CHAPTER 2
The Science of Always Delicious
Why do overweight people overeat?
More than any other, this question bewilders experts in nutrition and the public alike. One common explanation is that people with excess weight lack willpower, discipline, and motivation. In a world with ubiquitous tasty foods, they simply succumb to temptation too easily, too often.
To address this perceived deficiency, conventional obesity treatment typically focuses on psychological techniques to help people control their behavior. Cut back on fat, which contains twice as many calories per gram as carbohydrate or protein. Eat on a small plate to make your meal seem larger. When hungry, distract yourself with an activity. Get up an hour earlier to make time for exercise. Find other sources of pleasure in life than food.
The problem is, these methods rarely result in lasting weight loss. Unfortunately, the mind-set they reflect regularly causes suffering, by reinforcing the view of obesity as a personal failing. If losing weight is simply a matter of self-control, then everyone should be able to do it. Anyone who can’t must lack basic knowledge or have a serious character flaw.
But as we’ll explore here, this way of thinking is completely wrong. Obesity is more about biology than willpower. The essential problem is too little enjoyment from food, not too much. The solution is to break the vicious cycle of hunger, cravings, and overeating and instead create a victorious cycle of pleasure and long-lasting satisfaction from truly nourishing foods. We call this Always Delicious.
HUNGER
Considering the importance of weather to the Inuit peoples of the Arctic, it’s not surprising that they have at least fifty names for snow.1 Along the same lines, we’d argue that all languages need several words to describe hunger.
One kind of hunger actually feels pleasant—the stimulating sensations that heighten anticipation and enjoyment of a good meal. Some cultures, such as the French, embrace and prolong those sensations as a daily practice before dinner. An entirely different experience is feeling ravenous and in desperate need for food. More than any other factor, that kind of overwhelming hunger drives overeating and dooms weight loss diets.
So why do many people become ravenously hungry after just a few hours without food, especially when trying to cut calories, whereas others cruise along comfortably, even when skipping meals? The answer can be found in our fat cells.
All except the thinnest among us have enough calories stored in fat cells to supply the needs of the body for many weeks, reserves that helped our ancestors survive famine. Under normal conditions, hormones and other biological influences precisely control the size and number of our fat cells. After we eat, calorie-rich fuels in the form of glucose, amino acids, and fats flood into the bloodstream, and hormonal signals tell fat cells to store the excess. A few hours later, after the meal has been digested, other signals instruct fat cells to release some of their calories, providing energy until the next meal. Our brain, monitoring this process, then makes us feel hungry, and we eat just enough to replenish the fuel supply, keeping body weight in a healthy range. That’s why humans—for example, in the United States from the end of the Great Depression to the 1970s—could live amid an abundance of food and maintain stable body weight across the population, without counting calories. However, this carefully controlled system has recently been thrown out of balance.
As we explored in Always Hungry?, something has triggered our fat cells to hoard too many calories, leaving too few for the rest of the body. Although we typically view obesity as a state of excess, it’s also a matter of starvation—not enough calories in the bloodstream to meet the needs of the brain and other organs. That’s why we get so hungry, so soon after eating, and why metabolism slows. It’s a distribution problem, like having a clogged fuel line in your car. No matter how much gasoline you put into the tank, the engine will be starved for fuel and won’t function efficiently until the underlying problem is fixed.
What’s driving our fat cells into a feeding frenzy? The clear culprit is too much of the hormone insulin. Think of insulin as Miracle-Gro for your fat cells… just not the sort of miracle you want happening in your body! Under the influence of insulin, calories check in to fat cells, but they don’t check out.
Consider what happens in type 1 diabetes, a disease mainly of youth in which the body can’t make enough insulin. A child with newly diagnosed type 1 diabetes will have typically lost weight, no matter how much he or she has been eating: 3,000, 5,000, or even 7,000 calories a day. Treat that child with the right amount of insulin, and body weight returns to normal. Give that child too much insulin, and excessive weight gain will predictably occur.
