grown large but has failed to rupture and release an egg. Often, cysts don’t cause any symptoms or discomfort, but you may experience a disturbance in the normal menstrual cycle, an unfamiliar pain, or discomfort on one side in the lower abdomen. Pain during intercourse is another symptom. Cysts are sometimes found by a routine bimanual pelvic exam, then diagnosed with ultrasound. Often they disappear by themselves, though some types may have to be removed.
To determine whether a cyst requires treatment, wait a cycle or two for it to disappear. If it persists, a medical practitioner may use ultrasound to monitor it. Practitioners disagree about whether removing benign cysts is necessary, but small ones do not usually cause problems and may be left alone.
A large cyst is more of a health risk because it can rupture, causing severe abdominal pain and sometimes bleeding. A large cyst may also twist and damage the blood supply to the ovary. These two uncommon situations require prompt surgery. Pathological cysts, such as a dermoid cyst or a cyst of endometriosis, should usually be removed.
If your physician advises removal of the ovary along with a benign cyst, get a second opinion. Removing the ovary, though a conventional practice in the past, is unnecessary in many cases. Ovaries perform many functions, even after menopause.
Recurrent cysts may indicate a hormonal imbalance and/or life stresses. Changing your diet, learning how to reduce stress, and using acupuncture may also help to get your system back in balance.
Cancer of the ovaries accounts for only 3 percent of all cancers in women in the United States. About 22,000 cases were estimated for the year 2010 (with about 14,000 deaths expected). It is the ninth most common cancer among women in this country, but it is the deadliest among gynecologic cancers. Most ovarian cancer occurs among midlife and older women; more than half of all women diagnosed with ovarian cancer are over age sixty.
The exact causes of ovarian cancer are still unknown. Possible risk factors include a family history of ovarian cancer; few or no pregnancies; the use of fertility-stimulating drugs; a history of breast, colorectal, or endometrial cancer; exposure to industrial products, including asbestos, or to high levels of radiation; a diet high in fat; and the use of estrogens other than the birth control pill. (In one large study, the risk of developing ovarian cancer was higher in women who used menopausal hormone therapy than in women who never used such therapy, but the increased risks varied by type of hormone and regimen, as well as by whether a woman had had a hysterectomy).17
Using talcum powder in the genital area has long been suspected as a risk factor, but so far evidence points to an elevated risk for only one type of relatively rare ovarian cancer. Oral contraceptive use is protective against ovarian cancer, as is having multiple pregnancies. Having a tubal ligation also appears to reduce risk.
One reason the death rate is so high is that most ovarian cancer is found in the later stages, when it is harder to treat effectively. When it is found early, about 90 percent of the women treated survive at least five years.
Ovarian cancer does not always have clear symptoms. Its warning signs—which may be vague and are frequently dismissed as stress or nerves—include indigestion, gas, bowel disturbances, loss of appetite or weight, a feeling of fullness, enlargement or bloating of the abdomen, lower abdominal discomfort or pain, unexplained weight gain, frequent urination, fatigue, backache, nausea, vomiting, nonmenstrual vaginal bleeding, or pain during intercourse. Most of these are relatively common complaints in midlife women.
If you have persistent symptoms or a family history of ovarian cancer, your gynecologist should do a thorough evaluation. In some cases, you may need to be referred to a gynecological oncologist, who specializes in cancer diagnosis and treatment. The screening tests now available for ovarian cancer are not very accurate, so there is still no good routine testing method for women with no symptoms and no risk factors. A blood test for a protein called CA-125 is not enough to diagnose ovarian cancer, because many other conditions can also raise the level of CA-125 in the blood; therefore, it needs to be used in combination with other tests.
Diagnostic tests for cancer of the ovaries include pelvic ultrasound, computerized tomography (CT or CAT scan), magnetic resonance imaging (MRI), and surgery, the only conclusive diagnostic tool. Exploratory surgery (laparotomy) is used for diagnosis, staging, and, frequently, tumor reduction. (For more information on stages and different types of ovarian cancer, including borderline tumors not likely to become malignant, see Recommended Resources.)
About 5 to 7 percent of ovarian cancer cases are associated with an inherited risk factor, and removal of an ovary or ovaries (oophorectomy) has been shown to be an effective way to avoid breast cancer in women who carry a BRCA1 or BRCA2 gene mutation. Discuss all the benefits and harms of a prophylactic oophorectomy with your health care provider.
Early detection, prompt diagnosis, and accurate staging are necessary for the successful treatment of ovarian cancer. Treatment depends on the stage of the disease at the time of diagnosis, the type of cells that make up the tumor, and how fast the cancer is growing. The current standard medical options for treating ovarian cancer include surgery, chemotherapy, and/ or radiation. Immunotherapies, including interferon, interleukin, bone marrow or stem cell transplants, and monoclonal antibodies, are also available in clinical and/or research settings.
New cancer therapies often become available to patients through clinical trials. Information about some of these investigational treatments is registered with the National Cancer Institute (cancer.gov). Many women also explore supplemental or alternative treatments, alone or in conjunction with mainstream treatments. More research is still needed to better understand the causes of ovarian cancer and to find more effective diagnostic tests and treatments.
I had been complaining of the same problem—pain in my lower right abdomen—for a couple of years. I had severe menstrual irregularities, fevers, bleeding between periods, bleeding after intercourse, pains, and general malaise. Several times I was treated with antibiotics, which brought only some temporary relief. Never was the issue resolved as to what was causing this. Never were my sexual partners or practices mentioned.
Pelvic inflammatory disease (PID) is a general term for an infection that affects the lining of the uterus (endometritus), the fallopian tubes (salpingitis), and/or the ovaries (oophoritis). It is caused primarily by sexually transmitted infections that spread up from the opening of the uterus to these organs (see Chapter 11, “Sexually Transmitted Infections”). Nearly 1 million women in the United States develop PID every year, and 300,000 women are hospitalized for it. This may be a low estimate, because PID is underdiagnosed.
The primary symptom is pain in the lower abdomen. It may be so mild that you hardly notice it, or so strong that you may not even be able to stand. You may feel tightness or pressure in the reproductive organs, or an occasional dull ache. Part of the reason PID is so underdiagnosed is that women may also have some, most, or none of these other symptoms: abnormal or foul discharge from the vagina or urethra, pain or bleeding during or after intercourse, irregular bleeding or spotting, increased menstrual cramps, increased pain during ovulation, frequent or burning urination, inability to empty the bladder, swollen abdomen, sudden high fever or low-grade fever that comes and goes, chills, swollen lymph nodes, lack of appetite, nausea or vomiting, pain around the kidneys or liver, lower back or leg pain, feelings of weakness, tiredness, depression, and diminished desire to have sex.
The intensity and extent of the symptoms depend on which microorganisms are causing the problem, where they are located (uterus, tubes, lining of the abdomen, etc.), how long you have had PID, what if any antibiotics you have taken, and your general health. Doctors characterize PID as acute, chronic, or silent (when symptoms are not noticeable).
Most cases of PID are caused by microorganisms responsible for sexually transmitted infections. They can get into the body during sexual contact with an infected man or woman.18 If you are carrying these microorganisms, certain procedures or reproductive events can push them farther into your body, including miscarriage, childbirth, abortion, or other procedures involving the uterus, such as endometrial biopsy, hysterosalpingogram (X-ray of the reproductive tract), IUD insertion, or donor insemination. If you have chronic PID and antibiotic treatment doesn’t help, your sexual partner(s) may be reinfecting you. Men can be carrying the organisms that can cause PID without having symptoms, so they must be tested and treated, too, and they should use a condom during intercourse.
The risk for developing PID is higher if you are exposed to infected secretions—especially infected semen—during menstruation and ovulation, when your cervix is more open and your mucus is more penetrable. Women using some IUDs are also at higher risk during the first four months after insertion. In some parts of the United States, gonorrhea still causes most PID. In other areas, chlamydia is more often the cause of PID. Current guidelines recommend annual chlamydia screening for women age twenty-five and under who are having sex, to find and treat this infection before it causes PID.
The complications of PID can be very serious. If untreated, PID can turn into peritonitis—a life-threatening condition—or into a tuboovarian abscess. It can affect the bowels and the liver (causing perihepatitis syndrome). Months or years after an acute infection, infertility or ectopic pregnancy can result if your fallopian tubes were damaged or clogged by scar tissue. PID can also cause chronic pain from adhesions or lingering infection. In the most extreme cases, untreated PID can result in death.
Because so much PID is caused by sexually transmitted organisms, preventing PID involves preventing sexually transmitted infections. You can reduce your risk by using condoms and engaging in safer sex practices. For more information, see Chapter 11, “Sexually Transmitted Infections.”
If you could know right away exactly which organisms were causing your PID, you could get the right antibiotics. But pinpointing the organisms often takes some tests that may be expensive and not readily available. Sometimes organisms infecting the uterus and fallopian tubes don’t show up in a cervical culture. You may be told that your chronic cystitis is caused by trauma to the urethra during intercourse when it’s really a sign of PID, or that you got infected by wiping yourself from back to front, when you really have a sexually transmitted infection. You may be told that you have a spastic colon or an emotional, not a physical, problem, when that is not true. Try to have your situation thoroughly assessed, particularly if symptoms persist despite treatment, or seek a second opinion.
