Pediatric Emergencies and Resuscitation
Mary E. Hartman, Ira M. Cheifetz
Injuries are the leading cause of death in American children and young adults and account for more childhood deaths than all other causes combined (see Chapter 13 ). Rapid, effective bystander cardiopulmonary resuscitation (CPR) for children is associated with survival rates as high as 70%, with good neurologic outcome. However, bystander CPR is still provided for <50% of children who experience cardiac arrest outside medical settings. This failing has led to long-term survival rates of <40%, often with a poor neurologic outcome.
Approach to the Emergency Evaluation of a Child
The first response to a pediatric emergency of any cause is a systematic, rapid general assessment of the scene and the child to identify immediate threats to the child, care providers, or others. If an emergency is identified, the emergency response system (emergency medical services, EMS) should be activated immediately. Care providers should then proceed through primary , secondary , and tertiary assessments as allowed by the child's condition, safety of the scene, and resources available. This standardized approach provides organization to what might otherwise be a confusing or chaotic situation and reinforces an organized thought process for care providers. If at any point in these assessments the caregiver identifies a life-threatening problem, the assessment is halted and lifesaving interventions are initiated. Further assessment and intervention should be delayed until other caregivers arrive or the condition is successfully treated or stabilized.
General Assessment
On arrival at the scene of a compromised child, a caregiver's first task is a quick survey of the scene itself. Is the rescuer or child in imminent danger because of circumstances at the scene (e.g., fire, high-voltage electricity)? If so, can the child be safely extricated to a safe location for assessment and treatment? Can the child be safely moved with the appropriate precautions (i.e., cervical spine protection), if indicated? A rescuer is expected to proceed only if these important safety conditions have been met.
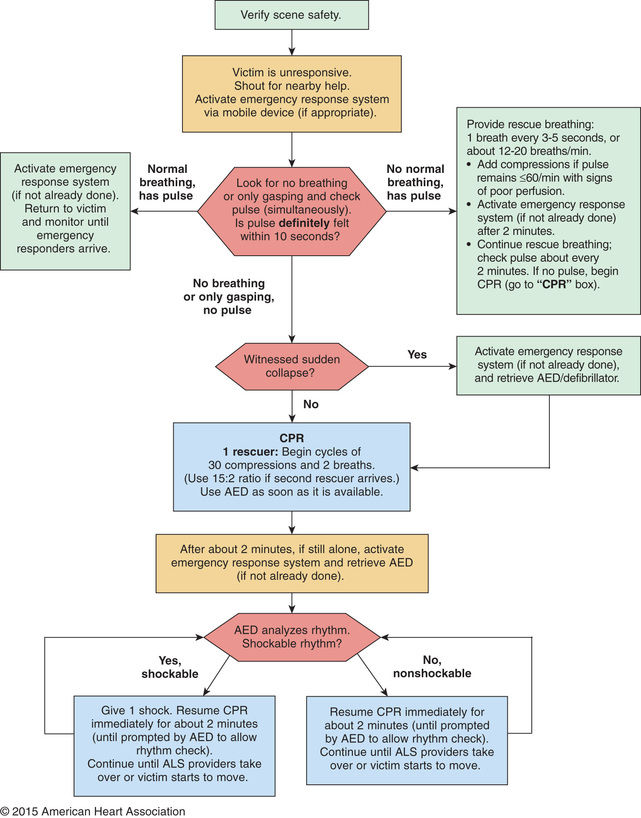
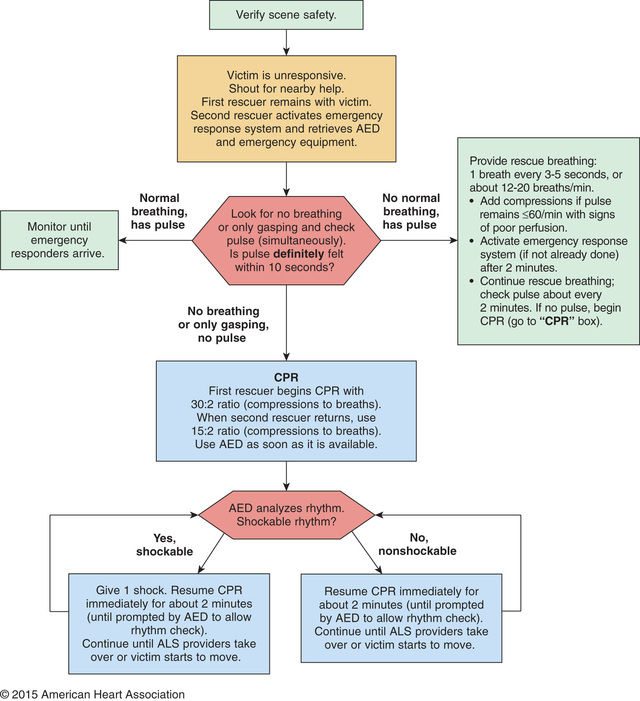
Once the caregiver and patient's safety has been ensured, the caregiver performs a rapid visual survey of the child, assessing the child's general appearance and cardiopulmonary function . This action should be only a few seconds and include assessment of (1) general appearance, determining color, tone, alertness, and responsiveness; (2) adequacy of breathing, distinguishing between normal, comfortable respirations and respiratory distress or apnea; and (3) adequacy of circulation, identifying cyanosis, pallor, or mottling. A child found unresponsive from an unwitnessed collapse should be approached with a gentle touch and the verbal question, “Are you OK?” If there is no response, the caregiver should immediately shout for help and send someone to activate the emergency response system and locate an automated external defibrillator (AED) . Figs. 81.1 and 81.2 present basic life support (BLS) pediatric cardiac arrest algorithms for 1 rescuer and 2 or more rescuers, respectively. The provider should then determine whether the child is breathing and, if not, provide 2 rescue breaths. If the child is breathing adequately, the circulation is quickly assessed. Any child with heart rate <60 beats/min or without a pulse requires immediate CPR. If the caregiver witnesses the sudden collapse of a child, the caregiver should have a higher suspicion for a sudden cardiac event. In this case, rapid deployment of an AED is crucial. Any interruptions in care of the child to activate EMS and locate the nearest AED should be very brief. If >1 caregiver is present, someone should always remain with the child and provide initial care or stabilization (see Fig. 81.2 ).
Primary Assessment
Once the emergency response system has been activated and the child is determined not to need CPR, the caregiver should proceed with a primary assessment that includes a brief, hands-on assessment of cardiopulmonary and neurologic function and stability. This assessment includes a limited physical examination, evaluation of vital signs, and measurement of pulse oximetry if available. The American Heart Association, in its Pediatric Advanced Life Support (PALS) curriculum, supports the structured format of airway, breathing, circulation, disability, exposure (ABCDE) . The goal of the primary assessment is to obtain a focused, systems-based assessment of the child's injuries or abnormalities, so that resuscitative efforts can be directed to these areas; if the caregiver identifies a life-threatening abnormality, further evaluation is postponed until appropriate corrective action has been taken.
The exam and vital sign data can be interpreted only if the caregiver has a thorough understanding of normal values. In pediatrics, normal respiratory rate, heart rate, and blood pressure have age-specific norms (Table 81.1 ). These ranges can be difficult to remember, especially if used infrequently. However, several standard principals apply: (1) a child's respiratory rate should not be >60 breaths/min for a sustained period; (2) normal heart rate is 2-3 times normal respiratory rate for age; and (3) a simple guide for pediatric blood pressure is that the lower limit of systolic blood pressure should be ≥60 mm Hg for neonates; ≥70 mm Hg for 1 mo-1 yr olds; ≥70 mm Hg + (2 × age) for 1-10 yr olds; and ≥90 mm Hg for any child older than 10 yr.
Table 81.1
Normal Vital Signs According to Age
| AGE | HEART RATE (beats/min) | BLOOD PRESSURE (mm Hg) | RESPIRATORY RATE (breaths/min) |
|---|---|---|---|
| Premature | 120-170* | 55-75/35-45 † | 40-70 ‡ |
| 0-3 mo | 100-150* | 65-85/45-55 | 35-55 |
| 3-6 mo | 90-120 | 70-90/50-65 | 30-45 |
| 6-12 mo | 80-120 | 80-100/55-65 | 25-40 |
| 1-3 yr | 70-110 | 90-105/55-70 | 20-30 |
| 3-6 yr | 65-110 | 95-110/60-75 | 20-25 |
| 6-12 yr | 60-95 | 100-120/60-75 | 14-22 |
| 12+ yr | 55-85 | 110-135/65-85 | 12-18 |
* In sleep, infant heart rates may drop significantly lower, but if perfusion is maintained, no intervention is required.
† A blood pressure cuff should cover approximately two thirds of the arm; too small a cuff yields spuriously high pressure readings, and too large a cuff yields spuriously low pressure readings. Values are systolic/diastolic.
‡ Many premature infants require mechanical ventilatory support, making their spontaneous respiratory rate less relevant.
Airway and Breathing
The most common precipitating event for cardiac instability in infants and children is respiratory insufficiency . Therefore, rapid assessment of respiratory failure and immediate restoration of adequate ventilation and oxygenation remain the first priority in the resuscitation of a child. Using a systematic approach, the caregiver should first assess whether the child's airway is patent and maintainable. A healthy, patent airway is unobstructed, allowing normal respiration without noise or effort. A maintainable airway is one that is either already patent or can be made patent with a simple maneuver. To assess airway patency, the provider should look for breathing movements in the child's chest and abdomen, listen for breath sounds, and feel the movement of air at the child's mouth and nose. Abnormal breathing sounds (e.g., snoring or stridor), increased work of breathing, and apnea are all findings potentially consistent with airway obstruction. If there is evidence of airway obstruction, maneuvers to relieve the obstruction should be instituted before the caregiver proceeds to evaluate the child's breathing.
