CHAPTER 49
Obstetric Anesthesia
Introduction
The aim of this chapter is to introduce the anesthesia technician to the care provided to obstetric patients by the anesthesia team in the delivery suite. The unique environment, the unique condition of pregnancy, and the particular challenges of provision of safe anesthesia care in this specialty area are considered.
When elderly women are asked to name the most memorable day of their lives, the most common response is the day of delivery of their first child. The birth of a child is usually a joyful time, although the experience may be attended with fear, anxiety, and severe pain. Historically, and in parts of the world still, childbirth is associated with a high maternal mortality rate and an even higher neonatal mortality rate. The safety of childbirth has improved considerably in developed countries (Fig. 49.1). Nonetheless, for the fetus, delivery remains a time of high risk. Delivery may be complicated by known or previously unknown congenital medical problems, in utero growth problems, placental or umbilical cord accidents, obstruction of passage through the birth canal, and related injuries. For the mother, childbirth remains a significant cause of mortality and morbidity even in wealthy countries. Complications occur related to preexisting medical conditions in the mother, especially cardiac disease, and medical conditions arising as a result of pregnancy, such as venous thromboembolism, as well as diseases unique to pregnancy such as preeclampsia and amniotic fluid embolus. Hemorrhage remains a major cause of maternal mortality, even in the best of settings. There are also increased risks associated with anesthesia during pregnancy to be considered.
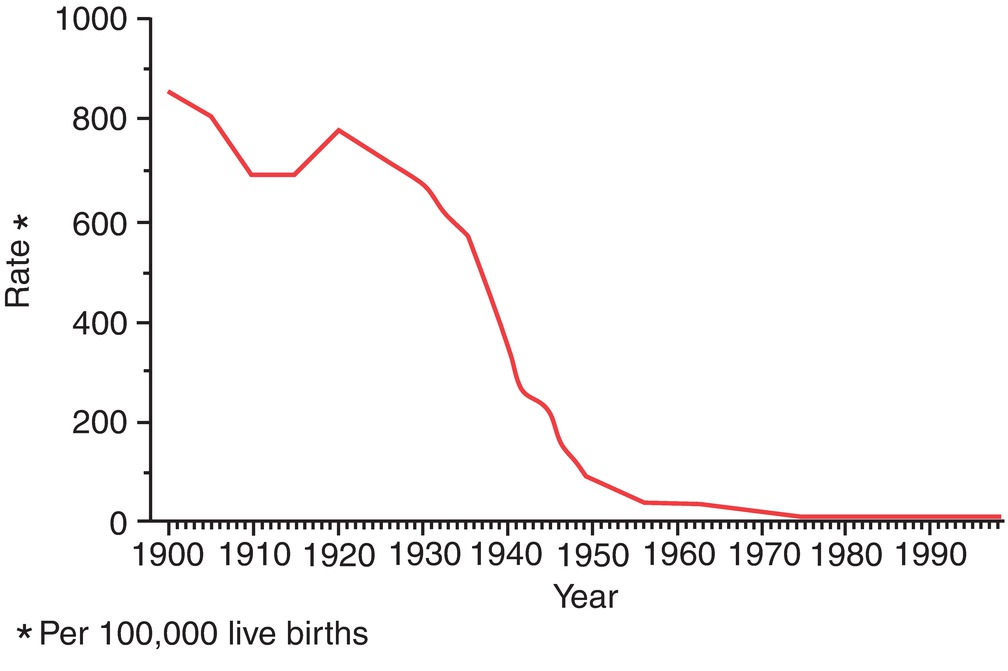
FIGURE 49.1. US maternal mortality rate by year (1900–1997). (Centers for Disease Control and Prevention (CDC). Healthier mothers and babies. MMWR Morb Mortal Wkly Rep. 1999;48(38):849-856. Available from: http://www.cdc.gov/mmwr/PDF/wk/mm4838.pdf. Accessed March 3, 2002.)
The role of the anesthesia team on the labor and delivery suite is to provide labor analgesia, safe anesthesia for surgical procedures, both elective and unplanned, and to respond to any emergencies as they arise, to ensure the safety of both the mother and child. Careful planning and preparation is the key to safe provision of anesthesia services on the delivery suite. One of the most critical roles of the obstetric anesthesiologist is to be available for care of the rare but frightening obstetric emergency. Similarly, the primary role of the anesthesia technician in the delivery suite is to ensure that the anesthesia provider has adequate, current supplies and equipment ready to hand not only for labor analgesia and for obstetric surgery but for all potential emergencies. Understanding the nature of obstetric anesthesia will help the anesthesia technician provide optimal support to anesthesia providers, mothers, and babies.
Design of Obstetric Units
Obstetric units are often remote from the main operating suite; indeed, they may be in distant buildings. Staffing assignments must ensure that adequate anesthesia coverage and technical support are available day and night. In rural settings and in small hospitals, anesthesia providers may not always be in-house at night. There will be a clear local policy as to acceptable times within which anesthesia services will be delivered. In the past, the American College of Obstetricians and Gynecologists (ACOG), the American Society of Anesthesiologists (ASA), and the Joint Commission standards dictated that units should be able to ensure a “decision-to-incision” interval of less than 30 minutes—that is, after the obstetrician decides that cesarean section is needed, surgery must begin within 30 minutes. However, in certain life-threatening situations, delivery of the neonate within 10-15 minutes improves outcomes. Achieving such rapid delivery safely requires preparation and teamwork. Anesthesia supplies must be ready and accessible at all times, operating rooms (ORs) must be prepared to receive a patient requiring an emergency cesarean section, and the anesthesia team should be prepared to provide anesthesia, including general anesthesia, at short notice. Although anesthesia technicians are an important part of the anesthesia team, many institutions do not provide a dedicated anesthesia technician to cover the obstetric suite.
The delivery suite is usually set up with delivery rooms, in which the anesthesia team may be involved in providing labor analgesia for labor and forceps or vacuum deliveries, and ORs in which both elective and emergency procedures are performed, including cesarean section, manual removal of placenta, tubal ligation, cervical suture, and in some centers fetal in utero procedures. In some units, ORs may be shared with the main operating area.