Blood tests can help indicate whether you have an infection but won’t always tell you which one. Sometimes an endometrial biopsy can find hard-to-culture organisms, but if it is not done carefully, this procedure can spread germs from the cervix and vagina to the uterus. In some cases, ultrasound, including vaginal ultrasound, may be useful. A definitive diagnosis often requires laparoscopic surgery.
Most experts seem to agree that since your health and fertility are at stake, you should start treatment while waiting for test results. Both you and your partner must be treated. If your partner continues to carry the microorganism(s), you will be reinfected. Taking the wrong drugs can make organisms more difficult to get rid of; however, the practical strategy is to begin treatment, then adjust it according to what cause is found. Once you start taking antibiotics, you cannot get an accurate culture again until at least a couple of weeks after you stop taking them.
Therapy lasts at least ten to fourteen days. You should receive two different kinds of antibiotics, since more than one organism may be involved. Remember to take all your antibiotics, even if your symptoms are gone, so that antibiotic-resistant strains of microbes will be less likely to develop. (See the Centers for Disease Control and Prevention website for more information about antibiotic resistance: cdc.gov/drugresistance.) Antibiotics can cause yeast overgrowth in the vagina, so you may need something to keep the yeast in check while trying to cure the much more serious PID (see “Yeast Infections”).
Many experts recommend that all women with PID be hospitalized for treatment, but not all physicians follow these recommendations. Most women are hospitalized in the event of an acute attack, to get intravenous (IV) antibiotics. If you’re still not cured, it may be because you got the wrong antibiotic, have a pelvic abscess, or were reinfected by a partner.
You may be urged to have a hysterectomy if the doctor thinks that PID has damaged your pelvic organs beyond repair. Also, emergency hysterectomies are done in some cases of acute PID (for example, when an abscess ruptures). If the infection is in your urinary tract, as it often is, then hysterectomy does not eliminate it. Hysterectomy is rarely necessary for PID, except in cases of persistent, debilitating PID.
Avoid intercourse until you have felt completely well through an entire monthly cycle and your partner(s) have had negative test results for all STIs. You can have a recurrence of PID months after the initial infection is cleared up, particularly if you don’t keep up daily health routines or are under too much stress.
There are some things you can do to help alleviate discomfort while you wait for test results to come back and for antibiotics to start working. Very hot baths and a heating pad applied directly to the lower abdomen help relieve pain and bring disease-fighting blood to your pelvis. You can soak a cotton cloth in castor oil, place it on the abdomen, cover it with plastic wrap, and then put a heating pad or hot water bottle on top to bring a maximum amount of heat to the pelvic area. Ginger root compresses and taro root poultices may relieve pain, keep the area loose and freer from adhesions, and dissolve already formed adhesions. Do not douche or use tampons; doing so may force microorganisms up into your uterus. Do not reuse a douche bag that may be harboring infectious organisms.
Certain herbs and teas may be useful against infection of the reproductive and urinary tracts. Raspberry leaf tea can strengthen the reproductive system; cranberry juice may help with UTIs. Try to eat wholesome, fresh foods and reduce stress as best as you can.
Endometriosis is a puzzling hormonal and immune system disease in which tissue like that which lines the inside of the uterus (endometrium) grows outside the uterus. It affects girls and women from before a first menstrual period to postmenopause and can cause pain, infertility, and other problems. There are an estimated more than 6 million girls and women in the United States alone who have endometriosis.
The most common symptoms of endometriosis are pain before and during menstrual periods, pain during or after sexual activity, infertility, fatigue, and heavy bleeding. Other symptoms such as lower-back pain with periods and intestinal upset with periods (including diarrhea, painful bowel movements, and/or constipation) are also common.
Many with endometriosis also experience a range of immune disorders, including allergies, asthma, eczema, and certain autoimmune diseases. Other symptoms may include irregular bleeding, pain related to urination, yeast infections (gastrointestinal or vaginal), and abdominal bloating. Infertility affects 30 to 40 percent of women with endometriosis, and about a third of women with infertility have endometriosis. (If you know you want to conceive, be aware that delay in diagnosis and treatment may make pregnancy less likely if the disease advances.)
Women and girls with endometriosis appear to be at higher risk for developing autoimmune diseases such as chronic fatigue syndrome, fibromyalgia, hypothyroidism, lupus, multiple sclerosis, rheumatoid arthritis, and Sjögren’s syndrome. Currently, researchers are studying whether there is a greater risk for certain types of cancers. Because of these risks, and because symptoms seem to worsen with time, early diagnosis is important.
Like the lining of the uterus, endometrial growths usually respond to the hormones of the menstrual cycle, building up tissue and then breaking it down. The result is internal bleeding, inflammation of the surrounding areas, and formation of scar tissue and adhesions. Complications of endometriosis can include formation and even rupture of cysts (which can spread endometriosis to new areas), intestinal bleeding or obstruction, or interference with bladder function. Symptoms often worsen with time, though cycles of remission and recurrence are sometimes the pattern.
The extent or size of endometrial growths may not have any correlation with the intensity of pain. Even tiny growths can produce substances called prostaglandins that are involved in pain (as well as in menstrual cramps).
Endometrial growths (also referred to as nodules, tumors, lesions, or implants) are usually inside the abdomen—on the ovaries, in the fallopian tubes, in the ligaments supporting the uterus, in the area between the vagina and the rectum, on the outer surface of the uterus, and on the lining of the pelvic cavity. The implants can also be found in internal abdominal surgery scars, or on the bladder, intestines, vagina, cervix, and vulva. Rarely, they develop in the lung, arm, thigh, and elsewhere in the body.
“Don’t be a baby, honey; all girls get cramps. Take two aspirin and go back to class,” the nurse at my high school told me when I was bent over double in tears. . . . I’m not a baby. I’m not a hypochondriac. . . . It took six years to find out. Looking back, I wish I had been a more aggressive patient. I should never have allowed myself to believe these occurrences were all in my head. . . . Don’t listen to the people who tell you to go away. Be persistent. Listen to your body.
Endometriosis is a major factor in decreasing the quality of life for many girls and women. It can be chronic and its seriousness is often underestimated. The Endometriosis Association (endometriosisassn.org), an international self-help organization founded in 1980 that conducts research collaboratively with the National Institutes of Health and Vanderbilt University School of Medicine, has collected data from four thousand women diagnosed with endometriosis and found that 79 percent said that they were unable to carry on normal work and activities at times, yet 69 percent had been told by a gynecologist that nothing was wrong.
I was diagnosed too late, though I complained bitterly about very painful, heavy periods since my midteens. I think it’s disgraceful that doctors aren’t more interested in treating this disease before things get so out of hand. . . . I am 36 and too destroyed (physically and emotionally) to carry on the fight to preserve my fertility.
Many doctors still don’t take menstrual pain seriously. The average time between onset of symptoms and diagnosis is more than nine years because doctors are slow to diagnose and, in part, because girls and women delay reporting their symptoms. A compelling reason to push for earlier diagnosis is that those who had taken a long time to be diagnosed were more likely to end up having a hysterectomy, according to Endometriosis Association data.
A definitive diagnosis of endometriosis currently requires a laparoscopy—an outpatient surgical procedure done under anesthesia, in which the patient’s abdomen is distended with carbon dioxide and the abdominal organs are checked by using a laparoscope (a fiber-optic tube with a light in it). Though growths can sometimes be detected during a manual pelvic exam or on ultrasound, endometriosis is sometimes confused with other disorders that have similar symptoms (PID, ectopic pregnancy, cysts, appendicitis, diverticulitis, irritable bowel syndrome, or even cancer). The Endometriosis Association has a diagnostic kit that helps.
There are a number of treatments for endometriosis, but not one that works for everyone. The most important thing to know is that you must educate yourself and make your own decisions about your treatments, and find the right health care practitioner(s) for you. In the process, you may want to consider your age, your symptoms, where and how severe the growths are, whether or not you want to get pregnant, your past experiences with hormones, and family history.
Hormonal treatments aim to stop or stabilize the production of various hormones for as long as possible. Recently, aromatase inhibitors have also been used to stop estrogen production in lesions and in fat cells. Hormonal treatments include gonadotropin-releasing hormone (GnRH), agonists (such as Lupron), testosterone derivatives (danazol), progesterone-like drugs (Provera), the Mirena IUD (which releases a progestogen, a progesterone-like substance), and oral contraceptives. New drugs are currently in development. Medications can be very expensive, and all cause side effects that are problematic for some women. All tend to work while you are taking them, but the disease usually returns when you stop.
Surgery ranges from conservative (removing growths) to radical (hysterectomy and removal of the ovaries). Radical surgery has been called the definitive cure for endometriosis, but the disease can continue or recur even when the ovaries are removed with the uterus. Minimally invasive gynecologic surgery through the laparoscope has largely replaced major abdominal surgery. As with any surgery, the skill and experience of the surgeon are of paramount importance.
