Respiratory Distress and Failure
Ashok P. Sarnaik, Jeff A. Clark, Sabrina M. Heidemann
The term respiratory distress is used to indicate signs and symptoms of abnormal respiratory pattern. A child with nasal flaring, tachypnea, chest wall retractions, stridor, grunting, dyspnea, and wheezing has respiratory distress. Taken together, the magnitude of these findings is used to judge clinical severity. Nasal flaring is nonspecific, but the other signs are useful in localizing the site of pathology (see Chapter 400 ). Respiratory failure is defined as inability of the lungs to provide sufficient oxygen (hypoxic respiratory failure) or remove carbon dioxide (ventilator failure) to meet metabolic demands. Therefore, whereas respiratory distress is determined by a clinical impression, the diagnosis of respiratory failure is indicated by inadequacy of oxygenation or of ventilation, or both. Respiratory distress can occur in patients without respiratory disease, and respiratory failure can occur in patients without respiratory distress.
Respiratory Distress
A careful physical examination must be performed when managing a child in respiratory distress. Nasal flaring , although nonspecific, is an extremely important sign of distress in infants. It may indicate discomfort, pain, fatigue, or breathing difficulty. The state of responsiveness is another crucial sign. Lethargy, disinterest in surroundings, and poor cry are suggestive of exhaustion, hypercarbia, and impending respiratory failure. Abnormalities of the rate and depth of breathing can occur with both pulmonary and nonpulmonary causes of respiratory distress. In diseases of decreased lung compliance, such as pneumonia and pulmonary edema, breathing is characteristically rapid and shallow (decreased tidal volume). In obstructive airway diseases, such as asthma and laryngotracheitis, breathing is deep with increased tidal volume, but less rapid. Rapid and deep breathing without other respiratory signs should alert the physician to possible nonpulmonary or nonthoracic causes of respiratory distress, such as response to metabolic acidosis (e.g., diabetic ketoacidosis, renal tubular acidosis) or stimulation of the respiratory center (e.g., encephalitis, ingestion of central nervous system stimulants). Chest wall, suprasternal, and subcostal retractions are manifestations of increased inspiratory effort, weak chest wall, or both. Inspiratory stridor indicates airway obstruction above the thoracic inlet, whereas expiratory wheezing results from airway obstruction below the thoracic inlet. Grunting is most commonly heard in diseases with decreased functional residual capacity (e.g., pneumonia, pulmonary edema) and peripheral airway obstruction (e.g., bronchiolitis).
Respiratory Disease Manifesting as Respiratory Distress
Clinical examination is important in localizing the site of pathology (see Chapter 400 ). Extrathoracic airway obstruction occurs anywhere above the thoracic inlet. Inspiratory stridor, suprasternal, chest wall, and subcostal retractions; and prolongation of inspiration are hallmarks of extrathoracic airway obstruction. By comparison, features of intrathoracic airway obstruction are prolongation of expiration and expiratory wheezing. Typical manifestations of alveolar interstitial pathology are rapid, shallow respirations, chest wall retractions, and grunting. The site of pathology can be localized and the differential diagnosis established on the basis of the clinical signs and symptoms (Tables 89.1 and 89.2 ).
Table 89.1
Typical Localizing Signs for Pulmonary Pathology
| SITE OF PATHOLOGY | RESPIRATORY RATE | RETRACTIONS | AUDIBLE SOUNDS |
|---|---|---|---|
| Extrathoracic airway | ↑ | ↑↑↑↑ | Stridor |
| Intrathoracic extrapulmonary | ↑ | ↑↑ | Wheezing |
| Intrathoracic intrapulmonary | ↑↑ | ↑↑ | Wheezing |
| Alveolar interstitial | ↑↑↑ | ↑↑↑ | Grunting |
Table 89.2
Examples of Anatomic Sites of Lesions Causing Respiratory Failure
| LUNG | RESPIRATORY PUMP |
|---|---|
| CENTRAL AIRWAY OBSTRUCTION | THORACIC CAGE |
| PERIPHERAL AIRWAY OBSTRUCTION | BRAINSTEM |
| ALVEOLAR-INTERSTITIAL DISEASE | SPINAL CORD |
| NEUROMUSCULAR | |
ARDS, Acute respiratory distress syndrome; CNS, central nervous system.
Respiratory Distress Without Respiratory Disease
Although respiratory distress most frequently results from diseases of lungs, airways, and chest wall, pathology in other organ systems can manifest as respiratory distress and lead to misdiagnosis and inappropriate management (Table 89.3 ). Respiratory distress resulting from heart failure or diabetic ketoacidosis may be misdiagnosed as asthma and improperly treated with albuterol, resulting in worsened hemodynamic state or ketoacidosis. Careful history and physical examination provide essential clues in avoiding misdiagnosis.
Table 89.3
Nonpulmonary Causes of Respiratory Distress
| SYSTEM | EXAMPLE(S) | MECHANISM(S) |
|---|---|---|
| Cardiovascular | ||
| Central nervous | Stimulation of brainstem respiratory centers | |
| Metabolic | Stimulation of central and peripheral chemoreceptors | |
| Renal | Renal tubular acidosis | Stimulation of central and peripheral chemoreceptors |
| Hypertension | Left ventricular dysfunction → increased pulmonary blood/water content | |
| Sepsis |
Cardiovascular Disease Manifesting as Respiratory Distress
A child with cardiovascular pathology may present with respiratory distress caused by either decreased lung compliance or cardiogenic shock (Table 89.4 ). Diseases that result in increased pulmonary arterial blood flow (e.g., left-to-right shunts) or increased pulmonary venous pressure (e.g., left ventricular dysfunction from hypertension or myocarditis, obstructed total anomalous pulmonary venous return) cause an increase in pulmonary capillary pressure and transudation of fluid into the pulmonary interstitium and alveoli. The increased pulmonary blood and water content lead to decreased lung compliance and result in rapid shallow breathing.
It is important to recognize that interstitial lung edema cannot only manifest as alveolar fluid, but as small airway obstruction as well. Wheezing as a sign of congestive cardiac disease is common in infants and young children and should be recognized. Patients with cardiac lesions, resulting in low cardiac output, often present in shock. For example, obstructive lesions of left side of the heart and acquired or congenital cardiomyopathy result in decreased perfusion and metabolic acidosis, as well as respiratory distress because of chemoreceptor and baroreceptor stimulation. The likelihood of a particular cardiovascular illness manifesting as respiratory distress depends on age at presentation (Table 89.5 ).
Table 89.5
Typical Chronology of Heart Disease Presentation in Children
| AGE | MECHANISM | DISEASE |
|---|---|---|
| Newborn (1-10 days) | ↑ Arteriovenous pressure difference | Arteriovenous fistula (brain, liver) |
| Ductal closure | Single ventricle lesions or severe ventricular outflow obstruction | |
| Independent pulmonary and systemic blood flow | Transposition of the great arteries | |
| Pulmonary venous obstruction | Total anomalous pulmonary venous return (TAPVR) | |
| Young infant (1-6 mo) | ↓ Pulmonary vascular resistance | Left-to-right shunt |
| ↓ Pulmonary artery pressure | Anomalous left coronary artery to the pulmonary artery | |
| Any age | Rate disturbance | Tachy- or bradyarrhythmias |
| Infection | Myocarditis, pericarditis | |
| Abnormal cardiac myocytes | Cardiomyopathy | |
| Excess afterload | hypertension |
Neurologic Disease Manifesting as Respiratory Distress
Central nervous system (CNS) dysfunction can lead to alterations in respiratory patterns and manifest as respiratory distress. Increased intracranial pressure (ICP) may manifest as respiratory distress. Early rise in intracranial pressure (ICP) results in stimulation of respiratory centers, leading to increases in the rate (tachypnea ) and depth (hyperpnea ) of respiration. The resultant decrease in arterial blood partial pressure of carbon dioxide (PaCO 2 ) and elevation of cerebrospinal fluid (CSF) pH lead to cerebral vasoconstriction and amelioration of intracranial hypertension. Stereotypical respiratory patterns are associated with dysfunction at multiple levels of the brain. Cerebral hemisphere and midbrain lesions result in hyperpnea as well as tachypnea. In such situations, arterial blood gas (ABG) measurements typically show respiratory alkalosis without hypoxemia. Pathology affecting the pons and medulla manifests as irregular breathing patterns such as apneustic breathing (prolonged inspiration with brief expiratory periods), Cheyne-Stokes breathing (alternate periods of rapid and slow breathing), and irregular, ineffective breathing or apnea (Table 89.6 ). Along with respiratory changes, other manifestations of CNS dysfunction and increased ICP may be present, such as focal neurologic signs, pupillary changes, hypertension, and bradycardia (see Chapter 85 ). Occasionally, severe CNS dysfunction can result in neurogenic pulmonary edema and respiratory distress, which may follow excessive sympathetic discharge resulting in increased pulmonary venous hydrostatic pressure as well as increased pulmonary capillary permeability. Central neurogenic hyperventilation is characteristically observed in CNS involvement by illnesses such as urea cycle defects and encephalitis. Bradycardia and apnea may be caused by CNS-depressant medications, poisoning, prolonged hypoxia, trauma, or infection (see Table 89.2 ).
Table 89.6
| INJURY | PATTERN* | COMMENTS |
|---|---|---|
| Normal | 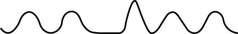
|
Variable VT with normal respiratory pauses and sighs |
| Cortex | 
|
Hyperpnea and tachypnea |
| Midbrain | 
|
Cheyne-Stokes breathing : Gradually increasing and decreasing VT |
| Pons | 
|
Apneustic breathing : Prolonged inspiration followed by prolonged expiration |
| Medulla and pons | 
|
Biot's breathing : Rapid and irregular respirations with pauses |
* Lung volume vs time.
VT , Tidal volume.
Toxic Metabolic States Manifesting as Respiratory Distress
Direct stimulation of respiratory centers resulting in respiratory alkalosis is encountered in intoxication involving agents such as salicylates and theophylline. Similarly, intoxication with general CNS stimulants, such as cocaine and amphetamines, may result in increased respiration. Presence of endogenous and exogenous toxins, such as organic acidemias, ingestion of methanol and ethylene glycol, and late stages of salicylism, cause metabolic acidosis and compensatory hyperventilation, which can manifest as respiratory distress. ABG measurements show decreased pH and compensatory hypocarbia with normal oxygenation. Metabolic disorders causing hyperammonemia, on the other hand, cause respiratory alkalosis (decreased PaCO 2 with increased pH) because ammonia stimulates the respiratory centers. Carbon monoxide and cyanide poisoning or methemoglobinemia may produce respiratory distress.
Other Nonpulmonary Entities Manifesting as Respiratory Distress
Sepsis and septic shock may cause an acute respiratory distress syndrome (ARDS) with hypovolemic stimulation of baroreceptors, cytokine stimulation of respiratory centers, and lactic acidosis. Other indirect causes of lung injury include systemic inflammatory conditions, trauma, transfusion-related acute lung injury, and pancreatitis. Similarly, renal disease may manifest as respiratory distress by causing metabolic acidosis (e.g., renal tubular acidosis or renal failure) or hypertensive left ventricular failure and fluid overload.
Respiratory Failure
Respiratory failure occurs when oxygenation and ventilation are insufficient to meet the metabolic demands of the body. Respiratory failure may result from an abnormality in (1) lung and airways, (2) chest wall and muscles of breathing, or (3) central and peripheral chemoreceptors. Clinical manifestations depend largely on the site of pathology. Although respiratory failure is traditionally defined as respiratory dysfunction resulting in arterial partial pressure of oxygen (PaO 2 ) <60 mm Hg when breathing room air and PaCO 2 >50 mm Hg resulting in acidosis, the patient's general state, respiratory effort, and potential for impending exhaustion are more important indicators than ABG values.
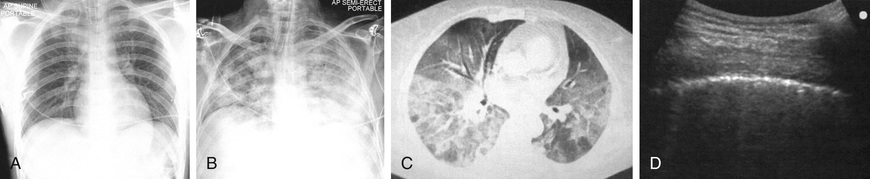
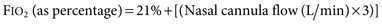
The Berlin definition of ARDS was once used to describe pediatric patients with ARDS, even though the pathophysiology is different between children and adults. The current pediatric definition differs in chest imaging findings, definition of oxygenation, consideration of both noninvasive and invasive mechanical ventilation, and consideration of special populations (Table 89.7 and Fig. 89.1 ).
