CHAPTER 53
Electrical Safety
Introduction
Electricity is used in the operating room (OR) to power many pieces of equipment, ranging from items associated with direct patient care to lighting, computers, and electronic devices that support patient care. Electrical power is essential for the performance of contemporary anesthesia and surgery, as well as nearly all functions throughout the hospital, yet remains mysterious and poorly understood by many users. Despite an excellent safety record, electricity is hazardous and poses a variety of risks. In order for electrical equipment to be used safely, it is necessary to understand the ways in which electricity can cause harm. This chapter reviews the risks associated with the use of electricity in the OR and methods for ensuring safety.
Harm related to the use of electricity can occur in four distinct ways (Fig. 53.1). Electrical currents flowing through the body can cause an electrical shock or result in skin or other tissues being burned. Electricity can also ignite fires (fire safety is covered in Chapter 61, Fire). The loss of electrical power can imperil patients if life-support equipment fails to function. Finally, electricity can interfere with the function of implanted devices such as pacemakers or defibrillators.
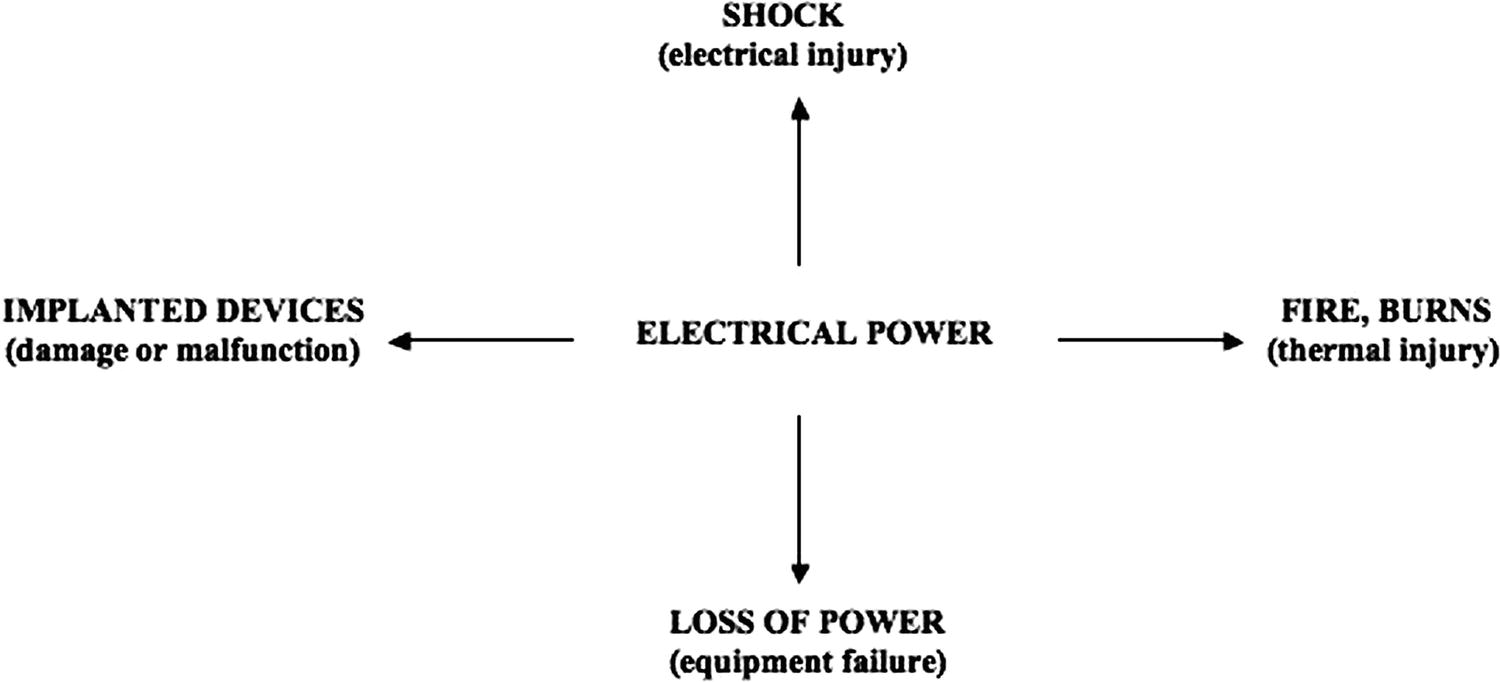
FIGURE 53.1. A framework for understanding the potentially harmful effects related to the use of electrical power in the operating room.