Complementary medicine—especially nutritional approaches, traditional Chinese medicine, environmental medicine, and other treatments—has proved helpful for some women. Contact the Endometriosis Association for more information and refer to comprehensive books on the subject.
Connecting with other women who also have endometriosis can be very helpful. One way is through the Endometriosis Association Facebook page (facebook.com/EndoAssn) or local meet-ups. Getting support can decrease feelings of isolation and provide opportunities to counteract misinformation or a lack of information, as well as to share experiences with others who understand what you’re going through.
The DES story is a cautionary tale of medical care gone awry.
DES (diethylstilbestrol) is a powerful synthetic estrogen that crosses the placenta of pregnant women and can damage the reproductive system of the developing fetus. DES may also affect other body systems: endocrine, immune, skeletal, and neurological. This drug was prescribed to an estimated 4.8 million U.S. women between 1938 and 1971 (and sometimes beyond) in the mistaken belief that it would prevent miscarriage. In fact, DES was untested for pregnancy use or safety, and studies showing that it did not prevent miscarriage were ignored for almost two decades. It was aggressively marketed and used worldwide, under more than two hundred brand names, in pills, injections, and suppositories, and sometimes in pregnancy vitamins, until it was found to be linked to a rare form of vaginal/cervical cancer (clear cell adenocarcinoma of the vagina or cervix) in women who were exposed when their mother took the drug during pregnancy.
DES exposure during an embryo’s development has lifelong effects that can’t be reversed. For example, the cells of the endometrium (uterine lining) of an adult woman who was exposed to DES in the womb will act differently from those of a woman who wasn’t exposed.
Outside the United States, DES was also prescribed during pregnancy in Canada, Ireland, France, the United Kingdom, the Netherlands, Australia, New Zealand, Israel, Russia, and Poland. Other countries may include Belgium, Czechoslovakia, Finland, Germany, Italy, Norway, Portugal, Spain, and Switzerland. DES use in some of these countries extended beyond the 1970s. Large generational studies of DES mothers, daughters, sons, and granddaughters by the National Cancer Institute DES Follow-up Study continue in the United States as a result of efforts by DES advocacy groups.
Several million people have been exposed to DES, most without knowing it. If you were born between 1938 and 1971, if your mother had problems with any of her pregnancies or remembers taking anything when she was pregnant with you, you could have been exposed. (DES was most widely used between 1947 and 1965, when “wonder drugs” were popular.) However, with the passage of time it has become increasingly difficult to be sure by finding medical records. Some health care providers or facilities no longer have old records or refuse to give out the information. Any women in the appropriate age group should try to find out if she is at risk. See DES Action (desaction.org) for the latest information about DES exposure.
One out of every thousand DES daughters is likely to develop clear-cell adenocarcinoma, a rare type of vaginal or cervical cancer. It has occurred in girls as young as seven and women up to age forty, with the peak at ages fifteen to twenty-two. Although the number of cases of clear-cell cancer has declined in the last three decades (mirroring decreased use of DES beginning in the 1970s), it continues to be found in DES daughters, some in their fifties. There is a suggestion of a possible increase in the number of cases as DES daughters reach menopause. If you are a DES daughter, you need a special yearly DES exam for the rest of your life.
Annual DES exams can find clear-cell cancer early, so it can be treated. This cancer grows quickly and sometimes has no symptoms in the early stages. Typical treatment for clear-cell cancer may include a radical hysterectomy, surgical removal of all or part of the vagina, and reconstruction of the vagina. Radiation treatment may be added. Eighty percent of women survive this cancer.
Studies show that DES daughters have a greater risk for a more common vaginal cancer, squamous cell carcinoma. You may also have adenosis—columnar cells where the usual squamous cells should be—around the cervix. If you do, you may be more vulnerable to precancerous or cancerous changes. Annual monitoring is recommended until any adenosis disappears; discuss this with your gynecologist and be sure she or he knows about your exposure. Dysplasia (abnormal cell change) is more common among DES daughters, but normal cell changes may be mistakenly seen as abnormal when your cervix is checked, leading to unnecessary treatment with possibly harmful effects. That’s why it’s important to find a health care provider with experience in DES screening.
Structural changes in the uterus and cervix are common in DES daughters. Cervical “collars” or “hoods” (adenosis) do not have to be treated and may disappear after age thirty. A smaller or T-shaped uterus may contribute to pregnancy problems (see below).
If you are a DES daughter over age forty, your risk for breast cancer may be almost two times greater than that of unexposed women.19 DES mothers, too, have developed more breast cancers than unexposed women—sometimes as long as twenty years after exposure—so both mothers and daughters should get a clinical breast exam every year, in addition to doing self-exams to become familiar with the normal look and feel of their breasts. Women exposed to DES should report any changes to their health care provider. Annual mammography or other additional screening exams are also appropriate for DES daughters.
Contraception for DES daughters poses some special considerations. Birth control pills may be risky, since they increase estrogen exposure in someone already at higher risk of hormone-related cancer. IUDs may not be safe because of cervical and uterine abnormalities. Barrier methods (condom, diaphragm) are probably the safest choice overall.
Pregnancy problems have resulted from structural abnormalities in the uterus and cervix of DES daughters. You might have trouble conceiving, or be more likely to miscarry, deliver prematurely, or have an ectopic (tubal) pregnancy (in the fallopian tube instead of the uterus). A pregnant DES daughter needs high-risk obstetrical care. Checking early in pregnancy for signs of problems may help prevent serious complications.
The doctor [who] was doing my DES exams didn’t know anything about pregnancy problems for DES daughters. So I brought him seven articles that DES Action gave me. We both read them, and as a result, he checked my cervix at every prenatal visit. It took fifteen seconds and took away tons of anxiety.
Other problems, including endometriosis, menstrual irregularities, and pelvic inflammatory disease, have been reported by many DES daughters. DES sons have increased risk of urogenital problems. Recent studies have shown that DES granddaughters may have delayed menstruation regularity and DES grandsons may have an increased risk of hypospadias (in which the urethral opening on the penis is in the wrong place). Tell your doctor if you are a DES grandchild and be vigilant for any new information about DES.
The annual DES exam for DES daughters is similar to a regular Pap test and pelvic exam, but it is more comprehensive, because changes caused by DES do not usually show up in routine exams. A copy of directions for doing the exam is available from DES Action for you to show your doctor. The exam should include careful visual inspection of the vagina and cervix, gentle palpation of the vaginal walls, Pap tests from the cervix and from the surfaces of the upper vagina, and a bimanual pelvic exam. Sometimes iodine staining (Schiller’s test) of the vagina and cervix is used to distinguish normal tissue (which stains brown) from adenosis (which does not stain). These tests will indicate anything that might need further testing by colposcopy or biopsy. Even after a hysterectomy, DES daughters still need an annual gynecological exam. Daughters can contact DES Action at 1-800-337-9288 or info@desaction.org.
The United States has the highest hysterectomy rate in the industrialized world. Statistics from 2004 indicate that about one-third of all U.S. women have had a hysterectomy by the age of sixty. Today, about 90 percent of hysterectomies are done by choice and not as an emergency or lifesaving procedure. Various studies have concluded that anywhere from 10 percent to 90 percent of those operations were not really needed, but many physicians continue to recommend them. This surgery has certainly saved lives and restored health for many women, but unnecessary operations have needlessly exposed women to risks. There is increasing understanding that a woman’s uterus and ovaries have value during midlife and beyond, so the view of a woman’s uterus and ovaries as “expendable” during later periods in our lives is now obsolete.
Both hysterectomy (removal of the uterus) and oophorectomy (removal of the ovaries) are major surgery and may have long-term effects on our health, sexuality, and life expectancy. Because of the controversy over high hysterectomy and oophorectomy rates, many insurance plans now require a second opinion from another physician before agreeing to pay for the procedures. Because some surgeons recommend hysterectomy routinely, women need to understand when the surgery is truly necessary (see sidebar).
Fortunately, diagnostic and therapeutic techniques such as sonography, Pap tests, hysteroscopy, endometrial ablation, and laparoscopy make it possible to avoid or delay many hysterectomies that might have been done in the past. It is important to consider and utilize these techniques before resorting to major surgeries.
The most recent data suggest that black women have a somewhat higher hysterectomy rate than white women, possibly because black women are more likely to have fibroids. In the past, hysterectomy was performed solely for the purpose of sterilization among many poorer women and women of color in the United States, and this history affects the overall rate of hysterectomy among women of color. The problem of sterilization abuse led to federal sterilization guidelines in 1979, but the practice of performing medically unindicated hysterectomies continued for many years. It is likely that the rates of unnecessary hysterectomies have dropped only relatively recently.
Whenever you have any doubts about the need for a hysterectomy and/or oophorectomy, seek one or more other opinions about possible alternative approaches (such as a myomectomy, which removes fibroids without removing the uterus).
