CHAPTER 57
Airway Emergencies
Introduction
Airway emergencies encompass a broad group of situations. They may be anticipated or arise unexpectedly. They may be due to the patient’s normal anatomy, a disease, or the procedure the patient is undergoing. They are always a challenge and require excellent team dynamics to prevent patient injury.
The American Society of Anesthesiologists has created practice guidelines for difficult airway management (Fig. 57.1). The guidelines were first published in 1993, as a result of an analysis of lawsuits against anesthesiologists pointing to numerous poor patient outcomes related to the inability to successfully obtain or maintain an airway. The guidelines were then revised and republished in 2003 and 2014. These guidelines help the anesthesiologist think proactively about factors that predict a patient might have a difficult airway, what to consider when creating a plan to manage the airway, and what to do if difficulties during airway management are encountered. They are guidelines and not standards—which means that they are recommendations for practice, not rules. The individual anesthesiologist may use his or her own judgment about how any individual patient may be appropriately treated and whether the patient condition or situation is best suited for following the guidelines or a different course of action.
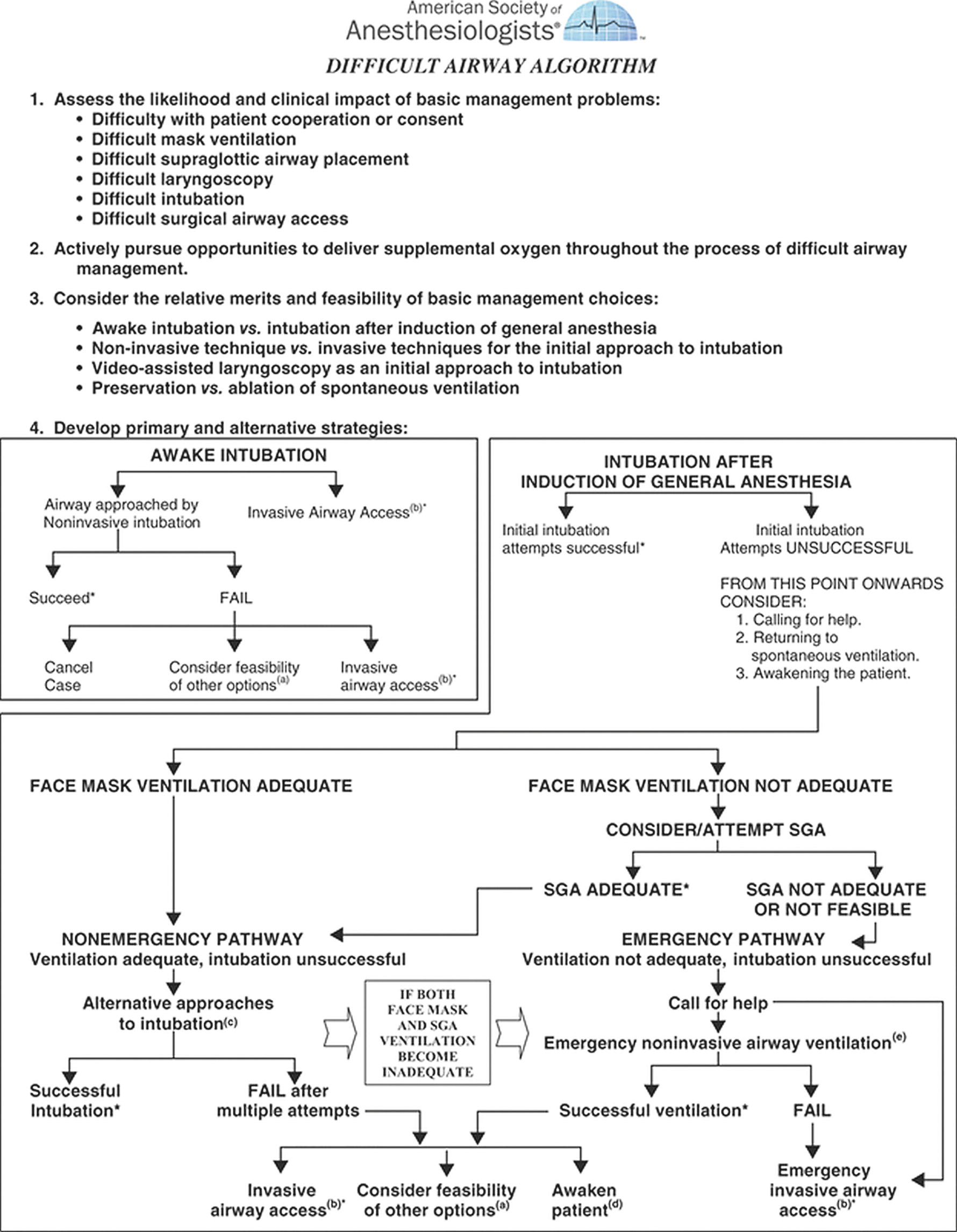
FIGURE 57.1. ASA Difficult Airway Algorithm 2013. (From Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118(2):251-270. doi: 10.1097/ALN.0b013e31827773b2.)
