Chapter 53 NURSING MANAGEMENT: female reproductive problems
1. Summarise the aetiologies of infertility and the strategies for diagnosis and treatment of the infertile woman.
2. Describe the aetiology, clinical manifestations, and nursing and collaborative management of menstrual problems and abnormal vaginal bleeding.
3. Analyse the risk factors, clinical manifestations and multidisciplinary care of ectopic pregnancy.
4. Describe the changes related to menopause and the nursing and collaborative management of the patient with menopausal symptoms.
5. Explore common problems that affect the vulva, vagina and cervix and the related nursing and collaborative management.
6. Apply knowledge of assessment, multidisciplinary care and nursing management to women with pelvic inflammatory disease and endometriosis.
7. Explain the clinical manifestations, diagnostic studies, multidisciplinary care and surgical therapy for cervical, endometrial, ovarian and vulvar cancers.
8. Summarise the preoperative and postoperative nursing management for the patient requiring surgery of the female reproductive system.
9. Differentiate between the common problems that occur with cystoceles, rectoceles and fistulas and the related nursing and collaborative management.
10. Summarise the clinical manifestations of sexual assault and the appropriate nursing and collaborative management of the patient who has been sexually assaulted.
Infertility
Infertility is the inability to conceive after 2 years of regular unprotected intercourse.1 During their reproductive years approximately 15% of couples in Australia and New Zealand take longer than 1 year to achieve a planned pregnancy.2 Assessment and therapy measures can be invasive, expensive and lengthy. Understandably, infertility can constitute both a physical and an emotional crisis.
AETIOLOGY AND PATHOPHYSIOLOGY
Infertility may be caused by either female or male factors, or combined factors. Conditions that cause male infertility are discussed in Chapter 54. However, in up to 30% of couples evaluated, the cause of infertility may not be identified. The factors most frequently causing female infertility include ovulation (anovulation or inadequate corpus luteum), tubal obstruction or dysfunction (endometriosis or damage from pelvic infection) and uterine or cervical factors (fibroid tumours or structural anomalies). Risk factors for infertility include tobacco and illicit drug use and an abnormal body mass index (BMI) indicating obesity or low body weight. In women the risk for infertility increases with age. In particular, the probability of becoming pregnant begins decreasing at age 35 and decreases even further after age 40.
DIAGNOSTIC STUDIES
A detailed history and a general physical examination of the woman and her partner provide the basis for selecting diagnostic studies (see Box 53-1). The possibility of medical, genetic or gynaecological diseases is explored before tests are performed to determine problems affecting general health, as well as fertility. These tests include hormone levels, ovulatory studies, tubal patency studies and postcoital studies.3
MULTIDISCIPLINARY CARE
Diagnostic studies
Ovulatory studies
A basal body temperature record is kept to determine whether there is regular ovulation (see Fig 53-1). The woman is instructed to take and graph her temperature, referred to as basal body temperature, on awakening before any activity. The same site for taking the temperature (e.g. oral, rectal) should be used each time. Any cause for variation, such as sleep problems or illness, should be noted. As ovulation approaches, the production of oestrogen increases. This may cause a drop in temperature. When ovulation occurs, progesterone is produced, causing a rise in temperature. The temperature graph thus helps detect ovulation and suggests the timing of intercourse if pregnancy is desired. Rigid adherence to a schedule for intercourse may produce psychological stress sufficient to inhibit sexual relations.

Figure 53-1 Basal body temperature chart. A, Typical biphasic temperature curve indicative of ovulation and normal progesterone effect. B, Irregular monophasic curve characteristic of anovulatory cycles. C, Ovulatory curve with sustained temperature elevation following conception and the first missed period.
Ovulation prediction kits are now available for use by women at home. These kits are generally used daily to measure luteinising hormone (LH) levels in urine samples. Ovulation occurs about 28–36 hours after the first rise of LH, so intercourse can be timed accordingly. Other tests for ovulation include cervical and vaginal smears, endometrial biopsy and plasma progesterone levels.
Tubal patency studies
Tubal factors (occlusion or deformity) are assessed most commonly by means of a hysterosalpingogram. This procedure consists of the radiographic visualisation of the uterus and tubes by injecting a radio-opaque dye through the cervix. Tubal patency, shape, position and any distortions of the endometrial cavity can be determined. Laparoscopy may be used when a hysterosalpingogram is contraindicated or other pelvic pathology appears likely.
Postcoital studies
Examination of the cervical mucus can reveal whether it undergoes favourable changes at ovulation, enabling penetration, survival and normal motility of the sperm. A postcoital test can determine whether the cervical environment is favourable for the sperm. The couple is asked to have intercourse about the time ovulation is expected and 2–12 hours before the surgery visit. Douching or bathing should be avoided before the test. The cervical and vaginal secretions are aspirated and examined for the number and motility of sperm present. Other screening tests for infertility include semen analysis and pelvic ultrasound.
 NURSING AND COLLABORATIVE MANAGEMENT: INFERTILITY
NURSING AND COLLABORATIVE MANAGEMENT: INFERTILITY
The management of infertility problems depends on the cause. If infertility is secondary to an alteration in ovarian function, supplemental hormone therapy to restore and maintain ovulation may be attempted.4 Drug therapy used to treat infertility is presented in Table 53-1. Chronic cervicitis and inadequate oestrogenic stimulation are cervical factors causing infertility. Antibiotic therapy is indicated for cervicitis. Inadequate oestrogenic stimulation is treated by the administration of oestrogen.
When a couple has not succeeded in conceiving while under infertility management, an option is intrauterine insemination with sperm from the partner or a donor. If this technique does not succeed, assisted reproductive technologies (ARTs) may be used. ARTs include in-vitro fertilisation (IVF), gamete intrafallopian transfer (GIFT), zygote intrafallopian transfer (ZIFT), donor gametes and embryo cryopreservation. IVF involves the removal of mature oocytes from the woman’s ovarian follicle via laparoscopy, followed by in-vitro fertilisation of the ova with the partner’s sperm. When fertilisation and cleavage have occurred, the resulting embryos are transferred into the woman’s uterus. The procedure requires 2–3 days to complete and is used in cases of fallopian tube obstruction, diminished sperm count and unexplained infertility. Frequently, multiple attempts are needed for successful implantation. IVF is financially costly and emotionally stressful. However, it has become an accepted method of therapy for infertile couples.
With the increasing sophistication of ARTs, couples have an increased potential for pregnancy. However, the use of ARTs often poses many ethical, legal and social concerns. Furthermore, the regulation and funding for ARTs differs between states and countries and is a factor of the relative strength of the various interest groups involved.2
Healthcare practitioners can assist women experiencing infertility by providing information about the physiology of reproduction, offering infertility evaluation and addressing the psychological and social distress that can accompany infertility. Reducing patients’ psychological stress can make them more relaxed and may assist in achieving a pregnancy.
Teaching and providing emotional support are major responsibilities throughout infertility testing and treatment. Feelings of anger, frustration, grief and helplessness may heighten as additional diagnostic tests are performed. Infertility can generate great tension in a marriage as the couple exhausts financial and emotional resources. Few insurance carriers cover the high cost of infertility testing or expensive infertility treatment. Recognising and taking steps to deal with the psychological factors that surface can assist the couple to better cope with the situation. Couples should be encouraged to participate in a support group for infertile couples, as well as individual therapy.
Abortion
An abortion is the loss or termination of a pregnancy before the fetus has developed to a state of viability. Abortions are classified as spontaneous (those occurring naturally) or induced (those occurring as a result of mechanical or medical intervention). Miscarriage is the common term for the unintended loss of a pregnancy. Habitual recurrent abortion is a history of three or more aborted pregnancies or miscarriages in succession.
SPONTANEOUS ABORTION
Spontaneous abortion is the natural loss of a pregnancy before 20 weeks of gestation. Fetal chromosomal anomalies account for 50% of miscarriages before 8 weeks of gestation. Other causes of spontaneous abortion include endocrine abnormalities, maternal infection, acquired anatomical abnormalities (e.g. uterine fibroids, endometriosis), immunological factors and environmental factors. About 10–15% of all pregnancies end as a result of spontaneous abortion.
Uterine cramping coupled with vaginal bleeding often indicates a spontaneous abortion. Cramping is usually absent if the vaginal bleeding is caused by other conditions, such as polyps. Serial serum βhuman chorionic gonadotropin (β-hCG) hormone and vaginal ultrasound examination of the pelvis are the most reliable indicators of early pregnancy viability. The gestational sac can be visualised using ultrasound as early as 6 weeks of gestation.
Treatment for a possible spontaneous abortion is limited. Although bed rest and avoiding vaginal intercourse are often recommended, there is no evidence that these measures improve the outcome. The woman is advised to report any bleeding to her healthcare provider. Most women proceed to abortion regardless of treatment. If the products of conception do not pass completely or bleeding becomes excessive, a dilation and curettage (D&C) procedure is generally performed. The D&C involves dilating the uterine cervix and scraping the endometrium of the uterus to empty the contents of the uterus.
Women who are experiencing bleeding and cramping during pregnancy may be admitted to hospital. Vital signs and estimated blood loss are monitored, and any tissue or blood clots that might contain tissue for products of conception are examined. Women are often very distressed and experience both physical and emotional pain during and following a miscarriage. Nurses should use comfort measures to provide needed physical and mental rest and arrange for someone to stay with the patient, as emotional support is important. Nurses should be aware of the grieving process that results from the loss of a pregnancy.4 Support of the patient and her family is essential.
CLINICAL PRACTICE
Situation
A recently married 39-year-old woman is informed that the results of her amniocentesis indicate that her fetus has major chromosomal abnormalities and is expected to have severe physical and mental disabilities. The patient has no children, but her husband has three children from a previous marriage. She asks you what she should do. How would you respond?
Important points for consideration
• Decisions about whether to continue a pregnancy with a child who has severe disabilities are extremely personal and emotional. The woman and her husband will need support and information to explore their options and their values.
• Pregnancy counselling is warranted about the woman’s choices, her feelings about the pregnancy, her desire to have a child with her husband, her concerns about raising a child with severe disabilities, her feelings about abortion and concerns about possible future pregnancies.
• Patient autonomy ensures that a woman may decide for herself whether or not to continue a pregnancy.
• Abortion or termination of a pregnancy is available in all states and territories in Australia and New Zealand provided a doctor considers it necessary to preserve the woman from serious danger to her life or to her physical or mental health. In Victoria and the Australia Capital Territory abortion is available on a woman’s request. Queensland has the most restrictive law, but all abortions may be the subject of criminal law. Each state and territory in Australia has legislation prohibiting unlawful abortion. Under the Crimes Act 1961 and the Contraception, Sterilisation and Abortion Act 1977 in New Zealand, abortion is permitted under certain circumstances.
• The role of the healthcare professional in these difficult situations is to provide education and support, to remain neutral and to facilitate a decision consistent with the patient’s values.
INDUCED ABORTION
Induced abortion is the intentional or elective termination of a pregnancy. Induced abortion is done for personal reasons (at the request of the woman) and for medical reasons. Several techniques are used to induce abortion, including menstrual extraction, suction curettage, dilation and evacuation (D&E), and drug therapy. Deciding which technique to use to terminate a pregnancy depends on the gestational age (length of the pregnancy) and the woman’s condition. Table 53-2 lists current methods for induced abortion.
Suction curettage may be performed up to 14 weeks of gestation and accounts for more than 90% of abortion procedures. Drug therapy is another method to induce abortion (medical abortion) early in pregnancy. The drug agents must be given within the first 49 days of pregnancy (day 1 being the first day of the last menstrual period). Mifepristone works by blocking progesterone, a hormone needed for pregnancy to continue. It is given in combination with misoprostol, an agent that produces uterine contractions, resulting in expulsion of the products of conception. In rare cases, fatal bacterial infections have been associated with mifepristone.5 Methotrexate, also given in combination with misoprostol, is another option for medically induced abortions. Methotrexate induces abortion because of its toxicity to trophoblastic tissue. Misoprostol induces uterine contractions.
Once the decision is made to have an abortion, the woman and her significant others need support and acceptance. The patient needs to be prepared for what to expect both emotionally and physically. Grief and sadness are normal emotions after an abortion. The patient needs to understand the procedure, including instructions for preprocedure and postprocedure care. The nurse’s caring attitude can be a positive factor in the patient’s experience.
