
Figure 22-1 A premature junctional contraction.
© Jones & Bartlett Learning.
As you can imagine, premature junctional contractions (PJCs) are junctional complexes that occur earlier than expected and are interspersed in the underlying rhythm for one or more cycles (Figure 22-1). The PJCs have the morphologic characteristics expected from any junctional complex (absent or buried P wave, inverted P waves in leads II, III, and aVF, and narrow supraventricular QRS complexes). PJCs are usually associated with a noncompensatory pause because the retrogradely conducted atrial impulse typically depolarizes and resets the sinoatrial (SA) node (discussed in Chapter 13, Premature Atrial Contraction). However, the pause may be fully compensatory when there is no retrograde conduction back toward the atria.

Figure 22-1 A premature junctional contraction.
© Jones & Bartlett Learning.
PJCs are a fairly common electrocardiographic phenomenon and can be found in people with and without structural and ischemic heart disease. They are typically caused by increased automaticity of the atrioventricular (AV) junction. They can occur singly or can be recurrent.
The coupling interval—the distance from the PJC to the previous QRS complex—can be fixed or variable. A fixed coupling interval (Figure 22-2) is commonly found in premature atrial contractions (PACs) and PVCs and represents an identical distance between the normal complex and the premature beat. PJCs typically do not have a fixed coupling interval, and the R-R interval between complexes is usually variable (Figure 22-3).
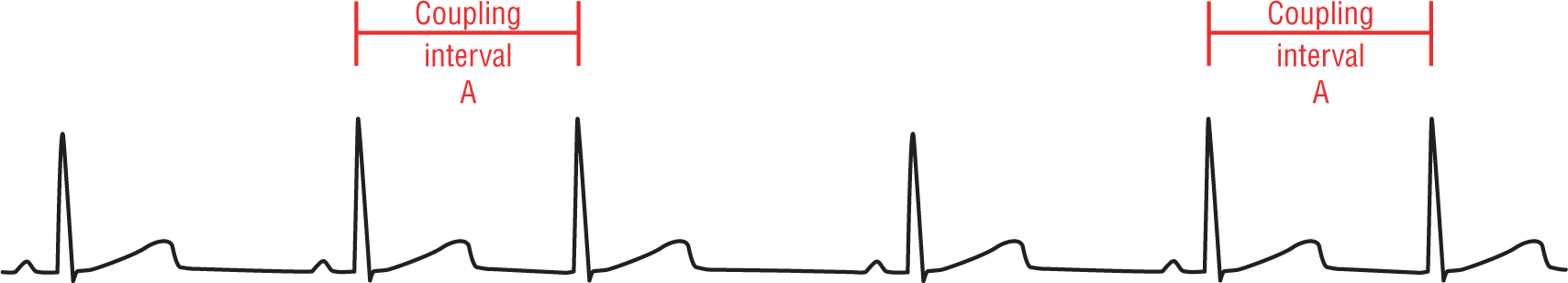
Figure 22-2 The coupling interval refers to the distance between the premature complex and the preceding normal beat found in the underlying rhythm. A fixed coupling interval is the same whenever an individual ectopic focus fires.
© Jones & Bartlett Learning.
