Chapter 10
The Respiratory System: Breathing Life into Your Body
IN THIS CHAPTER
 Understanding what the respiratory system does
Understanding what the respiratory system does
 Checking out the parts of the respiratory system
Checking out the parts of the respiratory system
 Drawing in some breathing knowledge
Drawing in some breathing knowledge
 Looking at some common respiratory system ailments
Looking at some common respiratory system ailments
The air we inhale more than 20,000 times each day is mostly made of nitrogen, but it also contains the vital, irreplaceable gas that is oxygen. Without oxygen, our cells can’t perform cellular respiration efficiently enough to generate the ATP they require (see Chapter 2). We do need nitrogen to build proteins, but we aren’t equipped to obtain nitrogen from the air we breathe. Getting the oxygen into our blood is what the respiratory system is all about, so take a deep breath and prepare to find out all about it in the pages ahead.
Functions of the Respiratory System
Your respiratory system manages the flow of air into and out of your body. It oversees a number of vital body functions, including the following:
- Ventilating: Ventilation — the act of breathing — isn’t the same as respiration — the exchange of gases. You don’t have to think about performing either task, but ventilation involves the physical movement of your diaphragm muscle, rib cage, and lungs to draw air in and push air out of the body. See the “Breathing: Everybody’s Doing It” section later in this chapter.
- Exchanging gasses: The job of the respiratory system is to supply oxygen and remove carbon dioxide from the blood as it circulates through the body. Chapter 9 discusses how the blood gets into and out of the lungs in the process of pulmonary circulation. This is sometimes called external respiration to distinguish it from cellular respiration. Gas exchange happens in the lungs, where the respiratory tissues and the circulatory tissues meet. See the “Gas exchange” section later in the chapter.
- Regulating blood pH: Maintaining blood pH within the homeostatic range requires coordination between the respiratory and urinary systems, with help from the endocrine system and, of course, the cardiovascular system itself.
- Producing speech: The ability of humans to consciously control breathing permits speech and singing.
Nosing around Your Respiratory Anatomy
The respiratory tract is the path of air from the nose to the lungs. It’s divided into two sections: the upper respiratory tract (from the beginning of the airway at the nostrils to the pharynx) and the lower respiratory tract (from the top of the trachea to the diaphragm). Turn to the “Respiratory System” color plate in the center of the book to get an idea of what the internal structures of the respiratory tract look like.
The respiratory tract is one of the places in the body where cells are replaced constantly throughout life (see Chapter 2).
Nose
This is one time that it’s okay to turn your nose up at your anatomy. Really. Point your nose up while looking in the mirror. (Yes, you have to put the book down.) See the two big openings? Those are your nostrils, and that’s one of two places where air enters and exits your respiratory system. Now, see all those tiny hairs in your nostrils? Those little hairs serve a purpose. They trap dirt, dust particles, and bacteria. Okay. You can put your head down now. The rest of your respiratory parts are way inside of your body, so you can’t see them in the mirror.
Just beyond your nostrils, the nasal septum separates your nasal cavities. Inside the nasal cavities, the three tiny bones of the nasal conchae provide more surface area inside the nose because they’re rolled up (like conch shells). The cells of the respiratory mucosa that lines the inside of the nasal cavity have tiny cilia that move the dirt-laden mucus toward the outside of the nostrils.
The lacrimal glands secrete tears that flow across the eye’s surface and drain through the openings in the corner of the eye (lacrimal puncta), into the nasolacrimal ducts and the nasal cavities. That’s why your nose runs when you cry.
Your sinuses are air spaces in your skull that lighten the weight of your head. The sinuses open into the nasal cavities so they can receive air as you breathe, and, like the nasal cavities, the sinuses are lined with mucous membranes. The sinuses also contribute to the tone of your voice.
Pharynx
Air passes through your pharynx on its way to your lungs. Along the way, it passes through and by some other important structures, like your larynx and tonsils.