After the procedure, the patient should be taught the signs and symptoms of possible complications, such as abnormal vaginal bleeding, severe abdominal cramping, fever and foul drainage. The nurse should also stress to the patient to avoid intercourse and vaginal insertions until re-examination, which needs to be in 2 weeks. Contraception can be started the day of the procedure or during the patient’s return visit in accordance with her needs and desires.
![]() DRUG ALERT—oral contraceptives (both oestrogen and progesterone)
DRUG ALERT—oral contraceptives (both oestrogen and progesterone)
• May increase the risk of cervical, liver and perhaps breast cancer.
• May elevate blood pressure and cholesterol (related to oestrogen).
• Increase the risk of cardiac disease if the patient also smokes.
• May impair the effectiveness of concurrent use of antibiotics.
• Are contraindicated in patients with migraine headaches and depression.
PROBLEMS RELATED TO MENSTRUATION
The normal menstrual cycle is discussed in Chapter 50, and the hormonal changes related to the menstrual cycle are shown in Figure 50-8. Menstruation may be irregular during the first few years after menarche and the years preceding menopause. Once established, a woman’s menstrual cycle usually has a predictable pattern. However, considerable normal variation exists in cycle length, as well as in the duration, amount and character of the menstrual flow (see Table 50-2).
Premenstrual syndrome
Premenstrual syndrome (PMS) is a symptom complex related to the luteal phase of the menstrual cycle.6 The symptoms can be severe enough to impair interpersonal relationships or interfere with usual activities. Because many symptoms may be associated with PMS, it is difficult to concisely define it. However, PMS symptoms always occur cyclically during the luteal phase before the onset of menstruation and are not present at other times of the month.
AETIOLOGY AND PATHOPHYSIOLOGY
The aetiology and pathophysiology of PMS are not well understood. It may have a biological trigger with compounding psychosocial factors. Neurotransmitters, such as serotonin, could also be involved. Some women may have a genetic predisposition to PMS. Other proposed causes of PMS include hormone imbalance and nutritional deficiencies. Premenstrual dysphoric disorder (PMD-D) is the term applied to a type of PMS. Women with PMD-D have a severe mood disorder in addition to PMS.
CLINICAL MANIFESTATIONS
PMS is extremely variable in its clinical manifestations. Variation is common between women and, for an individual woman, from one cycle to another. Common physical symptoms include breast discomfort, peripheral oedema, abdominal bloating, sensation of weight gain, episodes of binge eating and headaches. Abdominal bloating and breast swelling are caused by fluid shifts because total body weight does not generally change. Symptoms of autonomic nervous system arousal (e.g. heart palpitations, dizziness) have been reported by women with PMS. Anxiety, depression, irritability and mood swings are some of the emotional symptoms that women may experience.
DIAGNOSTIC STUDIES AND MULTIDISCIPLINARY CARE
PMS can be diagnosed only when other possible causes for the symptoms have been ruled out. A focused health history and physical examination should be undertaken to identify any underlying conditions such as thyroid dysfunction, uterine fibroids or depression that may account for the symptoms. No definitive diagnostic test is available for PMS. When PMS or PMD-D is a possible diagnosis, the patient is given a symptom diary to record her symptoms prospectively for two or three menstrual cycles. Diagnosis is based on an evaluation of the woman’s symptoms.
Non-drug and drug strategies can relieve some PMS symptoms (see Box 53-2). However, no single treatment is available. The goal of treatment is to reduce the severity of symptoms and enhance the woman’s sense of control and quality of life.
Several conservative approaches to managing PMS symptoms are considered helpful, including stress management, diet changes, exercise, education and counselling. Techniques for stress reduction include yoga, meditation, imagery and biofeedback. To decrease autonomic nervous system arousal, women should avoid caffeine, reduce their dietary intake of refined carbohydrates, exercise on a regular basis and practise relaxation techniques. Eating complex carbohydrates with high fibre, foods rich in vitamin B6 and sources of tryptophan (dairy and poultry) are thought to promote serotonin production, which improves the symptoms. Vitamin B6 may be found in foods such as pork, milk, egg yolks and legumes. Although no strongly supportive data exist, limiting salt intake before menstruation and increasing calcium intake have been proposed to alleviate fluid retention, weight gain, bloating, breast swelling and tenderness.
Exercise results in a release of endorphins, leading to mood elevation. Aerobic exercise can also have a relaxing effect. Because fatigue tends to exaggerate the symptoms of PMS, adequate rest in the premenstrual period is a priority.
Explanations about PMS will help the patient to understand the complexity of the disorder and ways that she can regain a better sense of control. Assuring women that their symptoms are real and they are not ‘crazy’ may be helpful. Teaching the woman’s partner about the nature of PMS assists the partner to better understand PMS and to provide support to the woman in making lifestyle changes to reduce the symptoms of PMS.
Drug therapy
Drug therapy is considered when symptoms persist or interfere with daily functioning. Presently, no single drug can treat all the symptoms associated with PMS. One therapy may be tried for a time, and if no improvement is noted, another approach can be tried. Many treatments are symptom specific. For fluid retention, diuretics such as spironolactone are used. For reducing cramping pain, backache and headaches, prostaglandin inhibitors such as ibuprofen are used. To improve negative mood, vitamin B6 supplementation (50 mg daily) may be used. Calcium and magnesium supplementation may also be effective in alleviating psychological and physiological symptoms. For anxiety, buspirone taken during the luteal phase helps some women. Women with PMD-D may benefit from taking antidepressants, including fluoxetine and tricyclic antidepressants (e.g. amitriptyline).
Other drug treatments are directed at PMS in general. Selective serotonin reuptake inhibitors (SSRIs; e.g. sertraline) have provided significant relief to some women with severe PMS.7 Other general treatment includes oral contraceptives containing oestrogen and progesterone. Evening primrose oil may help some women.
Dysmenorrhoea
Dysmenorrhoea is abdominal cramping pain or discomfort associated with menstrual flow. The degree of pain and discomfort varies with the individual. The two types of dysmenorrhoea are primary (no pathology exists) and secondary (pelvic disease is the underlying cause). Dysmenorrhoea is one of the most common gynaecological problems, affecting approximately 50% of all women.8
AETIOLOGY AND PATHOPHYSIOLOGY
Primary dysmenorrhea is not a disease. It is caused by an excess of prostaglandin F2α (PGF2α) and/or an increased sensitivity to it. Stimulation of the endometrium by oestrogen, followed by progesterone, results in a dramatic increase in prostaglandin production by the endometrium. With the onset of menses, degeneration of the endometrium releases prostaglandin. Locally, prostaglandins increase myometrial contractions and constriction of small endometrial blood vessels. This causes tissue ischaemia and increased sensitisation of the pain receptors, resulting in menstrual pain. Primary dysmenorrhoea begins in the first few years after menarche, typically with the onset of regular ovulatory cycles.
Secondary dysmenorrhoea is usually acquired after adolescence, occurring most commonly at 30 to 40 years of age. Common pelvic conditions that cause secondary dysmenorrhoea include endometriosis, chronic pelvic inflammatory disease and uterine fibroids. Because secondary dysmenorrhoea is caused by many conditions, symptoms vary. However, painful menses is present in all situations.
CLINICAL MANIFESTATIONS
Primary dysmenorrhoea starts 12–24 hours before the onset of menses. The pain is most severe the first day of menses and rarely lasts more than 2 days. Characteristic manifestations include lower abdominal pain that is colicky in nature, frequently radiating to the lower back and upper thighs. The abdominal pain is often accompanied by nausea, diarrhoea, loose stools, fatigue, headache and light-headedness.
Secondary dysmenorrhoea usually occurs after the woman has experienced problem-free periods for some time. The pain may be unilateral and it is generally more constant and continues longer than in primary dysmenorrhoea. Depending on the cause, symptoms such as dyspareunia (painful intercourse), painful defecation or irregular bleeding may occur at times other than menstruation.
MULTIDISCIPLINARY CARE
Evaluation begins with distinguishing primary from secondary dysmenorrhoea. A complete health history should be obtained, paying special attention to the menstrual and gynaecological history. A pelvic examination should be performed by the healthcare provider. The probable diagnosis is primary dysmenorrhoea if the history reveals an onset shortly after menarche, symptoms are only associated with menses and the pelvic examination is normal. If a specific cause of dysmenorrhoea is evident, the diagnosis is secondary dysmenorrhoea.
Treatment for primary dysmenorrhoea includes heat, exercise and drug therapy. Heat is applied to the lower abdomen or back. Regular exercise is beneficial because it may reduce endometrial hyperplasia and subsequent prostaglandin production. Primary drug therapy is non-steroidal anti-inflammatory drugs (NSAIDs) such as naproxen, which has anti-prostaglandin activity. NSAIDs should be started at the first sign of menses and continued every 4–8 hours to maintain a sufficient level of the drug to inhibit prostaglandin synthesis for the usual duration of discomfort. Oral contraceptives may also be used. They decrease dysmenorrhoea by reducing endometrial hyperplasia.
Acupuncture and transcutaneous nerve stimulation provide varying degrees of relief. (See Ch 7 for a discussion of acupuncture.) These methods may be used for women who obtain inadequate relief from medications or who prefer not to take medications. Patients who are unresponsive to these treatments should be evaluated for chronic pelvic pain.
Treatment of secondary dysmenorrhoea depends on the cause. Some individuals with secondary dysmenorrhoea will be helped by the approaches used for primary dysmenorrhoea. Depending on the underlying causes of dysmenorrhoea, additional drug or surgical interventions are used.
 NURSING MANAGEMENT: DYSMENORRHOEA
NURSING MANAGEMENT: DYSMENORRHOEA
One of the primary nursing roles is teaching. The nurse should instruct women on why dysmenorrhoea occurs, as well as how to treat it. This will provide them with a foundation for coping with this common problem and increase feelings of control and self-reliance.
Women often ask what can be done to relieve the minor discomfort associated with menstrual cycles. The nurse should advise that during acute pain, relief may be obtained by applying heat to the abdomen or back and taking NSAIDs for analgesia.9 Non-invasive pain-relieving practices such as distraction and guided imagery can also be suggested. Other healthcare measures to reduce the discomfort of dysmenorrhoea include regular exercise and proper nutritional habits. Avoiding constipation, maintaining good body mechanics and eliminating stress and fatigue, particularly during the time preceding menstrual periods, can also decrease discomfort.
Abnormal vaginal bleeding
Abnormal vaginal or uterine bleeding is a common gynaecological concern. Abnormalities include oligomenorrhoea (long intervals between menses, generally greater than 35 days), amenorrhoea (absence of menstruation), menorrhagia (excessive or prolonged menstrual bleeding) and metrorrhagia (irregular bleeding or bleeding between menses). The cause of abnormal bleeding may vary from anovulatory menstrual cycles to more serious causes such as ectopic pregnancy or endometrial cancer. The age of the woman provides direction for identifying the cause of bleeding. For example, a postmenopausal woman with abnormal bleeding must always be evaluated for endometrial cancer but does not need to be evaluated for possible pregnancy. For a 20-year-old woman with abnormal bleeding, the possibility of pregnancy must always be considered and the possibility of endometrial cancer would be unlikely. When bleeding is due to a disruption in the menstrual cycle (e.g. anovulation) it is called dysfunctional uterine bleeding.
Abnormal bleeding may be caused by dysfunction of the hypothalamic–pituitary–ovarian axis such as a pituitary adenoma. Another cause may be infection. Changes in lifestyle such as marriage, recent moves, a death in the family, financial stress and other emotional crises can also cause irregular bleeding. Because psychological factors can influence endocrine function, they should be considered when the patient is evaluated.
TYPES OF IRREGULAR BLEEDING
Oligomenorrhoea and secondary amenorrhoea
Anovulation is the most common cause for missing menses once pregnancy has been ruled out. Additional causes of amenorrhoea are listed in Box 53-3. Primary amenorrhoea refers to the failure of the menstrual cycle to begin by age 16 years or by age 14 years if secondary sex characteristics are present. Secondary amenorrhoea refers to the cessation of the menstrual cycle once established.
