Neurologic System
• Familiar objects (coins, keys, paper clip)
• Tongue blades (one intact and one broken with pointed and rounded edges)
• Tuning forks, 200 to 400 Hz and 500 to 1000 Hz
• Test tubes of hot and cold water
• Vials of aromatic substances (coffee, orange, peppermint, banana)
• Vials of solutions (glucose, salt, lemon or vinegar, quinine) with applicators
Examination
Assess the neurologic system as the rest of the body is examined. When history and examination findings have not revealed a potential neurologic problem, perform a neurologic screening examination as shown in the box on pp. 218-219, rather than a full neurologic examination. See Chapter 18 for evaluation of muscle tone and strength, because these findings are important for interpreting neurologic system examination findings. The mental status portion of the neurologic system examination can be found in Chapter 3.
Cranial Nerves I To XII
The following table summarizes the CN examination, and details of examination follow on pp. 220-224. When a sensory or motor loss is suspected, be compulsive about determining the extent of the loss.
Procedures for Cranial Nerve Examination
| Cranial Nerve (CN) | Procedure |
| CN I (olfactory) | Test ability to identify familiar aromatic odors, one naris at a time with eyes closed. |
| CN II (optic) | Test distance and near vision. Perform an ophthalmoscopic examination. Test visual fields by confrontation and extinction of vision. |
| CN III, CN IV, CN VI (oculomotor, trochlear, abducens) | Test extraocular movement. Inspect eyelids for drooping. Inspect pupil size for equality, and direct and consensual response to light and accommodation. |
| CN V (trigeminal) | Inspect face for muscle atrophy and tremors. Palpate jaw muscles for tone and strength when patient clenches teeth. Test superficial pain and touch sensation in each nerve branch. (Test temperature sensation if findings to pain and touch sensation are unexpected.) Test corneal reflex. |
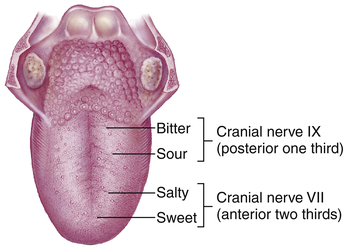
| CN VII (facial) | Inspect symmetry of facial features with various expressions (e.g., smile, frown, puffed cheeks, wrinkled forehead). Test ability to identify sweet, salty, sour, and bitter tastes on each side of tongue. |
| CN VIII (acoustic) | Test sense of hearing with whisper screening tests or by audiometry. Compare bone and air conduction of sound. Test for lateralization of sound. |
| CN IX (glossopharyngeal) | Test taste sensation (see CN VII). Test gag reflex and ability to swallow. |
| CN X (vagus) | Inspect palate and uvula for symmetry with speech sounds and gag reflex. Observe for swallowing difficulty. Evaluate quality of guttural speech sounds (presence of nasal or hoarse quality to voice). |
