 ‘Training is patient safety for the next 30 years’1
‘Training is patient safety for the next 30 years’1The Foundation Programme
Applying to the Foundation Programme
The FP curriculum and assessment
Starting as an F1
Communication
Quality and ethics
When things go wrong
Boring but important stuff
Your career
Specialty training applications
 ‘Training is patient safety for the next 30 years’1
‘Training is patient safety for the next 30 years’1
The UK Foundation Programme (FP) was established in 2005 as part of a series of reforms to UK medical training, known collectively as Modernising Medical Careers (MMC). The intention was to provide uniform, 2-year structured training for all newly qualified doctors working in the UK, to build upon medical school education and form the basis for subsequent training. Sadly, much of the introduction of MMC was a shambles. In relative terms the FP fared well, although the early days were not without problems and in 2010 it was still criticized for lacking a clearly articulated purpose.2 Two reports gave a number of recommendations that were taken forward through a series of workstreams that were reviewed in 2015.3 Though the FP continues to evolve, this review did find progress in a number of important domains, including trainee empowerment, assessment outcomes, and the variety of rotations available to trainees. Nationally, a new curriculum was introduced in 2016 (for review in 2021); however, locally the changes necessary to deliver better training are still filtering through. This process is an iterative one that trainees are encouraged to get involved in. Significant changes have been afoot since the 2013 ‘Shape of Training report’ (see Box 1.18,  p. 45).
p. 45).
The FP lasts 2 years, and in >90% of programmes, each year involves rotating through 3 different 4-month placements, which may be in hospital or community-based medicine. About a quarter of programmes involve a placement in a ‘shortage specialty’ (where the number of current trainees is likely to fall short of future consultant needs), and despite a shift towards the management of chronic disease in the community, much of the FP emphasis remains on the acute care of adult patients in a hospital setting. At the start of the FP, you will be required to hold ‘provisional registration’ with the General Medical Council (GMC) (Table 1.1;  p. 3). Strictly, the first FP year (F1) represents the final year of basic medical education and your medical school remains responsible for signing you off; this responsibility may be delegated for those doctors completing F1 in a different region from their medical school. After successfully completing F1, you will be issued with a Certificate of Experience, which entitles you to apply for full GMC registration and start F2. Successful completion of F2 results in the awarding of a foundation achievement of competence document (FACD) which opens the door to higher specialty, core, or GP training (
p. 3). Strictly, the first FP year (F1) represents the final year of basic medical education and your medical school remains responsible for signing you off; this responsibility may be delegated for those doctors completing F1 in a different region from their medical school. After successfully completing F1, you will be issued with a Certificate of Experience, which entitles you to apply for full GMC registration and start F2. Successful completion of F2 results in the awarding of a foundation achievement of competence document (FACD) which opens the door to higher specialty, core, or GP training ( p. 45).
p. 45).
All administrative aspects of the FP are overseen by the UK Foundation Programme Office (UKFPO) which provides many important documents at  www.foundationprogramme.nhs.uk, including the application handbooks, reference guide (the ‘rules’), curriculum (list of educational objectives), and advice for overseas applicants.
www.foundationprogramme.nhs.uk, including the application handbooks, reference guide (the ‘rules’), curriculum (list of educational objectives), and advice for overseas applicants.
Table 1.1 The FP hierarchy
| The GMC | Overall responsibility for setting the standards for medical practice and training in the UK |
| The UKFPO | Manages applications to and delivery of the FP |
| Local Education Training Boards (LETBs) | Part of the Department of Health’s ‘Health Education England’. Deliver the FP regionally and support financial costs of training and trainee salaries ( p. 38) p. 38) |
| Foundation schools | Deliver the FP locally. May overlap with the LETB |
| Director of postgraduate education | Responsible for overseeing all medical training in a hospital ( p. 39) p. 39) |
| Foundation training programme director (FTPD) | Responsible for the management and quality control of the FP in a hospital. Oversees the panel that reviews your annual progress. Responsible for signing off on successful completion of each foundation year |
| Acute Trust/Local Education Provider | Acute trusts provide the employment contract, salary, and HR for foundation doctors. For community placements (eg GP practice), the responsibility for education passes to this ‘Local Education Provider’ but the contract of employment remains with the acute trust. There can be conflicts between the needs of the acute trusts (doctors on the wards delivering services to patients) and some of the educational requirements of the FP ( p. 59) p. 59) |
| Educational supervisor | Doctor responsible for the training of individual foundation doctors. Ideally for a whole year but occasionally for a single attachment. Will review your progress regularly, check that your assessments are up to date, and help you plan your career |
| Clinical supervisors | Doctors who supervise your learning and training, day to day, for each attachment. In some posts (often your 1st) the roles of the educational supervisor and clinical supervisor may be merged |
| Academic supervisor | Those undertaking an academic FP (which includes a designated period of research) will be assigned an individual to oversee academic work and provide feedback |
| Local administrator | Individuals in each trust and Foundation school who help with FP registration and administration |
| FP representative | Leadership position(s) where willing trainees voluntarily facilitate two-way feedback between their peers and their local or regional educationalists |
| The Foundation Doctor | This is you! You are an adult learner with responsibilities for your own learning. You are expected to integrate with the educational processes of the FP, including providing feedback on the programme to your supervisors, trainee representatives, and via local and national training surveys |
All applications to the FP are through the online FP Application System (FPAS) at  www.foundationprogramme.nhs.uk. There are several stages.
www.foundationprogramme.nhs.uk. There are several stages.
Registration for FPAS You will need to be nominated. For final year students in the UK your medical school will do this for you. Those applying from outside the UK should contact the UKFPO Eligibility Office in good time to allow checks to take place.4 Before nomination you can register for an account but cannot access the application form.
Completing the application form Within a designated window each year (usually in early October), nominated applicants will be able to access the application form. This has a number of parts:
Personal Name, contact details, DoB, and relevant personal health.
Eligibility GMC status, right to work in the UK, and immigration status.
Fitness Criminal convictions and fitness to practise proceedings.
Referees Details of 2 referees (1 academic, 1 clinical). Their knowledge of your performance is more important than their seniority because they contribute to your pre-employment checks (re suitability for work) rather than your actual programme allocation.
Competences Educational qualifications ± postgraduate experience.
Evidence You will be asked to list any additional degrees for scoring against a very specific system and to upload a copy of certificates; 5 total percentage points are available for your degree, with 2 further points for publications (proof is required and will be assessed).
Clinical skills You will be asked to self-assess against a list of practical skills—this does not form part of the assessment process but will be used by Foundation schools to coordinate training.
Academic selection If applying to the academic FP ( p. 6).
p. 6).
UoA preferences Foundation schools are grouped into Units of Application (UoA) that process applications jointly. You will be asked to rank all UoA in order of preference, with successful applicants allocated to UoA in score order (you will be allocated to your highest preference UoA that still has places when your turn comes). Tables showing vacancies and competition ratios for previous years are available on the UKFPO website but these do tend to vary between years (see Box 1.1).
Equal opportunities To monitor NHS recruitment practices.
Declaration You are required to sign various declarations of probity.
Linked applications Two applicants can join their applications ( pp. 6–7).
pp. 6–7).
Scoring Your application will be scored based upon 2 components:
Educational Performance Measure (50 points) This comprises a score between 34 and 43 based upon which decile your medical school decides your performance falls in, relative to your peers (this is locally determined) with 7 further points for education achievements detailed on the application form as previously mentioned.
Situational Judgement Test (50 points) See Boxes 1.2 and 1.3.
Box 1.1 Units of Application and 2017 competition data
The 21 UoA shown are the Foundation Schools for the 2017 application. Note, in April 2017 NC and NE Thames merged into the North Central and East London Foundation School. Vacancy numbers for 2017 are shown, with figures in brackets representing the number of applicants ranking the UoA as their first preference, expressed as a percentage of this number of jobs. Source: data from  www.foundationprogramme.nhs.uk
www.foundationprogramme.nhs.uk
 Box 1.2 Situational Judgement Test (SJT)
Box 1.2 Situational Judgement Test (SJT)
These computer-marked tests of 70 questions sat under examination conditions over 2h 20min confront you with situations in which you might be placed as an F1 doctor, and ask how you would respond. There are two basic response formats: (i) rank five possible responses in order and (ii) choose three from eight possible responses. Marks are assigned according to how close to an ‘ideal’ answer you come, with marks for near misses and no negative marking. Raw scores are subject to statistical normalization and scaling to generate a final mark out of 50. Officially, you cannot ‘revise’ for the test, as it is an assessment of attitudes, but there is a strong weighting on medical ethics which can be revised, and you can familiarize yourself with what is expected and try to understand model answers.5 When introduced into FP selection for 2013 appointments, problems with SJT marking led to hundreds of altered offers. Ongoing controversy surrounds SJTs as a means of selection, the thin evidence base behind them, and the heavy weighting they receive. One prominent researcher and SJT advocate closely involved in the pilots is also a director of a company that provides SJTs, as well as being a key figure behind the selection process that so spectacularly failed during the 2007 MMC reforms. Nonetheless, it is difficult to argue that previous systems based upon answering generic questions or students competing to get references from a few blessed Professors were any better. Our advice for now: ‘Get studying!’
 Box 1.3 The Prescribing Safety Assessment (PSA)
Box 1.3 The Prescribing Safety Assessment (PSA)
Prescribing is a fundamental part of the FP and it is now a requirement for UK FP applicants to demonstrate their knowledge of the safe and effective use of medicines through completion of this national pass/fail prescribing skills assessment. Piloted in 2010 in response to a GMC-sponsored survey which showed that 9% of hospital prescriptions contain errors, applicants are tested on common prescriptions, medications, drug calculations, and monitoring regimens that are encountered during the FP. Exams take place at UK medical schools between February and June each year, and non-UK trainees can sit it during F1.6
For those interested in research, teaching, or management, the Academic FP offers 7450 programmes with time set aside for academic work (either a rotation or time spread across the year) ( p. 12, p. 66).7 Aside from extra sections on academic suitability, the application form is the same, ranking up to 2 ‘Academic’ UoAs (which differ slightly from standard UoAs) and some Academic FPs within them. Shortlisted candidates are interviewed and offers made in advance of the main FP selection process, so that unsuccessful applicants can still compete for a regular FP position.7
p. 12, p. 66).7 Aside from extra sections on academic suitability, the application form is the same, ranking up to 2 ‘Academic’ UoAs (which differ slightly from standard UoAs) and some Academic FPs within them. Shortlisted candidates are interviewed and offers made in advance of the main FP selection process, so that unsuccessful applicants can still compete for a regular FP position.7
Your total score will be used to determine your place in the queue for matching to a FP, and you will be offered a place in your highest preference UoA which still has FP vacancies when your turn comes. Results will be communicated by email and you will have a limited window to accept this. Allocation to an individual programme is done based on your total application score and your ranking of individual programmes. Some UoAs (eg those with more programmes) have a two-stage match process where you rank groups of trusts before ranking the programmes within the group to which you have been allocated. However, most UoAs use a one-stage process where you simply rank all of the individual programmes from the outset. Further information is available on each UoA website.
A typical F1 year usually consists of three placements of 4mth: one in a general medical specialty, one in a general surgical specialty; options for the third specialty vary widely in just about all areas of medicine. F2 posts also typically consist of three 4mth jobs; for 80% of F2s one of these will be a GP placement. Allocation to F2 posts varies between UoAs, with some assigning all F1 and F2 posts at the outset, while others may invite you to select F2 posts during your F1 year. Once you are appointed to the FP, you are guaranteed an F2 post in the same Foundation school, but often in a different acute trust. If you do not get an F2 post in a specialty you are particularly interested in, most will allow individual FP doctors to swap rotations, providing they have the support of their educational supervisors. Some Foundation schools will organize ‘swap shops’ to facilitate this process, but swapping can be notoriously difficult. You can also arrange ‘taster weeks’ in another specialty to help plan your career; to arrange these talk to your educational supervisor, clinical supervisor, and a consultant in the relevant specialty.
During the FPAS application process, it is possible for any two individuals to link their applications. In this case, you must both supply each other’s email addresses in the relevant section of the application form, and rank all UoAs in identical order. The score of the lower scoring applicant will then be used to allocate both applicants to the same UoA. Although policies vary between UoAs, linking does not necessarily guarantee appointment to the same trust or town—check individual UoA websites for their policies. Note also that if one of you accepts a place on an Academic FP or is put on the reserve list, the link is broken.
In recent years, the supply of applicants has threatened to exceed places on the FP. Those whose FPAS scores place them below the cut-off to be guaranteed a FP post will be placed on a reserve list and are often able to gain a training post when an unexpected event befalls another candidate. If you are not successful in securing a post first time round do not give up hope! If you feel you have been unfairly marked you may be able to appeal; discuss this with your medical school dean. Try to seek feedback from the application process in order to identify weaknesses that you may be able to amend in case you have to wait to reapply the next year. Should you still be without a post after you know you have qualified from medical school, contact LETBs and hospitals directly; some of your peers may not be able to take up their posts due to exam failure so you may be able to apply directly to these standalone posts.
Another option is to consider taking a year out, either to strengthen your application by doing research, further study, or other activities that add to your skills. Also consider applying overseas; it has been possible in previous years to do some or all of foundation training in Australia or New Zealand with prior approval of posts from a UK LETB. Alternatively, it is possible to apply to any post within the EU or to consider equivalency exams for other countries.
Finally, there is always the option of a career outside of medicine. Advice on this and other options will be available from your university careers office, from websites such as Prospects ( www.prospects.ac.uk) or certain courses/conferences (eg
www.prospects.ac.uk) or certain courses/conferences (eg  www.medicalsuccess.net).
www.medicalsuccess.net).
For those who meet the very specific criteria, it may be possible to be pre-allocated to a specific Foundation school, regardless of your FPAS score. These cases include if:
• You are a parent or legal guardian of a child <18yr, for whom you have significant caring responsibilities
• You are a primary carer for a close relative
• You have a medical condition or disability for which ongoing follow-up in the specified location is an absolute requirement.
If any of these apply to you, discuss with your medical school dean or tutor well in advance of the application process opening.
Those wishing to train less than full-time should apply through the FPAS alongside other candidates; upon successful appointment, they should contact their new Foundation school to discuss training opportunities and plans. Programmes have good arrangements for LTFT, whereby trainees are paid on a ‘pro rata’ basis for all work done, as a proportion of the full-time salary.
The FP Curriculum acts as a guide for what you will be expected to achieve over the 2 years of the FP, how you will get there, and how you will be assessed. There are 20 Foundation training outcomes (Box 1.4) that are grouped according to the GMC’s ‘Good Medical Practice’. To complete the FP you must keep a record of your experiences, reflections, and study (the NHS ePortfolio) to demonstrate that for each of the outcomes you have acquired the minimum level of competence required.
Box 1.4 Foundation Professional Capabilities
Source: data from  www.foundationprogramme.nhs.uk
www.foundationprogramme.nhs.uk
NHS ePortfolio The ePortfolio is an electronic record of your progress through the FP. The syllabus lies at its centre, to which you can link evidence of achievement of competence using a number of tools. Alongside this lies your supervisor and end-of-year reports. The ePortfolio may also be used for specialty training interviews to show competence and achievement and as a library for a wide range of support material (see Boxes 1.4, 1.5, and 1.19,  p. 8, p. 10, p. 57). It is vital that you engage with your ePortfolio early on and keep it updated, as it is the primary measure by which you are assessed. While the effort required is not small, the time and energy your supervisors need to review your ePortfolio should also not be underestimated. You are both helped by keeping your electronic and paper portfolios organized, current, and complete (Box 1.19,
p. 8, p. 10, p. 57). It is vital that you engage with your ePortfolio early on and keep it updated, as it is the primary measure by which you are assessed. While the effort required is not small, the time and energy your supervisors need to review your ePortfolio should also not be underestimated. You are both helped by keeping your electronic and paper portfolios organized, current, and complete (Box 1.19,  p. 57).
p. 57).
Assessment Assessment is based on observation in clinical practice, your ePortfolio evidence supporting curriculum competence (see Table 1.2), evidence of engagement in learning, and proficiency in the GMC’s core procedures. Direct observation comes from your supervisors but also other work colleagues in the form of a Team Assessment of Behaviour and feedback from your Placement Supervision Group. Formative assessments are ways of seeking feedback whereas summative assessments are to demonstrate competence—both are equally important. The burden of what many see as a tick-box exercise is still significant, though improving slowly with each FP curriculum revision. Assessment culminates in the Annual Review of Competence Progression (ARCP), which determines your eligibility to move on to training.
Meetings There are a number of meetings you need to record in your ePortfolio. These are detailed in Box 1.6.
Table 1.2 Supervised learning events (SLEs) and assessments
|
|
||
|
Direct observation of doctor/patient encounter: Mini-clinical evaluation exercise (mini-CEX) Direct observation of procedural skills (DOPS) |
≥9 per year—including ≥6 mini-CEX (≥2 per attachment)* | |
| For mini-CEX, you will be observed speaking to and/or examining a patient and receive feedback on your performance. For DOPS, you will be observed performing a clinical skill and receive feedback on your interaction with the patient. | ||
| Case-based discussion (CbD) | ≥6 per year (≥2 per attachment) | |
| You will present and discuss a case (or an aspect of a complex case) you have been closely involved in and discuss the clinical reasoning and rationale. | ||
| Developing the clinical teacher | ≥1 per year | |
| This requires you to deliver an observed teaching session—you will receive feedback based on your preparation, teaching, knowledge and audience interaction. | ||
|
|
||
| Core procedure assessment forms | 1 per procedure during F1 | |
| By the end of F1 you need to be signed off as competent in 15 core procedures: | ||
| Team assessment of behaviour (TAB) | 1 per year | |
| You will be required to engage in a Maoist process of self-criticism, then select a minimum of 10 colleagues who will be invited to provide anonymous feedback, including at least 2 consultants/GPs, 1 other doctor >FY2, 2 senior nurses >band 5, and 2 allied health professionals/other team members (eg ward clerks, secretaries, and auxiliary staff). Similar feedback comes from your Placement Supervision Group but they are nominated by your supervisor rather than by you. Your educational supervisor will then collate all the results and share them with you. | ||
*There is no minimum number of DOPS required per year.
 Box 1.5 Keeping the ePortfolio
Box 1.5 Keeping the ePortfolio
As well as recording your structured learning events, you can upload a wide range of other documents to your ePortfolio to serve as evidence of your progress. Some suggestions include:
• Copies of discharge/referral letters (anonymized)8
• Copies of clerkings (anonymized)8
• Attendance at clinic (date, consultant, learning points)
• Procedures (list of type, when, observing, performing, or teaching)
• Details of any complaints made against you and their resolution
• Incident forms you have been involved in (useful for reflective practice and demonstrating that you have learned from mistakes)
• Copies of presentations given
• Details of teaching you’ve done (with feedback if possible)
 Box 1.6 Meetings during the FP
Box 1.6 Meetings during the FP
There are a number of required meetings which you should record in your ePortfolio. The onus is on you to schedule and prepare for these meetings: you and your supervisors are all busy clinicians, and it can sometimes be difficult to arrange these in a timely manner. Be flexible but persistent!