Monitoring
Facilities for monitoring in delivery rooms may be limited to noninvasive monitoring including noninvasive blood pressure and pulse oximetry. Obstetric nursing staff routinely monitor these parameters during labor, along with cardiotocography and external monitors, which measure both the fetal heart rate and uterine contractions (Fig. 49.2). Fetal heart rate monitoring (analysis of cardiotocography patterns) allows assessment of the adequacy of uterine contraction and fetal well-being during labor. A normal fetal heart rate is between 110 and 160 beats/min, with variability and “accelerations.” The monitor may also show “decelerations” of various types, the most ominous of which are frequent late decelerations, which means that the deceleration occurs after the peak of the contraction. This suggests that uteroplacental perfusion is compromised during the contraction and the fetus may be at increased risk of a poor outcome including neurologic injury and even death (Fig. 49.3). The decision to proceed with urgent cesarean section is frequently made on the basis of this monitoring. A sustained fetal bradycardia suggests that the supply of oxygen to the fetus remains poor and is a clear emergency requiring immediate delivery.
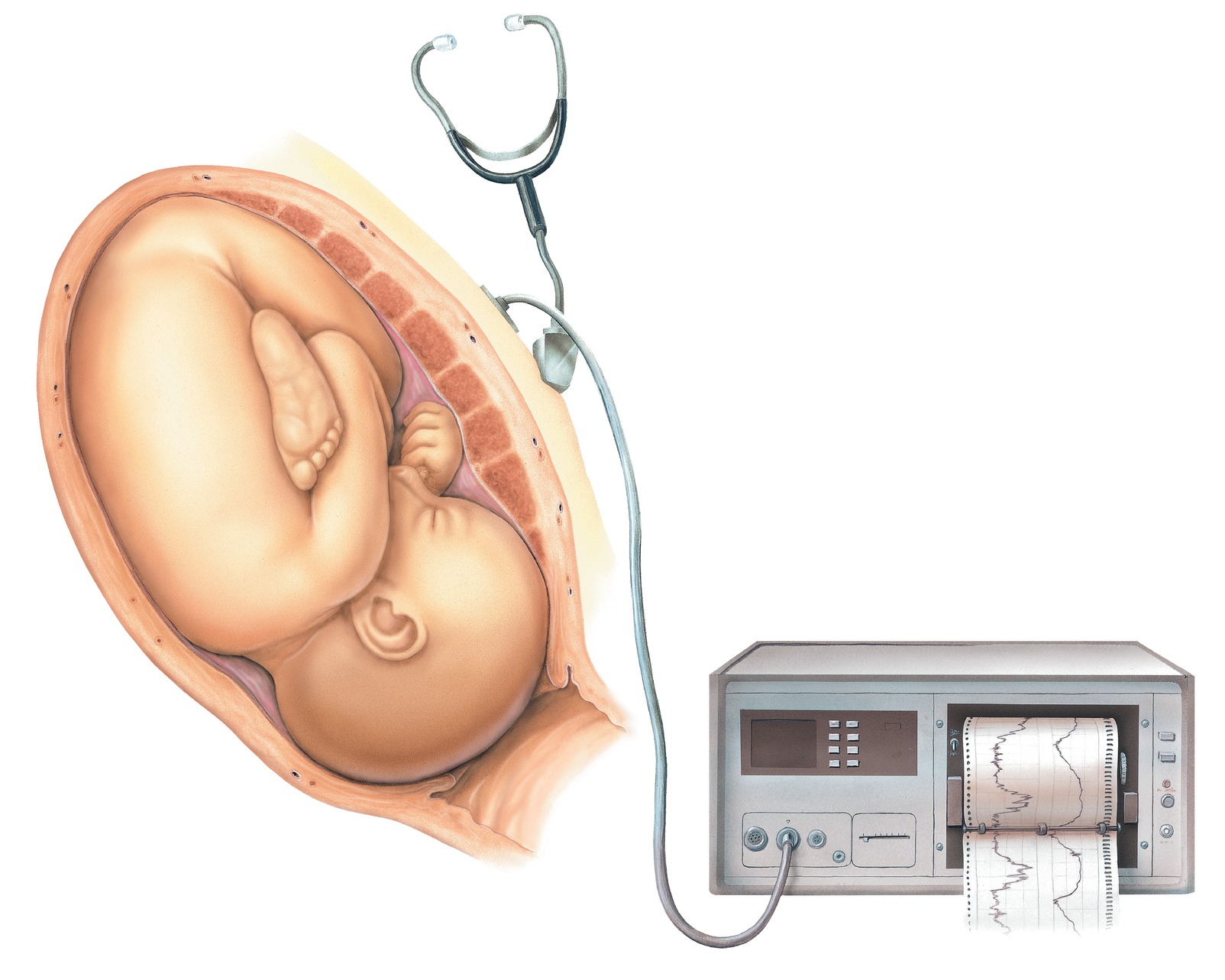
FIGURE 49.2. Conditions for cesarean section, fetal distress, and persistent and consistent late decelerations indicating fetal distress.
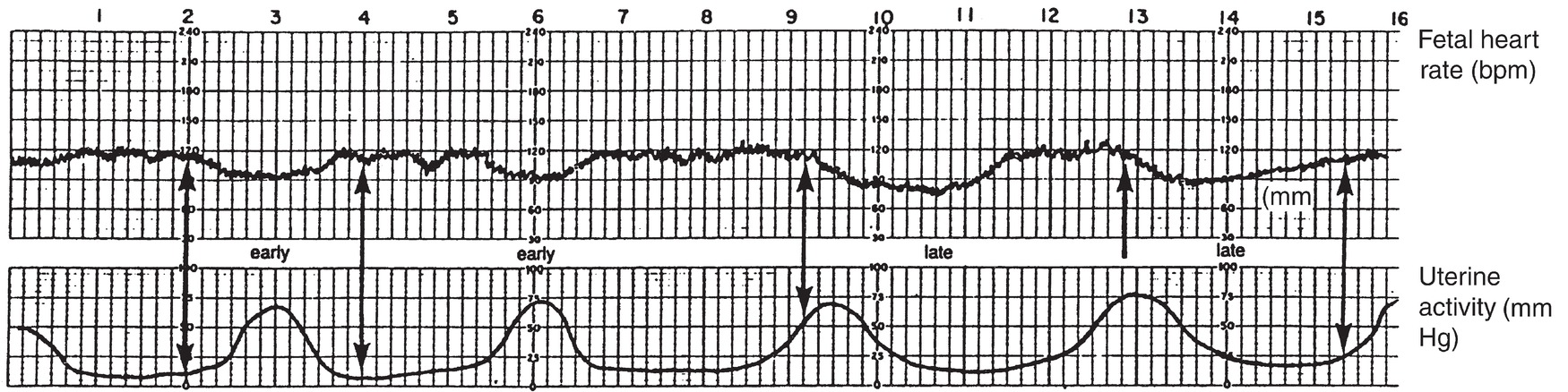
FIGURE 49.3. An early deceleration mirrors the contraction, is caused by head compression, and is benign, requiring no intervention. A late deceleration mirrors the contraction but is offset because a late deceleration begins after the contraction has started and ends after the contraction has ended. The cause is uteroplacental insufficiency, and interventions are aimed at improving blood flow to the placenta.
