IN THIS CHAPTER
 Looking at your blood and what’s in it
Looking at your blood and what’s in it
 Discovering arteries, veins, and capillaries
Discovering arteries, veins, and capillaries
 Breaking down the heart’s parts
Breaking down the heart’s parts
 Following blood along its path through your body
Following blood along its path through your body
 Looking at some cardiovascular system problems
Looking at some cardiovascular system problems
More than any other system, the cardiovascular system has contributed strong imagery to people’s daily language. “Heart” is a metaphor for love and for courage. People say they “nearly had a heart attack” to describe an experience of surprise or shock. Abstract but distinctive characteristic qualities are said to be “in one’s blood.” The blood itself runs cold, runs hot, and runs all over the place in informal speech and poetry. Scientifically speaking, emotions are more a matter of hormones than myocardium, and nobody’s blood is any redder or any hotter than anyone else’s. The heart is neither soft nor hard, but a muscular, fibrous pump, and blood is a complex biological fluid that must be kept moving through its specialized network of vessels. Ready to take a closer look?
Carrying Cargo: Your Blood and What’s in It
Blood — that deep red, body-temperature-warm, and metallic-tasting liquid that courses through your body — is a vitally important, life-supporting, life-giving, life-saving substance that everybody needs. And every adult-size body contains about five liters (1.3 gallons) of the precious stuff.
Blood consists of many different types of cells in a matrix called plasma. That’s what makes blood a connective tissue. The different types of cells — red blood cells, white blood cells, and platelets — are referred to as formed elements. They combine to 45 percent of the blood volume; the remaining 55 percent is plasma.
Watering down your blood: Plasma
Plasma is about 92 percent water. The remaining 8 percent or so is made up of plasma proteins, salt ions, oxygen and carbon dioxide gases, nutrients (glucose, fats, amino acids) from the foods you take in, urea (a waste product), and other substances carried in the bloodstream, such as hormones and enzymes.
The plasma proteins, produced in the liver, are made for the plasma. That is, they aren’t being transported anywhere. Their functions include
- Albumin: The smallest plasma protein and the most abundant, albumin maintains the osmotic pressure (tendency to pull water in) in the bloodstream within the homeostatic range.
- Fibrinogen: During the process of clot formation, fibrinogen is converted into threads of fibrin, which then form a meshlike structure that traps blood cells to form a clot.
- Immunoglobulin: This is another word for antibody — proteins that are created in response to an invading microbe (turn to Chapter 13 for more on the immunity).
Transporting oxygen and carbon dioxide: Red blood cells
Red blood cells (RBCs), or erythrocytes (erythro is the Greek word for “red”), are the most numerous of the blood cells and one of the most numerous of all cell types in your body. About one-quarter of the body’s approximately 3 trillion cells are RBCs. RBCs are among the cell types that must be constantly regenerated and disposed of. In fact, you produce and destroy a few million RBCs every second!
The cytoplasm of RBCs is full to the brim with an iron-containing biomolecule called hemoglobin. The iron-containing heme group in hemoglobin binds oxygen at the respiratory membrane (see Chapter 10) and then releases it in the capillaries. This is the sole mechanism by which all your cells and tissues get the oxygen they need to sustain their metabolism. RBCs containing heme-bound oxygen are bright red, the familiar color of the arterial blood that flows from wounds. RBCs in the venous system have less heme-bound oxygen and are a dark red.
 RBCs are so full of hemoglobin because they contain very little else. During differentiation, they lose their organelles, even their nucleus. Only their membranes retain their function.
RBCs are so full of hemoglobin because they contain very little else. During differentiation, they lose their organelles, even their nucleus. Only their membranes retain their function.
An RBC has about a four-month life span, at the end of which it’s destroyed by a phagocyte (a large cell with cleanup responsibilities) in the liver or spleen. The iron is removed from the heme group and is transferred to either the liver (for storage) or the bone marrow (for use in the production of new hemoglobin). The rest of the heme group is converted to bilirubin and released into the plasma (giving plasma its characteristic straw color). The liver uses the bilirubin to form bile to help with the digestion of fats.
At the same time as oxygen diffuses into a cell, carbon dioxide diffuses out, making its way in the interstitial fluid to the venous system. Some deoxygenated hemoglobin in the venous blood takes up carbon dioxide to form carboxyhemoglobin. At the respiratory membrane, carboxyhemoglobin releases the carbon dioxide and takes up oxygen again. Carbon dioxide is transported in several different ways in the blood to the respiratory membrane, where it enters the lung and is exhaled in the breath.
Plugging along with platelets
Platelets are tiny pieces of cells. Large cells in the red bone marrow called megakaryocytes break into fragments, which are the platelets. Their job is to begin the clotting process and plug up injured blood vessels. Platelets, also called thrombocytes (thrombus means “clot”), have a short life span — they live only about ten days.
Putting up a good fight: White blood cells
White blood cells (WBCs) are derived from the same type of hematopoietic stem cells as RBCs. However, they take different paths early in the process of differentiation. The WBCs, also called leukocytes, leave the red bone marrow and enter into circulation in their mature form. (Flip to Chapter 13 for more on WBCs and immunity.)