Oophorectomy is removal of either one (unilateral) or both (bilateral) ovaries. The fallopian tube(s) may be removed as well. Common reasons for oophorectomy include benign tumors of the ovary such as an endometrioma or dermoid; ovarian cancer; pelvic infection; and ectopic pregnancy (a pregnancy that occurs outside the uterus). In many cases, benign tumors, dermoid cysts, and endometriomas (cysts of endometriosis) can be removed without taking out the ovaries. Large functional cysts (fluid-filled sacs that often form during a menstrual cycle) can also be removed in this way, if they are not reabsorbed on their own. Women who have mutations of the BRCA1 or BRCA2 genes are at higher risk for ovarian cancer and sometimes have their ovaries removed as prevention.
If only one ovary is removed and not your uterus, you will continue to be fertile and have menstrual periods. However, you may experience an earlier menopause. If both ovaries are removed, you will experience surgical menopause. Even if one ovary is retained, you may have menopause-like symptoms due to loss of blood supply to the remaining ovary. (Such symptoms are also possible when both ovaries are retained after a hysterectomy.)
The ovaries usually continue to produce some hormones after menopause. Routine removal of healthy ovaries of women over forty-five during a scheduled hysterectomy should no longer be done,20 even though some doctors still try to justify an oophorectomy to prevent the possibility of future ovarian cancer. Evidence now shows that removing ovaries in this way does far more harm than good, because so many more women will die from heart disease and osteoporotic fractures resulting from the surgery than from the relatively small number of ovarian cancers that would be prevented. For more information, see “Hysterectomy and Ovarian Conservation” at ourbodiesourselves.org.
Although the death rate from hysterectomy is low (under 1 percent), surgical complications include the following:
• Infection. Most infections can be treated successfully with antibiotics, but some can be severe or even uncontrollable.
• Hemorrhage at the time of surgery or afterward (a transfusion or second operation may be necessary).
• Damage to your internal organs, most frequently the urinary tract and sometimes the bowel. Sometimes there is damage to the ureter (tube connecting the kidney to the bladder) or the bladder.
Less common surgical complications include blood clots, complications from the anesthesia, and intestinal obstruction from postsurgical scarring.
For those of us who are in our early forties or younger, removal of the uterus and ovaries may increase the risk of heart attack. Even if our ovaries are not removed, there is an increased chance of an earlier menopause. This is usually due to the decreased supply of blood to the ovaries, so that they lose their ability to produce hormones, either immediately or over time. Many physicians assure us that we can avoid these risks by taking estrogen, but estrogen therapy does not substitute for functioning ovaries (see Chapter 20, “Perimenopause and Menopause”).
Hormonal effects of hysterectomy with oophorectomy vary from one woman to the next. Some women suffer severe hot flashes and lack of lubrication. Some women use hormone therapy for a while, then gradually taper off. Long-term symptoms sometimes associated with hysterectomy and/or oophorectomy include constipation, urinary incontinence, bone and joint pain, pelvic pain, and depression.
Many women are concerned about the effect that hysterectomy, with or without oophorectomy, will have on sexual response. Some physicians and popular literature suggest that any sexual difficulties we may experience are “all in our head.” In fact, there is some physiological basis for these problems. For women who experience orgasm primarily when a partner’s penis or fingers push against the cervix and uterus (causing uterine contractions and increased stimulation of the abdominal lining), that kind of sensation may be lost if the uterus and cervix are removed. This is probably an individual response and has not been proved in studies. In addition, if the ovaries are removed, hormone levels drop sharply, and that can affect sexual feelings:
I had a hysterectomy two years ago at the age of 45. I went from being fully aroused and fully orgasmic to having a complete loss of libido, sexual enjoyment, and orgasms immediately after the surgery. I went to doctors, all of whom denied ever having seen a woman with this problem before and told me it was psychological. Before surgery, my husband and I were having intercourse approximately three to five times a week, simply because we have an open and loving relationship. Now I find that I have to work at becoming at all interested in intercourse. And I no longer have the orgasm that comes from pressure on the cervix, although I still have a feeble orgasm from clitoral stimulation.
Testosterone, a hormone that contributes to muscle strength, appetite, and sex drive, can increase sexual desire in women whose ovaries have been removed, but it may have masculinizing side effects, such as a lowered voice, acne, and facial hair. Side effects can be limited by using low-dose testosterone cream or gel. However, even in low doses, these products have not been adequately tested for long-term safety.
Local effects of surgery may occasionally cause problems. Vaginal lubrication tends to lessen after hysterectomy and oophorectomy, and intercourse may be uncomfortable if your vagina has been shortened by the operation, or if there is scar tissue in the pelvis or at the top of the vagina. In order to minimize scarring, preserve nerve function and ligament support, and avoid shortening the vagina, some physicians recommend leaving the cervix in if no cancer was involved.
However, for many women, sex is unchanged or even more enjoyable after hysterectomy, since painful symptoms are gone. In the words of a woman who had a hysterectomy because of huge fibroids:
I had terrible cramps all my life and genuine feelings of utter depression during my periods. My ovaries were not removed, and my libido was not affected. My sexual response, if anything, improved. I also had for the first time no fear of unwanted pregnancy and more general good health.
Consider the benefits of surgery against the possibility of changes in sexual desire or response that can’t be predicted in advance. Treatments less drastic than a hysterectomy can usually reduce pain and bleeding from benign uterine conditions and improve overall wellbeing.
Total hysterectomy, sometimes called complete hysterectomy: The surgeon removes the uterus and cervix, leaving the fallopian tubes and ovaries. You may continue to ovulate but will no longer have menstrual periods; instead, the egg will be absorbed by the body into the pelvic cavity.
Total hysterectomy with bilateral salpingooophorectomy: The surgeon removes the uterus, cervix, fallopian tubes, and ovaries. One ovary may be left in, if it is not diseased. In rare cases (usually to treat widespread cancer), the surgeon will remove the upper part of the vagina and perhaps the lymph nodes in the pelvic area. The latter is called radical hysterectomy.
Supracervical (or subtotal) hysterectomy: This procedure leaves in the cervix, to limit the effect of surgery on the function and anatomy of the vagina. It’s also less likely to interfere with nerves and arteries as well as ligaments that support the vagina. If the cervix is left in, you still need Pap tests.
The uterus can be removed either through an abdominal incision or through the vagina. Surgeons sometimes prefer an abdominal approach because it enables them to see the pelvic cavity more completely. The incision is made either horizontally, across the top pubic hairline, where the scar hardly shows afterward, or vertically, between the navel and the pubic hairline. Vertical incisions tend to heal more slowly.
Vaginal hysterectomy has the advantage of a shorter recovery period and faster healing. Because the incision is inside the vagina, you won’t have a visible scar. Laparoscopically assisted vaginal hysterectomy (LAVH) enables the surgeon to see an image of the pelvic cavity without the downside of a large incision. Vaginal hysterectomies are performed increasingly frequently and require greater skill, so it’s important to find a surgeon who does them regularly. Mistakes during surgery can result in permanent urinary tract difficulties. Other disadvantages include a possible shortening of the vagina, which can result in painful intercourse afterward and temporary (but severe) back pain.
Minimally invasive loparoscopic techniques (where the pelvic organs are visualized through a small scope placed through the belly button) are used more frequently now to avoid the long recovery and large scar associated with the abdominal approach. Because only small incisions are required, the recovery is dramatically better. Just be sure to find a surgeon experienced in these relatively new techniques.
After a hysterectomy, you may be in the hospital for as few as one or as long as several days, depending on the kind of procedure, the amount of anesthesia, and your general health. For the first day, you will probably have an IV and a catheter inserted in your bladder. You will usually be given medication for pain and nausea. Within a day, you can expect to be on your feet and encouraged to do exercises to get your circulation and breathing back to normal. You may also be told to cough frequently to clear your lungs. (Holding a pillow over an abdominal incision, or crossing your legs if you had a vaginal incision, will help reduce pain from coughing.) You may also have gas pains to contend with. A self-help technique to dispel abdominal gas uses heat applied to an acupressure point beneath the navel. Walking, holding on to a pillow and rolling from side to side in bed, and slow deep-breathing exercises may help, too. You can begin to have light solid foods, as well as fluids, when you feel able to keep them down. Hospital stays are growing shorter and shorter. This can be scary, but once your IV is out and you can keep down oral pain medications, being at home with good help may provide many comforts and avoids the risk of catching an infection in the hospital. Plan ahead to make sure you have the support you need (family, friends, or community support services).
After you go home, you may have light vaginal bleeding or oozing that gradually tapers off. You may also have hot flashes caused by estrogen loss, even if your ovaries were not removed. You will probably continue to have some pain, despite taking pain medication. Consult your medical practitioner if you have fever, nausea and vomiting, or foul vaginal discharge, as this may signal an infection.
Try to arrange for someone to take care of you for the first few days. You can expect to feel tired, so ask family and friends for help with household chores and children for at least the first few weeks. Your health care provider may tell you to avoid tub baths, douches, driving, climbing, or lifting heavy things for several weeks. If you have to drive or need to carry small children, ask for suggestions about how and when you can do these tasks safely.
Full recovery generally takes four to six weeks, but some women feel tired for as long as six months or even a year after surgery. Most medical practitioners also recommend waiting six to eight weeks before resuming sex and/or active sports, but some women return to them earlier. Start with light exercise, such as walking, and gradually build up to your old routines.
