Acute Care of Multiple Trauma
Cindy Ganis Roskind, Howard I. Pryor II, Bruce L. Klein
Epidemiology
Injury is a leading cause of death and disability in children throughout the world (see Chapter 13 ). Deaths represent only a small fraction of the total trauma burden. Approximately 140,000 children were treated in U.S. trauma centers in 2016 for serious injury. Many survivors of trauma have permanent or temporary functional limitations. Motor vehicle–related injuries and falls rank among the top 15 causes of disability-adjusted life years in children worldwide.
Trauma is frequently classified according to the number of significantly injured body parts (≥1), the severity of injury (mild, moderate, or severe), and the mechanism of injury (blunt or penetrating). In childhood, blunt trauma predominates, accounting for the majority of injuries. In adolescence, penetrating trauma increases in frequency, accounting for approximately 15% of injuries, and penetrating trauma secondary to a firearm is associated with a high case fatality rate of 11%.
Regionalization and Trauma Teams
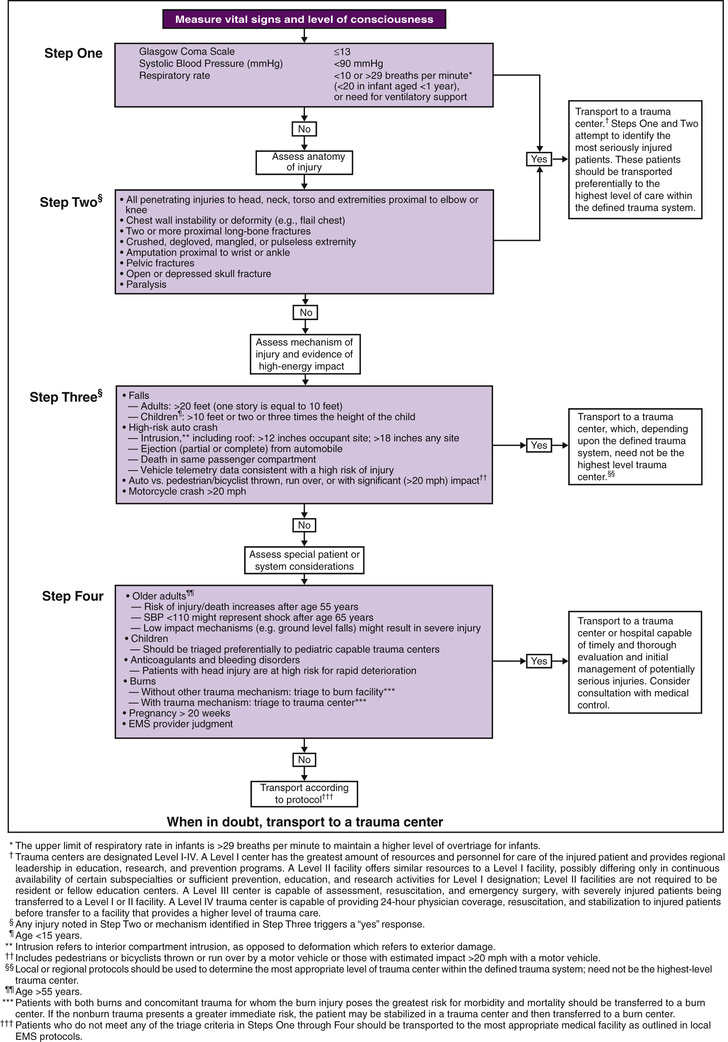
Mortality and morbidity rates have decreased in geographic regions with comprehensive, coordinated trauma systems. Treatment at designated trauma centers is associated with decreased mortality. At the scene of injury, paramedics should administer necessary advanced life support and perform triage (Fig. 82.1 ). It is usually preferable to bypass local hospitals and rapidly transport a seriously injured child directly to a pediatric trauma center (or a trauma center with pediatric commitment). Children have lower mortality rates, lower complication rates, and less operative interventions after severe blunt trauma when they are treated in designated pediatric trauma centers or in hospitals with pediatric intensive care units.