Looking at Your Blood Vessels
Your blood vessels comprise a network of channels through which your blood flows. But the vessels aren’t passive tubes. Instead, they’re very active organs that, when functioning properly, assist the heart in circulating the blood and influence the blood’s constitution. The innermost layer of the heart and of all vessels is continuous — it’s one very convoluted sheet of epithelium.
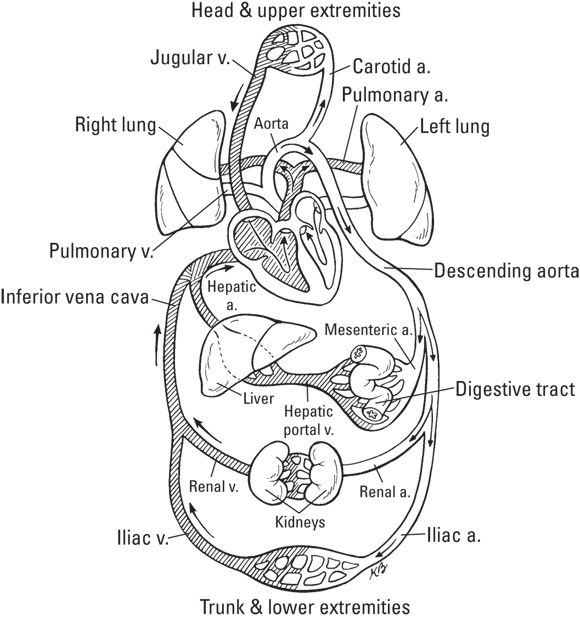
The vessels that take blood away from the heart are arteries and arterioles. The vessels that bring blood toward the heart are veins and venules. Generally, arteries have veins of the same size running right alongside or near them, and they often have similar names (turn to the “Arterial Components of the Cardiovascular System” color plate in the middle of the book for a diagram of the major arteries). The arterial vessels (arteries and arterioles) decrease in diameter as they spread throughout the body. Eventually, they end in the capillaries, the tiny vessels that connect the arterial and venous systems. The venous vessels become increasingly larger as they converge on the heart. The smaller venules carry deoxygenated blood from a capillary to a vein, and the larger veins carry the deoxygenated blood from the venules back to the heart.
Starting with the arteries
Your arteries form a branching network of vessels, with the main trunk, called the aorta, arising from the left ventricle and splitting immediately into the brachiocephalic trunk, left common carotid artery, and left subclavian artery, which serve the head and upper limbs. The descending aorta — which serves the thoracic organs, abdominal organs, and lower limbs — gives off several branches. The first are the mesenteric arteries, the main arteries of the digestive tract. It also gives off two renal arteries, which supply the kidneys; and the common iliac arteries, which supply the pelvis and lower limbs. The arteries branch into smaller and smaller vessels, becoming arterioles that end in capillary vessels.
Although an artery looks like a simple tube, the anatomy is complex. Arteries are made of three concentric layers of tissue around a space, called the lumen, where the blood flows (see Figure 9-1). The outside layer, the tunica externa, is a thick layer of connective tissue that supports the vessel and protects the inner layers from harm. The larger the artery, the thicker the connective tissue supporting it.
The next layer in, the tunica media, is a thick wall of smooth muscle and elastic tissue. This layer expands and contracts with every pulse wave (heartbeat), and sometimes it gives a little squeeze to increase the pressure and force the blood through. This layer controls vasoconstriction (decreasing diameter) and vasodilation (increasing diameter) of the vessels.
The inner layer, the tunica interna, is a single-cell thick layer of simple squamous epithelium that lines the lumen and is continuous through all the organs of the cardiovascular system. The vascular endothelium, as this tissue is also called, is very active metabolically, releasing into the blood various substances that influence blood circulation and vascular health. It also specializes in transporting oxygen, nutrients, and other substances from the blood flowing in the lumen to the smooth muscle fibers of the tunica media.
Cruising through the capillaries
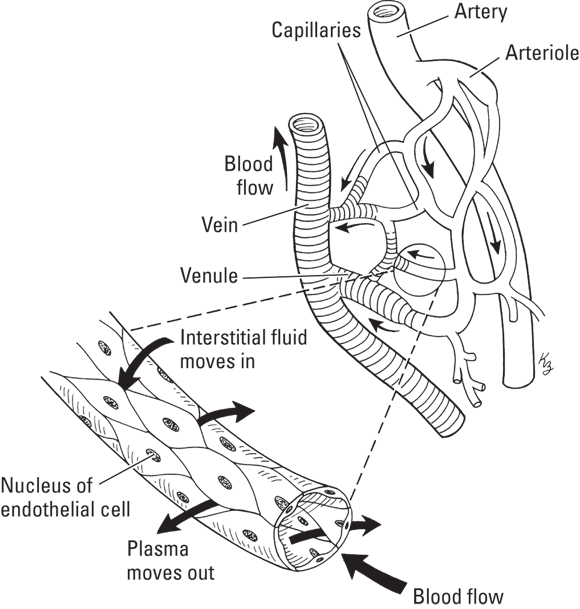
After passing from the arteries and the arterioles, blood enters the capillaries, which lie between larger blood vessels in capillary beds. A capillary bed forms a bridge between the arterioles and the venules.
