Even miracles take a little time.
Thirty-six-year-old Maria had been married for three years. Maria was a medium-framed woman with brown hair and green eyes who had the tendency to carry a little extra weight around her middle. As soon as she met her husband, they decided to begin their family. Unfortunately, Maria’s PCOS had something else in mind. Maria’s periods had never been very regular, and her cycles ranged from thirty-three to forty-three days. Maria also suffered from some of the other characteristics of PCOS. Last year, she had undergone a multitude of laser sessions to remove unwanted facial hair. Her joints ached on a daily basis, and she had various allergies. Maria’s ultrasounds showed the classic string-of-pearls appearance. Maria had Type 1 classic PCOS. Her factors included high androgens, ovulatory dysfunction, insulin resistance, and inflammation.
After trying to conceive for a whole year, not only was Maria still not pregnant, it also seemed more and more likely that she wasn’t ovulating very often at all. Her friends all seemed to become pregnant within a month or two, which only made matters worse. Every pregnancy announcement felt like a blow to the chest.
Concerned, Maria began tracking her cycle days carefully on a calendar, taking her temperature faithfully each morning and plotting it precisely on a graph. Her temperature line was a long jagged pattern and didn’t look like the beautiful two-sectioned charts that she would pore over during her late-night Internet searches. Frustrated, Maria moved on to the expensive ovulation sticks from the drugstore. Stick after stick was used, and nothing made sense: They seemed to constantly be negative, just like her pregnancy tests. In fact, it seemed like all she ever saw was one solid line and a second fainter line, instead of the strong positive line shown on the package. Her frustration grew.
Maria, at her breaking point, visited a local fertility clinic, where she endured several cycles of medication and artificial insemination treatments. These, too, proved unsuccessful. PCOS had wreaked havoc on Maria’s hormones, skin, and body: She was determined that this disorder would not also threaten her ability to have children.
Just like Maria, many women with PCOS have difficulty conceiving. PCOS is the cause of more than seventy-five percent of cases of anovulatory infertility and is a leading cause of infertility in general. Although many women with PCOS do not have any difficulty becoming pregnant, it is definitely one of the most challenging and stressful results of the disorder.
The reason that women with PCOS have trouble conceiving lies in three main concerns:
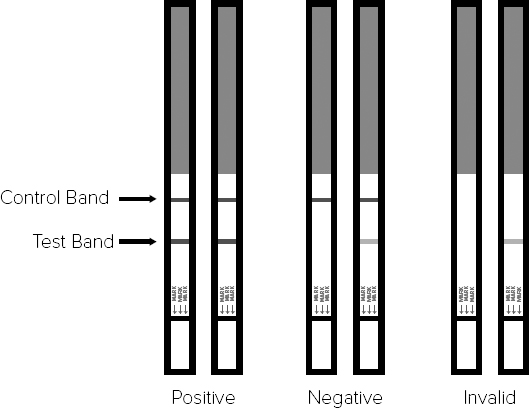
Since one of the three main criteria for PCOS includes delayed ovulation or lack of ovulation, it’s quite easy to see why fertility would be affected in many women: Not knowing when you are ovulating is a definite hurdle on the road to becoming pregnant. To make things even more challenging, ovulation prediction kits are often completely inaccurate in women with PCOS. The hormonal marker that is detected with ovulation prediction kits (OPK) is the luteinizing hormone (LH). The control strip of an OPK turns a solid color. The second line measures LH. When LH surges, the second line should turn as dark as the first line. A second line that is lighter than the first is not considered to be a true positive (Figure A-1). In PCOS, LH is often high at unusual times of the cycle. As a result, there can be false positives. OPKs may never register truly positive for women with significant female hormone imbalance and irregular ovulation. This just adds to the massive stress that goes along with trying to conceive.
In addition to not being able to use the most convenient at-home method to detect ovulation, many women like Maria may go several months without ovulating at all. In such cases, there may be little way to know when the most fertile time is coming. Women in these groups have to try to conceive without knowing when is the best time to get pregnant. As such, it’s pretty clear why it’s no easy to task to make a baby when you have PCOS. Another factor is the egg quality isn’t quite what it should be in women with PCOS, as the abundance of testosterone, insulin, and anti-Mullerian hormone alters the structure and function of the follicle.
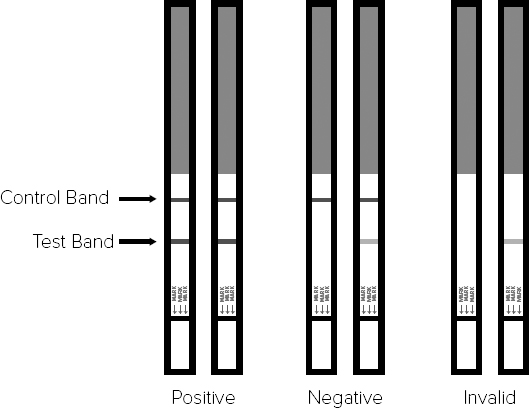
Figure A-1: Hormonal Markers and Ovulation Prediction Kits
When it comes to ovulation detection in PCOS, it’s not all bad news. One way that women with PCOS may be able to detect their fertile time is through the observation of the cervical mucus. After the menstrual period, a follicle should grow in preparation for ovulation and a dominant follicle will be selected. As the follicle grows, it produces increasing amounts of estrogen. Estrogen stimulates the cells of the cervix to produce a special type of mucus, known as “fertile mucus.” This mucus is very similar in texture to that of an egg white. It’s slippery and stretchy and can often be noticed when wiping (Figure A-2). At times of the month when fertility is low, the cervical mucus may range in texture from sticky to creamy. Watery cervical mucus is considered to be the second most fertile compared to the egg white texture. So go ahead and try to conceive if you see either of these two types of mucus!

Figure A-2. Testing Cervical Mucus. Copyright Menstrupedia.
When you have PCOS, there are important things you need to know about cervical mucus. When a woman has irregular ovulations, there may be occasions in which the egg begins to grow and release estrogen, and instead of ovulating, it stalls. This initial release of estrogen causes fertile-type cervical mucus to be produced without a corresponding ovulation. This is known as a “false peak.” Some women with PCOS even have fertile-type cervical mucus through their entire cycle. As such, we don’t know that every production of cervical mucus is a true ovulation, but if you’re trying to conceive and you see cervical mucus that is egg white-like in texture, it would definitely be a good idea to try to conceive at that time.
Basal body temperature (BBT) charting is an excellent way to track cycles in women with PCOS. Through this method, we can determine the length of the follicular phase (the period of time when the egg develops in the ovary prior to ovulation) and the luteal phase (the period of time after ovulation before the menstrual period starts). BBT charting is a very valuable tool for any woman with PCOS who is trying to conceive, so she can identify her patterns and check for luteal-phase defects or low progesterone. The downside of BBT charting is that it is not predictive and generally confirms ovulation after it has happened. This is because the basal temperature will rise 0.5–1 degree once ovulation has occurred. In a woman with PCOS, we often see that the first phase of the basal body temperature chart is longer than the typical fourteen days. This is because it takes longer for the eggs to develop under the influence of excess testosterone and LH. Women with PCOS often have a long follicular phase and a short or normal luteal phase. Women in the ovulatory phenotypes, however, may have a normal follicular phase.