| CN XI (spinal accessory) | Test trapezius muscle strength (shrug shoulders against resistance). Test sternocleidomastoid muscle strength (turn head to each side against resistance). |
| CN XII (hypoglossal) | Inspect tongue in mouth and while protruded for symmetry, tremors, atrophy. Inspect tongue movement toward nose and chin. Test tongue strength with index finger when tongue is pressed against cheek. Evaluate quality of lingual speech sounds (l, t, d, n). |
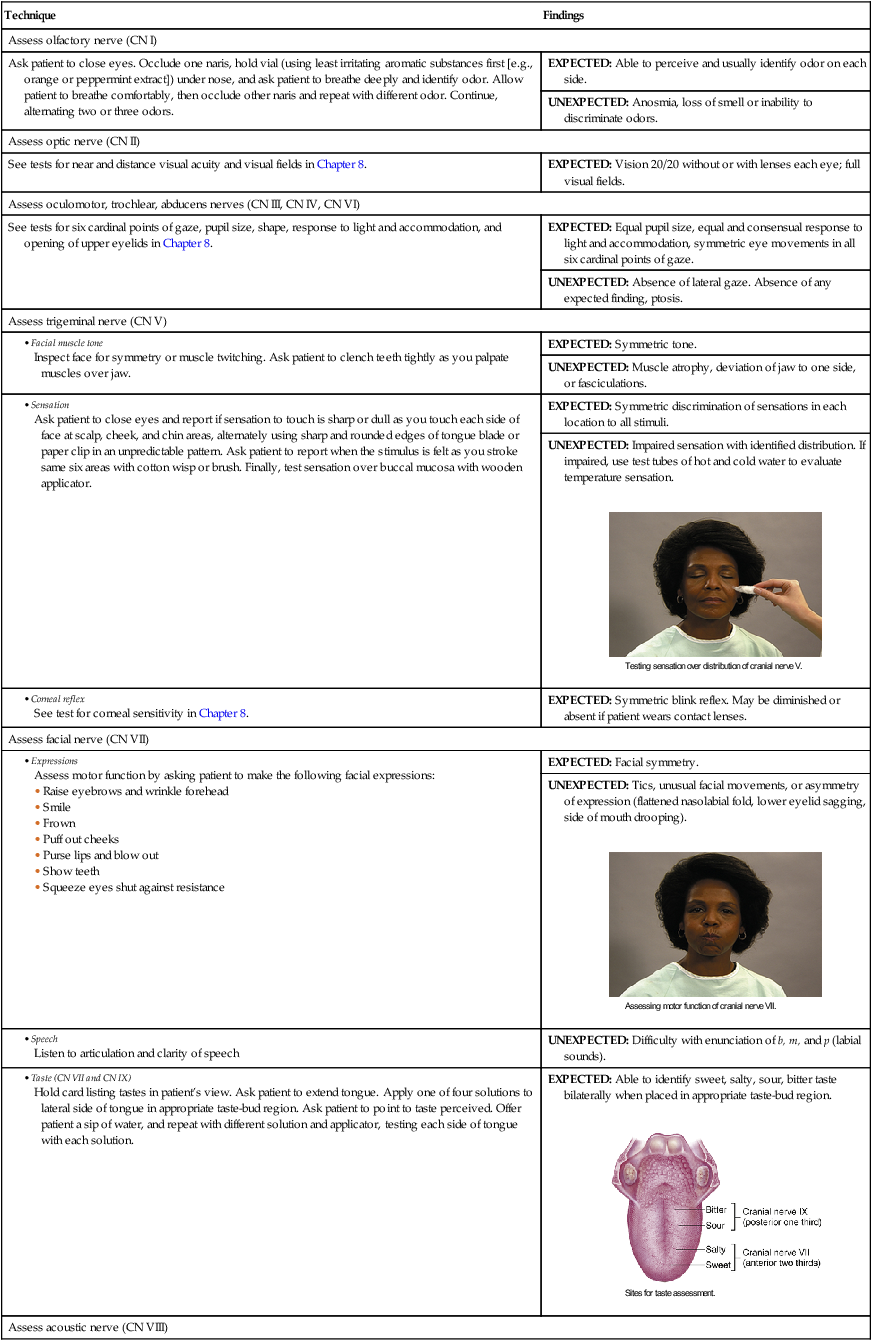
| Technique | Findings |
| Assess olfactory nerve (CN I) | |
| Ask patient to close eyes. Occlude one naris, hold vial (using least irritating aromatic substances first [e.g., orange or peppermint extract]) under nose, and ask patient to breathe deeply and identify odor. Allow patient to breathe comfortably, then occlude other naris and repeat with different odor. Continue, alternating two or three odors. | EXPECTED: Able to perceive and usually identify odor on each side. |
| UNEXPECTED: Anosmia, loss of smell or inability to discriminate odors. | |
| Assess optic nerve (CN II) | |
| See tests for near and distance visual acuity and visual fields in Chapter 8. | EXPECTED: Vision 20/20 without or with lenses each eye; full visual fields. |
| Assess oculomotor, trochlear, abducens nerves (CN III, CN IV, CN VI) | |
| See tests for six cardinal points of gaze, pupil size, shape, response to light and accommodation, and opening of upper eyelids in Chapter 8. | EXPECTED: Equal pupil size, equal and consensual response to light and accommodation, symmetric eye movements in all six cardinal points of gaze. |
| UNEXPECTED: Absence of lateral gaze. Absence of any expected finding, ptosis. | |
| Assess trigeminal nerve (CN V) | |
| EXPECTED: Symmetric tone. | |
| UNEXPECTED: Muscle atrophy, deviation of jaw to one side, or fasciculations. | |
|
Ask patient to close eyes and report if sensation to touch is sharp or dull as you touch each side of face at scalp, cheek, and chin areas, alternately using sharp and rounded edges of tongue blade or paper clip in an unpredictable pattern. Ask patient to report when the stimulus is felt as you stroke same six areas with cotton wisp or brush. Finally, test sensation over buccal mucosa with wooden applicator. |
EXPECTED: Symmetric discrimination of sensations in each location to all stimuli. |
| UNEXPECTED: Impaired sensation with identified distribution. If impaired, use test tubes of hot and cold water to evaluate temperature sensation. | |
|
See test for corneal sensitivity in Chapter 8. |
EXPECTED: Symmetric blink reflex. May be diminished or absent if patient wears contact lenses. |
| Assess facial nerve (CN VII) | |
