‘Here sighs and cries and shrieks of lamentation
echoed throughout the starless air of Hell.’
– Dante Alighieri, The Divine Comedy
You stub your toe, shut your fingers in a door, wake up with a bad neck or back after moving heavy furniture – or, worse, experience a sinister ache that could turn out to be a symptom of something very frightening indeed. Or perhaps you develop a pain that moves around your body, and you have no idea what is causing it. We all fear pain, believing – even if we don’t understand the source – that it is always the harbinger of bad news. We will do almost anything to avoid it – take to our beds; avoid activities or work we previously enjoyed; swallow medication that may prove addictive; even submit to surgery in the hope that the short-term intense pain of this will alleviate the longer-term agony.
But what if everything you thought you knew about pain and where it came from turned out to be wrong or only half the truth? What if I told you that your experience of pain in the present moment might in fact be connected with the very origins of Homo sapiens – that it might have evolved as a warning of imminent danger?
Don’t worry… I’m not about to suggest that your ankle fracture is all in the mind. It hurts, of course it does. No one is doubting that. But we now know there is a great deal more to the experience of the pain you have than just the broken bone, damaged disc or grazed skin. What I’m talking about is the new – but now well-evidenced – bio-psycho-social model of pain science. In these pages, I will endeavour to explain as clearly as possible this complex concept, to help you reframe how you experience pain and spur you into action to seek new ways of approaching and curing, or at least relieving, it.
It may not always be easy to find the help you need but there are enlightened practitioners out there. Slowly but surely, a community of joined-up specialists, providing new and visionary approaches to tackling pain, is growing. To date, the world of pain treatment has unfortunately been as much a mystery for the medical and scientific community as it has for the sufferer. This has been particularly true over the last 20 years, during which medicine and science have been driven predominantly by the pharmaceutical industries, who have tended to follow a reductionist approach, whittling things down to a molecular and cellular level rather than taking into consideration the multiple factors which are key to our understanding of pain. In most conditions A plus B does not necessarily equal C.
So be kind to yourself, for it is not you who have failed to get better but the system we currently have – the legacy of years of pain mismanagement – that has failed to help and educate you.
If we are going to discuss pain – and especially how to overcome it – then we have to start by identifying what it is. The International Association for the Study of Pain defines it as:
An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage
... which, although rather convoluted, is at least a fairly accurate definition and reflects much of our current understanding, because it highlights some of the curious aspects of pain that we will be covering: that it is both a sensory and an emotional experience and that it can be caused by both actual and potential tissue damage. Or, wait for it, even no damage at all. Confused? You won’t be, I promise.
One thing is undeniable: pain is unpleasant. It is also essential: an experience put there by evolution and nature to alert us to danger. It’s what will make us withdraw our finger from a hot plate, say, before any damage is done. Nature, being the cruel mother she is, doesn’t care about our contentment or physical well-being, simply that we succeed reproductively and achieve the survival of our genes. She has no remit to make us happy. And, in this sense, pain is our greatest guardian. Pain, nausea, sadness, fear and anxiety… they are all there to protect us from harm in different ways. If we accept them as a necessary part of living, our fear of them should in some way be salved.
But what about the more challenging fact that there needs to be no physical harm or injury for pain to exist? That you can experience severe, even disabling, pain without discernible disease or structural injury? Good examples of this are back pain, migraine, fibromyalgia, chronic fatigue syndrome and ME, all of which I will cover in more detail later on, with some helpful pointers for patients. Each of these conditions causes a great deal of suffering; the symptoms appear from nowhere and incapacitate the sufferer, and yet nothing shows up in blood tests or scans.
And, if that wasn’t mind-boggling enough, there are many well-documented cases of individuals who have suffered major injury but report no pain at all; for example, a Second World War veteran who had a chest X-ray which revealed that a bullet had been sitting in his chest for 60 years – with no ill effect.
