7 Thoracic Wall
Thoracic Skeleton
 The thoracic skeleton consists of 12 vertebrae thoracicae (p. 10), 12 pairs of costae with cartilagines costales, and the sternum. In addition to participating in respiratory movements, it provides a measure of protection to vital organs. The female thorax is generally narrower and shorter than the male equivalent.
The thoracic skeleton consists of 12 vertebrae thoracicae (p. 10), 12 pairs of costae with cartilagines costales, and the sternum. In addition to participating in respiratory movements, it provides a measure of protection to vital organs. The female thorax is generally narrower and shorter than the male equivalent.
Fig. 7.1 Thoracic skeleton
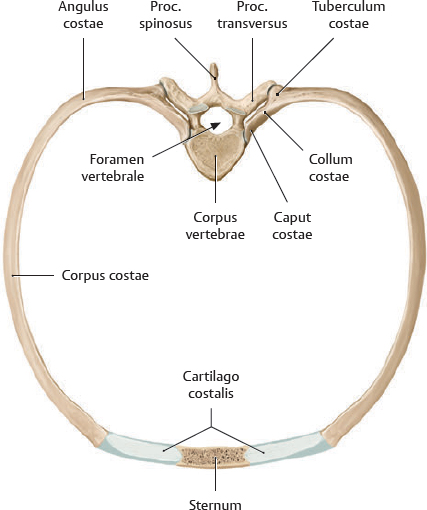
Fig. 7.2 Structure of a thoracic segment
Superior view of costa VI pair.
Table 7.1 Elements of a thoracic segment
Vertebra |
Costa |
Bony part (costal bone) |
Caput costae |
Collum costae |
Tuberculum costae |
Corpus costae (including angulus costae) |
Cartilaginous part (cartilago costalis) |
Sternum (articulates with cartilago costalis of costae verae only; see Fig. 7.3) |
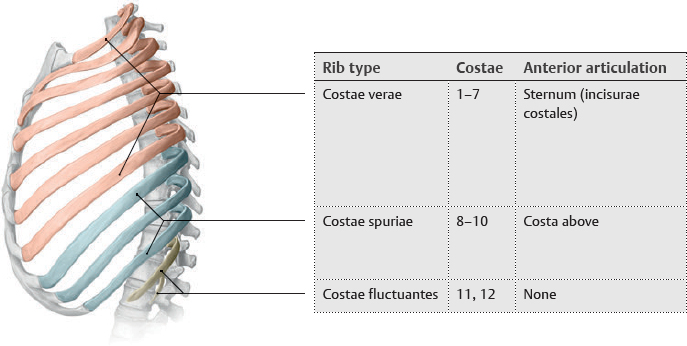
Fig. 7.3 Types of costae
Left lateral view.
Sternum & Costae
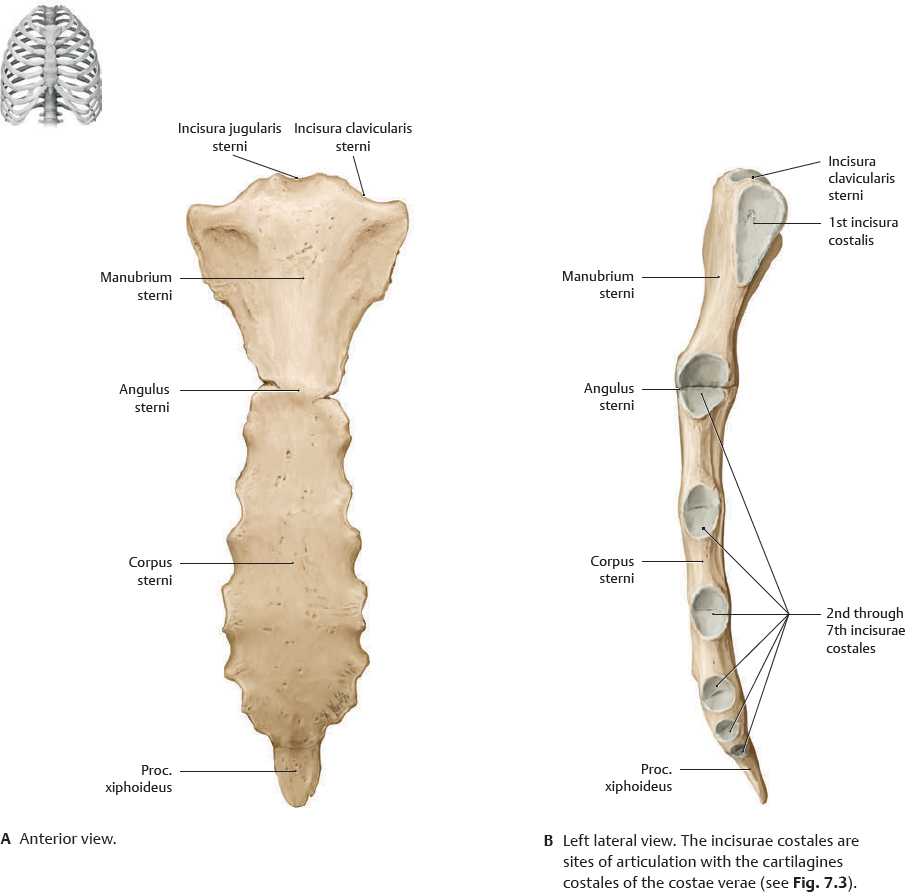
Fig. 7.4 Sternum
The sternum is a blade-like bone consisting of the manubrium, corpus, and proc. xiphoideus. The junction of the manubrium and corpus (the angulus sterni) is typically elevated and marks the articulation of the second costa. The angulus sterni is an important landmark for internal structures.
Fig. 7.5 Costae
Right costae, superior view. See pp. 298–299 for joints of the shoulder.
Joints of the Thoracic Cage
 The diaphragma is the chief muscle for quiet respiration (see p. 64). The muscles of the thoracic wall (see p. 62) contribute to deep (forced) inspiration.
The diaphragma is the chief muscle for quiet respiration (see p. 64). The muscles of the thoracic wall (see p. 62) contribute to deep (forced) inspiration.
Fig. 7.6 Thoracic cage movement
Full inspiration (red); full expiration (blue). In deep inspiration, there is an increase in transverse and anteroposterior (AP) dimensions, as well as the angulus infrasternalis. The descent of the diaphragma further increases the volume of the cavitas thoracis.
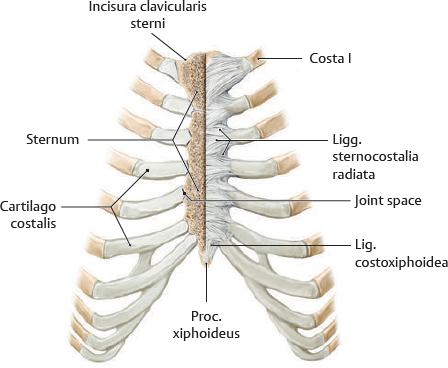
Fig. 7.7 Articulationes sternocostales
Anterior view with right half of sternum sectioned frontally. True joints are generally found only at costae II to V; ribs I, VI, and VII attach to the sternum by synchondroses.
