GENETICALLY MODIFIED PLANTS are now widely available to consumers, as discussed in chapter 6, and, as we have also seen, generate a significant amount of controversy. Yet genetically modifying plants may seem to many people to be much less controversial than tampering with the genetic blueprint of animals. This is due in part to our own view of animals. Indeed, for most people it is easier to relate to a dog, a goat, or even a mouse than it is to relate to a banana or a corn plant. What’s more, the genetic engineering of animals immediately brings to mind the prospect of genetically modifying human beings. In this chapter we will see how scientists have created genetically modified animals and how gene cloning is being explored to treat genetic diseases in humans.
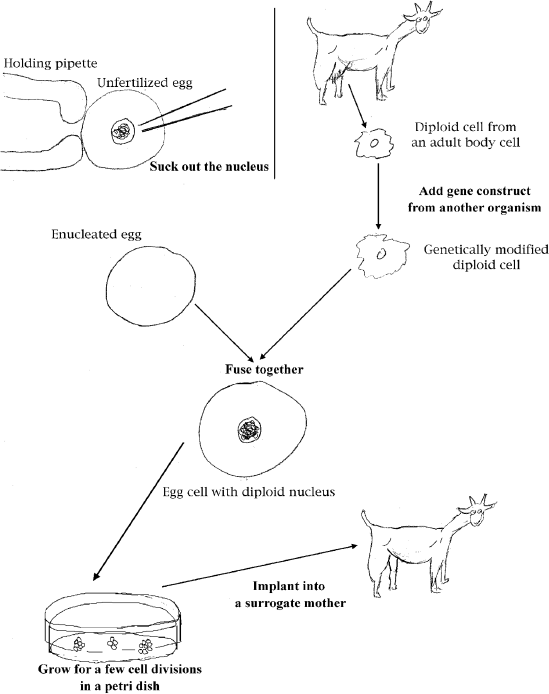
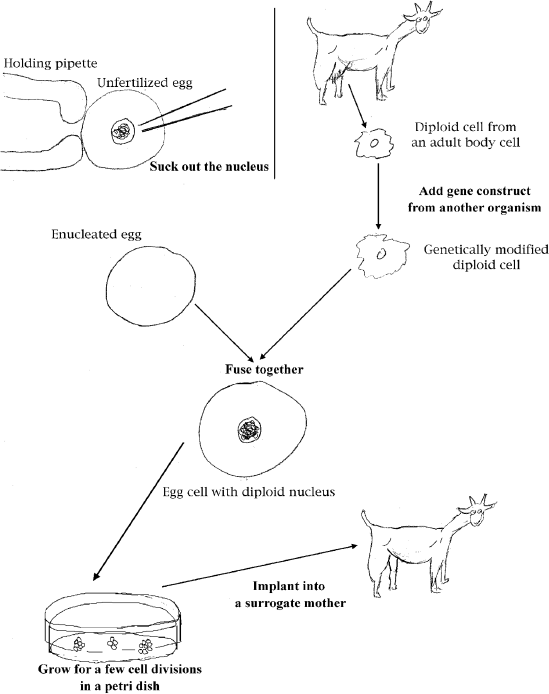
Today, most genetically modified animals are produced by the nuclear-transfer technique, a method that produced Dolly the Scottish sheep, the very first cloned mammal. To date, all sorts of animals have been cloned this way, including mice, pigs, goats, rabbits, cats, and cattle. In this procedure, an egg is removed from a female animal, and its nucleus, which contains the chromosomes, is carefully sucked out with a very fine glass needle. This operation removes the original DNA from the egg. Next, a diploid cell (in the case of Dolly, this was an udder cell) isolated from another animal is fused with that egg using an electric shock. This procedure forces the chromosomes of the diploid cell to penetrate the egg. Since the egg was rid of its own (haploid) set of chromosomes, the result is an egg cell that now contains two sets of chromosomes, both sets originating from the donor fused cell. This egg can now be coaxed to behave like a fertilized egg. However, contrary to a regular fertilized egg, in this case, the two sets of chromosomes come from only one parent, the donor of the fused cell. Since the processes of removing the nucleus and fusion with a diploid cell may injure the egg, scientists normally manipulate several eggs in a single experiment, not just one.