Your pharynx is divided into three regions based on what structures open into it:
-
Nasopharynx: The top part of your throat where your nasal cavities drain. If you press your tongue to the roof of your mouth, you can feel your hard palate. This bony plate separates your mouth (oral cavity) from your nose (nasal cavities). If you move your tongue backward along the roof of your mouth, you reach a soft spot. This spot is the soft palate. Beyond the soft palate is where your nasal cavities drain into your throat, your nasopharynx. Your soft palate moves backward when you swallow so that the nasopharynx is blocked.
 Normally, the soft palate blocking the nasopharynx keeps food from going up into your nose. But when you’re laughing and eating or drinking at the same time, your soft palate gets confused. When you go to swallow, it starts to move back, but when you laugh suddenly, it thrusts forward, allowing whatever’s in your mouth to flow up into your nasal cavities and immediately fly out of your nostrils to the delight of everyone around you.
Normally, the soft palate blocking the nasopharynx keeps food from going up into your nose. But when you’re laughing and eating or drinking at the same time, your soft palate gets confused. When you go to swallow, it starts to move back, but when you laugh suddenly, it thrusts forward, allowing whatever’s in your mouth to flow up into your nasal cavities and immediately fly out of your nostrils to the delight of everyone around you.
- Oropharynx: The middle part of your throat, frequently called “the back of the throat.” It extends from the uvula to the level of the hyoid bone. It’s the location of the epiglottis, a cartilage structure that guides materials passing though the mouth to the trachea or esophagus, as appropriate. It’s why your food comes close to your windpipe but rarely goes in. We mention the special characteristics of the hyoid bone in Chapter 5. We describe the esophagus, part of the digestive tract, in Chapter 11.
-
Laryngopharynx: The lower part of your throat adjacent to your larynx. The larynx (or voice box) is triangular. At the apex of the triangle is thyroid cartilage, commonly known as your “Adam’s apple.” If you could look down your throat onto the top of your larynx, you’d see your glottis, the opening through which air passes. When you swallow, a flap of tissue called your epiglottis covers your glottis and blocks food from getting into your larynx.
Inside your larynx are the vocal cords — gathered mucous membranes that cover ligaments. Your vocal cords vibrate when air passes over them, producing sound waves. Pushing more air over them increases the vibration’s amplitude, making the sound louder. When you tighten your vocal cords, the glottis narrows, and your voice has a higher pitch.
Trachea
Your trachea (windpipe) is a tube that runs from your larynx to just above your lungs. Just behind your sternum, your trachea divides into two large branches called primary bronchi (singular, bronchus) that enter each lung.
The trachea and bronchi are made of epithelial tissue, as well as smooth muscle and cartilage, which allow the airways to constrict and expand.
Lungs
Your lungs are large paired organs within your chest cavity on either side of your heart. They’re spongy and, like the heart, are protected by the rib cage. The lungs sit on top of the diaphragm, a powerful muscle that’s fixed to the lower ribs, sternum, and lumbar vertebrae. The heart sits in a depression between the lungs, called the cardiac notch.
The left lung is smaller than the right, to make room for the heart. Both lungs are separated into lobes (three on the right and two on the left). The lobes are further divided into segments and then into lobules, the smallest subdivision visible to the eye.
Pleural sac
Each lung is completely enclosed in the pleural sac. The pleural sac is similar to the pericardial sac in that it’s made up of two membranes, the parietal pleura, attached to the thoracic wall, and the visceral pleura, attached to the lung’s surface, with the pleural cavity between them. The pleural cavity contains a lubricating fluid called the intrapleural fluid.
The adhesive force of the fluid interface between the parietal pleura and the visceral pleura connects the lungs to the chest wall. In other words, the two membranes contain molecules that really like to “hold hands.” So when your chest rises as you inhale, the lungs expand with it and vice versa.
