

What is the brain? To look at it, not much. To live with? Ah, that’s another story entirely. Although it is out of sight and we often take it for granted, the brain is truly the organ that defines each of us as an individual, unique person and personality. With it, we perceive the world, we laugh, we cry, we scream, we talk, we joke, we learn, we relate to others. It governs our eating, sleeping, breathing, heartbeat, immune function, water balance, hormone output, and our sex drive, sexual fantasies, and sexual function. The heart may beat with a mechanical pump, and we still survive. If the brain dies, which it will in the absence of oxygen for more than just a few minutes, we lose all dimensions of who we are as an individual; indeed, perhaps our very soul is lost. The brain is a powerhouse organ, more creative and adaptable than the world’s fastest computer, yet soft enough to crush with your fingers without the protection of its bony case (the skull) and tough fibrous sac (dura mater) inside the skull. It is often compared to a computer, but that analogy hardly does it justice. If a computer is faced with a new command or task or is given incorrect directions, it simply shuts down; overloaded, it quits. Our brain, however, responds rapidly with new solutions; almost without even realizing it, we adapt and change to meet the new tasks or directions. The brain is able to remember and to forget; your computer can only remember. The computer operates only in an either-or, on-off, “binary” mode. Our brain appreciates infinite “shades of gray” along a continuum of choices and options. In many ways, it is far too complex for me to find a good metaphor or analogy for its function.
When talking about fears of disease in my seminars, I have commented on the way in which many magazine articles lump women together by calling breast cancer our greatest fear. It isn’t for me. My greatest health concern would be developing a disease that destroys my brain, since it is the organ that makes ME who I am. I could work and be ME without my breast. I could no longer work, and I could no longer exist as ME without my brain. It has only been in the last decade or so that we have truly come to appreciate just how completely the brain defines our total being.
As I mentioned in chapter 2, the brain is the master conductor of the “orchestra” made up of all the “instruments” of our body. Without the conducting, coordinating functions of our brain, there would be no “music” from our existence; all our body parts would be chaotically playing individual notes and pieces of tunes, like the discordant notes we hear as an orchestra is warming up, with all the musicians playing individual parts of songs and scales. Not the sort of music you attend a symphony to hear. But when the conductor appears on stage and brings the orchestra to life as an entity, the symphonic music begins. As we listen to the orchestra, we often forget how crucial the conductor’s role is or how many different individual instruments are being guided into playing together to create the drama and beauty of the music. The essence of the brain (and of woman) lies not in the parts, but in the connections between the parts that create the totality of the whole.
To give you an adequate appreciation of the many functions of the brain and its complex structure would require an enormous textbook. I would like to give you an overview of the major areas of the brain and some of the broad areas of function that are orchestrated by these key areas. This information is based on current understandings of the brain; keep in mind, however, that neuroscience research is an exploding area of new knowledge, increasing almost daily, so there will be more that we know about this marvelous organ in years to come. The brain diagram below will help you understand where these areas are and will serve as a reference point for the discussion of the hormone connections that follows.
The brain rests inside the bony protective cover of the skull, with a number of openings in the base of the skull through which pass the nerves and spinal cord. The spinal cord carries bundles of nerve tracts from the head down the back to the lower body. The cortex mediates thinking functions and is divided into two halves, the left and right cerebral hemispheres, which have different specialization of functions. The left hemisphere specializes in verbal, analytical, and sequential (or linear) information processing; the right hemisphere specializes in visual-spatial, nonverbal, intuitive (or nonlinear), and Gestalt information processing. Both hemispheres are further divided into areas called lobes, named for the overlying skull bones: frontal, temporal, parietal, and occipital. The cortex is the part of the brain that makes us uniquely human, since it governs speech, reading, and writing of language. There is overlap among many of the brain areas to a significant degree, both structurally and functionally, which gives us an enormous capacity for adaptability.
At the interior center of the brain, lying below the cortex, is the area of structures collectively called the limbic system. This collection of structures is the primary center integrating emotion, memory, pain, sleep, appetite, sex, and basic functions vital to life. The brainstem group of structures (lying below the cortex) regulates the “vegetative” functions that keep us alive, such as breathing, blood pressure, and heart rate. The cerebellum lies somewhat above the brainstem but below the cortex and is the primary center regulating movement, balance, and motor coordination. Bundles of nerve fibers leaving the cortex, limbic system, brainstem, and cerebellum come together to form the spinal cord that extends to the base of the vertebral column in the lower back area. Chart 4.1 summarizes these major functions; you may find it helpful to refer to it as I discuss the chemistry of mood and hormonal effects on various brain functions.
How do all these areas of the brain communicate with each other? We talk about “nerves,” which are fibers. But how do messages get from one nerve cell to another? I have found it helpful to think about the brain as an enormous three-dimensional network of many different “communication centers” that turn on and off rapidly, send out bursts of electrical impulses, and then communicate further by releasing chemical messenger molecules called neurotransmitters. The visual image that pops into my mind is the large flashing network of fibers in the TV commercial for a worldwide communications company. There are billions of nerve fibers, all with hundreds of potential connections to other nerve fibers. To try to comprehend all this complexity can be overwhelming to most of us.
The basic process of communication between nerve cells, or neurons, and other body cells is both electrical and chemical. The electrical impulse travels along the neuron to the end of the cell called the synapse, or junction point, where it fires off the release of the chemical messenger molecules that have been made in the cell and stored in little sacs called storage vesicles. The chemicals are released to travel across the space between cells, called the synaptic cleft. The messenger molecules fit into a receptor site, and this “unlocks” the next nerve cell to allow the message to be processed and acted upon. This is often illustrated as a neuron connecting with only one other neuron, but in reality, each neuron has perhaps hundreds of connections with other cells. What I have described is a greatly simplified version of a very complex, multidimensional, continuous process occurring every second of every day we are alive. It is awesome to consider the incredible intricacies of the body.
