
High Cholesterol and/or Triglycerides

• Elevations in cholesterol and/or triglycerides above accepted levels
The evidence overwhelmingly demonstrates that elevated cholesterol and triglycerides greatly increase the risk of death due to cardiovascular disease. It is currently recommended that total blood cholesterol be less than 200 mg/dl and triglycerides be lower than 150 mg/dl. In addition, low-density lipoprotein (LDL) cholesterol should be less than 130 mg/dl and high-density lipoprotein (HDL) cholesterol greater than 40 mg/dl in men and 50 mg/dl in women.
LDL and HDL are carriers for cholesterol in the blood. The major categories of lipoproteins are very low-density lipoprotein (VLDL), LDL, and HDL. Because VLDL and LDL are responsible for transporting fats (primarily triglycerides and cholesterol) from the liver to body cells, while HDL is responsible for returning fats to the liver, elevations of either VLDL or LDL are associated with an increased risk for developing atherosclerosis (hardening of the arteries), the primary cause of a heart attack or stroke. In contrast, higher levels of HDL are associated with a lower risk of heart attacks. The real problem is oxidized LDL, which fuels the inflammatory process involved in atherosclerosis, coupled with low levels of HDL.
Determining Risk
The ratios of total cholesterol to HDL cholesterol and LDL to HDL are referred to as the cardiac risk factor ratios because they reflect whether cholesterol is being deposited into tissues or broken down and excreted. The total cholesterol-to-HDL ratio should be no higher than 4.2, and the LDL-to-HDL ratio should be no higher than 2.5. The risk for heart disease can be reduced dramatically by lowering LDL cholesterol while simultaneously raising HDL cholesterol levels. For every 1% drop in the LDL cholesterol level, the risk for a heart attack drops by 2%. Conversely, for every 1% increase in HDL levels, the risk for a heart attack drops 3% to 4%.1
Although LDL cholesterol is referred to as “bad cholesterol,” there are some forms that are worse than others. For example, oxidized LDL is a persistent pro-inflammatory trigger for the progression of atherosclerosis and plaque rupture. Also, smaller, higher-density LDL molecules are associated with greater risk than larger, lower-density LDL molecules.2 In a small trial of nondiabetic subjects, researchers determined that smaller LDL particles are more likely than larger LDL particles to be attached to sugar molecules (glycated or glycosylated), strongly suggesting an explanation for why these particles are more likely to participate in the process of atherosclerosis, and highlighting the importance of avoiding high blood sugar levels and subsequent glycation.3
Recommended Cholesterol and Triglyceride Levels |
||
|
LEVEL (MG/DL) |
RESULT |
Total cholesterol |
<200 |
Desirable |
LDL cholesterol |
<100* |
Desirable |
HDL cholesterol |
<35 |
Low (undesirable) |
Triglycerides |
<150 |
Desirable |
* For very high-risk patients (those having cardiovascular disease with multiple risk factors such as diabetes, severe and poorly controlled risk factors such as continued smoking, or the presence of metabolic syndrome), the goal is <70 mg/dl for LDL.
Another marker that deserves mention is Lp(a), a plasma lipoprotein whose structure and composition closely resemble that of LDL but which has an additional molecule of an adhesive protein called apolipoprotein(a) that helps the LDL stick to the walls of the artery. Elevated plasma levels of Lp(a) are an independent risk factor for coronary heart disease, particularly in patients with elevated LDL cholesterol. In fact, in one analysis a high level of Lp(a) was shown to carry with it a 10 times greater risk for heart disease than an elevated LDL cholesterol level alone.4 Levels of Lp(a) below 20 mg/dl are associated with a low risk for heart disease; levels between 20 and 40 mg/dl are associated with a moderate risk; and levels above 40 mg/dl are associated with an extremely high risk for heart disease.
In the past, the relation between elevations of blood triglycerides (hypertriglyceridemia) and coronary heart disease has been uncertain. However, a large body of accumulating evidence indicates that elevated triglycerides are an independent risk factor for cardiovascular disease.5,6 When elevated triglycerides are combined with elevations in LDL cholesterol, the result is a recipe for an early heart attack. In one analysis, high triglycerides combined with elevated LDL cholesterol and a high LDL:HDL ratio (greater than 5) increased the risk of coronary heart disease by approximately sixfold.