Assessment of breathing includes evaluation of the child's respiratory rate, respiratory effort, abnormal sounds, and pulse oximetry. Normal breathing appears comfortable, is quiet, and occurs at an age-appropriate rate. Abnormal respiratory rates include apnea and rates that are either too slow (bradypnea) or too fast (tachypnea). Bradypnea and irregular respiratory patterns require urgent attention because they are often signs of impending respiratory failure and/or apnea. Signs of increased respiratory effort include nasal flaring, grunting, chest or neck muscle retractions, head bobbing, and seesaw respirations. Hemoglobin oxygen desaturation, as measured by pulse oximetry, often accompanies parenchymal lung disease apnea or airway obstruction. However, providers should keep in mind that adequate perfusion is required to produce a reliable oxygen saturation (SO 2 ) measurement. A child with low SO 2 is a child in distress. Central cyanosis is a sign of severe hypoxia and indicates an emergent need for oxygen supplementation and respiratory support.
Circulation
Cardiovascular function is assessed by evaluation of skin color and temperature, heart rate, heart rhythm, pulses, capillary refill time, and blood pressure. In nonhospital settings, much of the important information can be obtained without measuring the blood pressure; lack of blood pressure data should not prevent the provider for determining adequacy of circulation or implementing a lifesaving response. Mottling, pallor, delayed capillary refill, cyanosis, poor pulses, and cool extremities are all signs of diminished perfusion and compromised cardiac output. Tachycardia is the earliest and most reliable sign of shock but is itself fairly nonspecific and should be correlated with other components of the exam, such as weakness, threadiness, and absence of pulses. An age-specific approach to pulse assessment will yield best results.
Disability
In the setting of a pediatric emergency, disability refers to a child's neurologic function in terms of the level of consciousness and cortical function. Standard evaluation of a child's neurologic condition can be done quickly with an assessment of pupillary response to light (if one is available) and use of either of the standard scores used in pediatrics: the Alert, Verbal, Pain, Unresponsive (AVPU) Pediatric Response Scale and the Glasgow Coma Scale (GCS). The causes of decreased level of consciousness in children are numerous and include conditions as diverse as respiratory failure with hypoxia or hypercarbia, hypoglycemia, poisonings or drug overdose, trauma, seizures, infection, and shock. Most often, an ill or injured child has an altered level of consciousness because of respiratory compromise, circulatory compromise, or both. Any child with a depressed level of consciousness should be immediately assessed for abnormalities in cardiorespiratory status.
Alert, Verbal, Pain, Unresponsive Pediatric Response Scale.
The AVPU scoring system is used to determine a child's level of consciousness and cerebral cortex function (Table 81.2 ). Unlike the GCS, the AVPU scale is not developmentally dependent—a child does not have to understand spoken language or follow commands, merely respond to a stimulus. The child is scored according to the amount of stimulus required to obtain a response, from alert (no stimulus, the child is already awake and interactive) to unresponsive (child does not respond to any stimulus).
Table 81.2
A, Alert; V, verbal, P, pain, U, unresponsive.
From Ralston M, Hazinski MF, Zaritsky AL, et al, editors: Pediatric advanced life support course guide and PALS provider manual: provider manual, Dallas, 2007, American Heart Association.
Glasgow Coma Scale.
Although it has not been systematically validated as a prognostic scoring system for infants and young children as it has in adults, GCS is frequently used in the assessment of pediatric patients with an altered level of consciousness. The GCS is the most widely used method of evaluating a child's neurologic function and has 3 components. Individual scores for eye opening, verbal response, and motor response are added together, with a maximum of 15 points (Table 81.3 ). Patients with a GCS score ≤8 require aggressive management, generally including stabilization of the airway and breathing with endotracheal intubation and mechanical ventilation, respectively, and if indicated, placement of an intracranial pressure monitoring device. The Full Outline of Unresponsiveness (FOUR) score is another useful assessment and monitoring tool (see Table 85.1 ).
Table 81.3
| EYE OPENING (TOTAL POSSIBLE POINTS 4) | |||
| Spontaneous | 4 | ||
| To voice | 3 | ||
| To pain | 2 | ||
| None | 1 | ||
| VERBAL RESPONSE (TOTAL POSSIBLE POINTS 5) | |||
| Older Children | Infants and Young Children | ||
| Oriented | 5 | Appropriate words; smiles, fixes, and follows | 5 |
| Confused | 4 | Consolable crying | 4 |
| Inappropriate | 3 | Persistently irritable | 3 |
| Incomprehensible | 2 | Restless, agitated | 2 |
| None | 1 | None | 1 |
| MOTOR RESPONSE (TOTAL POSSIBLE POINTS 6) | |||
| Obeys | 6 | ||
| Localizes pain | 5 | ||
| Withdraws | 4 | ||
| Flexion | 3 | ||
| Extension | 2 | ||
| None | 1 | ||
Adapted from Teasdale G, Jennett B: Assessment of coma and impaired consciousness: a practical scale, Lancet 2:81–84, 1974.
Exposure
Exposure is the final component of the pediatric primary assessment. This component of the exam is reached only after the child's airway, breathing, and circulation have been assessed and determined to be stable or have been stabilized through simple interventions. In this setting, exposure stands for the dual responsibility of the provider to both expose the child to assess for previously unidentified injures and consider prolonged exposure in a cold environment as a possible cause of hypothermia and cardiopulmonary instability. The provider should undress the child (as is feasible and reasonable) to perform a focused physical exam, assessing for burns, bruising, bleeding, joint laxity, and fractures. If possible, the provider should assess the child's temperature. All maneuvers should be performed with careful maintenance of cervical spine precautions.
Secondary Assessment
For healthcare providers in community or outpatient settings, transfer of care of a child to emergency or hospital personnel may occur before a full secondary assessment is possible. However, before the child is removed from the scene and separated from witnesses or family, a brief history should be obtained for medical providers at the accepting facility. The components of a secondary assessment include a focused history and focused physical examination.
The history should be targeted to information that could explain cardiorespiratory or neurologic dysfunction and should take the form of a SAMPLE history : signs/symptoms, allergies, medications, past medical history, timing of last meal, and events leading to this situation. Medical personnel not engaged in resuscitative efforts can be dispatched to elicit history from witnesses or relatives. The physical examination during the secondary assessment is a thorough head-to-toe exam, although the severity of the child's illness or injury could necessitate curtailing portions of the exam or postponing nonessential elements until a later time.
Tertiary Assessment
The tertiary assessment occurs in a hospital setting, where ancillary laboratory and radiographic assessments contribute to a thorough understanding of the child's condition. A basic blood chemistry profile, complete blood count, liver function tests, coagulation studies, and arterial blood gas analyses give fairly broad (but somewhat nonspecific) estimates of renal function, acid-base balance, cardiorespiratory function, and presence or absence of shock. Chest radiographs can be useful to evaluate both the heart and lungs, although more detailed estimates of heart function and cardiac output can be made with echocardiography . Arterial and central venous catheters can be placed to monitor arterial and central venous pressure.
Recognition and Treatment of Respiratory Distress and Failure
The goals of initial management of respiratory distress or failure are to rapidly stabilize the child's airway and breathing and to identify the cause of the problem so that further therapeutic efforts can be appropriately directed.
Airway Obstruction
Children <5 yr old are particularly susceptible to foreign body aspiration and choking. Liquids are the most common cause of choking in infants, whereas small objects and food (e.g., grapes, nuts, hot dogs, candy) are the most common source of foreign bodies in the airways of toddlers and older children. A history consistent with foreign body aspiration is considered diagnostic. Any child in the proper setting with the sudden onset of choking, stridor, or wheezing has foreign body aspiration until proven otherwise.
Airway obstruction is treated with a sequential approach, starting with the head-tilt/chin-lift maneuver to open and support the airway, followed by inspection for a foreign body, and finger-sweep clearance or suctioning if one is visualized (Fig. 81.3 ). Blind suctioning or finger sweeps of the mouth are not recommended. A nasopharyngeal airway or oropharyngeal airway can be inserted for airway support, if indicated. A conscious child suspected of having a partial foreign body obstruction should be permitted to cough spontaneously until coughing is no longer effective, respiratory distress and stridor increase, or the child becomes unconscious.
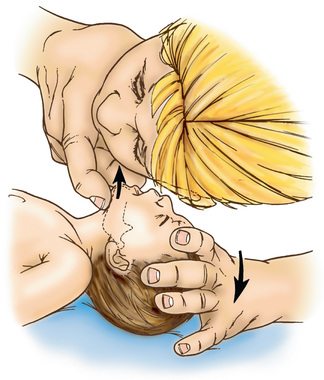
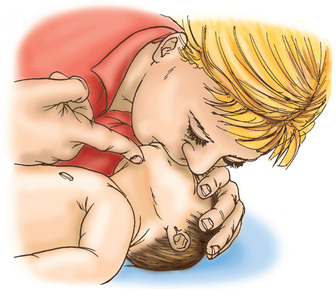
If the child becomes unconscious, the child should be gently placed on the ground, supine. The provider should then open the airway with the head-tilt/chin-lift maneuver and attempt mouth-to-mouth ventilation (Figs. 81.4 and 81.5 ). If ventilation is unsuccessful, the airway is repositioned and ventilation attempted again. If there is still no chest rise, attempts to remove a foreign body are indicated. In an infant <1 yr old, a combination of 5 back blows and 5 chest thrusts is administered (Fig. 81.6 ). After each cycle of back blows and chest thrusts, the child's mouth should be visually inspected for the presence of the foreign body. If identified within finger's reach, it should be removed with a gentle finger sweep. If no foreign body is visual, ventilation is again attempted. If this is unsuccessful, the head is repositioned and ventilation attempted again. If there is still no chest rise, the series of back blows and chest thrusts is repeated.