Next, the manipulated eggs are allowed to divide a few times in a petri dish and are subsequently implanted into yet another female that, if all goes well, will deliver a litter of cloned animals, all copies of the individual that donated its chromosomes. The procedure is depicted in figure 13.1.
It should be noted that nuclear transfer in mammals still needs improvement to become a routine procedure. In addition, many live offspring originating from the cloning procedure are crippled or deformed in one way or another. Stillbirths are also frequent. The reasons for this are poorly understood, and cloning (including genetic modification) by nuclear transfer is far from being well established.
The above technique is used for cloning, but up to this point, no genetic modifications of the cloned animals have really taken place. The twist however, is that the cells used as chromosome donors in a cloning experiment can be genetically manipulated before fusion with an egg. In that case, udder cells, as in the example of sheep, can be modified in the test tube with a gene from another species. Here also, an electric shock is used to prompt cells to pick up the DNA presented to them in their growth medium. For example, the Scottish scientists who created Dolly produced other cloned sheep using udder cells modified by the addition of gene for human blood-clotting factors. These cloned sheep did indeed produce the factors in their milk.
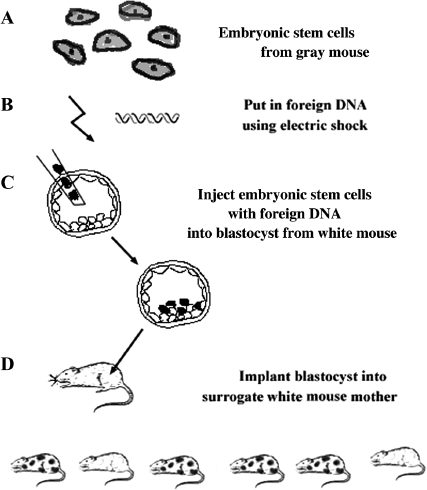
The drawback mentioned for cloning animals by nuclear transfer does not exist for a second technique used to produce genetically modified animals. This is a technique that genetically manipulates embryonic stem cells in the test tube and then injects them into a growing embryo. We saw in chapter 4 that stem cells isolated from very young embryos have the ability to form any kind of tissue. When injected into an embryo at the blastocyst stage (an embryo containing dozens of cells that have not yet formed any tissues or organs), embryonic stem cells join the cells of the developing embryo. Later, they follow the developmental and differentiation pattern of the cells surrounding them. In other words, an injected embryonic stem cell that finds itself next to cells destined to become a heart will also develop into a heart cell. If the embryonic stem cell finds itself next to cells destined to become gametes in the adult, it too will become a gamete.
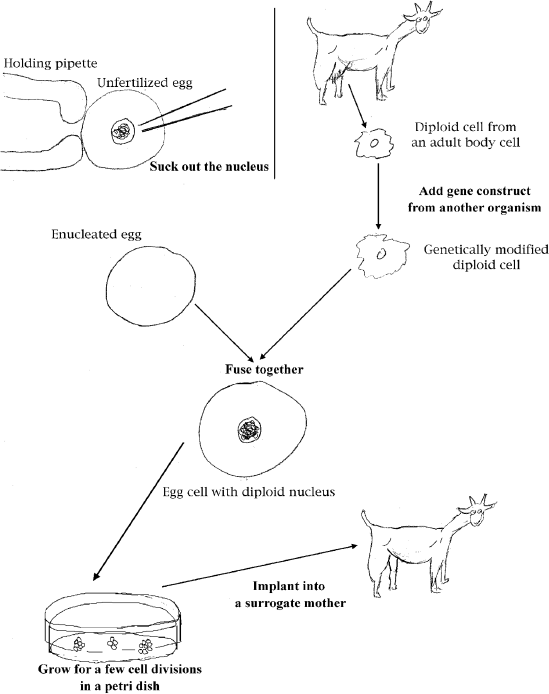
Figure 13.1 Making Genetically Modified Animals by Nuclear Transfer. First, the haploid nucleus of an unfertilized egg is sucked out of the egg with a very fine glass syringe. The enucleated egg is then fused with a diploid cell from the body of an adult animal. The egg, containing a diploid nucleus, is stimulated to divide in a petri dish. After a few divisions, the growing embryo is implanted into a surrogate mother that will carry it to term. The resulting cloned animal can be genetically modified by inserting a foreign gene into the diploid cell prior to fusion with the enucleated egg.
