CHAPTER 18
Principles of Airway Management
Introduction
The primary goal of airway management is to provide adequate oxygenation and ventilation to a patient. Anesthesia providers become particularly skilled in the field of airway management as anesthetic drugs and techniques impair a patient’s ability to perform these vital functions on his or her own. The induction of anesthesia is a critical time period for a patient. During this time, patients become apneic (stop breathing) and rely on their anesthesia provider to perform these vital functions for them. Failure to restore oxygenation and ventilation is the gravest risk in anesthesiology as anoxic brain injury ensues and ultimately cardiac collapse and death. Preparation of the patient for safe and effective airway management is the key element of safety for an anesthesia provider. This chapter focuses on those principles.
Airway Anatomy
Knowledge of the relevant airway anatomy is critical to safe airway management (see Chapter 7, Respiratory Anatomy and Physiology). The key anatomic structures involved include the nose, pharynx, larynx, and trachea (Fig. 18.1). The nose functions to warm and humidify air. It is the primary route of breathing except for situations of obstruction or increased demand where the mouth can move air at a lower resistance. Placement of devices within the nose poses a significant risk of nosebleed. While blood loss is typically not severe, it can dramatically impair the ability to subsequently view the airway. This impaired view is most pronounced with the use of video techniques as blood smears the lens. Direct techniques can also be impaired with nasal bleeding.
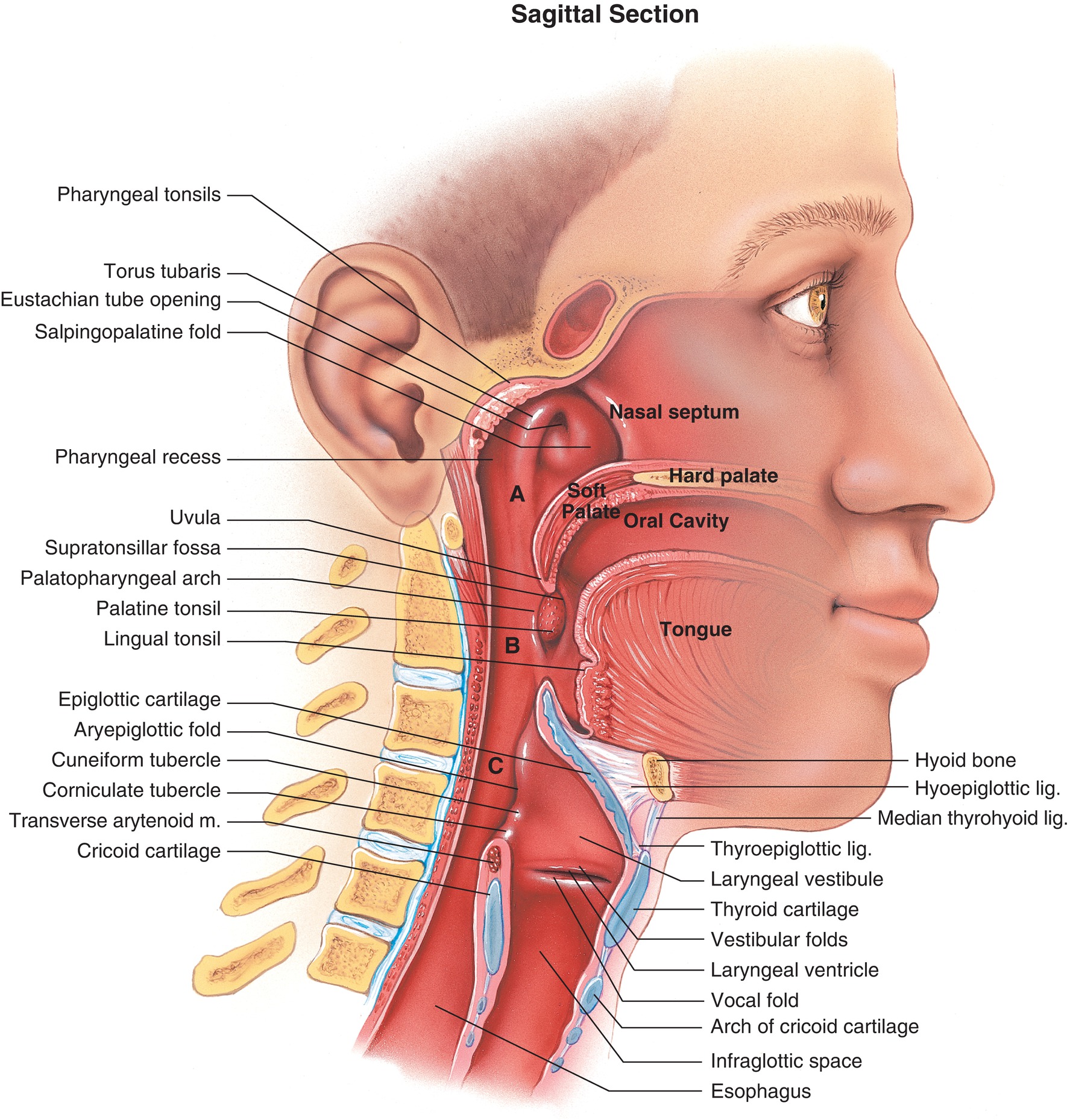
FIGURE 18.1. Pharynx sagittal section labeled. A. Nasopharynx, B. Oropharynx, C. Hypopharynx.
The mouth (oropharynx) and throat (pharynx) provide another passageway to the lungs. In normal patients, breathing through the mouth is used when ventilation increases or when the nasal passage is obstructed. Anesthesia providers frequently place devices in the oropharynx to assist with ventilation or to view the larynx (laryngoscopy). Injury to the lips, tongue, and teeth is possible. The teeth are particularly problematic as laryngoscopes apply pressure to upper teeth when laryngoscopy is poorly performed or when view of the larynx is difficult to achieve. When a patient is anesthetized or sedated in the supine position (lying down), airway obstruction is common as the tongue falls back against the pharynx. This obstruction can be effectively relieved by pulling the mandible forward (jaw thrust) or inserting an oral airway to bring the tongue forward and off of the posterior pharynx.
