Chapter 4
Getting the Skinny on Skin, Hair, and Nails
IN THIS CHAPTER
 Seeing what the integument does
Seeing what the integument does
 Explaining the integument’s structure
Explaining the integument’s structure
 Taking a closer look at hair, nails, and glands
Taking a closer look at hair, nails, and glands
 Understanding what your skin does for you
Understanding what your skin does for you
 Checking out the integument’s pathophysiology
Checking out the integument’s pathophysiology
The skin is the largest organ of the human body. In a human adult, the skin covers an area of about 20 square feet (almost 2 square meters), or about the size of a small blanket — a soft, pliable, strong, waterproof, and self-repairing blanket. It accounts for about 5 percent to 7 percent of the body’s weight.
The skin and its appendages (hair, nails, and so on) form your outer covering, or integument. Though it is one of the most beautiful parts of you, it’s also a complex organ system with numerous types of tissue and many specialized structures. The average square inch (about 6.5 square centimeters) of skin holds 650 sweat glands, 20 blood vessels, more than 1,000 hair follicles, half a million melanocytes (pigment cells), and more than 1,000 nerve endings. Refer to the “Skin (Cross Section)” color plate in the center of the book to see a detailed cross section of the skin.
Skin is made in layers, and layers within layers. New cells begin life in the lower levels and are gradually pushed to the surface to replace the old, dead ones. By the time the new cells reach the top, they’ve become hard and flat, like roof shingles. Eventually, they pop off like shingles blown from a roof in a strong wind.
Amazingly, every minute, 30,000 to 40,000 dead skin cells fall from your body. In approximately a month’s time, all the cells on the top layer have blown off and been replaced.
In this chapter, we show you what your skin is made of, and we explain how your hair and nails form. We also look at the functions of your skin and what diseases and conditions can take a toll on your integument.
Functions of the Integument
The entity known as you is bounded by your integument. The skin mediates much of the interaction between you and not-you — the environment. Your integument identifies you to other humans, a very important function for members of the hypersocial human species. Here’s a look at the integument’s other important functions:
- Protection: Skin protects the rest of the body by keeping out many threats from the environment, such as pathogens, damaging solar radiation, and nasty substances everywhere.
- Thermoregulation: The skin and its appendages in particular support thermoregulation (maintaining a consistent body temperature) in several ways. See the “Controlling your internal temperature” section later in this chapter.
- Water balance: The skin’s outer layers are more or less impermeable to water, keeping water and salts at an optimum level inside the body and preventing excess fluid loss. A small amount of excess water and some cellular waste are eliminated through the skin.
- Incoming messages: Many types of sensory organs are embedded in your skin, including receptors for heat and cold, pressure, vibration, and pain. See the “Your skin is sensational” section later in the chapter.
- Outgoing messages: The skin and hair are messengers to the outside environment, mainly to other humans. People get information about your state of health by looking at your skin and hair. Your emotional state is signaled by pallor, flushing, blushing, goose bumps, and sweating. The odors of sweat from certain sweat glands signal sexual arousal.
-
Substance production: Sebaceous glands in the skin, usually associated with a hair follicle, produce a waxy substance called sebum for waterproofing. Sweat glands in the skin make sweat. In fact, your skin has several different types of glands, and each makes a specific type of sweat. See the “Nothing’s bland about glands” section later in the chapter.
Skin cells produce keratin, a fibrous protein that’s an important structural and functional component of skin and is, essentially, the only component of hair and nails. See the “Caring about Keratins” sidebar later in the chapter.
 The root of integument is integr-, meaning “whole” as in integer (a whole number), integrate (to bring different parts together into one), integral (inseparable from the whole), and integrity (always a positive term, but more difficult to define).
The root of integument is integr-, meaning “whole” as in integer (a whole number), integrate (to bring different parts together into one), integral (inseparable from the whole), and integrity (always a positive term, but more difficult to define).