| EXPECTED: Facial symmetry. | |
| UNEXPECTED: Tics, unusual facial movements, or asymmetry of expression (flattened nasolabial fold, lower eyelid sagging, side of mouth drooping). | |
| UNEXPECTED: Difficulty with enunciation of b, m, and p (labial sounds). | |
|
Hold card listing tastes in patient’s view. Ask patient to extend tongue. Apply one of four solutions to lateral side of tongue in appropriate taste-bud region. Ask patient to point to taste perceived. Offer patient a sip of water, and repeat with different solution and applicator, testing each side of tongue with each solution. |
EXPECTED: Able to identify sweet, salty, sour, bitter taste bilaterally when placed in appropriate taste-bud region. |
| Assess acoustic nerve (CN VIII) | |
|
See screening tests in Chapter 9 or use an audiometer to test hearing. |
EXPECTED: Adequate hearing bilaterally. |
|
See Romberg test on p. 225. |
|
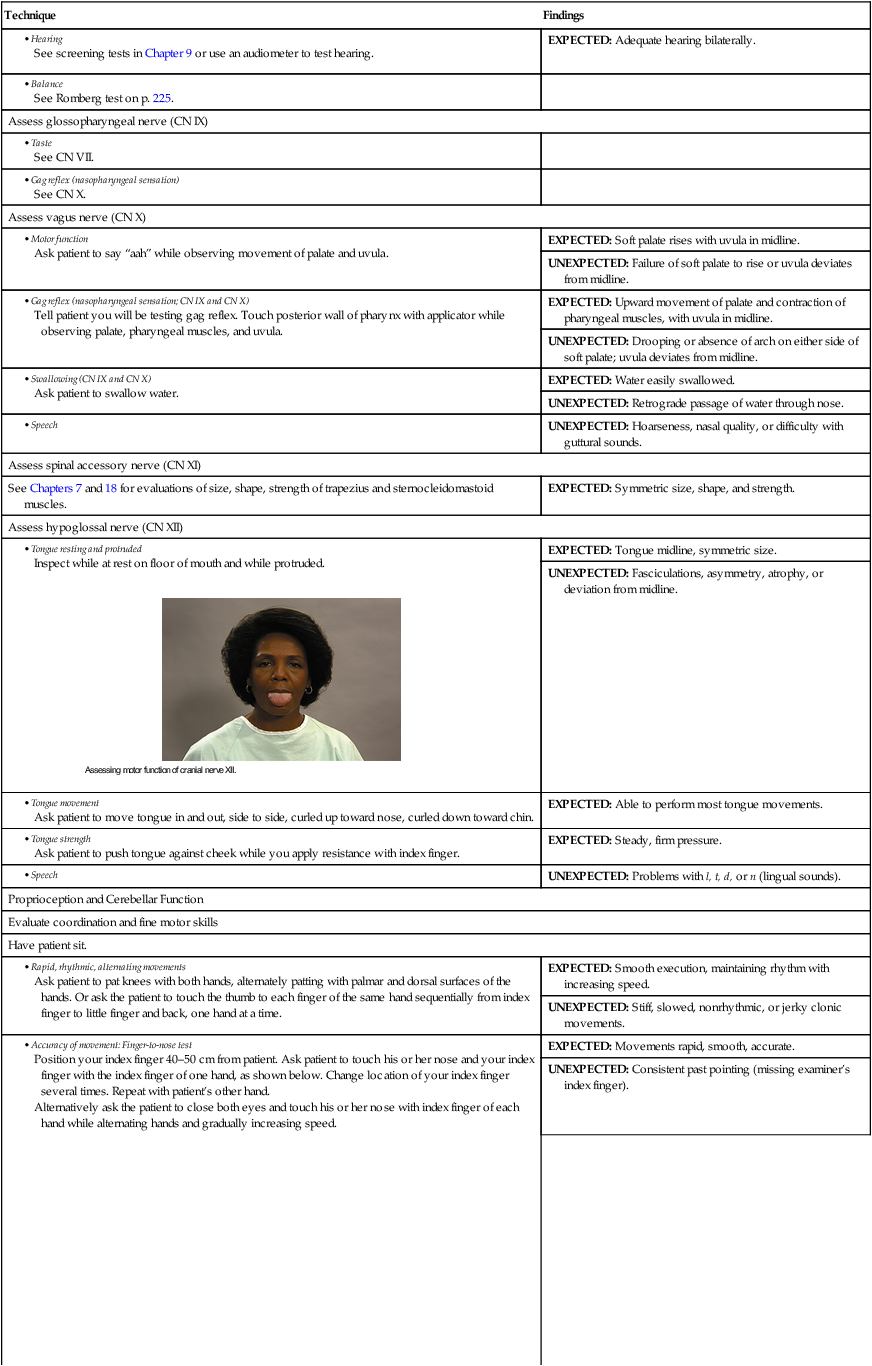
| Assess glossopharyngeal nerve (CN IX) | |
| Assess vagus nerve (CN X) | |
| EXPECTED: Soft palate rises with uvula in midline. | |
| UNEXPECTED: Failure of soft palate to rise or uvula deviates from midline. | |
| EXPECTED: Upward movement of palate and contraction of pharyngeal muscles, with uvula in midline. | |
| UNEXPECTED: Drooping or absence of arch on either side of soft palate; uvula deviates from midline. | |
| EXPECTED: Water easily swallowed. | |
| UNEXPECTED: Retrograde passage of water through nose. | |
| UNEXPECTED: Hoarseness, nasal quality, or difficulty with guttural sounds. | |
| Assess spinal accessory nerve (CN XI) | |
| See Chapters 7 and 18 for evaluations of size, shape, strength of trapezius and sternocleidomastoid muscles. | EXPECTED: Symmetric size, shape, and strength. |
| Assess hypoglossal nerve (CN XII) | |
| EXPECTED: Tongue midline, symmetric size. | |
| UNEXPECTED: Fasciculations, asymmetry, atrophy, or deviation from midline. | |
| EXPECTED: Able to perform most tongue movements. | |
| EXPECTED: Steady, firm pressure. | |
| UNEXPECTED: Problems with l, t, d, or n (lingual sounds). | |
| Proprioception and Cerebellar Function | |
| Evaluate coordination and fine motor skills | |
| Have patient sit. | |
| EXPECTED: Smooth execution, maintaining rhythm with increasing speed. | |
| UNEXPECTED: Stiff, slowed, nonrhythmic, or jerky clonic movements. | |
|
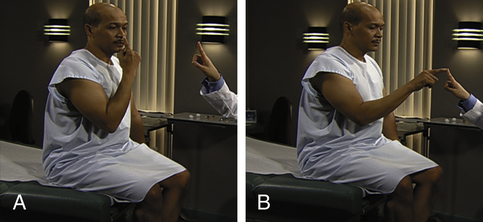
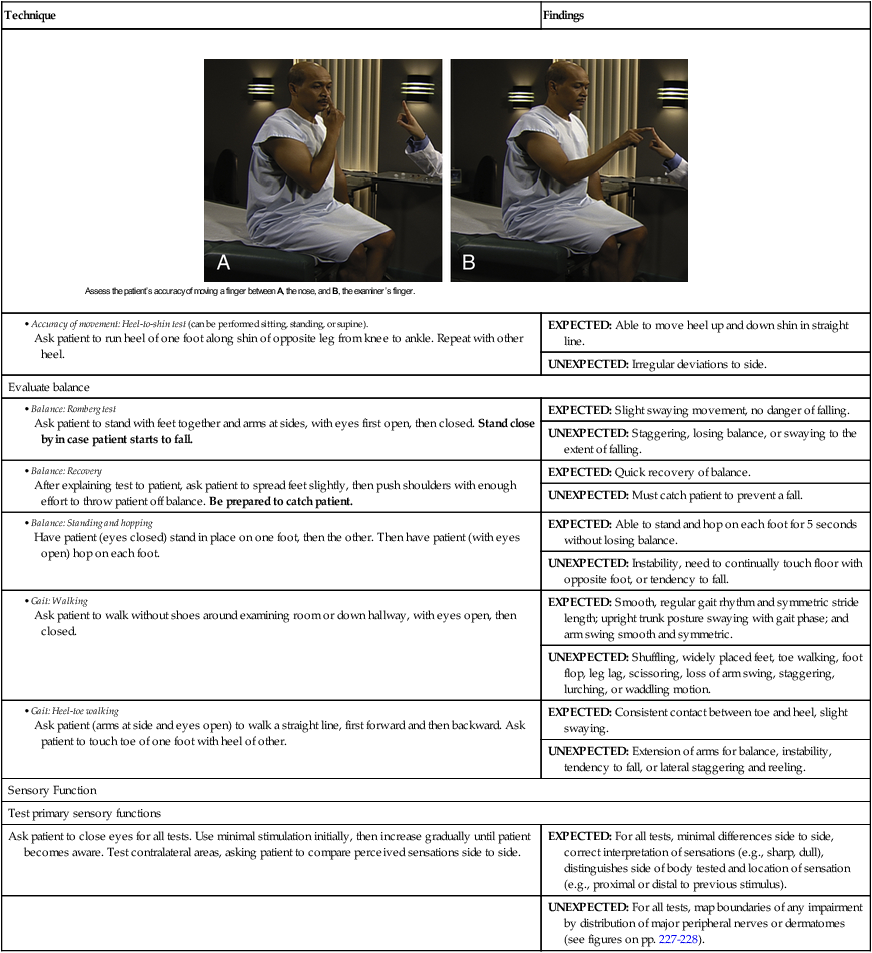
• Accuracy of movement: Finger-to-nose test Position your index finger 40–50 cm from patient. Ask patient to touch his or her nose and your index finger with the index finger of one hand, as shown below. Change location of your index finger several times. Repeat with patient’s other hand. Alternatively ask the patient to close both eyes and touch his or her nose with index finger of each hand while alternating hands and gradually increasing speed. |