BOX 53-3 Causes of amenorrhoea
Hypothalamic–pituitary axis
Ovaries
• Autoimmune disease (often involving thyroid, adrenal and islet cells)
• Congenital or genetic conditions (e.g. Turner’s syndrome)*
• Infection (e.g. mumps, oophoritis)
*Usually manifests as primary amenorrhoea.
Ovulation is often erratic for several years following menarche and before menopause. Thus oligomenorrhoea due to anovulation is common for women at the beginning and end of menstruation.10 In anovulatory cycles, the corpus luteum that produces progesterone does not form. This may result in a situation referred to as unopposed oestrogen. When unopposed by progesterone, oestrogen can cause excessive build-up of the endometrium. Persistent overgrowth of the endometrium increases a woman’s risk for endometrial cancer. To reduce this risk, progesterone or oral contraceptives are prescribed to ensure that the patient’s endometrial lining will be shed at least four to six times per year.
Menorrhagia
The excessive bleeding associated with menorrhagia can be characterised as an increased duration (more than 7 days) or an increased amount (more than 80 mL), or both. Anovulatory uterine bleeding is the most common cause of menorrhagia. An unopposed oestrogen state continues to build up the endometrium until it becomes unstable, resulting in menorrhagia. For young women with excessive bleeding, clotting disorders must be considered. Uterine fibroids (also called leiomyomas) and endometrial polyps are common causes of menorrhagia for women in their thirties and forties.
Metrorrhagia
Metrorrhagia, also referred to as spotting or breakthrough bleeding, is bleeding between menstrual periods. For all reproductive-age women, pregnancy complications such as spontaneous abortion or ectopic pregnancy must be considered as a possible cause. Other causes include cervical or endometrial polyps, infection and cancer. Spotting is common during the first three cycles of oral contraceptives. If spotting continues past the woman’s third cycle using oral contraceptives, a different pill formulation can be prescribed when other causes of metrorrhagia have been ruled out. Spotting with long-acting progestogen therapy (e.g. Mirena IUD) or progestogen-only pills is also common. For postmenopausal women, endometrial cancer must be considered whenever spotting is experienced. In postmenopausal women, exogenous oestrogen administration during hormone replacement therapy is a common cause of metrorrhagia. Menometrorrhagia is excessive bleeding that occurs at irregular intervals. It may be caused by endometrial cancer or uterine fibroids.
DIAGNOSTIC STUDIES AND MULTIDISCIPLINARY CARE
Because abnormal vaginal bleeding has multiple causes, the diagnostic and multidisciplinary care varies. A health history and physical examination directed at the most likely causes of vaginal bleeding for the woman’s age-group is the first step. These findings will provide the basis for selecting the necessary laboratory tests and diagnostic procedures. Treatment depends on the aetiology of the problem (e.g. menorrhagia, amenorrhoea), the degree of threat to the patient’s health and whether children are desired in the future.
Combined oral contraceptives may be prescribed for a woman with amenorrhoea to ensure regular shedding of the endometrium if she also wants contraception. If she wants to become pregnant, a fertility drug may be prescribed. If she does not need birth control, progesterone may be prescribed to ensure a shedding of the endometrial lining four to six times per year. Tranexamic acid, a non-hormonal product, may be used to treat heavy menstrual bleeding. This drug stabilises a protein that helps blood to clot. Side effects may include headaches, sinus and nasal symptoms, back pain, abdominal pain, muscle and joint pain, muscle cramps, anaemia and fatigue. Use of tranexamic acid while taking hormonal contraceptives may increase the risk of blood clots, stroke or heart attack. Women using hormonal contraception should take tranexamic acid only if there is a strong medical need.
The treatment goal for women with menorrhagia is to minimise further blood loss. If menorrhagia is the result of anovulatory cycles, the endometrium must be stabilised by a combination of oral oestrogen and progesterone.
Balloon thermotherapy is a technique for menorrhagia that involves the introduction of a soft, flexible balloon into the uterus; the balloon is then inflated with sterile fluid (see Fig 53-2). The fluid in the balloon is heated and maintained for 8 minutes, thus causing ablation (removal) of the uterine lining. When the treatment is completed, the fluid is withdrawn from the balloon and the catheter is removed from the uterus. The uterine lining sloughs off in the following 7–10 days. Uterine balloon thermotherapy is contraindicated for women who desire to maintain their fertility and for women with any suspected uterine abnormalities such as fibroids, suspected endometrial cancer, prior caesarean section or myomectomy. With severe bleeding, hospitalisation is indicated. All patients with menorrhagia should be evaluated for anaemia and treated as indicated.

Figure 53-2 Balloon thermotherapy for treatment of menorrhagia. A, A balloon-tipped catheter is inserted into the uterus through the vagina and cervix. B, The balloon is inflated with a sterile fluid that expands to fit the size and shape of the uterus. The fluid is heated to 87°C and maintained for 8 minutes while the uterine lining is treated. C, Fluid is withdrawn from the balloon and the catheter is removed.
Surgical therapy
Surgery may be indicated depending on the underlying cause of the abnormal vaginal bleeding. D&C was once a common therapy for excessive bleeding or for spotting in perimenopausal women. Now D&C is used only in extreme cases of bleeding or for older women when endometrial biopsy and ultrasonography have not provided the necessary diagnostic information. Endometrial ablation for menorrhagia may be done by laser, thermal balloon, cryotherapy, microwave energy or electrosurgical technique for patients who do not want to have children.10 If menorrhagia is caused by uterine fibroids, a hysterectomy (surgical removal of the uterus) may be performed. A myomectomy (removal of fibroids without removal of the uterus) may be performed if the patient wants to preserve her uterus. The myomectomy is done via laparotomy, laparoscopy or hysteroscopy. Hormonal regimens and embolisation of the blood vessels supplying the fibroid tumour are other treatment options.
 NURSING MANAGEMENT: ABNORMAL VAGINAL BLEEDING
NURSING MANAGEMENT: ABNORMAL VAGINAL BLEEDING
Infrequent or no menses may or may not be seen as a desirable state by the patient. Teaching women about the characteristics of the menstrual cycle will enable them to identify normal variations.
Table 50-2 includes characteristics of the menstrual cycle and related patient teaching. This knowledge can diminish apprehension and dispel misconceptions about the menstrual cycle. If the patient’s menstrual cycle pattern does not fall within the normal range, she should be advised to visit her healthcare provider. Myths concerning activities allowed during menstruation are common. The nurse should be prepared to clarify the facts: bathing and hair washing are safe; a daily warm bath may help relieve pelvic discomfort; women can swim, exercise, have intercourse and basically continue their usual daily activities.
Frequent changing of tampons or pads meets comfort and hygiene needs during menstruation. The selection of internal or external sanitary protection is a matter of personal preference. Tampons are convenient and make menstrual hygiene easier, whereas pads may provide better protection. Using a combination of tampons and pads and avoiding prolonged use of superabsorbent tampons may decrease the risk of toxic shock syndrome (TSS). TSS is a rare, but acute, life-threatening condition caused by a toxin from Staphylococcus aureus. TSS causes high fever, vomiting, diarrhoea, weakness, myalgia and a sunburn-like rash.11
Whenever excessive, the amount of the patient’s vaginal bleeding should be assessed as accurately as possible. The number and size of pads or tampons used and the degree of saturation should be reported and recorded. The patient’s fatigue level, along with variations in blood pressure and pulse, should be monitored because anaemia and hypovolaemia may be present. For the patient requiring a surgical procedure, the nurse should provide the appropriate preoperative and postoperative care.
Ectopic pregnancy
An ectopic pregnancy is the implantation of a fertilised ovum anywhere outside the uterine cavity. Ectopic pregnancy is a life-threatening condition. Earlier identification has contributed to a decrease in mortality rates; however, approximately 3 million women are diagnosed annually with ectopic pregnancy (up to 3% of all pregnancies).12 Approximately 98% of ectopic pregnancies occur in the fallopian tube (see Fig 53-3). The remaining 2–3% may be ovarian, abdominal or cervical.

Figure 53-3 Sites of implantation of ectopic pregnancies. Order of frequency of occurrence is ampulla, isthmus, interstitium, fimbria, tubo-ovarian ligament, ovary, abdominal cavity and cervix (external os).
AETIOLOGY AND PATHOPHYSIOLOGY
Any blockage of the tube or reduction of tubal peristalsis that impedes or delays the zygote passing to the uterine cavity can result in tubal implantation. After implantation, the growth of the gestational sac expands the tubal wall. Eventually the tube ruptures, causing acute peritoneal symptoms. Less acute symptoms usually begin within 6–8 weeks after the last normal menstrual period and weeks before rupture would occur.
Risk factors for ectopic pregnancy include a history of pelvic inflammatory disease, prior ectopic pregnancy, current progestin-releasing intrauterine device (IUD), progestin-only birth control failure and prior pelvic or tubal surgery. Additional risk factors for ectopic pregnancy include procedures used in infertility treatment, including IVF procedures, embryo transfer and ovulation induction.
CLINICAL MANIFESTATIONS
The classic symptoms of ectopic pregnancy are abdominal or pelvic pain, missed menses and irregular vaginal bleeding. Other symptoms include amenorrhoea, morning sickness, breast tenderness, gastrointestinal disturbance, malaise and syncope. Pain is almost always present and is caused by distension of the fallopian tube. It may start unilaterally and then spread to become bilateral. The character of the pain varies among women and can be colicky or vague. If tubal rupture occurs, the pain is intense and may be referred to the shoulder as a result of irritation of the diaphragm by blood released into the abdominal cavity. Symptom severity does not necessarily correlate with the extent of external bleeding present. With rupture, the risk of haemorrhage and hypovolaemic shock is present. Suspected rupture is treated as an emergency.
The vaginal bleeding that may accompany ectopic pregnancy is usually described as spotting. However, it is also possible that bleeding may be heavier and can be confused with menses.
DIAGNOSTIC STUDIES
Because of the life-threatening nature of ectopic pregnancy, it should be considered whenever pregnancy is even remotely possible. Ectopic pregnancy can be a diagnostic challenge because of its similarity to other pelvic and abdominal disorders, such as salpingitis, spontaneous abortion, ruptured ovarian cyst, appendicitis and peritonitis. A serum (radioimmunoassay) pregnancy test should be performed. If the test is negative, an ectopic pregnancy is not likely. If ectopic pregnancy cannot be excluded by the pregnancy test, further evaluation is warranted. If the patient is in a stable condition, a combination of serial serum β-hCG and vaginal ultrasonography is used. The β-hCG level is expected to double about every 48 hours in a normal pregnancy. If the β-hCG level fails to double, the patient may have an ectopic pregnancy. Transvaginal ultrasound can be used to confirm the presence of an intrauterine pregnancy once the β-hCG level has reached 1500–2000 mIU/mL.13
Absence of a normal intrauterine pregnancy means that the diagnosis is probably a spontaneous abortion or an ectopic pregnancy. With a spontaneous abortion serial serum β-hCG levels will decrease over time. A complete blood count is obtained when there is any concern regarding the amount of blood loss or if surgery is contemplated. A gradually decreasing haematocrit may indicate internal bleeding.
 NURSING AND COLLABORATIVE MANAGEMENT: ECTOPIC PREGNANCY
NURSING AND COLLABORATIVE MANAGEMENT: ECTOPIC PREGNANCY
Surgery remains the primary approach for treating ectopic pregnancies and should be performed immediately. However, medical management with methotrexate is being used with increasing success with patients who are haemodynamically stable and have a mass less than 3 cm in size. A conservative surgical approach limits damage to the reproductive system as much as possible. Removal of the pregnancy from the tube is preferred to removing the tube. Laparoscopy is preferable to laparotomy, because it decreases blood loss and the length of the hospital stay (see Fig 53-4). If the tube ruptures, conservative surgical approaches may not be possible. The patient may need a blood transfusion and supplemental intravenous (IV) fluid therapy to relieve shock and restore a satisfactory blood volume for safe anaesthesia and surgery. The use of microsurgery techniques has resulted in fewer repeated ectopic pregnancies and a higher rate of future successful pregnancies.
