All truth passes through three stages. First, it is ridiculed. Second, it is violently opposed. Third, it is accepted as being self-evident.
Arthur Schopenhauer (1788–1860)
To treat CFS/ME successfully one has to understand the exact nature of the disease and what is going wrong with the body. Once one comprehends the stages (see Table 1 on page 77) that lead to CFS/ME, one can start to correct the disturbances, otherwise the treatment will remain only palliative rather than curative.
Three predominant concepts surfaced from the clinical trials on CFS/ME patients carried out during my eleven years of research at the universities of Salford and Manchester.
The clinical trials 1994–2005
I embarked on my clinical research in 1989 following the success of my work with the cyclist, Mr E, mentioned at the start of Chapter 1. My first paper was published in the British Osteopathic Journal in 1993.1 The husband of one of my patients was a professor at the University of Salford, a large university in the Greater Manchester region with a major health sciences faculty. He showed my paper to his good friend, Professor Jack Edwards, a world-renowned bio-engineer. Professor Edwards invited me to lunch with psychology Reader, Dr Pat Hartley. Over the next three years we conducted the first clinical trial, which eventually led to the paper: ‘An evaluation of the effectiveness of osteopathic treatment on symptoms associated with Myalgic Encephalomyelitis. A preliminary report’, published in the Journal of Medical Engineering and Technology in 1998.2
Hardly any research into CFS/ME was being funded by grant bodies in the 1990s, and most of the research trusts that were offering funding stipulated that it had to be paid into another charitable trust. Consequently, the Fund for Osteopathic Research into ME (FORME) was born on 23 February 1995 at The Midland Hotel, Manchester. The FORME trust was set up together with a group of my patients and friends to help raise research funds and awareness of the physical nature of CFS/ME. Thanks to donations from grateful patients, and from interested members of the public, together with donations from other trusts, we raised around £250,000 to fund the entire project.
Once you have the funding and the volunteers for a clinical trial, you need official approval from the local health authority research ethics committee. This is even more rigorous than a congressional hearing, with a group of health authority administrators, doctors, scientists and legal representatives. We encountered many complex obstacles, but eventually, by changing the protocol a number of times and by satisfying every question, we were able to start the research projects. Research ethics committees are without doubt necessary (established following the horrors of the experiments conducted by the Nazis during World War II), but one wonders how many research projects, which could improve our knowledge and treatment of disease, do not go ahead due to the exhaustive and detailed process of obtaining the necessary approval.
The efficacy of my manual approach was tested using two separate clinical trials, both with groups matched for gender and age. In the first trial we recruited 40 CFS/ME patients who were to be treated using my technique and 40 CFS/ME patients who were given the treatment of their choice. The second trial was a smaller study using three groups of nine subjects each. The first group consisted of CFS/ME patients who received the Perrin technique. The second group was made up of CFS/ME patients who did not receive my treatment, with the third comprised of nine healthy volunteers. This research was carried out at the universities of Salford and Manchester between 1994 and 2005 under the guidance of bioengineer Professsor Jim Richards, neurobiologist Dr Vic Pentreath and neuro-radiologist Professor Alan Jackson:
- The first study examined the change in symptoms following a year of treatment.
- The second study repeated the first study and examined the possible mechanisms of any improvement.
The studies were designed to develop a greater understanding of the cause, diagnosis and treatment of CFS/ME, around which much scientific uncertainty exists. Phase 1 of the research trials examined overall symptom change. It included the patient completing a selection of self-report questionnaires which were answered periodically over the course of the year-long treatment. These eight questionnaires related to feelings of depression, anxiety, cognitive function, sleep and overall health. With post-exercise fatigue being a major symptom of CFS/ME, we tested the effects of the treatment by the amount of power the quadriceps muscle in the thigh lost after a specific isometrc exercise in which the subject pushed their right shin against a pressure pad with no actual movement of the leg. The pad was connected to a gauge that measured force.
The second trial, which included the same self-reporting questionnaires assessing symptom change as the initial trial, was divided into two parallel phases, phases 2 and 3. Phase 2 primarily took the form of brain analysis using magnetic resonance imaging (MRI) to confirm if brain abnormalities seen in previous research3,4,5 were found in sufferers of CFS/ME. Central lymph scans were also carried out to see if there was any possible enlargement in the thoracic duct of CFS/ME sufferers. In phase 3, isometric tests were carried out as in phase 1 but with much more accurate computerised equipment.6
The precise objectives of this research were:
- To determine whether or not spinal problems were related to the signs and symptoms arising from CFS/ME.