Table 89.7
Pediatric Acute Respiratory Distress Syndrome (PARDS) Definition
| BERLIN DEFINITION | PARDS | |
|---|---|---|
| Age | Adults and children | Excludes patients with perinatal-related lung disease |
| Timing | Within 1 wk of known clinical insult or new or worsening respiratory symptoms | Within 1 wk of a known clinical insult |
| Origin of edema | Respiratory failure not fully explained by cardiac failure or fluid overload. Need objective assessment (e.g., echocardiography) to exclude hydrostatic edema, even if no risk factor present. | Respiratory failure not fully explained by cardiac failure or fluid overload |
| Chest imaging a | Bilateral opacities not fully explained by effusions, lobar/lung collapse, or nodules. (Illustrative clinical cases and chest radiographs have been provided.) | Chest imaging findings of new infiltrate(s) consistent with acute pulmonary parenchymal disease |
| Oxygenation b | ||
| Mild | 200 mm Hg < PaO 2 /FIO 2 ≤300 mm Hg with PEEP, or CPAP ≥5 cm H2 O c |
Noninvasive mechanical ventilation: PARDS (No severity stratification) Full face-mask bilevel ventilation or CPAP >5 cm H2 O e SF ratio <264 d Invasive mechanical ventilation f : |
| Moderate | 100 mm Hg < PaO 2 /FIO 2 ≤200 mm Hg with PEEP ≥5 cm H2 O | |
| Severe | PaO 2 /FIO 2 <100 mm Hg with PEEP ≥5 cm H2 O | |
a Chest radiograph or CT scan in Berlin criteria only.
b If altitude is >1,000 m, the correction factor should be calculated as follows: PaO 2 /FIO 2 × Barometric pressure/760.
c This may be delivered noninvasively in the mild acute respiratory distress syndrome group.
d Use PAO 2 -based metric when available. If PaO 2 not available, wean FIO 2 to maintain SpO 2 <97% to calculate OSI or SF ratio.
e For nonintubated patients treated with supplemental oxygen or nasal modes of noninvasive ventilation, refer to reference below for “At Risk Criteria.”
f ARDS severity groups stratified by OI or OSI should not be applied to children with chronic lung disease who normally receive invasive mechanical ventilation or children with cyanotic heart disease.
In addition to the above, the Pediatric Acute Lung Injury Consensus Conference Group added definitions for special populations, including cyanotic heart disease, chronic lung disease, and left ventricular function.
CPAP, Continuous positive airway pressure; FIO 2 , fraction of inspired oxygen; PaO 2 , partial pressure of arterial oxygen; PEEP, positive end-expiratory pressure. OI, oxygenation index; OSI, oxygen saturation index.
Adapted from Pediatric Acute Lung Injury Consensus Conference Group, Pediatric Acute Respiratory Distress Syndrome: Consensus recommendations from the Pediatric Acute Lung Injury Consensus Conference, Pediatr Crit Care Med 16;428–439, 2015.
Pathophysiology
Respiratory failure can be classified into hypoxic respiratory failure (failure of oxygenation) and hypercarbic respiratory failure (failure of ventilation). Systemic venous (pulmonary arterial) blood is arterialized after equilibration with alveolar gas in the pulmonary capillaries and is carried back to the heart by pulmonary veins. The ABG is influenced by the composition of inspired gas, effectiveness of alveolar ventilation, pulmonary capillary perfusion, and diffusion capacity of the alveolar capillary membrane. Abnormality in any of these steps can result in respiratory failure. Hypoxic respiratory failure results from intrapulmonary shunting and venous admixture or insufficient diffusion of oxygen from alveoli into pulmonary capillaries. This physiology can be caused by small airways obstruction, increased barriers to diffusion (e.g., interstitial edema, fibrosis), and conditions in which alveoli are collapsed or filled with fluid (e.g., ARDS, pneumonia, atelectasis, pulmonary edema). In most cases, hypoxic respiratory failure is associated with decreased functional residual capacity and can be managed by lung volume recruitment with positive pressure ventilation. Hypercarbic respiratory failure is caused by decreased minute ventilation (i.e., tidal volume multiplied by respiratory rate). This physiology can result from centrally mediated disorders of respiratory drive, increased dead space ventilation, or obstructive airways disease. Hypoxic and hypercarbic respiratory failure may coexist as a combined failure of oxygenation and ventilation.
Ventilation-Perfusion Mismatch
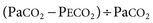
For exchange of O2 and CO2 to occur, alveolar gas must be exposed to blood in pulmonary capillaries. Both ventilation and perfusion are lower in nondependent areas of the lung and higher in dependent areas. The difference in perfusion (Q̇) is greater than the difference in ventilation (V̇). Perfusion in excess of ventilation results in incomplete arterialization of systemic venous (pulmonary arterial) blood and is referred to as venous admixture . Perfusion of unventilated areas is referred to as intrapulmonary shunting of systemic venous blood to systemic arterial circulation. Conversely, ventilation that is in excess of perfusion is wasted; that is, it does not contribute to gas exchange and is referred to as dead space ventilation . Dead space ventilation results in return of greater amounts of atmospheric gas (which has not participated in gas exchange and has negligible CO2 ) back to the atmosphere during exhalation. The respiratory dead space is divided into the anatomic dead space and the alveolar dead space. The anatomic dead space includes the conducting airways from the nasopharynx to the terminal bronchioles, ends at the alveoli, and has no contact with the pulmonary capillary bed. The alveolar dead space refers to areas of the lung where alveoli are ventilated but not perfused. Under normal conditions, this physiology usually occurs in West zone I, where alveolar pressure is greater than pulmonary capillary pressure. Under clinical conditions, this physiology may result from dynamic hyperinflation, high levels of positive end-expiratory pressure (PEEP), or large tidal volume in ventilated patients. Additionally, decreased pulmonary artery perfusion from pulmonary embolism or decreased cardiac output and hypovolemia can result in alveolar dead space. The end result is a decrease in mixed expired CO2 (PECO 2 ) and an increase in the PaCO 2 – PECO 2 gradient. Dead space as a fraction of tidal volume (VD /VT ) is calculated as:
Normal VD /VT is approximately 0.33. Venous admixture and intrapulmonary shunting predominantly affect oxygenation, resulting in a alveolar oxygen (PAO 2 ) to PaO 2 (A-aO 2 ) gradient without elevation in PaCO 2 . This physiology is caused by greater ventilation of perfused areas, which is sufficient to normalize PaCO 2 but not PaO 2 because of their respective dissociation curves. The relative straight-line relationship of the hemoglobin-CO2 dissociation allows for averaging of capillary PCO 2 (PcCO 2 ) from hyperventilated and hypoventilated areas. Because the association between oxygen tension and hemoglobin saturation plateaus with increasing PaO 2 , the decreased hemoglobin-O2 saturation in poorly ventilated areas cannot be compensated for by well-ventilated areas where hemoglobin-O2 saturation has already reached near-maximum. This physiology results in decreased arterial oxyhemoglobin saturation (SaO 2 ) and PaO 2 . Elevation of PaCO 2 in such situations is indicative of coincident alveolar hypoventilation. Examples of diseases leading to venous admixture include asthma and aspiration pneumonia, and those of intrapulmonary shunt include lobar pneumonia and ARDS.
Diffusion
Even if ventilation and perfusion are matched, gas exchange requires diffusion across the interstitial space between alveoli and pulmonary capillaries. Under normal conditions, there is sufficient time for the pulmonary capillary blood to equilibrate with alveolar gas across the interstitial space. When the interstitial space is filled with inflammatory cells or fluid, diffusion is impaired. Because the diffusion capacity of CO2 is 20 times greater than that of O2 , diffusion defects manifest as hypoxemia rather than hypercarbia. Even with the administration of 100% oxygen, PAO 2 increases to approximately 660 mm Hg from 100 mm Hg at sea level, and the concentration gradient for diffusion of O2 is increased by only 6.6 times. Therefore, with diffusion defects, lethal hypoxemia will set in before clinically significant CO2 retention results. In fact, in such situations, PaCO 2 is often decreased because of the hyperventilation that accompanies hypoxemia. Presence of hypercarbia in diseases that impair diffusion is indicative of alveolar hypoventilation from coexisting airway obstruction, exhaustion, or CNS depression. Examples of disease that impair diffusion are interstitial pneumonia, ARDS, scleroderma, and pulmonary lymphangiectasia.
Monitoring a Child in Respiratory Distress and Respiratory Failure
Clinical Examination
It cannot be overemphasized that clinical observation is the most important component of monitoring. The presence and magnitude of abnormal clinical findings, their progression with time, and their temporal relation to therapeutic interventions serve as guides to diagnosis and management (see Chapter 400 ). As much as possible, the child with respiratory distress or failure should be observed in the position of greatest comfort and in the least threatening environment.
Pulse oximetry is the most commonly used technique to monitor oxygenation. Noninvasive and safe, it is the standard of care in bedside monitoring of children during transport, procedural sedation, surgery, and critical illness. It indirectly measures arterial hemoglobin-O2 saturation by differentiating oxyhemoglobin from deoxygenated hemoglobin using their respective light absorption at wavelengths of 660 nm (red) and 940 nm (infrared). A pulsatile circulation is required to enable detection of oxygenated blood entering the capillary bed. Percentage of arterial oxyhemoglobin is reported as SaO 2 ; however, the correct description is oxyhemoglobin saturation as measured by pulse oximetry (SpO 2 ). Such precision is needed because SpO 2 may not always reflect SaO 2 . It is important to be familiar with the hemoglobin-O2 dissociation curve (see Chapter 400 ) to estimate PaO 2 at a given oxyhemoglobin saturation. Because of the shape of the hemoglobin-O2 dissociation curve, changes in PaO 2 above 70 mm Hg are not readily identified by pulse oximetry. Also, at the same PaO 2 , there may be significant change in SpO 2 at a different blood pH value. In most situations, SpO 2 >95% is a reasonable goal, especially in emergency care. In some adult studies of ARDS, the recommended saturation is 94–96% to avoid oxygen toxicity. There are exceptions, such as in patients with single-ventricle cardiac lesions, in whom the pulmonary and systemic circulations are receiving blood flow from the same ventricle (e.g., after Norwood procedure for hypoplastic left heart syndrome), or with large left-to-right shunts (e.g., ventricular septal defect, patent ductus arteriosus). In these types of pathophysiologic situations, a lower SpO 2 is desired to avoid excessive blood flow to the lungs and pulmonary edema from the pulmonary vasodilatory effects of oxygen, in the patient with a single ventricle, diverting blood flow away from the systemic circulation. Because most commercially available pulse oximeters recognize all types of hemoglobin as either oxyhemoglobin or deoxygenated hemoglobin, they provide inaccurate information in the presence of carboxyhemoglobin and methemoglobin. In carbon monoxide poisoning, carboxyhemoglobin absorbs light in the same (red) wavelength as oxyhemoglobin, leading to overestimation of oxygen saturation. Methemoglobin absorbs light in both the oxygenated and deoxygenated wavelengths, which can cause either an overestimation or underestimation of oxygen saturation. Data suggest that increasing methemoglobin concentrations tend to drive SpO 2 toward 85%, no matter the actual percent of oxyhemoglobin. At lower methemoglobin levels, the pulse oximetry reading is falsely low, whereas high levels lead to a falsely high pulse oximetry reading. Newer pulse oximeters may have the ability to distinguish dyshemoglobinemias and to prevent false readings, but these are not currently in widespread use. It should be recognized that dangerous levels of hypercarbia may exist in patients with ventilatory failure, who have satisfactory SpO 2 if they are receiving supplemental oxygen. Pulse oximetry should not be the only monitoring method in patients with primary ventilatory failure, such as neuromuscular weakness and CNS depression. It is also unreliable in patients with poor perfusion and poor pulsatile flow to the extremities. Despite these limitations, pulse oximetry is a noninvasive, easily applicable, and effective means of evaluating the percentage of oxyhemoglobin in most patients.
Volumetric capnography (end-tidal CO2 [PetCO 2 ] measurement) is helpful in non-invasively determining the effectiveness of ventilation and pulmonary circulation. The PetCO 2 can be used to determine the alveolar dead space fraction and is calculated as follows: [(PaCO 2 − PetCO 2 )/PaCO 2 ]. Changes in the alveolar dead space fraction usually correlate well with changes in the gradient of PaCO 2 and PetCO 2 (PaCO 2 – PetCO 2 ). Thus a change in PaCO 2 – PetCO 2 can be used as an index of changes in alveolar dead space. In healthy children the gradient is smaller than in adults and is usually <3 mm Hg. Diseases resulting in increased alveolar dead space (e.g., dynamic hyperinflation) or decreased pulmonary blood flow (e.g., pulmonary embolism, low cardiac output) lead to decreases in PetCO 2 and an increase in PaCO 2 – PetCO 2 . PetCO 2 alone may overestimate adequacy of ventilation.