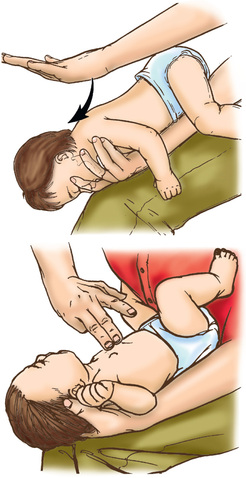
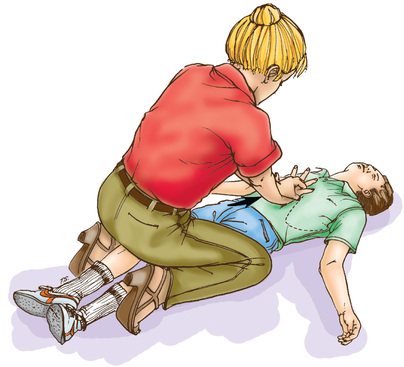
For a conscious child >1 yr old, providers should give a series of 5 abdominal thrusts (Heimlich maneuver ) with the child standing or sitting (Fig. 81.7 ); this should occur with the child lying down if unconscious (Fig. 81.8 ). After the abdominal thrusts, the airway is examined for a foreign body, which should be removed if visualized. If no foreign body is seen, the head is repositioned and ventilation attempted. If unsuccessful, the head is repositioned and ventilation attempted again. If these efforts are unsuccessful, the Heimlich sequence is repeated.

Airway Narrowing
Airway obstruction can also be caused by airway narrowing, in both the upper and lower airways. Upper airway obstruction refers to narrowing of the extrathoracic portion of the airway, including the oropharynx, larynx, and trachea. In the upper airways, narrowing is most often caused by airway edema (e.g., croup or anaphylaxis). Lower airway disease affects all intrathoracic airways, notably the bronchi and bronchioles. In the lower airways, bronchiolitis and acute asthma exacerbations are the major contributors to intrathoracic airway obstruction in children, causing airway narrowing through a combination of airway swelling, mucus production, and circumferential smooth muscle constriction of smaller airways.
Airway support for these processes is dictated by both the underlying condition and the clinical severity of the problem. In cases of mild upper airway obstruction, the child has minimally elevated work of breathing (evidenced by tachypnea and few to mild retractions). Stridor, if present at all, should be audible with only coughing or activity. Children with these findings can be supported with supplemental oxygen as needed. In cases with moderate obstruction, in which the child has a higher work of breathing and more pronounced stridor, nebulized racemic epinephrine and oral or intravenous (IV) dexamethasone can be added. Heliox (combined helium-oxygen therapy) administration may also be considered. Children with severe upper airway obstruction have marked intercostal retractions, prominent stridor, and decreased air entry on auscultation of the lung fields. Most children with significant airway obstruction are also hypoxic, and many appear dyspneic and agitated. A child in severe distress needs to be closely observed because the signs of impending respiratory failure may be initially confused with improvement. Stridor becomes quieter and intercostal retractions less prominent when a child's respiratory effort begins to diminish. The child in respiratory failure can be distinguished from one who is improving by evidence of poor air movement on auscultation and lethargy or decreased level of consciousness from hypercarbia, hypoxia, or both. When anaphylaxis is suspected as the cause for upper airway edema, providers should administer an intramuscular (IM) or IV dose of epinephrine as needed (see Chapter 174 ). No matter the cause, any child in impending respiratory failure should be prepared for endotracheal intubation and respiratory support. Prompt notification of providers trained in airway management is essential.
In cases of lower airway obstruction , therapies are targeted to both relieving the obstruction and reducing the child's work of breathing. Inhaled bronchodilators , such as albuterol, augmented by oral or IV corticosteroids, remain the mainstay of therapy in settings of mild to moderate acute distress caused by lower airway obstruction (e.g., asthma ). Children with more significant obstruction appear dyspneic, with tachypnea, retractions, and easily audible wheezing. In these cases, the addition of an anticholinergic agent, such as nebulized ipratropium bromide, or a smooth muscle relaxant, such as magnesium sulfate, may provide further relief, although the evidence for these measures remains controversial (see Chapter 169 ). Supplemental oxygen and IV fluid hydration can also be useful adjuncts. As in cases of upper airway obstruction, impending respiratory failure in children with lower airway obstruction can be insidious. When diagnosed early in a school-age child who is cooperative, respiratory failure can be averted through judicious use of noninvasive support, including heated, high-flow nasal cannula (HFNC) therapy, continuous positive airway pressure (CPAP), bilevel positive airway pressure (BiPAP), or heliox therapy. Endotracheal intubation should be performed only by skilled providers, preferably in a hospital setting, because there is a high risk of cardiorespiratory compromise in patients with lower airway obstruction during the procedure.
Parenchymal Lung Disease
Parenchymal lung disease includes a heterogeneous list of conditions, such as pneumonia, acute respiratory distress syndrome (ARDS), pneumonitis, bronchiolitis, bronchopulmonary dysplasia, cystic fibrosis, and pulmonary edema. The commonalities of these conditions are their effects on the small airways and alveoli, including inflammation and exudation leading to consolidation of lung tissue, decreased gas exchange, and increased work of breathing. Clinical management of these conditions includes specific treatment as indicated (e.g., antibiotics for bacterial pneumonia) and supportive care in the form of supplemental oxygen, noninvasive respiratory support (with HFNC, CPAP, or BiPAP), or invasive mechanical ventilation.
Advanced Airway Management Techniques
Bag-Valve-Mask Positive Pressure Ventilation
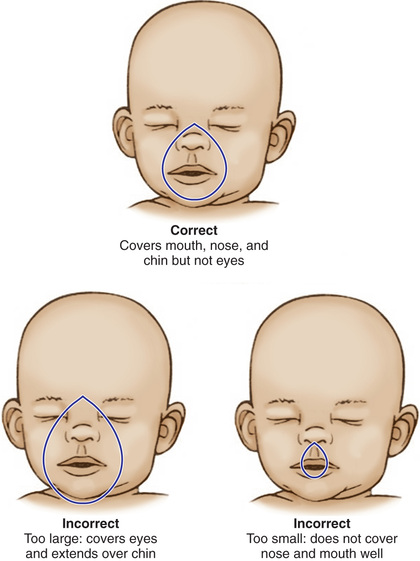
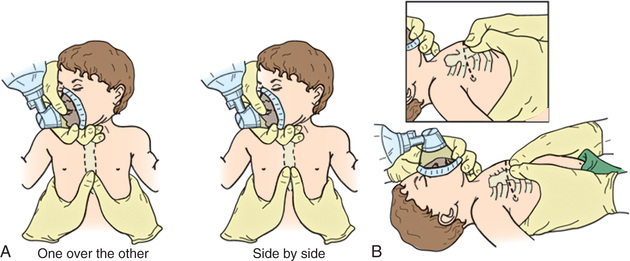
Rescue breathing with a bag-valve-mask apparatus can be as effective as endotracheal intubation and safer when the provider is inexperienced with intubation. Bag-valve-mask ventilation itself requires training to ensure that the provider is competent to select the correct mask size, open the child's airway, form a tight seal between the mask and the child's face, deliver effective ventilation, and assess the effectiveness of the ventilation. An appropriately sized mask is one that fits over the child's mouth and nose but does not extend below the chin or over the eyes (Fig. 81.9 ). An adequate seal is best achieved through a combination “C-E” grip on the mask, in which the thumb and index finger form the letter “C” on top of the mask, pressing the mask downward onto the child's face, and the remaining 3 fingers form an “E” grip under the child's mandible, holding the jaw forward and extending the head up toward the mask. Using this method, the care provider can secure the mask to the child's face with one hand and use the other hand to compress the ventilation bag (Fig. 81.10 ).
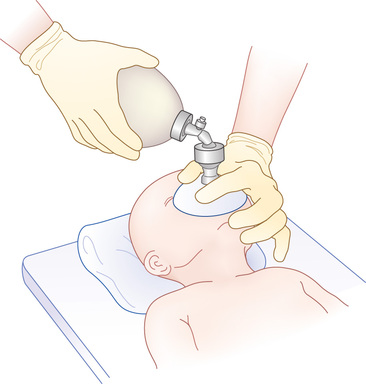
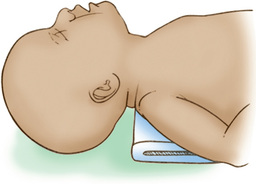
The provider may have to move the head and neck through a range of positions to find the one that best maintains airway patency and allows maximal ventilation. In infants and young children, optimal ventilation is often provided when the child's head is in the neutral sniffing position without hyperextension of the head (Fig. 81.11 ). Poor chest rise and persistently low SO 2 values indicate inadequate ventilation. In this setting the care provider should recheck the mask's seal on the child's face, reposition the child's head, and consider suctioning the airway, if indicated. If these maneuvers do not restore ventilation, the provider should consider noninvasive or invasive respiratory support (i.e., endotracheal intubation) as clinically indicated.
