Most parents-to-be expect their babies to arrive right around their due date, give or take a couple of days or weeks. And the majority of babies do arrive on schedule, allowing them plenty of time to prepare for life outside the uterus and their parents plenty of time to prepare for life with a baby.
But about 400,000 times a year in the United States, that vital preparatory time is cut unexpectedly—and sometimes perilously—short when baby is born prematurely and/or too small. Some of these babies weigh in at just a few ounces under the low-birthweight (5-pound, 8-ounce) cutoff, and are able to quickly and easily catch up with their full-term peers. But others, robbed of many weeks of uterine development, arrive so small that they can fit in the palm of a hand; and it can take months of intensive medical care to help them do the growing they were supposed to have done in the womb.
Many parents, too, are far from ready when birth comes too early. For them, the first postpartum days, sometimes weeks or months, are filled not with learning to diaper, getting adjusted to having a baby in the house, and writing thank you notes, but with reading hospital charts, learning to feed baby through a tube, and getting adjusted to not having a baby in the house.
Though the low-birthweight baby (whether born early or not) is still at higher risk than larger babies, rapid advances in medical care for tiny infants have made it possible for the great majority of them to grow into normal, healthy children. But before they are carried proudly home from the hospital, a long road often lies ahead for these babies and their parents.
If your baby has arrived too soon and too small, you’ll find the information and support you’ll need to navigate that road in the pages that follow.
Learning to eat outside the womb isn’t easy at first, even for a full-term baby—who must master the fine points of nursing from a breast or a bottle. For preterm babies, the challenges increase exponentially—and the younger and smaller the baby, the greater the challenges. Those who are born just three or four weeks early are usually able to breastfeed or take the bottle right after birth—again, after mastering those fine points. But babies born before 36 weeks have special nutritional needs that traditional feeding can’t satisfy—not only because they’re born smaller, but because they grow at a faster rate than full-term babies do, may not be able to suck effectively and/or may have immature digestive systems.
For one thing, these littlest babies need a diet that mirrors the nutrition they would be receiving if they were still in utero, and that helps them gain weight quickly. For another, these nutrients need to be served up in the most concentrated form possible, because preemies and low-birthweight babies can take only tiny amounts of food at a time—partly because their stomachs are so small, and partly because their immature digestive systems are sluggish, making the passage of food a very slow process. And since they can’t always suck well or even suck at all, they can’t take their meals from a bottle or a breast—at least not right away. Luckily, breast milk, fortified breast milk, or specially designed formulas can usually provide all the nutrients preemies need to grow and thrive.
As a parent of a premature infant, you will find that feeding and monitoring weight gain will become some of the most consuming aspects of caring for your baby in the hospital—both in terms of time and emotion. The neonatologists and nurses will do everything they can to ensure that your preemie receives the proper nutrition needed to gain weight. Just how your baby receives that nutrition depends on how early he or she was born:
IV feeding. When a very small newborn is rushed to the intensive care nursery, an intravenous solution of water, sugar, and certain electrolytes is often given to prevent dehydration and electrolyte depletion. Very sick or small babies (usually those who arrive before 28 weeks’ gestation) continue to receive nutrition through their IV. Called total parenteral nutrition (TPN) or parenteral hyperalimentation, this balanced blend of protein, fat, sugar, vitamins, minerals, and IV fluids is given until the baby can tolerate milk feedings. Once your baby is able to begin milk feedings by gavage (see below), TPN will decrease.
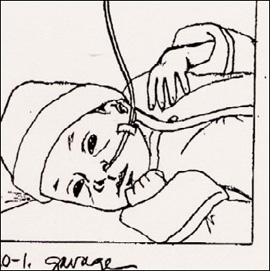
Gavage feeding. Babies who arrive between 28 and 34 weeks’ gestation and who don’t need IV nutrition are fed by gavage—a method not dependent on sucking, since babies this young usually have not yet developed this reflex. (This method is also used to feed babies who started out on TPN but have progressed to the point where they can tolerate milk feedings.) A small flexible tube (gavage tube) is placed into the baby’s mouth or nose and passed down to the stomach. Prescribed amounts of pumped breast milk, fortified breast milk, or formula are fed through the tube every few hours (see facing page for the advantages of using breast milk). Gavage tubes are either left in place between feedings or removed and reinserted for each feeding. (The tube won’t bother your preemie because the gag reflex doesn’t develop until about 35 weeks.)
Baby receives feedings through a gavage tube.
It may be a relatively long time before you’ll be able to feed your baby as you’d always imagined you would, through breast or bottle. Until then, you can still take part in feedings by holding the tube and measuring how much your baby takes; cuddling during tube feedings (if baby can be held); or giving your baby your finger to practice sucking on while he or she’s being fed (this helps strengthen the sucking reflex and may also help your baby associate sucking with getting a full tummy).
Nipple feeding. One of the most momentous milestones of your preemie’s stay in the hospital will be the switch from gavage feeding to nipple feeding. When it comes to readiness for this milestone, there can be some big differences among little babies. Some are ready to tackle the breast or bottle as early as 30 to 32 weeks’ gestational age. Others won’t be ready to take on the nipple until 34 weeks, still others, not until 36 weeks’ gestational age.
As parents of a premature or low-birthweight baby, you’ll be particularly anxious to start seeing the numbers on the scale creeping up. But don’t be discouraged if instead your baby seems to be losing weight at first. It’s normal for a premature infant (as it is for a full-term baby) to drop quite a few ounces—typically losing between 5 to 15 percent of his or her birthweight—before beginning a gain. As with a full-term baby, much of that weight loss will be water. Premature babies don’t usually regain their birthweight before they are two or more weeks old, at which point they can begin surpassing it.
The neonatologist will consider several factors before giving you the green light to begin breast or bottle feeding: Is your baby’s condition stable? Can he or she handle being fed in your arms? Have all the other physical requirements been met? (Baby has shown readiness by rhythmically sucking on a pacifier or feeding tube, can coordinate breathing and sucking, is awake for longer periods, has active bowel sounds, has passed meconium stools, and shows no sign of abdominal distension or infection).
Since nipple feedings are tiring for a small baby, they’ll be started slowly—one or two a day, alternated with tube feedings. Infants with respiratory problems may have an even harder time, requiring extra oxygen while feeding or experiencing short episodes of apnea (breathing cessation) while sucking (they might concentrate too hard on sucking and forget to breathe). For babies who have trouble mastering the suck, a specially designed pacifier may be used to help them practice and perfect their technique before graduating to breast or bottle.
EXPRESSING MILK FOR A PREMATURE BABY
The decision to breastfeed a preterm baby is not always an easy one, even for women who planned on nursing at term. A major attraction of breastfeeding, close mother–child contact, is usually absent, at least at first. Instead, a cold impersonal pump stands in the way of an intimate experience, making nursing a mother–machine–child affair. But though almost all women find pumping their breasts exhausting and time-consuming, most persevere, knowing that this is the one way in which they can contribute to the well-being of the baby from whose care they otherwise feel excluded.
The following tips can make the effort to feed a preterm baby in the best possible way more efficient and less tedious:
 See page 155 for tips on expressing breast milk. Ask about in-hospital facilities for expressing milk. Most hospitals have a special room (with comfortable chairs and an electric breast pump) set aside for mothers to use.
See page 155 for tips on expressing breast milk. Ask about in-hospital facilities for expressing milk. Most hospitals have a special room (with comfortable chairs and an electric breast pump) set aside for mothers to use.
 Begin expressing milk as soon after delivery as possible, even if your baby isn’t ready to take it. Express every two to three hours (about as often as a newborn nurses) if your baby is going to use the milk immediately; every four hours or so if the milk is going to be frozen for later use. You may find getting up to pump once in the middle of the night helps build up your milk supply; or you may value a full night’s sleep more.
Begin expressing milk as soon after delivery as possible, even if your baby isn’t ready to take it. Express every two to three hours (about as often as a newborn nurses) if your baby is going to use the milk immediately; every four hours or so if the milk is going to be frozen for later use. You may find getting up to pump once in the middle of the night helps build up your milk supply; or you may value a full night’s sleep more.
 It’s likely you will eventually be able to express more milk than your tiny baby can use. Don’t cut back, however, figuring you’re wasting too much. Regular pumping now will help to establish a plentiful milk supply for the time when your baby takes over where the machine leaves off. In the meantime, the excess milk can be dated and frozen for later use.
It’s likely you will eventually be able to express more milk than your tiny baby can use. Don’t cut back, however, figuring you’re wasting too much. Regular pumping now will help to establish a plentiful milk supply for the time when your baby takes over where the machine leaves off. In the meantime, the excess milk can be dated and frozen for later use.
 Don’t be discouraged by day-to-day or hour-to-hour variations in supply. Such variations are normal, although you wouldn’t be aware of them if you were nursing directly. Also normal when milk is expressed mechanically are an apparently inadequate milk supply and/or a drop in production after several weeks. Your baby will be a much more efficient stimulator of your milk supply than even the most efficient pump. When actual suckling begins, your supply is almost certain to increase quickly.
Don’t be discouraged by day-to-day or hour-to-hour variations in supply. Such variations are normal, although you wouldn’t be aware of them if you were nursing directly. Also normal when milk is expressed mechanically are an apparently inadequate milk supply and/or a drop in production after several weeks. Your baby will be a much more efficient stimulator of your milk supply than even the most efficient pump. When actual suckling begins, your supply is almost certain to increase quickly.
 When baby is ready for feeding by mouth, try to nurse first, before the baby is given a bottle. Studies show that low-birthweight babies take to the breast more easily than to the bottle. But don’t worry if yours does better on the bottle—use it while your baby gets the hang of breastfeeding (begin feeding sessions with nursing, then move to bottle), or use a supplemental nutrition system (see page 167).