BRAIN AREAS AND THEIR KEY FUNCTIONS
BRAIN AREA |
FUNCTIONS |
FRONTAL Lobe |
• integrates thinking, feeling, creative imagining, decision making • oversees “social appropriateness” of behavior, insight-judgment abilities • has role in expression of personality • helps control body movements |
TEMPORAL Lobes |
• process auditory information, • control language (usually left hemisphere) and memory, • help modulate emotions |
PARIETAL Lobes |
• receive information about body sensations (“somatosensory area”) • modulate spatial orientation ability |
OCCIPITAL Lobe |
• receives and processes visual information |
BRAINSTEM: Midbrain, Pons, and Medullas: |
• regulates “survival functions” such as: respiration, heart rate, blood pressure • receives information via multiple connections (brain and spinal cord) |
LIMBIC SYSTEM: Amygdala, Hippocampus, Mammillary Bodies, Fornix, Basal Ganglia (BG), Thalamus, Hypothalamus, Pituitary, and Cingulate Gyrus |
• memory processing • mood-emotion regulation • attention, alertness, focus • human “drives”: appetite, thirst, sex, aggression, sleep-wake cycles • governs “starting and stopping” behavior • hormone regulation (especially hypothalamus, and pituitary) • has role in modulating chronic pain, acute pain paths bypass limbic area • integrates sensory information and role in movement (basal ganglia) |
CEREBELLUM |
• integrates and coordinates movement (with cortex), balance, coordination |
SPINAL CORD |
• carries nerve tracts and chemical messengers back and forth between brain and body; • origin of nerve tracts to body areas |
© Elizabeth Lee Vliet, M.D., 1995
Diagram 3.2
ANDROGEN AND ESTROGEN RECEPTORS IN THE BRAIN
ANDROGEN RECEPTORS IN THE BRAIN
Cortex
Thalamus
Preoptic Region
Hippocampus
Pituitary
Amygdala
Brain Stem
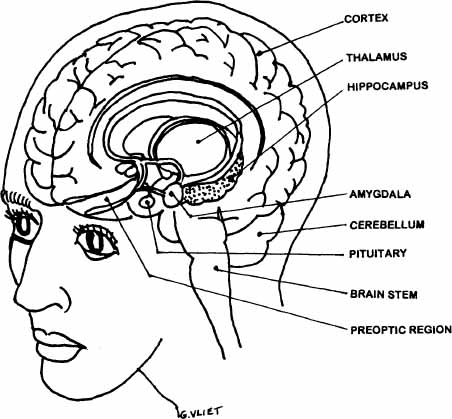
ESTROGEN RECEPTORS IN THE BRAIN:
Hippocampus (memory)
Pituitary
Amygdala (well-being, sexuality)
Cerebellum (balance, coordination)
Brain Stem: olive (synchronizes movements)
Cortex (higher cognitive functions)
© Elizabeth Lee Vliet, M.D., 1995, revised 2000
There has been an exponential growth in our understanding of the actual modes of communication between the brain and body since Dr. Candace Pert and Dr. Solomon Snyder first discovered the opiate receptor in the brain in 1973. This opiate receptor is the site where drugs such as morphine, heroin, and their derivatives plug into brain cells to produce their pain-relieving action. It seemed logical to these researchers that the brain would not be equipped with a special “lock” (receptor site) if it did not also produce a “key.” In 1975, they found the natural “key” for this “lock” in the discovery of the endorphin and enkephalin neuropeptides, the pain-killing molecules produced in the brain and body. Since that time, researchers have identified many more “molecular messengers” that provide the “courier information service” between the brain and various body sites. These biochemical information substances produced in the body have been grouped into various categories, including neurotransmitters, neuropeptides, hormones, growth factors, and lymphokines. They all have powerful effects on multiple aspects of body function, including mood and emotion. You can think of these informational molecules as “biochemical words” or messages used by the brain to “talk” directly to body cells and organs and by the body to “talk back” to the brain. These molecules link the brain and immune system, the endocrine and immune systems, the brain and the endocrine system, the brain and the gut, the brain and the heart, and so on throughout all the possible connections between brain centers and body organs.
Some of the most important chemical messengers I will be describing with regard to hormone influences on mood and physical symptoms are: serotonin (5-HT), norepinephrine (NE), dopamine (DA), acetylcholine (ACh), and gamma aminobutyric acid (GABA). These molecules function to convey and modulate information going back and forth between the brain and the body. They provide an important link between emotional and physical health. This link is not surprising in view of the critical role of emotions in regulating behavior that ultimately affects our very survival. These information-carrying substances are made in the brain and body from “building blocks” called amino acids found in the food we eat. The body’s metabolic processes to make the neurotransmitters require the presence of various vitamins and minerals as catalysts and cofactors for the synthesizing enzymes to work properly. Perhaps you are beginning to see why a healthy, balanced diet is so crucial to your good health and optimal function.
We are just beginning to discover the incredible diversity of roles and functions the neurotransmitters have. Serotonin research, for example, has given us extraordinary new insights about the biological basis of many behavior problems we previously thought were caused by psychological conflicts—everything from compulsive shoplifting to gambling, from compulsive sexual behaviors to hand-washing and hair-pulling (trichotillomania) behaviors. Overeating is mediated by serotonin imbalances, and so are pain and sleep patterns. Anxiety syndromes may be set off by changes in serotonin function, as well as by excessive production of norepinephrine. Mania results from excessive levels of norepinephrine and dopamine, while depression occurs when both of these and serotonin are either produced in inadequate amounts or the receptor sites are not functioning properly.
Major depression is a biological disorder occurring as a direct result of marked changes in these chemical messengers and an alteration in the receptor numbers and sensitivity—it is not a “character” problem or lack of willpower. Attention deficit disorders are also affected by the balance between serotonin and norepinephrine and affected by decline in estradiol and testosterone as women grow older. Abnormalities in dopamine production and function are thought to be the primary disturbances causing Schizophrenia and Parkinson’s Disease. Loss of acetylcholine, accentuated by loss of estradiol, is the primary deficiency leading to Alzheimer’s dementia. Irritable bowel syndrome and fibromyalgia are two of many so-called “vague” medical problems aggravated, if not caused by, serotonin and norepinephrine imbalances along with the loss of estradiol. As you can see, these deceptively simple molecules have a profound impact on many aspects of our health.
SUMMARY OF THE ROLES OF
TWO KEY NEUROTRANSMITTERS
 Increased Serotonin (ST, or 5HT)
Increased Serotonin (ST, or 5HT)
• diminishes anxiety
• lessens pain
• improves sleep
• diminishes depression
• decreases obsessions
 Increased Norepinephrine (NE)
Increased Norepinephrine (NE)
• diminishes depression
• worsens anxiety
• intensifies pain
• causes restless, fragmented sleep
• triggers palpitations
© Elizabeth Lee Vliet, M.D., 1995
Another fascinating connection that has been overlooked and under-appreciated in women’s health is the existence of specific estradiol, progesterone, and testosterone receptor sites in key areas throughout the brain and body. These hormone receptor sites are found throughout the body’s organs and tissues, far beyond reproductive organ sites you would expect to respond to circulating ovarian hormones. In the brain, the estrogen receptors in particular are heavily concentrated in the cortex and in the limbic system areas. As I described, the limbic system is the major center for regulating mood, memory, sleep, sex drive, appetite, and pain. There are multiple connections between the limbic system and all the other parts of the brain and spinal cord, which carries messages to all parts of the body. The rise and fall of estrogen alters serotonin, which affects pathways in the limbic system, which then produces changes in mood, sleep, memory, pain, appetite, and many other mind-body functions. Changes in hormone levels, in turn, affect the amount of neurotransmitters produced as well as the sensitivity of neurotransmitter receptors to the chemical messengers. No wonder changing hormone levels at puberty, in pregnancy, after delivery, and at menopause can produce such a wide variety of physical and emotional changes.
We have only begun to scratch the surface of appreciating how widespread these connections are. You may have been told that mood changes aren’t due to your hormones, but there is a great deal of science to explain the hormone connection. What you experience with menstrual mood changes is very real and has profound hormonal connections. Contrary to popular opinion, the brain and the body really are connected. It is not all in your head in the “imaginary” sense; it is “in your head” in the real physical changes that take place regularly between the hormone messengers and the brain’s own mood-altering messenger molecules.
It has long been observed in worldwide studies that both depressive syndromes and anxiety disorders are two to three times more common in women than in men. I think it is important to explore links between women’s hormone cycles and our expanded knowledge about mood-regulating mechanisms in humans. The cause of mood changes that occur around and during the menopausal transition or with the menstrual cycle luteal phase has been hotly debated in scientific journals and the lay media for a long time. There is a lot of intense emotion on both sides of the debate: Is it hormonal change? Is it the combination of life stresses? Consider this example from a nationally syndicated column by Jane Brody, published in September 1994. The headline in my newspaper was “Menopause Doesn’t Have to Be Depressing.” The article began this way:
In her newly published memoir, Barbara Bush reveals that in the mid-1970s she was overcome by depression so severe that she feared she might purposely end her life by crashing her car. The former first lady attributed her emotional distress to the hormonal changes of menopause compounded by the stress of her husband’s job as director of the Central Intelligence Agency. By linking her depression to menopause, Bush perpetuates a centuries-old belief that the hormonal swings that accompany this life stage can touch off what had long been called involutional melancholia (involutional is a term referring to the body’s changes at menopause).