Nursing care depends on the condition of the patient. Before the diagnosis has been confirmed, the nurse should be alert to patient signs of increasing pain and vaginal bleeding, which may indicate that rupture of the tube has occurred. Vital signs are monitored closely, along with observation for signs of shock. The nurse should give explanations and prepare the patient for diagnostic procedures when appropriate. Preparation of the patient for abdominal surgery may follow rapidly. The nurse should assess the patient’s emotional status and give reassurance and support for the surgery to the patient and her family. Postoperatively, the patient may express a fear of future ectopic pregnancies and have many questions about the impact of this experience on her future fertility.
Perimenopause and postmenopause
The perimenopause is a normal life transition that begins with the first signs of change in the menstrual cycle and ends after cessation of menses. Menopause is the physiological cessation of menses associated with declining ovarian function. It is usually considered complete after 1 year of amenorrhoea (absence of menstruation). Menopause starts gradually and is usually associated with changes in menstruation, including menstrual flows that are increased, decreased and/or irregular. Cessation of menses finally occurs. Postmenopause refers to the time in a woman’s life after menopause.
The age at which menopause occurs ranges from 44 to 55 years, with an average age of 51 years.14 Menopause may occur earlier due to illness, surgical removal of the uterus or both ovaries, side effects of radiation therapy or chemotherapy, or drugs. The age at which menopause occurs is not affected by age at menarche, physical characteristics, number of pregnancies, date of last pregnancy or oral contraceptive use. However, genetic factors, autoimmune conditions, cigarette smoking and racial/ethnic factors have been linked to an earlier age at menopause.15
Changes within the ovary start the cascade of events that finally result in menopause. The regression of the follicles within each ovary begins at puberty and accelerates after age 35. With age, fewer follicles remain that are responsive to follicle-stimulating hormone (FSH). FSH normally stimulates the dominant follicle to secrete oestrogen. When the follicles can no longer respond to FSH, the production of oestrogen and progesterone from the ovary declines. However, perimenopausal women can get pregnant until menopause has occurred. This is due to many women having long anovulatory cycles interspersed with shorter, ovulatory cycles.
With decreased ovarian function, decreased levels of oestrogen cause a gradual increase in FSH and LH as a result of the negative feedback process. By the time menopause occurs, there is a 10-fold to 20-fold increase in FSH. The elevated FSH level may take several years to return to the premenopausal level. The reduced oestrogen level also causes a decrease in the frequency of ovulation and results in changes in the reproductive organs and tissues (e.g. atrophy of vaginal tissue).
CLINICAL MANIFESTATIONS
Clinical manifestations of perimenopause and menopause are presented in Table 53-3. Perimenopause is a time of erratic hormonal fluctuation. Irregular vaginal bleeding is common. With decreasing oestrogen, hot flushes and other symptoms begin. The signs and symptoms of diminished oestrogen are listed in Box 53-4. The loss of oestrogen plays a significant role in the cause of age-related alterations. Changes most critical to a woman’s wellbeing are the increased risks for coronary artery disease (CAD) and osteoporosis (secondary to bone density loss). Other changes include a redistribution of fat, a tendency to gain weight more easily, muscle and joint pain, loss of skin elasticity, changes in hair amount and distribution, and atrophy of external genitalia and breast tissue.
Hallmarks of the perimenopause include vasomotor instability (hot flushes) and irregular menses. A hot flush is described as a sudden sensation of intense heat along with perspiration and flushing.16 These sensations may last from several seconds to 5 minutes and occur most often at night, thereby disturbing sleep. The cause of hot flushes, or vasomotor instability, is not clearly understood. It has been theorised that temperature regulators in the brain are in proximity to the area where gonadotropin-releasing hormone (GnRH) is released. The lowered oestrogen levels are correlated with dilation of cutaneous blood vessels resulting in hot flushes and increased sweating. The more sudden the withdrawal of oestrogen (e.g. surgical removal of the ovaries), the more likely the symptoms will be severe if no hormone replacement is provided. These symptoms subside over time with or without hormone replacement therapy. Hot flushes can be triggered by stress and situations that affect body temperature, such as eating a hot meal, hot weather or warm clothing.
Atrophic vaginal changes secondary to decreased oestrogen include thinning of the vaginal mucosa and the disappearance of rugae. Vaginal secretions also decrease and become more alkaline. As a result of these changes, the vagina is easily traumatised and more susceptible to infection, including a higher risk for human immunodeficiency virus (HIV) transmission if exposed. Dyspareunia (painful intercourse) may also occur. This can lead to unnecessary and premature cessation of sexual activity. Dryness is a problem that can be corrected easily with water-soluble lubricants or, if needed, hormonal creams or systemic hormone replacement therapy.
Atrophic changes in the lower urinary tract also occur with a decrease in oestrogen. Bladder capacity decreases and the bladder and urethral tissue lose tone. These changes can cause symptoms that mimic a bladder infection (e.g. dysuria, urgency, frequency) when no infection is present.
Whether decreasing oestrogen causes the psychological changes associated with perimenopause is unclear. The attributed depression, irritability and cognitive problems could result from life stressors or sleep deprivation from hot flushes. Depressive symptoms appear to improve when hormone levels stabilise.17
MULTIDISCIPLINARY CARE
The diagnosis of perimenopause should be made only after careful consideration of other possible causes for the woman’s symptoms. Depression, thyroid dysfunction, anaemia or anxiety could be responsible for the same symptoms. An accurate history of menstrual patterns should be reviewed as part of establishing the diagnosis.18 Because of the hormonal fluctuations that occur before menopause, routine testing of the serum FSH level is not indicated.
Drug therapy
Hormone replacement therapy (HRT) was once standard therapy in many Western countries for treating menopausal symptoms. HRT includes oestrogen for women without a uterus or oestrogen and progesterone for women with a uterus. Since 2002, findings from the Women’s Health Initiative (WHI) clinical trials have changed this practice. The data from this study showed that women who had taken oestrogen plus progestin had an increased risk of breast cancer, stroke, heart disease and emboli. However, the women in the study also had fewer hip fractures and a lower risk of developing colorectal cancer. In women who took only oestrogen there was an increased risk for stroke and emboli.19 However, these women had decreased risk for fractures with no increased risk for heart disease or breast or colorectal cancer. Neither oestrogen plus progestin nor oestrogen alone affected the risk of death.19
If women wish to consider taking HRT for the short-term treatment (4–5 years) of menopausal symptoms, the risks and benefits of therapy (e.g. minimises bone loss, hot flushes, vaginal atrophic changes) should be considered carefully. The decision to take HRT, and which hormones to take, should be discussed thoroughly between the woman and her healthcare provider. If a woman chooses to use HRT, the lowest effective dose should be used.20,21 The age that a woman starts HRT may determine her risk of heart disease. The risk appears to increase the further a woman moves away from menopause.
The side effects of oestrogen include nausea, fluid retention, headaches and breast enlargement. Side effects of progesterone include increased appetite, weight gain, irritability, depression, spotting and breast tenderness. A commonly used oestrogen preparation is 0.625 mg of conjugated oestrogen daily. For symptom relief, a higher dose may be needed. To receive the protective benefit of progesterone, 5–10 mg of medroxyprogesterone is indicated for 12 days of each month on a cyclic regimen or 2.5 mg if on a continuous regimen. If the oestrogen is increased for symptom relief, the progesterone should also be increased. Other forms of progesterone include micronised progesterone creams, dermal patches, gels and lotions; rings placed around the cervix; and subcutaneous pellets. Vaginal creams are especially useful for urogenital symptoms (e.g. dryness). Transdermal (skin patch) oestrogen has the advantage of bypassing the liver, but has the disadvantage of causing skin irritation.
Can hormone replacement therapy improve cognitive function?
EVIDENCE-BASED PRACTICE
Critical appraisal and synthesis of evidence
• 16 double-blind RCTs (n = 10,114) of postmenopausal healthy women 29 to >75 years old.
• Women without dementia on HRT (oestrogen alone or oestrogen and progesterone) for 2 weeks (short term) up to 5 years (long term).
• Cognitive function measured through global and specific tests including verbal and visual memory, attention and reasoning.
Implications for nursing practice
• Advise patients that HRT may be given as short-term therapy for menopausal symptoms such as intolerable hot flushes or night sweats.
• Counsel patients that current evidence does not support taking HRT to maintain cognitive function, and that HRT increases the risk of stroke and breast cancer.
P, patient population of interest; I, intervention or area of interest; C, comparison of interest or comparison group; O, outcome(s) of interest; T, time.
Antidepressants known as SSRIs, including paroxetine, fluoxetine and venlafaxine, are an effective alternative to HRT in reducing hot flushes. This effect is noted even if the user is not depressed.21 The mechanism of action is unknown. Clonidine, an antihypertensive drug, and gabapentin, an antiseizure drug, have also been shown to relieve hot flushes.
Selective oestrogen receptor modulators (SORMs), such as raloxifene, are also used in treating menopausal problems. These drugs have some of the positive benefits of oestrogen, such as preventing bone loss, without the negative effects, such as endometrial hyperplasia. Raloxifene competes with oestrogen for oestrogen receptor sites. It decreases bone loss and serum cholesterol while having minimal effects on breast and uterine tissue.
Bisphosphonates including alendronate and risedronate are also used to decrease the risk for osteoporosis in postmenopausal women. These drugs enhance bone mineral density by suppressing reabsorption. SORMs and bisphosphonates are discussed further in Chapter 63 with respect to their role in the management of osteoporosis.
Non-hormonal therapy
Because of the risks associated with HRT, alternative therapies are often tried by many women to relieve menopausal symptoms. Hot flush frequency and severity can be reduced by promoting measures that would lead to a decrease in heat production and an increase in heat loss. Keeping a cool environment and limiting caffeine and alcohol intake lowers heat production. Behavioural changes, such as relaxation techniques, may also help. To promote heat loss at night when hot flushes can disrupt sleep, increase air circulation in the room and avoid bedding that traps the heat (e.g. heavy quilts). Loose-fitting clothes do not retain body heat, whereas clothes with tight necks and wrists do. Cool cloths applied to flushed areas also aid in heat loss. A daily intake of vitamin E in doses up to 800 IU may also help reduce hot flushes in some women.
A focus on improving behaviours related to good nutrition with adequate amounts of exercise and sleep can help decrease anxiety and depression. Changing sleep patterns may be helped by avoiding alcohol and controlling hot flushes. Stress reduction techniques can promote a better night’s sleep by decreasing anxiety. A regular moderate program (three to four times per week) of aerobic and weight-bearing exercises can slow the process of bone loss and a tendency towards weight gain. Exercise is important for menopausal women in modifying CAD risk factors including stress, obesity, physical inactivity and hypertension.
Nutritional therapy
Good nutrition can decrease the risk of cardiovascular disease and osteoporosis in addition to assisting with vasomotor symptoms. A daily intake of about 125 kJ/kg of body weight is recommended. A decrease in metabolic rate and careless eating habits can cause the weight gain and fatigue often attributed to menopause. An adequate intake of calcium and vitamin D helps maintain healthy bones and counteracts loss of bone density. Postmenopausal women who are not receiving supplemental oestrogen should have a daily calcium intake of at least 1500 mg. Those who are taking oestrogen replacement need at least 1000 mg per day. Calcium supplements are best absorbed when taken with meals. Either dietary calcium or calcium supplements may be used (see Tables 63-8 and 63-9).
The diet should be high in complex carbohydrates and vitamin B complex, especially B6. Phyto-oestrogens from plant sources may reduce menopausal symptoms. Examples of foods containing phyto-oestrogens include soy, tofu, chickpeas and sunflower seeds. Herbal remedies, such as black cohosh, have become popular in treating menopausal symptoms (see Complementary & alternative therapies box). Consultation with an experienced herbal practitioner is recommended before initiating therapy. Many herbs can cause serious adverse effects.
Herbs and supplements for menopause
COMPLEMENTARY & ALTERNATIVE THERAPIES
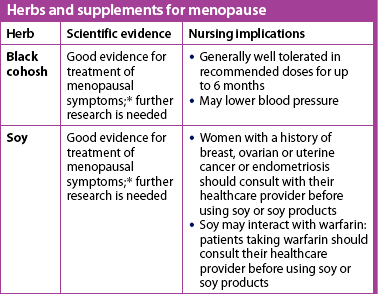
* Based on a systematic review of scientific literature. Available at www.naturalstandard.com, accessed 21 December 2010.