When baby is ready for feeding by mouth, try to nurse first, before the baby is given a bottle. Studies show that low-birthweight babies take to the breast more easily than to the bottle. But don’t worry if yours does better on the bottle—use it while your baby gets the hang of breastfeeding (begin feeding sessions with nursing, then move to bottle), or use a supplemental nutrition system (see page 167).
Preemies who are ready to move on to nipple feedings can be nourished either with breast milk, fortified breast milk, or formula:
 Breast milk. Breast is best not only when it comes to full-term infants. Most experts favor breast milk over formula for the preemie, too, and for a number of reasons: First of all, it’s custom designed for a preemie’s special nutritional needs. Milk from mothers who deliver early is different than milk from mothers who deliver at term. It contains more protein, sodium, calcium, and other nutrients than full-term breast milk does, but less than is found in formula. This preemie-perfect balance prevents tiny babies from losing too much fluid, which helps them maintain a stable body temperature. It’s also easier to digest and helps babies grow faster. Second, breast milk has important substances not found in formula. Colostrum (early breast milk) is extremely rich in antibodies and cells that help fight infection. This is especially important when babies are sick or premature and may have a higher chance of developing an infection. Third, research has shown that breastfed preemies have a lower risk of developing necrotizing enterocolotis, an intestinal infection unique to preemies (see page 623); have a better tolerance of feedings, less risk of allergies, and enhanced development; and receive all the benefits that a full-term baby gets from breast milk (see page 3). Even if you don’t plan to breastfeed long term, providing breast milk for your baby while he or she is in the hospital gives your baby the best possible start at a time when that start has begun too soon.
Breast milk. Breast is best not only when it comes to full-term infants. Most experts favor breast milk over formula for the preemie, too, and for a number of reasons: First of all, it’s custom designed for a preemie’s special nutritional needs. Milk from mothers who deliver early is different than milk from mothers who deliver at term. It contains more protein, sodium, calcium, and other nutrients than full-term breast milk does, but less than is found in formula. This preemie-perfect balance prevents tiny babies from losing too much fluid, which helps them maintain a stable body temperature. It’s also easier to digest and helps babies grow faster. Second, breast milk has important substances not found in formula. Colostrum (early breast milk) is extremely rich in antibodies and cells that help fight infection. This is especially important when babies are sick or premature and may have a higher chance of developing an infection. Third, research has shown that breastfed preemies have a lower risk of developing necrotizing enterocolotis, an intestinal infection unique to preemies (see page 623); have a better tolerance of feedings, less risk of allergies, and enhanced development; and receive all the benefits that a full-term baby gets from breast milk (see page 3). Even if you don’t plan to breastfeed long term, providing breast milk for your baby while he or she is in the hospital gives your baby the best possible start at a time when that start has begun too soon.
To ensure your baby is still getting enough nutrition in the early stages of breastfeeding (when baby’s suck may still be weak or your breasts not producing sufficient amounts of milk), talk to the doctor about the following supplemental feeding methods that don’t interfere with nursing:
 nursing with the gavage still in place
nursing with the gavage still in place
 using a supplemental nutrition system (see page 167)
using a supplemental nutrition system (see page 167)
 using a feeding system taped to your finger (finger feeding)
using a feeding system taped to your finger (finger feeding)
 cup feeding with specially designed cups
cup feeding with specially designed cups
 syringe feeding
syringe feeding
 bottle feeding with slower-flow bottle nipples
bottle feeding with slower-flow bottle nipples
For more on breastfeeding your premature baby, see page 614.
 Fortified breast milk. Sometimes, even the milk of a preemie’s mother isn’t adequate for the preemie. Since some babies, particularly very tiny ones, need even more concentrated nutrition—including more fat, proteins, sugars, calcium, and phosphorus, and possibly, more of such other nutrients as zinc, magnesium, copper, and vitamin B6—the breast milk being fed through a tube or a bottle may be fortified with human milk fortifier (HMF) as needed. HMF comes in a powered form that can be blended with breast milk, or in a liquid form for use when adequate amounts of breast milk are not available.
Fortified breast milk. Sometimes, even the milk of a preemie’s mother isn’t adequate for the preemie. Since some babies, particularly very tiny ones, need even more concentrated nutrition—including more fat, proteins, sugars, calcium, and phosphorus, and possibly, more of such other nutrients as zinc, magnesium, copper, and vitamin B6—the breast milk being fed through a tube or a bottle may be fortified with human milk fortifier (HMF) as needed. HMF comes in a powered form that can be blended with breast milk, or in a liquid form for use when adequate amounts of breast milk are not available.
 Formula. Babies can do well, too, when they’re fed formula specially designed for preemies. Even if you are breastfeeding, your baby may get additional feedings with a bottle or supplemental nutrition system. Preemies are fed using small plastic bottles marked in cubic centimeters (cc) or milliliters (ml). The nipples are specially designed and require less sucking strength from your baby. Ask a nurse to show you the correct position for bottle feeding a preemie—it may differ slightly from that for a full-term infant.
Formula. Babies can do well, too, when they’re fed formula specially designed for preemies. Even if you are breastfeeding, your baby may get additional feedings with a bottle or supplemental nutrition system. Preemies are fed using small plastic bottles marked in cubic centimeters (cc) or milliliters (ml). The nipples are specially designed and require less sucking strength from your baby. Ask a nurse to show you the correct position for bottle feeding a preemie—it may differ slightly from that for a full-term infant.
Once you’ve arrived home with your preemie, feedings will be as challenging and time-consuming as they were in the hospital. You’ll need to experiment with different nipples, bottles, nursing positions, and so on. As a general rule, preemies need to be fed smaller amounts and more often than full-termers. They feed slowly and tire easily. Depending on your baby’s progress, you may or may not need to continue using formula specifically designed for preemies. Often parents continue to use the same small bottles that were used in the hospital. But keep in mind that what worked in the hospital might not work as well once you’re home and your baby continues to grow in both size and maturity.
You can expect to encounter one or all of the following feeding concerns at home (though some lucky parents experience none at all):
 Sleepy baby. Many preemies tire easily and the desire to sleep sometimes overrides the desire to eat. But since all babies, especially those born small, need regular feedings, it is all the more important that you make sure your baby doesn’t sleep through feedings. For tips on how to rouse a sleepy baby, see page 122.
Sleepy baby. Many preemies tire easily and the desire to sleep sometimes overrides the desire to eat. But since all babies, especially those born small, need regular feedings, it is all the more important that you make sure your baby doesn’t sleep through feedings. For tips on how to rouse a sleepy baby, see page 122.
 Breath holders. Some preemies, especially those who were born without good suck-breath coordination, will forget to breathe when feeding. This is tiring for your baby and anxiety-producing for you. If you notice your baby hasn’t taken a breath after a number of sucks or looks pale while feeding, remove the nipple from baby’s mouth and let him or her take a breath. If your baby seems to be holding his or her breath all the time during feedings, regularly remove the nipple after every three to four sucks.
Breath holders. Some preemies, especially those who were born without good suck-breath coordination, will forget to breathe when feeding. This is tiring for your baby and anxiety-producing for you. If you notice your baby hasn’t taken a breath after a number of sucks or looks pale while feeding, remove the nipple from baby’s mouth and let him or her take a breath. If your baby seems to be holding his or her breath all the time during feedings, regularly remove the nipple after every three to four sucks.
 Oral aversion. Babies who have spent a lot of time in the NICU may have come to associate the mouth with unpleasant experiences (feeding tubes, ventilator tubes, suctioning, and so on) and often develop a strong aversion to having anything in or around their mouths once they are home. To combat this, try to replace the unpleasant oral associations with more pleasant ones. Touch your baby around the mouth in a soothing manner, give your baby a pacifier or your finger to suck, or encourage your baby to touch his or her own mouth or suck on his or her thumb or fist.
Oral aversion. Babies who have spent a lot of time in the NICU may have come to associate the mouth with unpleasant experiences (feeding tubes, ventilator tubes, suctioning, and so on) and often develop a strong aversion to having anything in or around their mouths once they are home. To combat this, try to replace the unpleasant oral associations with more pleasant ones. Touch your baby around the mouth in a soothing manner, give your baby a pacifier or your finger to suck, or encourage your baby to touch his or her own mouth or suck on his or her thumb or fist.
 Reflux. Many preemies are prone to excessive spitting up or GER because of their immature digestive systems. For tips on coping with spitting up and GER, see pages 174 and 558.
Reflux. Many preemies are prone to excessive spitting up or GER because of their immature digestive systems. For tips on coping with spitting up and GER, see pages 174 and 558.
 Starting solids. Like full-term babies, preemies should start receiving solids somewhere between four and six months. But for preemies, that date is based on their corrected age rather than chronological age (which means a preemie wouldn’t be ready for solids until six to eight chronological months). Because some preemies experience delays in development, solid feedings should not be started until the baby shows signs of readiness (see page 292), even if the corrected age says “it’s time” for solids. Some preemies have a more difficult time with solids—especially once they graduate to chunkier foods.
Starting solids. Like full-term babies, preemies should start receiving solids somewhere between four and six months. But for preemies, that date is based on their corrected age rather than chronological age (which means a preemie wouldn’t be ready for solids until six to eight chronological months). Because some preemies experience delays in development, solid feedings should not be started until the baby shows signs of readiness (see page 292), even if the corrected age says “it’s time” for solids. Some preemies have a more difficult time with solids—especially once they graduate to chunkier foods.
“My baby was rushed to the NICU immediately after birth. What can I expect when I visit him there for the first time?”
A first look at a neonatal intensive care unit can be frightening, especially if your baby is one of the tiny, helpless patients in it. Knowing what you’re looking at can keep your fears from overwhelming you. Here’s what you can expect in most NICUs:
 A main nursery area comprising a large room or a series of rooms, with designated bed areas along the walls. There may also be a couple of isolation rooms in an area separate from the main nursery. Adjoining may be several small family rooms where mothers can express milk (breast pumps are usually provided), and where families can spend cuddling time with their babies as they get stronger.