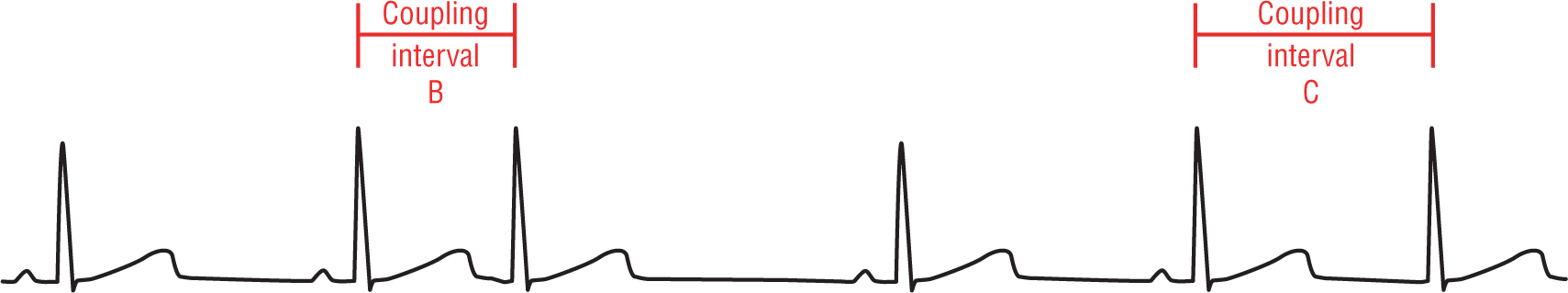
Figure 22-3 A variable coupling interval refers to a variability in the coupling distance every time the same ectopic focus fires.
© Jones & Bartlett Learning.
The supraventricular complexes of the PJCs typically have narrow QRS complexes associated with them. If the QRS complex is wider than 0.12 seconds, the usual causes include a preexisting bundle branch block, aberrantly conducted beats, electrolyte abnormalities, and fusion complexes with the T waves of the previous complexes.
Additional Information
PAC with Aberrancy vs. PJC with Aberrancy
We will look at the differential diagnosis of wide, aberrant complexes very closely in Chapter 27, Narrow-Complex Supraventricular Tachycardia, but certain points would be very helpful to discuss now. How can you tell if a complex is actually an aberrantly conducted PAC or an aberrantly conducted PJC? The answer is to look at the company it keeps. The events and appearance of the waves around it will be your best clue.
We have studied buried P waves before, but this topic deserves reinforcement. Start by looking at the T waves of the preceding complexes that are normally transmitted for that patient. The morphology of the T wave will most likely be identical from complex to complex. Mild variations may exist, but there should never be any gross differences. A gross difference in morphologic appearance, especially when associated with a premature complex, almost always signifies the presence of a buried P wave somewhere.
The morphology of a T wave will usually be altered by a buried P wave (Figure 22-4). This is because the ventricular repolarization process is slow and the forces that they generate are smaller than those that occur during an actual coordinated depolarization wave. Even the relatively low forces of atrial depolarization are enough to cause an electrocardiographic fusion to occur on the strip. (Notice that this refers to a fusion on the ECG because of the timing of the waves, and not an actual fusion of the waves themselves within the heart as we talked about in the last section.)
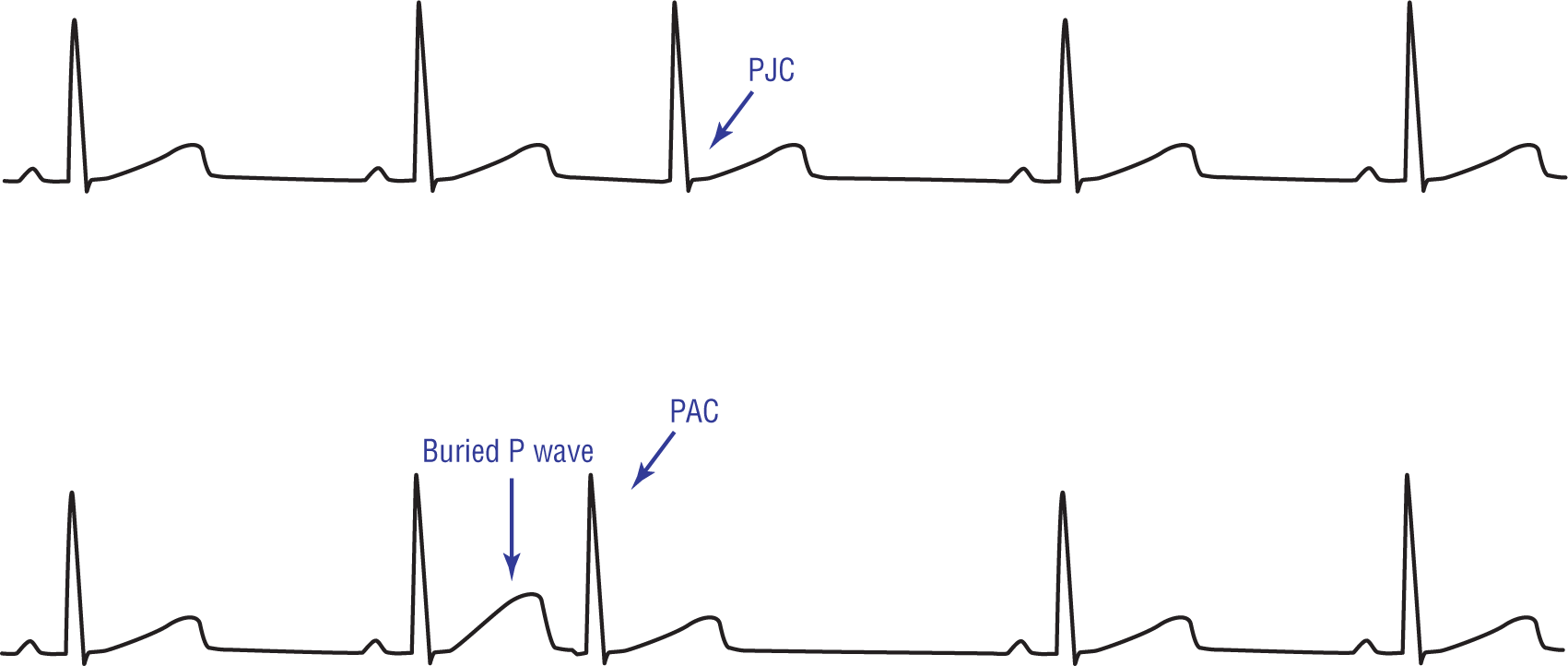