Embryonic stem cells can be cultivated in the lab and manipulated like any other kind of cells. Thus, scientists can genetically modify embryonic stem cells by adding cloned genes from any source (usually by subjecting them to an electric shock in the presence of DNA) and then inject these genetically modified embryonic stem cells into a blastocyst-stage embryo. The blastocyst is subsequently implanted into a surrogate mother, where it continues to develop. Genetically modified embryonic stem cells thus become an integral part of the growing embryo and, eventually, the adult individual. These adults are then formed partly from the cells of the embryo that was the blastocyst and partly from the injected stem cells, and thus they are not all genetically alike. Thus, if the embryonic stem cells were genetically modified, only the cells derived from those embryonic stem cells have the foreign gene. The full procedure is illustrated in figure 13.2. It should be emphasized that genetically modified animals are not yet used on an industrial scale and their products are not yet used for medical purposes.
The basic idea in making genetically modified animals is to turn animals into specialized protein factories, much like what was described for bacteria in chapter 5. The product made by this technique that may be furthest along in development is a blood-clotting factor produced in milk. However, some companies are trying to genetically engineer animals to produce useful proteins in their urine. This may seem repulsive, but there are some real advantages in producing compounds that are secreted in urine. While only females produce milk, both males and females produce urine, and urine is much less complex chemically than milk, so it may be easier to purify proteins produced in urine instead of milk. So far, experiments have produced genetically modified mice that produce small amounts of human-growth hormone. In addition to medically important proteins, scientists have also engineered animals that secrete other proteins of commercial interest, such as cows that produce silk protein in their milk.
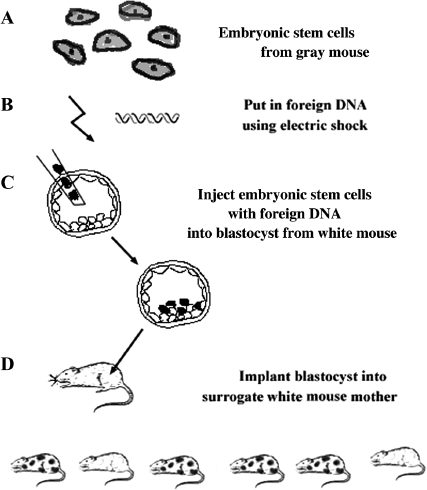
Figure 13.2 Genetic Modifications of Embryonic Stem Cells Using Mice of Different Colors. Note that the drawings are not to scale, the DNA, of course being much smaller than the cell, and the blastocysts being much smaller than the mice. A. Embryonic stem cells are obtained from the embryo of a gray-colored mouse. these cells are not actually gray; only the coat of the mouse is gray. The cells are shaded so that they can be distinguished from those of the white mouse. B. A foreign gene is transferred to the embryonic stem cells by electric shock. C. Embryonic stem cells with the foreign gene are injected into an early-stage embryo called a blastocyst. In this example, the blastocysts are derived from a white mouse so that we can distinguish the cells that have the foreign gene from those that do not. D. The blastocysts are then implanted into a surrogate mother that produces offspring. Some of the offspring are made up of a mixture of white-mice cells of the blastocyst and gray-mouse cells with the foreign gene, and for this reason they are called mosaics. If the cells from the gray mouse make the gametes, the sperm or the egg in these mosaics, breeding them will produce mice with the foreign gene in all their cells.
