 Serious debilitating illness (such as heart or kidney disease, or severe anemia), or extreme underweight (your body needs fat stores to produce milk)—though some women do manage to overcome these obstacles and breastfeed their babies.
Serious debilitating illness (such as heart or kidney disease, or severe anemia), or extreme underweight (your body needs fat stores to produce milk)—though some women do manage to overcome these obstacles and breastfeed their babies.After nearly nine months of waiting, there’s finally a light at the end of the tunnel (perhaps, even, effacement and dilatation at the end of the cervix). But with just weeks to go before D day, have you come to terms with your baby coming to term? Will you be ready for your baby’s arrival when he or she is ready to arrive?
Even former Scouts will find there’s no way to be completely prepared for the time when baby makes three (or more). But there are a myriad of steps that can be taken to make the transition a smoother one—from selecting the right baby name to selecting the right doctor, from deciding between breast and bottle to deciding between cloth diapers and disposables, from psyching yourself up for the changes the new arrival will bring to preparing the family dog. The flurry of activity as you attempt to get ready and set may occasionally seem frenzied, but you’ll find it good preparation for the even more hectic pace that awaits you after baby’s born.
Perhaps there’s never been a question for you. When you close your eyes and summon up a daydreamed snapshot of life with baby, you clearly see yourself suckling your precious bundle at the breast or, just as clearly, cuddling your newborn as he or she takes a bottle. Whatever your reasons—practical, emotional, or medical—your mind was made up about baby feeding early in pregnancy, perhaps even before conception.
Or maybe that snapshot isn’t quite so well focused. Maybe you can’t exactly see yourself breastfeeding, but you’ve heard so much about how breast milk is better for baby that you can’t see yourself bottle feeding either. Or maybe you’d really like to give breastfeeding a try but fear that it won’t mix well with working, or with sleeping, or with romance. Or maybe it’s your spouse’s mixed feelings—or a friend’s, or your mother’s—that are giving you second thoughts.
No matter what’s causing your indecision, or your ambivalence, or your confusion about the right baby-feeding method for you, the best way to bring that fuzzy picture into focus is to explore the facts, as well as your feelings. First of all, what are the facts?
No matter how far technology advances, there will always be some things that nature does better. Among them: formulate the best food and best food delivery system for babies—a system that is at the same time good for mothers. As Oliver Wendell Holmes Senior said well over a century ago, “A pair of substantial mammary glands has the advantage over the two hemispheres of the most learned professor’s brain in the art of compounding a nutritious fluid for infants.” Today, pediatricians, obstetricians, nurse-midwives, even manufacturers of infant formula concur: Under most circumstances, breast is best by far. Here are just some of the reasons why:
It’s custom-made. Tailored to the needs of human infants, breast milk contains at least 100 ingredients that are not found in cow’s milk and that can’t be synthesized in the laboratory. Moreover, unlike formula, the composition of breast milk changes constantly to meet a baby’s ever-changing needs: It’s different in the morning than it is in the late afternoon; different at the beginning of a feeding than at the end; different the first month than the seventh; different for a premature baby than for a term baby. The nutrients in breast milk are matched to an infant’s needs and his or her ability to handle them. For example, breast milk contains less sodium than cow’s milk formula, making it easier for a baby’s kidneys to handle.
It goes down easily. Breast milk is designed for a human baby’s sensitive and still-developing digestive system, rather than for a young calf’s. Its protein (mostly lactalbumin) and its fat are more easily handled by the baby than are the protein (mostly caseinogen) and fat in cow’s milk. Infants also have an easier time absorbing the important micronutrients in breast milk than those in cow’s milk (in which, again, nutrients are designed to be absorbed by the young calf). The practical result: Breastfed babies may be less likely to suffer from gas and excessive spitting up.
It’s safe. You can be sure that the milk served up from your breasts isn’t improperly prepared, spoiled, or contaminated (assuming that you don’t have an illness that would make breastfeeding unsafe for baby; few illnesses do).
It keeps allergies on hold. Babies are almost never allergic to breast milk. Though an infant may be sensitive to something a mother has eaten that has passed into her milk, breast milk itself is virtually always tolerated well. On the other hand, more than one out of ten infants, after an initial exposure, turn out to be allergic to cow’s milk formula. (A switch to a soy or hydrolysate formula usually solves the problem—though such formulas stray even farther from the composition of human milk than cow’s milk formula.1) Some studies also show that breastfed babies may be less likely to get childhood asthma and eczema than those babies fed formula.
It’s a tummy soother. Because of breast milk’s naturally laxative effect and because of the easier digestibility of breast milk, infants who nurse are almost never constipated. Also, though their movements are normally very loose, diarrhea is rarely a problem. In fact, breast milk appears to reduce the risk of digestive upset both by destroying harmful micro-organisms and by encouraging the growth of beneficial ones.
It keeps diaper rash away. The breastfed baby’s sweet-smelling movements are less likely to cause diaper rash, though this advantage (as well as the less objectionable odor) disappears once solids are introduced.
It’s an infection preventer. From the first time to the last time infants suckle at their mothers’ breasts, they get a healthy dose of antibodies to bolster their immunity to disease. In general, they will come down with fewer colds, ear infections, lower respiratory tract infections, urinary tract infections, and other illnesses than bottle-fed infants, and when they do, they will usually recover more quickly and with fewer complications. Breastfeeding also improves the immune response to immunizations for most diseases (such as tetanus, diphtheria, and polio). Plus, it may offer some protection against Sudden Infant Death Syndrome (SIDS).
It’s a fat flattener. Breastfed infants are often less chubby than their bottle-fed peers. That is, in part, because Breastfeeding puts baby’s appetite in charge of consumption. A breastfed baby is likely to stop when satiated, while a bottle-fed infant may be urged to continue sucking until the bottle’s emptied. In addition, breast milk is actually calorie controlled. The hindmilk (the milk a baby gets at the end of a nursing session) is higher in calories than the milk at the beginning and tends to make a baby feel full—a signal to stop sucking. Though all the research results aren’t in yet, it has also been suggested that the fat-defeating benefits of breastfeeding continue later in life. Some studies show that children who are mostly breastfed as infants are less likely to be overweight as teenagers than their formula-fed peers and that the longer an infant was breastfed, the less likely he or she is to be overweight (though more study needs to be done). Another potential health plus for nursers: Breastfeeding may be linked to lower cholesterol levels and lower blood pressure later in life.
It’s a brain booster. Breastfeeding appears to slightly increase a child’s IQ, at least through age fifteen, and possibly into adulthood. This may be related not only to the brain-building fatty acids (DHA) in breast milk but also to the closeness and mother-baby interaction that is built into breastfeeding, which possibly fosters intellectual development.
More sucking satisfaction. A baby can continue sucking at a nearly empty breast once a feeding is over. This nonnutritive sucking comes in especially handy if baby is distressed and needs to be calmed down. An empty bottle does not allow for continued sucking.
It builds stronger mouths. Mother’s nipples and baby’s mouth are a perfect match (though it often doesn’t seem so the first time mother and baby try to work together). Even the most scientifically designed artificial nipple fails to give a baby’s jaws, gums, teeth, and palate the workout he or she would get at mother’s breast—a workout that ensures optimum oral development and some perks for baby’s future teeth. Babies who are breastfed are less likely to get cavities later on in childhood.
There are also breastfeeding benefits for the mother (and father):
Convenience. Breast milk is the ultimate convenience food, always in stock, ready to use, clean, and consistently at the perfect temperature. No formula to run out of, shop for, or lug around, no bottles to clean or refill, no powders to mix, no feedings to warm. Wherever you are—in bed, on the road, at a restaurant, on the beach—all the nourishment your baby needs is always ready and waiting. Should baby and mother be apart for the night, the day, or even the weekend, breast milk can be expressed in advance and stored in the refrigerator or freezer for bottle feedings.
Lower cost. Breast milk is free, whereas bottle feeding can be an expensive proposition. With breastfeeding, there are no bottles or formula to buy; there are no half-emptied bottles or opened cans of formula to waste. There is also a savings in terms of health care costs. Whether you are paying, or your health care insurer is, the cost of treating additional illnesses that the average formula-fed baby is more susceptible to can add up.
Quicker postpartum recovery. All your motivations for breastfeeding don’t have to be selfless ones. Because breastfeeding is part of the natural cycle of pregnancy-childbirth-mothering, it is designed to be better not just for baby but for you as well. It will help your uterus shrink back to prepregnancy size more quickly (that’s the increased cramping you’ll likely feel during the first postpartum days as your baby suckles), which in turn will reduce your flow of lochia (the postpartum discharge) more rapidly, which means less blood loss. And it will help you shed leftover pregnancy pounds by burning upward of 500 extra calories a day. Some of those pounds were laid down in the form of fat reserves especially to help you produce milk; now’s your chance to use them.
Some protection against pregnancy. Ovulation and menstruation are suppressed in most (though not all) nursing mothers at least until their babies begin to take significant supplementation (whether in the form of formula or solids), often until weaning, and sometimes for several months afterward. (Which doesn’t mean that you can’t become pregnant. Since ovulation can quietly precede your first postpartum period, you can never be certain as to when the protection you’ve been receiving from breastfeeding will stop. See page 692 for more on birth control.)
Health Benefits. Plenty of perks here: Women who breastfeed have a slightly lower risk of developing uterine cancer, ovarian cancer, and premenopausal breast cancer. They’re also less likely to develop rheumatoid arthritis than women who don’t breastfeed. Plus, women who nurse have a lower risk of developing osteoporosis later in life than women who have never breastfed.
Enforced rest periods. Breastfeeding ensures frequent breaks in your day, especially at first (sometimes more frequent than you’d like). Whether or not you feel you have the time to relax, your postpartum body needs the time off your feet that breastfeeding forces you to take.
Less complicated nighttime feedings. Even parents who can’t get enough of their adorable infants during the day don’t always look forward to seeing them at 2 A.M. (or at any other time between midnight and dawn). But baby’s nighttime waking can be a lot easier to take when comfort is as close as your breasts, instead of far off in the refrigerator, needing to be poured into a bottle. (It’s even easier on mom if dad completes the transfer of baby from crib to breast and back again.)
Eventually, easier multitasking. Once you become proficient at nursing—and master the one-arm maneuver—you’ll find that you can nurse and do just about anything else at the same time—page through a magazine, check your e-mail, or read your toddler a favorite book. (Just make sure that you spend plenty of nursing time interacting with your baby, too.)
MYTH: You can’t breastfeed if you have small breasts or flat nipples.
Reality: In no way does outward appearance affect the production of milk or a mother’s ability to dispense it. Breasts and nipples of all shapes and sizes can satisfy a hungry baby. Inverted nipples that don’t become erect when stimulated don’t even usually need any preparation to make them fully functional; see page 28.
MYTH: Breastfeeding is a lot of trouble.
Reality: Never again will it be so easy to feed your children (once you get the hang of it). Breasts, unlike bottles, are ready when baby is. You don’t have to remember to take them with you when you’re planning a day at the beach, lug them in a diaper bag, or worry about the milk inside them spoiling in the hot sun.
MYTH: Breastfeeding ties you down.
Reality: It’s true that breastfeeding is naturally better suited to mothers who plan to be with their babies most of the time. But those who are willing to make the effort to express and store milk, or who prefer to supplement with formula, can satisfy both their need to work—or see a movie, or go to an all-day seminar—and their desire to breastfeed. And when it comes to stepping out with baby, it’s the breastfeeding mother who is more mobile, always having an ample supply of food along no matter where she goes or how long she plans to stay.
MYTH: Breastfeeding will ruin your breasts.
Reality: Much to the surprise of many people, it’s not breastfeeding that affects the shape or size of your breasts but rather pregnancy itself. During pregnancy, your breasts prepare for lactation, even if you don’t end up nursing—and these changes are sometimes permanent. Excessive weight gain during pregnancy, hereditary factors, age, or poor support (going braless) can also result in breasts that are less firm. Breastfeeding is blame free.
MYTH: Breastfeeding didn’t work the first time so it won’t work again.
Reality: Even if you had trouble Breastfeeding your first baby, research shows that you’ll likely produce more milk and have an easier time breastfeeding the second time around. The adage “If at first you don’t succeed, try, try again” emphatically applies to nursing.
MYTH: Breastfeeding excludes dad.
Reality: A father who wants to be involved in the care of his nursing infant can find ample opportunity—for bathing, diapering, holding, rocking, playing with, bottle feeding with expressed milk or supplemental formula, and, once solids are introduced, spooning those “trains into the tunnel.”
Strong mother-baby bond. As almost any mother who’s ever breastfed will tell you, the breastfeeding benefit you’re likely to treasure most is the bond it nurtures between mother and child. There’s skin-to-skin and eye-to-eye contact, and the opportunity to cuddle, baby-babble, and coo built right into the breastfeeding experience. True, you can enjoy the same pleasures when bottle feeding, but it takes more of a conscious effort (see page 110), since you may frequently be faced with the temptation to relegate the feeding to others when you’re tired, for example, or to prop the bottle when you’re busy. Another benefit for breastfeeding moms: Research suggests that women who breastfeed are somewhat less likely to suffer from postpartum depression.
If there were no advantages to bottle feeding, no one who was able to breastfeed would ever turn to formula. But there are some very real advantages, and for some mothers (and some fathers) they are compelling, even in light of breastfeeding’s many benefits:
Longer satisfaction for baby. Infant formula made from cow’s milk is more difficult to digest than breast milk, and the large rubbery curds it forms stay in a baby’s stomach longer, giving a feeling of satiety that can last several hours, extending the period between feedings to three or four hours even early on. Because breast milk is easily and quickly digested, on the other hand, many nursing newborns feed so often that it sometimes seems as though they’re permanently attached to their mothers’ breasts. Though this frequent nursing serves a practical purpose—it stimulates the production of milk and improves the supply—it can be time-consuming for mom.
Easy monitoring of intake. You know just how much a bottle-fed baby is taking. Because breasts aren’t calibrated to measure baby’s intake, a nursing mother may worry that her newborn isn’t getting enough to eat (though that’s rarely the case—especially once nursing is established—since breastfed babies tend to eat as much as they need). The bottle-feeding mother has no such problem—a glance at the bottle tells her exactly what she wants to know. (This can be a disadvantage, however, if anxious parents push babies to take more than they want.)