Elevations of blood cholesterol, triglycerides, or both can be due to genetic factors. These conditions are referred to as familial hypercholesterolemia (FH), familial hypertriglyceridemia (FT), and familial combined hyperlipidemia (FCH). Relatively speaking, these disorders are among the most common inherited diseases, as they affect about 1 in every 500 people.
The basic problem in FH is a defect in the receptor protein for LDL in the liver. Under normal situations the LDL receptor is responsible for removing cholesterol from the blood. When the liver cell takes up the LDL after it has bound to the receptor, it signals the liver cell to stop making cholesterol. In FH the result of the defect in the LDL receptor is that the liver does not receive the message to stop making cholesterol.
Damage to the LDL receptor occurs with normal aging and in several disease states, with diabetes being chief among them owing to increased glycosylation of the receptor proteins. As a result of LDL receptor damage, cholesterol levels tend to rise with age. In addition, a diet high in saturated fat and cholesterol decreases the number of LDL receptors, thereby reducing the feedback mechanism that tells the liver cell that no more cholesterol is necessary.
Fortunately, lifestyle and dietary changes can increase the function or number of LDL receptors, or both. The most dramatic effects are in people without inherited causes of elevated cholesterol or triglycerides, or both, but even people with FH can benefit.
FCH and FT result in defects similar to those seen in FH. In FCH the basic defect appears to be an accelerated production of VLDL in the liver. People with FCH may have only a high blood triglyceride level, only a high cholesterol level, or both. In FT there is only an elevation in blood triglyceride levels, and HDL cholesterol levels tend to be low. The defect in FT is that the VLDL particles made by the liver are larger than normal and carry more triglycerides. FT is made worse by diabetes, gout, and obesity.
Therapeutic Considerations
Lowering total cholesterol as well as LDL cholesterol and triglycerides is clearly associated with reducing the risk of cardiovascular disease. Most of the benefits noted with lowering LDL are based on a large number of randomized clinical trials involving the use of statin drugs (HMG CoA reductase inhibitors). Statin drugs owe their origin to red yeast (Monascus purpureus) fermented on rice. This traditional Chinese medicine has been used for more than 2,000 years. Red yeast rice is the source of a group of compounds known as monacolins (such as lovastatin, also known as monacolin K). The marketing of an extract of red yeast rice standardized for monacolin content as a dietary supplement in the United States caused controversy in 1997 because it contained a natural source of a prescription drug. The FDA eventually ruled that red yeast rice products could be sold only if they were free of monacolin content. Nonetheless, it appears some red yeast products on the market do contain these compounds.
In high risk patients the data are clear that statin drugs can produce decreases in total mortality, cardiovascular events, hospitalizations, and the need for revascularization procedures. The debate remains whether statin therapy represents the optimal treatment approach to primary prevention of coronary artery disease in patients whose only risk factor is elevated LDL, especially in light of the growing importance of risk factors such as C-reactive protein and nutritional factors.7,8 For example, one interesting study compared the Portfolio Diet (which emphasizes plant-based cholesterol-lowering foods) with lovastatin.9 The participants were randomly assigned to a control diet low in saturated fat, the control diet plus 20 mg lovastatin per day, or a diet like the Portfolio Diet (high in plant sterols, soy protein, soluble fiber, and almonds). After one month, the control, statin, and Portfolio Diet groups had mean decreases in LDL of 8%, 30.9%, and 28.6%, respectively. Respective reductions in C-reactive protein were 10%, 33.3%, and 28.2%. This study and subsequent studies show that including a diverse array of cholesterol-lowering components in the diet (as in the Portfolio Diet) increased the effectiveness of diet as a treatment for hypercholesterolemia, producing results comparable to a statin drug but without the side effects.10,11
The best clinical approach is not to rely on a single supplement, but rather to incorporate a broad-spectrum dietary approach that has a wide array of components shown to positively affect lipid levels (reducing saturated fat, trans-fatty acids, and cholesterol, as well as increasing monounsaturated fats, soluble fiber, and nuts). For example, while a meta-analysis of 27 randomized, controlled trials demonstrated that soy protein supplementation reduced total cholesterol, LDL, and triglycerides, the effect was greater when the soy protein was used in conjunction with other dietary interventions.12 In addition, the effects of isolated soy protein appear to be considerably less than those of increasing soy food consumption in general.13 Much of the cholesterol-lowering effect of soy foods may relate more to soy’s isoflavone and soluble fiber content than to the protein.