The intrapleural fluid completely surrounds the lungs. It keeps the pleural membranes moist and lubricated. Because of this fluid, the pleural cavity has a negative pressure (lower than atmospheric pressure), which keeps the lungs inflated.
The bronchial tree
After the primary bronchus enters the lung on each side, it splits into secondary and tertiary branches called bronchi. The tertiary bronchi divide into smaller branches called bronchioles, which transport air to the lobules. At the end of the smallest bronchioles are little structures that look like clusters of grapes; these are the alveolar sacs. The individual “grapes” are alveoli (singular alveolus). This is where the lungs interact with the blood vessels for gas exchange to occur.
 The lungs have a very large reserve volume relative to the oxygen exchange requirements when at rest. As a result, it’s possible to live many years with only one lung.
The lungs have a very large reserve volume relative to the oxygen exchange requirements when at rest. As a result, it’s possible to live many years with only one lung.
Diaphragm
The thoracic diaphragm is a dome-shaped sheet of muscle separating the base of the lungs from the liver, and, on the left side, from the stomach and the spleen. The diaphragm pushes up beneath the lungs to control their contraction and expansion during ventilation. The motor fibers in the phrenic nerves signal to the diaphragm when to contract and relax. The diaphragm can also exert pressure on the abdominal cavity, helping the expulsion of vomit, feces, or urine.
Breathing: Everybody’s Doing It
Breathing is essential to life, and thankfully, your body does it automatically. Air is alternately pulled into (inhaled) and pushed out of (exhaled) the lungs because of changes in pressure. When you inhale, your chest cavity expands, as do your lungs. This decreases the pressure inside the lungs, causing the air to flow through the bronchial tree and into the alveoli. When you exhale, the volume of the thoracic cavity decreases, which increases the pressure inside the lungs, forcing some air out (see Chapter 16). In the following sections, we take a look at how your body breathes under different conditions.
Normal breathing
When you’re sleeping, sitting still, and doing normal activity, your breathing rate is 12 to 20 inhalation/exhalation cycles per minute. Normal breathing (eupnea) is involuntary, which is why you never really forget to breathe, even when you’re sleeping. In many cases, breathing continues even during a coma. Impulses to the diaphragm come through a pair of spinal nerves, called the phrenic nerves. They initiate the regular, alternating contraction and relaxation of the diaphragm. The rhythm of the impulse is controlled by the autonomic system in the brain stem.
 While your respiration rate is involuntarily controlled by the respiratory center — the pons and medulla oblongata of your brainstem — you can also voluntarily control your breathing. The diaphragm is still triggered to contract, but the order originated from the cortex of the brain instead.
While your respiration rate is involuntarily controlled by the respiratory center — the pons and medulla oblongata of your brainstem — you can also voluntarily control your breathing. The diaphragm is still triggered to contract, but the order originated from the cortex of the brain instead.
Inspiration (breathing in) is the result of the diaphragm’s contraction. Seems backward, doesn’t it? When the diaphragm contracts, it pushes downward into the abdomen, creating more space in the thoracic cavity. The intercostal muscles (the muscles between the ribs) may also be stimulated to contract, helping to expand the lungs even more by pulling the ribs up and out. Air moves in at the top of the airway (through the nose or the mouth if necessary) and all the way down to take up the expanded space in the alveoli.
During normal breathing, expiration (breathing out) is a passive process requiring no energy or instruction. The brain simply stops sending impulses to the diaphragm, causing it to relax. As it settles back into position, the volume of the thoracic cavity decreases. Additionally, all the elastic tissue in the lungs recoils (think about stretching and then letting go of a rubber band). This increases the pressure in the lungs, forcing the air out through the respiratory tract (see Figure 10-1).
Breathing under stress
Keep in mind as you read this section that “stress” just means that an extra physiological demand is being placed. Stress isn’t necessarily negative — whether physical or emotional, stress can be painful or pleasurable, and is often both.