More freedom. Formula feeding doesn’t tie the mother to baby day and night. Want to take in dinner and a show with your spouse? Or even get away for a romantic weekend? A grandparent or a baby-sitter can stand in. Intend to go back to work when the baby is three months old? No weaning or expressing breast milk will be necessary—just a daily supply of bottles and formula for the childcare provider to use to feed your baby. (Of course, these options are also open to breastfeeding moms who express milk or supplement with formula.)
Fewer demands. The woman exhausted by a difficult labor may be grateful to have the option of sleeping through middle-of-the-night or crack-of-dawn feedings. Dad, grandma (if she’s come to stay), a baby nurse, a doula, or anyone else on hand can take over those honors. There’s also less of a physical drain on a newly delivered mother’s resources if she doesn’t have to add milk production to her many daily—and nightly—challenges.
More participation for father. Dads can share in the pleasures of baby feeding when baby is bottle fed in a way that’s impossible with the breastfed infant, unless you pump regularly or supplement with formula.
More participation for older siblings. An older child will feel very much involved in taking care of his or her “new baby” when giving a bottle. (Again, this option is also open to breastfeeders who supplement with expressed milk or formula.)
No interference with fashion. A bottle-feeding mother can dress as she pleases. The nursing mother’s wardrobe is not quite as limited as it was when she was pregnant, but most of the time she won’t be able to put fashion before practicality. She’ll have to forgo one-piece dresses that don’t button up the front. (Try accommodating a hungry baby by lifting your dress over your waist and you’ll see why.)
Less restriction on birth control methods. A breastfeeding mother has to limit her choice of contraception to those methods that are safe during lactation (but there are many; see page 692). The formula-feeding mom has no such restrictions.
Fewer dietary demands and restrictions. A formula-feeding mother can stop eating for two. Unlike the nursing mom, she can give up the extra protein and calcium, and she can forget about her prenatal vitamin supplements. She can have a few drinks at a party, take prescription medicine, eat all the spicy foods and cabbage she wants (though many babies won’t object to these tastes in breast milk), without worrying about the possible effect on her baby. After the first six weeks postpartum (but not before, when her body is still in the recovery phase), she can diet somewhat more strenuously to take off any pregnancy weight that lingers. This is something that the Breastfeeding mother can’t do until baby is weaned—though, because of the calories milk production requires, she may not have to diet at all to reach her goal.
Less embarrassment for the modest. While the nursing mother may receive curious (or unfortunately, sometimes glaring) glances when she chooses to breastfeed in public, no one will look twice or askance at a woman bottle feeding her baby. Neither will the bottle-feeding mother need to worry about the sometimes awkward procedure of redressing (refastening bra flaps, retucking in shirts, rebuttoning buttons) after the feeding is done. (These hang-ups, though, are often quickly hung up; many women who opt to try to breastfeed soon find it becomes second nature—even in crowded restaurants.)
Potentially, more lovemaking. After months of making love under somewhat less than ideal conditions, many couples look forward to picking up where they left off before conception. For some breastfeeding women, a vagina left dry by the hormonal changes of lactation, teamed with sore nipples and leaky breasts, can make lovemaking a challenge. For the bottle-feeding mother, once she’s recovered from delivery, nothing (except for an unexpectedly awake and crying baby) need stand between her and her mate.
The facts are before you; you’ve read them and reread them, considered them and reconsidered them. And yet perhaps you’re still left undecided. That’s because, as with many other decisions you’re making these days, the decision between breast and formula doesn’t depend just on facts. It also depends on feelings.
Do you feel that you really want to breastfeed but believe it’s impractical because you’re planning to go back to work soon after your baby is born? Don’t let circumstances deprive you and your baby of the experience. A few weeks of nursing are better than none at all; both of you stand to benefit from even the briefest encounter with it. And with a little extra dedication and planning (okay, maybe a lot of extra dedication and planning), you should be able to work out a system for continuing to breastfeed even after you’ve returned to your job (see page 250).
Do you feel fundamentally negative about breastfeeding yet find the facts in favor of it too convincing to ignore? Here again, you might give nursing a try. If your feelings don’t take a shift toward the positive, you can quit. At least your baby will have reaped the benefits of breastfeeding for a short time (which is better than no time at all), and you’ll know that you tried, erasing those nagging doubts. (It’s best not to quit before you’ve given nursing your best shot, however. A really fair trial would last at least a month, or better six weeks, since for some women it could take that long to establish a good nursing relationship even under the best of circumstances.)
Do you feel fundamentally uncomfortable with—even averse to—the idea of breastfeeding? Or have you previously breastfed and not enjoyed it? Even under these circumstances, it would still be wise to seriously consider a six-week trial run, which will give your child some of the benefits of breastfeeding and give you a chance to put your feelings to the test. If after this attempt, you still feel Breastfeeding is not for you, you can turn to formula without regret.
Do you fear that you won’t be able to nurse because of a high-strung (can’t-sit-still) temperament, but agree that breast milk is best for baby? Again, you have nothing to lose by trying, and you have everything to gain should your personality turn out to be more compatible with breastfeeding than you thought. Don’t judge the situation too early in the game, however. Even women ordinarily graced with saintlike calm can find the first few weeks of breastfeeding (or motherhood, for that matter) a time of high anxiety. Many, however, are surprised to find that once a smoothly working breastfeeding relationship is established, nursing is stress-reducing rather than stress-producing—the hormones released as baby suckles actually enhance relaxation, and the experience itself is one of the healthiest routes to tension relief. (At the beginning, give yourself the best chance of success by unwinding with some relaxation techniques before nursing your newborn.) Keep in mind that you can always switch to formula later, should your initial instincts prove correct.
If dad feels jealous or unsettled at the thought of your breastfeeding, have him read the facts, too. They may persuade him that his loss (which, after all, is only a temporary one) or his distaste (which will also be temporary; once breastfeeding begins, most fathers find they watch in wonder) will be baby’s gain. Also show him the section on breastfeeding and fathers in chapter 24. It may help to bring in a pediatrician, family practitioner, or lactation consultant to reinforce the facts. Talking to other fathers whose babies have breastfed will also help him feel more comfortable, while contributing to your already compelling case. Keep in mind that his support is extremely important and worth winning over. Though you can certainly breastfeed without it, studies show that women who have the wholehearted support of their partners during breastfeeding are far more likely to stick with it.
No matter the reasons that bring them to breastfeeding, most women ultimately find it an overwhelmingly positive experience—joyful, exhilarating, and incomparably fulfilling (at least, once they and their babies get the hang of it). Even those women who begin to breastfeed out of duty often continue to do it because of the pleasure it brings them. Many who, before baby arrives, can’t imagine engaging in such an intimate act in the company of strangers live to eat their words and to lift their shirts at the sound of baby’s first cry—on an airplane, in a crowded park, at a restaurant.
In the end, however, if you opt not to breastfeed (with or without a trial run), don’t feel guilty. Almost nothing you do for your baby is right if it doesn’t feel right for you—and that includes Breastfeeding. Even babies who were born yesterday are wise enough to sense feelings of uneasiness in their mothers; a bottle given lovingly can be better for your infant than a breast offered grudgingly.
For some women, the pros and cons of breastfeeding and formula feeding are academic. They don’t have the option of nursing their new babies, either because of their own health or their baby’s. The most common maternal factors that may prevent or interfere with breastfeeding include:
 Serious debilitating illness (such as heart or kidney disease, or severe anemia), or extreme underweight (your body needs fat stores to produce milk)—though some women do manage to overcome these obstacles and breastfeed their babies.
Serious debilitating illness (such as heart or kidney disease, or severe anemia), or extreme underweight (your body needs fat stores to produce milk)—though some women do manage to overcome these obstacles and breastfeed their babies.
 Serious infection, such as active, untreated tuberculosis (after two weeks of treatment, breastfeeding should be okay); or AIDS or HIV infection, which can be transmitted via body fluids, including breast milk. You can nurse if you are infected with hepatitis A (after baby receives gamma globulin) or hepatitis B (after baby receives gamma globulin and the hepatitis B vaccine.)2
Serious infection, such as active, untreated tuberculosis (after two weeks of treatment, breastfeeding should be okay); or AIDS or HIV infection, which can be transmitted via body fluids, including breast milk. You can nurse if you are infected with hepatitis A (after baby receives gamma globulin) or hepatitis B (after baby receives gamma globulin and the hepatitis B vaccine.)2
 A condition requiring regular medication that passes into the breast milk and might be harmful to the baby, such as anticancer, some antithyroid, or antihypertensive drugs; lithium, tranquilizers, or sedatives. A temporary need for medications, such as penicillin, even at the time you begin nursing, should not interfere with breastfeeding. Women who need antibiotics during labor or because of a breast infection (mastitis) can continue to breastfeed while on the medication. Always check with baby’s doctor before starting a new medicine during lactation.
A condition requiring regular medication that passes into the breast milk and might be harmful to the baby, such as anticancer, some antithyroid, or antihypertensive drugs; lithium, tranquilizers, or sedatives. A temporary need for medications, such as penicillin, even at the time you begin nursing, should not interfere with breastfeeding. Women who need antibiotics during labor or because of a breast infection (mastitis) can continue to breastfeed while on the medication. Always check with baby’s doctor before starting a new medicine during lactation.
 Drug abuse—including the use of tranquilizers, amphetamines, barbiturates, or other pills, heroin, methadone, cocaine, marijuana, or the abuse of alcohol (an occasional drink is okay; see page 96).
Drug abuse—including the use of tranquilizers, amphetamines, barbiturates, or other pills, heroin, methadone, cocaine, marijuana, or the abuse of alcohol (an occasional drink is okay; see page 96).
 Exposure to certain toxic chemicals in the workplace. To determine whether you have been exposed to toxic chemicals in your workplace, check with the Occupational Safety and Health Administration (OSHA), 200 Constitution Avenue, NW, Washington, DC 20210; 202-693-1999, www.osha.gov.
Exposure to certain toxic chemicals in the workplace. To determine whether you have been exposed to toxic chemicals in your workplace, check with the Occupational Safety and Health Administration (OSHA), 200 Constitution Avenue, NW, Washington, DC 20210; 202-693-1999, www.osha.gov.
 Inadequate glandular tissue in the breasts (this has nothing to do with the size of your breasts) or damage to the nerve supply to the nipple (as from injury or surgery). In some cases you may be able to attempt Breastfeeding, but under careful medical supervision, to be certain your baby is thriving. If you’ve had surgery for breast cancer in one breast, ask your doctor about the possibility of nursing from the other.
Inadequate glandular tissue in the breasts (this has nothing to do with the size of your breasts) or damage to the nerve supply to the nipple (as from injury or surgery). In some cases you may be able to attempt Breastfeeding, but under careful medical supervision, to be certain your baby is thriving. If you’ve had surgery for breast cancer in one breast, ask your doctor about the possibility of nursing from the other.
Some conditions in the newborn may make breastfeeding difficult, but not impossible (with the right medical support). They include:
 A metabolic disorder, such as PKU or lactose intolerance, that makes the baby unable to digest both human and cow’s milk. Treatment for babies with PKU involves supplementing with a phenylalanine-free formula. Formula feedings can be combined with breastfeeding as long as blood levels are carefully monitored and the amount of breastfeeding is controlled. In the case of lactose intolerance (which is extremely rare in infancy), expressed mother’s milk can be treated with lactase to make it digestible.
A metabolic disorder, such as PKU or lactose intolerance, that makes the baby unable to digest both human and cow’s milk. Treatment for babies with PKU involves supplementing with a phenylalanine-free formula. Formula feedings can be combined with breastfeeding as long as blood levels are carefully monitored and the amount of breastfeeding is controlled. In the case of lactose intolerance (which is extremely rare in infancy), expressed mother’s milk can be treated with lactase to make it digestible.
Just because you haven’t given birth to your baby doesn’t necessarily mean that you can’t breastfeed. With plenty of advance planning and preparation, adopting mothers can sometimes successfully breastfeed their infants (though usually not without supplementation) if they get started within a few days after birth. See page 656 for tips on breastfeeding an adopted baby.
 Cleft lip and/or cleft palate that interferes with suckling at the breast. In some cases, especially when only cleft lip is present, it is possible to breastfeed. Using a special mouth appliance can allow a baby with a cleft palate to breastfeed. Ask to see a lactation consultant before you make a feeding decision. It may also be feasible to express breast milk until after surgery (usually performed during the first few weeks of life), and to begin breastfeeding then.
Cleft lip and/or cleft palate that interferes with suckling at the breast. In some cases, especially when only cleft lip is present, it is possible to breastfeed. Using a special mouth appliance can allow a baby with a cleft palate to breastfeed. Ask to see a lactation consultant before you make a feeding decision. It may also be feasible to express breast milk until after surgery (usually performed during the first few weeks of life), and to begin breastfeeding then.
If you can’t breastfeed, or if you just don’t wish to, be assured that a commercial baby formula will almost certainly nourish your baby adequately (rare exceptions would include infants with multiple allergies who require special formulas). Millions of healthy, happy babies (possibly, you among them) have been raised on the bottle, and your baby can be, too.
“Everything’s ready for the baby—except me. I just can’t picture myself as a mother.”
Even those women who pictured themselves as mothers from the first time they held a baby doll often start to doubt the validity of their calling when it threatens to become a round-the-clock reality. Those who spurned dolls for relationships with trucks and soccer balls, mowed lawns instead of baby-sitting, and rarely gave passing strollers more than a passing glance (until the day their pregnancy test came back positive) may face delivery day with even greater trepidation.
But not only is this ninth-month crumbling of confidence normal, it’s healthy. Strolling into motherhood (or parenthood, for that matter) blithely self-assured may only set you up for a swift and unsettling jolt of reality when the job turns out to be more overwhelming than you’d imagined—which it almost always is, at least at first.
Whether you’re still impatiently awaiting baby’s arrival, or you’ve just brought your brand-new bundle of joy home, you probably have almost as many questions about how to care for yourself in the postpartum period as you do about how to care for your newborn. Turn to chapter 23 for information on the first postpartum year.