It is important that the anesthesia technician be intimately familiar with these guidelines as well; this familiarity will help the technician anticipate what equipment or maneuvers may be needed during management of a difficult airway. Can you have a key piece of equipment prepared and ready to be handed in before the anesthesia provider even asks for it? The first part of this chapter will focus on reviewing the ASA Difficult Airway algorithm.
Preparation
The first step in the algorithm is to evaluate the patient for potential difficulty with ventilation or intubation. This will include a history and physical exam looking for indicators that would suggest difficulty. For example, could there be difficulty with patient cooperation? Children, individuals with developmental delay, or intoxicated patients may be unable to cooperate with particular airway management techniques (starting an IV, awake fiberoptic intubation, etc.). Predictors of difficult mask ventilation include presence of a beard, obesity, absence of teeth, and history of sleep apnea. Predictors of difficult supraglottic airway placement include limited mouth opening and intraoral abscess. Predictors of difficult intubation include limited mouth opening, large tongue, limited neck extension, inability to push the mandible forward, or previous history of difficult intubation. The greater the number of these predictors that are present, the higher the risk. Additional factors that could make ventilation or intubation difficult and can even make establishing a surgical airway difficult include the presence of infection, a tumor, surgical changes in the neck, or any other condition that displaces the trachea or alters landmarks on the surface of the neck. Identifying potential problems in any of these areas will affect how the anesthesiologist plans for airway management. It is also important to realize that these factors are not 100% successful in predicting that a patient will be easy or difficult to mask ventilate or intubate. Every anesthesiologist has been uncomfortably surprised by the patient anticipated to have an easy airway but turned out to be difficult to ventilate or intubate.
The second step in the algorithm is the admonition to pursue the delivery of oxygen at all times during the process of airway management. One might think that this would be intuitively obvious; however, the task force recognized that there were many instances of patient harm that resulted from a failure to provide oxygen. The astute anesthesia technician can be watching for opportunities to facilitate oxygen delivery, such as holding the mask for preoxygenation or offering to place a mask with blow-by oxygen during a fiberoptic intubation.
The third step is developing a plan for airway management, and the algorithm asks the anesthesiologist to consider three steps in particular about the plan. First, the anesthesiologist needs to decide whether airway management should proceed awake or asleep. This will depend on several conditions, such as whether the patient is anticipated to have difficulty with both intubation and ventilation and whether the patient is able to cooperate. The second step is to decide whether the patient should have a noninvasive or invasive approach planned.
Invasive in this setting refers to a surgical airway, such as cricothyrotomy or tracheotomy. The task force specifically called out invasive airways because they wanted to remind practitioners to consider them as a legitimate first step in airway management. These procedures can be remarkably well tolerated by awake patients with good numbing techniques; however, many anesthesiologists are reluctant to consider these options and attempt other airway techniques first. In some situations, other techniques are not likely to succeed, and when an invasive airway becomes necessary, it is a true emergency and is much more difficult to perform than in the controlled circumstances that may have been present at the beginning of the airway management process. Noninvasive techniques include, essentially, every other usual anesthetic technique. Specifically, the guideline suggests considering whether video laryngoscopy (e.g., GlideScope® or CMAC) should be used as the initial method of intubation. The final step in planning airway management is deciding whether to maintain spontaneous ventilation, or in other words, should the patient be paralyzed or not? This will depend on the difficulty of anticipated mask ventilation. If difficulty with mask ventilation and intubation is anticipated, it is unwise to take away the patient’s ability to breathe on their own.
Plan Execution
Awake Intubation
The next boxes in the algorithm have to do with the actual execution of the plan. Box 4A is used if the initial attempt at establishing an airway is performed with the patient awake. Most often, this will be with a noninvasive technique such as fiberoptic bronchoscopy or video laryngoscopy such as GlideScope®. This will require numbing the airway with local anesthetic to make the procedure tolerable. There are many ways of doing this, and frequently, an atomizer is used to assist. The anesthesia technician may be helpful in both preparation of the equipment, such as setting up the fiberoptic scope loaded with an endotracheal tube, as well as with reassuring the patient during the procedure.
Alternatively, an invasive technique may be appropriate. Either the surgeon or anesthesiologist may perform an invasive airway, although if it is planned, it is more commonly performed by a surgeon. Hopefully, the planned technique is successful, but if it is not, there are three options outlined in the algorithm. First, give up and cancel the case. Send the patient home, let any swelling or bleeding resolve, and the patient will live to see another day. Second, consider whether the case could be done under regional anesthesia or with a supraglottic airway instead of intubating. Third, if it is an emergent case that requires a tracheal tube, an invasive technique might be used if it has not been attempted already.