Your capillaries are your smallest vessels: only the single-cell thick epithelial layer surrounds the lumen. The precapillary sphincters of the metarterioles (connectors of arteriole to capillary) can tighten or relax to control blood flow into the capillary bed.
Lacking the structure and complexity of arteries and veins, capillaries rely on simple diffusion to get their job done: moving oxygen and nutrients from the blood to the tissue and waste materials from the cells of the tissue to the blood. Molecules that are unable to diffuse exit the capillaries via filtration, driven out by the pressure applied on the capillary wall by the blood. Capillary exchange is the term used to describe these processes (see Figure 9-2).
The capillaries come into close contact with the cells of your tissues. At the end near the arteriole, oxygen diffuses out of the red blood cells and nutrient molecules out of the plasma, across the capillary membrane, and directly into the tissue fluid. The oxygen and nutrients dissolved in the tissue fluid diffuse across the membrane of the adjacent cells. (See Chapter 3 for more on diffusion.)
At the venule end, the carbon dioxide and other waste materials diffuse out of the tissue fluid and across the capillary membrane into the blood. Then, the blood continues on through the venous system, and those waste materials are deposited in the proper locations on their way out of the body. The carbon dioxide diffuses out of the bloodstream in the lungs, so it can be exhaled and thus removed from the body, while other metabolic waste is filtered through the kidneys.
 Capillary beds are everywhere in your body, which is why you bleed anywhere that you even slightly cut your skin.
Capillary beds are everywhere in your body, which is why you bleed anywhere that you even slightly cut your skin.
Besides aiding in the exchange of gases and nutrients throughout your body, capillaries serve two other important functions:
- Thermoregulation: Precapillary sphincters tighten when you’re in a cold environment to prevent heat loss from the blood at the skin surface. Blood is then shunted from an arteriole directly to a venule through a nearby arteriovenous shunt. When you’re in a warm environment or you’re producing heat through exertion, the precapillary sphincters relax, opening the capillary bed to blood flow and dispersing heat.
- Blood pressure regulation: When blood pressure (blood volume) is low, the hormones that regulate blood pressure stimulate the precapillary sphincters to tighten, temporarily reducing the total volume of the blood vessel system and, thus, raising the pressure. When blood pressure is high, the hormones stimulate the sphincters to relax, increasing overall system volume and reducing pressure. These hormones have the same effect on the larger vessels.
Visiting the veins
Small veins converge into larger veins, all merging in the inferior vena cava and superior vena cava, the largest vessels in the venous system. These major veins return blood from below and above the heart, respectively. The inferior vena cava lies to the right of, and more or less parallel to, the descending aorta. The superior vena cava lies to the right of, and more or less parallel to, the aorta.
In the lower body, the internal iliac veins, which return blood from the pelvic organs, and the external iliac veins, which return blood from the lower extremities, converge into the common iliac veins. The renal veins return blood from the kidneys. Both these major veins flow into the inferior vena cava.
Blood from the digestive tract travels in the hepatic portal vein to the liver. Specialized cells in the liver move glucose molecules from the blood into storage. Phagocytic cells in the liver destroy bacterial cells that make it through the digestive process and remove toxins and other foreign material from the blood. Blood exits the liver through the hepatic veins, which flow into the inferior vena cava. The inferior vena cava empties into the right atrium.
Deoxygenated blood from the head and upper extremities drains into the brachiocephalic veins. The veins of the upper extremity — the ulnar veins, radial veins, and subclavian veins — also drain into the brachiocephalic veins. The jugular veins of the head and neck also drain into the brachiocephalic veins, which connect to the superior vena cava, which enters the right atrium.
After the blood from the right atrium has been pumped into the right ventricle, it’s pumped into the lungs, where the blood is oxygenated, and then it flows back to the heart in the pulmonary veins, the only veins that carry oxygenated (red) blood.
Veins have a similar anatomy to arteries, although they tend to be wider and their walls thinner and less elastic. The tunica interna of a vein is also part of the continuous endothelial layer that lines the whole network. The tunica media has a layer of elastic tissue and smooth muscle, but this layer is much thinner in a vein than in an artery. The veins have virtually no blood pressure, so they don’t need a thick muscle layer to vary the vessel diameter or withstand fluid pressure. The outermost tunica externa is the thickest layer of a vein.
Because veins don’t have a thick muscle layer to push blood through them, they depend on contraction of skeletal muscles to move blood back to the heart. As you move your arms, legs, and torso, your muscles contract, and those movements “massage” the blood through your veins. The blood moves through the vein a little bit at a time. The larger veins have valves that keep blood from flowing backward. The valves open in the direction that the blood is moving and then shut after the blood passes through to keep the blood heading toward the heart.
Cardiac Anatomy
The cardiovascular system (formerly known as the circulatory system) consists of the heart and the blood vessels. The heart’s pumping action squeezes blood out of the heart, and the pressure it generates forces the blood through the blood vessels. The autonomic nervous system controls the rate of the heartbeat.