Culturally competent care: menopause
Menopause is a universal phase in a woman’s life, but the perception of this change varies by culture. Ethnic groups have their different traditions and beliefs regarding menopause. Nurses must be aware of the attitudes and beliefs regarding menopause among women from various ethnic and cultural backgrounds. In many cultures, menopause is considered a normal part of ageing and little emphasis is placed on the physical and emotional symptoms that accompany the loss of fertility. A study of Hindu women found that the women looked forward to menopause.22 In cultures where the elderly are revered, menopause is seen as a liberating transition to a state of being a ‘wise woman’.23
Western cultures generally have a negative attitude towards ageing and place high value on youth. Menopause is therefore often considered a disorder that requires treatment. Menopausal symptoms may be viewed as troublesome, with a strong need to treat hot flushes and mood swings. Numerous substances, from HRT to herbal preparations, are often used to treat menopausal symptoms.
Although menopause is experienced by all women, its meaning and symptoms vary. Menopause is a milestone in a woman’s life that is embedded in her own personality and her culture. Approaching the menopausal woman with this understanding is important in order to provide culturally competent care.
 NURSING MANAGEMENT: PERIMENOPAUSE AND POSTMENOPAUSE
NURSING MANAGEMENT: PERIMENOPAUSE AND POSTMENOPAUSE
Nurses have a key role in helping women to understand perimenopausal changes and options to minimise troublesome symptoms. Nurses should foster a positive image of perimenopause as a time of vitality and attractiveness. They should provide teaching and reassurance to perimenopausal women who experience difficulty in managing their symptoms, and explain that symptoms are normal and often are temporary. Non-drug approaches to managing symptoms should also be discussed, along with misconceptions about menopause, to reduce unnecessary anxiety.
Dry skin can be improved by the use of moisturising soaps and body lotions. Kegel exercises may help decrease stress incontinence (see Ch 46). Sexual function can continue with little change in the vast majority of postmenopausal women. Cessation of menstruation and ability to bear children should not be equated with cessation of sexual capability; in fact, it may be liberating. Femininity and libido do not disappear with menopause. Atrophic changes in vaginal epithelium associated with decreased oestrogen may lead to dyspareunia. A water-soluble lubricant is often effective in managing this problem. An active sex life helps increase lubrication and maintains the pliability of vaginal tissues. Provide the patient with an opportunity to candidly discuss concerns related to sexual functioning.
CONDITIONS OF THE VULVA, VAGINA AND CERVIX
AETIOLOGY AND PATHOPHYSIOLOGY
Infection and inflammation of the vagina, cervix and vulva commonly occur when the natural defences of the acid vaginal secretions (maintained by sufficient oestrogen levels) and the presence of Lactobacillus are disrupted. The woman’s resistance may also be decreased as a result of ageing, poor nutrition and the use of drugs that alter the bacterial flora or mucosa. Organisms gain entrance to the areas through contaminated hands, clothing and douche tips, and during intercourse, surgery and childbirth. Table 53-4 relates the specific aetiological factors, clinical manifestations and diagnostic methods, and multidisciplinary care of common infections and inflammations.
TABLE 53-4 Infections of the lower genital tract

HIV, human immunodeficiency virus; KOH, potassium hydroxide.
Most lower genital tract infections are related to sexual intercourse. Intercourse can transmit organisms, injure tissues and alter the acid–base balance of the vagina. Vulvar infections caused by viruses such as herpes and genital warts can be sexually transmitted when no lesions are apparent (see Ch 52 for discussion about sexually transmitted infections). Oral contraceptives, antibiotics and corticosteroids may produce changes in the vaginal pH and trigger an overgrowth of the organisms present. For example, Candida albicans may be present in small numbers in the vagina. An overgrowth of this organism causes vulvovaginitis.
CLINICAL MANIFESTATIONS
Abnormal vaginal discharge and reddened vulvar lesions are common clinical manifestations. In addition to a thick white curd-like discharge, women with vulvovaginal candidiasis (VVC) often experience intense itching and dysuria, which is the result of urine coming into contact with fissures and irritated areas on the vulva. The hallmark of bacterial vaginosis is the fishy odour of the discharge. Women with cervicitis may notice spotting after intercourse.
Common vulvar lesions include herpes infection and genital warts. Initial or primary herpes infections may be extremely painful. Herpes begins as a small vesicle followed by a superficial red ulcer. Most herpes lesions are painful. Dysuria is common when urine touches the lesion. Genital warts, caused by the human papillomavirus, vary in appearance. Irregularly shaped ‘cauliflower’ lesions are common. Genital warts are painless unless traumatised. (Herpes infection and genital warts are discussed in Ch 52.)
Postmenopausal older women may develop gynaecological problems such as lichen sclerosis.24 This chronic inflammatory condition is associated with intense itching in the genital skin area (e.g. labia minora, clitoris). The lesions are white with a ‘tissue paper’ appearance initially, although scratching produces changes in the appearance. The cause is unknown. High-potency topical corticosteroid ointment such as clobetasone helps to relieve itching.
MULTIDISCIPLINARY CARE
Genital problems should be evaluated by taking a history, performing a physical examination and obtaining the appropriate laboratory and diagnostic studies. Because many problems relate to sexual activity, a sexual history is essential. The nature of the problem directs specific aspects of the evaluation. Ulcerative lesions should be cultured for herpes. A blood test for syphilis may be done when ulcerative lesions are present. Genital warts are usually identified by their clinical appearance. Vulvar dystrophies may be examined via colposcopy with a biopsy taken for diagnosis.
Problems involving vaginal discharge are evaluated by microscopy and cultures. The most common vaginal conditions (i.e. bacterial vaginosis, VVC and trichomoniasis) are diagnosed by a procedure called a wet mount. The findings characteristic of each condition are shown in Table 53-4. To assess for cervicitis, endocervical cultures are obtained for Chlamydia and gonorrhoea. If purulent discharge is observed coming from the cervix, a sample of endocervical cells may be taken to conduct a Gram stain. The Gram-stained slide is examined with a microscope to identify white blood cells and gram-negative diplococci (indicative of gonorrhoea). (Sexually transmitted infections [STIs] are discussed in Ch 52.)
Drug therapy is based on the diagnosis and is shown in Table 53-4. Antibiotics taken as directed will cure bacterial infections. Antifungal preparations (in oral and cream preparations) are indicated for VVC. Women with vaginal conditions or cervical infection should abstain from intercourse for at least 1 week. Douching has been adversely linked to pelvic inflammatory disease, sexually transmitted infections and ectopic pregnancy and thus should be avoided.25 Sexual partners must be evaluated and treated if the patient is diagnosed with trichomoniasis, Chlamydia, gonorrhoea, syphilis or HIV.
Treatment of vulvar dystrophies is symptomatic because no cures are available. Treatment involves controlling the itching and hence the scratching. Interrupting the ‘itch–scratch cycle’ prevents further secondary damage to the skin.
 NURSING MANAGEMENT: CONDITIONS OF THE VULVA, VAGINA AND CERVIX
NURSING MANAGEMENT: CONDITIONS OF THE VULVA, VAGINA AND CERVIX
Nurses have the opportunity to teach women about common genital conditions and how to reduce their risks. Recognising symptoms that indicate a problem can help women seek care in a timely manner. Discussing problems that concern the patient’s genitals or sexual intercourse is frequently difficult. The nurse should use a non-judgemental attitude to make women feel more comfortable while empowering them to ask questions.
When a woman is diagnosed with a genital condition, the nurse should ensure that she fully understands the directions for treatment. Taking the full course of medication is especially important to decrease the chance of relapse. Because genitalia are such a private area, the use of graphs and models is especially helpful for patient teaching. When a woman will be using a vaginal medication for the first time, the nurse should show her the applicator and how to fill it, and explain where and how the applicator should be inserted (using visual aids or models). Vaginal creams should be inserted before going to bed so that the medication will remain in the vagina for a long period of time. Women using vaginal creams or suppositories may wish to use panty liners during the day when the residual medication may drain out.
Pelvic inflammatory disease
Pelvic inflammatory disease (PID) is an infectious condition of the pelvic cavity that may involve the fallopian tubes (salpingitis), ovaries (oophoritis) and pelvic peritoneum (peritonitis). A tubo-ovarian abscess may also form (see Fig 53-5). Chlamydia trachomatis and Neisseria gonorrhoeae are the most common causative organisms of PID. In Australia in 2007 notifications of Chlamydia infections were 250 per 100,000 population and Neisseria gonorrhoeae were 25 per 100,000 population.26 PID is not notifiable in New Zealand so it is difficult to know what the incidence is; however, an estimated 10–20% of women with Chlamydia may develop PID if they do not receive adequate treatment.27 PID is referred to as ‘silent’ when women do not perceive any symptoms. Other women with PID will be in acute distress. Pelvic pain may also be of a chronic nature.

Figure 53-5 Common routes of the spread of pelvic inflammatory disease. A, Direct spread of bacterial infection other than Neisseria gonorrhoeae. B, Direct spread of Neisseria gonorrhoeae.
AETIOLOGY AND PATHOPHYSIOLOGY
PID is often the result of untreated cervicitis. The organism infecting the cervix ascends higher into the uterus, fallopian tubes, ovaries and peritoneal cavity. These organisms, as well as anaerobes, mycoplasma, streptococci and enteric gram-negative rods, gain entrance during sexual intercourse or after pregnancy termination, pelvic surgery or childbirth. It is important to remember that not all cases of PID are the result of an STI.
Women at increased risk for Chlamydia infections (younger than 24 years of age, who have multiple sex partners or who have a new sex partner) should be routinely tested for Chlamydia. Chlamydia infections can be asymptomatic and unknowingly transmitted during intercourse. Silent PID is a major cause of female infertility.
Chronic pelvic pain is pain 6 months in duration or longer, and is located below the umbilicus and between the hips.28 Up to one-third of women have chronic pelvic pain after PID. Additional factors associated with chronic pelvic pain include interstitial cystitis, irritable bowel syndrome, adhesions, endometriosis and dysmenorrhoea.28
CLINICAL MANIFESTATIONS
Women with PID usually see a doctor because they are experiencing lower abdominal pain. The pain typically starts gradually and then becomes constant. The intensity may vary from mild to severe. Movement such as walking can increase the pain; pain is also frequently associated with intercourse. Spotting after intercourse and purulent cervical or vaginal discharge may also be noted. Fever and chills may be present. Women with less acute symptoms often notice increased cramping pain with menses, irregular bleeding and some pain with intercourse. Women who have mild symptoms may go untreated because either they did not seek care or the healthcare provider misdiagnosed their complaints.
PID is a clinical diagnosis based on the patient’s signs and symptoms. The diagnosis is determined from data obtained during the bimanual portion of the pelvic examination. Women with PID have lower abdominal tenderness, adnexal tenderness and positive cervical motion tenderness. Additional criteria useful for diagnosis may include fever and abnormal discharge (vaginal or cervical). Cultures for gonorrhoea and Chlamydia are also obtained, and a pregnancy test is done to rule out ectopic pregnancy. Drug therapy begins when minimal diagnostic criteria are met; thus treatment is not delayed for culture results. When the patient’s pain or obesity compromises the pelvic examination and a tubo-ovarian abscess may be present, a vaginal ultrasound is indicated.
COMPLICATIONS
Immediate complications of PID include septic shock and Fitz-Hugh–Curtis syndrome, which occurs when PID spreads to the liver and causes acute perihepatitis. The patient will have symptoms of right upper quadrant pain, but liver function tests will be normal. Tubo-ovarian abscesses may ‘leak’ or rupture, resulting in pelvic or generalised peritonitis. As the general circulation is flooded with bacterial endotoxins from the infected areas, septic shock may result. Embolisms may occur as the result of thrombophlebitis of the pelvic veins.
PID can cause adhesions and strictures to develop in the fallopian tubes. Ectopic pregnancy may result when a tube is partially obstructed because the sperm can pass through the stricture but the fertilised ovum cannot reach the uterus. After one episode of PID, the risk of having an ectopic pregnancy increases 10-fold. Further damage can obstruct the fallopian tubes and cause infertility.
MULTIDISCIPLINARY CARE
PID is usually treated on an outpatient basis. The patient is given a combination of antibiotics such as cefoxitin and doxycycline to provide broad coverage against the causative organisms. With effective antibiotic therapy, the pain should subside. The patient must have no intercourse for 3 weeks. Her partner(s) must be examined and treated. An important part of care is physical rest and oral fluids. Re-evaluation in 48–72 hours, even if symptoms are improving, is an essential part of outpatient care.