Advanced maternal monitoring such as electrocardiogram (ECG) and arterial or central venous pressure monitoring may be possible in the delivery room, although the training of obstetric nursing staff may limit its use. In addition, the supplies for these procedures are usually stocked in the OR, and not the delivery suite. During labor and delivery, there are very large changes in physiologic parameters as a result of pain and the metabolic demands of the contracting uterus; for example, cardiac output, already increased 50% by pregnancy itself, increases another 40% during labor and delivery. Effective labor analgesia is known to reduce such changes.
For some patients, safe delivery requires additional monitoring. Some options are the use of specialist obstetric nursing staff with additional training, intensive care nursing support, or the continuous presence of the anesthesiologist. It may be preferable for patients requiring invasive monitoring to deliver in an OR or an intensive care unit (ICU) setting. Occasionally, arterial pressure monitoring may be required for women with severe hypertension. When invasive monitoring is required for labor, it is usually for patients with severe cardiac or other underlying disease. Arterial lines and central lines are used more frequently than pulmonary artery catheters. Obstetric ORs may require stocking of a variety of invasive vascular access devices for use in emergencies or unanticipated escalation of care. Patients may need to be cared for in specialized obstetric units or ICUs depending on institutional policies.
The Physiologic Changes of Pregnancy
The risks associated with anesthesia are increased during pregnancy because of major physiologic changes occurring in the mother as a result of the pregnancy. These changes include the following:
1. An increased risk of aspiration of gastric contents because of decreased stomach emptying.
2. Increased oxygen consumption and decreased functional reserve capacity leading to rapid desaturation during induction of general anesthesia.
3. Increased edema. Difficult intubation is about ten times more common in the obstetric population, partly because of increased airway edema and partly because of increased obesity, positioning difficulties, and the need for rapid sequence induction with cricoid pressure.
4. Aortocaval compression leading to decreased venous return, decreased cardiac output, and hypotension in the supine position, particularly in the presence of central neuraxial blockade. The mass of the enlarged uterus and fetus compresses the vena cava and aorta. The patient should be positioned in left uterine displacement when supine, with a wedge under the right hip or the table tilted to ensure that the gravid uterus is moved away from these major blood vessels (Fig. 49.4).

FIGURE 49.4. Left lateral tilt to relieve aortocaval compression. (From MacDonald MG, Seshia MKK, et al. Avery’s Neonatology Pathophysiology and Management of the Newborn. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005, with permission.)
When possible, general anesthesia is avoided during pregnancy. Maternal mortality figures show declining mortality associated with anesthesia, in line with decreasing use of general anesthesia, and increasing use of regional anesthesia. In addition, general anesthesia is associated with increased risks for the fetus compared with regional anesthesia.
Labor Analgesia
Neuraxial analgesia is both the most effective and most invasive option for relief of labor pain. Lumbar epidurals are commonly used. Other options are spinals or combined spinal and epidural techniques (combined spinal epidural [CSE]). Optimal labor analgesia gives pain relief without motor blockade.
Labor is divided into three stages. The first stage occurs when the uterus is contracting regularly and painfully and the cervix dilates. The second stage occurs when the baby descends through the birth canal and the mother actively pushes. The third stage is the delivery of the placenta. The pain of the first stage of labor is transmitted via nerves supplying the contracting uterus, from T10-L1, whereas the pain of the second stage of labor is transmitted via nerves supplied by sacral nerve roots S2-S4.
The pain of labor is described as being among the most severe of all types of pain. Women’s expectations of the pain of labor are varied, as are their attitudes to analgesia. Some women plan for as much analgesia as possible, while others aim for minimal pain relief, or only noninvasive techniques (Table 49.1). Labor pain is particularly severe in the later first stage, as the cervix approaches full dilation. This may coincide with both mental and physical exhaustion, leading many to request epidural analgesia at this stage.
Table 49.1. Techniques of Labor Analgesia
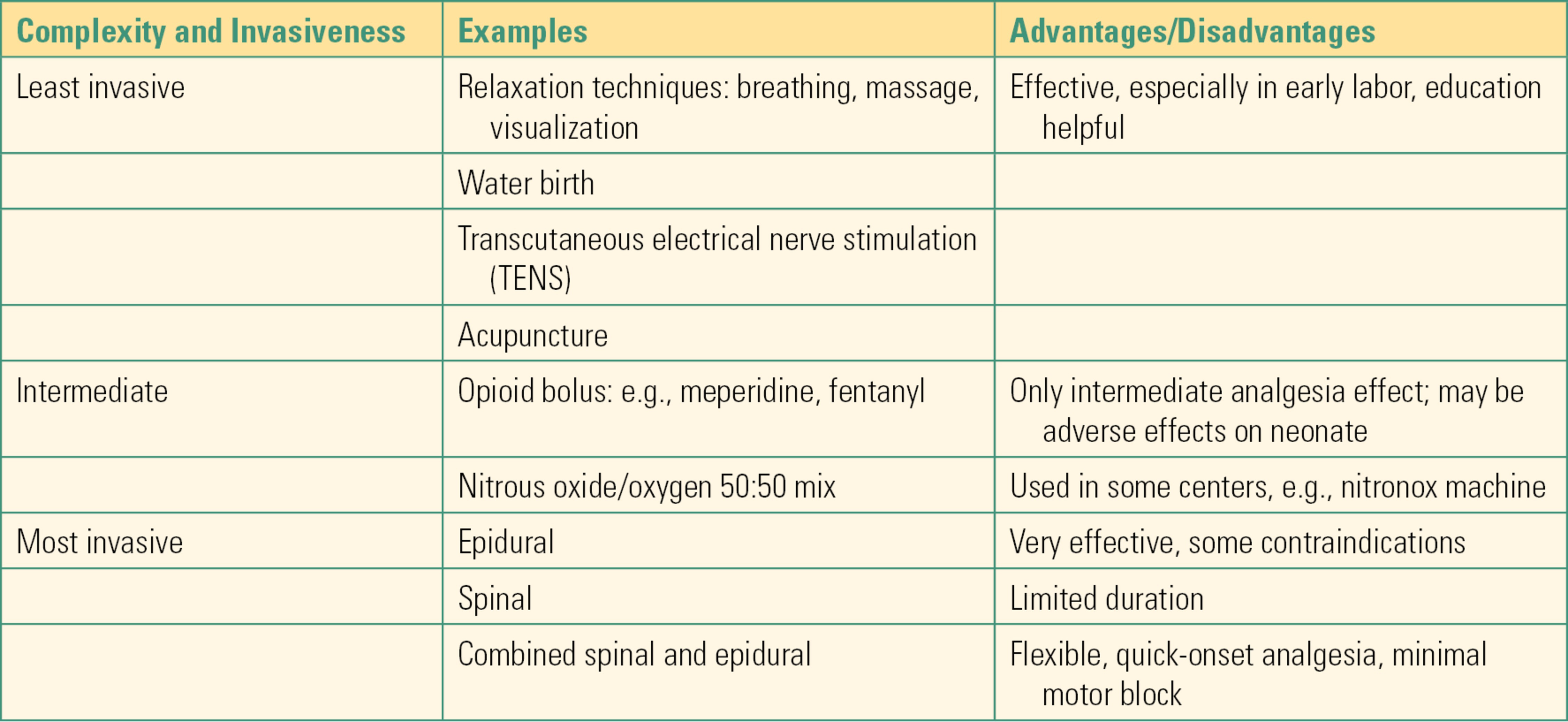
The pain of labor is unique in pain treatment, in that provision of as much analgesia as possible is not necessarily what the patient desires. Many women want to feel contractions. The labor epidural rate is approximately 60% in the United States. The majority of first-time mothers utilize neuraxial analgesia, whether or not that was part of their birth plan. Many women, particularly those who have had a baby before, those who have the support of a midwife, and those who have had good psychological preparation, do very well with minimal analgesia. However, others benefit enormously from neuraxial analgesia. Some women will be advised that a labor epidural is the safest option for them, particularly if they are at high risk of needing to be delivered by cesarean section or if they have particular medical conditions.
Labor Epidurals