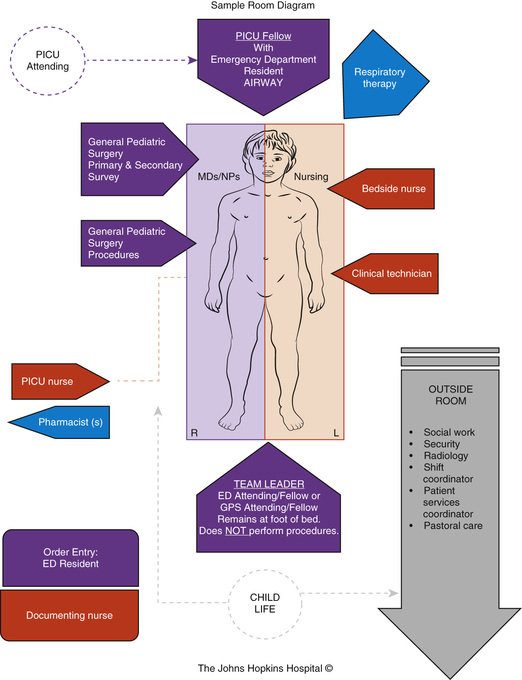
When the receiving emergency department (ED) is notified before the child's arrival, the trauma team should also be mobilized in advance. Each member has defined tasks. A senior surgeon (surgical coordinator) or, sometimes initially, an emergency physician leads the team. Team compositions vary somewhat from hospital to hospital; Fig. 82.2 shows the model used at The Johns Hopkins Hospital Bloomberg Children's Center (Baltimore, MD). Consultants, especially neurosurgeons and orthopedic surgeons, must be promptly available; and the operating room staff should be alerted.
Physiologic status, anatomic locations, and/or mechanism of injury are used for field triage as well as to determine whether to activate the trauma team. More importance should be placed on physiologic compromise and less on mechanism of injury. Scoring scales such as the Abbreviated Injury Scale (AIS), Injury Severity Score (ISS), Pediatric Trauma Score (Table 82.1 ), and Revised Trauma Score use these parameters to predict patient outcome. The AIS and ISS are used together. First, the AIS is used numerically to score injuries—as 1 minor, 2 moderate, 3 serious, 4 severe, 5 critical, or 6 probably lethal—in each of 6 ISS body regions: head/neck, face, thorax, abdomen and pelvic contents, extremities and bony pelvis, and external. The ISS is the sum of the squares of the highest 3 AIS region scores.
Table 82.1
Pediatric Trauma Score*
| COMPONENT | +2 | +1 | −1 |
|---|---|---|---|
| Size | ≥20 kg | 10-20 kg | <10 kg |
| Airway | Normal | Maintainable | Unmaintainable |
| Systolic BP | ≥90 mm Hg | 50-90 mm Hg | <50 mm Hg |
| CNS | Awake | Obtunded/LOC | Coma/decerebrate |
| Open wound | None | Minor | Major/penetrating |
| Skeletal | None | Closed fracture | Open/multiple fractures |
| Sum total points |
* Children with a Pediatric Trauma Score ≤6 are at increased risk of mortality as well as morbidity.
BP, Blood pressure; CNS, central nervous system; LOC, loss of consciousness.
From Tepas JJ 3rd, Mollitt DL, Talbert JL, et al: The Pediatric Trauma Score as a predictor of injury severity in the injured child, J Pediatr Surg 22:14–18, 1987 (Table 1, p 15).
Primary Survey
During the primary survey, the physician quickly assesses and treats any life-threatening injuries. The principal causes of death shortly after trauma are airway obstruction, respiratory insufficiency, shock from hemorrhage, and central nervous system (CNS) injury. The primary survey addresses the ABCDEs : Airway, Breathing, Circulation, neurologic Deficit, and Exposure of the patient and control of the Environment.
