5 | Heart failure
Heart failure occurs when the body’s demands for energy are not supplied properly because of a weakness in the heart itself. Heart failure from damage to the heart muscle is common and, at present, 0.3% of the UK population is affected each year. However, it becomes more of a problem with increasing age, as it affects 8% of those over 65 years of age. Put another way, many thousands of people develop heart failure each year, and this represents 5% of acute emergency admissions to hospital. Because heart failure is common in elderly people, one of the reasons why we are seeing more cases of heart failure is the fact that people are living longer. In total up to 2% of the population actually suffers – roughly 1 million people in the UK. Each year 120 000 people are admitted to hospital with heart failure and stay on average 11 days. Heart failure costs the NHS over £300 million per year. Heart failure, if not treated, can significantly shorten life and reduce its quality but we now have means of helping people to live longer and feel better.
CAUSES
Are the causes of heart failure known?
Heart failure usually occurs because of a weakness of the heart muscle. The heart then doesn’t pump as strongly as it should. The most common cause of damage to the muscle is a heart attack but it can also be due to:
•narrowing (hardening) of the coronary arteries;
•high blood pressure;
•narrow or leaking valves;
•a disease of the muscle itself (cardiomyopathy), where the muscle is affected directly, usually by a virus, and not as a consequence of other problems such as high blood pressure;
•excess alcohol consumption over many years.
My daughter has been diagnosed as having cardiomyopathy – what is this condition?
Cardiomyopathy (pronounced ‘car-dee-oh-my-opathee’) is a disease of the heart muscle. The muscles may be too thick – this is known as hypertrophic cardiomyopathy (hypertrophy means thickening) – or too thin and too weak so that the heart enlarges and looks flabby (doctors often call this a ‘saggy bag’ heart). Both conditions can cause heart failure. The commonest is the weak heart and the medical term for this is congestive cardiomyopathy. Hypertrophic cardiomyopathy is usually inherited and can be the cause of sudden death in apparently fit young people. Although coronary disease can weaken the heart muscle, your daughter’s diagnosis of cardiomyopathy is probably related to disease of the heart muscle even though she has normal coronary arteries.
I have read of footballers and other sports people dropping dead from HOCM – what is this?
Hypertrophic cardiomyopathy (see above question) can cause so much thickening of the heart muscle that it obstructs the flow of blood leaving the heart. It then becomes Hypertrophic Obstructive Cardiomyopathy or HOCM. This obstruction is increased when physical exercise or strong emotion increases the heart rate. It can then block the flow of blood or cause the heart’s electric system to become so irregular from lack of oxygen that the person collapses (we call this syncope – sudden loss of consciousness). Sadly, this collapse can be out of the blue and fatal. If the problem can be detected earlier, treatments are available with medication to help prevent a collapse. People with HOCM should be managed in specialised units to allow for optimal care, as it is not a straightforward condition.
How often do sports players collapse and die?
Hypertrophic cardiomyopathy affects one in 500 people and along with other very rare conditions, it is estimated that 0.2% of the athletic population may have a problem with the heart that could affect them at some time. Deaths during sports have been estimated at between one in 100 000 and one in 300 000 in young athletes. However, in older people, because of the increased chance of having coronary disease, the death rate varies from one in 15 000 for joggers to one in 50 000 for marathon runners. Dramatic and newsworthy death during sports is rare. Currently, the Football Association is using some of its income from TV coverage to screen all young would-be football stars by ECG and echocardiography – a commendable approach to safety in the sport.
My husband has heart failure but the doctor says his heart is OK, he’s just anaemic. How can this be?
The heart can fail because of other problems. If there isn’t enough blood (through anaemia or blood loss, e.g. after an accident), the heart will overwork until it fails, because there is so little blood to pump around. It may also fail if the thyroid gland is overactive (thyrotoxicosis) because an overactive thyroid gland drives the heart very fast and can cause it to go into atrial fibrillation (see Chapter 6). Usually the heart recovers when the conditions are treated.
If the heart valves are to blame for weakened muscle, can they be replaced?
Yes. An operation to replace defective heart valves is a successful way of relieving heart failure, providing the heart muscles (the ‘pump’) are not too severely damaged (see Chapter 7).