While patient safety is a primary concern when considering electrical hazards, OR staff are also at risk. As users of electrical equipment, anesthesiologists, surgeons, and other personnel can experience an electrical shock. For example, many surgeons have received an unpleasant jolt while using an electrosurgical device. Considerations for protection from shock apply equally well to the OR staff.
Electrical Shock
A shock is experienced when electric current passes through the body. The amount of current that flows will be a function of the voltage difference across the body and the resistance to current flow presented by the body. There must be a complete circuit for current to flow. In other words, there must be a continuous, unbroken path for current to flow from its point of origin through a circuit and back to its point of origin. The primary objective in electrical safety is to prevent patients or staff from becoming a part of that complete circuit.
Two points of contact must exist for current to flow through the body. Oftentimes, one of these contacts is established as a result of being grounded (e.g., by standing on the ground), so only one other point of contact needs to be made in order for current to flow and a shock to occur. For the purposes of this chapter, anything that is grounded, whether intentionally (e.g., an equipment case or the OR bed) or unintentionally (e.g., a patient or staff person in contact with a source of electrical power) will provide a pathway for current to return to its origin. Ideally, patients (and other individuals) should never be grounded, thus removing any possibility of becoming part of the electrical circuit. However, this is difficult and impractical to accomplish, so instead the OR power supply itself is kept isolated from ground (see below for a discussion of isolated power). Conversely, electrical equipment should always be grounded, to provide a low-resistance pathway for current to return to its source, rather than through some alternate pathway, such as a human being. For example, if a piece of equipment was not grounded, but it had a fault such that electrical power was in contact with the case, an individual coming into contact with that case would then serve as the sole pathway for the fault current to flow back to the source. By keeping the equipment grounded, the bulk of the fault current will be conducted by the equipment’s ground connection and only a small portion will flow through the person, thus significantly reducing the risk of shock.
Below roughly 1 milliamperes (mA), current is not perceptible. At current levels between roughly 1 and 10 mA, current may be perceived as a tingling, warm sensation. Currents in the range of 10-20 mA produce muscle spasm, and the individual cannot let go of the conductor. This is known as the “can’t let go” current. As current reaches 100 mA in magnitude, ventricular fibrillation (VF) and death occur.
Injuries that result from electric shock include burns and tissue damage, VF, and death. The injury that occurs will depend on the magnitude and duration of current flow through the body, as well as the cross-sectional area through which it flows. This is embodied in the concept known as current density, which is defined as the amount of current flowing through a given cross-sectional area, and can be thought of as a measure of how “concentrated” the current is. Macroshock refers to currents on the order of 1 mA or larger that are applied externally to the skin and are perceptible. There is a second phenomenon known as microshock that involves currents below the threshold of perception.
Microshock occurs in the electrically susceptible patient, that is, a patient with a direct conductive connection to the heart that bypasses the skin (e.g., a temporary pacemaker wire or a saline-filled catheter). This is important as the skin is normally a source of considerable resistance. Not only does the direct connection provide a low-resistance pathway to current flow, the connection contacts the heart in a very small area. As a result, despite the low current levels flowing (as low as 10-100 microamperes [μA]), the resulting current density is sufficient to cause VF. Because the current levels associated with microshock are below the threshold of perception, normal methods to detect hazardous situations and prevent shock don’t work. For example, line isolation monitors (LIMs) (see below) do not help to protect against microshock.
Many ORs utilize isolated power supplies, power sources that are isolated from ground (Fig. 53.2). These differ from the type of power supplies used in the home and other hospital locations in several important ways. A grounded power supply will have one hot lead and one neutral lead, which is physically connected to the ground conductor. If a person (who is typically going to be in contact with ground) should come into contact with the electric circuit, there is a potential for some current to flow from the point of contact through the individual to ground and thus back to its source. However, because electrical equipment is grounded, most of the current should flow along established grounding pathways and only a small fraction through the person.

FIGURE 53.2. Schematic of the power supply. The power grid supplies grounded power, with the neutral lead physically connected to the ground conductor. In the OR, after passing through an isolation transformer, line 1 and line 2 supply electrical power, but there is no connection with ground. Consequently, contact with either line 1 or line 2 cannot result in current return via the ground conductor.
