
INTRODUCTION
The last aspect of cognition that we will review is the ability to attend to external or internal stimuli. Like memory, attention is one of the oldest and most studied areas of cognitive science. One hundred years ago researchers used stopwatches and psychological tests to measure attention. In the latter half of the 20th century, the placement of microelectrodes into the brains of monkeys opened the door to investigating the capacity of individual neurons to attend. Now with brain imaging studies we can observe, in real time, the shifting focus of an awake human solving a puzzle—with or without medication. One hundred years of research has given us a better understanding of the power of the brain to focus on relevant stimuli, although many aspects of the neurobiology of attention remain mysterious.
Attention in a broad sense describes the mechanism that weighs the importance of various stimuli and selects the one that will receive the brain’s focus. The brain has limited capacity for attention. Numerous psychological tests have demonstrated the brain’s finite capacity to attend as more and more stimuli are added. A relevant example from modern life involves driving while talking on a cell phone. A recent study found that drivers using a cell phone had a fourfold increase in the chance of a serious accident. Handsfree phones were equally problematic. Attending to a conversation detracts the driver from attending to events on the road—contrary to what the driver thinks.
The capacity to concentrate and maintain one’s attention is inversely related to the ability to ignore other stimuli. Responding to other stimuli—whether internal or external—changes the brain’s focus. The brain cannot attend if it is wandering from one thought to another. The border collie in Figure 20.1 shows an example of highly selective attention. The dog is not only focused on the frisbee but also actively ignoring other objects of potential interest around him. In this state he will ignore female dogs, squirrels, children, and even food. He will not sniff the scent of other dogs or leave his own mark on the shrubbery. He appears to focus solely on the flying sphere.
Athletes provide another example of the intimate relationship between attending and ignoring. The quarterback who has dropped into the pocket and is able to ignore all the noise and violence around him while he searches for an open receiver is an extraordinary example of attending and ignoring. Likewise, when the artist or the absent-minded professor gets lost in work, they are ignoring most sensory inputs coming into their brain. Treatments that improve attention may be effective because they improve the brain’s capacity to screen out the unessential.

FIGURE 20.1  A border collie ignores everything else around him while focusing on the frisbee.
A border collie ignores everything else around him while focusing on the frisbee.
Measuring Attention
Continuous performance tasks (CPTs) give an objective estimate of an individual’s attention and impulsivity. Subjects watch a computer screen and hit a button or click a mouse whenever a specified sequence of symbols or letters appears (Figure 20.2A). Such tests reflect the subject’s capacity to attend as well as the ability to restrain impulsive answers. Results are compared with normative data for individuals in one’s age group.
Attention changes across the life span. Figure 20.2B shows the percent errors on one CPT (Test of Variables of Attention) for 1,590 individuals from the ages of 4 to 80+. Note how attention improves with age until the senior years. These findings appear to roughly correlate with the myelination of the white matter in the frontal lobes (see Figure 8.8).
WORKING MEMORY
Prefrontal Cortex
Working memory describes what is actively being considered at any moment. If the conscious brain is actually a tiny person inside a control room orchestrating the body’s responses, working memory would be what he sees on the monitors in front of him. It is temporary, limited in capacity, and must be continually refreshed. Traditionally, working memory has been associated with the prefrontal cortex (PFC). It most certainly resides there, but may also include connections with the parietal lobes.
ADHD AND ADULTHOOD
Attention-deficit/hyperactivity disorder (ADHD) was once considered a childhood disorder. More recently, it has become popular for adults to get treatment for this condition. However, a recent meta-analysis of follow-up studies found that most children with ADHD fail to meet the full criteria for the disorder as adults—only 10% to 15%.
Trauma to the PFC impairs working memory. Phineas Gage is the most famous case that shows the effects of frontal brain damage on working memory. He was the young railroad worker who had a tamping iron explode through his frontal cortex (see Figure 14.4). He went from being responsible and organized to impulsive and inattentive. His inability to sustain a thought in his working memory could be considered the root cause of his wandering attention.
Researchers developed a way to test working memory in monkeys, called the delayed-response task. In this task, a monkey is shown a piece of fruit being placed in one of two randomly chosen receptacles (Figure 20.3). This is called the cue. A screen is then pulled down obscuring the monkey’s view and lids are placed over both receptacles. When the screen is lifted, the monkey gets one chance to remove the correct lid and receive his reward. The significance of this test is that the monkey must hold the visual image of the location of the fruit in his working memory during the delay period. Healthy monkeys learn this task quickly. Monkeys with frontal lobe lesions perform poorly.