You can purchase a basal digital thermometer from any drugstore. The main difference is that most basal thermometers have an additional tenth of a digit and often have a memory that can store your last temperature. However, many women use a regular digital thermometer, which also works very well. Place the thermometer by your bedside and do your best to take your temperature at the same time each morning. Most women use the under-the-tongue method; however, vaginal temperatures are also accurate.
It is important that you take your temperature immediately upon waking, without moving about too much, as this can raise your core temperature. Other things that can decrease the accuracy of your reading are illness, alcohol consumption, insomnia, or taking your temperature at irregular times.
Plot your temperature on a graph. There is a graph for you to print and use on my website at http://drfionand.com/resources/bbtchart. Alternately, there are many wonderful apps available for tracking your basal body temperature—a few are listed in the resources section.
Once you have plotted your temperatures, draw a line connecting the dots on the graph. You should see two distinct patterns within your graph if you have ovulated. Many women with PCOS will not see these two distinct sections, particularly if they have not ovulated. Don’t worry if this is the case. BBT charting is really only a tool to learn more about your cycle. If you don’t ovulate regularly, you should see improvements in your chart as you undergo treatment, and this can be very exciting!

Fortunately, cervical position seems to be an accurate method of ovulation detection for women with PCOS. The cervix, which is the opening that the sperm must pass through to gain entrance into the uterus, will actually change position as a woman enters her fertile time. Although this method sounds difficult, it is actually quite simple. You’ll always want to check your cervical position around the same time each day, as sometimes the cervix will move higher into the vagina at night during sleep. Squatting or propping a foot on the toilet or bathtub can often make it easier to detect the position of the cervix. To check your cervical position, do the following:
At the beginning of your cycle, during menstruation, your cervix will feel very firm, like the tip of your nose, and it will be fairly low down and easier to find. The cervix opens during the period, to allow the menstrual fluid to be released. As you approach ovulation, your cervix begins to move up, deeper into the vagina, and may be harder to locate. As you get close to ovulation, the cervix will soften and will open slightly. After ovulation, the cervix closes, becomes firm again, and moves downward. It will remain closed until the period begins.
If you are attending a fertility clinic or seeing a gynecologist, you may be offered cycle monitoring. Typically, this monitoring involves going into your clinic daily for blood work and ultrasound. If you are menstruating, cycle monitoring will begin on Day 1. For women with PCOS who have irregular menses, cycle monitoring is often done after induction of the period with progesterone.
Bloodwork that is completed on the first day of cycle monitoring often includes follicle-stimulating hormone (FSH), luteinizing hormone (LH), thyroid-stimulating hormone (TSH), estradiol, and progesterone. After Day 1, bloodwork often includes LH, estradiol, and after ovulation, progesterone. To briefly review them, FSH and LH are pituitary hormones. These can indicate the “baseline” of ovarian health. If FSH is high, it can indicate poor egg quality or diminished ovarian reserve. We often see high LH in PCOS. Estradiol should be at a relatively low level on Day 3, and progesterone should be exceptionally low then. Estradiol increases as the follicle grows in preparation for ovulation. Progesterone is released after ovulation occurs.
Typically, cycle monitoring is done early in the morning, as it takes several hours to get the results, and if ovulation is detected, this allows timing of intercourse.
As your cycle progresses, your ovary will select a dominant follicle that is to be ovulated. As the follicle matures, it produces increasing amounts of estradiol, the main form of estrogen. The average estradiol level from a mature follicle is 200 to 400 pg/ml. As estradiol rises, the pituitary senses this and releases a sharp surge of LH, which triggers ovulation. As the doctor sees that the LH is rising, they may let you know that you are about to ovulate, and that this is a good time to conceive. After ovulation has occurred, the egg will burst from the follicle and begin its journey down the tube. The follicle, still in the ovary but now without its egg, transforms into the corpus luteum. The corpus luteum makes a large amount of progesterone for the rest of the luteal phase, after which time it disintegrates.
A small amount of progesterone is also continuously produced by the adrenal glands. As such, the baseline progesterone levels on cycle day 3 are typically around 1.5 ng/ml or less. Once ovulation has occurred, the progesterone levels rise to 10–18 ng/ml or more by seven days after ovulation (see Figure A-4).
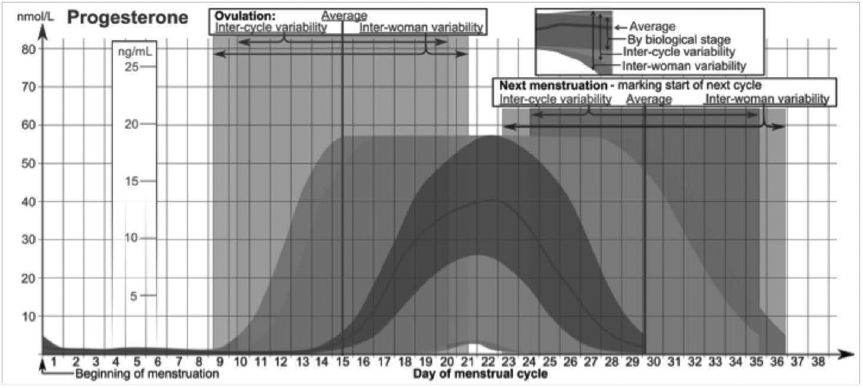
Figure A-4: Progesterone Levels During Menstrual Cycle
In conventional medicine, treatment for fertility in PCOS typically revolves around what is known as ovulation induction, or “super ovulation.” Since lack of ovulation is one of the most important factors impacting fertility in women with PCOS, medications are commonly used to stimulate the ovary to release an egg. However, it’s important to know that for women who already ovulate, this type of medication may not increase fertility very much!
Clomiphene is often the first-line intervention used to treat infertility in PCOS. This medication is known as a selective estrogen receptor modulator and is typically prescribed for five days during the cycle, typically from Day 5 to Day 9. The standard starting dose is 50 mg per day. In many clinics, progesterone will be prescribed after ovulation to help promote implantation. The success rate of clomiphene is approximately ten percent per month for a woman with PCOS who is under thirty-seven years old. For women who ovulate regularly, the success rate is actually only one percent higher than trying naturally.
Clomiphene works by blocking estrogen receptors in the hypothalamus, which is the hormone control center of the brain. With these receptors blocked, the hypothalamus and pituitary gland are tricked into believing that estrogen is low, and they try to make more by stimulating the ovary to produce an egg. If a woman does not ovulate on 50 mg of clomiphene, it is often increased by 50 mg increments during subsequent cycles.
For a medication, clomiphene also has a very long half-life of approximately seven days. That means that only half of the medication will be excreted in a week, resulting in a good amount of it lingering in the system for some time, particularly if cycles are done back-to-back.
