The Oral Microbiome
“The mouth houses the second most diverse microbial community in the body.”
—Mogens Kilian and colleagues; professor, Department of Biomedicine, Aarhus University, Denmark43
In this chapter we will find out where we get our oral microbiome from and who might have a similar one. We will review the benefits of our commensal microbes and why they are so vital to our health. We will talk about Streptococcus, the big bacterial player in the mouth, as well as the Firmicutes and Bacteroidetes phyla, which dominate the gut and the oral microbiomes.
Figure 5.1: Bacteria in the mouth. Both good and bad bacteria live in the mouth, but mostly good.
Twenty billion bacteria live in your mouth, representing a whopping 770 species. That’s nearly three times the Earth’s human population. These bacteria thrive in a sea of saliva. There are a number of different microenvironments in the oral cavity where bacteria can grow and make a home. As we discussed earlier, they may live in and on the tongue, throat, tonsils, and saliva; the gums, cheeks, and roof of the mouth; the teeth, above the gumline; and the teeth, below the gumline. Each of these ecological niches supports and sustains not just a few bacteria, but huge, complex communities of bacteria.
Most of your oral microbiota are normal and healthy. They can improve your health by balancing your immune system, keeping the bad bugs at bay, and helping keep a healthy barrier between your mouth and your bloodstream. There are also harmless bacteria, fungi, and viruses in the mouth. They don’t necessarily do anything good for you, but they cause no harm either. And of course, there are a few bad bugs lurking around and waiting for a chance to take over and cause trouble. They are often waiting for dysbiosis, or imbalanced microbial communities, which gives them a window of opportunity to move in and rise to power. We will learn more about dysbiosis of the oral microbiota and oral pathogens in Chapter 6.
Breakthroughs in DNA analysis led to an explosion of research on the microbiome, and since then, we have discovered countless new species that had been invisible up to that point. Our older methods of culturing bacteria in a petri dish missed approximately 50 percent of the bugs living in our mouths.44 We now use molecular methods that identify bacteria based on their genetic code; these are more precise and they don’t require that the bug grow in an artificial environment. Even in 2018, the Human Oral Microbiome Database admits that of 770 oral microbiome species we now know of, only 57 percent have names and have been properly characterized.45 When it comes to the microbes that live in our mouths and influence our whole-body health, we have only scratched the surface.
As a way to organize and understand the tremendous number of bacteria in the world, they are often categorized as aerobic or anaerobic. Aerobic bacteria can live in oxygen. Anaerobic bacteria don’t do well (and can die) in oxygen. Anaerobic bacteria tend to be found in deep, dark crevices where the air cannot reach them, such as the gut or on the teeth below the gumline.
Microbiologists also classify the big world of bacteria as gram-negative and gram-positive; this simply describes the cell walls of bacteria. Gram-positive bacteria have a thick cell wall with peptidoglycan and teichoic acids, which will stain purple. Gram-negative bacteria have a thin peptidoglycan layer and will not stain purple. This characterization is a throwback from the days when we couldn’t analyze bacteria based on their DNA, only on how they were tested or how they grew in a petri dish on a laboratory bench.
Benefits of the Microbiome
Commensal organisms, or indigenous organisms, are the microbes that naturally colonize our bodies and either benefit us or do no harm. These are the “good guys.” You don’t want to leave home without them. While we are still in the beginning stages of understanding how commensal microbes benefit our health, it seems that they may help to prevent allergies, eczema, asthma, reflux esophagitis, inflammatory bowel disease, irritable bowel syndrome, psoriasis, obesity, cancer, and cardiovascular disease.46, 47
Your commensal microbes protect you from invasion by foreign outsiders that mean to cause you harm. Bad bugs are always around, but with enough good bugs, you are protected. Good bugs work together to promote stability and resilience of the microbiome so that big changes, like those that occur after taking medication, don’t lead to a total crisis, such as an infection.
