Life is one long process of getting tired.
Samuel Butler (1835–1902)
What do we mean by the term ‘fatigue’? According to the Oxford English Dictionary definition, fatigue is ‘Lassitude or weariness resulting from either bodily or mental exertion. Physiologically as: A condition of muscles, organs or cells characterised by a temporary reduction in power or sensitivity following a period of prolonged activity or stimulation.’
Patients tend to express their feelings of fatigue as aches in muscles, severe pain in joints, weakness in one or more limb, and/or a lack of energy and vitality. Patients with CFS/ME may feel as though they have just run a marathon when they have only walked round the block, or that picking up their suitcase is as hard a task as trying to lift a ton weight. In other words, the resultant aches and pains are apparently unjustified in relation to the physical stress on the body.
What happens in fatigue
Muscle fibres contract due to stimulation from the nerves known as motor nerves. These motor nerves form part of the somatic nervous system, which is involved in the control of voluntary movements within the body. When over-exercising individual muscles, the contractile power within the muscle fibres is eventually depleted until a state of fatigue develops. This loss of power may be caused by a breakdown at different stages of the muscle-reflex pathway. In other words, there could be a failure in the transmission of somatic nerve impulses to the muscle, or there could be a collapse in the actual contractile mechanism inside the muscle.
Causes other than CFS/ME
Fatigue is often regarded by practitioners as being psychogenic (all in the mind) in origin. It may, of course, result from severe physical and/or mental activity, or lack of sleep. The degree of the fatigue will vary according to the personality and stamina of the individual.
Experiments have shown that if a movement of the hand is continued for long enough to initiate a state of fatigue, and if at this stage the blood flow into the hand is stopped by inflating a cuff around the upper arm, although the somatic motor nerves are still functioning, there is no recovery of power until the cuff is released and normal circulation is restored.1 As mentioned in chapter 3, the blood flow to muscles is under the influence of the sympathetic nervous system. Thus, if the sympathetic nerves are not functioning correctly, blood flow to certain muscles could be reduced. One could then reasonably assume that these muscles would be likely to suffer from some form of fatigue.
My work indicates that in CFS/ME normal activity within the sympathetic nervous system breaks down. The effect may be systemic, causing widespread aches and pains in the entire body, or the fatigue may be limited to one or two muscle groups.
As other disorders can cause fatigue symptoms, CFS/ME is generally judged to be the cause of fatigue only when these other diseases have been ruled out, and all other possible explanations have been explored. Although CFS/ME is a possibility in all cases of fatigue, it is good practice always to ensure that no other serious condition is at the root of the problem.
Anaemia
Lack of oxygen to the tissues of the body leads to fatigue. This happens if there is a reduction in the oxygen-carrying red blood cells, or the function of these cells becomes impaired, as in some cases of anaemia, a major symptom being that of lethargy and weakness. A common cause of anaemia is iron deficiency, since iron is the main constituent of the oxygen-transporting element (haemoglobin) within red blood cells. A simple blood test to determine the level of iron, or a red blood cell count will eliminate anaemia from the doctor’s investigation.
Heart conditions
Heart problems may lead to impaired blood flow to the rest of the body, which, subsequently, will lead to a reduced supply of nutrients and oxygen. This in turn will cause feelings of fatigue. Since pains in the chest and arms, as well as increased heart rate, are common signs and symptoms of heart disorders, the sufferer will often interpret these signs as an impending heart attack. However, these symptoms are very common in CFS/ME. After listening to the patient’s heart and running other tests, such as an electrocardiogram (ECG), the doctor should be in a position to discount heart disease as the cause of the problem. I have seen some CFS/ME patients in a serious state of anxiety over their chest pains and palpitations as in the case of Mr C (see Chapter 3). Practitioners should be aware of the distress these symptoms cause and ensure the patient is satisfied that a cardiac arrest is not imminent.
Lung disorders
Oxygen depletion occurs if the lungs are not functioning correctly. This will result in fatigue within the muscles and since CFS/ME can leave a person feeling breathless, lung function, as well as heart rhythms, should be thoroughly investigated.
Bowel and kidney disorders
These should be eliminated from the investigation, as the resultant metabolic changes that can occur may lead to fatigue.