Sizing up the heart’s structure
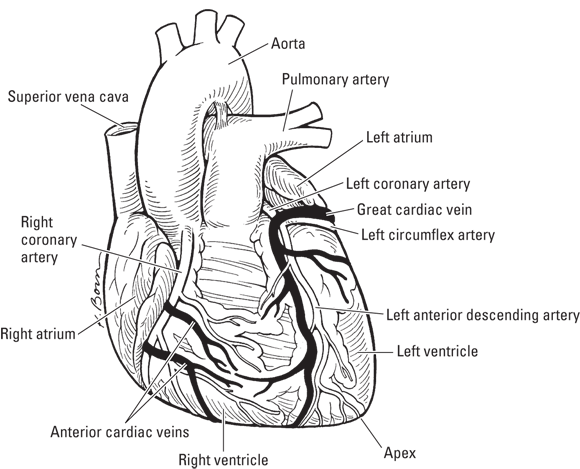
The heart is shaped like a cone and is about the size of your fist in width and about two fists in length. It lies between your lungs, just behind (posterior to) your sternum, and the tip (apex) of the cone points down and to the left (see Figure 9-3). In most individuals, the heart is situated slightly to the left of center in the chest.
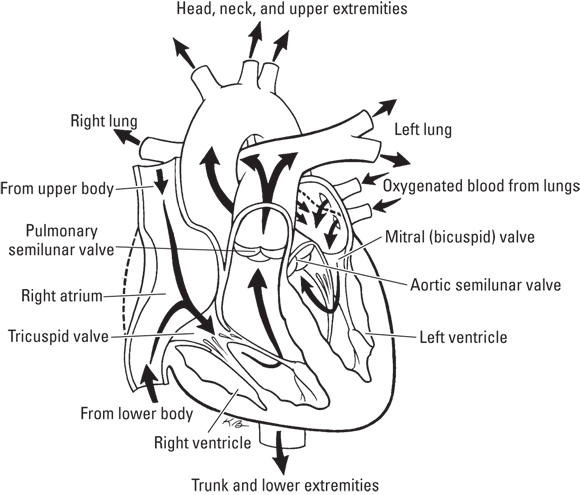
The four hollow spaces of the heart are called its chambers. You can check them out in the “Heart” color plate in the middle of the book. The heart is divided anatomically and functionally into left and right sides. Each side has one atrium and one ventricle, each with a separate function. A thin layer called the interatrial septum separates the atria; the interventricular septum separates the ventricles and is thick and muscular. The contraction of the heart muscle pumps blood into and out of all four chambers in a rhythmic pattern.
Between the chambers are valves that allow measured quantities of blood to flow into the chambers and keep blood flowing in the right direction. The valves’ names tell you their anatomical location or characteristics. The two atrioventricular (AV) valves lie between the atrium and the ventricle on each side; the bicuspid valve (BV), often called the mitral valve, has two flaps; and the tricuspid valve (TV) has three flaps. The semilunar valves (SV) are shaped like half-moons. In Figure 9-4, the arrows show the direction of blood flow through the chambers of the heart.
During one heartbeat, blood fills the right atrium from the vena cavae. It then passes through the tricuspid valve, filling the right ventricle. It’s then pumped through the pulmonary valve into the pulmonary artery. At the same time, the left atrium is being filled from the pulmonary veins. Blood then moves through the mitral valve into the left ventricle. It exits through the aortic valve into the aorta.
Examining the heart’s tissues
The tissues of the heart perform the functions required to keep the double-pump working strongly and steadily. Like other hollow organs, the heart is made up of layers of endothelial and connective tissue.
- Endocardium: A layer of endothelial tissue that lines the inside of the chambers. This layer is continuous with the vascular endothelium, which we talk about in more detail in the “Starting with the arteries” section.
- Myocardium: The thick, muscular layer of your heart. The myocardium (literally, “heart muscle”) is composed of cardiac muscle fibers that contract in a coordinated way to pump the blood out of the heart and into the aorta with enough force to carry it through the arterial system and out into the capillaries.
- Epicardium: The visceral layer of the pericardium. It’s a conical sac of fibrous tissue that closely envelopes the myocardium and surrounds the roots of the major blood vessels. The epicardium secretes pericardial fluid into the pericardial cavity, which lubricates the tissues as the heart beats.
- Pericardial cavity: A fluid-filled space between the epicardium and the parietal layer of the serous pericardium. The fluid reduces friction between the pericardial membranes.
- Parietal pericardium: A serous membrane that’s attached to the outermost layer of the heart, the fibrous pericardium. The fibrous pericardium is a thick, white sheet of fibrous connective tissue that anchors the heart and the major blood vessels, including the aorta, to the sternum and diaphragm. (Your heart is not just floating in your chest.) The parietal pericardium also secretes pericardial fluid into the pericardial cavity.