I have been told that I have heart failure. Is heart failure dangerous?
It can be if not treated properly. People with mild heart failure usually lead a normal life, but those with more severe heart failure will be restricted in what they can do: the weaker the heart, the greater the problem. The good news is that modern drugs, especially the ACE inhibitors (see the section Treatment below), can add many high quality years to the life of anyone with heart failure. If you have heart failure, ask your doctor about ACE inhibitors if you are not taking them – they are very important drugs, and can help you a lot.
SYMPTOMS
What are the symptoms of heart failure?
When your heart does not pump enough blood around the body, fluid builds up because there is not enough energy to push the fluid through the kidneys into your bladder. The medical word for a build-up of fluid is oedema (pronounced ‘ee-dee-ma’). If the fluid builds up in your lungs, you become breathless, with a wheeze or a cough, and you may produce frothy sputum. If the fluid builds up around your ankles, they will swell up and you will be able to see indentations from your shoes or socks or from pressing your skin with a finger (be careful, it can be painful).
My partner has been diagnosed with heart failure but no one would guess on meeting her. However, she does get breathless at night. Why is this?
Fluid builds up in her lungs when she lies down and, if she is asleep, her defences are down. She may wake up with a suffocating feeling. This is helped by standing or sitting up, as this will take the pressure off her lungs. Some people open the window, feeling the need to gulp in fresh air, others walk around or go downstairs to make a cup of tea. If you can reassure her that all is well, this will help her to keep calm. She should tell her doctor that this is happening as medication can help to relieve it.
I have heart failure. Am I right to be worried that I will not be able to lead an active life?
Patients with minimal heart failure usually have no limitations to ordinary physical activity. Mild heart failure leads to breathlessness on walking a mile on the flat, one or two flights of stairs or a long incline. Moderate heart failure tends to cause symptoms more readily – walking half a mile on the flat or one flight of stairs leads to needing a rest. Severe heart failure causes breathlessness on minimal effort and even at rest. Everyone is different, so personal issues are usually best discussed with your doctor.
The good news is that we have treatments that can relieve or at least improve any symptoms so that a better exercise ability and quality of life can be enjoyed. People with more severe symptoms have to learn to adapt their lifestyle once all treatments have been tried and they still remain limited. If you are overweight, reducing your weight can help by taking some of the workload off the weakened heart pump.
You will probably be able to go on holiday and travel as usual, but make your plans more carefully to avoid rushing to catch aeroplanes or trains. Discuss with your doctor if you are planning long journeys while you are on water tablets (see the section Treatment below) as these may need adjusting: dehydration can be a problem on long flights.
Sexual activity doesn’t usually present a problem and is not harmful. As in all forms of exercise, breathlessness might limit what you can manage, so take advice if this occurs (see Chapter 8). Some tablets can make you lose your sexual drive and, if this has happened, you should mention this to your doctor rather than accept it. Your doctor may be able to change your medication. Remember, don’t suddenly stop taking your medication as this could be dangerous.
People often keep to themselves their worries and anxieties. Don’t do this – most of your problems can be alleviated: don’t be afraid to let the doctor know what’s on your mind.
I had a heart attack recently. My cardiologist tells me that my heart has weakened and that I have now got heart failure. Will the symptoms be noticeable?
Your weight may go up from the retention of fluid (1 kg = 1 litre or 1 lb = 1 pint). Your doctor will monitor treatment by measuring your weight loss after you have been prescribed diuretics (these are pills to make you pass more water). There are other symptoms that you might notice:
•feeling tired and washed out;
•swollen ankles (‘I can’t get my usual shoes on’);
•swollen tummy (so your clothing is tight); and
•on occasions, you may get a bit confused.
My doctor says I have a hibernating myocardium. What does he mean?
Your heart muscle looks weak and damaged but is capable of getting a lot of its power back; the damage is not irreversible. The heart is literally hibernating. If your heart only appears to be damaged, it may be possible to strengthen it by angioplasty or surgery. If that is possible, your quality of life and length of life will be greatly improved.