Contrary to popular belief, healthy people often carry low levels of pathogens or disease-causing bacteria in their mouths.48 But these pathogenic bacteria don’t cause a problem because the mouth is protected by a strong defense of good commensal microbes.
Beneficial commensal organisms make chemicals that repel or destroy bad bacteria. They can even direct the immune system to a bad bug. It’s as if they say to the immune cells, “Hey! There’s the bad guy over there!”
Your good bacteria help to keep a strong mucosal barrier, thereby protecting you from the outside world. Commensal microbes prime, or teach, the immune system to tolerate “good bugs.” As we discussed in Chapter 4, the immune system’s default setting is inflammation and attack. Your commensal bacteria turn on T regulatory cells that teach acceptance and tolerance. With that knowledge, the immune system can spend its efforts seeking out and destroying bad bugs, not the good ones.49 Your commensal microbes can even help make blood pressure–lowering chemicals that boost your cardiovascular health (more on this in Chapter 8).
As if that weren’t enough, your commensal microbiota make nutrients and help you digest your food. Commensal bacteria make vitamin K, which helps your blood clot, builds healthy bones, and makes sure your blood flows smoothly through clean arteries. They also make biotin, a B vitamin that helps you make fuel from carbohydrates, fats, and proteins while giving you strong and beautiful hair, nails, and skin. Commensal bacteria ferment the food that you can’t digest, making fatty acids (called short-chain fatty acids) that actually boost the health of your gut cells and can help to prevent colon cancer.50 You can find a list of human commensal oral bacteria on page 85.
The Oral Mycobiome
While bacteria are the major players in the oral microbiome, fungi have a place in our mouths as well. Fungi make up a smaller percentage of the microbes in the mouth, with the average healthy mouth’s mycobiome (or fungal biota) carrying 9 to 23 species. Candida is the most common fungal genus found in the mouth and Candida albicans is the most common species. Candida has been found on dental plaque.51 Other fungal genera found in the mouth include Cladosporium, Aureobasidium, Saccharomyces, Aspergillus (or mold), Fusarium, and Cryptococcus.52
The Oral Virome
Viruses may trump the total bacteria count in the mouth by as much as 35 times!53 But most of these viruses in the oral virome (or viral biota) prey on bacteria, not humans. Bacteriophages are viruses that attack or even benefit bacteria. Therefore, wherever bacteria live (all over and in our bodies), bacteriophages live, too. Bacteriophages are the most numerous organisms on earth, and the diversity of bacteriophages closely aligns with the diversity of bacteria. Other viruses have been found in the oral cavity including herpes simplex virus (the virus that causes cold sores or genital herpes), varicella zoster virus (the virus that causes chickenpox or shingles), and human papilloma virus (the cause of warts on the skin or mucous membranes, including genital warts or cervical cancer).54
Your personal oral microbiome is unique. This has been one of the challenges in understanding the microbiome, because we cannot easily define what is a normal microbiome and what is dysbiotic. Researchers are trying to characterize core microbiomes, or enterotypes, to help us address the tremendous variation in the bacteria that colonize us, which is totally normal and healthy. For example, in a study of the oral microbiota, the same 78 bacterial species were found in almost everyone (90 percent of participants). Yet 24 bacterial species were found in every single person (100 percent of participants).55 Even though there is a lot of variety in the microbial communities in our mouths, there are common bugs that colonize most of us—hence a core microbiome.
Your oral microbiome is probably most similar to those of the people living in your home who eat a similar diet to you. You probably even share some oral microbes with your house pets! Laboratory testing, or at-home testing, of your oral microbiome is therefore helpful to monitor the makeup of your oral microbiome over time. We will talk about this in the “Testing” section of Chapter 9, Oral Microbiome Solutions.
