MARK S. GOLDBERG, GEOFFREY GARVER, AND NANCY E. MAYO
1. INTRODUCTION
Since the 1990s, the notion of “ecosystem health” has become prominent in the ecological literature (Aguirre et al. 2002; Costanza, Norton, and Haskell 1992; Jørgensen, Xu, and Costanza 2010; Rapport et al. 1998; Scow et al. 2000). A main motivation for the definition and use of the concept of “ecosystem health” was to provide a uniform framework for assessing the state and function of ecosystems and for managing ecosystems using knowledge that can be integrated from various disciplines (Rapport 1998b). Its relevance to ecological economics is clear: essential indicators of ecological function and their states are required in order to monitor unbridled human activities and to ensure that severe stress and destruction of ecosystems is monitored, avoided, and (where necessary) mitigated.
Rapport (1998a) discussed the strengths and limitations of using the human health metaphor. He indicated that ecosystem health can be defined operationally and quantitatively. It can be used for a systematic diagnosis of systems that are in stress, especially for the understanding of etiology; it also can be used both for the purposes of remediation and prevention. Nonetheless, he recognized that this metaphor cannot be used simply and would need to include multiple determinants of stress and disease. Indeed, Jørgensen (2010:3) indicated that “it is clear today that it is not possible to find one indicator or even a few indicators that can be used generally, as some naively thought when ecosystem health assessment … was introduced.”
Although the metaphor of ecological health is derived from its application to individual humans and human populations, it does not appear that an in-depth exploration of the paradigm of human health has been discussed in the ecological literature, although VanLeeuwen et al. (1999) provided a model whereby human health is embedded within the planet. This chapter emerged from an inquiry into how the health metaphor might be used to facilitate discussion of regional and global ecological boundaries that must be used to limit human activities. Even a superficial exploration of either the human health or ecological health literature shows that there has been much debate over the use of the metaphor. Such a review raises the question of whether the term “health” is truly useful, and, if so, under what circumstances it can be applied appropriately.
It appears that this metaphor or analogy was taken originally from human medicine. Some of the earliest writings on the subject suggest that the essential aspect relates to a physician diagnosing a disease in an individual using a set of measurements, mostly at the physiological level. For example, Jørgensen (2010) stated that “we go to a doctor to get a diagnosis … and hopefully initiate a cure to bring us back to normal (or healthy conditions). Doctors will apply several indicators/examinations (pulse, blood pressure, sugar in the blood, and urine, etc.) before they come up with a diagnosis and proper cure.” The purpose is practical and very important—a serious problem is identified, a clear diagnosis is made, the causes are identified, and remediation and subsequent management are affected.
A relatively simple case in ecology can be used to illustrate the parallels to human health. Consider the ramifications of treating agricultural runoff in a lake. Specific measurements are made to identify the extent of the eutrophication of the lake. The investigation reveals that the excess nitrogen and phosphorous entered the lake from runoff of adjoining farmlands and other sources. A straightforward solution is to reduce the use of fertilizers and associated runoff, although this is not trivial to implement. Räike et al. (2003) in Finland showed the effectiveness of control measures, finding that decreased loadings were observed after control measures were taken to reduce emissions from wastewater treatment plants and pulp and paper operations, as well as to reduce the use of nitrogen and phosphorous fertilizers among farmers. Other examples may involve less obvious signs of damage and may have multiple interacting factors operating through different pathways and with effects of different magnitude. Diagnosis and remediation are thus complex. The hope of using the metaphor of ecological health is that it will stimulate an interdisciplinary approach, making “diagnosis” and “treatment” more effective.
We show below that human health is far more than the absence of specific diseases, and that sole reliance on physiological indicators does not provide a means for its definition or its measurement. Indeed, human health is an elusive concept that defies a simple, comprehensive definition; it comprises so many dimensions that to define it, especially in quantitative terms, is essentially impossible. Measurement in humans of the vast panoply of indicators is problematic: in almost no situations that we are aware of would all aspects of health be measured in a particular individual. We discuss briefly some of the means by which various aspects of human health are measured, and some of the essential characteristics of these measurements. We thus argue that applying the analogy to ecosystems—which are of course not organisms but complex, hierarchical systems—has significant difficulties. In particular, the field of inquiry that is concerned with the measurement of indicators of function in an ecosystem defines the field of “ecosystem health,” but we conclude that measurement of selected indicators cannot be used to imply health, although they may imply lack of health. We also make some suggestions, which have been made previously by others, regarding the measurement of “states” in ecosystems.
