2 | Coronary heart disease
Coronary artery disease is caused by a hardening or narrowing of the arteries to your heart. The medical term is atheroma or atherosclerosis. Patches of the inner lining of the arteries become furred up from a mixture of fat, cholesterol and cells deposited in the wall. Veins, unlike arteries, do not ‘fur up’ unless they are asked to do the work of arteries, for example after a bypass operation (see Bypass surgery in Chapter 3). If you think of an artery as a three-lane motorway, the narrowed part of the artery is like a lane of the motorway being coned off; the flow of blood is restricted a bit like the traffic is slowed down as it tries to filter into the lanes that are open. The patches of narrowing are called plaque (pronounced ‘plack’), so you may hear doctors refer to atheromatous plaque or plaque disease. Plaque may cause a progressive narrowing of your arteries, restricting blood flow and causing angina (see Chapter 3), or it may rupture or tear causing clots to form, which totally block the artery, and this can lead to a heart attack.
The major causes of atheroma developing are:
•raised cholesterol level;
•cigarette smoking; and
•high blood pressure.
Usually symptoms develop leading to a diagnosis of angina, heart attack or heart failure. Occasionally, the first evidence may be when someone dies suddenly from a heart attack, but there is usually a warning and it is important to understand what the warning signs are.
There are some factors in a person’s life called risk factors. People with risk factors have an increased chance of developing a particular condition. For example, working with asbestos or down a coalmine increases the chance (or risk) of developing lung disease, and is thus considered a risk factor. Risk factors for coronary artery disease can be divided into those that can be avoided and those that can not (see Table 2.1). Avoidable risk factors, including diabetes, account for 90% of coronary disease. Risk factors for coronary disease are like penalty points on a driving licence, only they multiply rather than add up: smoking may give you 3 penalty points and high blood pressure 3 penalty points, but both risk factors at the same time may give you 9 penalty points; if you also have 3 penalty points for a high cholesterol level, then your penalty points may multiply to 27 in total.
Table 2.1 Avoidable and unavoidable risk factors for heart disease
Avoidable |
Unavoidable |
Cigarette smoking |
Male sex |
High blood pressure |
Family history |
High cholesterol |
Diabetes (unavoidable to some extent) |
Obesity |
Age (getting older) |
Diabetes (avoidable in many) |
|
Lack of exercise |
|
Stress |
|
Low intake of fruit and vegetables |
|
Excess alcohol |
Are there any risk factors that I can’t change?
Your parents, your age and your sex may increase your risks. Your race may also bring risk: people from the Indian subcontinent have more coronary disease, African-Caribbeans less. Having a family history of heart disease, being a male and getting older means that you need to take more care. A high risk family is one in which a close female relative aged 65 years or less, or a male relative aged 55 years or less, or both, developed coronary disease.
But remember that you can lessen many of your risk factors and improve your chances of not developing heart problems.
Prevention is always the best medicine so the first part of this chapter looks at what puts you at risk of developing coronary artery disease, and then how it can be prevented or treated.
RISKS OF SMOKING
I have smoked since my teens just as my father and grandfather did. My father is still alive and my grandfather lived until he was 65. What are my risks of heart disease?
There is overwhelming evidence that smoking causes hardening of the coronary arteries as well as hardening of your arteries to the brain and legs; this hardening leads to narrowed arteries and thus poor blood flow to your heart. It also leads to chronic lung diseases as well as lung cancer, and increases your chances of developing a stomach ulcer. Whilst some people escape the consequences of cigarette smoking, the majority do not.
There is a lot of talk about the harmful effects of passive smoking. Can other people’s smoke really harm me?
Smoking harms any non-smokers who are breathing in the same air as a smoker, increasing their chance of heart and lung disease. It may also cause sore red eyes, headaches and make asthma worse. This has become known as passive smoking. Children brought up in a household of smokers suffer more infections and disease, compared to those who live in non-smoking households.
The government gives us dire warnings about smoking but I know many people who smoke who are in their seventies or eighties. Are the statistics regarding the harmful effects of smoking really as bad as the press makes out?
Yes. Smoking causes one in five deaths in our population and at least a third of these are due to heart disease. This means that, in the UK, smoking kills over 100 000 people a year. It kills 90% of the 40 000 who die from lung cancer, 75% of the 20 000 who die from chronic lung disease such as emphysema, and 25% of the 117 000 who die each year from coronary artery disease. Smoking respects no one – it is an equal opportunity killer attacking both sexes and all races. Out of the total number of people who smoke, a quarter will die early as a result, losing an average 10–15 years of life. Worldwide, smoking kills three million people a year. This is predicted to increase to 10 million by 2025, which means that 200 million of today’s children and teenagers will be killed by tobacco. Add these to today’s adults and we get a staggering half a billion of the world’s population being killed by tobacco – 250 million dying young (aged 35–69 years) and each person losing 20 years of expected life. Many people die only after a long disabling disease.
I have changed to a low-tar brand of cigarettes, with a filter. Why will smoking be so harmful to me now?
Components of tobacco, such as tars, are harmful to your health but the main cause is the nicotine in cigarettes as this is an addictive drug. Nicotine increases your heart rate and blood pressure making your heart work harder, whilst at the same time narrowing the arteries. Oxygen is removed from the blood and replaced with carbon monoxide. Carbon monoxide reduces the ability of the blood to carry oxygen and, in heavy smokers, may reduce it by as much as 50%. We have all read of tragedies caused by faulty gas heaters – carbon monoxide build-up is the cause. This means that there is less energy circulating to your heart to cope with the demands that nicotine places on it. The carbon monoxide level in the blood after smoking one cigarette exceeds the legal limit for pollution allowed in industry by eight times. Low tar cigarettes are nice in theory, because it is the tar in cigarettes that causes lung cancer, but actually they make matters worse in that most low tar smokers inhale deeper and increase their carbon monoxide and nicotine blood levels.
Smoking can cause roughening of the smooth lining of your arteries (the endothelium) and this may lead to the development of narrowed areas in the arteries caused by fat being deposited there. Smoking lowers the good cholesterol known as the high density lipoprotein (HDL) (see the section Risks of high cholesterol levels) and increases the blood ingredient (fibrinogen) that promotes clotting. Smoking therefore not only causes hardening of your arteries but increases the chance of clots forming on the narrowed areas and thus a heart attack.
I have tried again and again to give up smoking. Are there any ‘safe’ cigarettes?
No. All cigarettes, ‘light’ or not, are just as harmful to your heart. Filters have no advantages and may actually increase the carbon monoxide inhaled. Changing to low tar/nicotine cigarettes may reduce your risk of lung cancer, but not heart disease, and it is heart disease that is the major killer.
I cannot stop smoking. Would it help if I just cut down on my smoking?
Yes, but there is no such thing as safe smoking. Smoking five cigarettes a day doubles your risk of heart disease and smoking 20 a day increases your risk by at least 10 times. Reducing the number of cigarettes smoked helps, but quitting is better.
Both my husband and I smoke one pack of cigarettes a day. I have recently read that women are as much at risk as men. Is this true?
Yes and, if anything, more so (see Figure 2.1). Women seem to be more sensitive to the effects of cigarettes, so for a similar number smoked (20 per day) you are twice as likely as your husband to develop coronary artery disease. Smoking is especially dangerous if you are on the contraceptive pill, particularly if you are aged over 35 years or have been continuously on the pill for 5 years or more (see Women and coronary artery disease on p. 73).
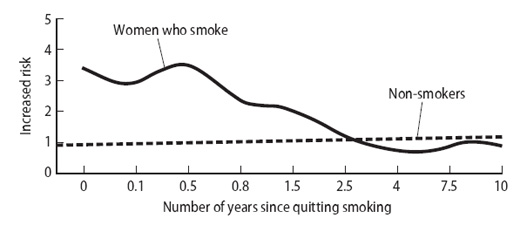
Figure 2.1 Women who smoke have almost four times as great a risk of heart attack but, three years after quitting, the risk is the same as for non-smokers. Solid line = women who smoke; dotted line = non-smokers.
If I could stop smoking, would this do any real good?
The benefits of stopping begin quickly. By 24 hours the carbon monoxide is eliminated from the blood and the lungs begin to clear the mucus. Smell and taste improve by 48 hours. By 3 months, breathing is easier as the circulation improves, making exercise easier. By one year, the risk of a heart attack is halved, and four to five years after quitting smoking your risk of heart disease will be the same as for a non-smoker. Stopping smoking is one of the most important actions you can make – not starting is the best educational message of all (Figure 2.2). The benefit to your lungs regarding cancer takes longer – about 20 years in total, but the risk is halved by 10 years.

Figure 2.2 Cigarette smoking is the biggest risk factor for sudden death. The best advice is: If you smoke – QUIT; if you don’t smoke – DON’T START.
I am 58 and have been smoking for many years. Is it ever too late to stop?
No. The benefit to your heart is rapid and helps you, no matter what your age.
My girlfriend has suggested that I change to a pipe as she is convinced that pipes and cigars are safer than cigarettes. Is this true?
Smoke from pipes and cigars contains a higher concentration of tar and nicotine compared with cigarettes, but pipe and cigar smokers usually inhale less than cigarette smokers so the risks are less, but they are still greater than in non-smokers. Cigarette smokers who switch to a pipe usually inhale the smoke automatically, thereby not significantly reducing their risks. Inhaling from a large cigar is the same as inhaling from a pack of 20 cigarettes!
Studies have shown that smokers who switch to pipes and cigars, and don’t inhale, reduce their risks of lung cancer and heart disease by 50%, but the risk is still 50% higher than quitting altogether. However, by not inhaling, pipe and cigar smokers increase the risk to non-smokers from passive smoking. The best option is not to smoke at all. The principal reason pipe smokers have less risk is that they spend most of their time trying to light the pipe rather than puffing on it!
I have tried to stop smoking but always lapse. What can I do to quit smoking and avoid the temptations?
Stopping smoking is difficult but it is the biggest single improvement to your health that you, as a smoker, can make. Some people find that reading a book on quitting gives them the confidence that they need to actually stop. There are some suggestions on book titles that may be helpful in Appendix 3.
Cutting down is a help but only if your aim is to stop completely (see question above). Remember that after 3–5 years you will have your heart’s health back. Here are some guidelines to help you.
•Make a list of your reasons for stopping, keep it with you and read it every day. The best reasons are:
–it is bad for my health;
–the cough is unpleasant;
–my clothes always smell;
–it is expensive;
–I cannot taste my food;
–non-smokers are upset by my smoking.
•Set a day to stop or take part in a sponsored ‘stop’ with friends or business colleagues.
•Take time for exercise, drink plenty of water and have plenty of fresh fruit to hand (not cakes or biscuits).
•Each day place the money saved to one side and put it into a savings account. After 1 week you will have saved over £30, by 1 month over £120, and by 6 months at least £720, which you can spend on a well-earned holiday. Put another way, if you place the price of a packet of cigarettes at around £4 per day into an individual savings account (ISA), after 20 years the fund could be worth £44 100 (at 6% interest). In a pension plan, it could give you £4,350 (at 7% interest) per year in extra annual income! The more the price rises, the move you will save. Of course, if you carry on smoking, you may never reach your pensionable age.
•Be disciplined and don’t talk yourself into smoking ‘to calm me down’. If the craving is unbearable, go for a brisk walk, relax with a hot bath and drink plenty of water.
•Think positively.
•Don’t carry matches or a lighter.
•Go to the dentist and have your teeth cleaned to get rid of the tobacco stains.