Before I go any further, let’s be very clear. Your pain is real; it hurts; and the symptoms associated with it, such as fatigue and anxiety, are also real. We clinicians have to remember that a patient is always in exactly as much pain as they say they are, and that pain does not have to come from a tangible source to be a valid problem.
How else could we explain Couvade syndrome, a condition in which men have been known to physically experience some of their expectant partners’ symptoms, including labour pains? Pain can be a shared phenomenon (more on this later).
What I am about to explain is going to require some processing and mental leaps, but if I do my job right, it will change your whole mindset towards your pain, forever. Knowledge and insight have the power to transform, and in my clinical experience I have found that insight can often be more helpful to people than advice. As the palliative care and addiction expert Dr Gabor Maté says: ‘If we gain the ability to look into ourselves with honesty, compassion and with unclouded vision we can identify the ways in which we need to take care of ourselves.’1
Frustratingly for me and my practitioner colleagues in the fight against pain, there are very few good descriptive words in the English language to describe the concept of pain and its elements. This is partly because all of the sensory processes that occur in the body and brain, which combine to produce pain, occur at an unconscious or subconscious level. Yes, that’s right: it is only when the subconscious brain decides that the information it is getting is important enough that it makes us consciously aware of it so that we experience it as pain. In fact, most of the time pain is the conscious manifestation of a multitude of responses and processes which occur at a neuro-psychological level.
However, say anything that contains the word ‘psychological’ to a patient and you risk being misconstrued as insinuating that their pain is ‘all in the head’ or, worse, that they are neurotic or wimpy or simply bonkers – whereas nothing could be further from the truth.
Another reason we are so ill-equipped to explain pain is that our current understanding of it is but a few years old. Until recently, medicine operated in a Cartesian world. René Descartes (1596–1650) was the Cogito ergo sum (I think therefore I am) guy, a French philosopher who wrote extensively on consciousness and existence and had a profound influence on the philosophy of healthcare and medicine. He was among the first to introduce the idea that mind and body were separate entities, and this remained the accepted view of the human condition until as recently as the 1970s.
Medical practice is slow to change and, regrettably, there are still remnants of this reductionist mind versus body approach in our healthcare system – i.e. relying on what is known as the biomedical model, which focuses on purely biological factors and excludes psychological, environmental and social influences. However, we are now increasingly, as I say, moving towards a more nuanced, holistic approach – the bio-psycho-social model – and this is thanks in no small part to an enlightened American doctor and psychiatrist named George Engel.2
In 1977, Engel came up with the bio-psycho-social model after observing that doctors tended to see pain as a disease entity separate from man, something caused by an external factor. He also noted that patients themselves, regardless of their knowledge and education, tended to blame their illness on something that had happened to them, such as infection or a fall, and thought of pain as something almost apart from themselves.
The pain-as-separate-entity theory was an appealing one, at least for some practitioners, as it removed the necessity to deal with the emotional elements of a patient’s problem. However, as Engel argued, pain is clearly something very much part of ourselves and it is impossible to treat it without looking at it in an integrated, 360-degree way.
It is a medical approach that sees pain as an experience that results from the deep interrelation of three domains: biology, psychology and sociology.
That’s it!
A simple sentence encapsulating a massive idea.
Biology (genetics, biochemistry), psychology (mood, personality, behaviour) and sociology (culture, family, socio-economics) are the three realms or domains that influence our physical and mental health. When the balance is lost between these three interlinking planes, pain and suffering occur. The ideal place to be is right at the intersection of the three circles – here is a pain-free world where you are able to cope with all of the internal and external factors in your life (see Figure 3 on p79). You juggle them like plates on sticks, managing them all without getting tired or stressed, or using up too much energy. Your universe is balanced. However, if you are not positioned happily in the centre of the three concentric circles – if one of the three elements is under strain or out of sync in some way – then you are likely to be suffering pain. The challenge for any physician is to work out from where in the system the pain is arising.