However much fun you are or are not having, stress increases metabolism. More oxygen is consumed, and more carbon dioxide is produced. An increase in carbon dioxide will decrease your pH, triggering chemoreceptor cells in the carotid arteries and aorta. Surprisingly, the amount of oxygen in your blood does little to influence your respiratory center.
Once your respiratory center is alerted, both inspiration and expiration become active processes. Your breathing is deeper and more frequent. The intercostal muscles contract more forcefully, and the pectoralis and sternocleidomastoid may also assist in the process. This decreases the pressure even more and air rushes in. During exhalation, the abdominal muscles will contract, forcing the diaphragm up and pushing out more air (so that a greater volume can be brought in with the next breath). These processes restore homeostasis and support the elevated metabolism.
 The forcible exhalation involved in coughing or sneezing is aided by the sudden contraction of the abdominal muscles, raising the abdominal pressure. The rapid increase in pressure pushes the relaxed diaphragm up against the pleural cavity, forcing air out of the lungs.
The forcible exhalation involved in coughing or sneezing is aided by the sudden contraction of the abdominal muscles, raising the abdominal pressure. The rapid increase in pressure pushes the relaxed diaphragm up against the pleural cavity, forcing air out of the lungs.
Controlled breathing
As far as has been determined, humans are the only animals who can bring their breathing under conscious control. Breathing also allows people to speak and sing, as well as moderate other physiological systems.
Holding your breath
You can stop breathing (hold your breath), at least for awhile, when unpleasant odors, noxious chemicals, or particulate matter is in the air around you, while you swim underwater, or just for the fun of it. The cerebral cortex sends signals to the rib muscles and the diaphragm that override the respiratory center signals — temporarily.
Holding your breath long enough to cause damage to your own brain from a lack of oxygen isn’t possible. So when a little kid says he’s going to hold his breath until you give him what he wants, you don’t need to worry. Metabolism and gas exchange continue as usual while you hold your breath. Carbon dioxide concentration increases in the blood. At a certain point, long before brain damage is even a possibility, the chemoreceptors that work with the respiratory center are stimulated to the point where they override the cerebral cortex. At the extreme, you lose consciousness. (The evolutionarily older brainstem puts the whippersnapper cerebral cortex into time out.) You exhale and the system rapidly returns to normal.
Speaking and singing
Speech requires breath control. The exhalation passes breath over the vocal cords, causing sound waves to be emitted, and the lips and tongue shape the sound waves into speech. The rate of exhalation is lower while you’re speaking, controlled by the diaphragm, the intercostal muscles, and the abdominal muscles. Singing requires even more breath control than speaking.
Controlling other systems
The relationship between the autonomic nervous system and the respiratory system appears to be two-way. For example, anxiety prompts hyperventilation, and hyperventilation produces symptoms of anxiety. Consciously controlling the rate and depth of breathing, mainly by achieving awareness and control of the diaphragm, has been demonstrated to decrease anxiety and sympathetic nervous system activation.
Controlled breathing is a feature of many religious, spiritual, and physical disciplines in all traditions. Clinical benefits have been demonstrated for meditation and controlled breathing in a wide variety of conditions of the neural, cardiovascular, and respiratory systems.
Gas Exchange
So, we’ve got the air in the lungs. How do we get the oxygen into the blood? This process is called gas exchange and occurs only at the alveoli.
The respiratory membrane
Each of the approximately 300 million alveoli is wrapped with capillaries, whose walls, like the alveoli’s walls, contain simple squamous epithelium. Because each wall is only one cell layer thick, this tissue is well suited for the exchange of materials. The interface of the simple squamous epithelium of an alveolus and the simple squamous epithelium of a pulmonary capillary (along with its supporting connective tissue) is called the respiratory membrane. That’s where gas exchange actually occurs. Check out the “Structures of the Respiratory Membrane” color plate in the center of the book for a diagrammatic look at this physiologically crucial interface.