Despite research documenting the benefits of nondrug approaches, it is unlikely that they will replace the use of statin drugs as a primary therapy anytime soon. In 2011, more than one of every six adults—nearly 40 million people—took a statin drug to lower LDL. Therefore, the focus for many will be on how to support statin therapy. For example, it appears that individuals taking statins need supplemental coenzyme Q10. HMG-CoA reductase is required not only for the synthesis of cholesterol but also for the production of CoQ10. Thus administration of statins might compromise CoQ10 status by decreasing its synthesis. Even modest dosages of various statins have been shown to lower blood CoQ10 levels. Researchers have concluded that inhibition of CoQ10 synthesis by statin drugs could explain the most commonly reported side effects, especially fatigue and muscle pain, as well as the more serious side effects such as rhabdomyolysis.14,15 CoQ10 supplementation in subjects on statin drugs has also been shown to reduce markers of oxidative damage.
Elevations in cholesterol may be the result of low thyroid function (hypothyroidism); see the chapter “Hypothyroidism.”
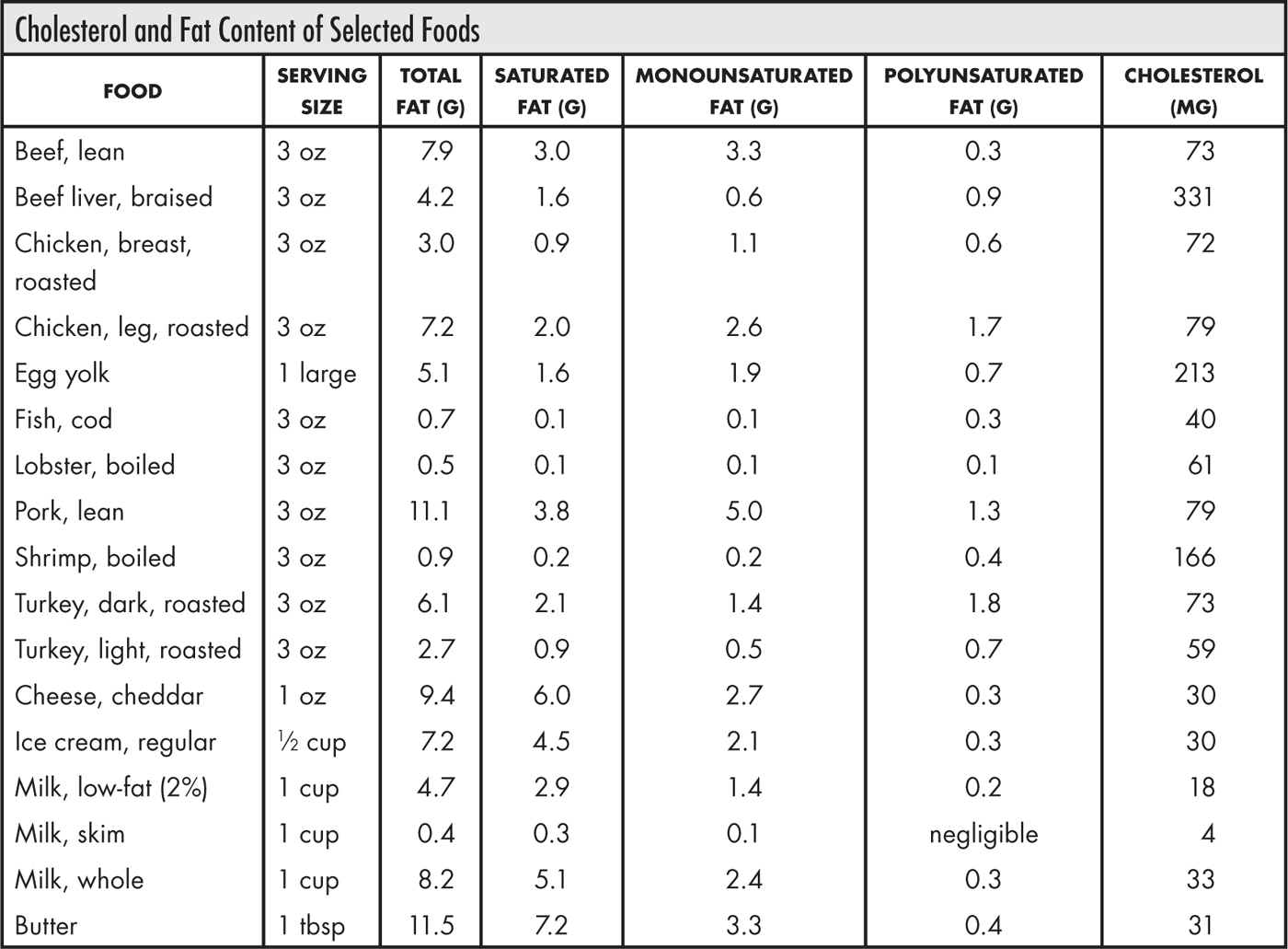
While the liver is the major source of blood cholesterol, dietary cholesterol can be an important contributor. Diets high in cholesterol are associated with an increased risk for heart disease, cancer, and stroke. However, it may turn out that the level of saturated fats in these foods is more relevant than their cholesterol content. This opinion is supported by a statistical analysis of 224 dietary studies carried out over the past 25 years that investigated the relationship between diet and blood cholesterol levels in more than 8,000 subjects.16 What investigators found was that saturated fat in the diet, not dietary cholesterol, influences blood cholesterol levels most, and that for most people dietary cholesterol has very little effect on blood cholesterol levels. Nonetheless, it is generally recommended that a healthy person should restrict dietary cholesterol intake to 300 mg per day, while someone with high cholesterol or heart disease should consume no more than 200 mg cholesterol per day. In addition, keep saturated fat intake to a bare minimum, certainly no more than 10 to 15 g per day and ideally even less.
It is well established that the soluble fiber found in legumes, fruit, and vegetables is effective in lowering cholesterol levels.17 The greater the degree of viscosity or gel-forming ability, the greater the effect of a particular type of dietary fiber on lowering cholesterol levels; new, highly viscous blends of soluble fiber provide greater effects than single fiber sources.18,19 The table below shows the effects of various soluble fiber products.20