If you don’t have diabetes, the most important influence on insulin levels is the amount and type of carbohydrate you eat.2 Calorie for calorie, processed, fast-digesting (high-glycemic-load) carbohydrates raise blood sugar and insulin more than any other food. These include all those starchy and sugary foods that flooded our diets during the forty-year low-fat craze: white bread, white rice, potato products, cookies, crackers, chips, candy, and sugary drinks. In fact, refined starchy foods can be just as much a problem as sugar. Starches are nothing more than molecules of the sugar glucose in a long chain. Try this experiment yourself. Take a bite of a bagel and chew it thoroughly. Do you notice it begins to taste sweet? That’s sugar popping off the starch under the weak effects of enzymes in saliva. Once that bagel hits the powerful enzymes lower down in the digestive track, it literally melts into glucose. By contrast, natural carbohydrates like nonstarchy vegetables, whole fruits, beans, and minimally processed grains have a much gentler effect on blood sugar and insulin.
Proteins also cause some release of insulin, but less so than most processed carbohydrates. And unlike carbohydrate, protein raises levels of the hormone glucagon, which counteracts insulin and encourages fat cells to release calories. For this reason, balanced proportions of protein play an important role in the Always Delicious meal plan, including vegetarian options.
The third major nutrient, dietary fat, has virtually no effect on blood sugar and insulin at all, a key point in designing a more effective approach to control hunger and lose weight. Despite what we were told during the last forty years, low-fat diets are clearly inferior to all higher-fat diets, such as Mediterranean diets, low-carbohydrate diets, very-low-carbohydrate diets, and ketogenic diets—the grandfather of all high-fat diets, with up to 80 percent fat!3 And as every chef knows, fat is tasty, making recipes delicious without having to resort to sugar and artificial additives. You’ll find an abundance of healthy high-fat foods among the recipes—including nuts and nut butters, full-fat dairy, avocado, rich sauces and spreads, and real dark chocolate!
In addition to the major nutrients, other aspects of diet influence fat cells in various ways. Micronutrients (vitamins and minerals), phytochemicals (protective plant chemicals), prebiotics (fiber), and probiotics (microbes that promote healthy gut function) can lower insulin levels, calm chronic inflammation, and directly communicate with fat cells. Always Delicious recipes provide a rich source of these beneficial dietary components.
Beyond diet, lifestyle has a major influence on fat cells, too, which is why the program in Always Hungry? includes a focus on stress relief, quality sleep, and enjoyable physical activities.
In summary, the standard “eat less, move more” approach to weight control rarely works, because it ignores the underlying problem. Sure, you can lose weight for a short while by restricting calories, but the body fights back, with rising hunger and slowing metabolism. That’s a battle we’re destined to lose. A better approach is to target the biological cause of excessive hunger—fat cells stuck in calorie-storage overdrive. When fat cells calm down, the cycles of ravenous hunger and overeating naturally subside, along with other remarkable changes in the body, as we shall see in the next sections.
CRAVINGS
Have you ever eaten enough to be full, but somehow still felt unsatisfied? While others contentedly sipped coffee or tea after dinner, you couldn’t keep your mind off those cookies in the kitchen cabinet. You didn’t need more food. You weren’t even hungry. Oddly, you may not have especially liked those cookies before, but you wanted them now, and your mind wouldn’t leave you alone until you succumbed.
Though we tend to associate hunger with cravings, they are quite distinct experiences controlled by different regions of the brain. Hunger comes primarily from the hypothalamus, a deep brain region that also regulates metabolism. Damage to the hypothalamus, from an injury or a tumor for example, can cause massive obesity that defies treatment. In contrast, cravings arise from dopamine-rich brain areas involved in reward and “saliency” (how important something is right now). These areas, centered around the nucleus accumbens, play a critical role in the classic addictions to alcohol, nicotine, cocaine, heroin, and even gambling.
Thousands of scientific studies have explored the psychological aspects and environmental triggers of eating. However, this research often overlooks the strong biological basis of food cravings, and without this understanding, treatment of binge eating and related conditions may miss the mark. As with hunger, cravings aren’t inherently harmful. Instead, they’re a signal that the body has an unmet need or is otherwise out of balance. For this reason, attempts to simply ignore or resist cravings often fail, and can actually make matters worse over the long term.