The larynx is a structure of cartilage that supports sound for speech. It includes the epiglottis, arytenoid cartilages, cricoid cartilage, thyroid cartilage (Adam’s apple), trachea, and vocal cords. An endotracheal tube is passed beyond the larynx and into the trachea for proper placement. A supraglottic airway (e.g., LMA™ [laryngeal mask airway]) is positioned in the pharynx in such a way that the tip sits in the esophageal inlet and the lumen sits above the vocal cords.
The trachea is a round tissue structure supported by cartilage that extends from the larynx to the main bronchi. The carina is the cartilaginous structure at the bifurcation of the trachea to the bronchi. The trachea is lined with nerve fibers that are very sensitive to stimulation from gases or tracheal tubes. These receptors trigger cough or bronchospasm. The carina is particularly sensitive to stimulation. An endotracheal tube that is positioned too deep can either irritate the carina, causing cough and bronchospasm, or enter the bronchi (usually the right side). A tube improperly positioned in the right mainstem bronchus may cause hypoxia as ventilation is provided only to a portion of the lungs.
Indications for Tracheal Intubation
An endotracheal tube is placed for airway protection and/or the need for positive pressure ventilation. The airway requires protection from either aspiration of gastric contents or obstruction from an outside source of compression. Patients at risk for aspiration are those who are sedated, anesthetized, or intoxicated and have a full stomach from a recent meal or poor digestion. Patients with an empty stomach may still be at risk for aspiration if they have disease of the esophagus or abdominal pathology that slows digestion and increases stomach volume. Specific patient conditions that are commonly considered to be a higher aspiration risk include pregnancy, trauma, bowel obstruction, diabetes, and obesity.
The airway may also require protection from external compression. That compression can come in the form of a tumor mass, abscess, or hematoma (bleeding). The postsurgical patient with bleeding in the neck is particularly concerning as the hematoma may expand rapidly to occlude a patient’s airway. Any form of external compression can make intubation of the trachea more technically challenging. Therefore, it is important to act quickly to secure an airway before the compression source grows and intubation becomes difficult and/or airway occlusion ensues.
The majority of intubations are performed because of the need for positive pressure ventilation. Under normal physiologic conditions, oxygen enters the chest through a negative pressure mechanism. The diaphragm contracts downward to expand the lungs and draw oxygen into them. Certain scenarios make this type of ventilation inadequate. Positive pressure reverses the physiology and instead pushes oxygen into the lungs. This pressure can be delivered via a face mask or a supraglottic airway device and, most definitively, through an endotracheal tube. The patient under general anesthesia is exposed to drugs that suppress ventilatory effort, and positive pressure is often needed. The use of muscle relaxation (paralytics) makes it impossible for the patient to breathe on his own and requires positive pressure ventilation.
Certain patient conditions may also impair a patient’s ability to maintain negative pressure breathing and thus require positive pressure ventilation through an endotracheal tube. Neurologic conditions such as stroke and neuromuscular disease cause weakness that may become severe enough to require positive pressure ventilation. More commonly, diseases of the lung make the added work of breathing difficult, and a patient may fatigue in his or her effort to improve ventilation. In intensive care units, diseases such as pneumonia, pneumothorax, or pulmonary fibrosis may result in conditions of impaired oxygenation and ventilation that can only be overcome with positive pressure ventilation delivered via an endotracheal tube.
Complications Associated with Intubation
The gravest risk in airway management is the inability or failure to intubate a patient who requires it. This failure may be recognized or unrecognized. The development of in-line CO2 monitoring has changed the field of anesthesia and dramatically reduced the occurrence of unrecognized esophageal intubation. Today, failure more commonly occurs in a recognized situation. The consequence of failure to intubate can be severe if other means to oxygenate (mask ventilation) fail or are attempted too late. This risk is particularly important in anesthesia as the medications used to facilitate intubation impair the patient’s ability to ventilate.
More commonly observed complications are related to trauma during the process of laryngoscopy. Lip lacerations are the most common form of injury but rarely result in long-standing problems. Dental injury is a common occurrence as laryngoscope blades make contact with the upper incisors. These injuries are among the most common source of litigation against anesthesia providers. Depending on the route of intubation (oral vs nasal), trauma can occur anywhere along the course of the tracheal tube including the vocal cords and nerves to the vocal cords. These injuries can result in temporary or permanent voice problems.
Another complication associated with intubation is related to the cardiovascular system. Placement of a tracheal tube is remarkably stimulating to an awake or even an anesthetized patient. Commonly, there is a dramatic rise in heart rate and blood pressure if active measures are not taken to blunt these responses. The gravest risk of this heart rate and blood pressure response is stress on the heart, which may cause injury or even death of some heart muscle, or rupture of a blood vessel in the brain, leading to stroke. Detailed knowledge of the patient’s preexisting medical problems helps the anesthesiologist optimize an anesthetic induction drug cocktail to balance the effects of the stimulation of intubation with the relative depressant effects of anesthesia induction drugs.
Laryngospasm is a complication that is often seen before or after tracheal tube placement. A partially anesthetized airway that is irritated from instrumentation, blood, or secretions is prone to spastic closure. This closure can make airway movement impossible, even if the patient retains respiratory effort. If left untreated, patient breathing against a closed larynx can draw fluid into the lung cavity (pulmonary edema). In addition, laryngospasm can last long enough that the patient can become hypoxic. Recognition of this obstructed breathing pattern is important as rapid action can prevent dangerously low–blood oxygen content. Application of positive pressure through a face mask can “break” the laryngospasm. If this treatment fails, a rapidly acting paralytic should be given to relax the vocal cords.