The doctor will check your heart to see what its strength is, either with an echocardiogram, perhaps a nuclear (thallium) scan, or a technique known as positron emission tomography (PET for short). See the section Tests below.
Should I discuss the diagnosis of heart failure with my family?
It is always important with any illness to discuss its effects with close family and friends and, if appropriate, workmates. Having heart failure may limit you because of breathlessness, fatigue and weakness. Your family and friends will be worried about you – by bringing them into the picture they will be able to help and support you.
TESTS
It is important to know the cause of heart failure because, if it is mechanical (such as a leaking valve), you will need a mechanical solution (a new valve). If it is heart muscle failure, you will need tablets. A high blood pressure will need urgent treatment. Investigations sort this out. Usually you will have an ECG (see Chapter 2), a chest X-ray, blood tests and an echocardiogram. These are all discussed below.
The doctor at the hospital told me that I have heart failure. For some reason, he told me to report back for a chest X-ray. Why do I need a chest X-ray for heart failure?
An X-ray picture of your chest will tell him about the size of your
heart and its shape; this will help the doctor work out the cause of your heart failure. He will also get a picture of your lungs and can tell whether there is any infection or fluid there.
You will be asked to stand in front of an X-ray plate, and then told to breathe in and hold your breath for a few seconds. As you hold your breath, the picture is taken. Holding your breath will prevent a blurred image occurring. The X-ray dose is very small and not in any way dangerous.
Why do I need blood tests for heart failure?
Your doctor will need to make sure that you are not anaemic, as this can make heart failure worse (see earlier question). Your kidney function will also be checked and any evidence of a congested liver looked for. Blood may also be taken to make sure that your thyroid gland is not under- or overactive. Any evidence of liver damage from alcohol will be monitored. Liver congestion is not unusual in heart failure and improves rapidly with treatment. A test for Brain Naturetic Peptide (BNP) is frequently performed and elevated levels identify heart failure.
My sister is very concerned that she has been given an appointment to have an echocardiogram. What is this?
This is a painless, simple test which tells us about the size of her heart, how well it is working, how strong the muscle is and how the valves are working. It is often used to assess the significance of a heart murmur and the size of a heart attack, to see if any clots are forming and to calculate the efficiency of the heart’s muscle pump.
How is an echocardiogram performed?
The room, in a hospital or at your family doctor’s, is usually darkened to allow the doctor or technician (cardiac physiologist) to see the screen. You may be asked to lie on your back or side (see Figure 5.1). A special type of jelly is put on your chest and a probe applied to the jelly. The probe is moved over your chest. Ultrasound waves (it is not an X-ray being taken) are bounced off your heart and a picture of the heart’s movements and structure made.
You are usually able to see what is happening and the pictures are stored on video or disc which the doctor may show you. It usually takes 20 minutes and is painless, with no side effects.
Doppler ultrasound is also used and this measures the blood flow. It makes a noise like a washing machine.
My doctor wants a special echocardiogram to see if I might benefit from a pacemaker. What is this about?
A new treatment for heart failure is a special pacemaker which is
used when the two heart pumps are out of synchrony, that is, not beating at the same time. A special echo measures the dysynchrony index. If this is abnormal, it suggests that the heart can be brought back in line with a cardiac re-synchrony pacemaker. The efficiency of the heart will be improved and you will feel better. Sometimes this special pacemaker will be combined with a defibrillator which may prevent you dying suddenly.
I have heard that some echocardiograms are done by the patient swallowing a tube. Is this true and, if so, what is happening here?
Yes, it is true. The reason is that your gullet is situated behind the heart, and a scan from the gullet (or oesophagus, pronounced ‘ee-sof-a-gus’) gives better pictures than one on the chest, when the probe has to steer round the lungs. This is known as transoesophageal (via your food pipe) echocardiography (TOE or TEE in America). It is done when we need specialised additional information, particularly on valve or clot problems. The tube is not large and is usually passed after you have been given relaxing medication and a local spray anaesthetic to the mouth. Some people do find it unpleasant but it is a very important test to help guide your treatment.

Figure 5.1 Having an echocardiogram taken.
I have an appointment at the hospital for a nuclear scan. This sounds rather dangerous to me. Is it harmful and how is a nuclear scan done?