If outpatient treatment is unsuccessful or if the patient is acutely ill or in severe pain, admission to the hospital is indicated. If a tubo-ovarian abscess is present, hospitalisation is also indicated. Maximum doses of parenteral antibiotics are given in the hospital. Corticosteroids may be added to the antibiotic regimen to reduce inflammation, allowing for faster recovery and improvement in subsequent fertility. Application of heat to the lower abdomen or sitz baths may improve circulation and decrease pain. Bed rest in a semi-Fowler position promotes drainage of the pelvic cavity by gravity and may prevent the development of abscesses high in the abdomen. Analgesics to relieve pain and IV fluids to prevent dehydration are also used.
An indication for surgery is the presence of an abscess that fails to resolve with IV antibiotics. The abscess may be drained by laparoscopy or laparotomy. In extreme cases of infection or severe chronic pelvic pain, a hysterectomy may be performed. When surgery is necessary, the capacity for childbearing is preserved whenever possible.
Treatment for chronic pelvic pain should focus on the underlying disorder.28 If the source of the pain is unknown, treatment is directed at managing the symptoms.
 NURSING MANAGEMENT: PELVIC INFLAMMATORY DISEASE
NURSING MANAGEMENT: PELVIC INFLAMMATORY DISEASE
Subjective and objective data that should be obtained from the patient with PID are presented in Table 53-5. Prevention, early recognition and prompt treatment of vaginal and cervical infections can help prevent PID and its serious complications. The nurse should provide accurate information about factors that place a woman at increased risk for PID and urge women to seek medical attention for any unusual vaginal discharge or possible infection of their reproductive organs. The nurse should also inform patients that not all discharge indicates infection, but that early diagnosis and treatment of an infection, if present, can prevent serious complications. Patients should be taught methods to decrease the risk of getting STIs and to recognise the signs of infection in their partner(s).
The patient may have guilt feelings about having PID, especially if it is associated with an STI. She may also be concerned about the complications associated with PID, such as adhesions and strictures of the fallopian tubes, infertility and the increased incidence of ectopic pregnancy. Discussing such feelings and concerns may assist the patient to cope more effectively with them.
For patients requiring hospitalisation, nurses have an important role in implementing drug therapy, monitoring the patient’s health status and providing symptom relief and patient teaching. The nurse records vital signs and the character, amount, colour and odour of the vaginal discharge. The nurse also explains the need for limited activity, being in a semi-Fowler’s position and increased fluid intake. Assessing the degree of abdominal pain will provide information about the effectiveness of drug therapy.
Endometriosis
Endometriosis is the presence of normal endometrial tissue in sites outside the endometrial cavity. The most frequent sites are in or near the ovaries, the uterosacral ligaments and the uterovesical peritoneum (see Fig 53-6). However, endometrial tissues can be in many other locations such as the stomach, lungs, intestines and spleen. The tissue responds to the hormones of the ovarian cycle and undergoes a mini–menstrual cycle similar to the uterine endometrium.
The typical patient with endometriosis will be in her late twenties or early thirties, white and never had a full-term pregnancy. Although it is not a life-threatening condition, endometriosis can cause considerable pain. It also increases the risk of ovarian cancer. Endometriosis is one of the most common gynaecological problems and is estimated to affect 10% of all women and between 30% and 50% of women with infertility.29
AETIOLOGY AND PATHOPHYSIOLOGY
The aetiology is poorly understood, and many theories about the cause of endometriosis have been proposed. A widely held view is that retrograde menstrual flow passes through the fallopian tubes carrying viable endometrial tissues into the pelvis. The tissue attaches to various sites shown in Figure 53-6. Another theory suggests that undifferentiated embryonic peritoneal cavity cells remain dormant in the pelvic tissue until the ovaries produce sufficient hormones to stimulate their growth. Other proposed causes include a genetic predisposition and altered immune function.
CLINICAL MANIFESTATIONS
In patients with endometriosis a wide range of clinical manifestations and severity exists. The magnitude of a woman’s symptoms does not necessarily correlate with the clinical extent of her endometriosis. Dysmenorrhoea after years of relatively pain-free menses and infertility may serve as clues to the presence of endometriosis. The most common manifestations are secondary dysmenorrhoea, infertility, pelvic pain, dyspareunia and irregular bleeding. Less common manifestations include backache, painful bowel movements and dysuria. These symptoms may or may not correspond to the woman’s menstrual cycle. With menopause, oestrogen is no longer produced in the ovaries. This may lead to the disappearance of the symptoms.
When the ectopic endometrial tissues ‘menstruate’, the blood collects in cyst-like nodules that have a characteristic bluish-black colour. Nodules in the ovaries are sometimes called chocolate cysts because of the thick, chocolate-colour material they contain. When a cyst ruptures, the pain may be acute and the resulting irritation promotes the formation of adhesions, which attach and fix the affected area to another pelvic structure. Endometrial lesions may become severe enough to cause a bowel obstruction or painful micturition.
MULTIDISCIPLINARY CARE
Endometriosis may be suspected from a patient’s history of the characteristic symptoms and the healthcare provider’s palpation of firm nodular lumps in the adnexa on bimanual examination. However, laparoscopy is necessary for a definitive diagnosis. The treatment of endometriosis is influenced by the patient’s age, desire for pregnancy, symptom severity, and extent and location of the disease. When symptoms are not disruptive, a ‘watch and wait’ approach is used (see Box 53-5). When endometriosis is identified as a probable cause of infertility, therapy proceeds more rapidly.
MULTIDISCIPLINARY CARE
GnRH, gonadotropin-releasing hormone; MRI, magnetic resonance imaging.
Drug therapy
Drug therapy is used to reduce symptoms. Pain may be relieved with non-steroidal anti-inflammatory drugs such as ibuprofen and diclofenac. Drugs to inhibit oestrogen production by the ovary are often given to shrink the endometrial tissue. These drugs imitate a state of pregnancy or menopause. Continuous use (for 9 months) of combined oral contraceptives causes regression of endometrial tissue. Ovulation is suppressed and pseudopregnancy (hyperhormonal amenorrhoea) is produced by progestin agents such as medroxyprogesterone. Another approach to hormonal treatment is danazol, a synthetic androgen that inhibits the anterior pituitary. This drug produces a pseudomenopause (ovarian suppression) with atrophy of ectopic endometrial tissue. Subjective relief of symptoms is noted within 6 weeks of danazol use. Side effects include weight gain, acne, hot flushes and hirsutism. These side effects and the expense of this drug restrict its use.
Another class of drugs used is GnRH agonists (e.g. nafarelin). These drugs cause a hypo-oestrogenic state resulting in amenorrhoea. The side effects reported by patients are usually the same as menopause (hot flushes, vaginal dryness and emotional lability). Loss of bone density has also been reported in women who remain on the therapy longer than 6 months. Endometriosis is controlled but not cured by hormonal therapy. Persistent lesions give rise to subsequent recurrences once the menstrual cycle is re-established.
Surgical therapy
The only cure for endometriosis is surgical removal of all the endometrial implants. Surgical therapy may be conservative or definitive. Conservative surgery is done to confirm the diagnosis or to remove implants. It involves removal or destruction of endometrial implants and lysing or excision of adhesions by means of laparoscopic laser surgery or laparotomy. GnRH agonist therapy can be administered for 4–6 months to reduce the size of the lesions before surgery. By reducing the extent of the surgery, this preoperative drug treatment helps reduce the development of adhesions that may further threaten fertility.
For women wishing to become pregnant, conservative surgical therapy is used to remove implants blocking the fallopian tube. Adhesions are removed from the tubes, ovaries and pelvic structures. Efforts are made to conserve all tissues necessary to maintain fertility.
Each woman should be actively involved in making the decision about preserving part or all of her ovaries, if surgically possible. The nurse should help the patient to explore her feelings about maintaining her cyclic ovarian function. The healthcare provider should assess the patient’s risk for ovarian cancer and provide this information as well for her consideration.
 NURSING MANAGEMENT: ENDOMETRIOSIS
NURSING MANAGEMENT: ENDOMETRIOSIS
The nurse should educate and reassure the patient that a life-threatening situation does not exist, which may permit her to accept a conservative and progressive treatment. When the symptoms are less severe, the nurse may teach the patient about non-drug comfort measures that may be helpful. Patients should be assisted to understand the drugs that have been ordered to treat their condition, including the action of the prescribed drugs, as well as the possible side effects. Psychological support may be needed for patients experiencing severe disabling pain, sexual difficulties secondary to dyspareunia, and infertility.
If conservative surgery is the treatment selected, care is similar to the general preoperative and postoperative care of a patient undergoing laparotomy (see Ch 42). If definitive surgery is planned, the care is similar to the patient undergoing an abdominal hysterectomy (see NCP 53-1 later in this chapter). Nurses should know the extent of the procedure so that appropriate preoperative teaching can be done.
Leiomyomas
AETIOLOGY AND PATHOPHYSIOLOGY
Leiomyomas (uterine fibroids) are benign smooth-muscle tumours that occur within the uterus (see Fig 53-7). Leiomyomas are the most common benign tumours of the female genital tract and it is estimated that 20–50% of women have leiomyomas during their lifetime.30 The cause of leiomyomas is unknown. They appear to depend on ovarian hormones because they grow slowly during the reproductive years and undergo atrophy after menopause.
CLINICAL MANIFESTATIONS
The majority of women with leiomyomas do not have any symptoms. Of the women who develop symptoms, the most common include abnormal uterine bleeding, pain and symptoms associated with pelvic pressure. Increased bleeding is associated with increased endometrial surface area that is associated with leiomyomas. Pain is associated with infection or twisting of the pedicle from which the tumour is growing. Devascularisation and blood vessel compression may also contribute to pain. Pressure on surrounding organs may result in rectal, bladder and lower abdominal discomfort. Large tumours may cause a general enlargement of the lower abdomen. These tumours are sometimes associated with miscarriage and infertility.
MULTIDISCIPLINARY CARE
Clinical diagnosis is based on the characteristic pelvic findings of an enlarged uterus distorted by nodular masses. Treatment depends on the symptoms, the age of the patient, her desire to bear children, and the location and size of the tumours. If the symptoms are minimal, the provider may elect to follow the patient closely for a time.
Persistent heavy menstrual bleeding causing anaemia and large or rapidly growing tumours are indications for surgery. The leiomyomas are removed by hysterectomy or myomectomy. A myomectomy is performed for women who wish to have children. In this case, only the fibroids are removed to preserve the uterus. Small tumours may be removed using a hysteroscope and laser resection instruments.
Uterine artery embolisation is an increasingly used alternative treatment for uterine fibroids. In the procedure, embolic material (small plastic or gelatine beads) is injected into the uterine artery and carried to the fibroid branches. Cryosurgery is another option. In cases of large leiomyomas, a GnRH agonist may be used preoperatively to shrink the size of the tumour. However, the risks and benefits of this drug should be fully discussed, including the potential for irreversible loss of bone mass. The treatment should not be used on women planning to have children.
Another treatment option uses magnetic resonance imaging (MRI)–guided focused ultrasound to target and destroy uterine fibroids. Treatment requires repeated targeting and heating of the fibroid tissue while the patient lies inside the MRI machine. The procedure can last as long as 3 hours.
Cervical polyps
Cervical polyps are benign pedunculated lesions that generally arise from the endocervical mucosa and are seen protruding through the cervical os during a speculum examination. Polyps are a characteristic bright cherry-red and are soft and fragile in consistency. They are generally small, measuring less than 3 cm in length, and may be single or multiple. Their cause is unknown. Symptoms are usually not present, but metrorrhagia and bleeding after straining for a bowel movement and coitus can occur. Polyps are prone to infection. When the polyp is small, it can be excised in an outpatient procedure. If the point of attachment of the polyp cannot be identified and is not accessible to cautery, a polypectomy is performed in the operating room. All tissue removed is sent for pathological review because polyps occasionally undergo malignant changes.