General aspects of the procedure for siting an epidural are described in Chapter 16, Regional Anesthesia. The anesthesia provider must review the patient’s medical history and examine the patient, including her airway, heart, and lungs. The patient must give informed consent after review of complications such as dural puncture headache, temporary or permanent nerve injury, infection, and bleeding, as well as immediate risks such as hypotension. Full equipment for resuscitation must be available, including a bed capable of being put in the Trendelenburg position, suction apparatus, oxygen, and a code cart. Standard packs for epidurals, spinals, and CSEs are very helpful, as is a well-stocked, lockable mobile cart. The ASA Practice Guidelines for Obstetric Anesthesia suggest that laryngoscopes and assorted blades, endotracheal tubes and stylets, a self-inflating bag and mask, medication for blood pressure support, muscle relaxation and hypnosis, a carbon dioxide detector, and a pulse oximeter should all be available during the initial provision of neuraxial anesthesia. In view of the risk of local anesthetic systemic toxicity (LAST) when epidurals are dosed, intralipid should be available (see Chapter 63, Local Anesthetic Toxicity). The epidural cart must be checked regularly, restocked, and outdated drugs and equipment replaced.
Patients often have family members accompanying them during labor. If a family member is to accompany the patient during the procedure, it may be prudent to insist that they are seated because vasovagal episodes are common.
Good sterile technique is vital during epidural placement. The delivery room is a less sterile environment than an OR. Surfaces such as tables must be cleaned before use as a workstation. Handwashing with surgical scrub solution, caps, masks covering the nose and mouth, sterile gloves, individual packets of skin preparation, and sterile draping are all recommended. Chlorhexidine is preferred. A gown may be worn.
The patient must have a functioning intravenous cannula and should have received 500 mL of intravenous crystalloid to prevent hypotension. She is positioned sitting or in the lateral fetal position. Optimal positioning for epidural placement is important and can be difficult, both because of pain and difficulty keeping still and the gravid uterus, making it difficult for the patient to flex her lumbar spine. Monitoring will include noninvasive blood pressure and pulse oximetry.
Immediate Complications of Labor Epidurals
After placement of the epidural catheter, an initial test dose of lidocaine with epinephrine is usually given. Immediate complications associated with epidural placement include both predictable responses to dosing an epidural catheter with local anesthetic solution and complications caused by incorrect location of the epidural catheter. The test dose is intended to identify misplacement of the catheter. Local anesthetic placed in the epidural space anesthetizes pain fibers but also sympathetic nerve fibers, which maintain vascular tone. Even when the catheter is correctly located in the epidural space, the patient may develop hypotension secondary to blockade of sympathetic nerve fibers, and this may occur with the test dose or with subsequent doses of local anesthetic. Aortocaval compression is an important contributing factor and predisposes laboring patients to become hypotensive with regional anesthesia. Hypotension may cause maternal nausea and vomiting, but in most healthy women, the most serious effect is likely to be on the fetus. Altered uterine artery blood flow may cause fetal bradycardia. Rarely, if the fetal heart rate does not improve with changes in maternal position, oxygen, boluses of fluid, and drugs such as phenylephrine or ephedrine, the patient may need to be moved to the OR emergently for delivery by emergency cesarean section.
High or Total Spinal
Epidural catheters should always be aspirated to check for cerebrospinal fluid. However, occasionally, a catheter is inadvertently placed intrathecally (through the dura and into the subarachnoid space), and its misplacement is not suspected. If a test dose of 3 mL of 1.5% lidocaine with epinephrine is administered into the cerebrospinal fluid in the subarachnoid space, the misplacement will usually be obvious, with motor blockade, a higher sensory level than expected, and maternal hypotension. If intrathecal placement is not recognized and a large dose of local anesthetic is given, it is possible to develop a “high spinal” or “total spinal,” with severe hypotension, bradycardia, breathing difficulties or apnea, and loss of consciousness, as progressively higher spinal levels and ultimately the brain are anesthetized. This is an emergency requiring immediate measures to secure the airway, ventilate, restore blood pressure, and deliver the fetus. When immediately recognized, and if all essential airway and resuscitation equipment is immediately available, a total spinal should still have a safe outcome for mother and fetus. An unconscious obstetric patient who has stopped breathing should be ventilated with a mask and Ambu bag, and cricoid pressure should be applied while preparations are made for intubation. Epinephrine may be required for the treatment of hypotension, and atropine may be required for the treatment of bradycardia. Left uterine displacement should never be forgotten. Preparations should be made to transfer the patient to the OR for immediate delivery if there are signs of fetal distress. It should be noted that the upper limit of the epidural space is at the foramen magnum. A high epidural block will not anesthetize the brain, but high spinals can.
