![]()
![]()
![]()
![]()
![]()
![]()
![]()
Ductal carcinoma in situ (DCIS) is a common form of breast cancer — it accounts for about 1 in 5 breast cancers diagnosed each year. A diagnosis of DCIS can be confusing for some women. A woman with DCIS may be told that she has stage 0 cancer, but at the same time, she is likely to hear that she needs surgery to remove the cancer and, possibly, additional treatment.
Why such aggressive treatment for a stage 0 cancer? While it’s possible that, left untreated, the cancer may never leave the breast duct where it’s located, there’s also a possibility that it will. Unlike lobular carcinoma in situ (LCIS), discussed in Chapter 9, DCIS is more likely to develop into invasive cancer in the future.
The name ductal carcinoma in situ also causes confusion for some women. They’re not certain what in situ means. And because their doctors may use terms like DCIS and stage 0, they’re not certain if what they have is truly breast cancer.
The term in situ means located in it’s natural or normal place. In this case, it means the cancer remains within the breast duct where it originated. Other terms used to describe the condition include intraductal carcinoma or noninvasive carcinoma. Unlike LCIS, which is considered a risk marker for a later breast cancer, DCIS is generally viewed as early stage cancer.
However, what researchers still don’t know, and what they’re hoping to learn, is which women with DCIS are more likely to develop invasive or recurrent breast cancer. By knowing those women most at risk, doctors could tailor treatment accordingly.
DCIS is usually found during mammogram screenings, but it can be difficult to detect. On mammograms, DCIS is often characterized by the presence of tiny groups of calcium deposits called microcalcifications. In some cases, a mass can actually be felt (palpated).
Because of increased mammography screening, the rate at which DCIS is diagnosed has increased dramatically in recent years. DCIS is typically diagnosed either with a core needle biopsy, a procedure that uses a needle to remove a small sample of tissue for examination, or by way of an open excisional biopsy, which involves a small surgical incision to remove a tissue sample. These biopsy procedures are discussed in more detail in Chapter 8.
Fortunately, the prognosis for women treated for DCIS is very good. According to most reports in medical journals, the survival rate is now approaching 100 percent. Different treatment options are available. Ideally, the therapy chosen should be one that neither overtreats, nor undertreats, the condition.
Ductal carcinoma in situ
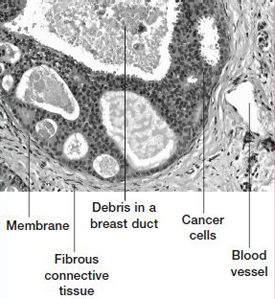
This slide shows a large duct in the center that’s expanded by layers of cancer cells. Debris from dying cells is present in the duct. Most importantly, the membrane around the duct is intact — there’s no invasion into surrounding tissue.
Several factors may influence the behavior or aggressiveness of DCIS, although the precise effect of each factor is still being studied. Treatment for each DCIS is generally based on the following factors:
Cell structure. Two major subtypes of DCIS are distinguished by the structure of their cells. One type is characterized by large, atypical cells with a central area of dead or degenerating cells (comedo necrosis). The other type is characterized by the lack of these qualities. The presence of comedo necrosis generally signifies a more aggressive DCIS. Tumors with comedo necrosis have a higher rate of recurrence than do DCIS tumors without comedo necrosis.
Women who have high-grade DCIS with comedo necrosis may be advised to have a procedure called sentinel node biopsy (see Chapter 11). This procedure is also sometimes done in women with DCIS who don’t have comedo necorsis.
In a sentinel node biopsy, the lymph nodes to which the cancer would most likely spread first are examined for the presence of cancer cells. Because DCIS with comedo necrosis has a higher risk of invasion than do other types of DCIS, studying the sentinel lymph nodes is a way to double-check for any cancer spread to the lymph nodes. If no cancer is found, chances are the cancer is still confined to the breast.
Three treatment options are generally considered in women with ductal carcinoma in situ:
Surgery
When a woman is diagnosed with DCIS, generally one of the first decisions she has to make is whether to treat the condition with a mastectomy or lumpectomy.
Mastectomy
Mastectomy is the medical term for surgical removal of the entire breast. For the treatment of DCIS, a simple (total) mastectomy is performed rather than a modified radical mastectomy. A simple mastectomy removes the breast tissue, skin, areola and nipple, but not underarm lymph nodes. A modified radical mastectomy removes all these components, including underarm lymph nodes.
Before mammograms were widely used to screen for breast cancer, DCIS was often detected later, when the mass was larger. Because of the size of the tumor, a simple mastectomy was the standard treatment. With regular mammography screening, doctors began identifying cancer earlier. This, combined with greater use of lumpectomy, made mastectomies less common. In some situations, though, mastectomy may be preferable to a lumpectomy:
Breast reconstruction is almost always an option after a mastectomy. It can be done during the same surgery or at a later time. See Chapter 12 to find out more about breast reconstruction.