So if you don’t feel ready for motherhood, don’t worry. But do prepare. Read at least the first few chapters in this book and everything else you can about newborns and infants (always keeping in mind that babies don’t always go “by the book”). Spend some time, if possible, with newborns or young babies; hold them, even diaper them as you get the scoop (and the poop) from their parents about the pleasures and challenges of caring for an infant. Taking a parenting course will also help prepare you for the toughest (and ultimately, the most fulfilling) job you’ll ever love. (All of this advice also applies for soon-to-be fathers approaching this new role with some trepidation.)
Most of all, realize that mothers (and fathers) are not born—they’re created on the job. A woman who’s gained some experience with other people’s infants may be somewhat more comfortable at first than the mother who’s a complete novice, but by the six-week checkup it will be difficult to tell them apart.
“I really look forward to having my baby. But I worry that the lifestyle my spouse and I have grown accustomed to will completely change.”
To be sure, diapers aren’t the only things that will be changing around your house once baby arrives. Most everything about your lifestyle—from your priorities to your attitudes, from your sleeping patterns to your eating patterns, from the way you spend your days and nights to the way you spend your weekends, from romance to finance—will change, at least to some degree. For instance, you may still be able to eat some lunches and dinners out (especially if you’re going back to work), but fewer of them may be at candlelit French bistros and more of them at family-style eateries with high chairs and a high tolerance for peas and carrots ground into the carpeting. Late nights in are likely to take the place of late nights out; breakfast in bed is likely to take on a whole new meaning (a 5 A.M. nursing session, rather than coffee, scones, and the weekend paper at 11); lovemaking is less likely to be inspired by passion than scheduled around baby’s nap (if it’s scheduled at all). Silk blouses and wool slacks will probably be tucked away in the back of the closet to make room for washables that can weather encounters with spit-up and leaky diapers; more movies will be seen on DVD than in theaters (and chances are once you do get back to the theater on a regular basis, it will be to catch the first runs of the latest animated blockbuster).
In other words, little babies make a big difference in how you live your life. But while every couple finds that their lifestyle changes somewhat once they become parents, just how much yours will change will depend on you, your spouse, and most of all, your baby. Some parents find they don’t miss their child-free lifestyles all that much; for the most part, cocooning as a cozy threesome suits them. Some parents find they don’t miss it as much as they thought, but also find they crave a little nightlife with their home life (in which case, regular Saturday-night baby-sitters can accommodate that craving). Some babies turn out to be more adaptable (which means they can be easily toted on evenings out and weekend excursions); others turn out to be slaves to their feeding and eating schedules (which means their parents will probably have to be, too).
So while the lifestyle changes are ones you’re better off preparing for now—at least emotionally—it’s hard to predict until parenthood is upon you how extensive yours will be and how you’ll feel about them. It helps to keep in mind that change, while always challenging, can be exciting, too. Though there’s no doubt your life will be different, there’s also no doubt that it will be—in so many ways—richer and better than ever. Just ask any parent.
As you read What to Expect the First Year, you’ll notice many references to traditional family relationships—to “wives,” “husbands,” “spouses.” These references are not meant to exclude mothers and fathers who are single, who have same-sex partners, or who have chosen not to marry their live-in partners. These terms are, rather, a way of avoiding phrases (for instance “your husband or significant other”) that may be more inclusive but also more cumbersome to read. Please mentally edit out any phrase that doesn’t fit and replace it with one that’s right for you and your situation.
“Every time I talk to a friend or read an article on the subject, I change my mind about whether or not to go back to work soon after my baby is born.”
Today’s expectant working woman has it all to look forward to: all the satisfaction of a fulfilling career, all the joy of raising a family—and all the guilt, anxiety, and confusion inherent in deciding which of the two will hold priority in her life after delivery.
But while it seems as though this is a choice you should make now, it really isn’t. Deciding, while you’re still pregnant, whether you’ll stay home or go back to work (and when) after baby is born is like choosing between a job you’re familiar with and one you know nothing about. Instead, assuming you have the options, keep them open until you’ve spent some time at home with your baby. You may find that nothing you’ve ever done—including your job—has ever given you as much satisfaction as caring for your newborn does, and you may postpone going back to work indefinitely. Or you may find that, as much as you enjoy being a mother, you’re not cut out for full-time parenting—you miss your career too much. Or you may find that you’d like to combine the best of both worlds by taking a part-time position, job sharing with another parent, or working from home full- or part-time. Keep in mind that there are no “right” decisions when it comes to this very personal question—only the decision that’s right for you. Remember, too, that you can always change your mind if the decision you think is right turns out to be all wrong. (See page 710 for some advice on making the decision once baby appears on the scene.)
There’s no better way for a fledgling family to get to know each other than by spending the first few weeks at home, undisturbed by work or other distracting obligations. It’s also the best way for new moms and dads to learn the ropes of the parenting business. And that’s why more and more fathers are joining the ranks of mothers who take advantage of the Family Medical Leave Act. The FMLA allows both moms and dads to spend up to twelve weeks with their newborn babies without having to dip into vacation time. The bad news is that not all employees qualify for FMLA (and that the time taken is usually unpaid); the good news is that some family-friendly companies offer even better plans for new parents. Check with your company, and see page 715 for more details.
“My mother has her bags packed and is ready to fly in ‘to give me a hand’ the moment the baby arrives. The idea makes me nervous because my mother tends to take over, but I don’t want to hurt her feelings and tell her not to come.”
Whether it’s loving and warm, distant and frosty, or tottering on the brink somewhere in between, a woman’s relationship with her mother (or mother-inlaw) is one of the most complicated in her life. It becomes even more so when daughter becomes mother, and mother becomes grandmother. Though there may be hundreds of times in the next couple of decades when your wishes will come into conflict with those of your parents, this may be the one situation that will set the precedent for those to come.
In other words, the timing of the first grandparents’ visit is one of the first decisions you’ll make as parents. You should base it, like most decisions you’ll make as parents, on what’s right for the two of you and for your new arrival. If you feel that yours is a threesome that wouldn’t benefit from company right now—particularly the kind of company that tends to bring a lot of baggage (and we’re not talking just suitcases)—then your decision should reflect this. Let your parents (and your in-laws, too, if necessary) know that you and your spouse need to spend some time alone with the baby before they pay their first visit. Explain that this time will allow you to become more comfortable in your new roles, to adjust to your new life, and to bond with your new family member. Assure them that their company and their help with the baby and around the house will be most welcome in a few weeks. Remind your mother, too, that the baby will be more responsive, more interesting, more awake, and more photogenic by then (sleeping babies all tend to look alike, anyway).
Your mother may feel a little hurt at first, even a little rejected or angry—and she may even deploy that not-so-secret maternal weapon, guilt. But don’t worry (and don’t cave in). Once she holds her grandchild in her arms, chances are all will be forgiven and forgotten. What won’t be forgotten is that you and your spouse are the ones who set the rules for your family, an important concept to relay to parents and in-laws early (particularly those with the tendency to take charge).
On the other hand, many new moms and dads feel an urge to renew or strengthen the bonds with their own parents during pregnancy and afterward. And some new parents welcome the experience, the extra sets of hands, and perhaps the hot dinners and vacuumed carpets that come with a postpartum visit from grandparents. Just as those who feel the need to say, “Mother, I’d rather do it myself,” shouldn’t be plagued by guilt, those who feel they need the help shouldn’t have qualms about saying, “I’d rather not do it myself.” The decision that’s right for you is the right decision to make.
“My in-laws have opinions on everything having to do with our baby and how we’re going to raise her—from feeding and sleeping schedules to whether I should go back to work. I love them, but how do I get them to butt out?”
It’s not an easy concept to grasp at first (though it does sink in eventually, usually in the middle of a 3 A.M. feeding or a four-hour colic bout): You are the parents now. It’s a job that comes with enormous pleasures, but also with enormous responsibilities. And one of the first responsibilities you’ll have is letting your in-laws know that you and your spouse are responsible for the care, feeding, and raising of your new daughter. The sooner you convey this message, the sooner everyone can start feeling comfortable in their new roles (you as parents, your in-laws as grandparents).
Say it early (and often, if necessary), say it firmly, but most of all, say it lovingly. Explain to your well-meaning but interfering in-laws that they did a great job of raising your spouse, and now it’s his turn and yours to be the parents. There will be times when you’ll welcome their advice (especially if grandma has cataloged somewhere in her vast reserves of experience a surefire trick for calming a crying newborn), but other times when you’ll want to learn from your pediatrician, your baby books, and your mistakes—much as they probably did. Explain, too, that not only is it important for you to set the rules (as they did when they first became parents), but that many of the rules have changed (babies are no longer put to sleep on their tummies or fed on a schedule) since they were in the parenting game, which is why their way of doing things may no longer be recommended. And don’t forget to say it with humor. Point out that chances are, the changing tables will turn once again when your daughter becomes a parent—and accuses you of dispensing old-fashioned advice.
That said, keep two things in mind. First, the wisdom that grandparents bring with them is invaluable. Whether you feel your parents (or your spouse’s) did a great job raising you or just a fair one, there is always something to be learned from their experience, even if it’s only what not to do. Though plenty of fine-tuning and refashioning is inevitably necessary, there’s no point in completely reinventing the wheel—or parenting practices—with every generation. And second, if parenthood is a responsibility, grandparenthood is the reward—one you will someday want to enjoy yourself. As you assert your independence as parents, be sure you don’t deprive your in-laws of their reward.
“My spouse’s parents are deceased. Mine are elderly and live in another state. I feel I have no family to talk to about my pregnancy and about the baby. I think it will be worse when she arrives.”
You’re not alone in feeling alone. While in generations past the extended family rarely extended beyond the county line (and often no farther than the house next door), millions of couples in today’s mobile society live hundreds or thousands of miles from parents and family. Never is this separation more keenly felt—on both sides—than when a new generation is being added.
Keeping in touch with your parents by phone, e-mail, videos, photos, and regular visits will help fill the gap between far-flung generations, and will also help your baby get to know her grandparents as she grows. But for the kind of emotional and practical support you’ll be craving after the baby’s born, and might otherwise get from your parents if they lived nearby, you’ll need to find surrogates. Parent groups, which sometimes evolve out of childbirth education or exercise classes, or simply develop spontaneously among casual acquaintances, can provide that kind of support (plus a plethora of swapped baby-care tips). So can places of worship, especially those with a strong sense of community and lots of young families. You might also consider spending time with a senior citizen (or senior couple) in your area who is far from his or her family, too, and misses the company of grandchildren as much as you miss the company of a grandparent. Weekly visits and joint outings can give you and your baby a sense of family, while giving your “adopted” grandparent or grandparents a sense of being needed—filling the void all around.
“Some of my friends hired baby nurses when their babies were born. Do I need one, too?”
If you’ve determined there’s enough money in your budget for a baby nurse (they don’t come cheap), you’ll need to consider several other factors before deciding whether or not to hire one. Here are some reasons why you might opt for the help:
 To get some hands-on training in baby care. If you haven’t had experience or taken a parenting class and feel you’d rather not learn from the mistakes you make on the job and on your baby, a good baby nurse will be able to instruct in such basics as bathing, burping, diapering, and even Breastfeeding. If this is your reason for hiring a nurse, however, be sure that the person you hire is as interested in teaching as you are in learning. Some won’t tolerate novice parents peeping over their shoulders; one with such a dictatorial take-charge attitude can leave you as inexperienced and unsure when she departs as you were when she arrived.
To get some hands-on training in baby care. If you haven’t had experience or taken a parenting class and feel you’d rather not learn from the mistakes you make on the job and on your baby, a good baby nurse will be able to instruct in such basics as bathing, burping, diapering, and even Breastfeeding. If this is your reason for hiring a nurse, however, be sure that the person you hire is as interested in teaching as you are in learning. Some won’t tolerate novice parents peeping over their shoulders; one with such a dictatorial take-charge attitude can leave you as inexperienced and unsure when she departs as you were when she arrived.
 To avoid getting up in the middle of the night for feedings. If you’re formula feeding and would rather sleep through the night, at least in the early weeks of postpartum fatigue, a baby nurse, on duty twenty-four hours a day or hired just for nights, can take over or share this feeding responsibility with you and your spouse.
To avoid getting up in the middle of the night for feedings. If you’re formula feeding and would rather sleep through the night, at least in the early weeks of postpartum fatigue, a baby nurse, on duty twenty-four hours a day or hired just for nights, can take over or share this feeding responsibility with you and your spouse.
 To spend more time with an older child. Some parents hire a baby nurse so that they can be more available to their older children, and hopefully spare them the pangs of jealousy that are often provoked by new arrivals. Such a nurse might be hired to work just a few hours a day during the time you want to spend with your older child. If this is your major reason for hiring a nurse, however, keep in mind that her presence will probably serve only to postpone feelings of sibling jealousy. See chapter 25 for sibling issues.
To spend more time with an older child. Some parents hire a baby nurse so that they can be more available to their older children, and hopefully spare them the pangs of jealousy that are often provoked by new arrivals. Such a nurse might be hired to work just a few hours a day during the time you want to spend with your older child. If this is your major reason for hiring a nurse, however, keep in mind that her presence will probably serve only to postpone feelings of sibling jealousy. See chapter 25 for sibling issues.
 To give yourself a chance to recuperate after a cesarean or difficult vaginal birth. Since you probably won’t know if you’re going to have a difficult time beforehand, it’s not a bad idea to do some scouting around for nurses in advance, just in case. If you have the name of a potential nurse or two, or at least have spoken to an agency, you can call shortly after you deliver and have a helper hired before you get home.
To give yourself a chance to recuperate after a cesarean or difficult vaginal birth. Since you probably won’t know if you’re going to have a difficult time beforehand, it’s not a bad idea to do some scouting around for nurses in advance, just in case. If you have the name of a potential nurse or two, or at least have spoken to an agency, you can call shortly after you deliver and have a helper hired before you get home.