Common side effects can include temporary enlargement of the ovaries as well as hot flashes. Some women also experience mood changes, psychiatric concerns, GI effects, breast discomfort, and visual disturbances. Unfortunately, clomiphene also has some anti-fertility effects, including thinning the endometrial lining and drying up cervical mucus, which is not ideal.
Clomiphene is also associated with an increased risk of multiple births. Overall, the chances of conceiving twins on clomiphene is around seven percent, with a one percent chance of conceiving higher-order multiples, such as triplets or quadruplets. Multiple pregnancies are at higher risk than single pregnancies and can be particularly risky in women with PCOS who may have other complicating factors, such as gestational diabetes.
-Clomiphene
-Letrozole
-Gonadotrophins
-Metformin
-Progesterone
-Low-dose aspirin
-Immune-modulating medication
Clomiphene does not appear to be very successful in women who ovulate normally, with only a five percent success rate per cycle (compared to four percent without). In women who have difficulty ovulating, the pregnancy success rate is much higher, ranging from ten to thirty percent. For women who do not have fertility problems, the chance of conceiving on any one cycle is around ten to twenty-five percent.
Many clinics recommend that a couple not complete more than three consecutive clomiphene cycles due to its long half-life as well as the fact that eighty-five percent of successful clomiphene cycles occur within the first three cycles. To make it short, if it doesn’t work in three cycles, it’s pretty unlikely to work after that, and the negative effects may outweigh success. Some clinics, however, will do up to six consecutive cycles.
Letrozole is a medication that is used off-label for fertility purposes. It is actually a medication that has been developed for the treatment of postmenopausal breast cancer, but doctors have found that it can also trigger ovulation if used in a similar way to clomiphene. Letrozole blocks what is known as aromatase, which is an enzyme that converts testosterone to estrogen. As such, the brain perceives a low level of estrogen and then hopefully stimulates ovulation.
Letrozole appears to have a lower side effect profile than clomiphene, as it is excreted much more quickly, and its overall action is different. A Canadian study that was presented at the American Association for Reproductive Medicine Conference in 2005 suggested that there was an increased risk of birth defects for women using letrozole.1 This was countered later by a more detailed follow-up study that found it, in fact, caused a lower rate of congenital malformations (2.4 percent) and chromosomal abnormalities than clomiphene’s 4.8 percent.2
Progesterone is often added to medicated cycles after ovulation, as it helps to prepare the lining for implantation. This is particularly important for women with PCOS, since many have low progesterone-to-estrogen ratios. This low ratio occurs because the first half of the cycle is typically longer than the second half, resulting in a relative excess of estrogen to progesterone.
Progesterone is particularly important in IVF because after the follicles are retrieved from the ovary, the corpus luteum isn’t able to produce enough progesterone because it is punctured when the eggs are retrieved. As such, very high doses of progesterone, such as 400+ mg per day, may be commonly used in women with PCOS who are undergoing in vitro fertilization (IVF).
For patients who have had recurrent miscarriages or implantation failures, some doctors are now prescribing medications to calm the immune system. These include steroids, such as dexamethasone; anti-clotting agents (aspirin or low molecular weight heparin, for instance); and immune modulators (such as IVIG, intralipids, or lymphocyte immunization therapies). One common side effect of immune suppressants in particular is an increased risk of infection. For anti-clotting agents, there is an increased risk of bleeding.
Gonadotropins are injectable fertility drugs that can stimulate ovulation. These stronger drugs are often used when a woman does not respond to, or achieve pregnancy after, clomiphene or letrozole. Gonadotropins are actually forms of FSH and LH, which are the same hormones that are produced by the pituitary gland to stimulate the ovary naturally. Injections usually begin on Day 3 or 4 of the menstrual cycle and last approximately eight to ten days. During injections, patients are carefully monitored through bloodwork and ultrasound to determine the number of follicles and the staging of ovulation.
Once it appears that ovulation is imminent, patients are given a “trigger shot” of human chorionic gonadotropin (hCG) to stimulate ovulation. At this point, intrauterine insemination (IUI) is often performed. These same medications are also used in IVF, which is a more involved process. In IVF, after the trigger shot causes the eggs to mature, they are extracted from the ovary and fertilized and then reim-planted into the uterus.
As injectable gonadotropins are much more direct and powerful than medications such as clomiphene, many more follicles will mature during the cycle. In women with PCOS, who often have an abundance of follicles in the first place, gonadotropins are even more risky.
Women with PCOS are at increased risk for ovarian hyperstimulation syndrome (OHSS) and may produce a large number of follicles on stimulation. OHSS can be a serious condition resulting in severe abdominal water retention and even hospitalization, so women with PCOS must be monitored carefully when using gonadotropins. In women with PCOS, a GnRH agonist called leuprolide is often used to stimulate ovulation instead of hCG, as it reduces risks of hyperstimulation syndrome. Coasting is another method used to prevent OHSS in women with PCOS undergoing IVF. In coasting, gonadotropins are stopped at a certain point, allowing follicles to “coast” and estradiol levels to calm before the trigger shot.
The risk of twins and even triplets or higher-order multiples is also greatly increased with gonadotropins, particularly when IUI is used. This is because in an IVF cycle, one embryo can be selectively transferred back into the uterus. In an IUI with injectables, all eggs that have matured will have the opportunity to be fertilized. As such, women with PCOS are often prescribed very low doses of gonadotropins during an IUI cycle.
Metformin is also commonly used during fertility treatment for women with PCOS. It can be used as a stand-alone treatment, as research suggests that it may increase the number of natural ovulations in women with PCOS. Metformin works by increasing insulin sensitivity, hence reducing the harmful effects of high insulin on the ovary. That said, metformin may not translate into live births and take-home babies. In most trials on this subject, clomiphene and metformin were combined, and in the women taking metformin, there was only a slightly increased rate of live births. However, to counter, there was also an increased rate of miscarriage in metformin groups. As mentioned before, metformin may interfere with one-carbon metabolism and mitochondrial function, and therefore more research needs to be done to fully understand its effects on fetal development. As discussed in chapter 3, the most common side effects of metformin are gastrointestinal, including cramping, nausea, and loose stools.
We have discussed the medications used in conventional fertility care. Now, I’ll outline what happens during the most common fertility clinic procedures for women with PCOS.
Intrauterine insemination is when washed sperm are injected directly into a woman’s uterus. To wash sperm, the sample is taken and individual sperm are separated from the seminal fluid. This helps to remove any dead or unhealthy sperm, mucus, or white blood cells. Also, in order to inject the sperm into the uterus, the seminal fluid must be removed, as it contains prostaglandins that can cause cramping. Normally, the cervix will filter out much of the prostaglandins.
IUI can be useful if there is any issue with male-factor infertility. It can be done naturally or teamed up with medications, such as clomiphene or gonadotropins. As mentioned previously, IUI may not be performed on a woman with PCOS if injectables are given, as there may be multiple follicles that have matured and the risk of multiples would be much higher.
You’ve probably heard quite a lot about IVF, as it’s definitely the most popular and well-known fertility procedure. IVF involves the use of gonadotropins (injectables) to help the ovary produce multiple follicles and eggs (see Figure A-5). The follicles are then retrieved from the ovary through the wall of the vagina while the patient is under sedation.