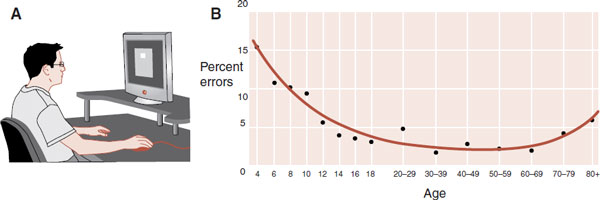
FIGURE 20.2  A. A continuous performance task provides an objective measure of attention and concentration. B. Percent errors as measured by the Test of Variables of Attention are age dependent. (Adapted from Greenberg LM, Crosby RD. A Summary of Developmental Normative Data on the T.O.V.A. ages 4 to 80+. Unpublished manuscript available through The TOVA company; 1992.)
A. A continuous performance task provides an objective measure of attention and concentration. B. Percent errors as measured by the Test of Variables of Attention are age dependent. (Adapted from Greenberg LM, Crosby RD. A Summary of Developmental Normative Data on the T.O.V.A. ages 4 to 80+. Unpublished manuscript available through The TOVA company; 1992.)
FIGURE 20.3  The delayed-response task. A. The screen is raised and the monkey observes a piece of fruit placed in one of the wells. B. The screen is lowered and the wells are covered. C. After a specific period of time the screen is raised and the monkey has one chance to remember the correct location of the fruit. (Adapted from Purves D, Augustine GJ, Fitzpatrick D, et al. Neuroscience. 5th ed. Sunderland, MA: Sinauer; 2011.)
The delayed-response task. A. The screen is raised and the monkey observes a piece of fruit placed in one of the wells. B. The screen is lowered and the wells are covered. C. After a specific period of time the screen is raised and the monkey has one chance to remember the correct location of the fruit. (Adapted from Purves D, Augustine GJ, Fitzpatrick D, et al. Neuroscience. 5th ed. Sunderland, MA: Sinauer; 2011.)
In the 1970s, researchers began putting microelectrodes into individual neurons in the PFC of monkeys while they participated in the delayed-response task (Figure 20.4A). They found that neurons reacted differently during the task. Some neurons were active only during the cue and response periods, whereas other neurons became active during the delay period (Figure 20.4B).
The delay neurons start firing with the presentation of the cue and stop with the response. These neurons seem to hold the memory of the task—literally the neural equivalent of working memory. When the monkeys incorrectly responded, the delay neurons were usually inactive. If the monkeys were distracted during the delay period, the delay neurons would usually settle down and the monkeys would make incorrect responses or not respond at all.
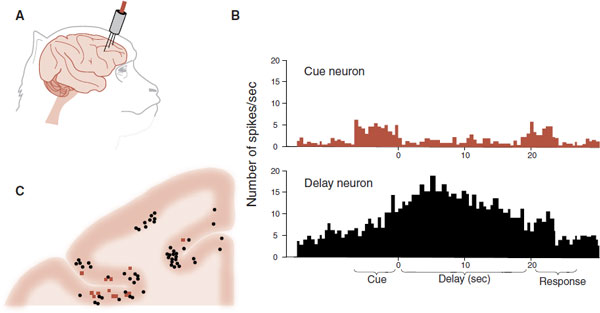
FIGURE 20.4  A. Microelectrodes placed into individual neurons in the prefrontal cortex (PFC) and monitored during the delayed-response task. B. Neuronal activity in cue neurons (top) and delay neurons (bottom) during the delayed-response task. C. The location of the cue and delay neurons in the right PFC. (Adapted from Fuster JM. Unit activity in prefrontal cortex during delayed-response performance: neuronal correlates of transient memory. J Neurophysiol. 1973;36(1):61-78.)
A. Microelectrodes placed into individual neurons in the prefrontal cortex (PFC) and monitored during the delayed-response task. B. Neuronal activity in cue neurons (top) and delay neurons (bottom) during the delayed-response task. C. The location of the cue and delay neurons in the right PFC. (Adapted from Fuster JM. Unit activity in prefrontal cortex during delayed-response performance: neuronal correlates of transient memory. J Neurophysiol. 1973;36(1):61-78.)
After the studies, the researchers sacrificed the monkeys and identified the location of the microelectrodes. The results from several of the monkeys from one section of their right PFC are condensed and are shown in Figure 20.4C. The cue neurons and delay neurons are shown in different colors. Note how the delay neurons are more common than the cue neurons and cluster together. It is likely the delay neurons do not work independently but are part of a network that holds the image in working memory.