One can imagine that animals could be engineered for innumerable human medical purposes. In fact, pigs have been engineered to produce human hemoglobin for blood transfusions. Other pigs have been genetically modified so as not to express antigens recognized as foreign by humans. The organs of these engineered pigs could potentially be used as transplants in human patients because they would not be rejected. However, so far such applications have not yet been implemented. One danger is that viruses that infect animals could easily and inadvertently enter humans through the organs or blood products from engineered animals. Such viruses may not be transmitted easily now because of natural barriers to transmission, but organ transplant will facilitate transmission. Because we know very little about pig viruses, we do not know the risks of a pig virus causing a major disease in humans. If even a single pig virus caused disease in humans and was easily transmissible, we could be faced with a catastrophic epidemic. Scientists are well aware of these risks and take them very seriously. In short, animal genetic modification is still at an experimental stage. At this point, it is unclear whether genetically modified animals should be or will ever be used as tissue donors, protein factories, or for other purposes.
It may seem undignified to discuss humans in a chapter devoted to genetically modified animals, yet from a purely biological viewpoint, humans are no different than other mammals in regard to science’s ability to modify their genetic material. As you know, it is possible to fertilize human eggs with sperm in a laboratory dish and implant the young, dividing embryo into the uterus of the future mother. That mother may or may not be genetically related to the embryo. This technique is called in vitro fertilization, or IVF. This technique is now routinely used to help infertile couples have children.
As we saw, some animals have been engineered with foreign genes, one such gene being the one that codes for a blood-clotting factor. Why not then, one can reason, directly add a functional blood-clotting factor gene to a fertilized human egg that would otherwise become a hemophiliac? At this point, one answer is that this technique would be too dangerous. A point not mentioned previously is that when we insert a foreign gene into an organism, this gene randomly inserts into the genome of the host cell. It does not necessarily replace a copy of that gene in the genome, defective or not. A foreign gene can, by chance, insert into the middle of a gene, effectively mutating it. Thus, the blood-clotting factor gene injected into an egg could insert itself in a place of the genome where it could disrupt other genes. The effect of this disruption would be totally unpredictable; we would not know what gene might be affected and what the effect of the disruption would be on the organism. Another objection that many have is that changing the genetic features of a whole individual will result in genetically altered future generations of this individual. This change in the gametic cells, as compared to change in all the other cells of our body that will not produce future generations, is considered taboo by many.
Human beings can be genetically altered by adding genes to some of the cells of an affected individual rather than manipulating the egg, a procedure that will alter the genes of all the cells in an individual, including the cells destined to be gametes. Thus, gene therapy is being pursued for diseases in which a single gene defect affects primarily one type of tissue whose cells are accessible. In order for the disease to be treatable by this method, we first need to understand which gene is defective. This is an arduous process that we briefly discussed in chapter 9. Once the genetic defect is identified and the normal copy of that gene is isolated, there are two different approaches toward gene therapy. One method is to remove some of the affected cells or cells that will develop into affected cells from the patient, genetically modify those cells, and then return them to the patient. This type of procedure is called ex vivo gene therapy. The second method is to treat the patient directly through DNA injection into his or her organs. This type of procedure is called in vivo gene therapy.