Airway/Cervical Spine
Optimizing oxygenation and ventilation, while protecting the cervical spine (C-spine) from potential further injury, is of paramount importance. Initially, C-spine injury should be suspected in any child sustaining multiple, blunt trauma. Although C-spine injuries occur less often in children than adults, children are at risk for such injuries because of their relatively large heads in proportion to the rest of their body, which augment flexion-extension forces, and weak neck muscles, which predispose them to ligament injuries. To prevent additional spinal injury, paramedics have traditionally been taught to immobilize the cervical (and thoracic and lumbar) spine in neutral position with a stiff collar, head blocks, tape or cloth placed across the forehead, torso, and thighs to restrain the child, and a rigid backboard.
Airway obstruction manifests as snoring, gurgling, hoarseness, stridor, and/or diminished breath sounds (even with apparently good respiratory effort). Children are more likely than adults to have airway obstruction because of their smaller oral and nasal cavities, proportionately larger tongues and more tonsillar and adenoidal tissue, higher and more anterior glottic opening, and narrower larynx and trachea. Obstruction is common in patients with severe head injuries, partly because of decreased muscle tone, which allows the tongue to fall posteriorly and occlude the airway. With trauma, obstruction can also result from fractures of the mandible or facial bones, secretions such as blood or vomit, crush injuries of the larynx or trachea, and foreign body aspiration.
If it is necessary to open the airway, a jaw thrust without head tilt is recommended. This procedure minimizes cervical spine motion. In an unconscious child, an oropharyngeal airway may be inserted to prevent posterior displacement of the mandibular tissues. A semiconscious child will gag with an oropharyngeal airway but may tolerate a nasopharyngeal airway. A nasopharyngeal airway is contraindicated when there is a possibility of cribriform plate fracture. If these maneuvers plus suctioning do not clear the airway, oral endotracheal intubation is indicated. When endotracheal intubation proves difficult, a laryngeal mask airway can be used as a temporary alternative. A laryngeal mask airway consists of a tube with an inflatable cuff that rests above the larynx and thus does not require placement of the tube into the trachea. Video-assisted laryngoscopy or the use of a bougie can also be helpful in the management of a difficult airway. Emergency cricothyrotomy is needed in <1% of trauma victims.
Breathing
The physician assesses breathing by counting the respiratory rate; visualizing chest wall motion for symmetry, expansion, and accessory muscle use; and auscultating breath sounds in both axillae. Continuous waveform capnography monitoring should also be used as an adjunct; however, it is less reliable in patients with shock. In addition to looking visually for cyanosis, pulse oximetry is standard. If ventilation is inadequate, bag-valve-mask ventilation with 100% oxygen must be initiated immediately, followed by endotracheal intubation. End-expiratory carbon dioxide (CO2 ) detectors or capnography help verify accurate tube placement.
Head trauma is the most common cause of respiratory insufficiency. An unconscious child with severe head injury may have a variety of breathing abnormalities, including Cheyne-Stokes respiration, slow irregular breaths, and apnea.
Although less common than a pulmonary contusion, tension pneumothorax and massive hemothorax are immediately life threatening (Tables 82.2 and 82.3 ). Tension pneumothorax occurs when air accumulates under pressure in the pleural space. The adjacent lung is compacted, the mediastinum is pushed toward the opposite hemithorax, and the heart, great vessels, and contralateral lung are compressed or kinked (see Chapter 439 ). Both ventilation and cardiac output are impaired. Characteristic findings include cyanosis, tachypnea, retractions, asymmetric chest rise, contralateral tracheal deviation, diminished breath sounds on the ipsilateral (more than contralateral) side, and signs of shock. Needle thoracentesis, followed by thoracostomy tube insertion, is diagnostic and lifesaving. Hemothorax results from injury to the intercostal vessels, lungs, heart, or great vessels. When ventilation is adequate, fluid resuscitation should begin before evacuation, because a large amount of blood may drain through the chest tube, resulting in shock.