In contrast, isolated power supplies provide electrical power through two leads, line 1 and line 2, neither of which is connected to ground. The two lines are electrically isolated from ground by having power supplied by an isolation transformer located in the OR. Electrical equipment is still grounded through a third conductor; however, there is no pathway for current to flow from either line 1 or line 2 back to its source via the ground. As a result, if a person in contact with ground comes into contact with either line 1 or line 2, there is no pathway for establishing a complete circuit, and no shock can result. Only when an individual comes into contact with both lines 1 and 2 does a complete circuit result that allows current to flow and a shock to occur. The use of isolated power supplies thus provides an added layer of protection against electrical shock.
Isolation is not perfect, however, and leakage currents do exist. The leakage can become significant enough to defeat the isolation, in which case the power supply then functions as a grounded supply. This will not affect equipment function, nor does it cause a shock, but it does remove that extra layer of protection. Since equipment continues to function, such a change will go unnoticed. An LIM is used to monitor the quality of the isolation from ground and will alarm if the impedance to ground drops low enough that significant current (5 mA) could flow (Figs. 53.3 and 53.4).

FIGURE 53.3. An older-style line isolation monitor. (Courtesy of Bender, Inc.)
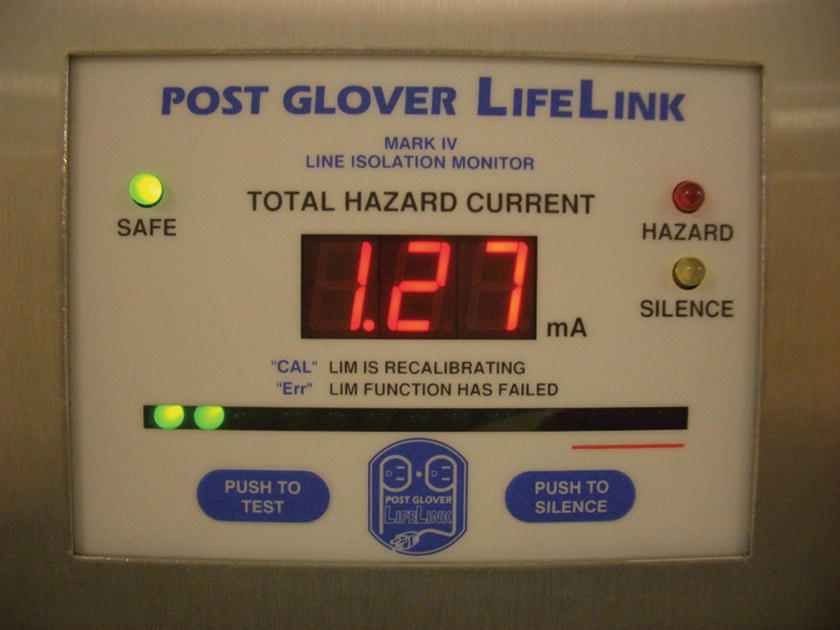
FIGURE 53.4. A more contemporary line isolation monitor. (Courtesy of PG LifeLink.)
There are two ways in which isolation could fail. The first occurs when a piece of equipment has a “ground fault,” that is, when there is an unintended connection between either line 1 or line 2 and ground. The second way in which a system could lose isolation is if enough pieces of equipment, each with about 100 μA of leakage, are plugged into the supply. This would lower the impedance to the point of converting the isolated system to a grounded supply. As previously noted, in both situations, equipment will continue to function normally, hence the need for the LIM. If an LIM should alarm, the cause needs to be determined. Is it a faulty piece of equipment, or just too many pieces of equipment? The recommended practice is to unplug equipment, one piece at a time, starting with the last piece plugged in, until the alarm stops. A faulty piece of equipment is likely to be associated with a larger change in the hazard current displayed by the LIM than just having too many items plugged in. If the cause for the alarm is still unclear, equipment can be taken to another room and plugged in; if faulty, it should alarm there, too. A faulty piece of equipment should be removed from service.
A significant advantage of the LIM is that equipment will continue to function, and critical life support functions will not be interrupted. An alternative piece of equipment that also protects against shock and ground faults is known as a ground fault circuit interrupter (GFCI), routinely used in wet environments in commercial and residential construction. The GFCI differs in one important way from the LIM. Rather than an alarm that notifies the user that isolation has been defeated, it simply stops the flow of current. Any electrical equipment connected to a circuit utilizing a GFCI will cease to function. This is an obvious disadvantage in situations where life-support equipment is being used. For that reason, these devices are not used in the OR.