Induction At the start of each placement you should meet with both your educational and clinical supervisors9 to agree learning objectives and review what opportunities are available during the placement.
Midpoint Meetings in the middle of each placement with your supervisors to review progress are encouraged, particularly where you or they have concerns, but are not compulsory. You may also decide to have a mid-year review with your educational supervisor.
End of placement Both your supervisors should meet with you separately to review your achievements, pass on the observations of the team, provide advice, and listen to your feedback.
End of year You should meet your educational supervisor to discuss your total progress. Your supervisor will complete a report for the panel performing your annual review to inform their decision to sign you off.
The NHS is the world’s 5th largest employer and while impossible to appreciate fully, a general understanding helps contextualize your role. Since its inception in 1948, the NHS has aimed to provide quality care that is free at the point of use and based on clinical need alone. It is an important part of our UK identity and by global standards, per capita, is good value for money.
Government Since 1999, devolved governments in Wales, Scotland, and N Ireland have had control over their NHS and healthcare budgets. Funding comes almost entirely from taxation, totalling £120bn/yr in England. Department of Health Government department led by the Health Secretary responsible for healthcare policy and overseeing the NHS in England. Health and Social Care Act A 2012 parliament act and the largest NHS reorganization since 1948, legislated for more healthcare regulation and patient involvement, and decentralization of healthcare/budget responsibility. Allowed business to compete with NHS providers for service provision. Commissioners With two-thirds of the total NHS budget, GPs, nurses, hospital doctors, and lay members now lead >200 clinical commissioning groups (CCGs) in buying (commissioning) local services (including secondary care, mental health, and community services). GPs themselves as well as highly specialized services are still commissioned nationally. Providers Commissioners purchase services from providers, which can be GPs, the private sector, voluntary sector, or hospitals. Most trusts are ‘Foundation’ Trusts, that is, have more financial and managerial freedom (the intention being to provide more flexibility to better suit local patient needs).
Arm’s-length bodies Non-departmental public bodies that are associated with but have some independence from the Department of Health. Health Education England Ensures the workforce has the skills to support healthcare and drive improvements. Coordinates training locally through 4 LETBs and 13 deans, including the 20 Foundation schools ( p. 3). Healthcare regulators The Care Quality Commission (for care quality) and NHS Improvement (for finances) are responsible for monitoring, inspecting, and reporting on providers to ensure they provide quality care within the resources available. Both have powers to advise and intervene if necessary. National Institute for Health and Care Excellence (NICE) By balancing the potential gains in quality and quantity of life against financial costs, NICE provide guidance to patients and providers on the efficacy and cost-effectiveness of new treatments and technologies over previous ones.
p. 3). Healthcare regulators The Care Quality Commission (for care quality) and NHS Improvement (for finances) are responsible for monitoring, inspecting, and reporting on providers to ensure they provide quality care within the resources available. Both have powers to advise and intervene if necessary. National Institute for Health and Care Excellence (NICE) By balancing the potential gains in quality and quantity of life against financial costs, NICE provide guidance to patients and providers on the efficacy and cost-effectiveness of new treatments and technologies over previous ones.
Outside agencies ( p. 3, p. 12)
p. 3, p. 12)
Trade unions Represent doctors and if supported by members can call for industrial action over employment disputes. Campaign for better conditions and comment on health issues. British Medical Association The largest doctors’ trade union, for GPs and hospital doctors alike. Hospital Consultants and Specialists Association Focuses on the needs of hospital doctors. General Medical Council An independent regulator responsible for maintaining the official register of UK medical practitioners, controlling entry onto the register, and removing members where necessary. The GMC sets the standards that doctors and medical schools should follow. Medical Royal Colleges Independent professional bodies that develop and provide training in the various medical specialties. 21 are members of the Academy of Royal Colleges which promotes and coordinates their work. Faculty of Medical Management and Leadership A faculty of the Academy of Royal Colleges that is dedicated to medical leadership. A good resource for trainees interested in medical leadership and management.
The prices quoted change frequently; they are intended as a guide.
General Medical Council (GMC) To work as a doctor in the UK you need GMC registration with a licence to practise; £50 for F1 (provisional registration), £150 for F2 (full registration), and £390 thereafter.
NHS indemnity insurance This covers the financial consequences of mistakes you make at work, providing you abide by guidelines and protocols. It automatically covers all doctors in the NHS free of charge.
Indemnity insurance This is essential; do not work without it. These organizations will support and advise you in any complaints or legal matters that arise from your work. They also insure you against work outside. There are three main organizations; all offer 24h helplines ( pp. 614–615):
pp. 614–615):
• Medical Protection Society (MPS)—£10 for F1, £20 for F2
• Medical Defence Union (MDU)—£10 for F1, £20 for F2
• Medical and Dental Defence Union of Scotland—£10 for F1, £35 for F2.
British Medical Association (BMA) Membership benefits include employment advice, a contract checking service, a postal library, and a weekly subscription to the BMJ. Annual costs are £115 for F1s and £226 for F2s.
Hospital Consultants and Specialists Association Alternative trade union for those planning a career in hospital medicine. Benefits include employment advice, contract checking, personal injury service, and legal services. Annual cost is £100 for foundation trainees.
Income protection Pays a proportion of your basic salary ± a lump sum (rates vary) until retirement age if you are unable to work for health reasons. Check if it covers mental health problems, and if it still pays if you are capable of doing a less demanding job. NHS sickness benefits are not comprehensive (providing F1s 1mth full pay, 2mth half pay, and F2s 2mth full pay, 2mth half pay): Available from various providers, typically starting at £24/mth as an F1, rising according to age, pay, illness, and risks.
2015 NHS Pension Scheme A proportion of your pay is put into the scheme to be returned, with additional interest and employer contributions, during your retirement. Despite bringing the retirement age in line with the state pension, an increase in the cost of personal contributions, and a shift from final salary to career-averaged earnings, the 2015 NHS Pension Scheme remains the best pension available; do not opt out.
P45/P60 tax form When you leave a job you will receive a P45; if you continue in the same job you will receive a P60 every April. These need to be shown when starting a new job.
Bank details Account number, sort code, and proof of address.
Hepatitis B You need proof of hep B immunity and vaccinations. You should keep validated records of your immunizations and test results.
GMC registration certificate This proves you are a registered doctor.
Disclosure and Barring service (DBS) certificate (formerly CRB checks) It is the employer’s responsibility to perform these checks. You must complete all paperwork in good time, but payment is the responsibility of the trust.10
Preparation for professional practice This mandatory week of paid induction is usually online and face-to-face but there is a difference between what you want to know before starting and what trusts are obliged to tell you. The best people to talk to are your predecessors, but a little background reading about your first rotation specialty also helps. To reduce the cost of face-to-face induction there is a trend towards eLearning, but the BMA is clear: induction is work and if done outside of work should be reciprocated financially or with time off in lieu.
Pay roll It can take over a month to adjust pay arrangements so it is vital to give the finance dept your bank details on or before the first day if you want to be paid that month. Hand in a copy of your P45/P60 too.
Parking Check with other staff about the best places to park and ‘parking deals’; you will probably need to get several people to sign a form.
Cycling Trusts usually provide safe storage for bikes and sometimes you can save money on repairs/new purchases with ‘cycle to work’ schemes.
ID badge Used to access secure parts of the hospitals. If you need more access than most (e.g. crash team members) then request ‘access all areas’. If the card doesn’t give access then return it or get it fixed.
IT Computer access allows you to access results, the Internet, and your trust email. Also ask for an NHS.net account so you can access it securely from home and keep the same email when moving between trusts. Memorize all the passwords, usernames, etc and keep any documents handed out. Ask for the IT helpdesk phone number in case of difficulty.
Rota coordinator You should get to know your medical staffing department well as they can make your life a lot easier. If you haven’t received your rota in advance then get in touch with them.
Mobiles and social media Induction may be the last time for a while you are all in one place. Exchanging numbers makes social activities, rota swaps, and learning opportunities easier to organize, but there will usually be rolling, trust-wide WhatsApp groups you can join. If not, create one/ask your FP representative to coordinate efforts (Box 1.7).
Try to get a map; many hospitals have evolved rather than been designed. There are often shortcuts.
Wards Write down any access codes and find out where you can put your bag. Ask to be shown where things are kept including the crash trolley and blood-taking equipment.
Canteen Establish where the best food options are at various times of day. Note the opening hours—this will be invaluable for breaks on-call.
Cash and food dispensers Hospitals are required to provide hot food 24h a day. This may be from a machine.
Doctors’ mess Essential. Write down the access code and establish if there is a fridge or freezer. Microwave meals are infinitely preferable to the food from machines. For problems, contact the mess president.
Most hospitals have an occupational health department that is responsible for ensuring that the hospital is a safe environment for you and your patients. This includes making sure that doctors work in a safe manner. You can find your local unit at  www.nhshealthatwork.co.uk
www.nhshealthatwork.co.uk
During the FP, your contact with occupational health is likely to be one of the following:
Initial check Depending on the procedures you will be undertaking, you may require a blood test to show you do not have hepatitis C or HIV; they will need to see photographic proof of identity, eg a passport.
Hepatitis B booster This depends on local policies and your antibody levels.
Needle-stick/sharps injury/splashes ( p. 108).
p. 108).
Illness Illness that affects your ability to work may require a consultation.
Patients are commonly infected by pathogens from the hospital and ward staff. The infections are more likely to be resistant to antibiotics and can be fatal. It is important to reduce the risk you pose to your patients:
• If you are ill, stay at home, especially if you have gastroenteritis
• Keep your clothes clean and roll up long sleeves to be bare below the elbows in clinical areas
• White coats, ties, and long sleeves are generally discouraged
• Avoid jewellery (plain metal rings are acceptable) and wrist watches
• Clean your stethoscope with a chlorhexidine swab after each use
• Wash your hands or use alcohol gel after every patient contact, even when wearing gloves; rinsing all the soap off reduces irritation. Clostridium difficile spores are resistant to alcohol, so always wash your hands after dealing with affected patients
• Be rigorous in your use of aseptic technique
• Use antibiotics appropriately and follow local prescribing policies. For more information, contact your local infection control team.
As a doctor you will come into contact with bodily fluids daily. It is important to develop good habits so that you are safe on the wards:
• Wear gloves for all procedures that involve bodily fluids or sharps. Gloves reduce disease transmission if penetrated with a needle—consider wearing two pairs for treating high-risk patients
• Dispose of all sharps immediately; take the sharps bin to where you are using the sharps and always dispose of your own sharps
• Vacutainers are safer than a needle and syringe. Most hospitals now stock safety cannulas and needles for phlebotomy, use of which decreases the risk of needle-stick injuries yet further
• Mark bodily fluid samples from HIV and hepatitis B+C patients as ‘High Risk’ and arrange a porter to take them safely to the lab
• Consider wearing goggles if bodily fluids might spray
Black pens These are the most essential piece of equipment. Carry a few as people often lose theirs. Blood bottles are usually labelled with printed stickers but specimen bottles may still need a ballpoint pen.
Stethoscope A Littmann® Classic II or equivalent is perfectly adequate, however better models do offer clearer sound.
Money and cards Out-of-hours loose change is useful for food dispensers but most places will take cards.
ID badge Should be supplied on day 1 and may come with a printer fob.
Bleep Often at switchboard, in handover, with colleagues or on the ward.
Mobile phone A plethora of medical apps can make your life much easier; however, signal can be variable so don’t forget your bleep. Always check who has written your apps and whether it is a reliable source. Most Oxford Handbooks, including this one, are now available as an app. Although previous rules restricting their use have largely been eased, it does not look good to be always on your phone, and it remains the case that they can interfere with monitoring equipment in ICUs, CCUs, and surgical theatres.
Clipboard folder  p. 18.
p. 18.
Pen-torch Useful for looking in mouths and eyes; very small LED torches are available in ‘outdoors’ shops or over the Internet and can fit onto a keyring or be attached to stethoscopes to prevent colleagues borrowing and not returning them.
Tendon hammer These are hard to find on wards. Collapsible pocket-sized versions can be bought for £12–15.
Alcohol gel Clip-on alcohol gels are cheap, will mean you never have to go searching, and can be more ‘predictable’ than those on the ward.
Patients and staff have more respect for well-dressed doctors, however it is important to be yourself; be guided by comments from patients or staff.
Hair and piercings Long hair should be tied back. Facial metal can be easily removed while at work; while ears are OK, other piercings draw comments.
Shoes A pair of smart, comfy shoes is essential—you will be on your feet for hours and may need to move fast.
Scrubs Ideal for on-calls, especially in surgery. Generally they should not be worn for everyday work. Check local policy.
 Box 1.7 Social media
Box 1.7 Social media
The GMC, BMA, and individual trusts publish guidance for doctors regarding their use of social media. While Facebook, Twitter, and WhatsApp have many benefits for us as professionals and individuals, all blur the line between public, private, and professional life and none guarantee confidentiality. In using them we must remember our duty of confidentiality, to treat colleagues fairly, and to maintain trust in the profession. Any posts should consider the impact on patients, yourselves, and the profession, avoiding derogatory or offensive comments. Misuse can lead to action by trusts or the GMC.
Being an F1 involves teamwork, organization, and communication—qualities that are not easily assessed during finals. As well as settling into a new work environment, you have to integrate with your colleagues and the rest of the hospital team. You are not expected to know everything at the start of your post; you should always ask someone more senior if you are in doubt.
As an F1, your role varies greatly (ask your predecessor) but includes:
• Clerking patients (ED, pre-op clinic, on-call, or on the ward)
• Updating patient lists and knowing where patients are ( p. 18)
p. 18)
• Participating in ward rounds to review patient management
• Requesting investigations and chasing their results
• Liaising with other specialties/healthcare professionals
• Practical procedures, eg taking blood ( pp. 528–529), cannulation (
pp. 528–529), cannulation ( pp. 532–533)
pp. 532–533)
• Administrative tasks, eg theatre lists ( p. 114), TTOs (
p. 114), TTOs ( pp. 80–81), rewriting drug charts (
pp. 80–81), rewriting drug charts ( pp. 171–172), death certificates (
pp. 171–172), death certificates ( pp. 98–99)
pp. 98–99)
• Speaking to the patient and relatives about progress/results.
Discharge letters are your responsibility and without them patients cannot leave the hospital. Not only are well patients very keen to be at home, unwell patients needing admission also need to leave the Emergency Department and come into their bed. This process is called patient flow and is vital in the day-to-day running of the hospital and making sure patients are being cared for in the right environment. While there are many factors that slow down patient flow, patients, clinicians, and management staff will thank you if high-quality discharge letters are prepped well in advance. Keeps tabs on estimated discharge dates and if you’re not sure, enquire with your colleagues about who may be going home tomorrow.
Missing breaks does not make you appear hard-working—it reduces your efficiency and alertness. Give yourself time to rest and eat (chocolates from the ward do not count); you are entitled to 30min for every 4h worked. Use the time to meet other doctors in the mess; referring is much easier if you know the team you are making the referral to.
If you are unsure of something, don’t be embarrassed to ask a senior, particularly if a patient is unwell. If you are stuck on simple tasks (e.g. cannulation), take a break and either try later or ask a colleague to try.
F1s may have to make difficult decisions, some of which may have potentially serious consequences. Always consider the worst-case scenario and how to avoid it. Be able to justify your actions and document everything carefully.
For all patients under your care, seniors will reasonably expect you to know the current problem list, medication, and the details of any recent procedures or investigations, including key recent blood results. Initially this may well seem impossible, but with time and careful practice, your memory for such details will improve.
What at first seems like a badge of having ‘made it’ quickly becomes the bane of your existence. When the bleep goes off repeatedly, write down the numbers then answer them in turn. Try to deal with queries over the phone; if not, make a list of jobs and prioritize them, tell the nurses how long you will be, and be realistic. Ask nurses to get useful material ready for when you arrive (eg an ECG, urine dipstick, the obs chart, notes, equipment you may need). Encourage ward staff to make a list of routine jobs instead of bleeping you repeatedly. The bleep should only be for sick patients and urgent tasks. Learn the number of switchboard since this is likely to be an outside caller waiting on the line. Crash calls are usually announced to all bleep holders via switchboard. If your bleep is unusually quiet, check the batteries. Consider handing over your bleep to a colleague when breaking bad news, speaking to relatives, or performing a practical procedure.
Dropping the bleep in the toilet This is not uncommon; recover the bleep using non-sterile gloves. Wash thoroughly in running water (the damage has already been done) and inform switchboard that you dropped it into your drink.
Other forms of bleep destruction You should not have to pay for a damaged bleep, no matter how dire the threats from switchboard; consider asking for a clip-on safety strap.
You need to be proactive to learn interpretation and management skills as an F1. This is especially true when most of the decisions you make will be reviewed by a senior almost immediately. Despite this, ‘Bloods, CXR, senior r/v’ is not an adequate plan and represents a failure to engage with a learning opportunity. Formulate an impression, differential diagnosis, and management plan for each patient you see and compare this with your senior’s version; ask about the reasons for significant differences. See Box 1.8.
 Box 1.8 Service provision vs training?
Box 1.8 Service provision vs training?
Acute trusts need doctors to see patients so that they can be treated, discharged, and the trust reimbursed. Behind this simple fact lies an important point of tension between the aims of the trust and those of the individual doctor who will want to develop and acquire new skills. As a foundation doctor, you are in an educationally approved post, for which the LETB releases funds to the trust. It is therefore important that you should be given the opportunities to train and develop, and that you should be released from routine ward work to attend all dedicated training sessions. At the same time, the discharge summaries need to be typed, the drug charts rewritten, and a seemingly endless number of venflons resited. The challenge for all involved is to achieve educationally useful outcomes within these constraints. This situation is not unique to the FP—all doctors within the NHS have to balance these demands and some of those tasks you aspire to be able to perform will be the same tasks that have become routine and even frustrating for your seniors. There are no magic answers, but a preparedness to work hard, a keenness to seize educational opportunities whenever they present, and a supportive educational supervisor will all go a long way.
Your organizational abilities may be valued above your clinical acumen. While this is not why you became a doctor, being organized will make you more efficient, ensure you go home on time, and free up time to make the most of learning opportunities as and when they arise.
Your ward All departments have different ways of working and these will usually have evolved this way over time for good reason. Equally, some things may have become out of date and may need updating. If you have an idea, discuss it with your predecessors and seniors and consider taking the lead on an audit or quality improvement project.