Ms. Brody then goes on to say that “studies show there is no particular link between depression and menopause; if anything, it is far more common among younger women than in those from 45–55 when most women enter menopause.”
But in reality, we do not have adequate studies that have addressed this issue. None of the studies Ms. Brody referred to measured hormone levels, a fairly critical factor, if you are trying to see whether there’s a link between hormones and depressive symptoms! Most of these studies did not even determine whether a woman was still menstruating or whether she had undergone a hysterectomy. Many have based menopausal status on age alone, which you will find as you read further is not at all accurate in identifying which women are actually menopausal by endocrinological measures.
Under Barbara Bush’s picture is this quote (in large type and bold letters), which I think reflects even worse stereotypes of women and certainly is not based on well-done studies:
Barbara Bush had led a traditional family life with her major role being raising children. As her children left home, the loss of this role may have made her more vulnerable to depression at that time. When women are not in the work force, depression may be more common at menopause, reflecting the woman’s stage of life, not necessarily her hormones. (Myrna M. Weissman, Ph.D, as quoted in the nationally syndicated column by Jane Brody, September 27, 1994)
How does this quote make you feel? Is Dr. Weissman perpetuating the old stereotype that women “can’t cope” with life-stage changes and become depressed? I think this attitude perpetuates an appalling stigma, one that unfortunately continues today in the new millennium. I also think it is rather arrogant to suggest that women who are “in the work force” somehow cope better with menopause because they work. Any woman who is a full-time homemaker will tell you she has a full-time job, even if she isn’t paid for her labor.
Moreover, Dr. Weissman’s view still hasn’t been confirmed by sound research. Dr. Philip Sarrel of Yale has found the opposite: Women in the work force describe more severe symptoms of menopausal distress than women who do not work outside the home, perhaps related to the higher levels of stress experienced by women who are juggling multiple roles of home and career. Such stresses can further decrease ovarian hormone levels. Dr. Sarrel reported his research findings at the inaugural meeting of the North American Menopause Society in the fall of 1989, but most doctors still don’t take this seriously. Dr. Sarrel said,
Most important in impairing a woman’s capacity to function [at her optimal ability] in the workplace are symptoms due to hormone deficiency: sleep disturbance, hot flashes, anxiety attacks, depression, and altered [i.e., decreased] short-term memory. In approximately 67 percent of women who work outside of the home, and approximately 50 percent of homemakers, menopausal symptoms [such as above] have a moderate to severe effect on the ability to do work.
These observations have been borne out as we evaluate more women now going through the “perimenopausal” phase.
We are not facing our “mother’s” menopause. Women today lead much more complex lives and want a higher level of cognitive performance and energy level than our mothers commonly had. Women today experience greater demands than ever before—at work, at home, taking care of the extended family, taking care of home repairs—just look around Home Depot on a Saturday! More and more women are tackling multiple roles and jobs that used to be “men’s work” but then still have to carry out the traditional female roles as well. This is not to complain, it is to acknowledge that our lives are much more complex. The old pats on the back or standard treatments will not do and are not acceptable now. Our society demands we operate at a constant high-performance level; we also expect this of ourselves and find it devastating when we can’t.
As one woman so eloquently said it, “I survived the depression era, I raised six kids, my parents died when I was in my twenties. When I was 32, my husband was killed. I have had lots of stress in my life. Why did everyone say it’s ‘stress’ causing my sleep problems and irritability when I went through menopause? Relative to what I had already lived through, menopause was not a stressful time, but I certainly had a lot of bothersome symptoms.” Many women I see tell me that they feel validated in their own perceptions when I find low hormone levels contributing to their unpleasant symptoms.
Perhaps the hormonal changes, along with life stresses, were factors that aggravated Mrs. Bush’s symptoms around the time of her menopause. In addition to overlooking the reality of hormone effects on brain function, I do not think any of us should assume that Barbara Bush became depressed because her role as a mother had changed. This statement is made as if it were an established fact, but Dr. Weissman’s quote was not based on a confirmed causal connection. So, once again, a stereotype is perpetuated and possible physical factors are discounted. I think there are at least two possible endocrine causes for Mrs. Bush’s depression: her thyroid condition, a condition which has been recognized for 100 years or more to cause depression; and the changing ovarian hormone levels around the time of menopause that affect brain chemicals regulating mood. Instead of such an “either-or” mentality evident in the Brody article, why not approach these issues with a “both-and” mindset and look at all the interrelating factors that make women unique and contribute to the observed higher frequency of depressive symptoms and disorders in women?
If we look at the patterns of major depression, we have known for more than fifty years that there are several common predisposing factors (this is true worldwide):
• prior depressive episodes
• family history of depression
• female gender
• postpartum state
• severe, prolonged, or unanticipated stress
Two of the five factors that have been known for ages as predisposing factors to the medical (biological) illness of depression are directly related to being female: female gender, and the postpartum state. Since these patterns of female dominance have been noted in primitive and industrialized cultures, there must be some biological reasons for this. Why do we continue to stigmatize and blame women as being “weak” and “not coping well” because they have a higher frequency of depression? I find it hard to fathom why researchers and physicians haven’t made, or paid attention to, these hormonal connections long before now. Perhaps they don’t want to see them. Perhaps that’s a product of the concern expressed by many feminists that if we acknowledge the hormonal influences, we may lose some of the gains women have made to move into new occupational fields. I understand such fears. We have all suffered long enough from the stereotype of the bitchy, cranky, moody woman. But on the other hand, if we don’t acknowledge possible hormonal factors, we cannot develop the most effective therapies to help women who do have these problems. Such women will continue to suffer from lack of recognition or from overuse of other medication or surgery that may have more side effects or higher costs. I believe these are crucial issues that must be addressed.
A good example of profound hormone change is seen in the postpartum phase. A woman’s hormonal levels drop over a hundred-fold in the twenty-four to thirty-six hours after delivery. That’s a major adjustment for both the brain chemistry and the chemical messengers that regulate sleep and mood. Then add to that the fact that there is now an infant who’s keeping you up much of the night, so you’re not sleeping very well. Sleep deprivation is also known to cause biological depression. But a woman who becomes significantly depressed following her baby’s birth is still more likely to be told she has psychological conflicts about being a mother. The biological factors are overlooked. There are social and cultural factors involved, and these have been studied exhaustively. But I think we have not paid enough attention to the obvious hormonal changes, especially postpartum, that have to do with the biology of being female and may profoundly disrupt mood-regulating chemical messengers in the brain. In Europe, and in my own practice, there are good reports of the positive response to estradiol therapy after delivery in women who have a postpartum depression due to hormonal decreases. Dr. John Studd from England has published studies of successful use of transdermal 17-beta estradiol patches to treat postpartum depression. Many of these women then did not need antidepressant medication. If the postpartum depression is severe, some women benefit from the combination of estradiol and a serotonin-augmenting antidepressant. We need to be more open-minded to individualization of the best options for a given woman.
I have long been struck by the repetitive, commonly occurring pattern of mood changes and physical symptoms and their relation to the normal changes in estrogen and progesterone levels throughout the menstrual cycle. Most women who have menstrual periods (or ovarian cycles if they have had a hysterectomy) have some physical or emotional cues that tell them that their periods are about to begin. Women also experience changes that signal the beginning of the midlife transition, or climacteric. In my medical practice, I have found a significant percentage of patients who have luteal-phase PMS symptoms severe enough to interfere with optimal function at home, at work, and in relationships. These women would like to at least have someone check their hormone levels and offer some constructive, well-thought-out options to help them feel better on these days. I don’t think that is too much to ask of a health system that can now achieve successful organ transplants, develop Viagra to enhance men’s erections, clone sheep, and other wonders.