Some women feel only relief following hysterectomy, especially when the operation eliminates a serious health problem or chronic, disabling pain. But even if you were prepared for it and did not expect to feel depressed, you might cry frequently and unexpectedly during the first few days or weeks after surgery. This may be due to sudden hormonal changes. Many of us are also upset by losing any part of ourselves, especially a part that is so uniquely female. Acknowledging feelings of anger and grief after losing a part of yourself or some of your sexual responsiveness is an important part of the recovery process.
Some gynecologists recommend psychiatric help and prescribe antidepressants or tranquilizers (or other habit-forming drugs) while ignoring treatment of underlying physical or sexual conditions caused by the surgery. Often, talk therapy alone—or conversations with friends and family—enables us to cope with any posthysterectomy depression. Some women have started their own postsurgery support groups by networking in their community. Visit HERS Foundation (hersfoundation.org) for more resources.
Vulvitis, or inflammation of the vulva, may be caused by one of several medical conditions, medicated creams, or external irritants. It can also be caused by an injury; oral sex; a bacterial, viral, or fungal infection; sitting in a hot tub; allergies to common commercial products such as body soaps, powders, and deodorants; or irritation from sanitary napkins, synthetic underwear, or panty hose. Vulvitis often accompanies vaginal infections. Stress, inadequate diet, and poor hygiene can increase the likelihood of vaginal infections. Women with diabetes may develop vulvitis because the sugar content of their cells is higher, increasing susceptibility to infection. Postmenopausal women often develop vulvitis because as hormone levels drop, the vulvar tissues become thinner, drier, and less elastic and therefore more prone to irritation and infection.
Symptoms of vulvitis include itching, redness, swelling, burning, and pain. Sometimes fluid-filled blisters form that break open, ooze, and crust over (these could also be herpes). Scratching can cause further irritation, pus formation, and scaling, as well as secondary infection. Sometimes, as a result of scratching, the skin whitens and thickens.
Women with this problem tend to overclean the vulva, contributing to further irritation. Wash once a day with warm water only.
The first step in treating vulvitis medically is to make a diagnosis. Depending on the cause, your health care provider may prescribe antifungal creams or antibacterial treatment. Cortisone cream or other soothing lotions can relieve severe itching. (Low-dose cortisone creams are good for a short time; fluorinated ones can cause thinning and atrophy of the skin if used for a long time, though these may be required for some conditions.) Postmenopausal women may be given a form of local estrogen. If you have a vaginal infection or herpes, treating these problems will usually clear up the vulvitis as well.
If the vulvitis persists or worsens, you may need a vulvar biopsy to rule out the possibility of cancer or chronic vulvar conditions such as lichen sclerosus, a skin disease that can produce itching, bruising, pain, and scarring. This biopsy can be done in the practitioner’s office with local anesthetic.
Discontinue using any substances that might be a cause of vulvitis. All commercial preparations may be irritating, including antifungal agents and lubricants containing propylene glycol. Keep your vulva clean, cool, and dry—and remember to wipe from front to back. Hot boric acid compresses and hot sitz baths with comfrey tea are soothing. Use unscented white toilet paper (as perfumes and dyes may be aggravating) and soft cotton or linen towels, and wear cotton underwear to prevent chafing. Aveeno colloidal oatmeal bath and cold compresses made of plain, unsweetened, live-culture yogurt or cottage cheese also help relieve itching and soothe irritation. Calamine lotion can be used to address itching. Use a sterile, nonirritating lubricant such as K-Y jelly or Astroglide during intercourse and other genital sex.
Vulvodynia is the term developed in 1976 by the International Society for the Study of Vulvovaginal Disease to describe chronic vulvar pain. Women with vulvodynia experience severe burning, pain, itching, stinging, and/or irritation in the vulva (external genitals).
Vulvar pain can be related to a known disorder such as a bad yeast infection or a herpes outbreak. Recently clinicians have learned that pelvic floor muscle spasm or tightness (caused by a variety of conditions) is a major source of vulvar pain.
Vulvar pain in the absence of relevant visible finding or clinically identifiable disease is called vulvodynia. There are two kinds of vulvodynia. In generalized vulvodynia, symptoms occur in different areas of the vulva, at various times and sometimes even when the vulva is not being touched. In localized vulvodynia (formerly called vestibulodynia, vulvar vestibulitis, or localized vulvar dysesthesia), women feel pain mainly in an area just around the vaginal opening (the vestibule), usually when that area is touched or pressed. (For more information about the anatomy of the vulva, see Chapter 1, “Our Female Bodies.”)
As many as 3 to 15 percent of women have chronic vulvar pain.21 Even so, it can be hard to get a proper diagnosis for it, let alone successful treatment. If your vulva hurts, it is essential to find a health care provider who is familiar with vulvodynia. To rule out vulvovaginal conditions that are known causes of pain, she or he should do a full history, pelvic exam and pH examination of vaginal secretions (wet mount), and vaginal cultures if indicated. During a pelvic exam, the practitioner evaluates the architecture and appearance of your vulva. Then she or he will lightly touch areas on your vulva with a cotton swab (Q-tip) to see where it’s sensitive. This may be painful; feel free to bring a close friend or partner with you into the exam room.
It started within the first few times I ever had sexual intercourse. Here I was with this wonderful partner, but the sex hurt so much it made us both cry—me from the physical pain, him because I hurt so much. Once it started, the pain would come back whenever something touched my vulva: a tampon, a finger, a speculum (that was the worst). I saw several nurses and doctors; the first doc told me I was just “tight” and needed to relax. Did she have any idea how insulting, demoralizing, and belittling that was? Finally, I found a physician who respected me, recognized that my pain was real, and was able to give it the label of vulvodynia. Even having a name for it helped. I’ve since tried many treatments, some more successful than others. Three years later, I’m thrilled to report that my wonderful partner and I are able to have pain-free sexual intercourse (as well as continue to share other kinds of physical intimacy)—my [vulvodynia] isn’t totally gone, but it’s on its way out!
Because the causes of vulvodynia remain uncertain, there is no standard treatment. You and your clinician will first attempt to identify and treat possible pain triggers, including:
• Irritants applied to the vulva or activities that have an impact on the vulva
• Inflammatory problem such as Candida or inflammatory vaginitis (an uncommon vaginitis)
• Viral infections such as herpes
• Vulvar skin problems
• Interstitial cystitis (causing urinary and bladder pain)
• Blocked Bartholin duct (a Bartholin gland cyst occurs when a pea-sized organ under the skin on either side of the labia gets blocked and fluid fills up in the gland)
• Pelvic floor muscle spasms
If pain persists, treatment may include:
• Application of estrogen cream in the vagina, especially if there is atrophy in the vaginal walls.
• Low-dose tricyclic antidepressant, such as amitriptyline, to reduce central nervous pain; some clinicians think there is a connection between pain and the abundance of nerves in the vulva area in some women.
• Physical therapy to evaluate and treat the back and/or pelvic floor; even if there are no apparent muscle spasms, pelvic floor exercises have been found to strengthen pelvic muscles and reduce vulva pain caused by touch.
• Topical anesthetic ointment applied prior to or after intercourse.
• Exploring possible relationship issues or past sexual experiences that could contribute to painful sex; referral to a sex therapist or counselor if needed.
Experts agree that it is a combination of treatments, not any one modality, that is usually successful. If other treatments fail, some experts offer surgery such as vestibulectomy, which is the surgical removal of the vestibule and the hymen. Others feel that the studies showing success of surgery are flawed because of lack of clear definitions of pain and a lack of clear criteria for selecting the women. Other experimental treatments include Botox, which some small studies have found helpful.
Find a supportive practitioner who is knowledgeable about the vulva and has the time and knowledge to explore treatment options with you. If you have a partner, it is important to educate him or her about vulvodynia and, together, explore options for physical intimacy (see Chapter 8, “Sexual Challenges”). Also consider connecting with a support group to share stories and successes.
The National Vulvodynia Association (nva.org) offers more information on pain management and treatment, including helpful lists of potential irritants, and can help you find referrals to clinicians and support groups in your area.
Vulvar cancer is relatively rare. Women who have had HPV infections seem to be at greater risk, and some experts believe that vulvar cancer rates will rise sharply in the future because of increased rates of HPV infections. There is no screening test for vulvar cancer, however, and many women are treated for other conditions before realizing a biopsy should be done.
Be aware of changes in your vulvar area such as persistent itching or irritation, and especially growths. Don’t be afraid to look. Request a biopsy if you find a suspicious lump or lesion. Because vulvar cancer typically grows slowly, early detection can mean the difference between minor surgery and the more emotionally and physically devastating experience of losing one’s genitals. More extensive surgery is also more likely to lead to complications such as problems with sexual functioning. If lymph glands are removed, fluid buildup in the thighs can cause swelling, making mobility difficult.
All women secrete moisture and mucus from the membranes that line the vagina and cervix. This discharge is clear or slightly milky and may be somewhat slippery or clumpy. When dry, it may be yellowish. When a woman is sexually aroused, under stress, or at midcycle, this secretion increases. It normally causes no irritation or inflammation of the vagina or vulva. If you want to examine your own discharge, collect a sample from inside your vagina—with a washed finger—and smear it on clear glass (such as a glass slide).
