The Oral-Systemic Connection
The mouth is a “mirror of health or disease” and it may be an early indicator of disease in other tissues and organs in the body.
—Surgeon General’s Report on Oral Health, 2000
Kissing, a pretty smile, great teeth…there are so many reasons to love the mouth. On the other hand, a sick mouth can be a real turn-off. It turns out that there is more to these first impressions than meets the eye. The mouth tells us a lot about a person’s whole-body health. It can be an indicator of health or disease elsewhere in the body. As we discussed in Chapter 6, dysbiosis in the mouth can cause cavities, gingivitis, periodontal disease, and bad breath. In the US, nearly 50 percent of people over the age of 30 have periodontal disease.117 But dysbiosis of the oral microbiome doesn’t just spell trouble for the mouth—it also can lead to a domino effect of problems at distant sites, including the heart, gut, and joints.
The Link Between Oral and Heart Health
Heart disease is the number one killer in the United States. Since gum disease is highly associated with heart disease, it makes sense to address oral health as a way to promote cardiovascular health. Inflammation is a critical underlying disease process in both atherosclerosis and periodontal disease, as inflammation and dysbiosis in the oral cavity can spill over into the bloodstream. This could cause injury and damage to artery walls and contribute to the development of heart disease.
One of the most astounding discoveries is that oral pathogenic bacteria have been found in atherosclerotic plaques in the cardiovascular system. Atherosclerotic plaques are basically clots, or scabs, on the inside lining of blood vessels. If they get displaced, they can block blood vessels and cause a stroke or heart attack.118 So, the harmful substances involved in heart disease can actually contain oral pathogens like P. gingivalis, discussed in Chapter 6. A list of oral bacteria in heart disease plaques can be found on page 86.
By balancing the oral microbiome, you are treating systemic disease.
When people with periodontal disease get treatment, their blood tests for inflammation normalize and indicators of heart disease go away. And that’s not all. People who don’t keep up with brushing and flossing their teeth are more likely to have high inflammatory markers in their blood and they have a higher risk of heart disease. In fact, brushing and flossing your teeth can immediately reduce your risk of future heart attacks. Get back on the wagon with brushing, flossing, and dental check-ups and presto!, you have low risk of heart disease again. It is uncanny.119, 120
What Is Atherosclerosis?
Atherosclerosis is a type of heart disease that narrows and hardens the arteries due to plaque build-up on the artery walls. When the arteries are filled with “junk” and stiffen up, they can’t pump blood and it can block blood flow to the heart and other parts of the body. Inflammation is a central feature of atherosclerosis and plaque build-up.121 Harmful inflammatory chemicals can put little nicks or injuries in the lining of the blood vessels. LDL, sometimes called the “bad” cholesterol, starts to stick to the blood vessel walls, which forms plaque. It goes on to attract immune cells and free radicals, which worsen the plaque production. The final result is plaque made of lipids, immune cells, and scar tissue covering the blood vessel walls. This stiffens the blood vessels so they can no longer pump blood smoothly. When a plaque breaks open, clots can form, blocking blood flow to critical areas of the body, or even causing a stroke or heart attack.
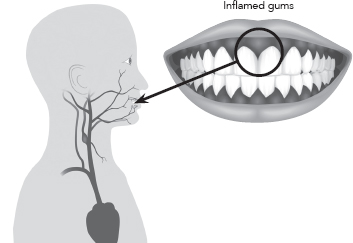
What are oral microbiota doing in the circulatory system, anyway? They simply jump on the blood superhighway. In Chapters 3 and 4, we talked about the oral mucosa being permeable and fragile. It tries to keep bad stuff out and let good stuff in. But it is porous, not air tight. For this reason, bacteria can spread from the mouth to the heart through the bloodstream.