The trade-off
The respiratory membrane is where blood is reoxygenated in the process of pulmonary circulation (see Chapter 9). The process of gas exchange at the respiratory membrane is almost exactly the same as the capillary exchange process (also described in Chapter 9). Here, it’s just reversed. There is more oxygen in the alveoli than in the blood, and because there are merely two layers of cells between them, the oxygen easily diffuses through.
 Though we think of the respiratory system as our means of obtaining oxygen, it’s important to remember that it serves a waste management function as well. The carbon dioxide created as waste during cellular respiration is carried around in the bloodstream. Because there is less of it in the alveoli, it diffuses in as the oxygen is coming out. When you exhale, the air in your lungs is forced out, carrying this waste out with it.
Though we think of the respiratory system as our means of obtaining oxygen, it’s important to remember that it serves a waste management function as well. The carbon dioxide created as waste during cellular respiration is carried around in the bloodstream. Because there is less of it in the alveoli, it diffuses in as the oxygen is coming out. When you exhale, the air in your lungs is forced out, carrying this waste out with it.
Study Figure 10-2 carefully to gain an understanding of the events of respiratory gas exchange.
 The driving force of diffusion is a concentration gradient; that is, the molecules naturally move to areas where there is less of them (if they are not blocked). With gases, concentration isn’t the proper measurement. Instead, it is partial pressure. In your textbook, when you see a comparison of “pO2,” there’s no need to let that complicate the matter. In this context, you may think of it as concentration.
The driving force of diffusion is a concentration gradient; that is, the molecules naturally move to areas where there is less of them (if they are not blocked). With gases, concentration isn’t the proper measurement. Instead, it is partial pressure. In your textbook, when you see a comparison of “pO2,” there’s no need to let that complicate the matter. In this context, you may think of it as concentration.
Pathophysiology of the Respiratory System
The structures of the airway and respiratory membrane are in constant contact with the air, with its constant threats of temperature extremes, desiccation (drying out), harmful chemicals and particles, and pathogens.
Hypoxemia
Fluctuations in oxygen concentration in tissues is part of normal physiology — for example, during times of increased demand such as strenuous exercise or emotional stress. In a healthy body, homeostatic mechanisms kick in rapidly and effectively when oxygen levels fall below the normal range.
Hypoxemia (low oxygen concentration in the arterial blood), however, is a respiratory system disorder resulting from any condition that interferes with gas exchange at the respiratory membrane, such as an obstructed (blocked) airway or alveolar scarring. Because all cells and tissues require an adequate oxygen supply to function optimally, hypoxemia harms all structures and inhibits all physiological processes to one extent or another.
A further complication of hypoxemia occurs when a low blood oxygen level stimulates the production of more red blood cells (RBCs). However, if iron is in short supply in the diet, which is a common condition worldwide, the body can’t make enough hemoglobin for all these RBCs, and many of them are dysfunctional, a condition called polycythemia. The blood is low in oxygen despite the excess of RBCs.
The other side of gas exchange is affected, too. Blood carbon dioxide levels rise, acidifying the blood and disrupting its normal function. Many enzymes, for example, are sensitive to pH.
Note: Don’t confuse hypoxemia with hypoxia. Hypoxemia can cause hypoxia, but they are technically not the same thing. Hypoxemia is low oxygen content in the blood (low supply), and hypoxia is low oxygen in the tissues.
Airway disorders
Airway disorders are similar in their local and systemic effects. Many are chronic and all lead to hypoxemia, which may be mild, moderate, or severe.
Asthma
Asthma is classified as a chronic disorder involving a “reactive airway.” This means that the airway (bronchi and bronchioles) becomes inflamed (swollen) or constricted in reaction to certain triggers. The bronchial tubes may spasm. The mucosa lining the tubes may secrete excess or very thick mucus. Any or all of these conditions make breathing difficult. Treatment often involves the use of an inhaler, which delivers a bronchodilator to the respiratory tract, decreasing the inflammation.