We are all unique and have vastly differing biological and genetic make-ups. This, together with the experiences we have and the influences exerted upon us throughout our lives, defines our ability to cope with our world. The degree to which we are sensitised or hardened by life depends on all of these elements and how they interact. And so, unsurprisingly, we all experience pain differently.
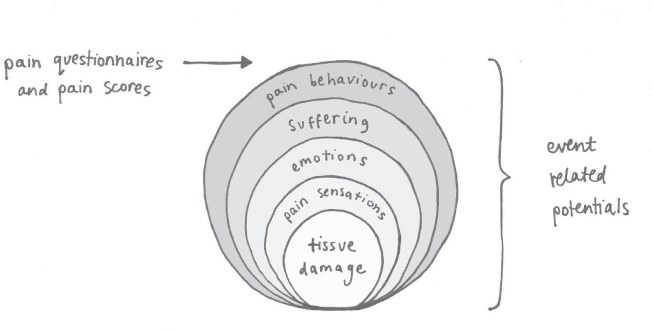
In the 1980s, John Loeser,3 a neurosurgeon and pain researcher based in Washington, Seattle, devised his ‘onion model’ to demonstrate the individual’s tolerance and experience of pain (see Figure 1 below). In it, the onion represents the pain experience and the layers that make up the onion put the pain in context. Interestingly, from his work in paediatrics, Loeser learned that even childhood experiences could modulate the pain experience into adulthood. Premature babies, for example, who routinely have to undergo more medical tests and painful procedures than those born at full term, have been found to be extra-sensitised to pain in adulthood (I go into more detail on this in Chapter 9). They also fear pain more. In addition, it has been well correlated that, due to their longer stays in hospital away from the love and physical contact of their parents, they associate pain with feelings of loss.
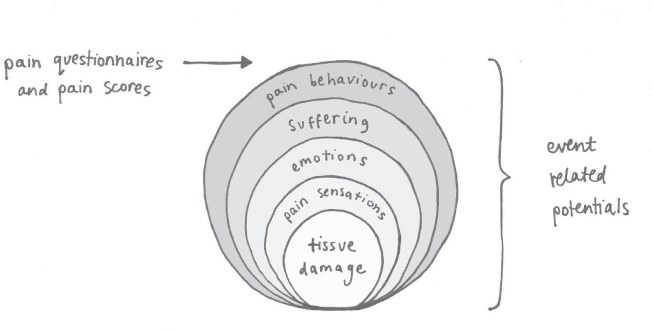
Figure 1: The 'onion model', demonstrating the individual's experience of pain
Pain exists deep inside us, and the practitioner, through history-taking and analysis, must work out which layer of the ‘pain onion’ they can peel away first to get to the cause: how are the elements of the pain overriding and controlling a return to normal? We may never be able to remove some elements but we can hopefully reduce their importance or simply eliminate the extra burden of minor ones so that the patient can cope once more.
Remember earlier, when I said that pain occurs mostly on a neuro-psychological level? Well, what I meant by that was that pain exists predominantly in the nervous system and all its parts. In fact, it could be described as a disease of the nervous system.
Now, this may at first seem like a digression, but I am going to use an analogy here to explain how the nervous system works. It is essentially a sophisticated intelligence-gathering system, and to this extent it is very similar to the CIA. Both systems have a headquarters: for the CIA, it’s Langley, and for the nervous system, it’s the brain. The CIA’s HQ is where all executive decisions are ultimately processed and made. And to make these decisions, HQ relies on a vast network of peripheral monitoring systems (satellite, video, audio, spy reports, encryption etc.) that feed into the centre from around the world, mainly through electronic channels. In the same way, nerves all over the body conduct their information to the brain by means of electrical impulses via the spinal cord which acts like a trunk cable channelling the messages to the brain.