Predicting Difficulty with Ventilation
The consequences of failure to ventilate are so severe; it is critical to anticipate the potential difficult airway and craft an airway management plan that is safe and comfortable for the patient. The strongest predictor of difficulty is a history of difficult airway management. Anesthesia providers must predict the difficulty of both failed bag-mask ventilation and failed intubation. Unfortunately, the available bedside testing measures for predicting difficult intubation or ventilation have a poor predictive value. In other words, intubation may fail even with patients who are predicted to be easy. Conversely, a patient with multiple predictors of difficulty may be fairly easy to intubate.
Bag-mask ventilation is made more difficult by several patient conditions. Commonly, the obese patient presents difficulty as soft tissue in the pharynx collapses under anesthesia or sedation. Other predictors of difficult bag-mask ventilation include older age, presence of a beard, lack of teeth, history of neck radiation, high Mallampati classification scale score (see below), and history of obstructive sleep apnea.
Difficult intubation can be predicted by several bedside examinations. The risk of failed intubation rises with a greater number of predictors present. The most commonly referenced bedside examination tool is the Mallampati classification score (Fig. 18.2). This bedside test correlates a patient’s mouth opening to tongue size to derive a scale of 1-4, with a score of 4 predicting the most difficulty. Other measurements that predict difficulty are a small mouth opening, small distance from the thyroid cartilage (“Adam’s apple”) to the chin, reduced neck mobility, inability to protrude the jaw forward, a neck mass, and large neck circumference. The presence of obesity as a predictor of difficult intubation is debated in the literature. A high body mass index may not make intubation more difficult if a patient is properly positioned. However, a large neck circumference is associated with intubation difficulty. Appropriate positioning of an obese patient in a “ramped” position improves the adequacy of mask ventilation and eases intubation. Despite these concerns, the obese patient is at particular risk of grave consequences if intubation fails as bag-mask ventilation may be more difficult, aspiration risk is higher, and oxygen saturation falls more quickly.
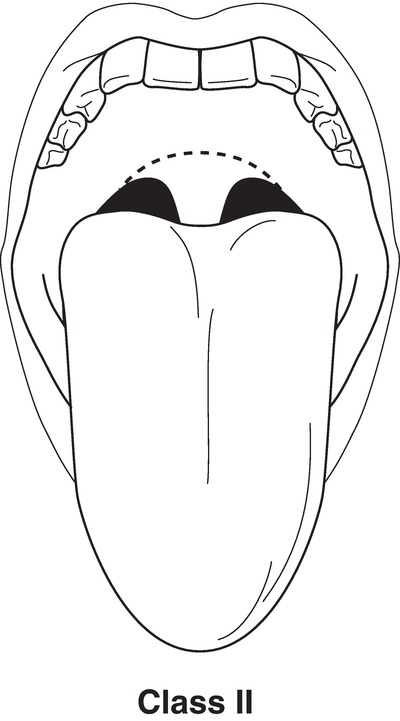
FIGURE 18.2. Mallampati classification. Class II: cannot see tonsillar pillars. (From Blackbourne LH. Advanced Surgical Recall. 2nd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2004, with permission.)
Beyond the bedside exam, patient history predicts difficulty. Patients with pathology of the neck can be very difficult to intubate. Neck trauma, masses in the neck area, infection around the neck, previous neck radiation, and disease of the spine can make both mask ventilation and intubation difficult.
Induction Sequence
After appropriate room setup, preparation of devices, and monitoring, an adult patient is typically preoxygenated. The purpose of this step is to “buy time” after anesthesia induction and anticipated apnea. Preoxygenation is effectively achieved by supplying 100% oxygen via a face mask on a circuit with reservoir (anesthesia machine, Jackson-Rees circuit). After 3 minutes of normal breathing or five full capacity breaths, the nitrogen in the lungs is replaced by oxygen. With the lungs full of oxygen, an anesthetized patient will consume the oxygen in the lungs for several minutes before blood oxygen levels fall. Some patient conditions are more prone to a rapid fall of oxygen levels (desaturation). These conditions include infancy, obesity, pregnancy, and poor baseline lung gas exchange.
After preoxygenation, anesthetic induction is typically performed with intravenous (IV) agents in adults or inhalational agents in children. Muscle relaxation (paralysis) is commonly employed to facilitate intubation as intubation success improves with use of paralytics. These drugs offer the benefit of easier intubation but carry risks as the patient becomes apneic and will not restore ventilation again until the induction drugs and paralytics have appropriately been metabolized or reversed. Therefore, paralytic medication is used cautiously in the anticipated difficult airway.
Rapid Sequence Induction
Rapid sequence induction is performed on patients at risk for aspiration (full stomach, pregnant, abdominal pathology). The goal of a rapid sequence induction is to rapidly intubate the trachea and avoid bag-mask ventilation, which pushes gas into the stomach and increases the chance of regurgitation with time. More acidic stomach content is associated with worse lung injury when aspirated into the lungs. A higher volume of stomach content is also associated with worse lung injury when aspirated. Medications such as sodium citrate, metoclopramide, or ranitidine may be given prior to anesthetic induction to alter the acid content of the stomach secretions or improve emptying of the stomach into the bowel. Standard care is to apply cricoid pressure during a rapid sequence induction. This maneuver is applied by an assistant. It is performed by applying pressure with the thumb and index finger over the cricoid cartilage directly posteriorly to occlude the esophagus and prevent passive aspiration of stomach contents up into the airway. This pressure is maintained throughout the induction sequence until tracheal tube placement is confirmed by end-tidal CO2. This pressure should be applied with 10 N of pressure initially and then 30 N of pressure when the patient becomes unconscious. Think of the weight of a gallon of milk as an appropriate pressure to apply. Cricoid pressure is not released until the anesthesia provider asks: most commonly, this is not until the tube is confirmed by auscultation and capnography to be in the trachea. This means that if there are several attempts at intubation, with intermittent ventilation, it becomes even more important for the assistant to remember to maintain cricoid pressure and not become distracted by an increasingly busy scenario. Conversely, cricoid pressure may make placement of the laryngoscope or visualization of the larynx more difficult, and in this case, the anesthesia provider may ask the assistant to release pressure or may even move your hand in a specific direction.