Table 82.2
Differential Diagnosis of Immediately Life-Threatening Cardiopulmonary Injuries
| TENSION PNEUMOTHORAX | MASSIVE HEMOTHORAX | CARDIAC TAMPONADE | |
|---|---|---|---|
| Breath sounds | Ipsilaterally decreased more than contralaterally | Ipsilaterally decreased | Normal |
| Percussion note | Hyperresonant | Dull | Normal |
| Tracheal location | Contralaterally shifted | Midline or shifted | Midline |
| Neck veins | Distended | Flat | Distended |
| Heart tones | Normal | Normal | Muffled |
Modified from Cooper A, Foltin GL: Thoracic trauma. In Barkin RM, editor: Pediatric emergency medicine , ed 2, St Louis, 1997, Mosby, p 325.
Circulation
Signs of shock include tachycardia; weak pulse; delayed capillary refill; cool, mottled, pale skin; and altered mental state (see Chapter 88 ). The most common type of shock in trauma is hypovolemic shock caused by hemorrhage. Cardiac tamponade, which is a form of obstructive shock, may be suspected clinically or diagnosed by focused assessment with sonography in trauma (FAST) examination or echocardiography. Cardiac tamponade is best managed by thoracotomy or pericardial window, although pericardiocentesis may be necessary as a temporizing maneuver (see Table 82.3 ).
Early in shock, blood pressure remains normal because of compensatory increases in heart rate and peripheral vascular resistance (Table 82.4 ). Some individuals can lose up to 30% of blood volume before blood pressure declines. It is important to note that 25% of blood volume equals 20 mL/kg, which is only 200 mL in a 10 kg child. Losses >40% of blood volume cause severe hypotension that, if prolonged, may become irreversible. Direct pressure should be applied to control external hemorrhage. When direct pressure does not control hemorrhage, a tourniquet should be applied to a proximal pressure point. Blind clamping of bleeding vessels, which risks damaging adjacent structures, is not advisable.
Table 82.4
Systemic Responses to Blood Loss in Pediatric Patients
| SYSTEM | MILD BLOOD LOSS (<30%) | MODERATE BLOOD LOSS (30–45%) | SEVERE BLOOD LOSS (>45%) |
|---|---|---|---|
| Cardiovascular | Increased heart rate; weak, thready peripheral pulses; normal systolic blood pressure; normal pulse pressure | Markedly increased heart rate; weak, thready central pulses; peripheral pulses absent; low normal systolic blood pressure; narrowed pulse pressure | Tachycardia followed by bradycardia; central pulses very weak or absent; peripheral pulses absent; hypotension; narrowed pulse pressure (or undetectable diastolic blood pressure). |
| Central nervous | Anxiety; irritability; confusion | Lethargy; dulled response to pain | Coma |
| Skin | Cool, mottled; capillary refill prolonged | Cyanotic; capillary refill markedly prolonged | Pale and cold |
| Urine output | Low to very low | Minimal | None |
Adapted from American College of Surgeons Committee on Trauma: Advanced trauma life support for doctors: student course manual, ed 9, Chicago, 2012, American College of Surgeons.
Cannulating a larger vein, such as an antecubital vein, is usually the quickest way to achieve intravenous (IV) access. A short, large-bore catheter offers less resistance to flow, allowing for more rapid fluid administration. Ideally, a 2nd catheter should be placed within the first few minutes of resuscitation in a severely injured child. If IV access is not rapidly obtainable, an intraosseous (IO) needle should be inserted; all medications and fluids can be administered intraosseously. Other alternatives are central venous access using the Seldinger technique (e.g., in the femoral vein) and, rarely, surgical cutdown (e.g., in saphenous vein). Ultrasonography should be used to facilitate central venous catheter placement, if possible.