•Keep being positive, keep reading your reasons for quitting, reward yourself with a treat after your first week of not smoking – you’ve saved enough money, so go ahead!
•Avoid certain activities that are linked with smoking:
•Try to avoid alcohol and take a drink that is not associated with smoking, such as a tomato juice.
•After a meal, instead of a cigarette, clean the table, wash up, brush your teeth and go for a walk.
•Do not have cigarettes in the car; have chewing gum to hand instead.
•Outside the UK and Ireland, avoid smoky restaurants and bars.
•Holiday in countries where smoking is not allowed in public places, such as the UK or France.
•Tell your smoking friends that you will be unavailable other than on the ’phone, unless they are giving up as well.
•Keep your hands busy (fiddle with paper clips, write a letter, do the crossword, clean the car, help in the garden or with the housework).
•Use sugarless chewing gum to replace the urge to put a cigarette in your mouth.
•Take deep breaths, relax your muscles, and think of anything but cigarettes, for example your holiday plans or a previous happy experience.
•Remove everything from the house that reminds you of cigarettes: get rid of your ashtrays and matches, then have a spring clean to remove all the smell and stains of smoking, open the windows and let the fresh air circulate.
If you tell yourself you don’t want to smoke rather than wishing you could smoke, you can reinforce this by noticing that your breath is better, your clothes are cleaner, the car smells better, food tastes again and that early morning cough has improved or stopped! Remember the 10 million people who have already broken the habit. The first few days are always the worst, so it does get easier! Remember that you will save over £1,825 a year.
I’ve given up smoking but I am afraid that I might begin again. Will it put me back to square one if I start again?
Try to avoid the urge but, if you do slip, don’t despair: you can get back the ground you’ve lost, but you must act quickly. It is not a crime, you are not a failure, and you must not feel guilty. Look for the reason: were you tense or stressed? Were you upset or angry? Were you in a situation that you automatically associated with smoking? Then take action to avoid it happening again.
I have heard that meditation can help people to stop smoking. Do you think it works and is it worth the effort?
A lot of people benefit from learning to relax and meditate. It is particularly useful in times of stress. Relaxation tapes are available and can be helpful, as can relaxing music.
A friend of mine went to an acupuncturist to help her stop smoking and she has not smoked now for some months. I have also read that hypnosis can help. Do you think that any of these methods is any good?
There is no trial (research) evidence that acupuncture or hypnosis is effective in helping people stop smoking. However, if you are struggling, it may be worth trying either or both as they are popular with smokers and people can be helped by unproven methods. Make sure that you go to registered practitioners and keep an open mind. Always enquire about the cost before treatment begins.
I don’t do much exercise. Would exercise help me to give up smoking?
Exercise is very helpful. It not only improves your overall physical condition, but it is also a great way of relieving stress and improving your mood. It takes your mind off cigarettes as well as helping to control your appetite and weight. Before you exercise, practise deep breathing and repeat this as you cool down afterwards. Dynamic exercise is best and this includes walking as briskly as possible, cycling, swimming and playing tennis or golf (see Chapter 10).
I know people who have given up smoking, but then put on weight. How can I avoid this?
People who smoke are on average 3–4 kg (7–8 lb) lighter than non-smokers. It is, however, the wrong way to stay slim. When you stop it doesn’t automatically mean your weight will go up, but gaining 1 kg (2–3 lb) is not as important as quitting cigarettes.
Weight is gained when you eat more than you burn up. The trick is to watch what you eat and take up regular exercise. You need to plan positively not to let it happen.
Eat fresh fruit and vegetables; avoid cakes, chocolate and biscuits; use wholegrain cereals, porridge without sugar, pasta and bread; and drink plenty of water or low calorie drinks. You will not control your weight unless you match your intake with regular exercise – you must do both (see Chapters 9 and 10). Think of it as a lifestyle change, not a ‘diet’.
It is not a good idea to stop smoking just as you go on holiday, as there will be a temptation to overeat anyway. Weigh yourself no more than once a week, at the same time of day and in the same or no clothing, to monitor your progress. Try not to become obsessed by weight. Do not start to smoke if your weight goes up; watch what you are eating and take plenty of exercise.
I’ve not yet tried quitting as I am frankly unable to cope with going ‘cold turkey’. What can I expect as withdrawal symptoms when I stop smoking?
There is often a worsening of the smoker’s cough until all the rubbish is out of your lungs. You may feel thirsty, in which case drink water and avoid caffeinated drinks and excess alcohol. Some people become constipated and hungry, and this is helped by fresh fruit and a high fibre diet (see Chapter 9). Some people become anxious, irritable and have difficulty concentrating – these feelings may last up to 4 weeks but are worse in the first 2 weeks. Drink plenty of water and take regular exercise; try to fill your time with positive activities (see the question above).
I have seen adverts for nicotine gum and patches. I smoke about 20 a day. Would nicotine replacement help me?
Some people are so addicted to nicotine that they need to be weaned off – they tend to be the people who need their first cigarette within 30 minutes of waking in the morning.
There are five sorts of nicotine replacements.
•The patch is like a thin plaster, which slowly gives out nicotine through the skin. It does not help if you have a sudden craving but, if you normally smoke steadily over a day, it will almost certainly suit your needs. Studies have shown that people using the patch, compared to those using a dummy patch (with no nicotine), had twice the success rate in stopping smoking. Patches come in different strengths, and heavy smokers (over 20 a day) may need to start high, weaning down to lower strengths over 2–4 weeks. Common products are Boots and Nicorette (5, 10 and 15 mg) and Nicotinell and NiQuitin CQ (7, 14 and 21 mg).
•Nicotine gum, inhalator, tablet or nasal spray help you respond to a sudden craving because they act quickly – so you may be more likely to need these if you smoke in response to sudden stress. Boots, Nicorette and Nicotinell gum (flavoured or plain) come in two strengths, 2 and 4 mg, and can be bought in chemist shops. Again, heavy smokers may need to start with the 4 mg strength; 8–12 pieces of either strength each day are recommended starting doses.
•The Nicorette nasal spray is prescription only (one spray each nostril up to twice an hour for 16 hours in every 24).
•Boots and Nicorette inhalators consist of a mouthpiece and replaceable nicotine cartridge – you should suck the nicotine vapour into the mouth (it does not reach the lungs). Each cartridge provides up to three 20-minute periods of intense use, and you may need 6–12 cartridges a day for 8 weeks, reducing to zero over the following 4 weeks. These can be bought in chemist shops.
•The Nicorette tablet (Microtab) is placed under the tongue and dissolves over 30 minutes, providing 1 mg of nicotine from a 2 mg tablet. You may need one or two every hour at first, and they can be bought in chemist shops.
The instructions must be followed carefully, and any concerns should be discussed with your family doctor or chemist. Do not use nicotine products if you are pregnant or breastfeeding.
Are there any side effects to the nicotine preparations?
For most people, side effects are not a problem. The gum may be awkward if you have dentures, and the patches may cause the skin to itch, so you may need to move them to a different place each day. The nasal spray may irritate the nose and throat and make your eyes water; the inhalator may cause a cough or irritation of the throat. The tablet can mildly irritate the mouth, but this tends to wear off with use. Sleep disturbance, vivid dreams, flushing or rashes, and nausea sometimes occur. Nicotine can upset a stomach (peptic) ulcer, so, if you are on treatment for an ulcer, check with your doctor first. If you have a history of heart attack, stroke, high blood pressure, diabetes or hardening of the arteries generally, check with your doctor first. If you are taking warfarin, inform your clinic, as there may be an interaction between the two drugs. Too much nicotine may make you feel sick, so do not smoke at the same time as using gum or patches. Whilst combining nicotine preparations is not recommended by the manufacturers, some studies have shown improved success rates when the gum and patches, or the nasal spray and patches, are combined. Only do this after getting your doctor’s advice.
Can I become addicted to the nicotine patches?
This is not a problem with the patches. However, the gum, spray, tablet or inhalator, which deal with cravings, may need to be used for over a year. When you are trying to stop using nicotine replacements, wean off gently to avoid a withdrawal reaction. You will be more successful if you combine nicotine replacement with the support of smokers’ clinics and family, rather than going it alone.
How much do these products cost?
These are the approximate costs for 3 months, if you are paying yourself.
•Boots 2 mg gum £120
•Nicorette inhalator £300
•Nicorette spray £110
•Nicorette patches up to £150.
You will save your money and your life for many years ahead – think of this cost as a down payment towards better health. The good news is that nicotine replacement therapy is now approved by the National Health Service and is regarded as the drug treatment of choice. The family doctor and the patient must follow an agreed protocol and set a target stop date before a prescription is allowed.
I have been trying to find a support group – can they help me?
They certainly help. You will feel less alone, get support and help from others and be amongst people all trying to succeed. Phone QUIT on 020 7388 5775, or check with your local health authority for locations. QUITLINE (0800 00 22 00) provides trained counsellors to give advice, support and encouragement. The website is www.quit.org.uk (see Appendix 2).
There are now NHS helplines in England and Wales (0800 169 0169), Scotland (0800 84 84 84) and Northern Ireland (0800 85 85 85). Also try www.sickofsmoking.com to see what other smokers say. Other good sites are www.ash.org.uk and www.givingupsmoking.co.uk.
Are herbal cigarettes or dummy cigarettes worth trying?
Dummy cigarettes, such as Crave Away, Flowers or Everlasting Cigarettes, are neither harmful nor proven to be effective. Herbal cigarettes do not contain nicotine but still expose your body to tar and carbon monoxide, and are of no proven value.
Would it be better if I used a filter?
Filters can be a good idea, but unfortunately do not work for most people. Nicobrevin may help in the first weeks but should not be relied on as a long-term prop. It should be avoided if you are pregnant. Note that filters remove some of the tar but little of the risk of heart disease!
Why do some people smoke like chimneys but live a long life all the same?
Most people know someone like this. It is all about statistics: if 90% of people die from smoking, then 10% won’t. The point is that the odds are against you, and trying to get away with it, or believing it can’t happen to you, is courting disaster.
If someone introduced a product onto the market now that was addictive, removed oxygen from your blood, caused blood clotting, heart attacks and lung cancer, do you think they would get a licence?
I have heard a lot about Zyban. Does it help stop smoking and how does it work?
Zyban is the trade name for the drug buproprion. It is a drug used to treat depression but it was also found to help people stop smoking. How it does this is unclear but it seems to reduce the urge for nicotine and is effective for some people. It should be started 1–2 weeks before the target stop date and continued for 7–9 weeks after. It should not be used in anyone with a history of seizures (fits) or eating disorders. It also has the potential to react with some drugs. Zyban should only be used after careful discussion with your family doctor – it is available on NHS prescription.
One of my friends is taking Champix – does it work?
Champix is one of the trade names for varenicline, a new prescription-only drug which acts like nicotine and so reduces the craving for smoking. It has been shown to be very effective. You need to start it 1–2 weeks before the target stop date you agree with your doctor. The course of the treatment is about 3 months and can be repeated to prevent a relapse, though the evidence to support this is limited. Side effects include stomach upsets, dry mouth, taste disturbance, headaches, sleep disturbance, dizziness and abnormal dreams. If stopped suddenly, irritability and depression can occur. There are reports of hallucinations, suicidal thoughts and reports of suicide after starting varenicline. No definite connection with Champix has been made, but any change in mood or behaviour should be reported to your doctor.
I had a heart attack a year ago when I was 61. Is it too late to stop smoking?