Blood Gas Abnormalities
Arterial blood gas analysis offers valuable assistance in diagnosis, monitoring, and management of a child in respiratory distress and failure. Because of technical difficulties in obtaining an arterial sample in children, a capillary blood gas (CBG) sample is most often obtained in emergency situations. A properly arterialized CBG sample obtained by warming the digit and obtaining free-flowing blood is acceptable. The blood sample needs to be processed without delay. CBG provides a good estimate of PaCO 2 and arterial pH, but less so for PaO 2 . In patients who mainly require monitoring of ventilation (especially those whose oxygenation is being monitored with pulse oximetry) a venous blood gas sample provides reliable estimate of arterial pH and PaCO 2 values, provided tissue perfusion is reasonably adequate. Venous PCO 2 (PvCO 2 ) is approximately 6 mm Hg higher and pH approximately 0.03 lower than the arterial values. PvO 2 has a poor correlation with PaO 2 . Mixed venous O2 saturation obtained from a central venous catheter in the right atrium is an excellent marker of the balance between oxygen delivery and oxygen consumption. In patients with a constant arterial O2 content and O2 consumption, mixed venous O2 saturation offers valuable information about cardiac output.
Blood gas analysis is important not only for determining the adequacy of oxygenation and ventilation but also for determining site of respiratory pathology and planning treatment (see Chapter 400 ). Briefly, in the presence of pure alveolar hypoventilation (e.g., airway obstruction above carina, decreased CO2 responsiveness, neuromuscular weakness), the blood gas will show respiratory acidosis with an elevated PaCO 2 but a relative sparing of oxygenation. V̇/Q̇ mismatch (peripheral airway obstruction, bronchopneumonia) will be reflected in increasing hypoxemia and variable levels of PaCO 2 (low, normal, high) depending on severity of disease. Intrapulmonary right-to-left shunting and diffusion defects (alveolar-interstitial diseases such as pulmonary edema, ARDS) will be associated with a large A-aO 2 gradient and hypoxemia with relative sparing of CO2 elimination, unless there is coincident fatigue or CNS depression.
Acid-Base Abnormalities
It is crucial to analyze the magnitude and appropriateness of changes in pH, PaCO 2 , and bicarbonate concentration ([HCO3 − ]) because they provide useful clues to the underlying pathophysiology and presence of more than 1 disorder. To do so, it is useful to assume baseline values of pH 7.40, PaCO 2 40 mm Hg, and [HCO3 − ] 24 mEq/L. Newborns have lower renal threshold for bicarbonate and therefore have slightly different baseline values of pH 7.38, PaCO 2 35 mm Hg, and [HCO3 − ] 20 mEq/L.
Metabolic Acidosis With Respiratory Compensation
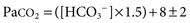
Patients with metabolic acidosis have decreased pH resulting from decreased serum [HCO3 − ]. Chemoreceptor stimulation results in hyperventilation and respiratory compensation that may clinically manifest as respiratory distress. Normal compensation does not completely correct the pH but rather minimizes a change in pH that would otherwise occur without compensation. The adequacy of respiratory compensation is judged by the extent of the decline in PaCO 2 in response to the decline in [HCO3 − ] or pH. A normal compensation for metabolic acidosis results in a fall in PaCO 2 by 1.2 mm Hg for every 1 mEq/L fall in [HCO3 − ]. The most commonly used method to analyze the adequacy of respiratory compensation is Winter's formula:
A quick method is to look at the last 2 digits of pH (provided it is not <7.10), which should be within 2 mm Hg of PaCO 2 . For example, pH 7.27, PaCO 2 26 mm Hg, and [HCO3 − ] 12 mEq/L represents metabolic acidosis with a normal respiratory compensation response. On the other hand, pH 7.15, PaCO 2 30 mm Hg, and [HCO3 − ] 10 mEq/L constitutes metabolic acidosis with inadequate respiratory compensation. The reasons for inadequate compensation include decreased CO2 responsiveness (e.g., narcotic poisoning, cerebral edema), abnormalities of lungs and airways, or neuromuscular weakness. A decrease in PaCO 2 that is greater than what could be expected as a normal compensatory response to metabolic acidosis is indicative of a mixed disorder. A pH 7.20, PaCO 2 15 mm Hg, and [HCO3 − ] 7.5 mEq/L represents metabolic acidosis with a concomitant respiratory alkalosis because the decline in PaCO 2 is greater than what can be expected as normal compensation. Combination of metabolic acidosis and respiratory alkalosis is often encountered in serious conditions such as cardiogenic shock (e.g., anxiety, stimulation of baroreceptors), sepsis, or toxic-metabolic states (e.g., salicylates, organic acidemia).
Respiratory Acidosis With Metabolic Compensation
Patients with respiratory acidosis have decreased pH as a result of elevated PaCO 2 . An acute increase in PaCO 2 of 10 mm Hg results in a decrease in pH by 0.08. Thus a child with severe status asthmaticus and a PaCO 2 of 60 mm Hg will have blood pH of approximately 7.24. Chronically elevated (>3-5 days) PaCO 2 is accompanied by renal compensation and increase in serum [HCO3 − ], limiting the fall in pH to 0.03 for every 10 mm Hg rise in PaCO 2 . Thus an infant with bronchopulmonary dysplasia who has a basal PaCO 2 of 60 mm Hg will have blood pH of approximately 7.34. These findings are helpful in distinguishing acute from chronic changes in PaCO 2 . Also, for a given level of CO2 accumulation, a decrease in pH that is greater than expected is indicative of concomitant metabolic acidosis, and a decline in pH that is less than expected is caused by accompanying metabolic alkalosis.
Assessment of Oxygenation and Ventilation Deficits
For standardizing management, following clinical progress, and determining prognosis for patients with defects in oxygenation or ventilation, the following indicators have been proposed, each with its strengths and limitations:
- A-aO 2 gradient is calculated by the subtraction, PAO 2 − PaO 2 . For the comparison to be valid, both values must be taken at the same time and with the same fraction of oxygen in the inspired gas (FIO 2 ).
- PaO 2 /FIO 2 ratio (P/F) is calculated by dividing PaO 2 by FIO 2 . In hypoxic respiratory failure, a PaO 2 /FIO 2 value <300 mm Hg is consistent with acute lung injury, and a value <200 mm Hg is consistent with ARDS. Although the intent is to measure V̇/Q̇ mismatch, intrapulmonary shunt, and diffusion defect, the status of alveolar hypoventilation could have a significant impact on PaO 2 /FIO 2 .
- SpO 2 /FIO 2 ratio is a surrogate measure of oxygenation when PaO 2 is not available. It is calculated by dividing the pulse oximeter saturation by the FIO 2 . P/F ratios of 200 mm Hg and 300 mm Hg correlate approximately with S/F ratios of 235 and 315 respectively. This relationship is most valid for SpO 2 values between 80% and 97%.
- PaO 2 /PAO 2 ratio is determined by dividing PaO 2 by PAO 2 . The level of alveolar ventilation is accounted for in the calculation of PaO 2 . Therefore, PaO 2 /PAO 2 is more indicative of V̇/Q̇ mismatch and alveolar capillary integrity.
-
Oxygenation index
(OI) is aimed at standardizing oxygenation to the level of therapeutic interventions, such as mean airway pressure (MAP) and FIO
2
used during mechanical ventilation, which are directed toward improving oxygenation. None of the indicators of oxygenation mentioned above takes into account the degree of positive pressure respiratory support.
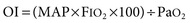
The limitation of OI is that level of ventilation is not accounted for in the assessment. -
Ventilation index
(VI) is aimed at standardizing alveolar ventilation to the level of therapeutic interventions, such as peak inspiratory pressure (PIP), positive end-expiratory pressure (PEEP), and ventilator rate ([R) directed toward lowering PaCO
2
.

Management
The goal of management for respiratory distress and respiratory failure is to ensure a patent airway and provide necessary support for adequate oxygenation of the blood and removal of CO2 . Compared with hypercapnia, hypoxemia is a life-threatening condition; therefore initial therapy for respiratory failure should be aimed at ensuring adequate oxygenation.
Oxygen Administration
Supplemental oxygen administration is the least invasive and most easily tolerated therapy for hypoxemic respiratory failure. Nasal cannula oxygen provides low levels of oxygen supplementation and is easy to administer. Oxygen is humidified in a bubble humidifier and delivered via nasal prongs inserted in to the nares. In children, a flow rate <5 L/min is most often used because of increasing nasal irritation with higher flow rates. A common formula for an estimation of the FIO 2 during use of a nasal cannula in older children and adults follows:
The typical FIO 2 value (expressed as percentage rather than fraction of 1) using this method is between 23% and 40%, although the FIO 2 varies according to the size of the child, the respiratory rate, and the volume of air moved with each breath. In a young child, because typical nasal cannula flow rates are a greater percentage of total minute ventilation, significantly higher FIO 2 may be provided. Alternately, a simple mask may be used, which consists of a mask with open side ports and a valveless oxygen source. Variable amounts of room air are entrained through the ports and around the side of the mask, depending on the fit, size, and minute volume of the child. Oxygen flow rates vary from 5-10 L/min, yielding typical FIO 2 values (expressed as percentage rather than fraction of 1) between 30% and 65%. If more precise delivery of oxygen is desired, other mask devices should be used.
A Venturi mask provides preset FIO 2 through a mask and reservoir system by entraining precise flow rates of room air into the reservoir along with high-flow oxygen. The adapter at the end of each mask reservoir determines the flow rate of entrained room air and the subsequent FIO 2 . (Adapters provide FIO 2 of 0.30-0.50.) Oxygen flow rates of 5-10 L/min are recommended to achieve the desired FIO 2 and to prevent rebreathing. Partial rebreather and non-rebreather masks use a reservoir bag attached to a mask to provide higher FIO 2 . Partial rebreather masks have 2 open exhalation ports and contain a valveless oxygen reservoir bag. Some exhaled gas can mix with reservoir gas, although most exhaled gas exits the mask via the exhalation ports. Through these same ports, room air is entrained, and the partial rebreather mask can provide FIO 2 up to 0.60, for as long as oxygen flow is adequate to keep the bag from collapsing (typically 10-15 L/ min). As with nasal cannulas, smaller children with smaller tidal volumes entrain less room air, and their Fio2 values will be higher. Non-rebreather masks include 2 one-way valves, 1 between the oxygen reservoir bag and the mask and the other on 1 of the 2 exhalation ports. This arrangement minimizes mixing of exhaled and fresh gas and entrainment of room air during inspiration. The 2nd exhalation port has no valve, a safeguard to allow some room air to enter the mask in the event of disconnection from the oxygen source. A non-rebreather mask can provide FIO 2 up to 0.95. The use of a non-rebreather mask in conjunction with an oxygen blender allows delivery of FIO 2 between 0.50 and 0.95 (Table 89.8 ). When supplemental oxygen alone is inadequate to improve oxygenation, or when ventilation problems coexist, additional therapies may be necessary.
Table 89.8
| DEVICE | FLOW (L/min) | FIO 2 DELIVERED |
|---|---|---|
| Nasal cannula | 0.1-6 | 0.21-0.4 |
| Simple face mask | 5-10 | 0.4-0.6 |
| Partial rebreather | 6-15 | 0.55-0.7 |
| Non-rebreather | 6-15 | 0.7-0.95 |
| Venturi mask | 5-10 | 0.25-0.5 |
| Hood/tent | 7-12 | 0.21-1.0 |
| High-flow systems | 1-40 | 0.21-1.0 |
* Individual delivery varies and depends on the patient's size, respiratory rate, and volume moved with every breath.
Airway Adjuncts
Maintenance of a patent airway is a critical step in maintaining adequate oxygenation and ventilation. Artificial pharyngeal airways may be useful in patients with oropharyngeal or nasopharyngeal airway obstruction and in those with neuromuscular weakness in whom inherent extrathoracic airway resistance contributes to respiratory compromise. An oropharyngeal airway is a stiff plastic spacer with grooves along each side that can be placed in the mouth to run from the teeth along the tongue to its base just above the vallecula. The spacer prevents the tongue from opposing the posterior pharynx and occluding the airway. Because the tip sits at the base of the tongue, it is usually not tolerated by patients who are awake or whose gag reflex is strong. The nasopharyngeal airway , or nasal trumpet , is a flexible tube that can be inserted into the nose to run from the nasal opening along the top of the hard and soft palate with the tip ending in the hypopharynx. It is useful in bypassing obstruction from enlarged adenoids or from contact of the soft palate with the posterior nasopharynx. Because it is inserted past the adenoids, a nasopharyngeal airway should be used with caution in patients with bleeding tendencies.