- To test if my method of osteopathic treatment reduced symptoms associated with CFS/ME compared with those of a matched control group, who received no such treatment.
- To reveal the sustainability of any improvement by a one-year follow-up study and to investigate the likely replication of the initial study, thus strengthening the argument of a relationship between set osteopathic procedures and the improvement in signs and symptoms associated with CFS/ME.
- To determine if there is a visible disease process in the brain that may be causing the symptoms of CFS/ME.
- To determine if there is any intrinsic muscle disorder that may be causing the symptoms of fatigue in CFS/ME.
Conclusions of the research
I. The first stage of the research showed that the major signs and symptoms associated with CFS/ME showed an average of 40 per cent improvement in the treated group compared with an average worsening of 1 per cent in the untreated group. Muscle fatigue was shown to be significantly reduced in the treated group compared with little change in the untreated patients.
II. In the second stage of the trials it was concluded that muscle fatigue is of a functional nature rather than resulting from any known muscle disease. Secondly, following scanning the brain with magnetic resonance imaging (MRI) to examine the white matter, blood flow and cerebrospinal fluid flow, we discovered that in the CFS/ME patients there was no detectable pathological structural abnormality in the brain. (This contradicts other studies that have shown brain anomalies.3,4,5 This conundrum may be explained by there being severe cases of CFS/ME in which the brain structure is damaged. However, our research showed that even though a person may have CFS/ME, it does not mean, necessarily, that any damage will be visible on scans. The fact that no major physical abnormality was seen in any of our CFS/ME patients suggests that visible structural trauma of the brain using standard MRI scanning methods itself is uncommon rather than the norm.)
III. Thirdly, when examining the effects of the treatment programme in both clinical trials, it seems likely that the improvement in the muscular fatigue together with the overall reduction in all CFS/ME symptoms was a result of increasing toxic drainage from the central nervous system.
The downward spiral
With careful consideration of the clinical findings, I have formulated a theoretical model to explain the cause, signs and symptoms of CFS/ME and the effectiveness of my treatment regime. My belief is the osteopathic approach does not set out directly to eliminate poisons from the body; rather, it facilitates the patient’s own inbuilt mechanisms responsible for toxin elimination. By reducing the intensity of incoming sympathetic impulses, by means of relaxing the muscles and improving circulation and drainage, the signs and symptoms of CFS/ME are diminished.
My theoretical model of the stages of development of CFS/ME (see Table 1, page 77) may be applied to all the CFS/ME patients I have seen since the late 1980s.
Table 1 The stages of development of CFS/ME
| Stage 1 | Patients with CFS/ME all seem to have a predisposing history of sympathetic nervous system overload: |
| a. Physically – by being an overachiever at work, during study, or in sports. Rarely, it may be the opposite by being too sedentary. |
|
| b. Chemically – by constant exposure to environmental pollution. | |
| c. Immunologically – by chronic infections or hypersensitivities to multiple allergens. | |
| d. Psychologically/emotionally – by family and/or work related mental stress. | |
| Stage 2 | In Stage 2 either Stage 2a or Stage 2b can occur before the other or they can occur concurrently, depending on the causes of the restricted flow of lymphatic drainage in the head and spine. |
| Stage 2a | Lymphatic drainage of the central nervous system shows signs of being impaired, mostly in the cribriform plate region of the ethmoid bone above the nasal passages. |