A main nursery area comprising a large room or a series of rooms, with designated bed areas along the walls. There may also be a couple of isolation rooms in an area separate from the main nursery. Adjoining may be several small family rooms where mothers can express milk (breast pumps are usually provided), and where families can spend cuddling time with their babies as they get stronger.
 A bustling atmosphere. There will be many nurses and doctors busily moving about, treating and monitoring babies. Parents may also be caring for or feeding their own infants.
A bustling atmosphere. There will be many nurses and doctors busily moving about, treating and monitoring babies. Parents may also be caring for or feeding their own infants.
 Relative quiet. Though it’s one of the busiest places in the hospital, it’s typically also one of the quietest. That’s because loud noises can be stressful for tiny babies or even harmful to their ears. To help keep the sound level down, you should talk quietly, close doors and isolette portholes gently, and take care not to drop things or place items loudly on the tops of incubators. (One sound that is important for your preemie, however, is the sound of your voice; see page 611.) Since still-sensitive eyes need protection, too, NICU staff usually tries to control the brightness in the nursery. Occasionally, however, the lights in certain areas can become intense to allow doctors and nurses to perform procedures.
Relative quiet. Though it’s one of the busiest places in the hospital, it’s typically also one of the quietest. That’s because loud noises can be stressful for tiny babies or even harmful to their ears. To help keep the sound level down, you should talk quietly, close doors and isolette portholes gently, and take care not to drop things or place items loudly on the tops of incubators. (One sound that is important for your preemie, however, is the sound of your voice; see page 611.) Since still-sensitive eyes need protection, too, NICU staff usually tries to control the brightness in the nursery. Occasionally, however, the lights in certain areas can become intense to allow doctors and nurses to perform procedures.
 Strict hygiene standards. Keeping germs that can spread infection (and make sick babies sicker) out of the nursery is a major priority in the NICU. Each time you visit, you’ll need to wash your hands with antibacterial soap (there’s usually a sink for this purpose right outside the nursery doors). You may be asked to put on a hospital gown, too. If your baby is in isolation, you may also need to wear gloves and a mask.
Strict hygiene standards. Keeping germs that can spread infection (and make sick babies sicker) out of the nursery is a major priority in the NICU. Each time you visit, you’ll need to wash your hands with antibacterial soap (there’s usually a sink for this purpose right outside the nursery doors). You may be asked to put on a hospital gown, too. If your baby is in isolation, you may also need to wear gloves and a mask.
 Tiny babies everywhere. You’ll see them in clear incubators or isolettes (bassinets that are totally closed except for four porthole-like doors that allow you and the staff to reach in and care for your baby) or in open bassinets. You’ll also see some on warming tables under overhead heat lamps. Some babies may be wrapped in cellophane to minimize the loss of fluids and body heat through the skin. This helps preemies keep warm (particularly those under 4 pounds, who lack the fat necessary to regulate body temperature, even when they’re swaddled in blankets).
Tiny babies everywhere. You’ll see them in clear incubators or isolettes (bassinets that are totally closed except for four porthole-like doors that allow you and the staff to reach in and care for your baby) or in open bassinets. You’ll also see some on warming tables under overhead heat lamps. Some babies may be wrapped in cellophane to minimize the loss of fluids and body heat through the skin. This helps preemies keep warm (particularly those under 4 pounds, who lack the fat necessary to regulate body temperature, even when they’re swaddled in blankets).
 An endless array of apparatus. You’ll notice an abundance of technology near each bed. Monitors that record vital signs (and will warn, by setting off an alarm, any changes that need prompt attention) are hooked up to babies via leads that are either stuck on the skin with gel or inserted by needle just under the skin. In addition to a monitor, your baby may also be linked to a feeding tube, an IV (via the arm, leg, hand, foot, or head), a catheter in his umbilical stump, temperature probes (attached to his skin with a patch), and a pulse oximeter that measures the oxygen level in his blood with a small light attached to his hand or foot. A mechanical ventilator (breathing machine) may be used to help your baby breathe normally if he’s under 30 to 33 weeks’ gestation. Otherwise, he may receive oxygen through a mask or delivered into the nose through soft plastic prongs attached to tubing. There will also be suction setups that are used periodically for removing excess respiratory secretions, as well as lights for phototherapy (bililights), used to treat babies with jaundice. (Babies undergoing this treatment will be naked except for eye patches, which protect their eyes from the bililights.)
An endless array of apparatus. You’ll notice an abundance of technology near each bed. Monitors that record vital signs (and will warn, by setting off an alarm, any changes that need prompt attention) are hooked up to babies via leads that are either stuck on the skin with gel or inserted by needle just under the skin. In addition to a monitor, your baby may also be linked to a feeding tube, an IV (via the arm, leg, hand, foot, or head), a catheter in his umbilical stump, temperature probes (attached to his skin with a patch), and a pulse oximeter that measures the oxygen level in his blood with a small light attached to his hand or foot. A mechanical ventilator (breathing machine) may be used to help your baby breathe normally if he’s under 30 to 33 weeks’ gestation. Otherwise, he may receive oxygen through a mask or delivered into the nose through soft plastic prongs attached to tubing. There will also be suction setups that are used periodically for removing excess respiratory secretions, as well as lights for phototherapy (bililights), used to treat babies with jaundice. (Babies undergoing this treatment will be naked except for eye patches, which protect their eyes from the bililights.)
 A place for parents to sit and cuddle their babies. In the midst of all this high-tech equipment, there will likely be rocking chairs where you can feed or hold your baby.
A place for parents to sit and cuddle their babies. In the midst of all this high-tech equipment, there will likely be rocking chairs where you can feed or hold your baby.
 A large team of highly trained medical specialists. The staff caring for your baby in the NICU might include a neonatologist (a pediatrician who has had special training in newborn intensive care); pediatric residents and neonatal fellows (doctors undergoing training); a physician assistant or nurse practitioner; a clinical nurse specialist; a primary nurse (who will most frequently take care of your baby and teach you how to care for him); a nutritionist; a respiratory therapist; other physician specialists depending on your baby’s particular needs; social workers, physical and occupational therapists; X-ray and lab technicians; and lactation specialists.
A large team of highly trained medical specialists. The staff caring for your baby in the NICU might include a neonatologist (a pediatrician who has had special training in newborn intensive care); pediatric residents and neonatal fellows (doctors undergoing training); a physician assistant or nurse practitioner; a clinical nurse specialist; a primary nurse (who will most frequently take care of your baby and teach you how to care for him); a nutritionist; a respiratory therapist; other physician specialists depending on your baby’s particular needs; social workers, physical and occupational therapists; X-ray and lab technicians; and lactation specialists.
 Being part of the team yourself. Remember that you are one of the most important partners in your baby’s care. Educate yourself as much as possible about the NICU’s equipment and procedures, and familiarize yourself with your baby’s conditions and progress. Ask for explanations of how ventilators, machines, and monitors are helping your baby. Request written information that explains the medical jargon you’ll be hearing. Learn as much as you can about the routine: visiting hours and visitor restrictions, when nurses change shifts, when doctors make rounds. Find out who will give you updates on your baby’s progress and when you’ll get them. Give the staff your cell phone and pager number, so they can always reach you if necessary.
Being part of the team yourself. Remember that you are one of the most important partners in your baby’s care. Educate yourself as much as possible about the NICU’s equipment and procedures, and familiarize yourself with your baby’s conditions and progress. Ask for explanations of how ventilators, machines, and monitors are helping your baby. Request written information that explains the medical jargon you’ll be hearing. Learn as much as you can about the routine: visiting hours and visitor restrictions, when nurses change shifts, when doctors make rounds. Find out who will give you updates on your baby’s progress and when you’ll get them. Give the staff your cell phone and pager number, so they can always reach you if necessary.
“The nurses warned me that having my daughter in the NICU would be like being on a roller coaster with all its ups and downs. But I’m surprised at the incredible range of emotions I’m feeling.”
You’re not alone. Most parents whose babies are in the NICU experience a wide spectrum of ever-changing emotions, including shock, anger, stress, panic, fear, numbness, frustration, disappointment, confusion, sadness, intense grief, and equally intense hope. All for good reason. You may feel overwhelmed by all the medical equipment attached to your baby and the constant activity of nurses and doctors. You may be frightened of the procedures your baby is undergoing or frustrated by feelings of helplessness. You may feel disappointed that your daughter isn’t the dimpled, adorable full-term baby you’d been expecting (and envisioning) throughout your pregnancy, frustrated that you can’t take her home to begin your life together, and guilty about both emotions. You may also feel guilty for not feeling happy about your baby’s birth or guilty about not being able to keep the pregnancy going longer (even if there was absolutely nothing you could have done to prevent your daughter’s prematurity). You may feel distraught at the uncertainty of your baby’s future, particularly if she’s very small or sick. You may even unconsciously distance yourself from her for fear of becoming too attached or because you find bonding difficult to accomplish through the portholes of an isolette. Or, you may feel unexpectedly strong feelings of affection, deepened, instead of compromised, by the challenges you and your baby are facing. You may be angry at yourself for your reactions, at your spouse for not reacting the same way you are, at your family and friends for not understanding what you’re going through or for acting as if nothing has happened, at your doctor for not preventing this. Confusing these emotions may be the fact that they may often conflict or fluctuate wildly—for instance, leaving you feeling hopeful one minute, hopeless the next, deeply in love with your baby one day, afraid to love her the next. Compounding them may be the physical exhaustion that comes from keeping a round-the-clock vigil at your baby’s bedside, which may be more debilitating still if you haven’t yourself recovered from childbirth.
