20 Factors in Bipolar Disorder
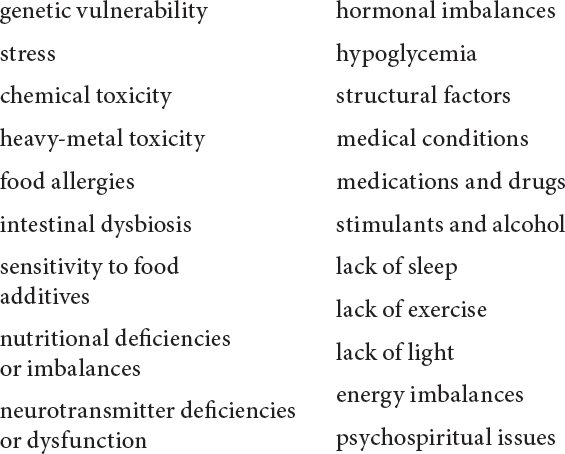
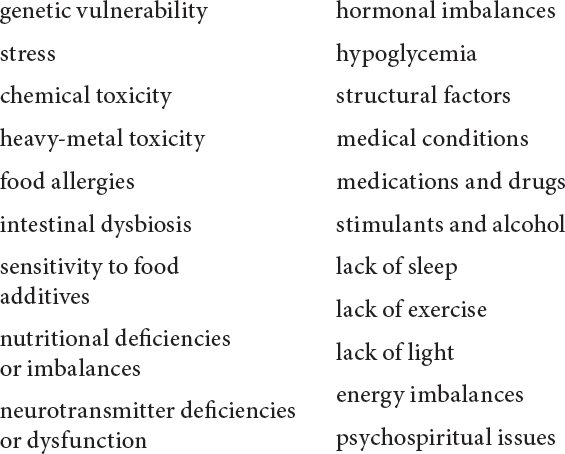
The following can exacerbate or contribute to bipolar disorder:
The cause of bipolar disorder is unknown, beyond a general belief that there is an as yet unidentified genetic component. As with other “mental” illnesses, it appears that environmental factors combine with genetic vulnerability to trigger the disorder. Science does not know what impels the episodic shifts once bipolar disorder has developed, as they often occur independent of obvious influences.
The reality is that, in spite of their widespread acceptance in the medical community, the disease model that resulted in the classification of bipolar disorder and schizophrenia as mental illnesses, the genetic component, and the focus on neurotransmitter dysfunction as the source of the problem are all suspect.
Here is what some eminent psychiatrists and researchers had to say on the subject:
“[T]here is no proven physical cause for any psychiatric disorder … [W]hy are so many … convinced that the origins of mental illnesses are to be found in biology, when, despite more than three decades of research, there is still no proof ? … The absence of any well-defined physical causation is reflected in the absence of any laboratory tests for psychiatric diagnoses—much in contrast to diabetes and many other physical disorders.”
—CHARLES E. DEAN, MD, director of psychiatric residency at the Minneapolis Veterans Medical Center, quoted in the Minnesota newspaper Star Tribune (November 22, 1997)75
“Contrary to what is often claimed, no biochemical, anatomical or functional signs have been found that reliably distinguish the brains of mental patients.”
—ELLIOT VALENSTEIN, PHD, University of Michigan neuroscientist and professor emeritus of psychology, author of Blaming the Brain: The Truth About Drugs and Mental Health76
“[W]e have no identified etiological agents for psychiatric disorders.”
—GARY J. TUCKER, MD, professor and chairman of psychiatry and behavioral sciences at the University of Washington School of Medicine, quoted in the American Journal of Psychiatry (February 1998)77
“Through the 1970s and 1980s, a curious circularity invaded psychiatry, as ‘diseases’ began to be ‘modeled’ on the medications that ‘treat’ them. If a drug elevated serotonin in test tubes, then it was presumptuously argued that patients helped by the medication must have serotonin deficiencies even though we lack scientific proof for the idea.”
—Joseph Glenmullen, MD, clinical instructor in psychiatry at Harvard Medical School and author of Prozac Backlash78
From a holistic viewpoint, a single physiological cause or even one such cause in combination with a genetic abnormality is not the sum total of a condition such as bipolar disorder. Perhaps research has been unable to identify an “etiological agent” because “mental illness” is the outcome of body-mind-spirit disturbance caused by physical, psychological, emotional, spiritual, and energetic influences, each of which affects all of the other areas, so no influence can be considered in isolation.
If we acknowledge that body, mind, and spirit cannot be separated (conventional medicine acknowledges at least the first two; even the surgeon general of the United States has stated that mind and body are “inseparable”79), then we should not look only to one area for the cause and the solution. Even if the source arises in one area, the reverberations, like ripples in a pond, extend throughout the body, mind, and spirit and are soon indistinguishable as cause or effect.
To recover from bipolar disorder, we need not know the exact mechanism in operation, but we do need to address the factors that combine to produce the disorder. This means identifying and treating the imbalances in each individual case of bipolar disorder; the approach must be individualized because the combination of factors differs and the specifics of each factor vary from person to person.
With that in mind, this chapter looks at 20 factors that can play a role in bipolar disorder. While a particular factor may seem to be predominantly physical, psychological, or spiritual in nature, remember the ripple-in-the-pond effect and know that it will have an effect on the other areas as well.
“No claim of a gene for a psychiatric condition has stood the test of time, in spite of popular misinformation,” states Joseph Glenmullen, MD, in Prozac Backlash.80 This statement is made more significant when you consider the amount of research hours, energy, and money that has gone into looking for the genes.
The statistics for occurrence of mood disorders within families (see chapter 1) seem to support the existence of a genetic component. The fact that only 65 percent of the identical twins of a twin with bipolar disorder develop the disorder,81 however, suggests that environmental factors play a role as well. This is what is meant by “genetic vulnerability”; a genetic abnormality sets the stage for environmental factors to trigger the disorder. Environmental in this usage simply means not genetic, so toxins, traumatic events, and nutritional deficiencies from a poor diet, for example, all fall in the environmental category.