Traditionally, fluids are administered aggressively early in hemorrhagic shock to reverse and prevent further clinical deterioration. Isotonic crystalloid solution, such as lactated Ringer injection or normal saline (20 mL/kg), should be infused rapidly. When necessary, repeated crystalloid boluses may be given. Most children are stabilized with administration of crystalloid solution alone. However, if the patient remains in shock after boluses totaling 40-60 mL/kg of crystalloid, packed red blood cells should be transfused. Massive transfusion protocols (including fresh-frozen plasma) should be initiated early to prevent coagulopathy. When shock persists despite these measures, surgery to stop internal hemorrhage is usually indicated. Although literature is emerging regarding the benefits of permissive hypotension, hemostatic resuscitation, and damage control surgery for adult trauma patients, currently there are no pediatric data.
Neurologic Deficit
Neurologic status is briefly assessed by determining the level of consciousness and evaluating pupil size and reactivity. The level of consciousness can be classified using the mnemonic AVPU : Alert, responsive to Verbal commands, responsive to Painful stimuli, or Unresponsive.
At least 75% of pediatric blunt trauma deaths are accounted for by head injuries. Primary direct cerebral injury occurs within seconds of the event and is irreversible. Secondary injury is caused by subsequent anoxia or ischemia. The goal is to minimize secondary injury by ensuring adequate oxygenation, ventilation, and perfusion, and maintaining normal cerebral perfusion pressure. A child with severe neurologic impairment—i.e., with a Glasgow Coma Scale (GCS; see Chapter 85 ) score of ≤8—should undergo endotracheal intubation and supportive mechanical ventilation.
Signs of increased intracranial pressure (ICP), including progressive neurologic deterioration and evidence of transtentorial herniation, must be treated immediately (see Chapter 85 ). Hyperventilation lowers the arterial partial pressure of carbon dioxide (PaCO 2 ), resulting in cerebral vasoconstriction, reduced cerebral blood flow, and decreased ICP. Brief hyperventilation remains an immediate option for patients with acute increases in ICP. Prophylactic hyperventilation, or vigorous or prolonged hyperventilation, is not recommended, because the consequent vasoconstriction may excessively decrease cerebral perfusion and oxygenation. Mannitol lowers ICP and may improve survival. Because mannitol induces an osmotic diuresis, it can exacerbate hypovolemia and must be used cautiously. Hypertonic saline may be a more useful agent for control of increased ICP in patients with severe head injury. Neurosurgical consultation is mandatory. If signs of increased ICP persist, the neurosurgeon must decide whether to operate emergently.
Exposure and Environmental Control
All clothing should be cut away to reveal any injuries. Cutting is quickest and minimizes unnecessary patient movement. Children often arrive in the ED mildly hypothermic because of their higher body surface area-to-mass ratios. They can be warmed with use of radiant heat as well as heated blankets and IV fluids.
Secondary Survey
During the secondary survey, the physician completes a detailed, head-to-toe physical examination.
Head Trauma
A GCS or Pediatric GCS score (see Chapter 85 ) should be assigned to every child with significant head trauma. This scale assesses eye opening and motor and verbal responses. In the Pediatric GCS, the verbal score is modified for age. The GCS helps categorize neurologic disability, and serial measurements identify improvement or deterioration over time. Patients with low scores 6-24 hr after injuries have poorer prognosis.
In the ED, cranial CT scanning of the head without a contrast agent has become standard to determine the type of injury in patients with concerning findings. Diffuse cerebral injury with edema is a common and serious finding on CT scan in severely brain-injured children. Focal hemorrhagic lesions (e.g., epidural hematoma) that can be evacuated occur less often but may require immediate neurosurgical intervention (Fig. 82.3 ).
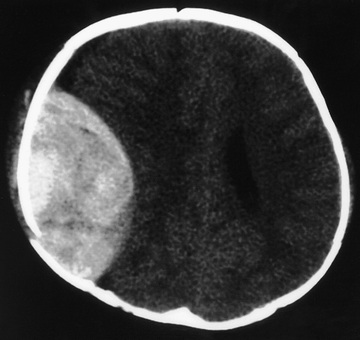
Monitoring of ICP should be strongly considered for children with severe brain injury, particularly for those with a GCS score of ≤8 and abnormal head CT findings (see Chapter 85 ). One advantage of an intraventricular catheter over an intraparenchymal device is that cerebrospinal fluid can be drained to treat acute increases in ICP. Hypoxia, hypercarbia, hypotension, and hyperthermia must be aggressively managed to prevent secondary brain injury. Cerebral perfusion pressure (i.e., the difference between mean arterial blood pressure and mean ICP) should be maintained >40 mm Hg, at least (and an even higher minimum, >50 mm Hg, especially for older children).
