Food Allergy and Adverse Reactions to Foods
Anna Nowak-Węgrzyn, Hugh A. Sampson, Scott H. Sicherer
Adverse reactions to foods consist of any untoward reaction following the ingestion of a food or food additive and are classically divided into food intolerances (e.g., lactose intolerance ), which are adverse physiologic responses, and food allergies, which are adverse immunologic responses and can be IgE mediated or non–IgE mediated (Tables 176.1 and 176.2 ). As with other atopic disorders, food allergies appear to have increased over the past 3 decades, primarily in countries with a Western lifestyle. Worldwide, estimates of food allergy prevalence range from 1–10%; food allergies affect an estimated 3.5% of the U.S. population. Up to 6% of children experience food allergic reactions in the 1st 3 yr of life, including approximately 2.5% with cow's milk allergy, 2% with egg allergy, and 2–3% with peanut allergy. Peanut allergy prevalence tripled over the past decade. Most children “outgrow” milk and egg allergies, with approximately 50% doing so by school-age. In contrast, 80–90% of children with peanut, tree nut, or seafood allergy retain their allergy for life.
Genetics
Genetic factors play an important role in the development of food allergy. Family and twin studies show that family history confers a 2-10–fold increased risk, depending on the study setting, population, specific food, and diagnostic test. Candidate gene studies suggest that genetic variants in the HLA-DQ locus (HLA-DQB1*02 and DQB1*06:03P), filaggrin, interleukin-10, STAT6, and FOXP3 genes are associated with food allergy, although the results are inconsistent across different populations. In a genome-wide association study, differential methylation at the HLA-DR and -DQ regions was associated with food allergy. Epigenetic studies implicate DNA methylation effects on interleukins 4, 5, and 10 and interferon (IFN)-γ genes and in the mitogen-activated protein kinase (MAPK) pathway.
Pathogenesis
Food intolerances are the result of a variety of mechanisms, whereas food allergy is predominantly caused by IgE-mediated and cell-mediated immune mechanisms. In susceptible individuals exposed to certain allergens, food-specific IgE antibodies are formed that bind to Fcε receptors on mast cells, basophils, macrophages, and dendritic cells. When food allergens penetrate mucosal barriers and reach cell-bound IgE antibodies, mediators are released that induce vasodilation, smooth muscle contraction, and mucus secretion, which result in symptoms of immediate hypersensitivity (allergy). Activated mast cells and macrophages may release several cytokines that attract and activate other cells, such as eosinophils and lymphocytes, leading to prolonged inflammation. Symptoms elicited during acute IgE-mediated reactions can affect the skin (urticaria, angioedema, flushing), gastrointestinal (GI) tract (oral pruritus, angioedema, nausea, abdominal pain, vomiting, diarrhea), respiratory tract (nasal congestion, rhinorrhea, nasal pruritus, sneezing, laryngeal edema, dyspnea, wheezing), and cardiovascular system (dysrhythmias, hypotension, loss of consciousness). In non-IgE food allergies, lymphocytes, primarily food allergen–specific T cells, secrete excessive amounts of various cytokines that lead to a “delayed,” more chronic inflammatory process affecting the skin (pruritus, erythematous rash), GI tract (failure to thrive, early satiety, abdominal pain, vomiting, diarrhea), and respiratory tract (food-induced pulmonary hemosiderosis). Mixed IgE and cellular responses to food allergens can also lead to chronic disorders, such as atopic dermatitis, asthma, eosinophilic esophagitis, and gastroenteritis.