Endotracheal Intubation
A child generally requires intubation when at least one of these conditions exists: (1) the child is unable to maintain airway patency or protect the airway against aspiration (as occurs in settings of neurologic compromise); (2) the child is failing to maintain adequate oxygenation; (3) the child is failing to control blood carbon dioxide levels and maintain safe acid-base balance; (4) sedation and/or paralysis is required for a procedure; and (5) care providers anticipate a deteriorating course that will eventually lead to any of the first 4 conditions. It should be noted that in centers experienced in noninvasive respiratory support , a trial of HFNC, CPAP, and/or BiPAP may be indicated based on the specific clinical scenario.
There are few absolute contraindications to tracheal intubation, but experts generally agree that in settings of known complete airway obstruction, endotracheal intubation should be avoided, and emergency cricothyroidotomy performed instead. Another important consideration is to ensure that caregivers provide appropriate cervical spine (C-spine) protection during the intubation procedure when neck or spinal cord injury is suspected.
The most important phase of the intubation procedure is the preprocedural preparation, when the provider ensures all the equipment and staff needed for safe intubation are present and functioning. An easy pneumonic for this is SOAP MM : suction (Yankauer suction catheter attached to wall suction); oxygen (both preoxygenation of the patient and devices needed to deliver oxygen, such as a bag-valve-mask); airway (appropriately sized endotracheal tube and laryngoscope); people (all those needed during and immediately after the procedure, including respiratory therapists and nurses); monitor (SO 2 , heart rate, blood pressure, capnography); and medications (sedation and often neuromuscular blockade to allow the provider(s) to control the airway). A simple formula for selecting the appropriately sized endotracheal tube (ETT) is:
Uncuffed ETT size (in mm)=(age in years4)+4
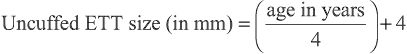
Cuffed ETTs should generally be 0.5 mm smaller. Providers should always have a range of ETTs available given the heterogeneity of patients and airway size.
Analgesia is recommended to reduce metabolic stress, discomfort, and anxiety during intubation. Pretreatment with a sedative, an analgesic, and possibly a muscle relaxant is recommended unless the situation is emergent (i.e., apnea, asystole, unresponsiveness) and the administration of drugs would cause an unacceptable delay.
Because many intubations in critically ill children are emergency procedures, caregivers should be prepared for rapid sequence intubation (RSI) (Fig. 81.12 and Table 81.4 ). The goals of RSI are to induce anesthesia and paralysis and to complete intubation quickly. This approach minimizes elevations of intracranial pressure and blood pressure that may accompany intubation in awake or lightly sedated patients. Because the stomach generally cannot be emptied before RSI, the Sellick maneuver (downward pressure on the cricoid cartilage to compress the esophagus against the vertebral column) should be used to prevent aspiration of gastric contents.
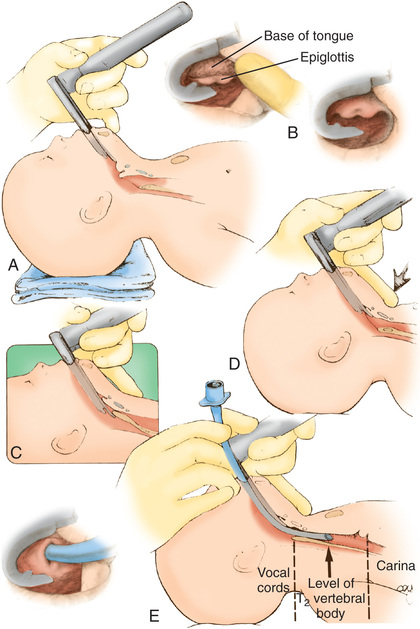
Table 81.4
| STEP | PROCEDURE | COMMENT/EXPLANATION |
|---|---|---|
| 1 | Obtain a brief history and perform an assessment. | Rule out drug allergies; examine the airway anatomy (e.g., micrognathia, cleft palate). |
| 2 | Assemble equipment, medications, etc. |
ETT: select the proper size for the age and weight of the child. Laryngoscope blades: a variety of Miller and the Macintosh blades. |
| 3 | Preoxygenate the patient. | With bag/mask, nasal cannula, hood or blow-by. |
| 4 | Position the patient. | Patient supine; neck is extended moderately to the “sniffing” position. |
| 5 | Premedicate the patient with lidocaine, atropine. | Lidocaine minimizes the ICP rise with intubation and can be applied topically to the airway mucosa for local anesthesia. |
| Atropine helps blunt the bradycardia associated with upper airway manipulation and reduces airway secretions. | ||
| 6 | Perform a Sellick maneuver. | Pressure on the cricoid cartilage, to occlude the esophagus and prevent regurgitation or aspiration. |
| 7 | Induce sedation and analgesia. | Sedatives |
| Midazolam (0.1 mg/kg): onset ~1 min; elimination in 30-40 min. | ||
| Ketamine (2 mg/kg, may repeat as clinically indicated): onset 1-2 min; elimination in 30-40 min. May cause hallucinations if used alone; can cause higher ICP, mucous secretions, increased vital signs, and bronchodilation. | ||
| Analgesics | ||
| Fentanyl (3-5 µg/kg, may repeat as clinically indicated): onset ~1 min; elimination in 20-30 min. Rapid administration risks “tight chest” response, with no effective ventilation. Effects wear off in 20-30 min. | ||
| Morphine (0.05-0.1 mg/kg dose): may last 30-60 min; may lead to hypotension in hypovolemic patients. | ||
| 8 | Administer muscle relaxants. | Option 1: Rocuronium (1 mg/kg): rapid onset and short duration. Other nondepolarizing agents include vecuronium and pancuronium, both dosed at 0.1 mg/kg. |
| Option 2: Succinylcholine dose is 1-2 mg/kg; causes initial contraction of muscles, then relaxation. This depolarization can, however, increase ICP and blood pressure. Onset of paralysis in 30-40 sec; duration is 5-10 min. Pretreat with a small dose of a nondepolarizing paralytic agent, with intent of diminishing the depolarizing effect of succinylcholine. | ||
| 9 | Perform endotracheal intubation. | Performed by trained personnel. |
| 10 | Secure the tube, and verify position with radiograph. | ETT secured with tape to the cheeks and upper lip or to an adhesive patch applied to the skin near the mouth. |
| 11 | Begin mechanical ventilation. | Verify tube placement before ventilating with positive pressure; if an ETT is in 1 bronchus, barotraumas may occur. |
ETT, Endotracheal tube; ICP, intracranial pressure.
Once the patient is intubated, proper ETT placement should be assessed by auscultation of breath sounds, evidence of symmetric chest rise, and analysis of exhaled carbon dioxide (CO2 ) by a colorimetric device placed within the respiratory tubing near the ETT or a device that directly measures CO2 elimination (capnogram or capnograph). Chest radiography is necessary to confirm appropriate tube position.
Recognition and Management of Shock
In simple terms, shock occurs when oxygen and nutrient delivery to the tissues is inadequate to meet metabolic demands (see Chapter 88 ). The definition of shock does not include hypotension, and it is important for care providers to understand that shock does not begin when blood pressure drops; it merely worsens and becomes more difficult (refractory) to treat once blood pressure is abnormal.
Early compensated shock, whereby oxygen delivery is mostly preserved through compensatory mechanisms, is defined by the presence of normal blood pressure. When compensatory mechanisms fail, the shock progresses to decompensated shock, as defined by hypotension and organ dysfunction. In irreversible shock, organ failure progresses and death ensues.
Shock is also often described according to the underlying pathophysiology, which dictates the appropriate therapeutic response. Hypovolemic shock is the most common type of shock in children worldwide, usually related to fluid losses from severe diarrhea. Hemorrhage is a cause of hypovolemic shock after trauma or intestinal hemorrhage. When hypovolemia occurs because of third spacing of intravascular fluids into the extravascular compartment, the shock is described as distributive shock . The most common causes of distributive shock are sepsis, anaphylaxis, and burn injuries, in which release of inflammatory cytokines causes massive capillary leak of fluid and proteins, leading to low oncotic pressure and intravascular volume. In settings of profound myocardial dysfunction, a child has tissue hypoperfusion from cardiogenic shock . The most common causes of cardiogenic shock are myocarditis, cardiomyopathy, and congenital heart disease, generally in the postoperative setting. Obstructive shock occurs when cardiac output is lowered by obstruction of blood flow to the body, as occurs when a ductus arteriosus closes in a child with ductus-dependent systemic blood flow, pericardial tamponade, tension pneumothorax, or massive pulmonary embolism.
The evaluation of a child in shock should proceed as described in the preceding sections on primary, secondary, and tertiary assessments. If the child presents in a hospital setting, providers should generally place a central venous line to provide secure venous access and an arterial line to permit continuous blood pressure monitoring and a more thorough laboratory assessment of organ systems, including studies of renal and liver function, acid-base balance and presence of lactic acidosis, hypoxemia and/or hypercapnia, and evidence of coagulopathy or disseminated intravascular coagulation. Chest radiography and echocardiography may also be useful. Respiratory and cardiovascular support should be provided as clinically indicated.