≈≈≈≈≈≈≈
Exactly when does ductal carcinoma in situ become invasive cancer? Sometimes, it can be hard to tell. There’s a continuum of change that occurs at the cellular level between DCIS and a diagnosis of invasive cancer. At times it can be difficult for a pathologist to determine whether a particular breast tumor is a noninvasive cancer or an invasive one.
Some breast tumors labeled as DCIS show some evidence of microinvasion — the beginnings of invasive cancer. In these situations, a surgeon will likely recommend a sentinel node biopsy to provide better assurance that the cancer hasn’t spread to the lymph nodes under the arm.
≈≈≈≈≈≈≈
Lumpectomy
Lumpectomy, also known as breast-conserving therapy, removes only a portion of tissue from your breast. The procedure allows you to keep as much of your breast as possible and, depending on the amount of tissue removed, usually eliminates the need for reconstructive surgery.
When lumpectomy combined with radiation became an accepted treatment for invasive breast cancer, doctors questioned the use of mastectomy for less aggressive conditions such as DCIS. Researchers studied lumpectomy as a potential treatment for DCIS, leading to its widespread use today. Lumpectomy followed by radiation therapy is the most common treatment for DCIS. Although no study has officially compared lumpectomy with removal of the entire breast (mastectomy) for the treatment of DCIS, research suggests that lumpectomy combined with radiation produces survival rates similar to those of mastectomy. Most women with DCIS are candidates for lumpectomy although, as just discussed, in some situations mastectomy may be preferred.
For DCIS, a lumpectomy generally doesn’t involve removal of lymph nodes from under the arm because this is a noninvasive cancer and the chance of finding cancer in the lymph nodes is exceedingly small. However, a surgeon may recommend a sentinel node biopsy if there’s a large area of DCIS, the area is a mass that can be felt, or the biopsy suggests possible spread. Chapter 11 discusses lumpectomy and lymph node removal in more detail.
Radiation therapy
Radiation therapy after lumpectomy reduces the chance that DCIS will come back or progress to invasive cancer. This was illustrated by a study that randomly assigned women with DCIS to receive either lumpectomy alone or lumpectomy with radiation. After an average follow-up of 15 years, researchers found that women who underwent radiation had less risk of recurrent DCIS and invasive breast cancer in the affected breast (see the table below).
Some doctors have suggested that in the study just mentioned, the amount of normal breast tissue removed with the DCIS tissue may not have been large enough to assure that all the DCIS was removed, leading to the higher risk of recurrence in the lumpectomy alone group. They contend that if larger areas of normal tissue are removed, radiation therapy might not be needed. Nonetheless, this study forms the basis for why radiation therapy is recommended for most women with DCIS who have a lumpectomy.
Radiation therapy uses high-energy X-rays to kill cancer cells or damage them to the point where they lose their ability to grow and divide. Cells that grow out of control, such as cancer cells, are more vulnerable to the effects of radiation than are normal cells and thus are more likely to be damaged.
The two basic types of radiation therapy are external radiation and internal radiation. For treatment of DCIS, external radiation therapy is most commonly used. See Chapter 11 for more information on radiation therapy.
| Risk of recurrent DCIS and invasive cancer in the same breast |
|||
| Lumpectomy alone | Lumpectomy plus radiation | ||
| Recurrent DCIS | 15% | 9% | |
| Invasive breast cancer | 20% | 11% | |
Source: Wapnir IL, Dignam JJ, Fisher B, et.al., Long-term outcomes of invasive ipsilateral breast cancer recurrences after lumpectomy in NSABP B-17 and B-24 randomized clinical trials for DCIS. J Natl Cancer Inst, 2011;103:478.
![]()
The stories that follow highlight three women diagnosed with DCIS and the choices each made regarding her treatment. Each of the women took a different treatment route, feeling it was the best choice in her particular situation.
Geraldine was 68 years old when she was diagnosed with DCIS. The diagnosis came at the same time she learned that she had some abnormal cells in her cervix. After a biopsy of her right breast, where a mammogram detected a small abnormality, she had a double surgery. Doctors removed abnormal tissue in her right breast with a lumpectomy, followed by removal of abnormal cells in her cervix.
After the surgery, Geraldine knew she had some decisions to make. One of them was whether to undergo radiation therapy to the remaining tissue in her right breast. Geraldine wanted to thoroughly study the matter before making a decision. After reviewing the medical literature, Geraldine decided that radiation therapy wasn’t for her. She decided to undergo monitoring every six months with mammography. She also has a Pap test regularly to monitor the health of her cervix.
Geraldine’s decision not to have radiation was based on several factors:
After weighing the risks versus the benefits, Geraldine felt, with the support of her doctors, that the advantages to be gained from radiation therapy weren’t significant enough to outweigh the disadvantages in her situation. Her children worried about her decision but they were supportive. As Geraldine likes to point out, it’s her life and she’s the one who has to live with her decisions.
Geraldine is quick to emphasize the need to make your own decision and not let others control your life. She continues to do well and sums up, “Do research, put your life in God’s hands and make a choice that’s good for you.”