Inhaled Gases
Helium-oxygen mixture (heliox) is useful in overcoming airway obstruction and improving ventilation. Helium is much less dense and slightly more viscous than nitrogen. When substituted for nitrogen, helium helps maintain laminar flow across an obstructed airway, decreases airway resistance, and improves ventilation. It is especially helpful in diseases of large airways obstruction in which turbulent airflow is more common, such as acute laryngotracheobronchitis, subglottic stenosis, and vascular ring. It is also used in patients with severe status asthmaticus. To be effective, helium should be administered in concentrations of at least 60%, so associated hypoxemia may limit its use in patients requiring >40% oxygen.
Inhaled nitric oxide (iNO) is a powerful inhaled pulmonary vasodilator. Its use may improve pulmonary blood flow and V̇/Q̇ mismatch in patients with diseases that elevate pulmonary vascular resistance, such as occurs in persistent pulmonary hypertension of the newborn, primary pulmonary hypertension, and secondary pulmonary hypertension as a result of chronic excess pulmonary blood flow (e.g., ventriculoseptal defect) or collagen vascular diseases. iNO is administered in doses ranging from 5 to 20 parts per million of inspired gas. Although administration of iNO to unintubated patients is possible, it is usually administered to patients undergoing mechanical ventilation via an endotracheal tube, because of the need for precision in iNO dosing.
Positive Pressure Respiratory Support
Noninvasive positive pressure respiratory support is useful in treating both hypoxemic and hypoventilatory respiratory failure. Positive airway pressure helps with aeration of partially atelectatic or filled alveoli, prevention of alveolar collapse at end-exhalation, and increase in functional residual capacity (FRC). These actions improve pulmonary compliance and hypoxemia, as well as decrease intrapulmonary shunt. In addition, positive pressure ventilation is useful in preventing collapse of extrathoracic airways by maintaining positive airway pressure during inspiration. Improving compliance and overcoming airway resistance also improves tidal volume and therefore ventilation. A high-flow nasal cannula delivers gas flow at 4-16 L/min and up to 60 L/min, with newer systems for older children and adolescents, capable of providing significant continuous positive airway pressure (CPAP) . In this setting, the amount of CPAP provided is not quantifiable and varies with each patient, depending on the percentage of total inspiratory flow that is delivered from the cannula, airway anatomy, and degree of mouth breathing. In small children the relative amount of CPAP for a given flow is usually greater than in older children and may provide significant positive pressure. The FIO 2 can be adjusted by provision of gas flow through an oxygen blender. Another benefit of a high-flow nasal cannula system is the washout of CO2 from the nasopharynx, which decreases rebreathing of CO2 and dead space ventilation. When delivering high-flow air or oxygen, adequate humidification is essential, by using a separate heated humidification chamber. CPAP can also be provided through snugly fitting nasal prongs or a tight-fitting face mask attached to a mechanical ventilator or other positive pressure device. Noninvasive CPAP is most useful in diseases of mildly decreased lung compliance and low FRC, such as atelectasis and pneumonia. Patients with diseases of extrathoracic airway obstruction, in which extrathoracic negative airway pressures during inspiration lead to airway narrowing (e.g., laryngotracheitis, obstructive sleep apnea, postextubation airway edema), may also benefit from CPAP. Potential risks include nasal irritation, hyperinflation from excessive CPAP in smaller patients, and abdominal distention from swallowed air.
Noninvasive positive airway pressure ventilation (NIPPV) provides positive airway pressure during exhalation, and bilevel modes can apply additional positive pressure during inspiration (see Chapter 89.1 ).
Endotracheal Intubation and Mechanical Ventilation
When hypoxemia or significant hypoventilation persists despite the interventions already described, endotracheal intubation and mechanical ventilation are indicated. Additional indications for intubation include maintaining airway patency in patients who have the potential for airway compromise, such as those with actual or potential neurologic deterioration, and in patients with hemodynamic instability.
Proper monitoring is essential to ensuring a safe and successful endotracheal intubation. Pulse oximetry, heart rate, and blood pressure monitoring are mandatory and should be forgone only in situations calling for emergency intubation. All necessary equipment, including bag-mask ventilation device, laryngoscope, endotracheal tube (ETT) with stylet, and suction equipment, must be available and working properly before the procedure of intubation. The proper internal diameter (ID) for the ETT can be estimated using the following formula:
ID=(Age [yr]/4)+4

Table 89.9 provides average values for age, size, and depth of insertion for tracheal tubes. Preoxygenation of the patient with high FIO 2 is essential and will allow maximum procedure time before the onset of hypoxemia. Although intubation can be accomplished without sedation and pharmacologic paralysis in selected patients, the physiologic benefits of these measures to the patient as well as to the facilitation of the intubation usually far outweigh the risks. Administration of a sedative and analgesic followed by a paralytic agent is a common pharmacologic regimen for facilitating intubation. In fact, sedation and paralysis with neuromuscular blocking agents should be considered standard unless contraindicated. The particular type and dose of each agent often depends on the underlying disease and clinician preference. Table 89.10 lists commonly used agents. Dexmedetomidine has been a standard sedating agent for maintenance during mechanical ventilation. An alternative to this pharmacologic approach is rapid sequence intubation , used when endotracheal intubation is urgent, or the patient is suspected of having a full stomach and at increased risk of aspiration (see Chapter 81 ).
Table 89.9
Average Size and Depth Dimensions for Tracheal Tubes
| PATIENT AGE | INTERNAL DIAMETER (mm) | OROTRACHEAL DEPTH (cm) | NASOTRACHEAL DEPTH (cm) |
|---|---|---|---|
| Premature | 2.0-3.0 | 8-9 | 9-10 |
| Full-term neonate | 3.0-3.5 | 10 | 11 |
| 6 mo | 4.0 | 11 | 13 |
| 12-24 mo | 4.5 | 13-14 | 16-17 |
| 4 yr | 5.0 | 15 | 17-18 |
| 6 yr | 5.5 | 17 | 19-20 |
| 8 yr | 6.0 | 19 | 21-22 |
| 10 yr | 6.5 | 20 | 22-23 |
| 12 yr | 7.0 | 21 | 23-24 |
| 14 yr | 7.5 | 22 | 24-25 |
| Adult | 8.0-9.0 | 23-25 | 25-28 |
Table 89.10
Medications Commonly Used for Intubation
| DRUG | DOSE | ONSET (min) | DURATION (min) | COMMENTS |
|---|---|---|---|---|
| SEDATIVES/ANESTHETICS | ||||
| Midazolam | 0.1 mg/kg IV | 3-5 | 60-120 |
Amnesia Respiratory depression |
| Lorazepam | 0.1 mg/kg IV | 3-5 | 120-240 |
Amnesia Respiratory depression |
| Ketamine |
1-2 mg/kg IV 4-6 mg/kg IM |
2-3 | 10-15 |
↑ HR, BP, and ICP Bronchodilation |
| Propofol | 1-3 mg/kg IV | 0.5-2 | 10-15 |
↓ BP Apnea |
| Thiopental | 4-7 mg/kg IV | 0.5-1 | 5-10 |
↓ BP Apnea |
| ANALGESICS | ||||
| Fentanyl | 2-5 µg/kg IV | 3-5 | 30-90 |
Respiratory depression Chest wall rigidity |
| Morphine | 0.1 mg/kg IV | 5-15 | 120-240 |
↓ BP Respiratory depression |
| NEUROMUSCULAR BLOCKING AGENTS | ||||
| Vecuronium | 0.1 mg/kg IV | 2-3 | 30-75 |
↑ HR Renal elimination |
| Rocuronium |
0.6-1.2 mg/kg IV 1 mg/kg IM |
5-15 | 15-60 |
↑ HR Renal elimination |
| Cisatracurium | 0.1 mg/kg IV | 2-3 | 25-30 |
Histamine release Nonrenal elimination |
BP, Blood pressure; HR, heart rate; ICP, intracranial pressure; IM, intramuscularly; IV, intravenously.
Once adequate sedation and/or paralysis have been achieved, ventilation should be assisted with a bag-mask device . After optimal preoxygenation, intubation can be performed. The clinician uses the dominant hand to open the patient's mouth and insert the laryngoscope blade gently along the tongue to its base. The airway opening can be visualized by applying lift up-and-away from the clinician, along the axis of the laryngoscope handle. When a straight (Miller) laryngoscope blade is used to visualize the glottis, the tip of the blade lifts the epiglottis anteriorly. When a curved (Macintosh) blade is used to visualize the glottis, the tip of the blade should be advanced into the vallecula and then lifted. Secretions often obscure visualizations at this step and should be suctioned clear. Once clear visualization of the vocal cords is accomplished, the ETT can be placed through the vocal cords. Rapid confirmation of ETT placement is essential and should be assessed by as many of the following steps as possible: presence of PetCO 2 determined by a monitor attached in-line with ETT; auscultation of both lung fields as well as the epigastrium for equal breath sounds; and, good air movement and evaluation of the abdomen for increasing distention. Adequate, bilateral chest expansion and misting inside the ETT with each breath confirm proper tube placement. An increasing heart rate, if heart rate has decreased during the attempt, and a rising or normal SpO 2 reading are suggestive of successful tube placement. Preoxygenation may significantly delay any drop in SpO 2 with improper tube placement, leading to a significant delay in its recognition. Confirmation of exhaled PetCO 2 is mandatory, using a disposable colorimetric CO2 detector or with capnography. In situations of very low pulmonary perfusion, such as cardiac arrest, PetCO 2 may not be detected. A chest radiograph should also be obtained to confirm proper placement of the ETT, which should lie with the tip about halfway between the glottis and the carina (see Chapter 81 ).
Transient Manual Ventilation in Immediate Preintubation and Postintubation Periods
Establishment of supportive ventilation via bag-mask or bag-ETT is required before transport of the patient to a setting of continued critical care. The technique of manual ventilation should take into account the underlying pathology. Mechanical ventilation of patients with diseases characterized by low FRC (e.g., pneumonia, pulmonary edema, ARDS) should include the application of PEEP to prevent alveolar derecruitment. Lung volume recruitment can be accomplished with a PEEP valve on a self-inflating ventilation bag or by careful manipulation of exhaust gas using an anesthesia bag. Such diseases are also characterized by a short time constant for lung deflation and therefore are best managed with relatively small tidal volumes and high ventilation rates.
In contrast, diseases characterized by airway obstruction have prolonged deflation time constants and are therefore best managed with relatively slow rates and high tidal volumes.
Mechanical Ventilation
Ashok P. Sarnaik, Christian P. Bauerfeld, Ajit A. Sarnaik
The decision to institute support with mechanical ventilation is based mainly on the need to assist lung function; supporting left ventricular (LV) performance and treating intracranial hypertension are additional indications. Although there are no absolute criteria for derangement of gas exchange, PaO 2 <60 mm Hg while breathing >60% oxygen, PaCO 2 >60 mm Hg, and pH <7.25 are often reasons to initiate mechanical ventilation. Clinical impressions of fatigue and impending exhaustion are also indications for ventilatory support, even in the presence of adequate gas exchange. Positive pressure ventilation is a powerful means of decreasing LV afterload, and it is used for this purpose in patients with cardiogenic shock resulting from LV dysfunction. Mechanical ventilation is also used in patients whose breathing is unreliable (e.g., unconscious patients, those with neuromuscular dysfunction) and when deliberate hyperventilation is desired, such as in patients with intracranial hypertension.
Mechanical ventilation is not intended to normalize gas exchange, nor is it a cure. The goals are to maintain sufficient oxygenation and ventilation to ensure tissue viability until the disease process that has compromised the patient's lung function has resolved, while minimizing any complications. Thus, PaO 2 , PaCO 2 , and pH levels are maintained in ranges that provide a safe environment for the patient, while protecting the lungs from damage caused by oxygen toxicity, pressure (barotrauma ), tidal volume overdistention (volutrauma ), atelectrauma , and cytokine release (biotrauma ) (Figs. 89.2 and 89.3 ).
Basic Concepts of Ventilator Management
Equation of Motion
A pressure gradient is required for air to move from one place to another. During natural spontaneous ventilation, inspiration results from generation of negative intrapleural pressure from contraction of the diaphragm and intercostal muscles, drawing air from the atmosphere across the airways into the alveoli. During mechanical ventilation, inspiration results from positive pressure created by compressed gases through the ventilator, which pushes air across the airways into alveoli. In both spontaneous and mechanical ventilation, exhalation results from alveolar pressure generated by the elastic recoil of the lung and the chest wall. Pressure necessary to move a given amount of air into the lung is determined by 2 factors: lung and chest wall elastance and airway resistance. Fig. 89.4 describes the relationship in pressure gradient, compliance, and resistance. Elastance —defined as the change in pressure (ΔP) divided by the change in volume (ΔV)—refers to the property of a substance to oppose deformation. It is opposite of compliance (ΔV ÷ ΔP), the property of a substance to allow distention or lengthening when subjected to pressure. Compliance (C) is therefore expressed as 1/elastance.