Glandular fever
One specific disease that is frequently mistaken for CFS/ME, and vice versa, is infectious mononucleosis (better known as glandular fever), due to infection by the Epstein-Barr virus. An analysis of the blood will reveal a large increase in mononuclear, agranular white cells. A specific blood test, known as the Paul Bunnell test, will confirm if the signs and symptoms are caused by glandular fever. The test is readily available at your family doctor’s.
Addison’s disease
This disorder, which can cause fatigue, plagued American president John F. Kennedy (1917–1963), for much of his life. Addison’s disease is due to a disturbance in the normal function of the adrenal glands, situated next to the kidneys. The dysfunction leads to a deficiency of the hormones produced by the adrenals. The condition is improved by hormone replacement therapy and, often, steroids.
Patients with Addison’s disease usually present with muscle wasting and a darkened pigmentation of the skin. Their blood pressure is often lowered and sufferers may lose their appetite and experience nausea and vomiting. Although there are some similarities between this disease and CFS/ME, the skin discoloration, a drop in the serum levels of the adreno-cortical hormones and a fall in blood pressure are all signs of Addison’s that are easily detectable by clinical tests.
Myasthenia gravis
Nerves transmit their impulses by means of chemicals known as neurotransmitter substances. When a motor nerve, which controls muscles, enters the muscle fibre, it releases the transmitter substance, acetylcholine, which stimulates the fibre to contract. In the rare disease myasthenia gravis, which affects mostly young women, there is a disturbance in the production of acetylcholine, which results in a marked weakness in the muscles. The patient feels this frailty especially at the end of the day. The muscles in the head are often affected first, causing difficulty in swallowing and chewing. The eyelids become very heavy and even holding up the head can become arduous. The muscular weakness in myasthenia gravis can be quickly relieved by the administration of certain medications, such as endrophonium chloride. The rapid improvement is the key to establishing the diagnosis. As discussed in Chapter 5, during the early stages of CFS/ME there is often an overproduction of acetylcholine in the brain leading to too much choline.2
Gilbert’s syndrome
This benign hereditary disorder, another cause of fatigue, is associated with an excess amount of bile pigment in the blood, known as bilirubin. Gilbert’s syndrome is characterised by mild, intermittent jaundice, occasional bowel disturbances and often by weakness and fatigue. A simple blood test will confirm whether or not the patient’s fatigue is caused by this disorder.
Infection
Chronic infections, such as toxoplasmosis, an infection caused by a microscopic parasite that can live inside the cells of humans and animals, especially cats and farm animals, should be eliminated in the diagnostic process. Diagnosis of toxoplasmosis is usually conducted through blood tests.
Lyme disease is an infection that originates from a tick bite. The disease has a variety of symptoms, including changes affecting the skin, heart, joints and nervous system. It is also known as borrelia or borreliosis. A diagnosis of Lyme disease is more likely if the patient can remember a tick bite and has the characteristic erythema migrans rash.
To make a diagnosis the doctor may take a blood sample to determine whether or not the patient has developed an antibody towards Lyme disease. However, a live blood analysis, preferred by some physicians, is more accurate.
Early stages of HIV infection may resemble symptoms of CFS/ME and should be ruled out by a blood test.
Hormonal disorders
In CFS/ME it is very common for hormonal levels to be slightly higher or lower than normal and this is due, primarily, to the hypothalamus not functioning correctly. Many other primary hormonal disorders, such as hypothyroidism, thyrotoxicosis, diabetes mellitus and hyperparathyroidism, may cause symptoms common to CFS/ME. These disorders can be verified by means of blood tests.
Thyroid function tests should be carried out to monitor the production of thyroxine (T4) and triiodothyronine (T3) in the thyroid gland. Thyroid-releasing hormone (TRH) is secreted by the hypothalamus and stimulates the production of thyroid-stimulating hormone (TSH) from the anterior pituitary gland. TSH in turn stimulates the production and release of T4 and T3 from the thyroid. Blood tests for TSH, T3 and T4 should be done in order to verify that the thyroid is functioning correctly.