A child with a severe brain injury must be treated aggressively in the ED because it is difficult to predict the long-term neurologic outcome.
Cervical Spine Trauma
Cervical spine injuries occur in <3% of children with blunt trauma—with the risk being substantially higher in those with GCS scores ≤8—but they are associated with significant mortality and morbidity. Bony injuries occur mainly from C1 to C4 in children younger than 8 yr. In older children, they occur equally in the upper and lower cervical spine. The mortality rate is significantly higher in patients with upper C-spine injuries. Spinal cord injury without radiographic abnormalities (SCIWORA) on plain films or CT may be present. Patients with SCIWORA have neurologic symptoms, and spinal cord abnormalities are nearly always noted on MRI. Approximately 30% of all patients with C-spine injuries have permanent neurologic deficits.
Evaluation begins with a detailed history and neurologic examination. Identifying the mechanism of injury helps in estimating the likelihood of a C-spine injury. Both the patient and the paramedic should be asked whether any neurologic symptoms or signs, such as weakness or abnormal sensation, were present before arrival in the ED. In a child with neurologic symptoms and normal findings on C-spine plain radiographs and CT scan, SCIWORA must be considered.
Whenever the history, physical examination, or mechanism of injury suggests a C-spine injury, radiographs should be obtained after initial resuscitation. The National Emergency X-Radiography Utilization Study (NEXUS) cervical spine rule helps identify low-risk patients who may not require radiographs (Table 82.5 ). The standard series of plain radiographs includes lateral, anteroposterior (AP), and odontoid views. Some centers use cervical spine CT as the primary diagnostic tool, particularly in patients with abnormal GCS scores and/or significant injury mechanisms, recognizing that CT is more sensitive in detecting bony injury than plain radiographs. CT is also helpful if an odontoid fracture is suspected, because young children typically do not cooperate enough to obtain an open-mouth (odontoid) radiographic view. Use of cervical spine CT scan must be balanced with the knowledge that CT exposes thyroid tissue to 90-200 times the amount of radiation from plain films. MRI is indicated in a child with suspected SCIWORA and in the evaluation of children who remain obtunded.
Rapid diagnosis of spinal cord injury is essential. Initiating high-dose IV methylprednisolone within 8 hr of spinal cord injury has been reported to improve motor outcome, but this treatment has become controversial.
Thoracic Trauma
Pulmonary contusions occur frequently in young children with blunt chest trauma. A child's chest wall is relatively pliable; therefore, less force is absorbed by the rib cage, and more is transmitted to the lungs. Respiratory distress may be noted initially or may develop during the 1st 24 hr after injury.
Rib fractures result from significant external force. They are noted in patients with more severe injuries and are associated with a higher mortality rate. Flail chest, which is caused by multiple rib fractures, is rare in children. Table 82.6 lists indications for operative management in thoracic trauma. (See Table 82.2 for the differential diagnosis of immediately life-threatening cardiopulmonary injuries.)
Abdominal Trauma
Liver and spleen contusions, hematomas, and lacerations account for the majority of intraabdominal injuries from blunt trauma. The kidneys, pancreas, and duodenum are relatively spared because of their retroperitoneal location. Pancreatic and duodenal injuries are more common after a bicycle handlebar impact or a direct blow to the abdomen.