Bacteria and chemicals can get through the oral mucous membrane and into the blood on a regular and constant basis. A high amount of bacteria measured in the blood is called “bacteremia.” Every time you brush your teeth, get a tooth pulled, or even chew your food, your blood is hit with a flood of oral bacteria.122 Well, it may not be every single time. The original study from 1954 showing this phenomena saw it occur with 40 percent of periodontal treatments, 35 percent of tooth extractions, 24 percent of brushing teeth, and 17 percent of chewing.123
Remember from Chapter 5 that most oral bacteria are beneficial and friendly. But if you have oral dysbiosis, you are effectively sending undesirable bugs coursing through your veins. Something else to know about bacteremia is that the body clears it. I think bacteremia is just a normal fact of life. But bacteremia could be much, much worse in people who have bleeding, puffy, sore gums or “leaky mouth,” which we talked about in Chapter 4. Knowing that the oral microbiome has such ready access to the whole body makes it plausible that microbial imbalances and inflammation in the oral cavity could have real impacts on the rest of the system.
Figure 8.1: Blood supply from the heart to the mouth. Note that major arteries go from the heart to the mouth. Blood returning from the mouth has direct access to the heart, which then pumps blood elsewhere in the body.
How Oral Pathogens Might Cause Heart Disease
One popular hypothesis to explain how oral disease leads to heart disease is that periodontal disease causes low-grade inflammation in the bloodstream. Remember that periodontal disease is an out-of-control inflammatory reaction to oral dysbiosis. Red, inflamed gums are like an open, weeping wound that releases high levels of inflammatory biological weapons. If you recall from our discussion in Chapter 4, the immune system is a force to be reckoned with, launching highly toxic chemical and biological warfare against overgrown oral bacteria. The large area of inflamed wound tissue, together with excessive levels of oral bacteria and frequent episodes of bacterial surges in the blood, can lead to low-grade chronic inflammation in the body, damaging the cardiovascular system.124, 125
Another hypothesis for how the oral microbiome influences heart health is that pathogenic oral bacteria from the mouth invade the bloodstream and then directly damage the walls of the circulatory system. The oral pathogens can produce toxins that damage the blood vessels and trigger inflammation (or biological warfare), which further damage the blood vessels. When the blood vessels cannot expand and contract to pump blood, it leads to atherosclerosis. Some experts have suggested that pathogenic oral microbes are involved in the instability of these plaques. Perhaps they make plaque more dangerous because a dislodged plaque can cause a clot, heart attack, or stroke. Five periodontal pathogenic bacteria that are involved in heart disease are Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis, Tannerella forsythia, Treponema denticola, and Fusobacterium nucleatum126
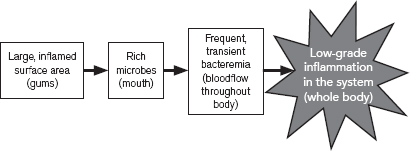
Figure 8.2: This figure illustrates one hypothesis for how oral dysbiosis can spiral out of control and cause disease in the cardiovascular system. In periodontal disease, oral bacteria grow out of control and the immune system launches a powerful, but ineffective, attack. A large area of inflamed gums, high levels of oral bacteria, and frequent surges of bacteria through the bloodstream can produce low-grade, chronic inflammation, which can damage the cardiovascular system and other organ systems.127
High-Sensitivity C-Reactive Protein
If inflammation is a central feature of heart disease, then a test that monitors inflammation would be very useful. A biological marker in blood, called high-sensitivity C-reactive protein (hs-CRP), can measure your systemic inflammation. Hs-CRP is released in the blood in response to infection, inflammation, or trauma and is widely used to monitor various inflammatory states. CRP tests are often used to measure a person’s risk of heart disease. Blood hs-CRP is often high in heart disease and in periodontal disease and can decrease into the normal range after successful treatments.128 Hs-CRP can be an important test for determining whole body disease as a result of oral dysbiosis. It’s a routine and convenient lab test and can help you monitor inflammation in your body (see more on this in Chapter 9). Hs-CRP is also called CRP, which was the original test name, until it was upgraded to be “high sensitivity.” The only difference between hs-CRP and CRP is the sensitivity. Hs-CRP can measure inflammation at much lower levels and therefore has a lower reference range. Use the physician-dentist letter on page 87 if you want to make sure your oral health isn’t revving up your inflammation.