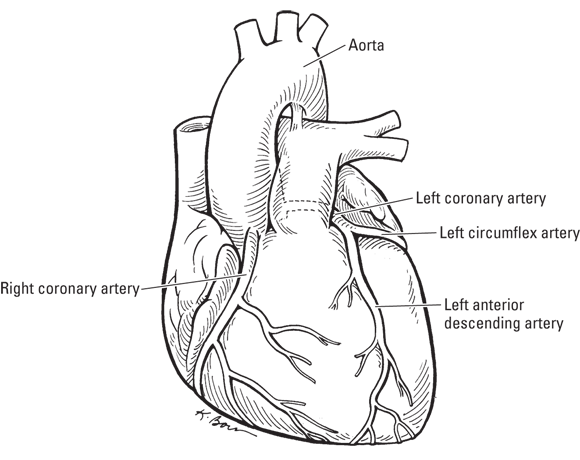
Supplying blood to the heart
Blood flows in and out of the heart every second of your life, and some of that blood needs to supply the cells of the heart itself with oxygen and nutrients. Unfortunately, the heart cannot access it from the blood filling its chambers — capillary exchange still must take place in the myocardium. The coronary arteries supply oxygenated blood to the heart, while cardiac veins return deoxygenated blood to the pulmonary circulation loop (for the two loops of circulation, flip ahead to Figure 9-8).
- Coronary arteries: Two large coronary arteries and their many branches supply blood to the heart. These large arteries branch off the aorta and carry blood to the left and right sides. They’re called the left and right coronary arteries because they sit atop and encircle the heart, looking like a crown (see Figure 9-5). The right coronary artery and its two major branches, the marginal artery and the posterior interventricular artery, primarily supply the right atrium and ventricle with oxygenated blood and nutrients. The left coronary artery and its two branches, the anterior descending coronary artery and the left circumflex coronary artery, primarily supply the left atrium and ventricle with oxygenated blood and nutrients.
- Cardiac veins: The cardiac venous system is similarly branched, often lying alongside the coronary arteries and their branches. Like everything about the heart, the cardiac venous system is composed of two parts, left and right. The left cardiac venous system receives deoxygenated blood from most of the superficial veins of the heart. The right cardiac venous system is composed of veins that originate on the anterior and lateral surfaces. The cardiac veins merge into the coronary sinus, which drains blood into the right atrium. The smallest vessels (the venae cordis minimae) drain the myocardium directly into the chambers.
Cardiac Cycle
In order to keep our blood flowing smoothly and consistently through our bodies, the contractions of the heart must be intricately timed. Both atria must contract at the same time, followed by both ventricles shortly thereafter, creating one complete heartbeat. The cardiac cycle is defined as the series of events required to generate a single heartbeat. This section explores how the heart’s electrical system triggers contractions and how those contractions generate pressure changes that push the blood along its path.
Generating electricity
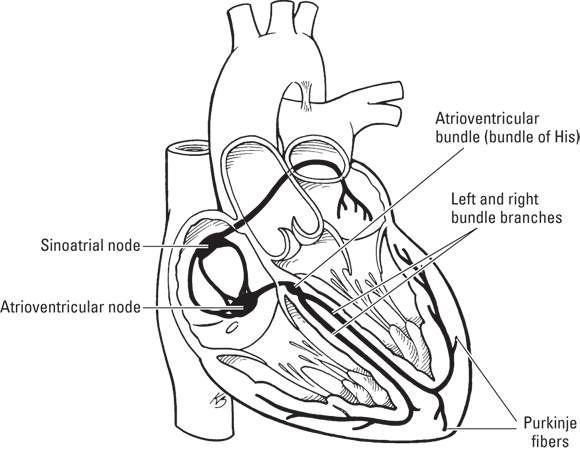
Certain structures of the heart, together called the cardiac conduction system, specialize in initiating and conducting the electrical impulses that induce your heartbeat, keeping it regular and strong in every part of the organ as it moves the blood through. The series of events that generate a single heartbeat is known as the cardiac cycle.
Throughout the myocardium (muscle wall of the heart) are specialized myocardial fibers (cells). Instead of being designed to contract, these fibers only carry impulse. These conducting fibers branch throughout their respective chambers so that the stimulus reaches the contracting fibers at the same time, creating the syncytium. The contracting fibers work in the same manner as the skeletal muscle fibers (see Chapter 6).
Anatomy of cardiac conduction
Five structures comprise the cardiac conduction system (see Figure 9-6):
- Sinoatrial (SA) node: A small knot of cardiac muscle-like tissue (the conducting cells look like cardiac muscle cells, but they’ve lost the ability to contract) located on the back wall of the right atrium, near where the superior vena cava enters the heart. Once nervous input establishes the rhythm, the SA node becomes self-stimulating, which is why it’s considered the heart’s pacemaker. It does not require stimulus from a neuron to tell it to contract every time — only to tell it to speed up or slow down.
- Arterioventricular (AV) node: A similar small mass of tissue located in the right atrium but near the septum that divides the right and left atria from the ventricles. Its function is to relay the impulses it receives from the SA node to the next part of the conduction system.
- Atrioventricular (AV) bundle (bundle of His): A bundle of fibers that extends from the AV node into the interventricular septum (which divides the heart into right and left sides). The AV bundle transmits cardiac impulses.
