4 |
Examination of the Peripheral Ocular Motor System |
In examining and treating motor anomalies (of the eye), one never loses an uneasy feeling of incompetence until he has become thoroughly familiar with the physiologic fundamentals from which the signs and symptoms of those anomalies are to be derived. Therefore, a discussion of motor anomalies of the eyes should begin with a synopsis of the physiology of the sensorial and motor apparatus of the eyes.
I. OCULAR ALIGNMENT AND DIPLOPIA
A. The goals of the ocular motor system
1. The ocular motor system finds, fixates, focuses/aligns on, and follows visual targets. In a word, the system foveates. To foveate means to align each eye so as to cause the central light ray to fall on the fovea and the entire retinal image to fall on corresponding retinal points of both eyes (Figs. 4-1 and 4-3).
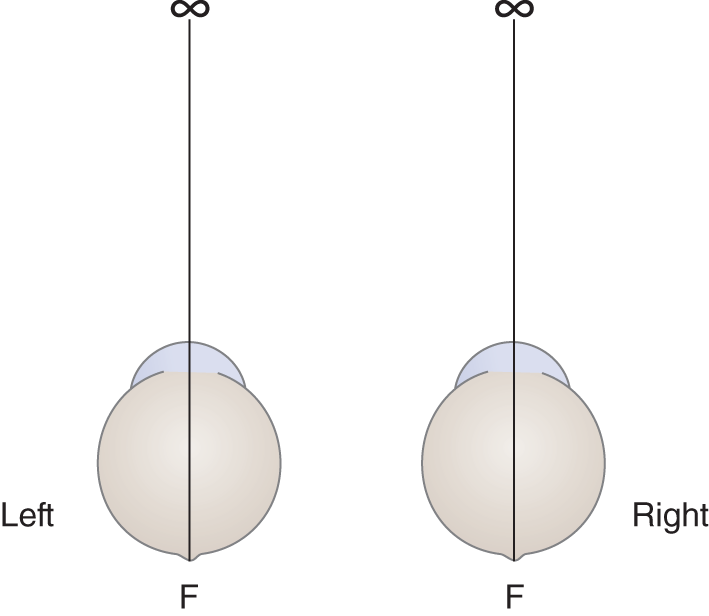
FIGURE 4-1. Visual axes with the eyes in the primary position, fixating on infinity distance. F = fovea.
2. The eyes must continually foveate whether the target remains fixed or moves or whether the eyes remain fixed or move in any direction: horizontal, vertical, rotatory, and vergences (convergence and divergence). Foveation promotes visual acuity and a single (fused) mental image and secures the advantages of binocular stereoscopic vision for survival.
B. Ocular alignment, the visual axes, and diplopia
1. To examine ocular alignment, start with the patient (Pt) looking straight ahead, the so-called primary position of the eyes. Theoretically, the point of fixation in the primary position is at infinity (Fig. 4-1).
2. A line drawn from the fovea centralis of one eye to the center of its visual field defines the visual axis. This line runs through the center of the media of the eye, striking the fovea centralis without undergoing any refraction. It is the “line of sight” of that eye. In Fig. 4-1, line F-∞ defines the _________
3. With the eyes in the primary position, fixating on infinity, the visual axes are  convergent/
convergent/ essentially parallel/
essentially parallel/ divergent. (
divergent. ( essentially parallel (Fig. 4-1))
essentially parallel (Fig. 4-1))
4. In Fig. 4-2, draw the visual axes where the eyes fixate on a point closer than infinity.
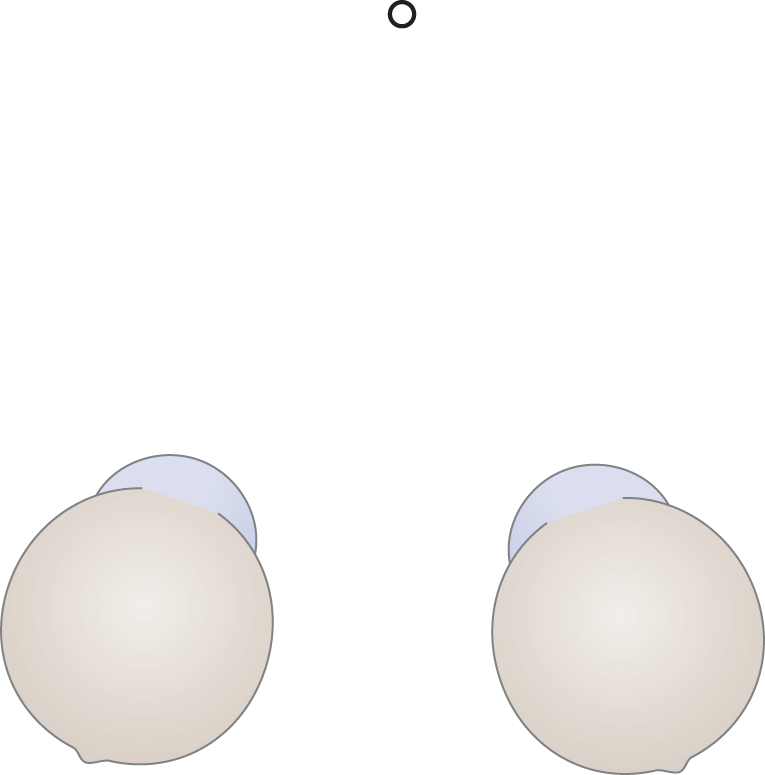
FIGURE 4-2. Blank for drawing the visual axes when the eyes fixate on a near point.
5. When looking at a near point, the eyes converge (adduct). Because each eye adducts, the central light ray from the fixation point remains on the fovea, the region of maximum visual acuity.
6. In Fig. 4-3, draw in the visual axes (from the fovea centralis to the center of the arrow). Study Fig. 4-3 to understand how binocular fixation brings the retinal images onto corresponding parts of the two retinas. To prove you understand the drawing, reproduce it sight unseen.
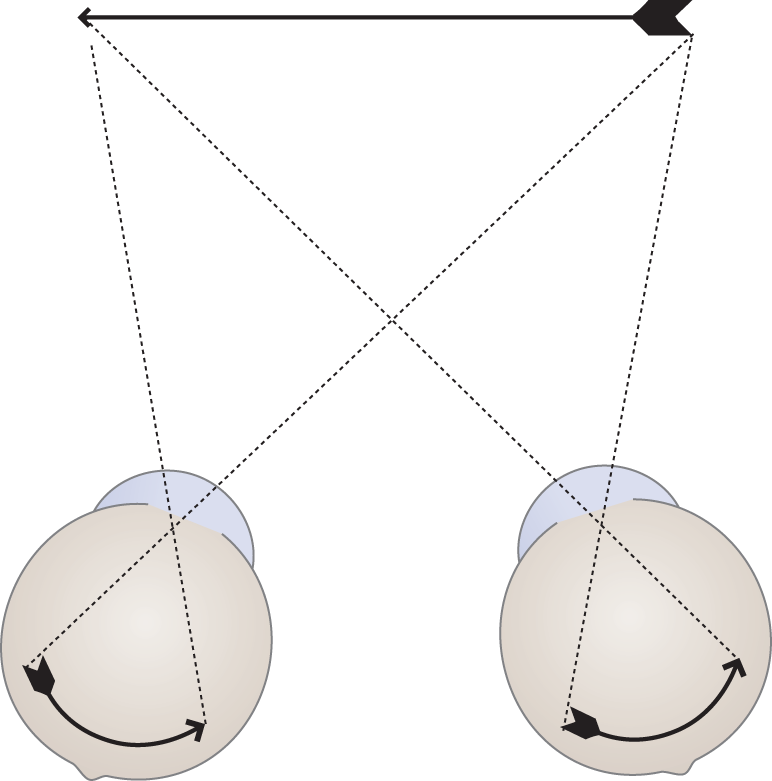
FIGURE 4-3. Binocular retinal image formed when the visual axes of the two eyes align properly on the center of the target. Rays along the visual axes strike the foveae. The remainder of the image falls on corresponding (but not precisely identical) temporal or nasal parts of the retina.
C. Self-demonstration of the visual axis of the dominant eye
1. With both eyes open, fixate strongly on a doorknob across the room. Then place your index fingertip 20 cm away from your eye, so that the knob appears to rest on the fingertip. Be sure to maintain fixation on the doorknob, but see the fingertip secondarily.
2. Alternately, wink the right and then the left eye as you fixate on the doorknob. (If you cannot wink each eye independently, cover one and then the other with your free hand.) What happens to the image of the finger?_________
3. Explanation of the shifting image: The shift occurs because you fixate primarily along the visual axis of the dominant eye; the other eye angles secondarily onto the target.
D. Self-production of physiologic diplopia
1. With both eyes open, first strongly fixate on the doorknob, and then hold up your fingertip to make the doorknob seem to balance on it. Then fixate strongly on your fingertip but secondarily attend to the doorknob. Alternate focusing strongly on one target while you attend to the other target.
2. What happens to the appearance of the doorknob when you strongly focus on the fingertip or to the fingertip when you strongly focus on the doorknob? _________
3. Figure 4-4 explains why the previous experiment disclosed physiologic diplopia.
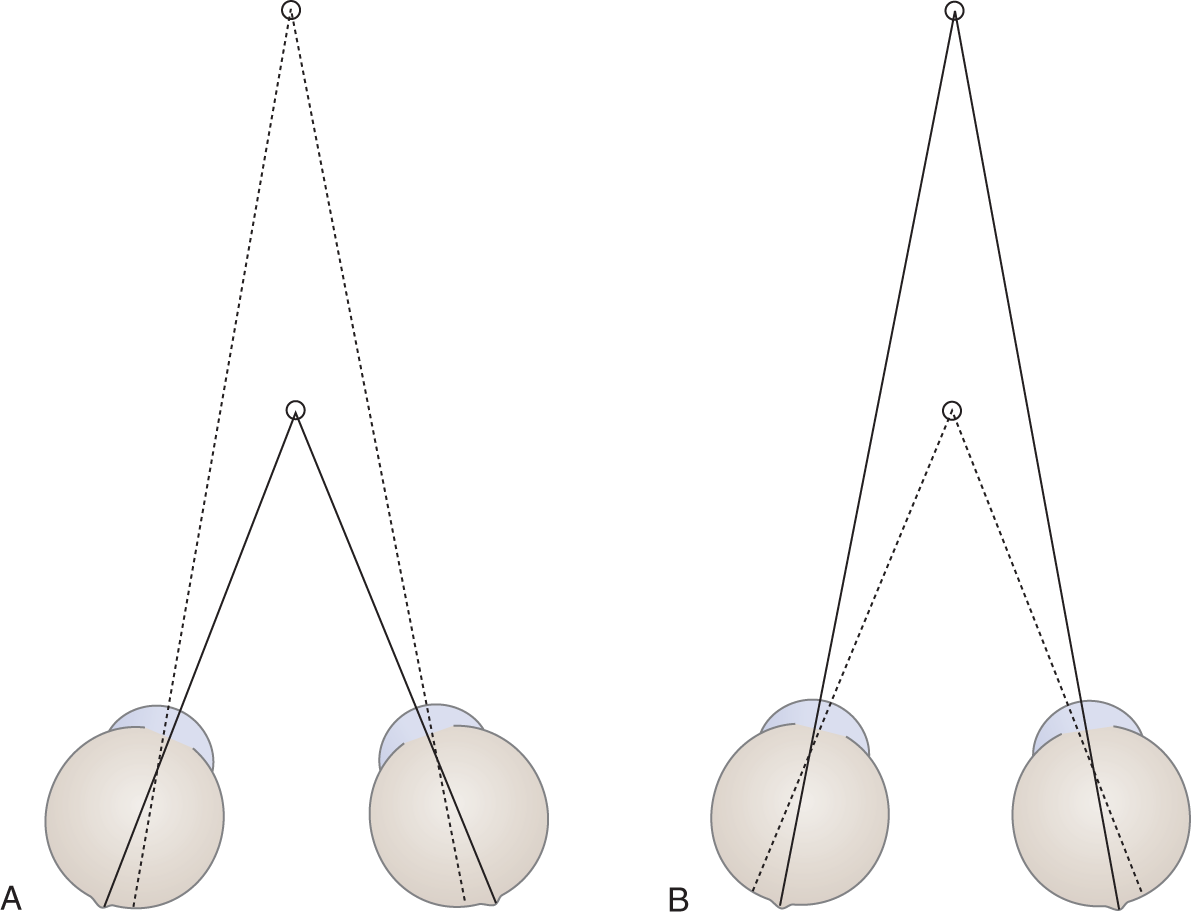
FIGURE 4-4. Changes in the angulation of the visual axes (solid lines) when the eyes diverge from a near fixation point (A) to a distant one (B). The rays from any other point in the visual field (dotted lines) fall off the fovea and macula and cause diplopia when attended to.
a. In Fig. 4-4, rays from only one distance, the fixation point, strike the fovea. All other rays deviate from the fovea in proportion to their distance from the fixation point. Only the rays coming in along the visual axes strike correspondingly on the fovea centralis of each eye.
b. Why do not we have diplopia all the time? Recall that you had to consciously attend to the point of nonfixation to get diplopia. Ordinarily, we have learned to suppress physiologic diplopia. It only appears when we make a determined effort to break through its physiologic suppression. We attend only to the nondiplopic images.
E. Self-production of pathologic diplopia by canthal compression
1. Place the tip of your right index finger on your right lateral canthus, as shown in Fig. 4-5.

FIGURE 4-5. Position of finger for lateral canthus compression to produce diplopia when gazing at the opposite finger.
2. Hold up your left index finger at arm’s length and fixate on it.
3. While fixating, press very gently on your right eyelid just above the canthus with your right index finger. By changing the pressure, you should experience diplopia. If you fail to produce diplopia when looking at your finger, look across the room at a distant object.
4. Repeat the experiment, but this time hold the outstretched finger horizontally. With the finger properly angled, you should get diplopia. It may be greater with the finger in one position than another, and it may change each time you try the experiment, depending on the deviation of the eyeball.
5. Identifying the faulty image in diplopia: While your right finger compresses your right lateral canthus, choose the best angle of the left finger to get diplopia.
a. While experiencing diplopia, try to identify the faulty image. You can identify it by:
i. Alternating the pressure on the eye, causing the faulty image to move while the other image remains on target.
ii. Winking the displaced eye.
iii. Noticing which image is the sharpest. Can you explain why the image from the displaced eye is not as sharp as that from the nondisplaced eye? _________
b. While producing diplopia, move your left finger to the right. What happens to the distance between the diplopic images as you move your target finger away from its starting position?
_________
6. Explanation for diplopia produced by canthal compression.
a. For description, the visual image of the aligned eye is called the true image, and that of the misaligned eye is called the false image. Of course, one image is no more “true” or “false” than the other, because both are visual images that the mind imposes on the afferent data.
b. Consider now the diplopia produced with the target finger vertical. (Even if you failed to get diplopia this way, you can follow the explanation.) With the finger vertical in the midline, you obtained one or, with practice, two results: one image was projected to the right or to the left of the true position of the finger. The direction of displacement of the eyeball determines the direction of projection of the false image. Study Fig. 4-6.
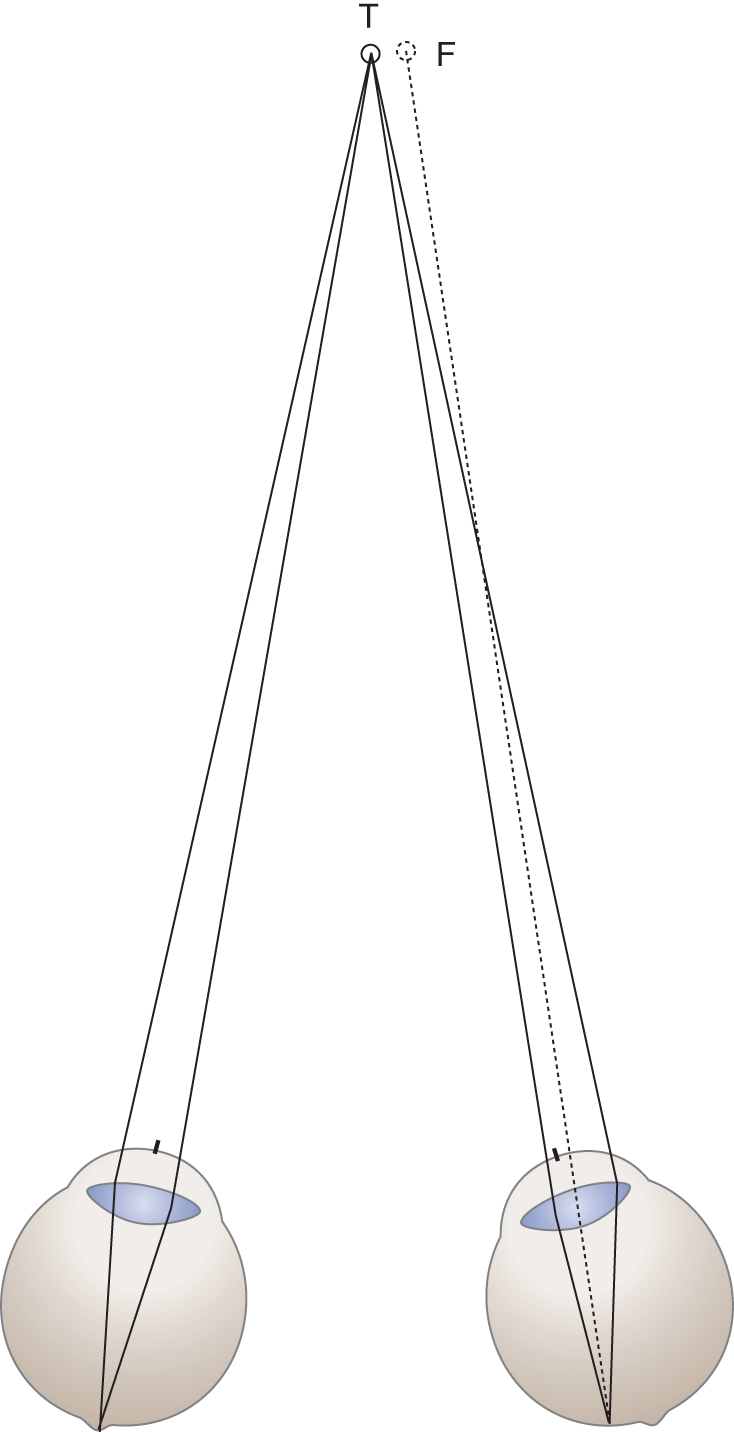
FIGURE 4-6. Diagram explaining projection of the false image to the right when the right eye fails to abduct. With a colored pencil, draw the visual axis of each eye, from the fovea through the corneal center to the target region. Notice how much the visual axis from the right eye misses the target, T. F = false image; T = true image.
7. Explain why the false image appears to the right of the true image in Fig. 4-6.
_________
8. The eyeball displacement experiment shows that both eyes have to align properly to bring the retinal images onto the corresponding retinal areas, thus avoiding the penalty of diplopia and decreased visual acuity.
II. THE ACTIONS OF THE INDIVIDUAL EXTRAOCULAR MUSCLES
We find that many students automatically reject model making as a waste of time. Let us say this: You will never really understand the ocular rotations unless you experience these actions by seeing them happen and feeling them with your own fingers. It might interest your skeptics to know that Leonardo da Vinci (1452–1519), who dissected many human bodies to learn about the actions of muscles, devised the method of tugging on tapes attached to the insertion of muscles to teach himself how the muscles worked. To experience the actions of the muscles, get these materials to make the two models:
1. To make an axial rotation model get:
a. A small ball of clay, a piece of a kitchen sponge, or even a wad of gum
b. Three toothpicks or, better, thin round applicator sticks
2. To make an eyeball rotation model get:
a. A soft, sponge rubber ball, 2 to 3 in. in diameter, that you can stick pins into
b. Several straight pins, preferably with large heads
c. A piece of leather (from the tongue of an old shoe) or plastic
d. Scissors
A. Model 1: Axial rotation of the eyeball around three axes
1. Each eye has to aim its visual axis at any point within the perimeter of movement. To achieve infinitely variable movement within that perimeter, the eyeball rotates axially around three axes: a vertical axis, a lateral axis, and an anteroposterior axis (A-P; Fig. 4-7).
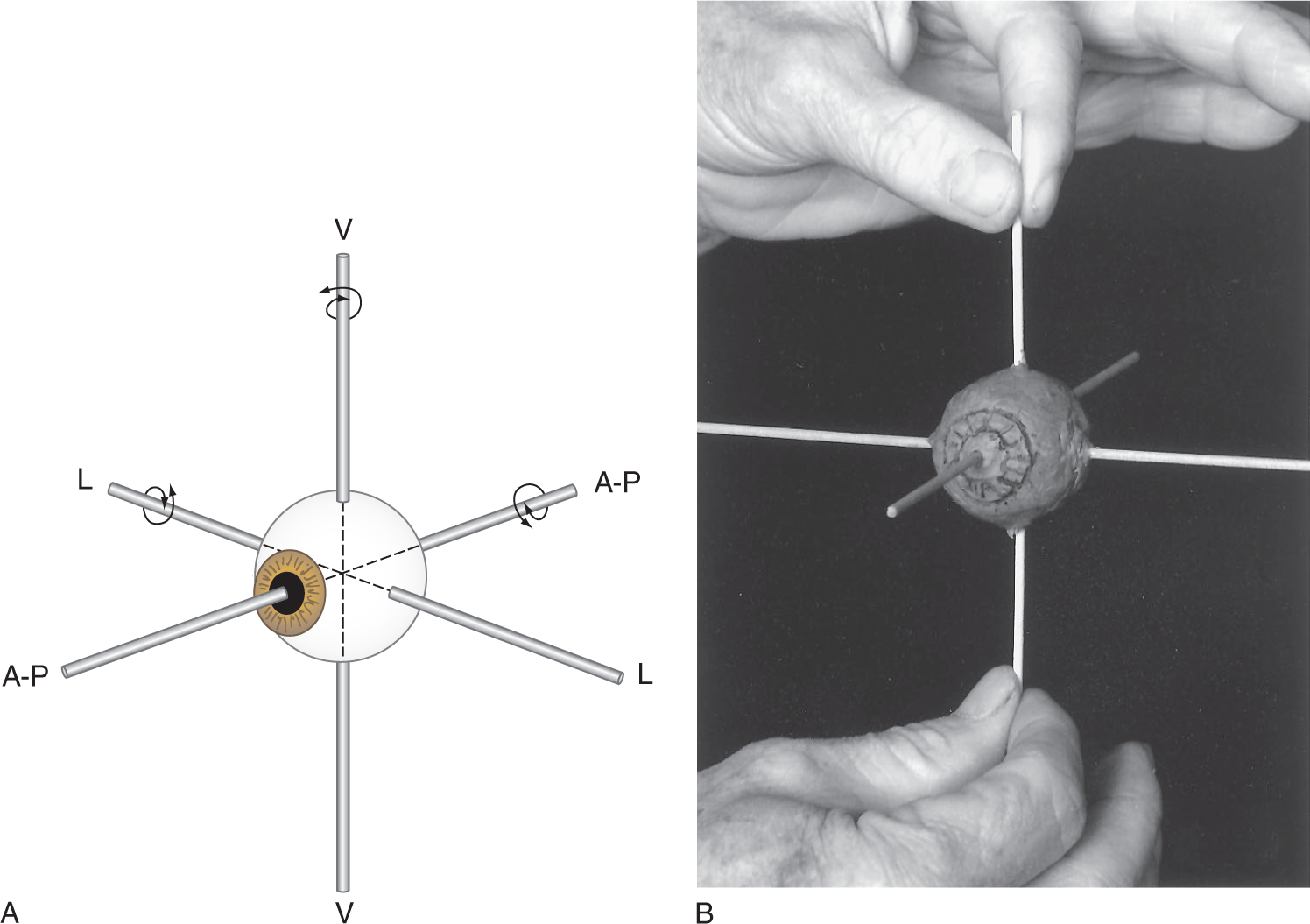
FIGURE 4-7. (A) The three rotational axes of the eye. A-P = anteroposterior; L = lateral; V = vertical. (B) Holding the model as shown, spin it on each of its three axes. You must make the model and spin it between your fingers to fully appreciate the meaning of axial rotation around three axes.