The eggs are then fertilized in the laboratory and matured for either three or five days. This is where the term “test-tube baby” came from. After the embryos have developed, they are then transferred selectively back to the uterus.
Most modern clinics will do a single embryo transfer to reduce the likelihood of twins and multiple births, but in cases where there has not been success in the past, or when the embryo quality does not look ideal, more than one embryo may be transferred.
During IVF, embryos are graded on their quality, which is decided upon by the number of cells and overall structure. An embryo that has developed to five days and has reached the stage known as blastocyst is considered to have the best chance of success in implantation.
Now we enter the fascinating world of how to treat subfertility in PCOS naturally. Note that I said subfertility, rather than infertility. In almost all cases, women with PCOS can conceive. It simply takes the right treatment.
As is always the case, the first step is to address nutrition and lifestyle. As outlined in chapter 9, women with PCOS oft en do best eating foods that create lower insulin responses and on a plan that is high in vegetable intake and moderate in high-quality lean proteins and healthful fats. This way of eating lowers insulin levels, reducing any harmful impact on the ovaries. Exercise is also a helpful strategy for women with PCOS who are trying to conceive. I oft en recommend a moderate strength-training program three to four times per week.
In many cases, treatment with nutrition and exercise are all that is needed for women with PCOS to be able to conceive. In other cases, it may not be enough. Fortunately, there are some supplements that can be exceptionally helpful for women with PCOS when it comes to getting pregnant.
Inositols are profoundly important for women with PCOS who are trying to conceive. Studies have suggested that inositol plays a crucial role in cell growth and development. Myo-inositol regulates the secretion from glands, such as the ovaries, and may be responsible for important signals essential for egg development. Numerous studies have confirmed that the presence of myo-inositol in the follicular fluid has a positive correlation with egg quality and maturation, particularly for women with PCOS.3
When it comes to fertility, inositol has been involved in some fascinating research in the PCOS world. A study published in 2012 in the Archives of Gynecology and Obstetrics found that a combination of D-chiro-inositol (DCI) and myo-inositol in a ratio of 1 to 40 was able to improve egg quality and pregnancy rates in women with PCOS undergoing IVF.4
Overall, it has been found that myo-inositol can improve ovarian responsiveness to the natural hormones FSH and LH that are made by a woman’s pituitary gland and can help to reestablish timely ovulation. This can increase the chances of a spontaneous pregnancy. Other research has found that myo-inositol is simply an excellent “ovary vitamin,” as it can improve follicle health and implantation rates during IVF cycles for women without PCOS as well.5
I can recall one patient in particular, Suzanne, a twenty-seven-year-old woman with PCOS, who after trying to conceive for over a year began on a course of myo-inositol and swiftly became pregnant within just two months. She was amazed at how quickly it worked for her and at how relaxed she felt with the treatment. Myo-inositol has another wonderful benefit: It reduces anxiety. This is always helpful for those on the stress-inducing infertility journey.
The inositols are generally very well tolerated. Rare side effects can include mild gastrointestinal upset and/or loose stool.
D-chiro-inositol (DCI) has been used in combination with myo-inositol for the treatment of infertility. It seems that DCI has quite a beneficial effect on insulin resistance in PCOS. A study looking at fifty-four women with PCOS provided increasing doses of DCI, ranging from 300 to 2,400 mg of DCI.
Unfortunately, however, women in the groups receiving the three highest DCI doses had poorer egg quality and lower-quality embryos in fertility treatment.6 As such, and as the study noted above suggests, DCI may be best utilized in fertility patients at lower doses. That being said, it appears that DCI is, in fact, a beneficial product for women with PCOS who are trying to conceive, particularly when used in the recommended doses. DCI is generally very well tolerated. Rare side effects can include mild gastrointestinal upset and/or loose stool.
It’s currently thought that the optimal ratio of myo-inositol to DCI for fertility may be 40:1. This is the ratio found in plasma. This specific ratio appears to be more effective than either myo-inositol or DCI alone when it comes to metabolic health and ovulatory function without negatively impacting oocyte health. This would be the equivalent of 4 grams of myo-inositol along with 100 mg of D-chiro-inositol per day, often in two divided doses.
N-acetyl cysteine (NAC) is another supplement that has been researched for the treatment of PCOS-related infertility. NAC is a compound that comes from the sulphur-containing amino acid L-cysteine and has been traditionally used to thin out mucus during bronchitis or other chest conditions. It has also been used in conventional medicine to prevent liver damage from alcohol and acetaminophen. This same compound has been researched for fertility in PCOS.
One of the first studies on NAC for fertility in PCOS was a 2005 study on women who previously did not ovulate when given clomiphene. Giving NAC to these women in addition to the clomiphene increased the rates of ovulation and pregnancy significantly.7 Another study repeated this finding in 2012, discovering that in a group of 180 women with PCOS, 1.2 grams per day of NAC plus clomiphene improved the number of follicles retrieved, the thickness of the endometrial lining, and ovulation and pregnancy rates when compared to clomiphene alone.8
The reason that NAC seems to be such a powerful therapeutic treatment for PCOS lies in several properties. It is a powerful antioxidant and increases the amount of the master antioxidant glutathione produced in the ovary, which is crucial for fertility. It also increases insulin sensitivity, is anti-inflammatory, and reduces serum testosterone levels and the free-androgen index.9 Women with high androgens, anovulation, insulin resistance, and inflammation can all benefit from NAC.
Rare side effects of NAC are heartburn, nausea, or changes in bowel movements. Many patients find that taking it with food is very helpful in preventing these side effects.
Vitamin D is a crucial compound for women with PCOS who wish to achieve pregnancy. Although commonly known as a vitamin, it is actually an important hormone involved in many processes of the reproductive cycle. Vitamin D receptors have been found in the ovary, endometrium, and placenta. A deficiency of this hormone can even contribute to the arrested development of follicles in the ovary of women with PCOS, stopping ovulation. Mice whose vitamin D receptors have been genetically removed demonstrate severe abnormalities in the folliculogenesis process (the growth of the eggs).
In a study on 368 women undergoing IVF, the patients that were deficient in vitamin D had lower pregnancy rates.10
Deficiencies of vitamin D have been linked to alterations of LH and sex hormone-binding globulin, testosterone levels, insulin resistance, and serum insulin levels in women with PCOS. Women with deficiencies of this key vitamin have even been found to have close to half the success rate in IVF cycles compared to women with optimal vitamin D levels. Vitamin D receptors also play an important role in estrogen production in the ovary, and it is known that vitamin D deficiency is also linked very clearly to insulin resistance in PCOS.
So now that it’s clear that women with PCOS need to have excellent vitamin D status in order to achieve pregnancy, my general recommendation is that women with this condition should have their vitamin D levels checked regularly. A goal for women with PCOS should be 50–70 ng/ml (or 124–175 nmol/l).
The best form of vitamin D is vitamin D3, also known as cholecalciferol, which is the natural form of D that your body makes from sunlight. The vitamin D3 that is readily available is usually manufactured from sheep’s lanolin, which provides the same type of vitamin D that your body manufactures. For deficient patients, 4,000 IU may be taken daily to restore levels.