Children who develop IgE-mediated food allergies may be sensitized by food allergens penetrating the GI barrier, referred to as class 1 food allergens , or by food allergens that are partially homologous to plant pollens penetrating the respiratory tract, referred to as class 2 food allergens . Any food may serve as a class 1 food allergen, but egg, milk, peanuts, tree nuts, fish, soy, and wheat account for 90% of food allergies during childhood. Many of the major allergenic proteins of these foods have been characterized. There is variable but significant cross-reactivity with other proteins within an individual food group. Exposure and sensitization to these proteins often occur very early in life. Virtually all milk allergies develop by 12 mo of age and all egg allergies by 18 mo, and the median age of 1st peanut allergic reactions is 14 mo. Class 2 food allergens are typically vegetable, fruit, or nut proteins that are partially homologous with pollen proteins (Table 176.3 ). With the development of seasonal allergic rhinitis from birch, grass, or ragweed pollens, subsequent ingestion of certain uncooked fruits or vegetables provokes the oral allergy syndrome . Intermittent ingestion of allergenic foods may lead to acute symptoms such as urticaria or anaphylaxis, whereas prolonged exposure may lead to chronic disorders such as atopic dermatitis and asthma. Cell-mediated sensitivity typically develops to class 1 allergens.
Table 176.3
Natural History of Food Allergy and Cross-Reactivity Between Common Food Allergies
| FOOD | USUAL AGE AT ONSET OF ALLERGY | CROSS REACTIVITY | USUAL AGE AT RESOLUTION |
|---|---|---|---|
| Hen's egg white | 0-1 yr | Other avian eggs | 7 yr (75% of cases resolve)* |
| Cow's milk | 0-1 yr | Goat's milk, sheep's milk, buffalo milk | 5 yr (76% of cases resolve)* |
| Peanuts | 1-2 yr | Other legumes, peas, lentils; coreactivity with tree nuts | Persistent (20% of cases resolve) |
| Tree nuts | 1-2 yr; in adults, onset occurs after cross reactivity to birch pollen | Other tree nuts; co-reactivity with peanuts | Persistent (9% of cases resolve) |
| Fish | Late childhood and adulthood | Other fish (low cross-reactivity with tuna and swordfish) | Persistent † |
| Shellfish | Adulthood (in 60% of patients with this allergy) | Other shellfish | Persistent |
| Wheat* | 6-24 mo | Other grains containing gluten (rye, barley) | 5 yr (80% of cases resolve) |
| Soybeans* | 6-24 mo | Other legumes | 2 yr (67% of cases resolve) |
| Kiwi | Any age | Banana, avocado, latex | Unknown |
| Apples, carrots, and peaches § | Late childhood and adulthood | Birch pollen, other fruits, nuts | Unknown |
* Recent studies suggest that resolution may occur at a later age, especially in children with multiple food allergies and lifetime peak food-specific IgE >50 kUA /L.
† Fish allergy that is acquired in childhood can resolve.
§ Allergy to fresh apples, carrots, and peaches (oral allergy syndrome ) is typically caused by heat-labile proteins. Fresh fruit causes oral pruritus, but cooked fruit is tolerated. There is generally no risk of anaphylaxis, although in rare cases, allergies to cross-reactive lipid transfer protein can cause anaphylaxis after ingestion of fruits (e.g., peach) and vegetables.
Adapted from Lack G: Food allergy, N Engl J Med 359:1252–1260, 2008.
Clinical Manifestations
From a clinical and diagnostic standpoint, it is most useful to subdivide food hypersensitivity disorders according to the predominant target organ (Table 176.4 ) and immune mechanism (see Table 176.1 ).
Table 176.4
From Boyce JA, Assa'ad A, Burks AW, et al: Guideline for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel, J Allergy Clin Immunol 126(6):S1–S58, 2010 (Table IV, p S19).
Gastrointestinal Manifestations
GI food allergies are often the 1st form of allergy to affect infants and young children and typically manifest as irritability, vomiting or “spitting-up,” diarrhea, and poor weight gain. Cell-mediated hypersensitivities without IgE involvement predominate, making standard allergy tests such as skin-prick tests and in vitro tests for food-specific IgE antibodies of little diagnostic value.