Consider what happens in Addison’s disease, a hormone deficiency that causes the kidneys to lose too much sodium in the urine. People with this disease characteristically develop intense cravings for salty foods in the body’s attempt to avoid dangerously low levels of sodium in the blood. Indeed, salt cravings in someone with unrecognized Addison’s can be life-saving. But eating more salt will restore sodium levels and satisfy the cravings only temporarily, unless the underlying problem—loss of sodium in the urine—is corrected with replacement of the missing hormone.
So what drives food cravings? Let’s have a look at three illuminating studies.
An extraordinary experiment from 1946 used somewhat unsettling methods to examine taste preferences during severe hypoglycemia.7 The investigators examined one hundred patients receiving an intentional insulin overdose for treatment of psychiatric disease (a method abandoned by medicine decades ago). The patients were asked to sample five solutions as their blood sugar plummeted after the insulin injection, for as long as they stayed conscious and able to communicate:
1. Water
2. Water with 5 percent sugar (similar in sweetness to a sports drink)
3. Water with 30 percent sugar (extremely sweet)
4. Water with saccharin matched in sweetness to 30 percent sugar
5. Water with salt
While blood sugar remained close to normal, virtually all the patients rejected the 30 percent sugar solution as too sweet. But as hypoglycemia progressed, most reversed their preferences and chose that solution over all the others. Of particular interest, some people seemed to lose the ability to perceive the saccharin solution as sweet during hypoglycemia, suggesting that at this critical time, the body can distinguish natural sweeteners (which raise blood sugar) from artificial sweeteners (which don’t).
A more recent (and perhaps more ethical) study also used insulin injections to drive down blood sugar, but this time taking precautions to ensure safety.8 Before the insulin injection, very few subjects reported food cravings of any sort, whereas during hypoglycemia, most did. The items craved most frequently were bread, cereal, pizza, and sandwiches—that is, processed carbohydrates high in glycemic load.* When subjects were given choices of high-carbohydrate, high-protein, or high-fat foods, they expressed the greatest desire for the carbohydrates.
A third study administered insulin infusions by vein under two conditions: either with enough glucose, also by vein, to keep blood sugar normal (88 milligrams per deciliter); or with somewhat less glucose, to produce slightly low blood sugar (67 milligrams per deciliter).9 Then, scans of brain activity were done as the subjects viewed images of high-calorie foods. Under both conditions, the subjects reported liking the foods to the same degree. However, with the lower blood sugar, they reported wanting the foods more, and scans showed increased activity in the reward and addiction areas of the brain, including the nucleus accumbens.
These findings demonstrate that food craving is another trick your brain uses, in addition to hunger, to make you eat when your blood sugar is low, especially if other fuels (like fatty acids) have been locked away by high insulin levels. We specifically crave processed carbohydrates—rather than unprocessed carbohydrates like apples, fats like butter, or proteins like egg whites—because they raise blood sugar fast. The problem is, they also raise insulin the most, setting the stage for the next surge/crash cycle.
So the concept of “food addiction,” often dismissed by experts,10 may not be farfetched after all. Fortunately, the same approach used to control hunger also calms cravings, and relief can be just one meal away!
SATIETY
The word “satiety” comes from the Latin satietatem, meaning abundance, sufficiency, and fullness.12 Satiety, basically the opposite of hunger, refers to how long we feel full after eating, and from this perspective, the number of calories eaten at any one time doesn’t tell the whole story. A 2-ounce snack of cotton candy provides fewer calories than the same amount of nuts. But if you became much hungrier much sooner after the candy, you wouldn’t be better off by the end of the day—another reason why focusing exclusively on calories makes little sense.