EXPECTED: Movements rapid, smooth, accurate. |
| UNEXPECTED: Consistent past pointing (missing examiner’s index finger). | |
| EXPECTED: Able to move heel up and down shin in straight line. | |
| UNEXPECTED: Irregular deviations to side. | |
| Evaluate balance | |
| EXPECTED: Slight swaying movement, no danger of falling. | |
| UNEXPECTED: Staggering, losing balance, or swaying to the extent of falling. | |
| EXPECTED: Quick recovery of balance. | |
| UNEXPECTED: Must catch patient to prevent a fall. | |
| EXPECTED: Able to stand and hop on each foot for 5 seconds without losing balance. | |
| UNEXPECTED: Instability, need to continually touch floor with opposite foot, or tendency to fall. | |
| EXPECTED: Smooth, regular gait rhythm and symmetric stride length; upright trunk posture swaying with gait phase; and arm swing smooth and symmetric. | |
| UNEXPECTED: Shuffling, widely placed feet, toe walking, foot flop, leg lag, scissoring, loss of arm swing, staggering, lurching, or waddling motion. | |
| EXPECTED: Consistent contact between toe and heel, slight swaying. | |
| UNEXPECTED: Extension of arms for balance, instability, tendency to fall, or lateral staggering and reeling. | |
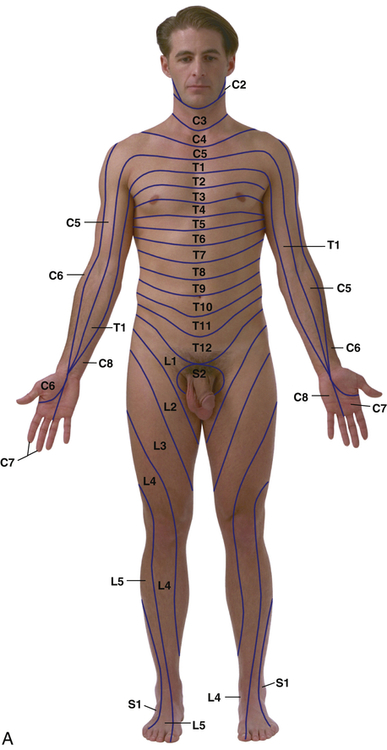
| Sensory Function | |
| Test primary sensory functions | |
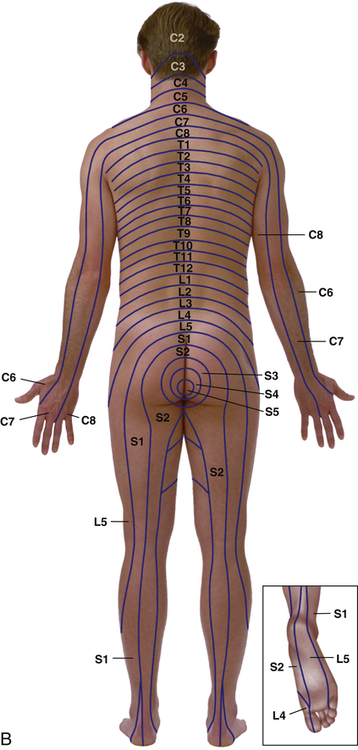
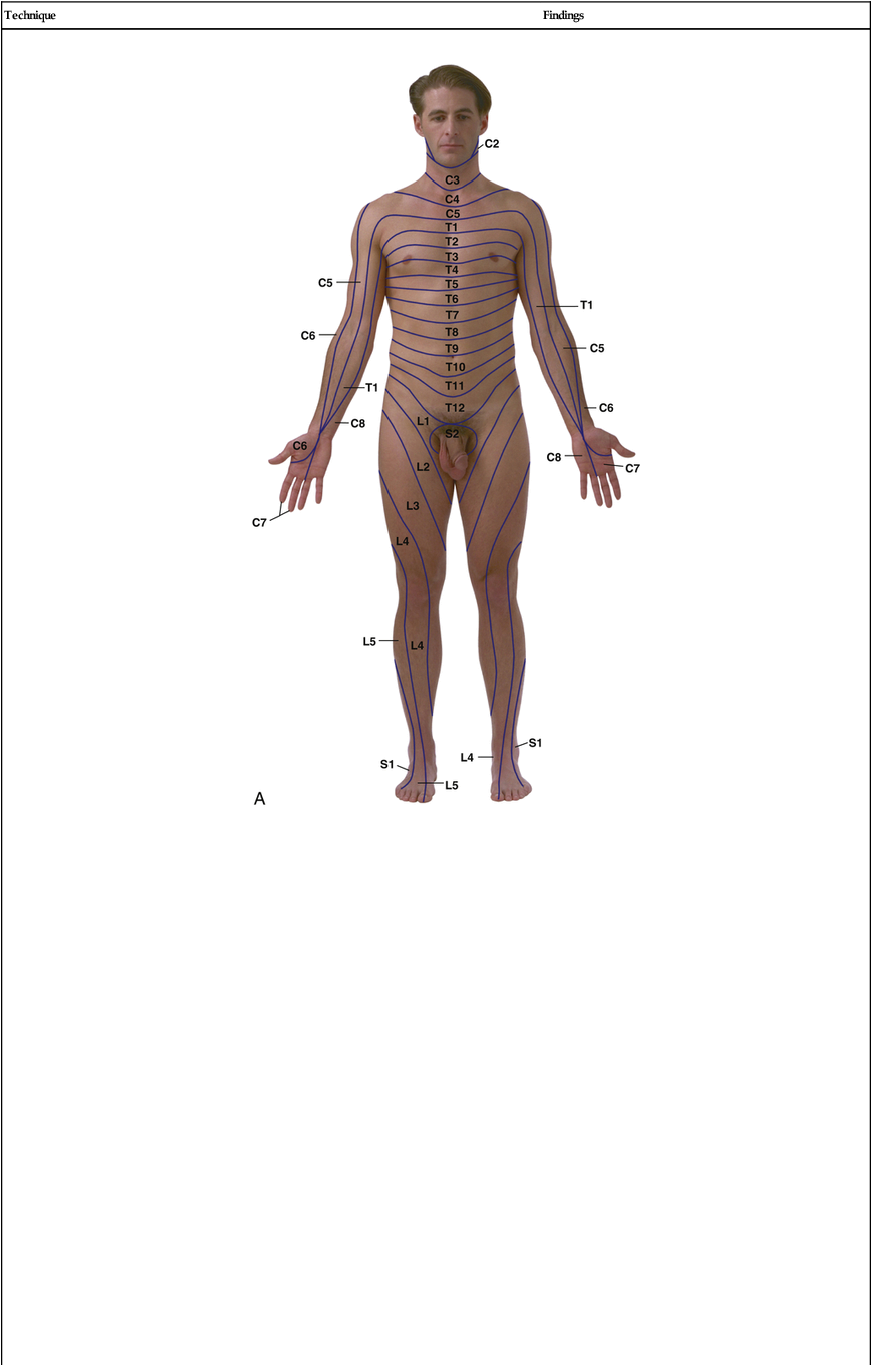
| Ask patient to close eyes for all tests. Use minimal stimulation initially, then increase gradually until patient becomes aware. Test contralateral areas, asking patient to compare perceived sensations side to side. | EXPECTED: For all tests, minimal differences side to side, correct interpretation of sensations (e.g., sharp, dull), distinguishes side of body tested and location of sensation (e.g., proximal or distal to previous stimulus). |
| UNEXPECTED: For all tests, map boundaries of any impairment by distribution of major peripheral nerves or dermatomes (see figures on pp. 227-228). | |
 |
|
| EXPECTED: Distinguishes between hot and cold and location of sensation. | |
| EXPECTED: Discomfort with deep pressure. | |
|
|
EXPECTED: Sensation felt at all sites touched.UNEXPECTED: Loss of sensation at any site. |
|
Place stem of vibrating tuning fork against several bony prominences (e.g., toes, ankle, shin, finger joints, wrist, elbow, shoulder, sternum), beginning distally. Ask patient when and where sensation is felt and what it feels like. Dampen tines occasionally to see whether patient notices the difference. |