Catecholamines
Working memory is modulated by the catecholamines: dopamine (DA) and norepinephrine (NE). Pharmacologic interventions that increase DA and NE in the PFC enhance working memory and improve attention. Alternatively, agents that block DA receptors, such as haloperidol, have been shown to degrade performance on delayed-response tasks.
Phillips et al. examined the relationship between accuracy on a delayed-response task and DA release in the PFC. They placed microdialysis probes in the PFC of rats (see Figure 12.4A), which allowed continual analysis of extracellular DA concentrations while the rat performed the task. The rats were tested using an eight-arm radial maze (Figure 20.5A). In the training phase, rats were given 5 minutes to explore a radial arm maze that had four randomly chosen arms baited with food. During the delay, the rats were confined at the center of the maze in the dark from 30 minutes to 6-hours. In the test phase, food was placed on the opposite arms from the training phase and the rats were given 5 minutes to locate the rewards. Errors were scored as entries into unbaited arms. Extracellular DA was analyzed at baseline and during the testing phase.
EXECUTIVE FUNCTION VERSUS WORKING MEMORY
The terms executive function and working memory are often used synonymously in the literature. Some researchers prefer one term while others prefer the other, but they are not synonymous. Executive function includes working memory as well as other higher level cognitive skills such as organizing priorities and planning initiation strategies. Although executive function and working memory describe different functions in the brain, they share the same underlying mechanisms. Both reside in the PFC, are impaired with frontal lobe damage, and fluctuate with catecholamine modulation.
The results show an inverse correlation between extracellular DA in the PFC during the testing phase and errors (Figure 20.5B). When the delay was only 30 minutes, the efflux of DA into the PFC increased over the baseline by 75% and the rats made only few error journeys into unbaited arms. However, as the delay was increased, the DA efflux decreased and the errors mounted.
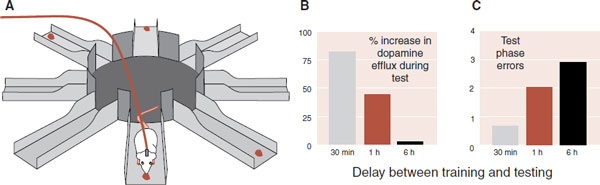
FIGURE 20.5  A. Radial arm maze with four arms baited. B. Percent increase in extracellular dopamine at the testing phase. C. Errors at the testing phase. (Adapted from Phillips AG, Ahn S, Floresco SB. Magnitude of dopamine release in medial prefrontal cortex predicts accuracy of memory on a delayed response task. J Neurosci. 2004;24(2):547-553.)
A. Radial arm maze with four arms baited. B. Percent increase in extracellular dopamine at the testing phase. C. Errors at the testing phase. (Adapted from Phillips AG, Ahn S, Floresco SB. Magnitude of dopamine release in medial prefrontal cortex predicts accuracy of memory on a delayed response task. J Neurosci. 2004;24(2):547-553.)
Biofeedback
Neurofeedback (also called electro encephalogram [EEG] biofeedback) is a treatment option that allows patients to exercise their brain to improve attention and concentration. The EEG frequencies are divided into four groups (see Figure 15.3). β waves are the frequency pattern produced when a person is alert and concentrating. The goal of neurofeedback is for the patient to generate more β rhythm and less α and θ rhythms.
Neurofeedback utilizes a computer that interprets the EEG frequencies from the user and provides them with feedback through a symbol on the computer screen. For example, the symbol will move up with β rhythm and down with all other EEG frequencies. The user learns to move the image up the screen by producing β rhythms, which in turn strengthens the neurons that focus attention. It is the mental equivalent of lifting weights.
Although there have not been large, randomized controlled trials, results in the literature are about 75% positive. Recently a group in Montreal completed a small controlled trial with functional imaging before and after biofeedback treatment in children with ADHD. Treatment consisted of 40 sessions of neurofeedback, each lasting an hour, over 15 weeks. The neurofeedback group not only improved their scores on measures of attention but also increased the activation of the anterior cingulate cortex (Figure 20.6). Once again, we see that the brain is not a static organ and responds to exercise and training.
The inverse is also true. That is, not exercising the brain—or worse, watching “mindless” television—seems to impair attention. Longitudinal studies have linked childhood television viewing with subsequent attentional problems in adolescence—more TV results in poorer focus. A recent study examined the immediate effects on 4-year-old children of watching a segment of SpongeBob. Children who watched 9 minutes of the cartoon show, as compared with those who spent 9 minutes drawing, showed impairments in executive function (self-regulation, delay of gratification, and working memory) when tested immediately after the intervention. The fast-paced nature of some television fails to train the brain to focus and attend. Is this one reason we are seeing a surge in the diagnosis of attentional disorders?