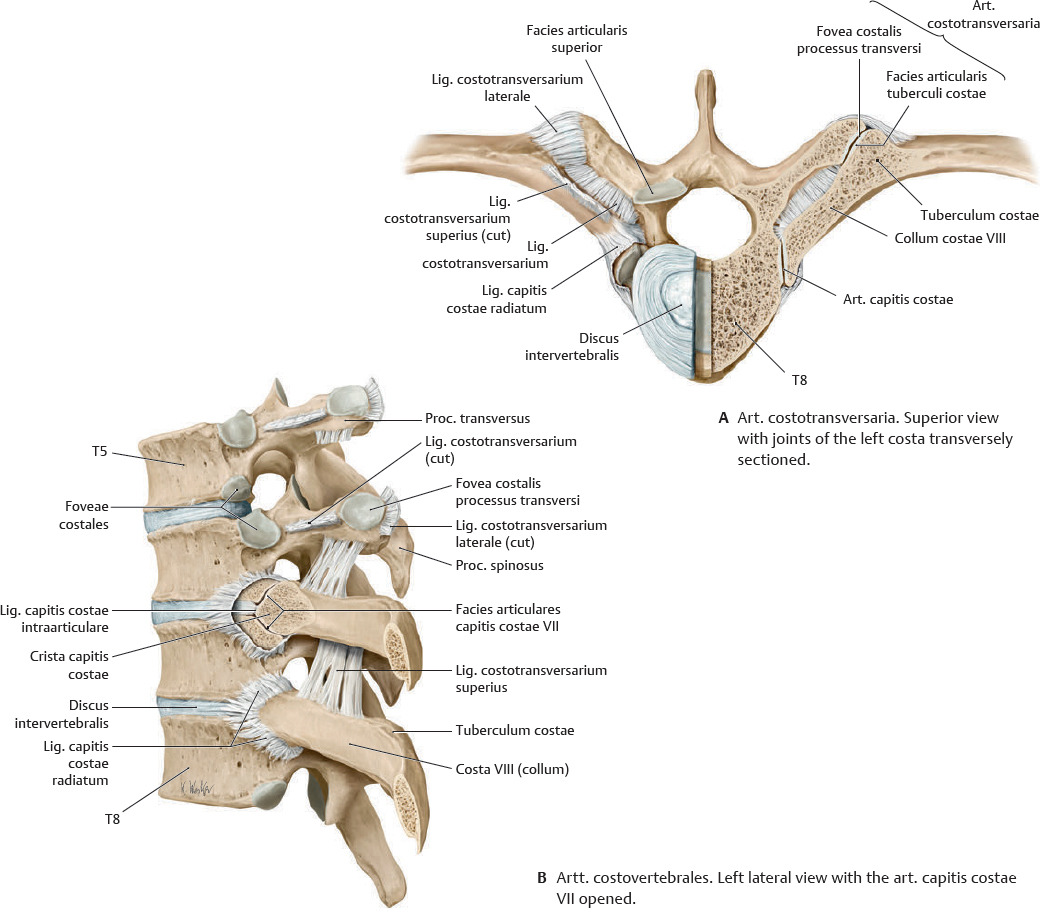
Fig. 7.8 Articulationes costovertebrales
Two synovial joints make up the art. costovertebralis of each costa. The tuberculum costae of each costa articulates with the fovea costalis processus transversi of its accompanying vertebra (A). The head of most costae articulates with the vertebra of its own number and the vertebra immediately superior. Costae I, XI, and XII typically articulate only with their own vertebrae.
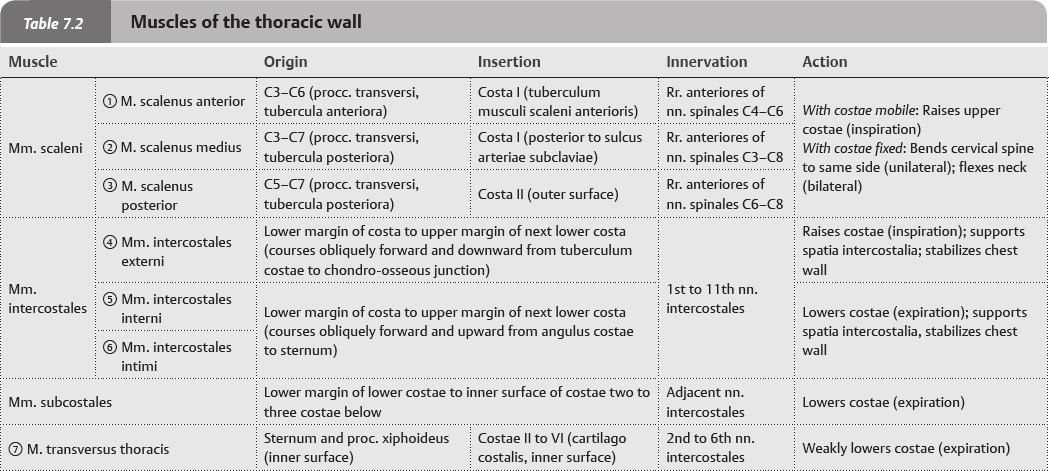
Thoracic Wall Muscle Facts
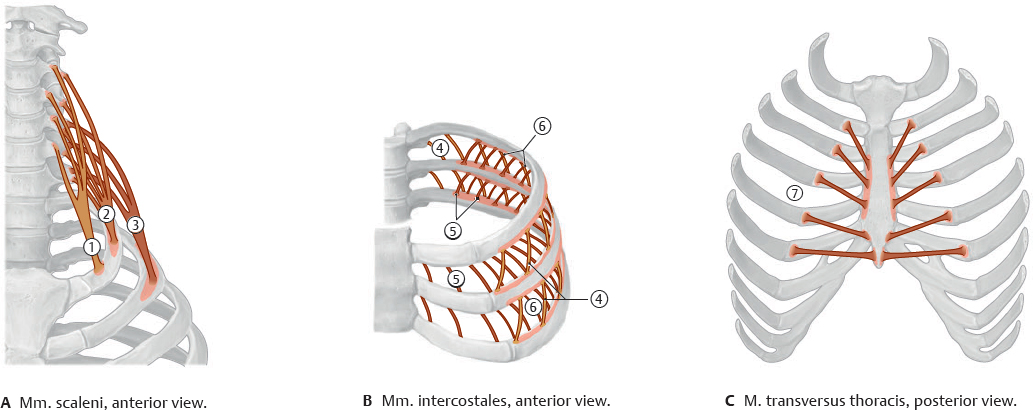
 The muscles of the thoracic wall are primarily responsible for chest respiration, although other muscles aid in deep inspiration: the mm. pectoralis major and serratus anterior are discussed with the shoulder (see pp. 314–315), and the m. serratus posterior is discussed with the back (see p. 32).
The muscles of the thoracic wall are primarily responsible for chest respiration, although other muscles aid in deep inspiration: the mm. pectoralis major and serratus anterior are discussed with the shoulder (see pp. 314–315), and the m. serratus posterior is discussed with the back (see p. 32).
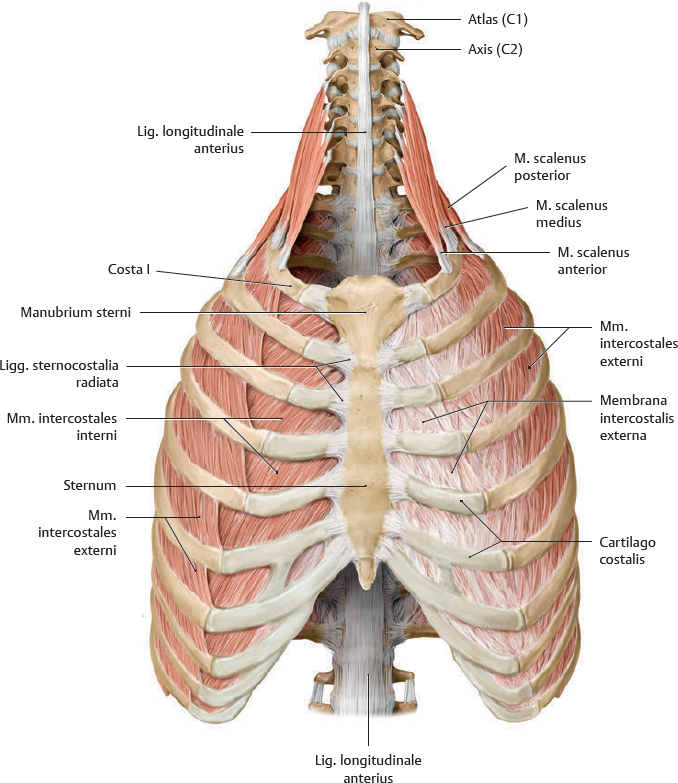
Fig. 7.9 Muscles of the thoracic wall
Fig. 7.10 Muscles of the thoracic wall
Anterior view. The mm. intercostales externi are replaced anteriorly by the membrana intercostalis externa. The mm. intercostales interni are replaced posteriorly by the membrana intercostalis interna (removed in Fig. 7.11).