Many bacteria normally grow in the vagina of a healthy woman. Some of them, especially lactobacilli, help to keep the vagina healthy, maintaining an acid pH (less than 4.5), and control overgrowth of potentially bad bacteria.
When vaginal infections occur, you may have abnormal discharge, mild or severe itching and burning of the vulva, chafing of the thighs, and (in some cases) frequent urination. Chronic vaginal (and vulvar) symptoms sometimes result from skin conditions of the vulva and vagina, such as eczema or psoriasis.
Vaginal infections may be due to lowered resistance (from stress, lack of sleep, poor diet, other infections in our bodies); douching or use of scented sprays; pregnancy; taking birth control pills, other hormones, or antibiotics; diabetes or a prediabetic condition; cuts, abrasions, and other irritations in the vagina (from childbirth, intercourse without enough lubrication, tampons, or using an instrument in the vagina medically or for masturbation). Infections are also transmitted during sex with an infected partner (see Chapter 11, “Sexually Transmitted Infections”). Chronic vaginal infections are infrequently a sign of serious medical problems such as HIV infection and diabetes.
The usual treatment for vaginitis is some form of antibiotic—which can also disturb the delicate balance of bacteria in the vagina and may actually encourage other infections (such as yeast) by altering the vagina’s normal acid/alkaline balance (pH). Some antibiotics also have unpleasant or even dangerous side effects.
As an alternative to antibiotics for vaginitis, some women find that natural and herbal remedies can help restore the normal vaginal flora and promote healing, though there are no studies showing how effective most of them are. Some women have tried soothing herb poultices or sitz baths (sitting in the tub with just enough water to immerse your thighs, buttocks, and hips). You should not rely on these remedies if you have an infection that involves your uterus, fallopian tubes, or ovaries.
Below is information about yeast (candida) infections and bacterial vaginosis. Trichomoniasis (“trich”), another common vaginal infection, is almost always transmitted sexually and thus is discussed in Chapter 11, “Sexually Transmitted Infections.”
Candida albicans, a yeast fungus often called simply candida, grows in the rectum and vagina. It grows best in a mildly acidic environment. The pH in the vagina is normally more than mildly acidic. When we menstruate, take birth control pills or some antibiotics, are pregnant, or have diabetes, the pH becomes more alkaline. In a healthy vagina, the presence of some yeast may not be a problem. When our system is out of balance, yeastlike organisms can grow profusely and cause a thick white discharge that may look like cottage cheese and smell like baking bread. Sometimes this causes intense itching, while at other times it just causes intermittent burning or a sense of irritation.
One study about the risk of recurring yeast infections found that sexual behaviors, rather than the presence of candida fungus on the male partner, were associated with recurrences. Women who had not had candida infections in the vulvovaginal area during the previous year were able to masturbate with saliva without increasing their risk of a candida infection, whereas women with a recent history of such infection in the vulvovaginal area increased the likelihood of a recurrent infection if they masturbated with saliva.22
The only way to be sure that an infection is caused by candida and not something else is to have vaginal secretions analyzed under a microscope. In some cases, it helps to get a lab culture done. Other conditions causing vaginal irritation may respond temporarily to treatment for candida and then recur a short time later, so accurate diagnosis is important. Self-diagnosis is inaccurate more than half the time, so hold off from self-treatment until diagnosis by a health care provider.
Treatment usually consists of some form of vaginal suppository or cream or an oral antifungal. The former is available over the counter, while pills require a prescription. Antifungal external creams such as clotrimazole may reduce or even eliminate the symptoms, sometimes without actually curing the infection. A small percent of woman have recurrent or chronic yeast infections. Prolonged oral treatment is sometimes required but should be based on a yeast culture. Suppositories and creams have fewer side effects than oral medications, and they can be used during pregnancy. If a woman has a yeast infection when she gives birth, the baby will be likely to get yeast in its throat or digestive tract. This is called thrush and is treated orally with nystatin drops.
Other treatments for candida infection involve boric acid capsules or painting the vagina, cervix, and vulva with gentian violet. The latter is bright purple and stains, so a sanitary pad must be worn. This procedure can help, but in occasional cases, women have a severe reaction to gentian violet. Side effects are rare with boric acid, but it may cause vaginal burning and itching. Do not use boric acid near any cuts or abrasions, as it can enter the bloodstream and may cause nausea, vomiting, diarrhea, dermatitis, and kidney damage. Boric acid is never taken orally and is typically used only after other FDA-approved treatments have failed.
Some of us have had success with the following remedies: acidifying the system by drinking eight ounces of unsweetened cranberry juice every day, or taking cranberry concentrate supplements; inserting plain, unsweetened, live-culture yogurt in the vagina; inserting garlic suppositories (to prevent irritation, peel but don’t nick a clove of garlic, then wrap in gauze before inserting). An effective and inexpensive treatment for candida infection is potassium sorbate, commonly used as a preservative in home brewing of beer. Dip a cotton tampon in a 3 percent solution (15 grams of dry potassium sorbate in 1 pint of water), then insert into the vagina at night and remove in the morning.
Also try to boost your immune system by reducing sugar in your diet and getting more rest. Avoid douches and don’t use tampons for your period when you have an infection. If you have a male sex partner, have him apply antifungal cream to his penis twice a day for two weeks, especially if he’s not circumcised.
For a long time I felt as though I were on a merry-go-round. I would get a yeast infection, take Mycostatin for three weeks, clear up the infection, and then find two weeks later that the itching and the thick, white discharge were back. Finally, I discovered that reducing my sugar intake and drinking unsweetened cranberry juice would help prevent repeat infections.
Bacterial vaginosis (BV) is a disturbance of the ecology of the vagina, with an overgrowth of certain microorganisms (possibly including mycoplasmas, gardnerella, and anaerobic bacteria). Many women with BV are unaware that they have it. Some practitioners believe it can be caused by routine douching; it may also be triggered by infections, including STIs. The symptoms can be confused with those of trich, though the discharge tends to be creamy white or grayish and is especially foul-smelling (some call it “fishy”), especially after intercourse. It sometimes comes and goes, getting better after a period and worse again as a woman’s cycle progresses.
Medication treatment is usually either metronidazole or clindamycin, taken orally or vaginally for five to seven days. Single-dose oral metronidazole may also be effective but less so (cure rates range from 40 to 60 percent). Metronidazole is sometimes used first, because it spares the lactobacilli in your vagina and is less likely to trigger a yeast infection. Vaginal treatment avoids systemic side effects but is more expensive than the five-to-seven-day pill regimens.
Some women will have another BV outbreak within nine months of initial treatment. Long-term condom use may help to prevent recurrent infection. Women with BV have more frequent infections following gynecologic surgery, and some studies suggest that BV increases the risk of giving birth prematurely if you have it during pregnancy.
Self-help treatments include general vaginitis prevention measures and taking extra vitamins B and C. You can help prevent recurrences by minimizing the use of tampons, avoiding douching, and using condoms (to offset the alkaline effect of semen). Alternative treatments may provide temporary relief but not an actual cure. Vaginal and oral use of yogurt doesn’t help with BV.
The urinary bladder is an expandable muscular organ that stores our liquid waste (urine) so we can excrete it intermittently. This organ is obviously not exclusively female, but because it sits so close to the other organs that are unique to women, gender-specific issues exist.
Urinary tract infections (UTIs) are so common that most of us get at least one at some point in our lives. They are usually caused by bacteria, such as E. coli, that get into the urethra and bladder (and occasionally the kidneys) from the gastrointestinal system. Trichomoniasis, chlamydia, and viruses can also cause UTIs. Low resistance, poor diet, stress, and trauma to the urethra from childbirth, surgery, and catheterization can predispose you to getting them. A sudden increase in sexual activity can be a trigger (hence the term “honeymoon cystitis”). Pregnant women are especially susceptible, as pressure from the growing fetus keeps some urine in the bladder and ureters (the tubes carrying urine from the kidneys to the bladder), allowing bacteria to grow.
Postmenopausal women are also susceptible because of the effect of hormonal changes on the bladder and urethra. Occasionally, UTIs are caused by a congenital anatomical abnormality or, mostly in older women or women who have had many children, a prolapsed (fallen) urethra or bladder.
Cystitis (inflammation or infection of the bladder) is by far the most common UTI in women. While the symptoms can be frightening, cystitis in itself is not usually serious. If you suddenly have to urinate every few minutes and it burns like crazy even though almost nothing comes out, you probably have cystitis. There may also be blood and/or pus in the urine. You may have pain just above your pubic bone, and sometimes there is a peculiar, heavy odor when you first urinate in the morning.
It’s also possible to get mild temporary symptoms (such as peeing frequently) without actually having an infection, simply because of drinking too much coffee or tea (both are diuretics), premenstrual difficulties, food allergies, vaginitis, anxiety, or irritation to the area from bubble baths, soaps, or douches. As long as you are in good health and not pregnant, you can usually treat mild symptoms yourself for twenty-four hours before consulting a practitioner.