The radioactive levels are low and not at all dangerous – you won’t glow in the dark! A scanning machine takes pictures of your heart following an injection of a radioactive material (usually thallium or sestamibi) into a vein. If your heart is healthy, the thallium is absorbed and an even picture will be shown. If there is damage to your heart, the thallium will not be taken up well by the bits of your heart that are not working efficiently. If there is scar tissue from a heart attack, there will be a gap or a hole in the picture as no thallium will be taken up. If your heart is made to work hard by an exercise test or by the injection of a stimulant to speed it up, the thallium will not travel well to any areas where there is a poor blood supply (such as in that caused by coronary narrowing). When your heart rests between beats and the demand for blood falls, thallium can reach this area. In this way, the scanner can give a very accurate and useful picture to your doctor. First it shows a deficit, but then shows whether this deficit can be rectified. If the scanner shows a hole in the picture which does not improve, then it is likely that the muscle is dead and cannot be improved.
The hospital has written to me and told me that I need a test called a SPECT. What is this?
This is single photon emission computed tomography. It is a 3-D scanning system. You will lie on a table and the scanner rotates to take pictures from different angles, again helping to identify damaged muscle or muscle suffering from a lack of blood supply. It is a sophisticated test but simple to do – like a standard sestamibi scan but with bells on!
I have had test after test until I feel that I could not be tested further. I now have been summoned for a nuclear scan. When is nuclear scanning specifically helpful?
Nuclear scanning can be very useful for people with angina, after a heart attack and when there is heart failure. It is a means of trying to assess the importance of each narrowing present, and whether any good can be done by treatment. It is more expensive than an exercise test but useful when exercise tests cannot be done (for instance if you have arthritis), or when specific information on your heart muscle is needed that a treadmill exercise test cannot provide.
My wife was told that she is going to have a PET scan. How is PET different from SPECT?
PET is positron emission tomography and this is a very specialised technique involving nuclear scanning, and it accurately tells us about blood flow and whether the heart muscle is hibernating or not. It is a very expensive test, so is used only when really necessary. It can, however, identify where help might be possible when other tests have not been able to show what can done; so, used carefully, it represents value for money.
TREATMENT
I have been told that I have heart failure but was also informed that I will not need treatment for some time; why not? And, if I have to have treatment in the future, what might it consist of?
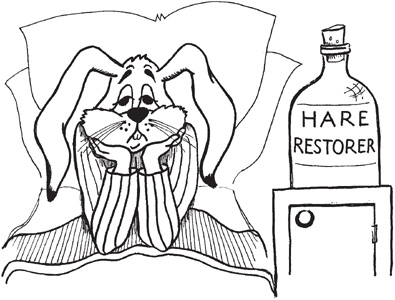
First of all, the tests will decide on the cause of your heart failure. A high blood pressure, coronary artery disease, severe lung damage, excess alcohol and problems with the valves are all possible causes. A leaking valve may be repaired or replaced; a narrow valve can be replaced or stretched by a large balloon (see Chapter 7), and a big scar from a heart attack, which causes the muscle to stretch (aneurysm, pronounced ‘ann-ure-ism’), can be cut out. Most of the time the problem is likely to involve the muscle pump and your treatment then is with tablets (see Box).
I have had an unpleasant jolt, having a heart attack. I suppose that I ignored the advice and warnings. Now I am determined not to lose control again. My doctor says it’s heart failure. What can I do to help myself with my heart problem?
The main thing is to guard against increasing the fluid build-up in your body (in your lungs or legs particularly). Therefore:
•try to lose weight;
•keep as active as you can;
•avoid salty foods or adding salt at the table;
•weigh yourself every day to check to see if you have put on weight which might be due to increased fluid;
•take your medicine as directed;
•keep in touch with your support nurse for advice.
If you find it harder to breathe, your ankles puff up, or you feel generally washed out, go and see your doctor. Don’t let the fluid build up too much as it alters the absorption of some medications making treatment more difficult.
Medication
I have been prescribed diuretics. What are these?