Structure of the Integument
The integument wraps around the musculoskeletal systems, taking the shape of your bones and muscles and adding its own shape-forming structures. Although your skin feels tight, it’s really loosely attached to the layer of muscles below. In spots where muscles don’t exist, such as on your knuckles, the skin is attached directly to the bone.
Without losing sight of the reality, it’s sometimes helpful to imagine that you can unzip and remove your skin, spread the living skin out on a table, and look at it. What would you see, feel, and smell?
One of the most obvious features you’d notice is that the skin, itself a thin layer, is made up of several layers. The layering is visible to the unaided eye because each layer is different from the others and the transitions between layers appear to be relatively abrupt. The superficial (or outermost) layer is the epidermis followed by the dermis and then the hypodermis. We look at each of these layers in the following sections.
 The epidermis is on top of the dermis. The prefix epi- means “on top of.” Many anatomical structures are on top of other structures, so you see this prefix in many chapters throughout this book. Other related terms you may see are endo (within), ecto (outside), and hypo (beneath or lower).
The epidermis is on top of the dermis. The prefix epi- means “on top of.” Many anatomical structures are on top of other structures, so you see this prefix in many chapters throughout this book. Other related terms you may see are endo (within), ecto (outside), and hypo (beneath or lower).
 In this discussion, up and above mean “toward the surface of the body,” and down and below mean “toward the center of the body.” These terms don’t mean “toward the head” and “toward the feet,” respectively. Anatomists use the terms superficial and deep to mean the same thing.
In this discussion, up and above mean “toward the surface of the body,” and down and below mean “toward the center of the body.” These terms don’t mean “toward the head” and “toward the feet,” respectively. Anatomists use the terms superficial and deep to mean the same thing.
Touching the epidermis
The most familiar aspect of the integument is the epidermis; it’s the part you see when you look in the mirror or at others. The epidermis feels soft, slightly oily, elastic, resilient, and strong. In some places, the surface contains dense, coarse hairs; in other spots, it has a lighter covering of finer hairs; and in a few places, it has no hairs at all. The nails cover the tips of the fingers and toes.
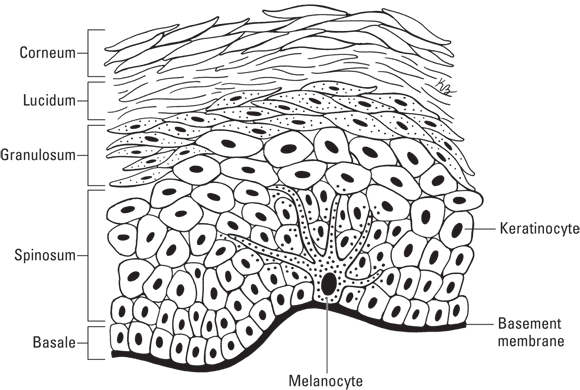
The epidermis is composed of stratified squamous tissue and has no direct blood supply. Its nourishment diffuses through the basement membrane from the dermis below. As your skin cells age and get pushed further away from the resource supply, they weaken and eventually die. This gives the epidermis its layered appearance (not visible to the naked eye though). Figure 4-1 illustrates the layers of the epidermis.
The healthiest, happiest layer of epidermal cells is along the basement membrane, called the stratum basale (or stratum germinativum). This layer is the only one that has cells that reproduce. The older cells shift upward, becoming spindle-shaped, forming the stratum spinosum, the thickest of the epidermal layers. Next is the stratum granulosum; cells in this layer are flattened and the nuclei and organelles start to shrivel. The most superficial layer is the stratum corneum; these are hardened, dead cells full of keratin. Thick skin, such as the palm of your hands, has an additional layer between the granulosum and corneum called the stratum lucidum; named because the cells appear lucid (or clear) under a microscope, this layer is built up for added protection in areas receiving a lot of wear and tear.
 Cells are shed continuously from the top of the epidermis and replaced continuously by cells that are pushed up from the deeper layers. The entire epidermis is replaced approximately every six to eight weeks throughout life.