Fig. 7.11 Musculus transversus thoracis
Anterior view with thoracic cage opened to expose posterior surface of anterior wall.
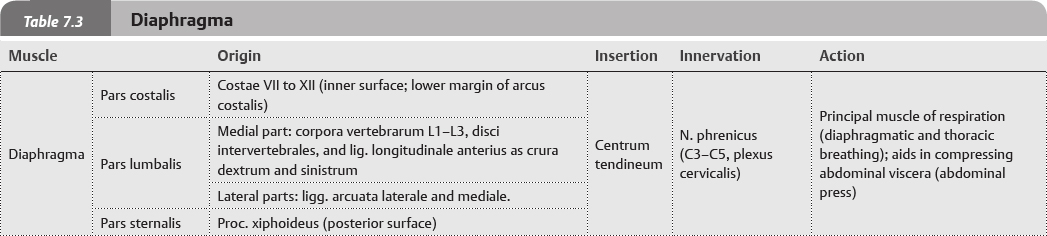
Diaphragma
Fig. 7.12 Diaphragma
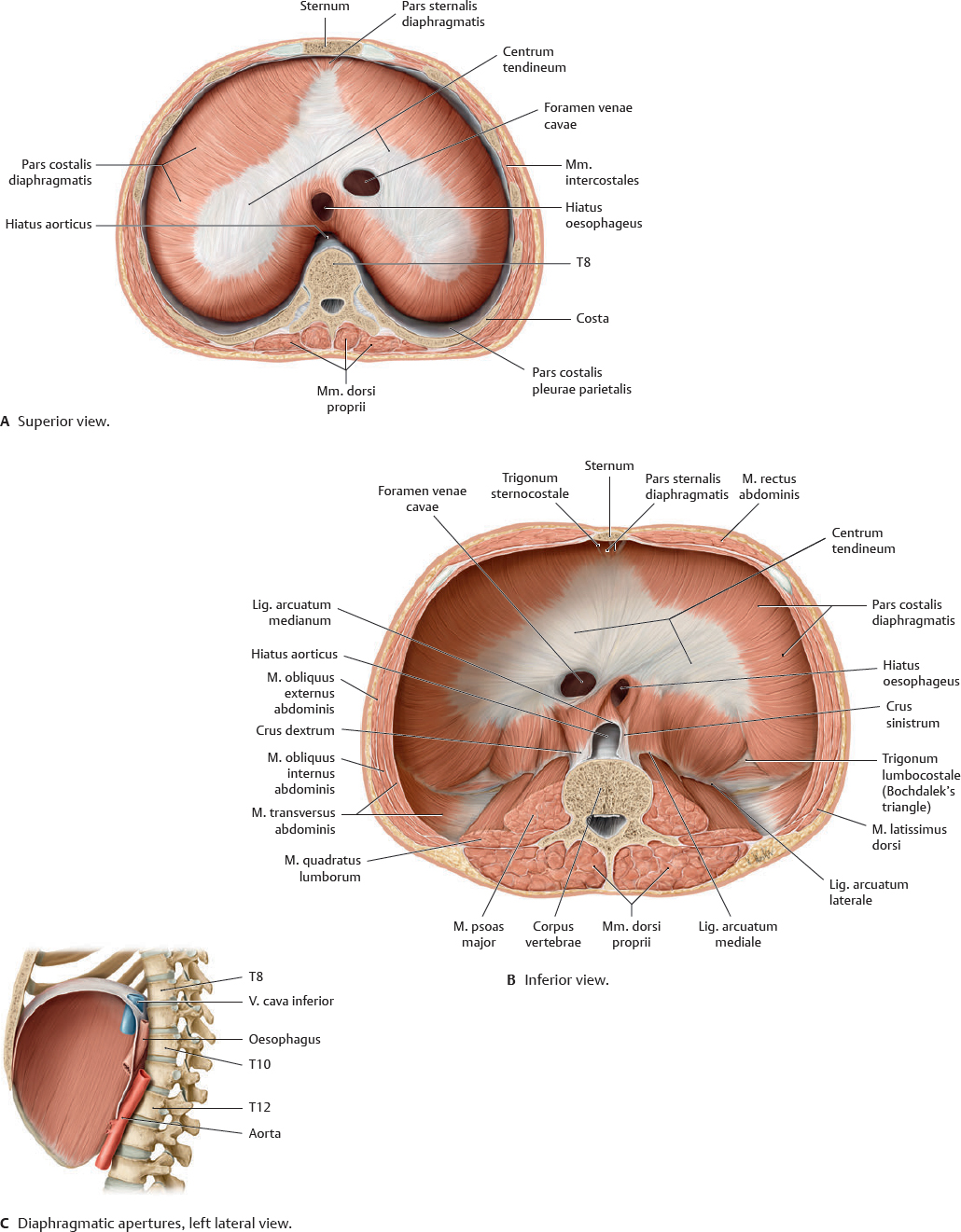
The diaphragma, which separates the thorax from the abdomen, has two asymmetric domes and three apertures (for the aorta, v. cava, and oesophagus; see Fig. 7.13C).
Fig. 7.13 Diaphragma in situ
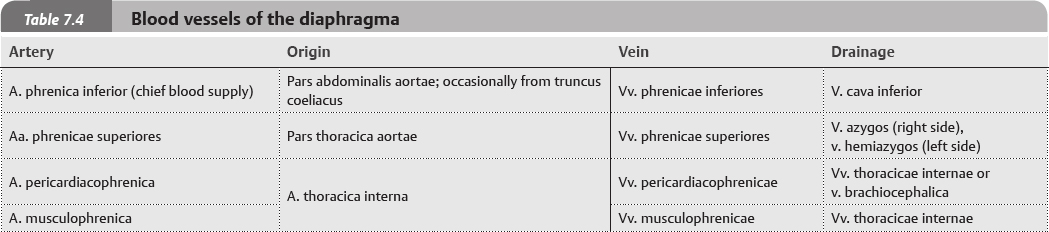
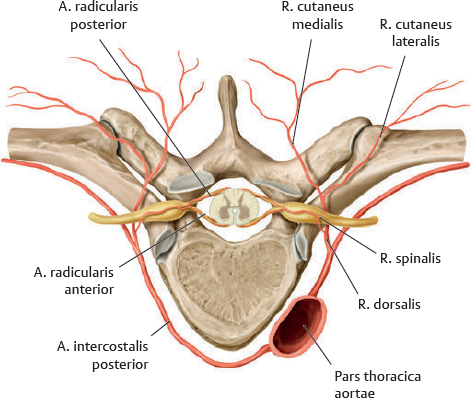
Neurovasculature of the Diaphragma
Fig. 7.14 Neurovasculature of the diaphragma
Anterior view of opened thoracic cage.