Bag-Mask Ventilation
If a patient has minimal aspiration risk, bag-mask ventilation is typically performed for some time after induction agents have been administered. This allows the muscle relaxant to take effect and to deepen anesthetic depth. This step is critical as oxygenation and ventilation are taken over by the anesthesiologist. If intubation fails, bag-mask ventilation is resumed as a life-preserving maneuver. During a routine general anesthetic, a mask is applied with proper seal over the nose and mouth. The mask is connected to a breathing circuit that, in turn, is connected to the anesthesia machine. Ventilation is performed by squeezing the reservoir bag in the anesthetic circuit while controlling the inspired pressure with the pop-off valve (see Chapter 24, The Anesthesia Machine). If an anesthesia machine is not being used, ventilation will be performed with a self-inflating bag-valve-mask system (e.g., Ambu bag) (Fig. 18.3). When mask ventilation is difficult, it can be improved by optimizing the head position into a “sniff” position, with the neck flexed at the shoulder and extended at the junction of the head and neck. Airway devices can also be used to overcome airway obstruction in a difficult mask scenario. An oral airway is used to push the tongue away from the posterior pharynx in an anesthetized patient, or a nasopharyngeal airway can be used if the patient is not fully anesthetized as it elicits less gag reflex.
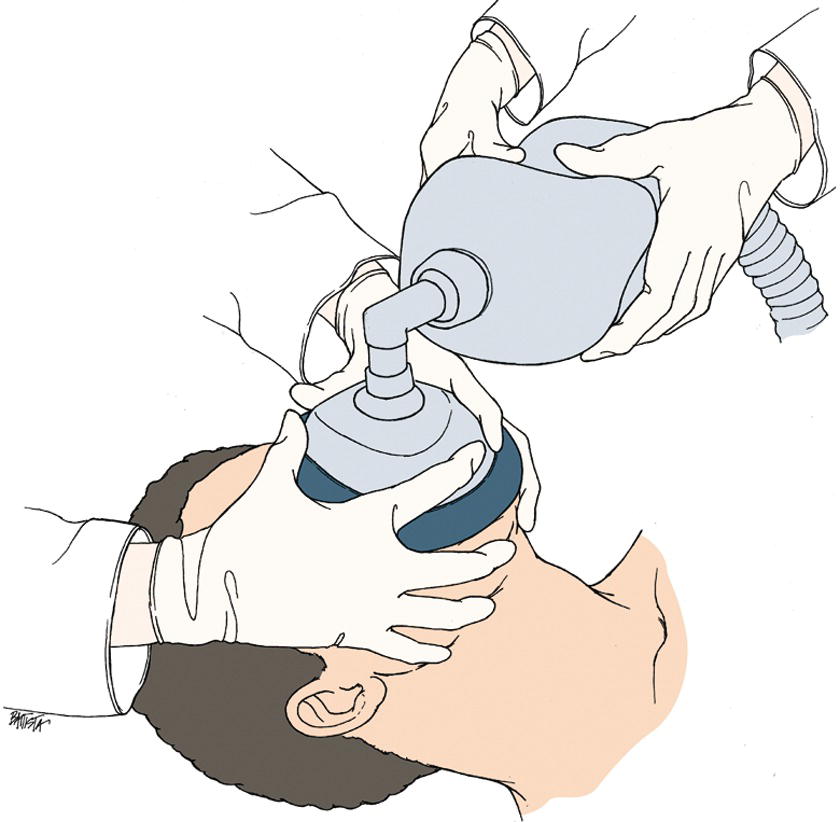
FIGURE 18.3. Ventilation, bag-mask, two-person bag-mask ventilation; two-person fitting technique; one person secures the mask to the face while an assistant delivers breaths. (Reproduced with permission from LifeART image. Copyright © 2012 Lippincott Williams & Wilkins. All rights reserved.)
Supraglottic Airways
A patient at low risk for aspiration can be managed with a supraglottic airway. This term encompasses several devices that are commonly referred to, together, as an LMA™. This is an incorrect usage—the LMA™ was the first to be invented but is now one of many kinds and brands of supraglottic airway (see Chapter 39, Devices Placed in the Airway). Your institution may stock one or more SGAs, which may or may not include a variant on the original LMA™. The supraglottic device acts like a bag-valve-mask device but holds its seal in the pharynx as opposed to the outside of the mouth (Fig. 18.4). It allows the anesthesia provider to free his or her hands and perform the anesthetic with the patient breathing spontaneously or with the support of assisted or controlled breaths through the anesthesia machine. The benefits of the supraglottic airway compared to a tracheal tube include possible reduced trauma during placement of the device, less hemodynamic stimulation, and avoidance of the need for muscle relaxation (paralytics) to facilitate placement. In addition, supraglottic airways are placed “blind,” without the need for laryngoscopy to visualize the larynx. The trachea is not secured with a cuff, so aspiration risk persists. The decision to place a supraglottic airway as opposed to an endotracheal tube is at the comfort and discretion of the provider and is usually dictated by surgical duration, potential need for muscle relaxation to facilitate surgery, and aspiration risk. The supraglottic airway plays a key role in difficult airway management. When intubation and ventilation fail, the supraglottic airway can be used in some cases to restore ventilation and save the patient from serious injury or even death. In these situations, the airway can continue to be managed with the supraglottic airway alone, with intubation through the supraglottic airway, or by other means.