A baby nurse may not be the best solution to your postpartum needs if:
 You’re breastfeeding. Since a nurse can’t feed a nursing newborn, and feeding is one of the most time-consuming tasks in the care of a young baby, she may not prove to be all that helpful. For the nursing mother, household help—someone to cook, clean, and do laundry—is probably a wiser investment, unless you can find a nurse who will do these chores and also offer breastfeeding tips.
You’re breastfeeding. Since a nurse can’t feed a nursing newborn, and feeding is one of the most time-consuming tasks in the care of a young baby, she may not prove to be all that helpful. For the nursing mother, household help—someone to cook, clean, and do laundry—is probably a wiser investment, unless you can find a nurse who will do these chores and also offer breastfeeding tips.
 You’re not comfortable with a stranger living in your home. If the idea of having a nonfamily member sharing your bathroom, your kitchen, and your table twenty-four hours a day makes you uneasy, hire a part-time nurse rather than a live-in, or opt for one of the other sources of help described below.
You’re not comfortable with a stranger living in your home. If the idea of having a nonfamily member sharing your bathroom, your kitchen, and your table twenty-four hours a day makes you uneasy, hire a part-time nurse rather than a live-in, or opt for one of the other sources of help described below.
 You’d rather do it yourself. If you want to be the one to give the first bath, catch sight of the first smile (even if they say it’s only gas), soothe your baby through the first bout of crying (even if it’s at 2 A.M.), don’t hire a nurse, hire household help to free you up for fun with baby.
You’d rather do it yourself. If you want to be the one to give the first bath, catch sight of the first smile (even if they say it’s only gas), soothe your baby through the first bout of crying (even if it’s at 2 A.M.), don’t hire a nurse, hire household help to free you up for fun with baby.
 Dad would rather do it, too. If you and your spouse are planning to share baby care, a nurse may get in the way. There may also not be much left for her to do—except to collect her paycheck—especially if dad’s around full-time while he’s enjoying paternity leave. In that case, the money could probably be more sensibly spent on cleaning help.
Dad would rather do it, too. If you and your spouse are planning to share baby care, a nurse may get in the way. There may also not be much left for her to do—except to collect her paycheck—especially if dad’s around full-time while he’s enjoying paternity leave. In that case, the money could probably be more sensibly spent on cleaning help.
If you decide that a baby nurse is right for you, the best way to go about finding one is to ask for recommendations from friends who’ve used one. Be sure to find out if the nurse in question has the qualifications and qualities you’re looking for. Some cook, some don’t. Some will do light housework and laundry, others won’t. Some are gentle, motherly women who will nurture your innate mothering ability and leave you feeling more confident; others are bossy, cold, and patronizing and will leave you feeling totally inadequate. Many are licensed practical nurses; some have also been trained specifically in caring for mother as well as baby, in mother-child relations, and in teaching breastfeeding and childcare basics. A personal interview is extremely important, since it’s the only way to know whether you are going to feel comfortable with a particular candidate. But excellent references (do check them out) are a must. A nurse hired through an agency should be licensed and bonded. It’s also very important that a nurse—or anyone else you hire who may come in contact with the baby—has been screened for TB. She should also be trained in CPR and child safety, as well as be up-to-date on baby-care practices (putting baby to sleep face up; keeping toys, pillows, and blankets out of the crib, and so on).
You might also consider a postpartum doula. Like a baby nurse, a doula helps a new mother with the baby. Unlike most nurses, she’ll also take charge of the household care. She’ll set up the nursery, give baby-care tips, cook, clean, run errands, help care for an older child (or spend time caring for the newborn so you have more time to baby your older child) and more, depending on your needs. She will also likely be a good source of Breastfeeding tips and will nurture you, the new mother (much as a labor doula does), so you can better nurture your baby. In other words, a doula mothers the mother, providing a sympathetic ear and serving as an antidote for the isolation many new mothers experience. Postpartum doulas usually charge by the hour (unlike nurses, who usually charge by the week), so they can get costly—but if you use her time effectively, a doula can be well worth the price.
For more information on doulas or to locate one in your area, contact Doulas of North America: 206-324-5440, www.dona.com; the Childbirth and Postpartum Professional Association, www.childbirthprofessional.com; check under “doula” in your local Yellow Pages; or ask your practitioner or hospital for a recommendation.
“With the loss of my income, we just can’t afford the expense of a baby nurse. Since I may need a cesarean—my baby’s in a breech position—I wonder if I will be able to manage without help.”
Just because you can’t afford—or don’t want to hire—a baby nurse doesn’t mean you have to go it alone. Most women, in fact, rely on other sources of help, at least one of which is probably available to you:
The new father. If your spouse can arrange his schedule so that he can be with both of you for the first few weeks (or can take time off through the Family Medical Leave Act), he is probably your best helper. Together and without outside assistance or interference, you’ll both learn more about your baby and baby care than you would any other way. No experience is necessary for the job; you’ll both catch on quickly. Do take a baby-care class together at a local hospital or community center (there are also classes for dads only), and read a childcare book or two before baby arrives to pick up some of the basics beforehand. Consider turning to family, friends, the baby’s doctor, the hospital nursery staff, La Leche League, and other sources of information and advice to fill in the blanks. Your partner-in-parenting should also be prepared to perform more than his share of the household chores in those first six weeks postpartum, when you’ll still be recovering no matter how you end up delivering.
A grandma. If you have a mother or mother-in-law whom you’d be comfortable having around on a live-in or come-in basis for the first weeks (and who you think can “help out” without “taking over”—a fine line that some grandparents have trouble not crossing), this may provide another good solution. Grandmothers (and many grandfathers) have at least 101 uses: they can rock a crying baby, cook a splendid supper, wash and fold the laundry, do the marketing, and much, much more. This kind of arrangement works particularly well if you can handle a little well-meant interference good-naturedly. Of course, if the grandparent in question has an already busy life and isn’t interested in revisiting the changing table, this won’t be an option.
If you’re lucky, a doula. Some hospitals and birthing centers offer the services of a doula, free of charge and for a short (but invaluable) time, as part of their delivery package. Check to see if your hospital or center has such a program in place.
Your freezer. You won’t be able to put baby on ice when you’re tired, but you will be able to pull meals out of the deep freeze if you prepared some during the last weeks of pregnancy when, if you weren’t working, you may have had too much time on your hands anyway. A few nutritious casseroles, a roasted chicken ready to reheat, or a prepared pasta sauce will ease the pressure of having to feed yourself and the rest of your family nightly. Then you can focus more on feeding baby (which you may find a full-time job for a while if you’re nursing). Don’t hesitate to stock up on frozen vegetables, too; they take little preparation time and are nutritious as well.
Your favorite takeout. If you don’t have the time or the opportunity (or the energy, or the ambition) to prepare meals in advance, you still won’t have to cook in those busy postpartum days. Nearly every neighborhood has one or more takeout shops where you can get meats, chicken, sometimes fish, and side dishes ready to heat and eat—and, increasingly, fresh salads that require only a fork and an appetite to enjoy. Put favorite takeout restaurants on speed dial, and don’t forget the salad bar at your local supermarket.
Paper goods. When dinner is over, whether home-prepared or takeout, there are always dishes to do—unless you rely on paper plates, plastic flatware, and disposable cups. Disposables will also come in handy for serving snacks to visitors who have come to admire the baby. (Keep such entertaining to a minimum, however, if you want to survive the postpartum period.)
Cleaning help. If there’s one job that most new parents would gladly relinquish, it’s cleaning. Give it up—to a cleaning service, a cleaning person, someone you’ve used before, or someone new—anyone who can vacuum and dust, mop floors and scour bathrooms, so that you and your spouse can have more time and energy to devote to baby, any older children, yourselves, and each other. This is a good route for parents who want to do most of the newborn care themselves but don’t want to sacrifice their health, sanity, or the condition of their home in the deal.
Remember, even if you hire help, and most especially if you don’t, there will inevitably be things that don’t get done during those early weeks. As long as caring for your baby and getting rest for yourself aren’t among them, don’t worry—but do get used to it. Though a certain amount of order will eventually be restored to your home, life with children will almost always include living with at least a few untied ends—not to mention a few unwashed dishes in the sink … a few dust balls under the coffee table … a few loads of laundry that still need folding …
“I thought that circumcision was pretty much routine nowadays, but the pediatrician I’ll be using said that it’s not really necessary.”
Circumcision is probably the oldest medical procedure still performed. Though the most widely known historical record of the practice is in the Old Testament, when Abraham circumcised Isaac, its origins are lost in antiquity, probably going back before the use of metal tools. Practiced by Muslims and Jews throughout most of history as a sign of their covenant with God, circumcision became widespread in the United States in the late nineteenth century, when it was theorized that the removal of the foreskin would make the penis less sensitive (it doesn’t), thus making masturbation a less tempting pursuit (it didn’t). In the years that followed, many other medical justifications for routine circumcision have been proposed—among others that it might prevent or cure epilepsy, syphilis, asthma, lunacy, and tuberculosis—none of it true.
Circumcision does reduce the risk of infection of the penis, but careful attention to cleaning under the foreskin once it is retractable (usually around the second birthday) will do as well. It also eliminates the risk of phimosis, a condition in which the foreskin remains tight as the child grows and can’t be retracted as it normally can in older boys. Phimosis can be extremely painful and sometimes interferes with erection. It is estimated that between 5 and 10 percent of uncircumcised males have to undergo the discomfort of circumcision sometime after infancy because of infection, phimosis, or other problems.
In 1999, an American Academy of Pediatrics (AAP) task force determined that, although existing scientific evidence demonstrates medical benefits of newborn circumcision, these medical benefits are not significant enough to recommend circumcision as a routine procedure. While studies do show the risk of developing a urinary tract infection (UTI) in the first year of life is higher for baby boys who are uncircumcised, the AAP concluded that the actual risk of an uncircumcised boy developing a UTI is very low—about 1 percent. They also concluded that though the risks of developing penile cancer or contracting sexually transmitted diseases, including AIDS, may be very slightly increased in an uncircumcised male, these risks, too, are extremely low and may not be compelling when weighed against a parent’s wishes to leave their son’s foreskin intact—or against the also remote risk of complication during or following circumcision. Complications from circumcision, while rare, could include heavy bleeding, infection (which is treatable with antibiotics), and a foreskin that may be cut too short or left too long, or that heals improperly (very rarely, a second operation may be needed to correct such a problem).
Circumcision remains controversial, with information and evidence supporting schools of thought both for and against it. The AAP recommends that parents be made aware of the potential risks and benefits of circumcision and that ultimately, they should do what they feel is in the best interest of their child. With that in mind, you should make your decision about circumcision in conjunction with your baby’s doctor and based upon a full consideration of medical benefits and risks as well as on esthetic, social, cultural, and religious factors—and most important, what feels right for you. If you do decide to have your son circumcised, the AAP recommends that pain relief (using a local anesthetic) be provided.
Presently more than half of all boys in the U.S. are circumcised, down from more than 80 percent in the early 1980s. The most common reasons parents give for opting for circumcision, in addition to just “feeling it should be done,” include:
 Religious observance. The religious laws of both Islam and Judaism require that newborn boys be circumcised.
Religious observance. The religious laws of both Islam and Judaism require that newborn boys be circumcised.
 Cleanliness. Since it’s easier to keep a circumcised penis clean, cleanliness is next to godliness as a reason for circumcision in the U.S.
Cleanliness. Since it’s easier to keep a circumcised penis clean, cleanliness is next to godliness as a reason for circumcision in the U.S.
 The locker-room syndrome. Parents who don’t want their sons to feel different from their friends or from their father or brothers often choose circumcision. (This may be less of a consideration as fewer boys are circumcised.)
The locker-room syndrome. Parents who don’t want their sons to feel different from their friends or from their father or brothers often choose circumcision. (This may be less of a consideration as fewer boys are circumcised.)
 Appearance. Some feel removal of the foreskin makes the penis more attractive.
Appearance. Some feel removal of the foreskin makes the penis more attractive.
 Health. The hope of reducing the risk of infection, cancer, or other future problems (including possible later circumcision) prompts many to elect to do the surgery immediately after birth.
Health. The hope of reducing the risk of infection, cancer, or other future problems (including possible later circumcision) prompts many to elect to do the surgery immediately after birth.
The reasons why more and more parents are deciding against circumcision include:
 The lack of medical necessity. Many question the sense of removing a part of an infant’s body without good cause.
The lack of medical necessity. Many question the sense of removing a part of an infant’s body without good cause.
 Fear of bleeding and infection. Though complications, particularly when the procedure is carried out by an experienced physician or a ritual circumciser with medical training, are rare, many parents are nevertheless understandably apprehensive about the possibility.
Fear of bleeding and infection. Though complications, particularly when the procedure is carried out by an experienced physician or a ritual circumciser with medical training, are rare, many parents are nevertheless understandably apprehensive about the possibility.
 Concern about pain. Evidence shows that newborns circumcised without analgesia experience pain and stress measured by changes in heart rate, blood pressure, and cortisol levels. The AAP’s policy states that analgesia (such as topical EMLA cream, dorsal penile nerve block, or the subcutaneous ring block) is safe and effective in reducing the pain associated with circumcision.
Concern about pain. Evidence shows that newborns circumcised without analgesia experience pain and stress measured by changes in heart rate, blood pressure, and cortisol levels. The AAP’s policy states that analgesia (such as topical EMLA cream, dorsal penile nerve block, or the subcutaneous ring block) is safe and effective in reducing the pain associated with circumcision.
 The wish for the child to be like his uncircumcised father. Another version of the like-father/like-son belief.
The wish for the child to be like his uncircumcised father. Another version of the like-father/like-son belief.
 A belief in children’s rights. Some parents wish to leave the decision to the child at a later date.
A belief in children’s rights. Some parents wish to leave the decision to the child at a later date.
 To allow optimal sexual enjoyment. There are those who still believe an uncircumcised penis is more sensitive, though there’s no scientific support for this position.
To allow optimal sexual enjoyment. There are those who still believe an uncircumcised penis is more sensitive, though there’s no scientific support for this position.
 Less risk of diaper irritation. It’s been suggested that the intact foreskin may protect against diaper rash on the penis.
Less risk of diaper irritation. It’s been suggested that the intact foreskin may protect against diaper rash on the penis.