Figure 22-4 A strip showing a PJC and a strip showing a PAC with a buried P wave. Note the difference in the appearance of the T wave of the complex immediately before the PAC. The morphologic difference is due to the additive effects of the ectopic P wave and the T wave.
© Jones & Bartlett Learning.
DescriptionThe other thing that will help you to differentiate between a PAC with a buried P wave and a PJC is the type of pause involved. PACs are usually associated with noncompensatory pauses because the sinus node is usually reset by an ectopic atrial impulse. PJCs can have either compensatory or noncompensatory pauses. PJCs are associated with compensatory pauses when there is no retrograde conduction of the depolarization wave back toward the atria. PJCs are associated with noncompensatory pauses when the sinus node is reset by a retrograde P wave. Therefore, the presence of a compensatory pause favors the diagnosis of PJC.
Remember from Chapter 13, Premature Atrial Contraction, that ectopic atrial pacemakers may be associated with inverted P waves in leads II, III, and aVF. The P wave becomes inverted when the ectopic pacemaker is inferior and near the AV junction. By definition, therefore, a PJC will always have inverted P waves in leads II, III, and aVF. In addition, the PJC’s P wave can be before, after, or buried within the QRS complex. If the P wave occurs before the QRS complex in a PJC, the PR interval is almost always shorter than normal (<0.12 seconds) because it doesn’t have to undergo the full physiologic block because of its site of origin.
One of the toughest things in arrhythmia recognition is to correctly identify an aberrantly conducted PJC. To accomplish this feat, you need to keep a very close eye on the “company it keeps” and to look very closely at the area right at the start of the QRS complex.
An aberrantly conducted morphology occurs when a normally transmitted depolarization wave traveling down the electrical conduction system hits an area that is refractory to impulse transmission (Figure 22-5). From that point on, the impulse has to be transmitted down to the rest of the ventricles via direct cell-to-cell transmission. Because the very early portion of the QRS complex is always transmitted down the normal electrical conduction system, that portion will always be identical to the normally conducted complexes.