EXPECTED: Buzzing or tingling sensation, correct location of stimulus. |
| UNEXPECTED: Does not distinguish vibration from touch of nonvibrating tuning fork. | |
|
|
EXPECTED: Patient correctly identifies position of joint. |
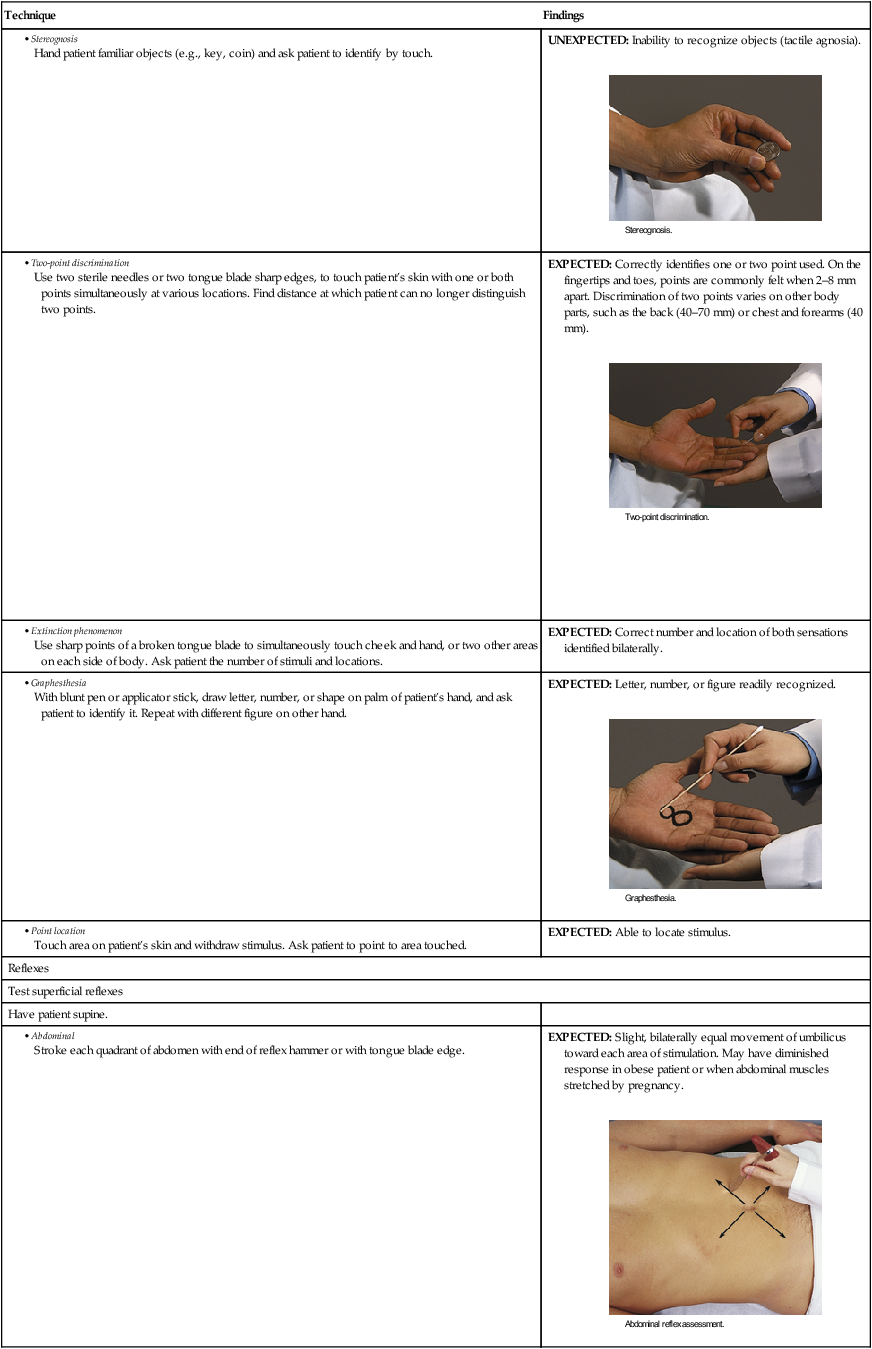
| Test cortical sensory functions | |
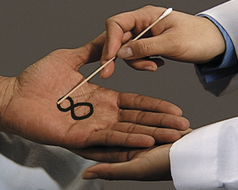
| Ask patient to close eyes for all tests. | |
| UNEXPECTED: Inability to recognize objects (tactile agnosia). | |
| EXPECTED: Correctly identifies one or two point used. On the fingertips and toes, points are commonly felt when 2–8 mm apart. Discrimination of two points varies on other body parts, such as the back (40–70 mm) or chest and forearms (40 mm). | |
| EXPECTED: Correct number and location of both sensations identified bilaterally. | |
| EXPECTED: Letter, number, or figure readily recognized. | |
| EXPECTED: Able to locate stimulus. | |
| Reflexes | |
| Test superficial reflexes | |
| Have patient supine. | |
| EXPECTED: Slight, bilaterally equal movement of umbilicus toward each area of stimulation. May have diminished response in obese patient or when abdominal muscles stretched by pregnancy. | |
| EXPECTED: Testicle and scrotum rise on stroked side. | |
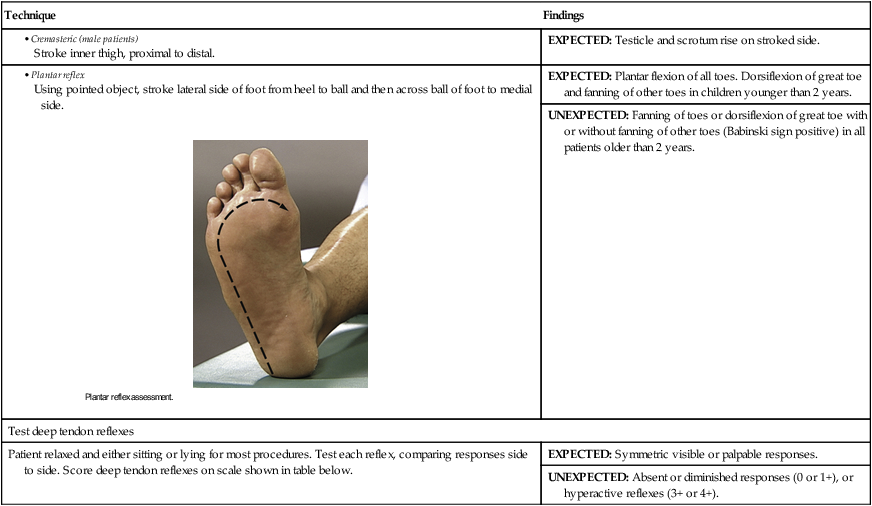
|
|
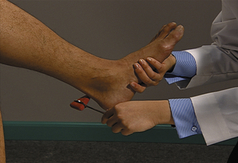
EXPECTED: Plantar flexion of all toes. Dorsiflexion of great toe and fanning of other toes in children younger than 2 years. |
| UNEXPECTED: Fanning of toes or dorsiflexion of great toe with or without fanning of other toes (Babinski sign positive) in all patients older than 2 years. | |
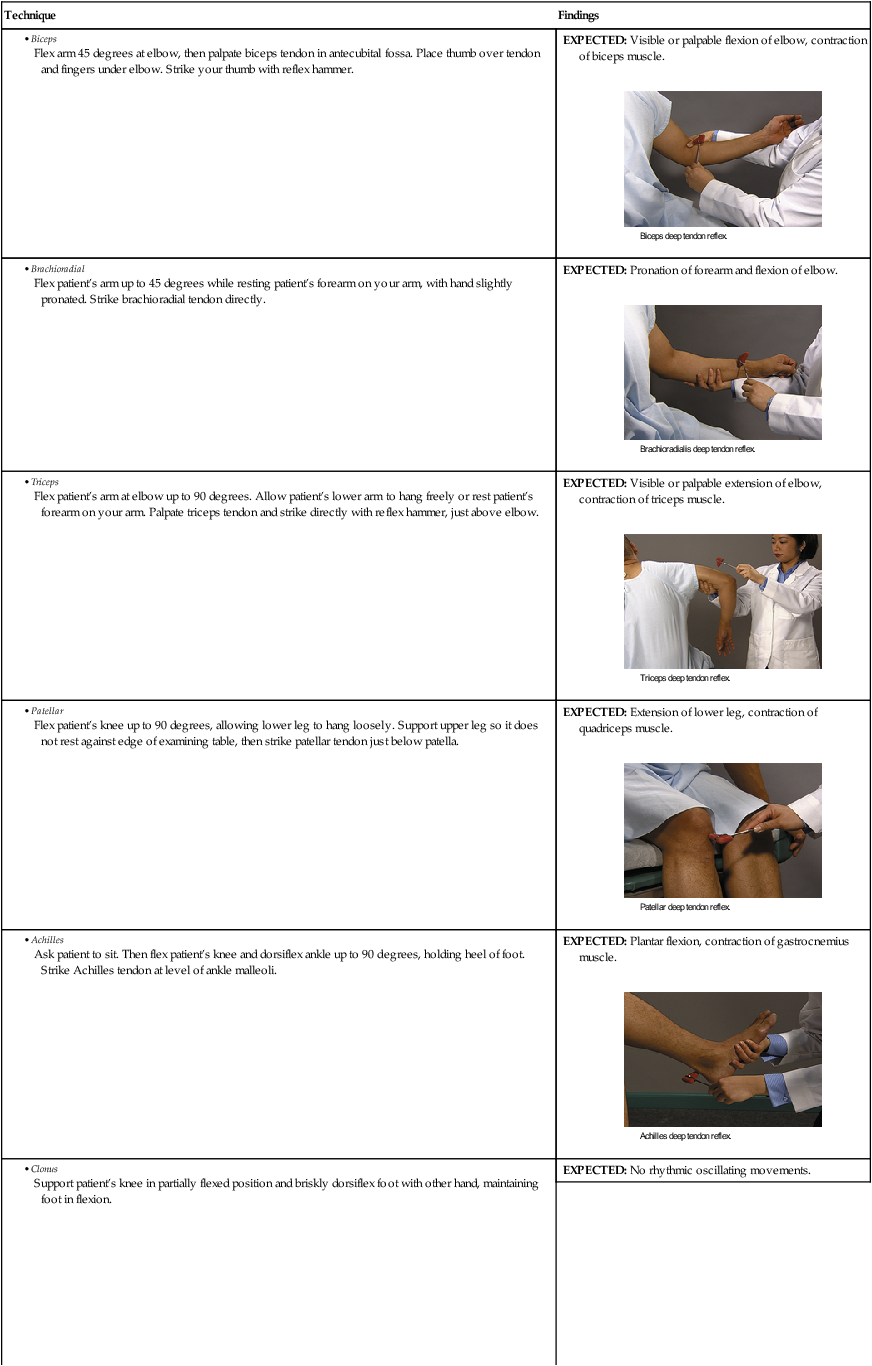
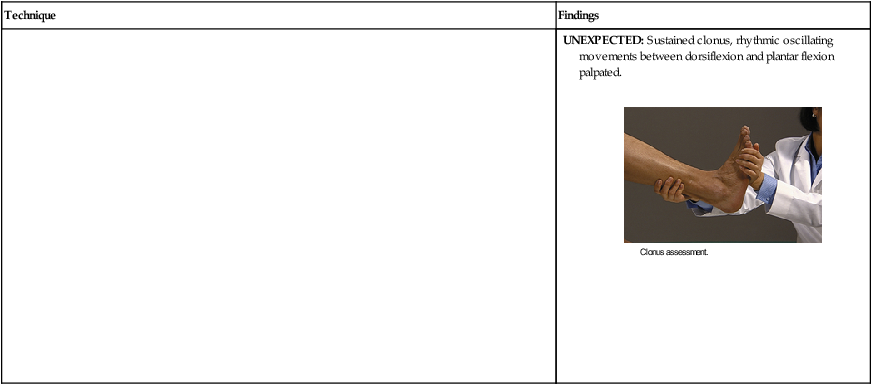
| Test deep tendon reflexes | |
| Patient relaxed and either sitting or lying for most procedures. Test each reflex, comparing responses side to side. Score deep tendon reflexes on scale shown in table below. | EXPECTED: Symmetric visible or palpable responses. |
| UNEXPECTED: Absent or diminished responses (0 or 1+), or hyperactive reflexes (3+ or 4+). | |


| Grade | Deep Tendon Reflex Response |
| 0 | No response |
| 1+ | Sluggish or diminished |
| 2+ | Active or expected response |
| 3+ | More brisk than expected, slightly hyperactive |
| 4+ | Brisk, hyperactive, with intermittent or transient clonus |
| Technique | Findings |
| EXPECTED: Visible or palpable flexion of elbow, contraction of biceps muscle. | |
| EXPECTED: Pronation of forearm and flexion of elbow. | |
| EXPECTED: Visible or palpable extension of elbow, contraction of triceps muscle. | |
| EXPECTED: Extension of lower leg, contraction of quadriceps muscle. | |
| EXPECTED: Plantar flexion, contraction of gastrocnemius muscle. | |
| EXPECTED: No rhythmic oscillating movements. | |