Even when women have had a hysterectomy, many who still have their ovaries can describe quite well the body-brain markers of the residual ovary cycle. They tell me they have breast tenderness, bloating, food cravings, constipation, and other markers, just like they used to the week before their menses began. Or they will describe a few days of restless, fragmented sleep, emotional changes, crying easily, loss of energy, feeling mentally “foggy,” or having anxiety attacks and palpitations like they did the first few days of bleeding (when estradiol is at its lowest point of the cycle). Yet they are often told they “couldn’t possibly” have PMS. I think many physicians forget the ovaries still cycle and produce these changes. Another cause of these changes is the fact that ovaries decline sooner after hysterectomy due to interruption in ovarian blood flow when arteries are tied off in order to remove the uterus. Many women, and doctors, don’t know this.
It has been my hypothesis from years of observing patients, listening to the ways women describe their experiences, and studying the extensive science of hormone effects on brain function, that there is an unrecognized and unaddressed connection between declining estrogen levels in women and the pattern of female dominance in depression and anxiety disorders. Consider these observations (based on women who still have regular menstrual cycles):
• PMS symptoms commonly become worse in the late thirties and early forties.
• The late thirties to early forties represent the peak age range of new onset depression and anxiety syndromes in women, but not in men.
• The late thirties to mid-forties is the time frame for onset of erratic and declining ovarian hormone production, creating the potential for adverse effects on brain neurotransmitters to destabilize mood-regulating mechanisms.
• By the time menses have stopped at menopause, hormone levels are “even” at a new lower level, and no longer cycle, making mood swings less likely.
• Researchers, however, have focused only on the time of menopause in trying to correlate hormone changes and depression.
• In most studies of depression around menopause, hormone levels are not measured.
I think a key factor in the connection between hormones and mood effects is the degree of fluctuation, or rate of change, in hormone levels. In all the studies I have reviewed, this crucial factor has not been addressed. I have studied this connection by measuring hormone levels at times in the menstrual cycle when women describe their most distressing mood symptoms, and at times in the cycle when estradiol is at its lowest point and its highest point. Then I “connect the dots” to see the pattern that emerges as I show the symptom clusters side by side with the actual hormone results. It has been striking to find that approximately 85 percent or more of these women in their mid thirties and early forties who described “worsening PMS” had below normal estradiol levels at these points during their menstrual cycle.
The prematurely low estradiol levels were even more likely to be present in women who had experienced a surgical procedure that affected blood flow to the ovaries, such as tubal ligation or hysterectomy (even when the ovaries were left in place). According to the currently accepted age-based definitions, these women were too young in most cases to be considered pre- or perimenopausal. When I measured the hormone levels, however, I confirmed that they indeed had reached the endocrinological stage of perimenopause. I offered these women treatment with low-dose estrogen supplementation to optimize their estrogen levels instead of using antidepressants. I have been astonished at the results. Women who fit this profile described a consistent pattern of improved mood, diminished irritability, improved sleep, improved libido, improved energy level, and diminished mood swings prior to their periods, after starting on a low dose of natural human estradiol. Only a few of these women required the addition of antidepressants once hormone levels were returned to the usual optimal levels for a menstruating woman. (See menstrual cycle diagram in chapter 2 for desirable ranges.)
A variety of studies in recent years has demonstrated that neuroreceptors respond to circulating hormones of all kinds, including the sex hormones estradiol, progesterone, and testosterone. Researchers have shown that hormones can increase or decrease the release of neurotransmitters. Hormones have both presynaptic and postsynaptic nerve cell actions, as well as indirect influences that modify the function of neurons. Both the brain (central) and the body (peripheral) nervous systems have cells with receptor sites sensitive to 17-beta estradiol, progesterone, and testosterone. The brain clearly responds to the withdrawal and absence of these ovarian hormones. There are a wide variety of physical phenomena and psychological effects of decrease or withdrawal of the ovarian hormones, and I discuss these connections in the next sections, as well as in chapters 4–7. But first, I think it is important to clarify some descriptions of terms you will see in various articles, which may be one of the reasons there is so much confusion about hormone effects on mood.
As you read the upcoming sections, it is important to keep in mind the difference between (1) experiencing symptoms on an episodic or cyclic basis with your menstrual periods and (2) having sustained physical and emotional changes that would be severe enough to be considered a disorder or an illness. Many women have mild to moderate symptoms or experience mood, sleep, and energy-level changes around the time of hormonal changes or in conjunction with situations that are stressful. When I talk about this cyclic type of pattern, I am not referring to the illness of major depression, which indicates a more severe, debilitating degree of depression. The same is true with anxiety. The term anxiety may be used in many different ways, so it is important to know how it is being used in a given context. Some people use it to mean a mood: “I’m in an anxious mood now,” or “I’m feeling anxious.” Others use it to mean a characteristic or trait of a person—“He’s always been anxious and uptight.” It may mean a brief symptom: “I had an attack of anxiety over my bounced check.” It may be used to mean a sustained pattern of physical and emotional changes that we call generalized anxiety disorder. In these chapters on hormone connections, I am generally referring to fairly short-lived, episodic anxiety symptoms that occur in relation to changes in physiological variables such as levels of glucose, thyroid hormone, estrogen, testosterone, and progesterone.
As a global observation, I have not found the hormone shifts of the menstrual cycle to be a primary cause of the psychiatric syndrome generalized anxiety disorder, since this illness typically is present on an almost daily basis. On the other hand, I do commonly see women who have panic attacks only around the menstrual-cycle phase of dropping estrogen and progesterone levels. I think this pattern of menstrually-related panic attacks is different from the psychiatric syndrome we call panic disorder. The cluster of symptoms (I sometimes use the nonmedical, descriptive word phenomena instead of symptoms) is often the same because the same brain-body pathways are involved. In my view, the pattern of a particular symptom cluster provides the most important clues to contributing causes. I certainly am not saying that all women who experience premenstrual depressed moods or feelings of anxiety are suffering from a psychiatric disorder. Quite the contrary. I think far too many women are given a psychiatric diagnosis and psychotropic medication, without the realization that the “symptoms” are occurring around the menstrual period and may be triggered by hormonal changes.
There still have not yet been good systematic, prospective studies of the effect of rate of change in estrogen levels on the frequency and severity of mood symptoms in perimenopausal women. We have known for a long time, however, that estrogen does affect many brain-mediated phenomena. Experimental data indicate that the sex hormones (estradiol, testosterone, progesterone) are the most potent body-generated chemical signals affecting nerve cell activities in the brain. All three major sex hormones alter the electrical and chemical features of cells in the central nervous system (CNS), especially in the hypothalamus and limbic system—areas that regulate key functions like sleep, mood, memory, pain, sex drive, appetite, weight, temperature, and thirst. Changes in levels of estrogen and progesterone have been shown to influence multiple brain-chemical messengers: dopamine, norepinephrine, acetylcholine, and serotonin, all of which are powerful modulators of mood.
Dr. Malcolm Whitehead and his associates did an excellent study that showed marked improvement in memory, anxiety, and irritability in menopausal women taking estrogen, compared with menopausal women not taking estrogen. This information isn’t exactly hot off the presses; it was published in the British medical literature in 1977. So we’ve had this kind of information in the medical literature for a long time; it has just been ignored. Women tell me every day that they have been told categorically by their doctors: “Hormones don’t affect mood. Your memory changes aren’t due to hormones. It’s just stress. See a therapist and learn to relax.”