Some kind of vulnerability is clearly operational in bipolar disorder, given the family statistics and the fact that not everyone develops the condition. The way this vulnerability is viewed depends on one's medical orientation. While conventional researchers and physicians focus exclusively on gene abnormality passed down through families as the source of the vulnerability in some people, those who understand the electromagnetic field of the human body and how energy functions in health and disease might consider the contribution of an inherited energy imbalance or an energy legacy passed down from generation to generation (see “Energy Imbalances” in this chapter).
Some scientists believe that a phenomenon called “gene penetrance” may now be operational in bipolar disorder. Gene penetrance refers to the increasing development of a genetic disorder the further along the generational chain it has been passed. In other words, descendants may be more likely than their forebears to develop bipolar disorder.82 This phenomenon could also be viewed in energetic terms, with the energetic influence becoming more powerful the more times it is passed down, much in the way that a homeopathic remedy, which is an energy-based medicine, becomes more potent the more times it is diluted (see chapter 9).
Regardless of what genetic research discovers or how you view the inherited vulnerability, that predisposition does not translate as “hopeless or incurable,” as biochemical researcher William J. Walsh, PhD, says in chapter 5. By considering the nineteen other factors cited here and addressing those that you think or discover have relevance to your condition, you open the way for the restoration of your health.
The subject of stress is a natural follow-up to genetic vulnerability because stress is one of the major environmental influences in bipolar disorder. In fact, the rest of the factors cited in this chapter could be called stressors, in that they put stress on the system and thus add to a person's total stress load.
Chronic stress wreaks havoc on the body, mind, and spirit and creates a vicious circle. On the physical level, stress drains nutrients and lowers immunity. The nutritional deficiencies result in compromised neurochemistry in the brain, which in turn reduces the body's ability to cope with stress. Lowered immunity also reduces the stress-coping capacity and opens the body to the development of disease. In addition, it creates disturbances in the energy system of the body, which affects all levels of functioning.
Chronic stress also impairs the body's natural homeostatic ability, that is, the ability to maintain its internal balance. Someone who is born vulnerable to developing bipolar disorder already has “a diminished ability to adapt smoothly to the changing planetary environment—or to accommodate to the turmoil of chronic stress—and recover homeostatic balance once the challenges have passed,” says Peter C. Whybrow, MD, author of A Mood Apart: The Thinker's Guide to Emotion and Its Disorders.83 This means that the genetic or energetic vulnerability leaves a person less able to deal with stress.
Episodes of both depression and mania in the early course of bipolar disorder are often connected to stressful life events. As the disorder progresses, however, episodes often occur independent of life occurrences. This is known as the “kindling phenomenon,” which refers to increased vulnerability to the recurrence of mood episodes, with less stress required to trigger an episode each time, until the episodes arise independent of stress and recur more and more often. Dr. Francis Mondimore calls this the point at which “the illness has become sufficiently ‘kindled’ that stress management no longer has much of an impact … ”84
This is a strong argument for reducing the amount of stress in your life, whether through avoidance of known stressful situations, making changes in your circumstances or lifestyle, and/or practicing meditation and relaxation techniques. Attending to the rest of the factors in this chapter can significantly reduce your stress load.
Toxic overload places tremendous stress on the body and contributes to the development of disease. Humans today are exposed to an unprecedented number of chemicals. Testing of anyone on Earth, no matter how remote the area in which they live, will reveal that they are carrying at least 250 chemical contaminants in their body fat.85 The onslaught of chemicals begins in the womb, with the transmission of toxins from the toxic mother to the fetus, and continues during breast-feeding. An infant in the United States or Europe imbibes “the maximum recommended lifetime dose of dioxin” in only six months of nursing. Dioxin, a pesticide by-product, is one of the most toxic substances on Earth.86 The point is that we start life with an already accumulating toxic load.
In their report In Harm's Way—Toxic Threats to Child Development, the Greater Boston Physicians for Social Responsibility summarize research on lead, mercury, cadmium, manganese, nicotine, pesticides (many of which are commonly used in homes and schools), solvents (used in paint, glue, and cleaning products), and dioxin and PCBs (polychlorinated biphenyls; both PCBs and dioxin stay in the food chain once they enter it, as they pervasively have).
The report notes that in one year alone (1997), industrial plants released more than a billion pounds of these chemicals directly into the environment (air, water, and land). Further, almost 75 percent of the top 20 chemicals (those released in the largest quantities) are known or suspected to be neurotoxicants.87 (Neurotoxicants are substances that are toxic to the brain and the nervous system in general.) Other sources report that of 70,000 different chemicals being used commercially, only 10 percent have been tested for their effect on the nervous system.88 In addition to the pesticides used directly on crops, the chemicals in the air, water, and soil are fully integrated into our food supply.
The neurotoxic effects of the chemical onslaught emerge as mood disorders, in addition to many other symptoms and diseases. “In the earliest form of chronic toxicity, mild mood disorders predominate as the patient's chief complaint,” states an official at the National Institute for Occupational Safety and Health.89
“Everyday chemicals have the potential to interfere with the metabolism of brain neurotransmitters or happy hormones in a myriad of pathways,” says Sherry A. Rogers, MD, author of Depression—Cured at Last! “They interfere with synthesis and metabolism, they block receptor sites, poison enzymes, and much more.”90
As just one example of how this works, consider the hydrazines, a family of widely used chemicals, notably in pesticides, jet fuels, and growth retardants. Hydrazine is sprayed on potatoes to prolong their shelf life. In the body, this chemical blocks serotonin production by blocking the action of vitamin B6, which is needed at every step in the series of enzyme actions required in the manufacture of serotonin. In just one bag of potato chips or one serving of fast-food French fries, there is sufficient hydrazine to knock out all the B6 in your body.91
While we can't avoid toxic exposure entirely, given the state of our planet, avoiding the use of toxic cleaning and other home and garden products, eating organically grown food, drinking pure bottled or filtered water, and avoiding other sources of toxic exposure wherever possible can at least reduce our toxic loads.