| UNEXPECTED: Sustained clonus, rhythmic oscillating movements between dorsiflexion and plantar flexion palpated. |
Differential Diagnosis of Upper and Lower Motor Neuron Disorders
| Assessment Parameters | Upper Motor Neuron | Lower Motor Neuron |
| Muscle tone | Increased tone, muscle spasticity, risk for contractures | Decreased tone, muscle flaccidity |
| Muscle atrophy | Little or no muscle atrophy, but decreased strength | Loss of muscle strength; muscle atrophy or wasting |
| Sensation | Sensation loss may affect entire limb | Sensory loss that follows the distribution of dermatomes or peripheral nerves |
| Reflexes | Hyperactive deep tendon and abdominal reflexes; positive Babinski sign | Weak or absent deep tendon, plantar, and abdominal reflexes, negative plantar reflex, no pathologic reflexes |
| Fasciculation | No fasciculations | Fasciculations |
| Motor effect | Paralysis of voluntary movements | Paralysis of muscles |
| Location of insult | Damage above level of brainstem will affect contralateral side of body, damage below the brainstem will affect the ipsilateral side of the body | Damage affects muscle on ipsilateral side of body |
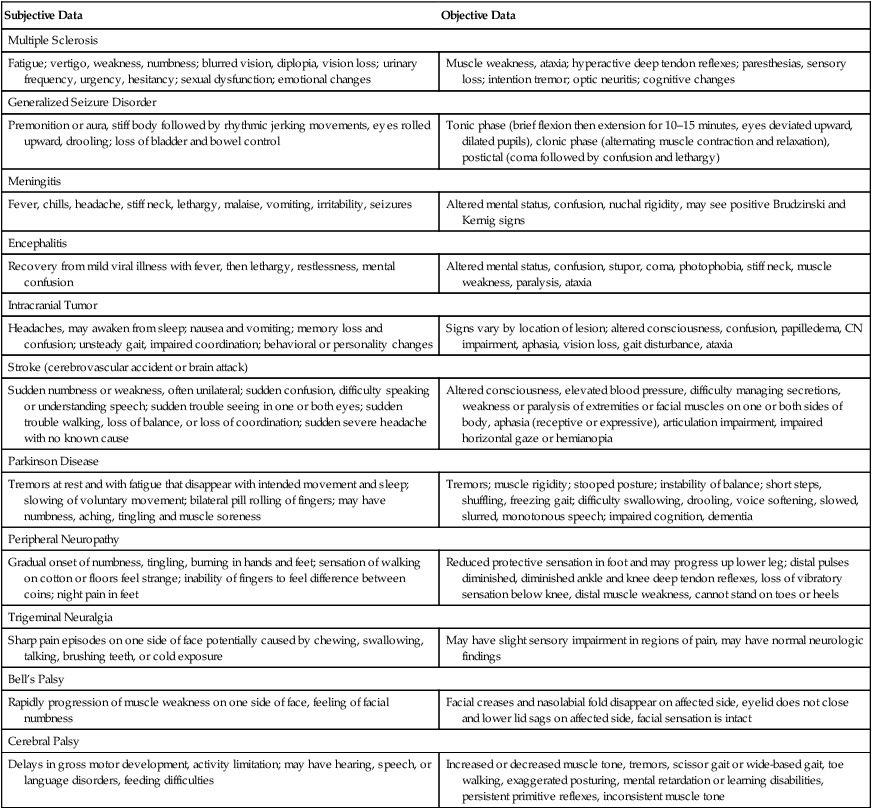
Aids To Differential Diagnosis
| Subjective Data | Objective Data |
| Multiple Sclerosis | |
| Fatigue; vertigo, weakness, numbness; blurred vision, diplopia, vision loss; urinary frequency, urgency, hesitancy; sexual dysfunction; emotional changes | Muscle weakness, ataxia; hyperactive deep tendon reflexes; paresthesias, sensory loss; intention tremor; optic neuritis; cognitive changes |
| Generalized Seizure Disorder | |
| Premonition or aura, stiff body followed by rhythmic jerking movements, eyes rolled upward, drooling; loss of bladder and bowel control | Tonic phase (brief flexion then extension for 10–15 minutes, eyes deviated upward, dilated pupils), clonic phase (alternating muscle contraction and relaxation), postictal (coma followed by confusion and lethargy) |
| Meningitis | |
| Fever, chills, headache, stiff neck, lethargy, malaise, vomiting, irritability, seizures | Altered mental status, confusion, nuchal rigidity, may see positive Brudzinski and Kernig signs |
| Encephalitis | |
| Recovery from mild viral illness with fever, then lethargy, restlessness, mental confusion | Altered mental status, confusion, stupor, coma, photophobia, stiff neck, muscle weakness, paralysis, ataxia |
| Intracranial Tumor | |
| Headaches, may awaken from sleep; nausea and vomiting; memory loss and confusion; unsteady gait, impaired coordination; behavioral or personality changes | Signs vary by location of lesion; altered consciousness, confusion, papilledema, CN impairment, aphasia, vision loss, gait disturbance, ataxia |