2. To visualize the axial rotation of the eyes, reproduce Model 1 as shown in Fig. 4-7B and label the axes. Rotate each of the three sticks around the vertical, lateral, and A-P axes. Actually hold the stick between your thumb and forefinger and spin the model. Then and only then, as you see it and your fingers feel it, will you understand that ocular rotation is axial rotation, not eccentric rotation. In Fig. 4-8 check the eye which shows the correct, axial rotation.
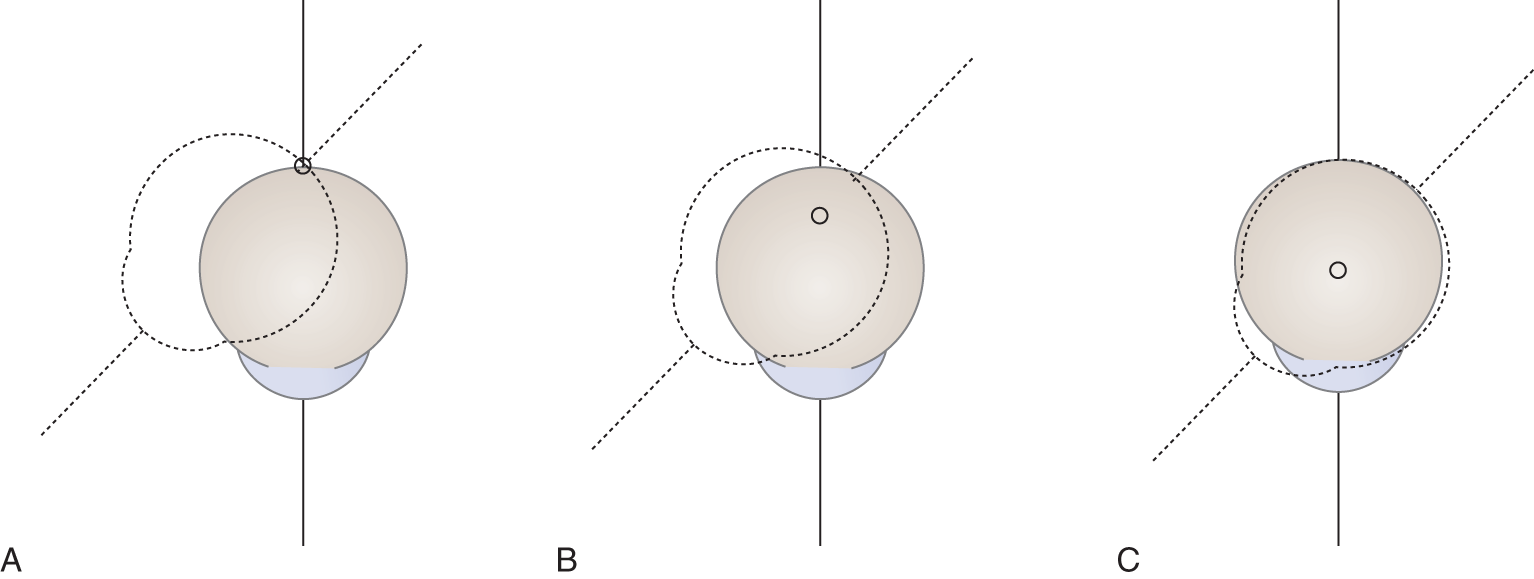
FIGURE 4-8. Diagram showing the alternative ocular rotations. Select the correct axial rotation:  A/
A/ B/
B/ C.(
C.( C)
C)
B. Model 2: Eyeball rotation model to demonstrate the pull of the extraocular muscles
1. On your rubber ball, draw a pupil and an iris. Then place dots for the points of emergence of the three axes and label them (Fig. 4-9).

FIGURE 4-9. Ball with leather strip pinned in place to simulate the right eye. The left hand holds the ball with the thumb and second digit pinching the vertical axis. When the right hand pulls back on the LR, the eyeball will rotate to the right around the vertical axis (abduct). LR = lateral rectus muscle.
2. Cut two strips of leather. Mark them MR and LR for the medial and lateral rectus muscles, respectively. Consider this model as the right eyeball.
3. Draw an arrow along the strips to represent the vector or line of pull of the contracting muscle (see the arrow in Figs. 4-9 and 4-11).
4. Stick a pin through the anterior end of each strip and into the ball. Stick the pin anterior to, but exactly in line with, the lateral axis. If you insert the pin posterior to the lateral axis, the muscles would retract, not rotate, the eyeball (Fig. 4-9).
5. Although in vivo the muscular actions differ somewhat from a mechanical model, the model provides valuable insights with regard to these actions.
C. Types of eye movements and nomenclature
1. The eyeball can rotate laterally or medially around its vertical axis, upward or downward around its horizontal axis, and torsionally (rotate in or out) around its A-P axis.
2. Ductions are monocular rotations when the opposite eye is covered, for example, adduction.
3. Versions are binocular parallel rotations to the sides, up, or down.
4. Vergences are binocular nonparallel rotations, for example, convergence or divergence.
D. Action of the medial and lateral rectus muscles
1. The simplest way to move the eyes around two axes is by four muscles (Fig. 4-10). Label the axes in Fig. 4-10 and learn the names of the four rectus muscles. Especially note their insertion anteriorly on the eyeball.
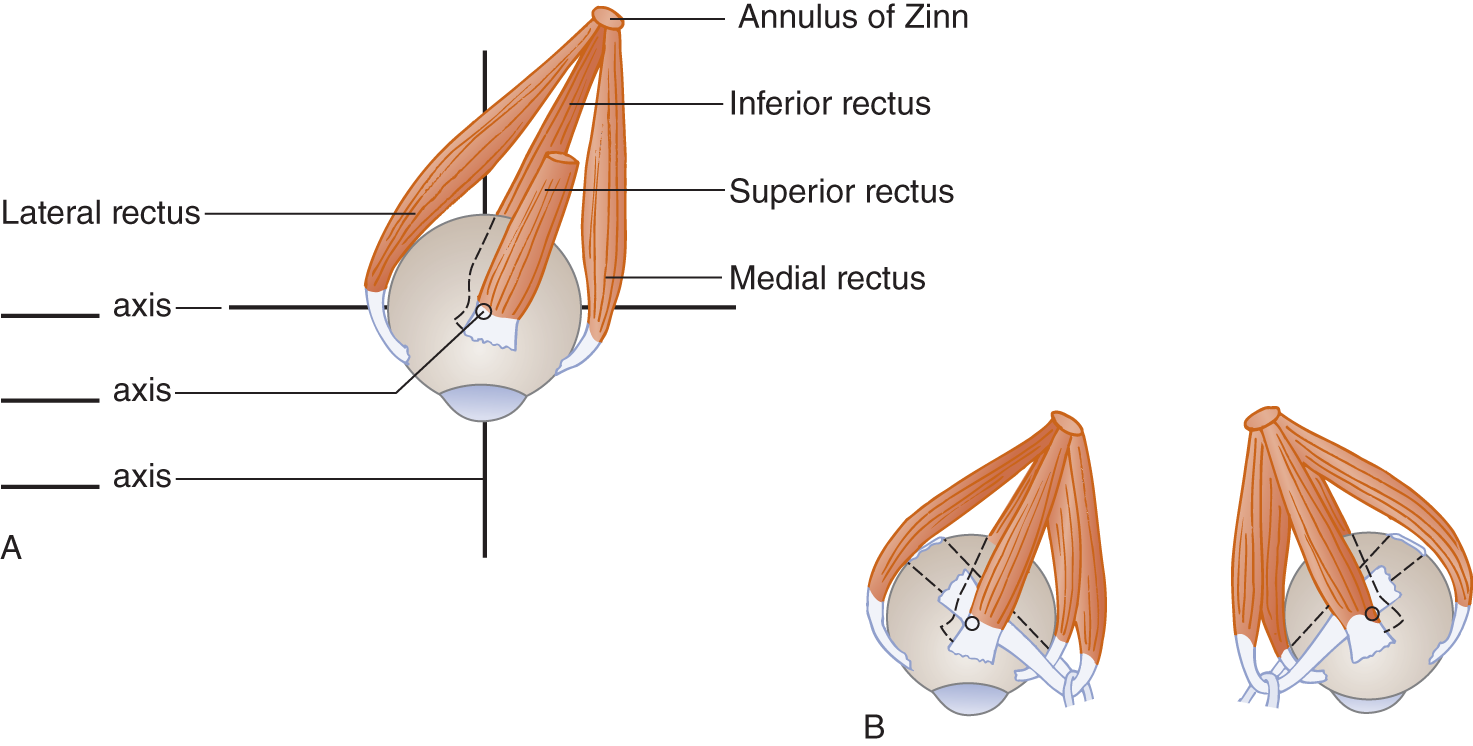
FIGURE 4-10. Origin and insertion of the ocular muscles. (A) Right eye, superior view, showing the origin and direction of insertion of the four recti with the eye in the primary position. (B) Both eyes, showing all six ocular rotatory muscles.
2. While holding the rubber ball with your index finger on the top of the vertical axis and your thumb on the bottom (pincer grasp), pull straight back on the lateral rectus strip with your other hand. Alternately pull the medial or lateral recti strips and observe the exact axial rotation of the ball around the vertical axis. Study Fig. 4-11 and label the axes.
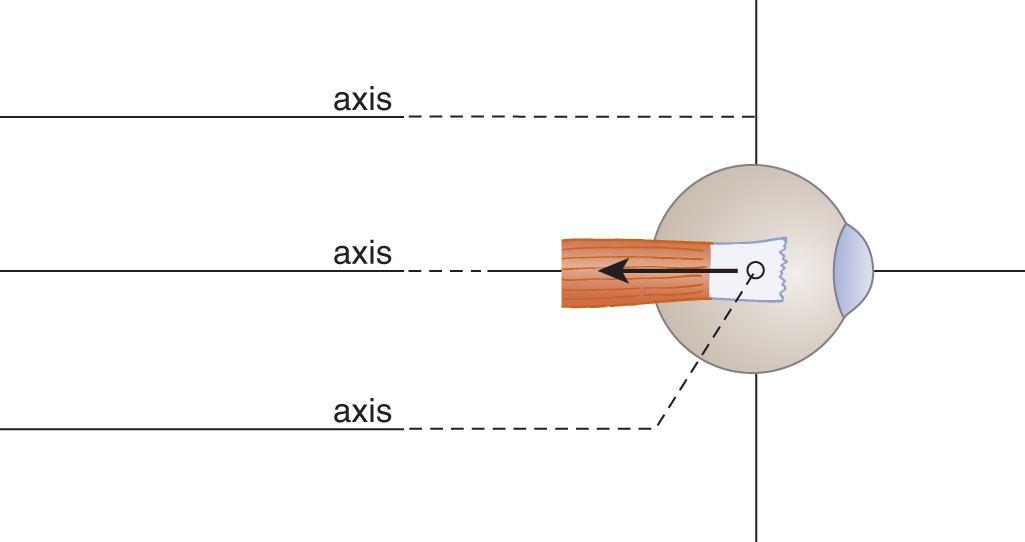
FIGURE 4-11. Lateral view of the right eye showing the direct pull of the lateral rectus muscle over the lateral axis (rotation around the vertical axis).
3. Only from your model will you fully appreciate this fact: You have to pull exactly straight back on the strips that represent the medial and lateral recti, along the vector arrow shown in Fig. 4-11, or the eye will wobble around rather than demonstrating precise axial rotation around the vertical axis.
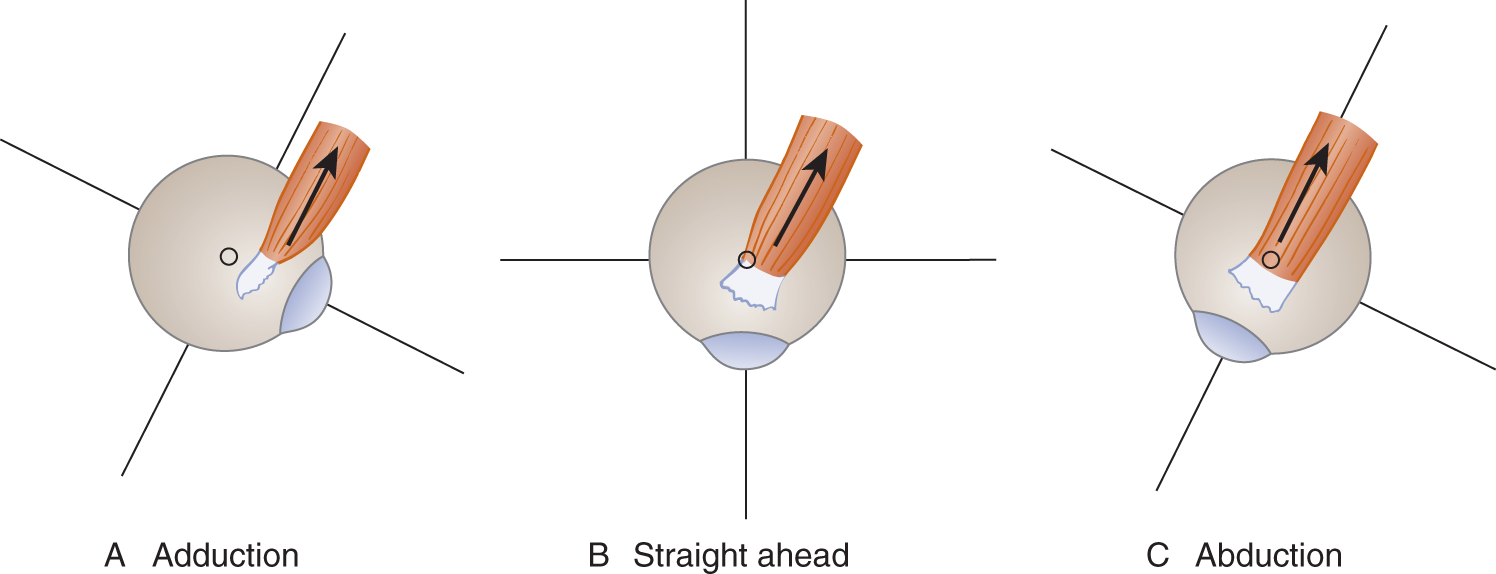
FIGURE 4-12. Right eye and superior rectus muscle, superior view (A-C). Notice how the position of the eye changes the relation of the muscle insertion to the vertical axis and, hence, changes the effective action of the muscle.
4. Because the medial and lateral recti pull exactly straight “on center,” they have one and only one action: to adduct or abduct the eye. The actions of the medial and lateral recti rotate the eye around the _________
E. Action of the superior rectus muscle
1. Attach another leather strip, label it SR for superior rectus, and draw an arrow to represent its vector or line of pull. Figure 4-12B shows that contraction of the superior rectus would rotate the eye upward around the _________
2. The angulation, or “off center” pull, of the superior and inferior recti causes a difference in the strength of the primary action and permits secondary and tertiary actions, depending on the position of the eye. To understand how the actions of some ocular muscles change as the eyes rotate, you must know the origin and insertion of the muscles in relation to the axes of the eyeball.
3. The recti all originate from the annulus of Zinn, a cuff that encircles the optic foramen. In Fig. 4-10 (top view of the right eye), note that from their origin the recti angle  laterally/
laterally/ medially.(
medially.( laterally)
laterally)
4. Figure 4-12B shows that, with the eyes in the primary position, the superior rectus runs somewhat  medial to/
medial to/ lateral to the vertical axis. (
lateral to the vertical axis. ( medial to)
medial to)
a. We have already seen that the superior rectus has the primary action to rotate the eye _________
b. To analyze the other actions of the superior rectus, angle the strip along the normal line of pull of the muscle, as in Fig. 4-12B. Now hold the eyeball by its vertical axis and notice that the ball rotates medially when you pull back on the strip.
c. Because its line of pull runs slightly medial to the vertical axis, the superior rectus has a secondary action to rotate the eye medially around the vertical axis. The muscle whose sole action is medial rotation of the eye is the _________
5. To better visualize the secondary and tertiary actions of the superior rectus, imagine the eye in a position of extreme adduction, as in Figs. 4-12A and 4-13. Hold the ball by the A-P axis and pull on the superior rectus strip after the ball has been turned medially, as in Fig. 4-13. You will find that it rotates inward.
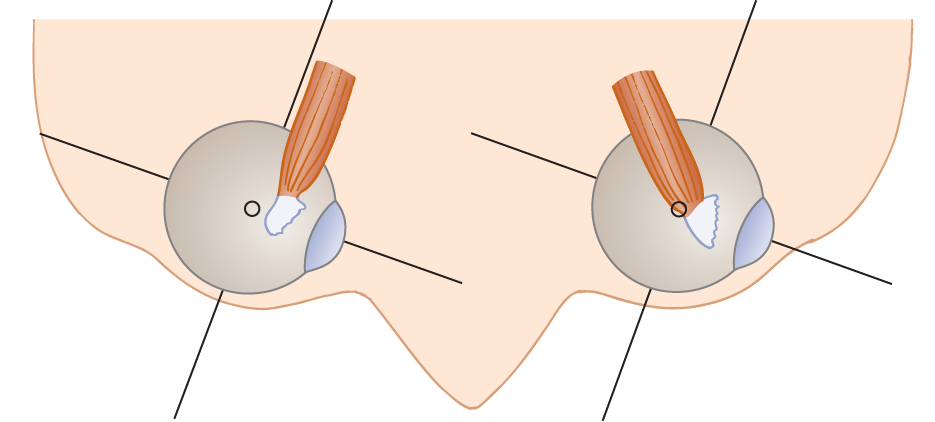
FIGURE 4-13. Superior view of the eyes illustrating the relation of the pull of the superior rectus muscle to the ocular axes when the eyes rotate to the left (rotation exaggerated).
6. Now you have observed that the superior rectus can elevate the eye, adduct it, and tilt the vertical axis inward. Inward tilting of the vertical axis is called intorsion, as shown in Fig. 4-14.
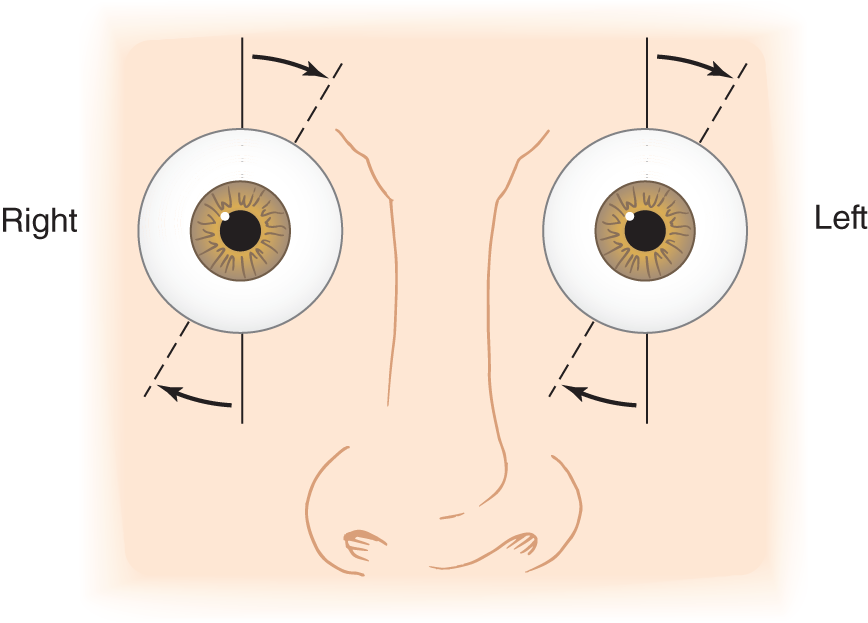
FIGURE 4-14. Torsion of the eyes. The right eye shows intorsion, and the left shows extorsion. Naming the torsions depends on whether the top of the vertical axis tilts in (intorsion = medially) or out (extorsion = laterally).
7. In Fig. 4-14, the right eye has rotated around the A-P axis, tilting the top of the vertical axis in. This action is called  intorsion/
intorsion/ extorsion. (
extorsion. ( intorsion)
intorsion)
8. In the left eye of Fig. 4-14, the top of the vertical axis tilts out. Therefore, it is called _____torsion. (extorsion)
9. The torsions involve rotation of the eye around the _____ axis. (A-P)
10. When the eye is abducted, the point of insertion of the tendon of the superior rectus shifts laterally in relation to the vertical axis, as shown in Fig. 4-12C. The vector (arrow) now pulls directly over the vertical axis.
11. Would the superior rectus act to adduct or intort when the eye is abducted?  Yes/
Yes/ No. (See next frame.)
No. (See next frame.)
12. With the eye abducted, the superior rectus pulls directly over the vertical axis. It dissipates none of its strength in adduction or intorsion. Therefore, the superior rectus elevates the eye most strongly when the eye is  adducted/
adducted/ straight ahead/
straight ahead/ abducted. (
abducted. ( abducted)
abducted)
13. In what position of the eye would the superior rectus have the weakest action of elevation? _________
14. In summary, the primary action of the superior rectus is _________
a. The secondary and tertiary actions of the superior rectus are _________
b. What direction would you ask the Pt to look to test the strongest elevating action of the right superior rectus?