It is never too late. Stopping smoking after a heart attack reduces by half your chance of having another one in the next 5 years. Stopping smoking after a heart bypass operation reduces your chances of a bypass failure over the next 10–15 years and helps prevent further disease developing.
What is a smoking cessation clinic – is it worth a try?
Special clinics and specially trained nurses and smoking cessation advisors provide support and achieve high success rates in smoking cessation (quitting). Support is usually given in groups over 6 weeks and most services also offer one-to-one counselling. Clinics take direct referrals from those wanting to stop (in a walk-in service) as well as working in partnership with family doctors. They are recommended for heavily dependent smokers needing intensive support or pregnant women especially. However, they are available to all, either in a clinic setting or as part of a local primary care service. Stopping smoking is so important: if you are having any difficulty, certainly give them a try.
RISKS OF HIGH BLOOD PRESSURE
Facts and figures
Can you tell me more about blood pressure? Why is it serious if it becomes high?
We need a blood pressure to send blood around our bodies (see Chapter 1). It is needed to overcome the resistance of the smaller blood vessels. The arteries in the body have muscle in their walls to give them tone. If this muscle is supple, the arteries can relax, their size or width increases and blood flows more easily. Think of the artery like a garden hose pipe: if you turn the tap on, water flows easily – now clamp the pipe to reduce its size by half and water will need more pressure to get through to give the same flow. In a similar way, the heart pumps the blood through the arteries but, if your arteries get smaller, the pressure will need to rise in order to force the blood through (see Figure 2.3). The top pressure, known as the systolic pressure (pronounced ‘sis-tol-ick’), is the pressure created by your heart beating and coincides with your pulse; the bottom pressure, known as the diastolic pressure (pronounced ‘die-a-stol-ick’), is the reading when your heart is relaxing. The readings should not be more than 140/90 mmHg. Hg is the symbol for mercury which used to be in the column of the blood pressure machine.
Blood pressure can clearly be raised at rest, for example 220/120 mmHg (when it is known as hypertension, see below) or normal, e.g. 120/80 mmHg, but there are areas where it is borderline, and you need regular checks to keep an eye on it. A pressure consistently above 140/90 mmHg should be investigated, but age should be taken into account as well. At 80 years this figure might be okay, but at 30 years it would not be. So although doctors talk generally of blood pressure, any decision to investigate or treat will be made on a very individual basis.
Hypertension (pronounced ‘hi-per-ten-shun’) is the medical word for a high blood pressure. ‘Hyper’ means too much, and ‘tension’ refers to the pressure. You may be asked to attend a hypertension clinic or a screening clinic to keep a check on your blood pressure.
What causes high blood pressure?
In the vast majority of cases there is no single cause, just as there is no single cause for people being short or tall. The medical name is essential or primary hypertension. Tests may be done to check the kidneys, adrenal gland and heart. Some people’s blood pressure is raised as a side effect of their medication, particularly anti-arthritis medications. Always tell your doctor or practice nurse what medicines you have (including complementary or herbal medicines) or, preferably, bring along any that you are taking to show your doctor.
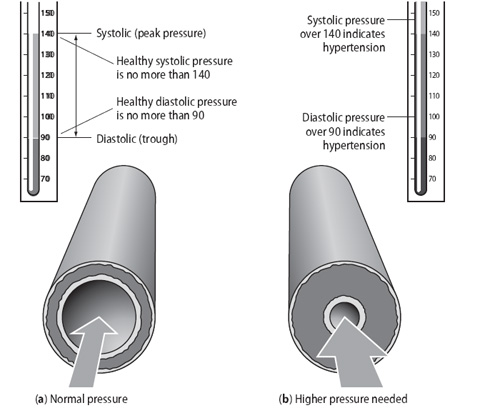
Figure 2.3 (a) Healthy arteries are elastic and blood flows easily
without meeting a resistance. (b) Arteries can lose their elasticity for unknown reasons or suffer from disease or hardening with age.
They then become less able to relax and a higher pressure is needed
to force the blood through.
You may have been told that you have secondary hypertension – this is the term used when a cause for your high blood pressure has been found (this happens in only 5% of cases). The normal or target pressure is 140/90 mmHg or less. In people with diabetes, chronic renal disease or coronary disease the target is 130/80 mmHg.
What tests can I expect to have if my blood pressure is found to be raised?
The heart may be checked with an ECG (see under Tests in Chapter 3) or echocardiogram (see under Tests in Chapter 5). A chest X-ray may be taken to look at the heart and lungs. Blood and water (urine) tests will look for any signs of anaemia (low blood count) or kidney problems, and your urine may be collected for 24 hours to see if there is too much adrenaline coming from your adrenal gland. Sometimes a scan or X-ray is taken of the kidneys.
I am not too sure what the adrenal glands are for. Can you explain their purpose?
The adrenal glands sit on top of your kidneys. They produce adrenaline. This is a hormone which speeds up your heart when you exert yourself or are emotionally excited or very frightened (white with fear), and you feel your heart pounding. Adrenaline keeps your blood pressure up if you are shocked or losing blood. Too much adrenaline that is not needed, for example in a person who is not exercising, will keep the blood pressure high unnecessarily. A tumour of the adrenal gland can do this and, although they are very rare, we check the blood or urine for excess adrenaline in younger people. If an excess is found and a tumour shown on a scan, it can be removed surgically.
My wife and I went to the doctor’s to get our blood pressures checked. Hers was different to mine. Why?
Blood pressure varies from person to person and also changes in the same person. Blood pressure constantly changes within a normal range depending on what you are doing. During physical work your muscles need a greater supply of food and, to meet this extra demand, your blood flow has to be increased. To achieve this, your heart must beat faster and your blood pressure rises.
Blood pressure is lowest at night when you are asleep, but even then there are fluctuations which are presumably due to the influence of dreams. During the day the fluctuations are greater and more frequent and reflect the sort of work you are doing. Mental as well as physical stress can increase your blood pressure.
From this you will see that a doctor may need to take several readings of your blood pressure to make sure that a diagnosis of high blood pressure is a true reflection, and not due to an isolated event that could be responsible for a temporary rise in pressure. For this reason your doctor may ask you to call back to the surgery over a period of a few days or weeks in order to eliminate any temporary cause for the high level.
You can help your doctor in this respect by arriving early for your appointment, so as to avoid a rush, or worrying that you will be late. When you arrive in the surgery, relax as much as possible, because it is important to your doctor, when he is judging the level of blood pressure, to know that you are rested and calm at the time the measurement is taken (see next question).
When I went to the clinic to have my blood pressure checked, I was told that I had white coat hypertension. What is this?
This is a high reading caused by anxiety or stress when you visit your doctor –who may be wearing a white coat! At other times your blood pressure is usually normal. It may be worth checking the readings at home and during the day with a blood pressure machine that can be worn while you are walking about (an ambulatory machine; see the question later on about this.) Do several readings with your own or a borrowed machine. Blood pressure often rises under stress; throughout the day we are exposed to many stresses, so if several elevated readings occur because of environmental stress, treatment will be of value. If no elevated readings occur, your doctor should monitor your pressure regularly anyway, because we don’t know if white coat hypertension is a warning for true hypertension in the future. You cannot afford to be complacent.
When I was 16, my blood pressure was lower than it is now that I am 45. Is this OK?
Yes, as a natural part of growing old, your arteries tend to lose their elastic properties to some degree. Also, the walls of your arteries tend to thicken after middle age and, consequently, the internal diameter of the vessel is slightly reduced (the hose pipe gets narrower). All these changes require a very slight increase in blood pressure, which is perfectly normal as you get older.
What are the dangers if I can’t get my high blood pressure down?
If a raised blood pressure is left untreated over a 12-year period, you are more likely to die from this risk than if you had been treated. Here are some other statistics about raised blood pressure.
•It is present in 70% of people who have a stroke.
•It increases the risk of coronary heart disease by 2–3 times for men and women.
•It causes heart and kidney failure.
•It causes hardening of the arteries to the legs resulting in pain on walking owing to poor blood flow. The medical term for this is claudication, pronounced ‘claw-dee-ca-shun’.
•It is responsible for a third of all heart diseases.
•It causes 7 out of 10 strokes in women and 4 out of 10 in men.
•In the UK, 300 people die every 6 weeks as a result of a high blood pressure and most of these deaths are avoidable; if a jumbo jet with 300 people on board crashed every 6 weeks, something would be done about it!
Are there any specific risk factors for high blood pressure that might apply to me?
You are more likely to have a high blood pressure if you:
•have someone in your family who has had high blood pressure;
•are African-Caribbean;
•are aged over 60 years of age;
•are very overweight;
•drink heavily;
•eat a lot of salt;
•had a high blood pressure in pregnancy, or pre-eclampsia;
•have a lot of stress in your life.
I have read about the rule of halves, but did not understand it. Could you explain?
This is a medical paradox but in reality it demonstrates some alarming facts about blood pressure and lack of treatment.
•Half the people with high BP have not been diagnosed.
•Half of those diagnosed have not been treated.
•Half of those treated have not got their blood pressure under control.
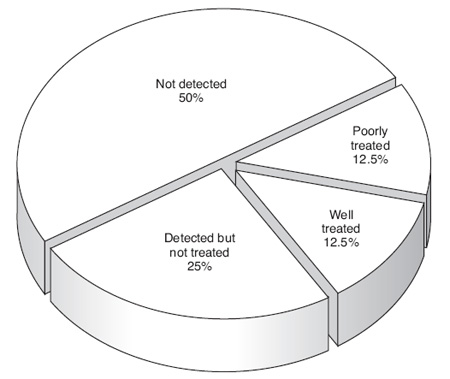
Figure 2.4 The rule of halves in people with high blood pressure:
they remain poorly detected and poorly treated. Half the people with
a high blood pressure do not know that they have it (not detected);
half who have it may not have been told or may not have attended for treatment; half of those on treatment are not well controlled and finally half of those on treatment are properly treated and have normal pressures as a result – not a good record!
•Half of those treated are well treated.
•Only one-eighth of people with high blood pressure are being properly treated (see Figure 2.4).
So the responsibility is yours to keep nagging your doctor or practice nurse to check your blood pressure, whenever you go to the surgery. You must take charge of your own health.
How would I know if my blood pressure was raised?
Most people feel nothing until there is a problem, which is why it is known as ‘the silent enemy’. It is thought that half the people with high blood pressure do not know they have it, because they cannot feel it and a doctor has not checked it. It is therefore important to have a blood pressure check every few years if it is normal, or more frequently if it is slightly raised or ‘borderline’. If you go to your doctor for another reason, ask for it to be checked then.
Measurement of blood pressure
I have often seen home blood pressure monitoring machines in high street chemists, but they are pricey. Are they any good?
Some are, but others are not accurate or reliable. Ask your doctor for advice on which one to buy and then get it checked against the doctor’s machine. Ask the nurse if you are not sure how to use it – go through a practice run in the surgery. Some doctors can loan you a machine for a couple of days. This is the best option because the most reliable electronic machines are the most expensive – a medical centre can buy one or two and keep an eye on their accuracy by regular checks, making sure the cuff is the right size and the batteries fresh. Digital monitors have a cuff, which inflates and deflates at the touch of a button. The Omron has been approved and validated but, for up-to-date advice, contact the British Hypertension Society (see Appendix 2).
How is blood pressure measured in the clinic?
Your doctor or nurse takes the blood pressure with an instrument called a sphygmomanometer (often abbreviated to sphyg). It is pronounced ‘s-fig-mo-man-omeater’. The Greek word for pulse is sphygmos and it is the appearance and disappearance of the pulse at the elbow that the doctor or nurse listens for (see Figure 2.5).