Heart Health Benefits of the Oral Microbiome
The oral microbiome can cause trouble when it is out of balance, but your oral microbiome can also promote heart health. Did you know that your oral bacteria can lower your blood pressure? Bacteria that live in your mouth help you make a chemical called nitric oxide. Nitric oxide plays a critical role in your cardiovascular system to help relax and open the pipes that transport your blood—when your blood vessels are relaxed, blood can flow more smoothly. The result is healthy blood pressure and low risk of heart disease, heart attacks, and strokes. It’s good stuff.
Brush your teeth. Your heart will thank you for it.
And our oral bacteria help us make about 25 percent of our total daily needs of nitric oxide by processing foods such as leafy greens and beets.129 In one experiment, when the participants used antiseptic mouthwash to kill off some of the oral microbiota, the bacteria could no longer help with nitric oxide production, and blood pressure increased! It really makes you think twice about killing your oral microbes with antiseptic mouthwash—that is one reason I don’t recommend antiseptic mouthwashes often. The bugs that help lower blood pressure by creating nitric oxide are listed on page 85.
Oral microbiota detected in atherosclerotic plaques include Streptococcus species, Veillonella species, Neisseria species, and the periodontal pathogens P. gingivalis, F. nucleatum, and T forsythia. Notice that some of these are normal oral bacteria like Streptococcus species. In addition, S. sanguinis, P. gingivalis, T. denticola, and A. actinomycetemcomitans (the latter three are periodontal pathogens) were found in unstable plaques or clots in patients who had heart attacks.130
As if oral dysbiosis harming your heart health weren’t enough, oral dysbiosis can harm your joints, too. Rheumatoid arthritis (RA) is an autoimmune inflammatory joint disease that eventually destroys a joint and its function. Autoimmune diseases, like rheumatoid arthritis, are examples of what happens when the immune system becomes confused and launches an attack against the host by mistake. It’s kind of like a guard dog who gets confused and accidentally bites its owner. In rheumatoid arthritis, the joints are on fire because the immune system is attacking them. Over time, the powerful biological and chemical weapons of the immune system do serious damage to the knee, finger, or hip joints of someone with RA. It damages cartilage and bone and even deforms the joints. Does this sound a little bit like periodontal disease? It’s no coincidence. RA and periodontal disease cause similar inflammatory processes and immune system damage to bones and tissues.131, 132
The association between RA and periodontal disease is not as strong as the one between cardiovascular disease and periodontal disease, but there are still a lot of compelling similarities. People with RA have a much higher chance of having periodontal disease. If you have rheumatoid arthritis, you are more likely to have bleeding gums, gingivitis, and deep tooth pockets, which are characteristic of periodontal disease. And when rheumatoid patients are treated for periodontal disease, sometimes their joints feel much better afterward and their systemic markers of inflammation calm down (like hs-CRP, on page 59). This isn’t a new phenomenon. Even Hippocrates saw arthritis improve after pulling a patient’s tooth.133, 134
One of the most definitive red flags is that certain pathogenic oral microbes have been found in the fluid surrounding sick joints of people with RA! The fact that oral bacteria can leave their homes in the mouth and reach the joints and set up shop there seems otherworldly. But if anyone can work magic tricks like that, it would be bacteria. Other oral bacteria found in diseased joints were Prevotella intermedia, P. gingivalis, Fusobacterium nucleatum, and Serratia proteamaculans.135
There are a lot of questions about how this happens and what this means. One interesting theory is that a certain oral bacteria that is high in periodontal disease has the ability to make a special kind of protein that activates rheumatoid arthritis. Citrullinated peptides are a kind of altered protein that seem to trigger inflammatory responses in autoimmune diseases, such as RA. In the vast majority of RA patients (70 percent), their immune system is attacking these citrullinated peptides.136 In fact, citrullinated peptides are such a key factor to the disease that they are used to diagnose it and monitor treatment. It just so happens that P. gingivalis, a common oral pathogen, carries an enzyme that can citrullinate, or alter, proteins, which then provoke an immune attack.137, 138
Almost 2,500 years ago, Hippocrates, the father of medicine, wrote that pulling a person’s tooth could cure arthritis.