_________
F. Action of the inferior rectus muscle
1. The inferior rectus muscle has the same direction of origin and insertion as the superior rectus (Fig. 4-10). The primary action of the inferior rectus is to  depress/
depress/ elevate the eye. (
elevate the eye. ( depress)
depress)
2. Its secondary action would be to _________
3. To analyze the tertiary inferior rectus action, pin another strip to the rubber ball to represent the inferior rectus. Hold the ball by the A-P axis and consider the inferior rectus action with the eye adducted. Then, when the inferior rectus contracts, the top of the vertical axis should tilt  internally/
internally/ externally. (
externally. ( externally)
externally)
4. External tilting of the vertical axis is called _________
5. What is the only eye position in which the superior and inferior recti could rotate the eye in the same direction? _________
6. The superior and inferior recti are ineffective adductors until the medial rectus muscle, the most critical muscle for adduction, has already begun to act.
7. To test the strongest action of the right inferior rectus as a depressor, in what direction would you ask the Pt to look?
_________
8. In summary, list the primary and two supplementary actions of the inferior rectus muscle. _________
G. Action of the superior oblique muscle
1. The superior oblique muscle originates from the lesser wing of the sphenoid bone, just above the annulus of Zinn. Its tendon runs through a trochlea (pulley) attached to the rim of the bony orbit (Fig. 4-15A). When the tendon runs to the eye, it inserts posteriorly to allow the superior oblique to have an effective pull when contracting. In so attaching, the tendon runs somewhat medial to the vertical axis, like the superior and inferior recti. Cut another strip, label it SO (superior oblique), and draw an arrow to represent its vector along the line of the tendon.
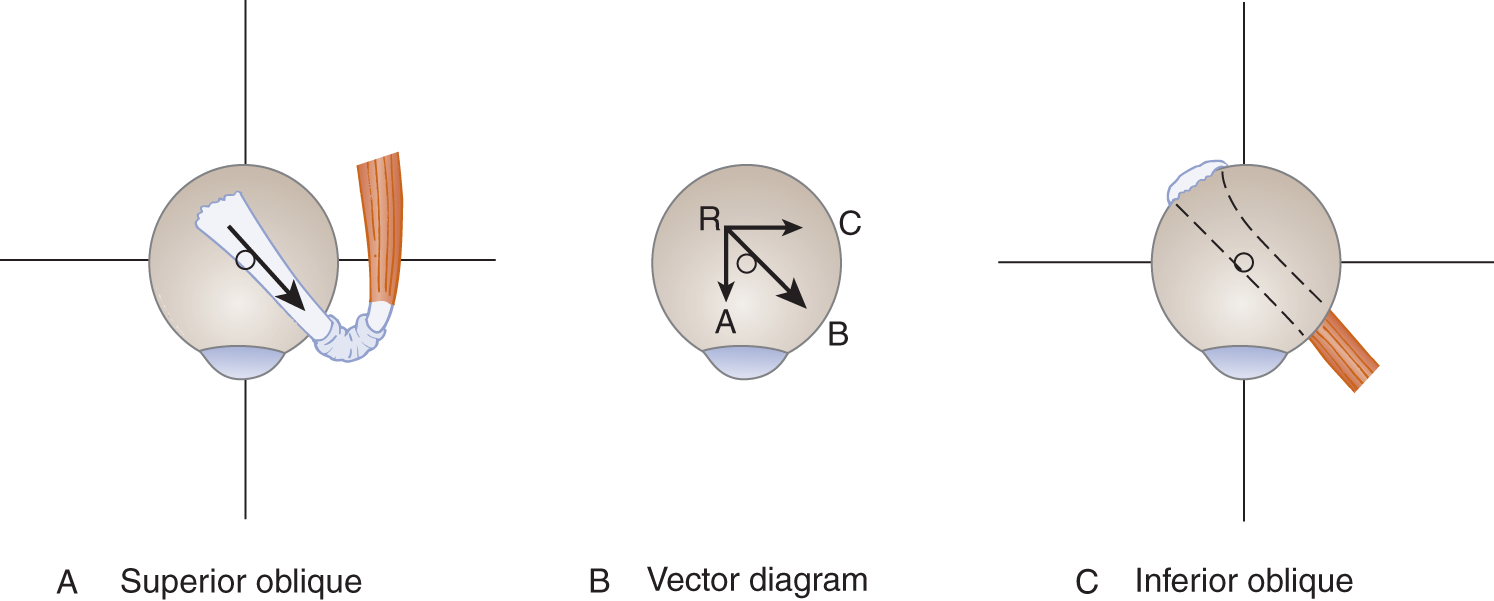
FIGURE 4-15. Right eye, superior view, showing the actions of the superior and inferior oblique muscles (A-C). (A) The arrow represents the line of pull of both muscles. This vector runs somewhat medial to the vertical axis. Notice that vector R-B originates at R, posterolateral to the vertical axis.
2. The vector diagram of Fig. 4-15B resolves arrow R-B into effective components.
a. Vector R-A  depresses/
depresses/ elevates the eye around the _________
elevates the eye around the _________ depresses; lateral)
depresses; lateral)
b. Vector R-C  abducts/
abducts/ adducts the eye around the _________
adducts the eye around the _________ intorts/
intorts/ extorts the eye around the _________
extorts the eye around the _________ abducts; vertical;
abducts; vertical;  intorts; A-P)
intorts; A-P)
c. Therefore, vector R-B acts to _________
3. To recapitulate: Contraction of the superior oblique, when the eye starts in the primary position, causes:
a. A primary action to  depress/
depress/ elevate the eye. (
elevate the eye. ( depress)
depress)
b. A secondary action to  adduct/
adduct/ abduct/
abduct/ elevate the eye. (
elevate the eye. ( abduct)
abduct)
c. A tertiary action to  intort/
intort/ extort the eye. (
extort the eye. ( intort)
intort)
4. With the eye in the primary position, the line of pull of the superior oblique tendon runs medial to the vertical axis (arrow in Fig. 4-15A). Complete Fig. 4-16 to show the relation of the vertical axis of the eye to the line of pull of the superior oblique tendon when the eye is adducted.
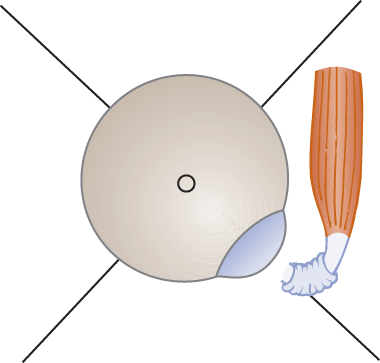
FIGURE 4-16. Blank to be completed to show the relation of the line of pull of the superior oblique tendon to the vertical axis when the eye is adducted.
5. When the eye is adducted, the tendon of the superior oblique pulls directly over the vertical axis. Therefore, none of the depressor action of the muscle is dissipated in the other actions, which are to _________
6. In what position of the eye does the superior oblique show the strongest primary action of downward rotation of the eye? _________
7. Hence, the clinical test for the strongest action of the superior oblique is to ask the Pt to look _________
H. Action of the inferior oblique muscle
1. The inferior oblique muscle, in contrast to the other ocular muscles, originates from the medial inferior rim of the bony orbit. No other ocular muscle originates anteriorly. It inserts on the posterior part of the eyeball. To attain sufficient resting length, it wraps further around the eye than the other muscles.
2. The inferior oblique muscle passes posteriorly, somewhat medial to the vertical axis. Its obliquity and alignment with the vertical axis matches the superior oblique (Figs. 4-15A and 4-15C).
a. The primary action is exactly antagonistic to the superior oblique. The inferior oblique acts to _________
b. The secondary action is to _________
c. The tertiary action is to _____ the eye, antagonistic to the superior oblique. (extort)
d. The one direction in which the superior and inferior obliques rotate the eyeball the same way is _________
3. The obliques can abduct strongly only after the lateral rectus has already started to rotate the eye laterally. After lateral rectus paralysis, the obliques cannot initiate abduction and the eye cannot be abducted. We run squarely into a problem. Intorsion, the so-called tertiary action of the superior oblique, is clinically one of its most important actions. Therefore, in classifying intorsion as a tertiary action, we do not dismiss it as a negligible action.
I. A vector diagram of ocular muscle action
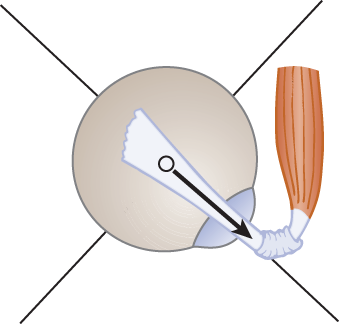
1. In the blanks of Fig. 4-17, place the initials of the muscles represented by the vector arrow numbers.
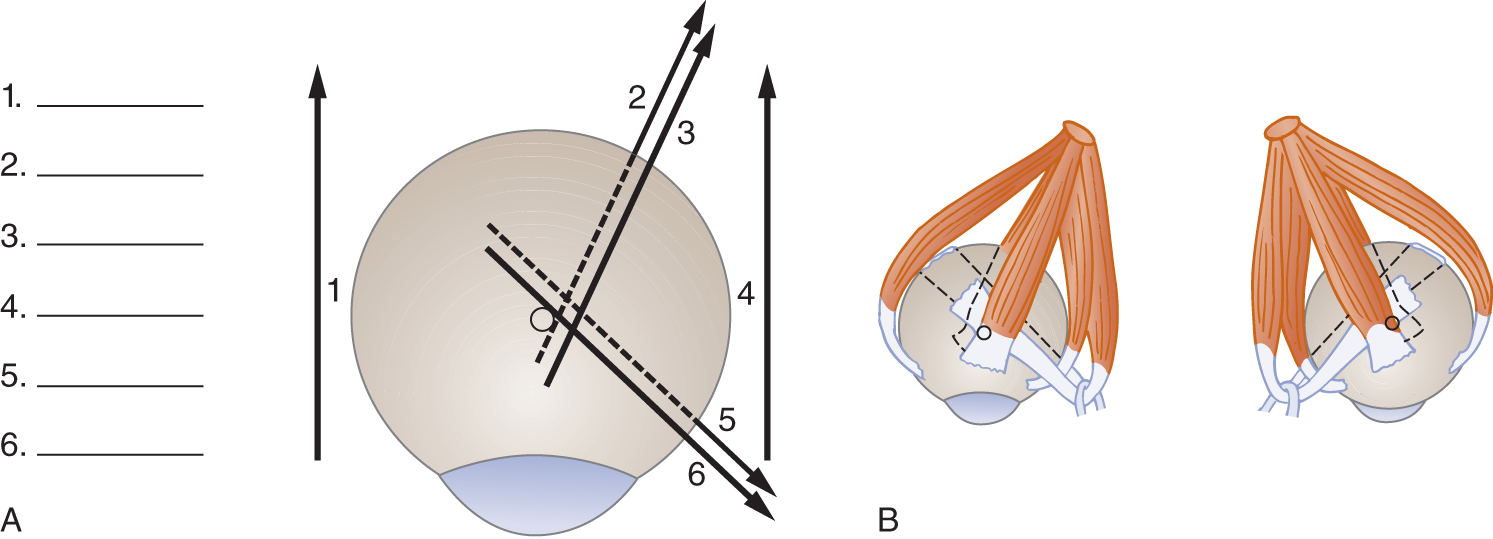
FIGURE 4-17. Eyes viewed from above. (A) Composite vector diagram showing the effective direction of pull of the muscles with the right eye in the primary position. Fill in blanks 1 to 6 with initials corresponding to the muscle represented by the vector. (B) Composite drawing of all six ocular rotatory muscles. Match them with the vectors shown in (A).
1. LR
2. IR
3. SR
4. MR
5. IO
6. SO
2. The vector diagram combined with a knowledge of the origin and insertion enable you to remember forever the actions of the ocular muscles. We can state that, when the eye is in the primary position, the pull or vector of all the ocular muscles is medial to the vertical axis except for the _________
3. Because four of the ocular muscles pull “off center,” that is, medial to the vertical axis, they display their particular secondary and tertiary actions. The four muscles that pull off center when the eye is in the primary position are the _________
4. The two muscles that always pull “on center” and therefore have only primary actions are the _________
5. Cover the answers in Table 4-1 and recite them. Use drawings or the ball model, when necessary, to deduce the answers.
TABLE 4-1 • Summary of Actions of the Individual Extraocular Muscles
Muscle |
Primary action |
Secondary |
Tertiary |
Medial rectus |
Adducts |
||
Lateral rectus |
Abducts |
||
Superior rectus |
Elevates |
Adducts |
Intorts |
Inferior rectus |
Depresses |
Adducts |
Extorts |
Superior oblique |
Depresses |
Abducts |
Intorts |
Inferior oblique |
Elevates |
Abducts |
Extorts |
J. Mnemonic summary of the actions of the ocular rotatory muscles
K. Yoking of ocular muscles
1. The ocular muscles of the two eyes collaborate with each other to keep the eyes aligned. If a Pt has diplopia when looking to the left, you would suspect weakness of the abductor of the left eye or the adductor of the right eye.
a. The strongest abductor of the left eye is the muscle whose only function is abduction, the _________
b. The strongest adductor of the right eye is the muscle whose only function is adduction, the _________
c. When muscles of the two eyes act in unison for conjugate gaze, we say that they are yoked.
2. Suppose a Pt complains of diplopia only when looking up and to the left.
a. When the left eye is abducted, the strongest elevator is the _________
b. When the right eye is adducted, the elevating power of its superior rectus is diverted to the secondary action of the muscle, _________
c. As the superior rectus loses its elevator strength during adduction, the muscle that converts its action solely to elevation is the _________
d. During adduction of an eye, the elevator action of the superior rectus  decreases/
decreases/ increases, and the elevator action of the inferior oblique simultaneously
increases, and the elevator action of the inferior oblique simultaneously  decreases/
decreases/ increases. (
increases. ( decreases;
decreases;  increases)
increases)
e. Thus for upward gaze to the left, the muscle that elevates the left eye, the _________
f. Which muscle has the strongest depressant action when the eye is adducted? _________
g. The muscle with the strongest depressor action with the eye abducted is the _________
h. A Pt looking to the right has diplopia when he looks down. Which of the yoked muscles should you suspect of weakness: the _________
3. Hering law (Ewald Hering, 1834–1918) of equal stimulation of the yoke muscles. The law states that the muscles yoked for conjugate eye movements receive equal stimulation by the nervous system. Thus, if the right lateral rectus is stimulated to rotate the right eye to the right, the left medial rectus receives equal stimulation. This principle is called Hering law. State Hering law in your own words. _________
4. A summary of the yoke muscles. If you studied pages 123 to 131, complete Fig. 4-18 by writing in the initials of the muscles most important for the movement indicated by the arrows. If you did not read those pages, simply copy in the correct initials for reference.
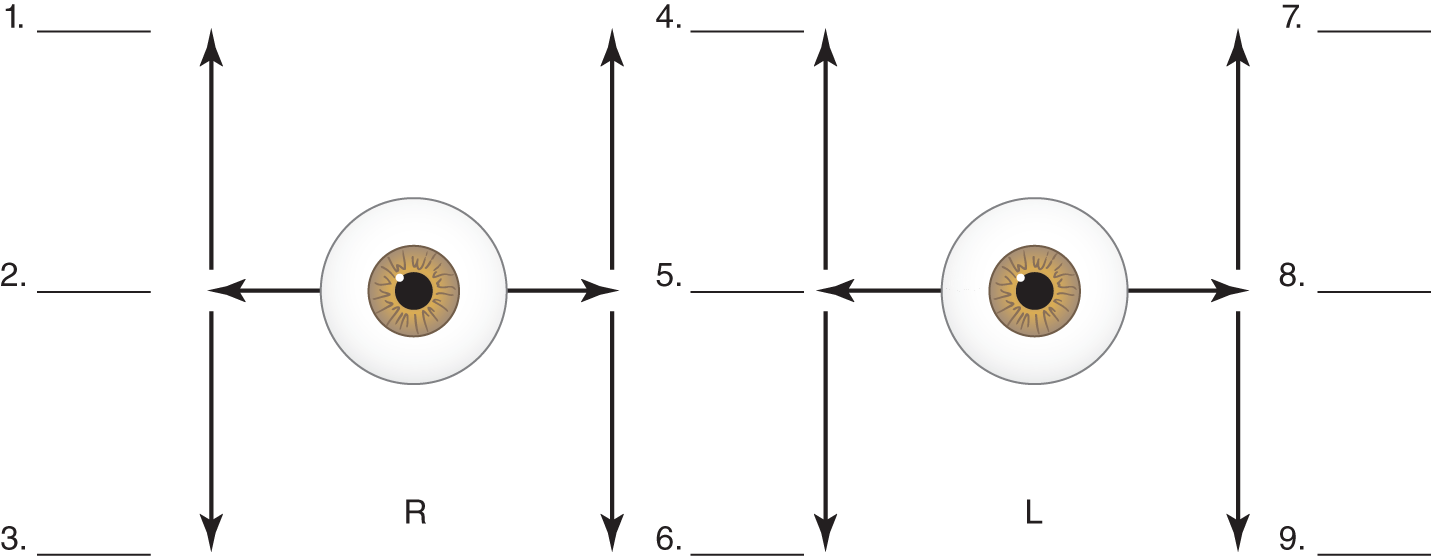
FIGURE 4-18. Yoking of the strongest actions of ocular muscles in moving the eyes in the cardinal directions of gaze. In blanks 1 to 9, place the initials of the muscle whose strongest action is indicated by the arrow. Then read across the diagram, for example, 1 to 4 to 7, to see which muscles pair up. Thus, in looking to the right and up, the superior rectus muscle (1) of the right eye is yoked with the inferior oblique muscle (4) of the left eye. L = left; R = right.
1. SR 4. IO 7. SR
2. LR 5. MR 8. LR
3. IR 6. SO 9. IR
L. Oppositional action of pairs of ocular muscles of one eye and the tonic innervation of the extraocular muscles
1. The medial and lateral recti of one eye exemplify a general law of the EOMs: The muscles of one eye act in agonist and antagonist pairs. For each direction of eye movement, one or more muscles act in exactly the opposite direction.
2. An electromyographic needle inserted into the EOMs records a continuous play of nerve impulses called tonic innervation that maintains light tension in the muscles with the eyes still and in the primary position. Other skeletal muscles are electrically silent when the part they move is at rest. During conjugate movement of the eyes, Sherrington law of reciprocal inhibition holds: The muscle or muscles in one eye that cause the rotation are actively innervated, whereas the antagonists are inhibited. After the eye movements stop, tonic innervation resumes.
3. Because each agonist–antagonist pair of EOMs receives a tonic, equal play of nerve impulses, the pull of one muscle balances the pull of the other, like opposing rubber bands under slight tension. Thus, the position of the eyes is always positively determined.
4. After paralysis of one EOM, the eye deviates in the direction of pull of the intact, oppositional muscle, which continues to receive its tonic innervation. After paralysis of the lateral rectus muscle (VI nerve palsy), tonic innervation of the medial rectus causes the eye to rotate  inward/
inward/ outward. (
outward. ( inward)
inward)
M. Review of actions of the extraocular muscles
1. List the six ocular rotatory muscles and their origins and insertions in relation to the axes of ocular rotation.
2. The muscles (or tendons in the case of the superior obliques) all insert distal to the way they approach the globe (Fig. 4-17).
3. With the eyes in the primary position, the vector of only one muscle, the lateral rectus, pulls lateral to the vertical axis (Fig. 4-17).
4. Only one muscle, the inferior oblique, originates anteriorly, and only one muscle, the superior oblique, runs through a trochlea (pulley).
5. Reason out the position of the eye when only one muscle is paralyzed. The eye turns away from the pull of the paralytic muscle because the intact muscles act unopposed.
6. Reason out the position of the eye when only one nerve is intact.
7. Distinguish between the possible movements of the muscle according to the mechanics of origin and insertion and the strongest movements of the muscle when the eye is rotated into the optimum position.
III. CLINICAL TESTS FOR OCULAR MALALIGNMENT AND THE RANGE OF EYE MOVEMENTS
A. Initial inspection of the relation of the limbus to the eyelid
Initially, inspect the relation of the limbus to the lid margins as the Pt gazes straight ahead. Then look for gross malalignment of the eyes, but beware of first impressions, particularly if the Pt has asymmetrical eyelids or canthus dystopia, as many young children do. Depend on the corneal reflection test as the best test for ocular malalignment (Helveston, 1967; Keane, 1993; Shaunak et al, 1995; Von Noorden, 1996).
B. Technique for the corneal light reflection (Hirschberg) test
Use a partner, if available, but the instructions assume that you have no partner and will use a hand mirror.
1. Darken the room and locate one distant light source such as a light bulb or an otoscope light.
2. Face the light source and gaze straight ahead into the mirror while holding it as far away as possible to avoid convergence. Observe that one bright diamond of light reflects off each cornea. By slight mirror movements, try to center these diamonds simultaneously on the two corneas. What is the exact location of the corneal light reflection with respect to the true geometric center of each cornea?_________
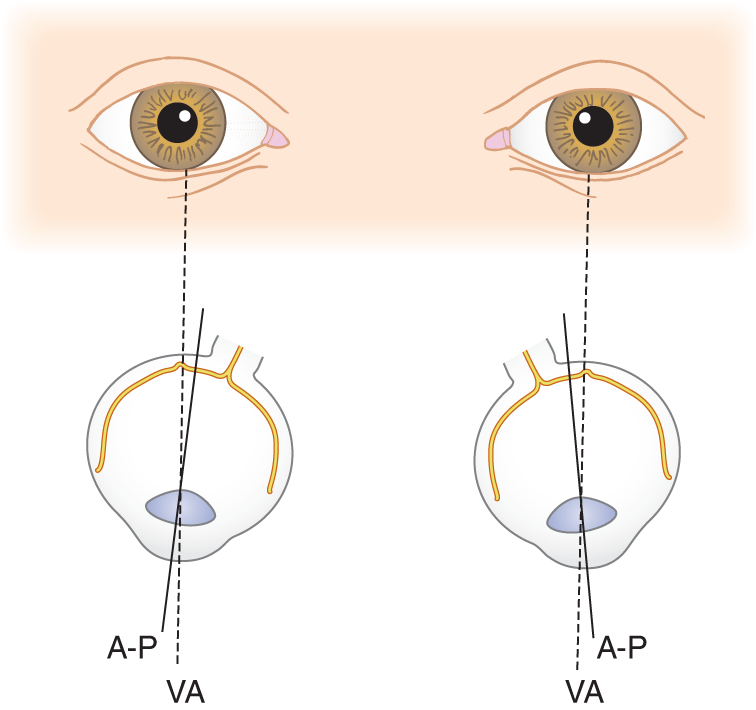
FIGURE 4-19. Diagram to show why the corneal light reflections are slightly medial to the true geometric centers of the corneas. The patient is looking straight ahead. The fixation reflexes have automatically aligned the visual axes parallel to each other, to bring the parallel light rays from infinity onto the foveae. The true, geometric A-P axes of the eyes now diverge slightly. A-P = anteroposterior axis; VA = visual axis.