Ex vivo gene therapy is used for diseases that arise from problems with blood or bone marrow cells. These cells, such as our red blood cells and cells of the immune system, circulate in our blood stream. The very first case of human gene therapy used this ex vivo approach. It was applied to a genetic condition called severe combined immunodeficiency (SCID). This disease results from a mutation in a gene coding for the enzyme adenosine deaminase (ADA). In the absence of ADA, affected individuals cannot develop a functioning immune system and soon die from even minor infections. The first SCID patient treated with gene therapy was a young girl named Ashanti DiSilva. Some of Ashanti DiSilva’s T cells (important components of the immune system) were removed from her blood, treated with a correct ADA gene, and reinjected into her body. Today, Ms. DiSilva leads a normal life, over twelve years after her treatment, and her ADA levels are normal. Since this pioneering clinical trial, several additional children with this condition have been treated with gene therapy. However, recently three of the treated children developed the same unusual form of leukemia, a cancer of the blood cells. It seems that all three diseases were caused by the insertion of the corrective gene into or near a cancer-causing gene. This is one danger of gene therapy, and a danger that is unpredictable. Thus gene therapy is still at an experimental stage even for cells that can be easily removed and added back to the patient.
A more general approach to gene therapy is to give a dose of the correct gene directly to the patient. However, this requires a safe vector that can target the gene to the right cells. Recall from chapter 5 that vectors are pieces of DNA that carry foreign DNA into cells. In gene therapy these vectors can be either plasmid or viral and must be able to carry the good copy of the gene to the cells that are affected. Viruses were considered good candidates for vectors for human gene therapy because some viruses, by their very nature, infect only a certain type of cells. For example, the flu virus typically infects cells in our respiratory tract and lungs. Yet an important consideration is that no negative effects be caused by the procedure. This is especially important if the vectors are viral DNA. Indeed, viral vectors must be able to invade the target cells, but they should not cause disease or an allergic response. Because of the potential dangers of viral vectors, some researchers are testing other type of vectors that are not of viral origin to transport DNA into cells.
Viral DNA vectors have already been used in human gene therapy trials aimed at correcting metabolic disorders. One such vector is DNA isolated from adenovirus, a rather benign virus responsible for one form of the common cold. When injected into the liver, for example, this virus is not expected to cause any symptoms. Unfortunately, this is not what happened to Jeff Gelsinger, a patient suffering from a defect in the gene that codes for an enzyme called ornithine transcarbamylase. This enzyme removes ammonia from the blood. The correct version of the gene was cloned into an adenovirus vector and injected into Jeff Gelsinger’s main liver artery. Shortly after the treatment, he started showing severe allergic response and died soon after. The autopsy showed that the viral DNA had propagated to all his organs and had triggered a massive immune response that killed him. As a result, clinical trials of human gene therapy using an adenovirus vector have been stopped. However, research continues with other viral vectors, particularly for the treatment of cystic fibrosis, a disease that has major manifestations in the lung cells. Clearly, much work is needed to ensure that gene therapy can be done safely.
Nevertheless, other gene-therapy trials are currently in progress. In the case of hemophilia, for example, one could insert a human blood-clotting factor gene into a viral DNA vector and inject the recombinant virus into the liver of the patient. If this procedure succeeded, the liver cells would make enough of the factor to ensure correct clotting of the blood. The first clinical trials of gene therapy for hemophilia were done on patients who made less than 1 percent of the normal amount of clotting factor. Though initial work was done more to test the safety of the procedure than to see if the disease could be cured, the three patients began to produce normal clotting factor. Though not cured, their symptoms were less severe.
Heart specialists also use gene therapy on a limited scale. It has been shown that the gene coding for vascular endothelial growth factor (VEGF), when injected into human muscle cells promotes the formation of blood vessels. As we know, many heart conditions are due to plugged-up arteries that can no longer supply the heart with oxygen. Injection of the VEGF gene into the heart can alleviate pathological symptoms through the formation of new blood vessels in the heart itself.