Cystitis often disappears without treatment. If symptoms persist beyond forty-eight hours, recur frequently, or are accompanied by chills, fever, vomiting, and/or pain in the kidneys (near the middle of the back), see a doctor. These symptoms suggest that infection has spread to the kidneys, resulting in pyelonephritis, a serious problem that requires medical treatment. Also see your provider if you have blood or pus in the urine, pain on urination during pregnancy, diabetes or chronic illness, or a history of kidney infection or diseases or abnormalities of the urinary tract. Untreated chronic infections can lead to serious complications, such as high blood pressure or premature births (if occurring during pregnancy).
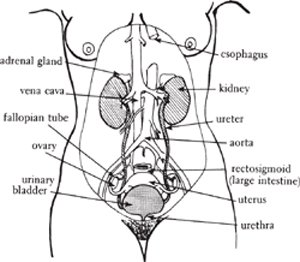
© Nina Reimer
When cystitis does not respond to self-help treatments within twenty-four hours, or it recurs frequently, get a urine test. Make sure your provider asks for a clean voided specimen23 and does a pelvic exam to rule out other infections. Your urine should be examined for evidence of blood and pus, then cultured. Sometimes, even when you have symptoms, the culture may come back negative (not show any infection). False-negative cultures may be due to mishandling or too-dilute urine; you may also get a false-negative report if your cystitis is caused by something other than bacterial infection. White blood cells in the urine plus a negative culture (acute urethral syndrome) may indicate a chlamydia infection. Some women have bacteria in the urine without symptoms; especially in pregnant women, this should be treated with antibiotics to prevent kidney infection and other complications.
For symptoms that are severe or indicate a kidney infection, medications are usually started immediately. For milder infections, many health care providers prefer to wait for culture results before prescribing a drug. Most UTIs respond rapidly to a variety of antibiotics. Drugs commonly used include ampicillin, nitrofurantoin, tetracycline, ciprofloxacin, a sulfamethoxazole and trimethoprim combination (Bactrim/Septra), and sulfonamides (Gantrisin). (Women who have a deficiency of glucose-6-phosphate dehydrogenase should not take sulfonamides.) You may get a single large dose or several doses spread out over three to ten days.
If symptoms persist longer than two days after you start taking drugs, contact your health care provider again. The organisms may be resistant to the antibiotics you are using. Eating plain, unsweetened live-culture yogurt or taking acidophilus in capsule, liquid, or granule form may help to prevent diarrhea or yeast infection by replacing the normal bacteria in your intestines that can be destroyed by the drugs.
Acetaminophen may relieve pain from UTIs. Some practitioners recommend a drug called Pyridium, an anesthetic that relieves pain but does not treat the infection itself. (Pyridium dyes the urine a bright orange, which will permanently stain clothing. It also can cause nausea, dizziness, and possibly allergic reactions.)
Surgical treatment for UTIs should be limited to specific situations in which a woman’s anotomy is clearly causative. Pelvic exercises known as Kegels can forestall the need for this operation and help prevent future infections.
Even with drugs and/or surgery, many women continue to have recurrent urinary tract infections. Sometimes it helps to treat chronic infections with long-term, low-dose medications.
Urinary incontinence is a condition where women lose urine unintentionally. It often first appears during pregnancy as a result of pressure from the growing fetus on the bladder. Damage related to birth traumas may cause ongoing urinary incontinence, as can pelvic surgery. Some women will develop incontinence with advanced age, even without any specific traumas. If the condition is mild, simply using menstrual pads to collect leaking urine may be an adequate solution. A thorough evaluation can help determine what treatment approaches might be most effective. These include bladder training, pelvic flow exercises, medication, and surgery.
Painful bladder syndrome/interstitial cystitis (PBS/IC) was for many years thought to be an inflammatory condition of the bladder wall, but recently it has been recognized as poorly understood chronic pain syndromes that develop for multiple reasons. A clinical diagnosis is based primarily on symptoms of urgency/frequency of urinating and pain in the bladder and/or pelvis.24 Standard treatments of many decades are no longer routinely considered effective. One large urological study from 2000 concluded that “no current treatments have a significant impact on symptoms with time.”25
PBS/IC is at least five times more common in women than men, affecting close to 500,000 females in the United States, with an average age of onset of about forty years; 25 percent of those affected are under age thirty.
PBS/IC has symptoms similar to those of the common urinary tract infection known as cystitis. However, with PBS/IC, routine urine cultures are negative, and there is usually no response to antibiotics. You may feel pelvic pain and pressure and an urgent need to urinate, sometimes as often as sixty to eighty times a day. You may also have vaginal and rectal pain. Pain during sexual intercourse is common. The symptoms can vary from mild to severe.
PBS/IC may be incorrectly diagnosed as urethral syndrome or trigonitis, or you may be told there’s nothing wrong and that you have a “sensitive bladder.” A complete battery of urologic tests typically produces negative results. Conditions that have similar symptoms include bladder infections, kidney problems, vaginal infections, endometriosis, and sexually transmitted infections (STIs).
There is no consistently effective treatment or cure for PBS/IC. However, the most commonly recommended approaches are:
• Medication, including nonsteroidal anti-inflammatory drugs, antispasmodics, and antihistamines. Pentosan polysulfate sodium (Elmiron), an oral medication, may protect the bladder from irritants in the urine.
• Low-dose antidepressants, which appear to have antipain properties
• Diet changes, eliminating caffeinated beverages, alcohol, artificial sweeteners, spicy foods, citrus fruits, and tomatoes
• Transcutaneous electrical nerve stimulation (TENS) to block pain, using a small portable unit worn on the body
The following approaches all involve surgery, the benefits of which are sometimes unproved, and all of which pose significant risks:
• Bladder distention (hydrodistention) stretches the bladder by filling it with water while you are under regional or general anesthesia.
• Dimethyl sulfoxide (DMSO, Rimso-50), an anti-inflammatory medication, is placed directly into the bladder.
• Oxychlorosene sodium (Clorpactin) is placed directly into the bladder; regional or general anesthesia may be necessary for this.
• Major surgery (partial or complete removal of the bladder, or of certain nerves leading to the bladder) is often followed by severe complications and should be done only as a last resort.
Developing effective IC therapies is a major challenge facing all researchers in this field. The American Urological Association is planning to publish the first guidelines regarding methodology for diagnosis and treatment during 2011. In 2010, a large multicenter NIH-funded study reported on findings that myofascial physical therapy (specialized stretching of the thin tissue that covers all the organs of the body) was shown to be effective when compared with conventional massage techniques.28
Obstetric fistula is a childbirth injury that typically affects girls and women living in acute poverty throughout Africa and South Asia. Fistula is caused by prolonged and obstructed labor when the constant pressure of the baby’s head against the soft tissues of the vagina creates a hole between the bladder and the vagina, and sometimes between the rectum and the vagina. This leaves girls and women leaking urine and/or feces continuously from the vagina. It may also cause serious nerve damage to the legs, making it difficult or impossible to walk. Girls and women with fistula are often isolated and highly stigmatized. In most cases, the cost of an operation and the distance to a medical facility providing fistula services make surgical repair impossible. Fistula is entirely preventable, and it rarely or never occurs in the developed world. Women with this condition who immigrate to the United States or Canada may encounter health care providers who have never seen it before. For more information, see “Obstetric Fistula” at ourbodiesourselves.org.
Female genital cutting (FGC)—also called female genital mutilation or female circumcision—is a traditional cultural practice in some African countries as well as in several countries in Asia and the Middle East. It involves cutting parts of the external genitals of girls or young women as a rite of passage into womanhood and to curb sexuality. FGC may consist of removing the hood of the clitoris, part or all of the clitoris and/or labia minora (inner lips), and, in some cultures, part or all of the external genitalia. The vaginal opening may also be narrowed or stitched (infibulation). Pricking, piercing, burning, scraping, slashing, and corroding the female genitals are also considered to be FGC by the World Health Organization (WHO). As a result of an influx of refugees and immigrants, thousands of women in the United States are living with the results of these practices.
Short-term health complications of FGC include excessive bleeding, infection, and shock, mostly due to unsanitary conditions, failed procedures by inexperienced circumcisers, or inadequate medical services once a problem occurs. Long-term health complications are abscess formation, scar neuromas, dermoid cysts, keloids, recurrent urinary tract infections, painful sexual intercourse, and vulval adhesions that block the vagina. In women who are infibulated, obstruction of the urethra and vagina by scar tissue may result in urine retention and urethral and bladder stones, irregular or prolonged menstrual flow, chronic urinary tract infections, and chronic pelvic infection, which often leads to scarring of the fallopian tubes and infertility. Sexual and psychological issues are likely to emerge over time. In 2006, a major World Health Organization study provided strong evidence that FGC increases the risk of complications during childbirth and can lead to one to two additional perinatal deaths per one hundred births. For more information, see “Female Genital Cutting,”
Many circumcised women seek treatment for problems or issues related to FGC but may not always acknowledge or understand the connection. It is critical for health care providers to be sensitive to women in both discussing this issue and treating its negative consequences.