The overwhelming majority of studies have demonstrated that individuals with high cholesterol levels experience significant reductions with frequent oatmeal or oat bran consumption. In contrast, individuals with normal or low cholesterol levels see little change. In individuals with high cholesterol levels (above 200 mg/dl), the daily consumption of the equivalent of 3 g soluble oat fiber typically lowers total cholesterol by 8 to 23%. This is highly significant, as with each 1% drop in serum cholesterol level there is a 2% decrease in the risk of developing heart disease. One bowl of ready-to-eat oat bran cereal or oatmeal has approximately 3 g fiber. Although oatmeal’s fiber content (7%) is less than that of oat bran (15 to 26%), it has been determined that oatmeal’s polyunsaturated fatty acids contribute as much to its cholesterol-lowering effects as its fiber content does.
To help lower cholesterol, try to eat 35 g fiber per day from fiber-rich foods (a full listing can be found in Appendix B). Achieving higher fiber intake is associated not only with lower cholesterol levels but also with lower levels of inflammatory mediators such as C-reactive protein.21
The cardiovascular benefits of the long-chain omega-3 fatty acids EPA and DHA have been demonstrated in more than 300 clinical trials and are detailed in the chapter “Heart and Cardiovascular Health.” Supplementation with EPA + DHA has little effect on cholesterol levels but does lower triglyceride levels significantly and has a myriad of additional beneficial effects in protecting against cardiovascular disease.22 In general, for cardiovascular protection the dosage recommendation is 1,000 mg EPA + DHA per day, but for lowering triglycerides the dosage is 3,000 to 5,000 mg EPA + DHA.23 Lower dosages of EPA + DHA exert only mild effects on triglyceride levels (e.g., intakes of 200 and 500 mg per day lower triglyceride levels by 3.1% and 7.2% respectively).24 In one double-blind study, after eight weeks of supplementation a daily dosage of 3.4 g EPA + DHA lowered triglycerides by 27%, while a lower dosage of 0.85 g had no significant effect.25 These results clearly indicate that lowering triglycerides with fish oils requires dosages of 3 g EPA + DHA per day. In patients with triglyceride levels above 500 mg/dl, approximately 4 g per day of EPA + DHA reduced triglyceride levels by 45%. Fish oils work to lower triglyceride levels by reducing the formation of triglycerides while increasing their breakdown into energy.26
In many cases dietary therapy, while important, is not sufficient alone to reduce lipid levels to the desired ranges. Fortunately, several natural compounds can lower cholesterol levels and other significant risk factors for cardiovascular disease. In fact, when cost, safety, and effectiveness are all considered, the natural alternatives presented here may offer significant advantages over standard drug therapy, especially when used together rather than as isolated therapies.