Folders and clipboards These are an excellent way to hold patient lists, job lists, handbooks, and spare paperwork along with a portable writing surface. Imaginative improvements can be constructed with bulldog clips, plastic wallets, and dividers.
Contents Spare paper, drug charts, DNAR forms, phone numbers, job lists, patient lists, theatre lists, spare pens, and ward access codes.
Patient lists Juniors are often entrusted with keeping a record of the team’s patients (including those on different wards, called ‘outliers’) along with their background details, investigation results, and management plans. With practice, most people become good at recalling this information, but writing it down reduces errors. They are usually electronic and may be manually or automatically generated, allowing every team member to carry a copy. Lists can be invaluable for discussing/referring a patient while away from the ward but must be kept confidential and disposed of securely ( p. 83).
p. 83).
Job lists During the ward round make a note of all the jobs that need doing either on your list or on a separate piece of paper. At the end of the round, these jobs can be distributed among your other team members.
Serial results Instead of simply writing blood results in the notes, try writing them on serial results sheets (with a column for each day’s results). This makes patterns easier to spot and saves time.
Timetables Along with ward rounds and clinical jobs there will be many extra meetings, teaching sessions, and clinics to attend. There are three blank timetables at the end of this book to use for this purpose.
Important numbers It can take ages to get through to switchboard so carrying a list of common numbers will save you hours (eventually you will remember them). At the end of this book there are three blank phone number lists for you to fill in. Blank stickers on the back of ID badges can hold several numbers.
Ward cover equipment Finding equipment on unfamiliar wards wastes time and is frustrating. You can speed up your visits by keeping a supply of equipment in a box. Try to fill them with equipment from storerooms instead of clinical areas. Alternatively, if you are bleeped by a nurse to put in a cannula, you could try asking them nicely to prepare the equipment ready for you for when you arrive (it works occasionally).
Despite the years spent at medical school preparing for finals and becoming a doctor, being efficient is one of the most important skills you can learn in the FP and one that you will value throughout your career.
Working hours While you are contracted to work a fixed number of hours you will usually work more, especially towards the beginning of your career. To make your day run as smoothly as possible consider arriving early, before your seniors, to prepare for the day (e.g. review unwell patients, overnight events, nursing concerns, patient lists, and latest test results).
Time management You will nearly always seem pressed for time, so it is important to organize your day efficiently. Prioritize tasks in such a way that things such as blood tests can be in progress while you chase other jobs. Requesting radiology investigations early in the day is important as lists get filled quickly, whereas writing blood forms for the next day and prescribing warfarin can wait till later on. Prepare discharge summaries and TTOs well in advance to avoid being the rate-limiting step in getting patients home.
On-call It will seem like your bleep never stops going off, especially when you are at your busiest. Always write down every job, otherwise you run the risk of forgetting what you were asked to do. Consider whether there is anyone else you could delegate simple tasks to, such as nurse practitioners or ward staff while you attend to more urgent tasks.
• Make a list of common bleeps/extensions ( p. 622)
p. 622)
• Establish a timetable of your firm’s activities ( p. 623)
p. 623)
• Make a folder/clipboard ( p. 18)
p. 18)
• Prioritize your workload rather than working through jobs in order. Try to group jobs into areas of the hospital. If you’re unsure of the urgency of a job or why you are requesting an investigation, ask your seniors
• If you are working with another foundation trainee, split the jobs at the end of the ward round so that you share the workload
• Run through the patient list throughout the day to review progress
• Submit phlebotomy requests at the start/end of each day (find out what time the phlebotomists come); if a patient will need bloods for the next 3 days then fill them all out together with clear dates
• Be aware of your limitations, eg consent should only be taken by the doctor performing the procedure or one trained in taking consent for that particular procedure
• Bookmark online or get a copy of your hospital guidelines/protocols, eg pre-op investigations, anticoagulation, DKA, pneumonia etc.
• Get a map of the hospital if you haven’t got your bearings
• Remember the names and faces of your colleagues and patients
• Talk to your predecessors to get hints and tips specific to your ward.
The traditional medical model made the patient a passive recipient of care. Healthcare was done to people rather than with them. Many patients were happy with this.
Our task as clinicians is to find out our patients’ expectations of their relationship with their doctors and then try to fulfil these. From ‘whatever you feel is best doc’ to reams of printouts and self-diagnoses from the Internet, neither extreme is wrong and our task is to help.
Find out whether your patient wants guidance regarding what treatment may be best.
Respect their right to make a decision you believe may be wrong. If you feel that they are doing so because they do not fully understand the situation or because of flawed logic, then alert your team to this so that things can be explained again.
Find out their other influences, these can be very powerful. Examples include: religious beliefs, friends, the Internet, and death/illness of relatives with similar conditions.
Patients may have clear expectations of their treatment (eg an operation or being given a prescription). These expectations are important sources of discontentment when not fulfilled. Find out what their expectations are and why. Useful questions may include: ‘What do you think is wrong with you?’ ‘What are you worried about?’ ‘What were you expecting we’d do about this?’
Make time to imagine yourself in your patient’s shoes. Isolation or communication difficulties will heighten fear at an already frightening time. Long waits without explanation are sadly common. Aggression from friends or relatives is often simply a manifestation of anxiety that not enough is being done. Ask yourself ‘How would I want my family treated under these circumstances?’ then do this for every patient.
Hospitals can rob people of their dignity. Wherever and whenever possible help restore this:
• Keep your patients covered (including during resuscitation)
• Ensure the curtains are around the bed on the ward round
• Make sure they have their false teeth in to talk and glasses/wigs on whenever possible
Patients are often clerked over four times for a single admission. This is frustrating for them and often seen as indicative of a lack of coordination within the hospital. Patients may need to be clerked and examined more than once, but the context of this should be explained carefully—is this to gain more insight about their condition or to allow a training doctor to learn? People rarely mind when they understand the reasons. Keep examinations which are invasive or cause discomfort to an absolute minimum.
Good communication with patients and colleagues is a vital part of the job.
Whenever you are communicating with another health professional (see Box 1.9), include your name and role, the patient’s name, location, and primary problem, what you would like them to do and how urgently, and how they can contact you if there are any problems
 Box 1.9 Handover
Box 1.9 Handover
Reductions in working hours, a move towards shift-based rotas, and the increased cross-cover between specialties mean the number of doctors caring for a patient during their stay has increased, making the effective transfer of information more important. Handover occurs at the start and end of every shift, and it is vital that it is given enough time and thought. Some are formal handover meetings chaired by a senior while others are more informal. Either way, the incoming doctor must get a clear idea of the situation including the names, locations, and clinical details for unwell patients and those needing review, as well other outstanding tasks that need going. Giving and receiving a good handover is a key skill and one you should pride yourself on perfecting.
 Clinical notes p. 76.
Clinical notes p. 76.
 Referral letters p. 84.
Referral letters p. 84.
 Sick notes p. 82.
Sick notes p. 82.
Self-discharge If your patient wants to discharge themselves, speak to them, ask why, manage their concerns, and explain why they need hospital management and what may happen if they leave. If they have capacity, then ask them to sign a ‘self-discharge form’ and do a TTO as normal.
As a doctor you are a respected member of society and a representative of the medical profession, and people will expect you to act in a certain way. While this does not mean you cannot be yourself, there is a big change from medical school and you must be aware of expectations:
• Always introduce yourself, especially over the telephone or when answering a bleep; ‘Hello’ is not enough
• Wear your ID badge at all times in hospital
• Never be rude to colleagues/ward staff; you will get a bad reputation
• Never be rude to patients, no matter how they treat you
• Never: shout, swear, scream, hit things, or wear socks with sandals
• Do not gossip about your work colleagues; address any problems you have with a colleague directly and in private
• When you do something wrong, apologize and learn from your mistake; it’s a natural part of the learning curve
• If you are going to be late, let the person know in advance especially for handover or ward rounds
• If you think it is not appropriate for you to do a job then run it by the ward staff or your seniors. Ask for help if you feel overrun with tasks.
Communication with relatives can be difficult if done badly, or rewarding if done well. They may be scared, assuming the worst and be in the frustrating position of not knowing what is going on. They could have a full-time job that prevents them coming in during the day:
• If you are on-call and do not know the patient well then be honest about this, but attempt to answer simple questions as best possible using the notes; explain what times the usual ward staff will be present
• Try to arrange a time when you can discuss the patient’s progress in a quiet room (ask a colleague to hold your bleep)
• To avoid repeating yourself, speak to the family collectively or ask them to appoint a representative
• Check the patient is happy to have their confidential medical details discussed ( p. 29) and encourage them to be present if possible
p. 29) and encourage them to be present if possible
• Address concerns and answer each question in turn
• Be honest about your limitations and involve seniors where necessary
• Document the date, time, what was discussed, and who was present.
A patient’s perception of your abilities as a doctor depends largely on your communication skills. Remember that patients are in an alien environment, often feel powerless, and are worried about their health.
Introductions Always introduce yourself to patients and clearly state your name and position. Ask your patient how they wish to be addressed (eg Denis or Mr Smith). Patients meet many staff members daily so reintroduce yourself each time you see them (see Box 1.10).
General advice Try to avoid using medical jargon. Be honest with your replies to them, and give direct answers when asked a direct question. If you do not know the answer, be honest about this too.
Results Explain why a test was done, what it shows, and what it means.
Diagnosis Try to give the everyday name rather than a medical one (heart attack instead of MI). Explain why this has happened. A patient who understands their condition is more likely to comply with treatment.
Prognosis Along with the obvious questions about life expectancy ( p. 86), patients are most interested in how their life will be affected. Pitch your explanation in terms of activities of daily living (ADLs), walking, driving (
p. 86), patients are most interested in how their life will be affected. Pitch your explanation in terms of activities of daily living (ADLs), walking, driving ( p. 619), and working. Bear in mind that patients may want to know about having sex, but are often too embarrassed to ask.
p. 619), and working. Bear in mind that patients may want to know about having sex, but are often too embarrassed to ask.
 Box 1.10 Hello my name is…
Box 1.10 Hello my name is…
Kate Granger was a geriatrician, patient, and campaigner for compassionate and personalized care who sadly died at the age of 34 in 2016. She was diagnosed with terminal cancer in 2011 and spent her subsequent years campaigning for better communication between doctors and patients. Frustrated at the lack of introductions from healthcare staff caring for her in hospital, she started the #hellomynameis campaign in 2013. Founded on the simple idea of reminding staff that a confident introduction is often all that is needed to put patients at ease, the campaign raised £250,000 for cancer charities and has received widespread public and professional support. It is a reminder to us all never to forget something as simple as introducing ourselves properly.
Ideally, breaking bad news should always be done by a senior at a predetermined time when relatives and friends ± specialist nurses can be present. In reality, you are likely to be involved in breaking bad news, often while on-call. It can be a positive experience if done well.
Preparation Read the patient’s notes carefully and ensure that all results are up to date and for the right patient. Be clear in your mind about the sequence of events and the meaning of the results. Consider the further management and likely prognosis—discuss with a senior.
Consent and confidentiality ( p. 31, p. 29) A patient has a right to know what is going on or to choose not to know. Ask before the investigations are done and document their response. If a patient does not want their relatives to know about their diagnosis you must respect this. Always ask, do not assume—many families have complex dynamics.
p. 31, p. 29) A patient has a right to know what is going on or to choose not to know. Ask before the investigations are done and document their response. If a patient does not want their relatives to know about their diagnosis you must respect this. Always ask, do not assume—many families have complex dynamics.
Warning shot Give a suggestion that bad news is imminent so it is not completely out of the blue, eg ‘I have the results from … would you like anyone else here when I tell you them/shall we go to a quiet room?’.
How to do it The SPIKES model is often used:
Setting Ask a colleague to hold your bleep, set aside suitable time (at least 30min), silence your mobile phone, use a quiet room, and invite a nurse who has been involved in the patient’s care. Arrange the seats so you can make eye contact and remove distractions. Introduce yourself and find out who everyone is.
Perception Find out what the patient already knows by asking them directly; this will give you an idea of how much of a shock this will be and their level of understanding to help you give appropriate information.
Invitation Explain that you have results to give them and ask if they are ready to hear them. It helps to give a very brief summary of events so they understand what results you are talking about.
Knowledge Break the bad news, eg ‘A doctor has looked at the sample and I’m sorry to say it shows a cancer’. Give the information time to sink in and all present to react (shock, anger, tears, denial). Once the patient is ready, give further information about what this means and the expected management. Give the information in small segments and check understanding repeatedly. Prognosis can be difficult; never give an exact time (‘months’ rather than ‘4 months’). Be honest and realistic. Try to offer hope even if it is just symptom improvement or leaving hospital.
Empathy Acknowledge the feelings caused by the news; offer sympathy. This will take place alongside the ‘Knowledge’ step. Listen to their concerns, fears, and worries. This will guide what further information you give and help you to understand their reactions.
Summary Repeat the main points of the discussion and arrange a time for further questions, ideally with a senior and yourself present. Give a clear plan of what will happen over the next 48h. Document the discussion in the patient’s notes (diagnosis, prognosis, expectations) with your name and contact details.
For patients who can’t understand or speak the same language as you, the consultation can leave them feeling isolated, frustrated, and anxious. You may have to rely on a third party to translate for you (see Box 1.11).
Professional interpreters can be arranged before the appointment—ask ward staff or phone switchboard.
• Allow extra time for the consultation and check the interpreter is acceptable to the patient
• Address both the patient and the interpreter and look at the patient’s non-verbal response to gauge their level of understanding
• Ask simple, direct questions in short sentences to avoid overloading or confusing the interpreter; avoid jargon
• Use pictures or diagrams to explain things wherever possible; provide written/audiovisual material in the patient’s own language to take away
• If you cannot organize an interpreter, you may be able to contact a telephone interpreting service who can translate for you and the patient directly over the phone (ask nurses or switchboard)
• Document that a trained interpreter has been used with their name and contact details so that the same interpreter can accompany the patient for future appointments.
Never assume you know what the patient wants without asking them.
There are many reasons why family members and friends should not be used as interpreters. Nevertheless, in emergency situations, this may prove necessary. Address the patient directly and look carefully at the patient’s response to gauge their understanding. Record the fact that a family member was used for interpretation in the notes.
Friends and relatives They are commonly used as informal interpreters. The main drawbacks are the lack of confidentiality and the bias the relative may have on the patient’s decision-making—particularly when underlying family issues are present (you may be unaware of these).
Children They can interpret for their parents from an early age, but again their views can bias the consultation and its outcome (eg sexual health and vulnerable adults) and even routine clinical questions can be very frightening or inappropriate for children. Use only as a point of last resort.
Conflict of interests If you think the relative is biasing the conversation or it is an important issue, then explain that you are professionally obliged to request a trained interpreter.
Consent Relatives cannot consent on behalf of adults ( p. 31).
p. 31).
Box 1.11 Who can interpret?
Outside agencies who could enquire about your patients include: police, media, solicitors, fire brigade, paramedics, GP, researchers, and the patient’s employer. Patient confidentiality must be respected.
• Do you really know who you are talking to?
• Check and arrange to call them back unless certain
• Do they have any right to the information they are seeking?
•GPs, healthcare professionals, and ambulance staff may well do, police have limited rights (see later in this topic), many others do not
• Should you be the one discussing this or should it be a more senior member of the team?
• Do not talk to the media about a patient/your hospital unless:
• You have the patient’s permission, and
• You have permission from your consultant/management (for trust issues), and
• Do not ‘chat’ to a police/prison officer about a patient, no matter what the alleged circumstances; all patients have an equal right to privacy
• Breaching a patient’s confidentiality without good cause is treated as misconduct by the GMC.
Immediate investigation of assaults The police may well ask the clinical condition of an assault victim. ‘Is it life-threatening, doctor?’ The purpose of this question is to know how thoroughly to investigate the crime scene. It is reasonable to give them an assessment of severity.
In the public interest In situations where someone may be at risk of serious injury, disclosure is permitted by the GMC. This should be a consultant-level decision.
The Road Traffic Act Everyone has a duty to provide the police with information which may lead to the identification of a driver who is alleged to have committed a driving offence. You are obliged to supply the name and address, not clinical details. Discuss with your seniors first.
Inform your clinical supervisor; they should accompany you to court. Remember you are a professional witness to the court so your evidence should be an impartial statement of the facts. Do not get rattled by the barristers—stick to the facts, do not give opinions, explain the limits of your knowledge/experience. Address your remarks to the judge. Dress smartly. Get an expenses form from the witness unit to claim your costs back.
You may be asked to provide patient details for research. Ask the researcher to provide you with ID and if they have consent from the patient. Unless the researcher has specific permission to screen medical notes, they may ask you to seek initial permission from any potential participant before passing on the patient’s details to the researcher.
DH definition: ‘Clinical governance is the system through which NHS are accountable for continuously improving the quality of their services and safeguarding high standards of care, by creating an environment in which clinical excellence will flourish.’
• You are responsible for your clinical practice which you should be aiming to continuously improve
• You need a mechanism for assessing the standard of your practice
• While in training, this is done for you by your consultant/trainer as part of your regular appraisal process. Additionally, you may have audits and regular departmental meetings
• You should be aiming to continuously learn and improve your care for patients. Again, while still in training, this almost goes without saying; revising for endless examinations and diplomas helps too.
• You should ensure you stick to departmental or hospital protocols and don’t undertake procedures for which you have not been trained
• You will be asked to participate in regular departmental audits, usually of morbidity and mortality. These are used to ensure consistency of practice and to pick up problems early
• You should attend departmental and hospital-wide audit meetings and grand rounds to keep up to date with changes
The clinical governance structure in every hospital includes:
• Audit of practice (eg reattendances within 1wk or wound infections)
• Appraisal and revalidation structures
• Regular departmental meetings (eg morbidity and mortality) to allow clinicians to compare their care and highlight common concerns
• Clear routes of accountability for all staff. It can be obvious when these have broken down, leading to problems which everyone can identify but seemingly no one is responsible for fixing
• A risk management structure to identify practices which jeopardize high-quality patient care (critical incident reporting,  p. 34)
p. 34)
• A complaints department to respond to complaints and ensure lessons are learned from them; may be part of the risk management department
• A clinical governance/quality committee structure which oversees and ensures compliance with all of the above.
Compliance with clinical governance/quality mechanisms are measured both regionally and nationally through quality boards.
Ethics are moral values, and in the context of medicine are supported by four main underlying principles:
Autonomy This is the right for the individual to make decisions for themselves, and not be overtly pressurized or swayed by others (namely doctors, nurses, relatives, etc). Patients should be allowed to contribute when decisions are made about their care. If an individual lacks capacity ( p. 30) then it might not be appropriate to let them make important autonomous decisions.
p. 30) then it might not be appropriate to let them make important autonomous decisions.