Though the risks of circumcision are minimal, complications can occur. To reduce the risk, be sure the person who is performing the procedure is experienced, and if he’s a ritual circumciser, that he is well trained and comes highly recommended. Also be sure that the surgery is done not in the delivery room but rather when your baby is stabilized, usually after at least twelve to twenty-four hours. And do not permit cauterization with a metal clamp, which could cause serious burns.
If you remain undecided about circumcision as delivery day approaches, read about circumcision care on page 198, and discuss the issue with the doctor you have chosen for your baby—and possibly with friends who have gone either route.
“Everyone I know uses disposable diapers, and they do seem a lot less of a mess than cloth ones. But are they as good for baby?”
Ever since Eve, parents have had to confront the problem of how to cover baby’s bottom. And over the millennia, some ingenious—though not necessarily convenient—solutions evolved. For instance, American Indian mothers apparently kept their babies (and their own backs) dry and comfortable by packing their papoose boards with the soft shredded insides of cattails.
Luckily, as a parent in the twenty-first century, you won’t have to wade daily into the marshes to choose the softest and most absorbent cattails to pad your Snugli. But you will have to choose among a plethora of possibilities, ranging from several types of cloth diapers (to launder yourself or order from a diaper service) to a bewildering and ever-changing array of disposables.
The choice that’s right for you and your baby many be different from the one that’s right for your neighbors and their infants. Personal factors will be of major significance since, scientifically and economically, there’s no conclusive winner in the diaper derby. Consider the following in making your choice:
Disposable diapers. The parents’ choice by far, disposables are most often selected for their convenience. And for busy parents (is there another kind?), that’s a major advantage. There are no dirty diapers to collect, tote around, and pile up for weekly pickup or laundry. Disposables also save a certain amount of time and effort; they’re faster and easier to put on and take off (especially important if your baby is a wriggler). Newer (and more costly) styles are increasingly more absorbent and theoretically less likely to cause diaper rash. They’re trimmer, better fitting, and less apt to leak.
These desirable features also add up to a distinct disadvantage: Since disposables soak up so much urine and often “feel” dry when they’re far from it, parents are less likely to change diapers frequently enough, and infrequent changes can lead to diaper rash. The super absorbency of these diapers also makes it hard to tell how much your newborn is urinating, to gauge if his or her milk intake is sufficient. Additionally, the new superbreed of diaper keeps babies so comfortable when wet that toilet learning may eventually be more difficult to accomplish. Also on the minus side is the effect that paper diapers have on the environment as they’re loaded into landfills. (Though cloth diapers also take a toll on Mother Nature in terms of power and water use, as well as soap runoff.) Having to shop for and lug the diapers home is also a potential disadvantage, when weighed against the convenience of a diaper service, but this drawback can be avoided if you order by phone or on-line.
Home-delivered cloth diapers. To those who are reluctant to encase their infant’s bottom in paper and plastic, soft, comfortable, sterilized, and possibly ecologically preferable cotton diapers are appealing, especially when they are delivered to the door weekly. Some studies (which diaper services are fond of quoting) show a lower incidence of diaper rash with such diapers; others (cited by paper diaper manufacturers) show super-absorbent disposables yielding a lower incidence of rash. If cloth diapers are continued into toddlerhood (many parents switch to paper before this), toilet learning may be easier to accomplish, because direct contact between a sopping wet cloth diaper and skin makes a child very uncomfortable, more aware of being wet, and, hopefully, more inspired to use the potty.
There are disadvantages, however. Separate waterproof pants are usually needed to avoid having to change baby, crib, and often parent’s clothes every time baby wets (though there are “allin-ones”—fitted cloth diapers with the waterproof cover already sewn on). These waterproof pants increase the risk of rash by keeping air out and moisture in, though breathable diaper pants or wraps made of cotton or wool (sometimes with airy mesh linings and/or absorbent foam fillings) can reduce or even eliminate this problem. Because there’s more fussing and fiddling involved (though technical advances in the cloth arena—such as fitted diapers and easier fasteners—continue to reduce this drawback significantly), diaper changes are generally more trouble with cloth diapers, particularly as baby becomes more proficient in squirming. Because absorbency is more limited, double diapers are usually needed at night, and, for some heavy wetters, during the day. Boys, who concentrate their urine in front, may need paper diaper liners. And then there are the plastic bags of soiled diapers to be carried home from outings and the ever-present pail of dirty diapers, which is never truly odor free (though the same can be said for disposable diapers if kept for too long in a diaper pail).
Finally, though cloth diapers don’t end up in landfills, their laundering does have a negative impact on the environment; whether it’s as significant as the impact from disposables is debatable.
Home-laundered cloth diapers. These may be the clear loser compared to the other two choices. Because they can’t be adequately sanitized, home-laundered diapers are, according to studies, more likely to cause diaper rash. And though they seem to be far less expensive than either of the other diaper choices, they are only slightly so, when one considers the cost of soap, water, and power used. In addition, they demand a greater expenditure of time and effort—to soak, wash, dry, and fold between uses.
Some parents decide to use cloth diapers for the first few months, a time when baby usually spends more time at home than on the go, and then graduate to disposables as the logistics of toting cloth become too much like hard work. They will often, however, use disposables on outings and, sometimes, at night (because their greater absorbency keeps baby more comfortable longer and may ensure a better night’s sleep) from the start.
Whichever diaper you decide on now, you may find that your baby develops diaper rash frequently later. This could point to a sensitivity to your choice. If this occurs, don’t fight it—switch. Try a different type of diaper (switch from cloth to paper or vice versa) or a different brand of disposable. Also see tips for preventing and treating diaper rash on page 269.
“Except for the first few months of pregnancy, when I couldn’t smoke because it made me queasy, I never managed to give it up entirely—and neither has my spouse. How much will smoking around our baby affect her?”
Nothing you can buy in a layette department, splurge on in a toy store, or put away into a trust fund can match the gift to your newborn of growing up in a smoke-free environment. Smoking by parents has been linked to an increased risk of Sudden Infant Death Syndrome (SIDS), to more respiratory illnesses (colds, flu, bronchiolitis, asthma) and ear infections during the first year of life, to impaired lung function and reduced lung capacity, as well as to an increased risk of tooth decay later on in childhood. Not only are the children of smokers sick more often than children of nonsmokers, but their illnesses also last longer. They are also more likely to be hospitalized in the first three years of life. The more smokers in the household, the more severe the negative effects, since the amount of smoke a child inhales is related to the number of smokers she is exposed to on a regular basis. And the risks aren’t eliminated even when parents step outside the house to light up. Researchers have found that children in households with smokers who smoke only outside are still exposed to 70 percent more damaging lung particles than those in nonsmoking households.
Perhaps worst of all, offspring of smokers are more likely to become smokers than children whose parents don’t smoke. So quitting may not only keep your child healthier in childhood, it may, by lessening the chance of your child smoking later in life, also keep her alive and well longer. And if that’s not motivation enough, keep this in mind, too: By quitting you’ll be giving your baby the gift of healthier parents.
If you haven’t been able to quit up until now, it obviously won’t be easy. As they would with any drug addiction (particularly such a powerful one), your body and your mind will align against you. But if you’re determined to fight back—for your sake and your baby’s—you can triumph over both. And the best time to do it is now, before baby is born. Giving up smoking before delivery will increase the oxygen available to your baby during childbirth. And your newborn will come home from the hospital to clean, breathable air and, if you’re breastfeeding, to nicotine-free milk. If you are still in the early months of pregnancy, quitting now will also reduce the risk of premature delivery and of having a low-birthweight baby. (Any time, however, is a good time to quit, especially when there’s a new set of lungs in the house. If you don’t manage to do it before delivery, redouble your efforts once baby’s sharing the air in your home.)
“I’ve always been unhappy with my name. How can we be sure our son won’t be unhappy with the name we choose?”
What’s in a name? To a newborn baby, not much. Feed him, clothe him, comfort and entertain him, and you can call him “Rover” for all he’ll care. Once friends and the outside world begin to play a bigger role in your child’s life, however (usually early in elementary school), antipathy to the name you selected may develop. Though there’s no way to guarantee baby will love for a lifetime the name you choose, careful and sensitive selection will lessen the chance of a name turning out to be Trouble. Here are some tips to keep in mind when selecting a name for your baby:
 Make sure both you and your spouse like the name—the way it sounds and looks, and the connotations it carries. Ask yourselves, “Would I like it if it were my name?”
Make sure both you and your spouse like the name—the way it sounds and looks, and the connotations it carries. Ask yourselves, “Would I like it if it were my name?”
 Select a meaningful name—name your baby after a loved family member, a respected historical or biblical character, or a favorite character in literature. Such a name gives the child a sense of belonging, of being part of an extended family or of the greater world.
Select a meaningful name—name your baby after a loved family member, a respected historical or biblical character, or a favorite character in literature. Such a name gives the child a sense of belonging, of being part of an extended family or of the greater world.
 Select a name that fits. Melanie, for example, which means “black” or “dark,” would be fitting for a dark-haired girl; Dustin, “a fighter,” might be appropriate for a boy who made it through a difficult delivery. Or one that fits you spiritually, symbolizing, perhaps, a quality you wish for him or her, such as Hope, or Faith, or Christian. Or that reflects your feelings about the birth—Joy, for example, or Ian (“gracious gift of God”). A fitting name can make a child feel extra special, though to match baby up with such a name you may have to postpone the decision until after birth.
Select a name that fits. Melanie, for example, which means “black” or “dark,” would be fitting for a dark-haired girl; Dustin, “a fighter,” might be appropriate for a boy who made it through a difficult delivery. Or one that fits you spiritually, symbolizing, perhaps, a quality you wish for him or her, such as Hope, or Faith, or Christian. Or that reflects your feelings about the birth—Joy, for example, or Ian (“gracious gift of God”). A fitting name can make a child feel extra special, though to match baby up with such a name you may have to postpone the decision until after birth.
 How will the name sound to others? Are there any possible hidden meanings or soundalike words that might someday make the name embarrassing to your child? Check the initials; do they spell something that could make your child the butt of jokes or teasing? The name Anna Samantha Smith, for example, just might be the source of schoolyard torment for a child. What about possible nicknames? Could they trigger childish insults? If it’s an extremely unusual name, or one that’s very ethnic, consider whether it may be difficult for your child to live with later on.
How will the name sound to others? Are there any possible hidden meanings or soundalike words that might someday make the name embarrassing to your child? Check the initials; do they spell something that could make your child the butt of jokes or teasing? The name Anna Samantha Smith, for example, just might be the source of schoolyard torment for a child. What about possible nicknames? Could they trigger childish insults? If it’s an extremely unusual name, or one that’s very ethnic, consider whether it may be difficult for your child to live with later on.
 Include a middle name so that if your child turns out to be unhappy with his first name, the middle name can be substituted.
Include a middle name so that if your child turns out to be unhappy with his first name, the middle name can be substituted.
 Consider choosing a name that’s easy to say and spell. A very unusual name that teachers are always mispronouncing or a name that’s always being misspelled could become a burden—not only in school but also later on in life. On the other hand, some children (and later, adults) ultimately enjoy having an unusual name because it will separate them from the pack.
Consider choosing a name that’s easy to say and spell. A very unusual name that teachers are always mispronouncing or a name that’s always being misspelled could become a burden—not only in school but also later on in life. On the other hand, some children (and later, adults) ultimately enjoy having an unusual name because it will separate them from the pack.
 Avoid the trendy or the political. Don’t saddle your child with this year’s hot name (after a TV or film star or politician who’s making every magazine cover). When the famous namesake turns out to be a flash in the pan or worse, the name may become outdated or place your child in a light that is uncomfortable.
Avoid the trendy or the political. Don’t saddle your child with this year’s hot name (after a TV or film star or politician who’s making every magazine cover). When the famous namesake turns out to be a flash in the pan or worse, the name may become outdated or place your child in a light that is uncomfortable.
 Use a real name instead of a diminutive (Robert, not Bob; Elizabeth instead of Liz.) You can use the diminutive form throughout childhood, but your child then has the option of switching to the more dignified version when he or she ventures out into adulthood.
Use a real name instead of a diminutive (Robert, not Bob; Elizabeth instead of Liz.) You can use the diminutive form throughout childhood, but your child then has the option of switching to the more dignified version when he or she ventures out into adulthood.
 If you don’t want your child to be one of six Emilys or seven Sams in the class, avoid picking a name from the year’s Top Ten. Many parenting magazines and Web sites run an annual piece on the subject of popular names, so check the Internet for this year’s winners. You can also gauge which are the most popular names in your neighborhood by reading the birth announcements, or taking a stroll in the playground and listening to the (proper) names parents call their children.
If you don’t want your child to be one of six Emilys or seven Sams in the class, avoid picking a name from the year’s Top Ten. Many parenting magazines and Web sites run an annual piece on the subject of popular names, so check the Internet for this year’s winners. You can also gauge which are the most popular names in your neighborhood by reading the birth announcements, or taking a stroll in the playground and listening to the (proper) names parents call their children.
 Consider family feelings, but don’t let them dominate. If there’s a family name that you don’t love but your parents would like to see perpetuated out of either tradition or sentiment, try it as a middle name, alter it so that it’s more appealing to you, choose another form of the same name (most names actually have several forms), or select a name with the same meaning. A good baby name book will be helpful here. And remember, no matter what names you choose, your parents and grandparents will love the kids—even if they’re not happy with the names at first.
Consider family feelings, but don’t let them dominate. If there’s a family name that you don’t love but your parents would like to see perpetuated out of either tradition or sentiment, try it as a middle name, alter it so that it’s more appealing to you, choose another form of the same name (most names actually have several forms), or select a name with the same meaning. A good baby name book will be helpful here. And remember, no matter what names you choose, your parents and grandparents will love the kids—even if they’re not happy with the names at first.
 Be sure the name or names are euphonic with the last name and with each other. A good general rule: a short last name goes well with a long first name (Abigail Jones) and vice versa (James Martinez), while two-syllable firsts usually complement two-syllable lasts (Hannah Kramer).