REWARD AND IMPULSE CONTROL
Sustained attention to a particular task requires an individual to ignore other appealing stimuli. Controlling the impulse to take the immediate, smaller reward and waiting for the larger, delayed reward is essential for completing any project. People who cannot control these impulses are at a disadvantage. In an amazingly simple study, a group at Stanford examined the ability of children to wait for the larger reward and then followed up their outcome as adolescents.
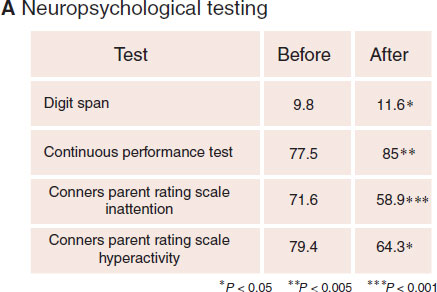
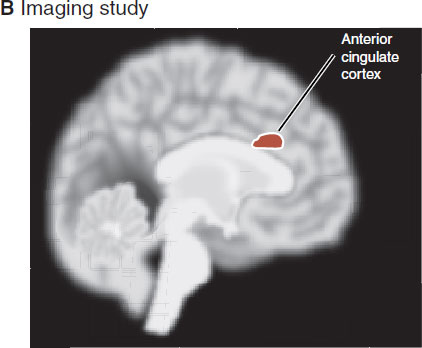
FIGURE 20.6  A. Neuropsychological testing improved after 40 sessions of neurofeedback. B. The anterior cingulate cortex showed greater activity after the neurofeedback treatment. (Adapted from Levesque J, Beauregard M, Mensour B. Effect of neurofeedback training on the neural substrates of selective attention in children with attention-deficit/hyperactivity disorder: a functional magnetic resonance imaging study. Neurosci Lett. 2006;394(3):216-221.)
A. Neuropsychological testing improved after 40 sessions of neurofeedback. B. The anterior cingulate cortex showed greater activity after the neurofeedback treatment. (Adapted from Levesque J, Beauregard M, Mensour B. Effect of neurofeedback training on the neural substrates of selective attention in children with attention-deficit/hyperactivity disorder: a functional magnetic resonance imaging study. Neurosci Lett. 2006;394(3):216-221.)
In the study, 4-year-old children were sequestered in a room with an assistant who placed a marshmallow on a table. The children were told that the assistant had to run an errand and would be stepping out of the room. They were also told they could eat the one marshmallow, but if they could wait until the assistant returned, they could have two marshmallows. The assistant left the room for approximately 15 minutes and the childrens’ response was monitored. Some children ate the marshmallow as soon as the assistant exited the room, whereas the rest showed varying degrees of self-restraint.
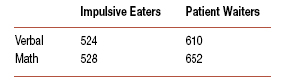
The social and academic performance of these children was reassessed in their adolescence. The children who were better at inhibiting the impulse to immediately eat the one marshmallow were more resilient, confident, and dependable as adolescents. Additionally, they were more successful students and even scored higher on the SAT. The SAT scores for the more impulsive children are contrasted with those who showed more self-control. The total scores of the two groups differ by approximately 100 points.
Clearly, the ability to suppress the desire to grab the immediate reward was associated with behaviors that have a profound impact on one’s life. People who can delay gratification and control their impulses appear to achieve more in the long run.
Nucleus Accumbens and Dopamine
Attention and impulsivity are opposite sides of the same coin. Both are controlled, in part, by DA activity in the nucleus accumbens (NAc). Pleasurable activities increase the release of DA in the NAc (see Figure 12.6). People are less likely to respond to other stimuli if they are engaged in activities they enjoy. Stimulant medications also increase the DA released at the NAc and increase impulse control. People report that stimulants enable them to block out irrelevant stimuli with greater ease.
Clearly, other areas of the brain influence the NAc. For example, the orbitofrontal cortex, the hippocampus, and the amygdala are three regions with important projections to the NAc (see Figure 12.3). However, the NAc is uniquely wired to focus attention on the more favorable rewards.
Other evidence of the role of the NAc in impulsive behavior comes from lesion studies on rats. Rats can learn to choose a larger, delayed reward over a smaller, immediate reward. Lesions of the NAc will reverse this behavior. The rats with damaged NAcs become more impulsive and choose the immediate reward more frequently.
Impulsivity and Youth
Why are adolescents so impulsive and prone to taking risks? One possible explanation is that the frontal cortex has not yet matured—an issue discussed in Chapter 14, in the context of explaining impulsive aggression. Another explanation points to the NAc and dopaminergic tone.