Although a thorough examination for intraabdominal injuries is essential, achieving it often proves difficult. Misleading findings can result from gastric distention after crying or in an uncooperative toddler. Calm reassurance, distraction, and gentle, persistent palpation help with the examination. Important findings include distention, bruises, and tenderness. Specific symptoms and signs give insight into the mechanism of injury and the potential for particular injuries. Pain in the left shoulder may signify splenic trauma. A lap belt mark across the abdomen raises concern for bowel or mesentery injury. The presence of certain other injuries, such as lumbar spinal fractures and femur fractures, increases the likelihood of intraabdominal injury.
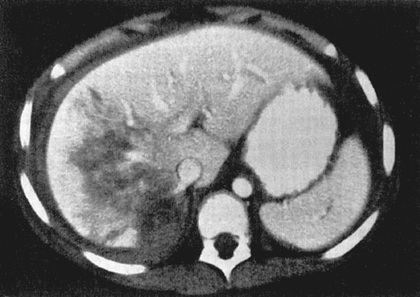
An abdominal (and pelvic) CT scan with IV contrast medium enhancement rapidly identifies structural abnormalities and is the preferred study in a stable child. Negative abdominal CT scan has been shown to have a negative predictive value (NPV) of 99.6%. It has excellent sensitivity and specificity for splenic (Fig. 82.4 ), hepatic (Fig. 82.5 ), and renal injuries, but is less sensitive for diaphragmatic, pancreatic, or intestinal injuries. Small amounts of free fluid or air or a mesenteric hematoma may be the only sign of an intestinal injury. Administration of an oral contrast agent is not routinely recommended for all abdominal CT scans, but it sometimes aids in identifying an intestinal, especially a duodenal, injury.
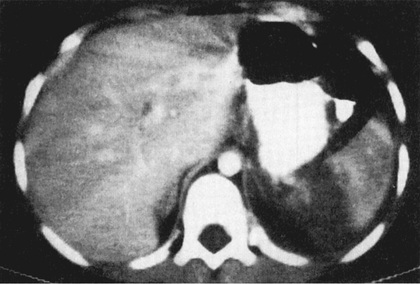
Although the FAST examination helps detect hemoperitoneum, the variably low sensitivity of this test in children suggests that it should not be used alone to exclude intraabdominal injury in patients with a moderate to high pretest probability for injury. A positive FAST exam for hemoperitoneum requires further investigation. Serial FAST exams over time (by a skilled ultrasonographer) may be used to rule out injury in need of intervention. The FAST exam is most clinically useful in patients who have blunt trauma and are hemodynamically unstable or in patients who require operative intervention for nonabdominal injuries, because in these cases the performance of a CT scan may not be feasible.
Nonoperative treatment has become standard for hemodynamically stable children with splenic, hepatic, and renal injuries from blunt trauma. The majority of such children can be treated nonsurgically. In addition to avoiding perioperative complications, nonoperative treatment decreases the need for blood transfusions and shortens hospital stay. When laparotomy is indicated, splenic repair is preferable to splenectomy.
Pelvic Trauma
Pelvic fractures in children are much less common than in adults, occurring in approximately 4% of children with more severe blunt trauma. Pelvic fractures are typically caused by high forces (e.g., high-speed motor vehicle crashes or pedestrian impacts) and are often associated with intraabdominal and/or vascular injuries. The pelvis itself forms a ring, and high-force impacts can lead to disruption of this ring. When the ring is disrupted in >1 location, such as the symphysis pubis and the sacroiliac joint, the ring can become unstable and displaced, potentially injuring large pelvic vessels and leading to massive blood loss. Catheter-directed embolization to control bleeding, performed by an interventional radiologist, may be required.
The pelvis should be assessed for stability by means of compression-distraction maneuvers. If instability is noted, immediate external fixation with a pelvis-stabilizing device or a sheet should be applied and orthopedic consultation sought. A trauma patient with a potential pelvic fracture should receive an AP pelvic radiograph in the trauma bay, or a CT scan, if there is high suspicion of injury. Children without a high-risk clinical finding (i.e., GCS <14; abdominal pain or tenderness; pelvic tenderness, laceration, ecchymosis, or abrasion; gross hematuria or >20 red blood cells/high-power field on urinalysis; or femur fracture) or a high-risk mechanism of injury (i.e., unrestrained motor vehicle collision, motor vehicle collision with ejection, motor vehicle collision rollover, auto vs pedestrian, or auto vs bicycle), however, are unlikely to have pelvic fractures.