Neuromuscular disorders
Neuromuscular diseases such as multiple sclerosis (MS), a disorder that affects the central nervous system, should be eliminated as a possible cause of fatigue. MS, also known as disseminated sclerosis, is a chronic, inflammatory disease that can cause a variety of symptoms, including changes in sensation, visual problems, muscle weakness, depression, difficulties with coordination and speech, severe fatigue and pain. A fatty layer, known as the myelin sheath, surrounds and protects some nerves: this layer helps the nerves carry electrical signals. In MS the myelin is gradually destroyed, in patches, throughout the brain and spinal cord, causing a variety of symptoms, depending upon which signals are interrupted. MS can usually be detected by MRI scans and analysis of cerebrospinal fluid taken by means of a lumbar puncture. A number of other neuromuscular disorders can also cause fatigue.
Tumours
Malignant disease such as undiagnosed lymphomas and other tumours should be ruled out by investigations such as blood tests and, when necessary, scans such as MRI.
Auto-immune diseases
Diseases of the immune system, such as rheumatoid arthritis and systemic lupus erythematosus (SLE), are important to consider when diagnosing CFS/ME. SLE is a chronic, autoimmune disease of the joints, skin, kidney, brain, heart, lungs and gastrointestinal tract. It occurs mostly in women of childbearing age. While SLE patients usually have joint swelling and pain, CFS/ME patients may suffer painful joints but they do not usually experience swelling. A characteristic redness on the cheeks and nose of patients, the so-called ‘butterfly rash’, hair loss and a history of multiple miscarriages are all symptoms of SLE; however, some CFS/ME cases have similar symptoms. Blood tests can identify the antibodies produced in autoimmune diseases.
More than one disease
This chapter demonstrates just a few of the many other origins of fatigue and shows that only by comprehensive tests can other possibilities be eliminated from the investigation. However, even if tests show other reasons for the symptoms, it does not necessarily exclude the diagnosis of CFS/ME. It continues to worry me how many CFS/ME patients are diagnosed primarily by the exclusion of other better understood diseases. It is perfectly possible, and common, for people to suffer more than one disease or disorder at one time.
In my years of research and treating hundreds of sufferers since the early 1990s, I have observed physical signs, time and again, that are common to all CFS/ME patients. These signs, which are discussed in detail later in the book, can be detected by any trained practitioner and provide a much needed aid in diagnosis.
The case of Miss L
Age: 12 years
Occupation: school student
This case illustrates the diagnostic confusion that surrounds CFS/ME. Miss L had been severely disabled with an unknown disorder for the previous eighteen months. She had been wheelchair-bound for some of the time and unable to attend her regular school for more than a few hours a week. She had mostly spent the day at home, cared for by her devoted single mother, who had two other young daughters to look after. She had been taken to a local health authority school for a few hours each week; even that had often been too taxing for her ailing body.
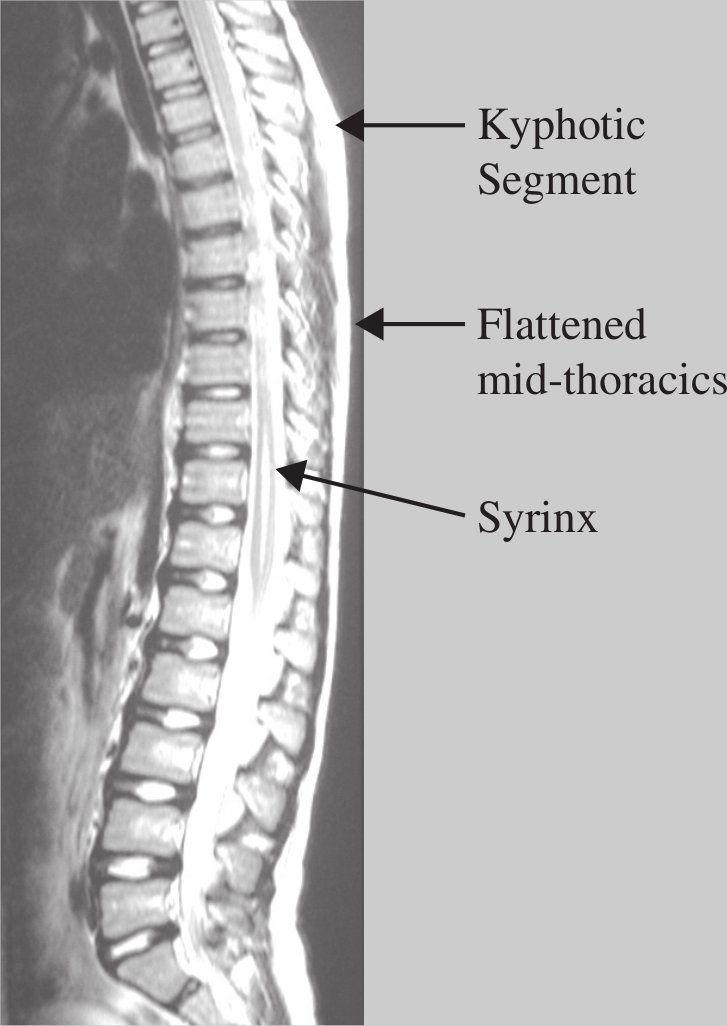
Figure 7. MRI sagittal image showing spinal defect in 12 year old girl with CFS/ME.