Benign ovarian tumours
There are many different types of benign tumours. The cause of most of them is unknown. They can be divided into cysts and neoplasms. Cysts are usually soft, are surrounded by a thin capsule and may be detected during the reproductive years. Follicle and corpus luteum cysts are common ovarian cysts (see Fig 53-8). Multiple small ovarian follicles may occur in a condition called polycystic ovary syndrome (PCOS) (discussed in the next section). Epithelial ovarian neoplasms may be cystic or solid, or small or extremely large. Cystic teratomas, or dermoid cysts, originate from germ cells and can contain bits of any type of body tissue, such as hair or teeth.
Ovarian masses are often asymptomatic until they are large enough to cause pressure in the pelvis. Constipation, menstrual irregularities, urinary frequency, a full feeling in the abdomen, anorexia and peripheral oedema may occur, depending on the size and location of the tumour. There may be an increase in abdominal girth. Pelvic pain may be present if the tumour is growing rapidly. Severe pain results when the cyst twists on its pedicle (ovarian torsion).
Pelvic examination reveals a mass or an enlarged ovary that demands further investigation. If the mass is cystic and smaller than 8 cm, the patient is asked to return for re-examination in 4–6 weeks. If the mass is cystic and greater than 8 cm or is solid, laparoscopic surgery or laparotomy is performed. Immediate surgery is necessary if ovarian torsion occurs, causing the ovary to rotate and cutting off circulation. Surgical techniques are used to save as much of the ovary as possible.
POLYCYSTIC OVARY SYNDROME
Polycystic ovary syndrome is a chronic disorder in which many benign cysts form on the ovaries. It most commonly occurs in women under 30 years old and is a cause of infertility. It affects about 5–10% of women of reproductive age.31 PCOS is due to hormonal abnormalities in which the ovaries produce oestrogen and excess testosterone but not progesterone. Fluid-filled cysts develop from mature ovarian follicles that fail to rupture (thereby releasing an egg) each month (see Fig 53-9). This problem affects both ovaries.
Clinical manifestations include irregular menstrual periods (particularly long cycles), amenorrhoea or oligomenorrhoea, dysfunctional uterine bleeding, infertility, hirsutism, obesity and acne. Many women start with normal menstrual periods but after 1–2 years the periods become irregular and then infrequent. If left untreated, cardiovascular disease and abnormal insulin resistance with type 2 diabetes mellitus may develop.
Pelvic ultrasound will reveal enlarged ovaries with multiple small cysts. Successful management includes early diagnosis and treatment to improve quality of life and decrease the risk of complications. Oral contraceptives are useful in regulating the menstrual cycle. Hirsutism may be treated with spironolactone. Hyperandrogenism can be treated with flutamide and a GnRH agonist such as nafarelin. Metformin reduces hyperinsulinaemia and has been shown to improve hyperandrogenism and restore ovulation. For women desiring to become pregnant, fertility drugs (e.g. clomiphene) may be used to induce ovulation. If all other treatments are unsuccessful, a hysterectomy with bilateral salpingectomy and oophorectomy may be performed.
The patient should be taught the importance of weight management and exercise to decrease insulin resistance. Obesity exacerbates the problems related to PCOS. The nurse should monitor lipid profile and fasting glucose levels, and stress the importance of regular follow-up care to monitor the effectiveness of therapy and to detect any complications.
Cervical cancer
Approximately 200 Australian and 70 New Zealand women die from cervical cancer annually.32,33 Non-invasive cervical cancer (in situ) is about four times more common than invasive cervical cancer. The mortality rate for cervical cancer in Australia is higher among Indigenous Australian women than for non-Indigenous women.32 Similarly, the rates of cervical cancer among Māori and Pacific women in New Zealand are higher than among women of European descent.33 These higher rates of incidence are associated with lower rates of participation in screening programs and efforts are being made to increase participation in cervical screening programs among these women.33 An increased risk of cervical cancer is also associated with low socioeconomic status, early sexual activity (before 17 years of age), multiple sexual partners, infection with human papillomavirus (HPV), immunosuppression and smoking.
The number of deaths from cervical cancer has fallen steadily over the past 40 years.32 This is due to better and earlier diagnosis with the widespread use of the Pap smear test. In addition to cancer, the Pap smear test screens for precancerous changes. By treating precancerous lesions, progression to cervical cancer can be prevented.
AETIOLOGY AND PATHOPHYSIOLOGY
The progression from normal cervical cells to dysplasia and then to invasive cervical cancer appears to be related to repeated injuries to the cervix. The progression occurs slowly over years rather than months. There is a strong relationship between dysplasia and HPV infections. HPV types 16 and 18 together cause about 70% of cervical cancers.
CLINICAL MANIFESTATIONS
Precancerous changes are asymptomatic. This highlights the importance of routine screening. The peak incidence of non-invasive cervical cancer is in women in their early thirties. The average age for women with invasive cervical cancer is 50 (see Fig 53-10). Early cervical cancer is generally asymptomatic, but leucorrhoea and intermenstrual bleeding eventually occur. The discharge is usually thin and watery but becomes dark and foul smelling as the disease advances, suggesting the presence of an infection. The vaginal bleeding is initially only spotting but, as the tumour enlarges, it becomes heavier and more frequent. Pain is a late symptom and is followed by weight loss, anaemia and cachexia.
DIAGNOSTIC STUDIES
Australian and New Zealand guidelines recommend that Pap smear testing should begin at age 18 years, or 2 years after first sexual intercourse, and should be performed every 2 years.34 Women who have had a total hysterectomy (uterus and cervix removed) do not need to be screened for cervical cancer, unless the surgery was done for cervical precancer or cancer.
The two types of HPV that have been associated with most cases of cervical cancer (types 16 and 18) can now be identified through DNA testing. HPV DNA tests help determine whether women with abnormal Pap smear test results need further follow-up. Recent research suggests that HPV testing may be better than the Pap smear test in screening for cervical cancer.35
Pap smear tests are less than 100% accurate in screening for cervical cell abnormalities. There are problems with both false-positive and false-negative reports. ThinPrep, a newer liquid-based technique for Pap smear tests, has reduced the number of inaccurate test results.
The finding of an abnormal Pap smear indicates the need for follow-up. The type of follow-up depends on the findings. Women with minor changes may be followed with a repeated test in 4–6 months for 2 years. Up to 80% may revert to normal spontaneously. Women with more prominent changes will receive additional procedures, such as colposcopy and biopsy, before a definitive diagnosis can be made. Colposcopy involves examination of the cervix with a binocular microscope with low levels of magnification (10× to 40×). The procedure helps in the identification of possible epithelial abnormalities and suggests areas for biopsy. The LUMA Cervical Imaging System may be used with colposcopy to identify these sites. Biopsies are sent to pathology for evaluation. Colposcopy and biopsy have improved diagnosis and allow more focused treatments to be selected.
The type and extent of the biopsy vary with the abnormality seen. A punch biopsy may be done on an outpatient basis with special punch biopsy forceps. The excision of a cone-shaped section of the cervix may be used for both diagnosis and treatment. Conisation is accomplished using one of several techniques. The choice of procedure is determined by the healthcare provider’s experience and the availability of equipment. Cryotherapy (freezing) and laser cone vaporisation destroy the tissue. Laser cone excision and loop electrosurgery excision procedure (LEEP) remove the identified tissue and allow for histological examination to ensure that all micro-invasive tissue has been removed. These procedures can be performed as outpatient procedures with mild analgesics or sedation. Complications of these procedures include excessive bleeding and possible cervical stenosis after healing.
MULTIDISCIPLINARY CARE
Vaccines against HPV reduce the incidence of both cervical-related neoplasia and cervical cancer due to infection from HPV types 16 and 18. It is recommended for females aged 9 to 26. (Vaccines are discussed further in Ch 52.)
The treatment of cervical cancer is guided by the stage of the tumour and the patient’s age and general state of health (see Table 53-6). There are four procedures in which fertility can be preserved. Conisation may be the only type of therapy needed for non-invasive cervical cancer if analysis of removed tissue demonstrates that a wide area of normal tissue surrounds the excised tissue. Laser treatments can be used, in which a directed infrared beam is employed to destroy abnormal tissue. Cautery and cryosurgery may also be used.
Invasive cancer of the cervix is treated with surgery, radiation and chemotherapy as single treatments or in combination. Surgical procedures include hysterectomy, radical hysterectomy (involving adjacent structures) and, rarely, pelvic exenterations (surgical removal of all pelvic organs). Radiation may be by external (e.g. cobalt) or internal implants (e.g. caesium, radium). Standard radiation treatment is 4–6 weeks of external radiation followed by one or two treatments with internal implants (brachytherapy). (Radiation therapy is discussed in Ch 15.) Cisplatin-based chemotherapy regimens have benefit for patients with cancer spread beyond the cervix.36
Endometrial cancer
Endometrial cancer is the most common gynaecological malignancy in the industrialised world.37 In Australia about 1700 new cases of endometrial cancer are diagnosed each year and about 230 women die of the cancer each year.38 About 315 new cases of uterine cancer (which includes endometrial cancer) are diagnosed in New Zealand each year.39 Endometrial cancer has a relatively low mortality rate, because most cases are diagnosed early. The survival rate is over 95% if the cancer has not spread at the time of diagnosis.
AETIOLOGY AND PATHOPHYSIOLOGY
The major risk factor for endometrial cancer is oestrogen, especially unopposed oestrogen. Additional risk factors include increasing age, nulliparity, late menopause, obesity, smoking, diabetes mellitus and having a personal or family history of hereditary non-polyposis colorectal cancer (HNPCC) (see the Health disparities box on HNPCC in Ch 42). Obesity is a risk factor because adipose cells store oestrogen, thus endogenous oestrogen is increased. Pregnancy and oral contraceptives are protective factors.
Endometrial cancer arises from the lining of the endometrium. Most tumours are adenocarcinomas. The precursor may be a hyperplasic state that progresses to invasive carcinoma. Hyperplasia occurs when oestrogen is not counteracted by progesterone. The cancer directly extends into the cervix and through the uterine serosa. As invasion of the myometrium occurs, regional lymph nodes, including the paravaginal and para-aortic, become involved. Haematogenous metastases develop concurrently. The usual sites of metastases are the lungs, bone, liver and eventually the brain. Malignant cells can be found in the peritoneal cavity, probably having arrived by transport through the fallopian tubes.
Prognostic factors include histological differentiation, myometrial invasion, peritoneal cytology, lymph node and adnexal metastases, and tumour size. Endometrial cancer grows slowly, metastasises late and is curable with therapy if diagnosed early.
CLINICAL MANIFESTATIONS
The first sign of endometrial cancer is abnormal uterine bleeding, usually in postmenopausal women. Because perimenopausal women have sporadic periods for a time, it is important that this sign not be ignored or attributed to menopause. Pain occurs late in the disease process. Other manifestations that may arise are related to metastasis to other organs.
MULTIDISCIPLINARY CARE
Endometrial biopsy is the primary diagnostic test for endometrial cancer. It is carried out on an outpatient basis and involves obtaining endometrial tissue from the uterus. Any occurrence of abnormal or unexpected bleeding in a postmenopausal woman mandates obtaining a tissue sample to exclude endometrial cancer. The Pap smear test is not a reliable diagnostic tool for endometrial cancer, but it can rule out cervical cancer.
Treatment of endometrial cancer is a total hysterectomy and bilateral salpingo-oophorectomy with lymph node biopsies. Although they are not in widespread use, molecular markers help identify high-risk groups who could benefit from postoperative adjuvant therapy. These markers include p53 and p16 over-expression (tumour markers of high proliferative activity) and the expression of oestrogen and/or progesterone receptors by the tumour cells. The absence of oestrogen and progesterone receptors is a poor prognostic indicator.
Most cases of endometrial cancer are diagnosed at an early stage when surgery alone may result in cure. Surgery may be followed by radiation, to either the pelvis or abdomen externally or intravaginally, to decrease local recurrence.36
Treatment of advanced or recurrent disease is difficult. Progesterone hormonal therapy (e.g. megestrol) is the treatment of choice when the progesterone receptor status is positive and the tumour is well differentiated. Tamoxifen, either alone or in combination with progesterone therapy, is also effective in women with advanced or recurrent endometrial cancer. Chemotherapy is considered when progesterone therapy is unsuccessful. Agents used include doxorubicin, cisplatin, fluorouracil carboplatin and paclitaxel.