Beneficence This is concerned with doing what is right for the patient and what is in their best interests. This does not necessarily mean we should do everything to keep a 90-year-old patient alive who has widespread metastatic disease. There will be times when it is beneficent to keep a patient comfortable, and allow them to die naturally.
Non-maleficence This ensures care-givers refrain from doing harm to the patient, whether physical or psychological. An example of a breach in nonmaleficence would be if a patient came to harm as a result of a doctor performing a procedure in which they had inadequate training or supervision.
Justice This requires that all individuals are treated equally and that both the benefits and burdens of care are distributed without bias. Justice also covers openness within medical practice and the acknowledgement that some activities may have certain consequences—specifically legal action.
Two further principles are important to consider:
Dignity This should be retained for both the patient and the people delivering their healthcare.
Honesty This is a fundamental quality which doctors (as well as other care-givers) and patients should be expected to exhibit in order to strengthen the doctor–patient relationship.
Ethical dilemmas frequently arise in clinical practice and are probably not discussed enough. While the principles listed do not necessarily provide an immediate answer, they do create a framework on which the various components of the conflict can be teased out and addressed individually. All doctors should be able to discuss common ethical dilemmas by analysing how each principle is relevant and weighing them up against one another. In ethics there are no right answers, but careful thought and discussion of situations can allow a harmonious solution to be found.
It is quite common that apparently complex ethical issues arise because of a failure in communication between the patient or their loved ones and healthcare professionals. The solution to most of these conflicts is the establishment of effective and transparent lines of communication.
To breach patient confidentiality is unlawful and unprofessional; several doctors are disciplined and even struck off the medical register each year for this. You should be careful when talking about patients in public places, including within the hospital environment, and only disclose patient information to recognized healthcare staff as appropriate. Pieces of paper with patient information on must never leave the hospital and should be shredded if they are no longer required. Do not leave patient lists lying around. Personal electronic databases of patients should be disguised so individual patients cannot be identified. Electronic devices on which patient information is stored outside of the hospital should be encrypted and registered under the Data Protection Act. You avoid giving any information (names or nature of injuries) to the police, press, or other enquirers; ask your seniors for advice when dealing with these ( p. 26).
p. 26).
Publications Medical journals will often insist that any article which involves a patient must be accompanied by written consent from the patient for the publication of the material, irrespective of how difficult it would be to track down and identify that patient.
Presentations and images If you are talking about a patient to a group of healthcare workers in your own hospital you do not need to obtain consent, but doing so is courteous. If you are talking to an audience from outside your hospital it is advisable you seek the patient’s consent unless the patient is fully anonymized. Equally, if you want to keep copies of radiographs or digital images, ensure these are made anonymous and if this isn’t possible obtain the patient’s written consent. Bear in mind that presentations can easily end up online and be accessed by those other than your original audience.11
Relatives Your duty lies with your patient and if a relative asks you a question about the patient, it is essential you obtain verbal consent from the patient to talk to the relative; alternatively offer to talk to the relative in the presence of the patient. Relatives do not have any rights to know medical information. If the patient lacks capacity then seek senior advice before talking to the relatives. Document all conversations in the notes.
Children As described for adults, if the child has capacity to give consent (see ‘Gillick competence’/Fraser guidelines  p. 30), you must seek verbal consent from the patient to tell the relatives (parents) about their health. If the patient refuses, then offer to talk to the patient about their condition in the presence of their relatives. If you sense the situation will be difficult, seek senior advice/support.
p. 30), you must seek verbal consent from the patient to tell the relatives (parents) about their health. If the patient refuses, then offer to talk to the patient about their condition in the presence of their relatives. If you sense the situation will be difficult, seek senior advice/support.
Telephone calls Wards receive many telephone calls asking how patients are and if they have had tests or operations yet. The potential to break patient confidentiality here is great. Often there is a telephone by each bed, so encourage callers to speak to the patient directly. Otherwise, inform the patient who the caller is and relay a message from the patient to the caller. Apologize to the caller for not being able to offer any further information and suggest that you could talk things over with both themselves and the patient when they visit. See ‘Outside agencies’  p. 26.
p. 26.
Someone who has capacity can comprehend and retain information material relevant to the decision, especially as to the consequences of not having the intervention in question, and must be able to use and weigh this information in the decision-making process.
For a patient to have capacity they must:
• Be able to understand the information relevant to making the decision and consequences of refusal
• Retain the information long enough to allow for decision-making
Remember that:
Capacity is most often impaired by chronic neurological pathology such as dementia, learning difficulties, and psychiatric illness, but is also impaired by acute states such as delirium, acute severe pain, alcohol and drug intoxication (both recreational and iatrogenic—eg morphine).
Children and capacity Children under 16yr of age were once regarded as lacking capacity to give consent, but now if the child meets the criteria then they are regarded as having ‘Gillick’ competence (Fraser guidelines12), and may give consent (Box 1.12). It is always advisable, however, to involve the parent or guardian in discussions about the patient’s care if the patient allows (see also  p. 417).
p. 417).
No capacity When the patient does not have capacity and is over 18, family and friends are not able to make a decision on the patient’s behalf; their views should, however, be listened to. Where the patient lacks capacity and there is no next of kin to consult, an Independent Mental Capacity Advocate (IMCA)13 may need to be appointed who advises clinicians in making decisions on behalf of the patient in their best interests. In an emergency situation, the patient is treated under the ‘doctrine of necessity’, that is, doing what is in the patient’s best interests until they attain capacity to make the decisions themselves.
 Box 1.12 Gillick competence/Fraser guidelines
Box 1.12 Gillick competence/Fraser guidelines
Although 16 years is the usual age at which people are automatically allowed to give their own consent, younger people can consent to most treatments or operations if they are capable. This follows a famous case in 1986 when Victoria Gillick went to the courts to get authority to be informed if her daughters sought contraceptive treatments. The law disagreed and decided that if a child was competent, he/she could consent to treatment without parental knowledge—this is often referred to as being ‘Gillick’ competent when a child meets the criteria in that case.
Understanding consent and obtaining it satisfactorily can be difficult. If you are ever unsure, seek senior help.
Obtaining consent The individual who obtains consent from the patient should be aware of the risks and benefits and be able to communicate the procedure in a language that the patient will understand. If you do not regularly perform the procedure yourself or are not trained to take consent for the procedure then you must not obtain consent for it. Obtaining consent satisfactorily is a skill that can be learned from senior colleagues, so initially shadow your seniors when they are taking consent from a patient to learn how to do it properly, then have a senior colleague supervise you the first few times to ensure you include all the relevant information.
Informed consent In order to give informed consent, patients must first be deemed to have capacity to consent under the specific circumstances ( p. 30). Consent should reflect the fact that the patient is aware of what is going to happen and why. They should be aware of the consequences of not undergoing the procedure, the potential benefits, and any alternatives, and be free from any coercion. The common risks and side effects should be discussed, as should the potentially rare but serious consequences of the procedure. As a rule, any risks which might affect the decision of a normal person should be discussed—plus any risks that might be of specific importance for the individual patient, such as where the profession of the patient makes a normal trivial risk of special importance (eg a tiny risk of postoperative vertigo might be of particular importance for a window cleaner). The patient should be provided with information well in advance of the procedure to allow them to think it over and prepare any questions they may wish to ask.
p. 30). Consent should reflect the fact that the patient is aware of what is going to happen and why. They should be aware of the consequences of not undergoing the procedure, the potential benefits, and any alternatives, and be free from any coercion. The common risks and side effects should be discussed, as should the potentially rare but serious consequences of the procedure. As a rule, any risks which might affect the decision of a normal person should be discussed—plus any risks that might be of specific importance for the individual patient, such as where the profession of the patient makes a normal trivial risk of special importance (eg a tiny risk of postoperative vertigo might be of particular importance for a window cleaner). The patient should be provided with information well in advance of the procedure to allow them to think it over and prepare any questions they may wish to ask.
Types of consent There are three main types of consent:
Implied The patient offers you their arm as you approach them with a needle and syringe to take blood.
Expressed—verbal You explain that you are going to perform a lumbar puncture, by describing the procedure and potential complications, and the patient agrees to have it done.
Expressed—written The patient is given an extensive explanation of the procedure and complications and informed of the alternatives. A record of the consultation is made which both patient and doctor sign. This document should be completed prior to the planned treatment or procedure, and consent verified at the time of the procedure.
Difficult situations There are many situations where problems arise with consent issues. If in doubt, seek senior advice or consult one of the medical defence unions ( p. 2) which have 24h telephone support.
p. 2) which have 24h telephone support.
If a patient has capacity to give or withhold consent, and chooses not to receive treatment even in the face of death, then treating that patient against their will is potentially a criminal offence. This includes patients with psychiatric illness. Note that this situation is distinct from that of a patient with a psychiatric illness who may lack capacity to make decisions regarding psychiatric treatment, and may be detained and given psychiatric (but not medical treatment) under the Mental Health Act ( p. 371).
p. 371).
Every doctor makes mistakes, from the trivial and correctable to the severe and avoidable.
• Stabilize the patient, call for senior help early
• Do not compound the error by trying to cover it up or ignoring it
• Correct where possible, apologizing to the patient as appropriate
• Don’t underestimate the seriousness of the situation
• If serious and you have time, start documenting events, including times
• If after the error you wish to add more details, then do so but make it clear when they were added. This is perfectly acceptable
• Amending notes, without making it clear that your entry was made retrospectively and with a clear date and time, is serious misconduct.
• An apology is not an admission of guilt, so apologize and explain to the patient early. Apologize that the event has taken place (Box 1.13), it is not necessary to ‘give confession’ at this stage
• Inform your senior/consultant immediately. If you believe your error has caused the patient significant harm then you should speak to your defence organization ( p. 614) as soon as practical.
p. 614) as soon as practical.
Disciplinary procedures If you have made a serious error the hospital may exclude you from working temporarily pending preliminary enquiries. This is not a judgemental act but allows a quick and calm investigation, but you must be informed why you have been excluded. You may be asked not to talk to others involved. If this happens, speak with your defence organization at once. You should be given a named person to contact within the hospital and cannot be excluded for more than 2wk without review. Let the hospital and others know how to get hold of you. Less serious errors should be treated as training issues and dealt with by your consultant or tutor. A period of close supervision or retraining may be appropriate.
Clinical events Consultant, supervisors and defence organizations.
Non-clinical events Your consultant, the postgraduate dean, the BMA.
Don’t forget friends and family, and remember these events resolve very slowly, sometimes years in big cases, so don’t expect answers quickly.
 Box 1.13 Duty of candour
Box 1.13 Duty of candour
Candour is being open and honest. While our ethical and professional duties of candour are well established, since 2015 trusts and their employees have a legal duty of candour towards their patients. If an unexpected/unintended incident occurs that could/did result in death, psychological harm for >28d, permanent reduction in function or non-permanent but significant physical harm needing an increase in treatment (e.g. longer admission, another procedure, treatment cancellation, transfer to higher-level care), then trusts are legally obliged to apologize and explain to the patient, and notify them as investigations evolve. Failure to do so may result in prosecution by the CQC.
Every doctor has complaints made about them. These can be about your clinical ability, conduct, or communication skills. They may be justified or spurious but they are inevitable, therefore do not feel your world has fallen apart when you are told a complaint has been made about you.
How the system handles complaints There are two types of complaints—formal and informal. If a patient complains to you informally it is in everyone’s best interest, and will save many hours of clinical time, if you are able to resolve the situation to the patient’s satisfaction there and then. If you are unable to do so, but feel the problem may be solvable by more senior input, then call for help. Don’t agree to do something which you are unable to carry out.
• All formal complaints are collated centrally in the hospital. In the rare event you are sent a complaint personally, do not respond but pass it to the complaints department. In most trusts, the department that handles complaints is known as PALS (Patient Advice and Liaison Service). They also provide more general advice and support for patients
• If a patient makes a complaint to you about care they have received from a colleague (doctor, nurse, or other) then listen to them but try to avoid appearing to agree or support their position, no matter how much you may share their opinions. Depending on the seriousness of their allegations (Box 1.14), either offer to feedback the comments or advise them to discuss matters further with PALS
• If a complaint has been made about the care of a patient you saw, you may be asked for a statement. This is an internal document and should be written as a letter, but bear in mind that if the case goes to court, this document could be requested by the patient’s lawyers
• Simply state the facts as you see them, do not try to apportion blame. You may be able to expand on your notes, particularly the details of conversations which may not have been documented
• If you feel it is clear how any error could be avoided in future then state this as well. Patients are often satisfied by knowing that any mistake they suffered will not be repeated for others
• All the statements made by the staff involved are then collated and a letter is written on behalf of the chief executive (and usually signed by them) to the patient. This usually ends the matter
• There are further steps, both with the trust and then regionally, if this is not enough.
Box 1.14 Serious errors
These are defined as:
• Anything which harms patients’ care or disrupts critical treatment
• An event which could potentially lead to harm if allowed to progress (‘near misses’). They range from minor incidents, eg incorrect results, to life-threatening, eg wrong blood group in a blood transfusion.
Non-clinical incidents These include:
• Incidents which involve staff, relatives, or visitors
• Incidents which involve non-clinical equipment or property.
The aim of incident reporting is to highlight adverse incidents or ‘near misses’, assess them, and review clinical practice as a result. Ultimately it is designed to reduce clinical risks and improve overall quality of patient care.
• Make sure the patient is safe
• Complete a trust critical incident reporting form (usually online)
• Forward the form to the clinical risk coordinator (usually automatic if form is electronic)
• Ensure your seniors are aware of what has happened
• Consider completing some formal reflective practice in your ePortfolio.
• Blood samples from two different patients being confused
• Failure to report or follow-up abnormal results
• Drugs prescribed to patients who have a documented allergy
• Delay in treatment/management.14
• Fill in an incident form as soon as you can after the event so that you don’t forget any relevant information
• Check you are filling in the correct form. All NHS trusts now use online incident reporting systems though there may be paper backups
• Include the time, date, staff involved, as well as the issues being reported
• Check if the named consultant needs to fill in/sign the form
• If you are reporting an incident involving your colleagues, inform them and explain the situation. Learn from their mistakes without judging them.
The critical incident form is copied to clinical risk directors for evaluation at panel meetings, where changes to clinical practice are discussed.
• If a critical incident form is filed involving yourself, don’t assume you’re a bad doctor; use it as a learning experience
• Find out the reason and circumstances and clarify the situation with the person filing the report
• Go over the incident and review your actions, asking if there is anything you would change; if it helps, discuss it with a colleague.
Many of us may have worked with a colleague who worried us professionally—‘I wouldn’t want to be treated by Dr X’. When does this become enough to do something? And what do you do?
• The GMC is quite clear that we all have a clinical duty to report colleagues who we believe to be incompetent. This does not equate to pointing out every fault of every other doctor but it does mean that you cannot ignore serious concerns if you believe patients are at risk of harm
• Serious concerns about a trainee should be passed to the relevant consultant. Ask to see them in private. It may be easiest to open the conversation with a question, to ask them to put your mind at rest: ‘I don’t know if you are aware that Dr X does not use chaperones? I’ve always been told we should use them for intimate examinations. I’m here because two women told me that they had felt uncomfortable with Dr X.’
• If the problem is with a consultant then you should either talk to another consultant or, if it is very serious, the medical director
• If you are unsure whether a problem exists, or how serious it is, then talk to a friendly consultant informally (eg your supervisor or a clinical lecturer you got on with at medical school).
• There is a clear difference between a doctor occasionally drinking too much while off-duty and one who helps themselves to controlled drugs or who has developed an alcohol problem
• Likewise, regardless of substance, there is a difference between what someone does that only affects themselves and actions which affect quality of patient care. Any colleague who appears on duty while badly hungover is a potential risk to patient care and should be removed from clinical duties (and should be encouraged to recover in the mess or go home). Repetitive behaviour of this kind should be discussed with the colleague, and/or their educational supervisor
• Drinking during working hours, arriving drunk, or use of controlled drugs are totally unacceptable and you have a duty to alert your consultants to any such problem. They will consider the GMC guidance and following a meeting with the individual involved will decide if GMC referral is appropriate or if a local warning and period of ‘probation’ is needed These problems are better tackled early while solvable than left until they cause patient harm and ruin a career.
• Every year, doctors develop serious psychological illnesses just like the rest of the population and doctors are just as bad at self-diagnosis
• The more common problems include frank depression and hypomania, the rare include psychosis and schizophrenia ( p. 14); the symptoms often come on gradually such that even close colleagues may not notice the transition from mildly eccentric to frankly pathological
p. 14); the symptoms often come on gradually such that even close colleagues may not notice the transition from mildly eccentric to frankly pathological
• Depression is commonly masked well while at work
• Talk to an individual directly, or their consultant, if you are concerned about their health.
Experiencing problems at work is common and usually transient. If you find things do not improve, try to identify the problem. However difficult things are at work, you should always remain polite, punctual, and helpful. If you don’t, you may be the one perceived to be the problem.
The responsibility that comes with being a doctor, the demands of your job, fear of litigation, and high expectations from peers and patients can leave you physically and mentally exhausted. If you feel things are getting on top of you, reassess your workload. Speak to colleagues to find out if there are easier ways of doing things. Take annual leave and upon your return approach your work schedule differently to help regain control of things. Ensure you have time to relax away from work and keep up your outside interests. If things don’t improve, talk to a friend, contact the BMA ( p. 614) for advice, or discuss the situation with a trusted senior or mentor.
p. 614) for advice, or discuss the situation with a trusted senior or mentor.
If you can find no other option and you are clear medicine isn’t for you, you can always leave your job. Find out how much notice you are required to give and who to direct your letter of resignation to. During your last weeks, stay an active member of the team rather than taking a short-timer’s attitude. Complete any outstanding work and tidy up loose ends before leaving.
Bullying can be from your seniors, peers, other healthcare professionals, patients, or their relatives. If you feel you are being bullied, discuss it with someone, either at work or independently (eg the BMA). Speak to your predecessors to find out if they had similar difficulties and how they handled the problem. Keep a diary of relevant events, together with witnesses, and approach your consultant. If it is your consultant who is the problem, approach another consultant you trust or contact BMA counselling ( p. 614).
p. 614).
This may start very innocently and gradually escalate into intimidating behaviour which may affect your work, social life, and confidence. In the first instance, make it clear that their advances are not welcome and confide in someone you trust. Find out if other colleagues are also being harassed and report the harassment to your educational supervisor. Again, the BMA can be a useful source of advice.
All employers must abide by an equal opportunities policy that includes standards on treating all employees. Before deciding to take things further, confide in a trusted senior colleague. Keep a record of any events that stand out as being discriminatory, documenting dates, times, and witnesses. Contact the BMA for advice. You may have to submit a formal letter outlining your concerns, so make sure you are prepared to pursue a formal complaint before committing yourself on paper.