The parents of full-term newborns may be surprised when they first see their babies. The parents of preterm infants are often shocked. The typical preemie weighs between 1,600 grams (about 3½ pounds) and 1,900 grams (about 4 pounds, 3 ounces) at birth, and some weigh considerably less. The smallest can fit in the palm of an adult hand and have wrists and hands so tiny that a wedding band could be slipped over them. The preemie’s skin is translucent, leaving veins and arteries visible. It seems to fit loosely because it lacks a fat layer beneath it (making it impossible for baby’s temperature to self-regulate), and often it is covered with a fine layer of prenatal body hair, or lanugo, that has usually been shed by full-term infants. Because of an immature circulatory system, skin coloring changes when the infant is handled or fed. The preemie’s ears may be flat, folded, or floppy because the cartilage that will give them shape has yet to develop. The preemie often lies with arms and legs straight rather than curled or tucked in because of the lack of muscle strength.
Sexual characteristics are usually not fully developed—testicles may be undescended, the foreskin in boys and the inner folds of the labia in girls may be immature, and there may be no areola around the nipples. Because neither muscular nor nerve development is complete, many reflexes (such as grasping, sucking, startle, rooting) may be absent. Unlike term babies, a preemie may cry little or not at all. He or she may also be subject to periods of breathing cessation, known as apnea of prematurity.
But the physical characteristics of preemies that make up this portrait are only temporary. Once preterm newborns reach forty weeks of gestation, the time when, according to the calendar, they should have been born, they very much resemble the typical newborn in size and development.
Coping with these emotions may be extremely difficult, but keeping the following in mind may help:
 What you’re feeling, saying, and doing are perfectly normal. Such extreme and sometimes contradictory emotions are experienced by nearly every parent of a premature baby at some time or another (though you may often believe that no one else has ever felt the way you do).
What you’re feeling, saying, and doing are perfectly normal. Such extreme and sometimes contradictory emotions are experienced by nearly every parent of a premature baby at some time or another (though you may often believe that no one else has ever felt the way you do).
 There is no one right way to feel. Your emotions may differ from those of your spouse, the parents of the baby in the next isolette, or your friends who’ve also had premature babies. Everyone will react to it a little differently—and that’s normal too.
There is no one right way to feel. Your emotions may differ from those of your spouse, the parents of the baby in the next isolette, or your friends who’ve also had premature babies. Everyone will react to it a little differently—and that’s normal too.
 It’s important to express your emotions. Keeping them inside will only make you feel more isolated and helpless. Let the NICU staff know what your feelings and fears are. Not only will they understand what you’re going through (since helping parents is almost as important a part of their job as helping babies), they may offer insights that can help you cope.
It’s important to express your emotions. Keeping them inside will only make you feel more isolated and helpless. Let the NICU staff know what your feelings and fears are. Not only will they understand what you’re going through (since helping parents is almost as important a part of their job as helping babies), they may offer insights that can help you cope.
 Don’t shut out your spouse. You can both gain strength by leaning on each other. Open communication can also help keep the stress inherent in parenting a preemie from hurting your relationship.
Don’t shut out your spouse. You can both gain strength by leaning on each other. Open communication can also help keep the stress inherent in parenting a preemie from hurting your relationship.
 Support best comes from those who know. Try talking with other parents in the NICU. You’ll find that they also feel alone, unsure, and scared. Friendships are easily formed in the NICU because other parents need you as much as you need them. Many hospitals make support available through groups run by the NICU social worker, or can hook you up with support families whose babies have left the NICU. No one can relate better to what you’re experiencing—and share more wisdom and empathy—than parents who’ve experienced it themselves. You can find additional empathetic support by joining one of the many parents-of-preemies discussion groups on the Internet.
Support best comes from those who know. Try talking with other parents in the NICU. You’ll find that they also feel alone, unsure, and scared. Friendships are easily formed in the NICU because other parents need you as much as you need them. Many hospitals make support available through groups run by the NICU social worker, or can hook you up with support families whose babies have left the NICU. No one can relate better to what you’re experiencing—and share more wisdom and empathy—than parents who’ve experienced it themselves. You can find additional empathetic support by joining one of the many parents-of-preemies discussion groups on the Internet.
 It will take time. You probably won’t be on an even emotional keel at least until your baby’s on an even physical one. Until then, you’ll have good days and bad days (usually corresponding to your baby’s ups and downs). Reminding yourself that your feelings are normal—that all parents of preemies ride an emotional roller coaster until their babies are safely home and completely well—won’t make the feelings go away, but it will help give you the perspective you need to cope with them.
It will take time. You probably won’t be on an even emotional keel at least until your baby’s on an even physical one. Until then, you’ll have good days and bad days (usually corresponding to your baby’s ups and downs). Reminding yourself that your feelings are normal—that all parents of preemies ride an emotional roller coaster until their babies are safely home and completely well—won’t make the feelings go away, but it will help give you the perspective you need to cope with them.
If you have another child at home, helping him or her cope with anxiety will be a priority; see page 613.
“How do I know that our premature baby—she’s only a little more than 2½ pounds—is getting the best possible care?”
The first step in making sure your baby gets the best possible care is making sure she’s being cared for in the hospital that’s best for her needs. The hospital system in this country is arranged in three levels. Small community hospitals make up level one—they provide care for uncomplicated cases of all types, including low-risk deliveries and normal newborns, but do not have neonatal intensive care units for very premature, low-birthweight, or sick newborns. Second-level hospitals have somewhat more sophisticated facilities, can care for more complicated cases including many high-risk deliveries, and do have neonatal intensive care units that can care for most babies in trouble. Third-level, or tertiary, hospitals are the major medical centers, boasting the most highly trained specialists, the most sophisticated facilities, and state-of-the-art neonatal intensive care units (NICUs) ready to care for the tiniest and sickest of newborns.1
Though healthy babies, including preemies who weigh in at close to 5 pounds or more, do equally well at first-, second-, and third-level hospitals, very small babies (those who are at the highest risk, weighing less than 3 pounds, 5 ounces or 1,500 grams at birth) do best at major medical centers. Having your baby at such a facility is the best guarantee you can get of good care. If your baby is not in a tertiary hospital, discuss the possibility of having her transferred to one with her pediatrician, the present NICU staff, and the staff at the medical center you are considering.
Wherever your baby is, your input will be important in ensuring optimum care. Become knowledgeable about low-birthweight babies in general, and about any special problems your baby has, by reading books and by asking questions. Whenever you’re uncomfortable or unhappy about the course your baby’s treatment is taking, raise your concerns with her pediatrician and/or the hospital nurses or neonatologists. You may be satisfied with their explanation, or perhaps things can be done differently. If you aren’t satisfied, ask for a consultation with another neonatologist. If you feel uncomfortable challenging doctors, find a friend or relative to act as advocate.
“We’d expected to bond with our baby right after birth. But since she arrived six weeks early and weighed only 3½ pounds, she was whisked away before we had a chance to even touch her. We’re worried about the effect this will have on her—and on our relationship with her.”
During this stressful time, the last thing you need is another worry. And the last thing you need to worry about is bonding at birth. Love and attachment between parent and child develops over many months, even years, blossoming over a lifetime rather than bursting into full bloom during the first few moments of life. So instead of regretting the first few moments (or even days) you’ve lost, start making the most of the months of parenthood that lie ahead. Though it isn’t necessary to begin bonding at birth, you may be able to initiate the process while your baby is still in the hospital. Here’s how:
Ask for a picture, along with a thousand words. If your baby has been moved from the hospital you delivered in to another hospital for upgraded intensive care (possibly essential to her survival), and you are not yet able to be discharged, ask that pictures of her be brought to you. Your spouse or the hospital staff can take them, and you can enjoy looking at them until you’re able to look at the real thing. Even if more tubing and gadgetry is visible than baby, what you see will likely be less frightening and more reassuring than what you might have imagined. As helpful as a picture may be, you’ll still want those thousand words—from your spouse, and later the medical staff—describing every detail of what your baby is like and how she’s getting along.
Feast with your eyes. Just watching her in her isolette or warming mattress may help bring you closer.
Lay on the hands. Though it may seem that such a tiny and vulnerable infant is better off not being touched, studies have shown that premature infants who are stroked and lightly massaged while they are in intensive care grow better and are more alert, active, and behaviorally mature than babies who are handled very little. Start with her arms and legs, since they are less sensitive at first than the trunk. Try to work up to at least 20 minutes of gentle stroking a day. (For some very premature babies, touching is extremely stressful. If the neonatologist suggests that you minimize physical contact, spend as much time as you can with your baby—just without physical contact.)
For a tiny baby who should still be in the peaceful and relatively dark uterine environment, too much light can be stressful—causing irregular heart rates and decreased sleep—and even harmful to sensitive eyes. It may also keep your baby from opening his or her eyes to look around and interact with you. On the other hand, there’s also some evidence that constant dim light poses some problems, too, disturbing body rhythms and slowing development of normal sleep-wake cycles. Research suggests that preemies who are exposed to natural cycles of light and dark that mimic day-night rhythms gain weight faster than those kept around-the-clock in either bright light or low light. (Ask the neonatologist if this can be done for your baby, if appropriate.)
Most NICUs do their best to keep the lights down to simulate life in the womb, though bright lights may be necessary at least occasionally so that medical personnel can perform procedures. Though there’s probably not much you can do about the light level in the NICU, putting a blanket over your baby’s isolette when the lights are bright may help somewhat.
Kangaroo care. Marsupials have the right idea. Skin-to-skin contact can not only help you get close to your baby, it can help her grow and get better faster. In fact, studies have shown that babies who receive so-called kangaroo care are likely to leave the NICU sooner. To cuddle your baby marsupial-style, place her on your chest under your shirt so that she’s resting directly on your skin (she’ll probably be wearing only a diaper and hat; the hat prevents heat loss via the head). Loosely place your shirt over her to keep her warm or cover her with a blanket.