While your arm is relaxed and resting on a desk or supported by the doctor or nurse, a rubber cuff is wound round your upper arm just above the elbow. If your arm is large, a big cuff will be used. The cuff is attached to a column of mercury. The cuff is inflated by air being pumped into the cuff; you will feel a squeezing. The pressure in the cuff is increased until the blood flow to your hand is cut off (you may feel a tingling or numbness). Whilst the doctor listens with a stethoscope to the artery at the elbow (the brachial artery, pronounced ‘brake-e-al’), the pressure in the cuff is lowered. The level of mercury shown in the column when the blood begins to flow again (felt as a thumping) is measured as the systolic pressure and, when no noises are heard (you don’t feel this), it is measured as the diastolic pressure. Always ask what your reading is and keep your own records.
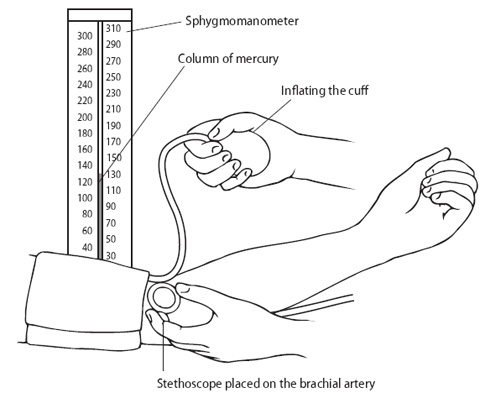
Figure 2.5 Getting your blood pressure checked in the surgery.
The mercury sphyg is being replaced by electronic measuring devices. Your practice may have changed to automatic machines but the cuff will still be put on your arm above the elbow; the wrist devices are not accurate.
How often should my blood pressure be checked?
Once a year if it is normal – try and make a note in your diary to make an appointment for the following year. If it is raised, your doctor will take several readings and keep an eye on it until it is normal. Your blood pressure will then be checked at regular intervals, usually every 3–6 months. Make sure that you ask for this measurement at least twice a year.

Figure 2.6 An electronic measuring device for blood pressure.
My doctor tells me that my systolic pressure is very high, although the diastolic pressure is normal. Does this matter?
It used to be thought that only the diastolic blood pressure rise was important, but modern research has shown that in people over the age of 45 years, the rise in systolic blood pressure over the normal of 140, and certainly over 160, is an important cause of subsequent heart disease and strokes. Treatment of this rise in systolic blood pressure is an important factor in reducing the risk of these serious complications.
Self-help
My mother had high blood pressure and she suffered a stroke when she was 65. Can I avoid having hypertension myself?
First of all, if someone in your family has had high blood pressure, make sure that you and your relatives have regular check-ups. Although you may feel no benefit now, you may help to prevent illness in the future, so adopt a positive approach: for yourself and those you care about. Other ways of helping yourself include:
•a healthy diet (see Chapter 9);
•exercise (see Chapter 10);
•avoiding getting overweight;
•avoiding excess alcohol;
•avoiding eating excess salt.
I’m 62 and my doctor is making me cut down on salt as she says that I am getting more sensitive to salt. What does this mean?
People over 60 years, African-Caribbeans and American Blacks have been found to have less tolerance to too much salt. Salt-sensitive people can lower their systolic and diastolic blood pressure by 5–10 mmHg by cutting down on salt. Most, however, get a benefit of up to 4 mmHg, but every little bit helps to lower blood pressure and reduce the need for medication.
My husband has been told that he has a high blood pressure. The doctor gave him a diet sheet. How can a better diet help him?
Your husband should not overeat as, apart from anything else, this will make him put on weight, and being overweight is a major risk factor for and cause of high blood pressure. The single most important thing anybody with high blood pressure can do to help themselves is to lose weight. In some lucky people the raised pressure disappears completely and, in others, fewer tablets may be needed. If your husband is overweight, a reducing diet to get him to an optimum weight is an essential part of treatment. Losing 1 kg in weight could take 2 mmHg off his systolic blood pressure reading, so losing 3 kg (half a stone) can make a borderline pressure normal. However, his pressure will still need watching and will go back up again if the weight is put back on. See Chapter 9 for advice on a healthy diet and how to lose weight.
Treatment
I am bitterly disappointed because I have lost weight and reduced my salt intake, but I have been told that my blood pressure is still raised. What should I do?
You will need medication. Lowering your blood pressure to normal removes your chances of having a stroke and protects your heart, brain and kidneys from damage.
The good news is that treatment is very effective. Controlling high blood pressure helps prevent all the problems developing and restores you to a normal life expectancy. We now have many effective medications available to treat hypertension that need to be taken only once a day; if one causes a side effect, there is no need to despair because we have lots of choices and we can always find another drug that lowers the pressure to suit you.
Table 2.2 Common drugs for raised blood pressure
Generic (real) name |
Trade name (can vary in different countries) |
Diuretics |
|
bendroflumethiazide (bendrofluazide) |
Aprinox, Neo-NaClex |
chlortalidone (chlorthalidone) |
Hygroton |
hydrochlorothiazide |
Hydrenox, Hydrosaluric |
indapamide |
Natrilix |
Potassium-sparing diuretics |
|
amiloride |
Usually in combination |
triamterine |
Dytac |
spironolactone |
Aldactone |
Beta-blockers |
|
acebutolol |
Sectral |
atenolol |
Tenormin |
bisoprolol |
Emcor, Cardicor |
carvedilol |
Eucardic |
celiprolol |
Celectol |
labetalol |
Trandate |
metoprolol |
Betaloc, Lopresor |
nebivolol |
Nebilet |
pindolol |
Visken |
propranolol |
Beta-Prograne, Inderal |
timolol |
Betim |
Calcium antagonists |
|
amlodipine |
Istin |
diltiazem |
Tildiem, Adizem, Dilzem |
felodipine |
Plendil |
isradipine |
Prescal |
lacidipine |
Motens |
lercanidipine |
Zanidip |
nicardipine |
Cardene SR |
nifedipine |
Adalat, Adalat LA, Cardilate MR, Coracten XL, |
nisoldipine |
Syscor MR |
verapamil |
Securon, Cordilox, Univer |
ACE inhibitors |
|
captopril |
Capoten, Acepril |
cilazapril |
Vascace |
enalapril |
Innovace |
fosinopril |
Staril |
lisinopril |
Carace, Zestril |
moexipril |
Perdix |
perindopril |
Coversyl |
quinapril |
Accupro |
ramipril |
Tritace |
trandolapril |
Gopten |
Alpha-blockers |
|
doxazosin |
Cardura |
indoramin |
Baratol |
prazosin |
Hypovase |
terazosin |
Hytrin |
Angiotensin II antagonists |
|
candesartan |
Amias |
irbesartan |
Aprovel |
losartan |
Cozaar |
olmesartan |
Olmetec |
telmisartan |
Micardis |
valsartan |
Diovan |
Combination products |
|
atenolol + chlorthalidone |
Tenoret 50, Tenoretic |
atenolol + nifedipine |
Tenif, Beta-Adalat |
captopril + hydrochlorothiazide |
Capozide, Acezide |
enalapril + hydrochlorothiazide |
Innozide |
lisinopril + hydrochlorothiazide |
Zestoretic |
losartan + hydrochlorothiazide |
Cozaar-Comp |
metoprolol + hydrochlorothiazide |
Co-Betaloc |
propranolol + bendrofluazide |
Inderetic |
perindopril + indapamide |
Coversyl Plus |
irbesartan + hydrochlorothiazide |
Co Aprovel |
valsartan + amlodipine |
Exforge |
Table 2.3 Blood pressure-lowering drugs and their possible side effects
Drug type |
Possible side effects |
Beta-blockers |
Cold hands and feet with or without numb feeling (pins and needles); lethargy, poor concentration; heavy |
Diuretics |
Impotence; rashes; gout; possible problems for people with diabetes; muscle cramps; spironolactone: swollen or painful breasts |
Calcium antagonists |
Flushing, headaches and dizziness; swollen ankles which may be painful; bloated feeling and constipation |
ACE inhibitors |
Dry hacking cough; rash; stomach upsets |
Alpha-blockers |
Tiredness; dizziness; dry mouth |
Angiotensin II antagonists |
No major or common ones reported |
Drugs that act on the brain |
Weakness, drowsiness, dizziness on |
(e.g. methyldopa, moxonidine) |
standing; dry mouth; depression; impotence |
There seem to be a lot of different medications on the market for raised blood pressure. Why have I been given one and not another?
There are various types of medications in common use. Table 2.2 lists the most commonly prescribed medications for raised blood pressure and Table 2.3 lists some of their possible side effects. The drugs have a generic or chemical name and a trade name under which they may be marketed. The trade names vary between countries so always check against the generic name to make sure that you are on the recommended medication.
Diuretics or ‘water tablets’ are commonly used. They remove excess salt and water from the body. They can also wash out too much potassium (and this may cause cramps) which can be dangerous if digoxin is also being taken. In some people, diuretics cause gout, and if you have diabetes they can raise your blood sugar, upsetting control of your diabetes. Common medications in this group include bendroflumethiazide, indapamide (Natrilix) and chlortalidone (Hygroton) To reduce the loss of potassium, so-called potassium-sparing agents can be prescribed and these include spironolactone, triamterene or amiloride. These two sorts of medications may be combined, as in Aldactide, Moduretic or Dyazide, in order to try and get the best results. Diuretics in general are safe and effective and side effects are not common. Fresh fruit is a good way of replacing potassium – a banana a day may do the trick.
Beta-blockers are now less frequently prescribed. These act to slow your heart rate and lower your blood pressure by blocking the effects of adrenaline. Commonly used medications are atenolol (Tenormin), metoprolol (Betaloc, Lopresor) and bisoprolol (Cardicor). The commonest side effects are cold hands and feet, heavy legs, lethargy and a ‘zombie-like’ feeling. Beta-blockers may cause wheezing and are not used in people with asthma. They may also hide the signs of a low sugar level in people with Type 1 (insulin-dependent) diabetes. They do not tend to mask the perspiration that goes with a hypoglycaemic attack (low sugar episode), so this warning sign is preserved. If the diabetes is stable and well controlled, they are used, but more often if there is also angina present (see Chapter 3).
As a group, the beta-blockers are useful medications, and although they are no longer first line, if you have had a heart attack you may live longer if you are prescribed them. They can be combined with diuretics for an additive effect and may be available with a diuretic in a single tablet, such as Tenoretic.
Calcium antagonists act to expand the arteries, making it easier for blood to flow (like widening the hose pipe). They can be used with diuretics and some can be used with beta-blockers. The exception is verapamil (Securon, Cordilox, Univer) as the heart rate can get dangerously slow. Calcium antagonists are helpful if you have asthma, and do not affect the medications that you may be receiving if you have diabetes. Commonly prescribed medications are amlodipine (Istin), diltiazem (Tildiem, Adizem, Dilzem), nifedipine (Adalat), verapamil (Securon) and felodipine (Plendil). Side effects include water retention (causing swollen ankles and legs), headaches, constipation (especially verapamil), occasional palpitations and sore gums. Impotence is unusual. Again these are useful medications which seem to be of more value in the elderly and African-Caribbeans. Older people and African-Caribbeans have a different hormone pattern from the kidneys, which makes calcium antagonists more effective.
ACE inhibitors and angiotensin II (AII) antagonists are widely used. ACE stands for angiotensin-converting enzyme. This enzyme is normally present in the body; blocking it causes the blood vessels to relax (the blood pressure falls as it meets less resistance) and reduces salt and water retention. Angiotensin II antagonists act in the same way but at a different point from ACE inhibitors – the end result is the same but the cough side effect of the ACE inhibitors (see below) is usually avoided.