| Stroke (cerebrovascular accident or brain attack) | |
| Sudden numbness or weakness, often unilateral; sudden confusion, difficulty speaking or understanding speech; sudden trouble seeing in one or both eyes; sudden trouble walking, loss of balance, or loss of coordination; sudden severe headache with no known cause | Altered consciousness, elevated blood pressure, difficulty managing secretions, weakness or paralysis of extremities or facial muscles on one or both sides of body, aphasia (receptive or expressive), articulation impairment, impaired horizontal gaze or hemianopia |
| Parkinson Disease | |
| Tremors at rest and with fatigue that disappear with intended movement and sleep; slowing of voluntary movement; bilateral pill rolling of fingers; may have numbness, aching, tingling and muscle soreness | Tremors; muscle rigidity; stooped posture; instability of balance; short steps, shuffling, freezing gait; difficulty swallowing, drooling, voice softening, slowed, slurred, monotonous speech; impaired cognition, dementia |
| Peripheral Neuropathy | |
| Gradual onset of numbness, tingling, burning in hands and feet; sensation of walking on cotton or floors feel strange; inability of fingers to feel difference between coins; night pain in feet | Reduced protective sensation in foot and may progress up lower leg; distal pulses diminished, diminished ankle and knee deep tendon reflexes, loss of vibratory sensation below knee, distal muscle weakness, cannot stand on toes or heels |
| Trigeminal Neuralgia | |
| Sharp pain episodes on one side of face potentially caused by chewing, swallowing, talking, brushing teeth, or cold exposure | May have slight sensory impairment in regions of pain, may have normal neurologic findings |
| Bell’s Palsy | |
| Rapidly progression of muscle weakness on one side of face, feeling of facial numbness | Facial creases and nasolabial fold disappear on affected side, eyelid does not close and lower lid sags on affected side, facial sensation is intact |
| Cerebral Palsy | |
| Delays in gross motor development, activity limitation; may have hearing, speech, or language disorders, feeding difficulties | Increased or decreased muscle tone, tremors, scissor gait or wide-based gait, toe walking, exaggerated posturing, mental retardation or learning disabilities, persistent primitive reflexes, inconsistent muscle tone |
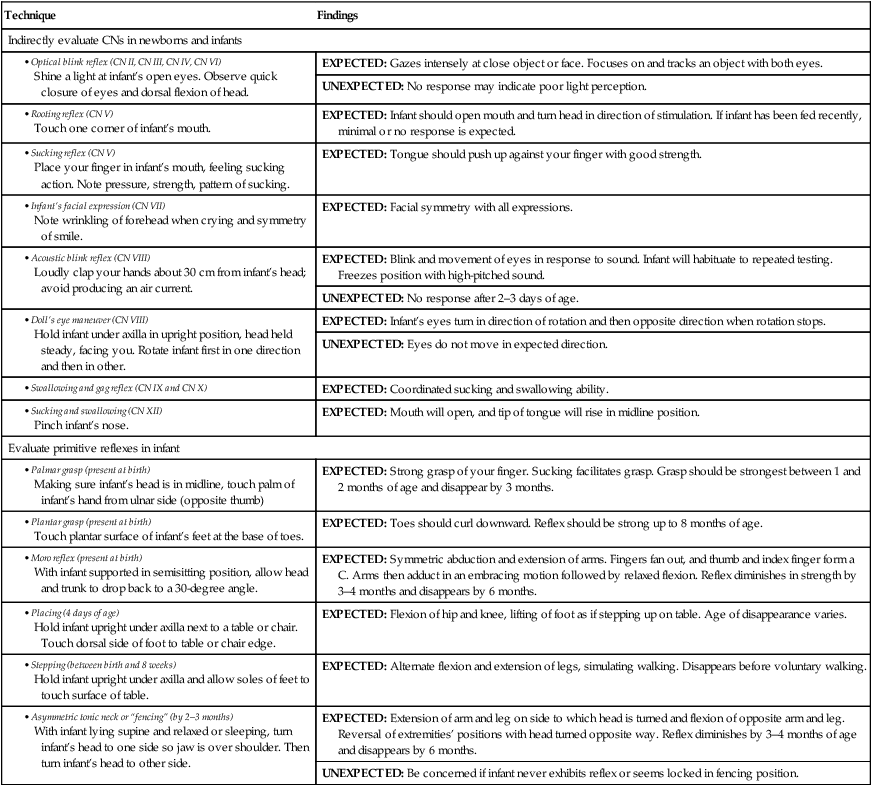
PEDIATRIC VARIATIONS
EXAMINATION
Neurologic findings in the infant and child change as the child matures. (For a complete description of expected developmental findings by age, see Chapter 21.)
| Technique | Findings |
| Indirectly evaluate CNs in newborns and infants | |