| Stage 2b | Lymphatic drainage of the central nervous system is subject to disturbance in the spine, usually in the cervical or thoracic region, due to either a congenital, hereditary, or postural defect and/or prior trauma. |
| Stage 3 | Toxic effects due to the long-term dysfunction of the central nervous system drainage will compound the chronic hyperactivity of the sympathetic nervous system; this further overloads the hypothalamus and subsequently, the sympathetic nervous system. |
| Stage 4 | A final trigger factor strikes, which usually arises from a viral infection, but may be physical or emotional in nature. |
| Stage 5 | There will be a disturbance in autonomic, as well as hormonal, function, because toxins in the cerebral blood flow and ventricular system directly affect control of the hypothalamus. Hormonal transport within the cerebrospinal fluid may be directly affected by toxic overload. |
| Stage 6 | Dysfunction of sympathetic control of the thoracic duct leads to a reflux of toxins in the resultant retrograde lymph flow, causing varicose lymphatic vessels predominantly in the abdomen, neck and chest. This further reduces flow of cerebrospinal fluid into the lymphatics. |
| Stage 7 | Further impairment of toxic drainage of the central nervous system, due to the retrograde lymphatics, results in increased hypothalamic dysfunction and an even greater reduction of lymphatic drainage. |
| Stage 8 | The continuing irritation of the sympathetic nervous system results in further systemic disturbances, leading to a chronic adaptive state known as CFS/ME. |
The physical signs of CFS/ME
The concept of CFS/ME being primarily a physical rather than psychological disorder is foreign to most of the medical profession. However, many doctors recognise that CFS/ME causes physical signs and symptoms.7–10 There are physical components within the internationally recognised criteria that verify the diagnosis of CFS/ME.8 These include sore throat, tender lymph nodes in the neck and armpits, and muscle and joint pain. In the twenty years since I started to examine and treat patients with CFS/ME, repeated patterns of physical signs have emerged among all the sufferers that cannot be dismissed as pure coincidence. All physical phenomena seen in CFS/ME can be understood when the disease is viewed as the consequence of impaired drainage of the central nervous system, resulting in dysfunction of the sympathetic nervous system. The main physical signs are shown below.
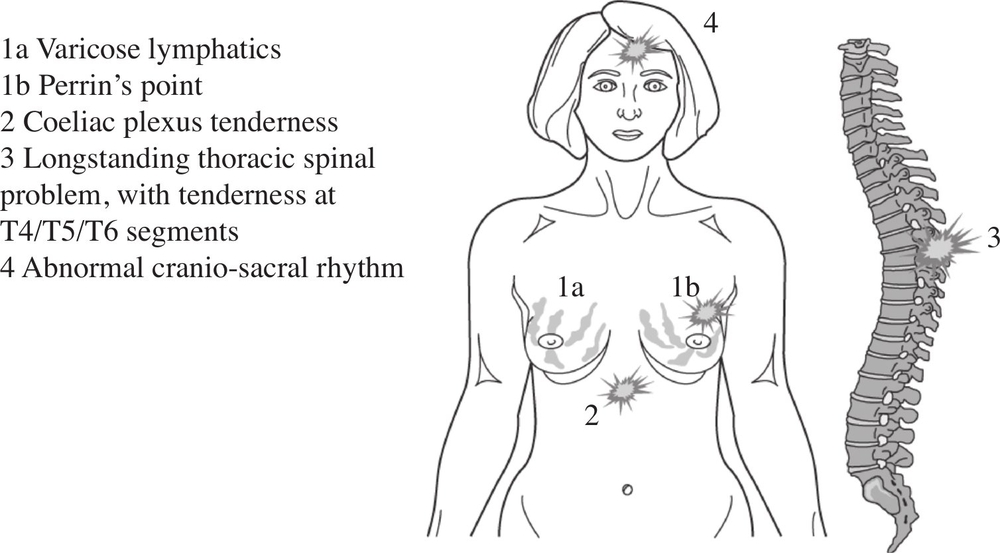
Figure 9. The observed physical signs of CFS/ME.
These regions of tenderness or dysfunction have been identified in all CFS/ME sufferers seen by the author since 1989 in both the university and clinical settings.
Varicose lymphatics and Perrin’s Point
In every CFS/ME patient, whether male or female, there was a very tender area in the upper lateral region of the breast tissue, roughly 2 cm superior and lateral to the left nipple (Figs 9 and 10). This is the area where the pectoral muscles and lymphatic tissue overlap. This finding is significant because the tender area almost always lies on the left side and is level with the position at which the thoracic duct turns to the left. The heart and the main blood vessels are supplied with sympathetic nerves via a bundle of nerves called the cardiac plexus, which has a greater concentration of nerves on the left than the right. Sympathetic nerves run alongside the larger nerves that control movement and sensation in the body (the somatic nerves). There are often impulses crossing over from sympathetic nerves to somatic and vice versa.11 When the cardiac rhythm is affected in CFS/ME the sympathetic nerves send messages to the sensory nerves on the left side of the chest. The thoracic duct travels from the right side to the left side of body above the level of the nipple and so, sympathetic nerves controlling the thoracic duct’s pumping action are more left-sided. Thus, when these nerves are irritated, they also disturb the adjacent sensory nerves. The resultant pain is at the confluence of these two sets of sensory nerves: I refer to this tender spot as Perrin’s Point.