Like Geraldine’s, Cathy’s DCIS was first detected on a routine mammogram. Cathy was 42 years old at the time. She had had a baseline mammogram at age 38 and thought it would be a good time to have another mammogram. A practicing radiologist, Cathy had ready access to the mammography suite and had her examination while a friend was working in the area. Before long, they were getting extra views of the affected breast. Cathy recognized new clusters of microcalcifications that didn’t appear either obviously benign or definitely malignant, but worrisome enough to warrant a biopsy.
A biopsy revealed DCIS with at least three areas of calcifications. Because of this, Cathy opted for a mastectomy. A sentinel node biopsy performed at the same time confirmed that the cancer hadn’t spread to the lymph system. This gave Cathy assurance that all the DCIS areas had been removed and that no cancer had spread to the lymph nodes. After a six-month follow-up mammogram and clinical exam of her other breast, she has returned to annual screening of her remaining breast.
Cathy decided against immediate reconstructive surgery in case additional treatment might be needed after her surgery. She wears a prosthesis and is keeping reconstruction as an option when her children are older.
Cathy continues to do well and her advice to other women is to regularly perform breast self-examinations and to have clinical examinations and mammograms on a regular basis.
Agnes was 72 years old when a biopsy revealed that she had DCIS. She was given the treatment option of a lumpectomy followed by radiation or a mastectomy. Agnes decided on a lumpectomy with radiation, and she also had a sentinel node biopsy to provide some assurance that the cancer hadn’t spread. Agnes’ surgery went smoothly, as did the follow-up radiation therapy. She had almost no side effects from her daily radiation sessions.
Standing by to offer Agnes support were two close friends and a sister-in-law with similar cancer experiences. One friend had been disease-free for eight years after undergoing a lumpectomy and radiation, a factor that helped Agnes make her decision.
Agnes has been satisfied with her decision. She also is doing well and she hopes that the future will continue to confirm that her decision was the right one.
![]()
Tamoxifen
Tamoxifen is a synthetic anti-estrogen hormone that’s been shown to be beneficial in the treatment of invasive breast cancer. It’s also used as a cancer prevention agent for women at high risk of breast cancer.
Due to this drug’s success in treating invasive breast cancer, doctors wanted to know if it might benefit women with DCIS. That question was addressed in a study called the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-24 trial. It involved approximately 1,800 women with DCIS who had undergone lumpectomies and radiation therapy. The women were randomly assigned to receive either tamoxifen or an inactive pill (placebo) for five years. The results of the study led to the Food and Drug Administration’s approval of tamoxifen as a treatment for DCIS.
Researchers wanted to know if women taking tamoxifen experienced reduced rates of recurrent DCIS and invasive breast cancer, compared with women taking a placebo.
The table at the end of this chapter shows 15-year follow-up results from the study. All breast cancer events — recurrent DCIS and invasive breast cancer in the same breast and the development of cancer in the opposite breast — decreased by 6 percent in women who received tamoxifen for five years compared with those who received a placebo. The most benefit from tamoxifen use was in the reduction of cancers in the opposite breast.
What the original study didn’t address, though, was whether hormone receptor status was an important factor in the study’s results. (See Chapters 8 and 11 for more on hormone receptor status.) A group of researchers went back and addressed this issue. They found that 70 percent of the women treated in this clinical trial had positive estrogen receptors in their biopsy specimens and these women benefited from taking tamoxifen, whereas women with negative estrogen receptors didn’t. As a result, hormone receptor status is a key factor in determining treatment.
For women who have a mastectomy, there’s less reason to use tamoxifen. With a mastectomy, the risk of invasive breast cancer or DCIS in the small amount of remaining breast tissue is almost zero. Any potential benefit from tamoxifen would apply only to the opposite breast.
The bottom line is that tamoxifen is a treatment option to be considered among women with DCIS. However, for some women, it may not provide much benefit. Discuss the pros and cons of tamoxifen with your doctor. For more information on tamoxifen, see Chapter 11.
Because not all DCIS is the same, it’s important to consider treatment options in the context of your own situation and to make a decision that you feel comfortable with.
If you’re trying to decide whether to have a lumpectomy or a mastectomy, Chapter 11 contains a list of several questions to ask yourself that may help you. If you’re deciding whether to have radiation therapy after a lumpectomy, discuss the benefits and risks with your doctor.
Finally, if you haven’t already, read the stories of three women with DCIS. Each of the women made a different choice regarding her treatment, based on her individual circumstances.
| Tamoxifen vs. a placebo: A 15-year follow-up of women with DCIS |
|||
| Issue | Placebo group | Tamoxifen group | |
| All breast cancers | 29% | 23% | |
| Cancer in the same breast as the original tumor | |||
| All cancers DCIS Invasive |
18% 8.3% 10% |
16% 7.5% 9% |
|
| Cancer in the opposite breast All cancers |
11% |
7% |
|
| Deaths Breast cancer All causes |
2.7% 2.3% |
17% 14% |
|
Modified from Wapnir IL, Dignam JJ, Fisher B, et.al., Long-term outcomes of invasive ipsilateral breast cancer recurrences after lumpectomy in NSABP B-17 and B-24 randomized clinical trials for DCIS. J Natl Cancer Inst, 2011;103:478.