Diuretics are commonly known as water tablets. They act to stimulate the kidney to get rid of the excess fluid which causes breathlessness and swollen ankles. Some tablets, such as furosemide and bumetanide, act quickly: you will notice that you need to go to the toilet a lot over the first four hours or so after you have taken the tablet. This occurs every time you take the tablets but is usually over with by six hours. You need to plan when to take the tablets, so that you are not caught short. Some, the thiazides, are milder and gentler than others and these help to spread the passing of water over a 10–12 hour period.
Most diuretics flush potassium out of the body and this may need to be replaced by tablets. Blood tests will help the doctor keep an eye on the chemicals in your blood. Doctors measure the ‘urea and electrolytes’ levels in a blood sample; these levels monitor your kidney function, potassium and sodium (you can remember them as ‘electric lights’). In addition, as estimated glomerular filtration rate (eGFR) is now routinely calculated to monitor kidney function more precisely.
How will I know if the diuretics are working?
You will be able to breathe better and your ankles will be less swollen. Your weight will go down as the fluid is urinated out. If your weight goes up, you will need more water pills but, if it drops too low, you may need them reducing, as you may have got rid of too much fluid. We try to use the lowest doses possible.
Sometimes the tablets don’t work and the drugs have to be temporarily given by an injection in a vein. This usually needs specialised treatment in a hospital. Once the fluid levels have been controlled, the tablets will be started again and this usually keeps the fluid at bay.
My doctor tells me that I need digoxin to help my heart. Why?
Digoxin is a tablet which in some people helps regulate an irregular heartbeat (atrial fibrillation: see Chapter 6) and makes the heart more efficient. It is also used to strengthen the heart muscle, giving it more pumping power. If the drug builds up too much in your blood, it can cause loss of appetite and nausea. Your doctor may check the level of digoxin in the blood with a blood test and adjust the dose to get the best effect without side effects.
My doctor has taken me off water tablets and put me on ACE inhibitors, which don’t agree with me at all – they just make me cough all the time. Why?
ACE inhibitors stands for angiotensin-converting enzyme
inhibitors. These are very important medicines that, in some people, increase their ability to exercise, as well as reducing breathlessness and fatigue. People will feel better on this medication and their life can be prolonged. Side effects are not common but occasionally people get a dry hacking cough. This is more common in women and Chinese people. If your cough is a problem (and is not due to fluid), ACE inhibitors can be switched to AII antagonists (see under Treatment in the section Risks of high blood pressure in Chapter 2) which have similar effects without producing the cough. Research studies show they are very effective drugs and may improve treatment by being prescribed in addition to ACE inhibitors as well as an alternative if ACE inhibitors cannot be tolerated. Studies with candesartan and valsartan have given impressive results, which are probably applicable to the other AII drugs.
Generally, doctors try to get everyone with heart failure to take ACE inhibitors if at all possible. ACE inhibitors are prescribed with diuretics and have the advantage of retaining the potassium that the diuretics wash out. They are quite often prescribed with diuretics and digoxin. Commonly used ACE inhibitors are captopril, enalapril, lisinopril, ramipril and perindopril.
It is likely that more people will be on ACE inhibitors or AII drugs either alone, or in combination, as the research suggests patients with mild failure do not develop a more severe condition and overall well-being is improved.
My wife has heart failure and gets very breathless. She was prescribed nitrates at her last visit to the doctor. What are these for?
Nitrate tablets (isosorbide mononitrate or dinitrate) are sometimes used to help breathlessness, particularly if heart failure and angina occur together. Although the treatment is effective, headaches can be a limiting side effect (see the section Treatment in Chapter 3).
I have been prescribed warfarin. I thought this was rat poison! Why am I taking it?
Warfarin is a blood-thinning medicine and is used to prevent clot formation if your heartbeat is irregular (atrial fibrillation: see Chapter 6) or if the echocardiogram shows something that might mean you may develop clots. It may kill rats but for you it helps prevent a stroke. Warfarin reacts with many medicines and alcohol, so make sure you get a list of these drugs from your doctor. Regular sensible alcohol intake should not be harmful as the reaction between warfarin and alcohol will be constant, but drinking in bouts, or heavily, is dangerous as it may not only disturb the warfarin control but further damage the heart. Heart failure caused by alcohol means that you will have to stop drinking alcohol completely – the heart may improve as a result.