The postural disturbance of the thoracic spine in most cases of CFS/ME is usually not too severe, often with evidence of old osteochondrosis with a flattened upper thoracic region. A syrinx (cyst within the spinal canal) seen in this MR image is rare but demonstrates the extent of possible spinal dysfunction.
Miss L was born with a syrinx in the middle of her spine (see Fig. 7). A syrinx is a cyst that forms within the spinal cord and usually leads to a condition known as syringiomyelia. This neurological condition leads to a loss of pain sensation and reduction of normal sensory function on one side of the body, in other words, a different set of symptoms to CFS/ME. Miss L also had a defect at the top of her neck. A small section of her brain was slightly protruding down into the spinal canal (see Fig. 8). When this latter condition is severe, it is known as a Chiari malformation and is responsible for many symptoms common to CFS/ME as it affects normal spinal cord function. Chiari malformation often presents in a patient who also has a syrinx.
Cases of Chiari malformation and cervical stenosis, in which the spinal canal has narrowed and the health and function of the spinal cord are compromised, have been observed in CFS/ME patients.3
Miss L had two conditions that could have caused major neurological problems, but her symptoms, which included severe fatigue, headache, lack of concentration, sleep disturbance, irritable bowel and irritable bladder, sore throat and pains in her neck, back, chest and extremities, were diagnosed at her local hospital as mostly psychological. The syrinx, in their opinion, had nothing to do with the symptoms and the upper spine problem was not severe enough to be classified as a Chiari malformation and was considered to be unrelated to her condition. CFS/ME was never mentioned and when her mother brought her in to see me, I found it difficult to believe that the only treatment Miss L was receiving was regular sessions with the hospital psychologist. Miss L’s paediatric neurologist dismissed the idea that she had CFS/ME. However, as her treatment slowly progressed and her symptoms started to improve, Miss L’s doctors began to take notice. I explained to them how the girl’s spine was extremely flattened in the upper part of her back. Her breastbone was slightly malformed, showing a slight concavity, which would have affected her respiratory mechanics. She had lymphatic swelling in her chest and neck as well as the tender areas familiar to all the CFS/ME patients that I had seen (see Chapter 8). Although Miss L’s doctors continued to be sceptical, they could see the encouraging results my treatment and they then included me in Miss L’s case-management meetings at the hospital.

Figure 8. Upper cervical defect in the same 12 year old girl.
A defect at the uppermost region of the cervical spine is found in many cases of CFS/ME. The sagittal MR scan shows a partial herniation of the cerebellar tonsil into the spinal canal. (If the herniation penetrates further into the cervical region it is known as a Chiari Malformation).
Miss L eventually restarted mainstream school and at the time of writing no longer needs the wheelchair. She is at present a very active 15 year old with a full life. Even though she had other health issues, the main cause of her symptoms was restricted lymphatic drainage aggravated by her syrinx and upper neck malformation. This was evident in the response to my treatment. The hospital neurologist has discharged her and she now comes to me for check-ups every couple of months.
Notes
1. Merton PA, Marsden CD, Morton HB. Is the Human Stretch Reflex Cortical Rather Than Spinal? Lancet 1973; 1 (7806): 759–761.
2. Puri BK, Counsell SJ, Zaman R, Main J, Collins AG, Hajnal JV, Davey NJ. Relative increase in choline in the occipital cortex in chronic fatigue syndrome. Acta Psychiatr Scand 2002; 106: 224–226.
3. Hoh D. Spine, and Skull surgery may help many with CFIDS, FMS: Chiari-malformation or cervical stenosis may be common in CFIDS & Fibromyalgia. The CFIDS Chronicle 1999; May/June, 10–12.