- Left and right bundle branches: Where the septum widens, the AV bundle splits into the right and left bundle branches, each extending down toward the apex and then up along the outside of the ventricles. These bundles carry cardiac impulses.
- Purkinje fibers: At the ends of the AV bundle branches are the Purkinje fibers, which deliver the impulse up and around to the myocardial fibers, causing the ventricles to contract.
 The word node is used in many different contexts, and not only in anatomy. In general, it describes a local connecting point of component parts, literal and figurative. In cardiac anatomy, a node is a specialized type of tissue that looks like muscle and generates electrical impulses like nervous tissue.
The word node is used in many different contexts, and not only in anatomy. In general, it describes a local connecting point of component parts, literal and figurative. In cardiac anatomy, a node is a specialized type of tissue that looks like muscle and generates electrical impulses like nervous tissue.
The sequence of events
The cardiac conduction system is responsible for keeping the cardiac cycle going. If the cardiac cycle stops for too long, you experience serious consequences (see the “Cardiac disorders” section later in the chapter). It is also responsible for the timing of the cycle. A single heartbeat actually consists of two contractions. First, both the right and left atria contract together, pushing blood down into the ventricles. Moments later, the right and left ventricles contract together pushing the blood out of their respective arteries.
Here’s how the cycle goes:
-
The electrical impulse is initiated in the SA node.
The conducting fibers spread the impulse throughout the atrial syncytium. The right and left atria contract simultaneously, pumping blood into the right and left ventricles, respectively.
-
The impulse passes to the AV node, which sends it to the AV bundle.
Some of the fibers connected to the SA node carry the impulse to the AV node. These fibers are narrower, providing the delay between the atria and ventricles contracting.
-
The impulse passes into the right and left bundle branches and ultimately into the Purkinje fibers, causing the ventricles to contract.
By the time the ventricles begin to contract, the atria are relaxing. The impulse is carried to the apex first and then back up for two reasons:
- To further ensure the delay before the ventricles contract
- To allow the ventricles to contract in a pattern
The purkinje fibers weave into the myocardium of the ventricles in a spiraling pattern. This causes the ventricular syncytium (walls of both ventricles) to contract in an upward, twisting motion.
-
The ventricles relax.
All chambers remain relaxed until the SA node generates the next impulse, starting the cycle over again.
Moving blood through the heart
In order for the blood to move on its well-timed path through the heart, we must coordinate the valves opening and closing just as we do the contractions. It’s reasonable to conclude that the contractions are the cause of the valves opening and closing, but it’s actually more complicated than that.
At the start of the cardiac cycle, all the chambers are relaxed and all the valves are closed. When a chamber is relaxed, it is said to be in diastole; the contraction phase is called systole. The sequence of events is as follows:
-
Blood begins filling the atria, the pressure on the AV vale pushes it open.
Both chambers are still in diastole.
-
Blood flows into the ventricle to equalize the pressure between the two chambers.
Blood stops flowing when about 70 percent of the volume to be pumped out is in the ventricle.
- The atria contract, pushing the remaining blood into the ventricles.
-
The atria relax, the ventricles contract, and the AV valves close.
This drop in pressure of the atria creates a vacuum, which pulls the flaps of the AV valves closed. The papillary muscles contract with the walls, pulling on the chordae tendinae to ensure the valves stay closed (see the “Heart” color plate for the location of these structures).
-
Ventricles continue contracting.
The atria are relaxed, all valves are closed.
-
The ventricular systole increases the pressure inside the ventricles, pushing open the semilunar valves.
Blood exits into the pulmonary artery and aorta.
-
The ventricles relax, decreasing the pressure, which pulls the semilunar valves closed.
The drop in pressure causes blood to start to flow backward, but it catches in the cups of the valves, snapping them shut.
 The movement of blood through the heart is more a result of pressure changes than contractions directly. The intricate timing provided by the conduction system triggers the contractions, which provide the pressure changes that both open the valves so the blood may exit and close them to prevent backward flow.
The movement of blood through the heart is more a result of pressure changes than contractions directly. The intricate timing provided by the conduction system triggers the contractions, which provide the pressure changes that both open the valves so the blood may exit and close them to prevent backward flow.
The heartbeat
If you’re a fan of medical dramas, you’re no doubt familiar with the heart rate monitor — those squiggly lines moving across the screen. The implication is that those waves correspond to the contraction of the chambers. Actually, this isn’t quite the case.
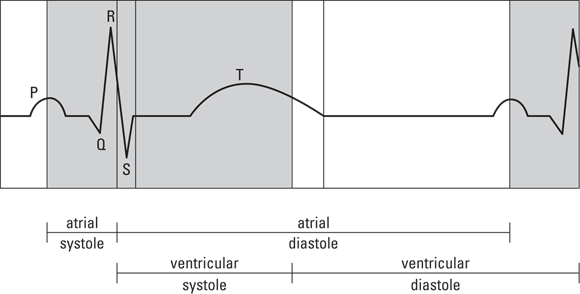
The heart’s electrical signals can be measured and recorded digitally to produce an image called an electrocardiogram (ECG or EKG). Three major waves appear on the EKG, each showing the electrical signals as they move through the heart (see Figure 9-7). The first wave, called the P wave, records the spread of impulse through the right and left atria. The second and largest wave, the QRS wave, shows the spread of impulse through the right and left ventricles. The third wave, the T wave, records the recovery of the ventricles.