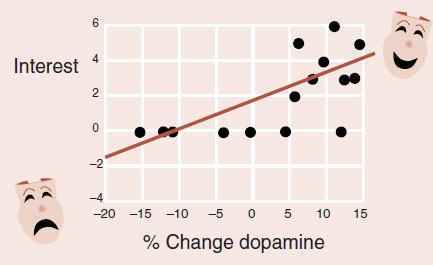
The DA reuptake pump (called the DA transporter) has been used as a measure of dopaminergic tone. New technology allows the imaging of the DA transporter density. Studies have examined the DA transporter density at the striatum (the region that contains the NAc). Figure 20.7 shows the decline in the DA transporter with age. Note the more precipitous drop in early adulthood.
BOREDOM
It is no great revelation to say that people have a hard time staying focused on boring tasks. The stimulant medications may improve attention (at least in part) by increasing the level of interest perceived by the brain. Volkow et al. gave methylphenidate or placebo to normal young men and imaged their brains while they solved math problems. When taking methylphenidate, the men found math less boring and more exciting (see figure).
Changes in extracellular dopamine at the striatum correlated with interest in normal adults solving math problems. (Adapted from Volkow ND, Wang GJ, Fowler JS, et al. Evidence that methylphenidate enhances the saliency of a mathematical task by increasing dopamine in the human brain. Am J Psychiatry. 2004;161(7): 1173-1180.)
Other researchers have shown that drug-naïve patients with ADHD have, on average, a slightly higher density in DA transporter at equivalent ages. For example, a 30-year-old patient with ADHD has the DA transporter density of a normal 22-year-old. Therefore, it appears that high DA transporter density (seen with younger individuals and patients with ADHD) correlates with more impulsive behavior, while lower density correlates with better impulse control.
Drug Addiction
The cravings that drug addicts experience at times for their drug of choice might be the most extreme example of seeking immediate gratification. When a drug addict gets this kind of urge, there are few concerns about long-term consequences. Every clinician knows about horror stories of addicts who have squandered the family savings just to get high. What is the role of the NAc in addictive behavior?
FIGURE 20.7  A. The density of the dopamine transporter at the striatum as a function of age. B. Distribution of DA transporter in the human brain. (Adapted from Mozley PD, Acton PD, Barraclough ED, et al. Effects of age on dopamine transporters in healthy humans. J Nucl Med. 1999;40(11):1812-1817.)
A. The density of the dopamine transporter at the striatum as a function of age. B. Distribution of DA transporter in the human brain. (Adapted from Mozley PD, Acton PD, Barraclough ED, et al. Effects of age on dopamine transporters in healthy humans. J Nucl Med. 1999;40(11):1812-1817.)
We know that chronic cocaine use downregulates the DA receptors at the NAc (see Figure 12.11). Likewise, we have shown that amphetamines and opioids alter the morphology of dendritic spine on neurons in the NAc (see Figure 12.13). These results and the behavior of the addicts suggest that drug abuse damages the NAc. Such an effect might be the pharmacologic equivalent of lesioning the NAc—an effect that enhances impulsive behavior.
ATTENTION-DEFICIT/HYPERACTIVITY DISORDER
Genetics
ADHD travels in families. It is one of the most heritable psychiatric disorders we know. Pooled analyses of twin studies suggest the heritable rate may be as high as 76%, but the search to identify the specific genes has been disappointing. Pharmacologic and neuroimaging studies suggest a dopaminergic hypothesis for ADHD. Indeed the genes for the DA transporter and the D4 DA receptor have been implicated in numerous studies. However, not all studies are positive and meta-analysis finds only small effects of the individual genes, which explains only a tiny part of the genetic contribution to the disease.
Several genome-wide association studies have been conducted in an unbiased search for candidate genes (five studies as of 2009). Unfortunately, there is little overlap in the findings between the studies, and “classic” transmitters (DA, NE, and serotonin) were not even among the top findings. Other more basic processes such as cell adhesion, neural migration, and neural plasticity have been implicated by the genome-wide studies, but none are statistically significant. Franke concluded, “ADHD is a multifactorial disorder, in which many genes, all with a small effect, are thought to cause the disorder in the presence of unfavorable environmental conditions.” Probably not a bad description about the genetics of all psychiatric disorders, as we currently understand them.
Brain Size
As discussed earlier, working memory and impulse control are important features of attention and are usually impaired in patients with ADHD. As would be expected, dysfunction in the PFC and striatum is the most common abnormal brain findings reported for ADHD.
However, the most comprehensive neuroscientific studies on children with ADHD come from Judith Rapoport’s laboratory at the National Institute of Mental Health. They have conducted several large prospective case–control magnetic resonance imaging (MRI) studies of the brains of children with ADHD. One study produced multiple MRI scans of 150 children with ADHD and 139 age- and sex-matched controls. Sixty percent of the participants had at least two scans.