Have a break There are few problems that must be solved immediately. Leave the ward, ask someone to hold your bleep, and take 5min to unwind. Take deep breaths and concentrate on the feeling of the air rushing in and out of your lungs. Count the breaths and try to clear your mind. Try squeezing the muscles in your feet then feeling them relax; do this with all the muscle groups from your legs to your neck. Think about something you are looking forward to.
Do not let medicine take over your life. In particular, value and cultivate your non-medical friendships—these can be hard to sustain under the strains of shiftwork but you will value an external perspective on life beyond the NHS. It may not take much to make life seem better; try to:
There is no point worrying about things you have no control over; it is natural to feel concerned about future events but almost everything will turn out well in the end, even if it is not as you have planned it.
See  p. 19 on being efficient. The job gets much easier with time; these skills become second nature and you perform individual tasks quicker.
p. 19 on being efficient. The job gets much easier with time; these skills become second nature and you perform individual tasks quicker.
Be honest with yourself: are you tired? Everything is harder, slower, and more stressful when you have not had enough sleep.
Think about what makes you stressed and whether this is a problem with your attitude, the way you do the job, other people, or the nature of the job. Try to accept, change, or avoid these stressors.
If someone is annoying you then consider telling them so. Plan how you will tell them, do it in private, and do not blame them; just explain how it makes you feel. Most people will be apologetic and try to change.
| ► If you feel it is all getting too much and/or nobody cares, try speaking to: | |
| BMA counselling (you don’t need to be a member) | 08459 200 169 |
| Samaritans | 08457 90 90 90 |
In August 2017, the new junior doctors’ terms and conditions of service replaced the previous 2002 contract (updated in 2008). The most significant changes were pay increments rewarding responsibility rather than time served, new safeguards against poor training and overwork (Box 1.15), and an extension of normal working hours until 9pm on weekdays. However, many details were contentious and despite concessions on both sides, sticking points remained. As a result, the country bore witness to an unprecedented and lengthy dispute between the BMA and NHS Employers over the precise terms of the contract (see Box 1.16). Even now, employers, trainers, and trainees are getting to grips with the details, with national reviews planned for 2018 and transitional arrangements until 2022. You should read your contract carefully as we provide only a summary, the details are important, and your seniors may be quite unfamiliar with its intricacies.
Box 1.15 Limits on working hours
• Employees and doctors are responsible for doctors’ safe working
• Limits on hours include no more than 48h work during the average working week (56h if opted out of the European Working Time directive), or 72h in any 7d stretch. The average working week is defined as starting at midnight between Sunday and Monday, is averaged over 26wk, and includes locums ( p. 40)
p. 40)
• Mandatory 11h rest between shifts, with time off within 24h if less
• No shift (except non-resident ‘availability’ shifts) should exceed 13h
• Consecutively no more than 8d of work, 5 long shifts (10h+), 4 long shifts that finish after 11pm, or any 4 shifts that include 3 of the hours between 11pm–6am (with 2d mandatory break after each)
• 30m break during a 5h shift or 2 during a 9h shift; not within an hour of starting/finishing, ideally in the middle, and can be merged into 1h
• Safeguards are there for breaches or inadequate training ( p. 39).
p. 39).
The following elements vary depending on your rota but are added up to generate your salary (payslip  p. 41):
p. 41):
Basic salary Depends on grade and responsibility, based on 40h/week.
Additional hours An allowance for up to 8h extra per week.
Weekend allowance A % added to the basic salary depending on the frequency of weekends you work (3% for 1 in 7, 10% for 1 in 2).
Night duty 37% on top of the basic salary for hours worked 9pm–7am.
Availability allowance 8% on top of the basic salary for when you can be at home but may be telephoned for advice or called in to work.
Flexible pay premia Supplements for those in GP, academic, oral and maxillo-facial, and hard-to-fill programmes to support workforce development, time out of training, and/or the extra degrees required.
Exceptional pay premia Supplements for activities of broader interest to the NHS (e.g. time out of training to assist in public health crises).
Pay in exception circumstances Money received from fines ( p. 39).
p. 39).
Pay protection A cash floor to protect the wages of doctors already in training programmes when the new contract started in 2016/2017.
These protect against poor training and excessive service provision:
Work schedule Contractual plan for your service provision and training provided by trusts and agreed in advance with your supervisors.
Fines Departments are fined at 4× the hourly rate if doctors are worked >48h during the average working week (Box 1.15), >72h in any consecutive 7d, or have <8h rest between consecutive shifts. Contractual breaches not meeting these criteria are reciprocated with time off or pay for all work done. Complete an ‘exception report’ as soon as possible.
Exception reporting The way of informing trusts when work varies from the agreed schedule (e.g. differences in hours, breaks, patterns, training, or support). If patient safety is at risk, it must be raised orally at the time to the responsible senior clinician, otherwise electronic forms distribute the details and should be submitted within 14d (7d if claiming pay, 24h if patient safety breach). Outcomes may be fines, extra income, time off, a work schedule review, or system change.
Work schedule review To ensure that schedules remains fit for purpose. Triggered in writing by doctors, supervisors, employers, exception reports, or the guardian of safe working hours. If dissatisfied, escalate to a level 2 work schedule review and then a ‘formal grievance procedure’.
Guardian of safe working hours (GOSWH) ‘Independent’ champion of safe working hours (but employed by the trust and approved by junior doctors). Responsible for escalating working hours problems to senior management, distributing money from fines, and reviewing exception reports. Accountable to junior doctors and the executive board.
Junior doctors’ forum A forum for junior doctors to raise concerns and decide on the allocation of fines (from fines, 1.5× basic pay goes to the individual and 2.5× to training/trainees). Made up of elected junior doctor representatives, the GOSWH, the chair of the local negotiating committee, and the director of postgraduate education.
Director of postgraduate education Responsible for training in the trust.
 Box 1.16 The junior doctors’ contract dispute
Box 1.16 The junior doctors’ contract dispute
Employers and employees both want improved patient care and keeping contracts up to date with the demands of current healthcare is part of this. Negotiations between the BMA and employers began in 2012, continuing on and off for 3 years. By 2015, the Secretary of State for Health Jeremy Hunt threatened to ‘impose’ a new contract as the debate became increasingly political and emotional. One sticking point was Hunt’s insistence on extending core working hours without increasing the total ‘pay envelope’, citing concerns regarding higher mortality at weekends while overlooking a weight of statistical evidence suggesting that this was unrelated to junior doctor staffing levels. Hunt’s continued use of misleading figures, combined with the accumulated perception of a political rather than clinical agenda, all set against a backdrop of understaffing, rota gaps, and low morale, contributed to a backlash from junior doctors that culminated in an overwhelming vote for strike action. In total there were 8 days of industrial action and the first withdrawal of emergency care ever in the UK. Some employer concessions were made, which along with a damaging series of mistakes by the BMA leadership contributed to a decrease in effective opposition. By late 2016, the dispute drew to a close, with lasting damage perhaps done to morale and reputations on both sides.
There are several ways to make money in addition to your basic income (Fig. 1.1). You must keep records of all additional income and declare these in your self-assessment to the Inland Revenue at the end of each tax year.15
Research There are usually several research projects being undertaken in most hospitals which require volunteers. These range from a 5min interview to a week-long study and in most circumstances the volunteers are rewarded financially (eg £5 to >£1000). These may carry a risk of harm.
Locums Most hospitals employ locum doctors to cover staff sickness or busy periods. They can be internal or external. Internal locums have their substantive post at the hospital and are working additional hours from the NHS staff bank. External locums are working away from their base hospital (or do not have one), often on behalf of private locum agencies. There are many locum agencies that you can register with; they are often advertised in BMJ Careers. To reduce spending on locums, two key measures have been introduced. The first of these, caps on total hourly rates, seems to have had little success. The capped rates are much lower than those previously offered such that trusts that enforce them have a much harder time filling rota gaps, resulting in unfilled slots and increased strain on other doctors. An ‘exceptional circumstances’ clause allowing the cap to be broken has been widely used by many trusts, with several continuing to pay rates similar to or above those offered before the introduction of the cap. Rates of pay will vary and can still be negotiated, but an F1 can expect pre-tax rates of £20–30/h, and F2s £25–35/h. The second new measure is a clause in the 2016 junior doctors’ contract specifying that those doctors planning to take locum work must initially offer their services for the proposed shift time to their employing trust staff bank. The trust must respond in a timely manner indicating if they require the doctor’s services. The doctor is under no obligation to take any extra shifts on, but would not be able to take an agency locum if the trust had offered staff bank work at an appropriate level (not a lower grade). Importantly, you should discuss locum shifts with your supervisor and include them in your work schedule to ensure contractual limits on individual and average weekly working hours (48h or 56h depending on if you’ve opted out of the EWTD) are not exceeded.
Cremation certificates The cremation form has two parts ( pp. 100–101). The first is completed by a ward doctor (usually the F1) and the second by a senior doctor, often from another department. Under arrangements prior to 2017, junior doctors were paid around £70 for completing the form; this fee is under review as part of ongoing reforms (
pp. 100–101). The first is completed by a ward doctor (usually the F1) and the second by a senior doctor, often from another department. Under arrangements prior to 2017, junior doctors were paid around £70 for completing the form; this fee is under review as part of ongoing reforms ( pp. 100–101). The bereavement office handles the forms and issues any cheques. Make sure you see the body, checking identity and that there is no implantable device that needs removing (
pp. 100–101). The bereavement office handles the forms and issues any cheques. Make sure you see the body, checking identity and that there is no implantable device that needs removing ( p. 100); they really do explode if incinerated.
p. 100); they really do explode if incinerated.
Gifts The GMC is clear in its message that you should not encourage patients or their families to give, lend, or bequeath gifts to yourself, others, or to organizations.16 If you are given a gift, then it is acceptable to take it as long as it has negligible financial value. If you are given money, then pass this to the ward sister to put into ward funds.
Always check your payslips carefully, before storing them safely: make backups of electronic payslips and never throw paper copies away. They can be a useful record of tax, pension, and loan payments long after you have enjoyed spending the money. If you think a mistake has been made, contact the salaries and wages division of the HR office for your trust, quoting your assignment number (employee number). In the event of significant underpayment, you can request an interim payment be made pending the resolution.
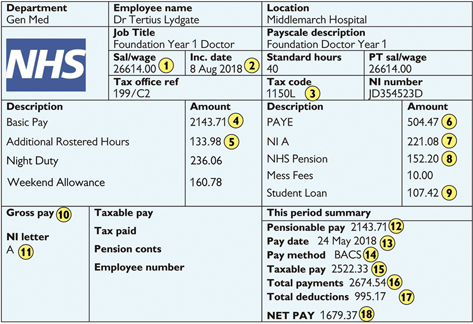
1 This is the total annual basic salary for your nodal pay point (‘1’ for FY1s, ‘2’ for FY2s). Latest updates are released as ‘Pay Circulars’ on the NHS Employers website  www.nhsemployers.org
www.nhsemployers.org
2 This is the date when you are next due to go a point up the pay scale, usually 12 months of full time employment after your previous date (or date of first starting working as a doctor). When changing trusts mistakes can be made so always check this date is correct.
3 Your tax code shows the amount of income you are entitled to earn in the current tax year that you do not pay any tax on. This figure should be multiplied by 10 to give your total allowance. This will be the basic personal allowance for the tax year, as set by the government, adjusted to take account of any under- or over-payments you may have made in previous years. Each tax year runs from April to April. After your first tax year in paid employment, you will receive a P60 summarising your tax paid during that year with the code that should apply to you in the next tax year. A copy should also be sent to your trust, but if you move trusts around this time, the new trust may not receive the correct information unless you show them your copy of the P60. If your new trust does not know the correct code for you, they will use an ‘emergency’ code, set as the basic personal allowance, which may or may not be correct. The letter after the code should be an ‘L’ unless very specific circumstances apply to you. See also  www.hmrc.gov.uk
www.hmrc.gov.uk
4 This will be approximately 1/12 of your basic annual salary.
5 This lists the pay you receive on top of your basic pay for additional hours over 40h, nights, and weekends. Details of how these are calculated are provided in the pay circulars and related junior doctor contract information available from the NHS employers website. Do check that the medical staffing department have provided correct details of your rota to the payroll team since early evidence from the introduction of the new contract would suggest a number of instances of errors in this regard.
6 Under the ‘Pay as you earn’ scheme (PAYE), your trust will automatically deduct your tax from your income each month. Both your basic pay and your pay for additional hours, nights, and weekends are taxable. In your first few months of employment, you may not pay any tax until your income has risen above the personal allowance for that year. Enjoy this while it lasts!
7 National Insurance contributions pay for certain state benefits, including your state pension. These are not optional, and will be deducted automatically, according to thresholds. The current rate is 12% of income over £157/week, though this is subject to annual review.
8 The NHS pension scheme remains a very good deal, although terms and conditions have been changed significantly in recent years and are subject to further negotiations. Your pension contributions are not taxed and will also be deducted automatically according to various earnings thresholds, unless you opt out of the scheme. Pension contributions are calculated from your basic pay (including any London weighting) - pay for additional hours, nights, and weekends is not subject to any deductions. See also  www.nhsbsa.nhs.uk/nhs-pensions
www.nhsbsa.nhs.uk/nhs-pensions
9 Repayment for any student loan is taken automatically from your pre-tax earnings when your income reaches a certain threshold. Although the landscape around tuition fees, repayment thresholds and interest rates is constantly changing, in 2017/2018 the minimum contribution is 9% of earnings above the threshold. Specific thresholds and repayment timings then depend on when and where you trained. If you trained in Scotland or Northern Ireland, or in England or Wales and started before 1st September 2012, repayments start in the April of the first year after you graduate (the start of the financial year) and are taken from any pre-tax earnings above an annual threshold of £17,775. In this case pay slips before April in the first year after you graduate may not contain loan deductions. If your course was in England or Wales but started on or after 1st September 2012, student loan contributions are taken as soon as you graduate on any monthly pre-tax earnings over £1,750 (equivalent threshold of £21,000 per year). You can repay faster if you wish. Keep a record of all payments you make and check them against annual statements. Errors are common when changing trusts. Payments that appear to have gone missing can be credited to your account easily if you can provide a copy of your payslips. See  www.studentloanrepayment.co.uk.
www.studentloanrepayment.co.uk.
10 The numbers in this section will keep a tally of your total payments from that employer during the current tax year. If you change trusts, the numbers will be reset, but your tax thresholds should not be.
11 Your NI letter reflects the contribution group you fall into. For almost all of those in the NHS pension scheme, this will be ‘A’.
12 Pensionable pay does not include any pay for additional hours, nights, and weekends.
13 Pay dates will vary between trusts but are generally around the last Thursday in the month. It can be difficult to get paid on time at the start of employment with a new trust.
14 Trusts will transfer the money into your bank account by BACS transfer. These can take up to 3 working days.
15 Your taxable pay includes your basic pay (including London weighting) and pay for additional hours, nights, and weekends, less any pension contributions.
16 Don’t get too excited by this number…
17 …and try not to get too sad about this one…
18 … because this is what you’re going to have to spend until next month comes around.
Fig. 1.1 A sample pay slip.
The level of medical graduate debt has increased markedly in recent years. On average, new FP trainees from England owe £40,000 in tuition fee loans, sometimes up to £80,000 if you include maintenance loans.17 Financial management priorities have therefore changed drastically. This section is not comprehensive but aims to give some important pointers and warnings.
Most graduates have three different types of debt:
(1) Short-term High-interest debts (eg credit cards ± overdraft, if at full charge). Pay these back first and as fast as possible. Try not to extend them just because you have an income
(2) Medium-term Commercial loans (eg a high street bank graduate studies loan). These should be paid back next, as spare funds allow
(3) Student-loans At very low rates of interest—pay these back last.
Pay close attention to the annual percentage rate (APR) and charges attached to any loan arrangement. Interest-free loans or credit cards can help in the short term but ensure you don’t get saddled with a high APR later. Loans are a competitive market so shop around—especially for something like a car loan where the car dealer rarely offers the best rate. Think ‘total cost’ not just ‘monthly repayments’.
Short term Clear debts with the highest interest as soon as possible.
Medium term Try to accumulate about 1 month’s net salary as ‘emergency’ savings.
Long term The NHS Pension Scheme remains the best available at present and you will be automatically enrolled in it unless you opt out. With this taken care of, you could think about trying to save for the deposit on a property (even if just £100/mth). With interest rates currently low, home ownership is an attractive option if you can raise a deposit. Bear in mind that there are large up-front costs to house buying (eg legal fees), you will be responsible for all maintenance and will not be able to take the property with you when you move to another part of the country.
Since you now have a salary that increases incrementally and is virtually guaranteed for life, finance companies will swarm round you like wasps round jam. Beware of some very slick sharks—their aim is only to get you to buy their products. There is no altruism here:
• Truly independent financial advice is hard to obtain—ask how independent they really are
• Firms must now show what commission will be received for any product you choose, both to the individual who sold it to you as well as to their company
• Do not buy from the first or most persuasive salesperson, but take your time to consider what you really want and need.
Critical illness cover and income protection  p. 12. Check if it still pays if you are capable of doing a less demanding job. Check if it pays for all conditions you may get at work.
p. 12. Check if it still pays if you are capable of doing a less demanding job. Check if it pays for all conditions you may get at work.
Life insurance This pays out a lump sum if you die; only really makes sense if you have dependants.
Pension The NHS scheme is still better than commercial alternatives. You should revisit your retirement planning at regular intervals through your career. You will also receive a state pension through your national insurance (NI) payments.
BMA and HCSA Protection for non-clinical matters, eg wrong salary or poor accommodation; the trade unions for doctors ( p. 12).
p. 12).
Now that you are earning a salary you will be paying tax. Most will be collected by PAYE (Pay As You Earn). If you have no other sources of income then you can leave it at that (Box 1.17). If you have any other income then you should ask for a tax return and complete it.
Tax codes  p. 41.
p. 41.
Tax deductible It is possible to claim back the income tax you paid on:
• Job-related expenses (eg stethoscope); make sure you keep receipts
• Professional subscriptions, eg GMC, BMA, MDU/MPS, Royal College
• Examination fees and course fees (previously not deductible, but HMRC has relented on this since 2012).
Tax reclaims may be made through full self-assessment, but this is not essential. If you pay tax through PAYE, simply send a letter to HM Revenue and Customs, Pay As You Earn, PO Box 1970, Liverpool. L75 1WX, stating your name, NI number, and detailing your professional expenses as listed above. You must also include details of any additional, undeclared income, including cremation forms. Your tax code for subsequent years will be adjusted accordingly.
Tax returns A tax return is an online form asking for details of all the money you have received which may have tax owing on it. This includes your salary and other income whether earned (eg locum shifts or cremation fees) or unearned (eg lodger/flatmate, bank interest, and dividend yields).