3. While watching your corneal light reflections, move the mirror slightly to one side (or have your partner move his eyes). The points of light reflection from each cornea then displace the same distance from the corneal centers, to end on corresponding corneal points, if ocular alignment is normal in all fields of gaze. Move your mirror around full range, chasing the points of reflection over the surfaces of the corneas and noting the correspondence of the points of each eye.
4. Thus, the examiner (Ex) checks for ocular malalignment in two ways:
a. Abnormal relation of the corneal limbus to the margins of the eyelids
b. Noncorrespondence of the points of corneal light reflection
5. Why do you look for noncorrespondence of the corneal light reflections and abnormality of the limbus relation rather than for correspondence and normality? _________
C. Technique for evaluating the range of movement of the eyes
1. During the history, the Ex judges the range of volitional eye movements.
2. Start the formal examination with the Pt sitting. Gently press on top of the Pt’s head with one hand and fix the head in position by a “proprioceptive link” between yourself and the Pt, permitting only the eyes to move. Mentally retarded or demented Pts have difficulty separating eye and head movements.
3. Ask the Pt to fixate on your finger, which you hold up in the midline, about 50 cm away, at station l in Fig. 4-20.
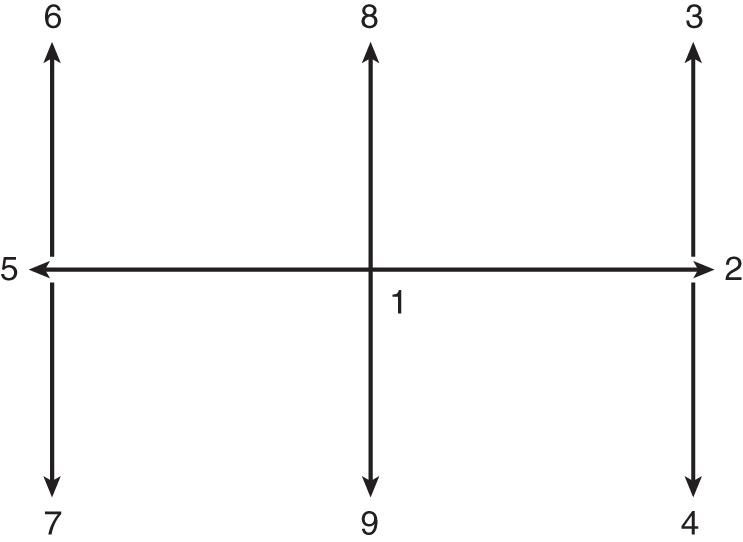
FIGURE 4-20. The H-shape through which the examiner moves his/her finger to test ocular motility.
4. Request the Pt to follow your finger horizontally with the eyes to station 2, the extreme end of lateral gaze. For testing horizontal eye movements and vergences, hold the finger vertically; for testing vertical movements, hold the finger horizontally. Then the Pt can more easily follow the finger and better appreciate any minimal separation of diplopic images that might occur.
5. Hold the finger at station 2 and inspect the corneal light reflections and the relation of the limbus to the lid margins, canthi, and caruncles. Look for nystagmus (discussed in Chapter 5).
6. Next, move to stations 3 and 4 at the extremes of lateral upward and downward gaze. Repeat the observations of step 4.
7. Move your finger back to the horizontal plane and across to station 5 and repeat all observations and maneuvers at stations 6 and 7.
8. Move your finger back to station 1 and say, “Look right at my finger,” as you move it in to touch the bridge of the Pt’s nose. Look for convergence and the accompanying pupilloconstriction. Usually, one eye breaks off convergence when the finger is several centimeters away from the nose.
9. Finally hold your finger horizontally and ask the Pt to follow it to stations 8 and 9.
10. Figure 4-21 shows the normal range of eye movements in millimeters. Notice that upward gaze has the least range. Diffuse brain disease impairs the relatively restricted upward movements more than other movements, but midbrain lesions can selectively impair upward or downward movements or both.
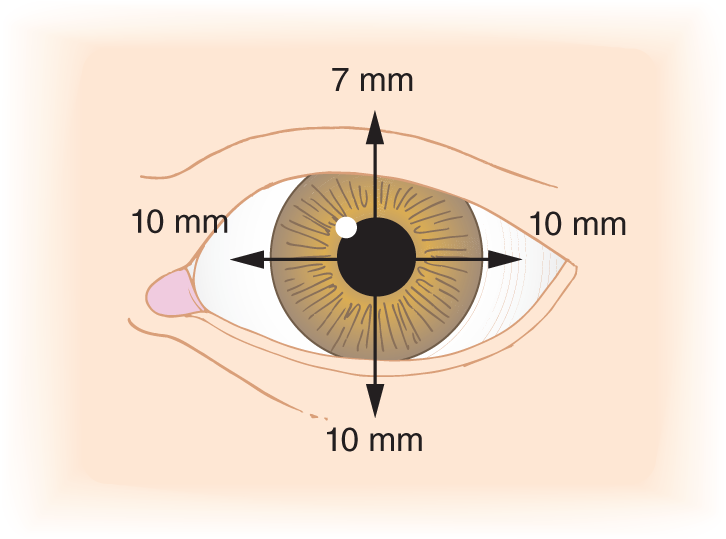
FIGURE 4-21. Range of ocular rotations, in millimeters.
11. Because the Pt may have experienced diplopia while observing your finger, ask the Pt about it. Select the best-phrased question:
a.  You are seeing two fingers instead of one, are not you?
You are seeing two fingers instead of one, are not you?
b.  Do you have diplopia?
Do you have diplopia?
c.  Do you see one or two fingers? (
Do you see one or two fingers? ( c)
c)
12. Students frequently make type a and b errors. The first question may force an erroneous answer, because the Pt expects the doctor to know what will happen. The second question uses a technical term, diplopia, unfamiliar to the Pt. Make a general rule about phrasing such questions.
_________
13. If the Pt reports double vision, darken the room and watch the corneal light reflections as the Pt pursues a tiny light, such as an otoscope lamp, through the configuration shown in Fig. 4-20.
D. The cover–uncover test for ocular malalignment
After inspecting the eyes in the primary position and through the whole range of movement, do the cover–uncover test (Fig. 4-22).
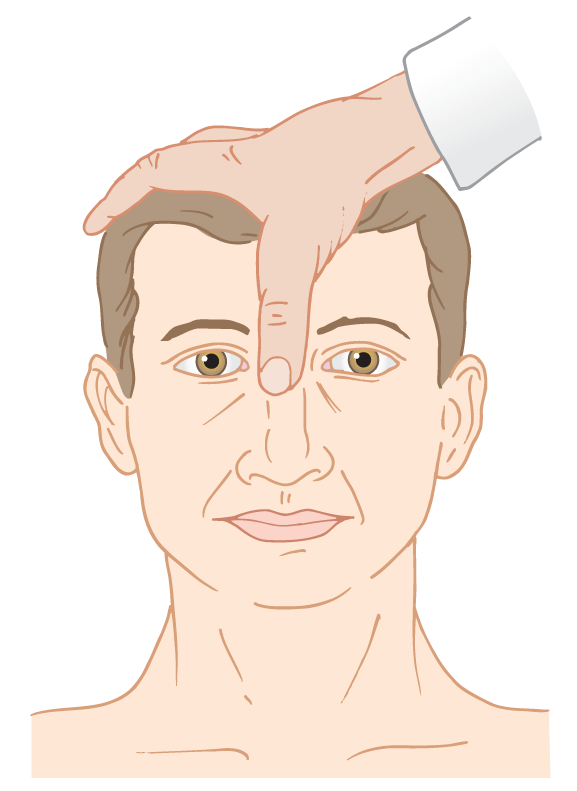
FIGURE 4-22. Resting position of the examiner’s thumb for the cover–uncover test.
1. Place your thumb between the Pt’s eyes, as shown in Fig. 4-22.
2. Instruct the Pt to stare at a distant point. Admonish the Pt to maintain fixation on the distant point, which is essential.
3. Move your thumb first in front of one eye, then back to the bridge of the nose, and then over the other eye. The thumb does not have to occlude all vision, only central, that is, foveal vision. Look for deviation of one or both eyes and for the corneal light reflections as you move the thumb from station to station.
4. Interpretation of the cover–uncover test: Covering one eye requires the other eye to foveate. When both eyes are locked together in fixation, neither eye moves: the Pt has no ocular malalignment. Movement of an eye after occlusion of central vision means a defective alignment lock of the eyes.
E. The heterotropias: naming overt ocular deviations
1. Medical terms for overt ocular malalignments are heterotropia and strabismus. The ophthalmologist speaks of “heterotropia,” and the neurologist speaks of “strabismus.” The layman speaks of “squints” or “cross-eyed” for convergent strabismus or “wall-eyed” for divergent strabismus.
2. Definition of heterotropia: Heterotropia (overt strabismus) is any ocular deviation detected by observing noncorrespondence of the corneal light reflections with the eyes in any position. This is an  operational/
operational/ interpretational definition. Explain.
interpretational definition. Explain.
_________ operational. Heterotropia is defined in terms of the maneuver or operation by which you can identify it. An operational definition states what operations you do, the actual steps and actions required, to personally verify something through your own senses.)
operational. Heterotropia is defined in terms of the maneuver or operation by which you can identify it. An operational definition states what operations you do, the actual steps and actions required, to personally verify something through your own senses.)
a. Suppose we stated that “Heterotropia is any overt deviation of the visual axis of an eye from the fixation point.” This would be an  operational/
operational/ interpretational definition. (
interpretational definition. ( interpretational)
interpretational)
This definition, based on an imaginary “visual axis” is an interpretational definition. It does not state the operations by which the observer may personally discover heterotropia.
b. The physician must clearly distinguish operational from interpretational definitions. Most dictionary definitions uncritically mix operation and interpretation. Suppose you wish to find the length of a meter. Some dictionaries will advise you that a meter is one ten-millionth of the distance between the equator and the poles, measured on a meridian of the Earth. Well, do not try to step that off. That obviously interprets the length of a meter in terms of something else. Try this definition: “A meter is the distance between two transverse lines on a platinum-iridium bar kept at the National Bureau of Standards, when the bar is at 0°C.” The definition implies the operation required to discover the length of a meter: you lay your own bar down beside the meter bar and mark the distance on it. Now that simple operation enables you to derive, verify, and actually experience the length of a meter. In other words, if you do this, you will find out that.
c. As operationally defined by the best test for it, heterotropia means any overt ocular deviation detected by _________
3. The heterotropias are named according to the direction of deviation of the errant eye:
Exotropia: eye deviates outward (laterally).
Esotropia: eye deviates inward (medially).
Hypertropia: eye deviates upward.
Hypotropia: eye deviates downward.
4. To give the full name, designate the right or left eye. Thus, left exotropia means that the left eye deviates  in/
in/ out/
out/ up/
up/ down. (
down. ( out)
out)
5. If both eyes deviate outward, the Pt would have bilateral _________. (exotropia)
6. The Pts shown in Figs. 4-23A to 4-23D fixate straight ahead in each case. In deciding whether the right or left eye is affected, remember that you face the Pt. In most ocular illustrations, the eyes will face you or face downward on the page to simulate the actual circumstance of looking at a Pt.
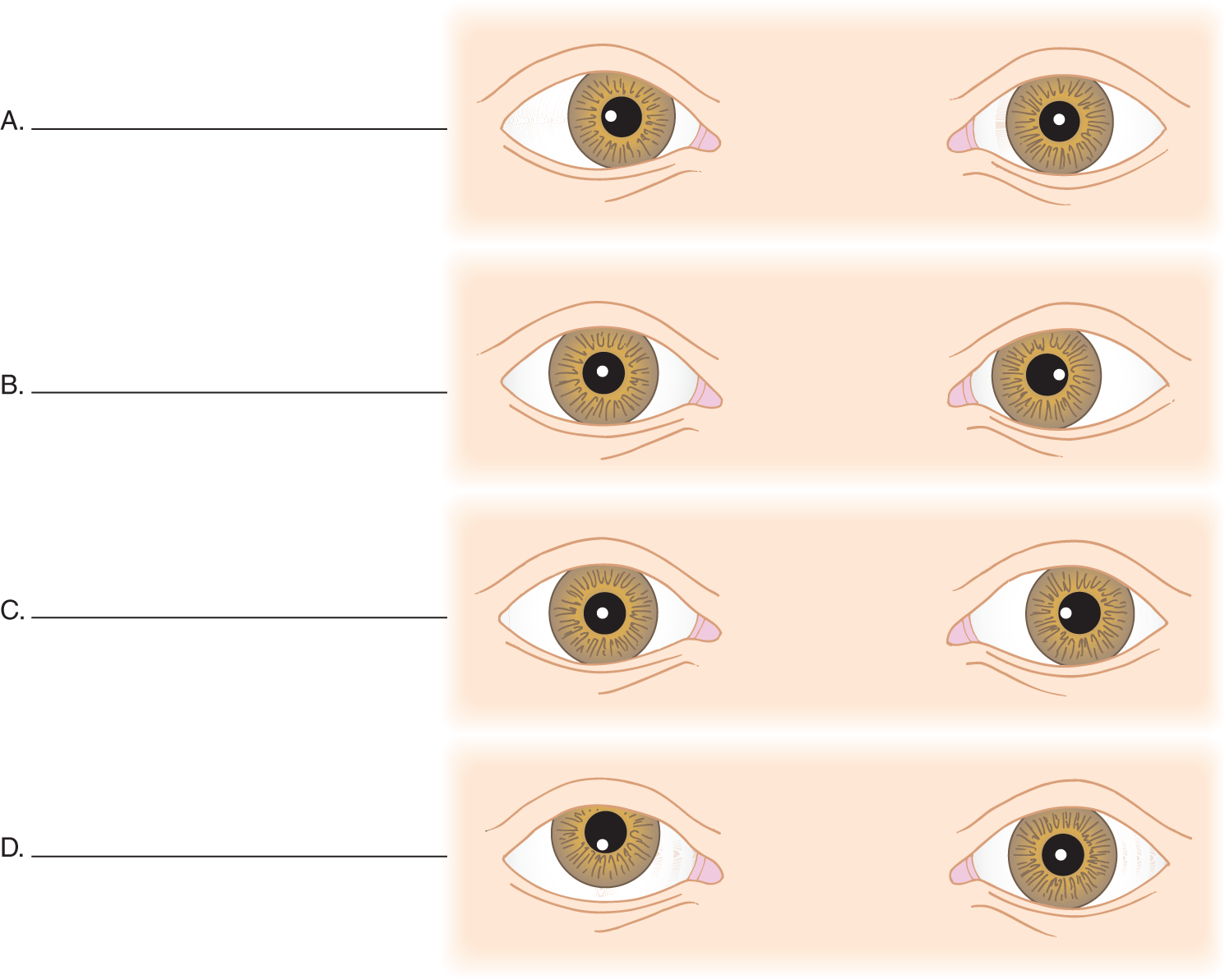
FIGURE 4-23. Location of the corneal light reflections in heterotropia. Write your diagnoses in blanks A to D and designate whether the abnormal eye is right or left.
A. R esotropia
B. L esotropia
C. L exotropia
D. R hypertropia
F. Analysis of the cover–uncover test in monocular heterotropia
1. Start with Fig. 4-24A, step 1 at the bottom of the figure. The Pt was instructed to look straight ahead. Being allowed free vision, the Pt fixates with the left eye, the dominant eye. This Pt appears to have the ocular malalignment called  right/
right/ left/
left/ ____. (
____. ( right esotropia)
right esotropia)
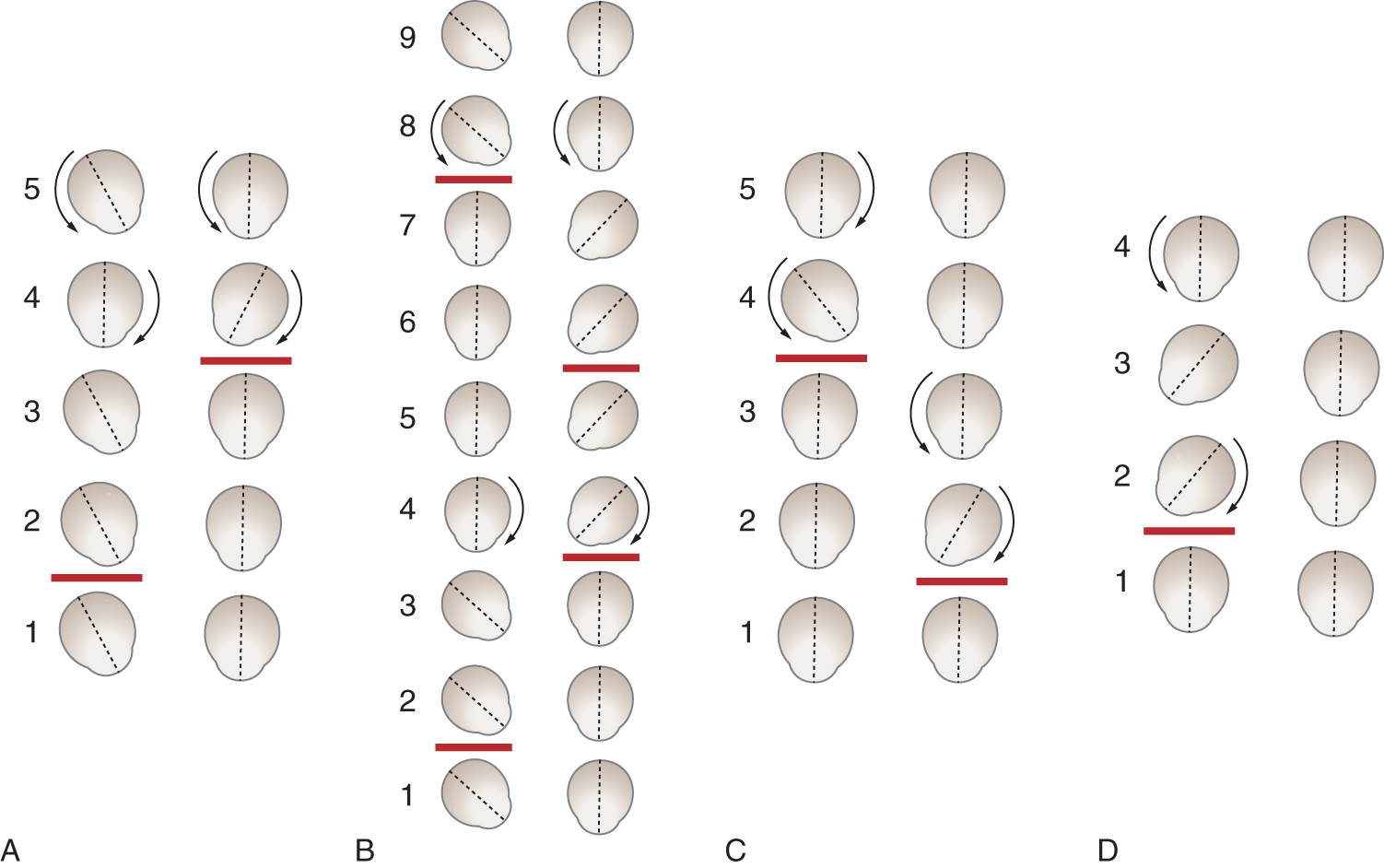
FIGURE 4-24. Results of the cover–uncover test for ocular malalignment. See text for explanation. (Adapted with permission from Strabismus JA. In: Holt L, ed. Pediatric Ophthalmology. Philadelphia, PA: Lea & Febiger; 1964, Chap. 20, 210–259.)
2. In step 2, the Ex’s thumb occludes central vision of the right eye. The ocular alignment of neither eye changes.
3. In step 3, the Ex replaces the thumb on the bridge of the Pt’s nose. The eyes maintain the same angulation of the visual axes.
4. In step 4, the Ex re-instructs the Pt to maintain fixation on the original distant point and covers the Pt’s left eye. The Pt’s right eye then shifts to bring the central light ray onto the fovea, and the left eye rotates inward (as explained later).
5. In step 5, the Ex replaces the thumb on the bridge of the Pt’s nose. The eyes shift to return fixation to the dominant left eye.
6. A Pt with right exotropia instead of esotropia would show a similar sequence of events. If you would like, draw the events of right exotropia alongside Fig. 4-24A, steps 1 to 5. In any event, work through Fig. 4-24A without using the instructions in the text.
G. Analysis of the cover–uncover test in alternating heterotropia
1. Work through Fig. 4-24B. In steps 1 and 2, the Pt ostensibly has the ocular malalignment called  right/
right/ left ____tropia. (
left ____tropia. ( right esotropia)
right esotropia)
2. Subsequent steps in Fig. 4-24B show that the Pt alternates fixation when allowed free vision. In step 1, the Pt fixates with the left eye, and in step 5 the Pt fixates with the right eye. In contrast, Fig. 2-24A shows that the Pt always returns to fixation with the left eye when allowed free vision. Because the right and left eyes of the Pt in Fig. 2-24B alternately deviate inward, the heterotropia is called alternating _________
3. Work through Fig. 4-24B, imagining that the Pt’s eyes deviated out rather than in. This heterotropia would be called _________
H. The cover–uncover test for heterophorias, the latent rather than the overt ocular deviations
1. When a normal person looks at infinity, the visual axes are parallel. The two retinal images “fuse” into one mental image. Binocular vision requires fusion of central vision and develops as the infant matures. Fusion and fixation reflexes operate to keep both eyes “on target” whenever the normal person’s eyes are open.
2. In some Pts, the eyes appear straight during preliminary testing and show normal motility, but upon blocking central vision in one eye, the eye deviates. After removal of the cover, thus re-establishing central vision, the fusion–fixation reflexes immediately realign the eye. Ocular deviations appearing only when central vision is blocked and disappearing when central vision is re-established are heterophorias.