Figure 10. Examining the patient for ‘Perrin’s point’.
Gentle pressure at a point slightly superior and lateral to the left nipple “Perrin’s Point”(X). The amount of sensitivity at this point appears to correspond to the severity of lymphatic engorgement in the breast tissue and also seems to mirror the gravity of the other symptoms.
The sensitive region, Perrin’s Point, together with congested lymph vessels in the cervical region and breast tissue, was palpated (felt) in the 40 patients chosen for my treatment in the first trial and all of the 18 CFS/ME patients in the second phase of the study. The consistency of these lymphatics can best be described as ‘beady’ and similar to varicose veins in the leg. Varicosities (see opposite) have been described in the lymphatic system.12,13,14 Large incompetent varicose lymphatics, known as megalymphatics, have often been seen when there is a back-flow of fluid within the lymphatic vessels, due to a disturbance of the normal pumping mechanism. However, varicosities in the lymphatics are rarely discussed in clinics, due to the misconception that lymph flow can only be unidirectional due to the valvular system in the lymphatic vessels. Sluggish lymph flow is known to exist in many disease states15 and is treated by many practitioners world-wide trained in manual lymphatic drainage. However, the concept of a reverse pump causing an actual back-flow is not generally recognised clinically. Thus the possibility of a varicose lymph vessel is rarely considered when a GP or hospital consultant conducts an examination.
Downward pressure due to thoracic duct pump dysfunction caused by sympathetic disequilibrium may lead to a contra-flow within the lymphatics,16damaging the valves and creating a pooling of lymphatic fluid with ‘beading’ of the vessels. Stasis (fluid not moving) in these varicose lymphatic vessels creates risk of toxic overload together with additional damage to the lymphatics and surrounding tissue. Reflux of toxins via lymphatic vessels back into the cerebrospinal fluid will further irritate the central nervous system. Increased toxicity within the central nervous system continues to overload the sympathetic nerves, resulting in a downward spiral of deteriorating health.
From the earliest days of osteopathy, the importance of good lymphatic drainage in the thoracic duct has been seen as paramount to sustain health.17–20 It was emphasised that, together with good blood supply, it was equally important to have perfect drainage. This is the pathway I believe to be compromised mechanically as part of the root of CFS/ME. Mechanical dysfunction such as this can be detected by palpation and can be released by gentle pressure and massage techniques applied to the cranium and the spine and surrounding soft tissue.
The healthy lymphatic vessel allows only unidirectional flow due to the valvular system as illustrated in Fig. 11. In CFS/ME, retrograde flow of the lymphatics is produced by the reverse peristaltic wave of the thoracic duct that arises from dysfunctional sympathetic control of the duct’s smooth muscle wall (see Fig. 12). Eventually, the lymphatic reflux causes damage to the valves and allows pooling of fluid in between the valves. This leads to distension of the vessel wall with the characteristic beaded appearance of a varicose vessel as illustrated in Fig. 13.
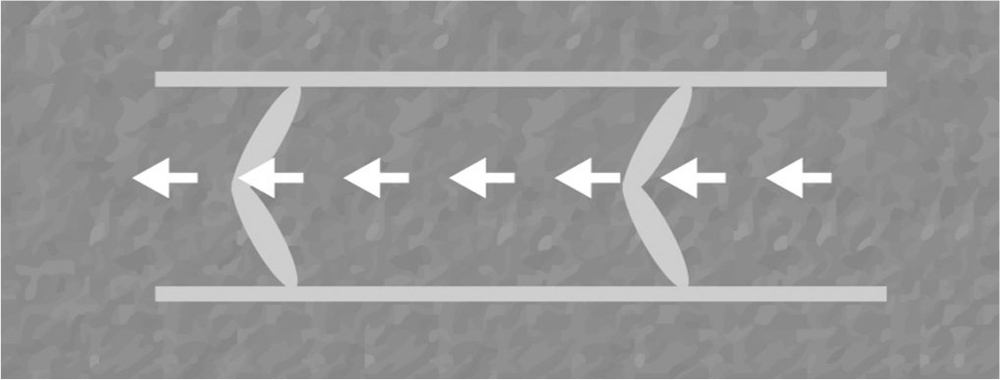
Figure 11. Schematic illustration showing normal flow within a healthy lymphatic vessel.