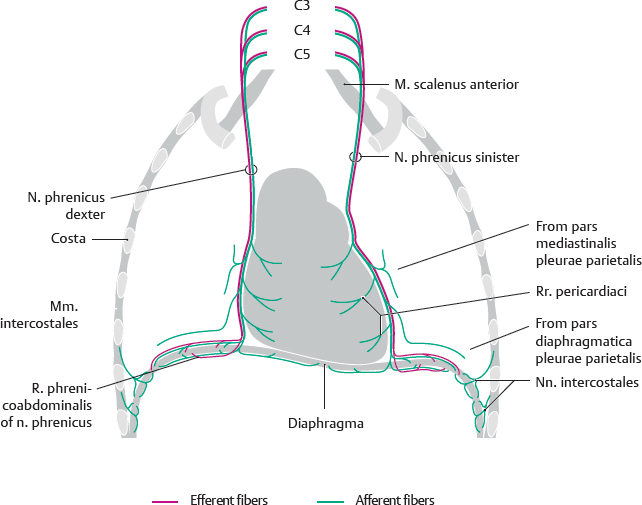
Fig. 7.15 Innervation of the diaphragma
Anterior view. The nn. phrenici lie on the lateral surfaces of the pericardium fibrosum together with the aa. and vv. pericardiacophrenicae. Note: The nn. phrenici also innervate the pericardium.
Fig. 7.16 Arteries and nerves of the diaphragma
Note: Structures of the mediastinum superius may also drain directly to the vv. brachiocephalicae via the vv. tracheales, oesophageales, and mediastinales.
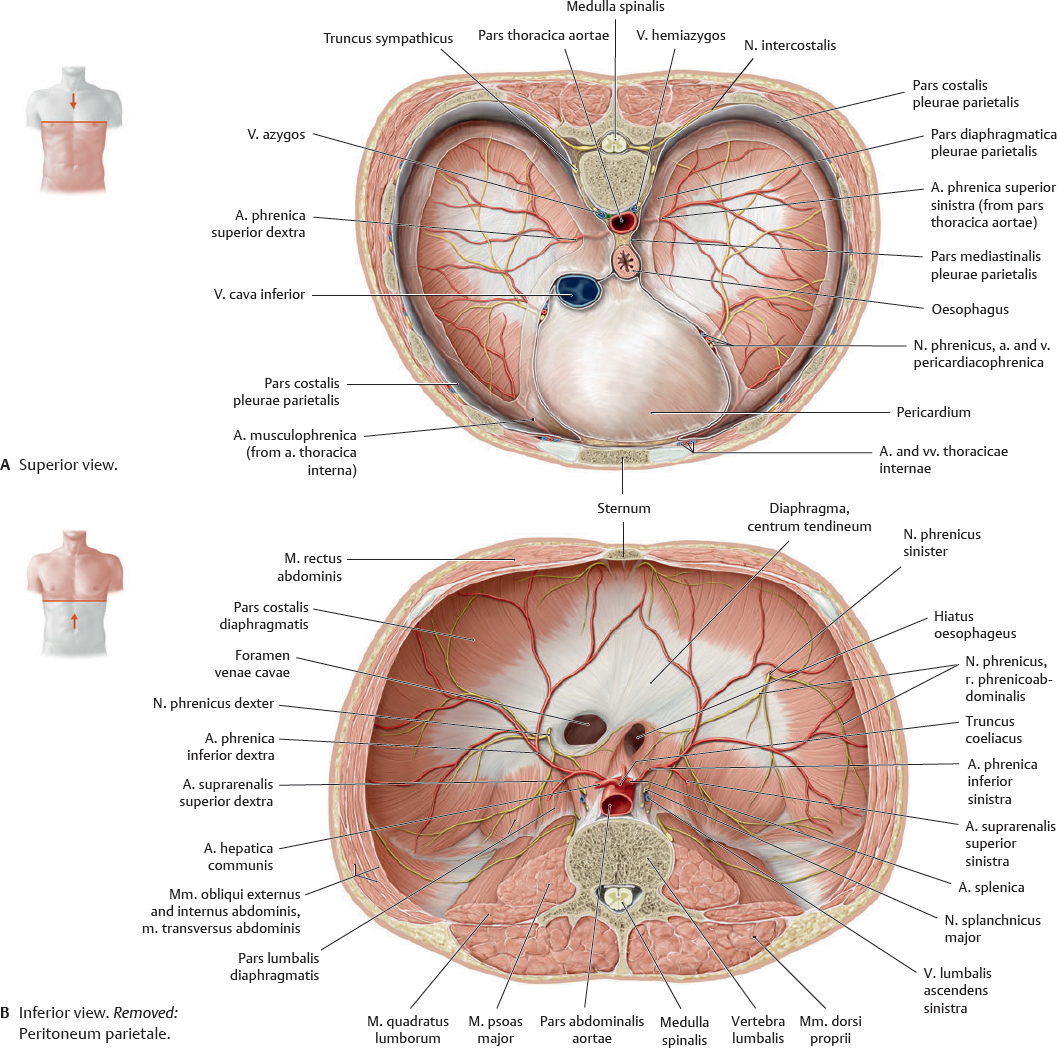
Arteries & Veins of the Thoracic Wall
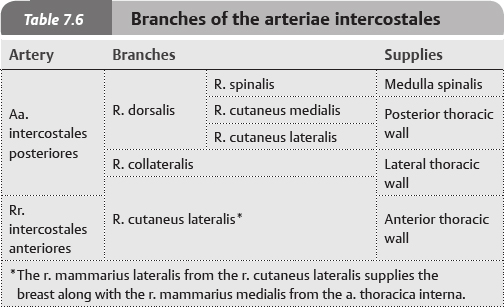
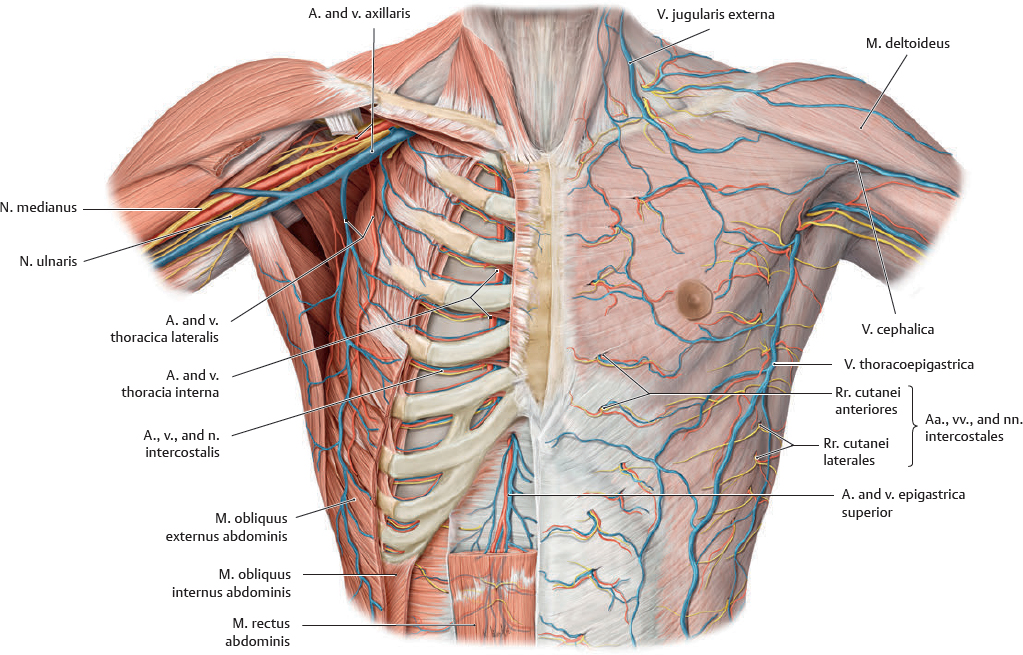
 The aa. intercostales posteriores anastomose with the rr. intercostales anteriores to supply the structures of the thoracic wall. The aa. intercostales posteriores branch from the pars thoracica aortae, with the exception of the 1st and 2nd, which arise from the a. intercostalis suprema (a branch of the truncus costocervicalis).
The aa. intercostales posteriores anastomose with the rr. intercostales anteriores to supply the structures of the thoracic wall. The aa. intercostales posteriores branch from the pars thoracica aortae, with the exception of the 1st and 2nd, which arise from the a. intercostalis suprema (a branch of the truncus costocervicalis).