Pelvic relaxation is a condition in which the muscles of the pelvic floor become slack and no longer support the pelvic organs properly. In severe cases, the ligaments and tissues that hold the uterus in place may weaken enough to allow the uterus to fall (prolapse) into the vagina. Women sometimes experience pelvic relaxation and/or uterine prolapse after one or more very difficult births, but the tendency can also be inherited. Uterine prolapse is often accompanied by a falling of the bladder (a condition known as cystocele) and rectum (rectocele).
The first sign of pelvic relaxation is often a tendency to leak urine when you cough, sneeze, or laugh suddenly. If your uterus has fallen into the vagina, you may have a dull, heavy sensation in your vagina or feel as if something is falling out. You may have constipation, difficulty accomplishing a bowel movement, or an inability to control your bowels. These symptoms are usually worse after you have been standing for a long time.
Medical intervention is usually not necessary for pelvic relaxation or even mild uterine prolapse. If the prolapse is severe enough to cause discomfort, you can ask your doctor to insert a pessary—a rubber device that fits around the cervix and helps to prop up the uterus. Disadvantages include difficulty in obtaining a proper fit, possible irritation or infection, and the need to remove and clean the pessary frequently. A surgical procedure called a suspension operation can lift and reattach a descended uterus, and often a fallen bladder or rectum as well. Many medical practitioners recommend hysterectomy for prolapsed uterus, but it is usually unncessary and should be done only as a last resort in appropriate cases. It’s best to consult a surgeon who has expertise in this area and keeps up with new research. Urologists have special training in this kind of pelvic surgery.
The best way to prevent pelvic relaxation and uterine prolapse is to do regular Kegel exercises and leg lifts, which strengthen the muscles of the pelvic floor and lower abdomen (see “How to Do Kegel Exercises”). Check whether your pelvic muscles are in good shape by trying to start and stop the flow of urine while sitting on the toilet. If you can’t stop the flow, you need to do more Kegels. Some health care providers recommend doing them up to a hundred times a day, especially during pregnancy, when the pelvic muscles are under particular stress. You may also strengthen a slightly prolapsed uterus by relaxing in the knee-chest position (kneeling with your chest on the floor and your bottom in the air) several times a day. Some women find that certain yoga positions, such as the shoulder stand and headstand, relieve the discomfort of a prolapsed uterus.
Polycystic ovary syndrome (also called anovulatory androgen excess, polycystic ovarian disease, or Stein-Leventhal syndrome) is the most common hormonal and reproductive problem that affects women of childbearing age. It is a medical condition that may include a variety of ailments, making it difficult to diagnose. PCOS usually starts around the time of puberty but may become noticeable when a woman is in her twenties or thirties. Between approximately 5 and 8 percent of women experience this disorder.
PCOS is defined by the presence of any two of the following characteristics:
• Irregular menstrual cycles or lack of ovulation (release of an egg) for an extended period of time
• Elevated levels of androgens (male hormones) in the blood, or evidence for elevated androgens such as acne or excess unwanted hair growth (and head hair loss)
• Many small follicles (benign fluid-filled sacs) on the ovaries (resulting from not releasing eggs)
PCOS is diagnosed in large part by excluding other possible conditions that can cause similar signs and symptoms. Your health care provider will first administer blood tests or other exams to see if your body is making high doses of steroids, or if there are pituitary, adrenal, or ovarian tumors.
The exact cause of PCOS is unclear, although risk increases in women who are overweight. PCOS is more common in certain families. There is evidence for a genetic cause, but the exact gene(s) responsible have yet to be identified.
PCOS results from a combination of several related factors. Many women with PCOS have insulin resistance, in which the body cannot use insulin efficiently. This leads to high blood levels of insulin, called hyperinsulinemia. It is believed that hyperinsulinemia is related to increased androgen levels, as well as to obesity and type 2 diabetes. In turn, obesity can also cause insulin resistance and increase the risk for or worsen PCOS.
Large amounts of androgens can block egg growth and ovulation. Because they are male sex hormones, they can also cause women to develop male secondary sex characteristics such as facial hair or hair thinning at the front of the head.
When a woman has an ovulatory problem, her reproductive system does not produce the necessary amounts of hormones to develop, mature, and release a healthy egg. In this case, the ovaries become enlarged and develop many small follicles. These follicles produce androgens, which further interfere with ovulation. Some researchers believe that the cysts contain eggs that didn’t mature and didn’t get released during ovulation. Others disagree. Studies have shown that not every woman with PCOS has these numerous follicles. Nor does every woman with these numerous follicles have PCOS. Some women with polycystic ovaries have regular menstrual cycles.
The signs and symptoms of PCOS are related to hormonal imbalance (excess male hormones), lack of ovulation, and insulin resistance and may include:
• Irregular, infrequent, or absent menstrual periods
• Hirsutism—excessive growth of body and facial hair including hair on the chest, stomach, and back
• Acne or oily skin
• Enlarged and/or polycystic ovaries
• Problems with fertility
• Being overweight or obese, especially around the waist (central obesity)
• Male-pattern baldness or thinning hair
• Skin tags—small pieces of skin on the neck or armpits
• Acanthosis nigricans—darkened skin areas on the back of the neck, in the armpits, and under the breasts
In addition, women with PCOS may be at increased risk for developing certain health problems, including:
• Type 2 diabetes
• Elevated cholesterol levels. Triglycerides—fatty acids in the bloodstream—may be higher than normal in some women with PCOS, whereas HDL, the “good cholesterol,” may be lower than normal. This could raise the risk of heart attacks because arteries and other blood vessels are more likely to be narrowed or clogged over time.
• High blood pressure
• Elevated blood clotting factors
• Missed periods followed by prolonged and heavy bleeding
• Endometrial cancer. Lack of ovulation for an extended period of time may cause excessive thickening of the endometrium (the lining of the uterus). Abnormal cells may build up in the lining of the uterus when it is not shed regularly during a menstrual period. Eventually, some of these abnormal cells may turn cancerous.
• Some studies show a relationship between PCOS and breast cancer.
The symptoms of PCOS may resemble other conditions or medical problems. Always consult your physician for a diagnosis.
In addition to a complete medical history, a physical examination, including a pelvic exam, can be used initially to diagnose PCOS.
A variety of tests can also be used to detect PCOS. Blood tests are used to detect increased levels of androgens and other hormones. Other blood tests can measure blood sugar, cholesterol, and triglyceride levels.
Physicians sometimes use an ultrasound (also called a sonogram)—a diagnostic technique that uses high-frequency sound waves and a computer to create images of blood vessels, tissues, and organs. Ultrasounds are used to view internal organs as they function and to assess blood flow through various vessels. Ultrasound can determine if a woman’s ovaries are enlarged and if cysts or follicles are present, and also evaluate the thickness of the endometrium.
Sometimes it can be difficult to diagnose PCOS with certainty because of how it varies, both from woman to woman and even over time in the same woman.
Specific treatment for PCOS will be determined by your clinician based on your age, overall health, and medical history. In addition, your health care provider will take into account the extent of the disorder and expectations for improvement; your tolerance for specific medications, procedures, and therapies; and your preferences. Treatment also depends on whether or not you want to become pregnant.
For women who do not want to become pregnant, treatment is focused on treating the symptoms and preventing long-term consequences of the condition. Treatment may include the following.
Weight reduction: A healthy diet and increased physical activity allow more efficient use of insulin and decrease blood glucose levels, and also lower risk of heart disease and diabetes. Some women with PCOS who lose weight will start having regular periods.
Oral contraceptives: Birth control pills may be prescribed to regulate menstrual cycles, decrease androgen levels, control acne, prevent balding or hair thinning, and decrease facial hair.
Cyclic progesterone: Can be prescribed intermittently to ensure women don’t go too long without a period.
Spironolactone: A less common but often helpful treatment that can minimize excess hair growth. Other procedures such as bleaching, electrolysis, and laser hair removal may also be used to decrease facial hair.
Diabetes medication: Metformin, a medication used in the treatment of type 2 diabetes, is often used to decrease insulin resistance in PCOS. Some preliminary studies of women with PCOS who are insulin resistant show that such drugs may also help reduce androgen levels, hair growth, acne, balding, and body weight and may help a woman ovulate more regularly. No long-term studies of this form of treatment are available. Some studies have shown a reduction in the risk of miscarriage in pregnant PCOS patients taking metformin, while others have not. Your clinicians will discuss this with you if you become pregnant.
For women who want to become pregnant, treatment is focused on weight reduction and promoting ovulation and may include the following.
Weight reduction: A healthy diet and increased physical activity allow more efficient use of insulin and decrease blood glucose levels and may help a woman ovulate more regularly.
Ovulation induction medications such as Clomid: These medications stimulate the ovary to make one or more follicles (sacs that contain eggs) and release the egg for fertilization. Metformin is sometimes used for this purpose as well.
Surgery: In cases of infertility where drugs don’t work, surgical techniques that make small holes in one or both ovaries may be suggested. This surgery often restores ovulation, though not always permanently. Adhesions—scar tissue that can twist the ovaries or make them cling to other organs—are a potential drawback. Because of these concerns, this procedure is rarely performed today.