Vitamin D2, which is often manufactured from a yeast source, is generally not as well absorbed as D3. Studies indicate that D2 is much less potent and has a shorter duration of action than vitamin D3. Overall, D3 has been estimated to be around three times as effective.
Historically, however, if a patient is severely deficient, single large doses of vitamin D can be prescribed in 50,000 IU capsules by a physician. Women with all expressions of PCOS should pay close attention to their vitamin D levels.
Side effects of vitamin D are extremely rare. However, it is not recommended to have levels above the reference range until there is more long-term data.
Berberine is a newer compound to the PCOS fertility scene. It’s an active component of several different plants ranging from barberry to goldenseal and is especially prominent in a variety of herbs rooted in the traditional Chinese medicine profession, such as Rhizoma coptidis and philodendron. In traditional Chinese medicine, berberine has been used to improve insulin resistance and treat diabetes for centuries. Modern studies have suggested that berberine actually has an action similar to metformin as an insulin sensitizer. Now, research suggests that this compound may also have an application for PCOS-related infertility.
A 2013 study on 150 women with PCOS who were undergoing IVF investigated the use of berberine. In this trial, the groups of women were placed either on metformin, berberine, or a placebo. Both metformin and berberine similarly improved the pregnancy rate and reduced ovarian hyperstimulation syndrome. Berberine did even better: It specifically improved live birth rate as well.11 Overall, it appears that berberine may be a viable alternative to metformin for the treatment of infertility in women with PCOS and is particularly useful for women who suffer from insulin resistance or who are overweight. Side effects of berberine include gastrointestinal upset and loose stool.
Grifola frondosa (also known as maitake mushroom) is a mushroom that has many different medicinal uses. Apart from its powerful effects on the immune system, maitake is a useful treatment for PCOS-related infertility. In 2010, a study conducted on eighty Japanese patients with anovulatory PCOS found that Grifola frondosa induced an ovulation rate of 76.9 percent at a dose of 250 mg of dried maitake mushroom powder per tab, at a dose of 3 tabs 3 times daily between meals.12 For patients who had previously been resistant to clomiphene, adding maitake to their regimes resulted in an ovulation rate of seventy-five percent.
Maitake’s positive action on ovulation is thought to be from its effects on insulin resistance, which have been well researched, as it is commonly used for the treatment of diabetes. As such, it’s very helpful for women with insulin resistance. Maitake mushroom is also well suited to women with high androgens, as it has been found to exert anti-androgenic effects.
Many women with PCOS have low progesterone levels, which commonly occurs due to poor follicle health and delayed ovulation. Overall, there is a relative excess of estrogen, given that the follicular phase is often quite lengthy, and the amount of progesterone supplied in the shorter luteal phase may not be enough to sustain a pregnancy. As such, many women with PCOS find it helpful to use natural progesterone products that are available over the counter. It is important not to use these products prior to ovulation, however, so a woman should be able to identify her ovulation timing before utilizing them. The cream is generally applied to the capillary rich surfaces, such as the face, neck, chest, breasts, inner arms, or palms.
Rotate the area of application daily to avoid saturating the same area with the cream. It is very important to cycle progesterone on and off, unless specifically prescribed by your doctor, to avoid creating a continuously high level of progesterone, which could inhibit ovulation. Natural progesterone cream can be used by women who don’t ovulate regularly or have luteal phase defects. It can also be used in women who don’t ovulate at all, but this is more complex and should be supervised by a health-care practitioner. Finally, it can also be used in early pregnancy to assist in preventing miscarriage. For women who have had or who have a family history of female reproductive or breast cancers, all hormones should be used under strict supervision of a physician.
Vitex agnus-castus is a beautiful plant with some remarkable properties. Also known as chaste tree or chasteberry, it is a very popular herb in women’s health. As described in detail in chapter 6, it is believed that vitex works primarily on the pituitary gland and the opiate system in the brain.
Vitex is a plant that may be either beneficial or detrimental to women with PCOS when it comes to fertility. There is some evidence that vitex can either reduce or increase the amount of prolactin, depending on the dosage used. Typically, vitex is most effective when a woman has a higher-than-average prolactin level, as prolactin hinders ovulation, disrupting the natural production of fertility-promoting progesterone.
Vitex is thought to be helpful for luteal phase defects, which are common in PCOS. Luteal phase defects are the result of low progesterone levels. A weak luteal phase from low progesterone can make it difficult for the embryo to implant successfully in the womb. In some cases, luteal phase defect may even be caused by “hidden” elevated prolactin levels, also known as latent hyperprolactinemia. One study found that in a group of fifty-two women with luteal phase defect due to latent hyperprolactinemia, there was a significant increase in the length of the luteal phase with vitex therapy.13 As previously discussed, vitex can also act to slow the pulsing of GnRH due to its effects on the hypothalamic neurons, a benefit for women who have pituitary-related ovulatory problems.
With respect to dosing and more about indications, please see the detailed information on vitex in chapter 6.
Black cohosh (Cimicifuga racemosa) is an intriguing women’s health botanical that provides clear benefits for the treatment of infertility in PCOS. An Egyptian study found that this cluster-flowered member of the buttercup family might be comparable to clomiphene in ovulation induction in women with PCOS. The study provided one group of women with black cohosh at 20 mg daily for ten days and a second group of women with clomiphene. The result for the cohosh group was similar to the clomiphene group with respect to FSH/LH ratios. Progesterone levels and endometrial thickness were both higher in the black cohosh groups. Most importantly, the pregnancy rate was also higher.14
Cohosh has also been combined with clomiphene in research, and it has been found to decrease some of the negative side effects associated with the drug, such as thin lining and scanty cervical mucus. In the groups where cohosh was combined with clomiphene, there was a thicker endometrial lining, increased progesterone, and an increased clinical pregnancy rate.15
Additionally, black cohosh possesses anti-inflammatory properties, which may be beneficial for PCOS. It’s important to note that in some patients, however, black cohosh may raise liver enzymes. As such, if you are using this herb, you should be monitored by a physician or naturopath to ensure that you can tolerate it. If you have liver disease, black cohosh may not be a good choice for you. Black cohosh may be particularly helpful for patients who have female hormonal imbalance and ovulatory dysfunction as a stronger factor in their case.
Dosing of black cohosh for fertility is typically 20 mg per day from Day 1 to Day 10 of your cycle.
Resveratrol is a natural polyphenol that is found in grapes, berries, nuts, and red wine. It has been widely studied for its benefits to the cardiovascular system and for its effects against cancer.
Resveratrol appears to stop the overgrowth of ovarian theca cells. In a PCOS ovary, there is an overgrowth of these testosterone-producing cells. These cells are involved in the enlarged, cystic appearance of the ovaries in PCOS, as they hinder ovulation. Resveratrol can regulate the overgrowth of theca cells, helping to normalize the structure and function of the ovary in women with PCOS.
