Nasal Polyps
Joseph Haddad Jr, Sonam N. Dodhia
Etiology
Nasal polyps are benign pedunculated tumors formed from edematous, usually chronically inflamed nasal mucosa. They commonly arise from the ethmoidal sinus and occur in the middle meatus. Occasionally they appear within the maxillary antrum and can extend to the nasopharynx (antrochoanal polyp).
It is estimated that between 1% and 4% of the population will develop nasal polyps at some point; the incidence of nasal polyps increases with age. Antrochoanal polyps represent only 4–6% of all nasal polyps in the general population but account for approximately one third of polyps in the pediatric population. Large or multiple polyps can completely obstruct the nasal passage. The polyps originating from the ethmoidal sinus are usually smaller and multiple, as compared with the large and usually single antrochoanal polyp.
Cystic fibrosis (CF; see Chapter 432 ) is the most common childhood cause of nasal polyposis, and up to 50% of CF patients experience obstructing nasal polyposis, which is rare in non-CF children. Therefore, CF should be suspected in any child younger than 12 yr old with nasal polyps, even in the absence of typical respiratory and digestive symptoms. Nasal polyposis is also associated with chronic sinusitis (see Chapter 408 ) and allergic rhinitis. Large population studies have noted a significant familial risk in having chronic rhinosinusitis with polyposis. Furthermore, it has been noted in a substantial number of studies that low vitamin D levels are correlated with polypoid chronic rhinosinusitis, likely related to the role vitamin D plays as an immunomodulator in the respiratory epithelium. In the Samter triad , nasal polyps are associated with aspirin sensitivity and asthma; this condition is rare in children.
Clinical Manifestations
Obstruction of nasal passages is prominent, with associated hyponasal speech and mouth breathing. Profuse unilateral mucoid or mucopurulent rhinorrhea may also be present. An examination of the nasal passages shows glistening, gray, grape-like masses squeezed between the nasal turbinates and the septum.
Diagnosis and Differential Diagnosis
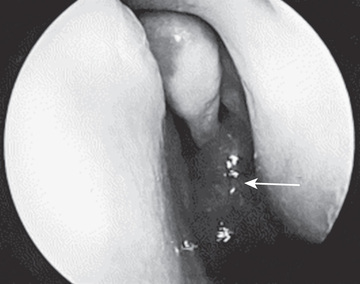
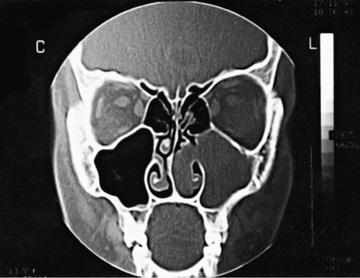
Examination of the external nose and rhinoscopy should be performed. Ethmoidal polyps can be readily distinguished from the well-vascularized turbinate tissue, which is pink or red; antrochoanal polyps may have a more fleshy appearance (Fig. 406.1 ). Antrochoanal polyps may prolapse into the nasopharynx; flexible nasopharyngoscopy can assist in making this diagnosis. Prolonged presence of ethmoidal polyps in a child can widen the bridge of the nose and erode adjacent osseous structures. Tumors of the nose cause more local destruction and distortion of the anatomy. CT scan of the midface is key to diagnosis and planning for surgical treatment (Fig. 406.2 ).
Treatment
Local or systemic decongestants are not usually effective in shrinking the polyps, although they may provide symptomatic relief from the associated mucosal edema. Intranasal steroid sprays, and sometimes systemic steroids, can provide some shrinkage of nasal polyps with symptomatic relief and have proved useful in children with CF and adults with nasal polyps. Topical nasal steroid therapy, fluticasone, mometasone, and budesonide appears to result in nasal symptom improvement, but were found to have no effect on those with CF. Doxycycline (100 mg daily) has a significant effect on the size of nasal polyps, nasal symptoms, and mucosal and systemic markers of inflammation. Polyps should be removed surgically if complete obstruction, uncontrolled rhinorrhea, or deformity of the nose appears. If the underlying pathogenic mechanism cannot be eliminated (such as CF), the polyps may soon return. Functional endoscopic sinus surgery provides more complete polyp removal and treatment of other associated nasal disease; in some cases, this has reduced the need for frequent surgeries. Nasal steroid sprays should also be started preventively, once postsurgical healing occurs.
Antrochoanal polyps do not respond to medical measures and must be removed surgically, typically via endoscopic sinus surgery, or alternatively with a mini-Caldwell procedure. Since these types of polyps are not associated with any underlying disease process, the recurrence rate is much less than for other types of polyps.