Carry on a conversation. To be sure, it will be a one-way conversation at first—your baby won’t be doing much talking, or even crying, while she’s in the NICU. She may not even appear to be listening. But she will recognize your voices, which she heard in utero, and will be comforted by the familiar sound. If you can’t be with your baby as often as you’d like, ask the nurses if you can leave a recording of you talking, singing, or reading quietly, which can be played for your baby. (Be sure to speak softly, however, whenever you’re around your baby, since her ears are still very sound-sensitive. In fact, for some very small preemies, any extra sounds can be extremely disturbing, so check with your baby’s doctor about what’s good for her and what isn’t.)
See eye-to-eye. If your baby’s eyes are shielded because she’s getting phototherapy for the treatment of jaundice, ask to have the bililights turned off and her eyes uncovered for at least a few minutes during your visit so that you can make eye-to-eye contact, an important part of parent-child bonding.
Take over for the nurses. As soon as your baby’s out of immediate danger, the NICU nurse will probably be happy to show you how to diaper, feed, and bathe her. You may even do some simple medical procedures for her. One of the first tasks parents feel comfortable doing is taking the baby’s temperature. Caring for her during your visits will help make you more comfortable with the role of parent, while giving you some valuable experience for the months ahead.
Don’t hold back. Many parents remain detached from their premature babies for fear of loving and losing. But that’s a mistake. First, because the odds are very much with your preterm baby; the great majority survive to be healthy and normal. And second, because if you do hold back and the unthinkable happens, you’ll always regret the moments you lost. The loss would be harder, not easier, to take.
“The first time I saw our baby in the intensive care nursery I was devastated. It’s horrible to think that our baby will spend the first weeks—maybe months—of his life in a sterile hospital room.”
Parents of preemies usually have to wait until their babies reach a gestational age of 37 to 40 weeks before taking them home—about as long as they would have had to wait if the babies had been carried to term. When a preemie faces other medical challenges besides being small, the wait can be longer still. But no matter how long your baby’s hospitalization ends up being, it will likely feel even longer. In order to make the most of that time and to even help it pass somewhat faster, try:
Striking up a partnership. Parents of a preemie often begin to feel that their baby belongs less to them and more to the doctors and nurses, who seem so competent and do so much for him. But instead of trying to compete with the staff, try working together with them. Get to know the nurses (which will be easier if your baby has a “primary” nurse in charge of his care at each shift), the neonatologist, and the residents. Let them know you’ll be happy to do little chores or errands for your baby, which can save them time, help you pass yours, and help you feel less like a bystander and more like an involved participant in his care.
Getting a medical education. Learn the jargon and terminology used in the NICU. Ask a staff member (when he or she has a free moment) to show you how to read your baby’s chart; ask the neonatologist for details about your baby’s condition and for clarification when you don’t understand. Parents of preemies often become experts in neonatal medicine very quickly, throwing around terms like “RDS” and “intubation” with the aplomb of a neonatologist.
Being a fixture at your baby’s side. Some hospitals may let you move in, but even if you can’t, you should spend as much time as possible with your baby, alternating shifts with your spouse. This way you will get to know not only your baby’s condition but your baby as well. (If you have other children at home, however, they’ll also need you now. Be certain that they get a substantial piece of mom and dad’s time, too.)
Making your baby feel at home. Even though the isolette’s only a temporary stop for your baby, try to make it as much like home as possible. Ask permission to put friendly-looking stuffed animals around your baby and tape pictures (perhaps including stimulating black-and-white enlargements of snapshots of mommy and daddy) to the sides of the isolette for his viewing pleasure. Tuck in a baby music box for a little night and day music or a tape recording of your voice (if the doctors say it’s okay). Remember, however, that anything you put in the baby’s isolette will have to be sterilized and should not interfere with life-sustaining equipment. Also be sure to keep noise levels low.
Readying your milk supply. Your milk is the perfect food for your premature baby (see page 604). Until he’s able to nurse, pump your breasts for indirect feedings and in order to keep up your milk supply. Pumping will also give you a welcome feeling of usefulness.
Hitting the shops. Since your baby arrived ahead of time, you may not have had time to order baby furniture, layette items, and other necessities. If so, now’s the time to get that shopping done. If you feel superstitious about filling your home with baby things before baby is discharged from the hospital, put in your orders pending his homecoming. You’ll not only have taken care of some necessary chores, you’ll also have filled some of the interminable hours of baby’s hospitalization and made a statement (at least to yourself) that you are confident of bringing him home.
“My baby wasn’t premature, but she was just under 5 pounds. The doctor said it was because of intrauterine growth restriction. What does this mean?”
Intrauterine growth restriction, often shortened to IUGR, appears to be nature’s way of ensuring a fetus’s survival in a uterus where, for some reason, she is not getting an adequate supply of nutrients through the placenta. The reduction in size allows a baby to get along well on the reduced intake of nutrients. Doctors surmise that this protective mechanism is called into action when the placenta isn’t functioning at optimal efficiency, limiting the passage of nutrients to the fetus, or when the mother’s nutrition is inadequate, because of illness, poor diet, smoking, or other, sometimes unknown factors.
The baby’s brain also appears to be protected by this survival mechanism, usually continuing to grow normally by taking more than its share of nourishment from what is available. That’s why most babies with IUGR have heads that are even larger in relation to their bodies than are those of full-size newborns.
Though a low-birthweight baby is at high risk for complications during the early days of life, most will do well with proper care. With good nutrition, preferably beginning with breast milk, you can expect your baby to start thriving. By the end of her first year she’ll likely have caught up on many, or even on all, fronts with her peers (90 percent of IUGR babies do). But should you decide to become pregnant again, try to determine first, with the aid of your doctor, what might have been responsible for the poor growing environment in your uterus so that your next baby won’t have to struggle with the same prenatal problems.
“We have a three-year-old daughter, and we don’t know what to tell her about her new premature sister.”
Children, even a child as young as yours, are able to understand and handle a lot more than we adults usually give them credit for. Trying to protect your daughter by keeping her in the dark about her new sibling’s condition will only make her anxious and insecure—particularly when you and your spouse suddenly, and to her, inexplicably, start spending so much of your time away from home. Instead, enlighten her fully, but on her level. Explain that the baby came out of mommy too soon, before she had grown enough, and has to stay in a special crib in the hospital until she’s big enough to come home. With the hospital’s okay, take your older daughter for an initial visit, and if it goes well and she seems eager, take her regularly. Children are just as likely to be fascinated by the wires and tubes as they are to be scared, particularly if their parents set the right tone—confident and cheerful rather than nervous and somber. Have her bring a present for the baby, to be placed in the isolette, which will help her feel that she’s a part of the team caring for her new sibling. If she would like to, and if you have the staff’s permission, let her scrub up and then touch the baby through the portholes. Like you, she will feel closer to the baby when that homecoming finally takes place if she has some contact now. (Read about sibling relationships in chapter 25.)
“I’ve always been determined to breastfeed my baby, and since she was born prematurely, I’ve been pumping milk to be fed to her through a tube. Will she have trouble switching to nursing later?”
So far, so good. From birth your baby has been provided with the best possible food for a premature newborn—her mommy’s milk—in the only way such a tiny baby is able to take nourishment, through a tube. Naturally, you’re concerned that she be able to continue to get this perfect food once she graduates to suckling.
Research indicates that you have little to worry about. One study found that premature infants weighing as little as 1,300 grams, or nearly 3 pounds, were not only able to suckle at the breast but were more successful at it than they were with the bottle. It took these infants between one and four weeks longer to become proficient at sucking from the bottle than at suckling from the breast. In addition, their bodies responded better to breastfeeding. When they nursed, their oxygen levels fluctuated little, whereas during bottle-feeding they showed significant drops in oxygen levels, with these levels staying down for varying periods after feeding. They were also comfortably warmer when being breastfed than when getting the bottle, which is important because preemies, whose thermostats aren’t operative, have trouble keeping themselves warm. This study and others like it show that some preterm infants begin to show the sucking reflex at 30 gestational weeks (though for other babies, the sucking reflex may not be strong enough till later).
Once you do put your baby to the breast, you’ll want to make conditions as conducive to success as possible:
 Read all about breastfeeding, beginning on page 66, before getting started.
Read all about breastfeeding, beginning on page 66, before getting started.
 Be patient if the neonatologist or nurse wants your baby monitored for temperature and/or oxygen changes during breastfeeding. This won’t interfere with the breastfeeding itself, and it will protect your baby by sounding an alarm in case she is not responding well to the feeding.
Be patient if the neonatologist or nurse wants your baby monitored for temperature and/or oxygen changes during breastfeeding. This won’t interfere with the breastfeeding itself, and it will protect your baby by sounding an alarm in case she is not responding well to the feeding.
 Be sure you’re relaxed and that your baby is awake and alert. A nurse will probably see to it that she is dressed warmly for this momentous event.
Be sure you’re relaxed and that your baby is awake and alert. A nurse will probably see to it that she is dressed warmly for this momentous event.
 Ask the staff if there is a special nursing area for preemie moms, a private corner with an armchair for you and your baby, or a privacy screen that can be put up to shield you.
Ask the staff if there is a special nursing area for preemie moms, a private corner with an armchair for you and your baby, or a privacy screen that can be put up to shield you.
 Get comfortable, propping your baby on pillows, supporting her head. Many women find a football hold comfortable (see page 72) as well as easy on the nipples.
Get comfortable, propping your baby on pillows, supporting her head. Many women find a football hold comfortable (see page 72) as well as easy on the nipples.
 If your baby doesn’t yet have a rooting reflex (she probably doesn’t), help her get started by placing your nipple, with the areola, into her mouth. Compress your breast lightly with your fingers to make it easier for her to latch on to (see page 73), and keep trying until she succeeds.