Food protein–induced enterocolitis syndrome (FPIES) typically manifests in the 1st several mo of life as irritability, intermittent vomiting, and protracted diarrhea and may result in dehydration (Table 176.5 ). Vomiting generally occurs 1-4 hr after feeding, and continued exposure may result in abdominal distention, bloody diarrhea, anemia, and failure to thrive. Symptoms are most often provoked by cow's milk or soy protein–based formulas. A similar enterocolitis syndrome occurs in older infants and children from rice, oat, wheat, egg, peanut, nut, chicken, turkey, or fish. Hypotension occurs in approximately 15% of patients after allergen ingestion and may initially be thought to be caused by sepsis. FPIES usually resolves by age 3-5 yr.
Table 176.5
Food Protein–Induced Gastrointestinal Syndromes
| FPIES | PROCTOCOLITIS | ENTEROPATHY | EOSINOPHILIC GASTROENTEROPATHIES* | |
|---|---|---|---|---|
| Age at onset | 1 day–1 year | 1 day–6 months | Dependent of age of exposure to antigen, cow's milk and soy up to 2 yr | Infant to adolescent |
| Food proteins implicated | ||||
| Most common | Cow's milk, soy | Cow's milk, soy | Cow's milk, soy | Cow's milk, soy, egg white, wheat, peanut |
| Less common | Rice, chicken, turkey, fish, pea | Egg, corn, chocolate | Wheat, egg | Meats, corn, rice, fruits, vegetables, fish |
| Multiple food hypersensitivities | >50% both cow's milk and soy | 40% both cow's milk and soy | Rare | Common |
| Feeding at the time of onset | Formula | >50% exclusive breastfeeding | Formula | Formula |
| Atopic background | ||||
| Family history of atopy | 40–70% | 25% | Unknown | ~50% (often history of eosinophilic esophagitis) |
| Personal history of atopy | 30% | 22% | 22% | ~50% |
| Symptoms | ||||
| Emesis | Prominent | No | Intermittent | Intermittent |
| Diarrhea | Severe | No | Moderate | Moderate |
| Bloody stools | Severe | Moderate | Rare | Moderate |
| Edema | Acute, severe | No | Moderate | Moderate |
| Shock | 15% | No | No | No |
| Failure to thrive | Moderate | No | Moderate | Moderate |
| Laboratory findings | ||||
| Anemia | Moderate | Mild | Moderate | Mild-moderate |
| Hypoalbuminemia | Acute | Rare | Moderate | Mild-severe |
| Methemoglobinemia | May be present | No | No | No |
| Allergy evaluation | ||||
| Food skin-prick test | Negative † | Negative | Negative | Positive in ~50% |
| Serum food allergen IgE | Negative † | Negative | Negative | Positive in ~50% |
| Total IgE | Normal | Negative | Normal | Normal to elevated |
| Peripheral blood eosinophilia | No | Occasional | No | Present in <50% |
| Biopsy findings | ||||
| Colitis | Prominent | Focal | No | May be present |
| Lymph nodular hyperplasia | No | Common | No | Yes |
| Eosinophils | Prominent | Prominent | Few | Prominent; also neutrophilic infiltrates, papillary elongation, and basal zone hyperplasia |
| Food challenge | Vomiting in 1-4 hr; diarrhea in 5-8 hr | Rectal bleeding in 6-72 hr | Vomiting, diarrhea, or both in 40-72 hr | Vomiting and diarrhea in hours to days |
| Treatment | Protein elimination, 80% respond to casein hydrolysate and symptoms clear in 3-10 days; rechallenge under supervision in 1.5-2 yr | Protein elimination, symptoms clear in 3 days with casein hydrolysate; resume/continue breastfeeding on maternal antigen-restricted diet; reintroduce at home after 9-12 mo of age | Protein elimination, symptoms clear in 1-3 wk; rechallenge and biopsy in 1-2 yr | Protein elimination, good response to casein hydrolysate, excellent response to elemental diet; symptoms clear in 2-3 wk, excellent acute response to steroids; rechallenge by introducing food at home and biopsy in 1-2 yr |
| Natural history |
Cow's milk: 60% resolved by 2 yr Soy: 25% resolved by 2 yr |
Resolved by 9-12 mo | Most cases resolve in 2-3 yr | Typically a prolonged, relapsing course |
| Reintroduction of the food | Supervised food challenge | At home, gradually advancing from 1 oz to full feedings over 2 wk | Home, gradually advancing | Home, gradually advancing |
* Eosinophilic gastroenteropathies encompass esophagitis, gastritis, and gastroenterocolitis.