Cells are shed continuously from the top of the epidermis and replaced continuously by cells that are pushed up from the deeper layers. The entire epidermis is replaced approximately every six to eight weeks throughout life.
The thin, impervious cover
Think of the stratum corneum as a sheet of self-repairing fiberglass over the other layers of the epidermis. It’s only 25 to 30 cells thick, dense, and relatively hard. All the cells are keratinized, as they became filled with this protein (keratin) while they are pushed toward the surface. The keratin and other proteins mechanically stabilize the cell against physical stress. Sebaceous glands in the dermis release sebum onto the surface of the stratum corneum for softening and waterproofing. The stratum corneum protects the entire body by making sure that some things stay in and everything else stays out. (See the nearby sidebar “Cosmetics and the stratum corneum.”)
One important thing that the stratum corneum doesn’t seal out, however, is ultraviolet radiation. This form of energy goes right through the skin’s surface and down to the layers below, where it stimulates the production of vitamin D. In high doses, it burns the skin and damages DNA, which can cause cells to become cancerous. Some exposure to UV radiation is necessary for our health, but too much UV radiation can clearly be problematic. Special cells in the stratum basale produce melanin, which absorbs harmful UV radiation and transforms the energy into harmless heat. More on this later in this section.
The transit zone
The stratum lucidum, found only on the palms of hands and soles of the feet (thick skin); the stratum granulosum; and the stratum spinosum lie in distinct layers below the stratum corneum. Old cells slough off above and new cells push up from below, finally getting up into the stratum corneum. The process takes about 14 to 30 days. Most of the cells that comprise the epidermis are called keratinocytes. These cells create structural proteins (like keratin), lipids, and even some antimicrobial molecules. As they are pushed away from the nutrient source (blood vessels in the dermis) they become progressively more keratinized. These layers also contain Langerhans cells, immune cells that arrest microbial invaders and transport them to the lymph nodes for destruction.
The cell farm
The stratum basale, also called the stratum germinativum or basal layer, is like a cell farm, constantly producing new cells and pushing them up into the layer above. This layer also contains melanocytes, which produce the melanin pigment that gives color to your skin, hair, and eyes and protects the skin from the damaging effects of UV radiation in sunlight. Melanin absorbs UV radiation and dissipates more than 99.9 percent of it as heat.
Everybody’s stratum basale has about the same number of melanocytes (half a million to a million or more per square inch of skin), but the amount of melanin produced varies depending mainly on genetics (heredity). The environment can also play a role in variety of skin color because exposure to UV radiation stimulates increased production of melanin. Human groups living close to the equator have evolved genes that stimulate melanocytes to produce more melanin as protection from UV radiation. Without the melanin, the radiation can burn the skin, damage DNA, and ultimately cause skin cancer.
Exploring the dermis
Below the layers of the epidermis and several times thicker is the dermis. The dermis itself is made up of two layers: the papillary region and the reticular region.
Under the basement
The papillary region is made up of the basement membrane, which sits just below the epidermis, and papillae (finger-like projections) that push into the basement membrane, increasing the area of contact between the dermis and the epidermis. In your palms, fingers, soles, and toes, the papillae projecting into the epidermis form friction ridges. (They help your hand or foot to grasp by increasing friction.) The pattern of the friction ridges on a finger is called a fingerprint.
 The papillary region is an example of a common anatomical “strategy” for increasing the surface area between two structures. More areas of direct contact lead to more chances for molecules to travel from one side to the other. Think about the difference between leaving a crowded parking lot after a concert with only 2 exits and one with 20 exits. We discuss another prominent example, the intestines, in Chapter 11.
The papillary region is an example of a common anatomical “strategy” for increasing the surface area between two structures. More areas of direct contact lead to more chances for molecules to travel from one side to the other. Think about the difference between leaving a crowded parking lot after a concert with only 2 exits and one with 20 exits. We discuss another prominent example, the intestines, in Chapter 11.