Let’s now look at where the intelligence gathering all starts, i.e. out there on the ground, where teams of field operatives, eavesdroppers and informers are constantly on the alert for intel about threats, potential or actual; in bodily terms, these guys are the sensors at the end of the nerves, and it is they who begin the collation of information and will report it to the station office if the amount of chatter is gathering momentum and could amount to ‘a story’. It is then up to the station office to feed back any intel to the regional bureau (the spinal cord) where it will be evaluated for priority and validity. At this stage, a few senior staff may be woken up to assess the situation but, if it is decided that it is just a few unhappy locals kicking off rather than any real threat afoot, then everyone goes back to bed.
So, as you see, throughout this system there is a hierarchy of stops and checks through which the data goes before it is transmitted ‘bottom up’ for HQ’s attention. All these reporting experts are employed for their innate ability as well as their experience and what they have learned along the way – any ‘noise’, disinformation and ‘fake news’ needs to be filtered out – and they will make snap decisions about what is important and what is not, accordingly.
Similarly, the nervous system will make a judgement about what to refer up to the brain, based on the context and quantity of information received, as well as its past experience. The entire nervous system behaves like a finely tuned, well-oiled intelligence agency that never sleeps, even when you do.
The medical word for all this, the body’s incredible system for gathering intelligence about pain, is nociception, and it is crucial to the understanding of pain. As we will see, there is a big difference between nociception (which you could translate as ‘the process of damaging-stimulus detection’) and the actual conscious experience of pain. And yet this is an area of pain science that is poorly understood by many people, including most doctors, as very little time is spent on it in their training.
In order to survive the multiple threats to our existence, humans have evolved an extraordinary array of special senses and receptors to warn us of danger. These dangers may come in the form of chemical changes (internal or external), thermal changes (extreme temperatures, dry or humid climates), or mechanical changes (physical invasion, such as when our body is struck or pierced, perhaps by a stab wound or needle prick).
All of our special senses are backed up by vision, hearing, smell and taste, which can further inform the brain regarding the level and degree of threat. Moreover, our intricate memory system equips us with the ability not to repeat the action or event which harmed us. This manifests as fear, anxiety or avoidance.
Nociception is basically the neural process of taking the information provided by all these senses and receptors and encoding it to communicate and contribute information to the brain on the potential to cause pain. The information provided by nociception is not necessarily by itself enough to trigger the perception of pain. It is the brain which decides this ultimately, once it has processed the information.
To give an example: imagine you have just slammed your finger in a car door. If your reflex response is quick enough you will withdraw your arm, minimising damage to the tissues. However, the crush effect will be enough to initiate the release of inflammatory chemicals in the skin and tissues, irritating the very small nerves in them. The sensors in the nerves will detect this flood of chemicals and fire impulses up to the spinal cord.
At this point, the spinal cord will assess the level of noise coming from these nerves and initially do two things. Firstly, it will initiate the motor response of pulling your finger back from the source of the damage to prevent further injury. Secondly, it will conduct some of the information to the brain as a report of events, so that the brain can make an ongoing decision about how bad the injury is and what it needs to do to protect you. For example, does it need to send messages to the damaged tissue to cause it to swell, heal, or fight invading bugs? The brain will also make a fleeting assessment of the more long-term impact of the injury – how it will affect your ability to function and carry out daily activities, what threat it may pose to your long-term survival. These assessments are done by the brain’s mood and emotional centres (the limbic centre) as well as the pre-frontal cortex. We know this because extensive research has been carried out, using fMRI technology, which has observed these parts of the brain ‘light up’ as pain is initiated. In some experiments, the effects of administering painful stimuli, such as hot lasers to the skin, in association with different emotions or pain-killing medicines, have been studied. And what these studies have shown is that the areas of the brain which light up change according to the stimulus.
If the healing mechanism for the crushed finger has been efficient and the tissues have recovered, the noise from the local nerves will settle, the spinal cord will lose interest and the brain will no longer be agitated. You won’t notice the pain and can start using the finger again. All is well.