The treatment of shock focuses on the modifiable determinants of oxygen delivery while reducing the imbalance between oxygen supply and demand. A multipronged approach is recommended consisting of optimizing the arterial oxygen content of the blood, improving the volume and distribution of cardiac output, correcting metabolic derangements, and reducing oxygen demand. Blood oxygen content is maximized when hemoglobin values are normal and 100% of available hemoglobin is saturated with oxygen. Transfusion may be considered in the presence of hemorrhagic or distributive shock, in which crystalloid volume resuscitation has led to hemodilution and anemia. Appropriate SO 2 may be achieved by simple maneuvers, such as oxygen administration by nasal cannula or face mask; supportive measures (e.g., HFNC, CPAP, BiPAP) or invasive mechanical ventilation may be necessary. Therapies to increase cardiac output should be selected on the basis of the underlying pathophysiology. For hypovolemic and distributive shock, aggressive volume resuscitation, guided by arterial and central venous pressures, is the mainstay of therapy. In obstructive shock, relief of the obstruction is critical. The ductus arteriosus can often be reopened with prostaglandin administration and tamponade physiology relieved with appropriate drainage.
Recognition of Bradyarrhythmias and Tachyarrhythmias
In the advanced life support (ALS) setting, arrhythmias are most usefully classified according to the observed heart rate (i.e., slow or fast) and its effect on perfusion (i.e., adequate or poor). If, in the primary survey, a caregiver finds a child with an abnormal heart rate plus poor perfusion and/or altered mental status, the rhythm is inadequate no matter its rate. In those settings the child is diagnosed with shock, and further evaluation is generally halted until appropriate resuscitation has been initiated.
Bradyarrhythmias
By definition, a child is bradycardic when the heart rate is slower than the normal range for age (see Table 81.1 ). Sinus bradycardia can be a harmless incidental finding in an otherwise healthy person and not usually associated with cardiac compromise. A relative bradycardia occurs when the heart rate is too slow for a child's activity level or metabolic needs. A clinically significant bradycardia occurs when the heart rate is slow and there are signs of systemic hypoperfusion (i.e., pallor, altered mental status, hypotension, acidosis). Symptomatic bradycardia occurs most often in the setting of hypoxia but can also be caused by hypoglycemia, hypocalcemia, other electrolyte abnormalities, hypothermia, heart block, and intracranial hypertension. Bradyarrhythmias are often the most common prearrest rhythms in young children.
Initial management of symptomatic bradycardia includes support or opening of the airway and confirming or establishing adequate SO 2 and ventilation (Fig. 81.13 ). After breathing has been secured, the child should be reassessed for continued bradycardia and poor perfusion. If cardiac compromise was solely the result of respiratory insufficiency, support of the child's airway and breathing may have been sufficient to restore normal hemodynamics. If respiratory support does not correct the perfusion abnormalities, further care is based on the quality of perfusion and degree of bradycardia. A heart rate <60 beats/min with poor perfusion is an indication to begin chest compressions. If the bradycardia persists, vascular access should be obtained; resuscitative epinephrine should be administered, and it should be repeated every 3-5 min for persistent symptomatic bradycardia. If increased vagal tone (e.g., in the setting of head injury with increased intracranial pressure) or primary atrioventricular block is suspected, atropine can also be given. For cases of refractory bradycardia, cardiac pacing should be considered. During the resuscitation of a child with bradycardia, providers should assess and treat factors known to cause bradycardia, referred to collectively as the 6 Hs —hypoxia, hypovolemia, hydrogen ions (acidosis), hypokalemia or hyperkalemia, hypoglycemia, and hypothermia—and 5 Ts —toxins, tamponade, tension pneumothorax, thrombosis (in either the pulmonary or cardiac circulations), and trauma (causing hypovolemia, intracranial hypertension, cardiac compromise or tamponade) (Table 81.5 ).
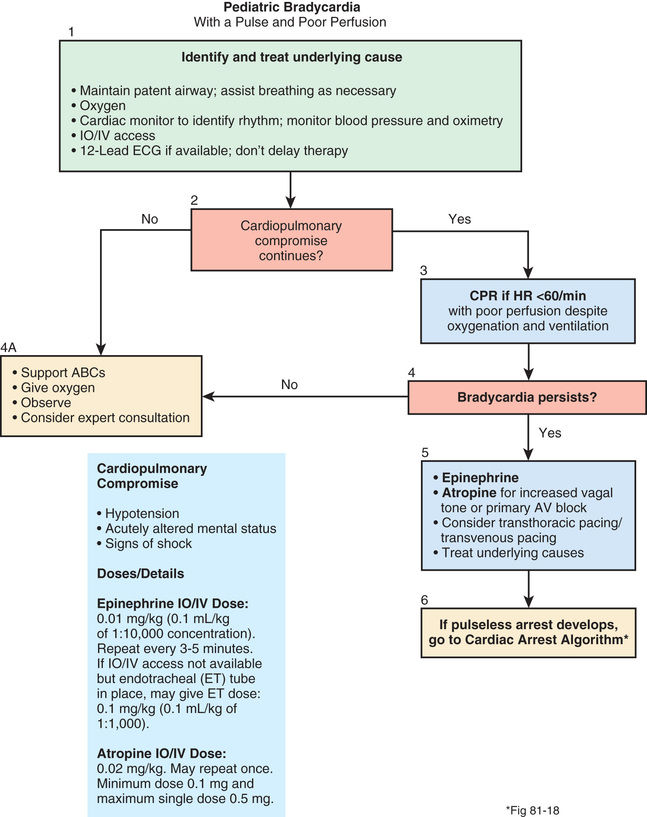
Table 81.5
| CONDITION | COMMON CLINICAL SETTINGS | CORRECTIVE ACTIONS |
|---|---|---|
| Acidosis | Preexisting acidosis, diabetes, diarrhea, drugs and toxins, prolonged resuscitation, renal disease, and shock |
Reassess the adequacy of cardiopulmonary resuscitation, oxygenation, and ventilation; reconfirm endotracheal tube placement. Hyperventilate. Consider intravenous bicarbonate if pH <7.2 after above actions have been taken. |
| Cardiac tamponade | Hemorrhagic diathesis, cancer, pericarditis, trauma, after cardiac surgery, and after myocardial infarction |
Administer fluids; obtain bedside echocardiogram, if available. Perform pericardiocentesis; immediate surgical intervention is appropriate if pericardiocentesis is unhelpful but cardiac tamponade is known or highly suspected. |
| Hypothermia | Alcohol abuse, burns, central nervous system disease, debilitated patient, drowning, drugs and toxins, endocrine disease, history of exposure, homelessness, extensive skin disease, spinal cord disease, and trauma |
If hypothermia is severe (temperature <30°C [86°F]), limit initial shocks for ventricular fibrillation or pulseless ventricular tachycardia to 3; initiate active internal rewarming and cardiopulmonary support. If hypothermia is moderate (temperature 30-34°C [86-93.2°F]), proceed with resuscitation (space medications at longer intervals than usual), passively rewarm child, and actively rewarm truncal body areas. |
| Hypovolemia, hemorrhage, anemia | Major burns, diabetes, gastrointestinal losses, hemorrhage, hemorrhagic diathesis, cancer, pregnancy, shock, and trauma |
Administer fluids. Transfuse packed red blood cells if hemorrhage or profound anemia is present. Thoracotomy is appropriate when a patient has cardiac arrest from penetrating trauma and a cardiac rhythm and the duration of cardiopulmonary resuscitation before thoracotomy is <10 min. |
| Hypoxia | Consider in all patients with cardiac arrest. | Reassess the technical quality of cardiopulmonary resuscitation, oxygenation, and ventilation; reconfirm endotracheal tube placement. |
| Hypomagnesemia | Alcohol abuse, burns, diabetic ketoacidosis, severe diarrhea, diuretics, and drugs (e.g., cisplatin, cyclosporine, pentamidine) | Administer 1-2 g magnesium sulfate intravenously over 2 min. |
| Poisoning | Alcohol abuse, bizarre or puzzling behavioral or metabolic presentation, classic toxicologic syndrome, occupational or industrial exposure, and psychiatric disease |
Consult a toxicologist for emergency advice on resuscitation and definitive care, including an appropriate antidote. Prolonged resuscitation efforts may be appropriate; immediate cardiopulmonary bypass should be considered, if available. |
| Hyperkalemia | Metabolic acidosis, excessive administration of potassium, drugs and toxins, vigorous exercise, hemolysis, renal disease, rhabdomyolysis, tumor lysis syndrome, and clinically significant tissue injury | If hyperkalemia is identified or strongly suspected, treat* with all the following: 10% calcium chloride (5-10 mL by slow IV push; do not use if hyperkalemia is secondary to digitalis poisoning), glucose and insulin (50 mL of 50% dextrose in water and 10 units of regular insulin IV), sodium bicarbonate (50 mmol IV; most effective if concomitant metabolic acidosis is present), and albuterol (15-20 mg nebulized or 0.5 mg by IV infusion). |
| Hypokalemia | Alcohol abuse, diabetes, use of diuretics, drugs and toxins, profound gastrointestinal losses, hypomagnesemia | If profound hypokalemia (<2.0-2.5 mmol of potassium) is accompanied by cardiac arrest, initiate urgent IV replacement (2 mmol/min IV for 10-15 mmol);* then reassess. |
| Pulmonary embolism | Hospitalized patient, recent surgical procedure, peripartum, known risk factors for venous thromboembolism, history of venous thromboembolism, or prearrest presentation consistent with a diagnosis of acute pulmonary embolism |
Administer fluids; augment with vasopressors as necessary. Confirm the diagnosis, if possible; consider immediate cardiopulmonary bypass to maintain patient's viability. Consider definitive care (e.g., thrombolytic therapy, embolectomy by interventional radiology or surgery). |
| Tension pneumothorax | Placement of a central catheter, mechanical ventilation, pulmonary disease (including asthma, chronic obstructive pulmonary disease, and necrotizing pneumonia), thoracentesis, and trauma | Needle decompression, followed by chest tube insertion. |
* Adult dose. Adjust for size of child. See Table 81.6 .