Be sure the name or names are euphonic with the last name and with each other. A good general rule: a short last name goes well with a long first name (Abigail Jones) and vice versa (James Martinez), while two-syllable firsts usually complement two-syllable lasts (Hannah Kramer).
“Our dog is intensely jealous of my affections—she always tries to come between me and my spouse when we hug. I’m worried about how she’ll react to the new baby.”
It’s hard for a dog who’s always been treated like a baby to roll over and play dog when a real baby appears on the scene. But that’s exactly what she’ll have to do when her place in your heart has to be shared by that tiny but threatening new human you’ll soon be bringing home from the hospital. Though a little initial moping around may be unavoidable, you’ll want to do whatever you can to prevent excessive jealousy and, of course, any aggressive reactions. Start now.
 Invest in an obedience training program for your dog if she isn’t trained already—and even if you’ve never felt there was the need for it before. Friskiness and puppy-like exuberance aren’t usually a problem in a childless home, but they could be in one with a new baby. Particularly because the baby’s behavior won’t be controllable or predictable, your dog’s must be. Obedience training won’t take the spirit out of your pet, but it will make her more stable, and thus less likely to harm your baby.
Invest in an obedience training program for your dog if she isn’t trained already—and even if you’ve never felt there was the need for it before. Friskiness and puppy-like exuberance aren’t usually a problem in a childless home, but they could be in one with a new baby. Particularly because the baby’s behavior won’t be controllable or predictable, your dog’s must be. Obedience training won’t take the spirit out of your pet, but it will make her more stable, and thus less likely to harm your baby.
 Get your dog used to babies now, if you can. Invite friends with babies over to the house, or let her (under careful supervision, and if the parent is willing) sniff near a baby in the park or be petted by a toddler, so that she can become familiar with their smells and their moves.
Get your dog used to babies now, if you can. Invite friends with babies over to the house, or let her (under careful supervision, and if the parent is willing) sniff near a baby in the park or be petted by a toddler, so that she can become familiar with their smells and their moves.
 Get your dog used to life with a baby in the house. Use a baby-size doll as a prop in her training (it’ll also be helpful in yours). Diaper the doll; carry, sing to, and rock it; “nurse” it; put it to bed in the crib; take it for a walk in the stroller (if you don’t mind the neighbors staring). Now and then, play a tape of a baby crying.
Get your dog used to life with a baby in the house. Use a baby-size doll as a prop in her training (it’ll also be helpful in yours). Diaper the doll; carry, sing to, and rock it; “nurse” it; put it to bed in the crib; take it for a walk in the stroller (if you don’t mind the neighbors staring). Now and then, play a tape of a baby crying.
 Get your dog used to sleeping alone, if that’s what the postpartum arrangement will be, so that the change doesn’t come as a shock. Fix up a comfortable doggie bed in a corner—with a favorite pillow or blanket for company. Consider keeping it in a baby-free zone; a crawling baby’s invasion of her sleeping space can provoke an aggressive reaction in the friendliest of canines.
Get your dog used to sleeping alone, if that’s what the postpartum arrangement will be, so that the change doesn’t come as a shock. Fix up a comfortable doggie bed in a corner—with a favorite pillow or blanket for company. Consider keeping it in a baby-free zone; a crawling baby’s invasion of her sleeping space can provoke an aggressive reaction in the friendliest of canines.
 Take your dog for a complete medical checkup. Be sure that your dog’s rabies shots are up-to-date, that she is flea- and tick-free (ask your vet about using a pill or another method that’s effective against these pests yet safe to use around your baby). Also be sure to have your dog checked for worms of any kind.
Take your dog for a complete medical checkup. Be sure that your dog’s rabies shots are up-to-date, that she is flea- and tick-free (ask your vet about using a pill or another method that’s effective against these pests yet safe to use around your baby). Also be sure to have your dog checked for worms of any kind.
 If your baby will have a separate room, train your dog to stay out of it while you’re not there. A gate to block the doorway will help discourage unsolicited visits. If your baby’s crib will be in your room or in a corner of the living room, train your dog not to go under the crib, since she could accidentally unlock the side, letting it fall.
If your baby will have a separate room, train your dog to stay out of it while you’re not there. A gate to block the doorway will help discourage unsolicited visits. If your baby’s crib will be in your room or in a corner of the living room, train your dog not to go under the crib, since she could accidentally unlock the side, letting it fall.
 If your dog’s feeding station is one your baby will later be able to get to easily, move it to the cellar, garage, or some other area that doesn’t invite a curious crawler, since even an easygoing dog can become vicious when her food is threatened. If you live in a small apartment, get your dog on an evening feeding schedule and remove her food dish during the day. Don’t even leave her food around when the dog is safely outside, because those tasty nuggets taste good not only to canines—many babies love sampling them, too, and they pose a choking hazard. And use a small nontip water bowl unless you enjoy mopping the floor frequently.
If your dog’s feeding station is one your baby will later be able to get to easily, move it to the cellar, garage, or some other area that doesn’t invite a curious crawler, since even an easygoing dog can become vicious when her food is threatened. If you live in a small apartment, get your dog on an evening feeding schedule and remove her food dish during the day. Don’t even leave her food around when the dog is safely outside, because those tasty nuggets taste good not only to canines—many babies love sampling them, too, and they pose a choking hazard. And use a small nontip water bowl unless you enjoy mopping the floor frequently.
 After delivery, but while you’re still in the hospital or birthing center, have your spouse bring home an unwashed piece of clothing your newborn has worn so that your pet can become familiar with the baby’s scent. When you arrive home, let your spouse hold the baby while you greet your pet. Then to satisfy her curiosity, let the dog sniff the baby—who should be well swaddled, with head and face protected by your arms. Once the baby’s snug in the crib, break out a special treat for the dog and spend a little time alone with her.
After delivery, but while you’re still in the hospital or birthing center, have your spouse bring home an unwashed piece of clothing your newborn has worn so that your pet can become familiar with the baby’s scent. When you arrive home, let your spouse hold the baby while you greet your pet. Then to satisfy her curiosity, let the dog sniff the baby—who should be well swaddled, with head and face protected by your arms. Once the baby’s snug in the crib, break out a special treat for the dog and spend a little time alone with her.
 Be attentive to your new baby, of course, but don’t act overprotective around your dog. This will only make the animal more jealous and insecure. Instead, as you would with a human sibling (though on a different level, naturally), try to get your pet involved with the new addition and let her know she’s still a loved member of the family. Pet her while you nurse, walk her while you take the baby out in the stroller, allow her into the baby’s room while you’re there. Try to make a point of spending at least five minutes every day alone with her. But should she show even the slightest aggressiveness toward your baby, reprimand her immediately.
Be attentive to your new baby, of course, but don’t act overprotective around your dog. This will only make the animal more jealous and insecure. Instead, as you would with a human sibling (though on a different level, naturally), try to get your pet involved with the new addition and let her know she’s still a loved member of the family. Pet her while you nurse, walk her while you take the baby out in the stroller, allow her into the baby’s room while you’re there. Try to make a point of spending at least five minutes every day alone with her. But should she show even the slightest aggressiveness toward your baby, reprimand her immediately.
 If, despite your efforts to prepare and reassure her, your dog seems hostile toward the new arrival, keep her tied up and away from the baby until you’re sure she’s worked out her feelings. Just because a dog has never bitten before doesn’t mean she’s not capable of it under duress. If tying up the dog only adds to her hostility, you may have to consider finding another home for her. (With male dogs, neutering may reduce aggressiveness.)
If, despite your efforts to prepare and reassure her, your dog seems hostile toward the new arrival, keep her tied up and away from the baby until you’re sure she’s worked out her feelings. Just because a dog has never bitten before doesn’t mean she’s not capable of it under duress. If tying up the dog only adds to her hostility, you may have to consider finding another home for her. (With male dogs, neutering may reduce aggressiveness.)
“I worry that our cat, who has always slept with us, may be jealous of the new baby.”
Even friendly cats can undergo personality changes when a baby arrives. And since cats are just as capable of harming an infant as dogs are, with their claws as well as with their jaws, it’s as important to make sure they are well prepared for the family expansion. Most of the above tips for preparing a dog can work for a cat as well. Be particularly careful to reassure your cat—through plenty of attention—that he is still a family favorite. And because cats usually love to cuddle next to a warm body and can quickly scale the sides of a crib, be sure to attach a specially designed mesh crib net securely over it to keep yours from bedding down with baby—a friendly gesture that could end in tragedy. Also keep cats (and dogs) from licking your infant’s face or any broken skin.
“I have a friend who insists that I should toughen my nipples in preparation for nursing. Is that a good idea?”
Female nipples are designed for nursing. And, with very few exceptions, they come to the job fully qualified, without the need for prior preparation. In fact, in some cases the procedures that used to be recommended for toughening up or otherwise readying the nipples for breastfeeding can do more harm than good. For instance, applying alcohol, witch hazel, or tincture of benzoin can dry the nipples and make them more, rather than less, likely to crack and fissure; even soap can be drying, and its use on the nipples should be avoided during the last trimester of pregnancy and during lactation itself. Ditto using a brush on nipples, which can irritate tender tissues, making them more—not less—likely to crack under the pressures of nursing. Massaging or using a breast pump to prepare nipples isn’t just counterproductive, it can be dangerous; such manipulations can stimulate contractions and occasionally even trigger a breast infection.
BREAST SHELLS
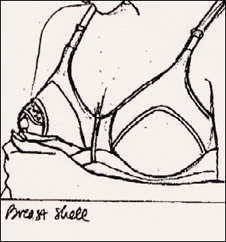
Breast shells exert constant yet painless pressure, which draws out inverted or flat nipples.
It may be tempting to try to express colostrum prenatally to see if it’s there—but don’t. Not only can such nipple manipulation cause uterine contractions, but it might also result in some loss of the valuable elements of this premilk. For more on colostrum, see page 77.
While the vast majority of nipples don’t need any preparation for Breastfeeding, a predelivery exam by your practitioner can screen your breasts for any anatomical features that might prove problematic once breastfeeding begins, such as underdeveloped glandular tissue or inverted nipples.
If you do have inverted nipples (your nipples retract into the breast tissue instead of sticking out when you’re cold or when you compress your breast with your fingers at the edge of the areola), ask your practitioner if they’ll need any preparation for breastfeeding. Though research shows that such preparation isn’t usually necessary (once breastfeeding is initiated, most inverted nipples do their job as well as any others), some practitioners continue to recommend the use of breast shells. These plastic shells gradually draw out flat or inverted nipples (see illustration) by exerting painless pressure on the breasts. On the downside, breast shells can be embarrassingly conspicuous and may also cause sweating and rashes.
More important than preparing your breasts for breastfeeding is preparing your mind. Learn all you can about breastfeeding: take a prenatal course, if possible; read chapter 3 and books on the subject; get in touch with your local La Leche League (an invaluable source of advice and support) or check out their Web site at www.lalecheleague.org; select a pediatrician who strongly advocates nursing; get tips and feedback from breastfeeding friends; and consider using a lactation consultant.
When you first started shopping around for a practitioner to deliver your baby, it was hard to imagine there was actually going to be a baby to deliver. Now, with tiny but powerful fists, feet, and knees using you regularly as a punching bag, you no longer have any doubts. Not only is there a baby in there—it’s eager to get out. And before it does, you’d better start shopping around for the practitioner who’ll care for it. Delaying your decision might mean having a doctor whom you don’t know care for your baby should you deliver early; no one to ask important questions of during those confusing first days; and no familiar face in case of a problem with your newborn.
Assuming you stay in the community and are relatively satisfied with the care, the doctor you choose could well be seeing baby—and you—through some eighteen years of runny noses, earaches, sore throats, high fevers, upset stomachs, bumps and bruises, maybe even broken bones; through dramatic physical and psychological developmental milestones that will both thrill and bewilder you; through moments you can’t now even conceive of. You won’t be living with your baby’s doctor during those years (though there will be times, particularly nights and weekends, when you’ll wish you were), but you’ll still want someone with whom you feel comfortable and compatible. Someone you wouldn’t hesitate to waken at 2 A.M. when your nine-month-old’s fever hits a new high, someone you wouldn’t be embarrassed to ask about your six-month-old’s sudden fascination with his genitals, someone you would feel free to question when you aren’t sure an antibiotic that’s been prescribed is necessary.
Before you start securing names, you need to make some basic decisions about the type of doctor you want to care for your baby.
When generations past had a runny nose or bothersome case of diaper rash, parents didn’t bundle baby up and head for the pediatrician. Chances are they took their precious bundle to the same doctor who brought him or her into the world, who treated father’s bursitis and grandmother’s arthritis, who removed uncle’s kidney stones and cousin’s tonsils: the family doctor, a general practitioner (GP), who hung out his shingle after medical school and a single year of internship. Today that breed of doctor is virtually extinct, and most runny noses and rashy bottoms are tended to by the pediatrician, a childcare specialist, or by the high-tech successor to the general practitioner—the family practitioner (FP). Deciding which type of practitioner is for you is your first step toward finding your Dr. Right.3
Choosing a health care plan is complicated enough when you don’t have children. But once you become a parent, there’s a lot more than just yourself (and your spouse) to consider. You’ll need to choose a plan (assuming you have the option of a choice) that best suits your family’s needs, considering, in particular, how the plan serves children. When looking for a health care plan, find out:
 What services the plan covers.
What services the plan covers.
 What limits, if any, there are on the number of well-baby or sick-baby visits.
What limits, if any, there are on the number of well-baby or sick-baby visits.
 What out-of-pocket expenses you’ll have to pay, such as copayments, deductibles, or monthly payments.
What out-of-pocket expenses you’ll have to pay, such as copayments, deductibles, or monthly payments.
 What level of care will be covered in case of an emergency or long-term needs.
What level of care will be covered in case of an emergency or long-term needs.
You should also know what specific services the plans you’re choosing from cover. These should include:
 Preventive and primary care (including routine checkups; immunizations; sick visits; speech, hearing, and vision tests; laboratory and X-ray services; prescription drugs).
Preventive and primary care (including routine checkups; immunizations; sick visits; speech, hearing, and vision tests; laboratory and X-ray services; prescription drugs).
 Major medical services (including consultation with specialists, hospitalization, ambulance services).