Fig. 7.17 Arteries of the thoracic wall
Anterior view.
Table 7.5 Arteries of the thoracic wall
Origin |
Branch |
A. axillaris |
A. thoracica lateralis |
A. thoracoacromialis |
A. subclavia |
Aa. intercostales posteriores (prima and secunda; see Fig. 4.1, p. 36) |
A. thoracica interna |
Pars thoracica aortae |
Aa. intercostales posteriores (3rd through 12th) |
A. thoracica interna |
Rr. intercostales anteriores |
A. musculophrenica |
A. epigastrica superior |
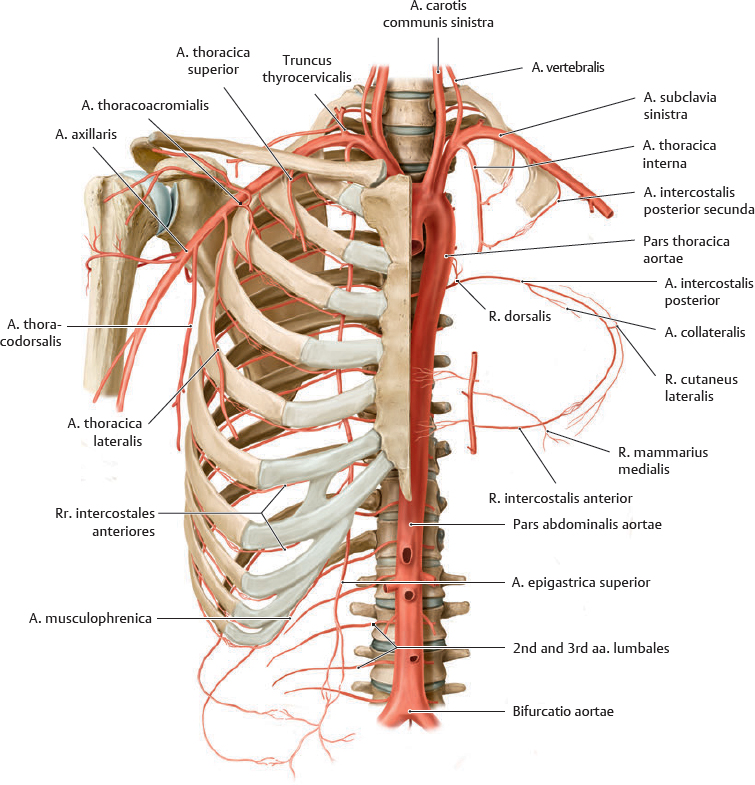
Fig. 7.18 Branches of the arteriae intercostales posteriores
Superior view.
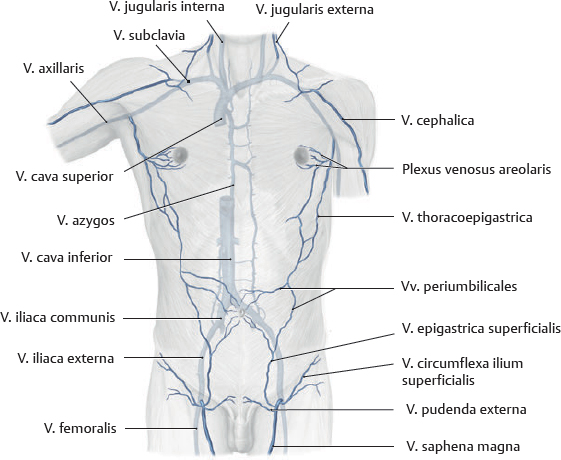
 The vv. intercostales drain primarily into the v. azygos system, but also into the vv. thoracicae internae. This blood ultimately returns to the heart via the v. cava superior. The vv. intercostales follow a similar course to their arterial counterparts. However, the veins of the columna vertebralis form a plexus venosus vertebralis externus that traverses the entire length of the spine (see p. 36).
The vv. intercostales drain primarily into the v. azygos system, but also into the vv. thoracicae internae. This blood ultimately returns to the heart via the v. cava superior. The vv. intercostales follow a similar course to their arterial counterparts. However, the veins of the columna vertebralis form a plexus venosus vertebralis externus that traverses the entire length of the spine (see p. 36).
Fig. 7.19 Veins of the thoracic wall
Fig. 7.20 Superficial veins
Anterior view. The vv. thoracoepigastricae are a potential superficial collateral venous drainage route in the event of v. cava superior or v. cava inferior obstruction.
Nerves of the Thoracic Wall
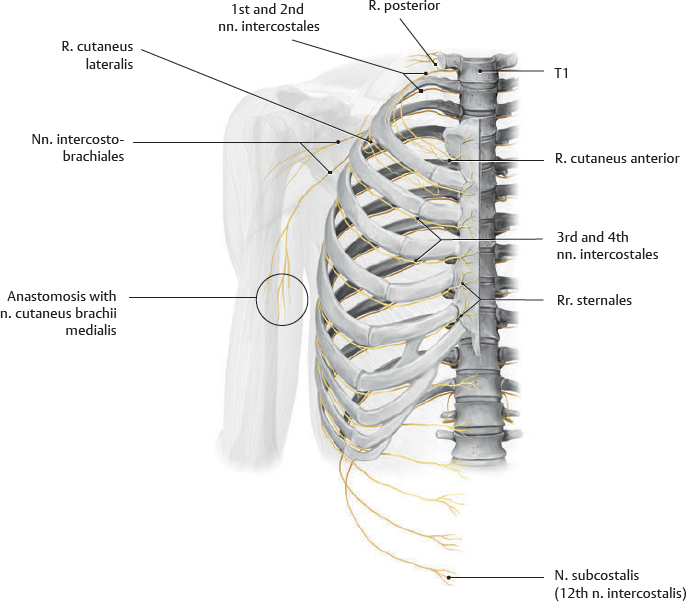
Fig. 7.21 Nervi intercostales
Anterior view. The costa prima has been removed to reveal the 1st and 2nd nn. intercostales.