Niacin
Since the 1950s niacin (vitamin B3) has been known to be effective in lowering blood cholesterol levels. In the 1970s the famous Coronary Drug Project demonstrated that niacin was the only cholesterol-lowering agent to actually reduce overall mortality. Niacin typically lowers LDL cholesterol by 16 to 23% while raising HDL cholesterol by 20 to 33%. These effects, especially the effect on HDL, compare quite favorably with those of conventional cholesterol-lowering drugs.27,28
It is now known that niacin does much more than lower total cholesterol. Specifically, niacin has been shown to lower LDL, the more harmful Lp(a), triglycerides, C-reactive protein, and fibrinogen while simultaneously raising beneficial HDL. Despite the fact that niacin has demonstrated better overall results in reducing risk factors for coronary heart disease compared with other cholesterol-lowering agents, physicians are often reluctant to prescribe it. The reason is a widespread perception that niacin is difficult to work with because of the bothersome flushing of the skin. In addition, because niacin is a widely available generic agent, it does not offer the drug companies the huge profits that the other lipid-lowering agents have enjoyed. As a result, niacin does not benefit from the intensive research and advertising that focus on the statin drugs. Despite the advantages of niacin over other lipid-lowering drugs, it accounts for less than 10% of all cholesterol-lowering prescriptions. Niaspan, a prescription niacin product, accounted for 952,000 prescriptions in 2002, translating to sales of $145.7 million—a dramatic 73% increase from 2001 levels. By 2010, sales had reached over $927 million, with approximately 100,000 prescriptions per week. The increasing sales of niacin reflect physicians’ growing awareness of the advantages of niacin over statin drugs.
Comparison of Niacin with Lovastatin |
||||
LIPOPROTEIN |
GROUP |
WEEK 10 (%) |
WEEK 18 (%) |
WEEK 26 (%) |
LDL cholesterol (reduction) |
Lovastatin |
26 |
28 |
32 |
|
Niacin |
26 |
28 |
32 |
HDL cholesterol (increase) |
Lovastatin |
6 |
7 |
8 |
|
Niacin |
20 |
29 |
33 |
Lp(a) lipoprotein (reduction) |
Lovastatin |
0 |
0 |
0 |
|
Niacin |
14 |
30 |
35 |
Several studies have compared niacin with standard lipid-lowering drugs, including statins. These studies have shown significant advantages for niacin. In the first published clinical study, niacin was compared with lovastatin directly in 136 subjects. Some of these subjects had LDL over 160 mg/dl and coronary heart disease or more than two coronary heart disease risk factors, or both; the others had LDL cholesterol levels greater than 190 mg/dl and did not have coronary heart disease or had fewer than two coronary heart disease risk factors.29 In the controlled, randomized, open-label, 26-week study, patients were first placed on a 4-week diet run-in period, after which eligible patients were randomly assigned to receive treatment with either lovastatin (20 mg per day) or niacin (1.5 g per day). On the basis of the LDL cholesterol response and patient tolerance, the doses were sequentially increased to 40 and 80 mg per day of lovastatin or 3 and 4.5 g per day of niacin after 10 and 18 weeks of treatment, respectively. In the two patient groups, 66% of those treated with lovastatin and 54% of those treated with niacin reached the maximum dose. The results (see the table below) indicate that while lovastatin produced a greater LDL cholesterol reduction, niacin provided better overall results despite the fact that fewer patients were able to tolerate a full dosage of niacin because of skin flushing. The percentage increase in HDL cholesterol, a more significant indicator for coronary heart disease, was dramatically in favor of niacin (33% vs. 7%). Equally impressive was the percentage decrease in Lp(a) for niacin. Although niacin produced a 35% reduction in Lp(a) levels, lovastatin did not produce any effect. Niacin’s effect on Lp(a) in this study confirmed a previous study that showed niacin (4 g per day) reduced Lp(a) levels by 38%, and a subsequent study that showed similar reductions in Lp(a) in patients with diabetes.30,31
Another comparative study evaluated the lipoprotein responses to niacin, gemfibrozil, and lovastatin in patients with normal total cholesterol levels but low levels of HDL cholesterol.32 The first phase of the study compared lipoprotein responses with lovastatin and gemfibrozil in 61 middle-aged men; gemfibrozil therapy increased HDL cholesterol levels by 10% and lovastatin increased them by 6%. In the second phase, 37 patients agreed to take niacin; 27 patients finished this phase at a dose of 4.5 g per day. In the second phase, niacin therapy was shown to raise HDL cholesterol by 30%.