3. An ocular deviation apparent when the Pt is permitted free central vision is called hetero_________
4. The critical operation of the cover–uncover test is to _________
5. Which maneuver must always restore ocular alignment to distinguish heterophoria from heterotropia? _________
6. Inward deviation, or adduction, of the eye only during occlusion of central vision is called  exophoria/
exophoria/ hyperphoria/
hyperphoria/ esophoria. (
esophoria. ( esophoria)
esophoria)
7. Overt in-turning of an eye when the Pt has free central vision is called _________
8. Abduction of an eye only during occlusion of central vision is called _________
9. Upward deviation of an eye only during occlusion of central vision is called _________
10. Fig. 4-24C depicts the cover–uncover test in heterophoria. Work through it. The latent deviation in Fig. 4-24C is called alternating _________
a. Suppose in step 5 of Fig. 4-24C that the right eye had not returned to proper alignment on removal of the cover. Such an overt inward deviation, not corrected all of the time by central vision, would be called  right/
right/ left esotropia. (
left esotropia. ( right)
right)
b. If one of the Pt’s eyes aligns sometimes after removal of the cover, but does not align at other times, the condition is called  intermittent/
intermittent/ alternating heterotropia. (
alternating heterotropia. ( intermittent)
intermittent)
11. Complete the definitions in 11a and 11b by stating the clinical maneuvers that disclose heterophoria and heterotropia:
a. Heterotropia is an  overt/
overt/ latent ocular deviation as detected by inspection for _________
latent ocular deviation as detected by inspection for _________ overt)
overt)
Noncorresponding corneal light reflections and abnormal relation of the corneal limbus to the eyelid margins.
b. Heterophoria is an  overt/
overt/ latent ocular deviation detected by _________
latent ocular deviation detected by _________ latent)
latent)
Seeing the eye shift when its central vision is blocked during the cover–uncover test and returning to alignment with restoration of central vision.
12. Now try to name the abnormality shown in Fig. 4-24D. Pay particular attention to step 3. Because the Pt starts and finishes with apparently straight eyes, the deviation of one eye is only intermittent. Therefore, the abnormality in Fig. 4-24D is called _________
13. The abnormality in Fig. 4-24D is a tropia rather than a phoria because _________
I. Clinical classification of heterotropia
1. To determine the cause of heterotropia, try to classify it into one of two types:
a. The paralytic type, caused by a neuromuscular lesion.
b. The nonparalytic type, usually caused by lesions that impair central vision in one eye and therefore impair fixation: refractive errors, opacification of the cornea or lens (refracting media), or macular lesions.
2. Effect of paralytic heterotropia caused by nerve or muscle lesions on yoke muscles.
a. After paresis or paralysis of an ocular muscle, the intact muscles act unopposed. Hence, the eye deviates  away from/
away from/ toward the direction of pull of the afflicted muscle. (
toward the direction of pull of the afflicted muscle. ( away from)
away from)
b. When the Pt looks in the direction of pull of the afflicted muscle, the normal eye moves more than the afflicted eye. Hence, the degree of heterotropia and diplopia  increases/
increases/ decreases when the Pt looks in the direction of action of the afflicted muscle. (
decreases when the Pt looks in the direction of action of the afflicted muscle. ( increases)
increases)
c. When turning in the direction of pull of a weak muscle, the eye rotates too little, whereas the normal eye may rotate too far as the brain strives to move the laggard eye. With a lateral rectus paralysis on the right, the Pt’s  right/
right/ left eye would adduct too far when the Pt looks to the right. Explain this result by Hering law.
left eye would adduct too far when the Pt looks to the right. Explain this result by Hering law.
_________
_________ left; see next frame)
left; see next frame)
d. Hering law states that the nervous system stimulates the yoke muscles equally. If a muscle is weak, the Pt automatically overstimulates in an attempt to rotate the afflicted eye. The normal yoke muscle receives the same excessive stimulus and contracts too strongly.
3. Use of the cover–uncover test to analyze neuromuscular heterotropia. Study Richard Scobee’s lucid description to understand primary and secondary deviations of the eyes when the paretic eye and the sound eye are alternately covered or uncovered.
Primary deviation is the deviation of the eye with the paretic muscle when the sound eye is fixing. Secondary deviation is the deviation of the sound eye when the eye with the paretic muscle is fixing. In paresis, secondary deviation is greater than primary deviation.
As an example of primary deviation, suppose the left lateral rectus is paretic, right eye dominant, and the Pt fixes upon some object straight ahead with the right eye. The right medial rectus and the right lateral rectus are normal muscles and require but a normal innervation to maintain fixation with the right eye. According to Hering law, similar normal innervations go to the yoke muscles of the right lateral rectus and the right medial rectus—to the left medial rectus and the left lateral rectus. The left lateral rectus is paretic and responds in subnormal fashion to normal stimuli; the left medial rectus is normal and thus not properly opposed by the subnormal tonus of its paretic antagonist. The left medial rectus will, therefore, seem to overact since it will pull the left eye inward toward the nose in adduction. The deviation produced is small but definite and is a left esotropia. This is deviation of the paretic eye with the sound eye fixing—primary deviation.
As an example of secondary deviation, suppose the left lateral rectus is paretic, left eye dominant, and the Pt fixes upon some object straight ahead with the dominant left eye. The left lateral rectus, in order to perform its usual functions, must be excessively innervated because it is paretic; its yoke muscle, the right medial rectus, receives the same excessive innervation according to Hering law. The right medial rectus is a normal muscle receiving an excessive innervation and it makes an excessive response, pulling the right eye well inward in adduction. This is a deviation of the sound eye with the paretic eye’s fixing—secondary deviation. In paresis, secondary deviation is greater than primary deviation and the reason should now be obvious.
4. The primary and secondary deviations exemplify this law: The fixating eye, the one that foveates, determines the amount of innervation to both eyes. This is a straightforward application of a previous law stated in this chapter, namely _________
To encourage the weak muscle to act when fixating, the central nervous system (CNS) sends out a strong stimulus that only the intact eye responds fully to.
5. Effect of neuromuscular (paralytic) heterotropia on head position
a. To avoid diplopia, the Pt tends to compensate for a paretic eye muscle by turning or tilting the head. A face turn implies a horizontally acting muscle palsy, chin elevation or depression implies a vertically acting muscle palsy, and a head tilt implies a torsional acting muscle palsy.
b. The Pt moves the head toward the action of the weak muscle. To avoid diplopia, a Pt with a right lateral rectus palsy would tend to keep the head turned to the right. Then the left eye abducts, lining up better with the in-turned right eye.
c. With a right superior oblique palsy, the Pt has weakness of  intorsion/
intorsion/ extorsion of the right eye, an action for which the superior oblique is mainly responsible. (
extorsion of the right eye, an action for which the superior oblique is mainly responsible. ( intorsion)
intorsion)
d. The unopposed action of the extortors would cause extorsion of the eye. In compensation, therefore, the Pt with a right superior oblique palsy tilts his or her head to the  right/
right/ left to prevent diplopia. (
left to prevent diplopia. ( left (If the answer is unclear, review Figs. 4-12 and 4-14.))
left (If the answer is unclear, review Figs. 4-12 and 4-14.))
e. A persistent head tilt or turn is called torticollis. Oblique muscle palsy is only one of its many causes. With a unilateral acute or acquired superior oblique muscle palsy, the Pt will tilt the head to the side opposite the paralytic muscle, turn the face to the same side, and keep the chin depressed—actions all designed to minimize the use of the superior oblique muscle (Brazis et al, In Press. 2016).
6. Effect of neuromuscular heterotropia on vision in infants: suppression amblyopia.
a. Infants with heterotropia learn to suppress the image from the errant eye, a condition called suppression amblyopia or amblyopia ex anopsia. If suppression continues for the first years of life, the deviant eye may become completely blind, even though the retina and visual pathways remain structurally intact. The strength of the suppressive forces that rid the visual image of confusing elements may prevent the child from ever recovering vision.
b. Suppression amblyopia is a preventable cause of monocular blindness, treated by the simple expedient of placing a patch intermittently over the sound eye to require the Pt to use the errant eye.
c. Suppression amblyopia occurs not only with heterotropia, but also with many monocular disorders of retinal image formation—refractive errors, opacification of the refracting media, or retinal lesions.
d. Never neglect ocular deviations or other impediments to vision because of a naive expectation that the infant will simply “grow out” of it. The infant may grow more and more “into” it. A complete eye examination of every infant will disclose this preventable cause of blindness.
J. Nonparalytic or concomitant heterotropia versus paralytic heterotropia
1. Of the two varieties of eye deviation, a concomitant heterotropia has the same amount of deviation in both eyes in all directions of gaze, but in nonconcomitant heterotropia, the angle of deviation changes with the position of the eyes.
2. With muscular paresis or paralysis, the eyes do not move concomitantly; one eye moves more or less than the other. Hence, we can classify paralytic heterotropia as nonconcomitant. In concomitant heterotropia or nonparalytic heterotropia, the eyes display the same degree of malalignment in all positions when both eyes are open, but each eye has vision and a normal range of movement (ductions) at monocular testing.
3. The Ex should complete the cover–uncover test in the nine cardinal directions of gaze (Fig. 4-20). If the eyes maintain the same degree of deviation in all directions of gaze, the heterotropia is  concomitant/
concomitant/ nonconcomitant. (
nonconcomitant. ( concomitant)
concomitant)
4. Concomitant heterotropia may be intermittent, but when present, the deviation is the same in all directions of gaze. What happens to the angulation of the eyes in heterotropia due to neuromuscular lesions when the eyes move? _________
5. Concomitant heterotropia usually results from a disturbance in image formation in one macula—cloudiness of the cornea, a severe refractive error, a cataract, or a macular lesion. It seems as if the retina establishes a new macula, off center from the true macula, and then the visual axis aligns on the new macula.
6. The Pt alternates in fixating with the normal eye and the abnormal one. The Pt learns to suppress vision from whichever eye that is not in use at the moment for fixation, much as you can learn to use a monocular microscope or an ophthalmoscope with both eyes open. Thus, the Pt alternately fixes with one eye and suppresses vision from the other eye. When fixation alternates between the two eyes, suppression amblyopia does not occur.
7. The clinical characteristics of concomitant heterotropia:
a. The deviation of the eyes is  the same/
the same/ different for the primary position and in all directions of gaze. (
different for the primary position and in all directions of gaze. ( the same)
the same)
b. In contrast to nonconcomitant heterotropia, the primary and secondary deviations disclosed by the cover–uncover test are  equal/
equal/ unequal in concomitant heterotropia. (
unequal in concomitant heterotropia. ( equal)
equal)
If they were not equal at all times, the Pt would have nonconcomitant heterotropia.
c. When either eye fixates alone, it shows a full range of motility. None of the individual muscles is paralyzed.
8. The term paralytic heterotropia is essentially synonymous with  concomitant/
concomitant/ nonconcomitant heterotropia. (
nonconcomitant heterotropia. ( nonconcomitant)
nonconcomitant)
9. The term nonparalytic heterotropia is essentially synonymous with _________
10. Complete Table 4-2 by making a check mark in the proper column.
TABLE 4-2 • Differential Diagnosis of Paralytic and Non-Paralytic Heterotropia*
Clinical characteristic |
Paralytic (non-concomitant) |
Non-paralytic (concomitant) |
Ocular deviation changes with eye movement |
||
Full movement when each eye is tested after covering the other |
||
Secondary deviation is greater than primary deviation |
||
Secondary and primary deviations are equal |
||
Frequently has opacity or severe refractive error in one eye |
||
Has diplopia if heterotropia occurs after young age |
||
Often has compensatory head turning or tilting |
||
*These rules apply to most patients. With longstanding heterotropia, fibrosis, contractures, and eccentric fixation or fusional problems at the cortical level may confound the diagnosis. |
||
P |
N-P |
✓ |
|
✓ |
|
✓ |
|
✓ |
|
✓ |
|
✓ |
|
✓ |
K. The laws of diplopia and the clinical analysis of diplopia
1. Repeat the canthal compression experiment and obtain diplopia with the finger vertical. Move the finger to the right and to the left while studying the distance between the true and false images. Identify the false image by its haziness. This is one law of diplopia: The aberrant or “false” image is always hazier than the “true” image.
a. If the false image projects to the right of the target finger (from weakness of the right lateral rectus muscle), the distance between the images increases as you move the target finger to the  left/
left/ right side (see Fig. 4-25). (
right side (see Fig. 4-25). ( right)
right)
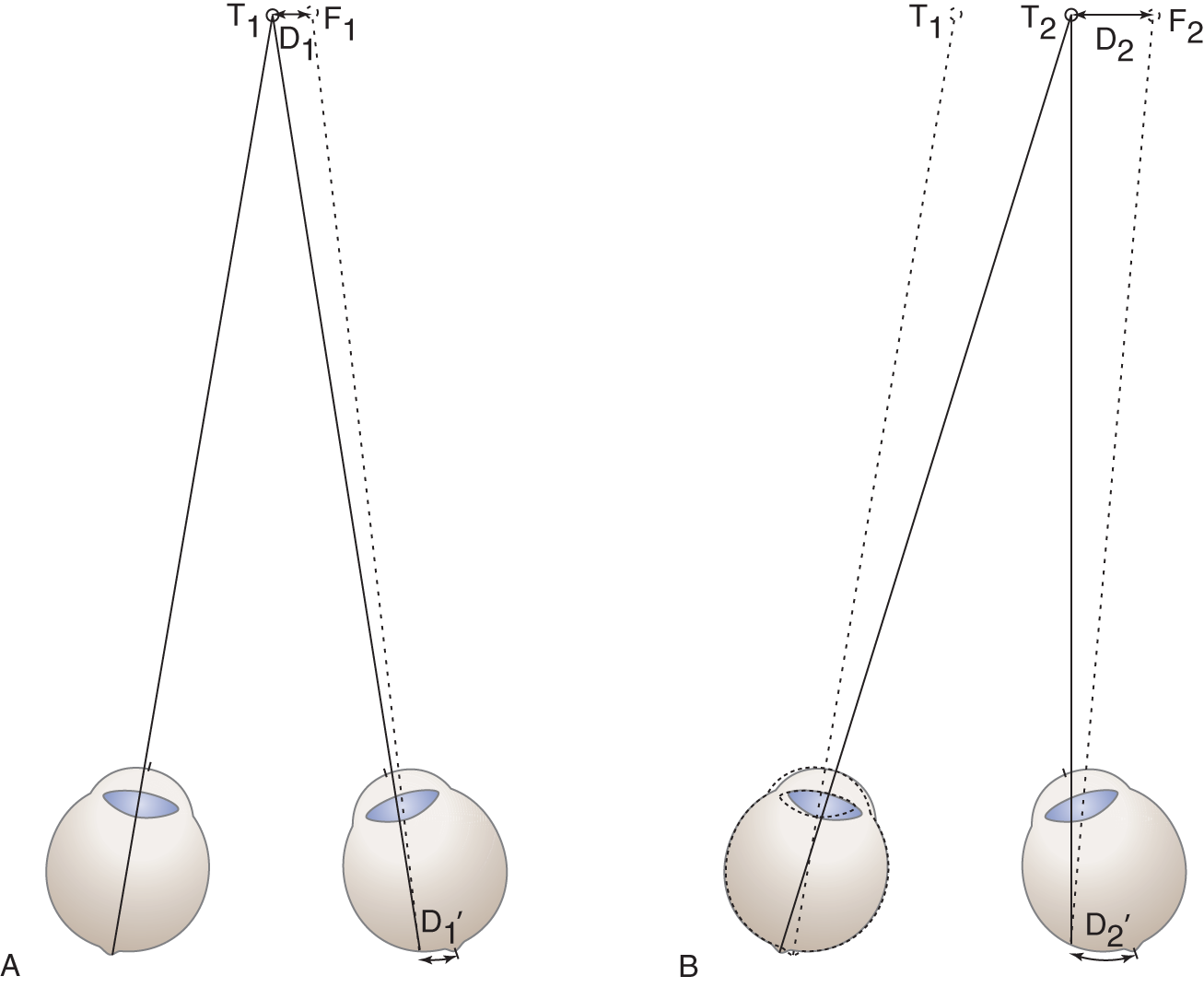
FIGURE 4-25. Illustration of a law of diplopia: the distance between the true and false images increases when the Pt looks in the direction of projection of the false image. The target has moved from site T1 to site T2, but the paralytic right eye has not moved. D1 = distance 1; D2 = distance 2; F1 = false image; T1 = true image.
b. If the false image projects to the left, the distance between the images increases as you move the target finger to the  left/
left/ right side. (
right side. ( left)
left)
c. If your eyes follow the images too far laterally, one disappears. Can you discover an explanation (look for the simplest one)?
The nose blocks the light rays from entering one eye. The brain no longer receives two confusing images.
2. As you move your finger away from the midpoint, the distance between the true and false images  increases/
increases/ decreases/
decreases/ stays the same. (
stays the same. ( increases. Go to the next frame for the explanation, unless you would like to try to work it out yourself.)
increases. Go to the next frame for the explanation, unless you would like to try to work it out yourself.)
3. Explanation for the increasing distance between the diplopic images:
a. In Fig. 4-25A, the left eye, aligned on target, receives the real image on its fovea. The mind projects the visual image back to the true target position (T1). The deviated right eye receives the real image on the nasal side of the fovea. The mind projects the visual image to the right of the true target position (F1).
b. In Fig. 4-25B, the mobile left eye follows the target to the right (T2). The paralytic right eye remains stuck in its original position, and, as the target moves rightward, the real image moves leftward (nasally) on the retina. The mind projects the visual image more and more rightward. Thus, D2 > D1.
4. No matter which way the false image deviates, it moves away from the true image. The true image remains centered on target. This is another law of diplopia: The false image appears peripheral to the true image.
5. If the false image is to the right of the true image, as in Fig. 4-25A, the eye is deviated to the left (or has not rotated sufficiently to the right). The false image projects in the  same/
same/ opposite direction of the eye deviation. (
opposite direction of the eye deviation. ( opposite)
opposite)
a. If the false image projects above the true image, the afflicted eye deviates  upward/
upward/ downward. (
downward. ( downward)
downward)
b. If the false image is to the left, the afflicted eye is deviated to the  right/
right/ left. (
left. ( right)
right)
6. This is another law of diplopia: the false image projects in the  same/
same/ opposite direction as the direction of eye deviation. (
opposite direction as the direction of eye deviation. ( opposite)
opposite)
7. In Fig. 4-25, with projection of the false image to the right, the right eye has failed to abduct to center its visual axis on target. Thus, the diagram depicts paralysis of the _________
8. This is another diplopia law: The false image projects  toward/
toward/ away from the normal direction of pull of the paretic muscle. (
away from the normal direction of pull of the paretic muscle. ( toward)
toward)
9. Thus, when the Pt looks in the direction of pull of the paretic muscle or the visual target moves in that direction, the distance between the diplopic images  increases/
increases/ decreases. (
decreases. ( increases)
increases)
10. Summarize the four laws of diplopia with respect to image projection:
a. The law stating whether the true or false image is the sharpest:
_________
b. The law of peripheral projection:
_________
c. The law of direction of projection with respect to eye deviation:
_________
d. The law relating the projection of the false image in relation to the pull of the paretic muscle:
_________
11. In summary, the use of the corneal light reflection test and the laws of diplopia permit you to diagnose the faulty muscle. Do not memorize these laws. Recover them whenever needed by pressing on your lateral canthus, your Aladdin’s lamp, and thinking through the foregoing exercises, particularly Fig. 4-25.
L. A summary of the clinical tests for diplopia
1. Observe the corneal light reflections: Locate them when the eyes look straight ahead and when held in the various directions of gaze (Fig. 4-20).
2. Identify the position of maximum diplopia: As you move your finger for examining light through all fields of gaze, have the Pt report when the two images are maximally separated. A red glass placed over one eye (by convention placed over the right eye) helps to keep track of the two images during motility testing. The point of maximum separation identifies the action of the weak muscle.
3. Identify the eye which produces the false image: The eye that produces the false image has the faulty muscle. The false image is the peripheral image. Identify it by occluding vision alternately in the two eyes. After occlusion of the normal eye, the sharp, central image disappears. After occlusion of the abnormal eye, the hazy, peripheral image disappears.
4. Reason out the muscle responsible for the deficient ocular action (Fig. 4-18 and Tables 4-1 and 4-4).
M. Analyze these patients
1. This Pt complains of double vision when looking to the left. Gazing to the left causes the greatest separation of the images.
a. The muscle pairs responsible for left lateral gaze are the _________
b. On occlusion of the right eye, the central image (true image) disappears. On occlusion of the left eye, the peripheral image (false image) disappears. Therefore, the afflicted eye is the  left/
left/ right eye and the afflicted muscle is the
right eye and the afflicted muscle is the  right/
right/ left _________
left _________ left;
left;  left; lateral rectus)
left; lateral rectus)
2. The next Pt complains of double vision when looking up. The images separate greatest when the Pt looks up and to the left.
a. The most important muscle for this action of the left eye is the _________
b. On occlusion of the right eye, the central image disappears. On occlusion of the left eye, the peripheral image disappears. Therefore, the afflicted eye is the  right/
right/ left and the afflicted muscle is the
left and the afflicted muscle is the  right/
right/ left _________
left _________ left;
left;  left; superior rectus)
left; superior rectus)
N. Localizing the lesion by thinking along the course of the ocular motor nerve
1. The lesion that interrupts an ocular motor nerve or any nerve causes different signs if it affects the central or peripheral course. Always start at the nucleus of origin of the nerve and think through to its termination.
2. A central lesion will usually also affect long tracts:
a. A lesion of cranial nerve (CrN) III in the midbrain will cause ataxia if the dentatothalamic tract is interrupted, contralateral tremor if the lesion also affects the region around the red nucleus, disturbances in vertical gaze if the lesion is dorsomedial to the red nucleus (Chapter 5), or hemiplegia if the lesion affects the midbrain basis (Fig. 2-18).
b. A lesion of CrN VI in the basis pontis will cause contralateral hemiplegia because that is where CrN VI comes into conjunction with the pyramidal tract (Fig. 2-16).
3. Peripherally each nerve generally comes into conjunction with another nerve or structure, and the lesion will affect more than one structure.
a. In the region of the cavernous sinus, CrNs III, IV, V, and VI and the carotid sympathetic nerve are related in different ways (Section VIII).
b. Within the orbit, a lesion will cause a different set of signs involving several of the same nerves. Brazis et al (2016) succinctly review the syndromes encountered by lesions along the course of the ocular motor nerves.
4. Remember the many diseases that can cause diplopia and ocular palsies, but do not directly interrupt ocular motor nerves: myasthenia gravis, hyperthyroidism, botulism, diabetes, arteritides, aneurysms, inflammation, and primary or metastatic neoplasms. Therefore, the “thinking through” process must also include the neuromyal junction, the muscles themselves, the adjacent anatomical structures, and the whole person: systemic disease.