The most interesting finding was that children with ADHD had smaller total brain volumes by approximately 5% compared with controls. The difference held true for all four cerebral lobes (including white matter and gray matter), as well as the cerebellum. The trajectory of the total brain volumes did not change as the children aged, nor was it affected by the use of stimulant medication.
Gray Matter Thickness
In a follow-up study, Rapoport’s group examined another 300 subjects, half of whom had ADHD. This time, with better technology, they measured regional gray matter thickness. The most unique feature of this second study was that they followed up the clinical outcome as well as the structural changes in the brain of the children over time. They were able to compare the children who grew out of the disorder with those that did not.
MINIMAL BRAIN DYSFUNCTION
In the past, ADHD was called minimal brain dysfunction, a term now considered derogatory. The findings from Rapoport’s laboratory suggest that those older clinicians, without the benefits of modern imaging studies, had a subtle but accurate understanding of the pathophysiology of ADHD.
The results showed that children with ADHD had global thinning of all the gray matter compared with the controls, although it was most prominent in the PFC. Additionally, both groups showed the usual pruning of the total gray matter as they grew through adolescence (Figure 20.8). However, two regions were unique when correlated with clinical outcome:
FIGURE 20.8  Total gray matter thickness for children with attention-deficit/hyperactivity disorder (ADHD) compared with controls. (Adapted from Shaw P, Lerch J, Greenstein D, et al. Longitudinal mapping of cortical thickness and clinical outcome in children and adolescents with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2006;63(5):540-549.)
Total gray matter thickness for children with attention-deficit/hyperactivity disorder (ADHD) compared with controls. (Adapted from Shaw P, Lerch J, Greenstein D, et al. Longitudinal mapping of cortical thickness and clinical outcome in children and adolescents with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2006;63(5):540-549.)
1. Children who remained impaired at follow-up had thinner gray matter in the medial PFC at the beginning of the study.
2. Children who grew out of the disorder showed a normalization of the gray matter thickness in the right parietal cortex.
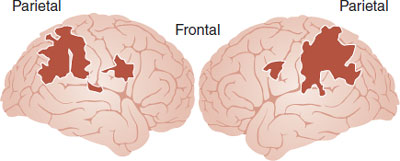
FIGURE 20.9  Regions of significantly greater activation in healthy subjects relative to the attention-deficit/hyperactivity disorder group during a target detection task. (Adapted from Tamm L, Menon V, Reiss AL. Parietal attentional system aberrations during target detection in adolescents with attention-deficit/hyperactivity disorder: event-related fMRI evidence. Am J Psychiatry. 2006;163(6):1033-1043.)
Regions of significantly greater activation in healthy subjects relative to the attention-deficit/hyperactivity disorder group during a target detection task. (Adapted from Tamm L, Menon V, Reiss AL. Parietal attentional system aberrations during target detection in adolescents with attention-deficit/hyperactivity disorder: event-related fMRI evidence. Am J Psychiatry. 2006;163(6):1033-1043.)
These results imply that the normalization of the parietal cortex may be a compensatory activation of the posterior attentional network. Indeed, research suggests that the parietal cortex may play a greater role in attention than previously considered. Imaging studies conducted while the subjects attempted to detect and respond to the presence of an infrequent stimuli (a variation on a CPT) showed greater activation of the bilateral parietal lobes in the controls compared with patients with ADHD (Figure 20.9).
NEGLECT SYNDROME
There is other evidence that the parietal lobes are important for good attention. Parietal lesions can cause a neglect syndrome in which patients ignore objects, people, and even parts of their body that are to one side of the center of gaze. The very existence of parts of the body on the ignored side can be denied. The figure shows an example of a patient after a right parietal stroke attempting to copy some drawings. Note how he fails to copy details from the left side of the drawings. It has been proposed that the parietal cortex is involved in attending to objects at different positions in extracellular space.
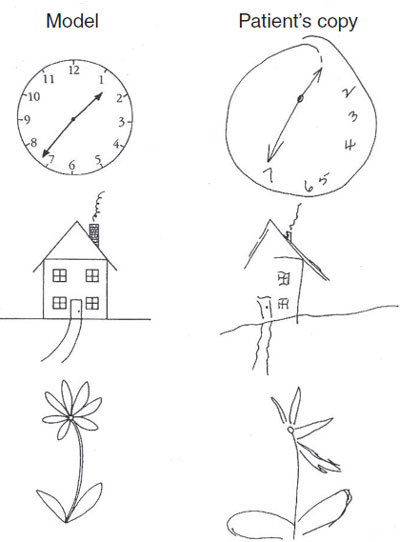
A patient after a right parietal stroke attempts to copy the drawings on the left. (From Springer SP, Deutsch G. Left Brain, Right Brain. New York, NY: Worth Publishers; 1998.)