Since the 1950s at least, a number of clinical reports have indicated that estrogen supplementation helps alleviate mood swings and depression as well as the physical symptoms such as hot flashes, headaches, insomnia, and memory disturbance associated with the midlife phase. Most have been dismissed because they were not double-blind, placebo-controlled studies. Instead of ignoring these important findings, researchers should have been using those early studies as guides for well-designed double-blind studies. With the development of the first modern psychotropic drugs in 1954, however, the brain effects of all kinds of hormonal influences have been forgotten and overlooked as the focus shifted to using antidepressants, antianxiety agents, neuroleptics, and sedatives. With exciting new information from neuroscience research in the past decade, and with the use of more refined diagnostic criteria rating scales to systematically assess mood characteristics, there is increasing measurable evidence that mood symptoms and physical reactions described by perimenopausal women are related to their hormone changes and may respond to supplemental estrogen even before menses stop.
Dr. Sarrel of Yale said in 1989 at the NAMS meeting that “estrogen addition over a six-month period appeared to relieve sleep disturbance most significantly, and resulted in a marked improvement in all categories of perimenopausal symptoms in 40 percent of women.” He went on to say that it was “of concern that women don’t realize how much their quality of life may be improved with proper estrogen therapy and that only 15 percent of all menopausal women received hormone therapy at all. Many women simply do not seek medical help, even though hormonal therapy may be a benefit to them.” Bruce McEwen, Ph.D., at Rockefeller University, has done extensive basic science research on brain-hormone connections and has found that estradiol, testosterone, and progesterone affect the brain directly, acting at specific hormone receptors unique for each hormone. These receptors are concentrated in areas of the brain that are highly hormone-sensitive and dense with receptor sites: the hypothalamus, limbic system, cortex, prefrontal regions and others. Current research indicates that progesterone and testosterone brain receptors in women must first be “primed” by estrogen in order to work properly.
Dr. McEwen and other scientists have shown that hormone effects on the brain can be gradual and long lasting, that is, on the order of hours, days, or even weeks in some cases; or may be rapid onset and shorter duration of effect. The rapid hormone effects typically occur at the cell membrane receptor, while the longer-lasting effects occur at the cell nucleus receptor. All of these observations have many profound implications for an interactive model of thinking about the role of women’s ovarian hormone cycles producing psychological phenomena such as mood changes. The brain mechanisms and pathways already exist. We need to put the pieces of the puzzle together to see the complete picture. The problem is that women’s health has some pieces left in the “box” of gynecology, and some pieces left in the “box” belonging to psychiatry, and they don’t get put together by separate specialists working on different body parts.
Acting at their specific receptor sites, hormones influence the production, release, and breakdown of the mood-regulating neurotransmitters. Antidepressants and antianxiety medications are also given to influence these same neurotransmitters to lift or stabilize moods. The ability of these medications to work optimally appear to be affected by circulating hormones, especially estradiol and progesterone. Dr. Kendall and coworkers found that the presence of estrogen increased the binding of the antidepressant drug imipramine (Tofranil) to serotonin-2 receptors involved in mood. In animals, this imipramine-receptor-binding effect was abolished if the ovaries were not present and was reestablished by giving estrogen. Many case reports describe similar changes in antidepressant response based on a woman’s phase in her menstrual cycle.
Early in my career, as I listened to women describe side effects with antidepressants, I found that I frequently needed to make dosage adjustments depending on menstrual cycle phase. Women often needed higher doses in the progesterone-dominated luteal phase and lower doses in the estrogen-dominated follicular phase. I never saw anything about this in the medical literature until 1993, but my patients taught me what they needed and I usually gave different doses depending on phase of menstrual cycle. This fits with what we know about estradiol having its own antidepressant effects on the brain centers, so less additional medication is needed when estradiol levels are high. Progesterone, on the other hand, has more of a “dampening-down,” a sedative, or (for some women) a depressant effect on mood-regulating neurotransmitters. Progesterone also decreases receptor binding of both estradiol and testosterone. Thus, when progesterone levels are high in the second half of the cycle, it is reasonable that more antidepressant medication may be necessary.
Ovarian hormones also have been found to have effects on several other mood-altering neuropeptides: endorphins (“morphine within” pain-reducing chemicals), oxytocin, vasopressin, and prolactin, which are involved in modulating memory, motor coordination, and a variety of behaviors. Studies have demonstrated a decrease in some serotonin measures (either plasma-free tryptophan or platelet serotonin) in the menopausal and perimenopausal years that correlates with the age of peak suicide rate for women (a comparable peak has not been seen in men). Recent studies have found that brain levels of 5-hydroxyindoleacetic acid (5-HIAA), a serotonin breakdown product, are low in patients who attempted or completed suicide. If 5-HIAA is low, it indicates that brain serotonin levels are also low. Decreases in serotonin production and increases in serotonin breakdown are seen in (1) the human aging process, (2) as an effect of declining estrogen in women, and (3) as an effect of prolonged stress, chronic alcohol overuse, and cigarette smoking. Numerous worldwide studies over the past two decades have shown that reduced serotonin levels are a primary cause of depressed mood, increased irritability, increased generalized anxiety, increased pain sensitivity, eating disorders, obsessive-compulsive disorders and disruption of normal sleep cycles.
If you then add the factor that declining estrogen also decreases serotonin, the symptoms of PMS, postpartum, perimenopause, and menopause make even more sense physiologically. Many factors affect serotonin balance, but the loss of estrogen may be a key gender difference that contributes to a greater susceptibility to depression and suicide in women. Along this line, investigators from several countries have a greater incidence of psychological symptoms (irritability, mood swings, etc.) in women aged forty to forty nine, when estrogen is decreasing most rapidly, compared with both younger and older women. You aren’t a hypochondriac. Your body is changing. Much later, after all the “ups and downs” of hormone change, women reach a new balance point with overall lower hormone levels, less estradiol, and more estrone. But while the changes are occurring, some women tell me they feel like they are on an emotional roller coaster. Most of us don’t like to feel so out of control, and these feelings are compounded when doctors do not explain what is happening to us.
Such mood changes, which are clearly cyclic and related to the menstrual cycle, often respond better to natural human 17-beta estradiol than to antidepressant or antianxiety medication because the addition of estradiol actually normalizes the body chemicals that are out of balance. A number of clinical studies that monitored psychological measures along with physical changes in perimenopausal and early menopausal women have found that giving estrogen does result in marked improvement in women’s sense of well-being, energy, clarity of thinking, short-term memory, and quality of sleep. At the same time, women report marked decreases in hot flashes, vaginal dryness, and other typical physical symptoms. I have certainly seen these kinds of dramatic improvements in the women I have treated for these problems over the past twenty years. In addition to the open clinical studies, such as the work I have been doing, recently published randomized double-blind placebo-controlled studies have also shown that estrogen therapy effectively improves general well-being, reduces the frequency of hot flashes, and objectively improves the quality of sleep as defined by increases in length of rapid-eye-movement (REM) sleep and total sleep time.
Changes in endorphins have also been shown to play a role in premenstrual and postpartum mood disorders, particularly the anxious-agitated depressive subtypes. Estrogen has an effect on levels of endorphins: High levels of endorphins occur in the late stage of pregnancy when estrogen levels are at their peak. At delivery, when the sharp drop in both estrogen and progesterone happens, there is a rapid decline in endorphin levels. The withdrawal of endorphins produces effects similar to withdrawal from heroin or morphine: irritability, tearfulness, anxiety, stomach upset, diarrhea, and sweating. I think it is reasonable to think that declining levels of estrogen associated with either postpartum, perimenopause, or menopause can cause reductions in endorphin levels and thereby play a contributing, if not a causative, role in the onset of the anxiety, depressive, and pain symptoms described by women in these phases.