Asleep Intubation
Box 4B describes the airway management plan for those patients starting out with general anesthesia. Usually, the result will be successful intubation without difficulty. However, intubation may be difficult in approximately 5.8% of cases. If initial attempts are unsuccessful, the anesthesiologist can try using a different laryngoscope or blade, changing the patient position, or even having a more experienced anesthesiologist perform the intubation. If difficulty persists, the algorithm asks the anesthesiologist to consider three things: (1) Call for help (anesthesia technicians should respond to calls for help in the operating room and be prepared to bring in equipment or lend a hand), (2) allow the patient to return to spontaneous ventilation, and/or (3) awaken the patient. These latter two choices will be dependent in part on which drugs and how much of them the patient has received. Rapid reversal of nondepolarizing paralytics with Sugammadex® may make it possible to regain spontaneous ventilation even if a patient has been paralyzed.
In between attempts to intubate, the anesthesiologist should try mask ventilation to maintain oxygen saturation. If mask ventilation is adequate and oxygenation can be maintained, even though there is difficulty intubating, the situation is not an emergency. Oxygen can be provided to the patient and carbon dioxide can be breathed out effectively if mask ventilation is working well. This means there is time to get additional equipment, such as fiberoptic bronchoscopes or other difficult airway equipment ready and available. Unfortunately, it is possible that mask ventilation may get more difficult over time, and so it is still important to move expeditiously. Both mask ventilation and intubation may also become progressively more difficult with each laryngoscopy attempt, if swelling or trauma occur; thus, each attempt must be chosen judiciously. In addition, patients at risk for aspiration are particularly vulnerable during this period before an endotracheal tube is successfully placed. There are a myriad of different options available for intubating at this point in the algorithm, such as fiberoptic intubation with either a rigid scope or flexible bronchoscope, retrograde wire intubation, or intubation through an LMA. These options are each discussed fully in other chapters (see Chapters 18, Airway Management; 39, Airway Devices; and 40, Airway Tools).
If mask ventilation is not effective, the situation rapidly becomes emergent. Steps to attempt to make mask ventilation work may include nasal trumpets, oral airways, or two-handed holding of the mask with an assistant to “squeeze the bag.” The anesthesiologist may need to focus both hands on opening the airway and achieving a good mask ventilation seal, and the anesthesia technician may be called upon to squeeze the ventilation bag if the anesthesia provider is using both hands to hold the mask. Proper manual ventilation with the bag should, ideally, employ pressures of less than 20 cm H2O and a rate of about 10 breaths/min, achieving tidal volumes of approximately 8 mL/kg. Most important however is that the chest visibly rise and fall and that some capnograph waveform be visible. Pulse oximetry is not a good measure of current ventilation; it indicates that the patient was receiving oxygen a few minutes ago and that the blood is still oxygenated from that period of time (see Chapter 7, Respiratory Anatomy and Physiology).
If these steps are not successful, then the next step suggested by the algorithm would be a supraglottic airway (e.g., LMA™) placement. The airway should be sized appropriately for the patient. It may be a supraglottic airway of any type, although there may be a preference toward a supraglottic airway that allows subsequent intubation without removing the airway (e.g., intubating laryngeal masks). However, there should be no delays in looking for one type of supraglottic airway over another in this critical situation. If ventilation is effective through the supraglottic airway, then there will be many sighs of relief as the situation then becomes nonemergent again.
Without successful ventilation, the patient’s life is in danger; this is when the difficult airway has become a true emergency. One of the most frightening experiences in an anesthesiologist’s career is dealing with the “cannot ventilate, cannot intubate” scenario. If no further oxygenation or ventilation happens in the next few minutes, the patient will die. The algorithm prompts the practitioner to call for additional help at this point. The anesthesiologist may attempt a different noninvasive technique for ventilation (though this has likely been attempted already) while preparing to proceed to an invasive airway.
Invasive Airway Techniques
Transtracheal Jet Ventilation
Transtracheal jet ventilation is best accomplished by advancing a catheter into the cricothyroid membrane. There are catheters that are specifically designed for this use and have the benefit of being wire reinforced to prevent kinking. However, if one is not immediately available, the largest available peripheral IV catheter may be used (e.g., 14 g). The catheter can be connected to a jet ventilator if readily available. The jet ventilator will need to be connected to oxygen and should be set to deliver oxygen at 50 psi (wall pressure). In nonemergent settings, the pressure should start lower, such as 25 psi, but in emergencies, the goal is to get oxygen into the patient as quickly as possible. The jet ventilator should be held on for one second and then off for one second, watching the chest rise and fall with each insufflation and exhalation. It is possible that there is an obstruction in the airway making it difficult to intubate or ventilate, and that obstruction could mean that the patient will have difficulty exhaling with the jet ventilation. If that is the case, you may not see the chest falling easily after a breath is administered. Further breaths should not be forced in if this is occurring as it may cause damage to the lungs. For this reason, jet ventilation is losing favor as an invasive method.