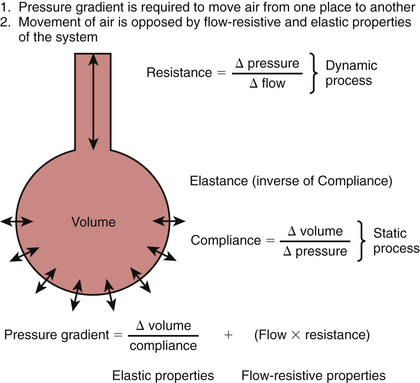
The pressure needed to overcome tissue elastance is measured in conditions in which there is no flow (at end-inspiration and end-expiration) and is therefore a reflection of static conditions in the lung. It is influenced by tidal volume (VT ) and compliance (P = ΔV ÷ C). It is increased with high VT and low compliance. This pressure gradient is used to calculate the static compliance of the respiratory system (CSTAT ).
Resistance (R) refers to the opposition to generation of flow. It is measured as the amount of pressure needed to generate a unit of flow (ΔP ÷ ΔFlow). Pressure needed to overcome airway resistance is calculated as flow multiplied by resistance. Because this pressure is needed only when the flow is occurring through the airways, it is referred to as the dynamic component . Pressure to overcome flow-resistive properties is measured when there is maximum flow and is therefore under dynamic conditions. It is increased in conditions with greater airway resistance and flow rate. Flow rate depends on the time allowed for inspiration and expiration. At higher respiratory rates, there is less time available for each inspiration and expiration, necessitating higher flows; therefore higher pressure is required to overcome flow-resistive properties. The pressure gradient necessary to move air from one place to another is the sum of pressure needed to overcome the elastic and flow-resistive properties of the lung. This pressure gradient is taken into account to calculate the dynamic compliance of the respiratory system (CDYN ). The difference in change in pressure between static conditions and dynamic conditions is attributable to airway resistance.
Functional Residual Capacity
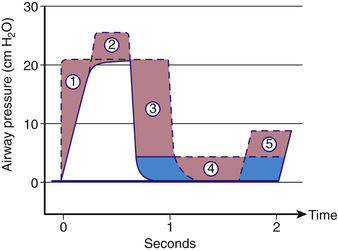
During inspiration, oxygen-enriched gas enters alveoli. During exhalation, oxygen continues to be removed by the pulmonary capillary circulation. FRC is the volume of gas left in the alveoli at end-expiration. It is the only source of gas available for gas exchange during exhalation. In diseases with decreased FRC (e.g., ARDS, pulmonary edema), PAO 2 declines sharply throughout expiration, resulting in hypoxemia. Two ventilator strategies used to improve oxygenation in such situations are the application of PEEP and increasing the inspiratory time (TI ) (Fig. 89.5 ). PEEP increases FRC, whereas a longer TI allows longer exposure of pulmonary capillary blood to a higher concentration of O2 during inspiration. (See also Chapter 400 .)
Time Constant
At the beginning of inspiration, the atmospheric pressure is higher than the pressure in the alveoli, resulting in movement of air into the alveoli. During mechanical ventilation, the ventilator circuit serves as the patient's atmosphere. As alveoli expand with air, the alveolar pressure rises throughout inspiration until it equilibrates with the ventilator pressure, at which time airflow ceases. Expiration starts when the ventilator pressure falls below the alveolar pressure. Alveolar pressure decreases throughout expiration until it reaches the ventilator pressure, at which time no further egress of air from the alveoli occurs. If inspiration or expiration is terminated before pressure equilibration between alveoli and the ventilator is allowed to occur, alveolar expansion during inspiration or alveolar emptying during expiration is incomplete. Incomplete inspiration results in delivery of decreased VT , whereas incomplete expiration is associated with air trapping and the presence of residual PEEP in the alveoli that is greater than the ventilator pressure, referred to as auto-PEEP . Some time is required for pressure equilibration to occur between alveoli and the atmosphere, which is reflected in the time constant (TC). It takes 3 TCs for 95% (and 5 TCs for 99%) of pressure equilibration to occur. The TC depends on compliance (C) and resistance (R), and their relationship is depicted in Fig. 89.6 . TC is calculated as compliance multiplied by resistance (C × R) and is measured in seconds.
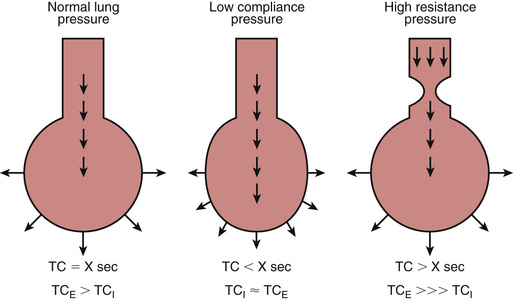
Diseases with decreased compliance (increased elastance) are characterized by high elastic recoil pressure, which results in more rapid equilibration of alveolar and ventilator pressures, thereby decreasing TC. Diseases with increased airway resistance are associated with slower flow rates, require longer time for movement of air from one place to another, and therefore have increased TC. Airways expand during inspiration and narrow during expiration. Therefore, expiratory time constant (TCE ) is longer than inspiratory time constant (TCI ). In intrathoracic airway obstruction (e.g., asthma, bronchiolitis, aspiration syndromes), airway narrowing is much more pronounced during expiration. Therefore, although both TCE and TCI are prolonged in such diseases, TCE is much more prolonged than TCI . Patients with such diseases therefore are best ventilated with slower rates, higher VT , and longer expiratory time than inspiratory time. In diseases characterized by decreased compliance, both TCE and TCI are short; however, the TCE is closer to TCI than in normal lungs because of the stiffer alveoli recoil with greater force. Patients with these diseases are best ventilated with small VT to prevent ventilator-induced lung injury and with a relatively longer inspiratory time in each breath to improve oxygenation.
Critical Opening Pressure
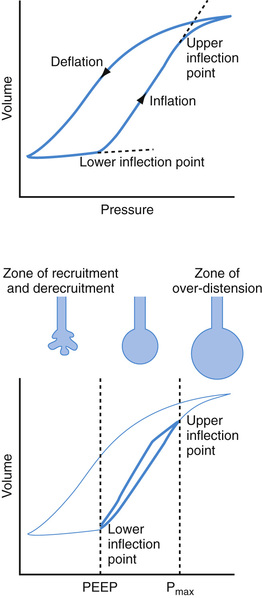
Collapsed or atelectatic alveoli require a considerable amount of pressure to open. Once open, the alveoli require relatively less pressure for continued expansion. The process of opening atelectatic alveoli is called recruitment . In a normal lung, alveoli remain open at end-expiration, and therefore the lung requires relatively less pressure to receive its VT . In a disease process in which the alveoli collapse at end-expiration (e.g., ARDS), a substantial amount of pressure is required to open the alveoli during inspiration. This pressure causes ventilator-induced lung injury by 2 mechanisms: barotrauma at the terminal airway–alveolar junction and volutrauma as a result of overdistention of alveoli that are already open (see Figs. 89.2 and 89.3 ). Although a pulmonary parenchymal disease process is rarely uniform, and each of the millions of alveoli may have its own mechanical characteristics, a composite volume-pressure relationship could be conceptualized for the whole lung (Fig. 89.7 ).
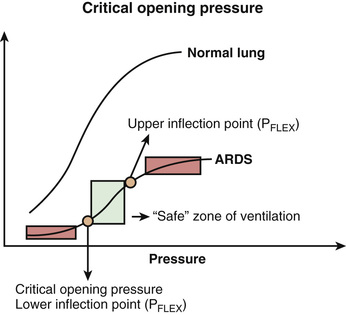
In these situations, the lower and upper portions of the curve are relatively horizontal, and the middle portion is more vertical. At the beginning of inspiration, atelectatic alveoli are being recruited, requiring high pressure for a relatively small increase in volume. Once they are recruited, further increase in volume requires relatively less pressure. The pressure at which most alveoli are open is called critical opening pressure ; this point is also referred to as the lower inflection point (lower PFLEX ). After the lower PFLEX , greater volume can be delivered for relatively less pressure until the upper PFLEX is reached, at which the volume-pressure curve again becomes relatively horizontal. The goal of mechanical ventilation in alveolar interstitial pathology is to deliver a VT between the lower and upper inflection points, the so-called safe zone of ventilation. If VT is delivered with a change in inflation pressure that includes the lower PFLEX , alveoli are likely to open and close during every breath, a process termed tidal recruitment that is injurious to the lung, especially at the terminal airway–alveolar junction. If VT is delivered with a change of pressure that includes the upper PFLEX , overdistention of alveoli is likely to occur, resulting in volutrauma and barotrauma. Keeping tidal ventilation between the upper and lower PFLEX values is accomplished by maintaining a level of PEEP to produce baseline alveolar recruitment and delivering a relatively small (6 mL/kg) VT . Called “open lung” strategy, this approach has proved to be beneficial in alveolar interstitial diseases such as ARDS.
Mechanical ventilation may be delivered either noninvasively with a patient-machine interface other than an ETT or invasively after endotracheal intubation.
Noninvasive Mechanical Ventilation
Delivering positive pressure mechanical respiratory support without the use of endotracheal intubation is called noninvasive positive pressure ventilation (NIPPV ). This type of respiratory support has been increasingly used in the pediatric intensive care setting.
The most common techniques applied are continuous positive airway pressure (CPAP ) or biphasic (inspiratory and expiratory) positive airway pressure (BiPAP ). A variety of devices with increasing sophistication has been developed in recent years, and different interfaces are available, such as nasal prongs, nasal and full-face masks, as well as helmets. Especially in the pediatric population a comfortable interface is critical for the successful application of NIPPV. NIPPV has been successfully used in acute and chronic hypoxic and/or hypercarbic respiratory failure. Indications range from acute lower airway obstruction such as asthma or acute upper airway obstruction including postextubation airway swelling, to parenchymal lung diseases such as pneumonia and ARDS. Acute and chronic respiratory failure, from neuromuscular weakness and chest wall deformities, has been the classic indication for its use. NIPPV can also be used to help prevent reintubation after prolonged mechanical ventilation.
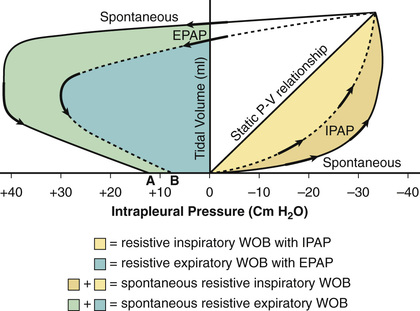
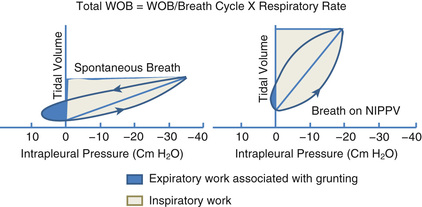
BiPAP provides positive airway pressure during exhalation and additional positive pressure during inspiration. These pressures can be adjusted independently to suit individual needs and comfort, and a respiratory rate can be delivered. The additional positive pressure during inspiration helps improve alveolar ventilation in low compliance and obstructive lung disease. During exhalation, expiratory positive airway pressure can decrease the effects of airway closure by raising intraluminal pressure and ameliorating intrathoracic airway collapse. During inspiration, inspiratory positive airway pressure can unload inspiratory muscle work.
These mechanics may explain many of the physiological benefits of NIPPV including an increase in lung compliance and FRC, a decrease of dynamic airway narrowing (“stenting” of the airway), augmentation of VT and alveolar ventilation, and decreased work of breathing. Physiologic benefits of NIPPV in obstructive (e.g., asthma) and restrictive (e.g., ARDS) lung disease are schematically presented in Figs. 89.8 and 89.9 . Additional benefits result from improving cardiopulmonary interactions, especially LV afterload reduction, thereby improving cardiac output in patients with acute or chronic LV dysfunction.
NIPPV is usually well tolerated and safer than invasive mechanical ventilation. Airway trauma from endotracheal intubation can be avoided, and less sedation is required. Breaks can be given for the application of oral medications and clearance of respiratory secretions, and selected stable patients can be fed by mouth. The number of nosocomial infections, ventilator-associated pneumonia, and ventilator-induced lung injury is expected to decrease as well. In addition, aerosol therapy driven by NIPPV, appears to be more effective.
Complications of NIPPV may include upper airway mucosal irritation, pulmonary hyperinflation with resulting interstitial emphysema and pneumothorax, abdominal distention, aspiration, and feeding intolerance. Patients initiated on NIPPV need close cardiorespiratory monitoring because the respiratory failure may progress, leading to the need for endotracheal intubation.