2. A COMMENTARY ON THE METAPHOR OF ECOSYSTEM HEALTH AS DERIVED FROM HUMAN HEALTH: MEASUREMENT OF DISEASE VERSUS CAPACITY TO FUNCTION
2.1. The Role of Physicians
The primary role of physicians is to “find it and fix it.” They are trained to identify and treat pathologies that require attention and remediation. For example, in the context of a routine visit to a general practitioner, often a standard physical examination will be conducted, evaluating such things as enlarged lymphatic glands and obvious breathing and heart abnormalities. The physician may ask questions regarding health and complaints, which may assist in uncovering specific problems. The history of the patient is important because previous illnesses will factor into the interpretation of the examination; results from previous tests are often reviewed.
In addition, a number of essential physiological measurements may be taken, including such things as height, weight, pulse rate, pupil size, blood pressure, and body temperature; blood tests also may be ordered. Many of the blood tests can serve as markers for specific bodily functions, such as liver function (through assays that measure liver-related enzymes). Most indicators have “normal” ranges that are defined from observations of distributions in “healthy” populations. Temperature, blood pressure, pulse rate, and respiration rate are essential vital signs. Within the context of a specific investigation, other tests may be ordered. There are many indicators that are not measured routinely, especially those that may predict future health, such as plaque in the blood vessels, arterial elasticity, and lung function. Lung function is a strong predictor of mortality in the distant future (Sabia et al. 2010); however, in routine clinical practice, only people showing frank lung dysfunction (e.g., chronic bronchitis, emphysema, or asthma) would be tested and usually only by a respirologist.
In “healthy” individuals, it would be expected that some prime physiological indicators, such as blood pressure, resting heart rate, lipids in blood, and sugar in urine, would all be in the “normal” range. However, this only tells part of the story. For example, people with back pain whose activities of daily life are constrained may also have normal values of essential biomarkers. Some other conditions are episodic; for example, people with asthma may look normal on pulmonary function tests when they are not experiencing an exacerbation, but they will appear abnormal during a crisis. In addition, there are conditions that show exacerbations and remissions during the course of life but may also be life-shortening (e.g., multiple sclerosis).
Human health certainly is affected by exogenous influences or contaminants, such as air pollution, excess sunlight, and Escherichia coli in a food product. However, many human illnesses are endogenous, arising from failure at the cellular, tissue, or organ level—often for unknown reasons. An ecosystem also has exogenous and potentially endogenous influences, such as acid rain (exogenous) and overpopulation of a species (endogenous).
Physicians have little to do with general matters of individual health, other than possibly suggesting to their patients that they should exercise or eat properly. Other indicators of consequence that are investigated rarely by general practitioners include the ability to conduct activities of daily living, levels of stress, and mental health. There are some medical specialties that deal with larger issues; for example, sports medicine physicians are concerned about musculoskeletal health and are quite attuned to providing support for rehabilitation and prevention of injury through an interaction with other health professionals, such as physiotherapists and athletic therapists. Occupational physicians are concerned with causes of disease and are trained to identify those that have origins in the workplace.
Physicians have little to do with the development of population health, which is a matter of public and societal issues.1 For example, the increase of diabetes in North America and elsewhere (Lipscombe and Hux 2007) is related in part to the fragmentation of our cities, so that transportation is mostly via the automobile, as well as to our consumer-based society that leads to overeating and general sedentariness, especially in children (Gortmaker et al. 1996). Physicians come late in the process in trying to deal with the complications of obesity, which include diabetes and heart disease. Other examples abound, including exposure to air pollution that causes manifold health problems (Chen, Goldberg, and Villeneuve 2008), ultraviolet light causing skin cancer (Leiter and Garbe 2008), and disinfection byproducts in water associated with the incidence of cancer (Richardson et al. 2007). The instruments that have been developed to measure various components of “health” come not from medicine but from allied fields that deal with outcomes, such as epidemiology.
2.2. The Role of Allied Health Fields in Measuring Indicators of Health
A number of indicators are used by nonphysicians to go beyond the measurement of specific physiological and pathological biomarkers. Indicators of health include freedom from symptoms of pain, fatigue, and emotional distress; the ability to carry out activities that are necessary for daily life (e.g., dressing, personal hygiene, moving around the home or community, purchasing and preparing food, maintaining a home); and engagement in family, social, and economic roles. Many tests and questionnaires exist to measure these aspects of health; some of these are tailored for specific subgroups of the population, such as the elderly or children.
Many of these other measures also have reference values that are derived from population-based distributions or from benchmarks for safety. For example, a common measure of community mobility required for basic activities of daily living is how far a person can walk in six minutes (American Thoracic Society 2002). The value will indicate whether the person is performing as expected for their age and sex, but the value does not provide any indication as to why a person walks only that distance or whether the limitation is temporary or permanent. There are also self-reported measures of overall and specific mental health (e.g., happiness, anxiety, depression) as well other measures of activities of daily life (e.g., simple things such as being able to tie one’s shoes, recreational activities).
Many of these indices were developed to assess health in specific populations or situations, whereas others are of a more global nature that is applicable in many situations. In addition to having population norms, their validity (i.e., they measure what they purport to measure) and reliability (repeatability) are also assessed before they are put into widespread use.