Cricothyrotomy
Cricothyrotomy is the placement of a tube into the cricothyroid membrane and is the preferred approach in an emergency because the landmarks are easier to find and the thyroid and cricoid cartilages hold the airway relatively stable. There are commercial kits that are sold to facilitate cricothyrotomy, such as the Melker Emergency Cricothyrotomy Kit®. These kits frequently have a needle and wire system. If there is time to do so, the skin of the neck can be prepped with chlorhexidine or alcohol. The needle is used to puncture the cricothyroid membrane. The wire is placed through the needle, much like when performing a central line. The needle is removed and a dilator and tracheal tube are slid over the wire into the airway. The tracheal tube can then be used for ventilation exactly like an endotracheal tube.
A special kit is not necessary and may not be available. The minimum required is a scalpel and any endotracheal tube. A vertical incision is made at the center of the neck through the skin to expose the larynx and hopefully avoid most of the blood vessels in the area. A horizontal incision may then be made through the cricothyroid membrane. The handle of the scalpel can be used to dilate the incision and hold it open, although it is helpful to have a cricoid hook to hold the trachea open if possible. A small endotracheal tube (6.0) can then be placed into the trachea and used to ventilate the patient. It will later need to be revised to a more permanent solution, but this can be used to save someone’s life in an otherwise dire situation. Many practitioners feel that this is the optimal way of establishing ventilation quickly in a true “cannot ventilate, cannot intubate” scenario, given that any upper airway obstruction is completely bypassed.
Difficult Airway Cart
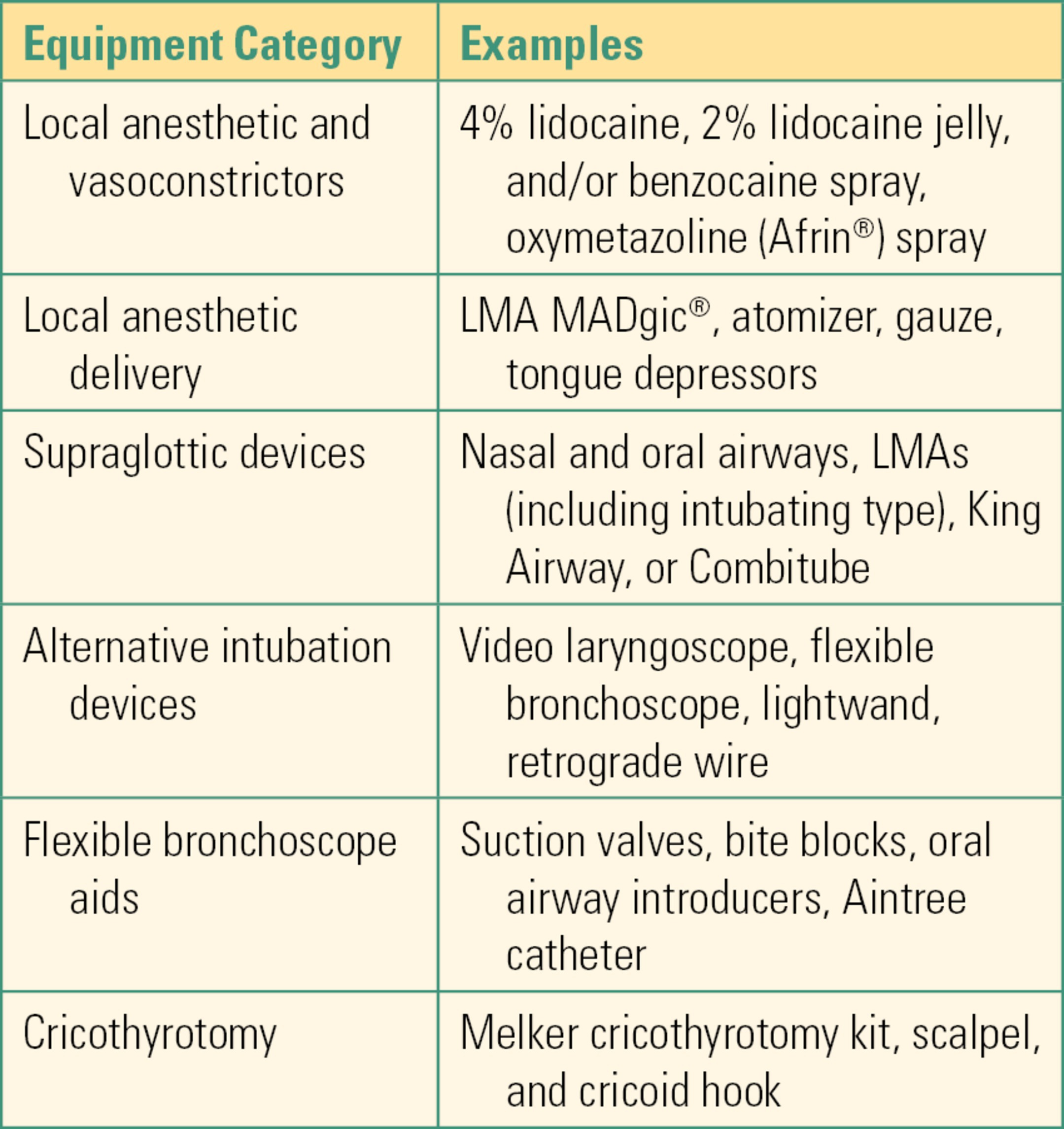