The conducting fibers spread impulse just as neurons do (see Chapter 7). The spikes on the EKG correspond to the movement of ions, measurable by electrodes on the skin because body fluids conduct this electricity. As the conducting fibers depolarize, the EKG line moves up and back down. The same happens when they repolarize (because the flow of K+ ions out is measurable electricity just as the flow of Na+ ions in). Because the repolarization of the atria occurs during the QRS, you don’t see a wave for it.
 The waves on an EKG show the electrical conduction in the heart, not the contraction. The atria would be contracting in the period of time between the end of the P wave and the start of the QRS (roughly). The ventricles are contracting from the end of the QRS to the T wave.
The waves on an EKG show the electrical conduction in the heart, not the contraction. The atria would be contracting in the period of time between the end of the P wave and the start of the QRS (roughly). The ventricles are contracting from the end of the QRS to the T wave.
Problems with signal conduction due to disease or abnormalities of the conducting system can occur anyplace along the heart’s conduction pathway. Abnormally conducted signals resulting in irregular heartbeat are called arrhythmias.
Physiology of Circulation
You do it 100,000 times every day. Waking or sleeping, from a moment early in fetal development until the moment you die, the beat goes on. It may speed up slightly when you’re working hard physically or you’re excited or stressed, and some people can slow theirs down with meditation techniques. But for most people, it just plugs along, the same thing over and over.
What is it? The heartbeat, of course. The beating heart pushes blood around a double-circuit — out through your arteries, ultimately into your capillary beds, then across your capillary beds and into your veins, and back to the heart. The blood passes through the heart to the lungs and then back to the heart and out through the arteries again. Each complete double-circuit takes less than one minute.
On the beating path: The circuits of blood through the heart and body
 The heart is a double-pump, so it has two circuits: heart to lungs and back to heart, and heart to body and back to heart. These are called the pulmonary circulation path and the systemic circulation path, respectively (see Figure 9-8). Every drop of your blood travels around the double-circuit about once per minute.
The heart is a double-pump, so it has two circuits: heart to lungs and back to heart, and heart to body and back to heart. These are called the pulmonary circulation path and the systemic circulation path, respectively (see Figure 9-8). Every drop of your blood travels around the double-circuit about once per minute.
Pulmonary circulation
Deoxygenated blood enters the heart’s right atrium from the largest veins in the body, the superior vena cava and the inferior vena cava. When the SA node initiates the cardiac conduction cycle, the right atrium contracts, pumping the blood into the right ventricle.
When the impulse is passed to the AV node and on to the AV bundle, the right bundle branch, and the Purkinje fibers, the right ventricle contracts, pumping blood into the pulmonary arteries, which take it to the lungs for gas exchange.
During the relaxation phase of the atria, the newly oxygenated blood flows into the left atrium.
 The pulmonary arteries are the only arteries that carry deoxygenated blood, and the pulmonary veins are the only veins that carry oxygenated blood.
The pulmonary arteries are the only arteries that carry deoxygenated blood, and the pulmonary veins are the only veins that carry oxygenated blood.
Systemic circulation
When the SA node initiates the cardiac conduction cycle, the left atrium contracts, pumping the oxygenated blood into the right ventricle.
When the impulse is passed to the AV node and on to the AV bundle, the left bundle branch, and the Purkinje fibers, the left ventricle contracts, pumping blood into the aorta. From the aorta, it travels through the arteries and arterioles to the capillary beds, and then back to the heart through the veins.
During the relaxation phase of the atria, the deoxygenated blood flows into the right atrium.
Putting your finger on your pulse
You can feel the rhythmic pulsation of blood flow at certain spots around your body, most commonly on the radial artery on the inside of the wrist or on the carotid artery of the neck. What you feel as you touch these spots is your artery expanding as the blood rushes through it and then immediately returning to its normal size when the bulge of blood has passed. This pulsation corresponds to your heart rate and is usually recorded as beats per minute.
 The entire cardiac cycle takes about 0.86 of a second, based on the average of 70 heartbeats per minute. If your cardiac cycles take less time, your heart is beating too fast (tachycardia); if there’s too much time between your cardiac cycles, your heart is beating too slowly (bradycardia).
The entire cardiac cycle takes about 0.86 of a second, based on the average of 70 heartbeats per minute. If your cardiac cycles take less time, your heart is beating too fast (tachycardia); if there’s too much time between your cardiac cycles, your heart is beating too slowly (bradycardia).
Going up, going down, holding steady: Blood pressure
Blood pressure is a term used to describe the force of blood pushing against the wall of an artery. It’s measured in millimeters of mercury at both the highest point (systole, when the heart is contracted) and the lowest point (diastole, when the heart is relaxed) in the cardiac cycle. The systole pressure is always higher than the diastole. The higher the systolic and diastolic values, the more pressure there is on the walls of the arteries. Two factors affect the blood pressure: the cardiac output, which is the amount (volume) of blood the heart pumps out per unit of time, and the peripheral resistance, a measure of the diameter and elasticity of the vessel walls.