There are also composite indicators of an individual’s health relative to a broader population of humans that are based on a number of constructs, with each construct defined by a series of questions. Two of the most widespread instruments are the Short-Form Health Survey (SF-36; Ware and Sherbourne 1992) and the Euroqol (Kind 1996). Questions are assigned numerical values and the calculation of an overall score is achieved by summing, or otherwise, the values of each item. There has been considerable progress in developing and validating these indicators so that their meaning has a grounded interpretation. They are often evaluated in “healthy populations” and the range of scores helps define what is defined as “normal,” providing a baseline by which to make comparisons. In addition, in formal studies comparisons between a group with some pathology, for example, will be compared to an otherwise comparable “healthy” one (e.g., comparing activities of daily life amongst those people with chronic back pain to those without). Thus, a complex numerical scale becomes meaningful. Nevertheless, as mentioned in chapter 4, acting on a disability in an individual requires specific knowledge of the problem, and it is only in evaluating the individual items in a complex indicator that the specific problem can be identified and treated.
Despite over a half a century of advancement in the measurement of health, markers of disease predominate the measures used in clinical practice. Often, the mismatch between what is measured clinically and how the person feels leads to suboptimal treatment and outcome. A person may show abnormally high levels of blood lipids but may feel very well; hence, he or she may not be motivated to start or continue with pharmacological therapy. Another person may feel very unwell but may not have markedly abnormal values on physiological parameters (a finding not uncommon with a condition such as fibromyalgia), and hence is dissatisfied with the lack of treatment or concern by the medical community.
In the health field, methods of measurement are now incorporating multiple indicators of health (most often measured on ordinal scales), calibrating the critical ordinal categories in a hierarchical manner, and creating measures that have interval-like properties. In this way, change in different aspects of health can be quantified and related to changes going at a cellular or organ level or at an environmental level (Andrich 2011).
2.3. Definitions of Human Health
The previous discussion indicates that physicians have a limited role in health: they can identify pathologies and some can be treated. As Richard Smith, a past editor of the British Medical Journal, wrote in a blog for that journal:
But what is health? For most doctors that’s an uninteresting question. Doctors are interested in disease, not health. Medical textbooks are a massive catalogue of diseases. There are thousands of ways for the body and mind to go wrong, which is why disease is so interesting. We’ve put huge energy into classifying disease, and even psychiatrists have identified over 4000 ways in which our minds may malfunction. Health for doctors is a negative state—the absence of disease. In fact, health is an illusion. If you let doctors get to work with their genetic analysis, blood tests, and advanced imaging techniques then everybody will be found to be defective—“diseased.” … So I’m not happy with health being defined as the absence of disease. Nor am I keen on the World Health Organisation’s definition of “Complete physical, psychological, and social wellbeing,” a state reached only at the moment of mutual orgasm, joked Peter Skrabanek. It’s a ludicrous definition that would leave most of us unhealthy most of the time. My favourite definition of the moment is Sigmund Freud’s definition, which was never written down by him, of “the capacity to love and work.”
(Smith 2008)
2.3.1. World Health Organization definition of health
In 1948, the World Health Organization (WHO) defined health as “a state of complete physical, mental and social well being, not merely the absence of disease or infirmity” (World Health Organization 1948). In 1986, WHO defined health as “a resource for everyday life, not the objective of living. Health is a positive concept emphasizing social and personal resources, as well as physical capacities” (World Health Organization 2006).
Richard Smith was not the only one to have issues with the WHO definition of health. Rodolpho Saracci argued that a serious pitfall with the WHO definition is that it does not discriminate between health and happiness (Saracci 1997). The connection with social well-being brings in the notion of happiness, so that any deviation from happiness, however defined (and like health, happiness is not trivial to define), implies a state of imperfect health. Larson (1999) discussed other problems with the WHO definition, including that there is no consensus on the meaning of well-being and social well-being; health is defined differently in different cultures; there is no clear ranking of health states; we all suffer from time to time from various complaints, so essentially no individual fits the definition; and the definition is so vague as to admit myriad ways to operationalize health. Larson (1999:123) also quoted other possible definitions, including that “health may be defined as the absence of illness, having strength and robustness, and high quality of life. It may be defined as quantity (length of life) and quality, or it may be defined as consisting of the absence of physical disability, psychological disability, and pain” (Brown et al. 1984; Feinstein 1992).
Larson (1999) discussed the conceptualization of health in terms of other models. Of interest is the wellness model that is “health promotion and progress toward higher functioning, energy, comfort, and integration of mind, body, and spirit” (Larson 1999:125, table 1). In this model, there is an integration with spiritual and mental functioning, having reserves to overcome illness, striving toward higher levels of functioning. VanLeeuwen et al. (1999) also discussed a number of models of human health, some of which were also discussed by Larson, that included ecological factors but also some of the concepts related to hierarchies found in nature. Their “butterfly model” embeds human health within the ecosystem (similar to ecological economics) and attempts to incorporate broad interacting links between the biophysical and socioeconomic environments.