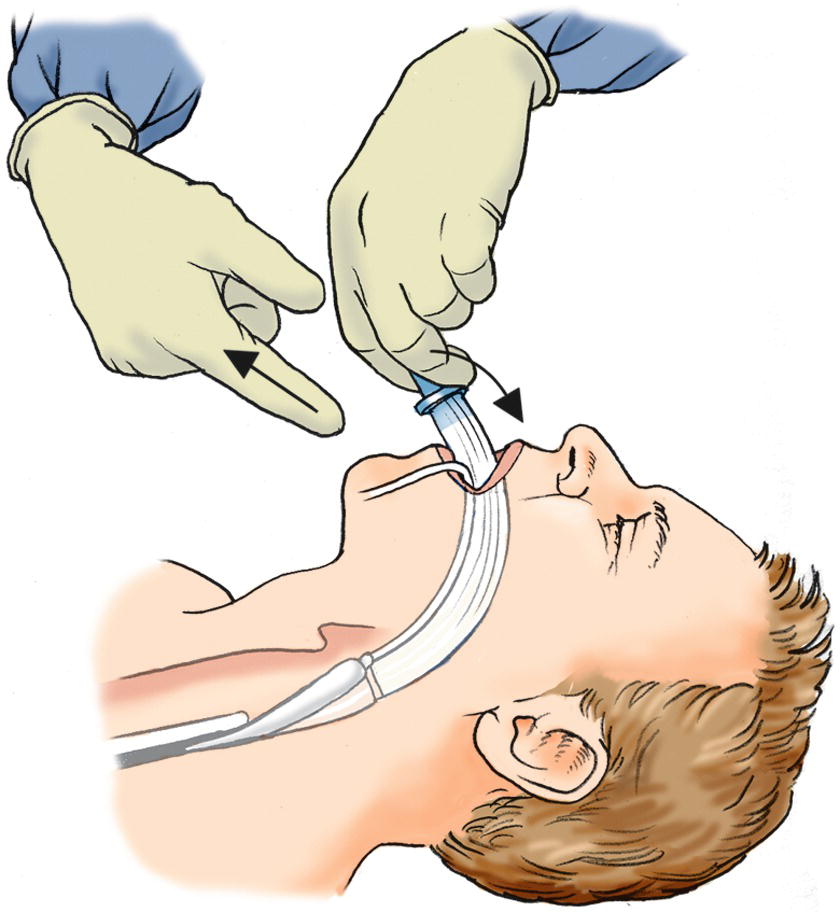
FIGURE 18.4. Laryngeal mask airway insertion. Inserting the laryngeal mask airway (LMA™). After the LMA™ is in place, gently remove your index finger while you place gentle pressure on the patient’s jaw with your opposite hand. After you remove your index finger, remove both hands. (From Springhouse. Lippincott’s Visual Encyclopedia of Clinical Skills. 1st ed. Philadelphia, PA: Wolters Kluwer Health; 2009, with permission.)
Direct Laryngoscopy
Intubation is most often performed with a direct laryngoscope. A laryngoscope blade is inserted into an open mouth, beyond the teeth, and down toward the epiglottis. A curved Macintosh blade tip should be placed where the base of the tongue meets the epiglottis (vallecula) (Fig. 18.5). The tongue is moved out of the view by sweeping it over to the left side of the oropharynx. Suspension pressure is applied to lift the jaw and epiglottis up and visualize the larynx and vocal cords to pass a tracheal tube. Unless contraindicated, the neck is extended to align the view from the mouth to the larynx. The view achieved of the larynx is commonly graded by the Cormack-Lehane scale. A full view of the vocal cords is graded I, a partial view of the cords is graded II, a view of the epiglottis only is graded III, and no view of any laryngeal structure is graded IV. A straight blade (Miller) is used to lift the epiglottis directly. The use of various blade types and sizes is a matter of provider preference. When a view cannot be achieved with one blade type, sometimes an alternate blade improves laryngeal view. Methods to improve this view include repositioning the patient’s head, neck, or shoulder. Application of cricoid pressure or external manipulation of the larynx may also bring the airway into view. When an adequate view cannot be obtained, sometimes the tracheal tube can be passed blindly. A gum elastic bougie may be an easier device to pass as it is thinner than a tracheal tube and can reach a larynx that is difficult to visualize. Once the bougie is passed, a tracheal tube can be passed over the bougie. Asking for alternate blades or a bougie should alert the anesthesia technician that the anesthesia provider may be having difficulty.
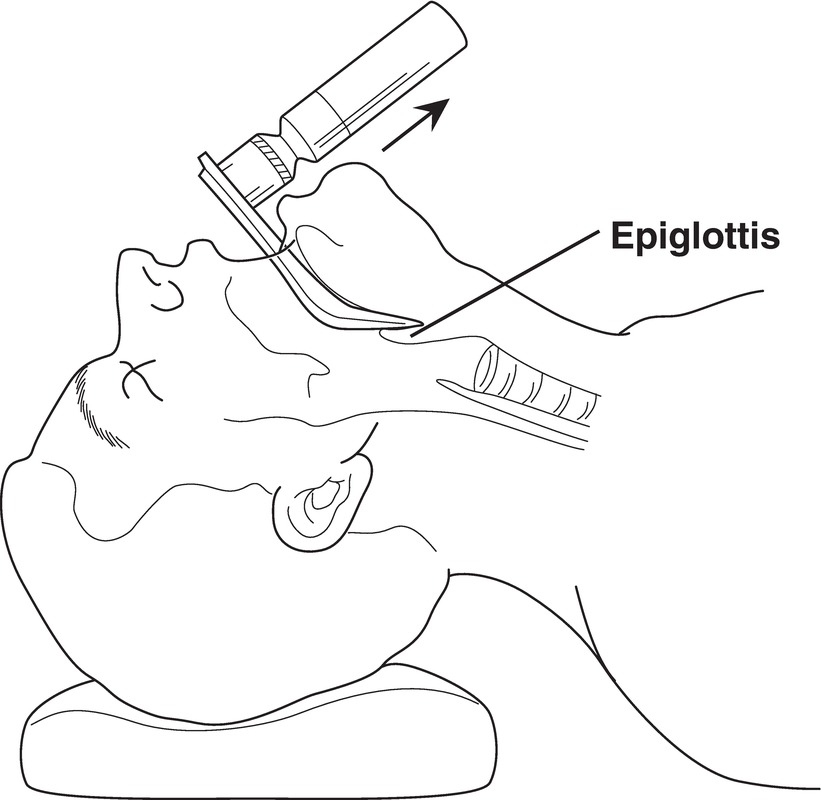
FIGURE 18.5. Intubation with a Macintosh blade. The blade is used anterior to the epiglottis. (From Blackbourne LH. Advanced Surgical Recall. 2nd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2004, with permission.)