As with chemicals, heavy metals contribute to the toxic burden our bodies are being forced to carry. In addition, heavy metals such as mercury, copper, lead, and aluminum have been linked to mood disorders. “Historians have theorized that one of the reasons the Roman empire declined was as a result of contamination from lead pipes,” says author Catherine Carrigan. “A hundred years from now, future historians may reckon that one of the reasons depression increased so rapidly in our society was as a result of widespread exposure to toxic metals.”92
The heavy metal mercury is well recognized as a neurotoxin and has been for centuries. Early hatmakers contracted what was known as “mad hatter's disease,” the result of poisoning from the mercury used in hatmaking, hence the saying, “mad as a hatter.” Physiologically, mercury's effects on the brain arise from its ability to bond firmly with structures in the nervous system, explains Dr. Dietrich Klinghardt, whose work is featured in chapter 3.
Research shows that mercury is taken up in the peripheral nervous system by all nerve endings (in the tongue, lungs, intestines, and connective tissue, for example) and then transported quickly via nerves to the spinal cord and brain stem. “Once mercury has traveled up the axon, the nerve cell is impaired in its ability to detoxify itself and in its ability to nurture itself,” says Dr. Klinghardt. “The cell becomes toxic and dies—or lives in a state of chronic malnutrition…. A multitude of illnesses, usually associated with neurological symptoms, result.”93
Mercury is bioaccumulative, which means that it doesn't break down in the environment or in the body. The result is that it is everywhere in our environment, in our food, air, and water, and each exposure adds to our internal accumulation. Many of us also carry a source of mercury in our mouths in the form of dental fillings; so-called silver fillings are actually composed of more than 50 percent mercury. These fillings leach mercury, predominantly in the form of vapor, 80 percent of which is absorbed through the lungs into the bloodstream. Chewing raises the level of vapor emission, and it remains elevated for at least 90 minutes afterward.94
Among the symptoms that improve after having mercury amalgam fillings replaced with nontoxic composite fillings are depression, anxiety, fatigue, lack of energy, nervousness, irritability, insomnia, headaches, memory loss, lack of concentration, allergies, gastrointestinal upset, and thyroid problems. In a survey of 762 people conducted by the Foundation for Toxic Free Dentistry of Orlando, Florida, 23.75 percent (181) of the subjects reported that they had suffered from depression prior to having their mercury fillings replaced, and 100 percent of them reported that the depression disappeared afterward.95
Copper is also found in dental fillings, often added as an alloy to gold fillings. Other sources of copper exposure are cigarettes, cookware, and water pipes. Lead exposure is often an occupational hazard; approximately one million Americans are exposed to lead on the job.96 Other sources of exposure include certain glazed ceramics, old paint, water pipes, fertilizers, and soft vinyl products. In 1996, cheap vinyl miniblinds were recalled due to a high lead content. Other products with even higher lead contents are still on the market. For example, one manufacturer's rainsuit for children tested at 2 percent lead, which is almost one hundred times the amount allowed in miniblinds.97
In addition to a potential role in depression, aluminum toxicity has been linked to Alzheimer's, gastrointestinal problems, and liver dysfunction.98 Among the common sources of aluminum exposure are cookware, aluminum salts in baking powder, aluminum-containing antacids, and many antiperspirants and deodorants.
Avoiding sources of these heavy metals both reduces your overall toxic load and removes a potential source of exacerbation of your symptoms.
Depression, fatigue, and headaches are the most common symptoms of food allergies in adults. Mood symptoms run the gamut from mild anxiety to serious depression.99 Many people are not aware that they are suffering from food allergies, as the symptoms are often not clearly linked with ingestion of the food, as is the case when someone breaks out in a rash after eating strawberries or experiences a dangerous constriction of air passages after eating shellfish.
A discussion of allergies involves both what happens in the body on a physical level as well as the imbalance in the energy field that an allergy entails. The latter is why NAET (Nambudripad's Allergy Elimination Techniques; see chapter 8), which employs acupuncture among other techniques to restore the body's energy flow in relation to the allergen (substance to which one is sensitive or allergic), is effective in eliminating allergies. Disturbances in the flow of energy by themselves produce a range of symptoms, including mood changes.
Seeming allergies may actually be intolerances or sensitivities resulting from compromised immune and digestive systems or energy disturbances. Once these factors are eliminated or eased, the food intolerances may disappear.
Food intolerances occur when the body doesn't digest food adequately, which results in large undigested protein molecules entering the intestines from the stomach. When poor digestion is chronic, these large molecules push through the lining of the intestines, creating the condition known as leaky gut, and enter the bloodstream. There, these substances are out of context, not recognized as food molecules, and so are regarded as foreign invaders.
The immune system sends an antibody (also called an immunoglobulin) to bind with the foreign protein (antigen), a process which produces the chemicals of allergic response. The antigen-antibody combination is known as a circulating immune complex, or CIC. Normally, a CIC is destroyed or removed from the body, but under conditions of weakened immunity, CICs tend to accumulate in the blood, putting the body on allergic alert, if you will. Thereafter, whenever the person eats the food in question, an allergic reaction follows.
It is important to consider here the concept of “brain allergies.” Until recently, allergies were thought to affect only the mucous membranes, the respiratory tract, and the skin. A growing body of evidence indicates that an allergy can have profound effects on the brain and, as a result, on behavior. An allergy or intolerance that affects the brain is known as a brain allergy or a cerebral allergy.
Gluten (a protein found in wheat and other grains) intolerance is especially indicated in bipolar disorder. See chapter 6 for a full discussion of this.
The intestinal dysfunction inherent in food allergies contributes to mood states, as discussed in the following section.
Intestinal dysbiosis is an imbalance of the flora that normally inhabit the intestines. Among these flora are the beneficial bacteria (known as probiotics) Lactobacillus acidophilus and Bifidobacterium bifidum, potentially harmful bacteria such as E. coli and Clostridium, and the fungus Candida albicans. When the balance among these flora is disturbed, the microorganisms held in check by the beneficial bacteria proliferate and release toxins that compromise intestinal function. This has far-reaching effects in the body and on the mind.