The effects of warfarin need to be monitored with regular blood tests. The INR(International Normalised Ratio) is a test for measuring the thinness of blood – normal is 1. On warfarin, the INR should be between 2.0 and 3.0. In some people the INR varies a lot for no obvious reason and blood tests have to be frequent for accurate monitoring. When the blood is stable, the test may be monthly or less frequent.
Machines are available to allow you to test and monitor yourself at home.
Should I be taking aspirin? I have heard a lot about it in the media recently.
Aspirin may be used instead of warfarin, particularly in milder
cases of heart failure or when the heart rhythm is regular (normal sinus rhythm, not atrial fibrillation). The dose is 75 mg daily. Aspirin can upset the stomach so you may prefer to take the soluble form in a glass of water or with food. Coated aspirin (such as Nu-seals) is available and may help protect the stomach if regular soluble aspirin upsets you. Clopidogrel 75 mg daily is an alternative.
Can I take other medicines while I am on any of these heart failure tablets?
Other medicines may be used for specific problems. Ask your doctor or chemist if there is any chance of a reaction. Do not take arthritis pills without first discussing them with your doctor, as they can interact with heart failure medication. Some antacids contain salt so ask the chemist about the choices available.
Should I be taking beta-blockers?
In the past, the response would have been a firm no. Now research has shown that, once the failure has been controlled, beta-blockers may improve both symptoms and length of survival. Dosage is very low to start with, and under hospital supervision. When starting beta-blockers, you may not feel as good at first but, after a week or two, you should gradually feel better.
I have heart failure – can you tell me which drugs I should be taking and why?
Yes. The list below should help (see also the box Drugs for Heart Failure on p. 181). Your doctor may prescribe one of these or a combination.
•Diuretics (water pills) These reduce fluid and relieve breathlessness and ankle swelling.
•ACE inhibitors Used to improve the heart’s pumping efficacy and improve life expectancy.
•Warfarin Used in atrial fibrillation and some other irregular heartbeats to reduce clots.
•Digoxin Used to help control atrial fibrillation and, in some severe cases in normal sinus rhythm, to improve symptoms.
•Beta-blockers Used to improve symptoms and length of survival.
•AII antagonists Used in cases where ACE inhibitors cause a cough, and in combination.
•Statins Used to reduce cholesterol when coronary disease is also present.
I recently read about spironolactone. Will this be given to me?
Spironolactone is an old diuretic (water pill). In a study of more severe cases, when it was added to diuretics, such as furosemide and ACE inhibitors, further improvement was noted. A problem arose in that the ACE inhibitors were used in lower doses than usually recommended, so we are unclear as to the exact benefit. If ACE inhibitors cannot be used or increased in dose because of side effects, spironolactone should certainly be considered.
My doctor placed me on eplerenone because I developed heart failure after a heart attack. How does it work?
It works like spironolactone, antagonising a hormone call aldosterone which becomes elevated in heart failure causing fluid retention. It helps prevent potassium loss, so like spironolactone needs to be carefully monitored with blood tests if used with ACE inhibitors or AII antagonists. It has been shown to improve length of survival when started 3–14 days after a heart attack when there is evidence of heart failure. Spironolactone can cause swollen breasts in men which may be tender and eplerenone avoids this.
Can I help monitor my heart failure at home?
The easiest way is to weigh yourself at the same time of day with no clothes on. The best time is first thing before breakfast. If you gain 1 kg, that is, 1 litre of fluid (2 pints), this points to the need to increase your diuretics. If you gain weight 2 days on the run, ask your doctor for advice. If you have been given a weight plan already, follow the instructions regarding extra diuretics (water pills). Your weight should return to the baseline – if it does not, visit your doctor.
Surgery
I have been diagnosed as having heart failure. Will I be able to have a heart transplant?
If your heart muscle is very weak and your activity remains very limited in spite of optimal medical treatment, transplantation is the best option available to give you a better quality and length of life. You must be aged less than 60 years and you will need to be mentally strong and have support and help available. Some people will not be suitable because of other serious illnesses or problems.