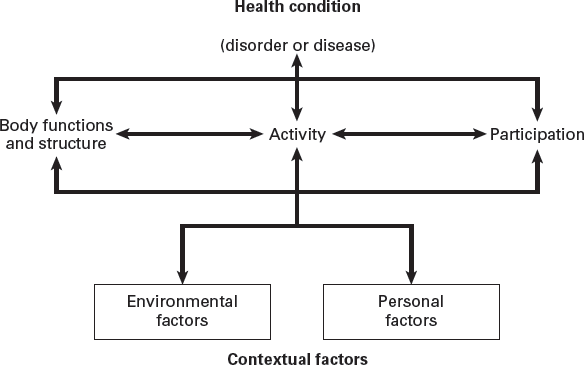
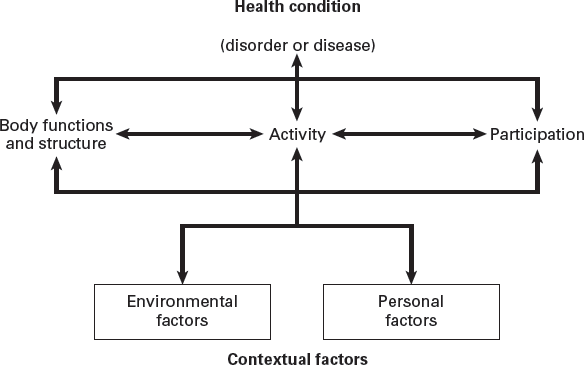
In response to these and other criticisms, the WHO developed a framework for defining constructs important to health: the International Classification of Functioning, Disability, and Health (World Health Organization 2014). The International Classification of Functioning, Disability, and Health is based on what is called a biopsychosocial model, which attempts an integration of the medical and social aspects of health. Figure 6.1 shows a conceptual model based on World Health Organization (2002).
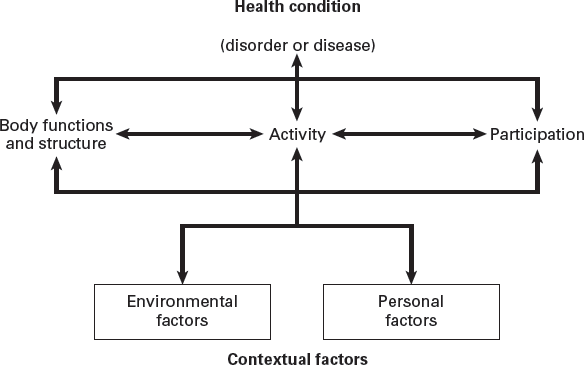
Figure 6.1. Conceptualization of the model of disability used in the International Classification of Functioning, Disability, and Health. The figure implies that disability and functioning result from the interaction of health conditions (diseases, disorders and injuries) and “contextual factors.” The contextual factors are distinguished by external factors, referred to as “environmental factors” that include social contexts and geographical and climatic ones and “personal factors” that relate to the individual (e.g., age, gender, education). These factors have a bearing on how individuals perceive disability, or lack of disability. The middle part of the box shows the main components of human function, and dysfunction relates to impairments (problems in body function or structure), limitations of physical activities, and limitations in participating in life activities. Source: World Health Organization (2002).
The International Classification of Functioning, Disability, and Health provides a unified and standard language and framework for the description of health and health-related states. It defines components of health, both positive (function) and negative (disability), and some health-relevant components of well-being. Constructs for disabilities, impairments, limitations, and restrictions are the objective and exteriorized signs of the individual, but what people “feel” about their function is considered akin to well-being. Measuring only well-being without measuring function, and vice versa, misses an essential dimension of the health of an individual, especially given that people adapt to poor function and a high degree of expressed well-being does not indicate need of care or services.
To summarize, although the definition of health by the WHO is cited widely, there is no singular definition of health. (Also, the model by which “one recognizes health when one sees it” is highly flawed; consider a person with latent lung cancer, who appears healthy one day and dies three months later.) Indeed, many models have been developed over time to attempt to capture various elements of human health. There have also been a number of instruments geared toward measuring different components of health, including the International Classification of Functioning, Disability, and Health, which is based mostly on the WHO definition; however, other instruments are also of considerable value (e.g., the SF-36 [Ware and Sherbourne 1992] and the Euroqol [Kind 1996]). Indeed, it is clear that the full spectrum of health goes beyond the internal signs, as reflected by physiological and pathological parameters measured by physicians; it even goes beyond the exteriorized signs of disability and includes the concept of “well-being”—or how a person “feels” about their health condition or its consequences. Moreover, health is an evolving process, and individuals change in different ways through time. In short, human health in its entirety cannot be measured in a specific individual and certainly not in groups.