If your baby doesn’t yet have a rooting reflex (she probably doesn’t), help her get started by placing your nipple, with the areola, into her mouth. Compress your breast lightly with your fingers to make it easier for her to latch on to (see page 73), and keep trying until she succeeds.
 Watch to be sure your baby is getting milk. The first few minutes at the breast, baby’s suckling may be very rapid, a nonnutritive motion aimed at stimulating let-down. Your breasts are used to mechanical pumping and will take a while to adjust to the different motions generated by your baby’s mouth, but soon you will notice that the movement has slowed and that your baby is swallowing. This lets you know that let-down has occurred, and your baby is getting milk.
Watch to be sure your baby is getting milk. The first few minutes at the breast, baby’s suckling may be very rapid, a nonnutritive motion aimed at stimulating let-down. Your breasts are used to mechanical pumping and will take a while to adjust to the different motions generated by your baby’s mouth, but soon you will notice that the movement has slowed and that your baby is swallowing. This lets you know that let-down has occurred, and your baby is getting milk.
 If your baby doesn’t seem interested in your breast, try expressing a few drops of milk into her mouth to give her a taste of what’s in store.
If your baby doesn’t seem interested in your breast, try expressing a few drops of milk into her mouth to give her a taste of what’s in store.
 Nurse your baby for as long a period as she’s willing to stay at the breast. Experts who’ve studied breastfeeding of premature babies recommend letting them remain at the breast until they’ve stopped active suckling for at least two minutes. Small preemies have been known to nurse for close to an hour before being satisfied.
Nurse your baby for as long a period as she’s willing to stay at the breast. Experts who’ve studied breastfeeding of premature babies recommend letting them remain at the breast until they’ve stopped active suckling for at least two minutes. Small preemies have been known to nurse for close to an hour before being satisfied.
 Don’t be discouraged if the first session or first several sessions seem unproductive. Many full-term babies take a while to catch on, and preemies deserve at least the same chance.
Don’t be discouraged if the first session or first several sessions seem unproductive. Many full-term babies take a while to catch on, and preemies deserve at least the same chance.
 Ask that any feedings at which you cannot nurse be given by gavage (through the nose) rather than by bottle. If your baby is given bottle feedings while you’re trying to establish breastfeeding, nipple confusion could interfere with your efforts. If human milk fortifier or other fortification is given to your baby to supplement the breast milk, ask that it, too, be given by gavage or by the supplementary nutrition system (see page 167).
Ask that any feedings at which you cannot nurse be given by gavage (through the nose) rather than by bottle. If your baby is given bottle feedings while you’re trying to establish breastfeeding, nipple confusion could interfere with your efforts. If human milk fortifier or other fortification is given to your baby to supplement the breast milk, ask that it, too, be given by gavage or by the supplementary nutrition system (see page 167).
You’ll be able to tell how well your baby is doing on the breast by following her daily weigh-in. If she continues gaining about 1 to 2 percent of her body weight daily, or about 3½ to 7½ ounces a week, she’ll be doing fine. By the time she reaches her original due date, she should be approaching the weight of a full-termer—somewhere around 6 to 8 pounds.
“So far I’ve handled our baby only through the portholes of her isolette. But I’m worried about how well I’ll be able to handle her when she finally comes home. She’s so tiny and fragile.”
When your baby finally makes that long-anticipated trip home, she may actually seem pudgy and sturdy to you, rather than tiny and fragile. Like many preemies, she’ll probably be double her birthweight by the time she hits the requisite 4 or 5 pounds necessary for discharge. And chances are you won’t have any more trouble caring for her than most new parents have caring for their full-term babies. In fact, if you have a chance to do some baby care at the hospital (something you should insist on) in the weeks before your baby’s homecoming, you’ll actually be ahead of the game. Which is not to say it will be easy—rare is the new parent (of preemie or full-termer) who finds it so.
When will that moment come? Chances are, the momentous homecoming will take place approximately at the same time it would have if your baby had been born full-term, at 40 weeks—though occasionally a baby may be discharged as early as two to four weeks before his or her due date. Most hospitals don’t have a specific weight requirement. Instead, babies are usually sent home once they meet the following criteria:
 are able to maintain normal body temperature in an open crib
are able to maintain normal body temperature in an open crib
 have graduated to breast or bottle feedings only
have graduated to breast or bottle feedings only
 are gaining weight on breast or bottle feedings
are gaining weight on breast or bottle feedings
 are breathing on their own
are breathing on their own
 show no sign of apnea (pauses while breathing)
show no sign of apnea (pauses while breathing)
If you’re wondering how well you and your baby will do without a nurse or neonatologist looking over your shoulder and ready to step in if anything goes wrong, be assured that hospitals don’t send home babies who are still in need of full-time professional care. Most NICUs offer parents the opportunity to spend the night with their baby in a family room close to the nursery but without any nursery staff supervision. Still, some parents, particularly those who come home with such extra paraphernalia as breathing monitors or oxygen hoods, find it comforting to hire a baby nurse who has had experience with preemies and their medical care to help them through the first week or two. Consider this option if you’re anxious about going at it alone.
“Though the doctor says our baby is doing well, I’m still afraid that he’ll come through this with some kind of permanent damage.”
One of the greatest miracles of modern medicine is the rapidly increasing survival rate for premature infants. At one time, a baby weighing in at 1,000 grams (about 2 pounds, 3 ounces) had no chance of making it. Now, thanks to the advances in neonatology, many babies who are born even smaller than that can be expected to survive.
Of course, along with this increased survival rate has come an increase in the number of babies with moderate to severe handicaps. Still, the odds of your baby’s coming home from his hospital stay both alive and well are very much in his favor. Only an estimated 10 percent of all preemies and 20 percent of those between 1½ and 3½ pounds end up with major handicaps. The risks of permanent disability are much greater for those who are born at 23 to 25 weeks and/or weigh less than 25 ounces; still, of the 40 percent of these infants who survive, more than half do well.
Overall, better than 2 out of 3 babies born prematurely will turn out to be perfectly normal, and most of the others will have only mild to moderate handicaps. Most often the baby’s IQ will be normal, though preterm infants do have an increased risk of learning problems.
As your baby grows, it will be important to keep in mind that he will have some catching up to do before his development reaches the normal range for his birth age. His progress is likely to follow more closely that of children of his corrected age; see next question. If he was very small, or had serious complications during the neonatal period, he is very likely to lag behind his corrected agemates too, particularly in motor development.
It may be slower going in the neuromuscular department, too. Some preemies may not lose such newborn reflexes as the Moro, tonic neck, or grasp reflexes as early as term infants, even taking corrected age into account. Or their muscle tone may be abnormal, in some cases causing the head to droop excessively, in other cases causing the legs to be stiff and the toes to point. Though such signs may be a sign that something’s wrong in full-term babies, they’re usually nothing to worry about in pretermers. (Still, they should be evaluated by the physician, and physical therapy should be begun if necessary.)
Slow developmental progress in a preemie is not cause for alarm, it is to be expected. If, however, your baby seems not to be making any progress week to week, month to month, or if he seems unresponsive (when he’s not ill), speak to his doctor. If the doctor doesn’t share your concerns but doesn’t allay them either, ask for a second opinion. Not infrequently, a parent, who sees her baby day in and day out, catches something the doctor misses. If there turns out to be no problem, which will most often be the case, the second opinion will help to ease your fears. If a problem is discovered, the early diagnosis could lead to treatment as well as ongoing training and care, which may make a tremendous difference in the ultimate quality of your baby’s life.
“Our son, who was born nearly two months early, seems very far behind compared with other three-month-olds. Will he ever catch up?”
He’s probably not “behind” at all. In fact, he’s probably just where a baby conceived when he was should be. Traditionally, in our culture, a baby’s age is calculated from the day he was born. But this system is misleading when assessing the growth and development of premature infants, since it fails to take into account that at birth they have not yet reached term. Your baby, for example, was just a little more than minus two months old at birth. At two months of age he was, in terms of gestational age (calculated according to his original due date), equivalent to a newborn. At three months, he’s more like a one-month-old. Keep this in mind when you compare him to other children his age or to averages on development charts. For example, though the average baby may sit well at seven months, your child may not do so until he’s nine months old, when he reaches his seventh-month corrected age. If he was very small or very ill in the neonatal period, he’s likely to sit even later. In general, you can expect motor development to lag more than the development of the senses (vision and hearing, for example).
Experts use the gestational age, usually called “corrected age,” in evaluating a premature child’s developmental progress until he’s 2 or 2½ years old. After that point, the two months or so differential tends to lose its significance—there isn’t, after all, much developmental difference between a child who is four years old and one who is two months shy of four. As your baby gets older, the behavior gap between his corrected age and his birth age will diminish and finally disappear, as will any developmental differences between him and his peers (though occasionally, extra nurturing may be needed to bring a preemie to that point). In the meantime, if you feel more comfortable using his corrected age with strangers, do so. Certainly do so when assessing your baby’s developmental progress.
Instead of looking for specific behaviors from your baby at specific times, relax and enjoy his progress as it comes, providing support as needed. If he’s smiling and cooing, smile and coo back at him. If he’s starting to reach for things, give him the opportunity to practice that skill, too. When he can sit propped up, prop him in different surroundings for a while each day. But always keep his corrected age in mind, and don’t rush him or push him.
Use the infant stimulation tips in this book (pages 242, 366, 502), gearing them to your baby’s behavior rather than his age, and be careful to stop when he signals that he’s had enough. You can, additionally, encourage motor development by placing your baby on his tummy, facing outward toward the room rather than toward the wall, as often and for as long as he’ll tolerate it (but only when he is carefully supervised). Since preemies and low-birthweight babies spend most of their early weeks, sometimes months, on their backs in isolettes, they often resist this “tummy to play” position, but it’s a necessary one for building arm and neck strength.