ACE inhibitors include captopril (Capoten, Acepril), lisinopril (Carace, Zestril) and enalapril (Innovace), whilst the AIIs include losartan (Cozaar) and valsartan (Diovan). They both act much the same way by blocking chemicals that constrict the arteries and retain salt and water. If you have heart failure, ACE inhibitors and AIIs can lengthen your life and can protect people with diabetes from kidney damage. The main side effect is a dry hacking cough. These are important medications which have few side effects and are not known to interfere with your quality of life. AIIs do not usually cause problems with men’s erections. ACE inhibitors have recently been shown to benefit patients with coronary artery disease in the absence of high blood pressure or heart failure.
Alpha-blockers act on nerve receptors to dilate the arteries – this in turn lowers the blood pressure. Prazosin (Hypovase) and doxazosin (Cardura) are the most common ones. They can cause tiredness and dizzy feelings. Their major advantage is the reduction in prostate symptoms in a man. They can be combined with all the other medications and are safe in people with asthma or diabetes.
Renin inhibitors are a new class of drugs that inhibit renin, a kidney hormone. Aliskiren (Rasilez) is now available and acts like ACE inhibitors and AIIs, relaxing the arteries. Diarrhoea can occur and checks on kidney function and blood tests for potassium are advised. Its role at present is limited.
I read in the newspaper and saw a report on TV that calcium antagonists can be dangerous – is this true?
Unfortunately for reasons that are not clear, there were scare stories about calcium antagonists. The evidence has been refuted by other researchers who looked at the claims in depth. Very high doses of nifedipine capsules can cause angina because of the speed of action of this preparation, but the capsules are not used routinely and very rarely in high doses. Claims made of an increased risk of heart attack or cancer do not stand up to careful scientific scrutiny –the claims are so devoid of scientific fact that the stories should not have been put out publicly. Much of what has been written about the dangers of calcium antagonists is nonsense and this has upset many patients and doctors. There is no danger if you take long-acting calcium antagonists, e.g. amlodipine, nifedipine LA (long-acting), and diltiazem LA, but you should avoid short-acting formulations, e.g. nifedipine capsules. The calcium antagonist scares are a classical example of media hype with commercial undertones.
Someone told me that one particular medication for blood pressure makes your hair grow – is this true?
Yes. Minoxidil is a very potent treatment used only in severe resistant blood pressure cases. It can make people put on weight because of water retention and is not used routinely for this reason. It also makes your hair grow – this can be an advantage in bald men but is not usually liked by women!
You have not mentioned Aldomet. I am pregnant and my doctor prescribed this medication for my blood pressure. Why did she choose this rather than the others that you have talked about?
Methyldopa (Aldomet) is an old and effective drug for lowering blood pressure but it does have a large number of side effects. It can cause drowsiness, sluggishness, a dry mouth, depression and impotence (see Chapter 8). Because of these effects, it is not used so much these days and has been replaced by more user-friendly medications. However, it is effective and its main use today is for raised blood pressure in pregnancy, as the medication does not cause harm to your baby. It is usually stopped on delivery to reduce the chances of depression following the birth.
I’ve read about a new medication called Physiotens which was called a breakthrough for blood pressure treatment in my newspaper. Should I get my doctor to put me on it?
Physiotens is the trade name for moxonidine. It acts via the brain and is advised for mild to moderate hypertension if other drugs are not appropriate or are not fully effective. Side effects include dry mouth, headache, fatigue, dizziness and sleep disturbance. It has an effective but limited place in treatment.
When I went to see my doctor, he measured my blood pressure and put me on tablets straight away. Why was this?
If your blood pressure was very high when it was first measured, it would be unlikely that changing your lifestyle alone would help. However, it is worth trying the measures discussed in the section Self-help earlier because these may help to reduce the amount of tablets you need.
I have been feeling tired and lethargic lately. Do you think my tablets are causing the problem?
All medications can cause side effects. We try hard as doctors to
prescribe the safest and most convenient medications. If you are concerned that a particular medication is causing a problem, let your doctor know. It may have occurred by chance but it may also be associated with your treatment and a change in your medicine could relieve the symptoms. For instance, if you feel that your sex life has been affected, it may be due to your medications.
I am on treatment for high blood pressure. I know that some medications cause side effects. What should I look for?
If you feel unwell and are taking tablets, do not stop or modify your treatment in any way, but contact your doctor. He will advise what changes or modifications are necessary. This is an important point to remember because a sudden stoppage of treatment can produce what is called a ‘rebound effect’ in the level of blood pressure (it shoots up).
Seek your doctor’s advice if you experience any of the following symptoms, but do not alter your treatment on your own.
•headaches
•visual disturbances (blurred vision)
•shortness of breath
•chest pain
•altered ability to concentrate
•memory loss
•passing more urine at night
•sexual problems/erectile dysfunction (impotence)
Remember that some of these symptoms are just as likely to be due to your blood pressure rising as to it being overtreated, so you may need to change, reduce or increase your tablets.
I have heard that blood pressure pills can affect your sex life – is this true?
The short answer is sometimes. The usual complaint is of men failing to get an erection firm enough or lasting long enough for sexual intercourse. Blood pressure itself can cause this problem and only occasionally are the drugs used to treat it, e.g. diuretics, incriminated. If it is drug-induced it will occur in the first 2–4 weeks of therapy and a different drug can then be tried. The least likely drugs to cause male erectile dysfunction (ED) are the AII antagonists (see Table 2.2) and the alpha-blockers. Female problems with lack of arousal have been reported with beta-blockers. Both men and women can get sexual problems as a result of heart disease and sometimes its treatment; if you have a problem, talk about it with your doctor or practice nurse. There is more on this subject in Chapter 8.
While I am taking my tablets, can I lead a normal life or is there anything I should avoid doing?
Although treatment controls blood pressure effectively through out the day, it is only sensible to avoid as much as possible any events or circumstances that increase your blood pressure, such as highly emotional or stressful situations (see the section Stress below)
Keep your weight under control (Chapter 9), moderate your alcohol, fat and salt intake and give up cigarettes if you smoke; you should then be able to live as normal a life as possible, including a normal sex life. Above all, you should not consider yourself an invalid – you are not!
I am told that I have high blood pressure and need treatment, but I don’t seem to have any symptoms. If I do not feel unwell, why should I need it?
Very often high blood pressure does not make you feel ill. This is possibly because the increase has been gradual over such a long time that you have adjusted to it. However, all the evidence shows that, if high blood pressure is left untreated, you have a greater chance of stroke, heart attacks and complications in the kidneys and eyes. When blood pressure is treated, there is overwhelming evidence that these risks are substantially reduced. Therefore, it is important, and in your interest, to take your medication exactly as prescribed by your doctor, even though you may feel quite well.
Now that I have been prescribed tablets, how long will my treatment last?
The treatment for high blood pressure, whether by lifestyle changes or drugs or both, continues for life, but as many of the medications used in its treatment need to be taken only once daily, interference with your normal lifestyle can be kept to a minimum in the majority of cases. Sometimes, if you have reached your target weight, you may have your tablets reduced or stopped, in order to see if you still need them. Ask your doctor if this is worth a try for you.
I don’t mind taking one tablet a day, but one of my friends has so many that she rattles. Will these tablets be all that I need to take?
Most blood pressure patients end up on more than one medication. With some patients other factors or conditions may complicate the situation and treatment for these may also be required; you may then have to take several tablets a day. For example, if you develop angina, the tablets may need to be changed to relieve you of your chest pain (see the section Treatment in Chapter 3). If you develop diabetes, specific diabetic tablets may be needed. We try to tailor the treatment to the individual, aiming to keep your quality of life as good as possible – so if a diuretic causes gout, we can change to a beta-blocker, and so on. We try to give you the minimum of inconvenience, but also to keep you in good health.
My blood pressure seems to be resistant to many drugs and I have now been put on spironalactone. How is this different?
Spironalactone is a diuretic (water tablet) that antagonises a hormone called aldosterone. It can be very useful when the blood pressure is proving difficult to control. Kidney function needs to be monitored, and as it retains potassium caution is needed if used with ACE inhibitors or AIIs. The commonest side effects are stomach upsets and swollen breasts, mainly in men (gynaecomastia), which can be painful. Erection problems in men, and period changes in women, can also occur.
What should I do if I forget to take my tablets?
For most people, there is no need to worry, as the blood pressure will only rise slowly, so you can get back on schedule the next day. If you are on a beta-blocker and also have angina, you should take the medication immediately you realise that you have forgotten it, as a means of catching up.
RISKS OF HIGH CHOLESTEROL LEVELS
Facts and figures
There is a lot of talk these days about lipids and cholesterol
and now I’ve seen something about triglycerides! I am rather muddled about it all. Can you tell me what all these words mean?
Cholesterol is a fatty or oily substance and is one of a group of fatty substances we call lipids.
Lipids are essential for the normal functioning of the body’s cells. Problems develop when there is too much lipid in the blood. It then settles in the walls of the arteries. The arteries then develop the narrowings which cause heart attacks and angina by restricting the flow of blood to the heart (see the Introduction to this chapter). Doctors often ask for a ‘lipid profile’: this is a check on the levels of cholesterol and triglycerides in your blood. (Triglyceride is another fatty substance – see below).
Cholesterol plays an essential role in helping our glands make hormones, but its biggest role is in the formation of cell walls. We are able to make all the cholesterol we need in the liver, where it is made from fat. Our problems begin if we have a higher blood cholesterol than we need; this is usually due to eating too much fat (see the question later on hypercholesterolaemia).
Triglycerides (pronounced ‘try-gli-sir-ides’) are the major form of saturated fats (see later question) which come from food and they are also made in the body to provide energy. If you have a high level of triglycerides and a low level of high density lipoproteins (see next question), you have a greater chance of developing coronary disease. Triglycerides are commonly raised in people who are very overweight, people with diabetes and those who have a high alcohol intake.
I was told that all cholesterol is bad for you. Now I read that there is a ‘good’ cholesterol and ‘bad’ cholesterol. What’s the difference?
Cholesterol and other fats do not dissolve in the blood. They hitch a ride on proteins which are the taxis transporting the fats around. The combination of fat and protein is a lipoprotein (pronounced ‘lie-po-pro-teen’). The ‘bad’ cholesterol is the low density lipoprotein (LDL): this is the main carrier of harmful cholesterol to your arteries where it builds up to cause narrowings. The high density lipoproteins (HDL) are the good guys: HDL tends to pick up excess cholesterol taking it away from the arteries and transporting it back to the liver for removal. So, for maximum protection, you need:
•your LDL low (L for lousy);
•your HDL high (H for happy).
I’m going to have a complete check-up next month. When I have my cholesterol profile checked, what levels should all these different fats be?
Your total cholesterol should not be above 5.0 mmol/litre.
The HDL (see question above) should be greater than 1.0 mmol/L in a man, and 1.3 mmol/L in a woman.
The LDL should be 3.0 mmol/L or less – the ideal is 2.6 or less.
Your triglycerides should be less than 1.7 mmol/L, ideally 1.6 or less.
As a rule of thumb, a total cholesterol of 5.0 equals an LDL of 3.0.
However, for coronary patients and those with chronic renal disease or diabetes, the targets are lower:
•cholesterol 4 mmol/L or less;
•LDL 2.0 mmol/L or less.