However, if the pain continues beyond a few hours the brain will become more agitated by it and continue with its evaluation. It will assess the injury in terms of how it will affect you and all aspects of your life – your job, caring for children or getting to work. Will I have to take a day off, maybe a week? My boss will be furious, my team rely on me. I have a mortgage to pay, I can’t afford this. Depending on this assessment, the brain may cleverly depress your mood in order to slow you down as a protective measure. On the plains, back in the day, this sort of slow-down was important: it prevented or discouraged you from continuing to use an injured body part and gave you time to recover from a serious infection. Today, it is widely believed that, as part of our evolved socialisation and need for community, such depression or low mood is also a way of showing others in your social group that you are injured and in need of help. Additionally, it alerts you to the danger that lies in becoming isolated – today it translates as ‘Why is Dad grumpy?’
But – and here’s the amazing thing – even in the worst-case scenario, with the noise of nociception at full volume, and all our receptors firing like billy-o, the body has the ability to heal itself. And this is because we are capable of bioplasticity. In fact, we are bioplastic: the sensors in our receptors are constantly being replaced or modified. They have a short life of just a few days and, as new ones replace the old, so we can revert to our previous state. For example, through physiotherapy, the mechano-receptors (which are sensitive to movement) will change their sensitivity and type, as movement is restored and the brain allows the fear element to disperse.
What this means is that our current state of pain is not fixed. On the contrary: because we can have an effect on the replacement of those sensors and their sensitivity, we can change our pain.
For example, if you twist your ankle and tear a ligament in it, yes, it will swell and immediately hurt. The sensors in the ligament and surrounding tissues will start firing all sorts of messages to the spinal cord about the state of the tissue and how badly it is injured. Chemicals released by the injured cells will leak onto sensitive nerves, which will send signals, and pain will be felt. It may be intense enough that you will hobble and stop using the joint to prevent further injury. In return, and at the same time, the brain will mobilise all of the inflammatory and healing chemicals and cells necessary to activate healing. This will continue for three weeks or so, during which time the swelling will subside as it is no longer needed, and, as the cells heal, the production of pain-sensitising chemicals will decrease. The receptors needed for the alarm state will no longer be necessary, and the brain will stop responding.
As you begin to use the ankle again, there will be a transition stage at the receptor level. When loaded with weight, the ankle will feel stiff as the stretch receptors wake up and more receptors are made by the cells to monitor and regulate movement. Once the brain has assessed that the load and movement are not dangerous and causing more injury, it will allow you to be more active. The local mechanoreceptors will change from being ones of alarm to ones of movement and activity.

You may have noticed that I have omitted to mention one particular type of receptor – pain receptors. That is because we don’t have any! Nor do we have any ‘pain nerves’ or ‘pain pathways’ or ‘pain centres’.
And that is because, as I suggested earlier, pain is what we experience once the brain has decided to notice it – usually as a result of it realising that the stimulus is actually or potentially dangerous and when it wants us to realise that some sort of protective response is necessary. And the brain’s decision to notice pain is brought about not just by sensors in our tissues but by the messages from them being filtered and added to by other parts of the nervous system, which assess, modify and decide on whether to make it a problem for us. Our bodies have a network of stations feeding into a ‘decision’ regarding whether to ‘hurt’.
Effectively, only the brain can truly experience hurt or suffering. You might have to think about that one for a minute.
And yet, even more strangely, if I made a neat slice through your cranium right now, flipped your skull open and stabbed you in the brain with a pencil, you wouldn’t feel any pain at all. Any pain you did feel would not be coming from the brain tissue itself but from the damaged nociceptive receptors in the skin, membranes and bone surfaces of the skull that surround it. Brain tissue contains no nociceptive receptors at all. Indeed, we make use of this fact every day in brain surgery, when patients are often awake during an operation, to help the surgeon avoid important territories which would be catastrophic if cut. This is why it may be surprising to hear that brain tumours very rarely present with headache as their main symptom. It is only when the tumour compresses important structures, preventing them from functioning properly, that the first symptoms, such as mood change or epilepsy, tend to occur.