From Eisenbery MS, Mengert TJ: Cardiac resuscitation, N Engl J Med 344:1304–1313, 2001.
Tachyarrhythmias
Tachyarrhythmias represent a wide variety of rhythm disturbances of atrial and ventricular origin (see Chapter 462 ). Sinus tachycardia is a normal physiologic response to the body's need for increased cardiac output or oxygen delivery, as occurs with fever, exercise, or stress. It can also occur in more pathologic states, such as hypovolemia, anemia, pain, anxiety, and metabolic stress. Tachyarrhythmias that do not originate in the sinus node are often categorized as narrow complex rhythms (i.e., originating in the atrium, such as atrial flutter or supraventricular tachycardia, SVT) and wide complex rhythms (i.e., rhythms of ventricular origin, such as ventricular tachycardia).
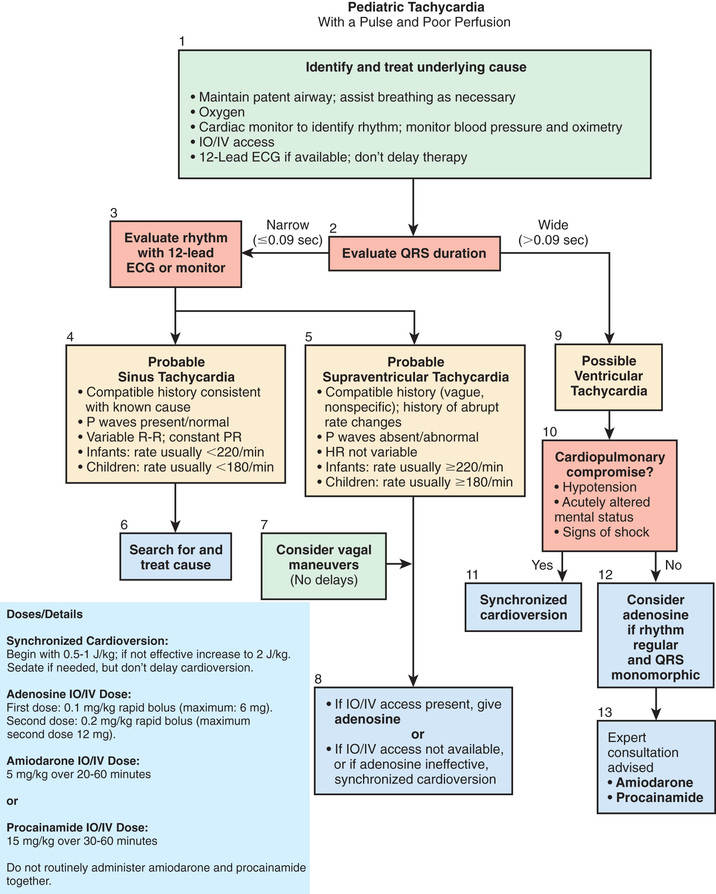
The initial management of tachycardia includes confirmation that the child has an adequate airway and life-sustaining breathing and circulation (Fig. 81.14 ). For children with persistent symptoms, further treatment is based on whether the QRS complex of the electrocardiogram (ECG) is narrow (≤0.09 sec) or wide (>0.09 sec). For narrow complex tachycardia, providers must distinguish between sinus tachycardia and SVT. In sinus tachycardia , (a) the history and onset are consistent with a known cause of tachycardia, such as fever or dehydration, and (b) P waves are consistently present, are of normal morphology, and occur at a rate that varies somewhat. In supraventricular tachycardia , (a) onset is often abrupt without prodrome, and (b) P waves are absent or polymorphic, and when present, their rate is often fairly steady at or above 220 beats/min. For children with SVT and good perfusion, vagal maneuvers can be attempted. When SVT is associated with poor perfusion, providers should rapidly move to convert the child's heart rhythm back to sinus rhythm. If the child already has IV access, adenosine can be given via IV access with rapid push. Adenosine has an extremely short half-life, so a proximal IV line is best, and the adenosine should be set up with a 3-way stopcock so it can be given and immediately flushed into the circulation. If the child does not have IV access, or adenosine does not successfully convert the heart rhythm back to sinus rhythm, then synchronized cardioversion , using 0.5-1.0 joule (J)/kg, should be performed. In cases of wide complex tachycardia, providers should generally move immediately to cardioversion and increase the dose to 2 J/kg if 1 J/kg is not effective. As with cases of bradycardia, providers should review the 6 Hs and 5 Ts to identify factors that might be contributing to the tachycardia (see Table 81.5 ).
Recognition and Management of Cardiac Arrest
Cardiac arrest occurs when the heart fails as an effective pump and blood flow ceases. Outwardly, the patient in cardiac arrest presents as unresponsive and apneic with no palpable pulse. Internally, the cessation of nutrient flow causes progressive tissue ischemia and organ dysfunction. If not rapidly reversed, cardiac arrest leads to progressive deterioration in brain, heart, and other organ function, such that resuscitation and recovery are no longer possible.
Pediatric cardiac arrest is rarely caused by a sudden coronary event or arrhythmia. Instead, cardiac arrest in children is most often the end result of progressive organ and tissue ischemia, caused by tissue hypoxia, acidosis, and nutrient depletion at the end stages of respiratory deterioration, shock, or heart failure. Therefore, the most important treatment of cardiac arrest is anticipation and prevention. Intervening when a child manifests respiratory distress or early stages of shock can prevent deterioration to full arrest . When sudden cardiac arrest does occur, it is often associated with an arrhythmia, specifically ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT). In sudden events such as these, the key to successful resuscitation is early recognition of the arrhythmia and prompt treatment with high-quality CPR and defibrillation.
The principle behind high-quality CPR is that adequate chest compressions—those that circulate blood around the body with a good pulse pressure—are the most important component of CPR. The caregiver providing chest compressions should push hard, push fast, allow for complete chest recoil, and minimize interruptions . Ideally, chest compressions should be interrupted only for a rhythm check or delivery of a defibrillating shock. Providers should refer to the most recent American Heart Association (AHA) guidelines for pediatric BLS and ALS (eccguidelines.heart.org ).
Cardiac arrest is recognized from general and primary survey findings consistent with a pale or cyanotic child who is unresponsive, apneic, and pulseless. Even experienced providers have a relatively high error rate when asked to determine presence or absence of pulse in a child. Therefore, any child found unresponsive and apneic can be presumed to be in cardiac arrest, and a rescuer should respond accordingly. A lone rescuer for an unwitnessed pediatric cardiac arrest in an outpatient setting should treat the arrest as asphyxial in nature, immediately initiate CPR, and activate the emergency response system via a mobile phone (if available). If a mobile phone is not immediately available, the rescuer should perform initial rescue breaths and 2 min of chest compressions and ventilations before leaving the child to activate the emergency response system. For an in-hospital arrest, the provider should call for help and have a team member activate the emergency response system while beginning CPR. A lone rescuer in an outpatient setting who witnesses a child's sudden collapse should treat the arrest as a primary arrhythmia, should immediately activate the EMS system, and obtain an AED. On returning to the child, the rescuer should confirm pulselessness, turn on the AED, place the leads on the child's chest, and follow the defibrillator's voice commands.
The initial step in CPR for a child of any age is to restore ventilation and oxygenation as quickly as possible. On confirmation of unresponsiveness, apnea, and/or pulselessness, resuscitation should follow current AHA Basic Life Support (BLS), (or Advanced Cardiac Life Support, ACLS) guidelines, as appropriate (eccguidelines.heart.org ).
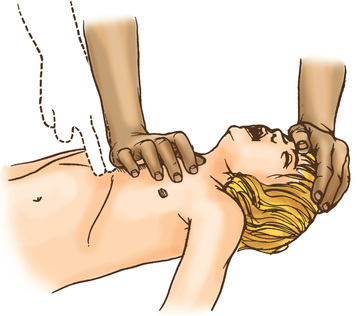
If a person is pulseless, chest compressions should be initiated. Chest compressions in infants <1 yr old may be performed by placing 2 thumbs on the midsternum with the hands encircling the thorax or by placing 2 fingers over the midsternum and compressing (Figs. 81.15 and 81.16 ). For children >1 yr old, the care provider should perform chest compressions over the lower half of the sternum with the heel of 1 hand, or with 2 hands as used for adult resuscitation (Fig. 81.17 ). In all cases, care should be taken to avoid compression of the xiphoid and the ribs. When feasible, a cardiac resuscitation board should be placed under the child's back to maximize the efficiency of compressions. CPR and rescue breathing should be performed based on current AHA BLS/ACLS guidelines.