The valves in this healthy vessel are intact preventing any backflow, thus maintaining a
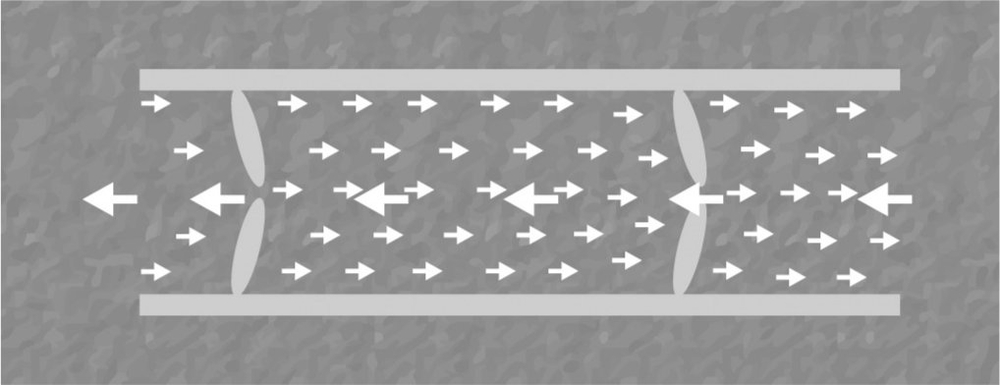
Figure 12. Schematic illustration showing retrograde lymphatic flow.
If the normal peristaltic wave of the thoracic duct is disturbed resulting in reflux, then the ensuing back-pressure will weaken the valves allowing a retrograde flow.
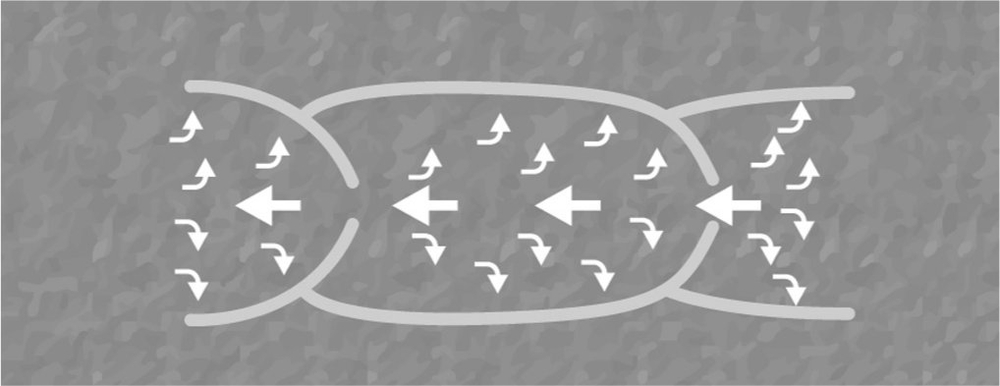
Figure 13. Schematic illustration showing the formation of lymphatic varicosities.
The walls between the collapsed valves become noticeably distended with further reflux of lymphatic fluid.
Fig. 14 shows the top right section of the chest of a 61 year old man. One can see the swollen, tortuous beaded vessels just beneath the collar bone adjacent to the right shoulder. The man suffered severely from CFS/ME for four years before being successfully treated with a two-year course of osteopathy. The beaded appearance in Fig. 14 is due to damaged valves and subsequent retrograde flow and pooling of lymphatic fluid. This is similar to the formation of varicose veins, although it lacks the darker, bluish hue of superficial varicose veins. The creamy appearance of lymph is almost apparent in these engorged vessels, which have a much larger diameter than in normal healthy superficial lymphatic vessels. It is extremely rare to see such pronounced superficial varicose megalymphatics as illustrated here. However, I have been able to feel the presence of varicose lymphatic vessels in the neck and chest of all the CFS/ME patients I have seen since 1989.