Intravascular Epidural Catheter Placement
An epidural catheter located in an epidural vein may become apparent when a test dose of local anesthetic with epinephrine is given. The patient is asked to report any symptoms she notices, and her heart rate is observed. An increase in maternal heart rate of more than 15 beats/min is considered a positive test because the intravenous epinephrine can raise the heart rate. However, heart rate changes with contractions are very common in labor, so the test dose may be less reliable in pregnancy. If local anesthetic is injected into a blood vessel instead of being slowly absorbed from the epidural space, LAST may occur. The major consequences of a toxic dose of local anesthetic are neurologic and cardiac. Early symptoms of local anesthetic toxicity include tingling of the lips or tongue, because of the high blood supply to this area, and ringing in the ears. Such early signs are not always present, and the presentation may be with seizures secondary to central nervous system toxicity, arrhythmias, or cardiac arrest. If a patient suffers a cardiac arrest, particularly after a dose of bupivacaine, advanced cardiac life support (ACLS) protocols should be followed, although resuscitation may need to be prolonged because bupivacaine binds tightly to cardiac myocytes. Intralipid is valuable in displacing bupivacaine from its binding sites on the heart and should be available.
Both the total spinal and LAST are life-threatening emergencies primarily prevented by careful “test dosing” and observation after the test dose, but either can happen with any epidural anesthetic. For this reason, one of the most critical functions of the anesthesia technician on the obstetric floor is frequent and regular checking of the emergency airway equipment, resuscitation and airway drugs in the mobile epidural cart, and the LAST and intralipid kit. Hopefully, items outdate time and time again without ever needing to be used.
Cesarean Section
Cesarean section is a very common operation, with 32% of babies currently delivered by cesarean section in the United States. Indications for elective cesarean section include prior cesarean section, breech presentation, twins, cephalopelvic disproportion, and maternal request. Indications for unplanned cesarean section include dysfunctional labor and fetal intolerance of labor, hemorrhage, and maternal medical conditions such as preeclampsia.
Regional anesthesia for cesarean section includes spinal, epidural, and combined spinal-epidural (CSE) techniques. General anesthesia is usually reserved for emergency situations when the life of the mother or fetus is in immediate danger and the fetus needs to be delivered as quickly as possible or situations when there is a contraindication to regional anesthesia.
Many units utilize a classification system to communicate regarding the urgency of cesarean sections. For example, a category 1 or red cesarean section indicates that there is an immediate threat to the life of the woman or fetus and that the fetus should be delivered as rapidly as is safely possible.
Spinal Anesthesia
Spinal anesthesia is also known as subarachnoid and intrathecal anesthesia. A detailed description of the procedure for subarachnoid anesthesia is given in Chapter 16, Regional Anesthesia. Spinal anesthesia is often the technique of choice for uncomplicated elective cesarean sections. The patient should have a freely running intravenous cannula of at least 18G. She will usually have already received 1 L of crystalloid to offset the anticipated vasodilation from a spinal, and she will receive a drink of sodium citrate to reduce the risk of aspiration pneumonitis. At a minimum, blood pressure and pulse oximetry are monitored during placement, which is often performed in the seated position. The obstetric team will monitor the fetal heart rate. Intrathecal local anesthetic, usually hyperbaric 0.75% bupivacaine, usually supplied in spinal anesthesia kits, is usually supplemented with opioid drugs, including fentanyl and preservative-free morphine. Obstetric patients are particularly prone to dural puncture headache; therefore, small-gauge Whitaker- and Sprotte-type needles (25G or smaller) are preferred.
The most common early complication of subarachnoid blockade is maternal hypotension. Cesarean section requires extensive dermatomal blockade to ensure maternal comfort during the surgery. The patient will develop a dense motor block, and on testing, the block level will often extend from the sacral dermatomes to as high as T2. There will also be a rapid-onset sympathectomy, sometimes accompanied by bradycardia as the cardiac acceleratory fibers are blocked. Left uterine displacement should be established. Blood pressure should initially be monitored frequently, and the ECG should be placed. Careful attention should be paid to the patient, who will often demonstrate perioral pallor or complaints of nausea, even before the blood pressure cuff confirms a drop in pressure. Alteration in uterine blood flow is a major concern. The fetus should be monitored during this time, and the response to developing hypotension should be prompt, because even small drops in maternal blood pressure can have detrimental effects on the fetus. Phenylephrine infusion is often started prophylactically. Spinal hypotension usually responds to fluid, phenylephrine, and ephedrine, and these should be readily available. Increasing left uterine displacement may be necessary.
Obstetric patients do not usually receive sedation, and it is important for all staff in the OR to be aware of this. It is common practice for the patient to have a support person of her choice accompanying her during cesarean sections performed under regional anesthesia. Visitors are not usually brought into the OR if the patient is to receive general anesthesia and will be asked to leave if the patient requires conversion to general anesthesia.
The extent and quality of the subarachnoid block are checked carefully before surgical incision. Delivery of the neonate usually proceeds promptly, although scarring and adhesions from prior procedures can slow delivery considerably. Following delivery of the baby, uterotonics will usually be given to help contract the uterus to prevent blood loss. Oxytocin is the drug most commonly used. A pressure bag or infusion pump may be useful.
Drug errors are a particular problem in obstetric anesthesia. Talking to the patient and her partner can be distracting for the anesthesia provider. Vomiting, hypotension, pain, or bleeding may require urgent interventions, which also make errors more likely. The anesthesia cart and anesthesia machine should be tidy and well organized at all times, and particular attention should be paid to routines intended to minimize the risk of errors.
Epidural Anesthesia for Cesarean Section
Epidural anesthesia is most commonly used for cesarean section in patients who have a functioning labor epidural in place. Epidural blockade can usually be rapidly extended to provide adequate anesthesia for cesarean section with administration of additional boluses of local anesthetic. In addition, an epidural catheter may be placed de novo in preference to a subarachnoid block for several reasons. Increments of local anesthetic can be given slowly, in a manner that minimizes the risk of severe hypotension. This is particularly important for patients who would not tolerate a rapid onset of sympathectomy, such as those with cardiac disease. Placement of an epidural catheter also allows the duration of neuraxial blockade to be extended, which is essential if a case is expected to be prolonged.