Another study compared niacin with atorvastatin (Lipitor).33 The average dosage was 3,000 mg niacin and 80 mg Lipitor. The patients selected had small, dense LDL particles linked to an increased risk for CVD and low levels of HDL2, a specific fraction of HDL associated with a greater protective effect than HDL alone. Although Lipitor reduced total LDL cholesterol levels substantially more than niacin did, niacin was more effective at increasing LDL particle size and raising HDL and HDL2 than Lipitor was (see the table below).
Because taking niacin at higher dosages (e.g., 3,000 mg or more) can impair glucose tolerance, many physicians have avoided niacin therapy with diabetics, but newer studies using slightly lower dosages (1,000 to 2,000 mg) of niacin have not shown it to adversely affect blood sugar regulation.34 For example, during a 16-week, double-blind, placebo-controlled trial, 148 type 2 diabetes patients were randomly assigned to receive either a placebo or 1,000 or 1,500 mg per day of niacin; in the niacin-treated groups there was no significant loss in glycemic control, and the favorable effects on blood lipids were still apparent.35 Other studies have actually shown hemoglobin A1C to drop, indicating improvement in blood sugar control.34
The most common blood lipid abnormalities in type 2 diabetic patients are elevated triglyceride levels, decreased HDL levels, and a preponderance of smaller, denser LDL particles. Niacin has been shown to address all of these areas much more significantly than the statins or other lipid-lowering drugs.33–35
Effects of Atorvastatin (Lipitor) and Niacin on Lipid Profiles |
||||||
VARIABLE |
ATORVASTATIN |
NIACIN |
ATORVASTATIN + NIACIN |
|||
BEFORE |
AFTER |
BEFORE |
AFTER |
BEFORE |
AFTER |
|
Total LDL (mg/dl) |
110 |
56 |
111 |
89 |
123 |
55 |
LDL peak diameter |
251 |
256 |
253 |
263 |
250 |
263 |
Lipoprotein(a) (mg/dl) |
45 |
44 |
37 |
23 |
54 |
35 |
HDL (mg/dl) |
42 |
43 |
38 |
54 |
38 |
54 |
HDL2 (%) |
30 |
42 |
29 |
43 |
32 |
37 |
Triglycerides (mg/dl) |
186 |
100 |
194 |
108 |
235 |
73 |
In addition to lowering cholesterol and triglycerides, niacin exerts additional benefits in battling atherosclerosis. Specifically, in patients with coronary artery disease niacin produces beneficial changes in lipid particle distribution that are not well reflected in typical lipoprotein analysis. Systemic markers of inflammation decrease in patients receiving niacin as well. In one study of 54 subjects with stable coronary artery disease, when a modest dosage of niacin (1,000 mg per day) was added to existing therapy for three months, there was a 32% increase in large-particle HDL2 (protective), an 8% decrease in small-particle HDL (nonprotective), an 82% increase in large-particle LDL (not associated with increased risk for CVD), and a 12% decrease in small-particle LDL (significantly associated with increased risk for CVD).36 Niacin therapy also decreased lipoprotein-associated phospholipase A2 and CRP levels (20% and 15%, respectively). No significant changes from baseline were seen in any tested variable in subjects who received a placebo. These results indicate that the addition of niacin to existing medical regimens for patients with coronary artery disease and already well-controlled lipid levels favorably improves the distribution of lipoprotein particle sizes and inflammatory markers in a manner expected to improve cardiovascular protection.
While niacin exerts significant benefit on its own, it does not appear to enhance the benefits of statins in patients whose lipid levels are well controlled. A study funded by the National Heart, Lung, and Blood Institute recruited 3,400 patients who were at risk for heart trouble despite the fact that their LDL cholesterol was under control with the use of the statin drug simvastatin (Zocor). The study ended 18 months early because there was no additional cardiovascular benefit in those taking niacin. Nonetheless, other studies are under way to determine the effect of niacin combined with a statin in patients with very low HDL levels and/or poorly controlled LDL levels.