• If you are asked to complete one then obtain a Government Gateway ID ( www.gov.uk) and password. This takes time, don’t leave it until January
www.gov.uk) and password. This takes time, don’t leave it until January
• Fill it in online and the maths is done automatically
• Return it before 31 January otherwise you will be fined £100 (if <3mth late), or more if >3mth late (depends on how late, and how much is due)
• Claim your deductible allowances but also list your additional income.
The Inland Revenue has been known to ask an undertaker to list all payments to doctors and then cross-check. If your tax is simple then tax returns are not hard to do, otherwise pay a company/accountant to do it for you.
Box 1.17 Documents to keep safe for at least 7 years
As a doctor working in the NHS you have certain entitlements, defined under your ‘Terms and Conditions of Service’. Those relating to salary are discussed in ‘Pay and contracts’ ( pp. 38–39). Some others are listed here. Your first point of contact for any questions is your medical staffing department and the Foundation school. Always ask for copies of their written policies.
pp. 38–39). Some others are listed here. Your first point of contact for any questions is your medical staffing department and the Foundation school. Always ask for copies of their written policies.
• Doctors in their first year after graduation are no longer entitled to free accommodation at their employing trust, except in Wales where, for the time being at least, funding for accommodation is still available
• Rooms may well be available on site at a market rate and can be useful when attached to a trust for a short period that would otherwise make finding local accommodation difficult.
• You are entitled to a total of 27d/yr of paid leave or 9d/4mth. You are also entitled to all bank holidays in addition—or compensatory days off if you are scheduled to work on any part of a bank holiday
• If a compensatory day off, eg after working nights, or pre-allocated annual leave falls on a bank holiday, you are entitled to an extra day off
• You are rarely allowed to carry leave over between jobs/years
• You need to give 6wk notice for leave; arrange this in good time and have your form signed by your consultant. There may be local allowances if rotas are received late or you are changing trust
• If you need leave in a forthcoming post (eg getting married), write to let them know. Ask for the rota position which is off for those dates
• Study leave is available for F1s but only for regular scheduled teaching. F2s have 30d per year that includes scheduled teaching but spare days can be used for courses/exams. Discuss leave with your supervisor.
• All women are entitled to up to 52wk of maternity leave and must be allowed to return to work after this. Those who have worked for the NHS for 12mth by the 11th wk of pregnancy are then entitled to full pay for 8wk, half pay for 18wk, and any remaining Statutory Maternity Pay for the remaining 13wk (pay calculators available online18). Those who have worked for <12m by the 11th week of pregnancy are entitled to Statutory Maternity Pay only
• Fathers are entitled to up to 2wk paid paternity leave if they have worked for over 6mth. You may also qualify for shared parental leave where existing maternity leave can be transferred to paternity leave14
• If you are absent from your F1 or F2 post for any reason for >4wk, you are unlikely to be signed off and will need to arrange to complete your training on your return. For practical reasons, your foundation school may ask you to repeat the whole year—ask your educational supervisor.
• FP doctors are entitled to train less than full-time if they have a valid reason
• A comprehensive list of valid reasons (eg having a baby or ill health) and advice on how to apply is available from your Foundation school.
After the FP you need to apply for specialty training. Although changes are on the horizon (see Box 1.18), at present there are 2 main options:
• Specialty training (ST) or core training (CT)—most junior doctors
• Academic clinical fellowship (ACF)—for those interested in research, recruitment occurs earlier to allow unsuccessful applicants to apply for regular ST/CT posts ( p. 66 and
p. 66 and  www.nihr.ac.uk).
www.nihr.ac.uk).
The goal of specialty training is to award a Certificate of Completion of Training (CCT). This allows you onto the GMC’s specialist/GP register and to become a consultant/GP. After the FP there are 2 routes to CCT:
Run-through training In some specialties (paediatrics, GP, neurosurgery) competitive entry at ST1 leads to a 4–8yr ‘run-through’ programme within a single region, with no further competitive entry points.
Core training In other ‘uncoupled’ specialties, competitive entry at CT1 leads to a ‘core training’ programme followed by another application to ‘higher specialty training’ (cardiology, colorectal) on completion. Core training programmes can be 2 years (Medicine, Anaesthetics, Surgery) or 3 years (Psychiatry, Acute Care Common Stem  pp. 48–49).
pp. 48–49).
CESR For those who do not follow a straightforward career path through to CCT, periods of time spent in training posts and experience gained may all be taken into consideration as part of an application to the GMC for a ‘certificate of eligibility for specialist registration’ (CESR). This route is especially useful for those who have spent considerable time overseas.
 Box 1.18 The ‘Shape of Training’ report (SOT)
Box 1.18 The ‘Shape of Training’ report (SOT)
The ‘Shape of Training’ report marks the evolution of a number of previous reports (‘Modernising Medical Careers’, ‘Time for Training’, ‘Foundation for Excellence’) examining how we can best adapt training programmes to the changing needs of society. Published in 2013 by Professor David Greenaway, it sets out a structure by which changes in patients (e.g. multiple comorbidities, complex conditions, ageing populations) and healthcare (rapidly shifting technologies and NHS restructuring) might be matched by medical training, without destabilizing current training and service delivery. In brief, the report advocates training clinicians who are more generalist, engaged, and adaptable to change. The 19 wide-ranging recommendations include full GMC registration after medical school, broader and longer training programmes after the FP (e.g. women’s health, child health, mental health), transferrable competencies allowing easier transition between programmes, postgraduate opportunities to work in recognized related fields (similar specialties, management, education), and subspecialty ‘credentialing’ (subspecialization only after ‘Completion of Specialty Training’ as driven by patient and work-force needs). Although officially independent, questions of political interference were raised after a Freedom of Information request uncovered minutes from a series of previously undisclosed meetings between representatives from the Department of Health, the GMC, and Professor Greenaway. The recommendations were accepted by the government. Organizations including the AoMRC and GMC have ongoing workstreams mapping out the practical implications of the report. Early changes are expected in the next few years, with longer-term changes likely to take between 10 and 15 years.
The application process varies between specialties and is rapidly evolving. Most recruitment is organized nationally by the appropriate Royal College or a ‘lead’ LETB using a web-based application system. A small number of specialties still recruit through local applications. There is no limit to the number of specialties you can apply to, providing you fulfil the eligibility criteria set out in the ‘person specification’. Begin preparing well in advance.
Choose a specialty/specialties ( p. 53) Considering person specifications and competition rates available at
p. 53) Considering person specifications and competition rates available at  specialtytraining.hee.nhs.uk.
specialtytraining.hee.nhs.uk.
Check your eligibility For applying to a training programme, eg GMC registration, right to work in the UK, language skills, prior experience.
Find suitable jobs ( p. 52) These will be advertised by recruitment offices according to a nationally agreed timetable.
p. 52) These will be advertised by recruitment offices according to a nationally agreed timetable.
Complete the application form Paying close attention to deadlines. For several specialties a single application portal called Oriel is used.
Wait As applications are reviewed applicants are shortlisted for interview; in certain specialties (eg GP) a further assessment is used in shortlisting.
Interview/selection centre ( p. 58) You should receive at least 5d notice, but this is not always adhered to; you need to bring a long list of supporting documentation, including your portfolio (
p. 58) You should receive at least 5d notice, but this is not always adhered to; you need to bring a long list of supporting documentation, including your portfolio ( p. 8). Formats will vary between a traditional panel-based interview (eg core training programmes) or performing a number of exercises in front of assessors (eg GP).
p. 8). Formats will vary between a traditional panel-based interview (eg core training programmes) or performing a number of exercises in front of assessors (eg GP).
Offers Are made electronically through the UK offers system according to a coordinated timetable. You will be asked to rank all LETBs where you would accept a job; successful applicants are then allocated to LETBs in score order (you will be allocated to your highest preference that still has places when your turn comes). You then have 48h to review offers and decide whether to accept, hold, or reject. You may also elect to receive automatic ‘upgrades’ if a higher ranking choice becomes available.
Re-advertisement To unfilled posts will take place in a 2nd application round. If you accept a job in round 1, you may still apply for a different post in round 2, but you need to inform all those concerned.
Employment checks And contract signing—remarkably NHS employers claim to need up to 2 months after you start work to get around to issuing a contract and some manage to miss even this. Speak to your BMA representative in the event of contract problems.
 ‘If you can trust yourself when all men doubt you, But make allowance for their doubting too … If you can dream—and not make dreams your master … If you can meet with Triumph and Disaster And treat those two impostors just the same … Yours is the Earth and everything that’s in it, And—which is more—you’ll be a Man, my son!’19
‘If you can trust yourself when all men doubt you, But make allowance for their doubting too … If you can dream—and not make dreams your master … If you can meet with Triumph and Disaster And treat those two impostors just the same … Yours is the Earth and everything that’s in it, And—which is more—you’ll be a Man, my son!’19
The nature of a competitive jobs field is that not everyone will get their first choice post on first application. In this instance, a miss and a mile are very different entities and it is important to ask for feedback to establish how far wide of the mark you were and whether you need to consider applying to a less competitive specialty. Discuss your options with your clinical and educational supervisors and consider how else you may enhance your CV.
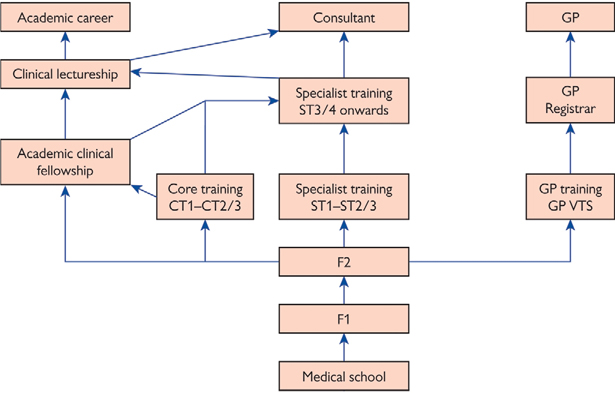
Fig. 1.2 Career structure for NHS doctors. VTS, Vocational Training Scheme.
There are 21 different training schemes that an F2 can apply for (see Table 1.3). In most specialties there are also academic clinical fellowships (ACFs). Applications for ACFs occur before the main recruitment process so that unsuccessful applicants can still apply for a regular training post. Most ACFs allow for run-through training, even in specialties that would normally have separate core and higher specialty applications.
For trainees with an interest in acute specialties, ACCS provides a core 2yr experience in acute medicine, anaesthetics, emergency medicine, and critical care, with a further training year spent in one of three streams (acute medicine, anaesthetics, emergency medicine). Choice of stream is determined at the point of application to ACCS. Although the curricula and competences gained are transferable between ACCS streams, it is not possible to move between career paths without further competitive selection.
Acute medicine CT1 and CT2 in ACCS specialties then a CT3 year spent in acute medicine. At the end of CT3 it is theoretically possible to switch specialties from acute medicine to a general internal medicine specialty.
Anaesthetics CT1 and CT2 in ACCS specialties then an extra CT2 year of anaesthetics; competitive entry to ST3 anaesthetics requires having passed the Primary FRCA ( p. 59). Anaesthetics can also be applied for directly as a 2yr core anaesthetics training programme.
p. 59). Anaesthetics can also be applied for directly as a 2yr core anaesthetics training programme.
Emergency medicine CT1 and CT2 in ACCS specialties then a CT3 year of emergency medicine; competitive entry to ST4 emergency medicine requires having passed the MCEM ( p. 59).
p. 59).
General practice has run-through training coordinated through a nationwide application. The application consists of four stages:
• Application form (establish eligibility)
• Computer-based testing (clinical problems and professional dilemmas)
• Assessment centre selection (communication and written exercises)
Successful applicants undertake 18mth spent in hospital specialties, followed by 18mth as a GP registrar during which the MRCGP must be completed to join the GP register and get a job.
These are popular uncoupled training schemes. You apply for core training, with most deaneries allowing a choice of specific rotations only after successful appointment into post. After 2yr of core training (CT1–CT2) there is a competitive application for ST3 in a specific surgical or medical specialty. To apply for ST3 in surgery you need full MRCS membership before your interview; for medical ST3 posts you need Part 1 of MRCP to apply, but need full MRCP by the date of starting your ST3 post. It should be possible to apply for specialties other than those in which you did your core training if you can demonstrate appropriate competences; it helps if you can arrange taster weeks, audit or research in the subspecialty you are applying for.
Table 1.3 Specialty training programmes at CT1/ST1 (2018)*
| Specialty | Recruitment contact details |
| Run-through specialties | |
| ACFs | NIHR Trainees Coordinating Centre  nihr.ac.uk nihr.ac.uk |
| Cardiothoracic surgery | Health Education Wessex  wessexdeanery.nhs.uk wessexdeanery.nhs.uk |
| Chemical pathology | Health Education East Midlands Meastmidlandsdeanery.nhs.uk |
| Clinical radiology | London recruitment  http://www.lpmde.ac.uk/ http://www.lpmde.ac.uk/ |
| Community sexual and reproductive health | Health Education East of England  heeoe.hee.nhs.uk/ heeoe.hee.nhs.uk/ |
| General practice | National GP recruitment  gprecruitment.hee.nhs.uk gprecruitment.hee.nhs.uk |
| Histopathology | London recruitment  http://www.lpmde.ac.uk/ http://www.lpmde.ac.uk/ |
| Neurosurgery | Health Education Yorkshire and the Humber  http://www.yorksandhumberdeanery.nhs.uk/ http://www.yorksandhumberdeanery.nhs.uk/ |
| Obs and gynae | Health Education North West  nwpgmd.nhs.uk nwpgmd.nhs.uk |
| Ophthalmology | Health Education South West  severndeanery.nhs.uk severndeanery.nhs.uk |
| MaxFax surgery | Health Education South West  severndeanery.nhs.uk severndeanery.nhs.uk |
| Paediatrics | Royal College of Paediatrics and Child Health  www.rcpch.ac.uk www.rcpch.ac.uk |
| Public health | Health Education East Midlands  eastmidlandsdeanery.nhs.uk eastmidlandsdeanery.nhs.uk |
| Uncoupled specialties | |
| ACCS—acute medicine | Royal College of Physicians  www.ct1recruitment.org.uk www.ct1recruitment.org.uk |
| ACCS—anaesthetics | Health Education West Mids  anro.wm.hee.nhs.uk anro.wm.hee.nhs.uk |
| ACCS—emergency medicine | London recruitment  http://www.lpmde.ac.uk/ http://www.lpmde.ac.uk/ |
| Anaesthetics | Health Education West Mids  anro.wm.hee.nhs.uk anro.wm.hee.nhs.uk |
| Core medical training | Royal College of Physicians  www.ct1recruitment.org.uk www.ct1recruitment.org.uk |
| Core surgical training | London recruitment  http://www.lpmde.ac.uk/ http://www.lpmde.ac.uk/ |
| Core psychiatry training | Health Education North West  nwpgmd.nhs.uk/ nwpgmd.nhs.uk/ |
*Source: data from  specialtytraining.hee.nhs.uk—this website is the best starting point.
specialtytraining.hee.nhs.uk—this website is the best starting point.
These list the required competences for that specialty. In making an application, you will need to provide evidence to prove that you have achieved the specified competences. Consult these as soon as you anticipate an application to a scheme so that you can see what you need to do. Full details are available at  specialtytraining.hee.nhs.uk
specialtytraining.hee.nhs.uk
If you are applying for an Academic Clinical Fellowship (ACF), you will need to meet the criteria in both the clinical person specification for your chosen specialty and level and the ACF person specification.
Competition for different specialties varies, as does competition for the same specialty in different parts of the country.
Competition ratios are published annually to allow applicants to view the previous year’s ratios. These typically show the number of applications received for each specialty and the number of posts available; a competition ratio is derived by dividing the former (number of applications) by the latter (number of posts). This ratio roughly represents the number of people applying for each available post (see Table 1.4).
Only the highest scoring candidates will stand a chance at getting a job in specialties with a high competition ratio; for specialties with a lower competition ratio the applicant must still meet the minimum requirements for the job to be offered it. Remember that applicants can apply for multiple posts so the actual chances of getting a job are higher than the ratio shown.
In previous years, applicants have had to factor in not only competition ratios by specialty, but also by deanery. The move to national recruitment has removed this element—you can rank all deaneries/LETBs where you would be prepared to accept a job without disadvantaging your chances in any one region. After completion of the assessment process you will be ranked nationally, and assigned to your highest choice deanery that still has a vacancy when your turn in the queue comes.
That said, it is important to consider what your own priorities are. If you are adamant that you want to stay in one particular area of the country, you may need to recognize that the area may be very popular (eg London). Are you happy to pick a less popular specialty to increase your chances? Equally, if you are determined that you want to enter a highly competitive specialty, are you willing to pick a region potentially miles away from your current home as the competition there is much less? These are decisions which should be talked through with friends, family, mentors, and your educational supervisor.
Although applications to specialty training are coordinated throughout the UK, within each of the four countries a degree of local structure remains.
England  specialtytraining.hee.nhs.uk
specialtytraining.hee.nhs.uk
Northern Ireland  www.nimdta.gov.uk
www.nimdta.gov.uk
Scotland  www.scotmt.scot.nhs.uk
www.scotmt.scot.nhs.uk
Wales  www.walesdeanery.org
www.walesdeanery.org
Table 1.4 Competition ratios for CT1/ST1 applications (2018)*
| Specialty | Applications | Posts | Competition ratio | Fill rate |
| ACCS emergency medicine | 675 | 340 | 1.9 | 91% |
| Anaesthetics inc ACCS | 1296 | 601 | 2.2 | 97% |
| Cardiothoracic surgery | 64 | 10 | 6.4 | 88% |
| Clinical radiology | 1021 | 267 | 3.8 | 100% |
| Community sexual and reproductive health | 99 | 4 | 24.8 | 100% |
| Core medical training | 2343 | 1657 | 1.4 | 91% |
| Core psychiatric training | 623 | 495 | 1.3 | 65% |
| Core surgical training | 1608 | 629 | 2.6 | 100% |
| General practice | 5097 | 3857 | 1.3 | 84% |
| Histopathology | 174 | 95 | 1.8 | 72% |
| Neurosurgery | 152 | 29 | 5.2 | 100% |
| Obstetrics and gynaecology | 555 | 263 | 2.1 | 100% |
| Ophthalmology | 405 | 77 | 5.3 | 100% |
| Oral and maxillofacial | 20 | 8 | 2.5 | 100% |
| Paediatrics | 580 | 437 | 1.3 | 89% |
| Public health | 718 | 77 | 9.3 | 100% |
*Source: data from  specialtytraining.hee.nhs.uk—visit website for most recent data. Data is not available for all training programmes. Applications and posts are for Round 1 only and do not count subsequent re-advertisements. Competition ratio represents the number of applicants per post—bear in mind that candidates may apply for multiple training posts. Fill rate is the final number of posts in each specialty that were filled—including appointments made in additional rounds of re-advertisement.
specialtytraining.hee.nhs.uk—visit website for most recent data. Data is not available for all training programmes. Applications and posts are for Round 1 only and do not count subsequent re-advertisements. Competition ratio represents the number of applicants per post—bear in mind that candidates may apply for multiple training posts. Fill rate is the final number of posts in each specialty that were filled—including appointments made in additional rounds of re-advertisement.