Some authorities have suggested independent predictors of NIPPV failure. Patients with more severe respiratory distress and those who do not show improvement of respiratory indices (i.e., respiratory rate, reduction in FIO 2 ) within 2 hr of initiation are more likely to fail. Underlying severe systemic diseases such as sepsis, multiorgan dysfunction, and malignancies are less likely to respond favorably to NIPPV. Absolute contraindications include loss of airway reflexes, acute severe neurologic insults, cardiorespiratory arrest, and severe hemodynamic instability. Patients with mid-face abnormalities or facial trauma and burns should not be considered as candidates for NIPPV. Other contraindications include the immediate postoperative period after facial and upper airway surgery, recent gastrointestinal surgery, or patients with bowel obstruction and vomiting. Patients who are severely agitated and confused should not be initiated on NIPPV. NIPPV has been shown to decrease intubation rates, as well as reintubation rates, and is increasingly used to treat acute or chronic respiratory failure in pediatric patients.
Invasive Mechanical Ventilation
Mechanical ventilation involves considering the four phases of the respiratory cycle: (1) initiation of respiration and a variable that is controlled, often referred to as mode ; (2) inspiratory phase characteristics, which determine the duration of inspiration and how the pressure or volume is delivered; (3) termination of inspiration, often referred to as cycle ; and (4) expiratory phase characteristics. Ideally, mechanical ventilation should not completely take over the work of breathing, but rather should assist the patient's own respiratory effort. In the absence of any patient effort, respiratory muscle deconditioning may occur, making weaning from mechanical ventilation more difficult.
Initiation of Inspiration and the Control Variable (Mode)
The initiation of inspiration may be set to occur at a predetermined rate and interval regardless of patient effort, or it could be timed in response to patient effort. Once inspiration is initiated, the ventilator breath either is controlled entirely by the ventilator (control mode ) or supports the patient's inspiratory effort to a predetermined inspiratory volume or pressure target (support mode ). Advances in technology allow for greater patient-ventilator synchrony to occur. The ventilator may be set to be triggered by the signal it receives as a result of patient effort. This feature may be in the form of lowering of either pressure (pressure trigger ) or airflow (flow trigger ) in the ventilator circuit generated by the patient's inspiratory effort. If no such signal is received because of lack of patient effort, the ventilator delivers a breath at an interval selected by the operator.
Control Modes
Intermittent Mandatory Ventilation Mode.
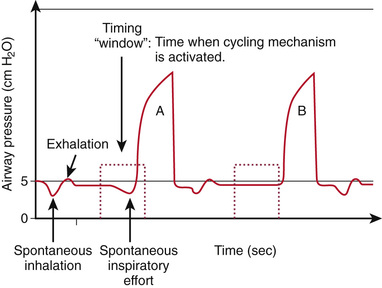
In intermittent mandatory ventilation (IMV ), the inspiration is initiated at a set frequency with a timing mechanism independent of patient effort. In between machine-delivered breaths, the patient can breathe spontaneously from a fresh source of gas. IMV allows for adjustment of ventilator support according to the patient's needs, making it useful in the weaning process. Lack of synchrony between machine-delivered breaths and patient efforts may result in ineffective ventilation and patient discomfort, especially when IMV is delivered at a high rate. In such cases the patient may require sedation and pharmacologic neuromuscular blockade for efficient delivery of VT . To obviate this problem, synchronized IMV (SIMV ) is used, whereby the machine-delivered breaths are triggered by the patient's inspiratory efforts (Fig. 89.10 ). In between the machine-delivered breaths, a fresh source of gas is available for spontaneous patient breaths. In the absence of patient effort, the patient receives a backup rate, as in IMV mode. Even with SIMV, ventilator-patient asynchrony can occur, because VT , inflation pressure, and inspiratory time are determined by the ventilator alone.
Assist-Control Mode.
In assist-control (AC) mode, every patient breath is triggered by pressure or flow generated by patient inspiratory effort and “assisted” with either preselected inspiratory pressure or volume. The rate of respirations is therefore determined by the patient's inherent rate. A backup total (patient and ventilator) obligatory rate is set to deliver a minimum number of breaths. On AC mode, with a backup rate of 20 breaths/min and a patient's inherent rate of 15 breaths/min; the ventilator will assist all the patient's breaths, and the patient will receive 5 additional breaths/min. On the other hand, a patient with an inherent rate of 25 breaths/min will receive all 25 breaths assisted. Although useful in some patients, the AC mode cannot be used in the weaning process, which involves gradual decrease in ventilator support.
Control Variable
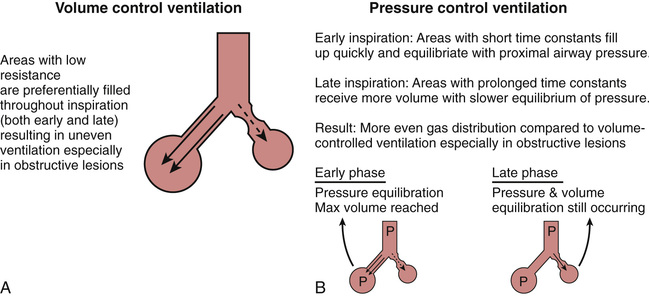
Once initiated, either the VT or the pressure delivered by the machine can be controlled. The machine-delivered breath is thus referred to as either volume controlled or pressure controlled (Table 89.11 ). With volume-controlled ventilation (VCV) , machine-delivered volume is the primary control, and the inflation pressure generated depends on the respiratory system's compliance and resistance. Changes in respiratory system compliance and resistance are therefore easily detected from changes observed in inflation pressure. In pressure-controlled ventilation (PCV) the pressure change above the baseline is the primary control, and the Vt delivered to the lungs depends on the respiratory system's C and R. Changes in respiratory system C and R do not affect inflation pressure and may therefore go undetected unless the exhaled Vt is monitored.
Table 89.11
VCV and PCV have their own advantages and disadvantages (Table 89.11 ). Generally speaking, PCV is more efficient than VCV in terms of amount of VT delivered for a given inflation pressure during ventilation of a lung that has nonuniform TC, as in asthma. In VCV, relatively less-obstructed airways are likely to receive more of the machine-delivered volume throughout inspiration than relatively more-obstructed airways with longer TC (Fig. 89.11 A ). This situation would result in uneven ventilation, higher peak inspiratory pressure (PIP), and a decrease in CDYN . In PCV, because of a constant inflation pressure that is held throughout inspiration, relatively less-obstructed lung units with shorter TC would achieve pressure equilibration earlier during inspiration than the relatively more-obstructed areas. Thus, units with shorter TCs would attain their final volume earlier in inspiration, and those with longer TCs would continue to receive additional volume later in inspiration (Fig. 89.11 B ). This situation would result in more even distribution of inspired gas, delivery of more VT for the same inflation pressure, and improved CDYN compared with VCV.
Pressure-regulated volume control (PRVC) combines the advantages of VCV and PCV. In this mode, the VT and TI are controlled as primary variables, but the ventilator determines the amount of pressure needed to deliver the desired VT . Inflation pressure is thus adjusted to deliver the prescribed VT over the TI , depending on the patient's respiratory C and R.
Support Modes
Pressure-support ventilation (PSV) and volume-support ventilation (VSV) are designed to support the patient's spontaneous respirations. With PSV, initiation of inspiration is triggered by the patient's spontaneous breath, which is then “supported” by a rapid rise in ventilator pressure to a preselected level. The inspiration is continued until the inspiratory flow rate falls to a set level (generally 25% of peak flow rate) as the patient's lungs fill up. Thus, TI is controlled by the patient's own efforts. PSV can be combined with SIMV so that any breath above the SIMV rate is supported by PSV. Allowing the patient to control as much of the rate, VT , and inspiratory time as possible is considered a gentler form of mechanical ventilation than SIMV, in which the VT (or inflation pressure) and TI are preset. PSV as the sole source of mechanical ventilator support is often not adequate for patients with severe lung disease. However, PSV is especially useful in patients being weaned and in those who require mechanical ventilation for relatively minor lung disease or for neuromuscular weakness.
VSV is similar to PSV, in that all the spontaneous breaths are supported. In VSV, inspiratory pressure to support spontaneous breaths is adjusted to guarantee a preset VT . If there is a change in respiratory mechanics or patient effort, the inspiratory pressure to support the breath initiated by patient effort is automatically adjusted to deliver the set VT .
Inspiratory Phase Characteristics
TI , inspiratory flow waveform, and pressure rise time can be adjusted in the inspiratory phase to suit the patient's respiratory mechanics.
In PCV the duration of TI is directly set in seconds. In VCV the TI can be adjusted by adjusting the inspiratory flow (volume/time). The choice of TI value depends on the respiratory rate, which determines the total duration of each breath, and on the estimation of inspiratory and expiratory TCs. Decreasing the flow rate delivery increases TI , and vice versa. With an increase in TI , the pulmonary capillary blood is exposed to a higher level of PAO 2 for a longer time. This feature is beneficial in diseases with decreased FRC, such as ARDS and pulmonary edema. An increase in TI also increases VT without increasing inflation pressure in PCV if inspiratory flow is still occurring at end-expiration. It must be recognized that at a given ventilator rate, an increase in TI decreases expiratory time (TE ). Therefore, any strategy that employs an increase in the inspiratory component of the respiratory cycle should ensure that the decreased TE is still sufficient for complete exhalation.
Inspiratory flow waveform can be adjusted in VCV mode as either a constant flow (square waveform) or a decelerating flow (descending ramp waveform). With a square waveform, flow is held constant throughout inspiration. In a descending ramp waveform, flow is maximal at the start of inspiration and declines throughout its duration. It is debatable which flow pattern is better for a given disease.
In PCV and PSV, the prescribed PIP is reached through delivery of airflow. Pressure rise time reflects the time required for the ventilator to reach PIP and can be adjusted by control of flow at the beginning of the inspiratory phase. The inspiratory flow rise time is adjusted to provide comfort for a patient who is awake and also to prevent an extremely rapid rise in inspiratory pressure, which might result in barotrauma.
Termination of Inspiration (Cycle)
The 2 most commonly used inspiratory terminating mechanisms in control modes are time-cycled and volume-cycled. With a time-cycled mechanical breath, inspiration is terminated after a preselected TI has elapsed, whereas with volume-cycled breath the inspiration ends after a preselected volume has been delivered by the machine into the ventilator circuit. A time-cycled breath is almost always pressure-limited, with the PIP held constant for the duration of inspiration. A volume-cycled breath can be pressure-limited as a safety mechanism to avoid barotrauma. The inspiration-terminating mechanism is set somewhat differently in support modes. In PSV the inspiration is set to end after the inspiratory flow decreases below a certain percentage (usually 25%) of peak inspiratory flow. This happens when the patient no longer desires to receive additional VT . Such a breath can be termed flow-cycled . In VSV the inspiration is terminated when the patient has received the desired VT .
Expiratory Phase Maneuvers
The most useful expiratory phase maneuver is the application of PEEP, which is applied to both the control breath and the assisted breath. The most important clinical benefits of PEEP are to recruit atelectatic alveoli and to increase FRC in patients with alveolar-interstitial diseases and thereby improve oxygenation. There is growing recognition that even a brief disconnection from a ventilator, and therefore having zero end-expiratory pressure (ZEEP), can result in significant alveolar derecruitment and decline in oxygenation. In patients with obstructive lesions in which insufficient exhalation results in air trapping and auto-PEEP, extrinsic PEEP (that applied through a mechanical device) can prevent airway closure during expiration and improve ventilation. Other salutary effects of PEEP include redistribution of extravascular lung water away from gas-exchanging areas, improved V̇/Q̇ relationship, and stabilization of the chest wall. The effect of PEEP on lung C is variable, depending on the level of PEEP provided and the patient's pulmonary mechanics. By shifting the VT ventilation to a more favorable part of the pressure-volume curve, PEEP may recruit more alveoli, delay airway closure, and improve lung C. Excessive PEEP, on the other hand, may lead to overdistention of alveoli and reduced C. The effect of PEEP in individual patients can be ascertained by measuring exhaled VT and calculating CDYN . Other deleterious effects of PEEP include decreased venous return, increased pulmonary vascular resistance, and decreased cardiac output.