Other immune and inflammatory mechanisms, bone destruction processes, and similar genetic underpinnings could also explain the association between RA and periodontal disease. While there is still more to understand about rheumatoid arthritis and oral health, for now it is safe to say that taking care of oral health could help reduce inflammation, keep bad bugs under control, and protect joints from disease. Also, for a person with rheumatoid arthritis, keeping on top of oral health and balancing the oral microbiome could help reduce joint pain and inflammation.
Connecting the Dots
Does your dentist ask about your heart health? Does your primary care doctor ask about your gum health? Or even your gut health, for that matter? These artificial divisions in medicine and dentistry give us the idea that all of our organs work in isolation. On the contrary, they are all connected. Your oral health is a factor in your gut health, and your heart health, and more. My dentist says, “It is not a closed system.” The mouth is a gateway to the body and it shows. Use the letter on page 87 to help your physician and dentist collaborate on your oral-systemic health.
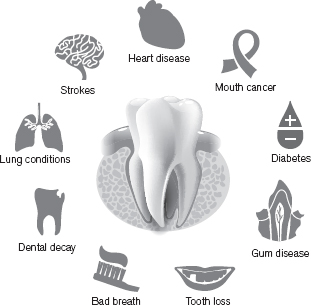
Figure 8.3: Gum disease and oral dysbiosis can manifest as many other conditions in the body.
I want to urge caution with pointing the finger at pathogenic oral bacteria as the cause of heart disease or rheumatoid arthritis. Yes, pathogenic bacteria from the oral cavity were detected in heart disease plaques and in diseased joints. It’s important to know. However, just one bug is not the problem. It is the whole microbial shift in the oral microbiome that allows a pathogen to rise to power. When oral dysbiosis occurs, a whole slew of negative things happen in the microbial communities, at the oral mucosal barrier, and with the immune system. Certain pathogens rising to power and creating havoc (like P. gingivalis) cannot simply be solved with a round of antibiotics. It’s not a one-bug-one-disease model anymore. If you learn anything in this book, please learn that antibiotics are good for serious, isolated infections but not for bigger, chronic problems with the microbiome. Instead, if you have heart disease or rheumatoid arthritis, then you will want to cultivate a healthier oral microbiome that protects you and pushes bad guys out. You want to fortify a stronger oral barrier that keeps bad guys out of the systemic circulation. You want to shift the microbial ecology from one that promotes disease to one that promotes systemic health. Diet, probiotics, dental hygiene, and other treatments can help to grow a healthy garden of good bacteria that protect you from the likes of periodontal pathogens like P. gingivalis. A comprehensive list of oral microbiome solutions can be found in Chapter 9.
Heart Disease Begins in the Mouth
A 62-year-old woman named Linda went to her doctor for her annual check-up. Dr. Ellie Campbell did the usual battery of tests on Linda, including blood sugar, cholesterol, and hs-CRP. Linda said she was feeling fine and didn’t report any major issues with her health. Linda’s lab tests came back and she had high levels of hs-CRP in her blood, which suggested that she had an infection or another source of inflammation in her body. Once Dr. Campbell found out Linda had high hs-CRP, she tested Linda’s oral bacteria with the MyPerioPath test from OralDNALabs (see an example in Chapter 9, Figure 9.1). She wanted to see if Linda’s marker of heart disease might have its origin in the mouth.
Linda’s oral DNA test showed elevations of eight different periodontal pathogens, including T. denticola and P. intermedia. Dr. Campbell started Linda on a protocol to improve her oral health by decreasing the unhealthy microbes in her mouth. Dr. Campbell recommended Linda use a stainless steel tongue scraper before brushing her teeth. She told Linda to add GUM soft picks to her flossing regimen. She also suggested that Linda add two drops of frankincense essential oil to her Waterpik.
When Linda came back for her next annual exam the following year, her hs-CRP had dropped by half. However, it was still elevated. Since her hs-CRP still hinted that there was unchecked inflammation, Dr. Campbell told Linda to continue on her protocol with the tongue scraper, the GUM soft picks, and the frankincense essential oil in the Waterpik. But this time she told Linda to start taking ProbioMax DDS (Xymogen) once per day, at bedtime. ProbioMax DDS is a chewable probiotic that contains the beneficial oral bacterium S. salivarius DSM 14685.