When direct laryngoscopy fails, help is needed. The most experienced provider available should assist with intubation. Focus should remain on maintaining adequate oxygenation with mask ventilation. Alternate devices may rescue the airway, so those devices should be retrieved if not immediately available. Useful rescue devices include rigid video laryngoscopes, flexible intubation scopes, and supraglottic airways. The details of managing the failed intubation are summarized in the American Society of Anesthesiologists Difficult Airway Algorithm. These scenarios are covered in depth in Chapter 57, Airway Emergencies, as are the components of a difficult airway cart, which should be preassembled so that all useful equipment can come simultaneously to this rapidly evolving emergency.
Video Laryngoscopy
Video laryngoscopes have a growing role in airway management. They are effective tools in the airway predicted to be difficult and are effective in rescuing failed direct laryngoscopy. For most devices, a video chip is embedded in the laryngoscope blade, and a magnified view of the airway is displayed on a video screen. Compared to direct laryngoscopy, the view of the larynx is improved. This better view translates to higher intubation success for those predicted to be difficult to intubate by direct laryngoscopy. Furthermore, other providers observing the intubation can help guide the intubation as they have access to the screen view. Not surprisingly, novices perform intubation with a higher success rate utilizing these devices compared to direct laryngoscopy because the view is improved and teachers gain visual access to the laryngoscopy. Just like a request for a bougie, an urgent request for a video laryngoscope should alert the anesthesia tech that providers may anticipate airway difficulty; it may be advisable to remain attentive for requests for further equipment or assistance.
Blind Intubation Techniques
At times, visualization of the larynx with direct or video means may be impossible due to patient conditions or blood in the airway. Options for blind intubation techniques include lighted stylets, blind nasal intubation, and retrograde wire techniques. A blind intubation most often utilizes the nasal route compared to an oral route as the tracheal tube is more likely to be directed into the larynx. The anesthesia provider will typically observe patient ventilation (awake or asleep), pass the tube, and watch for return of gas exchange through the tube. This is a trial-and-error technique.
Another blind technique is the use of a lighted stylet, or “lightwand.” A tube is preloaded on a stylet that carries a light bulb at the tip. The stylet is bent by the anesthesia provider at an angle that guides the stylet anteriorly into the larynx. With a dim room, the light is observed through the skin in the pharyngeal area, and then very brightly as it enters the larynx and down the trachea. Once light is observed in the trachea, the tube is properly positioned and the stylet is removed.
A retrograde intubation can be performed as a primary or rescue technique. A needle is passed through the cricothyroid membrane into the airway. Through the needle, a wire is passed up into the pharynx until it comes out into the mouth or nose. This wire then serves as a conduit to pass a tracheal tube into the glottis. This method is useful when other means dramatically impair the ability to visualize the glottis.
Flexible Scope Intubation
The gold standard for managing the airway known to be difficult or at high risk of difficulty is to perform an awake flexible video intubation. These devices are often referred to as fiberoptic scopes, but today most of these devices enable a video chip, not fiberoptic bundles for the video view. As this procedure can be rather uncomfortable, it is important to adequately prepare the patient and equipment prior to performing this procedure. The flexible scope can also be used to rescue failed airway management in a patient who is anesthetized or can be used to facilitate intubation through a supraglottic airway.
The key to successful awake flexible intubation is provider skill and patient preparation. The patient’s airway needs to be numbed of the uncomfortable sensations of the scope and tracheal tube passing through the airway. Anesthetizing the airway with a local anesthetic is achieved by many different means. Nerve blocks can be performed to block sensation to the airway. These blocks typically involve multiple injections targeting the superior laryngeal nerve, glossopharyngeal nerve, and recurrent laryngeal nerve on both sides of the neck. More commonly, topical anesthesia is applied. Topical anesthetic (lidocaine) can be applied via jelly, gargling, atomizer, nebulizer, or pledgets or injected directly through the bronchoscope on the affected tissue. When approaching the airway via a nasal route, the nose needs to be similarly numbed with a local anesthetic, and a vasoconstrictor should be used to reduce the chance of nose bleeding. Ultimately, the patient should have a suppressed gag reflex and be able to tolerate the application of the flexible scope and tube through the airway. Other drugs may facilitate this process including sedation medications and an agent that suppresses salivation such as glycopyrrolate.
Surgical Airway
The most conservative strategy to airway management is awake tracheostomy. This procedure is typically performed by surgeons with the use of a local anesthetic and an awake or lightly sedated patient. As this is a permanent surgical scar both visible on the neck and potentially causing long-term consequences in the trachea, it is reserved for the most troubling airways. A cricothyrotomy should be performed to rescue an airway that cannot be ventilated when other techniques have failed. A needle or knife incision is made through the cricothyroid membrane, and a tube is passed directly or over an exchange wire (Fig. 18.6). Additionally, jet ventilation can be utilized through a cricothyroidotomy needle or catheter. As this skill is not commonly practiced by anesthesia providers, they should be comfortable with location of equipment and know about available resources to assist with the procedure (see Chapter 57).