So remember 5 and 3, and 4 and 2.
Research has shown that lowering cholesterol to these levels in normal people, as well as in coronary patients, helps prevent heart disease in the future. The benefits apply to both men and women.
When I had a lipid profile done on my blood, the doctor told me I had hypercholesterolaemia. What does this mean?
Hypercholesterolaemia (pronounced ‘hi-per-kol-esterol-eemia’) means that the total cholesterol is high in the blood. Usually the LDL (see question above) is raised; in women the HDL is higher before the menopause – an effect of their hormones. It is always better to know both profiles (HDL and LDL), as well as the total level, because you don’t want to lower a high HDL by mistake. For example, a woman before the menopause may have a high total cholesterol (e.g. 5.8) which is made up mainly of the good HDL (e.g. 2.0).
When I look at a food label, there are different types of fats listed, such as saturated and unsaturated fats. Can you explain more about the differences between the types of fats?
There are two main sorts of fats.
•Saturated fats are mainly of animal origin. They are the bad fats and it is the saturated fat that raises your cholesterol levels.
•Unsaturated fats are mainly of vegetable origin and they lower your cholesterol levels.
Saturated fats are a mixture of alcohol, glycerol and fatty acids. The fatty acids contain long chains of carbon atoms – most commonly 12, 14 or 16. These are the most effective at raising the LDL (‘bad cholesterol’) in the blood. The more saturated fat we eat, the higher the cholesterol; if we eat less, our cholesterol will fall over 3–4 weeks.
Unsaturated fats contain carbon atoms that are joined (with double bonds) at certain points; this leads to the fats being liquid or soft at room temperature. When there is one double bond, the fat is monounsaturated; when there are two or more, it is polyunsaturated. Monounsaturated fats include olive, rapeseed and peanut oils and are contained in avocados, almonds and oily fish. Polyunsaturated fats include sunflower oil and most soft margarines (always read the label!). Polyunsaturated fats help prevent blood clots forming, which is another benefit in addition to their cholesterol-lowering effect.
As well as lowering your LDL (bad) cholesterol by switching you away from saturated fat, unsaturated fats also appear to have an additional good effect on lowering cholesterol. Monounsaturated fat may raise the HDL (good) cholesterol as well. All kinds of fat, whether saturated or unsaturated, are rich in calories, so you need to bear in mind, when you change to a healthy diet, not to go overboard on unsaturated fat.
Chapter 9 gives lots of information about which foods contain the different types of fats and gives you lists from which you can choose a healthy diet.
The media has also talked about the harmful effects of trans fatty acids. How can I avoid them?
Trans fatty acids are present in small quantities in meat and dairy products but are present in larger quantities in those oils which have been manufactured to be firmer at room temperature (i.e. when oils have been made into margarines or spreads) by a process known as hydrogenation. Trans fatty acids raise LDL and lower HDL cholesterol levels. When you are selecting vegetable oils and margarine it is important to look for the trans content. The best oils are blended vegetable oils, rapeseed oil and soft margarines that are low in saturates and trans fatty acids, but high in polyunsaturates and monounsaturates (see the question above). Always read the margarine label.
The article that I read also mentioned vitamin E as being beneficial. Why is it important?
Vitamin E is an antioxidant; antioxidants help protect the body from ‘free radicals’. Free radicals are produced by some of the normal chemical reactions in the body cells. They are unstable and, in excess, can damage the lining of the cells by oxidising LDL (‘bad’) cholesterol, causing it to stick to the walls of the arteries.
Antioxidants are present in fruit and vegetables and can prevent cholesterol being oxidised so that it does not tend to stick to the artery wall.
Some early studies suggested that vitamin E protects against heart disease, but unfortunately subsequent studies have not shown any benefit from tablet supplements. Vitamin E is present in food containing a lot of polyunsaturates, such as vegetable oils (especially sunflower) and deep green leafy vegetables. Nuts and vegetable oils, although good sources of vitamin E, are also high in calories, so these should not be eaten too frequently. There is a small amount of vitamin E in wholemeal bread. Some margarines are enriched with vitamin E. If your food intake is high in polyunsaturates, it will contain a lot of vitamin E. Because some of the major sources are high in calories, you may be advised to take extra vitamin E as supplementary tablets by some specialists to avoid putting on weight, but for most of us this will not be necessary. Chemists and health food shops sell vitamin E preparations and the recommended dose is 100–200 units a day (70–140 mg). However, as vitamin supplements have been shown to be of no benefit – save your money!
You have talked about vitamin E. What about vitamin C – isn’t this an antioxidant as well?
Yes, and it is safe to take, but medical trials have demonstrated no benefit for heart disease. It is found in citrus fruits (oranges, grapefruits, lemons), kiwi fruit, soft fruit (strawberries, raspberries, blackberries), red and green peppers and spring greens. Try to eat 150–200 g (6–8 oz) of this group a day and you will not need tablet supplements.
I have always believed taking vitamin supplements would protect me – are you saying this is not true?
Unfortunately yes. The Heart Protection Study involved thousands of patients and those taking vitamins did no better or worse than those taking placebos (fakes). In other words, vitamins do not protect against the effects of hardening of the arteries and are of no benefit to the heart. The vitamin story is a good example of an idea that is theoretically good but, when tested, does not work.
I know of people taking beta carotene supplements and our health food shop is always marketing it. What is beta carotene, and should I be taking it?
No. Beta carotene is converted in the body to vitamin A. It is an antioxidant and is found in brightly coloured fruit and vegetables (carrots, broccoli, tomatoes, melons, yellow and orange peppers, spinach, peaches). So you might think that extra supplements would be good for you. However, medical trials have failed to show that they have any benefit, and researchers are now worried that they may lead to an increased risk of some cancers and heart disease. Do not waste your money on beta carotene supplements – fruit and vegetables are all that you need.
I thought that people supplementing their diet with extra beta carotene from the health food shops had a lower chance of developing heart disease or cancer. You say that there may be risk of developing these conditions – which view is right?
This question is a good example of the need always to make sure that a good idea works when put into practice. Beta carotene has antioxidant properties and, in theory, could help prevent cancer and coronary heart disease. Indeed, people who took beta carotene supplements were observed to be less likely to develop these diseases – but an observation is not proof. Four research studies involving thousands of people set out to prove whether a benefit existed when beta carotene was compared to placebo (see the section Other treatments for angina in Chapter 3). These were proper scientific studies. Surprisingly and alarmingly, beta carotene supplements were shown to increase heart disease and cancer risks, especially in smokers and people exposed to asbestos. Ideas, whether based on good scientific theory, as in the case of beta carotene, or dreamed up in the bath, should always be validated! Beta carotene should be consumed normally in fresh fruit and vegetables.
There is so much advice about fat intake that I really don’t know what to believe. How much fat should we eat a day?
This depends on whether you need to reduce weight, that is, reduce calories. Remember that fat, whether good (unsaturated) or bad (saturated) is high in calories. We need 50–90 g of fat a day of which 22–27 g, only, should be saturates. Always look on the food labels to help you choose foods that contain less saturated fats.
Let’s work out some numbers. Doctors recommend that no more than 30% of your calorie intake is fat, and 10% of that is saturated fat, regardless of whether or not you are overweight. If your daily calorie intake is 1500 kcal, this means 50 g of fat at most (1 g of fat equals 9 kcal). If your daily calorie intake is 2000 kcal, this means 65–70 g of fat; if it is 2500 kcal, this means 85–90 g of fat. (See Chapter 9 for further information on fats in food. )
My father had a high cholesterol level and died aged 55. My wife is concerned that I may be like him – I am now 52. Can this be inherited?
Some people may inherit a high cholesterol level (usually over 8.0 mmol/litre). A good diet changes these people’s levels only marginally and they will need medication. Make sure that all members of your family are checked for an inherited pattern and, if this is detected, you will be recommended medication. Other people inherit a tendency to a high cholesterol level but respond to diet, plant stanols or, more usually, a combination of diet and medications.
Self-help
Should I know my cholesterol and other test level numbers? Will it do any good?
If you want to reduce your chances of heart disease, you must take charge of your lifestyle, and that includes knowing your numbers and keeping track of how they respond to any changes in your eating pattern or medication.
How well will a healthy diet lower my cholesterol?
A healthy diet may reduce your cholesterol by 10%. Obviously the
higher your cholesterol at the start, the more likely you will need medications as well, but a period of healthy diet restricting your fat intake for 3 months is normally recommended first (see Chapter 9). However, if you already have heart problems, most doctors advise immediate medication to take full advantage of its cholesterol-lowering effect.
Which is more important – to avoid foods high in cholesterol or saturated fats?
Cholesterol in your food has a smaller effect on the blood cholesterol level than do foods high in saturated fat. It is more important therefore to cut down on foods high in saturated fat. This means, for example, that you can have three to four eggs a week (the yolks are high in cholesterol). Cutting down on saturated fat (and all fats) will help you to lose weight (see Chapter 9).
I am told that I have a high cholesterol level. If I manage to lower this level, will this really prevent heart disease?
We now have overwhelming evidence that lowering your cholesterol level not only reduces your risks of heart disease by an average of over 30%, but also reduces the need for heart bypass surgery and angioplasty (see Chapter 3). If you lower your cholesterol over a 5-year period, you improve your chances of living longer by an amazing 30%. Treating a high cholesterol is one of the most important means of preventing and reducing the complications of coronary artery disease. Some doctors believe it is negligent not to lower a raised cholesterol.
What should I get my cholesterol levels down to in order to see a benefit to my heart?
Most of the benefit occurs when the LDL (‘bad’) cholesterol is lowered by 30% or more; your aim should be to get this level below 3.0 mmol/litre with an ideal of 2.0 mmol/litre, or less if you have coronary disease, diabetes or a chronic renal condition. This leads to removal of the soft part of the narrowings in the arteries making them less likely to tear or split. It is known as stabilising the plaque (see the Introduction to this chapter). Unstable plaque that ruptures releases soft cholesterol into the blood which then causes a clot to form and a possible heart attack to occur – removing the soft cholesterol helps to prevent this happening.
I have reduced my cholesterol level so that the tests are now normal. Can I go back to smoking?
No. Risk factors, which increase your chances of developing heart problems, are independent of each other. If you have more than one risk factor, however, they don’t just add up, they multiply.
Table 2.4 Cholesterol-lowering drugs
Drugs |
Effects |
Side effects |
Statins |
|
|
Fluvastatin (Lescol) |
||
Fibrates |
|
|
Ciprofibrate (Modalim) |
||
Resins |
|
|
Absorption inhibitors |
|
|
I have seen cholesterol self-testing kits in the chemists. Are these any good?
Not really. They are not as accurate as we had hoped they would be.
Do I need to starve for the blood test?
A blood sample which will show the levels for total cholesterol and
HDL can be taken at any time, and this will be a useful screening test. However, the LDL and triglyceride levels are influenced by diet and should be measured after at least nine hours of fasting, but you can drink water.
My doctor has only measured my total cholesterol level. Is this enough, or should I ask for all the different levels to be measured?
When your doctor is giving you a screening test, the total cholesterol level is a good guide. A total cholesterol of 5.0 or less is satisfactory and remember that 5.0 of total cholesterol is equivalent to 3.0 of ‘bad’ LDL. However, if your doctor is planning your treatment, a full lipid profile is needed to guide therapy properly. If you are going to be on medication for a long time, you need to be sure that you are on the right type.
When should I have a repeat cholesterol level test?
When you have been on your new healthy diet for 3 months, the doctor will ask you to come in for another test.