3. DEFINITIONS OF ECOSYSTEM HEALTH
The original motivation was to understand the etiology of “stressed” ecosystems and to provide a global method of assessment. As described previously, the literature on ecosystem health has its roots in the paradigm of the physician diagnosing illness and disease in a patient (Jørgensen 2010; Rapport 1992; Rapport, Regier, and Hutchinson 1985). Indeed, Schaeffer (1996) wrote that “the four-step sequential process that must be accomplished in making a diagnosis of a human or animal disease … also applies to ecosystem diseases.” Rapport (1992) discussed the need to superimpose human values on the assessment of ecosystem health; he cited the example of indigenous forests in New Zealand being converted to plantations of radiata pine for the purposes of human exploitation, with conservationists arguing against this transformation. For the purposes of humans evaluating their effects on the biosphere, some sort of ethics is required. Perhaps, the “land ethic” of Aldo Leopold (1949) could be a starting point (see chapter 7).
Regardless of the ethics, there is no debate about the importance of identifying problems with ecosystems, uncovering their etiology, and carrying out remediation. Essential to this purpose is the ability to measure characteristics or states of ecosystems and making comparisons to “normal circumstances,” as we do with humans, or to map out temporal trends. Presence of disease, dysfunction, out of the “normal range” of key indicators, and statistical correlations showing relationships with metrics of ill-health (e.g., acid rain and the loss of fish stock in lakes) would indicate an ecosystem’s ill health; perhaps some cure could be prescribed to make the system right.
Some investigators have attempted to operationalize the concept of ecosystem health. For example, Costanza (1992) suggested that ecosystem health is “a comprehensive, multiscale, hierarchical measure of system resilience (Holling 1986), organization, and vigor.” He suggested that health is “a measure of the overall performance of a complex system that is built up from the behavior of its parts.” A definition, developed at a conference, was proposed: “An ecological system is healthy and free from ‘distress syndrome’ if it is stable and sustainable—that is, if it is active and maintains its organization and autonomy over time and is resilient to stress.” From this, Costanza defined an ecosystem health index that was the product of indices measuring vigor, organization, and resilience. In a follow-up to this paper, Costanza and Mageau (1999) described a definition of ecosystem health as follows: homeostasis, absence of disease, diversity or complexity, stability or resilience, vigor or scope for growth, and balance between system components. They extended these previous definitions to propose “ecosystem health as a comprehensive, multiscale, dynamic, hierarchical measure of system resilience, organization, and vigor”2 (Costanza and Mageau 1999:106).
This is somewhat analogous to the original WHO definition, with “well-being” replaced by resilience, organization, and vigor. Costanza and Mageau (1999:106) indicated that “system health implies a weighted summation or a more complex operation over the component parts, where the weighting factors incorporate an assessment of the relative importance of each component to the functioning of the whole. … In the practice of human medicine, these weighting factors or values are contained in the body of knowledge and experience embodied in the medical practitioner.” Unfortunately, this last statement is patently false, as clinicians do not provide a judgment as to the health of an individual but rather to the presence or absence of specific diseases and the possibility of cure or management.
Moreover, as discussed in chapter 4, complex indicators are in fact difficult to interpret because their values can be ambiguous.3 Although benchmarking (validation) can overcome these drawbacks, they would still need to be disaggregated for specific remedial actions. Also, combining indices in either a multiplicative or additive framework is fraught with difficulty: there is the unverifiable assumption that one can develop a meaningful complex index by some mathematical formula that combines disparate indices. Validation of such an index is required and, as in studies of human health, must be benchmarked. Lastly, such indices are exceedingly difficult to interpret.
In 1993, Suter (1993) criticized the notion of ecosystem health as follows:
1. It misrepresents health. He noted that the original WHO definition of health was indeed subjective and that physicians do not in fact measure health, as we have shown previously.
2. It misrepresents ecology. Ecosystems are not organisms (and certainly they do not have central nervous systems).
3. Definitions of ecosystem health, such Karr et al.’s (1986) Index of Biotic Integrity, combine indicators that are heterogeneous and, because they cannot be benchmarked, have no intrinsic meaning. To quote Suter (1993:1533, Abstract): “They cannot be predicted, so that they are not applicable to most regulatory problems; they have no diagnostic power; effects on one component are eclipsed by responses of other components [this is the main issue of combining in an arbitrary fashion indices that measure different constructs and have different units]; and the reason for a high or low value is unknown [the issue of variability from a statistical framework].”