Once you have secured a training rotation, you still need to choose which specific jobs to do. There are also jobs outside of specialty training rotations that have a local application process. This section gives ideas about how to find and choose jobs.
Priorities Before looking for a job, write a list of factors that matter to you in making this potentially life-changing decision. Important considerations include:
Partner/spouse Can they get a job nearby?
Location Could you move? How far would you commute?
Family/friends How far away are you willing to go?
Career Is the job in the right specialty/specialties?
Duration Can you commit to several years in the same area?
Rota/pay What banding and rota do you want or need?
Type of hospital Large teaching hospital vs district general.
If you have no firm career intentions then choose by location and rota since these will affect your life most over the next few months. Look for suitable jobs on  www.jobs.nhs.uk,
www.jobs.nhs.uk,  specialtytraining.hee.nhs.uk, deanery websites, or in the BMJ.
specialtytraining.hee.nhs.uk, deanery websites, or in the BMJ.
Job offers A national timescale for FP and ST/CT job applications exists whereby all job offers are made at the same time. This allows you to accept the highest ranked job that you applied for. Bear in mind that you cannot change your job rankings after submitting your application.
Competition Medical jobs are competitive; it is important to maximize your chances of getting a job. Apply for several specialties; rank as many regions as possible; check competition ratios and person specifications ( p. 51,
p. 51,  specialtytraining.hee.nhs.uk); consider a back-up choice, eg a less competitive specialty or region. A good CV also helps (
specialtytraining.hee.nhs.uk); consider a back-up choice, eg a less competitive specialty or region. A good CV also helps ( pp. 56–57).
pp. 56–57).
Researching a job Adverts rarely give a true reflection of a job. Phone up hospitals within the region and ask to speak to the person doing the job at the moment. Quiz them on the types of placements available, hours, support, teaching, conditions, and what their interview was like. Would they accept the job again?
Contacts With HR departments and structured interviews, the days of jobs being just a consultant phone call away have gone. There is no doubt that some networking still occurs, with mixed results. Senior contacts are useful for tailored career guidance, CV advice, and giving realistic views of where your CV can get you.
Accepting a job With a move towards unified, online application processes, strict and automated rules are essential to ensure a rapid and fair allocation to posts. In order to allow for choice, under certain circumstances it may be possible to accept, or hold, an offer, and later upgrade, or apply to a different post, providing you notify all those concerned. Outside of this formal process, it is unacceptable to turn down a post you have already accepted unless you have an extremely good reason. The GMC take a clear position on your obligation to protect patient care by not compromising the recruitment process in this way, though notice periods vary by seniority.
The Certificate of Completion of Training (CCT) can be awarded in numerous specialties shown as follows. A selection of subspecialties are also shown with bullet points:20
Acute internal medicine
Allergy
Anaesthesia
•Paediatric anaesthesia
•Obstetric anaesthesia
•Pain management
Audiovestibular medicine
Aviation and space medicine
Cardiology
Cardiothoracic surgery
•Congenital cardiac surgery
Chemical pathology
•Metabolic medicine
Child and adolescent psychiatry
Clinical genetics
Clinical neurophysiology
Clinical oncology
Clinical pharmacology and therapeutics
Clinical radiology
•Interventional radiology
Community sexual health and
reproductive medicine
Dermatology
Diagnostic neuropathology
emergency medicine (eM)
•Paediatric emergency medicine
•Pre-hospital emergency medicine
endocrinology and diabetes mellitus
Forensic psychiatry
Gastroenterology
•Hepatology
General internal medicine
General practice
General psychiatry
•Liaison psychiatry
•Rehabilitation psychiatry
•Substance misuse psychiatry
General surgery
•Breast surgery
•Colorectal surgery
•Upper GI surgery
•Vascular surgery
Genito-urinary medicine
Geriatric medicine
•Stroke medicine
•Orthogeriatrics
Haematology
Histopathology
•Cytopathology
•Forensic pathology
Immunology
Infectious diseases
Intensive care medicine
Medical microbiology
Medical oncology
Medical ophthalmology
Medical psychotherapy
Medical virology
Neurology
Neurosurgery
Nuclear medicine
Obstetrics and gynaecology
•Gynaecological oncology
•Materno-foetal medicine
•Reproductive medicine
•Urogynaecology
Occupational medicine
Old age psychiatry
Ophthalmology
Oral and maxillo-facial surgery
Otolaryngology (eNT surgery)
Paediatric cardiology
Paediatric surgery
Paediatrics
•Child mental health
•Community child health
•Neonatal medicine
•Paediatric oncology
Palliative medicine
Pharmaceutical medicine
Plastic surgery
Psychiatry of learning disability
Public health medicine
Rehabilitation medicine
Renal medicine
Respiratory medicine
Rheumatology
Sport and exercise medicine
Trauma and orthopaedic surgery
•Hand surgery
•Spinal surgery
Tropical medicine
Urology
Vascular surgery
This is a Latin phrase which means ‘course of life’. In modern days it means a document by which you advertise yourself to a potential employer: a summary of you.
When will I use a CV? You will need a CV for many of the jobs you will apply for after graduating. If you join a locum agency, they will use your CV when finding you work. You should also upload your current CV to your ePortfolio in advance of every annual review.
What is included in a CV? The most important information to include are your contact details, a list of your qualifications (those already acquired and those you are studying for), any outstanding achievements, a summary of your employment to date, and the details of your referees. Other information can be included, but do not overcrowd your CV.
CV philosophy Your CV should not be a static piece of work—it should evolve with you and reflect your changing skills and attitudes. It is important to keep your CV up to date, and from time to time reformat it to freshen it up. Use your CV to demonstrate how you have learnt from your experiences rather than just listing them; a potential employer will be much more impressed if you indicate you learnt about the importance of clear communication while working at a holiday resort, than by the actual job itself.
Getting help HR departments and educational supervisors can give advice on writing a CV, and often you can find people’s CVs or templates on the Internet by searching for ‘CV’. Try to keep your CV individualized, so do not simply copy someone else’s template.
Before writing your CV Ascertain what a potential employer is looking for when sending in your CV; check the essential and desirable criteria and try to echo these. You need to alter the emphasis in your CV to match the position you are applying for, eg highlighting your communication skills or leadership experience.
Layout Your CV should look impressive; for many jobs hundreds of CVs are received and yours must stand out. It needs to be clearly laid out and easy to follow. The key information and your most important attributes should stand out prominently. Think about the layout before you start writing.
Length Two sides of A4 paper are ideal for a basic CV (and an optional front page); add more as your career progresses.
Remember For most jobs, the candidates applying will have very similar qualifications and so the only way you may stand out to be short-listed for interview is via your CV. Make it as interesting as possible, without it looking ludicrous.
Personal details Name, address which you use for correspondence, contact telephone numbers (home, work, mobile), and email address are essential. You must state your type of GMC membership (full/provisional) and number. Stating gender, date of birth, marital status, nationality, and other information is optional.
Personal statement This is very much an optional section. Some feel it gives you an opportunity to outline a little about yourself and where you see yourself in 10yr; others feel it is an irritating waste of space.
Education List your qualifications in date order, starting with the most recent or current and progressing backwards in time. Indicate where each was undertaken, the dates you were there, and grade. Highlight specific courses or modules of interest. GCSE and A-level results are less important once you have graduated.
Employment and work experience List the placements you have undertaken during the F1 and F2 years starting with the most recent. Include the dates, specialty, your supervising consultant, and address of the employer; consider adding key skills that you attained.
Interests An optional section which gives you a chance to outline what you like to do outside of medicine. A well-written paragraph here can show potential employers that you are interesting as well as intelligent.
Publications If you have not yet got your name in print, try to get a letter in a medical journal ( p. 60). If you have got publications, put the most recent first; ensure they are referenced in a conventional style (see
p. 60). If you have got publications, put the most recent first; ensure they are referenced in a conventional style (see  www.pubmed.com for examples).
www.pubmed.com for examples).
Referees Your referees should know your academic record as well as your ability to interact with others. State their relationship to you (such as personal tutor) and give contact address, telephone number, and email address. Ensure they are happy to provide a reference, give them a copy of your CV, and tell them when you are applying for jobs.
Headers and footers Having the month and year in either a header or footer shows the reader you keep it up to date.
Photographs Some people include a small passport-sized photograph of themselves near the start of their CV; this is optional but not necessarily recommended. Why should your physical appearance be of relevance for selection for any job outside perhaps fashion and media?
The finished CV Use the spell-checker and get a tutor or friend to read over it to identify mistakes and make constructive criticism; be prepared to make numerous alterations to get it right.
Technical points Use just one clear font throughout. To highlight text of importance use the underline, bold, or italic features. When printing your CV use good quality white paper and a laser printer if possible.
The covering letter Whenever you apply for a job, you must send a covering letter with your CV and application form. This should be short and to the point. Indicate the position you are applying for and briefly say why the job appeals to you, and highlight why you are suitable for the job.
| Name: | Charles J Flint |
| Address: | 14 Abbeyvale Crescent McBurney’s Point McB1 7RH |
| Home: | 0111 442 985 |
| Mobile: | 0968 270 250 |
| Email: | charles.flint@mcburney.ac.uk |
| Date of birth: | 12 June 1994 |
| GMC: | 0121231 (full) |
I am an outgoing doctor with an enthusiastic yet mature outlook. I have strong communication skills and experience of working independently, both as a team member and leader. I am conscientious, trustworthy, quick to learn, and to employ new skills. My long-term aim is to practise an acute specialty within the hospital environment.
| 2010–2015 |
| University of McBurney, McBurney’s Point, McB1 8PQ |
| MBChB: 2015 |
| BMedSci (Hons): Upper Second Class, 2013 |
| 5 Dec 17–to date | |
| 31 Jul 17–4 Dec 17 | |
| 3 Apr 17–30 Jul 17 | |
| 5 Dec 16–2 Apr 17 | |
| 31 Jul 16–4 Dec 16 |
During my F1 year I developed my clinical and practical skills and became confident with the day-to-day organization of emergency and elective admissions in both medicine and surgery. Since commencing F2 I have built upon these skills and now appreciate the wider role of the doctor in the smooth running of acute admissions and liaison with the community teams prior to, and after, hospital discharge. Formal skills I have include:
• I am currently involved in a research project comparing capillary blood gas analysis with arterial blood gases in acute asthmatics
• I undertook an audit of antibiotic prescribing on surgical wards to investigate whether patients were being managed in accordance with trust guidelines. I presented the data at a departmental meeting and repeated the audit after 2 months, demonstrating increased compliance
• During my SSM I researched the role of caffeine on platelet function.
I am a keen rock and ice climber and have continued to improve my grade since leaving university. I have organized several climbing trips to Scotland and one to the Alps. I am interested in medical journalism and have spent a week in the editorial office of the International Journal of Thrombophlebitis.
• Flint CJ. Letter: Student debt. Students’ Journal 2016;35(2):101
• Flint CJ and West DJ. Multiple Sclerosis in social class three. Journal of Social Medicine 2016;12(9):118
• Lee S, Flint CJ and West DJ. Caffeine as an activator of platelet aggregation. International Journal of Thrombophlebitis 2014;54(3):99.
Dr Ian Haler, Educational Supervisor, Department of Respiratory Medicine, McBurney’s Medical Centre, McBurney’s Point, McBurney, McB1 7TS Tel 0111 924 9924 ext 2370. ian.haler@mcburney.ac.uk
Box 1.19 The paper portfolio
Most interviews require a folder containing physical evidence of your achievements. Use the following structure as a guide to gather evidence long before interviews. Sections should be subdivided for ease of navigation.
Curriculum vitae At the front or the back, print on high quality paper.
Copy of application form For interviewers to refer back to.
Degrees and qualifications Diplomas, PGCerts, BSc, MSc, MD, PhD, etc.
Prizes, awards, and grants Local/national, undergraduate/postgraduate.
Oral and poster presentations Local, regional, national, or international.
Books, abstracts, and other publications First/last author or co-author.
Teaching experience Small group, lectures, or courses (with feedback).
Clinical audit and quality improvement Results, reports, and presentations.
Commitment to specialty Skills, membership exams, experience, etc.
Courses and conferences attended Local, national, or international.
References, testimonials, and feedback Feedback/testimonials from patients and colleagues can show reflective practice and professionalism.
Research projects Give a summary, your exact role, and any reports.
Logbook of practical procedures Including supervised and unsupervised.
Work-place based assessments Notable DOPS, CBDs, and CEX forms.
Management and leadership Trainee representation, committees, etc.
Reflective practice To demonstrate that you learn through reflection.
Achievements outside medicine Shows that you are well-rounded.
Employers must allow you time off to attend the interview itself; try to give them as much notice as possible. Look at the recruitment website for information about the format, questions, and what to bring; try to talk to previous applicants and arrange mocks.
Interview day Arrive at the interview with plenty of time, allow for all sorts of delays on the roads or train, even if this means you have to read the newspaper for an hour. Relax and be yourself with the other candidates before you are called in; most of them will have similar qualifications and experience as yourself and will be just as nervous. Dress smartly in a simple suit and tie for men and suit for women (trouser or skirt). You will normally receive specific instructions as to what documentation to bring, which you should follow exactly; as a minimum, bring a copy of your CV ( pp. 54–55) and a summary printout from your ePortfolio (
pp. 54–55) and a summary printout from your ePortfolio ( p. 8).
p. 8).
The interview Relax. The worst that can happen is that you are not offered the job, which is not the end of the world. The format of interviews varies, but there are usually 2–3 interviewers; introduce yourself to each of the panel and wait to be offered a seat. For some posts there will be a series of panels, each with a different brief (eg CV verification, clinical scenarios, personal skills), and you will rotate between panels. Take a few moments to think about the questions before answering and ask for a question to be rephrased if you don’t understand it. Always make good eye contact with all members of the panel and be aware of your own body language.
Common questions It is impossible to predict the questions you will be asked, but they are likely to include questions about your portfolio, relevant clinical scenarios, and current medical news/issues. Many questions have no correct answer and will test your communication skills, common sense, and ability to think under pressure:
• Talk us through your portfolio; what are you most proud of in it?
• What is missing from your portfolio?
• What qualities can you offer our training programme?
• Why have you chosen a career in …?
• What do you understand by ‘clinical governance’?
• Tell us about your audit. Why is audit important?
• If you were the Secretary for Health, where would your priorities lie?
• How would you manage … [specific clinical scenario]?
• Where do you see yourself in 5, 10 years’ time?
• If you were the CT1 in the hospital alone at night and you were struggling with a clinical problem, what would you do?
• Tell us about your teaching experiences. What makes a good teacher?
Clinical scenarios Interviewers should not ask you specific medical questions (eg ‘What is the dose of …’); they can pose scenarios to discuss your management of a situation. These often focus on key issues such as communication, prioritization, calling for senior help when appropriate, multidisciplinary teams, and clinical safety. For some specialties, a few formal OSCE-style stations may be included—you should be told about this in advance.
Results and feedback If you are unsuccessful, try to obtain some verbal or written feedback about how you could improve your CV or your interview skills. Remember, there are always medical jobs so you will find something.
To progress beyond the ST years you will need to complete the membership exams of your chosen specialty and meet the appropriate level of competency. The exams are difficult and expensive (though often tax deductible  p. 43). Most membership exams take place 2–3 times a year. You need to apply about 2–4mth before each exam. In the past, Foundation doctors have received advice not to sit membership examinations—this may well allow focus on other areas of development but you may then miss early opportunities to start building this aspect of your CV.
p. 43). Most membership exams take place 2–3 times a year. You need to apply about 2–4mth before each exam. In the past, Foundation doctors have received advice not to sit membership examinations—this may well allow focus on other areas of development but you may then miss early opportunities to start building this aspect of your CV.
Medicine Regional examination centres throughout UK and overseas; all centres use the same exams. The MRCP has three sections:
• Part 1 Written basic science, £419, ≥12mth after graduation
You need to have already passed Part 1 to apply for a medical ST3 post, and pass all parts of MRCP in order to commence such a post.
Surgery Regional examination centres throughout UK and overseas; all centres use the same exams. The MRCS has 2 parts, you are permitted 6 attempts to pass Part A, and 4 attempts to pass part B:
To apply for an ST3 position in surgery you need to have completed the entire MRCS.
General practice You need to be a GP registrar to take the MRCGP exams. There are 3 parts and no time limits though the GP registrar post is a year long; 10% fee reductions apply to associate RCGP members:
• CSA (clinical skills) OSCE stations, £1325
• ePortfolio similar to the FP portfolio. Access costs £611, but is free among other benefits for RCGP members (£163 registration, plus £369 annual cost).
You need to complete the MRCGP to become a GP.
Emergency medicine (MRCEM) Three-part exam (two written and one clinical) required to apply for ST4. Part A may be sat as early as F1, but all parts must be passed within 7 years of passing Part A.
Anaesthetics (FRCA) Full primary (MCQ and OSCE) exam only open to anaesthetic trainees, though F1 and F2 doctors can attempt MCQ component. Applications to ST3 are only permitted when all parts of the primary FRCA are passed.
Obstetrics and Gynaecology (MRCOG) Part 1 (written) eligible after graduation; part 2 (written + OSCE) within 7 years of passing part 1.
Pathology MRCPath normally completed during ST.
Paediatrics (MRCPCH) 3 written papers (attempted in any order after graduation); clinical exam after 12mth paeds experience and passing all written.
Radiology (FRCR) Can only be attempted after gaining training post.
Psychiatry (MRCPsych) Different requirements for part A (GMC registration), part B (psychiatry training), and the practical (24mth experience).
You will be assessed throughout the FP to ensure that you are developing as a doctor and learning new skills. This will be done by Foundation assessments ( p. 8), your ePortfolio (
p. 8), your ePortfolio ( p. 8), meetings with your clinical supervisor, informal feedback from ward staff, presentations, and attendance at teaching sessions. These assessments should not be difficult but it is essential that you complete them.
p. 8), meetings with your clinical supervisor, informal feedback from ward staff, presentations, and attendance at teaching sessions. These assessments should not be difficult but it is essential that you complete them.
Study leave F1 study leave is only for mandatory teaching, however F2 study leave is more flexible, including taster weeks in specialties of your choice. You may be allowed study leave for specific courses but this will be at the discretion of your clinical supervisor and policies vary widely between Foundation schools.
Study expenses F2s may get a study leave budget of £300–400 per 12mth though again this varies by Foundation school. Check with your postgraduate centre.