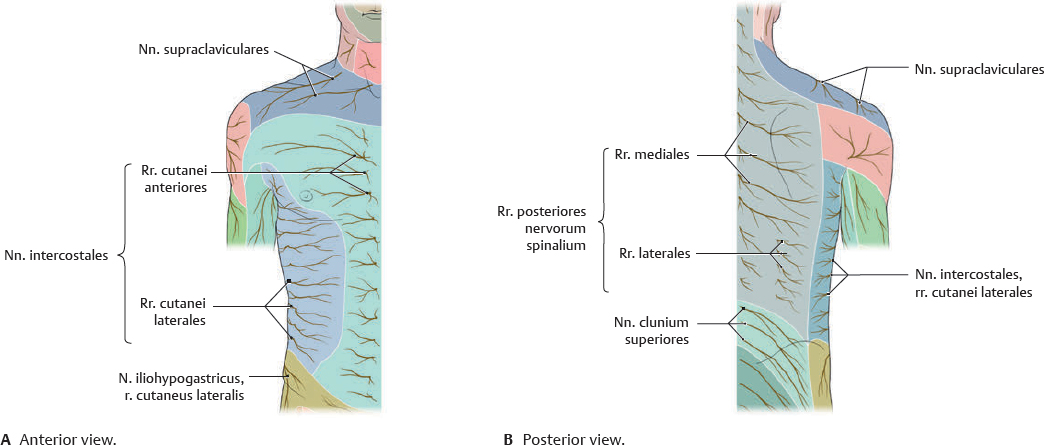
Fig. 7.22 Cutaneous innervation of the thoracic wall
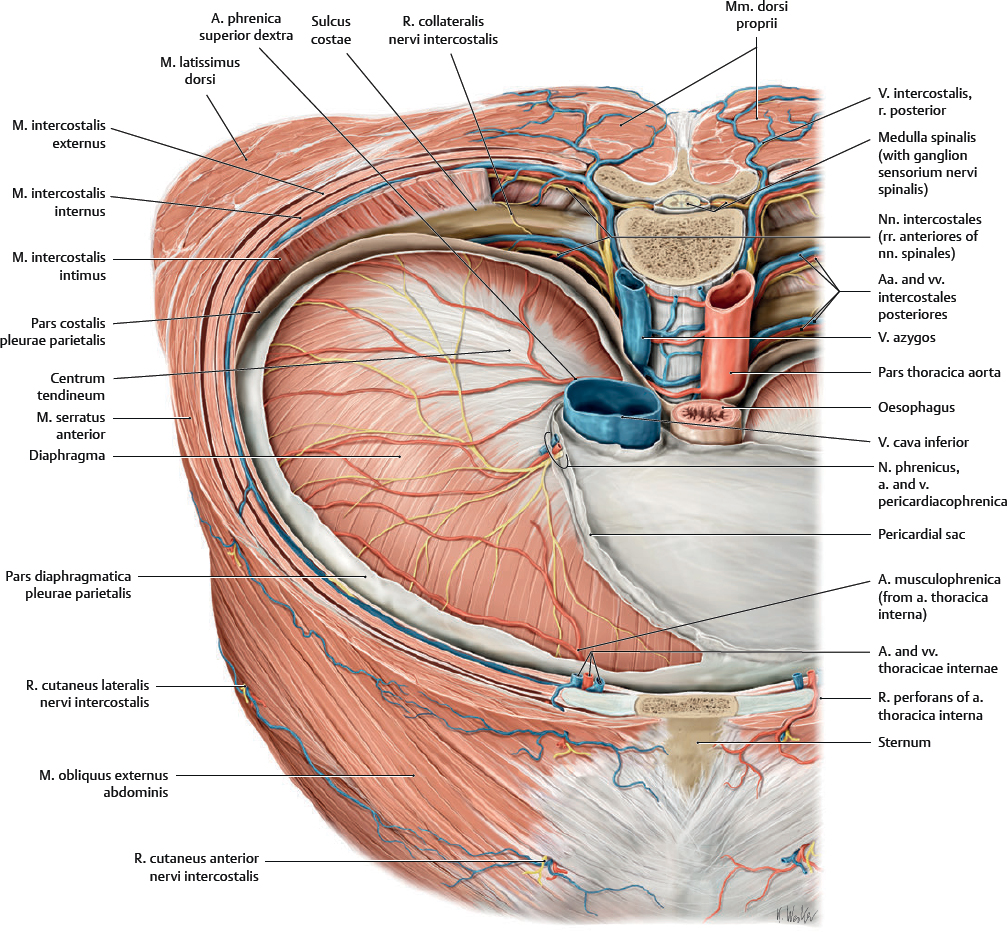
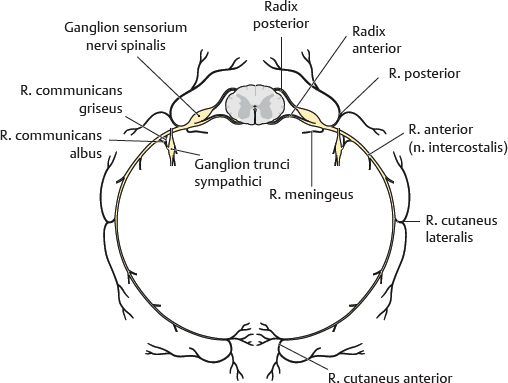
Fig. 7.23 Rami nervorum spinalium
Superior view. The n. spinalis is formed by the union of radices posteriores and anteriores. The radix posterior contains sensory fibers and the radix anterior contains motor fibers. The n. spinalis and all its subsequent branches are mixed nerves, containing both motor and sensory fibers. The n. spinalis exits the canalis vertebralis via the foramen intervertebrale. Its r. posterior innervates the skin of the dorsum and mm. dorsi proprii; its r. anterior forms the plexus cervicalis, brachialis, lumbalis, and sacralis, and the nn. intercostales. See p. 38 for more details.
Fig. 7.24 Course of the nervi intercostales
Coronal section, anterior view.
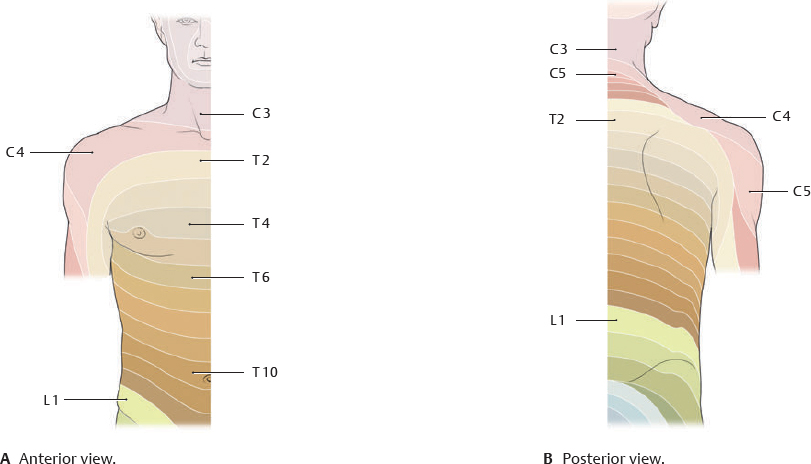
Fig. 7.25 Dermatomes of the thoracic wall
Landmarks: T4 generally includes the papilla mammaria; T6 innervates the skin over the proc. xiphoideus.
Neurovascular Topography of the Thoracic Wall
Fig. 7.26 Anterior structures
Anterior view (see Chapter 4 for neurovasculature of the back).
 Clinical box 7.1
Clinical box 7.1
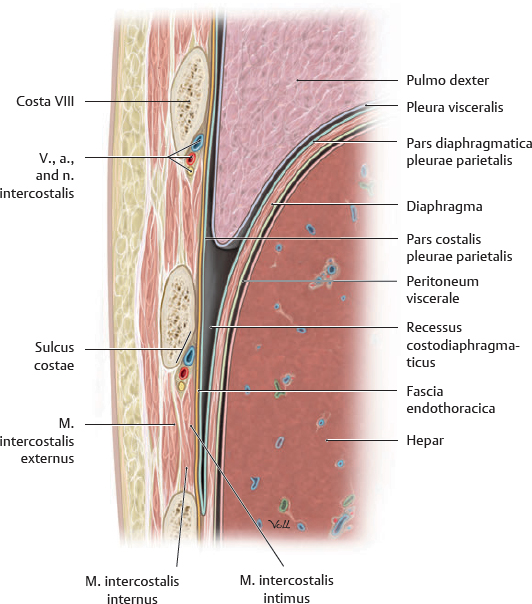
Insertion of a chest tube
Abnormal fluid collection in the cavitas pleuralis (e.g., pleural effusion due to bronchial carcinoma) may necessitate the insertion of a chest tube. Generally, the optimal puncture site in a sitting patient is at the level of the 7th or 8th spatium intercostale on the linea axillaris posterior. The drain should always be introduced at the upper margin of a costa to avoid injuring the v., a., and n. intercostalis. See p. 123 for details on collapsed lungs.
Fig. 7.27 Intercostal structures in cross section
Transverse section, anterosuperior view. The relationship of the intercostal vessels in the sulcus costae, from superior to inferior, is vena, artery, and nerve (see clinical box, p. 72).