When Linda did her testing in the following year, everything looked much better. Her hs-CRP was much improved and within the normal range. Likewise, her oral microbial DNA looked much better. Her pathogenic bacteria decreased by half. Where there were eight different bacteria present in her first test, her follow-up test showed only four. Linda’s marker of inflammation was much better after treating her oral health and this corresponded with an improvement in her oral microbiome. Linda’s risk of heart disease was reduced by restoring oral microbiome balance.
Dr. Campbell summed it up beautifully: “The moral of this story is that when CRP is high, always check the mouth with an oral bacteria test. Heart disease begins in the mouth! Treat the mouth and you can treat the inflammation. Reduce the inflammation and you reduce the risk for stroke and heart attack.”
The state of your gums seems to reflect on the state of your heart and your joints. But did you know it also can influence your sugar metabolism? Much like heart disease, there is a significant bidirectional association between type 2 diabetes and periodontal disease. Bidirectional means that having diabetes makes you more likely to develop gum disease, and having gum disease makes you more likely to develop diabetes. Here’s another way to look at it: Get your blood sugar under control and your gum disease goes away; boost your oral health and you can better control your blood sugar.139
Again, we don’t have a firm explanation for this uncanny relationship. We know that having diabetes means your risk of having gum disease is three times greater than if you didn’t have diabetes. And treatments for periodontal disease can improve measures of blood sugar, but not always. Since both diabetes and periodontal disease are characterized by excess inflammation, a common gene that alters immune function, the HLA genotype, may explain why both conditions show up together.140
Another theory for the close relationship of these two conditions is that in diabetes, the immune system is damaged from advanced glycation end products (AGEs), which are basically toxic sugar molecules (think of burnt sugar in the bottom of your oven). The damaged sugars cause the immune system to malfunction. Immune cells become hyper aggressive and hostile against bacterial biofilm, launching a violent assault. Remember that periodontal disease is a disease of an overactive immune response against oral dysbiosis. It destroys gums and bone, and can cause teeth to loosen and fall out. AGEs can damage tissues and slow down wound healing, further contributing to periodontal disease.141
The microbiome can affect metabolism, weight, and diabetes. Scientists have noticed patterns of gut microbes in people who are obese or lean. Firmicutes phyla are higher than Bacteroidetes phyla in people who are obese. Lean people have the opposite pattern. When researchers changed the participants’ diets, their Bacteroidetes increased, Firmicutes decreased, and they lost weight. While most of the research is on the gut microbiome, I wouldn’t be surprised if we find out one day that our oral microbes influence our weight and metabolism. We already know they can affect our blood sugar!
It is sometimes unbelievable that something as small and seemingly insignificant as the mouth could have such a huge impact on heart health, joint health, blood sugar control, metabolism, and more. Researchers are hard at work trying to discover how and why the oral microbiome is so pivotal to overall health. For now, we need to shift away from the outdated model of trying to kill off a single oral pathogen with antibiotics.
Instead, balance and repair your oral microbes to improve gut health, reduce inflammation, promote heart health, boost your metabolism, and reduce painful joints. In the next chapter, I will give you practical action steps and resources to get your oral microbiome, and whole body, in tip-top shape.
Takeaways
• Gum disease increases the chances of having heart disease and diabetes.
• Gum disease is common in people with rheumatoid arthritis.
• Excessive inflammation is a common theme in gum disease, heart disease, rheumatoid arthritis, and diabetes.
• Every time you brush, eat, or get a dental cleaning, a surge of bacteria courses through your bloodstream, a phenomenon called bacteremia.
• Oral bacteria can take a ride in the bloodstream and land in far-off sites.
• Forget the outdated model of one-bug-one-disease; cultivate healthy bacterial communities to ward off disease.
• Hs-CRP is a routine blood test that tells you your levels of inflammation; it is used to measure the risk of heart disease.
• If you have any of the conditions listed in this chapter, work on optimizing your oral microbiome and oral health.