BIBLIOGRAPHY · General References
Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins, Wolters Kluwer Health. In Press, 2016.
Shaunak S, O’Sullivan E, Kennard C. Eye movements. J Neurol Neurosurg Psychiatry. 1995;59:115–125.
Clinical Tests for Ocular Malalignment and the Range of Eye Movements
Helveston E. A two-step test for diagnosing paresis of a single vertically acting extraocular muscle. Am J Ophthalmol. 1967;64:914–915.
Keane JR. Fourth nerve palsy: historical review and study of 215 inpatients. Neurology. 1993;43: 2439–2443.
Von Noorden GK. Binocular Vision and Ocular Motility. 5th ed. St. Louis: Mosby; 1996.
IV. REFRACTION AND ACCOMMODATION
A. Refraction by negative and positive lenses
1. To understand lenses, start with the law of the prism: A prism bends light rays toward its base (Fig. 4-26A).
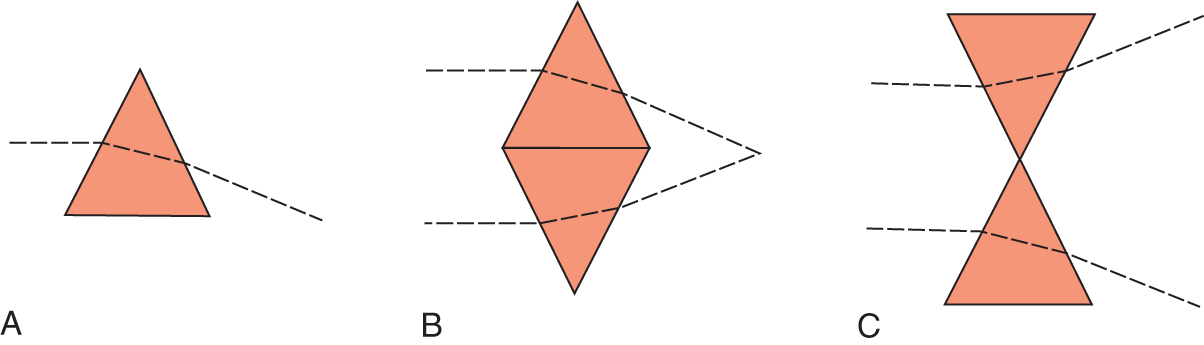
FIGURE 4-26. The law of the prism states that a prism refracts light toward its base. Two prisms base to base make a converging, positive lens or, if apex to apex a diverging, a negative lens.
a. Two prisms, placed base in, form a positive or converging lens (Fig. 4-26B).
b. Two prisms placed base out form a negative or diverging lens (Fig. 4-26C).
c. Rounding of the sides of the prism into the familiar lens shape reduces chromatic and spherical aberrations.
2. In bending light rays, a prism or lens bends violet more than red, thus causing chromatic aberration because the rays do not fall on one focal point but are spread out. Any defect in the curvature of the lens causes spherical aberration (astigmatism).
3. A pinhole aperture screens out the more peripheral light rays, which must undergo more refraction than the central rays, thus reducing chromatic and spherical aberrations (Fig. 4-27D).
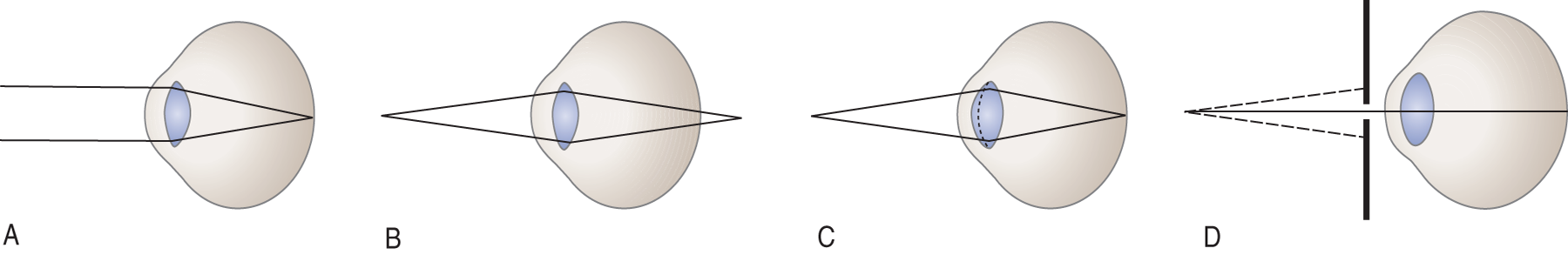
FIGURE 4-27. Schematic cross-sections of the eye to show the focal point of light rays in various conditions of refraction. (A) Emmetropic eye. Parallel rays from a distant object focus on the retina. (B) Emmetropic eye has not adjusted to accommodate for near vision. The light rays from the near point diverge as they travel to the eye; hence, they focus behind the retina. (C) Emmetropic eye accommodated for near vision. The lens has thickened, increasing its power of refraction. The divergent rays now focus on, rather than behind, the retina. (D) Pinhole effect. The pinhole allows the central nonrefracted rays to pass to the retina, but blocks the more peripheral rays.
B. Light refraction by the normal eye
The refracting media of the eye includes the cornea and lens. Learn Figs. 4-27A to 4-27D.
C. The accommodation reflex
1. Accommodation for near vision requires three muscles to complete three actions:
a. Convergence: medial recti (skeletal)
b. Pupilloconstriction: pupilloconstrictor muscle of the iris (smooth muscle, parasympathetic)
c. Lens thickening: ciliary muscle (smooth muscle, parasympathetic)
2. Functions of the three actions:
a. Convergence by the medial rectus muscles aims the visual axes onto the near fixation point (Fig. 4-3).
b. Pupilloconstriction by the pupilloconstrictor muscle of the iris causes cormiosis (pinhole effect; Fig. 4-27D), reducing spherical and chromatic aberrations.
c. Lens thickening increases its ability to refract the more divergent rays coming from the near fixation point. Contraction of the ciliary muscle, a sphincter, relaxes the suspensory ligament of the lens, allowing it to thicken by its natural elasticity.
3. Thus, during the accommodation reflex for near vision, three distinct events occur: The visual axes _________
4. Although volition initiates the act of looking at a near target, neural mechanisms lock the three events of accommodation into a single accommodation reflex. Thus, whenever a person voluntarily converges the eyes, neural circuits automatically cause pupilloconstriction and lens thickening. Complete Table 4-3.
TABLE 4-3 • The Accommodation Reflex and the Muscles Responsible
List the three events of the accommodation reflex |
List the responsible muscles |
(skeletal) |
|
(smooth) |
|
(smooth) |
(convergence; medial recti cormiosis; pupilloconstrictor muscle lens thickening; ciliary muscle)
D. Myopia and hyperopia
1. Learn Fig. 4-28.
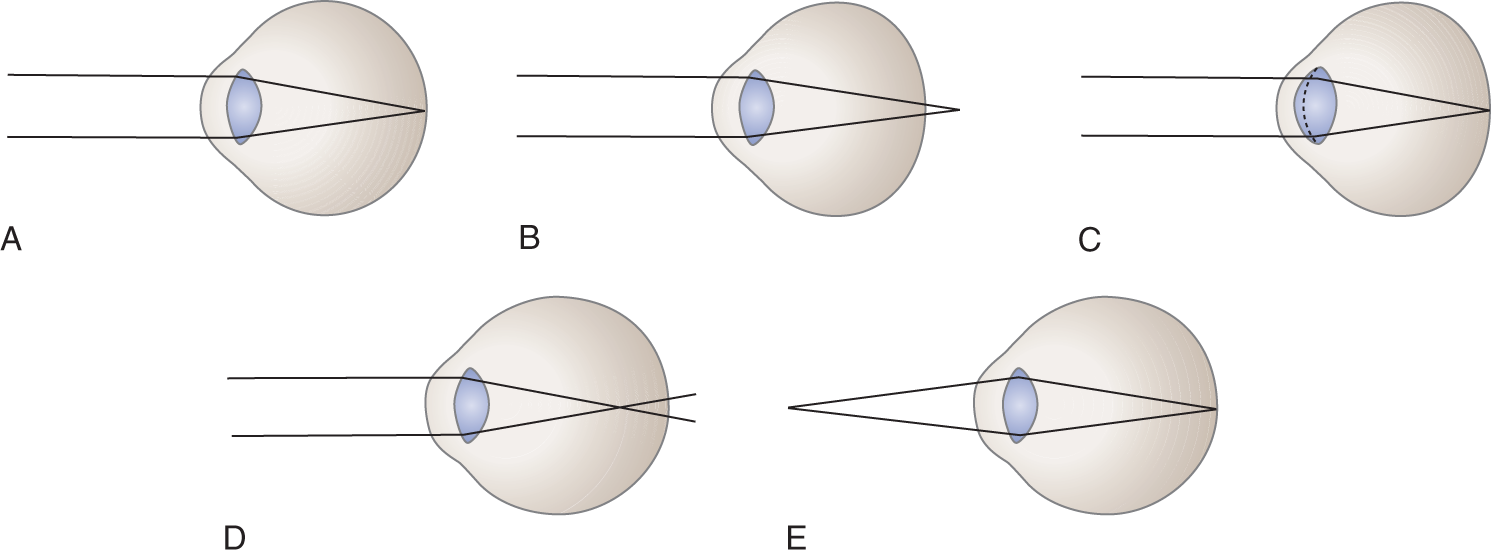
FIGURE 4-28. Focal point of light rays relative to the anteroposterior diameter and refractive power of the eye. (A) Emmetropia. The refracting power and the diameter of the normal eye match. Parallel rays from a distant source focus on the retina without accommodation. Divergent rays from a near source will require lens thickening to focus on the retina. (B) Hyperopia. The diameter of the eye is too short relative to its refracting power. Parallel rays focus behind the retina. (C) Hyperopia with accommodation. The lens of the hyperopic eye must thicken, thus increasing its focusing power, to bring parallel rays to focus on the retina. When looking at a near object, the hyperopic person has no accommodation reserve. (D) Myopia. The diameter of the eye is too long relative to its refracting power. Parallel rays focus in front of the retina. (E) Myopic eye focusing on near object. Divergent rays from the near object focus properly on the retina with little or no accommodation.
2. A person with sharp vision for objects that are far away and close is  emmetropic/
emmetropic/ myopic/
myopic/ hyperopic. (
hyperopic. ( emmetropic)
emmetropic)
3. For far vision, the emmetropic person’s muscles of accommodation are  active/
active/ relaxed. (
relaxed. ( relaxed)
relaxed)
4. A person with sharp vision for far objects, but blurred vision for close objects, is called farsighted. The technical term for farsightedness is  emmetropia/
emmetropia/ myopia/
myopia/ hyperopia. (
hyperopia. ( hyperopia)
hyperopia)
5. The hyperopic eye focuses parallel rays  behind/
behind/ in front of/
in front of/ on the retina. (
on the retina. ( behind (Fig. 4-28B))
behind (Fig. 4-28B))
a. The hyperopic Pt requires some activity of the accommodation reflex to thicken the lens  only when viewing far objects/
only when viewing far objects/ only when viewing close objects/
only when viewing close objects/ when looking at close and far objects. (
when looking at close and far objects. ( when looking at close and far objects)
when looking at close and far objects)
b. Normally, however, the accommodation reflex should act only during near vision. The hyperopic Pt requires some degree of accommodation at all times to bring the focal point forward onto the retina.
6. A person with blurred vision for distant objects but sharp vision for near objects is nearsighted. The technical term for nearsightedness is  emmetropia/
emmetropia/ myopia/
myopia/ hyperopia. (
hyperopia. ( myopia)
myopia)
a. The myopic eye focuses parallel rays from far objects  in front of/
in front of/ on/
on/ behind the retina. (
behind the retina. ( in front of)
in front of)
b. Which of the three events of the accommodation reflex actually work against the myopic Pt who is attempting to look at a near object? Explain.
_________
_________
7. On scrap paper, draw three eyeballs and show the focal points of parallel rays in emmetropia, hyperopia, and myopia. Compare with Figs. 4-28A, 4-28B, and 4-28D.
E. Relation of refractive errors to heterotropia and heterophoria
1. During the first months of life, infants must develop binocular fixation and fuse the images from the two eyes. The infant’s eyeball is too short relative to its refracting power. With maturation, the eyeball expands.
2. With the eyeballs too short in relation to the focal point of the lens, the infant is basically  myopic/
myopic/ emmetropic/
emmetropic/ hyperopic. (
hyperopic. ( Hyperopic. However, the smallness of the eyeball means that the infant lacks sharp vision for far objects.)
Hyperopic. However, the smallness of the eyeball means that the infant lacks sharp vision for far objects.)
3. As the eyeball increases in diameter with maturation, the hyperopia tends to change to emmetropia. If the child is more nearly emmetropic at birth, instead of hyperopic, he/she would become _________
4. Because of the small diameter of the eyeball relative to the focusing power of the lens, infants tend to keep their lenses thickened. In other words, they tend to accommodate all of the time. Detailed inspection of near objects places extra demands on the accommodation mechanism of the infant’s eyes. The need for accommodation may overcome the hyperopic child’s capacity for it.
a. Because one of the accommodation mechanisms is convergence of the eyes, the hyperopic child at first will show only a latent tendency to crossing of his/her eyes, that is,  esotropia/
esotropia/ esophoria/
esophoria/ exotropia/
exotropia/ exophoria. (
exophoria. ( esophoria)
esophoria)
b. With severe hyperopia, the esophoria may convert to an overt internal deviation of an eye, which is called _________
c. Thus, refractive errors or neuromuscular lesions may cause crossed eyes. Two eyelid anomalies in children may give a false impression of crossed eyes because the medial margin of the limbus appears to be too close to the medial eyelid margins. Name these two anomalies. (Dystopic canthi and epicanthal folds (Fig. 1-6))
5. Consider the infant who will become myopic at maturity. As his eyeball enlarges with age, he becomes  more/
more/ less myopic. Therefore, the nervous system adjusts by reducing accommodation. (
less myopic. Therefore, the nervous system adjusts by reducing accommodation. ( more)
more)
a. With an underactive accommodation mechanism, the child’s eyes would tend to  drift apart/
drift apart/ converge too much. (
converge too much. ( drift apart)
drift apart)
b. At first the eyes might show only a latent tendency to drift apart, which would be called _________
6. Tropias and phorias commonly accompany refractive errors.
a. Esophoria or esotropia in a child would raise the suspicion of a refractive error called  myopia/
myopia/ emmetropia/
emmetropia/ hyperopia. (
hyperopia. ( hyperopia)
hyperopia)
b. Exophoria or exotropia in a child would raise the suspicion of  myopia/
myopia/ emmetropia/
emmetropia/ hyperopia. (
hyperopia. ( myopia)
myopia)
7. Which child would experience increasing inability to read the chalkboard at school, requiring differentiation of neurologic and ophthalmologic causes for blurred vision, the  myope or
myope or  hyperope? (
hyperope? ( myope)
myope)
F. Presbyopia, blurred vision, myopia, and hyperopia
1. At the age of approximately 42 years, normal adults experience blurred vision when they try to read newsprint or look at near objects. The differential diagnosis then involves a neurologic versus an ophthalmologic disorder.
2. Because of aging, the lens loses its elasticity. It will no longer thicken to increase its refractive power during accommodation, a condition called presbyopia.
a. Who would suffer blurred near vision first and foremost from presbyopia, the  hyperope or the
hyperope or the  myope? Explain.
myope? Explain.
_________ hyperope. The presbyopic hyperope suffers first and foremost from blurred near vision, because the hyperope is already straining the accommodation mechanism. Any loss of elasticity will reduce refraction and thus blur close objects. The myope does not need much accommodation and therefore does not suffer much when it fails.)
hyperope. The presbyopic hyperope suffers first and foremost from blurred near vision, because the hyperope is already straining the accommodation mechanism. Any loss of elasticity will reduce refraction and thus blur close objects. The myope does not need much accommodation and therefore does not suffer much when it fails.)
3. Would placing a pinhole in front of the eye of the presbyopic hyperope improve near vision and help differentiate the visual blurring from presbyopia from blurring due to a lesion of the macula or optic nerve?  Yes/
Yes/ No. Explain.
No. Explain.
_________ Yes. A pinhole will block off the more peripheral rays from the near object, thus allowing only the central rays to reach the retina. The pinhole acts as a tiny pupil. The pinhole eliminates the need to increase refraction by lens thickening. Hence, restoration of visual acuity by the pinhole establishes a disorder of refraction, not a retinal or optic nerve lesion.)
Yes. A pinhole will block off the more peripheral rays from the near object, thus allowing only the central rays to reach the retina. The pinhole acts as a tiny pupil. The pinhole eliminates the need to increase refraction by lens thickening. Hence, restoration of visual acuity by the pinhole establishes a disorder of refraction, not a retinal or optic nerve lesion.)
4. The parallax test for positive or negative corrective lenses
a. The parallax test provides a quick way to test whether the Pt’s glasses correct for hyperopia or myopia. For the parallax test, hold the glasses over any vertical line, about a foot away, and slowly move the glasses to the right and left alternately.
b. With a divergent (negative) lens, the line will appear to move in the direction that you move the glasses. Myopia requires a divergent or negative lens to move the focal point  backward/
backward/ forward onto the retina. (
forward onto the retina. ( backward (remember the law of the prism, Fig. 4-26).)
backward (remember the law of the prism, Fig. 4-26).)
c. With a convergent (positive) lens, the line will appear to move in the opposite direction to the movement of the glasses. Hyperopia requires a convergent or positive lens to bring the focal point forward onto the retina.
d. In summary:
i. If the lens corrects for myopia, the image will appear to move in the direction that you moved the eyeglasses.
ii. If the lens corrects for hyperopia, the image will appear to move in the opposite direction.
5. If you understand all of this, explain why a presbyopic myope removes his/her glasses to read newsprint, whereas a presbyopic hyperope (who previously had fairly adequate accommodation) puts his/her glasses on to read but removes them for far vision. The question is: Which, the presbyopic myope or the presbyopic hyperope, benefits from half-frame or bifocal positive lens?
_________
G. Some commoner causes of blurred vision/blindness
1. Various ages: malformations, infections, vascular proliferative or occlusive disease, retinitis pigmentosa and other CNS degenerative diseases (some with cherry red macula), diabetes mellitus, neoplasia, retinal detachment, trauma, migraine, and toxic (methanol) (Miller et al, 2005; Shingleton and O’Donoghue, 2000).
2. Selected age-related causes of blurred vision/blindness.
a. Birth through childhood: opacities of the media, astigmatism, and refractive errors:
20/300-400 |
Birth, eyeball too short |
|
20/40-60 |
1 y |
|
20/30 |
3 y |
|
20/20 |
5 y |
b. In later childhood, ages 5 to 7 years, the myopic child has to sit closer and closer to blackboard as the eyeballs continue to grow, and the child becomes increasingly nearsighted.
c. Young adults: optic neuritis Leber hereditary optic neuropathy and other neuropathies/neuritides.
d. At ages 40 to 45 years:
i. Presbyopia: The lens loses its elasticity to focus on near objects (the “arms are too short” for the Pt to hold the newspaper far enough away to read the print).
ii. Glaucoma: Signs include high intraocular pressure, optic disc cupping, pupillodilation, and constricted peripheral fields.
e. Older than 50 years:
i. Cataracts and macular degeneration (Fine et al, 2000), both diagnosable by ophthalmoscopy.
ii. Central serous retinopathy.
iii. Temporal arteritis and ischemic optic neuropathy (Chutorian et al, 2002).
BIBLIOGRAPHY · Blurred Vision and Blindness
Chutorian AM, Winterkorn JMS, Geffner M. Anterior ischemic optic neuropathy in children: case reports and review of the literature. Pediatr Neurol. 2002;26:358–364.
Fine SL, Berger JW, Maguire MG, et al. Age-related macular degeneration. N Engl J Med. 2000;342:483–491.
Miller NR, Newman NJ, Biousse V, Kerrison JB, eds. Walsh and Hoyt’s Clinical Neuro-ophthalmology. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.
Shingleton BJ, O’Donoghue MW. Blurred vision. N Engl J Med. 2000;343:556–562.
V. INNERVATION OF THE OCULAR MUSCLES
A. Classification of ocular muscles into intraocular and extraocular
1. Each eye has 11 ocular muscles: four smooth muscles and seven striated muscles. Because they derive from somites, the striated muscles receive somite CrNs III, IV, and VI. Learn Fig. 4-29.
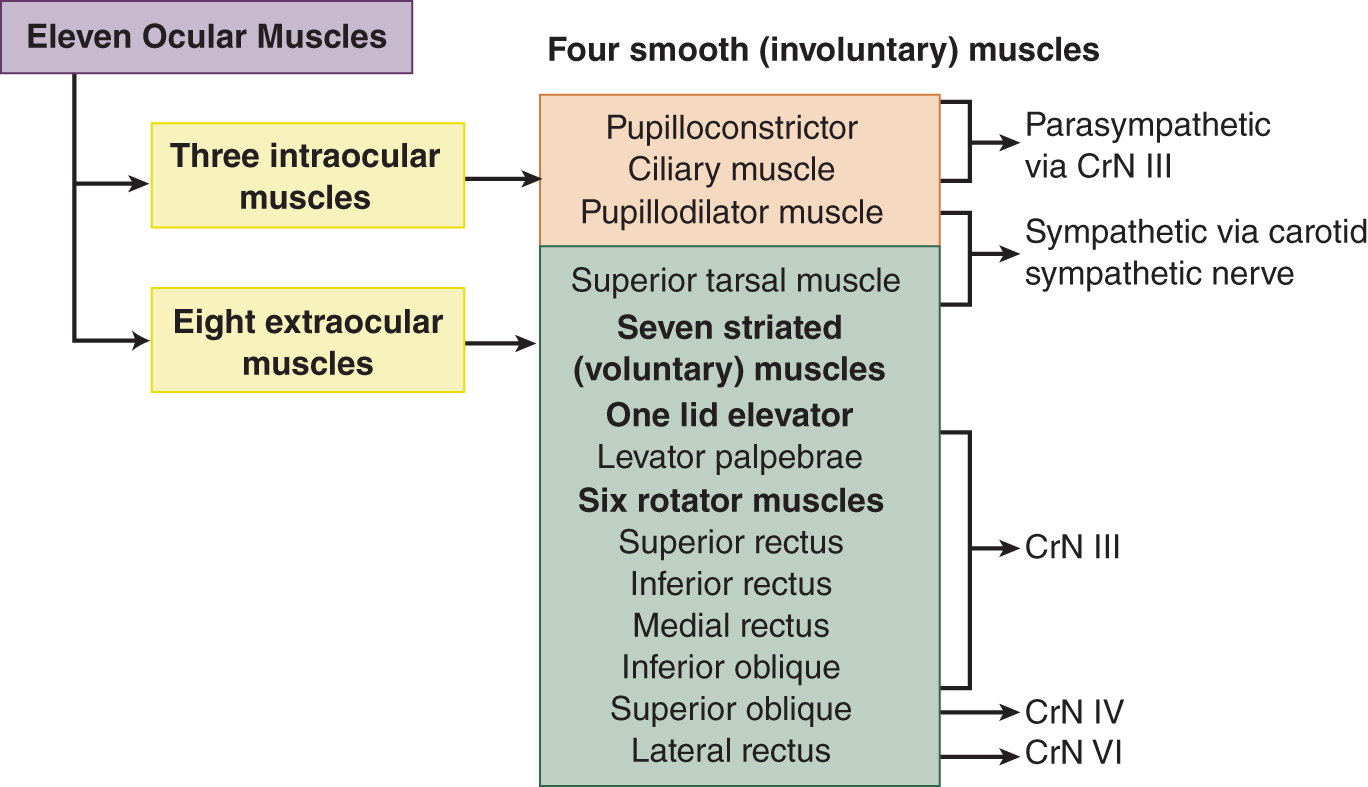
FIGURE 4-29. Classification of the 11 ocular muscles according to type and innervation. Note that the superior tarsal muscle is both a smooth and an extraocular muscle, the only one so classified.