As we considered earlier, fast-digesting carbohydrates raise insulin excessively, driving too many incoming calories into storage. Soon after eating, the body runs low on fuel, provoking hunger13 and cravings. However, whole natural carbohydrate, healthy fats, and protein in the right proportions produce long-lasting satiety. Other aspects of food also influence satiety, such as the total volume of a meal (determined mainly by water content), fiber, the type of protein and fat, and the types and intensity of flavors. The Always Delicious recipes take full advantage of these effects. In addition, environmental conditions (lighting, sound, presence of others), our psychological state (relaxed or stressed), and the pace of the meal can play significant roles, underscoring the importance of mindful eating.
Beyond physical sensations of hunger and fullness, the concept of satiety gets at something broader, involving our general well-being. With every meal, hormones, metabolism, and even the expression of genes throughout the body change according to what we eat. These biological changes can make all the difference between feeling awake and alert, or sluggish and sleepy for hours to come. Have you experienced the powerful effects of food on mood, long after eating? If not, the research linking fast-digesting (high-glycemic-load) carbohydrate to physical, emotional, and mental well-being may surprise you.
In one clever study, nineteen children from an economically disadvantaged school in Wales were recruited to participate in a “breakfast club.”14 Each school day for a month, the children were given one of three different breakfasts in random order: cornflakes and a waffle with reduced-fat milk and sugar (high glycemic load, and quite typical of what many kids have for breakfast); scrambled eggs, conventional bread, jam, and yogurt (medium glycemic load); or a ham and cheese sandwich with a special reduced-carbohydrate bread (low glycemic load). Then, their behavior and cognitive performance were monitored with video games and other tests two to three hours later. The children demonstrated better memory and ability to sustain attention, fewer signs of frustration, and more time on-task working individually in class on the morning following the low-glycemic-load breakfast. However, since the meals differed in many ways, it is hard to know what specific food components contributed to the observed effects.
Another study of sixty-four elementary school students in England compared the effects of two more comparable breakfasts, high-glycemic-index Cocoa Puffs or low-glycemic-index All-Bran cereal with milk.15 The investigators found that the children’s attention and memory deteriorated throughout the morning (a phenomenon no doubt bemoaned by teachers around the world), but the declines were less severe following the low-glycemic-index breakfast.
In another study, among seventy-one adult women, memory for hard words was impaired after a high-glycemic-index compared to low-glycemic-index cereal-based breakfast.16 As expected, this difference emerged after 2½ hours—that is, following the rise and fall in blood sugar. Similarly, executive function, selective attention, verbal memory performance, and working memory were worse among twenty-one patients with diabetes following a high-glycemic-index meal compared to a low-glycemic-index meal.17
Do the effects from these one-day studies persist? A clinical trial with eighty-two adults in the Seattle area suggests they do.18 The participants received two fully prepared diets in random order, low or high glycemic index, both with the same calories, carbohydrate, protein, and fat. After four weeks, those on the high-glycemic-index diet had significantly worse scores for total mood disturbances (55 percent), depressive symptoms (38 percent), and fatigue/inertia (26 percent). During a six-month weight loss study including forty-two overweight adults, worsening mood was observed among those given a high-glycemic-load diet compared to low-glycemic-load diet—a side effect that might weaken resolve to stick with that diet.19 Furthermore, in the Women’s Health Initiative Observational Study, higher dietary glycemic index, added sugar, and refined grains were each associated with a greater risk of developing depression over three years among about seventy thousand postmenopausal women.20 In contrast, whole fruits and vegetables were associated with lower risk.
The relationship between food and mood is, of course, complicated, and not all published studies have reached similar conclusions. But overall, the research indicates that—beyond the number of calories in a meal—the quality of those calories can help you feel full longer, have more energy, remain calm and focused, think more clearly, feel better, and be happier. As we’ll see in the next section, these positive experiences can lead to a remarkable transformation of taste perceptions, making healthful foods progressively more appealing with time.
TASTINESS
We typically think of tastiness, scientifically termed “palatability,” as an inherent component of food. Some foods by their very nature seem to give us a lot of pleasure; others simply don’t. Unhappily, items in the first category tend to be the most fattening. So must people with a weight problem inevitably choose between virtuous self-denial or harmful hedonism? Despite some early-life hardwiring, the answer is emphatically no.