Equipment for managing an airway emergency is typically kept together in a mobile cart that can be easily transported in an emergency. Like a “code cart,” the difficult airway cart should always be kept stocked and available to travel to unpredictable, life-threatening events rather than serving as a daily source of airway equipment that may become depleted. Carts vary between institutions and come in different sizes depending on the equipment included. The cart should have a variety of equipment useful in a difficult airway emergency. Examples of carts can be found in Figure 57.2A and B, and typical drawers from one cart are shown in Figure 57.3. Carts can have many different organizations but in general will need to include (1) at least one supraglottic airway (e.g., LMA, King) in multiple sizes, (2) at least two options other than direct laryngoscopy for intubating (most commonly video laryngoscopy, flexible fiberoptic bronchoscopy), (3) items to help topicalize the airway for awake intubation, and (4) items to perform invasive percutaneous access of the airway (cricothyrotomy, transtracheal jet ventilation). Both the carts shown have LMAs to help with ventilation, as well as to intubate through, video screens capable of being used with flexible fiberoptic bronchoscopes as well as video laryngoscopes, items useful for topicalization, as outlined in Table 57.1, and Melker cricothyrotomy kits.


FIGURE 57.2. A, B: Two examples of difficult airway carts. Note that each has video equipment and clearly labeled drawers. Cart “A” also has its standard location marked, and a seal to mark that it is fully stocked, indicating that it is for emergency use only.

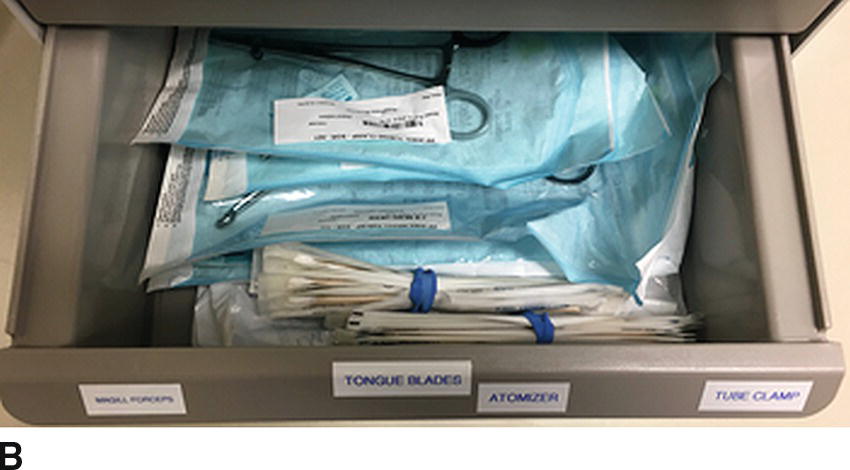
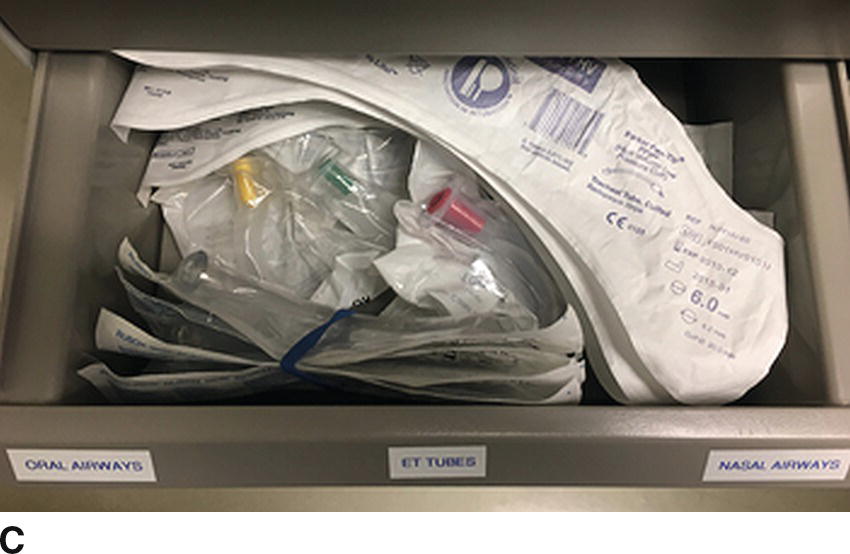
FIGURE 57.3. A-C: Sample contents of difficult airway cart.