The cardiac output is determined by the heart rate and the blood volume put out from a ventricle during one beat (reported in L/min.). When either of these rises, the blood pressure rises. Heart rate is increased by physical exertion, the release of epinephrine (a hormone), and other factors. The blood volume is influenced by the action of ADH (antidiuretic hormone) and other mechanisms in the kidneys to control the amount of water that’s removed from the urine and restored to the blood.
The arteries’ diameter changes locally and continuously. The pressure of the pulse wave increases pressure on the vascular endothelium, inducing it to release molecules, mainly nitrous oxide (NO), that induce relaxation in the tunica media. The endothelium’s ability to respond to the pulse-wave pressure is extremely important to vascular health. Resistance in the arteries to expansion as the blood rushes through raises the blood pressure.
As part of homeostasis, receptors in the arteries, called baroreceptors, measure blood pressure. If the blood pressure is above the normal range, the brain sends out impulses to cause responses that decrease the heart rate and dilate the arterioles, both of which decrease blood pressure.
Not going with the flow
Not the least amazing thing about blood is its ability to stop flowing. The term for this is hemostasis (literally, “blood stopping,” and not to be confused with homeostasis). Hemostasis is the reason why you didn’t bleed to death the first time you cut yourself. When vessels are cut, blood flows, but only for a moment, just about long enough to clean the cut. As you watch, the blood stops flowing, and a plug, called a clot, forms. Within a day or so, the clot has dried and hardened into a scaly scab. Eventually, the scab falls off, revealing fresh new skin.
A blood clot consists of a plug of platelets enmeshed in a network of insoluble fibrin molecules. The clotting cascade is a physiological pathway that involves numerous components in the blood itself interacting to create a barrier to the flow. Each step in the process triggers the next so the whole mechanism is an example of positive feedback (see Chapter 2). As soon as a blood vessel is injured, a signal is sent from the vascular endothelium to the platelets, also called thrombocytes (thrombo means “clot”), summoning them to the injury site. The platelets become sticky, and they start to adhere together. Proteins in the blood plasma, called coagulation factors or clotting factors, respond in a complex cascade to form fibrin strands, which strengthen the platelet plug. Within minutes, your blood is safe in your body, where it belongs.
A blood clot in the right place is something to be grateful for. But blood tends to start clotting whenever it’s not flowing freely, and this tendency can cause problems in the peripheral vessels (the arteries and veins of the legs). Clots also form on the inner wall of blood vessels when the endothelium is injured by disturbances in blood flow (turbulence) or by free radicals in the blood. These tiny clots adhere to the wall, further disturbing flow and causing more turbulence and more injury. Atherosclerotic plaque may begin to form around the clot (see the next section for a discussion of atherosclerosis). Worst of all, perhaps, is when the clot, with the plaque attached, breaks off from the vessel wall and floats free (sort of) in the bloodstream. Sooner or later, this embolus lodges somewhere in a vessel, sometimes with sudden and fatal consequences such as a stroke.
 Looking at your blood and what’s in it
Looking at your blood and what’s in it Discovering arteries, veins, and capillaries
Discovering arteries, veins, and capillaries Breaking down the heart’s parts
Breaking down the heart’s parts Following blood along its path through your body
Following blood along its path through your body Looking at some cardiovascular system problems
Looking at some cardiovascular system problems RBCs are so full of hemoglobin because they contain very little else. During differentiation, they lose their organelles, even their nucleus. Only their membranes retain their function.
RBCs are so full of hemoglobin because they contain very little else. During differentiation, they lose their organelles, even their nucleus. Only their membranes retain their function.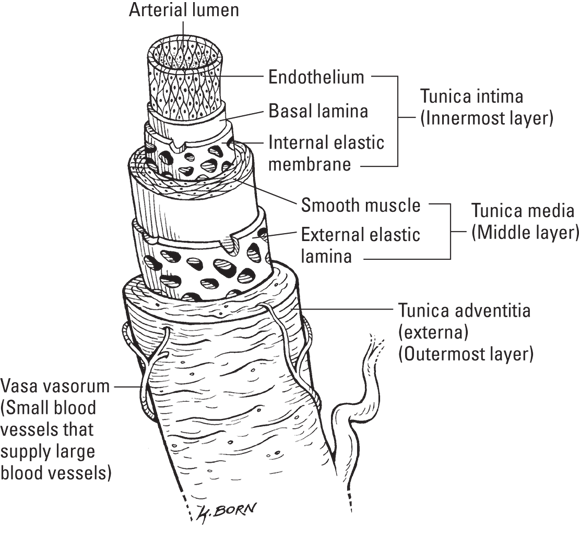
 Capillary beds are everywhere in your body, which is why you bleed anywhere that you even slightly cut your skin.
Capillary beds are everywhere in your body, which is why you bleed anywhere that you even slightly cut your skin.