The side effects of niacin are well known. The most common and bothersome side effect is the skin flushing that typically occurs 20 to 30 minutes after the niacin is taken. Other occasional side effects of niacin include gastric irritation, nausea, and liver damage. In an attempt to combat the acute skin flushing, several manufacturers began marketing sustained-release, timed-release, or slow-release niacin products. These formulations allow the niacin to be absorbed gradually, thereby reducing the flushing reaction. However, although these forms of niacin reduce skin flushing, early versions of timed-release preparations were proved to be more toxic to the liver than regular niacin. In one analysis 52% of the patients taking an early sustained-release niacin preparation developed liver toxicity, while none of the patients taking immediate-release niacin developed liver toxicity.37 The newer timed-released preparations on the market, referred to as “intermediate-release,” appear to have solved this problem, as relatively large clinical trials have shown them to be extremely well tolerated even when combined with statins.38–41 For example, the safety and tolerability of intermediate-release niacin preparation was evaluated in a multicenter study of 566 patients.41 The target dose was achieved by 65% of patients. Flushing was the most common side effect (42%), as expected, and 9.7% withdrew because of it. Other drug-related adverse reactions occurred at a low frequency (18.6%), and 8.7% withdrew for an adverse reaction other than flushing. Most adverse reactions were mild or moderate in severity. There was no liver toxicity or serious adverse muscle event.
Another safe form of niacin is inositol hexaniacinate. This form of niacin has long been used in Europe to lower cholesterol levels and also to improve blood flow in intermittent claudication. It yields slightly better clinical results than standard niacin and is much better tolerated, in terms of both flushing and, more important, long-term side effects.42,43
Regardless of the form of niacin you choose to use, your doctor should check your cholesterol and liver function periodically (minimum every three months). Niacin should not be used by anyone with pre-existing liver disease or elevation in liver enzymes. For these people, plant sterols, garlic, and pantethine are recommended.
For best results niacin should be taken at night, as most cholesterol synthesis occurs during sleep. If pure crystalline niacin is being used, begin with a dose of 100 mg a day and increase carefully over four to six weeks to the full therapeutic dose of 1.5 to 3 g per day. If you use an intermediate-release product (do not use any other form of time-release niacin) or inositol hexaniacinate, a 500-mg dosage should be taken at night and increased to 1,500 mg after two weeks. If after one month of therapy the dosage of 1,500 mg per day fails to effectively lower LDL cholesterol, the dosage should be increased to 2,000 mg; if that dosage fails to lower lipids, increase the dosage to 3,000 mg before discontinuing owing to lack of efficacy.
Plant Sterols and Stanols
Phytosterols and phytostanols are structurally similar to cholesterol and can act in the intestine to lower cholesterol absorption by displacing cholesterol from intestinal micelles (an aggregate of water-insoluble molecules, such as cholesterol, surrounded by water-soluble molecules that facilitate absorption into the body). Because phytosterols and phytostanols are poorly absorbed themselves, blood cholesterol levels will drop, owing to increased excretion. These compounds are being added to so-called functional foods (e.g., margarine and other spreads; orange juice) and are also available as dietary supplements.44
Phytosterols and phytostanols are effective in lowering LDL in some people. A meta-analysis of 41 trials showed that an intake of 2 g stanols or sterols per day reduced LDL by 10%.44 Taking higher dosages added little additional benefit. Phytosterols and phytostanols can be used in addition to diet or drug interventions, as they provide additional benefits. For example, eating foods low in saturated fat and cholesterol and high in stanols or sterols can reduce LDL by 20%; adding sterols or stanols to statin medication is more effective than doubling the statin dose. The individuals most likely to respond are those who have been identified as having high cholesterol absorption and low cholesterol biosynthesis. Phytosterols and phytostanols have also shown antiplatelet and antioxidant effects.45–47
Be aware, however, that at higher dosages, phytosterols or phytostanols may reduce carotenoid absorption. Human subjects consuming 6.6 g per day of phytosterols showed cholesterol-adjusted plasma reduction of alpha- and beta-carotene levels (19 to 23%), lutein (14%), and lycopene (11%). This effect was partially reversed by increased fruit and vegetable intake.48
Pantethine
Pantethine is the stable form of pantetheine, the active form of vitamin B5 (pantothenic acid). Pantothenic acid is the most important component of coenzyme A, which is involved in the transport of fats to and from cells as well as to the energy-producing compartments within the cell. Without coenzyme A, the cell’s fats cannot be metabolized to energy.