Research has revealed that what passes through the lining of the intestines (see “Food Allergies”) can make its way through the blood-stream to the brain.100 As an example of just one of the results of this relationship, in the brain certain intestinal bacteria can interfere with neurotransmitter function.101 Depression and fatigue are two of the many health problems that can result from intestinal dysbiosis.
Dysbiosis contributes to a buildup of toxins in the body in two ways. One, the harmful bacteria's normal metabolism processes release toxic by-products. Two, a compromised intestinal system cannot adequately filter toxins, which is one of the important functions of the intestinal lining. Normally, bile from the liver goes through the intestines, where toxins are filtered out, and the cleansed bile is then recirculated. When the intestines are not working correctly, bile is returned to the body with the old toxicity. This condition is known as enterohepatic toxicity (entero for intestines and hepatic for liver).
Depression, fatigue, and headaches, among numerous other symptoms, can result from an intestinal overgrowth of Candida albicans, the yeast-like fungus normally found in the body. Mercury is often implicated in this overgrowth because “the purpose of Candida in the human being is to protect the body from mercury by absorbing it,” says Thomas M. Rau, MD, director of the Paracelsus Klinik in Lustmühle, Switzerland. The mechanism was never intended, however, to deal with large amounts of mercury. Nevertheless, when mercury levels in the body are high, the population of Candida multiplies in a vain attempt to deal with the heavy-metal load.
Through its normal metabolic processes, Candida releases substances that are toxic to the brain and interfere with neurotransmitter activity.102 Another mechanism by which Candida overgrowth has an impact on mood is that the intestinal lining becomes inflamed, which interferes with the absorption of nutrients.103 As discussed later, nutritional deficiencies are implicated in bipolar disorder.
Candida overgrowth occurs when something intervenes to disturb the normal balance of flora in the intestinal environment. The main culprit is antibiotics, particularly the repeated use of antibiotics, which kill all the beneficial bacteria that keep potentially harmful flora such as Candida in check. Weakened immunity may also be a factor in yeast overgrowth.
Eliminating foods that “feed” Candida is a common treatment approach to restoring intestinal balance. The so-called Candida diet emphasizes avoiding all forms and sources of sugar, including fruit and fruit juice, carbohydrates, and fermented yeast products. According to Dr. Rau, however, the relationship between mercury and Candida means that until you detoxify the body of the mercury, you won't be able to get rid of the Candida overgrowth on any lasting basis, no matter how perfect your diet or what antifungal drug or natural substance you take. The fungus will just keep coming back.104
In addition to antibiotics, anti-inflammatory drugs, food allergies, and a poor diet can all help create intestinal dysbiosis.
Food additives can produce a range of effects, from depression, insomnia, nervousness, and hyperactivity to dizziness, blurred vision, and migraines. Research has established that aspartame (an artificial sweetener), aspartic acid (an amino acid in aspartame), glutamic acid (found in flavor enhancers and salt substitutes), and the artificial flavoring MSG (monosodium glutamate) are neurotoxins.105 Aspartame and MSG are particularly implicated in depression. Depression is one of the frequent aspartame-associated complaints the FDA receives.106 Aspartame alters amino acid ratios and blocks serotonin production.107 MSG has been shown to affect serotonin levels.108
The more than 3,000 additives used in commercially prepared food have not been tested by their manufacturers for their effects on the nervous system or on behavior.109 In addition to those mentioned, common food additives are artificial flavoring, artificial preservatives (BHA, BHT, and TBHQ are in this category), artificial coloring/food dyes, thickeners, moisteners, and artificial sweeteners.
Sensitivity to food additives varies; a high sensitivity may reflect an already large toxic load or weakened immunity. Noticing if your symptoms worsen after you ingest certain foods can start the process of elimination for determining which additives, if any, are problematic for you.
Nutritional deficiencies and imbalances are a common feature in bipolar disorder and other “mental” illnesses. Correcting these often produces dramatic improvement. Unfortunately, nutrient status testing and intervention are not standard practice in conventional psychiatric medicine.
“Nutrient-related disorders are always treatable and deficiencies are usually curable. To ignore their existence is tantamount to malpractice,” states Richard A. Kunin, MD,110 a practitioner of orthomolecular medicine (the supplemental use of substances that occur naturally in the body, such as vitamins, minerals, amino acids, and enzymes, to maintain health and treat disease).
Nutrient deficiencies most implicated in bipolar disorder are essential fatty acids, amino acids, the B vitamins, magnesium, and zinc.
Again, no two people with bipolar disorder will have the exact same nutritional condition. Blood chemistry analysis can determine the precise status of your nutrient levels. With this information, therapeutic intervention can then be tailored to your specific nutrient needs. Random supplementation may not address those needs and may even contribute to further skewing of nutrient ratios.
While other factors such as absorption problems or even a genetic disorder may be involved in nutritional deficiencies and imbalances, poor diet is a primary cause. Any factor that contributes to your vulnerability should be avoided if you suffer from bipolar disorder. Erratic eating habits or a nutrient-depleted diet, as in junk-food, fast-food, processed-food diets, definitely fall into the category of contributing to vulnerability. Without the proper nutrients to feed your brain and nervous system, you are more likely to cycle in and out of depression and mania.
Research has discovered a link between lipids and mental disorders. Lipids are fats or oils, which are comprised of fatty acids. Examples of saturated fatty acids are animal fats and other fats, such as coconut oil, that are solid at room temperature. Examples of unsaturated fatty acids, which remain liquid at room temperature, are certain plant and fish oils. Essential fatty acids (EFAs) are unsaturated fats required for many metabolic actions in the body.
There are two main types of EFAs: omega-3 and omega-6. The primary omega-3 EFAs are ALA (alpha-linolenic acid), DHA (docosahexaenoic acid), and EPA (eicosapentaenoic acid). ALA is found in flaxseed and canola oils, pumpkins, walnuts, and soybeans, while DHA and EPA are found in the oils of cold-water fish such as salmon, cod, and mackerel.
Two important types of omega-6 EFAs are GLA (gamma-linolenic acid) and linoleic acid or cis-linoleic acid. Evening primrose, black currant, and borage oils are sources of GLA, while linoleic acid is found in most plants and vegetable oils, notably safflower, corn, peanut, and sesame oils. The body converts omega-3 and omega-6 EFAs into prostaglandins, which are hormone-like substances involved in many metabolic functions, including inflammatory processes.