Stimulated by the success of animal cloning by nuclear transfer, some scientists have recently announced their intention to clone human beings by using the same technique. Basically, they would isolate nuclei from the cells of the donor wishing to be cloned, inject a diploid nucleus into an enucleated egg obtained from a volunteer female, and implant this egg into the womb of a surrogate mother. If all went well, the baby would be an almost exact genetic copy of the donor of the nucleus. We say “almost exact” rather than “exact” because human beings possess two types of genomes. The main genome resides in the cell nucleus and contains about 3.15 billion base pairs. However, human cells also contain mitochondrial DNA. Mitochondria are responsible for the production of energy and can be considered the energy factories of the cell. These bodies harbor a short piece of DNA that contains only about 16,600 base pairs. Thus, a human clone would still contain genes from mitochondrial DNA originating from the mitochondria present in the enucleated donor egg.
In principle, there is no reason to believe that human cloning would not work, given that it does work in several other mammalian species. However, it is clear that human cloning raises major ethical questions, simply because human beings and human embryos are involved. First, there is the high risk of fetal malformation as seen in the cases of all presently cloned animal species. Do we have the right to produce individuals that may end up crippled because of the procedure that led to their creation? Then there is the potential psychological impact on a clone (and perhaps on the nuclear donor) of being the almost perfect genetic copy of one of his or her parents, while sharing little with the egg donor. Further, there are the horrendous complications regarding the kinship of a clone. For example, let us assume that the nuclear donor is a man. His cloned boy will be his son, but this son will have no mother, only a paternal grandmother in the female category. And how should the clone look at the woman who donated the enucleated egg? Would she be his mother? In a genetic sense, this “mother” would have only contributed mitochondrial DNA. Finally, since human cloning is reputedly sought mostly by infertile couples, the birth mother of the clone could very well be a surrogate, totally genetically unrelated to the “parents.” In other words, the clone would have two “mothers” (the enucleated egg donor and the surrogate that brought him to term) and one father of whom he is a copy. Many other situations involving cloning can be imagined, and you are invited to do so.
All the mostly negative press given to human reproductive cloning has unfortunately obscured the potential benefits of cloning in the medical arena. The technique we will describe below does not directly involve human reproduction, but it uses human embryos as cell donors for medical purposes. Since human embryos are destroyed in the process, this technique is not without controversy either.
We saw in this chapter that genetic diseases could, in principle, be remedied by injection of a cloned “good” gene. However, not all diseases are amenable to treatment by gene injection. For example, heart disease, degenerative kidney disease, and arthritis (also a degenerative disease), as well as spinal-cord injuries, are not the result of the malfunctioning of a single gene. Going back to embryonic stem cells (see chapter 4), we have seen that they can differentiate into any kind of specialized tissue. Given that, they might be able to regenerate damaged heart, spinal-cord, kidney and joint tissues if injected into these organs. This has indeed been shown to a certain extent in other animals, such as the mouse. Why not then apply this technique to humans? The first problem is that embryonic stem cells from a donor will not be immunologically compatible with the cells of the recipient. These cells would quickly be rejected, though there is a way around this. Embryonic stem cells could be derived from an embryo that was the result of a nuclear transfer from the person suffering from the disease. In this case, since the embryo would be practically genetically identical to the nuclear donor, rejection would not happen.
However, a major problem is that one must first create this human embryo and then dissect it in order to use its cells. This procedure is not compatible with embryo survival. For some, this practice is equivalent to murder and cannot be condoned. For now, stem-cell research from cloned human embryos cannot be conducted with federal funds in the United States. Nevertheless, a private U.S. company has announced partial success in human embryo cloning by nuclear transfer, and research is also proceeding in other countries. The future of cloned embryonic stem cells in human medicine is presently uncertain.
The new genetic technology carries enormous potential for medical applications. These applications range from utilizing animals as biofactories to human gene therapy and to human therapeutic cloning. All the basic techniques to achieve these goals are available but must be refined. The use of human embryos, either for reproductive cloning or for therapeutic cloning, is highly controversial, however. As is often the case with new technologies, the good often comes with the bad. We hope that a thorough understanding of the genetic principles explained in this book will allow you to make objective decisions regarding all the potential—and sometimes unsettling—applications of genetics.