† If positive, may be a risk factor for persistent disease.
FPIES, Food protein–induced enterocolitis syndrome.
From Nowak-Węgrzyn A, Muraro A: Food protein-induced enterocolitis syndrome, Curr Opin Allergy Immunol 9:371–377, 2009 (Table 1, p 372).
Food protein–induced allergic proctocolitis (FPIAP) presents in the 1st few mo of life as blood-streaked stools in otherwise healthy infants (Table 176.5 ). Approximately 60% of cases occur among breastfed infants, with the remainder largely among infants fed cow's milk or soy protein–based formula. Blood loss is typically modest but can occasionally produce anemia.
Food protein–induced enteropathy (FPE) often manifests in the 1st several mo of life as diarrhea, often with steatorrhea and poor weight gain (Table 176.5 ). Symptoms include protracted diarrhea, vomiting in up to 65% of cases, failure to thrive, abdominal distention, early satiety, and malabsorption. Anemia, edema, and hypoproteinemia occur occasionally. Cow's milk sensitivity is the most common cause of FPE in young infants, but it has also been associated with sensitivity to soy, egg, wheat, rice, chicken, and fish in older children. Celiac disease , the most severe form of FPE, occurs in about 1 per 100 U.S. population, although it may be “silent” in many patients (see Chapter 364.2 ). The full-blown form is characterized by extensive loss of absorptive villi and hyperplasia of the crypts, leading to malabsorption, chronic diarrhea, steatorrhea, abdominal distention, flatulence, and weight loss or failure to thrive. Oral ulcers and other extraintestinal symptoms secondary to malabsorption may occur. Genetically susceptible individuals (HLA-DQ2 or HLA-DQ8) demonstrate a cell-mediated response to tissue transglutaminase deamidated gliadin (a fraction of gluten), which is found in wheat, rye, and barley.
Eosinophilic esophagitis (EoE) may appear from infancy through adolescence, more frequently in boys (see Chapter 350 ). In young children, EoE is primarily cell mediated and manifests as chronic gastroesophageal reflux (GER), intermittent emesis, food refusal, abdominal pain, dysphagia, irritability, sleep disturbance, and failure to respond to conventional GER medications. EoE is a clinicopathologic diagnosis. The diagnosis is confirmed when 15 eosinophils per high-power field are seen on esophageal biopsy following treatment with proton pump inhibitors. Eosinophilic gastroenteritis occurs at any age and causes symptoms similar to those of EoE, as well as prominent weight loss or failure to thrive, both of which are the hallmarks of this disorder. More than 50% of patients with this disorder are atopic; however, food-induced IgE-mediated reactions have been implicated only in a minority of patients. Generalized edema secondary to hypoalbuminemia may occur in some infants with marked protein-losing enteropathy.
Oral allergy syndrome (pollen-associated food allergy syndrome) is an IgE-mediated hypersensitivity that occurs in many older children with birch and ragweed pollen–induced allergic rhinitis. Symptoms are usually confined to the oropharynx and consist of the rapid onset of oral pruritus; tingling and angioedema of the lips, tongue, palate, and throat; and occasionally a sensation of pruritus in the ears and tightness in the throat. Symptoms are generally short lived and are caused by local mast cell activation following contact with fresh raw fruit and vegetable proteins that cross-react with birch pollen (apple, carrot, potato, celery, hazel nuts, peanuts, kiwi, cherry, pear), grass pollen (potato, tomato, watermelon, kiwi), and ragweed pollen (banana, melons such as watermelon and cantaloupe).