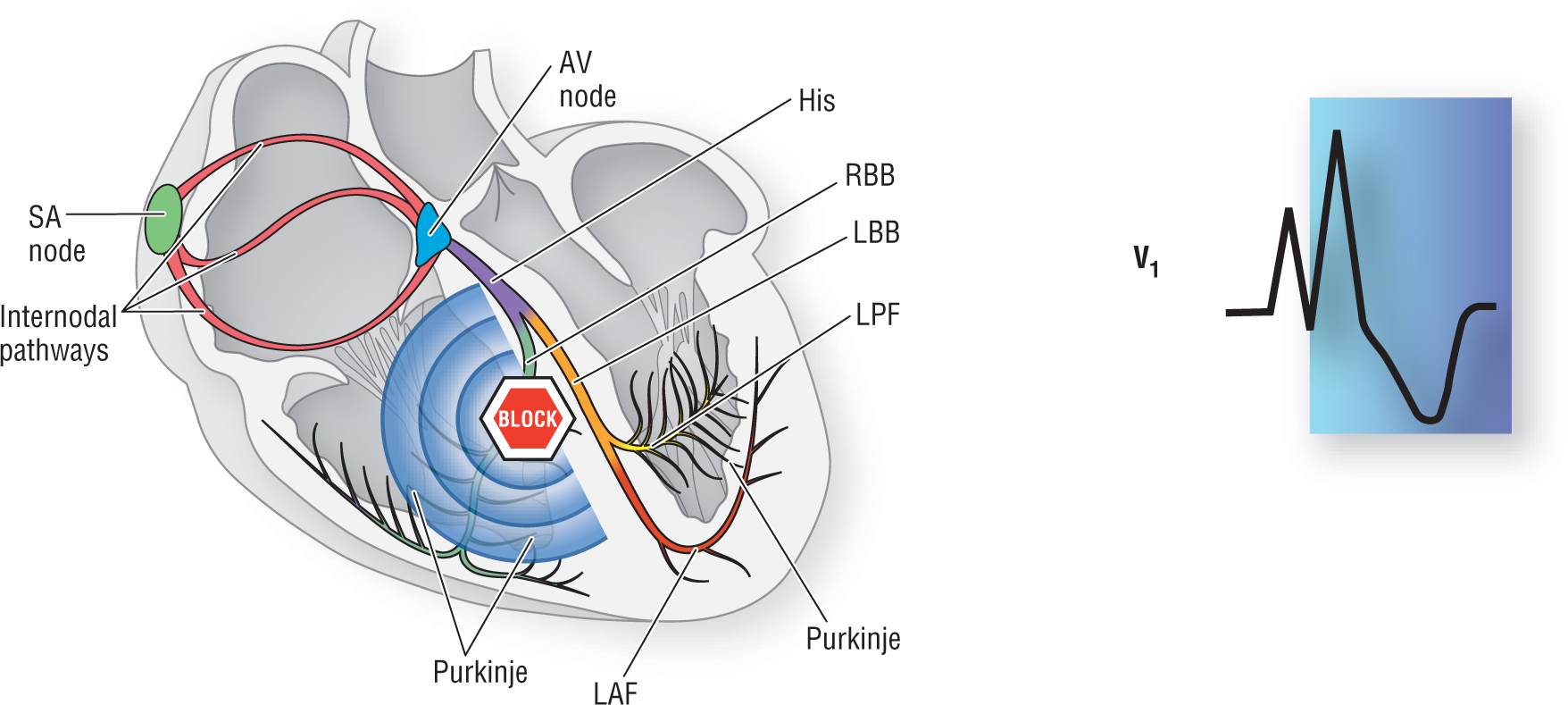
Figure 22-5 An aberrancy develops when an impulse traveling down the normal electrical conduction system hits an area of refractoriness. The cell-to-cell transmission that has to develop after that point causes the electrocardiographic aberrancy to develop.