2. One ocular-related muscle, the orbicularis oculi, a sphincter that closes the eyelids, derives from a brachial arch and belongs to the facial muscles, innervated by CrN VII.
B. Peripheral innervation of the extraocular muscles
Six nerves innervate the eye, four motor and two sensory (Table 4-4).
TABLE 4-4 • Afferent and Efferent Innervation of the Eye by Its Six Nerves
Number (name) of nerve |
Innervation |
Clinical effects of interruption of nerve |
Efferent |
||
CrN III (oculomotor nerve) |
Striated muscle: superior, medial, and inferior recti; inferior oblique |
Diplopia, eye abducted and turned down |
Levator palpebrae |
Ptosis (paralysis of volitional lid elevation) |
|
Smooth muscle: pupilloconstrictor; ciliary muscle |
Pupil dilated and fixed to light; loss of lens thickening |
|
CrN IV (trochlear nerve) |
Striated muscle: superior oblique |
Diplopia, most severe on looking down and in; eye extorted; head tilted to side opposite paralyzed eye |
CrN VI (abducens nerve) |
Striated muscle: lateral rectus |
Diplopia, most severe on looking to side of paralysis; eye turned in (adducted) |
Carotid sympathetic nerve |
Smooth muscle: superior tarsal and pupillodilator |
Horner syndrome (ptosis, miosis, hemifacial anhidrosis, vasodilation) |
Afferent |
||
CrN II (optic nerve) |
Visual afferents |
Blindness |
CrN V (trigeminal nerve) |
Corneal/conjunctival afferents Proprioceptive afferents |
Corneal anesthesia of cornea; loss of corneal reflex No known clinical effect |
ABBREVIATION: CrN = cranial nerve. |
||
1. Of the four essentially motor nerves, three convey somatic efferent fibers: CrNs III, IV, and VI (Videos 4-1 to 4-4).

Video 4-1. Right third nerve palsy with pupillary sparing due to diabetes mellitus with subsequent complete resolution.

Video 4-2. Traumatic brain injury (TBI) resulting in fourth nerve (CN IV) palsy.

Video 4-3. Left sixth nerve palsy of unknown etiology with complete resolution.

Video 4-4. Bilateral sixth nerve palsy following motorcycle accident.
a. Two of the three somatomotor nerves serve only one EOM: CrN VI innervates the lateral rectus, and CrN IV innervates the superior oblique. CrN III serves the remaining EOMs and two of the three intraocular muscles.
b. Only CrN III of the somite group also conveys parasympathetic (GVE) fibers. These fibers innervate two of the three intraocular smooth muscles, the pupilloconstrictor and ciliary muscles.
2. The fourth motor nerve of the eye, the carotid sympathetic nerve, innervates the third intraocular muscle, the pupillodilator muscle and one clinically important EOM, the superior tarsal. The carotid sympathetic nerve travels from the carotid artery at the level of the cavernous sinus into the superior orbital fissure and to the eyeball by hitchhiking along other orbital nerves (Fig. 4-31).
3. Test your knowledge of Table 4-4 by completing frames 4-12.
4. CrN III (oculomotor)
a. CrN III is called the _________
b. The EOMs innervated by III are _________
c. CrN III innervates two intraocular muscles and all EOMs, except for _________
d. In addition, CrN III innervates a muscle that elevates the eyelid, the _________
5. CrN IV
a. CrN IV is named the _________
b. CrN IV innervates the only EOM to have a trochlea, the _________
c. The superior oblique has three actions: _________
6. CrN VI
a. CrN VI is named the _________
b. The only action of the lateral rectus is to _________
VI. EXAMINATION OF THE PUPILS
A. Technique of pupillary examination
1. Start with normal illumination of the room, with no direct sunlight. Ask the Pt to gaze at a distant point to avoid pupilloconstriction from the accommodation reflex.
a. The pupils should appear black, equal in size, perfectly round and react to light and to accommodation. Normal pupils appear almost exactly centered in the iris, or very slightly inferomedially placed. A nonblack pupil, usually a whitish one, indicates an opacification of the cornea or lens.
b. Compare the size of the two pupils and record the pupillary size in millimeters. To measure pupillary diameter, compare the pupil with a series of circles graded in millimeters (Litvan et al, 2000) (Fig. 12-30).
i. Look for anisocoria. Benign congenital anisocoria in which both pupils react normally is relatively common.
ii. Look for faint rapid oscillations of the pupillary margins, called hippus. Although often benign, hippus may accompany a metabolic encephalopathy.
c. Inspect the limbus for a Kayser–Fleischer ring or an arcus senilis, also known as arcus corneae. The latter may indicate hyperlipidemia.
2. Check for pupillodilation and a dilation lag.
a. Dim the room lights and inspect the pupils immediately and after 5 to 15 seconds.
b. Normal pupils dilate promptly, within 5 seconds of dimming the light, because of activation of the pupillodilator fibers by the sympathetic nervous system.
c. A dilation lag of seconds to minutes indicates a lack of sympathetic innervation (Horner syndrome) or a myotonic pupil (Adie pupil; Table 4-5).
TABLE 4-5 • Differential Diagnosis of Argyll Robertson and Adie Pupils
Characteristic |
Argyll Robertson pupil |
Adie tonic pupil/syndrome |
Laterality |
Usually bilateral |
Usually unilateral (anisocorial) |
Size |
Cormiosis |
Mild corectasia |
Pupillary outline |
Irregular |
Regular (normal circle) |
Iris atrophy |
Present |
Absent |
Response to light |
None (neither direct nor consensual) |
Very slow direct and consensual response; remains myotonically contracted if light is removed |
Response to dark |
No pupillodilation |
Slow pupillodilation; delayed constriction on re-exposure to light |
Response to accommodation |
Constricts |
Constricts very slowly and remains myotonically constricted after elaxation of accommodation |
Response to mydriatics |
Poor or none |
Responds normally |
Other neurologic features |
Virtually pathognomonic of syphilis; if tabes dorsalis is present, the patient will have dorsal column signs and no muscle stretch reflexes |
Benign disorder, often associated with absent muscle stretch reflexes; no dorsal column signs: Adie syndrome |
Sex predeliction |
More men than women have neurosyphilis |
70% women/30% men |
3. Check the direct and consensual pupillary light reflexes.
a. Instruct the Pt to look at a distant point across the room. Beam a flashlight slowly in from the sides to illuminate each eye separately. Observe whether both pupils constrict promptly and equally to unilateral illumination. After the prompt initial constriction, the pupils normally dilate slightly.
i. Direct constriction of the pupil in the eye stimulated by light is called the direct light reflex.
ii. The consensual constriction of the opposite pupil when light stimulates only one eye is the consensual light reflex. Normally, the direct and consensual pupillary responses are equal.
b. Do not shine the flashlight abruptly into the Pt’s eyes from directly in front, for two reasons:
i. The Pt will automatically look at the light and accommodate for near vision.
ii. The bright light will cause discomfort, particularly if the Pt has photophobia, mental retardation, or dementia.
4. For the swinging flashlight test, alternately swing the light from one eye to the other and hold it on the new eye for 3- to 5-second intervals. Watch for equal reactions of both pupils. If the Pt has an afferent defect in one optic nerve (eg, due to optic neuritis), the pupils will dilate as the light swings from the normal to the affected eye (Marcus-Gunn pupil or relative afferent pupillary defect) rather than maintaining the same degree of constriction.
5. While the room is dimly lit, do the ophthalmoscopic examination.
6. Whenever a question exists about the duration of an ocular finding, such as anisocoria or ptosis, ask the Pt to bring in an old facial photograph.
7. Rehearse the foregoing steps of the pupillary examination (steps V-A-3 and 4 of the Standard NE).
8. In recording the pupillary reactions, many Exs write PERLA as shorthand for “pupils equal and react to light and in accommodation.” We often find that PERLA actually means “pupillary examination really lax.” But if the note says, “pupils 3 mm, equal, centered, react to light and in accommodation and dilate promptly in dim light,” the reader can trust in a meticulous examination. Such a baseline note in the chart is indispensable for the acutely ill hospitalized Pt whose neurologic signs may change abruptly and for the chronic Pt whose signs may change subtly over time.
B. Pathway for the pupillary light reflexes
1. Learn the pathway for the pupillary light reflex as if your life depended on it: someone else’s may. Evaluation of the pupillary reflexes is critical in coma, cerebrovascular disease, brain tumors, and head injuries. Study Fig. 4-30 this way:

FIGURE 4-30. Diagram of afferent (optic nerve) and efferent (III nerve) pathways for pupilloconstriction. The mesencephalon has been transected through its rostral part, encroaching on the geniculate bodies and pulvinar nuclei of the diencephalon. Learn this diagram. R = receptor in the retina. (Adapted from Crosby E, Humphrey T, Lauer E. Correlative Anatomy of the Nervous System. New York: Macmillan Company; 1962.)
a. Learn the names on the left hand side. Those on the right are for general orientation.
b. As typifies reflex arcs, the pupillary reflex arc has a receptor, an afferent limb, central nuclear synapse(s), an efferent limb, and an effector. Start at R, the receptors for light, the rods and cones. Always start at the receptor to analyze any reflex. Trace the path of impulses through the brainstem and back to the effector muscles.
c. Notice the alternate ipsilateral–contralateral course of axons through the optic chiasm.
d. Notice that, after the nerve impulses reach the mesencephalon, they are distributed bilaterally to the parasympathetic (GVE) nucleus of CrN III, called the Edinger–Westphal nucleus. Hence, light stimulation in one eye will constrict both pupils equally. The consensual pupillary constriction equals the direct constriction.
e. Efferent axons travel to the eye via both III nerves. Notice that, according to the general plan of the parasympathetic system, the ganglion of synapse of the GVE axon, the ciliary or episcleral ganglion, is near the end organs, the ciliary and pupilloconstrictor muscles. The same efferent pathway serves pupilloconstriction to light and in accommodation.
2. On scrap paper draw the axonal pathways for the pupillary light reflex and check your drawing against Fig. 4-30.
3. Patient analysis: A Pt has equal pupils and no direct light reflex in the left eye, but has a consensual light reflex on the left when the right eye is illuminated. The lesion is in the  right optic tract/
right optic tract/ left III nerve/
left III nerve/ left optic nerve. (
left optic nerve. ( left optic nerve)
left optic nerve)
4. Describe the result of the swinging flashlight test in the foregoing Pt.
_________
C. Physiology and pharmacology of the pupils
1. The eyeball contains three intraocular muscles, all smooth muscles: the pupillodilator, the pupilloconstrictor, and the ciliary muscles.
a. The pupilloconstrictor and pupillodilator muscles of the iris adjust the diameter of the pupil.
i. The pupillodilator muscle fibers run radially from the pupillary margin, like spokes in a wheel.
ii. The pupilloconstrictor muscle fibers form a sphincter around the pupillary opening.
b. The ciliary muscle is likewise a sphincter, adjusting the diameter of the lens by relaxing its suspensory ligament, to allow the lens to thicken by its own elasticity. The ciliary muscle does not control the pupils.
2. Role of smooth muscle in the tubular viscera: Smooth muscle adjusts the diameters of the apertures and lumens of the tubular viscera, the bowel, bronchi, blood vessels, ureters, bladder, and so on. Curiously, however, the heart, the one viscus that functions solely to change its diameter, is made of striated, not smooth, muscle. Striated muscle is specialized for quick, powerful phasic contractions, smooth muscle for slow, tonic contractions.
3. Tonic opposition of the pupilloconstrictor and pupillodilator muscles
a. Like the EOMs that act in tonically innervated, oppositional pairs, the pupilloconstrictor and pupillodilator muscles actively oppose each other to adjust the pupillary size.
b. The pupilloconstrictor muscle is parasympathetic and cholinergic; the pupillodilator is sympathetic and adrenergic (Low and Benarroch, 2008). Normally the outflow of tonic innervation by sympathetic and parasympathetic impulses balances out. After the pupil adopts any new size, the vector acting to increase pupillary diameter equals the vector acting to decrease it. Thus, a tug-of-war between the constrictor and dilator muscles always positively determines pupillary size.
c. If a lesion or drug blocks one system, sympathetic or parasympathetic, the other acts unopposed. The pupil assumes the size dictated by the tonic innervation that reaches the intact muscle.
i. Parasympathetic denervation of the eye results in  pupillodilation/
pupillodilation/ pupilloconstriction. (
pupilloconstriction. ( pupillodilation (corectasia, mydriasis))
pupillodilation (corectasia, mydriasis))
ii. Sympathetic denervation results in  pupilloconstriction/
pupilloconstriction/ pupillodilation. (
pupillodilation. ( pupilloconstriction (cormiosis))
pupilloconstriction (cormiosis))
4. Pupillodilation (mydriasis)
a. The ophthalmologist never presumes to do a complete funduscopic examination without dilating the pupil. Pharmacologically, pupillodilation can result from mimicking the  sympathetic/
sympathetic/ parasympathetic nervous system or by blocking the
parasympathetic nervous system or by blocking the  sympathetic/
sympathetic/ parasympathetic nervous system. (
parasympathetic nervous system. ( sympathetic;) (
sympathetic;) ( parasympathetic)
parasympathetic)
b. After sympathomimetic or parasympathetic blocking drugs have dilated the pupil, exposure to light will make the Pt uncomfortable, a symptom called photophobia. Which drug would also interfere with lens thickening by paralyzing the ciliary muscle (cycloplegia):  sympathomimetic or
sympathomimetic or  parasympathetic blocking agent? (
parasympathetic blocking agent? ( parasympathetic)
parasympathetic)
c. Although pupillodilator drugs (mydriatics) cause temporary blurring of vision, they are necessary to see the periphery of the fundus. The pupils of infants and deeply pigmented irises respond slowly to mydriatics.
i. For infants use cyclopentolate (Cyclogyl) in a 1% ophthalmic solution, two drops in each eye every 15 minutes for three doses or 1% tropicamide (Mydriacyl), ophthalmic solution or 2.5% phenylephrine (Neo-Synephrine), ophthalmic solution. To reduce burning and tearing, you can pretreat with a topical anesthetic, proparacaine, ophthalmic solution.
ii. For older Pts use one or two drops in each eye. Repeat in 15 to 20 minutes.
d. Because pupillodilation increases intraocular pressure, check the intraocular pressure of adults older than 40 years by tonometry before instilling mydriatics. Two percent of all adults older than 40 years have glaucoma. The danger of precipitating acute glaucoma with mydriatics is greater for the hyperopic Pts.
5. Determinants of pupillary size in addition to light
a. Local disease of the eye and iris.
b. Local ocular or systemic drugs affecting the autonomic nervous system.
c. Emotionality: sympathetic nervous system predominance causing pupillodilation and tachycardia.
d. Sleep and drowsiness: parasympathetic nervous system predominance during sleep causes pupilloconstriction and bradycardia.
e. Age: The pupils of the fetus are large and fail to react to light until the 30 to 32 weeks of gestational age (Isenberg and Vazquez, 1994). Then at term birth the pupils are small (“Gee, its bright out here”). The pupils enlarge through adolescence (the so-called “wide-eyed” innocent look). The size and reactivity then gradually diminish until senility when the pupils again become small and poorly reactive. Small pupils give the person a “flinty-eyed” miserly look, whereas large pupils are considered sexy and receptive, hence, the use of atropine by women who wanted to be la belladonna (the beautiful lady).
D. Patient analysis
A 51-year-old woman was admitted to hospital because of high blood pressure. She had no visual complaints, and the intern recorded a normal ocular examination. Her examination a few hours after the initial examination by the intern disclosed a dilated right pupil, but no eyelid ptosis, heterotropia, fundus lesions, visual field defects, or other ocular signs. She had no direct or consensual pupillary light reflex on the right and no pupilloconstriction in accommodation. The direct and consensual response of the left pupil to light was normal, and it constricted during accommodation. The best inference is
1.  The Pt is blind in the right eye and has a right CrN III lesion.
The Pt is blind in the right eye and has a right CrN III lesion.
2.  The Pt has an intact right optic nerve but has interruption of the right CrN III.
The Pt has an intact right optic nerve but has interruption of the right CrN III.
3.  The Pt has had eye drops placed into the right eye to dilate the pupil. (
The Pt has had eye drops placed into the right eye to dilate the pupil. ( 3. See the next frame)
3. See the next frame)
1. Alternative 1 is excluded because the presence of sight in both eyes, and the presence of the consensual reflex in the left pupil prove that the right optic nerve, the afferent pathway, from the right retina is intact. Alternative 2 is excluded by lack of ptosis or ocular malalignment. Alternative 3 is all that remains.
2. The previous frame emphasizes that a common cause of dilated, nonreactive pupils in medical student practice in teaching hospitals is that the intern or resident has previously (and properly) instilled eye drops to dilate the pupil for an adequate funduscopic examination. However, the intern erred in not recording the use of a mydriatic drug. The more general implication of the frame is that in “thinking through” a reflex arc, you must include the neuromyal junction and the effector as way stations in the reflex arc. The final lesson is: Always record on the chart that you have dilated the pupils.
E. Patient analysis
1. This 24-year-old man is drowsy because of a head injury, but he can be aroused. His left eye is turned down and out and does not turn in reflexly or on command, although the other eye moves on command. When the Pt attempts to look to the right and down, the left eye intorts strongly but remains turned down and out. The left pupil is dilated and fixed (nonreactive) to light or in accommodation. No eye drops were used. The right pupil shows a direct and a consensual response to light and reacts normally in accommodation. This Pt most likely has a lesion of his  left optic nerve/
left optic nerve/ right optic nerve/
right optic nerve/ left CrN IV only/
left CrN IV only/ left CrN III/
left CrN III/ a lesion of one nerve cannot explain the ocular findings. (
a lesion of one nerve cannot explain the ocular findings. ( left CrN III) (
left CrN III) ( No)
No)
2. Should you instill mydriatics in a Pt with a head injury?  Yes/
Yes/ No. Explain.
No. Explain.
_________
3. List two contraindications to pupillodilator drugs.
_________
F. The syndrome of parasympathetic paralysis of the eye (internal ophthalmoplegia)
1. The muscles innervated by the GVE, parasympathetic axons of CrN III, are  intraocular/
intraocular/ extraocular and
extraocular and  smooth/
smooth/ skeletal. (
skeletal. ( intraocular;
intraocular;  smooth)
smooth)
2. The GVE axons of CrN III constitute the only efferent pathway for active pupilloconstriction. Because the GVE and general somatic efferent (GSE) axons of CrN III originate from the same nuclear region and travel in the same peripheral nerve, lesions affecting CrN III generally involve both sets of axons, but important exceptions occur. State the symptoms and signs that would be caused by a pure parasympathetic paralysis of the eye.
_________
3. Apart from head injuries, causes of III nerve palsies include ischemia, as in diabetic III nerve palsy, an aneurysm of the circle of Willis, neoplasm, or inflammation. Often ischemic III nerve palsy spares the pupil, whereas aneurysmal III nerve palsy virtually always affects the pupil (Brazis et al, 1991).
G. The syndrome of sympathetic paralysis of the eye and face: Bernard–Horner or Horner syndrome
1. The sympathetic pathway to the eye: This pathway displays the typical features of all sympathetic innervation.
a. The upper motoneuron pathway begins in hypothalamic neurons and descends through the brainstem tegmentum to the spinal cord. Learn Fig. 4-31.