Table 57.1. Difficult Airway Cart contents
Special Diseases or Procedures
There are a few diseases and procedures that deserve special mention for their potential impact on airway management.
Airway Diseases
Two diseases are of particular note to the anesthesiologist as they are indications to come to the operating room (OR) for intubation. First, patients presenting with epiglottitis (an infection of the epiglottis where it becomes swollen and can obstruct the airway) and need intubation are treated as true difficult airways. These patients come to the OR for intubation emergently because of the high likelihood of needing a surgical airway. They are often mostly obstructed already, and sitting up, working hard to breathe. In children, the preferred approach is usually a mask induction and intubation after the patient is asleep either with fiberoptic bronchoscopy or laryngoscopy. All attempts are made to keep the child calm without medication prior to induction in order to prevent worsening of the airway obstruction. This may include bringing a parent to the operating room or not placing an IV until after induction. If the parent is present, a clear path to the door needs to be made so they can exit rapidly after induction. The patient is left in the sitting position until after induction. In adults, fiberoptic bronchoscopy either awake or asleep may be performed. In both children and adults, a surgeon will be ready to perform a surgical airway should there be any difficulty.
Similarly, the patient with infection of the tissues around the airway is also of great concern. The infection may be around the jaw or neck (called Ludwig angina) or in the back of the throat (retropharyngeal abscess). In all cases, the concern is that the airway will not only be difficult because of swelling distorting the anatomy but also be potentially more difficult to anesthetize for an awake fiberoptic intubation because of the infection. Additionally, if the wall of an infection is disrupted, pus can drain into the lungs and cause fatal pneumonia. Fiberoptic intubation or a surgical airway are the most common methods of intubation.
Airway Procedures
Surgical procedures involving the airway present special challenges for the anesthesiologist. One example is tracheal dilation for tracheal stenosis. In this case, a stenosis (tightening) of the trachea is known to make it difficult to pass air, and it may be impossible to pass an endotracheal tube through. This is usually known prior to the patient arriving in the OR, and appropriate plans, often including ventilation and dilation via surgical rigid bronchoscopy, may be made. Another example is bleeding in the airway. Any procedure or condition in the pharynx or lower airway that results in bleeding can make intubation, or reintubation if the airway is lost, especially difficult. For example, a patient having dental extractions or a tonsillectomy who has an inadvertent extubation during the procedure may have copious blood and secretions, and potentially gauze, in the airway that can make reintubation difficult. These can rapidly turn into very serious airway emergencies. Any surgical procedure involving the airway mandates close communication between surgical and anesthetic teams, and equipment (circuits, ventilation devices) may be shared between teams.
Finally, any procedure not involving an intubated patient may be complicated by laryngospasm, which is a spastic closing of the vocal cords causing obstruction of the airway. The airway obstruction can be life threatening if not treated promptly. Patients whose depth of anesthesia is not matched to the stimulation of the procedure, or during induction (going to sleep), or emergence (waking up) are at risk for laryngospasm. During light planes of anesthesia, airway sensitivity and reactivity have not been completely abolished and any stimulation in the pharynx can cause laryngospasm. The stimulus can be something as innocuous as saliva. Although laryngospasm is more common in the pediatric patient, it also may occur in adults. Emergency treatment for laryngospasm includes stopping any stimulus to the patient, applying continuous positive pressure via face mask, and deepening the anesthetic with rapid-acting intravenous agent (e.g., propofol). If these fail, immediate muscle relaxation to paralyze the vocal cords and cause them to relax with succinylcholine may be required, via IV, if present, or even by intramuscular injection. The anesthesia technician may be asked to help with medications in an emergency if the anesthesiologist’s hands are needed holding positive pressure. Because pediatric patients are at such high risk for laryngospasm at induction and emergence, many pediatric operating rooms have a practice of not stimulating small children during the critical periods of induction and emergence.