To summarize: Estradiol has multiple effects on the brain that collectively act in ways similar to antidepressants, memory enhancers, and nerve growth factors. Overall, these pharmacologic effects of estrogen on the nervous system fit well with current theories of antidepressant actions and the action of potent nervous-system-regulating molecules. It has always made sense to me that changes in any aspects of body chemistry, especially changes in such potent chemical messengers as hormones and neurotransmitters, might first be evidenced by changes in brain-mediated phenomena such as irritability, depression, anxiety, and sleep. These are symptoms women notice first, earlier in the climacteric, I think because the brain is so exquisitely sensitive to small changes in its biochemical balance and to alterations in the interactions of the various neurotransmitter systems. It is not an either-or split between psychological and biological. Both have to be seen as operating together in an integrated manner. There is much more to come in our understanding of this key female hormone, but it is clear that estrogen plays a major role in maintaining our sense of well-being, vitality, and zest.
ESTRADIOL EFFECTS ON THE BRAIN
• enhances CNS availability of norepinephrine and dopamine
• increases production and/or prolongs action of serotonin
• regulates sleep centers
• regulates body temperature, vasomotor tone
• improves pain tolerance, (raises pain threshold)
• inhibits the monoamine oxidase (MAO) enzymes that break down serotonin, dopamine, and NE (prolongs mood-lifting action of these chemical messengers)
• increases production of the enzyme needed to make acetylcholine, a crucial memory-enhancing neurotransmitter
• prolongs neuronal responses to excitatory amino acids in the cerebral cortex, cerebellum, hippocampus, hypothalamus, midbrain, and pons
• acts directly on glutamate receptor binding and inactivation
• enhances attention and concentration mechanisms
• increases sensory perception for fine touch, olfactory, and visual stimuli
• increases dendrite connections between nerve cells in memory centers
• has effects that alter seizure threshold, dependent upon type of seizure
© Elizabeth Lee Vliet, M.D., 1995, revised 2000
You hit age thirty-nine, have been in good health, maybe you exercise three or four times a week, and wham! All of a sudden you start having horrendous palpitations and pounding sensations as if your heart were going to literally jump out of your chest. Maybe you start feeling anxious; your stomach is a little upset; your skin is clammy. “What’s going on? This can’t be me? I’m healthy, and I never had these problems before. What is happening? I must be having a panic attack. Maybe I’m having a heart attack. No, that can’t be; I’m too young. What is this? I’d better see the doctor.” So you see your family doctor, who checks you over and says you’re fine, but you need to relax more and reduce your stress. With a deep sigh of relief, you leave and go on about your daily routine. Then, a few weeks later, it happens again. What is this?
If you have been checked out and do not have heart disease or thyroid problems or another medical condition that can trigger such episodes, it may be due to ovarian hormone changes. Have you noticed where in the menstrual cycle these palpitations or panicky episodes occur? You might find it helpful to keep track of this pattern. If your physical symptoms (heart flutters, heart racing or pounding, feeling queasy or nauseous, sweating, feeling anxious for no apparent reason) come right after ovulation, a day or so before your period starts, or the first two or three days of bleeding, you may be experiencing one of the brain effects of dropping estrogen levels. I can hear you saying to yourself as you read this, “How does estrogen affect the brain to cause heart symptoms?” Well, by some of those chemical messenger molecules I was just talking about. A drop in blood levels of estrogen affects the brain in several ways. Take a look at the following sequence of events:
Decreased estradiol (ovary) ——> Decreased estradiol (at the brain) ———> decreased brain endorphins ———> burst of brain adrenaline (increased norepinephrine—NE) ——> brain-body responses to the stimulation from norepinephrine: increased heart rate, palpitations, rise in blood pressure, being awakened suddenly from sleep, dilation of body blood vessels triggering the “hot flash,” sweating, “butterflies” in the stomach, diarrhea, headaches.
Diagram 3.3—BRAIN-BODY EFFECTS OF ESTRADIOL DECREASE
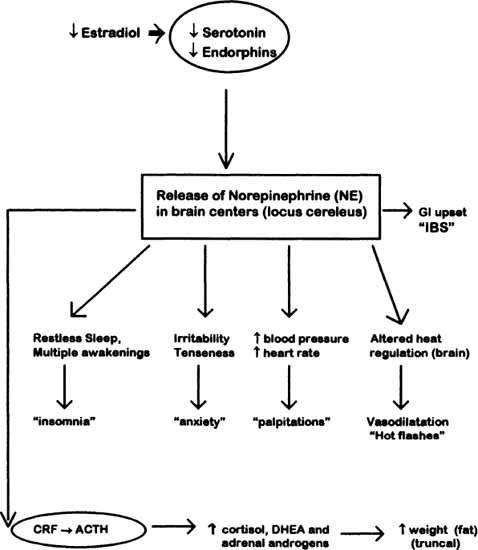
© Elizabeth Lee Vliet, M.D., 1990, revised 1995
So there you are, a whole cascade of events spreading over the body from a direct hormone-triggered release of brain chemicals. Remember that endorphins are the body’s natural painkillers and mood regulators, so you see how psychological (brain) symptoms can be related to the physical hormonal drop. This is such a common occurrence, many women don’t even notice it until the hormone drops become greater during perimenopause. As estrogen production declines, a fall in estrogen before menses triggers a much more pronounced physical response. Most doctors have not been taught these hormone-brain-body connections, so they don’t realize these are clues to hormone shifts for women. Women tell me they know “its a physical, chemical kind of thing,” and they are correct.
In fact it wasn’t until the late 1970s that doctors accepted scientific proof that women’s hot flashes were a real physical phenomenon. They had been assumed to be psychological and a figment of the woman’s imagination. The surging hormones prior to menopause trigger pulses of LH and drops in estradiol that fire off norepinephrine (NE) in the limbic system, and this burst of NE disrupts the normal function of the heat-regulating center in the hypothalamus. The thermoregulatory center then sends its chemical messengers to the arteries, dilating them to allow excess heat to dissipate. The dilation is accompanied by sweating, body temperature begins to drop, and you feel a chilly sensation sweeping over you. If it happens at night, this whole sequence wakes you up each time it happens, and you are often soaked in sweat.
When estrogen is dropping, it triggers a decrease in serotonin. Since serotonin helps maintain sleep and decrease anxiety, a drop in serotonin adds to the episodes of awakenings at night, and aggravates the adrenaline-induced feelings of irritability, tension, palpitations, and chest discomfort. It is important to have palpitations and chest discomfort evaluated and the possibility of heart disease ruled out. It is also important that we look at changing hormone levels as contributing factors and not immediately jump to the conclusion that it’s just psychological stress.
Situational and psychological stress obviously makes all this worse by further suppressing ovarian function along with its many other effects on the body. I will discuss the stress-induced connections in greater detail in upcoming chapters. A lot of the mood swings women experience are not due only to external stresses; mood swings also result from the interaction of external stresses and our internal body hormonal changes. These are also stressors requiring the body to change and adapt. So, when you experience heart flutters and palpitations, keep in mind that it’s not all in your imagination or just due to anxiety, it can also be your hormones changing.
With all the headlines talking about progesterone as a “wonder hormone” to prevent osteoporosis and solve all of women’s problems, I think it’s time to clarify what we know about this hormone. I will elaborate on this further in chapter 4 and just focus on brain effects here. Some of the promoters of the natural “wild yam” progesterone cream have got it backward as to which hormone does what in the female body—but then most of these promoters are men, who don’t live with our body experiences every month.
Many women have told me over the years that they become depressed when they take progesterone or use the “wild yam”–progesterone creams. This is to be expected due to progesterone’s effects on the brain, since several metabolic breakdown products of the natural human progesterone molecule are very potent depressants of brain (CNS) function. One of the metabolites of progesterone (3-alpha-OH-DHP) has been found to be about eight times more potent as a CNS depressant producing antianxiety, sedative effects than the most potent barbiturate known today, methohexital. Studies looking at the anticonvulsant actions of 3-alpha-OH-DHP have found it to be more potent than clonazepam (Klonopin), a high-potency benzodiazepine used for epilepsy and panic disorder. Depressed mood occurring with progesterone is similar to the depressant effects some women have when taking Klonopin or Valium.