A manufacturing site
The reticular region is chock-full of protein fibers and is a complex and metabolically active layer. Cells and structures of the reticular region manufacture many of the skin’s characteristic products: hair and nails, sebum, watery sweat, apocrine sweat. (See the “Accessorizing Your Skin” section later in the chapter.) The region also contains structures that connect the integument to other organ systems: sensory structures to communicate with the nervous system, lymphatic vessels, and a very rich blood supply.
The blood vessels in the dermis provide nourishment and waste removal from its own cells as well as from the stratum basale. The blood vessels in the dermis dilate (become larger) when the body needs to lose heat and constrict to keep heat in. They also dilate and constrict in response to your emotional state, brightening or darkening skin color, thereby functioning as social signaling.
Getting under your skin: The hypodermis
The subcutaneous layer (or hypodermis, or superficial fascia) is the layer of tissue directly underneath the dermis. It is mainly composed of connective and adipose tissue (fatty tissue). Its physiological functions include insulation, the storage of energy, and help in the anchoring of the skin. It contains larger blood vessels, lymphatic vessels, and nerve fibers than those found in the dermis. Its loosely arranged elastin fibers anchor the hypodermis to the muscle below.
The thickness of the subcutaneous layer is determined in some places by the amount of fat deposited into the cells of the adipose tissue, which makes up the majority of the subcutaneous layer. Recently, researchers have found that adipose tissue also plays a very active role in the endocrine system (see Chapter 8).
Accessorizing Your Skin
This section has nothing to do with tattoos or body piercing. It’s all about your skin’s accessory structures: hair, nails, and glands — structures that work with the skin.
Now hair this
Your body has millions of hair follicles, about the same number as the chimpanzee, humanity’s closest evolutionary relative. (Although we don’t know who counted all of them!) Like chimps, humans have hairless palms, soles, lips, and nipples. Unlike a chimpanzee, most of your hair is lightweight and fine. The hair on your head is coarser and longer to help hold in body heat. Puberty brings about a surge of sex hormones that stimulate hair growth in the axillary (armpit) and pelvic regions and, in males, on the face and neck. Women with hormonal imbalances can develop facial hair, too. Turn to Chapter 8 for more about hormones.
A hair arises in a hair follicle, a small tube made up of epidermal cells that extend down into the dermis to take advantage of its rich blood supply. Like the epidermis, cells at the bottom of the hair follicle, called the papilla, continually divide to produce new cells that are added to the end of the hair and push the older cells up through the layers of the epidermis. On their way up and out, the hair cells become keratinized. By the time you see it, the hair is mostly completely flattened, dead cells full of keratin. The curvature of the follicle causes the shape of the exposed hair, ranging from tight curls to stick straight.
Hair goes through cycles of growth and dormancy. When the cells of the papilla begin to divide again, the hair falls out. This is why the length of your hair maxes out. The hairs on your head live about three to four years before you shed them, and eyelashes live about three to four months before falling out. People don’t go bald overnight. Baldness (called alopecia) occurs when follicles go dormant do not reactivate.
Nailing nails
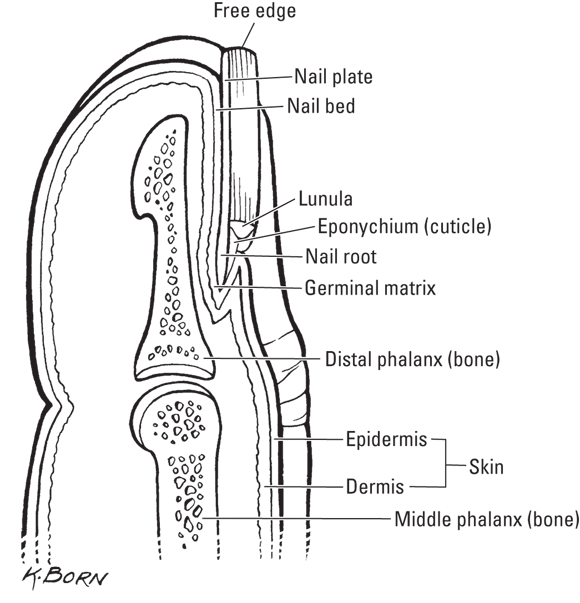
Your fingernails and toenails lie on a nail bed (not to be confused with a bed of nails). At the back of the nail bed is the nail root. Just like skin and hair, nails start growing near the blood supply that lies under the nail bed, and the cells move outward at the rate of about 1 millimeter per week. As they move out over the nail bed, they become keratinized. (See Figure 4-2.)