Some researchers suggest that deficits in time perception are an integral feature of ADHD. Children with ADHD are known to have problems with temporal information processing and the timing of motor tasks. Clinical tests such as estimates of time duration or the reproduction of timed sequences are frequently impaired in children with ADHD. The finger tapping studies by Ben-Pazi provide a specific example of this problem. Children were asked to replicate the same frequency of the presented stimuli by tapping the space bar on a computer. Children with ADHD were less capable of replicating the stimuli and tended to tap faster than the stimulus presentation—getting ahead of themselves.
Figure 20.10A, B shows a comparison between a healthy control and one with ADHD. Note how the healthy control accurately replicates the same frequency of the stimuli, whereas the child with ADHD was responding at a faster frequency. The propensity to hasten the response is greater for children with ADHD (Figure 20.10C). The authors speculate that the rhythmic tapping problems reflect an abnormal oscillatory mechanism for those with ADHD.
These rhythmic motor abnormalities may represent a larger timing problem for patients with ADHD. In other words, the problem is greater than just replicating the tapping of a metronome. The problems with timing may contribute to the impairments seen with higher cognitive skills required to plan and complete a project. Inconsistencies in performance, responding too fast or too slow, and procrastination are behaviors that may be impaired due to temporal processing deficits. For example, patients with ADHD typically overestimate the time left to finish a project. In short, patients with ADHD may have trouble with project planning and completion due to problems getting into a good rhythm and maintaining a consistent pace.
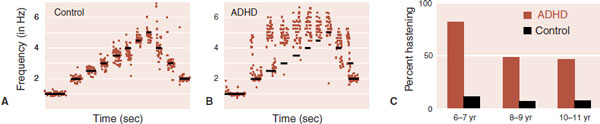
FIGURE 20.10  The stimulus to replicate is represented by the black lines in (A) and (B). The responses by an unaffected child and one with attention-deficit/hyperactivity disorder (ADHD) are shown with brown dots. C. The percentage of children who hasten their responses by tapping too quickly. (Adapted from Ben-Pazi H, Shalev RS, Gross-Tsur V, et al. Age and medication effects on rhythmic response in ADHD: possible oscillatory mechanisms? Neuropsychologia. 2006;44:412-416.)
The stimulus to replicate is represented by the black lines in (A) and (B). The responses by an unaffected child and one with attention-deficit/hyperactivity disorder (ADHD) are shown with brown dots. C. The percentage of children who hasten their responses by tapping too quickly. (Adapted from Ben-Pazi H, Shalev RS, Gross-Tsur V, et al. Age and medication effects on rhythmic response in ADHD: possible oscillatory mechanisms? Neuropsychologia. 2006;44:412-416.)
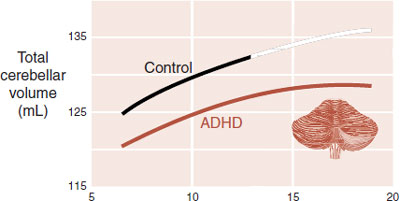
FIGURE 20.11  Children with attention-deficit/hyperactivity disorder (ADHD) have smaller total cerebellar volume compared with unaffected controls. (Adapted from Castellanos FX, Tannock R. Neuroscience of attention-deficit/hyperactivity disorder: the search for endophenotypes. Nat Rev Neurosci. 2002;3(8):617-628.)
Children with attention-deficit/hyperactivity disorder (ADHD) have smaller total cerebellar volume compared with unaffected controls. (Adapted from Castellanos FX, Tannock R. Neuroscience of attention-deficit/hyperactivity disorder: the search for endophenotypes. Nat Rev Neurosci. 2002;3(8):617-628.)
The cerebellum, traditionally conceptualized as controlling motor coordination, has been identified as a possible culprit in the etiology of ADHD. Studies such as those from Rapoport’s laboratory have documented smaller cerebellum volumes in patients with ADHD (Figure 20.11). Likewise, stimulant medications are known to activate the cerebellum. Finally, the cerebellum is believed to play an important role in timing responses. Taken together, these findings suggest that patients with ADHD may have impaired timing mechanisms, which may be due to cerebellar dysfunction.
In summary, it is clear that the PFC and striatum play large roles in the pathophysiology of ADHD. More recent studies suggest that the parietal cortex and cerebellum may also contribute to the problems patients experience.