The ratio of omega-3 to omega 6-EFAs is skewed in the standard American diet, which is deficient in omega 3s. High consumption of hydrogenated oils and beef contributes to the skewed ratio. Hydrogenated oils (which are oils processed to extend shelf life) are detrimental in two ways: not only does refining oil reduce its omega-3 content, but hydrogenated oils also take up the fatty acid receptor sites and interfere with normal fatty acid metabolism. Hydrogenated oils, also known as trans-fatty acids, are found in margarine, commercial baked goods, crackers, cookies, and other products. The problem with conventionally raised beef cattle is that they are grain-fed rather than grass-fed; grain is high in omega 6 and low in omega 3, while grass provides a more balanced ratio.111
Andrew Stoll, MD, a psychopharmacology researcher and an assistant professor of psychiatry at Harvard Medical School, states: “Omega-3 fatty acids … are essential nutrients for human brain development and general health. Over the past 50 to 100 years, there has been an accelerated deficiency of omega-3 fatty acids in most Western countries. There is emerging evidence that this progressive omega-3 deficiency is responsible, at least in part, for the rise in the incidence of heart disease, asthma, bipolar disorder, major depression, and perhaps autism.”112 (Note that in certain cases of bipolar disorder, those involving a condition called pyroluria, the EFA that is deficient is omega-6; see chapter 5.)
Lipids are necessary for the health of the blood vessels that feed the brain and comprise 50 to 60 percent of the brain's solid matter.113 More specifically, nerve cells in the brain contain high levels of omega-3 fatty acids.114 A deficiency could obviously have serious consequences. There is a large body of research demonstrating links between essential fatty acids and bipolar disorder, depression, and other mental disorders. The following is just a sampling of the extensive research findings:
 For more about essential fatty acid supplementation in the treatment of bipolar disorder, see chapters 3, 4, 5, and 6.
For more about essential fatty acid supplementation in the treatment of bipolar disorder, see chapters 3, 4, 5, and 6.
The production of neurotransmitters that regulate mood requires the presence of certain amino acids or precursors. Tryptophan is the amino acid precursor for serotonin; phenylalanine and tyrosine are the precursors for dopamine and norepinephrine. (GABA is an amino acid that also acts as a neurotransmitter.)
Amino acids are the basic building blocks for neurotransmitters, enzymes, hormones, and other proteins. The body does not manufacture most of the amino acids it requires, so they must be obtained through protein in the diet. With a deficient diet, the body is not able to produce sufficient neurotransmitters, which can contribute to bipolar disorder and depression, among other conditions.
Amino acid supplementation can be effective in alleviating bipolar disorder and serves as a safe and far less expensive alternative to prescription drugs that target the neurotransmitters. Although it may not address the root cause of amino acid deficiency, such as a poor diet, it corrects the problem, unlike antidepressants and other drugs. It also increases the supply of neurotransmitters naturally, by simply supplying the body with the building materials it needs, instead of forcing the brain and the neurotransmitters into unnatural function to keep the neurotransmitters available.
Research has found tryptophan may be beneficial in the treatment of mania, depression, anxiety, panic disorder, sleep disorders, and psychosis.121 One study of the effects of tryptophan supplementation was conducted with 11 patients whose depression was so severe that they were hospitalized. After just a month of supplementation, standard psychiatric tests revealed that the overall depressive states of the 11 patients had dropped by 38 percent. In seven of the 11, guilt, anxiety, weight loss, and insomnia were significantly reduced.122
In the body, tryptophan is converted into 5-HTP (5-hydroxy tryptophan) and then into serotonin. A plant extract form of 5-HTP, available as a supplement, can also be used to boost serotonin levels. A Swiss study found that the antidepressant effects of 5-HTP were equal to those of the conventional SSRI Luvox (fluvoxamine), with fewer of the subjects in the 5-HTP group experiencing side effects. (High dosages of 5-HTP may produce nausea, other gastrointestinal distress, and drowsiness.)
Research on phenylalanine and tyrosine indicates that they can also be beneficial in the treatment of depression.123
GABA has proven useful in the treatment of mania, acute agitation, anxiety, nervous tension, hyperactivity, insomnia, and other brain and nervous disorders. One of the signs of GABA deficiency is excessive mental activity, as is characteristic in a manic episode.124
For a full discussion of amino acids and their use in bipolar disorder, see chapter 6.
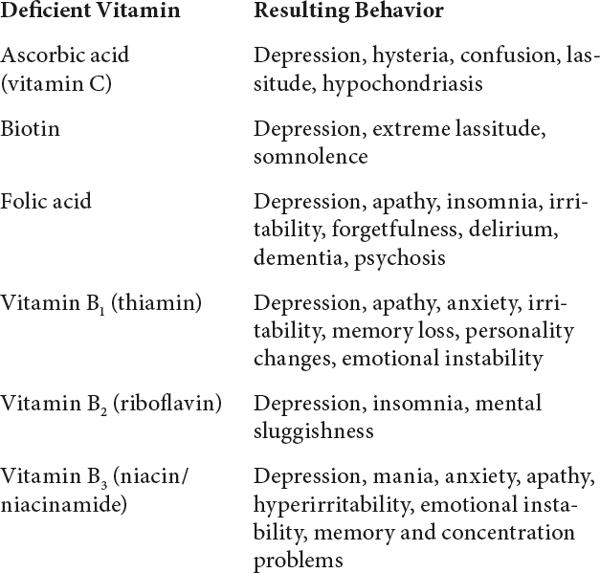
As you can see from the list of effects from vitamin deficiency in the accompanying sidebar, the whole vitamin B family is essential for mental health. As with amino acids, B vitamins are found in protein foods. Someone with an amino acid deficiency is often deficient in B vitamins as well. Based on the clinical experience of the practitioners in this book, the most common vitamin deficiencies associated with bipolar disorder are vitamin B3 (niacin/niacinamide), vitamin B6 (pyridoxine), B12 (cobalamin), and folic acid (a member of the vitamin B family), all of which are vital to neurotransmitter function. Biochemical researcher William Walsh, PhD, has found that a genetic disorder, which causes severe deficiency in both vitamin B6 and zinc, can be a factor in bipolar disorder (see chapter 5).