At the bottom of your nails is a white, half-moon-shaped area called the lunula. (Lun- is the Latin root for moon, as in lunar.) The lunula is white because this is the area of cell growth. In the nail body, the nail appears pink because the blood vessels lie underneath the nail bed. But many more cells fill in the area of growth. This layer is thicker, and you see white instead of pink.
Nothing’s bland about glands
Glands in the skin make and secrete substances that are transported to your body’s outer surface. The contraction of tiny muscles in the gland accomplishes this secretion. The two main types of skin glands are sudoriferous glands (sweat glands) and sebaceous glands (oil glands).
Sudoriferous glands
Your body contains two types of sudoriferous glands. Eccrine sweat glands are distributed all over the skin. These glands open to the skin’s surface, and when you’re hot, they release sweat to reduce body temperature by a process of evaporative cooling. When the sweat, which is mostly water, evaporates, it takes the heat with it.
Apocrine sweat glands start to develop during puberty and connect to the hair follicles of the armpits and groin. Apocrine sweat contains a milky white substance and may also contain pheromones, chemicals that communicate information to other individuals by altering their hormonal balance. (Some research has indicated that the apocrine secretions of one woman can influence the menstrual cycle of other women who live with her.) Apocrine glands become active when you’re anxious and stressed, as well as when you’re sexually stimulated. Bacteria on the skin that digest the milky white substance produce unpleasantly odiferous byproducts.
The milk-secreting glands in mammary tissue are thought to have evolved from apocrine sweat glands.
Sebaceous glands
Sebaceous glands secrete an oily substance called sebum into hair roots. Besides wreaking havoc with teenage facial pores, sebum has physiological functions. It helps maintain your hair in a healthy state, which is important in regulating body temperature. It flows out along the hair shaft, coating the hair and the epidermis, forming a protective, waterproof layer. Sebum prevents water loss to the outside. Sebum also helps to protect you from infection by making the skin surface an inhospitable place for some bacteria.
In the watery environment of the amniotic sac, the human fetus produces a thick layer of sebum, called the vernix caseosa. Ear wax (cerumen) is a type of sebum produced by specialized cells in the ear canal.
Your Skin Saving You
Your integumentary system participates in thousands of metabolic and homeostatic reactions, among them the thermoregulatory processes and the interaction of the skin and the nervous system.
Controlling your internal temperature
Your skin plays an important role in homeostasis, specifically thermoregulation (see Chapter 2). It has mechanisms that increase body temperature when you’re cold and decrease it when you’re hot.
Your body is continuously converting energy from food into energy in the form of ATP (see Chapter 3). About 60 percent of food energy is converted to heat in the metabolic reactions that produce ATP, and more heat is given off in the reactions that use ATP, such as muscle contraction. This heat replaces the heat that your body loses continuously to the environment. (See Chapter 16 for an overview of ten basic chemistry and physics concepts.)
Human physiology employs specially adapted integumentary structures for thermoregulation. When your internal temperature rises above its set point, the blood vessels in the dermis dilate, dissipating heat from the blood to the environment through the epidermis. The sweat glands are activated, and heat escapes the body as the sweat evaporates.
When your skin is cold, the sweat glands aren’t activated, thus slowing down evaporative cooling and raising your internal temperature by retaining the heat produced in metabolism. Blood vessels in the dermis constrict, limiting heat escape from the blood. If body temperature falls to about 97 degrees, shivering begins automatically, and these muscle contractions generate heat.