Combined Spinal Epidural
A CSE combines the benefits of both spinal and epidural anesthesia and is an excellent option for many patients. The spinal component can include a standard subarachnoid dose of local anesthetic or a smaller dose, which can then be extended as necessary using the epidural catheter, the advantage being less risk of hypotension than with a standard subarachnoid block, but quicker onset and denser sacral block than with an epidural. An additional advantage of the epidural catheter is that it can be used to extend the duration of block. The disadvantage of this technique is the increase in complexity. CSE techniques are used for both labor analgesia and for cesarean section.
General Anesthesia
General anesthesia is usually reserved for patients for whom regional anesthesia is contraindicated, and for emergencies necessitating very rapid delivery of the fetus, if the mother does not have a functioning epidural in place. Common examples of contraindications to regional anesthesia in obstetrics include cardiovascular instability, coagulation abnormalities, and sepsis. Examples of fetal emergencies include cord prolapse and abruption.
Preparation of equipment is vital to ensuring that general anesthesia can be provided to obstetric patients safely. General anesthesia may be used very seldom and difficult airway equipment even less often: one of the critical roles of the anesthesia technician is ensuring that machine, equipment, and supplies are always in good condition and full readiness for emergent general anesthesia with a potentially difficult airway or fiberoptic intubation. The anesthesia machine must be fully checked, including the breathing circuit, suction tubing, and suction apparatus. A common but potentially disastrous error is forgetting to replace suction tubing between cases. Airway equipment should be made available ahead of time including laryngoscopes, a choice of blades, oral and nasal airways, an intubating bougie, and endotracheal tubes. Endotracheal tubes of a smaller size than standard are usually chosen, because of the airway edema often occurring in pregnancy. For an average-size woman, a size 6.0 or 6.5 tube might be selected. For many anesthesiologists, video laryngoscopy (e.g., GlideScope, C-MAC) has become the technique of choice in situations where standard laryngoscopy is unsuccessful or appears likely to be difficult. Difficult airways are more common in the obstetric population. The rate of failed intubation after direct laryngoscopy is 1/300 compared to 1/3,000 in the general population. A difficult airway cart should be readily available. The ASA Practice Guidelines for Obstetric Anesthesia provide suggestions as to the contents of a portable storage unit, including alternative choices of rigid laryngoscope blades, laryngeal mask airways, endotracheal tube guides, retrograde intubation equipment, a device for emergency nonsurgical airway ventilation such as a supraglottic airway and a hollow jet ventilation stylet with transtracheal jet ventilator, fiberoptic intubation equipment, and emergency surgical airway access equipment, such as a cricothyroidotomy kit (see Chapter 57, Airway Emergencies). Preparation for airway emergency includes a protocol for an emergency surgical airway. Because the unanticipated difficult airway is a rare event in the obstetric suite, the anesthesia technician (who is likely to be experienced with airway equipment and assistance) can be an especially critical member of the team here.
Medications required for rapid sequence induction must be immediately available. Propofol and etomidate are both suitable agents. Ketamine is another option. Succinylcholine is the muscle relaxant of choice in most cases. Other emergency drugs such as atropine, epinephrine, ephedrine, and phenylephrine should also be readily available.
When the decision is made to proceed with emergency cesarean, achieving rapid, safe delivery of the fetus demands excellent teamwork. All personnel should be alerted promptly and should respond as quickly as possible. Many units utilize a team paging system for emergencies, which may include the anesthesia technician. A team effort to move the patient into the OR and onto the operating table rapidly and safely is important. During transfer, intravenous lines must be protected. The obstetric team may reassess the situation on arrival in the OR, including reevaluating the fetal heart rate tracing or repeating the vaginal examination, or may begin immediate preparation for cesarean section, including placing a urinary catheter, cleansing the abdomen with surgical antiseptic solution, and placing sterile drapes. During these preparations, the anesthesia team will proceed expeditiously, but without compromising safe anesthesia practices. Whenever possible, the anesthesia team will have seen and assessed the patient previously, although it may be necessary to perform a rapid history and examination. It is vital that the patient is properly positioned on the operating table, with her head on the adjustable headpiece and with elevation of her head and shoulders such as to achieve the “sniffing the morning air” intubating position. Proper patient positioning is especially important in pregnancy because of enlarged breasts, increased obesity, and increased incidence of difficult intubation. Left uterine displacement must not be omitted.
For most healthy women, induction of general anesthesia is accomplished with a rapid sequence induction with cricoid pressure. Pregnant women are assumed to have a full stomach. If they have been in labor, have received opioids, or have eaten, they are at particular risk of aspiration of gastric contents. Sodium citrate is given to reduce the acidity of stomach contents. Standard ASA monitors are applied and suction apparatus is placed within easy reach. The patient is preoxygenated. Preoxygenation is with four vital capacity breaths or 4 minutes of breathing 100% oxygen with a good seal around the mask on the patient’s face, as well as confirmation that capnography is working. To minimize exposure of the fetus to anesthetic gases, induction is delayed until the obstetrician is ready to make the skin incision, although surgery will not begin until induction is complete and the airway secured. Cricoid pressure is applied during induction of anesthesia and must not be removed except at the anesthesiologist’s request.
After induction, maintenance of anesthesia is usually with an inhalational agent at one-half minimum alveolar concentration (MAC), with 50% nitrous oxide until delivery of the fetus, and then 70% nitrous oxide. In pregnancy, the MAC for inhalational agents is reduced; it is desirable to minimize anesthetic effects on the fetus, and inhalational agents relax uterine muscle, which may increase bleeding. However, cases of awareness under anesthesia have been reported during cesarean sections. At the end of surgery, the patient can usually be extubated. Assessment of residual neuromuscular blockade is very important. The patient should usually be extubated fully awake, with intact protective airway reflexes, to minimize the risk of aspiration. The patient should be recovered in a safe location by qualified staff. The risk of airway complications is as high during emergence and recovery as on induction, with complications arising related to problems such as airway edema, bronchospasm, pulmonary edema, and residual muscle relaxation.
In the event of a failed intubation, the ASA’s difficult airway algorithm is adapted for obstetric patients to allow the anesthesiologist to take account of the needs of the fetus. In the event of a failed intubation, two questions determine what should happen:
1. Is surgery required for an emergency that is an immediate threat to the life of the mother or the fetus?
2. Is it possible to ventilate the patient?
In a situation other than an emergency posing an immediate threat to the life of the mother or the fetus, if possible, the patient will be woken up, and either intubated awake using advanced airway techniques or a regional technique will be employed. The increased risk of aspiration in obstetric patients makes awake fiberoptic intubation preferable to asleep fiberoptic intubation in most cases.