Wicklum and Davies (1995:997, Abstract) were also critical of the concept:
“The phrase ecosystem health is based on an invalid analogy with human health requiring acceptance of an optimum condition and homeostatic processes maintaining the ecosystem at a definable optimum state. Similarly, ecosystem integrity is not an objective, quantifiable property of an ecosystem. Health and integrity are not inherent properties of an ecosystem and are not supported by either empirical evidence or ecological theory.”
As with human health, assessments of ecosystem function and states do not require a clear definition of ecosystem health. Indeed, Rice (2003:236) used the term “indicators of ecosystem status” rather than “indicators of environmental health.” He stated that “a review prepared three years ago … found over two-hundred different indicators of ecosystem status, without being exhaustive. The challenge is not to find an indicator of ecosystem status to use. It is to choose the set that will serve the users’ needs best.”
Jørgensen, Xu, and Costanza (2010) discussed criteria by which indicators should be selected from management and scientific points of view, including being simple to apply and understand, relevant, scientifically justifiable, quantitative, reasonable cost, easy to use, sensitive to small variations (i.e., in terms of the language used in our chapter on measurement, they should be valid and reliable), independent of reference states, and widely applicable. These authors indicated that few indicators meet all of these criteria.
The notion of developing orthogonal qualitative descriptors, or perhaps “properties,” to define various components of health is indeed analogous to what is done in human health. For example, we speak of mental health, physical health, quality of life, etc. As in human health, it is unlikely that resilience, organization, and vigor are the only set of descriptors. Jørgensen, Xu, and Costanza (2010) classified ecosystem indicators into eight “levels”: presence and absence of species, ratio of populations of classes of organisms, concentrations of chemical compounds, populations or concentrations in trophic levels, rates of essential processes, composite indicators (e.g., complex indicators such as Odum’s [1971] set of indicators), holistic indicators (these are also complex and refer to concepts such as resistance and resilience), and thermodynamic variables (e.g., exergy).
4. DISCUSSION AND CONCLUSIONS
We have shown that a definition of human health is elusive, and the various definitions that have been attempted have serious shortcomings. As well, the myriad attributes and domains that make up the concept of human health cannot be measured uniquely in any individual or in populations. It is clear that human health goes beyond the diagnosis of disease and that there are many inherent properties of human health, and most of these are never measured by physicians. In fact, physicians play almost no role in assessing health; they deal with pathology, remediation, and possible cure. Health professionals working in various fields have defined many indices to capture the various dimensions inherent in human health. One of the essential components in defining and developing these indices is to measure their validity and reliability. Complex indicators in human health have no meaning unless they are benchmarked.
The current concept of ecosystem health is plagued by the incorrect analogy of physicians as the lead players in defining human health, although ecologists acting as physicians to diagnose and correct pathology is of course correct and essential. Moreover, as indicated by Suter (1993) and others, ecosystems are not organisms. An implication to ecology is that complex indices that have been defined to measure ecosystem health do not and cannot measure all of the dimensions in complex ecosystems. This has been acknowledged by a number of other ecologists (e.g., Jørgensen, Xu, and Costanza 2010).
Because we are not ecologists, we would be rather bold to presume that we have any expertise in developing relevant indicators. Surely, however, as in any scientific discipline, the assessment of states of ecosystems must be based on defining clearly the objectives of the research or the issues related to management. The job is then to make measurements of all relevant parameters that reflect these objectives accurately, as well as to be wary of combining these parameters into complex indices that have no intrinsic meaning. De Leo and Levin (1997) suggested “that it is much more useful to characterize in detail the functional and structural aspects of ecosystems to provide a conceptual framework for assessing the impact of human activity on biological systems and to identify practical consequences stemming from this framework.”
Human populations have relatively little variability in their genomic constitution as compared to the constitutions of the myriad types and numbers of ecosystems on the planet. This means that humans are much more homogeneous than ecosystems, and the task of measurement and assessment in humans should be much easier than with ecosystems. Nevertheless, perhaps we can speculate that the model of human functioning, disability, and health could be used by analogy in assessing ecosystem function: each ecosystem can be considered to have a capacity to function, which may or may not be altered; given a specific level of capacity, each component of the ecosystem may or may not perform “optimally” in achieving the activities and roles for which they have evolved to do. Each component in the system is interdependent and forms an integral part of the environmental cloth for the whole ecosystem. This would provide a measurement framework for ecosystem health that would go beyond only the physiological. On the other hand, perhaps the classification system for indicators of ecosystems by Jørgensen, Xu, and Costanza (2010) may be sufficient.
The above functional assessments probably are more closely related to concepts of the health of ecosystems and less generally to planetary systems, although it is likely that one would still need an array of “physiological” parameters to fully characterize health. Moreover, the monitoring of these parameters in time and space would be needed. It is thus unlikely that a proper measure of ecosystem health could ever be achieved using one complex, integrated index.