The neuroendocrine studies that have identified these progesterone metabolic products and their effects at brain receptors go back several decades, but much of this literature has not made its way into general clinical settings, particularly in the fields of psychiatry and gynecology. The progesterone metabolites above actually attach to GABA receptors, the same ones that bind the benzodiazepine drugs (Klonopin, Valium, Xanax, Ativan, and others in this group of medications). At higher levels, progesterone actually acts very much like these antianxiety medications by attaching to the GABA receptor sites and causing release of the inhibitory neurotransmitter GABA, just like Klonopin, Valium, and the others in this group of medicines do. Inhibitory action at the GABA receptor complex causes decreased anxiety, a decrease in seizures, increased sedation, delay in word recall and verbal responses, and potential increase in depression. The depressant effects seem to occur at higher doses than are needed for antianxiety effects, again similar to the type of effects we see with benzodiazepines. The depressant effects of progesterone are now thought to primarily occur from one of its metabolites, 3-alpha, 5-alpha-THP or allopregnanolone. Levels of allopregnanolone have been shown to correlate well with circulating levels of progesterone in the bloodstream.
An interesting observation in several studies is that progesterone given to either men or women produces effects like Valium (and others in the benzodiazepines) on such measurable variables as heart rate, blood pressure, respiratory rate, and the electrocardiogram patterns. It also causes quite pronounced daytime sleepiness for many, male or female. The flip side of this effect is that progesterone produces withdrawal effects similar to other medications that act at the GABA receptor, such as benzodiazepines and barbiturates. This effect has been shown in men and women. This withdrawal syndrome includes increased anxiety, restlessness, insomnia, tearfulness, among other effects.
The binding of progesterone metabolites to the GABA receptor complex appears to be one of the primary reasons that high doses of progesterone help decrease anxiety in some women with severe PMS. The doses typically used for PMS treatment may run anywhere from 400–1600 mg a day and produce blood levels actually higher than the levels of progesterone seen in the third trimester of pregnancy. Such high doses are actually providing a pharmacologic effect on the brain, similar to benzodiazepine medicines, rather than a physiologic one mimicking the levels and functions of a normal menstrual cycle. At these higher doses, the anxiety-relieving metabolites of progesterone are found to be depressogenic, much like what happens to some people when taking higher doses of Valium or Ativan over a period of time. The brain actions are essentially the same, so in susceptible women, using progesterone may initially relieve anxiety, but then over time, it can make depressed, dysphoric moods worse. There is clearly a lot of additional information we need about the varied brain effects of progesterone before any responsible physician should suggest that women buy over-the-counter progesterone creams to use on a daily basis.
Progesterone has some other rather interesting effects on the brain. It has been found to act as an antiestrogen (similar to Tamoxifen) to reduce estrogen binding at brain receptors and to also decrease testosterone effects by several mechanisms, including a down-regulation or “dampening” of estradiol and testosterone receptor activity in the brain, so that it offsets some of the usual mood-lifting effects of both estradiol and testosterone. Progesterone also increases the flow of calcium ions into nerve cells, decreasing the release of important chemical messengers (neurotransmitters) that boost mood. This is yet another way that progesterone and its metabolic breakdown products may trigger depressed mood, especially if a woman has a history of depression.
If you started using one of the progesterone creams and are wondering what happened to your sex drive, it turns out that progesterone also competes with testosterone for uptake from the blood into the brain and decreases the conversion of testosterone into its most active form. In fact, progesterone is sometimes described as one of the most potent naturally occurring antagonists of androgens. Progesterone competes with testosterone and other androgens at the receptor sites in androgen-dependent tissues and prevents these target tissues from overly responding to the androgens present in women. This reduction in the amount of active testosterone at the brain has the result of further decreasing sexual interest (libido), particularly if estrogen levels are also low. In addition, both estradiol and testosterone have mood-elevating effects, so when progesterone diminishes the binding of estradiol and testosterone at brain receptors, it’s not surprising that you may notice your mood is grumpy, irritable, tearful, and depressed.
Women who experience PMS, and those who have FMS that is worse in the second half of the menstrual cycle typically say that their mood and pain become progressively worse from right after ovulation through the first few days of bleeding, which tracks with the time that progesterone rises in the second half of the menstrual cycle. Irritable, depressed mood and increased pain is especially common if estradiol levels are lower than normal at the same time that progesterone is rising. While some women find the “calming” effects of progesterone pleasant, other women really are uncomfortable and “out-of-sorts” with the depression-producing effects of progesterone. The irritable dysphoric mood effects of progesterone and progestins have also been widely observed in menopausal women on HRT, who report feeling very well on the estrogen-only phase of hormones but then become lethargic, bloated, irritable, “PMSy,” depressed, and miserable during the days when progesterone or progestin is added.
If you have begun using a wild yam or progesterone cream and experience weight gain; an increase in FMS or bladder-vulvar pain; or a decrease in energy, sex drive, or mood, you may feel better by stopping the progesterone product. Have your hormone levels checked by a reliable method (not just saliva tests) to see what hormones may actually be low, and what you may need supplemented to restore your body to optimal levels. We once again come back to the importance of a healthy balance of the ovarian hormones Mother Nature provided us. There’s no quick fix, no magic bullet, and rarely is anything going to give us 100 percent positive effects, without the possibility for some offsetting negatives.
Studies of progesterone have also shown that it decreases the brain’s production of human growth hormone, GH. This is a desirable effect in late pregnancy to help the baby not grow too large to be born, but it is an undesirable effect in non pregnant women, especially those with FMS who need GH effects for normal muscle repair. This effect of progesterone was also demonstrated to occur in non-pregnant women in excellent medical studies from several centers (Frantz, 1965; Mintz, 1968; Tyson, 1969; Yen, 1967), published in the 1960s. Suppression of growth hormone by progesterone was shown to occur if the amount of progesterone given resulted in blood levels similar to late pregnancy. So what is the daily dose of progesterone that it takes to do that? Bhatia and colleagues at the Medical College of Wisconsin addressed this question in a 1972 study. They found that a daily oral dose of 300–400 mg of progesterone given to healthy nonpregnant women caused a significant blunting of GH concentrations in all patients, as well as produced the unwanted effect of significant rises in insulin levels and an exaggerated (abnormal) response of insulin to oral glucose. The rising levels of insulin also caused further decrease in GH release. The hypothesis was that progesterone decreased plasma levels of GH by a suppressant effect on the central nervous system, rather than by direct action on the pituitary cells that synthesize it.
Another critical point regarding progesterone effects on growth hormone is the duration of higher progesterone levels. Women in the Bhatia study were only given progesterone for slightly less than one week, but I routinely see patients that have been using it for months to years. The cumulative negative effects can be severe. Similar suppressive effects on GH secretion were also found for the synthetic progestin, medroxyprogesterone acetate (Provera and other brands) by Simon (1967), Lawrence (1970), and Malarkey (1971). The broad suppressive effects of progesterone (and progestins derived from it) on pituitary gonadotropin, ACTH, and GH release suggest that progesterone produced by the placenta is one of the major ways the pregnant body shifts its endocrine “manager” from pituitary control to control by the placenta as the baby grows. Such a shift helps to ensure that the mother’s body will change appropriately to nourish the growing baby.