The goal of CPR is to reestablish spontaneous circulation at a level that is compatible with survival. If resuscitative efforts do not succeed in reestablishing life-sustaining breathing and circulation, the medical team must decide whether continued efforts are warranted or whether the resuscitation should be stopped. If EMS care is en route, bringing the potential for further escalation in care, such as endotracheal intubation, vascular access, and medications, CPR should be continued as long as possible or deemed reasonable by the rescuers.
In the in-hospital setting, the ECG should dictate further resuscitative efforts. For children without a pulse and in asystole or electromechanical dissociation (pulseless electrical activity , PEA), providers should continue rescue breathing and CPR, obtain vascular access, and administer emergency IV epinephrine (Fig. 81.18 ). For continued asystole or PEA, epinephrine can be repeated every 3-5 min. Patient history, physical exam findings, and laboratory evaluation should be used to elicit correctable causes of arrest (e.g., 6 Hs, 5 Ts; see Table 81.5 ). CPR should be continued after epinephrine administration, to circulate the drug through the body. After 5 cycles of CPR, providers should reassess the child for the presence of a pulse or a change in the ECG rhythm that would necessitate a different response.
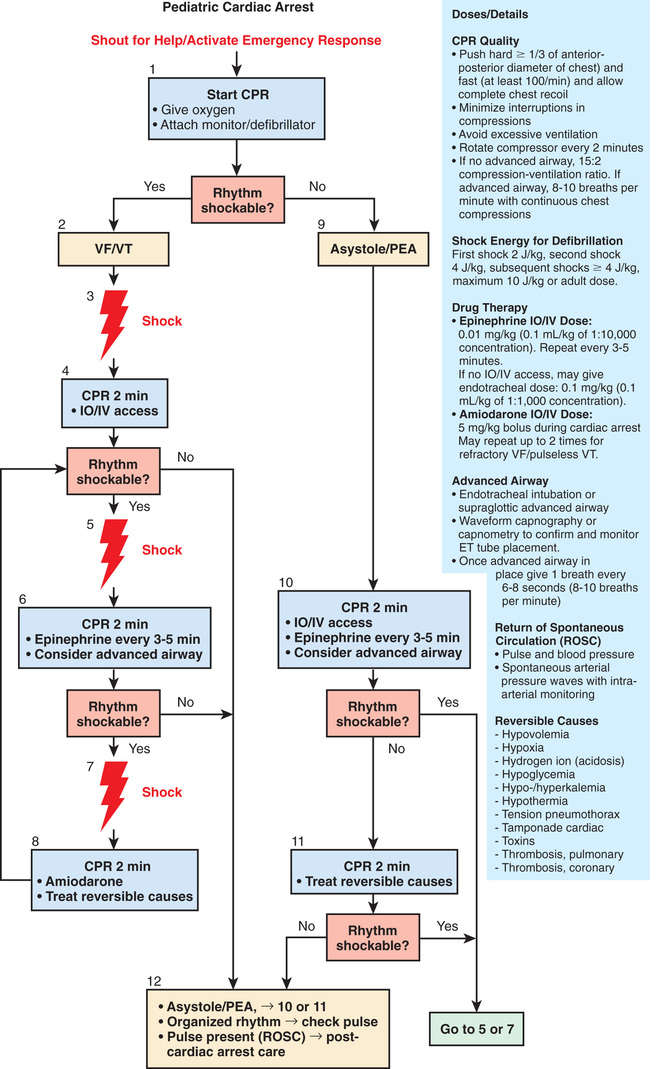
For those children with pulseless VT or VF, emergency defibrillation is indicated (Fig. 81.18 ). Providers should apply the pads to the child's bare chest and back and follow the verbal instructions given by the AED. For younger children, a defibrillator (if available) set to the dose of 2 J/kg should be used. Ideally, the AED used in a child ≤8 yr of age should be equipped with an attenuated adult dose or should be designed for children; if neither device is available, a standard adult AED should be used. CPR should be immediately restarted after defibrillation. Emergency dose epinephrine can also be administered with another 5 cycles of CPR to ensure its circulation throughout the child's body. If the ECG rhythm continues to show VF or VT, defibrillation can be alternated with epinephrine. For refractory VF or VT, an IV antiarrhythmic, such as lidocaine or amiodarone, can be given (Tables 81.6 and 81.7 ). Some adult studies have suggested that a combination of epinephrine, vasopressin, and methylprednisolone improves intact survival after CPR.
Table 81.6
Medications for Pediatric Resuscitation and Arrhythmias
| MEDICATION | DOSE | REMARKS |
|---|---|---|
| Adenosine | 0.1 mg/kg (max: 6 mg) | Monitor ECG. |
| Repeat: 0.2 mg/kg (max: 12 mg) | Rapid IV/IO bolus. | |
| Amiodarone | 5 mg/kg IV/IO; repeat up to 15 mg/kg | Monitor ECG and blood pressure. |
| Max: 300 mg | Adjust administration rate to urgency (give more slowly when perfusing rhythm is present). | |
| Use caution when administering with other drugs that prolong QT interval (consider expert consultation). | ||
| Atropine | 0.02 mg/kg IV/IO | Higher doses may be used with organophosphate poisoning. |
| 0.03 mg/kg ETT* | ||
| Repeat once if needed | ||
| Minimum dose: 0.1 mg | ||
| Minimum single dose: | ||
| Child, 0.5 mg | ||
| Adolescent, 1 mg | ||
| Calcium chloride (10%) | 20 mg/kg IV/IO (0.2 mL/kg) | Slowly |
| Adult dose: 5-10 mL | ||
| Epinephrine | 0.01 mg/kg (0.1 mL/kg 1 : 10,000) IV/IO | May repeat every 3-5 min |
| 0.1 mg/kg (0.1 mL/kg 1 : 1,000) ETT* | ||
| Max dose: 1 mg IV/IO; 10 mg ET | ||
| Glucose | 0.5-1 g/kg IV/IO | D10W: 5-10 mL/kg |
| D25W: 2-4 mL/kg | ||
| D50W: 1-2 mL/kg | ||
| Lidocaine | Bolus: 1 mg/kg IV/IO | |
| Max dose: 100 mg | ||
| Infusion: 20-50 µg/kg/min | ||
| ETT* : 2-3 mg | ||
| Magnesium sulfate | 25-50 mg/kg IV/IO over 10-20 min; faster in torsades de pointes | |
| Max dose: 2 g | ||
| Naloxone | <5 yr or ≤20 kg: 0.1 mg/kg IV/IO/ETT* | Use lower doses to reverse respiratory depression associated with therapeutic opioid administration (1-15 µg/kg). |
| ≥5 yr or >20 kg: 2 mg IV/IO/ETT* | ||
| Procainamide | 15 mg/kg IV/IO over 30-60 min | Monitor EGG and blood pressure. |
| Adult dose: 20 mg/min IV infusion up to total max dose of 17 mg/kg | Use caution when administering with other drugs that prolong QT interval (consider expert consultation). | |
| Sodium bicarbonate | 1 mEq/kg/dose IV/IO slowly | After adequate ventilation |
* Flush with 5 mL of normal saline and follow with 5 ventilations.
ECG, Electrocardiogram; ETT, endotracheal tube; IO, intraosseous; IV, intravenous.
From ECC Committee, Subcommittees and Task Forces of the American Heart Association: 2005 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, Circulation 112:IV1–203, 2005.
Table 81.7
| MEDICATION | DOSE RANGE | COMMENT |
|---|---|---|
| Inamrinone | 0.75-1 mg/kg IV/IO over 5 min; may repeat 2×; then: 2-20 µg/kg/min | Inodilator |
| Dobutamine | 2-20 µg/kg/min IV/IO | Inotrope; vasodilator |
| Dopamine | 2-20 µg/kg/min IV/IO in low doses; pressor in higher doses | Inotrope; chronotrope; renal and splanchnic vasodilator |
| Epinephrine | 0.1-1 µg/kg/min IV/IO | Inotrope; chronotrope; vasodilator in low doses; vasopressor in higher doses |
| Milrinone | 50-75 µg/kg IV/IO over 10-60 min then 0.5-0.75 µg/kg/min | Inodilator |
| Norepinephrine | 0.1-2 µg/kg/min | Inotrope; vasopressor |
| Sodium nitroprusside | 1-8 µg/kg/min | Vasodilator; prepare only in D5W |
* Alternative formula for calculating an infusion: Infusion rate (mL/hr) = [weight (kg) × dose (µg/kg/min) × 60 (min/hr)]/concentration µg/mL).
D5W, 5% Dextrose in water; IO, intraosseous; IV, intravenous.
From ECC Committee, Subcommittees and Task Forces of the American Heart Association: 2005 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, Circulation 112:IV1–IV203, 2005.
Traditionally, continuing CPR >20 min in children with in-hospital cardiac arrest has been considered futile. With current practice for CPR, survival for in-hospital cardiac arrest is approximately 40% for CPR duration <15 min, compared with approximately 12% for CPR lasting >35 min. Survivors had a favorable neurologic outcome in 70% with a CPR duration <15 min, compared with 60% for those requiring resuscitation for >35 min.