It is also anti-inflammatory and reduces clotting, making it helpful for endometrial lining health and implantation. Typical dosages of trans-resveratrol range from 100 to 250 mg per day. Resveratrol can thin the blood, so it should not be combined with other blood thinners unless under the supervision of a doctor.
Coenzyme Q10 (CoQ10) is a mitochondrial antioxidant and is definitely one of the most popular supplements to treat infertility in general. The mitochondria are the powerhouses of the cell, and their health is crucial to the health of the oocytes. Healthy oocytes contain a good number of mitochondria with healthy DNA, and when an embryo is formed, the mitochondria from the mother are transferred to the embryo, whereas those from the sperm are not, meaning that mitochondrial health has a large role to play in the formation of a healthy embryo. Women with PCOS often have concerns about egg quality due to the impact of androgens and insulin resistance on their ovaries. Supporting the mitochondria may provide great benefits for the diminished ovarian health common in PCOS.
A study published in March of 2014 investigated the use of CoQ10 in 101 women who suffered with infertility from PCOS and were resistant to clomiphene treatment. The CoQ10 group had a greater number of mature follicles, better endometrial lining, and a much greater ovulation rate (65.9 percent compared to 15.5 percent in the control group). The pregnancy rate was also higher in the CoQ10 group (37.3 percent compared to six percent in the control group).16
Overall, this study concluded that CoQ10 was an effective treatment for women with PCOS who are resistant to clomiphene. CoQ10 may be beneficial for all phenotypes of PCOS who are trying to conceive, particularly for women over thirty-five years of age.
My personal preference when it comes to CoQ10 for fertility is to use the reduced form, ubiquinol. This is the anti-oxidant form of CoQ10 and may be better absorbed than its counterpart ubiquinone (as shown in Figure A-6).
Both nutrients, however, can provide benefits, as ubiquinone can be converted into ubiquinol. If you are only able to get CoQ10, rather than ubiquinol, you can use a higher dosage. I would typically recommend 600–800 mg per day of ubiquinone and 200–300mg per day of ubiquinol.
Side effects of CoQ10 are rare, but can include a mild reduction in blood pressure.
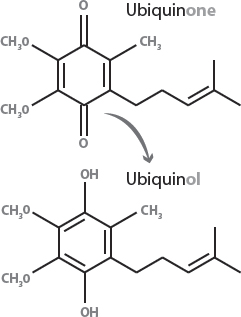
Figure A-6: Ubiquinone and Ubiquinol
Moira was a forty-two-year-old lean woman with PCOS who ovulated regularly, yet suffered from hirsutism and anxiety. Despite being in her forties, she still had numerous small follicles on her ultrasounds. When Moira was younger, she had exceptionally high DHEA levels, but these had decreased with age. Moira had been trying to conceive for two years without any luck. After trying both IUI and IVF, she felt frustrated. Doctors told her that she appeared to have a good follicle count for her age, yet these eggs didn’t seem to be of good quality. She was told that women with PCOS who are in their forties often retain more follicles but that the quality still declined with age.
After seeing Moira in the clinic, we found that her insulin levels were fairly normal; however, her vitamin D was exceptionally low. I began her on a regimen of 300 mg of ubiquinol for mitochondrial support, myo-inositol at 4 grams daily, and 5,000 IU of vitamin D per day. Knowing that focusing on her egg quality would be key, we also increased overall nutrition, including supplementing omega-3 fatty acids and following a whole-food, low insulin index, gluten-free diet. Within four months, Moira conceived naturally and carried to term a beautiful baby girl.
As we have learned, the follicles develop over many months prior to a cycle, which is why it takes several months to work on egg quality in women with PCOS. In Moira’s case, she conceived once the cycles of folliculogenesis brought forth new, healthy follicles.
White peony, or Paeonia lactiflora, is a mainstay in women’s health in traditional Chinese medicine. White peony has been shown to lower androgen levels in vitro. A compound known as paeoniflorin inhibits the production of testosterone and promotes the aromatase enzyme that converts testosterone into estrogen.
Similarly to vitex, peony may be helpful in decreasing serum prolactin levels. Other research has found that peony, as part of a traditional Japanese medicine compound, helps to promote ovulation.17
Often combined with peony for the treatment of PCOS, licorice has myriad fertility benefits. This herb is both anti-inflammatory and anti-androgenic.
A small trial found that licorice root significantly decreases testosterone levels in women. Licorice contains phytoestrogens, glycyrrhizin, and glycyrrhetic acid, which have a weak anti-androgenic effect. It also provides benefit for the adrenals. This herb is considered safe while trying to conceive, so it can be an excellent choice for women with PCOS who are experiencing infertility. It’s important to note, however, that it should be used with caution, as it may increase blood pressure. Licorice is most beneficial for women with androgen excess. Peony and licorice formula is typically taken at a dosage of 2 grams 3 times per day, and up to 4 grams 3 times per day.
Maria, our woman with PCOS from the beginning of the chapter, came to see me after her three-year fertility journey. As she still wasn’t ovulating regularly, we made some significant changes to her diet and exercise program and added some supplements and herbs. For Maria, we used peony root and licorice daily to regulate her hormones and improve ovulation. She also took berberine to reduce insulin resistance and myo-inositol for its many benefits. Following the diet for insulin resistance outlined in chapter 9, Maria was able to lose ten inches from her waist and twenty pounds. Over time, her cycles began to shorten and regulate. After only six months, she became pregnant. Nine months later, she delivered an adorable baby boy named William.
Anti-Androgenic |
Paeonia |
Ovulation Promoting |
Myo-inositol |
Insulin Resistance |
DCI |
Stress/Adrenal |
Licorice |
Inflammation |
Resveratrol |
Thyroid |
Iodine (low dose only) |
Table A-1: Natural Fertility Treatments by Factor
There is a good deal of research on the use of acupuncture to treat infertility in PCOS, much of which has been conducted by Elisabet Stener-Victorin from Sweden, an avid researcher on the effects of acupuncture on PCOS. Studies have found that among other benefits, electroacupuncture may decrease the overabundant nerve growth factor that occurs in PCOS, increase the rate of ovulation, and improve androgens in women with PCOS, which have clear benefits for fertility.18, 19
As we already know, women with PCOS have increased inflammation either in their bloodstream, within the ovary itself, or in other organs of the body, such as the liver. Inflammation is definitely detrimental for fertility. In the earliest stages of pregnancy, it’s important to enter into a calmer type of immunological state. Many women catch colds and flus in the early stages of pregnancy, and this is because the immune system down-regulates its function at that time, allowing the embryo to implant successfully.
With PCOS, women may have more challenges entering into this state, and as such, the immune system may not be in the most optimal situation for conception. Studies have found that women with PCOS have higher circulating levels of inflammatory mediators like C-reactive protein, TNF-alpha, and PAI-1. Treatment of insulin resistance can reduce these inflammatory mediators, and it’s also possible to affect them directly with anti-inflammatory treatments. Miscarriage rates are increased in PCOS, possibly as a result of localized inflammation and insulin resistance or poor egg quality, which is a result of the disorder.