Inositol (another member of the B complex family), phosphatidyl choline (found in lecithin), and magnesium are important for nervous system balance as well. Phosphatidyl choline exerts benefits for mania, while inositol does the same for depressive episodes.125 Magnesium, which functions in ratio to calcium, may be of use in bipolar disorder for the same reason that calcium channel blockers are sometimes prescribed, for the calming effect that results from blocking calcium channels in cells.126 Supplementation with magnesium can help restore the proper ratio and action of the two minerals. In addition, magnesium enhances vitamin B6 activity and, taken as a supplement, helps prevent the magnesium deficiency that can result from high doses of B6.
Poor diet and malabsorption due to gastrointestinal dysfunction are common causes of nutritional deficiencies. The depleted mineral content of the soil in which crops are grown, which translates into food with a lower mineral content than our forebears enjoyed, is a factor as well. Finally, many lifestyle practices and attributes of modern life deplete us of vitamins and minerals, regardless of how well we eat: stress, smoking, alcohol, caffeine, pollution, heavy metals such as the mercury in our dental fillings.
Given these factors, the recommended daily allowance (RDA: purportedly, the amount of an individual vitamin or mineral our body requires daily, whether from food or supplements) is likely far below our nutritive needs, in most cases. The RDA standard is based on a group norm for preventing nutritional deficiencies. There are two problems with that. One, individual needs diverge widely, and two, the level of deficiency the RDAs are designed to avoid is severe. The systems of the body can begin to be compromised long before that degree of deficiency registers. In other words, if you use the RDAs as your guideline, you could be walking around with moderate nutritional deficiencies.
Increasing your intake of foods that contain the nutrients cited above is a good idea if you are deficient. The following are dietary sources of these nutrients:
The role of the neurotransmitters serotonin, dopamine, norepinephrine, and GABA in bipolar disorder is covered in chapter 1. While the theory that problems with these brain chemicals is behind bipolar disorder has not been proven, the clinical results of supporting neurotransmitters with their amino acid precursors and other nutrients indicates involvement, if not causality.
The problem with the neurotransmitters can be one of supply, function, or both. A normal level of a given neurotransmitter does not guarantee that the mind and body will receive its benefits. For example, despite high blood levels of the neurotransmitter serotonin, reduced uptake in the brain may mean that the availability of this vital nerve messenger is actually limited.128
Attempting to correct neurotransmitter supply or even function does not address the root problem of why the supply is low or the neurotransmitters are not working properly. As you will learn in part II of this book, treating the root problems, which range from the physical to the spiritual, often results in the neurotransmitter deficiency or dysfunction self-correcting as the body is restored to its innate ability to heal itself.
Hormones “are probably second only to the chemicals of the brain in shaping how we feel and behave.”129 Hormonal imbalances influence brain chemistry and the nervous system.130 “Neurons are very sensitive to rapid changes in their hormonal environment,” states Dr. Whybrow. “Any rapid change in these hormone levels … demands immediate accommodation, and while adaptation is proceeding, mood is commonly unstable.”131 The hormones particularly implicated in mood are thyroid hormones, adrenal hormones (cortisol, DHEA, epinephrine, and norepinephrine), and reproductive hormones (estrogen, progesterone, and testosterone).132
The symptoms of thyroid and adrenal gland diseases are similar to those of depressive and manic episodes.133 Hypo- and hyperthyroidism (an underactive and overactive thyroid, respectively) are two thyroid conditions that can masquerade as bipolar disorder. Hypothyroidism is often overlooked as a cause of mood symptoms because it can be at a subclinical level and still produce such symptoms. If the thyroid condition continues undiagnosed, a vicious cycle can be created because taking lithium can contribute to hypothyroidism.134
Of the adrenal hormones, too little DHEA (dehydroepiandrosterone) or too high levels of the stress hormone cortisol have been linked with depression.135 As discussed in the previous chapter, epinephrine, or adrenaline, is involved in the stress response and anxiety, while norepinephrine, the form of adrenaline found in the brain, is one of the “feel good” neurotransmitters and as such has influence in affective disorders. Chronic stress, which involves continual release of the adrenal stress hormones, compromises the body's adaptive capacity, leaving a person with bipolar disorder more vulnerable to mood swings. Even a small stressor can then trigger a manic or depressive episode.
In women, too little of the hormone estrogen in relation to the other reproductive hormones tends to produce depression, while too much estrogen in relation to other hormones tends to result in anxiety.136 Too little progesterone can also lead to depression; this is often the underlying problem in both premenstrual and postpartum depression.137 Testosterone deficiency in both men and women (yes, women have testosterone) can result in depression as well.138
Postpartum mania due to the hormonal changes following childbirth can occur in women who do not have bipolar disorder, but women who do have it, or who have a family history of it, are twenty to thirty times more likely to have a manic episode triggered by childbirth.139
Toxic exposure, stress, diet, and exercise can all affect hormonal levels and balance.
Hypoglycemia is a condition in which the glucose level in the blood is low, and is otherwise known as low blood sugar. The symptoms are restlessness, irritability, fatigue, and, when severe, mental disturbances.
Psychiatrist and orthomolecular physician Michael Lesser, MD, among others, observed in clinical practice that patients with bipolar disorder also have “widely swinging blood sugar curves.” In charting a patient's moods in relation to blood sugar levels, Dr. Lesser discovered that the patient's depressions corresponded to times of low blood sugar. “Lithium, the mineral which ‘curbs’ the wide oscillations in mood characteristic of manic-depressive illness, also levels out the oscillations in blood sugar levels of manic-depressives,” he says. “Perhaps this is one of the reasons it works.”140
Of hypoglycemia in mood disorders, Dr. Walsh (see chapter 5) says, “This problem doesn't appear to be the cause … but instead is an aggravating factor which can trigger striking symptoms.”141
Structural factors such as cranial compression can be a component in bipolar disorder. Such compression, which is the result of skull distortion, can occur through birth trauma or a later physical trauma, such as a car accident. The impact of cranial compression has far-reaching effects throughout the body, but in the head the compression exerts pressure on the brain and cranial nerves, which compromises neurotransmitter function and brain function in general. This factor is explored in depth in chapter 7.