Tenderness at solar plexus
The largest major autonomic plexus, uniting two large coeliac ganglia, is known as the coeliac plexus, more commonly referred to as the solar plexus. This major confluence of nerves is level with the 12th thoracic/1st lumbar segment and is situated posterior to the stomach and in front of tendonous insertions of the diaphragm. Secondary plexuses connected to the coeliac plexus are: phrenic; splenic; hepatic; left gastric; intermesenteric; suprarenal; renal; testicular/ovarian; superior and inferior mesenteric, sending and receiving messages from all the abdominal organs and below.

Figure 14. Right subclavicular varicose lymphatics in patient with CFS/ME.
Four years after completing a 2 year treatment programme, one can clearly see five separate varicose lymphatic vessels under the skin at the anterior medial aspect of the right shoulder, the central one being the most pronounced.
Through its connections, the solar plexus is excellent as an indicator for any visceral disturbances from the waist down. Tenderness in this abdominal region, known as the epigastrium, seems to be directly related to the severity of any lower extremity fatigue and/or abdominal problem. This is due to impulses passing across the connections between adjacent sensory and sympathetic nerves.
Postural/structural dysfunction of the thoracic spine
A prevailing observation in the clinical findings of CFS/ME is a mechanical disorder of the thoracic spine, which may be due to bad occupational posture, or related to a congenital event or genetic predisposition. All of the patients in the studies that I undertook had a particular dysfunction in the thoracic region, whether it was inflammation, abnormal curvature, or just a restricted area.
A common structural disturbance seen by myself in CFS/ME patients was a flattening of the curvature in the mid-thoracic spine, usually accompanied by the presence of a kyphotic dorso-lumbar area (an abnormally exaggerated convex curvature in the lower back). An example of this defect is shown in Fig. 15a which can be compared with the healthy posture shown in Fig. 15b. This postural defect is often caused by a prior condition, osteochondrosis, also known as Scheurmann’s disease, which affects spinal development in adolescence and which may have occurred years before the onset of the characteristic symptoms of CFS/ME.
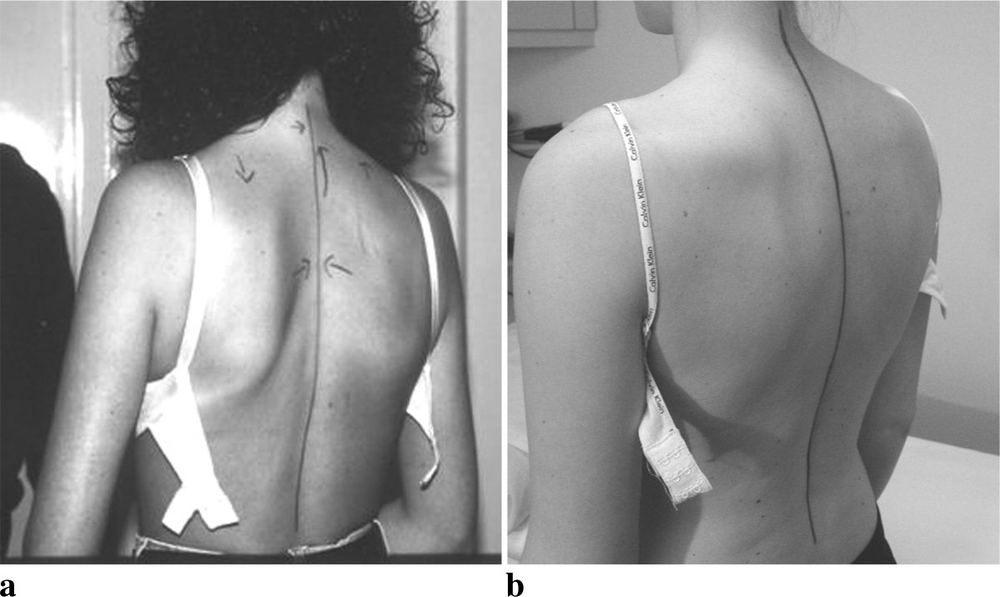
Figure 15. Comparative photographs showing a flattened mid-thoracic spine.
Photo a on the left shows the familiar flattening of the mid thoracic spine seen in many CFS/ME patients. This differs from a normal spinal posture in the healthy subject on the right, b.