Asthma is most often developed and diagnosed in childhood. Signs and symptoms of mild asthma include periods of coughing, shortness of breath, or wheezing (a whistling sound while breathing). The symptoms are often brought on by exercise, but sometimes they occur without that trigger. The condition may progress to moderate asthma, with more frequent and severe bouts of shortness of breath, trouble breathing while resting, and an increased respiration rate, sometimes lasting several days. In severe asthma, respiratory distress brings hypoxemia. Asthma is a chronic condition and can be fatal.
Clinically, asthma is diagnosed as intrinsic (triggered by factors in the body) or extrinsic (triggered by factors from outside the body) and treated accordingly. Intrinsic asthma may set in after a severe respiratory tract infection. Other triggers include hormonal changes, emotional stress, and fatigue. Extrinsic asthma triggers are common irritants and allergens.
Bronchitis
Bronchitis is inflammation of the bronchi. Acute bronchitis may follow respiratory infection or exposure to irritating substances or cold temperatures. As a result, the body produces copious mucus, causing a persistent cough.
Chronic bronchitis is caused by long-term exposure to irritating substances, such as chemicals or cigarette smoke. The cilia of the respiratory mucosal cells are damaged and are less effective at cleaning the bronchial tissue of the respiratory mucus and the entrapped debris. Coughing develops to help the excretion of the mucus, but coughing irritates the bronchi further. The airway swells and constricts.
Lungs
In spite of all the respiratory system’s defenses, inhaled pathogens, chemicals, and particles find their way to the lung. Once there, they can be difficult to push out again.
Pneumonia
The lung is an extremely hospitable environment for bacterial, viral, and fungal microbes. Pneumonia is a pathogenic infection in the lower respiratory system that results in mucus and pus building up in the airway. Pneumonia is classified by the location and extent of the infection as bronchopneumonia, lobular pneumonia (affecting part of a lobe), or lobar pneumonia (affecting the entire lobe).
Pathogens enter the respiratory system easily in inhaled air. A healthy respiratory system working with the immune system can eliminate almost all of them. Macrophages (see Chapter 13) patrol the alveoli to look for pathogens that make it past the mucus traps and eliminate them. As the body ages, both respiratory tissue and immune system functionality decline. Before the arrival of effective antibiotics in the pharmacological arsenal, bacterial pneumonia was a common cause of death in the elderly. (It even had a nickname, “the old man’s friend,” implying that a relatively quick death by pneumonia was a blessing.)
Tuberculosis (TB)
Pulmonary tuberculosis is an infectious disease of the lungs caused by the bacterium Mycobacterium tuberculosis. The bacterium may infect the lung without symptoms for a period of several months to many years. The infection may spread to the bones and other organs. The long asymptomatic period, during which the infected person can infect others just by breathing, is what makes TB such a stubborn public health problem.
In tuberculosis, areas of bronchial and lung tissue become inflamed and die, leaving a hole in the tissue from which air can leak. Air leaking out from the lung causes the lung to collapse.
Due to its structure, M. tuberculosis evades efforts by the immune system to eliminate it. The immune system responds to its presence as it does for any infection: White blood cells and macrophages rush to the site of infection, and the macrophages engulf the bacterial cells and carry them to the lymph nodes (see Chapter 13). But the macrophages then behave oddly — they clump together, forming tubercles. Wherever the tubercles lodge, the surrounding tissue is killed, and scar tissue forms around the tubercle. Eventually, the lymph nodes become inflamed and may rupture, allowing the bacterium to spread to surrounding tissue. Because lymph nodes exist all over your body, TB can easily spread from your lungs to other areas.