Additional Ventilatory Modalities
Airway Pressure Release Ventilation
Airway pressure release ventilation (APRV ) improves oxygenation in patients with severe hypoxemic respiratory failure resulting from alveolar-interstitial disease. This modality applies a CPAP, designated CPAPHIGH , to recruit and maintain FRC with brief intermittent release phases of CPAPLOW to allow alveolar gas to escape. CPAPHIGH is analogous to PIP, and CPAPLOW is similar to setting PEEP. In contrast to the patient receiving conventional mechanical ventilation, a patient receiving APRV spends the majority of time in the CPAPHIGH phase, which may last as long as 3-5 sec with a brief (0.3-0.5 sec) time in the CPAPLOW phase. These atypically long TI s are tolerated because of a floating expiratory valve in the ventilator circuit that permits spontaneous breathing during CPAPHIGH phase. Therefore, even if the CPAPHIGH phase can be considered “inspiratory” and the CPAPLOW phase “expiratory” in regard to the ventilator, the patient is able to breathe spontaneously during both these phases. The longer ventilator TI recruits lung units, and the ability to breathe spontaneously during this phase allows distribution of gas flow to atelectatic lung regions. The outcome benefit of APRV in pediatric hypoxemic respiratory failure has not been proved.
High-Frequency Ventilation
Mechanical ventilation at supraphysiologic rates and low VT , known as high-frequency ventilation (HFV ), improves gas exchange in a select group of patients who show no response to traditional ventilatory modalities. The mechanism of alveolar ventilation in HFV is very different from that in conventional ventilation, in that HFV is less dependent on VT and more dependent on asymmetric velocities and convective dispersion of inspired gas. Patients with severe persistent hypoxic failure are most likely to benefit from HFV. HFV is also helpful in patients with bronchopleural fistula and persistent air leaks. The main tenet of HFV is to recruit lung volume with a high MAP and produce smaller fluctuations in alveolar pressure during inspiration and expiration, thus maintaining a satisfactory FRC and reducing alveolar stretch. The 2 most investigated techniques of HFV are HFO and HFJV.
The most commonly used HFV modality is high-frequency oscillation (HFO) , which employs a mechanism to generate to-and-fro air movement. Additional air is drawn in (entrained) through a parallel circuit via a Venturi effect. Air is pushed in during inspiration and actively sucked out during expiration. The main determinants of oxygenation are FIO 2 and MAP, whereas ventilation is determined by changes in pressure (amplitude) from the MAP. Commonly used respiratory frequency varies from 5 Hz (300 breaths/min) in adults and older children, to 6-8 Hz (360-480 breaths/min) in young children, 8-10 Hz (480-600 breaths/min) in infants, and 10-12 Hz (600-720 breaths/min) in newborn and premature infants.
In high-frequency jet ventilation (HFJV) , a high-frequency interrupter is interposed between a high-pressure gas source and a small cannula that is incorporated in the ETT. The cannula propels tiny amounts of gas (jets) at high velocity and high frequency through the ETT. An additional amount of gas is entrained from a parallel circuit. Unlike in HFO, expiration occurs passively in HFJV as a result of elastic recoil of the lung and the chest wall. PEEP is set through the parallel circuit by a conventional ventilator in line. Respiratory rate is generally set at 420 breaths/min. Major determinants of oxygenation are Fio2 and PEEP, and the major determinant of ventilation is PIP.
Conventional Ventilator Settings
Fraction of Inspired Oxygen
The shape of the hemoglobin-O2 dissociation curve dictates that oxygen content in the blood is not linearly related to PaO 2 . A PaO 2 value that results in an oxyhemoglobin saturation of 94% is reasonable in most situations, because a higher PaO 2 would cause minimal increase in arterial oxygen content, and a modest (10 mm Hg) drop in PaO 2 would result in minimal decrease in oxyhemoglobin saturation. In most cases, a PaO 2 value of 70-75 mm Hg is a reasonable goal. FIO 2 values that are higher than those necessary to attain oxyhemoglobin saturations of approximately 95% expose the patient to unnecessary oxygen toxicity. Whenever possible, FIO 2 values should be decreased to a level ≤0.40 as long as oxyhemoglobin saturation remains ≥95%.
Mode
The choice of mode of ventilation depends on how much ventilator-patient interaction is desired and the disease entity that is being treated. SIMV or AC is chosen as the control mode; PCV, VCV, or PRVC as the variable that is to be controlled; and pressure support and volume support are the choices for support modes.
Tidal Volume and Rate
As previously discussed, alveolar ventilation, the chief determinant of PaCO 2 , is calculated using VT , respiratory rate, and VD . A change in VT results in a corresponding change in alveolar ventilation without affecting VD -ventilation. A change in respiratory rate will affect alveolar ventilation as well as the VD -ventilation. Choice of VT and rate depends on the TC. In a patient with relatively normal lungs, an age-appropriate ventilator rate and a VT of 7-10 mL/kg would be appropriate initial settings. Diseases associated with decreased TC (decreased static compliance; e.g., ARDS, pneumonia, pulmonary edema) are best treated with small (6 mL/kg) VT and relatively rapid rates (e.g., 25-40 breaths/min). Diseases associated with prolonged TCs (increased airway resistance; e.g., asthma, bronchiolitis) are best treated with relatively slow rates and higher (10-12 mL/kg) VT . In PCV the delivered VT depends on the C and R of the patient's respiratory system and needs to be monitored to ensure the appropriate amount for a given situation. An inflation pressure of 15-35 cm H2 O is sufficient for most patients, but it may need adjustment, depending on the volume of exhaled VT . It should be emphasized that achieving a normal PaCO 2 value is not a goal of mechanical ventilation. Mild hypercapnia (permissive hypercapnia) should be acceptable, especially when one is attempting to limit injurious inflation pressures or VT s.
Inspiratory Time and Expiratory Time
TI and TE are adjusted by setting inspiratory flow rate in VCV and by setting the precise TI in PCV. Increasing the TI results in increased MAP, improved oxygenation in diseases with decreased FRC, and better distribution of VT in obstructive lung disease. Sufficient expiratory time must be provided to ensure adequate emptying of the alveoli.
Positive End-Expiratory Pressure
The best level of PEEP depends on the disease entity that is being treated, and it may change in the same patient from time to time. Decisions are often based on the PaO 2 /FIO 2 ratio and the measurement of CDYN .
Patient-Ventilator Asynchrony
Patient-ventilator asynchrony occurs when the patient's respiratory pattern does not match that of the ventilator. This can occur during all phases of respiration. Adverse effects of patient-ventilator asynchrony include wasted effort, ineffective delivery of desired VT , excessive generation of intrathoracic pressure resulting in barotrauma and adverse effects on cardiac output, increased work of breathing, and patient discomfort. Although several mechanisms exist to facilitate patient-ventilator asynchrony, a certain amount of asynchrony is inevitable unless the patient is pharmacologically sedated and paralyzed.
Triggering the Ventilator
The patient must be able to trigger the ventilator without excessive effort. Ventilators can be pressure-triggered or flow-triggered. With pressure triggering , the inspiratory valve opens and flow is delivered when a set negative pressure is generated within the patient-ventilator circuit during inspiration. The amount of pressure required to trigger an inspiration depends on the pressure trigger sensitivity. In flow triggering the ventilator provides a base flow of gas through the ventilator-patient circuit. When a flow sensor on the expiratory limb of the patient-ventilator circuit detects a decrease in flow as a result of the patient's inspiratory effort, the inspiratory valve opens and a ventilator breath is delivered. The degree of change in flow required to trigger an inspiration depends on the flow trigger sensitivity. Flow triggering is considered to be more comfortable, primarily because the patient receives some flow before triggering the ventilator, in contrast to pressure triggering, in which no flow is provided until the ventilator breath is triggered. Increasing the trigger sensitivity by decreasing the change in either pressure or flow needed to trigger an inspiration decreases the work of breathing. However, reducing the required pressure or flow excessively could result in accidental triggering and unwanted breaths by turbulence, caused by condensation in the ventilator circuit, ETT air leaks, or cardiac oscillations.
Selection of Appropriate Inspiratory Time
The duration of TI should match the patient's own inspiratory phase. If TI is too long, the patient's drive to exhale may begin before the ventilator breath has cycled off. When this occurs, exhalation occurs against inspiratory flow and a closed exhalation valve, resulting in increased work of breathing, excessive rise in intrathoracic pressure, and discomfort. If TI is too short, the patient may be still inhaling without respirator support. In general terms, TI is usually initiated at 0.5-0.7 sec for neonates, 0.8-1 sec in older children, and 1-1.2 sec for adolescents and adults. Adjustments need to be made through individual patient observations and according to the type of lung disease present. In patients with severe lung disease (both obstructive and restrictive), unnatural TI and TE values may have to be selected, as discussed earlier. In such situations, adequate analgesia, sedation, and in extreme cases neuromuscular blockade may be needed.
Selection of Inspiratory Flow Pattern
In VCV, inappropriate flow may be another source of patient-ventilator dyssynchrony. After initiation of inspiration, if the set amount of flow is inadequate to meet patient demand, a state of flow starvation occurs, resulting in excessive work of breathing and discomfort. Such patients may require a decelerating inspiratory flow pattern, in which a higher flow is provided in the beginning of inspiration and less toward the end as the lungs fill up. On the other hand, such a pattern may be uncomfortable for a patient who desires more gradual alveolar filling. The selection of inspiratory flow pattern should be based on the individual patient's respiratory mechanics. In PCV and PSV, the inspiratory rise time determines the manner in which the airway pressure is raised and VT delivered. Considerations for choosing the appropriate rise time in PCV and PSV are similar to those for choosing the inspiratory flow pattern in VCV.
Use of Support Modes
A conscious patient should be allowed to have spontaneous breaths that are supported by either PSV or VSV. This approach minimizes the mandatory breaths generated by the ventilator that are beyond the patient's control to modulate. Therefore, continued assessments should be made to determine whether the patient is able to maintain ventilatory requirements more in support modes and less in control modes.
Use of Sedation and Pharmacologic Neuromuscular Blockade
Having a conscious but comfortable patient is a desirable goal during mechanical ventilation. Spontaneous breaths with good muscle tone and presence of cough are important for adequate clearance of tracheobronchial secretions. The patient's ability to indicate distress is also important in identifying and preventing potential injurious factors. In certain situations, management of patient-ventilator asynchrony assumes much greater importance when the asynchrony is causing unacceptable derangement of gas exchange and ventilator-induced lung injury. Both alveolar interstitial lung pathology and obstructive airway diseases may necessitate unnatural and uncomfortable settings for respiratory rate, TI , and inflation pressures. In such patients, deep sedation is often necessary; dexmedetomidine, benzodiazepines, and opiates are the agents most commonly used for this purpose. In extreme situations, pharmacologic neuromuscular blockade with a nondepolarizing agent, such as vecuronium, is required to abolish any patient effort and respiratory muscle tone. When such pharmacologic paralysis is used, deep sedation must be ensured so that the patient does not sense pain and discomfort. Pharmacologic sedation and paralysis can ensure total control of the patient's ventilation by mechanical means and may result in lifesaving improvement in gas exchange with reduction in inflation pressures. However, long-term use of such agents may be associated with undesirable consequences and higher morbidity. The risk of inadequate tracheobronchial secretions and atelectasis is potentially greater. Long-term use of pharmacologic sedation may be associated with chemical dependency and withdrawal manifestations, and prolonged neuromuscular blockade is associated with neuromyopathy in critically ill patients. The benefits of sedation and pharmacologic paralysis therefore should be carefully balanced with the risks, and periodic assessments should be made to determine the need for their continuation.
Cardiopulmonary Interactions
Mechanical ventilation can have salutary as well as adverse effects on cardiac performance. By decreasing oxygen consumption necessary for work of breathing, oxygen supply to vital organs is improved. Positive pressure breathing decreases LV afterload, thus enhancing stroke volume and cardiac output in patients with failing myocardium (e.g., myocarditis). On the other hand, the decreased systemic venous return may further compromise stroke volume in hypovolemic patients. Such patients will require intravascular fluid loading. Also, an increase in pulmonary vascular resistance (PVR) caused by positive intrathoracic pressure may result in further decompensation of a poorly performing right ventricle. PVR is at its lowest value at an optimum FRC. When FRC is too low or too high, PVR (and therefore the right ventricular afterload) is increased. Both desirable and undesirable effects of cardiopulmonary interactions may coexist and require ongoing assessment and necessary interventions (Table 89.12 ).
Table 89.12
APRV, Airway pressure release ventilation; ARDS, acute respiratory distress syndrome; HFO, high-frequency oscillation; HFJV, high-frequency jet ventilation; PCV, pressure-controlled ventilation; PRVC, pressure-regulated volume control; VCV, volume-controlled ventilation.
Monitoring Respiratory Mechanics
Exhaled Tidal Volume
Exhaled tidal volume (VTE ) is measured by a pneumotachometer in the ventilator circuit during exhalation. In VCV, part of the machine-delivered volume may leak out during inspiration and therefore never reach the patient. Measurement of VTE more accurately describes the VT that is contributing to the patient's alveolar ventilation. In PCV the VTE depends on the patient's respiratory system compliance and resistance and therefore offers valuable diagnostic clues. A decrease in VTE during PCV is indicative of either decrease in compliance or increase in resistance and is helpful in directing the clinician to appropriate investigation and management. An increase in VTE is indicative of improvement and may require weaning of inflation pressures to adjust the VTE .