Changes in cranio-sacral rhythm
There is a palpable rhythmic pulsation along the spinal cord and around the brain together with that of normal breathing, which is transmitted to the rest of the body and is termed the ‘involuntary mechanism’, ‘cranial rhythmic impulse’ (CRI), or the ‘cranio-sacral rhythm’. Most of the osteopathic profession believe the pulse to be a movement through the tension and continuity of membranes and fascia. The fascia consists of connective tissue that is continuous with the membranes that surround the brain and spinal cord, the meninges, thus allowing any motion within the nervous system to be transmitted throughout the body.
William Garner Sutherland (1873–1954), the founder of cranial osteopathy, proposed that there was a primary respiratory mechanism created within the central nervous system via the spinal cord; he believed that the bones in the cranium all moved in a rhythmic pattern together with the sacrum at the base of the spine.19
Sutherland proposed that the primary respiratory mechanism produces a rhythmic alternation of flexion and extension of structures in the midline. This movement occurs simultaneously with the rhythmic external and internal rotation of all paired lateral structures such as the kidneys.
It has been suggested that contractile lymph tissue exists throughout the body, which creates a powerful pumping mechanism.12 It has been shown that the thoracic duct pump influences the drainage of cerebrospinal fluid/lymph from the central nervous system. Together with the pulse rate and the effects of breathing, a separate underlying rhythm may be induced; this may be the aforementioned ‘involuntary mechanism’21. This rhythm echoes along the lymphatic system, resonating throughout the entire body and can be palpated by trained practitioners. In CFS/ME patients there is an abnormal rhythm which is often slow and weaker than in healthy subjects. I found this to be the case in all the CFS/ME patients that I examined clinically and during my research.
Conclusion
Recognition of the diagnostic signs that I have described (see Fig 9) can be taught, easily, to clinicians. There are plenty of practitioners trained in cranio-sacral techniques who can apply all the diagnostic procedures, described above, that may identify CFS/ME in its earliest stages. In fact, when examining siblings or children of CFS/ME patients, I have discovered that the physical signs often appear long before the symptoms present themselves fully. It is possible in such familial cases to diagnose a pre-CFS/ME condition and prevent individuals from succumbing to the full-blown illness. I believe that I am the only practitioner to claim that CFS/ME is preventable (see Chapter 11). One thing is certain: the earlier that a patient receives a definite diagnosis, and thus the correct treatment, the better are the chances of that person’s recovery.
The case of Mrs H
Age: 21 years
Occupation: Housewife
Marital status: Married for one year.
Mrs H’s symptoms began with abdominal pains and she had already been diagnosed with irritable bowel syndrome (IBS) when she first came to see me. This common disorder is thought to be due either to abnormal motility within the gut or a heightened sensitivity to distension of the intestine. In Mrs H’s case, the abdominal cramps were accompanied by aches in the limbs and dizziness, and she had felt lethargic for a few years. These symptoms are not usually associated with IBS, and she came to me feeling quite depressed.
When she first consulted me, she was a few weeks’ pregnant. She had informed me about a miscarriage which had occurred a few months earlier. The news of her pregnancy came just before I was to advise her of the need to use a contraceptive device until her symptoms had improved.
There are two viewpoints concerning pregnancy and CFS/ME. Some experts believe that pregnancy is a time when a better balance is achieved within the woman’s body and it can help reduce the symptoms of CFS/ME. However, this is unpredictable. Some healthy women blossom when pregnant: if the CFS/ME patient is lucky enough to be that type, her symptoms will probably reduce during pregnancy. However, if the mother-to be is one of those who generally have a difficult pregnancy, her CFS/ME symptoms may worsen for most of the nine months as her hormonal levels fluctuate, producing more nausea and fatigue.
The increase in weight and the changes in overall posture of the mother-to-be put much more mechanical strain on her back. From a mechanical point of view, some women may feel more mobility in the spine during pregnancy. This is due to the hormone relaxin, which is released from the ovaries throughout pregnancy. This hormone, as its name suggests, causes joints and ligaments to loosen. The relaxation of the joints prepares the body for the mechanical pressure put on the spine and pelvis during the later stages of pregnancy and, eventually, labour. The effects of the hormone lead to many pregnant women suffering from strained joints, for example, sprained ankles. However, the consequent increase in movement in the thoracic and upper spine may be beneficial in CFS/ME sufferers.
Mrs H’s upper dorsal spine was severely restricted. This stiffness probably dated back to an accident when she was only 15 years old, in which she had fallen badly and injured her head. Since then, she had suffered bouts of depression and had been prescribed antidepressants, which gave no relief. An antispasmodic pill was also prescribed for the abdominal cramps with no success.