According to the DSM-IV, the following medical conditions can produce mood symptoms that can be mistaken for bipolar disorder: Parkinson's disease; Huntington's disease; cerebrovascular disease, including stroke; hyper- and hypothyroidism (see “Hormonal Problems”); lupus; viral infections, including HIV, hepatitis, and mononucleosis; and pancreatic cancer. The DSM-IV also cites vitamin B12 deficiency as a medical condition that can cause mood disorder.142
Researchers have long been exploring a possible connection between viruses and bipolar disorder. While a viral cause has not been identified, prenatal viral infections may be implicated, as there is evidence that people who suffer from bipolar disorder are more often born during winter months.143
“Probably all antidepressants and stimulants are capable of causing mania,” state Drs. Breggin and Cohen. In one study of children with bipolar disorder, 65 percent had hypomanic, manic, and aggressive reactions to stimulant medications such as Ritalin, often prescribed for ADD/ADHD. The aggression was toward others and self. The parents of one child reported that he became “suicidal and tried to get run over by a car.” In the same study, 80 percent had manic, hypomanic, violent, and suicidal reactions to antidepressants. Regarding the latter, some children seemed to function well at first, but there was a gradual deterioration in the weeks and, in some cases, the months after the child began taking the drug.144
Tomie Burke, founder of Parents of Bipolar Children, and Martha Hellander, executive director of the Child and Adolescent Bipolar Foundation, said in the Journal of the American Academy of Child and Adolescent Psychiatry, “First hospitalizations occurred often among our children during manic or mixed states (including suicidal gestures and attempts) triggered or exacerbated by treatment with stimulants, tricyclics, or selective serotonin reuptake inhibitors.”145
Along with those two categories of drugs, the DSM-IV cites the following as sources of drug-induced mood symptoms: analgesics (pain relievers), anesthetics, anticonvulsants, antihypertensives (for high blood pressure), antipsychotics, antiulcer medications, benzodiazepines (tranquilizers), heart medications, oral contraceptives, muscle relaxants, and steroids, among others.146 Other medications that can cause depression are antihistamines, anti-inflammatories, drugs that lower cholesterol, and quinolone antibiotics (Cipro and Floxin).147
A bipolar episode can also be triggered when a person stops taking a psychiatric medication. Lithium, major tranquilizers, and antidepressants can all produce this effect. A shorter time to recurrence of an episode is also associated with abruptly reducing the dosage of these drugs.148 Research also indicates that, at least for some people, the very drugs they take to treat their psychiatric condition can in reality worsen the progression of that condition, making it necessary for them to stay on the drugs after more than three years of use.
Patty Duke believes that anesthesia and cortisone (a steroid) were responsible for triggering two of her episodes. The first manic episode she can recall came when she was 18 and had emergency surgery for a ruptured appendix and an ovarian cyst. “[A]fter I came home from the hospital, I literally went crazy. I was hallucinating and raving and ranting and not sleeping and not eating and spending a lot of money …. I recovered from this manic episode, which I'm convinced was brought on by the anesthesia I had during the surgery.” Many years later, another episode (with this one, she was at last diagnosed with manic-depression) followed a cortisone shot. Duke was seeing a psychiatrist at the time. “He told me that he had suspected for a long time that I might have this condition,” she recalls, “and he believed that it was the shot of cortisone that had triggered this episode.”149
Caffeine, cocaine, and amphetamines are well known as substances to avoid (or in the case of caffeine, limit) if you have bipolar disorder. Research has found that the level of caffeine ingested is positively correlated with the degree of mental illness among psychiatric patients,150 meaning that the more caffeine taken in, the worse the symptoms. People who drink a lot of coffee test higher for anxiety and depression and are also more likely than their more abstemious counterparts to develop psychotic disorders.151 Some people give up or cut down on coffee and black tea, but forget about the high caffeine content in colas. It is not unusual to hear people with bipolar disorder say that they were living on cigarettes and Pepsi or Coke before a manic episode started.
Caffeine does a lot more than give you a jittery edge. It actually affects your neurotransmitters, stimulating the release of norepinephrine and others. Habitual excessive intake can leave you with a neurotransmitter deficit, along with hypoglycemia and nutritional deficiencies, as it interferes with the absorption of important nutrients such as B vitamins, magnesium, calcium, potassium, and zinc.152 Note the overlap with nutritional deficiencies often present in bipolar disorder.
Obviously, for someone prone to mania, taking stimulants is a risky choice. The DSM-IV cites both use of, and withdrawal from, cocaine and amphetamines as able to produce mood disorders. Dr. Whybrow notes that “in individuals of bipolar temperament, cocaine commonly will precipitate a sustained manic episode … ”153
Alcohol also interferes with normal neurotransmitter function, by impeding the supply of tryptophan to the brain and thus reducing serotonin formation. This can cause depression and insomnia. As with caffeine, habitual drinking of alcoholic beverages is associated with hypoglycemia and nutritional deficiencies, notably of B vitamins, vitamin C, folic acid, zinc, potassium, and magnesium.154
There is a strong connection between sleep deprivation and the onset of a manic episode. even one night without sleep can be problematic for those who suffer from bipolar disorder. Long-distance jet travel, pulling an “all-nighter” in cramming for exams, and medical or family emergencies that result in sleep deprivation have all been associated with manic onset.155
“For me [sleep] is the bellwether of changing mood. When my sleep shortens I know I'm getting high, and if I'm fatigued it's a sure sign that a depression is approaching.”156
—STEPHAN SZABO
Sleep deprivation can trigger a depressive episode as well, or cause a switch from one pole to the other. A National Institute of Mental Health study found that following just one night without sleep, a group of people with rapid-cycling bipolar disorder who were in a depressive episode experienced a switch into mania or hypomania the very next day.157
Exercise stimulates the release of mood-regulating epinephrine, norepinephrine, and serotonin, along with endorphins, chemicals that lift our mood and reduce our stress level. Exercise can alleviate depression, anxiety, hyperactivity, irritability, insomnia, and schizophrenic symptoms.158 A German study of people with major depression found that exercise (thirty minutes of walking daily) reduced their depression in less than the time it typically takes antidepressants to work. Another study of depression in older adults found that exercise was more effective than antidepressants in alleviating the mood disorder.159 Research has also demonstrated that jogging for half an hour three times weekly can be equally or more beneficial for mental health than psychotherapy.160
Exercise increases oxygen supply to the brain, which improves cerebral function and the ability to cope with stress.161 Exercise also helps flush toxins out of the body, which as discussed previously has beneficial effects on mood and overall health.