Mamma (Breast)
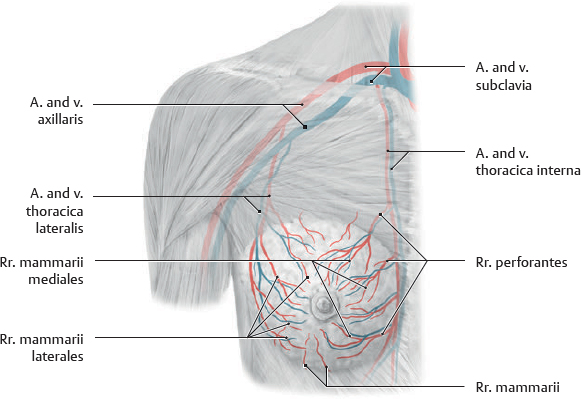
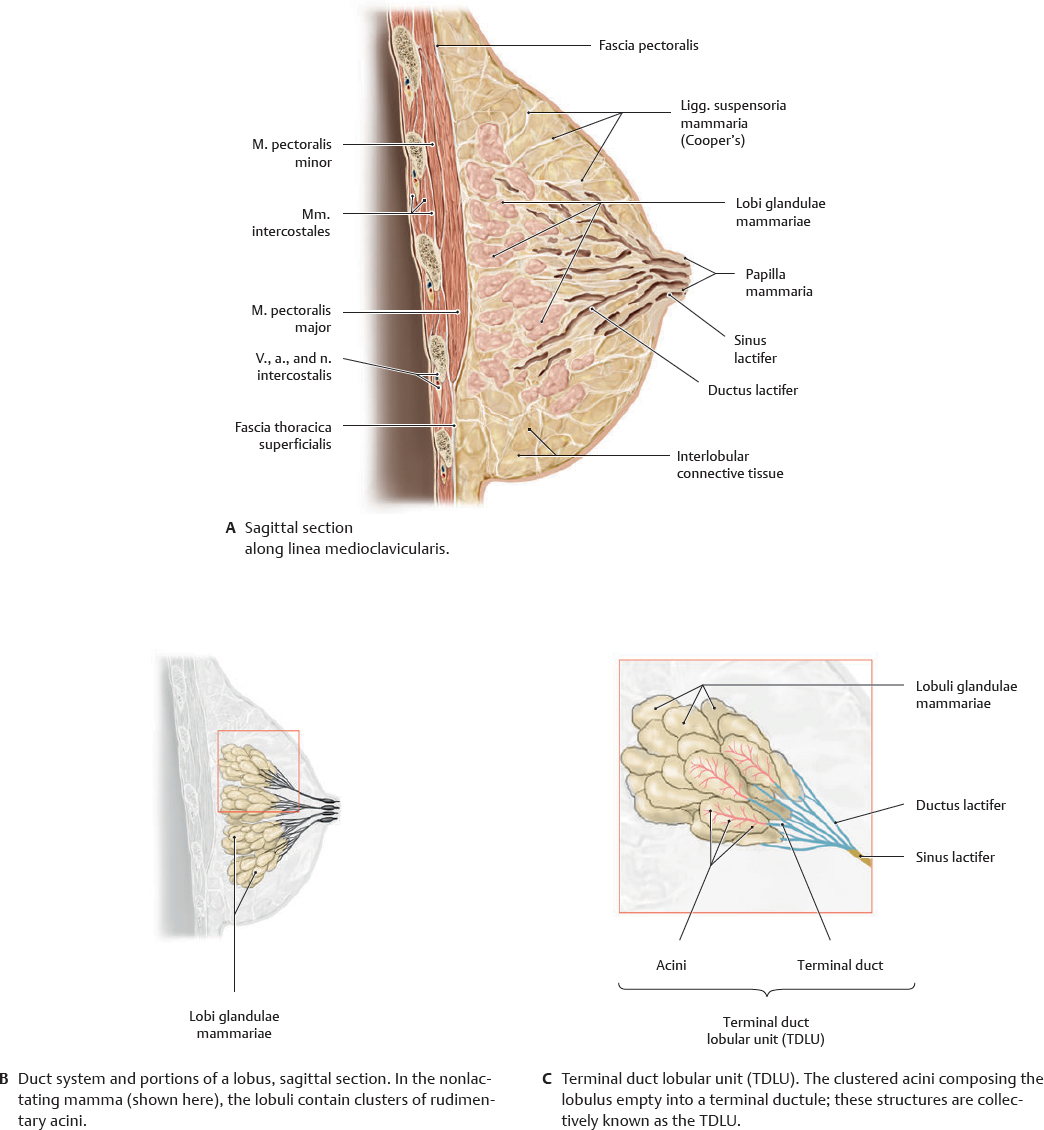
 The mamma, a modified gl. sudorifera in the tela subcutanea, consists of glandular tissue, fibrous stroma, and fat. The mamma extends from costa II to costa VI and is loosely attached to the fasciae pectoralis, axillaris, and investiens superficialis abdominis by connective tissue. The mamma is additionally supported by ligg. suspensoria. An extension of the mamma tissue into the axilla, the proc. axillaris, is often present.
The mamma, a modified gl. sudorifera in the tela subcutanea, consists of glandular tissue, fibrous stroma, and fat. The mamma extends from costa II to costa VI and is loosely attached to the fasciae pectoralis, axillaris, and investiens superficialis abdominis by connective tissue. The mamma is additionally supported by ligg. suspensoria. An extension of the mamma tissue into the axilla, the proc. axillaris, is often present.
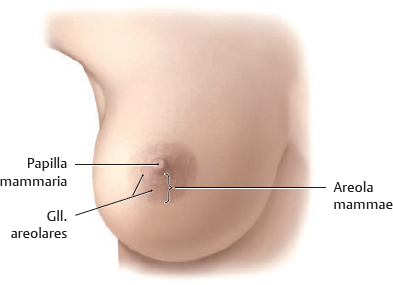
Fig. 7.28 Female mamma
Right mamma, anterior view.
Fig. 7.29 Cristae mammariae
Rudimentary gll. mammariae form in both sexes along the cristae mammariae. Occasionally, these may persist in humans to form mammae accessoriae (polythelia), although only the thoracic pair normally remains.
Fig. 7.30 Blood supply to the mamma
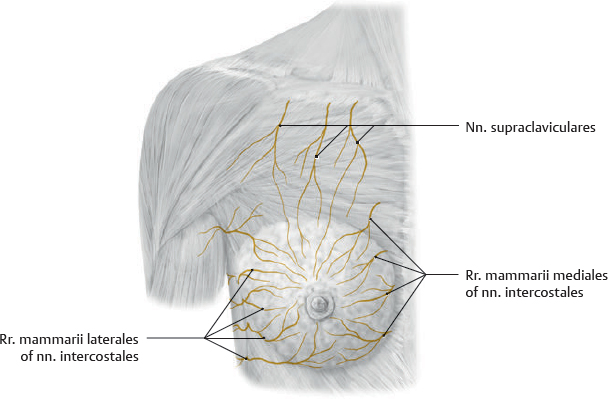
Fig. 7.31 Sensory innervation of the mamma
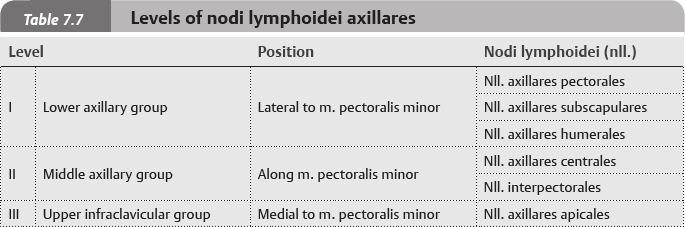
 The glandular tissue is composed of 10 to 20 individual lobi, each with its own ductus lactifer. The gland ducts open on the elevated papilla at the center of the pigmented areola. Just proxi mal to the duct opening is a dilated portion called the sinus lactifer. Tubercula areolae are the openings of the gll. areolares (sebaceous). The gll. mammariae and ductus lactiferi are surrounded by firm, fibrofatty tissue with a rich blood supply.
The glandular tissue is composed of 10 to 20 individual lobi, each with its own ductus lactifer. The gland ducts open on the elevated papilla at the center of the pigmented areola. Just proxi mal to the duct opening is a dilated portion called the sinus lactifer. Tubercula areolae are the openings of the gll. areolares (sebaceous). The gll. mammariae and ductus lactiferi are surrounded by firm, fibrofatty tissue with a rich blood supply.