Most airway management occurs in the controlled setting of the operating room. When airway emergencies occur, all the resources are available, and usually, the difficulty has been anticipated and a plan is in place. This is not true of airway emergencies outside of the operating room environment. Anesthesiologists may be called to intubate patients suffering cardiac arrest on the hospital ward, patients who have come to the emergency room with trauma, or patients whom have been undergoing procedures and have suffered respiratory arrest. Intubations outside of the OR are associated with a twofold increased risk of difficult airway. These situations are particularly challenging for many reasons. First, the patients are critically ill either from underlying disease or trauma or have been made ill from the procedures or drugs being done to them. This may influence which medications can be used to facilitate airway management. Second, other providers may have attempted to intubate and failed prior to the arrival of the anesthesiologist. These attempts can result in swelling or bleeding making subsequent attempts at intubation far more difficult. Third, the patient is very infrequently optimally positioned for airway management. For example, the patient receiving chest compressions will by necessity be flat on their back and moving with the compressions. Fourth, there is rarely specialized equipment available for intubation, such as fiberoptic scopes, as it is prohibitively expensive to have them everywhere in the hospital. Therefore, anesthesia technicians may receive urgent calls from an anesthesiologist asking them to bring equipment for difficult intubation to other places in the hospital. The anesthesia technician should be familiar with the hospital location and what resources may be required there and prepared to assist in this more hazardous environment.
Team Dynamics
As mentioned previously, there are very few situations that are as frightening as a true airway emergency. During an airway emergency, one of the obvious roles of the anesthesia technician will be to help facilitate getting equipment available and ready for use. This may include airway management equipment such as the fiberoptic bronchoscope and may also include IV equipment for the pediatric patient or patient rushing to the OR for airway management. It is important to maintain clear communication with the people in the room during this emergency (see Chapter 56, Simulation and Crisis Resource Management). That specifically means using closed-loop communication by acknowledging and repeating back what you are asked to do. For example, if you are asked to set up the fiberoptic scope, say, “OK, I’m setting up the adult fiberoptic bronchoscope.” Another version of this is the clarifying question. An example of this is if you are asked for an LMA, you might respond, “What size LMA?” or “Is a size 3 LMA OK?” as you are reaching for it.
All team members should feel empowered to make observations or suggestions. In an emergency, there are only so many things one person can pay attention to at once. This means that on occasion, the anesthesiologist focused on an airway emergency may not notice important information. For example, the anesthesiologist may be trying to complete a difficult fiberoptic intubation and the oxygen saturation goes from 99% to 70%. It might be that the anesthesiologist does not notice that the oxygen saturation has dropped to a very low level, or he or she may not be able to look away to the monitor to see what the saturation is. Either way, it may be helpful to her to have a team member such as the anesthesia technician say, “The sat is 70%.” Or if you notice the EKG suddenly looks different, alert the anesthesiologist to the change by saying, “The EKG looks different.” Certainly, the anesthesia technician is not primarily responsible for monitoring the vital signs, but if you do notice something, it may be valuable information for the anesthesiologist. A good team leader needs other team members to contribute their ideas in order to function optimally as a team.
Summary
In summary, airway emergencies are fortunately rare. This is in large part due to careful preparation and planning by the anesthesiologist. However, when the inevitable emergency does occur, it is necessary to act quickly to restore the airway. All members of the team contribute to the success of the outcome. The anesthesia provider’s attention is at a premium, and the help of the anesthesia technician is critical not only in providing but also in preparing equipment and assisting with tasks.
The anesthesia technician should be familiar with the ASA Difficult Airway algorithm, and be prepared to provide the following equipment and assistance to the anesthesia provider:
- Intravenous access equipment (multiple sizes of catheters, fluid and tubing setup, tourniquet, tape, gauze, alcohol wipes). Assistance with securing IV once catheter placed
- Oropharyngeal or nasopharyngeal airways appropriately sized for the patient
- Alternate laryngoscopes or blades, assembled, checked, and ready
- Oropharyngeal suction properly functioning. Assistance with performance of oropharyngeal suction if requested
- Endotracheal tubes of varying sizes, including stylettes
- Intubating bougie, light wand, or other airway adjuncts
- Video laryngoscope (power on, blade attached, monitor working and in proper position to be viewed by the anesthesiologist), with appropriate stylette if needed
- Supraglottic airways (e.g., LMA TM, Combitube, King airway)
- Supraglottic airways that allow for subsequent intubation without removal (e.g., Fastrach LMA™, air-Q LMA, with their accompanying intubating stylettes)
- Fiberoptic bronchoscope (power on, attached to light source, monitor functioning and in position to be viewed by the anesthesiologist, scope lubed, defogged, and loaded with right-sized or special endotracheal tube, e.g., Parker tube)
- Positioning aids and assistance in positioning the patient to facilitate ventilation or intubation (neck supports, bariatric ramp, linens)
- Assistance with preparation of emergency medications (e.g., propofol, succinylcholine, other muscle relaxants, advanced cardiac life support drugs), if this is within your scope of practice as defined by your institution
- Assistance with bag mask ventilation
- Emergency jet ventilator (jet ventilator, transtracheal jet catheter, oxygen source at 50-55 psi)
- Cricothyrotomy kit or other equipment for invasive airway access
Review Questions
1. Which of the following may be helpful in making mask ventilation easier?
A) Nasal airway
B) Oral airway
C) Two-handed mask ventilation
D) All of the above
Answer: D
When difficulty is encountered with mask ventilation, techniques to improve the ease of mask ventilation include nasal airways, oral airways, or two-handed mask techniques.