Grape seed extract and pine bark offer a decrease in the TH1-dominant inflammatory responses that can cause difficulty with implantation of an embryo. A high quality omega-3 fatty acid, in addition to its benefits for reducing testosterone, can also mitigate inflammation.
Fish oils are often best sourced from small fish, such as anchovies and sardines. Research also suggests that fish oil can lower androgen levels and should be used in women who have high levels of these hormones. Triglyceride forms of fish oils that are molecularly distilled to remove all heavy metals and environmental toxins are likely the best choice. Also look for a fish oil company that posts their third party batch testing results. For more information on anti-inflammatory approaches, please see chapter 2.
Women with PCOS who are trying to conceive should be checked for mutations in the methylenetetrahydrofolate reductase (MTHFR) gene, as it can be an additional complicating factor in fertility if present. Women with PCOS are particularly susceptible to MTHFR mutations, as the underlying metabolic condition can be additive with its effects.

Figure A-7: Conversion of Folic Acid to Methylfolate Impaired by Mutations in MTHFR
MTHFR can be associated with clotting and recurrent miscarriages, something common in PCOS. A mutation in MTHFR makes it difficult to convert folic acid into methylfolate, the form directly used in DNA repair and cell growth. Up to forty percent of people have a mutation in MTHFR. There are two different variants, MTHFR C677T and MTHFR A1298C. Of the two, the C677T causes a more serious problem in converting folic acid into methylfolate and is more highly associated with pregnancy losses.
If you are unable to get testing for MTHFR (see Resources section in Appendix E), it’s important to ensure that you are taking a prenatal vitamin that contains the type of folate that is active and can be used by cells even if you do have this mutation. L-5-methylfolate is the preferred source of folate for women with PCOS who are trying to conceive. In addition, as mentioned in chapter 3, metformin affects one-carbon metabolism and methylation, so extra precaution should be taken for women who have MTHFR and are taking metformin.
Sheri had Type 2 PCOS and a strong family history of high blood pressure and strokes. She had recurrent miscarriages, having experienced four, all of them quite early in pregnancy. On a subsequent pregnancy, after learning that she was homozygous for MTHFR C677T (the most severe form of MTHFR), she was able to carry the baby to term with the help of L-5 methyltetrahydrofolate and some gentle anti-clotting therapy: in her case, omega-3 fish oil.
For a thorough description of supplements for women who have problems with thyroid health, please see chapter 7. Subclinical hypothyroidism or sluggish thyroid function can increase the risk for miscarriage and developmental problems with babies.
As is generally recommended for women with PCOS, the American Thyroid Association recommends that TSH should be below 2.5 miU/ml for the first trimester. Some of the therapeutics mentioned in chapter 7 are not suitable for women who are trying to conceive. Table A-1 offers a listing of fertility-safe thyroid treatments; however, please consult with a practitioner on their suitability for your case.
Infertility is a very stressful condition. It involves facing the potential loss of mother-hood and all of the dreams that go along with life as a mother. Infertility also erodes our self-esteem and even our inherent value as women. Most girls grow up dreaming of being a mother, and when a woman learns that she may not be able to bring children into this world, it can be devastating. I would tell you to reach out and get all of the support that you can as you go through this difficult journey, whether that be through joining support groups or through a trusted counselor or therapist.
Although having children is a very real and important dream, fertility can have meaning beyond that of bringing a child into existence. My teacher Dr. Randine Lewis says, “You can give birth to any number of wonderful things in this world with your creative gifts.” For women struggling with their fertility, reconnecting with the feminine, creative forces within can give back part of what we feel has been lost. Many women find that embarking on a creative project such art, writing, crafting, or a new creative business venture can provide a great deal of emotional healing as they navigate this challenging terrain.
Overall, the picture can be quite complex for a woman with PCOS who is attempting to get pregnant, depending on her individual characteristics. It’s important to keep in mind that the vast majority of women with PCOS do have the ability to conceive, although the process often takes awhile longer.
Like Maria, Sheri, or Moira, the right treatment is often the boost that is needed to help a woman with PCOS get and stay pregnant. I always tell my patients that PCOS is associated with subfertility, rather than infertility. Stay hopeful, no matter how long you’ve been trying. Most women with PCOS can and do achieve pregnancy!
Mary had suffered many years while trying to conceive due to difficulties associated with her PCOS. She went through years of fertility treatment and finally achieved her goal after three miscarriages. She wanted this pregnancy to be as healthy as possible. Mary had always struggled with her weight and had managed to lose twenty pounds before becoming pregnant. She was worried that pregnancy would cause her to gain all of this weight back. She also worried about gestational diabetes, knowing that diabetes ran in her family history. She didn’t have any friends who had PCOS who were pregnant, so she came into the clinic to see what she could do to stay healthy. With the right diet, exercise, and nutritional program, she was able to have a healthy pregnancy carried to term and gave birth to a beautiful little baby girl.
Women with PCOS are commonly insulin resistant. This insulin resistance continues on in pregnancy, creating a variety of problems. We will go through the most common PCOS-related complications of pregnancy and the postpartum period and, most importantly, what you can do about them.
Supplements to support pregnancy in PCOS include—
Even after all of the challenges you’ve gone through to conceive, the threat of miscarriage can continue to loom for women with PCOS. It’s thought that the rate of miscarriage in PCOS can be close to double that of a typical pregnancy. The causes of miscarriage are thought to be linked to elevated insulin levels, which increase the risk of blood clotting—this can make delivering blood flow through the placenta a challenge. Some researchers have also found that the elevated androgens found in women with PCOS may be a culprit in miscarriage. It’s thought that the hormonal and metabolic dysregulations found in PCOS can alter the uterine lining and the way that the embryo implants. Another highly prevalent factor is egg quality—in the presence of inflammation and oxidative stress, egg health can be compromised, increasing the risk of miscarriage.
The first thing you should do is follow all 8 steps prior to becoming pregnant, in order to produce healthier eggs and a healthier reproductive and metabolic environment. Importantly, you can also continue the PCOS diet program in pregnancy, with a slightly higher amount of carbohydrates with each meal. Typically, you can increase your starchy vegetable intake to the size of one handful with each meal, and then have “mini meal” snacks, three times daily.
One German trial on 144 women with immunologically mediated recurrent miscarriages treated with systemic enzymes in pregnancy produced promising results, as 114 of the women were able to carry healthy babies to term with this therapy. More research should be completed on this treatment, and it should not be used without the supervision of a physician. Systemic enzymes also have blood-thinning action and should not be combined with other anticoagulant medications unless prescribed by a physician.
In chapter 2, I spoke about using an EPA-dominant, molecularly distilled omega-3 fatty acid. This is an excellent way to reduce inflammation and insulin resistance in pregnancy. I aim for a dosage of approximately 1,200 mg EPA and 500 mg DHA for pregnant women.
In many reproductive medicine clinics, low-dose (baby) aspirin is commonly recommended to thin the blood and prevent miscarriage. This should be done only with a doctor’s supervision and should not be combined with any other blood-thinning agents without the close supervision of a health-care professional. Typically, the risk of miscarriage is minimal after twelve weeks. After this point, you may do best shifting back to the general pregnancy recommendations.