FIGURE 18.6. Cricothyroidotomy procedure.
Pediatric Considerations
As the anatomy and physiology of an infant or a child are different from those of an adult, the approach to airway management is also different (Fig. 18.7). On an anatomical basis, children have a relatively larger head size and tongue size. The larynx of a child sits in a higher position in the neck. The narrowest portion of the larynx comes at the level of the cricoid cartilage rather than the vocal cords as seen in adults. For this reason, uncuffed tracheal tubes are sometimes placed in smaller children. The larynx of a child is more prone to laryngospasm from the effects of airway irritation than an adult. Generally speaking, difficult airways are encountered less often in the pediatric population than in the adult (see Chapter 48, Pediatric Anesthesia). However, children can have congenital and genetic abnormalities of the airway. Children’s respiratory regulation is also more unpredictable, resulting in more frequent laryngospasm and apneic events around induction and emergence from anesthesia.
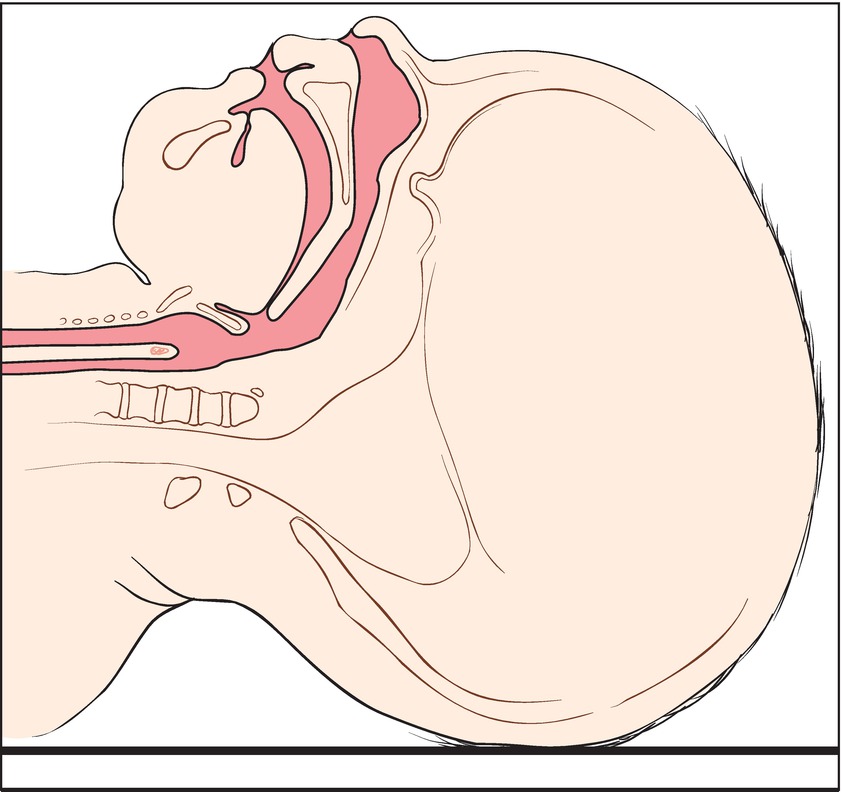
FIGURE 18.7. Airway, infant—Simple sagittal view of an infant’s head and neck showing the anatomy of the airway. (Reproduced with permission from LifeART image. Copyright © 2012 Lippincott Williams & Wilkins. All rights reserved.)
The key physiologic difference in children relates to oxygen consumption. Children consume oxygen at a relatively higher rate than adults. Therefore, failure to adequately oxygenate a child or prolonged intubation time can lead to a rapid fall in blood oxygen levels. So, while airway management in a child may be less difficult, the consequences of failure or prolonged airway management are more severe.
The greatest challenge for airway management in pediatrics often comes from lack of cooperation. Awake intubations are rarely feasible, so the airway is typically managed with an asleep technique. When an IV line is available, anesthetic induction can be performed in a similar fashion as in adults. However, cooperation with IV line placement often makes inhalation induction the preferred induction technique. In this fashion, a child breathes anesthetic gas through the circuit and maintains spontaneous ventilation until an IV line can be placed. This interval period can be dangerous because if the airway does become irritated and laryngospasm ensues, there is no venous access to deliver paralytic medications to break the laryngospasm. Once an IV line is placed, the airway can be managed with additional IV medications. In small children, muscle relaxation to facilitate intubation is often not needed.
Extubation
Removal of the tracheal tube (extubation) is another critical process in anesthesia care. During the course of a surgical procedure, an anesthetized patient cannot protect his or her airway, has impaired ventilation mechanics, and may be chemically paralyzed to impair breathing. These functions need to be reversed to ensure airway patency, oxygenation, and ventilation. Typically, extubation occurs in an awake patient who can follow simple commands to demonstrate that he or she will maintain his or her airway reflexes and who has adequate pulmonary dynamics. At times, extubation is performed on a deeply anesthetized patient who is spontaneously breathing through the tracheal tube. This technique may be performed to minimize excessive coughing that is associated with emergence from anesthesia with an irritating tracheal tube in place. It is important to not extubate a patient who is transitioning from a deeply anesthetized to an awake state as the vocal cords are more prone to laryngospasm and closure immediately after extubation. Either way, it is important to ensure that the airway is dry from blood or secretions with adequate pharyngeal suctioning prior to extubation. Immediately following extubation, it is important to ensure patency of the airway with adequate ventilation by applying supplemental oxygen through a mask and noting good gas exchange.