NOTES
1. Unless they are working as epidemiologists or in public or occupational health.
2. The resilience of a system refers to its ability to maintain its structure and pattern of behavior in the presence of stress. The vigor of a system is simply a measure of its activity, metabolism, or primary productivity. The organization of a system refers to the number and diversity of interactions between the components of the system.
3. For example, let us consider a complex indicator obtained by multiplying two variables (A, B) together. Let us assume for simplicity that each are coded as 0, 1, 2, 3. The interpretation of this complex indicator is ambiguous because different combinations yield the same product: for example, A(=1) × B(=2) = 2 and A(=2) × B(=1) also equals 2. See chapter 4.
Aguirre, A. Alonso, Richard S. Ostfeld, Gary M. Tabor, Carol House, and Mary C. Pearl, eds. 2002. Conservation Medicine: Ecological Health in Practice. Oxford: Oxford University Press.
American Thoracic Society. 2002. “ATS Statement: Guidelines for the Six-Minute Walk Test.” American Journal of Respiratory and Critical Care Medicine 166 (1): 111–117. doi: 10.1164/rccm.166/1/111.
Andrich, David. 2011. “Rating Scales and Rasch Measurement.” Expert Review of Pharmacoeconomics & Outcomes Research 11 (5): 571–585. doi: 10.1586/erp.11.59.
Brown, J. H., L. E. Kazis, P. W. Spitz, P. Gertman, J. F. Fries, and R. F. Meenan. 1984. “The Dimensions of Health Outcomes: A Cross-Validated Examination of Health Status Measurement.” American Journal of Public Health 74 (2): 159–161. doi: 10.2105/AJPH.74.2.159.
Chen, Hong, Mark Goldberg, and Paul J. Villeneuve. 2008. “A Systematic Review of the Relation between Long-Term Exposure to Ambient Air Pollution and Chronic Diseases.” Reviews on Environmental Health 23 (4): 243–298. doi: 10.1515/REVEH.2008.23.4.243.
Costanza, Robert. 1992. “Toward an Operational Definition of Ecosystem Health.” In Ecosystem Health: New Goals for Environmental Management, edited by Robert Costanza, Bryan G. Norton and Benjamin D. Haskell, 239–256. Washington, DC: Island Press.
Costanza, Robert, and Michael Mageau. 1999. “What Is a Healthy Ecosystem?” Aquatic Ecology 33 (1): 105–115. doi: 10.1023/A:1009930313242.
Costanza, Robert, Bryan G. Norton, and Benjamin D. Haskell, eds. 1992. Ecosystem Health: New Goals for Environmental Management. Washington, DC: Island Press.
Feinstein, Alvan R. 1992. “Benefits and Obstacles for Development of Health Status Assessment Measures in Clinical Settings.” Medical Care 30 (5): MS50–MS56. doi: 10.2307/3766229.
Gortmaker, S. L., A. Must, A.M. Sobol, K. Peterson, G. A. Colditz, and W. H. Dietz. 1996. “Television Viewing as a Cause of Increasing Obesity among Children in the United States, 1986–1990.” Archives of Pediatrics & Adolescent Medicine 150 (4): 356–362. doi: 10.1001/archpedi.1996.02170290022003.
Holling, C. S. 1986. “The Resilience of Terrestrial Ecosystems.” In Sustainable Development of the Biosphere, edited by W. C. Clark and R. E. Munn, 292–320. Cambridge, UK: Cambridge University Press.
Jørgensen, Sven Erik. 2010. “Introduction.” In Handbook of Ecological Indicators for Assessment of Ecosystem Health, edited by Sven Erik Jørgensen, Fu-Liu Xu, and Robert Costanza, 3–7. Boca Raton, FL: CRC Press.
Jørgensen, Sven Erik, Fu-Liu Xu, and Robert Costanza, eds. 2010. Handbook of Ecological Indicators for Assessment of Ecosystem Health. 2nd ed. Boca Raton, FL: CRC Press.
Karr, James R, Kurt D Fausch, Paul L Angermeier, Philip R Yant, and Isaac J Schlosser. 1986. Assessing Biological Integrity in Running Waters: A Method and Its Rationale. Champaign, IL: Illinois Natural History Survey.
Kind, Paul. 1996. “The Euroqol Instrument: An Index of Health-Related Quality of Life.” In Quality of Life and Pharmacoeconomics in Clinical Trials, edited by Bert Spilker, 191–201. Philadelphia: Lippincott-Raven.
Larson, James S. 1999. “The Conceptualization of Health.” Medical Care Research and Review 56 (2): 123–136. doi: 10.1177/107755879905600201.
Leiter, Ulrike, and Claus Garbe. 2008. “Epidemiology of Melanoma and Nonmelanoma Skin Cancer—the Role of Sunlight.” In Sunlight, Vitamin D and Skin Cancer, edited by Jörg Reichrath, 89–103. New York: Springer. doi:10.1007/978–0-387–77574–6_8.