Peak Inspiratory Pressure
In VCV and PRVC, the PIP is the secondary variable determined by the patient's respiratory system compliance and resistance. An increase in PIP in these modes is indicative of decreased C (e.g., atelectasis, pulmonary edema, pneumothorax) or increased R (e.g., bronchospasm, obstructed ET). During VCV and PRVC, decreasing the respiratory rate or prolonging the TI will result in a lower PIP in patients with prolonged TCs because more time will be available for alveoli to fill. In such patients, a decrease in PIP suggests increased C or decreased R of the respiratory system.
Respiratory System Dynamic Compliance and Static Compliance
The changes in PIP during VCV and PRVC, and in VTE during PCV, are determined by CDYN of the respiratory system (lung and chest wall). CDYN is calculated as follows:
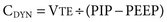
C DYN takes into account both the flow-resistive and the elastic properties of the respiratory system. Changes in CDYN can be used to assess effects of different levels of PEEP as tidal ventilation is shifted along the slope of the volume-pressure curve (see Fig. 89.7 ). An increase in PEEP in alveolar-interstitial diseases (increased elastance), resulting in an increase in CDYN suggests alveolar recruitment, whereas a decrease in CDYN may indicate overdistention. Similarly, in obstructive diseases (increased R), adjustment in PEEP levels to ameliorate airway collapse during exhalation can be guided by monitoring CDYN . To assess only the elastic recoil of the lung, measurement of CSTAT when there is no airflow is required. This measurement is performed by using an inspiratory hold maneuver with the patient under neuromuscular blockade and observing pressure-time and flow-time waveforms (Fig. 89.12 ). During this maneuver, inspiratory flow ceases while the expiratory valve continues to remain closed, thus allowing pressure to equilibrate throughout the ventilator circuit and the patient's lungs. This pressure, referred to as the plateau pressure (Pplat ), reflects alveolar pressure. CSTAT is calculated as follows:
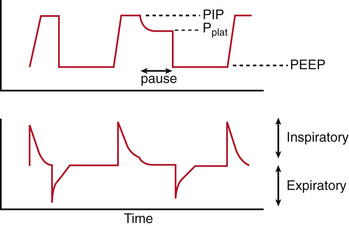
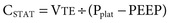
The difference between CDYN and CSTAT is attributable to airway resistance. This difference is minimal in alveolar-interstitial diseases but substantial in airway obstruction.
Assessment of Auto-PEEP
Auto-PEEP is assessed with the use of an expiratory pause maneuver in which inspiration is delayed and alveolar pressure is allowed to equilibrate with the airway. In diseases with airway obstruction, insufficient alveolar emptying may occur if exhalation time is not adequate. The alveolar pressure in excess of the set PEEP at the completion of the expiratory pause is measured as auto-PEEP or intrinsic PEEP. Auto-PEEP can have adverse effects on ventilation and hemodynamic status. It can be managed by decreasing the respiratory rate or TI and thus allowing longer time for exhalation. Auto-PEEP may also be managed by increasing the set PEEP (extrinsic PEEP), thereby delaying airway closure during exhalation and improving alveolar emptying.
Assessment of Dead Space Ventilation
Positive pressure ventilation and application of PEEP may result in a decrease in venous return, cardiac output, and therefore pulmonary perfusion as well. Ventilation of poorly perfused alveoli results in dead space ventilation, which does not contribute to gas exchange. The VD /VT fraction can be calculated (see Chapter 89). Normal VD /VT is 0.33. Increased VD /VT is indicative of poorly perfused alveoli. Patients with increased VD /VT may require intravascular volume infusion or other means of augmenting the cardiac output to improve pulmonary perfusion. The VD /VT fraction is calculated and displayed by commercially available capnographs, which measure endotracheal PetCO 2 continuously.
Ventilator-Induced Lung Injury
As with most medical therapies, mechanical ventilation can be harmful. Pathophysiology of ventilator-induced lung injury can be multifactorial. Large lung volumes and high pressures delivered with increased frequency cause cyclic strain, which may lead to disruption of the tight junctions between the alveolar epithelial and capillary endothelial cells, with intracapillary blebs resulting in alveolar and interstitial edema. This biotrauma may cause the release of proinflammatory cytokines that further injure the lung and travel in the blood outside the lung, leading to multiorgan failure. Evidence shows that in patients with ARDS, avoidance of VT ≥10 mL/kg and Pplat ≥30 cm H2 O limits diffuse alveolar damage.
Atelectrauma is shear stress on the alveolar walls caused by cyclic opening and closing of the alveoli. PEEP can be used to prevent collapse and keep alveoli open. It is important that alveolar units are neither overdistended nor collapsed. Careful adjustments of PEEP may also permit the clinician to wean a patient from a high FIO 2 , another potential source of lung injury (oxytrauma ). Although most patients receive an FIO 2 of 1.00 during endotracheal intubation and at the beginning of mechanical ventilation, increasing PEEP to recruit alveoli without overdistention should be quickly instituted to improve oxygenation and permit weaning of the FIO 2 . Although the FIO 2 value below which there is no risk of oxygen toxicity is unknown, most clinicians aim for a value <0.6. Regional mechanics may play a role in lung injury.
Ventilator-Associated Pneumonia
The pathophysiology of ventilator-associated pneumonia (VAP) is multifactorial. Aspiration of oral and/or gastric secretions, colonization of ETTs, and suppression of cough reflexes with sedation all play a role. New-onset fever and leukocytosis accompanied by demonstration of an infiltrative process on chest radiography are consistent with a diagnosis of VAP. This complication can lead to worsened gas exchange, increased duration of ventilation, and even death. Elevation of the head of the bed to 30 degrees after initiation of mechanical ventilation and use of a protocol for oral decontamination during mechanical ventilation are 2 means of reducing the risk for VAP. The most effective strategy to minimize any of the aforementioned complications is regular assessment of extubation readiness and liberation from mechanical ventilation as soon as clinically possible.
Weaning
Weaning from mechanical ventilation should be considered as a patient's respiratory insufficiency begins to improve. Most pediatricians favor gradual weaning from ventilator support. With SIMV, the ventilator rate is slowly reduced, allowing the patient's spontaneous breaths (typically assisted with pressure or volume support) to assume a larger proportion of the minute ventilation. When the ventilator rate is low (<5 breaths/min) such that its contribution to minute ventilation is minimal, assessment of extubation readiness is performed. An alternative method of gradual weaning is transition to PSV. In this mode, no ventilator rate is set, allowing all triggered breaths to be assisted with pressure support. The clinician reduces the pressure support slowly to a low value (<5-10 cm H2 O), at which point assessment of extubation readiness is performed. During either technique, weaning should be halted if tachypnea, increased work of breathing, hypoxemia, hypercapnia, acidosis, diaphoresis, tachycardia, or hypotension occurs.
The most objective means of assessing extubation readiness is a spontaneous breathing trial (SBT) . Before performance of an SBT, a patient should be awake with intact airway reflexes, capable of handling oropharyngeal secretions, and with stable hemodynamic status. In addition, gas exchange should be adequate, defined as PaO 2 >60 mm Hg while receiving FIO 2 <0.4 and PEEP ≤5 cm H2 O. If these criteria are present, a patient should be started on CPAP with minimal or no pressure support (≤5 cm H2 O). If this SBT is tolerated with no episodes of respiratory or cardiovascular decompensation, successful extubation is likely.
Some neonates and small children cannot be calmed or consoled long enough to complete the SBT. In this situation, extubation readiness must be assessed on a low level of ventilator support. Data suggest a low risk of extubation failure if the patient is comfortable and has stable hemodynamic status, with adequate gas exchange and spontaneous VT >6.5 mL/kg, while receiving <20% of total minute ventilation from the ventilator. Certain patient populations are at increased risk for extubation failure, such as young infants, children mechanically ventilated for >7 days, and patients with chronic respiratory or neurologic conditions. These children often benefit from transition to a noninvasive form of positive pressure ventilation (e.g., high-flow nasal cannula, CPAP, or BiPAP) delivered via nasal prongs or face mask to increase the odds of successful extubation.
The likelihood of postextubation upper airway obstruction , the most common cause of extubation failure in children, cannot be predicted on the basis of an SBT result or bedside measurements of physiologic variables. Traumatic endotracheal intubation and subglottic swelling from ETT irritation, especially in patients who exhibit agitation while receiving mechanical ventilation, are common causes of airway narrowing after extubation. Administration of intravenous corticosteroids (dexamethasone, 0.5 mg/kg every 6 hr for 4 doses before extubation) has been shown to minimize the incidence of postextubation airway obstruction. In patients in whom postextubation airway obstruction develops, the need for reintubation may be obviated by administration of nebulized racemic epinephrine and heliox.
Long-Term Mechanical Ventilation
See Chapter 446.4 .
Bibliography
Albuali WH, Singh RN, Frasier DD, et al. Have changes in ventilation practices improved outcome in children with acute lung injury? Pediatr Crit Care Med . 2007;8:324–330.
Bronicki RA, Anas NG. Cardiopulmonary interactions. Pediatr Crit Care Med . 2009;10:313–322.
Brower RG, Lanken PN, MacIntyre N, National Heart, Lung, and Blood Institute ARDS Clinical Trials Network, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med . 2004;351:327–336.
Campbell RS, Davis BR. Pressure-controlled versus volume-controlled ventilation: does it matter? Respir Care . 2002;47:416–424.
Chu DK, Kim LHY, Youg PJ, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet . 2018;391:1693–1704.
Combes A, Hajage D, Capellier G, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med . 2018;378(21):1965–1974.
Goligher EC, Ferguson ND, Brochard LJ. Clinical challenges inmechanical ventilation. Lancet . 2016;387:1856–1866.
Greenough A, Dimitriou G, Prendergast M, et al. Synchronized mechanical ventilation for respiratory support in newborn infants. Cochrane Database Syst Rev . 2008;(1) [CD000456].
Leme AC, Hajjar LA, Volpe MS, et al. Effect of intensive vs moderate alveolar recruitment strategies added to lung-protective ventilation on postoperative pulmonary complications. JAMA . 2017;317(4):1422–1432.
Mac Sweeney R, McAuley DF. Acute respiratory distress syndrome. Lancet . 2016;388:2416–2430.
Marraro GA. Innovative practices of ventilatory support with pediatric patients. Pediatr Crit Care Med . 2004;4:8–17.
Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome. JAMA . 2008;299:637–645.
Mercat A, Richard JCM, Vielle B, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome. JAMA . 2008;299:646–654.
Newth CJ, Venkataraman S, Willson DF, et al. Weaning and extubation readiness in pediatric patients. Pediatr Crit Care Med . 2009;10:1–11.
Papazian L, Forel JM, Gacouin A, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med . 2010;363(12):1107–1116.
Pearse RM, Young JD. Steroids to prevent postextubation laryngeal oedema. Lancet . 2007;369:1060–1061.
Pinhu L, Whitehead T, Evans T, et al. Ventilator-associated lung injury. Lancet . 2003;361:332–340.
Priestley MA, Helfaer MA. Approaches in the management of acute respiratory failure in children. Curr Opin Pediatr . 2004;16:293–298.
Randolph A. Management of acute lung injury and acute respiratory distress syndrome in children. Crit Care Med . 2009;37:2448–2454.
Reade MC, Eastwood GM, Bellomo R, et al. Effect of dexmedetomidine added to standard care on ventilator-free time in patients with agitated delirium. JAMA . 2016;315(14):1460–1468.
Sarnaik AP, Daphtary K, Meert KL, et al. Pressure controlled ventilation in children with status asthmaticus. Pediatr Crit Care Med . 2004;5:133–138.
Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomized controlled trial. Lancet . 2009;373:1874–1882.
Siemieniuk RAC, Chu DK, Kim LHY, et al. Oxygen therapy for acutely ill medical patients: a clinical practice guideline. BMJ . 2018;363:4169.
Spoletini G, Garpestad E, Hill NS. High-flow nasal oxygen or noninvasive ventilation for postextubation hypoxemia: flow vs pressure? JAMA . 2016;315(13):1340–1342.
Srinivasan R, Asselin J, Gildengorin G, et al. A prospective study of ventilator-associated pneumonia in children. Pediatrics . 2009;123:1108–1115.
Thompson BT, Chambers RC, Liu KD. Acute respiratory distress syndrome. N Engl J Med . 2017;377(6):562–572.
Xu XP, Zhang XC, Hu SL, et al. Noninvasive ventilation in acute hypoxemic nonhypercapnic respiratory failure: a systematic review and meta-analysis. Crit Care Med . 2017;45(7):e727–e733.