Loss of Electrical Power
A loss of electrical power is a potentially catastrophic situation that requires prompt and effective management to minimize the risk to patients. It is a very different problem than electrical shock. Whereas shock will generally affect only a single patient, the loss of electrical power can affect many patients. Electric shock has an immediate effect, such as VF, but the consequences of a power outage may extend over a long period of time. In the event of an outage, there is usually some form of backup electrical supply that allows critical equipment to continue functioning. This can take the form of a battery, such as in the anesthesia machine, or hospital generators. However, this does not ensure that equipment will continue to operate, since batteries have a limited duration and generators may fail.
The cause of an electrical power failure can be external to the institution and affect an entire facility, due to an interruption of the power company’s supply, or arise from internal failures that may affect only a portion of the facility. Patients whose lives depend on critical life-support equipment are at risk from equipment that stops functioning. Power outages can also interrupt and interfere with surgery or other invasive procedures.
Should there be a loss of power, several issues must be considered. First, patient status must be ascertained. Second, the status of the anesthetic and the surgery must be determined. If the surgical procedure must continue, how will the anesthetic be provided? For example, it is possible to use portable battery-powered monitors, intravenous infusion pumps to provide a total intravenous anesthetic, oxygen from tanks, and ventilation via a manually operated bag. Anesthesia technicians need to be prepared to make these items available, often rapidly to multiple ORs. Light can be provided from flashlights, laryngoscopes, and cell phones, although ORs may also have emergency lighting. All OR personnel should be familiar with the location of emergency light sources. Third, equipment function needs to be evaluated. The status of the anesthetic machine, monitors, light sources, and any powered surgical equipment must be clarified, so decisions about whether or not to continue surgery can be made. If it appears that the power outage will be of significant duration, steps should be taken to conclude the surgical procedure. Finally, and perhaps most importantly, the scope and duration of the outage must be determined. Is it confined to a single OR, to a number of ORs, or to some larger entity, such as one or more floors, the hospital or facility, or an entire community? The scope and expected duration of the interruption in power will significantly influence decision-making about what services can continue to be provided. For example, in August 2003, the northeastern United States experienced a massive failure of the electrical grid, resulting in loss of electrical power to a multistate region that lasted several days. As the event progressed, hospitals experienced problems with their backup generators, some of which were old or poorly maintained and, in some cases, ran out of (or came perilously close to running out of) fuel. As a result, what services were provided and what equipment could be used were limited. In addition, it is important to realize that having backup power is no guarantee of continued operations. There have been several instances where backup generators have failed, resulting in the OR, or institution, being completely without power.
Because a loss of power may occur, it is necessary to know which items of equipment have internal battery backup. It is important to keep batteries fully charged and to know how long the backup batteries will last; what functions will continue on backup power; how to provide light, computer, phone, and paging services; and how to provide alternatives to primary equipment and functions (e.g., portable monitors in place of normal physiologic monitors, or intravenous anesthesia via infusion pumps in place of inhaled anesthetics delivered by the anesthesia machine). Anesthesia technicians have a critical role in providing the equipment for many of these functions. Practicing what to do in the event of a power failure is an excellent simulation exercise (see Chapter 56, Simulation and Crisis Resource Management). In addition, it is important to understand how electrical power is provided to the OR, that is, which sockets are intended to function only under normal conditions (usually white sockets), and which will provide emergency power in the event of a power failure (usually red sockets). Essential equipment, such as anesthesia machines, should always be plugged into emergency (red) sockets.
Burns and Fire
The amount of heat produced by current flow depends on the magnitude of the current and the resistance through which it flows. A given current flowing through a small area will produce more heating than the same current flowing through a large area. The situation most commonly associated with burns in the OR is related to the use of an electrosurgical device (“the Bovie”). Electric current passes from a handheld electrode (sometimes known as the “pencil”) through the patient to a dispersive pad (often incorrectly called “the grounding pad”). Because the pencil tip is small, a high current density exists and significant heating occurs. However, the dispersive pad occupies a much larger surface area, resulting in much lower current density, effectively protecting against skin burns. However, if the conductive gel is dried out, the pad is incorrectly applied so it does not make good contact with the skin throughout its entire surface, or it is removed and reapplied, current can be concentrated at the point(s) of contact, resulting in skin burns. Ideally, the pad will be applied over well-muscled areas, such as the thigh, arm, or buttocks. It should not be placed over hairy areas (it won’t stick well) or over bony prominences or metal prostheses (the current can be concentrated at these points), and it should not be reapplied if it is removed (insufficient gel may remain). Otherwise, current may seek other pathways, such as through electrocardiographic electrodes, again resulting in a high enough current density to cause burns.