What does a heart transplant involve?
If you have been placed on a waiting list, you must be available within 2–3 hours of being called because the donor heart can only be transplanted within 6 hours of the death of the donor. You will usually be given a beeper or mobile phone. The donor heart should be of the same blood group and match yours, as well as matching your immune system. The race and sex of the donor and recipient do not matter but the size of the heart should be similar to yours, although it does not need to be exactly the same.
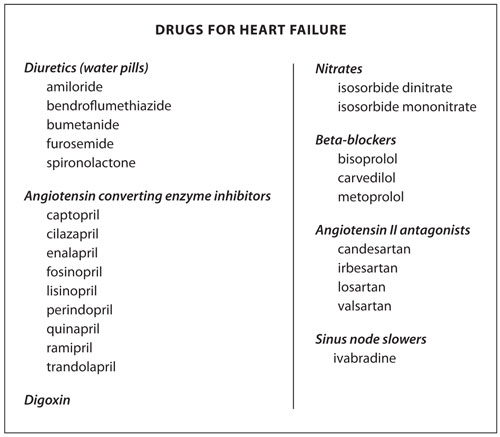
The operation is performed on the bypass machine. The diseased heart is removed by separating it from all the vessels connected to it but the back walls of the right and left atria are left in place. The new heart is then stitched onto the vessels and the atria, and the bypass is discontinued to allow the new heart to take over (see Figure 5.2).
After the transplant, which is a straightforward procedure, you will stay in hospital for 2–3 weeks whilst drugs are used to suppress rejection of the new heart. Biopsies via a small catheter are taken from the heart to look for signs of rejection. This is a simple, painless procedure performed under a local anaesthetic and uses a vein in the neck. You will remain on drugs always to keep rejection at bay, and you need to watch your lifestyle carefully: hardening of the arteries in the new heart is a particular problem and is checked for at regular intervals by your transplant doctor. A transplant that is successful will transform your life. After 1 year, 8 out of 10 patients will still be alive, and 6 out of 10 will live beyond 5 years.
Figure 5.2 Heart transplant operation. (a) Heart being removed, with cuts at A, B and C; (b) no heart in place; (c) new heart stitched on.
I’ve heard about an operation to reduce the size of the heart by cutting out a piece of heart muscle. It is claimed to help heart failure. Should I consider this before a transplant?
This is a debated operation. In many of the cases, a new mitral valve is also put in, so that it is difficult to sort out which part of the operation has been successful. It must remain a part of a careful evaluation programme before it is widely used. We need to know the risk of death at the time of the operation and if the operation works – for how long and what evidence there is for improved quality of life. It is still in its early phase of evaluation when caution should replace over-enthusiasm.
My doctor has mentioned cardiomyoplasty but was not very enthusiastic about it. What is this operation?
This was an idea for surgery for the failing heart. A large muscle taken from a patient’s back was loosened and then wrapped around the heart. A pacemaker was used to stimulate the muscle to squeeze the heart and give it more power. Initial enthusiasm has been replaced with disappointment as any benefit did not last long.
Is an artificial heart another option for me?
It may be a short-term help, if the heart is severely inflamed by a virus, when it might buy time for recovery. It might also buy time for a transplant donor to be found. At present, it does not offer a long-term solution, but it acts as a bridge to definitive therapy.
Can pacemakers be used to treat heart failure?
Pacemakers are usually used if there is an electrical fault with the heart (see the section How your heart works in Chapter 1). However, a special pacing technique has been developed for heart failure, which can be used even if the electrical connections are intact. It is used in more severe cases but is not suitable for everyone. Results have been very encouraging and it is certainly a treatment to consider. It is called resynchronisation therapy.
My cardiologist has advised a defibrillator as well as a pacemaker. Why both?
It is one combined unit. The pacemaker improves the heart’s efficiency and the defibrillator stops dangerous, life-threatening changes in heart rhythm by giving the heart a shock. It is recommended when heart failure is more severe or when dangerous rhythms have already occurred. It is inserted by cardiologists who specialise in electrical events affecting the heart, and regular follow-up checks are needed.