Leopold, Aldo. 1949. A Sand County Almanac and Sketches Here and There. New York: Oxford University Press.
Lipscombe, Lorraine L., and Janet E. Hux. 2007. “Trends in Diabetes Prevalence, Incidence, and Mortality in Ontario, Canada 1995–2005: A Population-Based Study.” The Lancet 369 (9563): 750–756. doi: 10.1016/S0140–6736(07)60361–4.
Odum, Eugene. 1971. Fundamentals of Ecology. Philadelphia: Saunders.
Räike, A., O. P. Pietiläinen, S. Rekolainen, P. Kauppila, H. Pitkänen, J. Niemi, A. Raateland, and J. Vuorenmaa. 2003. “Trends of Phosphorus, Nitrogen and Chlorophyll a Concentrations in Finnish Rivers and Lakes in 1975–2000.” Science of The Total Environment 310 (1–3): 47–59. doi: 10.1016/S0048–9697(02)00622–8.
Rapport, David J. 1992. “Evaluating Ecosystem Health.” Journal of Aquatic Ecosystem Health 1 (1): 15–24. doi: 10.1007/BF00044405.
Rapport, David J. 1998a. “Defining Ecosystem Health.” In Ecosystem Health, edited by David J. Rapport, Robert Costanza, Paul R. Epstein, Connie Gaudet, and Richard Levins, 18–33. Oxford: Blackwell Science.
Rapport, David J. 1998b. “Need for a New Paradigm.” In Ecosystem Health, edited by David J. Rapport, Robert Costanza, Paul R. Epstein, Connie Gaudet, and Richard Levins, 3–17. Oxford: Blackwell Science.
Rapport, David J., Robert Costanza, Paul R. Epstein, Connie Gaudet, and Richard Levins, eds. 1998. Ecosystem Health. Oxford: Blackwell Science.
Rapport, David J., H. A. Regier, and T. C. Hutchinson. 1985. “Ecosystem Behavior Under Stress.” The American Naturalist 125 (5): 617–640. doi: 10.2307/2461475.
Rice, Jake. 2003. “Environmental Health Indicators.” Ocean & Coastal Management 46 (3–4): 235–259. doi: 10.1016/S0964–5691(03)00006–1.
Richardson, Susan D., Michael J. Plewa, Elizabeth D. Wagner, Rita Schoeny, and David M. DeMarini. 2007. “Occurrence, Genotoxicity, and Carcinogenicity of Regulated and Emerging Disinfection by-Products in Drinking Water: A Review and Roadmap for Research.” Mutation Research/Reviews in Mutation Research 636 (1–3): 178–242. doi: 10.1016/j.mrrev.2007.09.001.
Sabia, Séverine, Martin Shipley, Alexis Elbaz, Michael Marmot, Mika Kivimaki, Francine Kauffmann, and Archana Singh-Manoux. 2010. “Why Does Lung Function Predict Mortality? Results from the Whitehall Ii Cohort Study.” American Journal of Epidemiology 172 (12): 1415–1423. doi: 10.1093/aje/kwq294.
Saracci, Rodolfo. 1997. “The World Health Organisation Needs to Reconsider Its Definition of Health.” BMJ: British Medical Journal 314 (7091): 1409–1410. doi: 10.2307/25174539.
Schaeffer, David J. 1996. “Diagnosing Ecosystem Health.” Ecotoxicology and Environmental Safety 34 (1): 18–34. doi: 10.1006/eesa.1996.0041.
Scow, K. M., G. E. Fogg, D. E. Hinton, and M. L. Johnson. 2000. Integrated Assessment of Ecosystem Health. Boca Raton, FL: Lewis Publishers.
Suter, Glenn W., II. 1993. “A Critique of Ecosystem Health Concepts and Indexes.” Environmental Toxicology and Chemistry 12: 1533–1539. doi: 10.1002/etc.5620120903.
VanLeeuwen, J. A., D. Waltner-Toews, T. Abernathy, and B. Smit. 1999. “Evolving Models of Human Health toward an Ecosystem Context.” Ecosystem Health 5 (3): 204–219. doi: 10.1046/j.1526–0992.1999.09931.x.
Ware, John E., Jr., and Cathy Donald Sherbourne. 1992. “The MOS 36-Item Short-Form Health Survey (Sf-36): I. Conceptual Framework and Item Selection.” Medical Care 30 (6): 473–483. doi: 10.2307/3765916.
Wicklum, D., and Ronald W. Davies. 1995. “Ecosystem Health and Integrity?” Canadian Journal of Botany 73 (7): 997–1000. doi: 10.1139/b95–108.
World Health Organization. 1948. Preamble to the Constitution of the World Health Organization as Adopted by the International Health Conference, New York, 19–22 June 1946. Accessed January 17, 2015. http://www.who.int/about/definition/en/print.html.