In a classic series of studies, researchers examined the facial expressions of newborn infants in response to sweet, sour, and bitter solutions placed on their tongues. The sweet solution elicited signs of satisfaction, including licking, sucking, and a slight smile. The other solutions produced distinct grimaces.22 These programmed preferences prime infants for breast milk (which tastes sweet) and protect them from ingesting potentially toxic substances. However, like the startle reflex, children normally outgrow this instinctual behavior, learning to like an increasingly broad range of tastes—including savory, spicy, sour, bitter, and pungent. That’s why Inuit children like muktuk (raw blubber), Korean children like kimchi (fermented cabbage), and Mexican children like hot pepper sauce.
In fact, taste perceptions can change quickly, at any age, as the 1946 study of psychiatric disease patients here demonstrated. For a less extreme scenario, imagine you had an unexpectedly long wait at a favorite restaurant and became ravenously hungry. When you were finally seated, the waiter brought a basket of freshly baked bread to the table. How do you think it would taste? Probably delicious. Now, suppose you had a huge meal—appetizers, wine, main course, side dishes, a rich dessert—and afterward, the waiter accidentally provided another basket of the very same bread, warm from the oven. How would it taste then? Probably unappealing.
These examples demonstrate a fundamental principle: Palatability isn’t intrinsic to food—it’s a response to food determined largely by our biology. We learn to like foods that make us feel good and dislike those that don’t. For this reason, many people savor beer and coffee—the pleasurable effects of alcohol and caffeine on our mood eclipse the intense bitterness of these beverages. Conversely, even a favorite food can become aversive for a long time, if we develop food poisoning soon after eating it. (From this perspective, we can also see why “forcing” kids to eat vegetables can be counterproductive, as it pairs the taste of healthful foods with the unpleasant experience of stress.)
The Standard American Diet keeps taste preferences in an infantilized state, but not because it’s inherently so tasty. Do we really think America leads the world in obesity because we’ve got the world’s most delicious diet? The French, Italians, Japanese, and others would probably beg to differ. As we learned from several studies mentioned earlier, the palatability of sugar and other processed carbohydrates increases rapidly after insulin injection as a biological response to low blood sugar. Changes in taste perception may be less dramatic if the insulin excess comes from within the body, in response to eating those fast-digesting carbohydrates in the first place, but the ultimate outcome is the same. It’s the secret to the processed food industry’s success—Cheetos, Froot Loops, Twinkies, Ritz Crackers, Coke, and of course Lay’s (“Bet you can’t eat just one”) potato chips become tastier the more you eat them. The good news is that this vicious cycle can be quickly broken.
FROM ALWAYS HUNGRY TO ALWAYS DELICIOUS
A low-fat diet high in processed carbohydrates propagates what we call the Always Hungry Vicious Cycle (as depicted in Figure 2.1). Soon after eating, blood sugar and insulin rise rapidly, providing intense but brief biological reward as calories flood into the body. However, the excess insulin directs too many calories into storage, especially into fat cells (promoting weight gain). About two hours later, the rest of the body starts to run low on fuel, and hunger rises. At that time, physical energy and mental abilities may wane. Craving for processed carbohydrate also occurs, making it more likely we’ll make the wrong choices at the next meal or snack, setting up another binge-crash cycle.