This is a common condition that women with PCOS are at increased risk for. Given that we have genetic predispositions to diabetes, it makes sense that gestational diabetes would be a risk we face as well. In particular, women over thirty-five have increased insulin resistance in pregnancy. Combine that with PCOS, and there is often gestational diabetes in older women as a result. The main risk of gestational diabetes is that it can cause your baby to grow too large. If the baby is too large, he or she will be at increased risk for a difficult birth or cesarean section.
It’s best to check for gestational diabetes around twenty-seven weeks of gestation. This is routinely done with an oral glucose tolerance test. If your readings come back showing you are at risk for gestational diabetes, you can also check your own fasting and post-meal glucose at home with a glucometer. Check your blood sugar two hours after eating and aim for levels below 6.7 mmol/l (approximately 120 mg/dl). When it comes to fasting glucose in the morning, you should aim for below 5.8 mmol/l (105 mg/dl). If a meal causes your blood sugar to spike, look closely at the contents. Did you consume a carbohydrate-heavy meal? Was there hidden sugar in the meal? Did you have enough protein and vegetables with the meal to slow down the absorption of food?
Following your PCOS nutrition plan is the best way to combat gestational diabetes. Insulin counting isn’t usually necessary: Simply structure your plate well, avoid sugar and excessive carbohydrates, and increase your vegetable intake. In addition, exercise can be a powerful weapon against this problem. There are many pregnancy-safe exercise videos available currently, and brisk walking or swimming is always an excellent form of exercise in pregnancy.
Fortunately, gestational diabetes almost always goes away immediately after delivering. However, having it does increase your future risk for diabetes, something women with PCOS are already quite aware of, unfortunately.
Some other tips that can help manage gestational diabetes include the following:
Women with PCOS are also at risk for hypertension in pregnancy. This is related to both insulin resistance and to the inflammatory environment created by the condition. This condition is also known as preeclampsia and can progress to a serious health condition for both mother and child. The chronic high blood pressure can restrict the blood flow to the baby through the placenta and can result in dangerous blood-clotting cascades in the mom. Like gestational diabetes, this condition resolves once you have had your baby. However, it puts you at risk for hypertension later on in life. Routine monitoring of protein in the urine as well as blood pressure is one of the ways that preeclampsia is picked up.
What can you do about hypertension during pregnancy? The following tips will help:
Once baby has arrived, women with PCOS may face a few different issues in the postpartum period. This section will outline these and provide solutions to help you adjust to your new life with baby!
You’ve had your baby and everything went well. Congratulations! Many women with PCOS can breastfeed their newborn wonderfully and without any issues whatsoever, but there are some women who do have some challenges with breastfeeding due to PCOS. That being said, try not to worry until you see how it goes for you, since the majority of women with PCOS can breastfeed successfully!
There are a few reasons that some women with PCOS have trouble with breast-feeding. As teenage girls, there can be high levels of androgens and insufficient female hormones, such as estrogen, to develop the breast glandular tissue. Women with PCOS may have less glandular and more fatty tissues in their breasts or have small “tubular” breasts that are not well developed. In other cases, however, breast development isn’t affected at all, and there are many women with PCOS who make ample milk and have a very easy time with breastfeeding.
The most important thing is to be gentle with yourself as you enter into your role as a new mom. Encouragement and support are important, so avoid anyone who makes you feel shame or guilt when you have tried your best.
To learn more, there are websites in the Resources section with tips on proper latching, compressions, and other important information you’ll need in order to have your most optimal breastfeeding relationship with your child.
Good nutrition and keeping insulin resistance at bay are important for the support of breastfeeding in women with PCOS. You’ll need more calcium and magnesium, and a supplement that has 1,000 mg of calcium and 500 mg of magnesium is often helpful.
You can continue to follow your PCOS nutrition recommendations, but you’ll need an extra three hundred to five hundred calories per day, so try to achieve your additional needs with some extra lean protein and healthy fats, rather than loading up too much on the carbohydrates.
Batch cooking on the weekend is a great practice while you are breastfeeding. You can prep meals for the slow cooker for the week that won’t take up too much time while you are caring for baby. Find easy solutions that allow you to continue your healthy eating patterns. For example, buy pre-chopped veggies or salads that make it easy to include the foods that will best support your health and that of your baby.
You should also drink plenty of water and take good care of yourself. Caring for a young infant is stressful, and the lack of sleep can disrupt your cortisol patterns, which can impact breastfeeding. Allow yourself breaks when possible, and find someone to cover for you while you nap.
In some cases, herbal medicines can improve a milk supply that is struggling. You can try these, particularly if you are sure that you’ve addressed all issues with latch and supply-demand with a lactation consultant.
Two herbs may be useful for women with PCOS who want to increase their milk supply. These are fenugreek and blessed thistle. Dr. Jack Newman of the International Breastfeeding Centre recommends taking three capsules of each, three times per day, and suggests that this should work within a day of starting them. Fenugreek should cause your skin to smell like maple syrup when taken in sufficient amounts.
Domperidone is a medication that is prescribed to increase milk supply in women. It works by increasing the hormone prolactin, which stimulates milk production. It works by blocking dopamine receptors in the pituitary gland. There are some women for whom this is drug is contraindicated. This includes women who have any history of cardiac arrhythmia or anyone with chronic illness, abnormal liver function, or gastric abnormalities. As women with PCOS can be in these categories, they should always consult with an experienced physician to see if this medication may be safe for them.
As women with PCOS have higher indices of depression and anxiety, the postpartum period may be a trigger for the onset of these conditions. Hormones, including progesterone, estrogen, and prolactin, are very high during pregnancy. Postpartum there is a huge crash of hormones, which can trigger mood disorders in many women. Be on the lookout for changes in your mood, lack of motivation, anxiety, or feeling unhappy with your role as a new mother.
If you aren’t feeling quite right after having your baby, the most important thing is to reach out for support. Accept help from your family and friends, and get counseling if your feelings are out of control. Some supplements that are generally safe to take when breastfeeding include—
*This supplement can help with anxiety and is also beneficial for PCOS.
The first four to six months after having a baby is the most likely time for problems to begin with thyroid function. As Hashimoto’s thyroiditis (autoimmune thyroiditis) is more common in women with PCOS, it’s important to look out for postpartum thyroiditis, an inflammatory condition that attacks the thyroid gland after having a baby. Therefore, be sure to check your thyroid antibodies six weeks after having a baby, particularly if you are feeling cold, tired, depressed, and are not able to lose weight.
Women with PCOS may have a longer period of what is known as postpartum amenorrhea, meaning that the time for the period to return is longer than for other women. This is related to the androgen excess and insulin resistance of the disorder. The best way to help move this along is to go through the 8 steps to reverse your PCOS that are shared in this book.
Pregnancy and new motherhood is a wonderful time in your life. Although PCOS may present many challenges to this period, the vast majority of women recover well and have healthy pregnancies and postpartum periods with the right diet and treatments. So, most of all, enjoy your special time with baby!