The Origins of Your Microbiome
So where do all of these microbes come from? Your mama. Seriously! You get your starter pack of bacteria, fungi, and viruses from your mother. And how we are born affects the oral microbiome and the gut microbiome. When a baby is slowly descending the birth canal, they get smeared with all of the vaginal microbes that colonize the mother. This is a major first inoculation. Lactobacillus bacteria are high in the vaginal microbiome, and babies born vaginally have high levels of this bug in their feces for their first few days of life. In fact, babies born vaginally end up with a gut microbiota that looks like their mom’s, to the tune of 83 percent similar. And they have a rich, diverse collection of microbes, which is an indicator of microbial health.56, 57
With nearly one-third of babies in the United States being born by Cesarean section, not all babies get this starter pack, unfortunately. Babies born by C-section have a fecal microbiota that is only 42 percent similar to that of their mothers. Since C-section babies are not getting exposed to their mother’s vaginal microbes, their microbiomes are composed of the bugs in their environment or the first things they touch or eat (like from mother’s skin microbiota). The majority of babies that were born by C-section had high levels of the periodontal pathogen Slackia exigua, but babies born vaginally were free of this microbe. C-section babies also have less diversity in their oral microbiomes than babies born vaginally.58, 59 Babies born by C-section are more likely to have asthma, allergies, and eczema, leading some experts to believe that the commensal bacteria from mother’s vaginal microbiome is key in preventing these diseases.60
Breastfeeding also delivers a package of healthy microbes to the baby’s mouth and gut. Breastmilk is high in probiotic bacteria and the prebiotics needed to feed them! Seeding the newborn gut with mother’s bacteria promotes a healthy response to inflammation, helps introduce it to commensal bacteria, and jumpstarts the immune system. Breastmilk also contains immune-boosting proteins that can prevent the spread of pathogenic bacteria. Secretory IgA from mother’s milk can destroy bacteria and protect the mucosal membranes. Delivering commensal bacteria, the prebiotics that feed them, and proteins that help to prevent dysbiosis means we have yet another thing to thank our moms for!61, 62
All bacteria live in biofilm. A biofilm is a group of microorganisms that attach themselves to a surface and cover themselves with a protective shield (or slime). This mechanism helps microbes stay attached to a surface so that they don’t get swept or washed away. The stuff that coats a biofilm is officially called “extracellular polymeric substance.” It’s made of polysaccharides, or a long chain of carbohydrates, which provide structure and can grab on to tougher minerals like magnesium and calcium to further strengthen the protective shield of the biofilm.
The first biofilm ever discovered was dental plaque! This was a tremendous realization to me, because we talk about microbial biofilms all the time when we talk about the gut microbiome. You might hear about treatments to break biofilms—these are used when trying to eliminate one or more pathogenic microbes.
Wherever there is microbial growth, it is pretty much guaranteed to be in biofilm. But biofilms don’t just help protect bacteria and other bugs from being brushed away. A biofilm is like a little castle where microbes live. Inside the biofilm are little villages of bacteria, fungi, and other organisms. These “microcolonies” are typically separated by water channels.63 For many years, scientists and doctors have been talking about bacteria as though they live in isolation. But just like humans, they live in communities with other microbes. They rarely live alone. Now it is widely accepted that microbes live in mixed ecological communities, not just a single microbe growing by itself in a petri dish.64
The microbes can also communicate with each other using chemical messages. They can live in harmony, but sometimes they compete with each other for control. The metabolic by-product of one bug can be a food source for another bug. Biofilms are a way that microbes can join together to protect themselves and survive treacherous conditions.65
Dental plaque was the first microbial biofilm ever discovered.
With their biofilm protection, microbes can evade the host immune system and dodge the lethal action of antibiotics. Biofilms make it easy for microbes to share genes that enhance their survival. The biofilm also appears to function as a unit, something that scientists call “quorum sensing.” This means that the biofilm can turn on genes and release chemical messages to increase or decrease its size, to produce antibiotics, to release toxins, to cooperate with other microbes, and more. The bacterial biofilm therefore operates like an organism. It’s pretty amazing that microbiota are able to do all of these things. Perhaps that’s why they have so successfully colonized the far reaches of the planet!66, 67
Every time you get a dental cleaning, your hygienist is scraping bacterial biofilms off of your teeth. Little villages of bacteria are being physically removed because their hard biofilm exterior makes it nearly impossible to get rid of them by brushing alone. Those are biofilms at work.