At times, extubation may occur with an airway that is at risk for collapse from airway edema or swelling. When concerns arise for airway swelling, anesthesia providers may deflate the cuff of a tracheal tube to ensure good passage of gas around the tube before extubation (cuff leak test). This step may provide an assurance that the airway is patent enough to stay open after extubation. Alternatively, providers may pass an exchange catheter or a bougie through the tracheal tube as a possible conduit to reintubation if the patient fails to adequately maintain his or her airway with good gas exchange.
Despite the best plans, extubation may fail. Patients may develop immediate or delayed airway obstruction from swelling or soft tissue collapse. Failure can also come from inadequate pulmonary mechanics due to painful breathing, residual neuromuscular blockade, or weak strength. These types of failures often have a delayed presentation as CO2 in the blood rises to a point that the patient becomes unresponsive. In any case, it is imperative to actively monitor the patient’s airway and breathing during transport to recovery areas via physical examination or patient monitoring. Continuous monitoring of vital signs and airway patency should continue in the recovery area until the patient has sufficiently recovered from the anesthetic.
Summary
Management of the airway is one of the most critical tasks in anesthesia. The provision of anesthesia to facilitate surgery frequently impairs the ability of patients to breathe on their own. Failure to manage the airway properly can result in severe injury or even death to the patient. Anesthesia technicians should be familiar with the different scenarios in which the airway will need support, the different techniques that can be used to secure an airway, and the equipment that may be required during airway management. This chapter reviews the anatomy of the airway and the implications for airway management during induction and emergence. This chapter also presents the most common airway management techniques including those for mask ventilation and intubation.
Review Questions
1. The indications for tracheal intubation include all of the following EXCEPT
A) A full stomach
B) External compression from a mass or bleeding
C) Inadequate spontaneous ventilation
D) A surgical procedure requiring paralysis and general anesthesia
Answer: A
A patient with a full stomach can protect his or her airway unless he or she has impaired reflexes from a neurologic condition, sedation, intoxication, or anesthesia. (Most people have a “full stomach” most of the time; only when the airway is unprotected is this a risk for aspiration.) An external compression may rapidly occlude an airway and requires protection from obstruction with urgent intubation. Inadequate patient ventilation necessitates intubation so that positive pressure can be delivered to improve gas exchange. While an airway can be managed with mask ventilation or a supraglottic airway, a prolonged surgical procedure should be managed with an endotracheal tube.
2. The most common legal claim against anesthesiologists related to airway management comes from which of the following?
A) Anoxic brain injury from failed airway management
B) Lip lacerations from laryngoscopy
C) Dental injury during laryngoscopy
D) Vocal cord dysfunction and speech problems from intubation
E) None of the above
Answer: C
Dental injury is not the most common or severe complication, but the injury requires expensive dental work to correct the problems and results in a high incidence of legal claims. Fortunately, anoxic brain injury is a rare and catastrophic event. It results in the largest claims and settlements. Lip lacerations are very common, but the injuries tend to heal without added intervention, so claims are rarely associated with these injuries. Vocal cord dysfunction may occur from traumatic intubation but is more likely from prolonged intubation and pressure of the tube cuff on the laryngeal nerve (e.g., intensive care unit patients intubated for several days). This dysfunction most often resolves with time and does not usually require intervention.
3. The most conservative approach to a difficult intubation is
A) Direct laryngoscopy
B) Rigid video laryngoscopy
C) Awake flexible fiberoptic intubation
D) Awake tracheostomy
E) None of the above
Answer: D
In experienced surgical hands, this procedure rarely fails and rarely results in hypoxia. As it results in a permanent scar, it is reserved for the most difficult airways, but is the most conservative approach. Direct laryngoscopy is the most common intubation procedure performed but carries a failure rate of about 6% in the predicted difficult intubation. Rigid video laryngoscopy likely has a higher success rate in the predicted difficult intubation, but failures still occur at a rate of 1%-3%. Awake flexible fiberoptic intubation is a conservative airway management approach but requires a skilled anesthesiologist, a cooperative patient, and good airway topicalization. However, a patient may still suffer hypoxia, aspiration, or laryngospasm during the performance of this technique.
4. The purpose of preoxygenation is
A) To remove nitrogen from the lungs
B) To improve baseline oxygen saturation
C) To create a reservoir of oxygen in the lungs for consumption during apnea
D) To demonstrate adequate mask seal and return of end-tidal CO2
E) All of the above
Answer: C
Preoxygenation serves to prolong the time period to oxygen desaturation during apnea by lung volume with oxygen. Nitrogen in the lungs is removed during preoxygenation, but nitrogen itself is not inherently harmful; replacing the nitrogen with oxygen is the critical safety step. Baseline oxygen saturation may be improved with preoxygenation, but even the patient who has perfect baseline oxygen saturation does not have “extra” oxygen in the blood, compared to the large reserve of oxygen gas that the lungs can be filled with, and will benefit from a prolonged desaturation time during apnea after preoxygenation. While it is important to demonstrate a mask seal and competence of the end-tidal CO2 system, this is not the purpose of preoxygenation.
5. Laryngospasm may be avoided or treated by all of the following EXCEPT
A) Deep extubation
B) Applying positive pressure ventilation via mask
C) Administration of a paralytic drug
D) Adequate suctioning of secretions in the pharynx
E) None of the above
Answer: A
Deep extubation can reduce coughing but does not prevent laryngospasm. Positive pressure maintained through a face mask can often break a laryngospasm. Paralytic drugs will break laryngospasm by relaxing the vocal cords. Adequate suctioning of the pharynx removes blood or saliva that stimulates the larynx to spasm.
SUGGESTED READINGS
Fleisher LA, Hazel M. Hussong Fund: Evidence-Based Practice of Anesthesiology. 2nd ed. Philadelphia, PA: Saunders Elsevier; 2009:516.
Marcucci C. Avoiding Common Anesthesia Errors. Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins; 2008:1030.
Miller RD. Miller’s Anesthesia. 6th ed. New York, NY: Elsevier/Churchill Livingstone; 2005:3203.