A deficiency in exposure to full-spectrum light (sunlight or indoor lighting that employs full-spectrum light bulbs) is linked to emotional instability, hyperactivity, anxiety, irritability, reduced ability to cope with stress, fatigue, apathy, seasonal affective disorder (SAD) and other types of depression, nutrient absorption problems, glandular problems, and weakened immunity, among other symptoms and conditions.162
For many people, lack of light has become a daily, round-the-year reality as a result of our technological age, which has so many of us spending the vast majority of our time indoors under artificial (non-full-spectrum) light.
Lack of light results in lower levels of serotonin. It also contributes to sleep disorders such as insomnia because it interferes with melatonin function. Melatonin, a hormone important in sleep regulation, is manufactured from serotonin. This helps to explain the intimate relationship between depression and sleep problems. The pineal gland, which manufactures melatonin, depends upon the proper cycle of darkness and light to stimulate or inhibit production. The body runs on a 24-hour cycle known as a circadian rhythm. The brain sets the body's internal clock to observe this cycle. People with bipolar disorder are particularly affected by any disruption of their internal clock. As their adaptive mechanisms are compromised, mood disturbances may follow.163
—ROBERT BOORSTIN, diagnosed with bipolar disorder at 24
The relationship of mood to light is reflected in the fact that bipolar disorder can have a seasonal pattern, with depressive episodes typically occurring in the seasons when there is reduced light—fall or winter. Manic episodes occur most frequently in the late summer. Suicides happen most often in the spring and fall, when the relationship of light and dark is undergoing the fastest changes.165
Spending more time outdoors and using full-spectrum light bulbs in your indoor environments are steps you can take to ameliorate lack of light. For a more focused treatment, light box therapy, in which you are exposed to more intensive full-spectrum light, may help.
There are a number of different ways to discuss the flow of energy in the human body. Physiologically, the salient point for mood disorders is that the nervous system operates on electrical charges. Extending outward, you could speak of the body's electromagnetic field and the far-reaching effects on mood and health caused by disturbances in that field (see chapter 3).
If you regard energy from the perspective of traditional Chinese medicine (which includes acupuncture), you analyze disturbance in the individual's vital force, or qi, as manifested by disturbed energy flow along the meridians, or energy channels, throughout the body (see chapter 8). If you consider energy from a shamanic or psychic viewpoint, you might explore the presence of foreign energy in an individual's energy field (see chapter 10). Homeopathy is also an energy-based medicine, with remedies that work to resolve a condition by restoring a person's energy to its natural equilibrium, which restores balance to the body, mind, and spirit (see chapter 9).
Whatever language you choose to employ to describe the phenomenon, a disturbance in an individual's energy field can contribute to mood disorders. The relationship of energy to other factors can be cyclical, with physical factors (such as nutritional deficiencies) or psychological or spiritual issues causing or being caused by a disturbance in energy flow. As mentioned in the earlier section on genetic factors, an inherited energy imbalance or an energy legacy passed down from generation to generation may also be operational (see chapter 3).
More detailed discussions of energy and methods for removing energy disturbances can be found throughout part II.
—PATTY DUKE
As noted, psychological/ emotional and spiritual issues have the capacity to throw the energy system out of balance and vice versa.
Along with their effect on mood and emotional stability, mind and spirit issues can produce a myriad of physical effects throughout the body, which in turn can compound bipolar disorder.
In keeping with the knowledge of the inseparability of body, mind, and spirit, it is important to consider possible issues in each as contributing to your bipolar disorder. Psychotherapy is one avenue for exploring the psychological and spiritual dimensions. Aside from the causal contributions in these areas, psychotherapy can provide an important forum for processing all the issues that arise from being diagnosed with, and living with, bipolar disorder. It could be considered as psychological and spiritual housecleaning or the maintenance work that taking good care of something requires. Taking good care of yourself means attending to the needs of body, mind, and spirit.
Many people with bipolar disorder find psychotherapy a vital part of their treatment program. As one person with bipolar disorder states it, “[P]sychotherapy heals, it makes some sense of the confusion, it reins in the terrifying thoughts and feelings, it brings back hope and the possibility of learning from it all.”167
A short-term intervention called cognitive therapy has been helpful to some people. Cognitive therapy operates on the principle that thoughts determine moods and emotions. While this is not to say that people with bipolar disorder ought to be able to control their mood swings, the therapy has application for learning how to monitor one's thinking as a warning of the early stages of an episode. Forewarned, people can then consciously change the thinking they have learned to recognize as their characteristically depressive or manic thinking, get more sleep, eat better, make sure they are exercising, or take other measures that they have learned can help them avert an episode. As one man who found cognitive therapy useful says, “I monitor my thinking patterns as an index of my emotional balance—rather like checking the blood sugar level in diabetes.”168
Bipolar disorder is a complex condition. No single factor is responsible for creating it, and no single therapeutic measure can reverse it. This means that you must discover what factors are involved in your case and take steps to ameliorate them.
The contribution of body, mind, and spirit elements in bipolar disorder is fully explored in part II. The first chapter provides a model that will help you make sense of the various levels of healing and how they relate to each other.
As a summary of the information in this chapter, the following are steps you can take to eliminate the causes, triggers, and contributors to your bipolar disorder.