After you get your starter pack of microbes from your mother, other major contributors are the people around you, the environment you live in, and your diet. Bacteria are thrilled to inhabit the mouth, where there is a constant stream of yummy food. All of our bugs have evolved alongside us for millennia. They eat what we eat: the break-down products of protein, fiber, sugar, fats, and plants. Your microbiome really likes plant-based foods. A diet rich in fiber and vegetables but moderate in calories is practically guaranteed to benefit your microbiome, because fiber and vegetables are high in prebiotics. One of the most powerful ways to shift your microbiome is to eat more plant-based foods and fiber.
Prebiotics are the nondigestible carbohydrates from your diet that feed and grow beneficial microbes. This is basically the “bulk” from your diet. Since they aren’t digestible, you can’t use them for your own nutrition. Enter, your microbes. They ferment (or eat) prebiotics, which are usually nonstarch polysaccharides or oligosaccharides (long-chain or short-chain carbohydrates). When your microbes ferment prebiotics, they make short-chain fatty acids, which help prevent the overgrowth of bad bugs, boost the health of your mucosal lining, and can prevent cancer.68 The more prebiotics you eat, the more you feed your good bugs, and the happier you and your bugs are. Examples of prebiotic foods are chicory root, Jerusalem artichoke, banana, and whole grain breakfast cereal.69 You can also take prebiotics in the form of a nutritional supplement powder. Prebiotic supplements include galacto-oligosaccharides, inulin, and larch arabinogalactan.
Before we talk about individual microbes, it will be helpful to do a quick primer on scientific names and taxonomy so you know what you’re reading. A really brilliant scientist, Carl Linnaeus, figured out that we need ways to identify all of the cool plants and animals in the physical world. Each organism is taxonomically classified, meaning it has been organized and given a name in the bigger scheme of lifeforms on Earth. You probably remember this line-up from a biology class along the way:
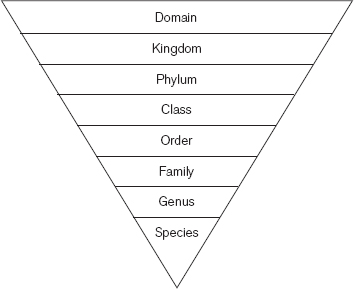
Figure 5.2: The taxonomic classification hierarchy.
Each species gets its own scientific name. It’s usually two words, and they are both italicized. The first word is the genus and the second word is the species. The genus is often abbreviated. The chart below shows two examples: one for Lactobacillus acidophilus, a common probiotic bacteria, and one for Escherichia coli (E. coli) O157:H7, the bacterium that can cause food poisoning.
Taxonomic Classification of E. coli and L. acidophilus
DOMAIN |
BACTERIA |
BACTERIA |
Kingdom |
Bacteria |
Bacteria |
Phylum |
Proteobacteria |
Firmicutes |
Class |
Gamma-proteobacteria |
Bacilli |
Order |
Enterobacteriales |
Lactobacillales |
Family |
Enterobacteriaceae |
Lactobacillaceae |
Genus |
Escherichia |
Lactobacillus |
Species |
coli |
acidophilus |
Strain (subspecies, serotype, etc) |
O157:H7 |
N/A |
Species name |
Escherichia coli O157:H7 or E. coli O157:H7 |
Lactobacillus acidophilus |
Species name is very important as you learn about the microbiome. There can be many species within one genus. For instance, Lactobacillus acidophilus is in the Lactobacillus genus, but so are Lactobacillus plantarum and Lactobacillus rhamnosus.