Major medical services (including consultation with specialists, hospitalization, ambulance services).
 Special care (including physical, speech, occupational, or other rehabilitation therapy; long-term care facility or home-care coverage; hospice care).
Special care (including physical, speech, occupational, or other rehabilitation therapy; long-term care facility or home-care coverage; hospice care).
You should also be familiar with the types of health care plans available today. Most people used to receive their health insurance coverage through traditional fee-for-service insurance plans—in which the insurance company paid all or part of any doctor’s bill. Today, most people who receive health insurance through their employer are in a managed care plan. Such types of plans include:
 Health Maintenance Organization (HMO), which offers a list of health services and health providers for a fixed monthly premium. Coverage is provided only if you go to a physician within the HMO system.
Health Maintenance Organization (HMO), which offers a list of health services and health providers for a fixed monthly premium. Coverage is provided only if you go to a physician within the HMO system.
 Preferred Provider Organization (PPO), which contracts with selected doctors and hospitals. Patients have the option of using those physicians, or of paying a little more to venture out of the network.
Preferred Provider Organization (PPO), which contracts with selected doctors and hospitals. Patients have the option of using those physicians, or of paying a little more to venture out of the network.
 Point of Service Plan (POS), in which patients have a primary care physician from within the network but can go out of the network for other care by paying a larger share of the cost.
Point of Service Plan (POS), in which patients have a primary care physician from within the network but can go out of the network for other care by paying a larger share of the cost.
The pediatrician. Babies, children, and sometimes adolescents are their business—their only business. In addition to four years of medical school, pediatricians have had three years of specialty training in pediatrics. If they are board certified, they have also passed a stringent qualifying exam. The major advantage of selecting a pediatrician for your baby is obvious—since they see only children, and lots of them, they are more familiar than other doctors with what’s normal and what’s not in young patients. They’re also more experienced in the care of sick children. And, perhaps most important, they are more likely to have the answers to the questions that nag new parents (having been asked them hundreds of times before), from “Why does he want to nurse all the time?” to “Why isn’t she sleeping more?” to “Why does he cry so much?”
A good pediatrician will be attuned to the whole family picture and will hopefully recognize when a child’s problem is rooted in what’s going on, either physically or emotionally, with a parent or other family member. The downside to choosing a pediatrician is that if the entire family comes down with something that requires medical treatment (strep all around), it may be necessary to call upon the services of two physicians.
The family practitioner. Like the pediatrician, the family practitioner usually has had three years of specialty training following medical school. But an FP residency program is much broader than a pediatric one, covering internal medicine, psychiatry, and obstetrics and gynecology, in addition to pediatrics. The advantage of choosing a family practitioner is that your entire family can be cared for by the same doctor, one who knows all of you as both people and patients and who can use this information in diagnosis and treatment. If you have already been using a family practitioner, adding your baby to the patient roll will have the added advantage of bringing the new family member to an old friend.
One potential disadvantage: Because he or she has had less training and experience in pediatrics than a pediatrician has, a family practitioner may be less accustomed to fielding the kinds of well-baby questions you may raise as well as be less astute at picking up the obscure diagnosis. To minimize this disadvantage, look for a family practitioner who sees a lot of babies, not just older children. Many do. Another potential drawback: The FP may be less willing, or less able, to care for your child during a hospitalization.
To some parents, the type of practice may be almost as important as the type of physician. There are several options; the one most appealing to you will depend on your personal preferences and priorities.
The solo practitioner. In such a practice, a doctor works alone, using another doctor to cover when he or she is away or otherwise unavailable. The major advantage of a solo practitioner is that such a doctor has the opportunity to build close one-to-one relationships with each of his or her patients. But there’s also a disadvantage to this: Solo practitioners aren’t likely to be on call around the clock and around the calendar. They’ll be around for scheduled appointments (unless called to an emergency), and on call most of the time, but they will take vacations and occasional nights and weekends off, leaving patients who require emergency care or consultation to a covering physician who may be unfamiliar to them. If you do select a solo practitioner, ask about who will be covering at such times, and be sure that in an emergency, your child’s records will be available even when the doctor is not.
The partnership. Sometimes two doctors are better than one. If one isn’t on call, the other almost always is. If you see them in rotation, you and your child often can, thanks to the frequent well-child visits during the first year, build good relationships with both. Though partners will probably concur on most major issues and will likely share similar philosophies of practice, they may occasionally offer different opinions. Having more than one opinion may in some instances be confusing, but hearing two approaches to a particularly confounding problem can be useful. (If one doesn’t seem to be able to solve your baby’s sleeping problems, maybe the other will.)
An important question to ask before deciding on a partnership: Can you schedule appointments with the physician of your choice? If not, and if you discover you like one but not the other, you may spend half your visits with a doctor with whom you’re not comfortable. Even if you can choose the preferred doctor for checkups, sick children must usually be seen by whoever is available at the time.
The group practice. If two are good, will three or more be better? In some ways probably yes; in others, possibly no. A group is more likely to be able to provide twenty-four-hour coverage by doctors in the practice, but less likely to ensure close doctor-patient relationships—again, unless you can select the same doctor (or two) for regular checkups. The more physicians a child will be exposed to on well-child and sick-call visits, the longer it may take to feel comfortable with each one, though this will be much less of a problem if all the doctors are warm and caring practitioners. Also a factor here: If you rotate physicians, contradictory advice can either enlighten or confound. In the long run, more important than the number of physicians in a practice will be the confidence you have in them individually and as a group.
A practice that has a pediatric nurse practitioner or physician’s assistant. Any of the above types of practices may include in their ranks one or more pediatric nurse practitioners (PNP), the equivalent of the nurse-midwife in the obstetrician’s office, or pediatric physician’s assistants (PA). The pediatric nurse practitioner is a BSN or RN with additional training (generally at the master’s degree level) in his or her specialty area; the pediatric PA is a licensed health care professional who works with physician supervision. A PNP or PA usually handles well-baby checkups and often the treatment of minor illnesses as well, consulting with physician colleagues as needed. Problems beyond the scope of a PNP or a PA are referred to one of the doctors in the office. Like the midwife, the PNP or PA will frequently spend more time with patients at each visit, often devoting as much attention to lifestyle questions as to medical ones. But because the level of training is not equal to that of the physician, you may have less confidence in the care your baby is receiving. This, however, isn’t necessarily a valid concern, since many studies have shown that nurse practitioners and physician’s assistants are, on the average, at least as successful as, and sometimes more successful than, physicians at diagnosing and treating minor illnesses. They also help keep costs down and reduce waiting time.
For every patient there is a Dr. Right. Once you know what kind of physician in what type of practice you’re looking for, you’re ready to start tracking yours down. Some communities have an on-line service for matching physicians and patients; if yours doesn’t, you’ll have to rely on more traditional, but usually reliable, sources:
Your obstetrician or midwife. Doctors generally recommend other doctors whose style and philosophy are similar to their own, whose work they are familiar with and respect. So if you’ve been happy with your pregnancy practitioner, ask for a suggestion. On the other hand, if you’ve been disappointed, look elsewhere for a recommendation.
An obstetric or pediatric nurse. If you know a nurse who works with pediatricians, in either an office or hospital setting, he or she is sure to be a good source of information on which doctors are competent, conscientious, caring, and relate well both to parents and children. If you don’t know a nurse, consider phoning the nursing station on the pediatric floor or the nursery at the hospital where you’re going to deliver to seek recommendations.
Parents. No one can tell you more about a doctor’s bedside manner than his or her satisfied (or dissatisfied) patients, or in this case, parents of patients. Recommendations are best when they come from friends or acquaintances who mirror you in temperament and child-rearing philosophy. Otherwise, the very qualities that make them swear by their pediatrician may make you want to swear at him or her.
The local medical society. While these organizations won’t recommend one physician over another, they will be able to provide a selection of reputable pediatricians in your area for you to choose from.
Hospital or other referral services. Some hospitals, medical groups, and entrepreneurs have set up referral services to supply the names of doctors in specific specialties. Hospitals recommend doctors who have privileges at their own institution; a referral service may be able to provide, in addition to information about a physician’s specialty, training, and board certification, information on whether or not he or she has been sued for malpractice.
Medical directories. The American Medical Directory and the Directory of Medical Specialties, often available at your public library or doctor’s office, or on-line at www.ama-assn.org/aps/amahg.htm, are other basic sources of prospects, providing a way to check credentials (education, training, and affiliations are all listed).
La Leche League. If breastfeeding is a priority, your local La Leche chapter (see the phone book or visit www.laleche league.org) can supply you with names of pediatricians who are particularly supportive of and knowledgeable about breastfeeding.
Health insurance provider. Your HMO or health insurance provider will likely give you a list of physicians available to you under your insurance plan.
The Yellow Pages. As a last resort, check under “Pediatrics” or “Family Practice” in the “Grouped by Practice Guide” under “Physicians” in your telephone directory. But keep in mind that these listings are incomplete; many doctors, particularly those who already have thriving practices, opt not to advertise in the Yellow Pages.
Procuring a list of names from any of the above sources is a good beginning in your search for Dr. Right. But to narrow down that list to a smaller one of candidates made of the “Right” stuff, and finally, to that one practitioner of your health care dreams, will take a little more investigative phoning and legwork, and personal interviews with a few finalists.
Hospital affiliation. It’s a definite plus if the doctor you choose is affiliated with a nearby hospital so that emergency treatment will be easily accessible. And it’s nice if that doctor has privileges at the hospital where you are planning to deliver so that he or she can examine your baby before discharge. But don’t eliminate from the running a good candidate who doesn’t have such an affiliation. A staff doctor can perform the hospital exam and arrange for discharge, and you can take baby to see the chosen doctor after you’ve left the hospital.
Credentials. A Harvard sheepskin looks great on the office wall, but even more important is a residency in pediatrics or family medicine and board certification by either the American Board of Pediatrics (ABP) or the American Board of Family Practice (ABFP).
Some doctors charge a fee for a consultation, others don’t. During your seventh or eighth month of pregnancy, make appointments with those on your short list and arrive ready to evaluate your prospective baby doctor, taking into account the following:
Office location. Lugging a size-42 belly with you everywhere you go may seem like a struggle now, but it’s traveling light compared to what you’ll be carrying around after delivery. Going unwalkable distances will require more planning than just hopping on a bus or subway or into a car, and the farther you have to go, particularly in foul weather, the more complicated outings will become. When you’re dealing with a sick or injured child, a nearby office is not just a convenience; it can also mean faster care and treatment. But when you make your decision, keep in mind: A truly one-of-a-kind practitioner may be worth a lengthier trip.
Office hours. What constitutes convenient office hours will depend on your own schedules. If one or both of you have 9-to-5 jobs, some early morning, evening, or weekend hours may be a major requirement.
Atmosphere. You can tell a lot about the atmosphere of an office before you even see it. If you’re treated curtly on the phone, chances are in-office experiences won’t be any more pleasant. If, on the other hand, you’re greeted by a cheerful welcoming voice, you’re likely to be met with concern and kindness when you come in with a sick, injured, or anxious child. You can gain further insight when you make your first visit to the office for an interview with the doctor. Is the receptionist friendly, or is her manner crisp and sterile? Is the staff responsive to and patient with its young clients, or is communication with them limited to “Get down,” “Don’t touch,” and “Keep quiet”?
Decor. A baby doctor needs more than a couple of magazines on the table and a few Expressionist prints on the wall to make the “Right” design statement in the waiting room. On your reconnaissance visit, look for features that will make waiting less painful for both you and your expected: a comfortable play area for toddlers as well as a waiting area for older children (if space permits); a selection of clean, well-maintained toys and books appropriate for a range of ages; low chairs or other sitting space designed for little bodies. Wallpaper in bold colors and intriguing patterns (orange kangaroos and yellow tigers rather than tastefully understated earth tones) and bright pictures (in both the waiting room and the examining rooms) will also give uneasy minds something comforting to focus on while anticipating or experiencing the poking and prodding of a checkup. (But keep in mind, not every good doctor is a Disney buff.) A welcome addition in the family practitioner’s office: separate waiting areas for adults only and adults with children.
Waiting time. A forty-five-minute wait when you’re pacing with a fussy infant or trying to distract a restless toddler with yet another picture book can be a trying experience for all involved. Yet such waits are not uncommon when the office is really busy. For some parents a long wait may merely be an inconvenience; for others it is something their schedules simply can’t accommodate.
In trying to gauge the average waiting time in a particular office, don’t go by how long you’re kept waiting for your consultation. Such visits are a courtesy, rather than a medical necessity; screaming infants or sick children will (and should) take priority. Instead, ask the receptionist, and if her answer is vague or noncommittal, pose the question to a few waiting parents.
A long average wait can be a sign of disorganization in the office, of over-booking, or of a doctor’s having more patients than he or she can handle. But it doesn’t tell you much about the quality of medical care. Some very good doctors are not very good managers. They may end up spending more time with each patient than allotted (something you will appreciate in the examining room but not in the waiting room). Or they may not like to turn down requests to fit sick children into an already full schedule (something you will definitely appreciate when it’s your child who’s sick).
All waiting doesn’t take place in the waiting room. The most uncomfortable wait is often in the examining room, holding an unhappy, undressed baby, with no space to pace, or trying to distract a frightened toddler without benefit of the toy collection just outside. While long waits in the examining room may not alone be sufficient reason for rejecting a doctor, if they do prove to be a problem, be sure to make a point of letting the nurse know that you would prefer to do most of your waiting in the waiting room.
House calls. Yes, a few pediatricians and family practitioners still make them. Most of the time, however, as your doctor will probably explain, house calls are not only unnecessary, they aren’t best for baby. At the office, a doctor can use equipment and perform tests that can’t be stashed in a little black bag. Still, occasions may arise when you will appreciate very much the doctor who is willing to put his or her bedside manner to work literally—as when junior is home from nursery school with a bad stomach flu, baby’s down with a high fever and a bronchial cough, and you’re on duty at home alone in a snowstorm.