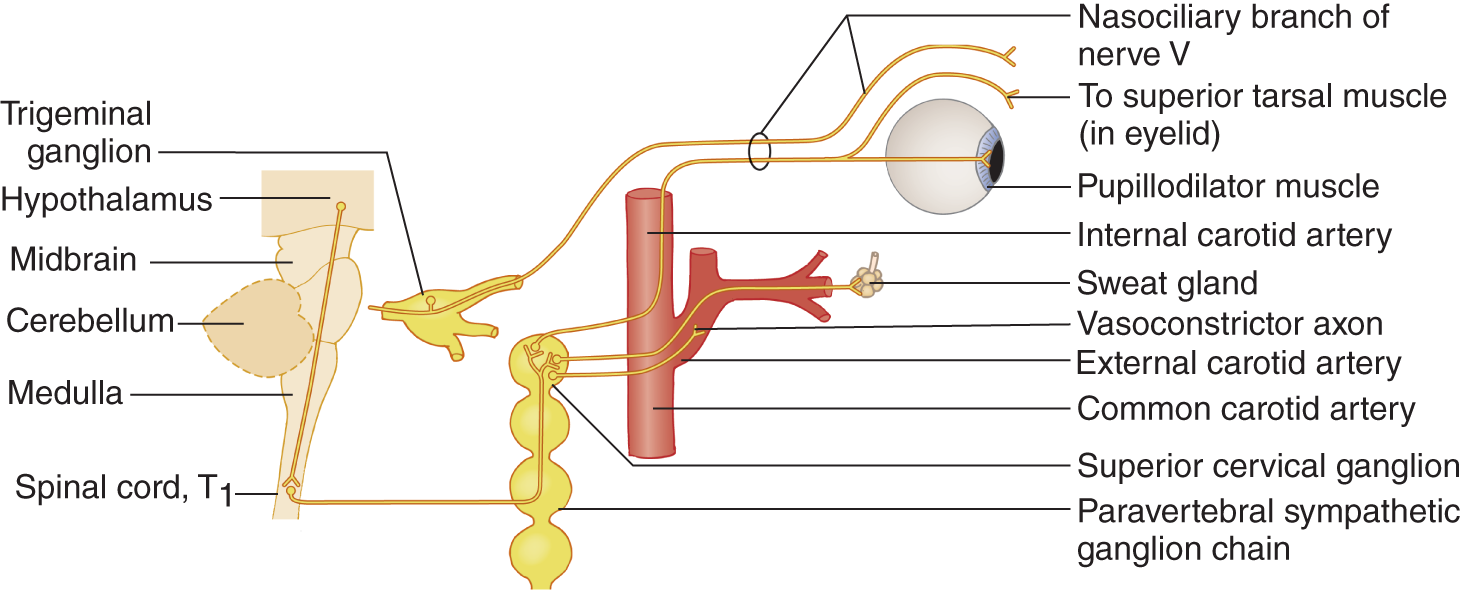
FIGURE 4-31. Diagram of the sympathetic pathway from the hypothalamus (part of the diencephalon) to the pupillodilator and superior tarsal muscles, sweat glands of the face, and the smooth muscle of the carotid arteries.
b. The upper motoneuron pathway synapses on the GVE lower motoneurons of the intermediolateral cell column of the spinal cord gray matter.
i. The sympathetic visceral efferent column extends in the spinal cord from T1 to L2 and L3.
ii. Axons to the eye derive from T1 and T2 (also called the ciliospinal center of Budge).
c. As is also typical, the sympathetic GVE axons, the second-order neurons in the sympathetic pathway, exit with a spinal nerve to synapse in a paravertebral ganglion.
d. From the paravertebral ganglion, the superior cervical for the carotid sympathetics, the third-order axons, then hitchhike as a plexus along blood vessels or nerves to their effectors.
e. The carotid sympathetic nerve innervates the smooth muscles of the vessels of the entire internal and external carotid systems.
i. The external carotid artery carries sympathetic axons to the sweat glands of the face.
ii. The internal carotid artery carries the sympathetic axons to the ocular smooth muscles and the sweat glands of the forehead.
f. The sympathetic axons innervate two ocular muscles, _________
g. Note: The sympathetic and parasympathetic systems differ in the location of the ganglion containing the secondary axon.
i. The ganglia of the sympathetic nervous system are located in the paravertebral chain.
ii. By contrast, the ganglia of the parasympathetic nervous system are located in or near the effector innervated.
2. Patient analysis: A 21-year-old man has suffered a stab wound in the neck interrupting the sympathetic innervation to one side of his face. Run down the right-hand labels of Fig. 4-31 to compile a list of signs that would occur.
_________
_________
3. These four features of sympathetic facial denervation constitute the Bernard–Horner or Horner syndrome. Although enophthalmos is also described as part of this syndrome in humans, it is more apparent, because of ptosis, than real.
a. Explain why miosis occurs after sympathetic denervation of the eye.
_________
b. After sympathetic paralysis, the miotic pupil will constrict further in response to light or accommodation, because the muscle receives an additive constrictor stimulus rather than simply a “tonic” stimulus.
c. A diagnostic feature of unilateral Horner syndrome is an increase in the degree of the anisocoria just after dimming the room light. Pupillodilation in the first 5 seconds depends on sympathetic activation. The normal pupil will dilate within 5 seconds, whereas the abnormal pupil has a dilation lag and briefly remains the same size. The anisocoria lessens in 15 to 20 seconds because of a decrease in parasympathetic innervation to the abnormal eye.
d. In bright light the miosis of the normal pupil will cause it to approximate the Horner pupil. Thus, the miosis may be missed without examining the Pt in a darkened room.
4. Separation of the components of Horner syndrome: The number of signs of sympathetic facial denervation varies depending on the location of the lesion along the sympathetic pathway:
a. If the lesion interrupts the sympathetic pathway distal to the origin of the external carotid artery, the only sympathetic denervation signs the Pt will show are _________
b. If the lesion interrupts the sympathetic pathway proximal to the external carotid artery (between hypothalamus and external carotid artery), the Pt will show, in addition to ptosis and cormiosis, the other two features of Horner syndrome: _________
c. The vasodilation is best seen in the conjunctival vessels.
d. With a congenital unilateral Horner syndrome, such as with an Erb brachial plexus injury, the ipsilateral iris often becomes heterochromic.
5. Clinical testing of the ocular sympathetic pathway to the eye: the faciociliary or spinociliary (ciliospinal) reflex.
a. To test the sympathetic pathway to the eye, pinch the skin over the face (CrN V afferent) or neck (C2 or C3 afferent) firmly for 5 seconds. Both pupils should dilate briskly—the faciociliary reflex or the spinociliary (ciliospinal) reflex.
b. Should you do the test in a darkened or a brightly lit room and with the Pt looking at a near or distant target? Explain.
_________
6. Causes of Horner syndrome: Apart from direct trauma, important causes include brainstem infarction that interrupts the descending axons from the hypothalamus (Fig. 4-31 and see Table 10-4); neoplastic or inflammatory masses in the lung apex, neck, base of the skull or orbit; and vascular diseases of the carotid artery, such as cervicocephalic arterial dissections, or aneurysms. A newly acquired Horner syndrome requires a search for such lesions (Videos 4-5 and 4-6).

Video 4-5. Horner syndrome in a patient with neuromyelitis optica (NMO).

Video 4-6. Postganglionic right Horner syndrome in a patient with right internal carotid artery dissection.
H. Abnormal pupillary reflexes with absent muscle stretch reflexes
1. Tabes dorsalis with an Argyll Robertson pupil (Sir Douglas Argyll Robertson, 1837–1909) caused by neurosyphilis and Adie tonic pupil syndrome (William Adie, 1886–1935) feature absent muscle stretch reflexes and abnormal pupillary responses (Table 4-5).
TABLE 4-6 • Differential Diagnosis of III Nerve and Sympathetic Ptosis
Feature |
Present with IIIrd nerve lesion |
Present with sympathetic pathway lesion |
Cormiosis |
||
Corectasia |
||
Reaction to light and accommodation |
||
Usually have heterotropia |
||
Elevation of eyelid on upward gaze |
||
Normal sweating |
III |
Sympathetic |
+ |
|
+ |
|
+ |
|
+ |
|
+ |
|
+ |
2. The neuropathy of diabetes mellitus may also cause abnormal pupillary reflexes and absence of muscle stretch reflexes. The Argyll Robertson pupil may also occur in neurosyphilis without tabes dorsalis. Table 4-5 show why you test pupillary constriction to light and in accommodation.
BIBLIOGRAPHY · Examination of the Pupils
Brazis PW. Localization of lesions of the oculomotor nerve: recent concepts. Mayo Clin Proc. 1991;66:1029–1035.
Isenberg SJ, Vazquez M. Are the pupils of premature infants affected by intraventricular hemorrhage? J Child Neurol. 1994;9:440–442.
Litvan I, Saposnik G, Maurino J, et al. Pupillary diameter assessment: need for a graded scale. Neurology. 2000;54:530–531.
Low PA, Benarroch EE, eds. Clinical Autonomic Disorders. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008.
VII. CLINICAL EVALUATION OF PTOSIS
A. Elevation of the eyelid
1. Two muscles elevate the eyelid and, hence, adjust the vertical diameter of the palpebral fissure: the superior tarsal (Müller) muscle and the levator palpebrae muscle.
a. The superior tarsal muscle, a smooth muscle, acts tonically to elevate the eyelid. It is innervated by the _________
b. The levator palpebrae muscle, a skeletal muscle, acts tonically and phasically to elevate the eyelid. It is innervated by _________
2. Try this experiment to understand eyelid elevation.
a. Look straight ahead into your mirror. The combined tonic action of the superior tarsal muscle and the levator palpebrae muscle sets the height of your palpebral fissure. Elevate and lower the mirror while observing the rise and fall of your upper lids, but do not allow your head to move.
b. Now try to elevate and lower your eyelids without moving your eyes and try to elevate and lower your eyes without allowing your upper lid to move. Can you separate the eyeball and eyelid movements?  Yes/
Yes/ No (By now you know not to look here for answers that you should work out for yourself.)
No (By now you know not to look here for answers that you should work out for yourself.)
c. Activation of the levator palpebrae muscle causes the quick or phasic rise and fall of the eyelid during vertical eye movements. Although eyelid elevation is linked automatically as an associated movement to the ocular muscles that elevate the eyeball, the levator palpebrae is a skeletal muscle. Inhibition of its action in the CNS allows the lid to follow the eyeball when it rotates down.
3. Levator palpebrae paralysis causes:
a. Severe ptosis, greater than with superior tarsal ptosis.
b. Paralysis of lid elevation during upward gaze.
4. Will the lid elevate when the Pt with sympathetic ptosis looks up?  Yes/
Yes/ No. Explain. _________
No. Explain. _________ Yes. The levator palpebrae is intact and will automatically elevate the lid when the eye rotates up.)
Yes. The levator palpebrae is intact and will automatically elevate the lid when the eye rotates up.)
5. Differentiation of sympathetic and III nerve ptosis: Complete Table 4-6 by placing a plus sign in column 2 or 3.
B. The causes of ptosis (blepharoptosis)
1. Sometimes ptosis comes neither from a III nerve lesion nor from sympathetic denervation. In myasthenia gravis, levator palpebrae weakness results from defective cholinergic transmission at the neuromyal junction (Video 4-7). Ptosis from nerve or neurohumoral transmission lesions is neuropathic ptosis. Ptosis from muscular dystrophies is myopathic ptosis. Sometimes ptosis is congenital and may or may not accompany other anomalies. After injury or inflammation, lid edema may cause ptosis. The point is this: In analyzing ptosis or any other neurologic sign, you must “think through” the possible lesion sites, down to and including the effector, and integrate each sign with other physical signs and the history. The lesion causing the ptosis may be:

Video 4-7. Eyelid ptosis due to myasthenia gravis in a patient with recurrent invasive thymoma. Positive ice pack test.
a. Central: at the hypothalamus, brainstem, or spinal cord.
b. Peripheral: along the course of the III or sympathetic nerves.
c. Neuromyal: at the nerve-muscle junction.
d. Local in the muscle itself: myopathic, congenital, inflammatory, or traumatic (Video 4-8).

Video 4-8. Complete external opthalmoplegia in a pregnant patient with Kearns-Sayre syndrome (KSS).
e. Other causes include edema of the eyelid and dehiscence of the levator muscle aponeurosis.
2. In Bell facial palsy from interruption of CrN VII, the eyelid may droop to the degree that it covers the eye. Normally frontalis contraction elevates the eyebrow. In Bell palsy, the drooping of the eyelid occurs because of paralysis of the frontalis muscle, which inserts into the eyebrow. Proof of the nature of this form of ptosis comes from the eyebrow-lifting test. Lifting of the eyebrow by the Ex corrects the ptosis in a VII nerve palsy, but it remains in a III nerve palsy (Ohkawa et al, 1997).
3. Cerebral ptosis: Pts with acute strokes may have unilateral or bilateral ptosis in association with hemiparesis. The lesion will be in the right cerebral hemisphere more often than in the left. The ptosis may appear ipsilateral to the lesion. The mechanism of this ptosis is uncertain. The development of complete bilateral ptosis may predict brain herniation (Averbuch-Heller et al, 2002).
4. The ptosis with myasthenia gravis will often fluctuate or fatigue throughout the examination and may become more evident on one side when the fellow lid is manually elevated (enhanced ptosis). Also an ice-bag test may improve the ptosis in patients with myasthenia gravis. In this test, an ice pack is held over one eye (both lids closed) for 2 minutes and afterward the position of the lid is observed. Lessening of the degree of ptosis often may occur in myasthenic patients probably due to improved neuromuscular transmission.
5. Thus ptosis, like all signs and symptoms, poses a puzzle to be solved. Every sign generates many diagnostic possibilities that the Ex must systematically sort through. Two important points of distinction for neuropathic ptosis are:
a. Other signs of interruption of CrN III usually accompany ptosis from levator palpebrae paralysis.
b. Other signs of interruption of the carotid sympathetic nerve usually accompany ptosis from superior tarsal muscle paralysis.
BIBLIOGRAPHY · Ptosis
Averbuch-Heller L, Leigh RJ, Mermelstein V, et al. Ptosis in patients with hemispheric stroke. Neurology. 2002;59:620–624.
Ohkawa S, Yamasaki H, Osumi Y, et al. Eyebrow lifting test: a novel bedside test for narrowing of the palpebral fissure associated with peripheral facial nerve palsy. J Neurol Neurosurg Psychiatry. 1997;63:256–257.
VIII. CONJUNCTION SYNDROMES OF THE CRANIAL NERVES
A. Conjunctions of cranial nerves with pathways of the central nervous system
1. The lesion that interrupts an ocular motor nerve (or any other nerve) causes different signs if it affects the central or peripheral course of the nerve. When considering a lesion of a specific nerve, always start at the nucleus of origin of the nerve and think through to its termination.
2. A central lesion will almost always also affect a neighboring long tract in addition to the CrN.
a. A midbrain lesion that causes a III nerve palsy lesion may interrupt the dentatothalamic tract and cause contralateral ataxia and tremor; or, if it affects the region dorsomedial to the red nucleus, it will paralyze down gaze; or, it will cause hemiplegia, if the lesion affects the midbrain basis (Fig. 2-18).
b. A contralateral hemiplegia usually will accompany a VI nerve lesion in the basis pontis because of the conjunction of CrN VI with the pyramidal tract at that site (Fig. 2-16).
B. Eponymic conjunction syndromes of the peripheral parts of ocular motor cranial nerves
1. CrN II, the ocular motor CrNs III, IV, and VI, CrN V, and the carotid sympathetic nerve run through the region of the cavernous sinus, the tip of the petrous bone, and the superior orbital fissure. Notice in Fig. 4-32 that CrNs III and IV and two sensory branches of CrNs V, V1, and V2 run in the lateral wall of the cavernous sinus and that CrN VI runs through the lumen. The lumen also contains the siphon of the internal carotid artery. The optic chiasm (not shown) sits just above the stalk of the pituitary gland.
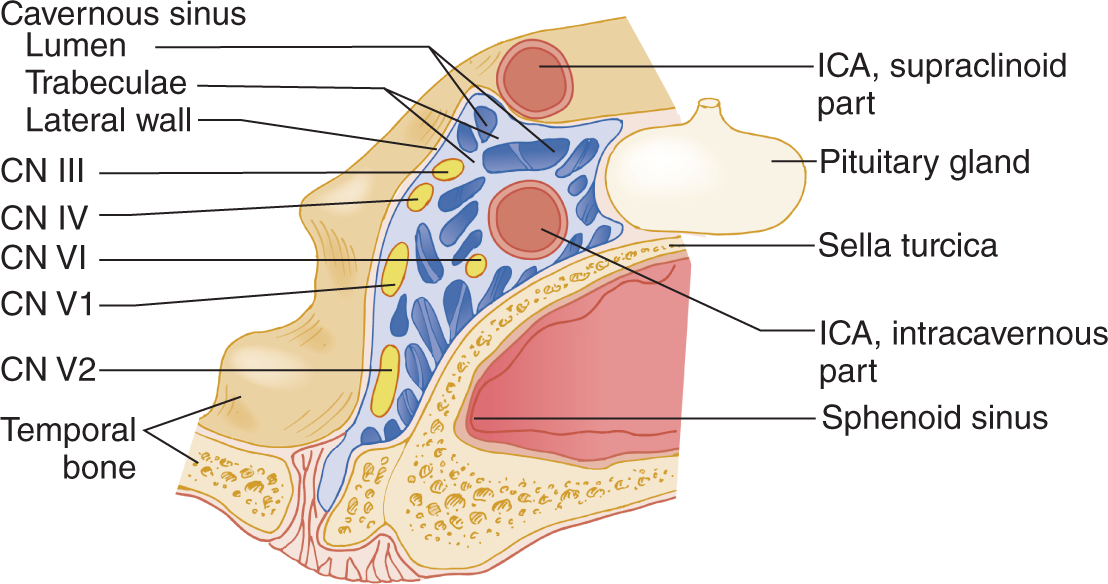
FIGURE 4-32. Coronal section through the cavernous sinus and pituitary gland. CN = cranial nerve. ICA = internal carotid artery; V = sensory division of CN V1 and V2.
2. The symptoms and signs consist of pain or numbness in the ophthalmic division of CrN V, palsies of the ocular motor nerves, with ptosis, either sympathetic or III nerve in origin, and visual defects from involvement of CrN II or the chiasm. A carotid-cavernous fistula adds proptosis. A painful ophthalmoplegia plus or minus sympathetic paralysis is the core feature. Depending on the particular combinations of nerves affected, the syndrome is called Gradenigo, Tolosa–Hunt (Brazis et al, 2016), or Raeder paratrigeminal (Goadsby, 2002). Typically the cause is inflammation, neoplasm, trauma, or an internal carotid artery fistula or aneurysm.
3. Remember that many diseases can cause diplopia and ocular palsies that do not directly interrupt optomotor nerves: myasthenia gravis, hyperthyroidism, botulism, and myopathies. Therefore, the “thinking through” process of differential diagnosis must also include the neuromyal junction, the muscles themselves, the adjacent anatomical structures, and systemic disease such as endocrinopathies.
C. Other cranial nerve conjunction syndromes
1. A single lesion in the cerebellopontine angle frequently affects CrNs VII and VIII at the internal auditory meatus and sometimes adjacent CrNs VI, and IX and others. Review Fig. 2-20.
2. CrNs IX, X, and XI come into conjunction at their exit site at the jugular foramen. Review Table 2-4.
BIBLIOGRAPHY · Eponymic Conjunction Syndromes
Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins, Wolters Kluwer Health. In Press. 2016.
DeMyer W. Neuroanatomy. Baltimore, MD: Lippincott Williams & Wilkins; 1998.
Goadsby PJ. “Paratrigeminal” paralysis of the oculopupillary sympathetic system. J Neurol Neurosurg Psychiatry. 2002;72:297–299.
D. Patient analysis
1. The 34-year-old woman in Fig. 4-33A suddenly noticed double vision.
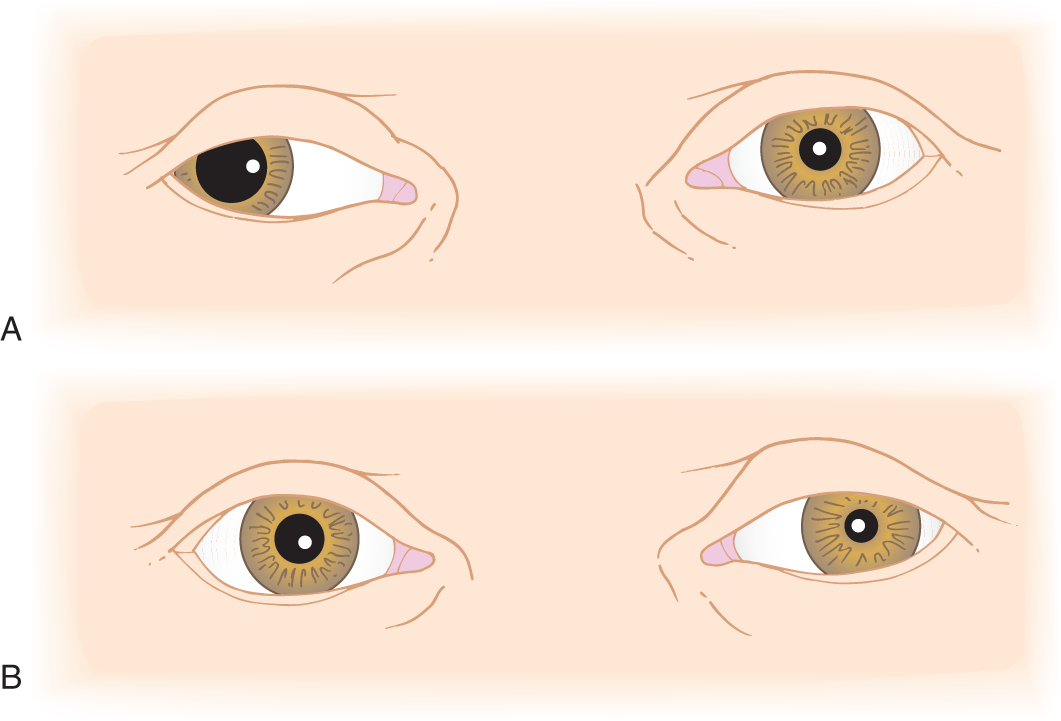
FIGURE 4-33. (A, B) Two Pts with ocular abnormalities.
2. She was unable to adduct, elevate, or depress her right eye, but it did intort when she attempted to look down and to the left. The right eyelid did not elevate on volitional upward gaze. The right pupil neither reacted directly nor consensually to light. The left pupil did react directly and consensually. All other neurologic functions were intact. These findings indicated a lesion affecting the _________
E. Patient analysis
1. The 21-year-old woman in Fig. 4-33B complained of deep pain behind her left eye for several weeks. She also noticed diplopia when looking far to the left. For some weeks her left eyelid had drooped. Examination showed ptosis that was corrected on upward gaze, miosis, and mild weakness of abduction of the left eye; however, the corneal light reflections remained aligned when she had her eyes in the primary position. She had no other neurologic abnormalities. At her doctor’s request, the Pt brought in old facial photographs that proved that the ptosis was new. Does the lesion localize to one nerve? If not, what nerves are implicated? _________
2. Because this Pt had only ptosis and miosis without hemifacial anhidrosis, the lesion must have affected her sympathetic pathway distal to the origin of her external carotid artery.
3. The conjunction site of the sympathetic pathway and the VI nerve is at the cavernous sinus region. This region receives its sensory innervation from CrN V. Hence, some lesion was progressively attacking successive sensory and motor nerves at the base of the skull.
4. Inspection of the nasopharynx disclosed a soft tissue mass. Radiographs of the skull base showed bony erosion. A biopsy disclosed a nasopharyngeal carcinoma. It had infiltrated the base of the skull and cavernous sinus and encircled the internal carotid artery, where it had interrupted the carotid sympathetic and VI nerves. Painful ophthalmoplegia of this type is called the Tolosa–Hunt syndrome. (Video 4-9)

Video 4-9. Tolosa Hunt syndrome.
IX. SUMMARY OF THE EXAMINATION FOR VISION AND THE PERIPHERAL OCULAR MOTOR SYSTEM
Now return to the Standard NE and rehearse Part VA15.
 Learning Objectives for Chapter 4
Learning Objectives for Chapter 4