Treatment
What happens if my second cholesterol level test is still raised?
You will need medication. Fortunately, the medications that you might be given are safe, simple to use and very effective – usually your cholesterol levels will begin to fall within 21 days.
What medications are there to treat high cholesterol levels and are there any side effects?
The commonest medications that you may be prescribed are known as the statins (see Table 2.4). They reduce the production of cholesterol in the liver. Side effects are rare but you may get indigestion, muscle aches and pains, sleep disturbance, rarely a rash, and possibly a reduced sex drive or impotence. After you have been on one of these medications for 3–4 weeks, your doctor will want to check your cholesterol again to make sure that the dose is right and that you are not suffering from any of these side effects. Always tell your doctor if you feel that you are having side effects.
The next most common group of medications is the fibrates. These are used more when your HDL is low and your triglycerides high. Stomach upsets and skin rashes occur sometimes as side effects.
Sachets of medications known as the resins are used less these days as they can cause a lot of stomach trouble and they taste like wallpaper paste (not that I have tried it) or sand. Ezetimibe acts to prevent the absorption of cholesterol and is often used when statins are not fully effective or causing side effects. It can be used in combination with statins to provide additional cholesterol lowering (see later).
A combination of medications is occasionally used to increase their effect, when a single medication is not enough to get the levels right.
I have been prescribed cholesterol-lowering medication, although I am only 50. Will I always need medication?
Usually, yes. Occasionally, after a time when you have been losing weight and eating healthily, the medication can be stopped for a month to see what happens; usually your cholesterol goes up again, but at least you’ve proved that you do need medication.
If you have coronary disease, lowering your cholesterol will help reduce your chances of a heart attack or the need for heart surgery or angioplasty. Lowering your cholesterol will also help to lengthen your life. For most people, one, or occasionally, two tablets a day plus a healthy lifestyle are all that is needed. The tablets are easy to take, with few side effects. This is one occasion when ‘keep on taking the tablets’ is very good advice and, in terms of healthcare, very good value.
When I have finally got my cholesterol level under control, how often should I have it checked?
Every 12 months.
I have been on cholesterol-lowering medication for some time now. When I go for a check-up, my doctor checks my liver. Why?
It is in the liver that the statins, in particular, get to work, and, very rarely, cause an upset; the tablets then have to be stopped. If you are unfortunate enough to have this side effect, you will be pleased to know that the liver will get better, once the medication has been withdrawn. Statins do not cause cancer.
Can lowering cholesterol levels be harmful, as I have read that lowering cholesterol increases the chances of suffering a violent death or suicide?
There were some reports suggesting this but, by proper scientific study, they have been disproved. This is called evidence-based medicine. Lowering cholesterol reduces your chance of dying from heart disease and does not increase your chance of dying from anything else. There is no increased risk of cancer.
I have had a heart attack and even though my cholesterol was only 4.5 I have been put on a statin – why is this?
If you have coronary disease, the level of cholesterol at which you developed it is too high for you. Studies have shown a significant benefit in reducing heart attacks, strokes or death in those with known coronary disease or those at high risk (such as those with diabetes), who start with a cholesterol as low as 3.5 mmol/litre. Statins have other properties other than lowering cholesterol and can reduce the inflammation in the narrowing of arteries, preventing disruption. So, once the disease is known about, the treatment is more aggressive because the benefits are substantial.
I have read about a new cholesterol drug called Ezetrol – when is this used?
Ezetrol is the UK trade name for ezetimibe; this is a drug that acts to prevent the absorption of cholesterol in the bowel. It is a fixed dose of 10 mg and lowers LDL cholesterol by 10–20% when acting on its own or added to statin therapy. Side effects are not common – mainly nausea and bloating and occur in only 2% of people taking it. It is used when statins are not tolerated at all or when the dose needed to achieve your target for LDL cholesterol causes side effects – it can then be added to a lower dose of statin, which is tolerated, to get an additive effect. To date there is no evidence that it reduces heart attacks, so statins are the number one choice. There has been some concern about an increased cancer risk but a detailed review of the research did not confirm this. Like all new drugs, its use will be carefully supervised.
OTHER RISK FACTORS
FOR CORONARY HEART DISEASE
Being overweight – obesity
I don’t feel overweight but the doctor says I am. Have I got more chance of developing heart disease because of this?
Very overweight (obese) people do have more chance of developing heart disease and this has been mentioned earlier (see the section Risks of high blood pressure). Being fat increases the work the heart has to do, causes high blood pressure and leads to abnormal blood lipids (hypercholesterolaemia). It can also lead to you developing diabetes (see below). You should try to reduce your weight – see Chapter 9 for advice about healthy eating and losing weight. Big bellies are bad for your heart!
Stress
I have a very stressful job. Am I more likely to get heart problems?
There is no proof that stress actually causes heart disease but it can contribute to the symptoms. It is like a trigger, setting things off.
Stress is a state of mind, not an illness, so it is difficult to obtain a precise measurement of it. We all feel stress but it affects us in different ways and we respond differently. Under stress people may smoke or drink more, overeat for comfort or have slightly higher blood pressures.
Stress can be fun as well as unpleasant, for example watching a close team match or taking part yourself in team games. A sudden acute stressful incident is the most dangerous (such as a near-miss on the motorway) but usually cannot be avoided. Stress interacts with your chances of developing heart disease and can make them worse.
Will I be able to recognise the symptoms of dangerous levels of stress?
Symptoms will vary but, in general, when stress is detrimental, you will become tense, nervous and often afraid; you may sleep badly, wake early and have tension pains in the muscles of the neck or back.
Is there any way I can reduce my stress levels?
Yes, there are various ways you can help yourself.
•Try to remove yourself from a stressful environment for some of the day. If work is stressful, go for a walk at lunch time. Keep physically active.
•Don’t rely on caffeine or alcohol and don’t smoke.
•Learn that you cannot solve all life’s problems alone and that they are not all caused by you.
•Try relaxation tapes, yoga or deep breathing exercises.
These work well for some people (see below).
•Spend less time with people who irritate you.
•Try to avoid rush-hour travel (leave for work earlier and walk the last mile or so).
•Talk through any problems at work or with friends (don’t repress them and let them fester).
•Avoid over-commitment – be positive but don’t be afraid to turn things down.
•Don’t rush about; take your time, plan what you are going to do and follow it through – again be positive and don’t be deflected.
•Most of all, keep life in perspective – yesterday is gone, tomorrow hasn’t happened, just get on with today and enjoy it.
The most important therapy is your own. Look at what you are doing and ask what your priorities are. If you had one day left in your life, would you shout and yell in traffic, or swear at the railway guard because the train is late (again!), or would you spend time with your loved ones, telling them how much they mean to you. Take deep breaths and keep the world in proportion. If you must do something, punch a pillow but laugh at yourself as you do it!
Really stressed people usually have other psychological problems which benefit from counselling or a support group. If you are unlucky enough to have a heart attack, a ‘cardiac rehabilitation programme’ is invariably helpful. It provides expert help and support as well as guidance on exercise and a healthy lifestyle. It is usually run by nurses who understand your fears and worries, and can help you regain your confidence.
Diffuse your feelings by using art, music, dance and exercise as a relief valve. There are many videos, tapes and books on stress management which people have found useful. Any relaxation technique will help. Yoga is a very useful exercise and is an ideal way to wind down and relax. Take evening classes which will allow you to meet others and get away from your normal daily routine.
Above all else, remember that by bringing stress under control you will not only benefit your heart but also improve your outlook on life, allowing better and more complete relationships with loved ones, friends and colleagues at work.
Why is so much emphasis placed on stress in the media?
There is a lot of money in stress management and it is an easy diagnostic dustbin. If you have a funny illness, it’s ‘a virus’; if you can’t explain something, it’s ‘stress’!
I have read about type ‘A’ and ‘B’ personalities having an effect on the heart. What is the difference between them?
Some psychiatrists divide the world into two groups, type A and type B people. Type A people are competitive, intense and driven by success. Type B are relaxed, unhurried and content with their lives and achievements. Type A personality has been linked to heart disease but several studies have failed to establish a direct connection. It may well be the consequences of a type A personality that establish a relationship with heart problems, reflecting the degree of anger and frustration that these people feel rather than their attitudes and activities alone.
Do different emotions affect the heart adversely?
Anger appears to be the most dangerous emotion, increasing heart
strain by raising blood pressure and increasing heart rate. If you are angry, write a letter about the person or problem, expressing your anger, then tear it up. (Don’t send it!) Yell and shout at a mirror, then laugh at yourself as you regain perspective. Learn to count to 10 slowly, while breathing deeply.
I feel that I am stressed at the end of the day. What can I do?
You are probably overdoing things and overcommitted. Look at your day: can you organise it better?
•Does anyone or any issue stress you more? If so, bring it into the open.
•Walk some of the way to work and try to get out at lunch time.
•If you feel trapped in your home all day, make the effort to go out – go window shopping, walk round a shopping mall if it is raining; walk in the park if it’s fine.
•Complete the day with deep breathing exercises, have a warm soak in the bath, clean your teeth and freshen up.
•Read a book, do a crossword, work on a hobby project, or ‘surf the net’ and think about your priorities.
•If you have a pet, pat it or stroke it – play with the cat, or walk the dog.
Stress is usually present when emotions are bottled up and everything gets out of perspective.
Diabetes
I have had diabetes for 30 years. What is the effect of diabetes on heart disease?
People with diabetes do have more heart disease than those without. Whilst very good and strict sugar control may reduce some of the risk, this is undone by an increased number of hypoglycaemic attacks. Although you can’t help having diabetes and, unfortunately, it cannot yet be cured, you can help the other factors that cause heart disease. Do not smoke, keep as fit as you can and avoid getting overweight; keep your cholesterol in check and aim for a normal blood pressure.
Many doctors routinely put people with diabetes on statins to reduce the risk no matter what their cholesterol level is.
I have diabetes and have now been told that I have insulin resistance and am at risk of heart disease – what is insulin resistance?
Normally, when you eat food, your blood sugar (glucose) levels go up; your body produces insulin as a response; insulin helps glucose to be taken up by the tissues, the glucose in your blood falls, and then your insulin level falls. It is called a negative feedback mechanism. If you are insulin-resistant the action of insulin in the tissues is less effective than it should be and glucose (sugar) is not used properly, so the sugar and insulin levels remain raised because the feedback is interrupted. Insulin in high levels can raise the blood pressure, cause salt and water retention and raise LDL (‘bad’) cholesterol and lower HDL (‘good’) cholesterol. Therefore, yes, insulin resistance can increase your risks of developing heart disease.
Being overweight, particularly abdominal obesity (a fat belly), is associated with or causes insulin resistance and Type 2 diabetes. By reducing weight, both diabetes and insulin resistance can be controlled or even overcome. It is more common among Indo-Asian people. Besides reducing your weight, you can also take medications to lower insulin resistance such as metformin or other anti-diabetic drugs.
Illegal drugs
I worry that my teenage daughter might have access to drugs. Do illegal drugs affect young people’s chances of heart problems?
Cannabis (or ‘pot’ or marijuana) increases the heart rate and blood pressure as well as body temperature. It also contains carbon monoxide in the smoke. Although it can help some medical problems, for example, the nausea of cancer therapy, severe pain and multiple sclerosis, heart problems is not one of them and it is therefore not recommended.
Cocaine (‘crack’) is a powerful addictive drug which can cause blood vessels to shut down (go into spasm; see Figure 2.7). It can raise blood pressure, cause strokes and lead to severe heart disease, provoking irregular heartbeats, inflaming heart muscle and causing heart attacks. Just one ‘fix’ can do it – my advice is don’t try it.