Postgraduate courses There are hundreds of these and the costs range from free to >£1000 per day, most are about £100–150 per day. During the FP years, Advanced Life Support (ALS) is important and may be compulsory. Check the BMJ advert section for potential courses and try to speak to other people who have done the course.
Exam planning Once you have decided on a career plan ( p. 53), you will need to consider taking the appropriate membership examination. Membership exams are difficult and expensive but essential for career progression, so start early. See
p. 53), you will need to consider taking the appropriate membership examination. Membership exams are difficult and expensive but essential for career progression, so start early. See  p. 59 or the relevant Royal College website (
p. 59 or the relevant Royal College website ( p. 615) for more detail.
p. 615) for more detail.
Having publications on your CV will give you a huge advantage when applying for jobs. It will be far easier to understand what sort of thing journals are looking for if you read a few regularly. There are many ways to get your name in print and you don’t have to write a book (which is not great for the social life).
Book reviews Get in touch with a journal and express interest in reviewing books for them; you don’t have to be a professor to give an opinion on whether a book reads well or is useful.
Case reports If you see something interesting, rare, or just very classical then try writing it up. Include images if possible; get a senior co-author and ensure you obtain patient consent in line with the journal’s policy.
Fillers Some journals have short stories or funny/moving one-liners submitted by their readers. Write up anything you see which others might be interested in; ensure you obtain patient consent.
Letters If an article is incorrect, fails to mention a key point, or has relevance in another field then write to the journal and mention this; it might be worthwhile asking a senior colleague to co-author it with you.
Research papers If you have participated in research make sure you get your name on any resulting publications. If your audit project had particularly interesting results you may be able to publish it.
Audit is simply comparing practice in your hospital with best practice or clinical guidelines. There are six main stages to the ‘audit cycle’:
(1) Define standards (eg replace cannulas every 72h)
(2) Collect data (duration of placement for 50 consecutive cannulas)
(3) Compare data to standards (87% of cannulas replaced in 72h)
(4) Change practice (present data to colleagues and propose new approaches, eg date of placement written on cannula dressings)
(5) Review standards (replace cannulas every 72h unless final dose in 2h)
(6) Reaudit (repeat data collection after 3mth—has anything changed?).
Without reaudit, the cycle is not complete and those assessing your audit will look for evidence of this.
Why does audit matter? The aim of audit is to improve the quality of patient care; it allows a unit to applaud areas of strength and improve areas of weakness. Audits will also benefit you as a FP doctor since they are important in job applications and interviews and without at least one it will be hard to get a ST job. Try to do ≥2 during your FP.
Choosing an audit Almost any aspect of hospital/ward life can be audited. Choose something simple that interests you; alternatively look at relevant guidelines and choose one that is simple to measure.
Defining standards Try searching the National Library for Guidelines (accessible via  www.library.nhs.uk); alternatively, define best practice yourself by asking seniors and supervisors about what is expected.
www.library.nhs.uk); alternatively, define best practice yourself by asking seniors and supervisors about what is expected.
Collecting data The simpler your audit, the quicker and easier this will be. There are many ways of doing this including checking clinical notes, questionnaires, and monitoring activities yourself. Try to make your methods objective so that you do the same for every set of notes/subject.
Compare data to standards The method for doing this depends on the type of data you have collected; it is easy to do some simple statistical tests on data—seek advice from your educational supervisor or other seniors.
Change practice Try to present your audit to relevant clinicians, eg an FP teaching session or a ward meeting; use your findings to propose feasible changes to practice and discuss these with the audience.
Review standards You may feel that the original standards you defined are still suitable; alternatively, the process of auditing may have shown you that these standards need updating.
Close the loop Repeat the data collection to see if the changes to practice have made a difference; it is a good way to stay in touch with old wards and looks fantastic on a CV.
Example audits A few ideas:
• Are ECGs performed within 20min in ED patients with chest pain?
• Are drugs prescribed in accordance with local guidelines?
• Do all patients have appropriate thromboprophylaxis prescribed?
• Do patients admitted with chest pain have their cholesterol measured?
The thought of having to give an oral presentation provokes anxiety in most of us. Being able to relay information to an audience is a valuable skill and one which gets easier with time and experience, though it is helped by a logical approach.
Types of presentation There are four main types of presentation: audit/research, journal club (critical appraisal of research), case presentation, and a teaching session.
When is the presentation? If you have months to prepare then you can really go to town, while if you have only a few hours you need to concentrate on the essentials.
How long should it last? A 5min presentation will still need to be thorough, but less detailed than that lasting an hour. The length of the presentation will also aid you in choosing the topic.
What is the topic? Clarify as early as possible the topic you are to present and any specific aspect of the topic you should be discussing. If you can choose the topic, select something you either know about or are interested in researching.
Audience Are you presenting to your peers, seniors, or juniors? Are they ignorant of the topic or world experts? This information will determine the level of depth you need to go into.
Venue and means of delivery How far away is the audience, how big is the screen (so all your text and diagrams are clear)? Will you use your laptop or their computer? Back-up on memory stick in current as well as an older version of PowerPoint in case your computer isn’t up to date.
Sources of information Do you already have books on the subject? Read about the topic on the Internet by undertaking a search with a website such as  www.bmj.com. Search PubMed using keywords; recent review articles are a good place to start.
www.bmj.com. Search PubMed using keywords; recent review articles are a good place to start.
If there is no information If you cannot find enough information then it is likely you are not searching correctly; ask library staff for help. If there really is a lack of information then consider changing the topic, or choose an easier approach to it.
How many slides? This depends on how much detail is present on each slide. On average 20–25 slides will last about 30min.
Slide format Don’t get too clever. Slides should be simple; avoid borders and complex animation. PowerPoint has numerous pre-set designs, though remember it is the content of your talk the audience needs to be focused upon. Consider using a remote slide advance device (<£15).
Presentation format The presentation is in essence an essay which the speaker delivers orally. It should comprise a title page with the topic, speaker’s name, and an introduction which states the objectives. The bulk of the presentation should then follow and be closed with either a summary or conclusion. Consider ending with a slide acknowledging thanks and a final slide with simply ‘Questions?’ written on it to invite discussion.
Titles Give each slide a title to make the story easy to follow.
Font Should be at least size 24. Ensure the text colour contrasts with the background colour (eg yellow text on blue background). Avoid using lots of effects; stick to one or two colours, bold, italics, or underline features.
Graphics Use graphics to support the presentation; do not simply have graphics adorning the slide to make it look pretty.
How much information Avoid overcrowding slides; it is better to use three short slides than one hectic one. Each slide should deliver one message and this should be in six bullet points or fewer.
Bullet points Use to highlight key words, not full sentences.
PowerPoint effects Keep slides simple. Avoid text flying in from all directions and don’t use sound effects as these distract the audience.
Rehearsing Go through the presentation a few times on your own so you know the sequence and what you are going to say. Then practise it in front of a friend to check timing and flow.
Audit/research Ensure you give a good reason why the audit or research was chosen and what existing research has already been undertaken. State your objectives, your method, and its limitations. Use graphs to show numerical data and clearly summarize your findings. Discuss limitations and how your audit/research may have been improved. Draw your conclusions and indicate where further research may be directed. Thank the appropriate parties and invite questions/discussion. See audit/ research section  p. 61, p. 66.
p. 61, p. 66.
Journal club Begin with a brief explanation of why you have chosen to discuss the particular clinical topic and list the articles which you have appraised. Aim to include why the study was undertaken, the appropriateness of the study, the methods and statistics used, the validity of the study, and make comparisons between different studies. Include latest guidelines and invite discussion regarding how the research may affect current clinical practice. Finish with a summary of the studies undertaken, their results, and where they were published for future reference (see Box 1.20).
Case presentation The presentation should tell a story about a patient and let the audience try and work out the diagnosis as though they are clerking the patient for the first time. Name the talk something cryptic, eg ‘Headache in the traveller’. Refer to your patient by initials only and make sure patient details are blanked on all images and test results. Present the history and physical examination. Invite audience suggestions for the diagnosis and management. Give the results of investigations and again invite the audience to comment. Give the diagnosis and discuss subsequent management. Summarize with an outline of the topic and management; end with a question/discussion session.
Teaching session It is helpful to base a topic around a patient if this is appropriate. Keep the session interactive; have question slides where the audience can discuss answers. Summarize with learning points; it is helpful to provide a handout of your slides for people to take away ( p. 65).
p. 65).
Equipment Make sure there is a projector/computer available and that it works. Leave enough time in case you need to find new equipment.
Timing Arrive early and check your slides project correctly. Leave the title page projected so the correct audience attends.
Speaking Speak loudly so you are heard at the back. A good speech delivered inaudibly disappoints more than a bad one delivered audibly.
Body language Stand at the front and avoid obstructing the projector. Talk directly to your audience to appear more confident and see their response.
Beginning Introduce yourself and your position, outline the topic, and explain why you chose it. Ask whether everyone can hear you.
To use notes or not You shouldn’t need notes but have them available.
Style Keep it professional, but show you are human; it is acceptable to be light-hearted and make the audience laugh.
Pacing You will talk faster than you think. Take your time and use silence.
Questions Decide before if you want questions during or after. Anticipate what they might be and prepare for them. Say if you don’t know.
Whenever possible ask for feedback and learn from the comments. Consider sending a ‘Developing the clinical teacher’ assessment ( p. 9).
p. 9).
Box 1.20 Critical appraisal
Critical appraisal is the assessment of data in scientific articles. Though many evidence-based resources are available, a basic understanding of academic skills such as critical appraisal forms part of the postgraduate curriculum and is a fundamental part of being a good doctor. During the FP, your skills may be tested via a journal club, research project, or by a complex patient. Becoming proficient is a lengthy process because scientific writing can seem strange and intimidating and research is by its nature highly specialist. The following is a useful structure to focus the mind when reading, contextualizing, and critiquing scientific papers:
Introduction What question is being asked? Is it important, original, interesting, logical, and testable? What does it add to what we already know?
Methods Do the methods answer the question? ‘TROPES’ is useful:
• Type of study—interventional or observational, retrospective or prospective?
• Risk factor—if observational, is the risk factor or disease clearly defined?
• Outcomes—primary (usually clinical), secondary or tertiary/exploratory
• Population—who was included/excluded; do they represent your patients?
• Ethical issues—was there funding, a conflict of interest and/or ethical approval?
Results Was follow-up long enough? Were the statistics appropriate?
Discussion Was the study valid internally (the study itself) and externally (generalizability to clinical practice)? Were biases identified/reduced? Remember that correlation does not equal causation.
Teaching will benefit you as much as the recipient; it will challenge you to fill any gaps in your knowledge and organize your thinking on the subject. You may not feel that you know enough to teach medical students but you are probably the best teacher on the ward for them, for two reasons:
• You have recently passed the finals exam that they are trying to pass, often at the same medical school
• Finals are meant to test core medical knowledge; this is what you do every day when you clerk and manage a patient.
Keep a record of teaching sessions, ideally with feedback (consider using a simple online survey tool). At least once a year you will need to complete a ‘Developing the clinical teacher’ form assessment ( p. 9).
p. 9).
Whatever information you are trying to convey, it is important to follow a few simple guidelines:
• Be clear about your objectives
• Plan what you are going to teach to give it structure
• Be interactive; this means that the students do some of the work and also are more likely to remember it
• Try not to use too much medical jargon
• Check the students’ understanding throughout and invite questions.
One of the worst parts of being a medical student is finding suitable patients to take a history from or examine. You can use your patient lists ( p. 18) and first-hand experience of the patients to guide medical students to conscious, orientated, and friendly folk or those with clinical signs. Better still, offer to introduce the student.
p. 18) and first-hand experience of the patients to guide medical students to conscious, orientated, and friendly folk or those with clinical signs. Better still, offer to introduce the student.
Offer to watch the student examine a patient and give feedback on their technique. You are likely to examine more patients in your first month as a doctor than in all your years as a medical student so your clinical skills will have advanced very quickly.
With all the recent changes to medical training, many students feel bewildered about what lies ahead. Once again you are in the ideal position to advise since you have already successfully applied for the FP. Simple advice about which are the best jobs, how to fill in the application form, or even showing a copy of your own form can be a great help.
You can also teach ‘how to be a doctor’-type skills that are rarely passed on. The trick is to choose a simple subject you know lots about, eg:
Whatever direction you see your future career heading in, the opportunity to undertake a period of research will help you gain insight into this vital area that underpins all of medical practice as well as to develop the skills necessary to understand research output. You don’t need to cure cancer—often the most successful projects are those that set out to answer a simple, well-formulated question.
Academia This is not turning your back on clinical medicine, but rather adding a new dimension to your clinical experience: most academic doctors do research alongside clinical work. There are many advantages (interest, worldwide conferences, really understanding your subject, making a difference) but pay is not one of them. There are various training routes for academics detailed as follows—there is no one single way in; if at any stage you want to do research or a PhD there are always opportunities if you look and ask.
Foundation years There are small numbers of 2yr Academic FPs ( p. 6). These are often a normal F1 year with a 4mth academic attachment in F2 (eg academic rheumatology); a few have academic components scattered throughout F2 ± F1.
p. 6). These are often a normal F1 year with a 4mth academic attachment in F2 (eg academic rheumatology); a few have academic components scattered throughout F2 ± F1.
ST years There are also academic ST positions called Academic Clinical Fellowships. Most of these are available for entry either at ST1 or ST3 level and are 2–3yr long, including clinical rotations alongside 25% of working time set aside for academic work. The first year will be almost entirely clinical; the purpose of the second and third years is to give you the opportunity to design a PhD/MD research project, generate preliminary data, and apply for funding. Once you successfully get funding, you enter the Training Fellowship.
Training fellowship This is a 3yr research project designed by you with the aim of getting a PhD (or alternatively a 1–2yr MD) with small amounts of protected clinical time to maintain your skills.
Clinical lectureship With a PhD/MD under your belt, you can apply for a 3–4yr lectureship post. This will give you clinical experience while training to consultant level, and allow you to pursue postdoctoral research interests. You will again need to apply for funding, eg a Clinician Scientist Fellowship. Once you have completed this post you will be eligible for consultant or senior lecturer positions.
Finding a project Although some academic posts will come with funding already tied to a specific laboratory or project, the most rewarding projects are often those that you design yourself, together with a senior academic mentor. It is important to speak to a range of people and read and discuss broadly. Keep three things in mind: (1) do I get on with the supervisor and have other clinicians had good experiences in the group? (2) Does the project interest me? (3) Where will the project lead (eg will you be able to apply for the career or subspecialty that you want?)?
Funding One of the challenges of academic medicine is that you often need to raise funding to pay for yourself and your research. The process can take time (eg >6mth) and involves filling in multiple forms. Always talk to your potential supervisor for advice on the best options.
1 Professor Sir John Temple, ‘Time for Training’, 2010 Crown Copyright available free at  www.mee.nhs.uk/pdf/JCEWTD_Final%20report.pdf
www.mee.nhs.uk/pdf/JCEWTD_Final%20report.pdf
2 Professor John Collins, ‘Foundation for Excellence: An Evaluation of the Foundation Programme’ available at  www.mee.nhs.uk/pdf/401339_MEE_FoundationExcellence_acc.pdf
www.mee.nhs.uk/pdf/401339_MEE_FoundationExcellence_acc.pdf
3 Health Education England, ‘Better Training, Better Care’, available at  https://www.hee.nhs.uk/our-work/hospitals-primary-community-care/learning-be-safer/better-training-better-care-btbc
https://www.hee.nhs.uk/our-work/hospitals-primary-community-care/learning-be-safer/better-training-better-care-btbc
4 These include evidence of the right to work in the UK; of having taken medical training solely in English or having IELTS scores of ≥7.5; of complying with GMC requirements for provisional registration which may include passing Professional and Linguistic Assessment Board test; a statement of support from your medical school dean; academic transcripts; proof of medical qualifications; and a practical clinical assessment exam. You should allow sufficient time for this complex process of verification.
5 Practice paper available on UKFPO website. Mock questions available in Situational Judgement Test (Oxford Assess and Progress), third edition (Metcalfe D, et al.), 2018. Oxford University Press.
6 More information available at  https://prescribingsafetyassessment.ac.uk
https://prescribingsafetyassessment.ac.uk
7 The ‘Rough Guide to the Academic Foundation Programme’ contains more information about the Academic FP and can be found at  http://www.foundationprogramme.nhs.uk/download.asp?file=academic_rough_guide_2013_interactive_web_version_final.pdf
http://www.foundationprogramme.nhs.uk/download.asp?file=academic_rough_guide_2013_interactive_web_version_final.pdf
8 Remember that all data you upload is subject to the Data Protection Act. This means that you should avoid recording patient identifiable information within your ePortfolio, since this is not the purpose for which it was collected. Using hospital numbers rather than names, or completely obscuring personal details is considered acceptable.
9 Separate meetings: your clinical supervisor should address what is expected of you and what is available to you; your educational supervisor should take an overview of your progress and goals. In reality, for some placements they will be the same person.
10 In theory, the medical staffing department of your trust should sort a lot of this out in advance of your first day; in reality, do not underestimate their ability to mislay your paperwork and request multiple copies—keep plenty of photocopies and do not part with originals.
11 For a good discussion of the ethical issues, see Draper H, Rogers W. Re-evaluating confidentiality: using patient information in teaching and publications APT 2005;11:115, available free at  apt.rcpsych.org/content/11/2/115.full.pdf
apt.rcpsych.org/content/11/2/115.full.pdf
12 Wheeler R. Gillick or Fraser? A plea for consistency over competence in children. BMJ 2006;332:807.
13 Mental Capacity Act (2005);  www.legislation.gov.uk/ukpga/2005/9/section/35
www.legislation.gov.uk/ukpga/2005/9/section/35
14 See  https://improvement.nhs.uk/documents/2266/Never_Events_list_2018_FINAL_v5.pdf for a list of events that should never happen (but sadly, still sometimes do).
https://improvement.nhs.uk/documents/2266/Never_Events_list_2018_FINAL_v5.pdf for a list of events that should never happen (but sadly, still sometimes do).
15  www.hmrc.gov.uk/sa/index.htm.
www.hmrc.gov.uk/sa/index.htm.
16  www.gmc-uk.org/guidance/good_medical_practice.asp
www.gmc-uk.org/guidance/good_medical_practice.asp
17 Ercolani MG, et al. The lifetime cost to English students of borrowing to invest in a medical degree: a gender comparison using data from the Office for National Statistics. BMJ Open 2015;5:e007335.
18  https://www.gov.uk/pay-leave-for-parents
https://www.gov.uk/pay-leave-for-parents
19 Rudyard Kipling (1865–1936): ‘If’, first published in ‘Rewards and Fairies’ (1910).
20 For more details on the career options available to doctors, including all of the above, see So You Want To Be A Brain Surgeon? (Eccles Set al.), Oxford University Press, 2009.