2. Which of the following would be suggested by the ASA practice guidelines for management of the difficult airway to establish ventilation if mask ventilation and intubation attempts have failed?
A) Retrograde wire intubation
B) Flexible fiberoptic intubation
C) Laryngeal mask airway
D) Blind nasal intubation
Answer: C
In the situation where mask ventilation and intubation attempts have failed, the next step is LMA placement. If this fails or is unfeasible, emergency ventilation techniques such as Combitube or jet ventilation may be pursued. If the saturation is dropping very quickly, it may also be appropriate to move directly to an invasive airway. It is not suggested to spend additional time on alternative noninvasive techniques.
3. Which of the following best describes the “cannot ventilate, cannot intubate” situation?
A) It is a true emergency and will rapidly lead to death without intervention within a few minutes.
B) It is a situation that is urgent and needs some sort of intervention over the next 15-20 minutes.
C) It is a stable situation that can be treated as time allows.
D) None of the above.
Answer: A
The “cannot ventilate, cannot intubate” scenario is a true emergency that must be resolved in a few minutes to avoid serious patient harm. If the patient is able to be ventilated by mask, supraglottic airway, or jet ventilation, then the situation is less urgent and may be resolved over a longer period of time.
4. Which of the following is true about emergency jet ventilation?
A) It is important to start the pressure low so that no trauma is caused to the lungs.
B) A blender should be used to decrease the amount of oxygen to prevent lung damage.
C) It should be performed through a large catheter placed in the cricothyroid membrane.
D) It cannot be performed without a specific jet ventilator.
Answer: C
Jet ventilation should be performed through a large catheter placed in the cricothyroid membrane. Wall pressure oxygen should be used initially. It may be administered with a jet ventilator (ideally) or by using equipment at hand. Oxygen toxicity from 100% oxygen will not manifest until several hours exposure.
5. Which of the following is true about the Combitube®?
A) It is reusable.
B) It may be used for emergency ventilation.
C) It may be used to intubate through.
D) It will only work if placed in the trachea.
Answer: B
The Combitube is a good choice for emergency ventilation because it has two lumens and may work whether it is placed into the esophagus or the trachea. It is single-use only and does not make a good conduit for intubation.
6. Which of the following would be indicated for the patient who has not been able to be ventilated by mask or by LMA or intubated and saturation is falling quickly?
A) Retrograde wire intubation
B) Blind nasal intubation
C) Cricothyrotomy
D) Fiberoptic intubation
Answer: C
If ventilation by mask and LMA and intubation have all failed, this is a true emergency and a reason for invasive airway such as cricothyrotomy. It would not be appropriate to spend additional time on noninvasive techniques.
7. Which of the following is true about emergency cricothyrotomy?
A) Bleeding can be minimized by staying in the midline.
B) It requires a special kit, such as the Melker® emergency cricothyrotomy kit.
C) A full chlorhexidine prep with scrub for 30 seconds should be performed to prevent infection.
D) Uncuffed tubes are preferred as they slip in more easily.
Answer: A
In emergency cricothyrotomy, time is of the essence. A full prep may be sacrificed for the time saved. A formal kit is useful, but not required. Any type of tube may be place into the trachea (a cuffed tube may be preferable as it protects the lungs from bleeding from the cricothyrotomy site and makes it easier to ventilate). Most blood vessels do not cross the midline, so bleeding may be minimized by staying in the midline.
SUGGESTED READINGS
American Society of Anesthesiologists Task Force on Management of the Difficulty Airway. Practice guidelines for management of the difficult airway. A report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 1993;78(3):597-602.
American Society of Anesthesiologists Task Force on Management of the Difficulty Airway. “Practice guidelines for management of the difficult airway: an updated report of the American Society of Anesthesiologists Task Force on Management of the Difficult Airway.” Anesthesiology. 2013;118(2):251-270.
Caplan RA, Posner KL, Ward RJ, et al. Adverse respiratory events in anesthesia: a closed claims analysis. Anesthesiology. 1990;72(5):828-833.
El-Ganzouri AR, McCarthy RJ, Tuman KJ. Preoperative airway assessment: predictive value of a multivariate risk index. Anesth Analg. 1996;82:1197-204.
Langernon O, Masso E, Huraux C, et al. Prediction of Difficult Mask Ventilation. Anesthesiology. 2000;92(5): 1229-1236.
Martin LD, Mhyre JM, Shanks AM, et al. 3,423 Emergency tracheal intubations at a university hospital: airway outcomes and complications. Anesthesiology. 2011;114(1):42-48.
Shiga T, Wajima Z, Inoue T, et al. Predicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performance. Anesthesiology. 2005;103(2):429-437.