I also want to emphasize the phylum (phyla, when plural). As you can tell from the taxonomic hierarchy, the phylum is a very high level of category, almost as high up on the hierarchy as kingdom. Certain phyla are very important in the human microbiome. As we continue, we will be talking about the Bacteroidetes and Firmicutes phyla. They happen to be the dominant players in the gut microbiome and the oral microbiome. Other important phyla in the oral microbiome are Proteobacteria, Actinobacteria, and Fusobacteria.70
As we discussed earlier, just because the gums, tongue, tonsils, saliva, and nose are all close to each other doesn’t mean they have similar microbiomes! Take a look at the figure on page 65 to see how the different phyla are represented in the mouth and nose. Different microbial communities are seen on the gums, tongue, tonsils, and saliva. Firmicutes and Bacteroidetes phylum make up over half of the oral microbiome at all of those sites. Fusobacteria and Proteobacteria also are represented there, but in smaller portions. Actinobacteria is mostly on the sidelines in the mouth, but dominates the nose.
Phyla are the high-level “buckets” of bacteria in the microbiome. When we are talking about a genus or an individual species, we are taking a more detailed view of a microbe. Streptococcus species is one of the dominant players in the oral microbiome (Streptococcus is a genus and there are many individual species that fall within that genus). Streptococcus has a large representation in the saliva, gums, tongue, and tonsils. It is also present in the cheeks, roof of the mouth, and in dental plaque above and below the gumline (see the Summary of Human Commensal Oral Microbiota on page 85). When it comes to the oral microbiome, Streptococcus is a major part of the community!
Streptococcus species are the most abundant bacteria in the mouth.
In addition to Streptococcus, other common genera in the mouth are Fusobacterium (referring to the genus in this instance, not to be confused with the related, but much bigger, Fusobacteria phyla, above), Gemella, Neisseria, Rothia, and Veillonella. These groups of bacteria give us protection against infection, tune our immune systems, and help us keep a strong barrier against outside invaders.
Figure 5.3: Bacterial composition of distinct ecological niches in the oral cavity and nose. Firmicutes phyla includes the genus Streptococcus. Bacteroidetes and Firmicutes make up over 50 percent of microbes in the mouth. Fusobacteria and Proteobacteria phyla are also represented, but less so. Actinobacteria dominates the nose, though it is also found in the mouth.
As I’ve mentioned, the oral microbiome includes 770 species with 20 billion microbes. It’s impossible—and not very practical—to learn them all, so I have compiled a list of the more common microbes that are found in the human oral cavity from birth through adulthood (see page 85). The table also shows where the bugs live in the oral cavity and whether they colonize us when we are babies or only when we are adults. Try to remember the phyla Firmicutes and Bacteroidetes, because these are major players in the mouth and in the gut.
You have never heard of most of these bacterial names because they are harmless or beneficial, so they don’t get much press. They are also nearly impossible to pronounce. But don’t sweep them under the rug. These good bugs can save lives by holding up a biological defense and keeping bad bugs at bay. In the next chapter, we will discuss what happens when the beneficial microbes in the oral microbiome get out of balance and how that can lead to a downward spiral of disease in the mouth and the body. Later, we will talk more about the pathogenic microbial species, the ones that have been blamed for all of our diseases and ills. Their names are usually well known and notorious.
• Your commensal bacteria help protect you from infection and teach your immune system who is good and bad.
• Your microbiota are not loners; they live in complex biofilm communities. Plaque was the first biofilm ever discovered.
• Bacteria use biofilms to protect themselves, trade DNA, get resources, and evade the immune system and antibiotics.
• How you were born and if you were breastfed can significantly affect your microbiome.
• Over 40 percent of the oral microbiome is still unnamed and uncharacterized.
• Streptococcus species are the most abundant bacteria in the oral cavity.
• Bacteroidetes and Firmicutes are the dominant phyla in the oral microbiome and in the gut microbiome.