Fig. 7.32 Structures of the mamma
Lymphatics of the Mamma
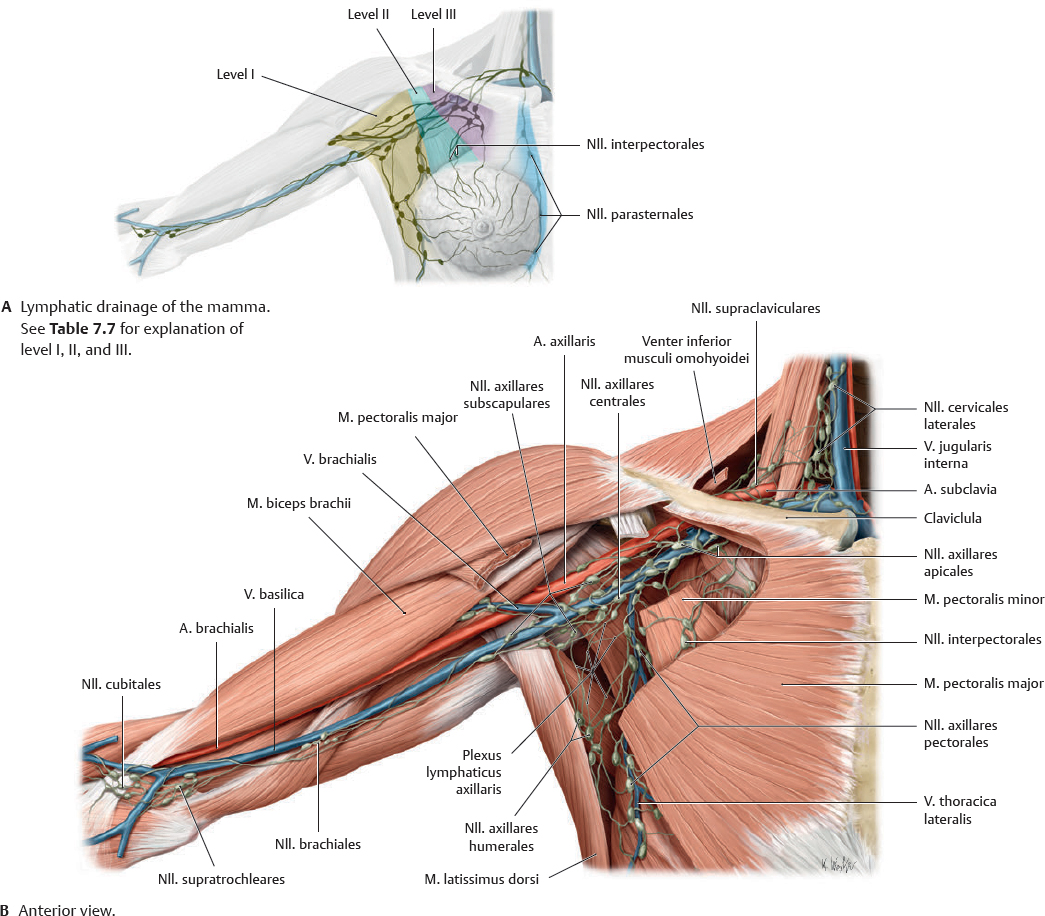
 The lymphatic vessels of the mamma (not shown) are divided into three systems: superficial, subcutaneous, and deep. These drain primarily into the nll. axillares, which are classified based on their relationship to the m. pectoralis minor (Table 7.7). The medial portion of the mamma is drained by the nll. parasternales, which are associated with the vasa thoracicae internae.
The lymphatic vessels of the mamma (not shown) are divided into three systems: superficial, subcutaneous, and deep. These drain primarily into the nll. axillares, which are classified based on their relationship to the m. pectoralis minor (Table 7.7). The medial portion of the mamma is drained by the nll. parasternales, which are associated with the vasa thoracicae internae.
Fig. 7.33 Nodi lymphoidei axillares
 Clinical box 7.2
Clinical box 7.2
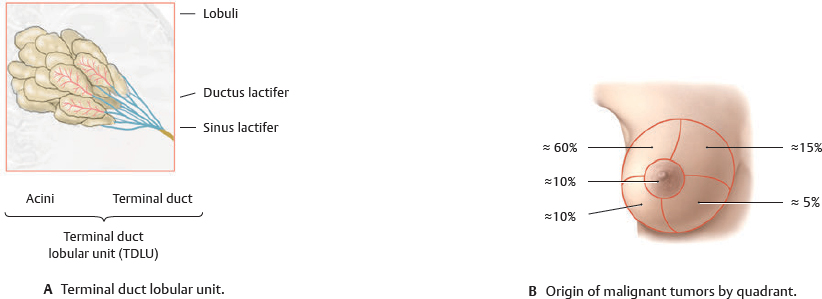
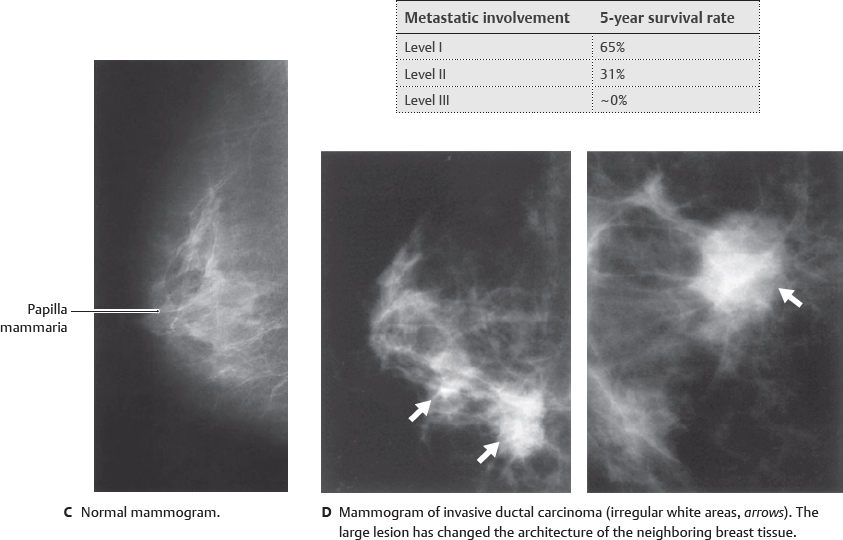
Breast cancer
makes the terminal duct lobular unit (TDLU) the most common site of origin of malignant breast tumors.
Tumors originating in the breast spread via the vasa lymphatica. The deep system of lymphatic drainage (level III) is of particular importance, although the nll. parasternales provide a route by which tumor cells may spread across the midline. The survival rate in breast cancer correlates most strongly with the number of nodi lymphoidei involved at the axillary nodal level. Metastatic involvement is gauged through scintigraphic mapping with radiolabeled colloids (technetium [Tc] 99m sulfur microcolloid). The downstream sentinel node is the first to receive lymphatic drainage from the tumor and is therefore the first to be visualized with radiolabeling. Once identified, it can then be removed (via sentinel lymphadenectomy) and histologically examined for tumor cells. This method is 98% accurate in predicting the level of axillary nodal involvement.
 The thoracic skeleton consists of 12 vertebrae thoracicae (p. 10), 12 pairs of costae with cartilagines costales, and the sternum. In addition to participating in respiratory movements, it provides a measure of protection to vital organs. The female thorax is generally narrower and shorter than the male equivalent.
The thoracic skeleton consists of 12 vertebrae thoracicae (p. 10), 12 pairs of costae with cartilagines costales, and the sternum. In addition to participating in respiratory movements, it provides a measure of protection to vital organs. The female thorax is generally narrower and shorter than the male equivalent.






 Clinical box 7.1
Clinical box 7.1