I think it is important to point out that the decrease in GH from progesterone was demonstrated with doses of progesterone lower than amounts being recommended today by some practitioners for PMS treatment and relief of menopause symptoms. Typical doses of progesterone used for PMS are often suggested as 400 mg to 1600 mg a day. And keep in mind, that this study used oral doses. If you use a non oral delivery, such as cream or suppository, the dose is supposed to be decreased to about 10 percent of the oral dose due to better absorption of the non-oral forms. This means that a 100 mg dose for oral use should be decreased to 10 mg per gram of cream, since the cream bypasses the liver when it is absorbed directly into the bloodstream through the skin. Yet, I have frequently had patients come in to my office using progesterone creams that are marked on the container 100 mg/gm, about ten times the recommended amount. No wonder they feel so bad!
In addition to incorrect dosages for prescription creams, many of the currently available over-the-counter “wild yam” and progesterone cream products deliver amounts of progesterone in excess of those in the Bhatia study. While this is not a complete list, some examples of progesterone-containing creams with greater than 400 mg/oz are Angel Care, DermaGest, EssPro7, Fair Lady, Fem Crème, FemGest, GreenPastures, Progestacare, ProGest, Today’s Man, YamCon (Pro) Extra (reference: PIC Analysis, Aeron Laboratories).
Based on my analysis of decades of medical literature summarizing the adverse metabolic consequences I describe, my medical opinion is that the concentration of progesterone in these products is far in excess of what is safe or reasonable for daily use. The extensive data on adverse effects of progesterone on major metabolic functions of the body, including growth hormone production, seems to be ignored by those who are advocating the regular daily use of supplemental progesterone in body creams and other forms, particularly since over-the-counter ones vary so greatly in the amount of progesterone added. If you are using an over-the-counter progesterone or wild yam product, please talk with your doctor and have the important lab tests I discuss in upcoming chapters.
In chapter 6, you will read how testosterone is crucial for normal sex drive in women, since it activates the brain “sexual circuits” in both women and men. For now, I just want to emphasize that it is another hormone produced by the ovary that helps to improve a woman’s sense of well-being, energy level, and stimulates normal bone growth and muscle development. We know that a certain level of estradiol (estrogen) must be present in our brain areas in order for testosterone to function properly. It is now thought that the brain testosterone receptor is created by the presence of estradiol. Without enough estrogen to “prime the pump” so to speak, testosterone produced by the ovary cannot attach properly in brain centers to stimulate sexual arousal for women. So your level of estradiol also plays a role in how well your body’s testosterone can work. When I have explained this biology to women and their partners, it has helped improve many hurts in relationships where the partner thought she was no longer attracted to him.
As another illustration of the connection between estradiol and testosterone, we have seen in women who have had breast cancer and cannot take estrogen, that providing supplemental testosterone may only partially improve their sexual desire and ability to have an orgasm. The important role of “estrogen-priming” for optimal testosterone response may explain these clinical observations. Other studies have demonstrated a mood-lifting or antidepressant effect of testosterone, which many women in my center also describe after testosterone therapy is added to their program. It is rewarding to me to hear my patients describe how they feel after taking natural testosterone, when they have typically experienced low testosterone levels for quite a long time: “GOSH, I FEEL LIKE MY OLD SELF AGAIN. I have my energy back. I’M INTERESTED IN SEX AGAIN. I have my get-up-and-go feelings.” Using natural testosterone at doses designed for women, it is uncommon that I see unwanted side effects. I will describe in chapter 6 the different types of testosterone available and how I use blood levels and women’s descriptions to find the right amount for a given person.
For centuries, medical observation has written about the connection between reproductive hormones and changes in mood and behavior, but these observations have been largely dismissed due to problems in methods, lack of “adequate” biological evidence, and lack of the necessary interdisciplinary studies. Recent developments in the study of the endocrine system and brain function have certainly shed light on the ways that changes in hormones through the menstrual cycle may contribute to perimenopausal mood disorders and symptoms. Mood disorders and milder mood-change symptoms are a significant source of distress to many women in the perimenopausal years; yet, they often fall between the cracks in our fragmented health care system.
The model I have developed for HER Place: Health Enhancement and Renewal for Women Centers in Tucson and Dallas–Ft. Worth are examples of the integrated approach we crucially need for women’s health care services, as well as educational and research paradigms. Now we need to view hormonal effects on mood from a similarly integrated perspective. We need to focus on the internal biological factors, such as hormones, that interact with external events to increase the likelihood of exaggerated or abnormal responses to normal hormonal changes. Areas of future research need to also include evaluation of the
• Possibility that different types of estrogens, progestins, and testosterone, as well as different doses, have very different effects on the brain, especially mood, sleep, and pain pathways;
• Mood effects of estrogen and progesterone in women who have never had previous depression;
• Effect of different hormone preparations in women who have a history of hormone-related depressions;
• Effects of different types of estrogens, testosterone, and progestins in various subtypes of depressed patients (unipolar, bipolar, those with normal estradiol levels, those with proven low estradiol levels, etc.);
• Differential effects of brief and ongoing estrogen use along with how it is taken;
• Prospective evaluation of estrogen and testosterone roles as an augmentation approach as traditional antidepressant medications;
• Evaluation of the role that stress plays in suppressing ovarian function;
• The effects of hormone interactions with other medications.
These are clearly critical areas affecting women. Why are these issues not being addressed? I think one factor is economic. There is more money to be made in the current proliferation in development and use of antidepressants rather than natural hormones, many of which have been around so long they have gone off patent. Once medications are off patent, the companies that developed them no longer make much money on them, and other companies begin to compete with generics. So the race is always to find new medications, new supplements, new products that will bring profit to the company that creates them.
But using antidepressants or over-the-counter supplements to reduce symptoms is like putting a Band-Aid on a wound that needs stitches—it may give some relief but doesn’t get at the underlying cause of the problem. Getting at the underlying hormone imbalance and finding the right “recipe” for a given person takes time and detective work. Time is expensive in today’s health care environment. It is easier—and takes less time—to write a prescription for an antidepressant than to check hormone levels properly, listen to the woman’s concerns, answer her questions, address her fears about hormones, and fine-tune a hormone prescription to achieve optimal hormonal balance. Many times, doctors can’t or don’t want to spend the time it takes, and many consumers aren’t willing to pay for the extra time or put up with the initial difficulties encountered trying to find the right combination. So there really isn’t any one “cause” or “fault” in all this; there are many factors. Only when women themselves have reliable information and become assertive about getting their needs met, will we have more individualized approaches widely used.
But if you really think about how valuable your health is, taking the approach I have outlined, is less expensive (in time and money) in the long run because you are addressing the underlying causes, and you are restoring body balance with natural hormones that your body has always made. If this is addressed really well, you will likely need far fewer other medications, hospitalizations, or surgeries to “fix” problems. Think about these points as you read the chapters ahead, in which I will give you many more specific examples and actual case stories from women themselves who have taken this journey. Remember, menopause is not a Prozac or Zoloft or Paxil deficiency. It is the loss of hormones that have overseen our body function for most of our lives. Don’t let anyone make you take the easy way out. Educate yourself—and ask to try approaches that feel natural and right for you.
There is a great deal of exciting work to be done to understand our awesome female body and these intricate interconnections. The need is great, and the list of unanswered questions is long. At HER Place, we strive to be among the leaders in these endeavors with an integrated approach to women’s health care encompassing Preventive Medicine, Gynecology, Endocrinology, Psychiatry/Psychology, Nutrition, Complementary Medicine, physical therapies (“body work”) and spiritual awareness. Speak out in your community and encourage the development of such integrated services for women. All of us working together can make a difference. It is crucial, in my view, that instead of focusing on fragmented treatment of women’s body parts, we must combine our therapeutic approaches in ways to provide effective and safe symptom relief and health enhancement (not just treatment) for women of all ages. Our goal is to have healthy, enjoyable, and productive lives for the additional years we now have the opportunity to live.