Protocol for taking phone queries. If new parents rushed to the doctor’s office every time they had questions about their babies’ health or development, their medical bills would skyrocket and physicians’ offices would be jammed day and night. That’s why most queries are answered and worries assuaged via the telephone. And why you’ll want to know in advance how your prospective baby doctor handles such calls. Some parents prefer the call-hour approach: A particular time is set aside each day for the doctor to field phone calls. No patients are seen during this time and distractions are few. This ensures almost immediate access to the doctor—though there may be several bouts with a busy signal or a brief wait for a callback. Other parents find it difficult to confine their worries to between 7 and 8 in the morning or 11 and noon, or worse, to wait until tomorrow’s call hour for relief from today’s worries. They prefer the doctor callback system: They call when a problem or question arises, and the doctor calls back when there’s a free moment between patients. Even if the callback doesn’t come for hours (in a nonemergency, of course), callers can at least unburden themselves on—and sometimes be reassured or counseled by—the person who takes the call. And there is the comfort of knowing they will talk to the doctor by the end of the day. Another option some pediatricians use is a nurse call service. With this system, on-call nurses answer common parent questions and dispense advice, passing on to the physician only more urgent or complicated medical issues. Still another, less common, option that a few practitioners employ is e-mail.
How emergencies are handled. When accidents happen—and they will—how your doctor handles emergencies will be of some consequence. Some doctors instruct parents to take emergencies straight to the emergency room at the local hospital, where the ER staff can provide treatment. (Some health insurance plans require patients to call their doctor before heading for the emergency room.) Others ask you to call their office first and, depending on the nature of the illness or injury, will see your baby in the office or meet you at the ER. Some physicians are available (unless they’re out of town) days, nights, and weekends for emergencies. Others use colleagues or partners to cover for them during off-hours.
Hospitalization. Thankfully, most children are never hospitalized. But in the unlikely event that your child does have to be admitted to a hospital, you’ll need to know which one the practitioner of your choice is affiliated with. Some hospitals are better equipped to care for sick children than others are (children’s hospitals are usually best, but they aren’t available in every neighborhood). You’ll also want to find out who would take care of your child in the hospital—your chosen physician or a hospital-based one?
Financial matters. For all except the very wealthy and the very heavily insured, how financial matters are handled is a prime consideration. Some offices request payment at the time of a visit (unless other arrangements are made in advance); others issue bills. Some offices offer a package deal for first-year care that covers any number of visits. Though the package costs more than the sum of fees for the year’s scheduled number of checkups, it is usually a good gamble: You will break even with two or three sick visits and come out ahead with more. Insurance reimbursements for sick visits, package deal or no, will be handled according to the terms of your coverage.
Payment schedules are also available in some offices, either routinely or under special circumstances, such as when financial hardship exists. If you anticipate needing such an arrangement, discuss this with whoever is in charge of billing.
Particularly if finances are tight, you might also want to ask whether routine lab work is done in the office; if so it will probably cost you less than tests sent to an outside laboratory.
Style. When you’re in the market for a doctor, as when you’re shopping for baby furniture, the style that’s right will depend on your style. Do you prefer a doctor who is easygoing and informal, formal and businesslike, or somewhere in between? Are you most comfortable with a father (or mother) figure, or with a doctor who treats you as a partner in your child’s care? Do you want a doctor who gives the impression of having all the answers, or one who is willing to admit, “I don’t know, but I’ll find out.”
As health maintenance organizations (HMOs) and other prepaid group medical insurance plans proliferate, more and more families are losing the right to choose their physicians. There may be only one pediatrician, or one obstetrician, or one family practitioner in their neighborhood on the “list.” If you find yourself in that position and are unhappy with the care given by the doctor assigned, let both your employer (or your spouse’s) and the health plan director know. Be specific in your complaints, but not argumentative. Your aim should be to improve the quality of health care offered by the plan and, thereby, the care your baby receives. If your complaint doesn’t effect a change, perhaps you can persuade the employer to switch to a different plan.
Just as there are certain features all parents look for in a crib or stroller (quality, workmanship, value), there are certain traits they all want in a prospective baby doctor: the ability to listen (without eyeing the next name in the appointment book); an openness to questions and a willingness to respond to them fully and clearly (without becoming defensive or feeling threatened); and, most of all, a genuine fondness for children.
Philosophy. Even in the best of marriages, spouses don’t always agree, and even in the best of doctor-patient relationships there may be points of difference. But, as with marriages, doctor-patient relationships are most likely to succeed if both partners agree on a majority of major issues. And the ideal time to find out whether you and your prospective baby doctor’s philosophies mesh is at your consultation interview, before you make a commitment.
Ask about the doctor’s positions on any of the following that you consider important:
 Breastfeeding. If you’re eager to nurse, a doctor who is only lukewarm toward or confesses to little knowledge of the subject may not provide the support and assistance novice nursers need.
Breastfeeding. If you’re eager to nurse, a doctor who is only lukewarm toward or confesses to little knowledge of the subject may not provide the support and assistance novice nursers need.
 Early release from the hospital. If you’d like to head home early, you’ll want a pediatrician who’ll accommodate your wishes and sign baby out with you, assuming all is well. (But not one who is so accommodating to your wishes that he or she puts them before baby’s best interest.)
Early release from the hospital. If you’d like to head home early, you’ll want a pediatrician who’ll accommodate your wishes and sign baby out with you, assuming all is well. (But not one who is so accommodating to your wishes that he or she puts them before baby’s best interest.)
 Circumcision. Whether you’ve decided for or against, you’ll want a doctor who will respect your choice.
Circumcision. Whether you’ve decided for or against, you’ll want a doctor who will respect your choice.
 Vegetarianism. If you and your family don’t eat meat or fish, it’s useful to have a doctor who not only accepts that but also knows something about meeting a growing child’s nutritional needs on a vegetarian or vegan diet.
Vegetarianism. If you and your family don’t eat meat or fish, it’s useful to have a doctor who not only accepts that but also knows something about meeting a growing child’s nutritional needs on a vegetarian or vegan diet.
 Preventive medicine. If you believe in more than an ounce of prevention, it’s a good idea to select a doctor who shares that philosophy—emphasizing the “well” in baby care (good nutrition, physical activity, immunizations, and so on).
Preventive medicine. If you believe in more than an ounce of prevention, it’s a good idea to select a doctor who shares that philosophy—emphasizing the “well” in baby care (good nutrition, physical activity, immunizations, and so on).
 Antibiotics. It’s a good idea to select a doctor who’s up-to-date on the latest recommendations for when and how often to prescribe antibiotics. Research indicates that many doctors prescribe antibiotics too frequently, often when the situation doesn’t warrant it (usually at the parents’ request).
Antibiotics. It’s a good idea to select a doctor who’s up-to-date on the latest recommendations for when and how often to prescribe antibiotics. Research indicates that many doctors prescribe antibiotics too frequently, often when the situation doesn’t warrant it (usually at the parents’ request).
 Complementary and alternative medicine. If a more holistic approach to your family’s health care is important to you, look for a doctor who is familiar with alternative and complementary medicine and open to incorporating nonconventional therapies that are safe and effective into your child’s care.
Complementary and alternative medicine. If a more holistic approach to your family’s health care is important to you, look for a doctor who is familiar with alternative and complementary medicine and open to incorporating nonconventional therapies that are safe and effective into your child’s care.
Once you’ve settled on a doctor for your baby, there are probably a number of issues—many of which are examined in this chapter and the next—that you’ll want to discuss in a consultation, among them:
Your obstetrical history and family health history. What impact will these have on the upcoming delivery and on your new baby’s health?
Hospital procedures. What medication will be used in baby’s eyes to prevent infection? Which tests are routine after birth? How will jaundice be handled? What are the criteria for early discharge?
Circumcision. What are the pros and cons? Who should perform the procedure and when, if you do opt for it? Will local anesthesia be used?
Breastfeeding. How can your baby’s doctor help you get a good start? Will he or she make sure you’ll be able to nurse in the delivery room? Can he or she give orders to prohibit the use of pacifiers and supplementary bottles in the nursery and to facilitate demand feeding if you don’t have rooming-in? Can an extra office visit at one or two weeks postpartum be arranged if you’re having difficulty nursing or want to assess your progress?
Bottle feeding. What type of bottles, nipples, and formula does the doctor recommend?
Baby supplies and equipment. Get recommendations on health supplies such as acetaminophen, thermometer, and diaper rash ointment, and equipment such as car seats.
Suggested reading. Are there any books and/or videos the doctor would like to specifically recommend, or to steer you away from?
Office etiquette. What should you know about the way the doctor’s office operates—for instance, the times that calls are taken or how emergencies are handled?
Once you’ve chosen Dr. Right, you can’t just drop your baby’s health care into his or her lap, sit back with a waiting room magazine, and relax, assured of the right results. As parents, you, and not your doctor, have the most significant impact on your baby’s health. If you don’t hold up your part of the partnership, even the best of doctors won’t be able to provide the best of care for your baby. To be the right patient-parent for Dr. Right, you have a long list of responsibilities.
Follow office etiquette. Arrive for appointments on time or, if the office perpetually runs late, call half an hour in advance of a scheduled appointment and ask how much later you can safely arrive; try to give at least twenty-four hours’ notice when canceling; and keep to arranged payment agreements. Remember, patients (or in this case, parents of patients) are partly responsible for the smooth operation of a doctor’s office.
Practice prevention. Though it’s wise to select a baby doctor who believes in preventive medicine and concentrates on well-baby care, the burden for keeping baby healthy will fall more heavily on you than on the physician. It’s you who must see that baby gets proper nutrition, enjoys a wholesome balance of rest and active play, is not exposed unnecessarily to infection or cigarette smoke, and is kept as safe as possible from accidental injury. It’s you who must help your baby establish good health and safety habits that can last and give benefit for a lifetime.
Put your worries on paper. Many of the questions you’ll come up with between checkups are worthy of your concern without being worthy of a special phone call (“Why doesn’t he have any teeth yet?” or “How can I get him to enjoy his bath?”). Jot these down as they occur to you, before they have a chance to escape in the course of a typically hectic day with baby. Then ask them at your next visit.
Take notes. The doctor gives you instructions about what to do if your baby has a reaction to her first shots. You get home, she has a fever, and you panic. What was it she said? It’s not surprising you’ve forgotten—the baby was crying after the shot and you could barely hear the instructions as you struggled to dress her, never mind remember them. The remedy for parental memory loss: Always bring a pen and paper to your doctor visits and jot down diagnoses, instructions, and any other information you may want to refer to later. This may not be easy while balancing baby on your lap (that’s why two-parent visits are ideal), but it’s worth the contortions that may be involved. Or, ask the doctor or nurse if they can jot down some of the information for you.
Take notes at telephone “visits,” too. Though you’re positive you’ll remember the name of the over-the-counter ointment the doctor recommended for baby’s rash or the dosage of acetaminophen prescribed for teething pain, these details can easily escape your mind when you hang up the phone to the sight of baby smearing sweet potatoes all over the kitchen wall.
Pick up the phone. Thanks to Alexander Graham Bell, the relief for your worries is only a phone call away. But don’t use your baby’s doctor as a ready reference; before making a call, try to find the answers to your questions in this or in another baby book on your shelf. If you’re unsuccessful, however, don’t hesitate to call for fear of abusing your telephone privileges. In the early months, baby doctors expect a lot of telephone calls, especially from first-time parents. Don’t call cold, however. Make the most of the conversation by glancing over the Before Calling the Doctor checklist starting on page 532 and call prepared.
Follow doctor’s advice. In any good partnership, both sides contribute what they know or do best. In this partnership, your baby’s doctor will be contributing years of training and experience. To get the most benefit from those contributions, it makes sense to take the doctor’s advice when feasible, and to inform him or her when you don’t intend to, or for some reason, can’t. This is particularly vital in medical situations. Say an antibiotic has been prescribed for baby’s earache. The baby spits up the medication and won’t touch another drop. Since the earache seems better anyway, you give up trying to force it down his or her little throat and don’t bother to let the doctor know. Then, two days later, baby’s temperature is up. What the doctor would have told you, had you called, is that once the medication is begun the baby may start to improve, but unless the full course of treatment is completed, the illness can return with greater force. He or she might also have been able to advise you on better ways of getting the medication down or of alternative ways of medicating.
Speak up. To say that it’s important to follow doctor’s advice is not to say that mother or father doesn’t sometimes know best—even better than doctor. Sometimes, parental instincts are as keenly accurate in picking up symptoms of illness as any instrument in a doctor’s black bag. If you sense the doctor’s diagnosis or treatment is off, say so (calmly and rationally, not in a challenging way). You may learn something from each other.
Speak up, too, if you’ve heard about a new treatment for colic or for runny noses, or anything else that you feel might benefit your baby. If it’s something you’ve read, bring in the source when possible. Perhaps the doctor has already heard about this advance and can give you additional information for or against it. If the doctor is unfamiliar with it, he or she will probably want to learn more about it before offering an opinion. Be aware, however, that medical reporting (especially on the Internet) can be uneven. With your doctor’s help, you should be able to sort out the useful from the useless.
End a relationship that’s not right.
There’s no such thing as a perfect doctor (any more than there’s such a thing as a perfect parent). And, again, even in the best of partnerships, there’s bound to be some disagreement. But if there seems to be more discord than harmony, try talking things out with the doctor before you consider ending the relationship. You may find that there’s a misunderstanding rather than serious philosophical differences behind the rift, in which case you may be able to make a fresh start with the same doctor. If the physician you’ve chosen turns out to be truly Dr. Wrong, you will begin the search for a new doctor a lot wiser and, hopefully, end up with better results. To make sure you don’t leave your baby without a doctor while you shop around again, avoid terminating your current relationship until you’ve found a replacement. When you have, be sure all of your child’s medical records are transferred promptly.

1. Soy milks, however, are not nutritionally adequate and should not be used for infant feeding. Neither is cow’s milk; babies should be fed formula only.
2. If you develop an infection while nursing, by the time the diagnosis has been made, the baby has already been exposed. Continue nursing so your baby receives your antibodies from your breast milk.
3. If prenatal diagnosis or family history suggests you may have a baby with a specific health problem (Down syndrome, allergies, asthma), you might consider choosing a pediatrician or family practitioner with special interest or expertise in caring for children with that kind of problem.