Emphysema
Emphysema is a chronic obstructive pulmonary disorder (COPD). Commonly known as a smoker’s disease, emphysema can also affect people who have had long-term exposure to pulmonary irritants, such as chemicals, asbestos, or coal. Eventually, the cumulative damage to the bronchioles causes them to collapse, trapping air inside them. The pressure of the trapped air can rupture the tiny alveoli, destroying the respiratory membrane in that area. The destroyed tissue may be replaced with inelastic scar tissue (fibrosis). The elasticity of the lungs is decreased, making it hard for a person with emphysema to breathe (dyspnea). As the disease progresses, the delivery of oxygen to the blood is compromised, resulting in hypoxemia.
 Understanding what the respiratory system does
Understanding what the respiratory system does Checking out the parts of the respiratory system
Checking out the parts of the respiratory system Drawing in some breathing knowledge
Drawing in some breathing knowledge Looking at some common respiratory system ailments
Looking at some common respiratory system ailments Normally, the soft palate blocking the nasopharynx keeps food from going up into your nose. But when you’re laughing and eating or drinking at the same time, your soft palate gets confused. When you go to swallow, it starts to move back, but when you laugh suddenly, it thrusts forward, allowing whatever’s in your mouth to flow up into your nasal cavities and immediately fly out of your nostrils to the delight of everyone around you.
Normally, the soft palate blocking the nasopharynx keeps food from going up into your nose. But when you’re laughing and eating or drinking at the same time, your soft palate gets confused. When you go to swallow, it starts to move back, but when you laugh suddenly, it thrusts forward, allowing whatever’s in your mouth to flow up into your nasal cavities and immediately fly out of your nostrils to the delight of everyone around you.
 Though we think of the respiratory system as our means of obtaining oxygen, it’s important to remember that it serves a waste management function as well. The carbon dioxide created as waste during cellular respiration is carried around in the bloodstream. Because there is less of it in the alveoli, it diffuses in as the oxygen is coming out. When you exhale, the air in your lungs is forced out, carrying this waste out with it.
Though we think of the respiratory system as our means of obtaining oxygen, it’s important to remember that it serves a waste management function as well. The carbon dioxide created as waste during cellular respiration is carried around in the bloodstream. Because there is less of it in the alveoli, it diffuses in as the oxygen is coming out. When you exhale, the air in your lungs is forced out, carrying this waste out with it.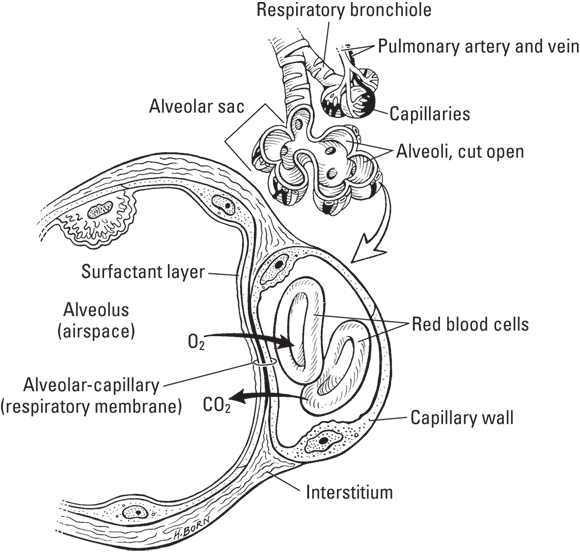
 The driving force of diffusion is a concentration gradient; that is, the molecules naturally move to areas where there is less of them (if they are not blocked). With gases, concentration isn’t the proper measurement. Instead, it is partial pressure. In your textbook, when you see a comparison of “pO2,” there’s no need to let that complicate the matter. In this context, you may think of it as concentration.
The driving force of diffusion is a concentration gradient; that is, the molecules naturally move to areas where there is less of them (if they are not blocked). With gases, concentration isn’t the proper measurement. Instead, it is partial pressure. In your textbook, when you see a comparison of “pO2,” there’s no need to let that complicate the matter. In this context, you may think of it as concentration.