There are two posited explanations for the lack of pain sensation in the brain. Firstly, the brain and spinal cord develop separately from the peripheral nerves of the body at embryo stage and so none of the three main types of nociceptor (mechanical, thermal and chemical) exist in the brain. Anthropologists believe that nature probably also decided that, by the time such receptors were being fired, it was ‘Goodnight Vienna’ anyway, as the degree of damage to ‘mission control’ was too great and so the space taken up by these receptors was better used for other functions.
But then why do we get headaches? Because there are plenty of pain-sensitive structures in the head and neck which can refer pain around the eyes and skull. Headaches are not actually of brain origin.
As I say, pain is what we experience once the brain has decided to notice it. And so it is that most of the time the body’s sensory and nervous systems will respond to ‘damage’ stimuli without us ever actually knowing it. It is only when the brain deems it necessary to ‘express’ these messages and when their summation is enough, that it will bring the problem to our attention consciously, either as a physical reaction (withdraw finger from flame) or as the experience of pain.
In summary, all of these systems are ultimately designed to alert us, raise the alarm in us or, most importantly, protect us. So, though it may be hard to believe, pain is actually good. We know this thanks to a very small group of special but unfortunate individuals who cannot feel pain at all. Some of them don’t live very long and most are besieged by problems they cannot detect as they do not have internal alarm systems (of this, more later.) On a philosophical level, one can also say that pain is important simply because it confirms we exist. Pain and suffering are part of the human condition.

Why is it, then, that some people seem to feel pain more intensely than others? René Descartes believed that pain intensity and type were correlated quite simply with the degree and extent of tissue damage. For example, the more a needle is pressed into the skin the more the pain perceived, regardless of who the individual is experiencing the pain. However, this theory was disproved by research carried out in 1956 by Dr Henry K. Beecher,4 a pioneering military anaesthetist. He compared a number of severely wounded soldiers with a civilian group, and found that less than a quarter of the soldiers had requested any pain relief in the form of morphine, compared to 83 per cent of the civilian group. The troops may of course have just been ‘tougher’, and there was a possibility, according to Beecher, that the soldiers’ ability to cope was also due to the context of the pain, in that for many of them their wound meant that they were out of the fight, they were going home and at least they weren’t dead! But this could not possibly account entirely for how little pain relief the soldiers seemed to need. The study showed that there is actually little correlation between the extent of a pathological wound and the pain experienced.
In 1965, neurobiologist Patrick Wall and psychologist Ronald Melzack got much closer to a viable concept of how pain is perceived and controlled by the central nervous system and spinal cord.5 Their idea came to be known as the ‘gate theory of pain’. It worked on the premise that groups of nerve cells opened and closed ‘gates’, thereby determining whether messages could pass through or not. This also allowed for the idea that there had to be sufficient messages to reach a ‘threshold’ before the central nervous system recognised them. And it showed that there were other processes and factors that determined how and when pain was felt.
In addition, Wall and Melzack experimented with using different stimuli to confuse the brain. They played around with setting contexts around pain stimulation, for example using stress and fear to see if there was a change in the level of pain the subjects reported, which there was. This research provided some insight into the curious fact that pain can continue long after the initial injury has healed, or even exist without injury or a disease process in the first place – a conundrum which has been wonderfully expressed by Dr Fabrizio Benedetti, professor of physiology and neuroscience at the University of Turin,6 and an expert on placebos, who succinctly states: ‘Pain is the product of bottom-up processes and top-down modulation.’
In this chapter we have covered the ‘bottom-up’ process of pain –– i.e. nociception, the nervous system’s sensory response to harmful stimuli – and in the next we will look at the ‘top-down’ bit, that is, how the brain experiences pain, how it reacts, as well as how it is that we can be in pain but not have any discernible physical cause or reason for it.