Lower Genitourinary Trauma
The perineum should be inspected and the stability of the bones of the pelvis assessed. Urethral injuries are more common in males. Findings suggestive of urethral injury include scrotal or labial ecchymosis, blood at the urethral meatus, gross hematuria, and a superiorly positioned prostate on rectal examination (in an adolescent male). Certain pelvic fractures also increase the risk for potential genitourinary injury. Any of these findings is a contraindication to urethral catheter insertion and warrants consultation with a urologist. Retrograde urethrocystogram and CT scan of the pelvis and abdomen are used to determine the extent of injury.
Extremity Trauma
Thorough examination of the extremities is essential because extremity fractures are among the most frequently overlooked injuries in children with multiple trauma. All limbs should be inspected for deformity, swelling, and bruises; palpated for tenderness; and assessed for active and passive range of motion, sensory function, and perfusion.
Before radiographs are obtained, suspected fractures and dislocations should be immobilized and an analgesic administered. Splinting a femur fracture helps alleviate pain and may decrease blood loss. An orthopedic surgeon should be consulted immediately to evaluate children with compartment syndrome, neurovascular compromise, open fracture, or most traumatic amputations.
Radiologic and Laboratory Evaluation
Most authorities recommend ordering multiple laboratory tests (e.g., complete blood cell count, electrolytes, glucose, blood urea nitrogen, creatinine, liver function tests, amylase, lipase, lactate, blood gas, prothrombin and partial thromboplastin times, type and cross-match, urinalysis) and x-ray films (e.g., lateral C-spine, AP chest, AP pelvis) in the ED. One benefit of standardizing the evaluation of patients with major trauma is that fewer decisions need to be made on an individual basis, possibly expediting ED management. Some of these studies have prognostic importance. A large base deficit is associated with a higher mortality rate, and elevated lactate values correlate with poor prognosis.
There are some limitations in standard tests. The lateral cervical spine radiograph can miss clinically significant injuries. Hemoglobin and hematocrit values provide baseline values in the ED, but they may not have yet equilibrated after a hemorrhage. Abnormal liver function test results or elevated serum amylase and lipase values may be noted in patients with significant abdominal trauma, but most patients with significant trauma to the abdomen already have clinical indications for CT scanning or surgery. The majority of previously healthy children have normal coagulation profiles; these may become abnormal after major head trauma. Although routine urinalysis or dipstick urine testing for blood has been recommended for children, other data suggest that this evaluation may be unnecessary in patients without gross hematuria, hypotension, or other associated abdominal injuries.
Clinical prediction rules that combine patient history with physical examination findings have been developed to identify those at low risk of injury for whom specific radiographic and laboratory studies may not be necessary. The NEXUS C-spine rule is a sensitive, easily applicable rule that was validated for adults and children, although there were fewer young patients studied (see Table 82.5 ). Several clinical prediction rules have been developed to identify children at low risk of traumatic brain injury (Table 82.7 ). Another clinical prediction rule has been developed to identify children at very low risk of clinically important intraabdominal injuries following blunt trauma (Table 82.8 ). Although this rule has an NPV of 99.9%, it needs to be externally validated before widespread implementation.
Psychological and Social Support
Serious multisystem trauma may result in significant long-term psychological and social difficulties for the child and family, particularly when there is a major head injury. Like adults, children are at risk for depressive symptoms and posttraumatic stress disorder. Caregivers face persistent stress and have been noted to have more psychological symptoms. Psychological and social support, during the resuscitation period and afterward, is extremely important. Parents often prefer to be offered the choice to be present during resuscitations. A member of the resuscitation team should be made responsible for answering the family's questions and supporting them in the trauma room.