| EXPECTED: Gazes intensely at close object or face. Focuses on and tracks an object with both eyes. | |
| UNEXPECTED: No response may indicate poor light perception. | |
| EXPECTED: Infant should open mouth and turn head in direction of stimulation. If infant has been fed recently, minimal or no response is expected. | |
| EXPECTED: Tongue should push up against your finger with good strength. | |
| EXPECTED: Facial symmetry with all expressions. | |
| EXPECTED: Blink and movement of eyes in response to sound. Infant will habituate to repeated testing. Freezes position with high-pitched sound. | |
| UNEXPECTED: No response after 2–3 days of age. | |
| EXPECTED: Infant’s eyes turn in direction of rotation and then opposite direction when rotation stops. | |
| UNEXPECTED: Eyes do not move in expected direction. | |
| EXPECTED: Coordinated sucking and swallowing ability. | |
| EXPECTED: Mouth will open, and tip of tongue will rise in midline position. | |
| Evaluate primitive reflexes in infant | |
| EXPECTED: Strong grasp of your finger. Sucking facilitates grasp. Grasp should be strongest between 1 and 2 months of age and disappear by 3 months. | |
| EXPECTED: Toes should curl downward. Reflex should be strong up to 8 months of age. | |
| EXPECTED: Symmetric abduction and extension of arms. Fingers fan out, and thumb and index finger form a C. Arms then adduct in an embracing motion followed by relaxed flexion. Reflex diminishes in strength by 3–4 months and disappears by 6 months. | |
| EXPECTED: Flexion of hip and knee, lifting of foot as if stepping up on table. Age of disappearance varies. | |
| EXPECTED: Alternate flexion and extension of legs, simulating walking. Disappears before voluntary walking. | |
| EXPECTED: Extension of arm and leg on side to which head is turned and flexion of opposite arm and leg. Reversal of extremities’ positions with head turned opposite way. Reflex diminishes by 3–4 months of age and disappears by 6 months. | |
| UNEXPECTED: Be concerned if infant never exhibits reflex or seems locked in fencing position. | |
Sample Documentation
Subjective
A 48-year-old man presents for his annual physical examination. No concerns about poor balance, loss of sensation, unsteady gait. History of diabetes mellitus type 1 for 30 years, well controlled.
Objective
CNs II to XII grossly intact. Gait is coordinated and even. Romberg negative. Rapid alternating movements coordinated and smooth. Superficial touch, pain, vibratory sensation are intact bilaterally. Deep tendon reflexes 2+ bilaterally in all extremities. Plantar reflex produces expected plantar flexion of toes. No ankle clonus. Monofilament test reveals decreased sensation on plantar surfaces of both feet.