Long-Term Effects of Stimulants
There are two kinds of stimulants widely used in our society. The first, cocaine and methylphenidate, are primarily obtained illegally on the street. The second, methylphenidate and amphetamine, are available with a prescription. Both classes of medication produce an outpouring of DA. One of the ironies of psychiatry is that the first group is studied by substance abuse clinicians, while the second group of stimulants is studied by clinicians treating ADHD. To a large extent, the two groups are focusing on different aspects of the effects of DA stimulation.
FIGURE 20.12  Prospective study of cortical thickness at the left middle/inferior frontal gyrus for 43 youths with attention-deficit/hyperactivity disorder. (Adapted from Shaw PS, Sharp WS, Morrison M, et al. Psychostimulant treatment and developing cortex in ADHD. Am J Psychiatry. 2009;166(1):58-63.)
Prospective study of cortical thickness at the left middle/inferior frontal gyrus for 43 youths with attention-deficit/hyperactivity disorder. (Adapted from Shaw PS, Sharp WS, Morrison M, et al. Psychostimulant treatment and developing cortex in ADHD. Am J Psychiatry. 2009;166(1):58-63.)
A recent multicriteria decision analysis of drug harm in the United Kingdom compared harm to the user for 20 drugs of abuse. The top three harmful drugs were crack cocaine, heroin, and methamphetamine. The next three were alcohol, cocaine, and amphetamine. Four of the top six harmful drugs are central nervous system stimulants. On the other side of the academic isle is research showing that stimulant medication may actually “normalize” some structural abnormalities in the brain. So on the one hand, stimulants of abuse damage the brain (see Figure 12.11), while on the other hand stimulant medications seem to normalize the brain. How can this be?
The difference appears to be this: when the subjects are analyzed. The substance abusers are evaluated once they are off the drugs. The stimulant users—typically patients with ADHD—are usually assessed on the medication. Almost no studies in the ADHD literature compare the effects on the brain of subjects who stay on the medication with those who stop it. Figure 20.12 shows the only exception.
Cortical thickness, which we know is thinner for patients with ADHD (see Figure 20.8), is normalized by regular stimulant use as shown in Figure 20.12. However, those patients who stopped the medication between the ages of 12.5 and 16.4 experienced a more rapid thinning of their cortical thickness in the left frontal lobe—an area of importance in ADHD. Clearly the “normalization” is the result of gene expression turned on by the stimulant medication. When the stimulants are stopped, the genes too shut down and the cortex thins. The relevant question is this: what effect have the medications had on the brain in the long term?
This is an important question because more people are taking more stimulant medications for a longer period of time, and what will their brains look like when the medications are discontinued? Will the brain resume the structure it would have had without any exposure to medication—or will it be worse—or will it be better? The importance of this question is highlighted by recent studies finding increased incidence of Parkinson’s disease in addicts abusing methamphetamine. And, more troubling is a large, but as yet unpublished analysis looking at the use of diet pills in the sixties and seventies and later problems in the nineties. Patients who had taken benzedrine and/or dexedrine to lose weight were 60% more likely to develop Parkinson’s disease as adults. More long-term studies are needed.
QUESTIONS
1. All of the following are true about continuous performance tasks (CPTs), except
a. They give an estimate of a subject’s ability to attend.
b. Scores change with age.
c. Treatment will affect the scores.
d. Elderly subjects perform worst.
2. A delayed-response task measures
a. The subject’s capacity to delay gratification.
b. Impulsivity.
c. Working memory.
d. Relative DA activity at the NAc.
3. The goal of neurofeedback is for the subject to improve their attention by spending more time in which rhythm?
a. α.
b. β.
c. θ.
d. Δ.
4. Stimulant medications improve attention and concentration through the following mechanisms, except
a. Increase NE efflux in the striatum.
b. Increase NE efflux in the PFC.
c. Increase activity in the cerebellum.
d. Increase interest in new activities.
5. Activity at the NAc (or striatum) helps explain all of the following, except
a. Drug addiction.
b. Impulsivity
c. Working memory.
d. Adolescent behavior.
6. Children who fail to grow out of ADHD show all of the following, except
a. Thinner total gray matter.
b. Compensatory thickening of the parietal gray matter.
c. Smaller total cerebellum volume.
d. Less prefrontal gray matter.
7. Which structure is associated with which finding in ADHD?
1. PFC |
A. Compensatory gray matter thickening |
2. Cerebellum |
B. Temporal processing |
3. NAc |
C. Working memory |
4. Parietal cortex |
D. Delay of gratification |
See Answers section at the end of the book.