Under certain conditions, fires can be ignited as a result of using electricity in the OR. As is true of any fire, three elements must coexist to have a fire: something to ignite the fire, a fuel, and an oxidizing agent (see Chapter 61, Fire). A common way for fires to ignite is by use of electrosurgical devices in the presence of an oxygen-enriched atmosphere. A typical scenario is the ignition of surgical drapes by the electrosurgical handheld electrode in a patient who is not intubated, but instead receiving supplemental oxygen via nasal cannula or a face mask. In such a situation, oxygen can accumulate under the drapes, and when the handheld electrode comes in contact with the drapes and is energized, fire can occur. Another common scenario is the patient undergoing a tracheostomy, and the handheld electrode is used to enter the airway, in the presence of elevated oxygen concentrations. In this circumstance, an airway fire is the result, with the endotracheal tube as the fuel. Fuller discussion of fire prevention and management can be found in Chapter 61.
Implanted Devices
The final category considered in this chapter has to do with patients who have implanted electronic devices, such as pacemakers, implantable cardioverter-defibrillators (ICDs), cochlear implants, and spinal cord or other stimulators. The risk is that these devices may be damaged or malfunction as a result of exposure to electrical currents, usually from an electrosurgical device, and may result in harm or death.
Of all the implantable devices, the malfunction of pacemakers and ICDs due to electromagnetic interference from electrosurgical devices poses the greatest risk to patients. (See Chapter 46, Pacemakers and Implantable Defibrillators.) A healthy heart is an electrical organ (see Chapter 4, Cardiovascular Anatomy and Physiology), and a pacemaker is a critical electrical appliance. Any patient with an electrical problem in the heart, who depends on an external electrical appliance for basic life functions, is exquisitely vulnerable to electrical injury in the OR. For this reason, many anesthesiologists are knowledgeable about pacemaker function. The typical reason for malfunction is that electrical currents from the electrosurgical unit pass in proximity to the implanted device or the leads emanating from it, resulting in a change to the device’s mode of operation (reprogramming), accidental firing of an ICD or stimulator, or damage to the device, causing it to stop functioning. Simple steps can usually prevent this from being a problem. The dispersive pad should be placed so the current does not cross the device, but instead travels away from it. For example, if a patient has a pacemaker on the left side of the chest, and surgery is being conducted on the right shoulder, the dispersive pad should not be placed on the left shoulder, or anywhere on the left side. Bipolar electrosurgical devices can be considered as an alternative to the usual monopolar device, as this will confine the current between the tips of the bipolar device. ICDs should be programmed OFF for the duration of surgery. Depending on the patient and the pacemaker, magnets or reprogramming can be used to convert pacemakers to an asynchronous mode of function.
The Role of the Anesthesia Technician
In general, in situations involving electrical safety issues, the anesthesia technician is an important resource for providing support to the anesthesia provider and operative team. The AT ensures that equipment is kept in good working condition to minimize the possibility that it will malfunction and pose a shock hazard. For example, electrical power cords where the external insulation has been damaged so that the inner wiring is exposed should be replaced or repaired. It is important to be familiar with the function of the LIM and the response should it alarm. In the event of a power failure, the technician will need to provide the backup equipment needed to support patient care, as well as help with tasks during this busy time. In addition, by ensuring that equipment is routinely plugged into the proper sources of electrical power (essential equipment into emergency sockets, nonessential equipment into white sockets), operations will be better able to continue if a power failure occurs. Finally, as with many other situations, recognizing potentially unsafe situations and identifying them to the appropriate individual (e.g., improper application or use of the dispersive pad for electrosurgical devices) can be an important step in preventing patient harm.
Review Questions
1. An LIM will protect against microshock.
A) True
B) False
Answer: B
As the term implies, microshock is caused by very low levels of current, which are nonetheless dangerous because they come into direct contact with the heart (e.g., via a pacemaker lead). An LIM is designed to detect current leakage associated with isolated power supplies, at much higher current levels than are seen with microshock. The detection of a leakage current by an LIM indicates either faulty grounding or a large-magnitude current leakage, but does not protect you from a microshock.