Acute gastrointestinal allergy generally manifests as acute abdominal pain, vomiting, or diarrhea that accompanies IgE-mediated allergic symptoms in other target organs.
Skin Manifestations
Cutaneous food allergies are also common in infants and young children.
Atopic dermatitis is a form of eczema that generally begins in early infancy and is characterized by pruritus, a chronically relapsing course, and association with asthma and allergic rhinitis (see Chapter 170 ). Although not often apparent from history, at least 30% of children with moderate to severe atopic dermatitis have food allergies. The younger the child and the more severe the eczema, the more likely food allergy is playing a pathogenic role in the disorder.
Acute urticaria and angioedema are among the most common symptoms of food allergic reactions (see Chapter 173 ). The onset of symptoms may be very rapid, within minutes after ingestion of the responsible allergen. Symptoms result from activation of IgE-bearing mast cells by food allergens that are absorbed and circulated rapidly throughout the body. Foods most commonly incriminated in children include egg, milk, peanuts, and nuts, although reactions to various seeds (sesame, poppy) and fruits (kiwi) are becoming more common. Chronic urticaria and angioedema are rarely caused by food allergies.
Perioral dermatitis is often a contact dermatitis caused by substances in toothpaste, gums, lipstick, or medications. Perioral flushing is often noted in infants fed citrus fruits and may be caused by benzoic acid in the food. It may also occur during nursing. In both situations the effect is benign. Flushing may also be caused by auriculotemporal nerve (Frey) syndrome (familial, forceps delivery), which resolves spontaneously.
Respiratory Manifestations
Respiratory food allergies are uncommon as isolated symptoms. Although many parents believe that nasal congestion in infants is often caused by milk allergy, studies show this not to be the case. Food-induced rhinoconjunctivitis symptoms typically accompany allergic symptoms in other target organs, such as skin, and consist of typical allergic rhinitis symptoms (periocular pruritus and tearing, nasal congestion and pruritus, sneezing, rhinorrhea). Wheezing occurs in approximately 25% of IgE-mediated food allergic reactions, but only 10% of asthmatic patients have food-induced respiratory symptoms.
Anaphylaxis
Anaphylaxis is defined as a serious, multisystem allergic reaction that is rapid in onset and potentially fatal. Food allergic reactions are the most common cause of anaphylaxis seen in U.S. hospital emergency departments. In addition to the rapid onset of cutaneous, respiratory, and GI symptoms, patients may demonstrate cardiovascular symptoms, including hypotension, vascular collapse, and cardiac dysrhythmias, which are presumably caused by massive mast cell–mediator release. Food-dependent exercise-induced anaphylaxis occurs more frequently among teenage athletes, especially females (see Chapter 174 ).
Diagnosis
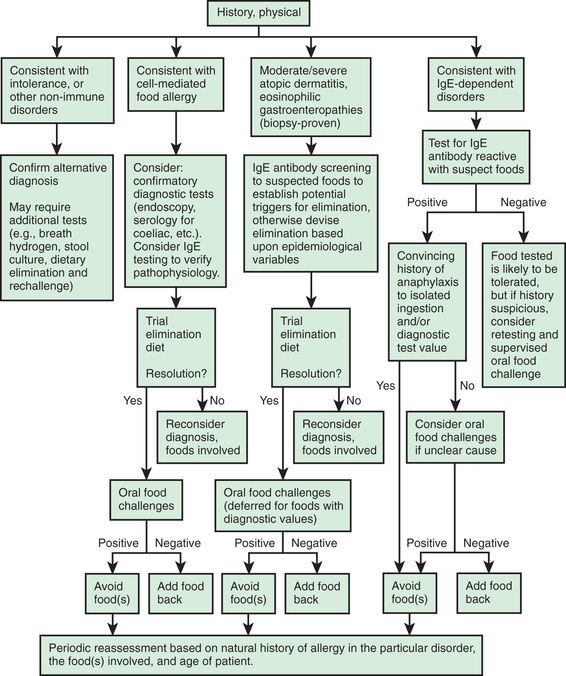
A thorough medical history is necessary to determine whether a patient's symptomatology represents an adverse food reaction (see Table 176.2 ), whether it is an intolerance or food allergic reaction, and if the latter, whether it is likely to be an IgE-mediated or a cell-mediated response (Fig. 176.1 ). The following facts should be established: (1) the food suspected of provoking the reaction and the quantity ingested, (2) the interval between ingestion and the development of symptoms, (3) the types of symptoms elicited by the ingestion, (4) whether ingesting the suspected food produced similar symptoms on other occasions, (5) whether other inciting factors, such as exercise, are necessary, and (6) the interval from the last reaction to the food.