Pantethine has significant lipid-lowering activity, while pantothenic acid has little if any effect in lowering cholesterol and triglyceride levels. Pantethine at 900 mg per day has been shown to significantly reduce levels of serum triglyceride (32%), total cholesterol (19%), and LDL cholesterol (21%) while increasing HDL cholesterol (23%).49,50 It appears to be especially useful in diabetics.51–53
Effects on Blood Lipids of Several Natural Compounds |
|||
|
NIACIN |
GARLIC |
PANTETHINE |
Total cholesterol (% decrease) |
18 |
10 |
19 |
LDL cholesterol (% decrease) |
23 |
15 |
21 |
HDL cholesterol (% increase) |
32 |
31 |
23 |
Triglycerides (% decrease) |
26 |
13 |
32 |
The lipid-lowering effects of pantethine are especially impressive because it has virtually no toxicity compared with conventional lipid-lowering drugs.
Garlic
Garlic (Allium sativum) appears to be an important protective factor against heart disease and stroke for many reasons. Garlic has been shown to lower blood cholesterol levels even in apparently healthy individuals. In numerous double-blind, placebo-controlled studies of patients with initial cholesterol levels greater than 200 mg/dl, daily supplementation with commercial preparations providing at least 10 mg alliin or a total allicin potential of 4,000 mcg can lower total serum cholesterol by about 10 to 12%, LDL cholesterol by about 15%, and triglycerides by around 15%, with HDL cholesterol levels usually increasing by about 10%. However, most trials not using products that can deliver this dosage of allicin fail to produce a lipid-lowering effect.54–58
![]()
QUICK REVIEW
• Elevated cholesterol levels in the blood are linked to heart attacks and strokes.
• Although in most cases high cholesterol is due to dietary and lifestyle factors, it can also be the result of genetic factors.
• Elevations in cholesterol may be the result of low thyroid function (hypothyroidism).
• The most important approach to lowering high cholesterol is a healthful diet and lifestyle.
• Soluble fiber from the diet and/or supplements can lower cholesterol levels.
• Fish oils do not significantly lower cholesterol but do exert exceptional triglyceride-lowering action.
• Niacin has been shown to both lower cholesterol and reduce overall early mortality.
• Niacin has demonstrated better overall results in reducing the risk for coronary heart disease compared with cholesterol-lowering drugs.
• Garlic has a positive effect provided that the dosage of allicin is sufficient.
• Pantethine improves cholesterol and triglyceride levels as well as normalizes platelet lipid composition and function and blood viscosity.
Although the effects of supplemental garlic preparations on cholesterol levels are modest, the combination of lowering LDL and raising HDL can greatly improve the HDL-to-LDL ratio, a significant goal in the prevention of heart disease and strokes. Garlic preparations have also demonstrated blood-pressure-lowering effects, inhibition of platelet aggregation, reduction of plasma viscosity, promotion of fibrinolysis, prevention of LDL oxidation, and positive effects on endothelial function, vascular reactivity, and peripheral blood flow.
![]()
TREATMENT SUMMARY
Keep in mind that cholesterol levels are just one piece of the puzzle of reducing cardiovascular disease. A comprehensive perspective is very important. Follow the recommendations given in the chapter “Heart and Cardiovascular Health.”
Numerous natural compounds can effectively improve cholesterol and triglyceride levels. Of the several described above, niacin produces the best overall effect. However, the others do have a place in the clinical management of high cholesterol and triglycerides. In particular, the benefits of fish oils extend far beyond their effect on blood lipids.
Typically, along with dietary and lifestyle recommendations, niacin (1,000 mg to 3,000 mg at night) reduces total cholesterol by 50 to 75 mg/dl in patients with initial total cholesterol levels above 250 mg/dl within the first two months. In patients with initial cholesterol levels above 300 mg/dl, it may take four to six months before cholesterol levels begin to reach recommended levels. Once cholesterol levels are below 200 mg/dl for two successive blood measurements at least two months apart, the dosage can be reduced to 500 mg three times per day for two months. If the cholesterol levels creep up above 200 mg/dl, then the dosage of niacin should be raised back up to previous levels. If the cholesterol level remains below 200 mg/dl, then the niacin can be withdrawn completely and the cholesterol levels rechecked in two months, with niacin therapy reinstituted if levels have exceeded 200 mg/dl. The same sort of schedule applies to other natural cholesterol-lowering agents as well.