If the patient can be ventilated using a mask and airway or laryngeal mask airway, in a life-threatening emergency situation, it is acceptable to proceed with the surgery, maintaining cricoid pressure if that does not interfere with ventilation. If the patient cannot be ventilated with optimal techniques and cannot be woken up, an emergency surgical airway will be necessary. Equipment for emergency cricothyroidotomy and jet ventilation should be available.
Other Obstetric Emergencies
Emergencies in the context of emergency cesarean section have been discussed, as have emergencies related to epidurals. In this section, seizures, hemorrhage, embolic events, and cardiac arrest will be considered. Hypertensive disorders, hemorrhage, and embolic disorders are major direct causes of maternal mortality and may present as these types of emergencies on the delivery suite.
Seizures
Seizures occurring in obstetric patients may be caused by eclampsia, although epileptic seizures are also common. Eclampsia is a condition that only occurs in pregnancy and the postpartum period. A seizure may be the first sign of the disorder, although it is frequently preceded by preeclampsia, which is defined as hypertension and proteinuria occurring after the 20th week of pregnancy. In severe preeclampsia, there are signs and symptoms of end organ damage in multiple organ systems, including the central nervous system, which may progress to seizures. Severe hypertension in itself may be an emergency requiring immediate management with intravenous medication and occasionally invasive monitoring. The treatment of eclampsia is oxygen, airway support as necessary, and magnesium. Magnesium is very effective in stopping eclamptic seizures and particularly in preventing a second seizure. Eclamptic seizures are usually self-limiting. Intubation is not usually required, although airway equipment should be available and prepared. Benzodiazepines are the first-line drugs in epileptic seizure management but are usually avoided in eclampsia because they increase postictal sedation and increase the risk of airway complications.
Hemorrhage
Hemorrhage in obstetric patients can be catastrophic. Hemorrhage is classified as antepartum or postpartum (before and after delivery, respectively). Antepartum causes of hemorrhage include abruption, when the placenta separates prematurely from the wall of the uterus; placenta previa, where the placenta is abnormally situated over the cervical opening; and uterine rupture. Postpartum hemorrhage may be caused by uterine atony or retained placental products or blood clots, which prevent the uterus from contracting down in the usual manner, leaving large blood vessels open and bleeding. By the end of pregnancy, the blood flow to the uterus is increased to 1 L/min. After delivery of the placenta, the uterus must contract to cut off its blood flow. If this does not happen rapidly, hemorrhage can be catastrophic. Hemorrhage may be the presenting problem when a patient arrives emergently at the hospital, may develop unexpectedly during or after cesarean section, and may occur unexpectedly after a normal vaginal delivery.
The expected blood loss after a vaginal delivery is 500 mL, with 1,000 mL at cesarean section. Unusually, rapid bleeding, or more than 700 mL or 1,200 mL, respectively, should prompt preparation for management of massive hemorrhage (see Chapter 62, Massive Hemorrhage). Equipment for the management of massive hemorrhage must be assembled quickly. It will be a matter of local policy what equipment is kept on the delivery suite vs in a central location.
Additional intravenous access must be secured promptly. Equipment for arterial and central line placement and monitoring should be available, including an ultrasound machine. In some cases, very large-bore access, such as introducers for pulmonary artery catheters or trauma lines, are required. A rapid infusion device may be necessary. Intravenous fluid warmers and a forced-air body warmer should be available and applied early to prevent hypothermia. Blood should be immediately available, including O negative blood. Good communication with the transfusion service is vital. In cases of massive hemorrhage, obstetric patients can rapidly develop coagulation abnormalities. Standardized transfusion regimes, such as 6:6:1 bags of red cells, fresh frozen plasma, and platelets, are recommended. The use of the cell saver has been limited in obstetrics because of concerns regarding the infusion of amniotic fluid particles, although it is becoming more widely used. It appears that cell savers can be used safely in obstetric patients, providing amniotic fluid is suctioned away from the field and the field is thoroughly irrigated first. An additional leukocyte depletion filter may be used as well. Cell savers may also be helpful in Jehovah’s witnesses who decline other blood products.
In cases of uterine atony, drugs used to improve uterine contraction include oxytocin, methylergonovine (Methergine), misoprostol, and prostaglandin F2alpha (Hemabate). Embolization of a uterine artery can be an effective way of halting obstetric hemorrhage. In this case, the patient may need to be transferred to the interventional radiology suite. An anesthesia machine should be prepared in that location along with monitoring equipment and equipment for managing hemorrhage, while preparations are made to transfer the patient. In some cases, the obstetrician may need to perform a hysterectomy to control hemorrhage. When the likelihood of massive hemorrhage is high, or if a patient develops massive hemorrhage after leaving the obstetric unit, management in the main operating suite may be preferable, if staffing and equipment are more easily accessible.
In some cases, the placenta may be known to abnormally adhere to the uterine wall and may even invade the uterine muscle or other organs. This is known as placenta accreta, increta, or percreta, with placenta percreta being invasion of other organs such as the bladder or bowel. This may necessitate a planned cesarean hysterectomy, which may be scheduled in a main OR location.
Embolism
Venous thromboembolism is more common in obstetric patients because of changes in coagulation factors during pregnancy, as well as mechanical obstruction of venous return by the pregnant uterus. Pulmonary embolus may present as chest pain, shortness of breath, or even cardiac arrest at any stage of pregnancy, with a particular risk in those with abnormal blood clotting and after cesarean section.
Amniotic fluid embolus is specific to pregnancy. Classically, this is described as sudden cardiovascular collapse, cyanosis, mental status changes, or massive hemorrhage in a parturient with forceful contractions, although it can occur at any time. Fetal cells from amniotic fluid are forced into the maternal circulation and can be found in the pulmonary vascular bed postmortem. The condition has a very high mortality for both mother and fetus. More recent research suggests that there may be an anaphylactoid response to amniotic material, rather than a mechanical obstruction of blood vessels. Treatment of amniotic fluid embolus includes management of cardiac arrest and support of the cardiovascular system, delivery of the fetus, management of hemorrhage, and support of the cardiovascular system. The patient is likely to require full invasive monitoring and ICU care if she survives the acute event.
Cardiac Arrest in Pregnancy
Cardiac arrest is rare in pregnancy. Causes include underlying cardiac disease, embolic disease, massive hemorrhage, anaphylaxis, and toxic doses of local anesthetic. In an obstetric patient, ACLS guidelines should be followed, but in addition, left uterine displacement should be instituted immediately. Aortocaval compression by the gravid uterus severely impairs venous return to the heart and hinders successful resuscitation. The outcome for the fetus is likely to be poor. However, to improve the chances of survival for the mother, the fetus should be delivered if a perfusing rhythm has not been reestablished after 4 minutes. To deliver the fetus rapidly, it should be possible to perform a cesarean section at the bedside, calling for personnel and the cesarean section tray as quickly as possible.