If, of course, your baby is far behind developmentally even after making allowances for his prematurity, and if he seems to stay that way, read page 472 and check with his doctor.
“My baby seems way too small for the infant car seat. Wouldn’t she be safer in my arms?”
It’s not only unsafe but illegal for a baby (premature or full-term) to ride in somebody’s arms rather than in a car seat. Every baby, no matter how tiny, must be buckled up safely, securely, and snugly each and every time he or she’s in a moving vehicle. But parents of low-birthweight babies often find that their especially little babies seem lost in a standard rear-facing infant car seat. The AAP recommends the following when choosing and using a car seat for your preemie:
 Select a car seat that will fit your baby. Look for ones that have less than 5½ inches from the crotch strap to the seat back. This will help keep your baby from slouching. Also, look for one that measures less than 10 inches from the lowest harness strap position to the seat bottom so that the harness won’t cross over your baby’s ears.
Select a car seat that will fit your baby. Look for ones that have less than 5½ inches from the crotch strap to the seat back. This will help keep your baby from slouching. Also, look for one that measures less than 10 inches from the lowest harness strap position to the seat bottom so that the harness won’t cross over your baby’s ears.
 Make it fit even better. Roll a towel or small blanket and arrange it so that it pads the seat at the sides of her head, or buy a ready-to-use head roll designed for infant car seats. If there’s a big gap between your baby’s body and the harness, use a folded towel or blanket to fill it in. But don’t place one under baby.
Make it fit even better. Roll a towel or small blanket and arrange it so that it pads the seat at the sides of her head, or buy a ready-to-use head roll designed for infant car seats. If there’s a big gap between your baby’s body and the harness, use a folded towel or blanket to fill it in. But don’t place one under baby.
Some premature babies have trouble breathing in the semipropped position the seat requires. One study has shown that these infants may show a decreased oxygen supply while riding in a car seat, and that this deficit may last for as long as thirty minutes or more afterward. Some may also experience short periods of apnea (breathing cessation) in car seats. Make sure your baby is observed and monitored in the car seat by the hospital staff before going home. If your baby does experience problems in the car seat, use a crash-tested infant car bed, in which the infant is lying down rather than propped and which protects her in case of a crash without compromising breathing. If for any reason you can’t obtain such a bed or a seat designed for a preemie, you may want to limit the amount of auto travel you do with your baby for the first month or two at home, especially if she has had spells of apnea previously. Or ask her doctor about monitoring her breathing when she’s in an ordinary car seat, at least for a while, to see if she is experiencing any problems.
For most of your premature baby’s first two years, his or her corrected age will be the one that counts most, except in one area: immunizations. Most of a baby’s vaccine schedule isn’t delayed because of prematurity, so instead of receiving vaccines according to gestational age, he or she will receive them according to birth age. In other words, if your baby was born two months early, he or she will still get those first shots at age two months—not age four months. There are, however, two exceptions. First, doctors will usually wait until a baby weighs 3 pounds, 5 ounces before vaccinating (most infants will weigh at least 4 pounds by age two months). Second, the hepatitis B vaccine is not given to a premature infant at birth (as it sometimes is for full-termers). Instead, doctors will wait until the baby weighs in at a minimum of 4 pounds, 6 ounces.
Don’t worry about your tiny baby’s not being able to produce antibodies to the vaccines. Researchers have found that at seven years, even children who were born extremely small have antibody levels similar to other children the same age.
The same breathing problems may occur in young premature babies in infant seats and baby swings, so don’t use either without the doctor’s approval.
“I know that I wasn’t as careful during my pregnancy as I should have been. And even though the doctor said it probably wasn’t my fault, I can’t help blaming myself for my son being born so early.”
There’s probably not one mother of a premature baby who doesn’t look back and regret something she did during pregnancy that she might have done better—something she fears might have contributed to her baby’s early arrival.
Such feelings of remorse are normal but not productive. Besides, it’s almost impossible to be sure just what factor or factors are responsible for your baby’s early arrival. In many cases, what a mother did or didn’t do during pregnancy had no impact (and no expectant woman does everything right). Even if you are sure that your behavior or lifestyle played a part, assigning blame is not going to help your baby. What your baby needs now is a mother who is strong, loving, and supportive, not one who is paralyzed by feelings of guilt.
Read chapter 21, which concerns newborns with special needs for some suggestions on how to deal with your feelings of guilt, anger, and frustration. It may also help to talk to other parents of preemies. You will find they share many of your feelings. Some hospitals have parent support groups; others feel parents do better consulting with the staff than with other parents. Do what seems to help you most.
HOME-CARE TIPS FOR PRETERM BABIES
Even once they’ve reached the age of full-term babies, preemies continue to need some special care. As you prepare to take your baby home, keep these tips in mind:
 Read the month-by-month chapters in this book. They apply to your preterm baby as well as to full-termers. But remember to adjust for your baby’s corrected age.
Read the month-by-month chapters in this book. They apply to your preterm baby as well as to full-termers. But remember to adjust for your baby’s corrected age.
 Keep your home warmer than usual, about 72°F or so, for the first few weeks that your baby is at home. The temperature regulating mechanism is usually functioning in premature infants by the time they go home, but because of their small size and greater skin surface in relation to fat, they may have difficulty keeping comfortable without a little help. In addition, having to expend a great many calories to keep warm could interfere with weight gain. If your baby seems unusually fussy, check the room temperature to see if it’s warm enough. Feel baby’s arms, legs, or the nape of the neck to be sure it isn’t too cool in the room. (However, don’t overheat the room.)
Keep your home warmer than usual, about 72°F or so, for the first few weeks that your baby is at home. The temperature regulating mechanism is usually functioning in premature infants by the time they go home, but because of their small size and greater skin surface in relation to fat, they may have difficulty keeping comfortable without a little help. In addition, having to expend a great many calories to keep warm could interfere with weight gain. If your baby seems unusually fussy, check the room temperature to see if it’s warm enough. Feel baby’s arms, legs, or the nape of the neck to be sure it isn’t too cool in the room. (However, don’t overheat the room.)
 Buy diapers made for preemies, if necessary. You can also buy baby clothes in preemie sizes, but don’t buy too many—before you know it, your baby will have outgrown them.
Buy diapers made for preemies, if necessary. You can also buy baby clothes in preemie sizes, but don’t buy too many—before you know it, your baby will have outgrown them.
 Sterilize bottles, if you’re giving them, by boiling them before the first use and running them through a hot dishwasher after each feeding. Though it may be an unnecessary precaution for a term baby, it’s a good one to take for preemies, who are more susceptible to infection. Continue for a few months, or until baby’s doctor gives you the okay to pack away the sterilizer.
Sterilize bottles, if you’re giving them, by boiling them before the first use and running them through a hot dishwasher after each feeding. Though it may be an unnecessary precaution for a term baby, it’s a good one to take for preemies, who are more susceptible to infection. Continue for a few months, or until baby’s doctor gives you the okay to pack away the sterilizer.
 Feed your baby frequently, even though this may mean spending most of your time nursing or bottle feeding. Preemies have very small stomachs, and they may need to fill them up as often as every two hours. They also may not be able to suckle as efficiently or effectively as full-termers, and so they may take longer—as long as an hour—to drink their fill. Don’t rush feedings.
Feed your baby frequently, even though this may mean spending most of your time nursing or bottle feeding. Preemies have very small stomachs, and they may need to fill them up as often as every two hours. They also may not be able to suckle as efficiently or effectively as full-termers, and so they may take longer—as long as an hour—to drink their fill. Don’t rush feedings.
 Ask the doctor if your baby should be receiving a baby multivitamin supplement. Preterm babies can be at greater risk of becoming vitamin deficient than full-termers and may need this extra insurance.
Ask the doctor if your baby should be receiving a baby multivitamin supplement. Preterm babies can be at greater risk of becoming vitamin deficient than full-termers and may need this extra insurance.
 Don’t start solids until your doctor gives the go-ahead. Generally, solids are introduced to a preterm infant when weight reaches 13 to 15 pounds, when more than 32 ounces of formula is consumed daily for at least a week, and/or when the corrected age is six months. Occasionally, when a baby is not satisfied with just formula or breast milk, solids may be started as early as four months, corrected age.
Don’t start solids until your doctor gives the go-ahead. Generally, solids are introduced to a preterm infant when weight reaches 13 to 15 pounds, when more than 32 ounces of formula is consumed daily for at least a week, and/or when the corrected age is six months. Occasionally, when a baby is not satisfied with just formula or breast milk, solids may be started as early as four months, corrected age.
 Relax. Without a doubt, your baby has been through a lot—and so have you. But once he or she is home, and once you’ve taken the above precautions, try to put the experience behind both of you. As great as the impulse may be to hover or overprotect, aim instead to treat your baby like the normal, healthy child he or she is now.
Relax. Without a doubt, your baby has been through a lot—and so have you. But once he or she is home, and once you’ve taken the above precautions, try to put the experience behind both of you. As great as the impulse may be to hover or overprotect, aim instead to treat your baby like the normal, healthy child he or she is now.
Prematurity is risky business. Tiny bodies are not fully mature, many systems (heat regulatory, respiratory, and digestive, for example) aren’t yet fully operative, and not surprisingly, the risk of neonatal illness is increased. As the technology for keeping such babies alive improves, more attention is being given to these common preemie conditions, and completely successful treatment is becoming more and more the norm for many of them. (New treatments are being developed almost daily and so may not be detailed here, so be sure to ask your neonatologist or pediatrician about recent advances.) The medical problems that most frequently complicate the lives of preterm infants include:
Respiratory distress syndrome (RDS). Because of immaturity, the premature lung often lacks pulmonary surfactant, a detergent-like substance that helps keep the air sacs (alveoli) in the lungs from collapsing. Without surfactant the tiny air sacs collapse like deflating balloons with each expiration, forcing the tiny baby to work harder and harder to breathe. Babies who have undergone severe stress in the uterus, usually during labor and delivery, are less likely to lack surfactant, as the stress appears to speed lung maturation.