Skin-prick tests and in vitro laboratory tests are useful for demonstrating IgE sensitization, defined as presence of food-specific IgE antibodies. Many fruits and vegetables require skin-prick testing with fresh produce because labile proteins are destroyed during commercial preparation. A negative skin test result virtually excludes an IgE-mediated form of food allergy. Conversely, most children with positive skin test responses to a food do not react when the food is ingested, so more definitive tests, such as quantitative IgE tests or food elimination and challenge, are often necessary to establish a diagnosis of food allergy. Serum food-specific IgE levels ≥15 kUA /L for milk (≥5 kUA /L for children ≤1 yr), ≥7 kUA /L for egg (≥2 kUA /L for children <2 yr), and ≥14 kUA /L for peanut are associated with a >95% likelihood of clinical reactivity to these foods in children with suspected reactivity. In the absence of a clear history of reactivity to a food and evidence of food-specific IgE antibodies, definitive studies must be performed before recommendations are made for avoidance or the use of highly restrictive diets that may be nutritionally deficient, logistically impractical, disruptive to the family, expensive, or a potential source of future feeding disorders. IgE-mediated food allergic reactions are generally very food specific, so the use of broad exclusionary diets, such as avoidance of all legumes, cereal grains, or animal products, is not warranted (Table 176.6 ; see also Table 176.3 ).
Table 176.6
Modified from Sicherer SH: Food allergy, Lancet 360:701–710, 2002.
There are no laboratory studies to help identify foods responsible for cell-mediated reactions. Consequently, elimination diets followed by oral food challenges are the only way to establish the diagnosis. Allergists experienced in dealing with food allergic reactions and able to treat anaphylaxis should perform food challenges. Before a food challenge is initiated, the suspected food should be eliminated from the diet for 10-14 days for IgE-mediated food allergy and up to 8 wk for some cell-mediated disorders, such as EoE. Some children with cell-mediated reactions to cow's milk do not tolerate hydrolysate formulas and must receive amino acid–derived formulas. If symptoms remain unchanged despite appropriate elimination diets, it is unlikely that food allergy is responsible for the child's disorder.
Treatment
Appropriate identification and elimination of foods responsible for food hypersensitivity reactions are the only validated treatments for food allergies. Complete elimination of common foods (milk, egg, soy, wheat, rice, chicken, fish, peanut, nuts) is very difficult because of their widespread use in a variety of processed foods. The lay organization Food Allergy Research and Education (FARE , www.foodallergy.org ) provides excellent information to help parents deal with both the practical and emotional issues surrounding these diets. Validated educational materials are also available through the Consortium of Food Allergy Research (www.cofargroup.org ).