Vascular Access
Venous Access
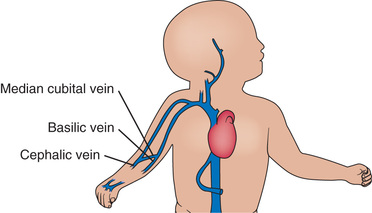
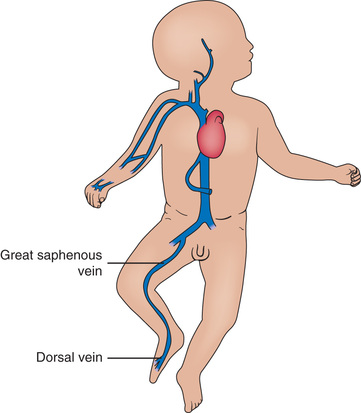
Veins suitable for cannulation are numerous, but there is considerable anatomic variation from patient to patient. In the upper extremities, the median antecubital vein , located in the antecubital fossa, is often the largest and easiest to access (Fig. 81.19 ). Many veins on the dorsum of the hand are also suitable for cannulation because they are often large and easily located, and their cannulation is generally well tolerated. The cephalic vein is usually cannulated at the wrist, along the forearm, or at the elbow. The median vein of the forearm is also suitable as it lies along a flat surface of the forearm. In the lower extremity, the great saphenous vein , located just anterior to the medial malleolus, is accessible in most patients. The dorsum of the foot usually has a large vein in the midline, passing across the ankle joint, but catheters are difficult to maintain in this vein because dorsiflexion tends to dislodge them. A 2nd large vein on the lateral side of the foot, running in the horizontal plane, usually 1-2 cm dorsal to the lower margin of the foot, is preferable (Fig. 81.20 ). The most notable scalp veins are the superficial temporal (just anterior to the ear) and posterior auricular (just behind the ear).
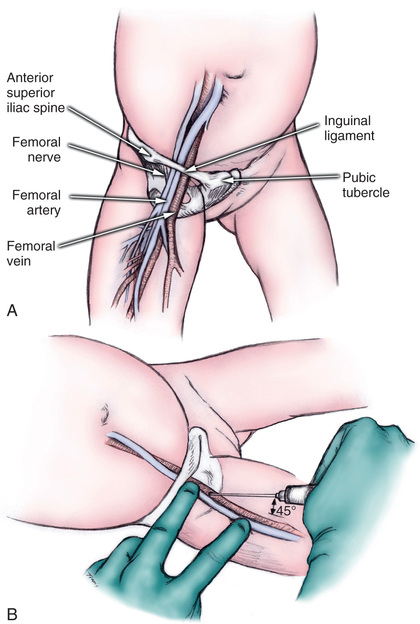
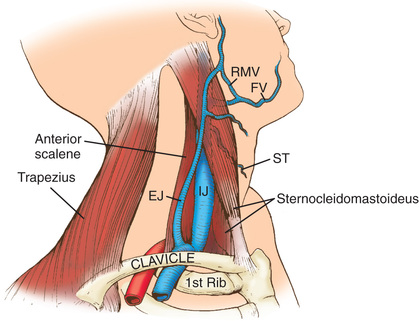
Deeper and larger central veins can provide more reliable, larger-bore access for medications, nutritive solutions, and blood sampling than peripheral venous lines. They may be reached by percutaneous cannulation or surgical exposure. In infants and young children, the femoral vein is often the easiest to access and cannulate, but the internal jugular and subclavian veins may also be used (Figs. 81.21 and 81.22 ). Because of its proximity to the median nerve, the brachial vein is not often recommended for cannulation.
Intraosseous Access
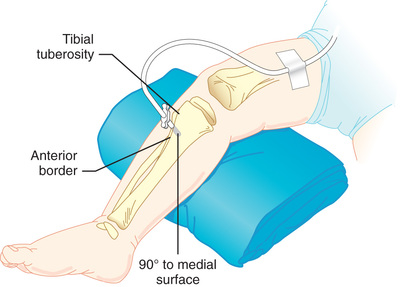
Intraosseous (IO) needles (for intramedullary venous plexus access) are special rigid, large-bore needles. IO cannulation is recommended for patients in whom IV access proves difficult or unattainable, even in older children. If venous access is not available within approximately 1 min in a child with cardiopulmonary arrest, an IO needle should be placed in the anterior proximal tibia (with care taken to avoid traversing the epiphyseal plate). The needle should penetrate the anterior layer of compact bone, and its tip is advanced into the spongy interior of the bone (Fig. 81.23 ). Commercially available IO kits frequently include drills that obviate the complications of needle placement associated with manual placement. All medications, blood products, and fluids may be administered through the IO route, including medications required for emergency resuscitation. Complications are uncommon but may include osteomyelitis with prolonged infusions and tibial fracture.
If IV and IO routes are unavailable in an intubated patient, medication can be given through the ETT (epinephrine, atropine, naloxone, vasopressin).
Arterial Access
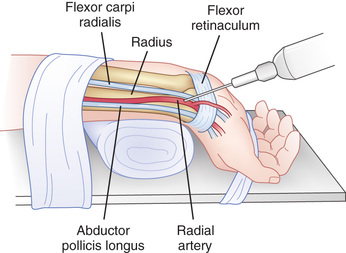
Arterial access is indicated when care providers need frequent blood sampling, particularly to assess adequacy of oxygenation, ventilation, or acid-base balance, and/or continuous blood pressure monitoring. The radial artery , the most commonly cannulated artery, lies on the lateral side of the anterior wrist, just medial to the styloid process of the radius (Fig. 81.24 ). The ulnar artery, just lateral to the tendon of the flexor carpi ulnaris, is used less often because of its proximity to the ulnar nerve. Useful sites in the lower extremity, particularly in neonates and infants, are the dorsalis pedis artery , on the dorsum of the foot between the tendons of the tibialis anterior and the extensor hallucis longus, and the posterior tibial artery , posterior to the medial malleolus. Arterial catheters require special care for insertion and subsequent management.
Nonvascular Emergency Procedures
Thoracentesis and Chest Tube Placement
Thoracentesis is the placement of a needle or catheter into the pleural space to evacuate fluid, blood, or air. Most insertions are performed in one of the intercostal spaces between the 4th and 9th ribs in the plane of the midaxillary line. After appropriate systemic and local anesthesia/sedation is performed as clinically indicated, a skin incision is made, and dissection through the chest wall is accomplished in layers with use of blunt dissection techniques. The needle (and later the chest tube) that enters the pleural space should penetrate the intercostal space by passing over the superior edge of the lower rib, because there are larger vessels along the inferior edge of the rib. Ideally, the chest tube should lie anterior in the pleural space for air accumulation and posterior for fluid accumulation. A radiograph must be obtained to verify chest tube placement and evacuation of the pleural space.
Pericardiocentesis
When fluid, blood, or gas accumulates in the pericardial sac, the heart may become compressed and may be unable to fill/empty with normal volumes of blood, leading to diminished cardiac output. The cardinal signs of such a restrictive pericardial effusion are tachycardia, hypotension generally with a narrowed pulse pressure, and decreased SO 2 . Pericardiocentesis includes needle aspiration of the pericardial sac, often followed by the placement of a catheter for continuous drainage. As with thoracentesis, chest radiography should be done to confirm catheter location as well as evaluate for any complications, such as pneumothorax or hemothorax. Pericardiocentesis may be performed with echocardiography.
Postresuscitation Care
After successful resuscitation, close observation in an intensive care unit, where the child can receive ongoing multiorgan system assessments and support, is critical. Optimal postresuscitation care includes ongoing support of cardiovascular and respiratory system function as needed and the identification and treatment of other organ system dysfunction that may have contributed to (or resulted from) the child's cardiopulmonary instability. Good postresuscitation intensive care also includes supportive services for the child's parents, siblings, family, and friends.
Induced hypothermia (32-34°C [89.6-91.4°F] versus targeted temperature 36.8°C (98.2°F) (range, 36-37.5°C [96.8-99.5°F]) for about 48 hr) has not been shown to improve survival and neurologic function in pediatric survivors of CPR. However, hyperthermia must be avoided. Hypoxic-ischemic encephalopathy with subsequent development of seizures, intellectual impairment, and spasticity, is a serious and common complication of cardiac arrest. In addition, hyperglycemia and hypoglycemia should be avoided.
Postresuscitation management generally has 2 phases. First, the providers must assess the child's airway and breathing and support oxygenation and ventilation as indicated. If the child has ongoing respiratory failure and has been supported with bag-valve-mask ventilation until this time, the providers should now move forward with intubation. Once the child is intubated, mechanical ventilation must be established and respiratory assessments performed, such as chest radiography and arterial blood gas analysis. The child's circulatory system must also be assessed and supported as needed. Continuous arterial blood pressure monitoring can help the provider determine the need for, and response to, inotropic and chronotropic medications (see Table 81.7 ). Once the ABCs have been managed, providers can move on to full organ system assessments. A systematic approach should be used, with a full physical exam and laboratory evaluation to reveal the child's respiratory, cardiovascular, neurologic, gastrointestinal, renal, and hematologic system function.
Communication with the patients’ family is an essential element of postresuscitation care. The family should be thoroughly briefed on the elements of the resuscitation performed, the child's condition, and ongoing medical concerns, uncertainties, or issues by the most senior provider available . This provider should be available to answer the family's questions, clarify information, and provide comfort. Other support staff, including social workers and chaplains, should be contacted, as the family wishes, to provide additional support and comfort. For situations in which the resuscitation is ongoing and the child is not expected to survive, it is recommended that the provider make every effort possible to have the family present at the bedside, if they wish. Family presence during CPR or other emergency resuscitative efforts, even if the child dies, is associated with a more positive medical experience than if they are excluded. In situations where the child is critically ill but stable, the family should be brought to the bedside as soon as the healthcare team deems it safe and appropriate (see Chapter 7 ).