 Normal body temperature for a human is 97 to 100 degrees Fahrenheit (F). This is the optimal range for the very temperature-sensitive reactions of metabolism. A few degrees higher, and the body goes into convulsions. A few degrees lower, and metabolism gradually shuts down, sending the body into what may be its final sleep.
Normal body temperature for a human is 97 to 100 degrees Fahrenheit (F). This is the optimal range for the very temperature-sensitive reactions of metabolism. A few degrees higher, and the body goes into convulsions. A few degrees lower, and metabolism gradually shuts down, sending the body into what may be its final sleep.
Other mammals, including other primates, rely on a more or less dense covering of hair on the epidermis to conserve body heat. During the evolution of the human species, natural selection favored the development of a very light coat of hair over most of the body. Turn to Chapter 17 for some information related to that evolution.
Your skin is sensational
So how does your body know when it’s cold or hot? How do you know when you get a cut or splinter? How can you tell the difference between being tickled with a feather and punched with a fist? Because the dermis contains nerve endings that serve as specialized receptors for hot and cold, touch, pressure, and pain. The receptors, such as lamellated (Pacinian) corpuscles, tactile (Meissner’s) corpuscles, and Ruffini’s corpuscles, are sprinkled throughout the dermis and are connected to the nerves that run through the dermis and subcutaneous layer (hypodermis). See Chapter 7 for more about these receptors.
Not every square inch of skin contains all types of nerve endings. At one spot on your skin, you may sense light touch, while a few centimeters away, you may sense pressure; some spots sense cold, and some spots sense heat. These mixed messages connect with the network of nerves up to your brain, which does a pretty good job of making sense of the different kinds of information.
Your skin is self-healing
Damage to the skin, such as a cut, triggers epidermal cells to divide more rapidly, trying to fill in the space. If the cut extends into the dermis or deeper, and a blood vessel is broken, the clotting blood will first cover the area allowing time for the epidermal cells to divide and fill in the space. A covering, natural (like a scab) or otherwise (like a Band-Aid) keeps nutrient-rich fluids from seeping out, as well as germs from getting in. Special cells called phagocytes will come in and clean up the debris. Inflammation is also an essential part of this process. The dilation of the blood vessels brings more resources to the area to speed the process.
If the cut is particularly deep, the skin cells will not be able to divide fast enough to fill it in. As a result, special cells in the dermis, called fibroblasts, will be triggered to produce collagenous fibers. These bulky fibers are what can lead to a scar.
Pathophysiology of the Integument
Being in contact with the external environment, the integument inevitably encounters some nasty stuff: pathogens (disease-causing organisms like some bacteria, fungi, protists, and viruses), UV radiation, and harmful forces like fire, chemicals, and sharp objects. There are also hereditary pathophysiologies. Chances are that you’ve experienced — or known someone who has experienced — one of the conditions described in the following sections.
Skin cancer
Many cases of skin cancer are related to UV exposure. Skin cancers are classified as a melanoma (a malignant or spreading type) or a nonmelanoma (a limited-to-one-portion-of-the-skin type).
- Basal cell carcinoma is the most common form of skin cancer. UV radiation can cause a cancerous tumor to develop in the stratum germinativum. The immune system becomes increasingly unable to detect the tumor as it grows. This type of tumor is relatively easily removed and is usually easily cured.
- Squamous cell carcinoma is a melanoma type that starts in the epidermis. Squamous cell carcinoma is more likely to spread to a nearby organ than basal cell carcinoma, and for every 100 people diagnosed with squamous cell carcinoma, one is likely to die from it.
- Malignant melanoma starts in the melanocytes, the cells that produce melanin. The appearance of a malignant melanoma are almost black with irregular borders. These cancerous spots look like a spot on your garage floor where you spilled oil. Malignant melanoma occurs mostly in light-skinned people who have a history of severe sunburns, especially when they were kids. One in five people diagnosed with malignant melanoma die from it within five years.