Children with asthma and IgE-mediated food allergy, peanut or nut allergy, or a history of a previous severe reaction should be given self-injectable epinephrine and a written emergency plan in case of accidental ingestion (see Chapter 174 ). Because many food allergies are outgrown, children should be reevaluated periodically by an allergist to determine whether they have lost their clinical reactivity. A number of clinical trials are evaluating the efficacy of oral, sublingual, and epicutaneous (patch) immunotherapy for the treatment of IgE-mediated food allergies (milk, egg, peanut). Combining oral immunotherapy with anti-IgE treatment (omalizumab) may improve safety compared to oral immunotherapy alone. Furthermore, extensively heated milk or egg in baked products are tolerated by the majority of milk and egg–allergic children. Regular ingestion of baked products with milk and egg appears to accelerate resolution of milk and egg allergy. Table 176.7 provides vaccination recommendations for egg-allergic children who require immunization.
Table 176.7
| VACCINE | ACIP, CDC, 2016 | AAP, 2016 |
|---|---|---|
| MMR/MMRV | May be used | May be used |
| Influenza | Receive with no special precautions* | Receive with no special precautions* |
| Rabies | Use caution | No specific recommendation |
| Yellow fever | Contraindicated, but desensitization protocols may be followed to administer vaccine if necessary (citing PI) | Contraindicated, but desensitization protocols may be followed to administer vaccine if necessary (citing PI) |
* In 2016, recommendations changed to suggest all children with any severity of egg allergy receive the injectable influenza vaccine as appropriate for age in a medical setting without any special testing and with the same precautions as those suggested for other vaccinations, including a 15 minute observation period and being in a setting where personnel and equipment are available to recognize and treat allergic reactions and anaphylaxis.
ACIP, Advisory Committee on Immunization Practices, Centers for Disease Control and Prevention; AAP, American Academy of Pediatrics; PI, product insert.
From Boyce JA, Assa'ad A, Burks AW, et al: Guideline for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel, J Allergy Clin Immunol 126(6):S1–S58, 2010 (Table V, p S31).
Prevention
It was once thought that avoidance of allergenic foods and delayed introduction to the diet would prevent allergy, but the opposite is probably true; delayed introduction of these foods may increase the risk of allergy, especially in children with atopic dermatitis. A trial of early introduction of dietary peanut randomized 640 infants age 4-11 mo with severe eczema, egg allergy, or both to consume or avoid peanut until age 60 mo. The early introduction of peanut dramatically decreased the development of peanut allergy among children at high risk for this allergy. A theory behind this approach is that early oral introduction of peanut induces oral tolerance that precedes the potential sensitization to peanut via the disrupted skin barrier. Infants with early-onset atopic disease (e.g., severe eczema) or egg allergy in the 1st 4 to 6 mo of life might benefit from evaluation by an allergist or physician trained in management of allergic diseases to diagnose any food allergy and assist in implementing appropriate early peanut introduction. The clinician can perform an observed peanut challenge for those with evidence of a positive peanut skin test response or serum peanut-specific IgE >0.35 kUA /L to determine whether they are clinically reactive before initiating at-home introduction of infant-safe forms of peanut. Additional details for the early introduction of peanut are available from the National Institute of Allergy and Infectious Diseases (NIAID).*
There is no compelling evidence to support the practice of restricting the maternal diet during pregnancy or while breastfeeding, or of delaying introduction of various allergenic foods to infants from atopic families (Table 176.8 ). Exclusive breastfeeding for the 1st 4-6 mo of life may reduce allergic disorders in the 1st few yr of life in infants at high risk for development of allergic disease. Potentially allergenic foods (eggs, milk, wheat, soy, peanut/tree nut products, fish) should be introduced after this period of exclusive breastfeeding and may prevent the development of allergies later in life. Use of hydrolyzed formulas may be beneficial if breastfeeding cannot be continued for 4-6 mo or after weaning, especially to prevent eczema in high-risk families, but this approach remains controversial. Probiotic supplements may also reduce the incidence and severity of eczema. Because some skin preparations contain peanut oil, which may sensitize young infants, especially those with cutaneous inflammation, such preparations should be avoided. Since inflamed/disrupted skin barrier is a risk factor for food allergy, trials are underway to enhance the skin barrier from birth, using emollients and decreasing bathing frequency, to reduce the incidence of atopic dermatitis in high-risk neonates.