RDS, the most common lung disease of premature infants, was once frequently fatal, but more than 80 percent of babies who develop RDS today survive, thanks to an increased understanding of the syndrome and new ways of treatment. Extra oxygen is given via a plastic oxygen hood, or via continuous positive airway pressure (CPAP), which is administered through tubes that fit into the nostrils of the nose or mouth. The continuous pressure keeps the lungs from collapsing until the body begins producing sufficient surfactant, usually in three to five days. For babies with severe RDS, a breathing tube is placed and the baby put on a respirator. Surfactant is then administered directly to the baby’s lungs via the breathing tube. Sometimes, when lung immaturity is detected in utero, RDS can be prevented entirely by the prenatal administration of a hormone to the mother, to speed lung maturation and production of surfactant.
A mild case of RDS usually lasts for the first week of life, though if the baby is placed on a respirator, the recovery may be much slower. Babies with severe cases of RDS may be at an increased risk of colds or respiratory illnesses during their first two years of life, a greater likelihood of childhood wheezing or asthmalike illnesses, and a greater likelihood of being hospitalized in their first two years.
Bronchopulmonary dysplasia (BPD). In some babies, particularly those born very small, long-term oxygen administration and mechanical ventilation appear to combine with lung immaturity to cause BPD, or chronic lung disease. The condition, which results from lung injury, is usually diagnosed when a newborn still requires increased oxygen after reaching 36 weeks’ gestation. Specific lung changes are generally seen on X rays, and these babies frequently gain weight slowly and are subject to apnea. Treatment of BPD includes extra oxygen; continued mechanical ventilation; medications such as bronchodilators (to help open the airways) or steroids (to reduce inflammation); limiting fluids or giving diuretics (to reduce excess fluid, which can worsen breathing); RSV and influenza vaccinations. A few babies continue to require oxygen when they go home, and all require a high caloric intake to improve growth. Often the condition is outgrown as the lungs mature, though babies with BPD may be at increased risk for respiratory infections.
Apnea of prematurity. Though apnea, periods of breathing cessation, can occur in any newborn, this problem is much more common among premature infants. Apnea of prematurity occurs when preemies’ immature respiratory and nervous systems cause them to stop breathing for short periods. It is diagnosed when a baby has such periods that last more than 20 seconds or that are shorter but are associated with bradycardia, a slowing of the heart rate. It is also considered apnea if the cessation of breathing is associated with the baby’s color changing to pale, purplish, or blue. Almost all babies born at 30 weeks or less will experience apnea.
Apnea is treated by stimulating the infant to start rebreathing by rubbing or patting the baby’s skin, administering medication (such as caffeine or theophylline), or by using continuous positive airway pressure (CPAP), in which oxygen is delivered under pressure through little tubes into the baby’s nose. Many babies will outgrow apnea by the time they reach 36 weeks’ gestation. Occasionally, monitoring at home may be required, though most babies no longer show signs of apnea by the time they are ten weeks past their due date. Apnea of prematurity is not associated with SIDS. If a baby has breathing pauses after apnea goes away, it is not considered apnea of prematurity and is more likely due to some other problem.
Patent ductus arteriosus. While baby is still in the uterus, there is a duct connecting the aorta (the artery through which blood from the heart is sent to the rest of the body) and the left pulmonary artery (the one leading to the lungs) called the ductus arteriosus. This duct shunts blood away from the nonfunctioning lungs and is kept open during gestation by high levels of prostaglandin E (one of a group of fatty acids produced by the body) in the blood. Normally, levels of prostaglandin E fall at delivery, and the duct begins to close within a few hours. But in about half of very small premature babies (those weighing 3 pounds, 5 ounces), and in some larger babies, levels of prostaglandin E don’t drop and the duct remains open or “patent.” In many cases there are no symptoms, except a heart murmer and a little shortness of breath on exertion and/or blueness of the lips, and the duct closes by itself sooner after birth. Occasionally, however, severe complications occur. Treatment with an antiprostaglandin drug (indomethacin) is often successful in closing the duct; when it isn’t, surgery generally does the job.
Retinopathy of prematurity (ROP). This condition, caused by abnormal growth of the blood vessels in an infant’s eye, affects 85 percent of babies born earlier than 28 weeks. Though babies born between 28 and 34 weeks are also at risk (though not at such a high percentage), typically only the smallest premies, no matter what their gestational age, have the highest risk. It was once thought to be caused by excessive oxygen administration, but it is now known that a high level of oxygen is only one of the factors involved, and doctors are still trying to determine what other factors might contribute to ROP. Close monitoring of blood gases in the infant when oxygen therapy is given is now routine and does seem to help minimize the risk of ROP.
Since ROP can lead to scarring and distortion of the retina, increased risk of nearsightedness (myopia), wandering eye (amblyopia), involuntary rhythmic movements of the eye (nystagmus), and even blindness, a newborn with ROP will need to be seen by a pediatric ophthalmologist. Infants with severe ROP may require treatment to stop the progression of the abnormal vessels. With treatment, the inner lining of the eye at the ends of these vessels is killed to prevent further abnormal growth of the blood vessels.
Intraventricular hemorrhage (IVH). IVH, or bleeding in the brain, is extremely common among premature infants because the vessels in their developing brains are very fragile and can bleed easily. Intraventricular hemorrhage strikes 15 to 20 percent of preemies weighing less than 3 pounds, 5 ounces, most often within the first 72 hours of life. The most severe hemorrhages (which strike only 5 to 10 percent of extremely premature babies) require close observation to correct any further problems that develop—for example, hydrocephalus (blockage of spinal fluid). Regular follow-up ultrasounds are usually ordered for such hemorrhages until they are resolved. Babies with the more severe-grade hemorrhages are also at greater risk for seizures immediately, and handicaps later on. There is no specific treatment for IVH. Surgery will not prevent or cure the bleeding. In mild cases (and most cases are), the blood is absorbed by the body. Usually the follow-up head ultrasound is normal and the baby’s development is normal for a preterm baby.
Necrotizing enterocolitis (NEC). NEC is an inflammation of the intestines that doesn’t occur until feedings have begun. The cause is unknown, but because the more premature a baby is, the greater the risk of NEC, doctors speculate that the intestines of very premature babies are not developed enough to completely handle digestion. Babies fed breast milk get NEC less often than babies fed formula. The symptoms of this serious bowel disease include abdominal distension, bilious vomiting, apnea, and blood in the stool. A baby with necrotizing enterocolitis is usually put on intravenous feedings and antibiotics. If there is serious deterioration of the intestine, surgery is usually performed to remove the damaged portion.
Anemia. Many premature infants develop anemia (too few red blood cells) because their red blood cells (like all babies’) have a shorter life than red blood cells of adults (this may be exaggerated if the baby’s blood type is different from the mother’s), they make few new red blood cells in the first few weeks of life (like all infants), and the frequent blood samples that must be taken from the baby to do necessary laboratory tests make it difficult for red blood cells to replenish. Mild anemia may not need treatment if the number of red blood cells is enough to carry oxygen to meet the baby’s needs. Severe anemia is usually treated by giving the baby a blood transfusion. Since preemies, whether they’re anemic or not, are born with low levels of iron, they are usually given iron supplements to help them build up the reserves necessary to produce red blood cells.
Infection. Premature infants are most vulnerable to a variety of infections because they are born before the transfer of disease-fighting antibodies from the mother that normally occurs toward the end of pregnancy. Preemies also have an immature immune system, making it more difficult to fight germs, including those that are introduced via feeding tubes, IV lines, and blood tests. Among the infections preemies are more likely to come down with are pneumonia, urinary tract infections, sepsis (infection of the body or bloodstream), and meningitis. Babies whose blood, urine, or spinal fluid cultures come back positive for signs of infection are treated with a full course of IV antibiotics.
Happily, most premature babies who go home from the hospital stay home. But sometimes, a preemie ends back in the hospital during the first year, usually for the treatment of a respiratory illness or dehydration. When this happens, it’s particularly tough on the parents, who have been struggling to put the time spent in the NICU behind them and begin a normal life with their babies. Memories and all-too-familiar emotions may come flooding back if your baby is rehospitalized, from feelings of guilt (“What did I do wrong?”) to feelings of fear and panic (“What happens if my baby gets sicker?”). After finally having your baby home and under your care, you may also feel as though you’ve lost control again.
Try to keep in mind that rehospitalization usually doesn’t last long, and that, like your child’s stay in the NICU as a newborn, the stay in the hospital (more likely to be in the PICU, or pediatric intensive care unit) will also come to an end—at which point you’ll be able to bring your baby home once again, this time, hopefully, for good.
Jaundice. Premature babies are much more likely to develop jaundice than are full-term infants. Also, their bilirubin levels (the measure of jaundice) are likely to be higher and the jaundice longer lasting. Read about the condition on page 129.
Hypoglycemia. Low blood sugar in an infant is often unrecognized and untreated because symptoms may be absent or not apparent. Consequently, it can lead to such serious complications as brain damage. It’s most commonly a problem among multiples, when the smaller or smallest baby weighs less than 4½ pounds, and in babies of diabetic moms (who usually have high, rather than low, birthweights). Hypoglycemia is routinely screened for during the first 24 to 48 hours, and if it’s found, treatment to normalize sugar levels is begun immediately.
Low blood pressure. This condition is common in preemies after birth because of blood loss before or during delivery, fluid loss after delivery, infection, or medications given to the mother before delivery. Low blood pressure also often accompanies RDS. It is treated by increasing fluids, by giving the baby medications to increase blood pressure, or by giving a blood transfusion, if necessary.

1. In some hospitals, this unit is called an intensive care nursery (ICN).