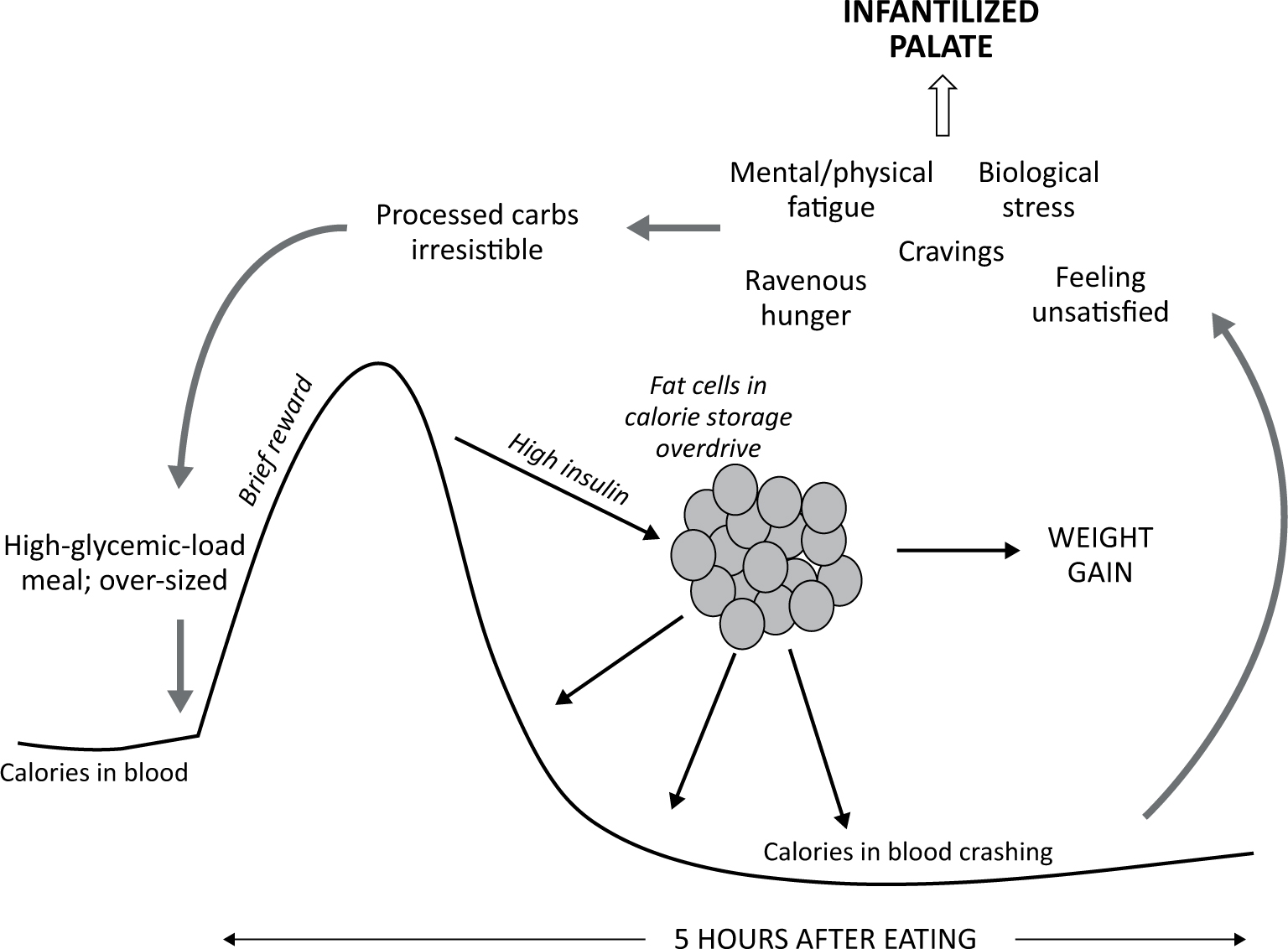
Figure 2.1: The Always Hungry Vicious Cycle
The solution is a higher-fat diet, with slow-acting carbohydrates and the right amount of protein to lower insulin (and reduce chronic inflammation, insulin’s troublemaking twin). As insulin levels drop, fat cells calm down, releasing their pent-up calories back into the body. Hunger and cravings diminish, energy increases, well-being improves, and these enjoyable bodily experiences feed back to our taste preferences, helping them evolve spontaneously. Soon, the power of hyperprocessed products over us wanes, as we activate the Always Delicious Victorious Cycle (see Figure 2.2). When you reprogram your fat cells, you automatically reprogram your taste buds—resolving the conflict between nutritious and delicious once and for all.
In the next chapter, we’ll prepare to put these principles into action with a step-by-step guide to becoming an Always Delicious chef.
Figure 2.2: The Always Delicious Victorious Cycle