Dermatitis
Dermatitis is inflammation of the skin that takes the form of a rash that itches and burns. The inflammation can have many causes: infection, insect bites, irritation from chemicals, allergy, skin abrasion from shaving, or sunburn. A genetic predisposition is frequently involved, as in seborrheic dermatitis, or eczema, which often affects the scalp and hair as well as the skin of the hands, feet, face, or just about anywhere else.
Many people have an episode of dermatitis at some time in their lives, and some people suffer chronic dermatitis. Although the cause can vary, the treatment is often relatively simple: some combination of avoiding the cause or eliminating the infectious organism (fungus, for example) and applying a hydrocortisone cream to calm the inflammation and allow the skin to heal.
Alopecia
Alopecia is the medical term for abnormal hair loss — that is, over and above the normal rate of hair loss caused by the follicles taking a break once in a while. Like dermatitis, the causes are quite various.
The most prevalent type is androgeic alopecia, or male pattern baldness. Androgeic alopecia is an inherited condition that affects about 25 percent of men before the age of 30 and two-thirds of all men before the age of 60. The condition is less common and less extreme in women. It can develop in older adults, resulting in an overall thinning of all the scalp hair rather than complete baldness.
Alopecia areata is a type of hair loss in which the immune system attacks hair follicles causing it to fall out in large patches. The root cause (sorry!) is unknown, but damage to the follicle is usually temporary. Alopecia areata is most common in people younger than 20, but children and adults of any age may be affected. Alopecia areata can be treated but not cured.
Temporary alopecia can result from a long list of causes, including stress, severe illness or surgery, nutritional deficiencies, treatment with certain drugs (notably chemotherapy agents for cancer, which attack all actively dividing cells), and certain medicines for arthritis, depression, heart problems, and high blood pressure. Use of some hair cosmetics or hair abuse (wearing the hair pulled back tightly over a long period of time) can harm the hair shaft or follicle. Trichotillomania, or compulsive hair pulling, can also eventually lead to alopecia.
Nail problems as signs of possible medical conditions
Unhealthy nails can be a symptom of an underlying disease and can be of help in diagnosis. For example, bluish nail beds are caused by poor circulation. More specific indications include the following:
- Brittle, concave (spoon-shaped) nails with ridges may indicate iron-deficiency anemia.
- Nails separating from the nail bed can result from a thyroid disorder in which too much of a thyroid hormone is produced, such as Graves disease.
- Black marks that look like tiny splinters under the nails can help diagnose respiratory disease or heart disease.
- Hard, curved, yellow nails may indicate bronchiectasis (chronic dilation of bronchial tubes) and lymphedema (fluid retention in lymph glands).
 Seeing what the integument does
Seeing what the integument does Explaining the integument’s structure
Explaining the integument’s structure Taking a closer look at hair, nails, and glands
Taking a closer look at hair, nails, and glands Understanding what your skin does for you
Understanding what your skin does for you Checking out the integument’s pathophysiology
Checking out the integument’s pathophysiology The root of integument is integr-, meaning “whole” as in integer (a whole number), integrate (to bring different parts together into one), integral (inseparable from the whole), and integrity (always a positive term, but more difficult to define).
The root of integument is integr-, meaning “whole” as in integer (a whole number), integrate (to bring different parts together into one), integral (inseparable from the whole), and integrity (always a positive term, but more difficult to define). The epidermis is on top of the dermis. The prefix epi- means “on top of.” Many anatomical structures are on top of other structures, so you see this prefix in many chapters throughout this book. Other related terms you may see are endo (within), ecto (outside), and hypo (beneath or lower).
The epidermis is on top of the dermis. The prefix epi- means “on top of.” Many anatomical structures are on top of other structures, so you see this prefix in many chapters throughout this book. Other related terms you may see are endo (within), ecto (outside), and hypo (beneath or lower).