With regular treatment throughout her pregnancy, I was able to maintain some mobility in her upper spine, and her general condition improved slightly. The most encouraging factor was that her symptoms did not worsen. In the latter months, with the help of relaxin, the mobility in her spine greatly increased and she noted how well she felt during the last few weeks of pregnancy.
I advised her to deliver the baby on her side. The left-lateral position is commonly used when patients have spinal problems. Lying on the back in the standard position of delivery puts enormous strain on the spine, and this would have caused a worsening of her symptoms after the birth.
She eventually gave birth to a healthy 8 lb (3.6 kg) baby girl. There were no complications during labour and a few weeks after the birth, when Mrs H came for a check-up, she was feeling much healthier and more energetic. She coped extremely well with her new baby and the aches and pains were no longer a problem.
Notes
1. Perrin RN. Chronic fatigue syndrome: a review from the biomechanical perspective. British Osteopathic Journal 1993; 11: 15–23.
2. Perrin RN, Edwards J, Hartley P. An evaluation of the effectiveness of osteopathic treatment on symptoms associated with Myalgic Encephalomyelitis. A preliminary report. Journal of Medical Engineering and Technology 1998; 22 (1): 1–13.
3. Keenan P. Brain MRI abnormalities exist in chronic fatigue syndrome (Editorial). Journal of Neurological Sciences 1999; 171: 1–2.
4. Lange G, Deluca J, Maldjian JA, Lee H, Tiersky LA, Natelson BH. Brain MRI abnormalities exist in a subset of patients with chronic fatigue syndrome. Journal of Neurological Sciences 1999; 171 (1): 3–7.
5. Costa DC, Brostoff J, Tannock C. 1995. Brainstem Spect Studies in Normals, ME/CFS and Depression. Nucl Med Commun 1995; 15: 252–253.
6. Farrell M, Richards JG. Analysis of the reliability and validity of the kinetic communicator exercise device. Med Sci Sports Exer 1986; 18 (1): 44–49.
7. Hutchinson A, Pinching L, Chambers T, Waterman J, Wayne N. (eds.). A Report of the CFS/ME Working Group to the Chief Medical Officer. HMG, 2002.
8. Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Annals of Internal Medicine 1994; 121 (12): 953–959.
9.Sharpe M, Archard L, Banatvala J. 1991. A report: chronic fatigue syndrome: guidelines for research. Journal of the Royal Society of Medicine 1991; 84:118–121.
10. Carruthers B. Definitions and aetiology of Myalgic Encephalomyelitis (ME): how the Canadian Consensus Clinical Definition of ME works. Journal of Clinical Pathology 2007; 60 (2): 117–119.
11. Gasser HS. Properties of dorsal root unmedullated fibres on the two sides of the ganglion. Journal of General Physiology 1955; 38: 709–728.
12. Kinmonth JB. The Lymphatics, 2nd edition. London: Edward Arnold; 1982; 80.
13. Kinmonth JB. Some aspects of cardiovascular surgery. Journal of the Royal College of Surgeons of Edinburgh 1960; 5: 287–297.
14. Kinmonth JB. Sharpey-Schafer. Manometry of Human Thoracic Duct. Journal of Physiology 1959; 177: 41.
15. Vodder E. Le drainage lymphatique, une nouvelle méthode thérapeutique. Paris, France: Santé Pour Tous; 1936.
16. Browse NL. Response of lymphatics to sympathetic nerve stimulation. Journal of Physiology 1968; 19: 25.
17. Still AT. Philosophy of Osteopathy. Published by the Author, Kirksville, Mo. 1899.
18. Still AT. The Philosophy and Mechanical Principles of Osteopathy Kansas City USA: Hudson-Kimberly; 1902: 47.
19. Sutherland WG. The Cranial Bowl Mankato, Minnesota: Free Press Company; 1939.
20. Wales AL. (ed). Sutherland WG. Teachings in the Science of Osteopathy. Sutherland Cranial Teaching Foundation, Fort Worth, Texas; 1990.
21. Perrin RN. Lymphatic drainage of the neuraxis and the CRI: a hypothetical model. Journal of the American Osteopathic Association. In press (accepted Jan 2007).