You may have heard that morphine helps the heart. It is not that simple. Children may begin with the idea of taking heroin (related to morphine) in small amounts and keeping it under control, but the addiction takes over, infection risks rise (from dirty needles or impure products), the heart valves can become severely damaged and the heart, overwhelmed by disease, gives up functioning properly. This leads to heart failure, resulting in a rapid and inevitable premature death.
If you think your child may be addicted, seek help. Help is available for recovery but an addict needs to admit to addiction, want to end it and accept help from professionals.
Ecstasy has been very much in the news. Taking even one ecstasy tablet is akin to committing suicide. It may cause a very high fever, irreversible brain damage and heart failure.
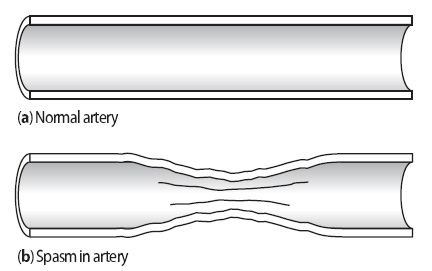
Figure 2.7 Lengthways section of (a) a normal artery and (b) an artery
in spasm, which narrows the opening available for blood flow.
WOMEN AND CORONARY HEART DISEASE
I am a mother aged 53. I am concerned to read that coronary heart disease is a major risk for me. Isn’t this a man’s disease?
Of the deaths from heart attacks each year, nearly half are in women. All forms of heart and blood vessel diseases added together claim twice as many women’s lives as do all forms of cancer. Although fewer women have heart disease than men at the age of 50, they have caught up by 65–70 years of age. The main difference between men and women as regards heart disease is not if they are going to get coronary disease, but when; the difference in its timing is about 10 years.
Coronary heart disease is therefore your – and other women’s – biggest problem too. It is becoming more of a woman’s disease as women tend to live longer; coronary disease is partly a problem of getting older, so more women will eventually develop it. The problem is going to increase as the population ages in general. More men and women are now surviving heart attacks, so they are likely to encounter heart problems later – an increased chance of angina or a further heart attack, unless they try to reduce their risks. Women are more vulnerable to the risks of cigarette smoking and high blood pressure but less so to that of cholesterol. Having diabetes sadly wipes out any advantages that women may have had over men (see above).
My father had heart disease and I am concerned that my daughter might develop heart disease also. I know that she smokes. How can I help her avoid heart disease?
Your daughter may have an increased risk of heart disease if it runs in your family but one of the best ways to help prevent coronary heart disease is to get her to stop smoking. It is well known that there has been an increase in the numbers of young women smoking; their chances of heart disease in later life consequently are rising. If your daughter smokes, she should stop now. If she is thinking about starting, she should think again!
I have read that women’s natural hormones protect us from heart disease. Is this true?
To a degree they do, but if you smoke, have high blood pressure or have diabetes, women lose a lot of this protection. Following the menopause, the normal protection that oestrogen gives disappears anyway. Hormone replacement therapy (HRT; see below) unfortunately does not appear to help.
I have been taking the pill on and off since I was 18. I have just been through the menopause. Am I at any greater risk of heart disease because I have been using oral contraceptives?
Very few women on the pill (taking oral contraceptives) develop heart disease and the low hormone dose pills do not increase the coronary risk. So long as you do not smoke, the low dose pill may actually protect you against heart problems. In women under 35 years of age we do not know what the risk is from taking the pill, nor do we know about its long-term use (over 5 years), although it is unlikely you will be harmed. Cigarette smoking and also taking the pill is not a good combination and should be avoided at all costs. In general the low dose pills are safe, but smokers should preferably stop smoking, or use alternative contraception.
I have felt well since being on HRT but I am worried about its effect on my heart and the risk of breast cancer – what should I do?
There is no doubt that HRT helps with the distressing symptom of menopausal flushes and protects against thinning of the bones (osteoporosis). Initial enthusiasm regarding HRT and heart disease has been replaced with sound scientific evidence of a lack of benefit. Currently HRT is not recommended as a treatment to prevent heart disease developing or to benefit women who have heart disease already. If coronary disease has been diagnosed, other protective treatments should be used – for example statin therapy. Some studies have suggested HRT can actually increase the risk of heart disease, but this risk does not appear to be present if the cholesterol is normal or a statin is also being taken.
A very big study – The Million Women Study – has identified an increased risk of breast cancer if HRT is taken for 5 years or more. We are looking at 1 extra case of breast cancer in 166 women treated for 5 years or 1 extra case in 53 women treated for 10 years. There is no need to panic about these figures, but clearly women on HRT for many years should see their family doctor about discontinuing.
The HRT story is a sad journey from the belief of benefit to the proof of potential harm. There is no role for HRT in women who do not have menopausal symptoms (such as flushes). When flushes are a problem (this happens in 10–20% of women), the risks must be weighed against the benefit, and HRT used for as short a time as possible.
Most women are on combined medications of oestrogen and progestogen but, if they have had a hysterectomy (removal of the womb), they will be on oestrogen alone. All increase the breast cancer risk. With regard to the heart, we are not sure about oestrogen alone but, with all the information we have, HRT cannot be considered a treatment for heart disease.
Whether this advice will change when we know more about raloxifene (see next question) is debatable, but it is obviously important to continue research in this area and advise women on up-to-date scientific facts.
I have read in the paper about a new drug called raloxifene – what advantage does this have?
Raloxifene is one of a class of drugs called Selective Estrogen
(American spelling) Receptor Modulators, or SERMS. Tamoxifen is the one we already have but tamoxifen can sometimes, as a side effect, cause the uterus (womb) lining to overgrow and become troublesome. Raloxifene acts the same as tamoxifen in benefiting the heart and bones, avoids breast cancer risks and does not affect the womb. It is an important drug but like tamoxifen does not reduce hot flushes. It may be an important advance in HRT for women because it looks to have the major benefits without the major risks. A lot of research is taking place to determine how valuable it will be to the heart – proof is not yet available, but early results do not show any harm.
Does HRT have any side effects?
All medication can give side effects and HRT is no exception. You
may feel nauseous but it usually goes after 2 weeks or so – taking tablets after a meal can help this. Breast tenderness and swelling may occur and, again, wear off. If they are persistent, you may be given a different form of HRT to try.
Women worry about gaining weight whilst on HRT. The many research trials do not report weight gain but you should remember that everyone is an individual and if you gain weight, it is you that matters, not the statistics. It is probably due to eating more as you feel better on HRT! Watching your weight is important anyway, so at this time take note of what you are eating and make sure that you take plenty of exercise.
On average, women take 3 months to settle into their HRT therapy.
Does HRT raise blood pressure?
Very rarely. Your doctor or nurse will always check your blood pressure when HRT is prescribed. If you have high blood pressure, you can still take HRT because the chances of your control being upset are so small.
I have breast cancer which is now controlled, and I have also had a heart attack – will HRT help me?
It will not obviously help the heart and it could make the breast cancer worse, so it is not recommended. HRT is not an alternative to proven heart attack treatments.
What sort of HRT therapy is available?
The choice of therapy is best discussed with your doctor. There are two sorts: the first is oestrogen only and this type is for women who have had a hysterectomy (removal of the womb) – this is known as ‘unopposed oestrogen’. The second type is ‘combined’ HRT (containing oestrogen and progesterone) for women who still have a womb, because oestrogen alone in these women will cause excess stimulation of the lining of the womb.
I have been advised to go on HRT but I am resisting as I have read that it doubles your chances of getting blood clots in the legs – is this true?
Yes, this is true. Your normal risk of getting a dangerous blood clot is 1 in 10 000 and it increases to 2 in 10 000 on HRT. So the risk is very small and remains very small on HRT. The risk is higher in those over 60 years of age, but HRT is rarely started in this age group. Smoking and being overweight increase the risk. Talk to your doctor about this, if you think that you may be at risk.
I’m fit and active with no risk factors for heart disease – will I benefit from HRT?
If you have no risks for heart disease, HRT will not improve this as your risk is very low anyway, but you may benefit from HRT by avoiding osteoporosis (thin bones). This is more common in slim women. HRT also helps to relieve hot flushes. Check with your doctor about the possibility of having a bone density scan if you think you may be at risk for osteoporosis.
From the point of view of heart health, who will benefit most from taking HRT?
No one.
I have been taking HRT for 7 years and I think that it is wonderful – I now feel a new woman! However, my doctor says that I should stop it soon. How long should I continue taking HRT?
HRT is usually taken for hot flushes for up to 5 years. Bone benefits continue on beyond 10 years, but the breast cancer risk increases. So, at present, we recommend HRT is stopped.
I’m on HRT at the moment. Do I need regular check-ups?
It is very important that you attend for regular check-ups at first every 3 months and then 6-monthly, and follow your doctor’s instructions. For these check-ups, make a note of any queries or concerns that you might have and discuss them with your doctor.
I have been on oral HRT for some months and my doctor has arranged for me to have a lipid test. Why?
The doctor is checking to make sure that you are not at risk of heart disease, which is good medical practice. Up to the menopause, women usually have a raised high density lipoprotein level (HDL) (greater than 1.3) which helps protect them from coronary disease. This HDL gradually falls after the menopause unless HRT is taken. It is important that women should always have a ‘full lipid profile’ taken (HDL as well as LDL) because a high total cholesterol may reflect good (HDL) rather than bad (LDL) cholesterol levels. Reducing your total cholesterol in this situation might reduce the protective HDL and be counter-productive.
A full lipid profile will also tell you about your triglycerides. Oral HRT can raise triglycerides, but HRT patches have no effect on triglyceride levels. A high triglyceride level is more of a risk in women than in men; the best means of lowering it is by weight loss and regular exercise, along with a low saturated fat diet. An underactive thyroid and too much alcohol can also be a cause.
I do find the advice on HRT confusing – can you clarify it for me?
I’ll try, but doctors find it confusing too!
•HRT definitely helps menopausal symptoms, e.g. hot flushes.
•It definitely helps prevent thin bones (osteoporosis).
•It does not protect against heart disease developing.
•In those with coronary disease, it does not benefit them, so it is not a treatment for heart disease.
•In those with heart disease, it still helps menopausal symptoms and osteoporosis.
•HRT increases the risk of breast cancer.
•Overall, HRT is indicated only if menopausal symptoms are severe and intolerable. It is then given for as short a time as possible and at as low a dose as possible.
I’m concerned that my wife is at risk of heart disease and I want her to take it seriously; she smokes and is rather well padded! However, her doctor does not seem to be bothering either. What should I tell her?
You should point out that women are just as vulnerable to coronary disease as men. Some women don’t recognise this and play down any symptoms of chest discomfort. They usually put their family first. Sometimes they might hide things from the doctor, which makes diagnosis difficult for both angina and a heart attack.
Your wife and every other woman should take heart disease seriously and her doctor, like all doctors, should recognise that women with a mixture of symptoms need taking seriously. Women may be reassured too easily because most women believe themselves to be less likely to have heart disease than men.
Post-menopausal women are at more risk and, even when the symptoms are not typical, these should be discussed and heart disease ruled in or out.
Women are just as likely as men to develop coronary disease if they smoke and just as likely to benefit if they stop. Keeping to a sensible weight and taking regular exercise are also important preventative measures. Tell her that heart disease is an equal opportunity killer and that she should do her best to avoid it for her sake and that of her family.
Send for the British Heart Foundation’s booklet Women and heart disease and present it to her!