Other Emergencies
Any anesthesia or medical emergency may occur in the delivery suite. Plans should be in place for dealing with rare emergencies such as malignant hyperthermia. Isolated units must be stocked with equipment such as a malignant hyperthermia cart, if it cannot be easily and quickly fetched from elsewhere.
Summary
Obstetric emergencies can be extremely difficult to manage. This is because of the rapidity with which a situation can change from routine to emergency and error to care for two patients simultaneously, the mother and the fetus. As mentioned previously, anesthesia technicians are important members of the anesthesia team. All technicians who may be called to assist with a procedure or emergency in the obstetric suite should be familiar with the general layout, anesthesia machine, airway equipment, and vascular access equipment available in the obstetric suite. This is especially true if the anesthesia technician only occasionally works in the obstetric department.
Obstetric anesthesia is a very rewarding specialty area in which to work. The anesthesia technician can be of great assistance as part of the anesthesia team, particularly by ensuring that equipment is well stocked and maintained and by responding rapidly to emergencies as they arise. Obstetric emergencies often arise rapidly, may be unpredictable, and can be life threatening for both the mother and fetus. Managing these events requires thorough preparedness and excellent teamwork.
Review Questions
1. As an anesthesia technician in an obstetric unit, you should expect all of the following except:
A) Access to the OR at any hour of day or night.
B) Decision-to-incision interval less than 15 minutes.
C) Adequate anesthesia coverage and technical support 24/7.
D) Anesthesia providers may not always be in-house at night.
E) None of the above.
Answer: B
Although in certain life-threatening situations delivery of the neonate within 10-15 minutes improves outcomes, the standards set by the American College of Obstetricians and Gynecologists, the American Society of Anesthesiologists, and the Joint Commission dictate that the decision to incision interval be less than 30 minutes, not less than 15 minutes. Obstetric units should always provide adequate anesthesia coverage and technical support, and you should always expect to have access to the OR, regardless of time of day. However, in rural areas and/or at small hospitals, there may not be an anesthesia provider in-house at night.
2. A woman in labor has an epidural catheter and is being prepared for a cesarean section delivery, when she begins complaining of ringing in her ears. You should be most concerned that what is occurring?
A) Epileptic seizure; ringing in the ears is a symptom of seizures
B) High spinal, because the epidural catheter may be intrathecal
C) Hypotension, because the block is setting up quickly
D) Early signs of local anesthetic systemic toxicity (LAST), because the epidural catheter may be intravascular
E) Cardiac arrhythmia due to local anesthetic
Answer: D
Early symptoms of local anesthetic toxicity include tingling in the lips and ringing in the ears. LAST may develop into seizures secondary to CNS toxicity, arrhythmias, or cardiac arrest. Signs of high spinal are hypotension, bradycardia, breathing difficulties and/or apnea, and loss of consciousness. Hypotension often causes nausea and/or vomiting.
3. Which of the following statements regarding tracheal intubation during pregnancy is FALSE?
A) The rate of failed intubation is increased.
B) Rapid sequence induction with cricoid pressure is usually used.
C) The risk of airway complications is higher during emergence and recovery than induction.
D) In the event of a failed intubation, the anesthesia provider will attempt to awaken the patient, given that the mother and fetus are not in immediate danger.
E) After induction, maintenance of anesthesia is usually with an inhalational agent at one-half minimum alveolar concentration (MAC), with 50% nitrous oxide until delivery of the fetus, and then 70% nitrous oxide.
Answer: C
The risk of airway complications is just as high during emergence and recovery as they are during induction. In pregnant women, the rate of failed intubation is increased. In the event of a failed intubation, the anesthesia provider will attempt to awaken the patient, as long as the mother and fetus are not in immediate danger. Rapid sequence induction with cricoid pressure is usually used; after induction, maintenance of anesthesia is usually with an inhalational agent at one-half MAC, with 50% nitrous oxide until delivery of the fetus and 70% nitrous oxide after delivery.
4. Identify the incorrect statement about obstetric emergencies.
A) Magnesium is used to stop and prevent eclamptic seizures.
B) You should begin preparation for management of massive hemorrhage if blood loss exceeds 700 mL after vaginal delivery or 1,200 mL after cesarean section.
C) Pulmonary embolus is described as sudden cardiovascular collapse, cyanosis, mental status changes, or massive hemorrhage.
D) Recent research suggests that for cases of amniotic fluid embolus, there may be an anaphylactoid response to amniotic material, rather than a mechanical obstruction of blood vessels.
E) In the event of a cardiac arrest, the fetus should be delivered if a perfusing rhythm has not been reestablished after 4 minutes.
Answer: C
The symptoms listed in (C) above describe amniotic fluid embolus, which is unique to pregnancy. Pulmonary embolus instead marked by chest pain, shortness of breath, or cardiac arrest.
5. Blood flow to the pregnant uterus around the time of delivery is
A) 500 mL
B) 1,000 mL/min
C) Reduced by left uterine displacement
D) Directly monitored by fetal cardiotocography
Answer: B
Blood flow to the pregnant uterus is as high as 1,000 mL/min at term; thus, obstetric hemorrhage can be very rapid. (Flow is measured as a volume per unit time, e.g., mL/min.) Typical blood loss at vaginal delivery is 500 mL. Uterine blood flow is increased by left uterine displacement, which moves the uterus off the inferior vena cava and aorta and permits increased perfusion to the lower half of the body, including the uterus. Cardiotocography monitors fetal heart rate and uterine contractions; fetal heart rate patterns are associated with changes in fetal and/or placental, but not necessarily uterine, perfusion. Uterine contractions are also not reflective of uterine blood flow.
SUGGESTED READINGS
American Society of Anesthesiologists Task Force on Infectious Complications Associated with Neuraxial Techniques. Practice advisory for the prevention, diagnosis, and management of infectious complications associated with neuraxial techniques: a report by the American Society of Anesthesiologists Task Force on infectious complications associated with neuraxial techniques. Anesthesiology. 2010;112(3): 530-545.
American Society of Anesthesiologists Task Force on Obstetric Anesthesia. Practice guidelines for obstetric anesthesia: an updated report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia. Anesthesiology. 2007;106:843-863.