2. The proper response to an LIM alarm is to
A) Shut off power to the OR
B) Silence the alarm and address the problem with engineering at the end of the day
C) Notify the power company that there is a grounding problem
D) Unplug equipment one piece at a time, starting with the last item plugged in
E) None of the above
Answer: D
The LIM alarms when it has detected a current leakage in an isolated power supply above its alarm threshold. The most common reason is one or more devices connected to the power supply have a ground fault. To determine which device has the fault, disconnect each device from the power supply, one at a time, until the alarm stops.
3. Microshock occurs
A) In the electrically susceptible patient
B) In small amounts over time
C) In the use of microscopes
D) In microbiology
E) When a transformer has failed
Answer: A
Very small amounts of current below the threshold of perception are generally not harmful to patients; however, when a patient has a direct conductive connection to the heart (e.g., saline-filled vascular catheter or a pacing wire), the current may be sufficient to induce an arrhythmia. When this happens, the patient has received a microshock.
4. The dispersive pad for an electrosurgery device
A) Should be placed over the hairiest possible part of the body
B) Should be placed over a patient’s total hip replacement
C) Should be placed over a well-muscled area such as the thigh
D) Should be placed over a bony prominence
E) Is not necessary most of the time
Answer: C
The dispersive pad is an important piece of equipment to allow return of electrical currents from an electrosurgery unit. Good contact of the dispersive pad and a large surface area lower the current density and impedance to return of the current. Poor contact with the skin (e.g., dry gel, hairy body, incomplete contact from poor or repeated application) can all increase the impedance and reduce the area through which the current returns, thus increasing the current density. Patients may suffer burns if the current density is high enough. Bony prominences or metal objects in the patient can also concentrate the current, causing heating or burning.
5. Because of concerns about a loss of power, essential equipment in the OR should be plugged into
A) White sockets
B) Red sockets
C) Either socket, because it doesn’t matter
D) Neither, it should be run off battery power
E) Surge protectors
Answer: B
Red sockets are designed to have backup power in case of a loss of power. All essential equipments should be plugged into a red socket. White sockets are not designed to have backup power. Surge protectors protect the equipment from fluctuations in the power supply but do not have a backup power supply.
6. An LIM stops the flow of electricity when a fault is detected.
A) True
B) False
Answer: B
A GFCI stops the flow of electricity when a fault is detected. The advantage of an LIM is that it will sound an alarm when a fault has been detected but will not stop the flow of electricity to critical equipment.
7. An electrical shock occurs when
A) Electrical shock does not occur in the OR environment.
B) Equipment is not kept in good working condition.
C) Electric current flows through the body.
D) A piece of equipment has a ground fault.
Answer: C
Although a piece of equipment that has been poorly maintained or that has a ground fault surely increases the risk for electrical shock, electrical shock only occurs when current flows through the body.
8. Grounded equipment cannot cause electrical shock.
A) True
B) False
Answer: B
Grounded equipment reduces the risk of receiving an electrical shock should there be a short in the equipment. In grounded equipment, the bulk of the fault current will be conducted through the ground line and only a small portion will flow through the person.
SUGGESTED READINGS
Barker SJ, Doyle JD. Electrical safety in the operating room: dry versus wet. Anesth Analg. 2010;110:1517-1518.
Carpenter T, Robinson ST. Response to a partial power failure in the operating room. Anesth Analg. 2010;110:1644-1646.
Dillon JD, Botney R, Dull RO. Remember that the line isolation monitor is based on a simple principle of electrical safety: make sure the patient does not become part of a grounded circuit. In: Marcucci C, Cohen NA, Metro DG, et al, eds. Avoiding Common Anesthesia Errors. Philadelphia, PA: Lippincott Williams & Wilkins; 2008:419-422.
Eichhorn JH, Hessel EA. Electrical power failure in the operating room: a neglected topic in anesthesia safety. Anesth Analg. 2010;110:1519-1521.
Fung DL. Electrical hazards. In: Sosis MB, ed. Anesthesia Equipment Manual. Philadelphia, PA: Lippincott Williams & Wilkins; 1997:313-323.
Smith TL, Smith JM. Electrosurgery in otolaryngology-head and neck surgery: principles, advances, and complications. Laryngoscope. 2001;111:769-780.
Venkatraghavan L, Chinnapa V, Peng P, Brull R. Non-cardiac implantable electrical devices: a brief review and implications for anesthesiologists. Can J Anesth. 2009;56:320-326.