© Jones & Bartlett Learning.
DescriptionAlways look at the first few milliseconds of the normally conducted QRS complex and compare it to the aberrantly conducted beat in question (Figure 22-6). As mentioned, this area is always identical to that of the normally conducted complexes. The number of milliseconds that are identically transmitted depends on the site of refractoriness that causes the aberration. If the refractory site is very close to the AV node, the amount of time will be very, very short. If the refractory site is farther down the electrical conduction system, the amount of aberrancy will be longer.

Figure 22-6 A normal sinus complex is shown in the first example, followed by an aberrantly conducted beat. Note how the initial few milliseconds of the two complexes are exactly identical. The number of milliseconds that are identically transmitted depends on the site of refractoriness that causes the aberration. If the refractory site is very close to the AV node, the amount of time will be very, very short. If the refractory site is farther down the electrical conduction system, the amount of aberrancy will be longer.
© Jones & Bartlett Learning.
DescriptionA good clinical tip to keep in mind is that if the complexes start in the same direction, especially if it occurs in multiple leads, the wide complex is probably an aberrantly conducted complex (Figure 22-7). If they start in opposite directions in multiple leads, it is most assuredly ventricular ectopic complex. We will be discussing this in greater detail in Chapter 30, Premature Ventricular Contraction.
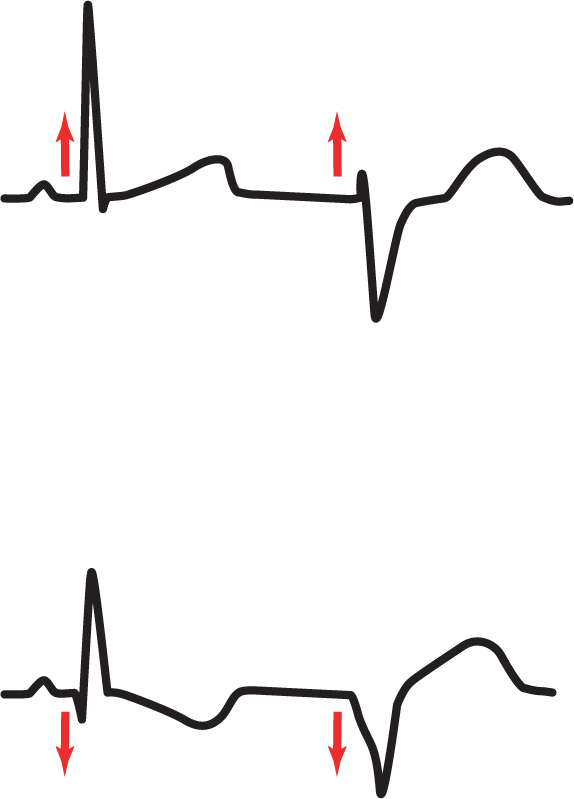
Figure 22-7 Always take a look at the direction of the start of the QRS. If the complexes are headed in the same direction, it is probably an aberrancy.
© Jones & Bartlett Learning.
DescriptionARRHYTHMIA RECOGNITION
Premature Junctional Contractions
| Rate: | Usually single events |
| Regularity: | Regular with an event |
| P wave:
Morphology: Upright in II, III, and aVF: |
Variable
Inverted Inverted |
| P:QRS ratio: | Variable |
| PR interval: | Short, if present |
| QRS width: | Normal |
| Grouping: | None |
| Dropped beats: | None |
DIFFERENTIAL DIAGNOSIS
Premature Junctional Contractions
This list is not all-inclusive, as the causes of PJCs are extensive. Normally, PJCs are benign and cause no hemodynamic compromise. However, hemodynamic compromise can occur rarely.