Ovarian cancer
Ovarian cancer is a malignant tumour of the ovaries and accounts for nearly 4% of all cancers.40 It is the sixth leading cause of cancer deaths in women in the world and the second most commonly occurring gynaecological cancer in Australia.41 In New Zealand about 175 women die of ovarian cancer each year.42 Most women with ovarian cancer have advanced disease at diagnosis. It occurs most frequently in women between 55 and 65 years of age.
AETIOLOGY AND PATHOPHYSIOLOGY
The cause of ovarian cancer is not known. Women who have mutations of the BRCA genes have an increased susceptibility for ovarian cancer.43 The BRCA genes are tumour suppressor genes that inhibit tumour growth when functioning normally. When they mutate, they lose their tumour suppressor ability. This results in an increased risk for women to develop ovarian or breast cancer (see the Health disparities box).
The major risk factor for ovarian cancer is family history (one or more first-degree relatives). Having a family history of breast or colon cancer is also a risk factor. Other risk factors include a personal history of breast or colon cancer and HNPCC (see the Health disparities box on HNPCC in Ch 42). Women who have never been pregnant (nulliparity) are also at higher risk. Other risk factors include increasing age, high-fat diet, increased number of ovulatory cycles (usually associated with early menarche and late menopause), HRT and possibly the use of infertility drugs. The use of oral contraceptives is associated with lower ovarian cancer risk.
Breastfeeding, multiple pregnancies, oral contraceptive use (greater than 5 years) and early age at first birth seem to reduce the risk of ovarian cancer. These factors may have a protective effect because they reduce the number of ovulatory cycles, and thus reduce exposure to oestrogen.
About 90% of ovarian cancers are epithelial carcinomas that arise from malignant transformation of the surface epithelial cells. Germ cell tumours account for another 10%. Histological grading is an important prognostic determinant. Tumour cells are graded according to the level of differentiation. These include well differentiated (grade I), moderately well differentiated (grade II) and poorly differentiated (grade III). Grade III lesions carry a poorer prognosis than the other grades.
HEALTH DISPARITIES
Incidence
• About 10% of cases of ovarian cancer are related to hereditary factors.
• Women with BRCA1 mutations have a 25–40% lifetime risk of developing ovarian cancer.
• Women with BRCA2 mutations have a 10–20% lifetime risk of developing ovarian cancer.
• Family history of both breast and ovarian cancer increases the risk of having a BRCA mutation.
• BRCA mutations occur in 10–20% of patients with ovarian cancer who have no family history of breast or ovarian cancer.
• The family of genes associated with hereditary non-polyposis colorectal cancer accounts for 10% of ovarian cancers.
Ovarian cancer metastasises by shedding malignant cells, which frequently implant on the uterus, bladder, bowel and omentum. Ovarian cancer can also metastasise by lymphatic spread.
CLINICAL MANIFESTATIONS
Symptoms are vague in the early stages. An accumulation of fluid initially causes abdominal enlargement. Non-specific symptoms identified as warranting further evaluation if they occur on an almost daily basis for at least 3 weeks include: (1) pelvic or abdominal pain; (2) bloating; (3) urinary urgency or frequency; and (4) difficulty in eating or feeling full quickly.37 Women who have one or more of these symptoms, especially if they are new, persistent or worsening, are advised to see their healthcare provider. Vaginal bleeding rarely occurs and pain is not an early symptom. Later signs are increased abdominal girth, unexplained weight loss or gain and menstrual irregularities.
DIAGNOSTIC STUDIES
No screening test exists for ovarian cancer. Because early ovarian cancer has vague symptoms, yearly bimanual pelvic examinations should be performed to identify the presence of an ovarian mass (see Box 53-6). Postmenopausal women should not have palpable ovaries, so a mass of any size should be suspected as possible ovarian cancer. An abdominal or a transvaginal ultrasound can be performed to detect ovarian masses. An exploratory laparotomy may be used to establish the diagnosis and stage the disease.
A test called OVA1 can help detect whether a pelvic mass is benign or malignant. OVA1 uses a blood sample to test for levels of five proteins that change due to ovarian cancer. It is not intended for ovarian cancer screening or for a definitive diagnosis of ovarian cancer.
For women with a high risk for ovarian cancer, screening using a combination of the tumour marker (CA-125) and ultrasound is often recommended in addition to a yearly pelvic examination. CA-125 is positive in 80% of women with epithelial ovarian cancer and is used to monitor the course of the disease. However, levels of CA-125 may be elevated with other non-ovarian malignancies or with benign conditions such as fibroids or endometriosis. Clinical trials are actively investigating serum biomarkers that may detect ovarian cancer at an early stage.44 Currently, only 20% of ovarian cancers are diagnosed at an early stage.
MULTIDISCIPLINARY CARE
Women identified as being at high risk based on family and health history may require counselling regarding options such as prophylactic oophorectomy and oral contraceptives. It is important to note that although oophorectomy will significantly reduce the risk of ovarian cancer, it will not completely eliminate the possibility of the disease.
Ovarian cancer staging is critical for guiding treatment decisions. Stage I describes disease limited to the ovaries; stage II describes disease limited to the true pelvis; stage III describes disease limited to the abdominal cavity; and stage IV describes distant metastatic disease. The overall survival rate is 89% with early disease, 36% with local spread and 17% with distant metastases.
The treatment for stage I ovarian cancer is usually a total abdominal hysterectomy and bilateral salpingo-oophorectomy with removal of as much of the tumour as possible (i.e. tumour debulking). The addition of chemotherapy or the instillation of intraperitoneal radioisotopes is often suggested for stage I cancer that is poorly differentiated. Patients with stage II disease may receive external abdominal and pelvic radiation, intraperitoneal radiation or systemic combined chemotherapy after tumour-reducing surgery. After completion of systemic chemotherapy in patients who are clinically free of symptoms, a ‘second-look’ surgical procedure is often performed to determine whether there is any evidence of disease. This option does not necessarily improve the outcome. If no disease is found, the patient is monitored for recurrent disease.
Chemotherapy (e.g. cisplatin carboplatin) is used for the treatment of stage III and stage IV disease. Paclitaxel and topotecan are used to treat metastatic ovarian cancer. Surgical debulking is often done in conjunction with chemotherapy for advanced disease. Intraperitoneal chemotherapy is being used for patients who have minimum residual disease after surgery for advanced ovarian cancer.45 Gemcitabine, in combination with carboplatin, is used to treat recurrent ovarian cancer.
With metastasis, recurrent pleural effusion often causes shortness of breath requiring frequent paracentesis. Palliative radiation and chemotherapy may be used to shrink the tumour to relieve pressure and pain.
Vaginal cancer
Primary vaginal cancers are rare.46 The peak incidence is between 50 and 70 years of age. Vaginal tumours are usually secondary sites or metastases of other cancers such as cervical or endometrial cancer. The most common type of vaginal cancer is squamous cell carcinoma. Intrauterine exposure to diethylstilboestrol (DES) places a woman at risk for clear cell adenocarcinoma of the vagina. Treatment of vaginal cancer depends on the type of cells involved, the stage of the disease, and the size and location of the tumour. Squamous cell carcinomas can be treated with both surgery and radiation.
Vulvar cancer
Worldwide, cancer of the vulva is relatively rare.46 Similar to cervical cancer, preinvasive lesions referred to as vulvar intraepithelial neoplasia (VIN) precede invasive vulvar cancer. The invasive form occurs mainly in women over 60 years of age, with the highest incidence being in women in their seventies. Patients with vulvar neoplasia may have symptoms of vulvar itching or burning, pain, bleeding or discharge. Women who are immunosuppressed and/or have diabetes mellitus, hypertension or chronic vulvar dystrophies are at a higher risk for developing vulvar cancers. Several subtypes of HPV have been identified in some but not all vulvar cancers. Vaccines are now available to protect against some vaginal and vulvar cancers that are caused by these HPV subtypes. (Vaccines are discussed further in Ch 52.)
Diagnosis of vulvar cancer is determined by the pathology report on the biopsy of the suspicious lesion. VIN is managed by eradicating the lesion medically with fluorouracil or surgical excision. Larger lesions may require more extensive surgery and skin graft. The traditional treatment for vulvar cancer has been radical vulvectomy, but this procedure results in extensive morbidity related to scarring and wound breakdown. For this reason, more conservative surgical techniques such as radical hemivulvectomy are being used. Cure rates are comparable between radical vulvectomy and hemivulvectomy, but morbidity and loss of function have been significantly decreased with hemivulvectomy.
Surgical procedures
A variety of surgical procedures are performed when benign or malignant tumours of the genital tract are found (see Table 53-7). A hysterectomy (removal of the uterus) is performed for excision of cancerous tumours of the female reproductive system. It may be done either vaginally or abdominally. The vaginal route is often used when vaginal repair is done in addition to removal of the uterus. The abdominal route is used when large tumours are present and the pelvic cavity is to be explored or when the tubes and ovaries are to be removed at the same time (see Fig 53-11). The abdominal route can present more postoperative problems because it involves an incision and the opening of the abdominal cavity.

Figure 53-11 A, Cross-section of subtotal hysterectomy. Note that cervical stump, fallopian tubes and ovaries remain. B, Cross-section of total hysterectomy. Note that fallopian tubes and ovaries remain. C, Cross-section of vaginal hysterectomy. Note that fallopian tubes and ovaries remain. D, Total hysterectomy, salpingectomy and oophorectomy. Note that uterus, fallopian tubes and ovaries are completely removed.
In both vaginal and abdominal hysterectomies, the ligaments that support the uterus are attached to the vaginal cuff so that the normal depth of the vagina is maintained. The cervix may or may not be removed depending on the findings. See NCP 53-1 for care of the patient after a total abdominal hysterectomy
A modified approach to a vaginal hysterectomy is laparoscopic-assisted vaginal hysterectomy (LAVH). LAVH utilises a laparoscope to assist with the removal of the uterus. Another alternative is laparoscopic subtotal hysterectomy, which allows the cervix to remain. The advantage of these laparoscopic procedures is quicker recovery time and fewer complications.47
Radiation therapy
Radiation is used to cure, control or act as a palliative measure for cancers of the female reproductive system either alone or in combination with other treatments. The goal of radiation therapy is to deliver a specific amount of high-energy (or ionising) radiation to the cancer with minimal damage to the normal surrounding tissue. Radiation therapy may be external or internal (brachytherapy).
EXTERNAL RADIATION THERAPY
With external radiation therapy, a source outside of the body delivers electromagnetic radiation in the form of waves. (External radiation therapy and related nursing care are discussed in Ch 15.)
BRACHYTHERAPY
Brachytherapy allows the radiation to be placed near or into the tumour. This method can deliver a high dose of radiation directly to the tumour. The dose decreases sharply further away from the source, causing less damage to the surrounding normal tissue. A variety of forms are used to deliver brachytherapy, including wires, capsules, needles, tubes and seeds. Brachytherapy is used in the management of cervical and endometrial cancer because of the accessibility of these body parts and the favourable results obtained. Radium and caesium are two commonly used isotopes. In preparing the patient for the treatment, a cleansing enema is given to prevent straining at stool, which could cause displacement of the isotope. An indwelling catheter is inserted to prevent a distended bladder from coming into contact with the radioactive source.
A variety of applicators have been developed for intrauterine treatment. Applicators are inserted into the endometrial cavity and vagina of the anaesthetised patient in the operating room. When the applicator contains the radioactive material, this is known as preloading. In afterloading, the applicator is implanted in the operating room but is not loaded with the radioactive material until its correct placement is verified and the patient has been returned to her room. Radiation exposure to the patient is precisely controlled. Radiation exposure to the medical team involved in the implantation is reduced when the afterload technique is used. The applicator is secured with vaginal packing and is left in place for 24–72 hours. The radiation oncologist determines the exact amount of radioactive substance to be used and the length of time it will be left in place so that destruction of cancer cells can occur with minimal damage to normal cells.
During the treatment the patient is placed in a lead-lined private room and is on absolute bed rest. She may be turned from side to side. The presence of an intrauterine applicator produces uterine contractions that may require analgesics. The destruction of cells results in a foul-smelling vaginal discharge; a deodoriser is helpful. Nausea, vomiting, diarrhoea and malaise may develop as a systemic reaction to the radiation.
At the end of the prescribed period of radiation, the radioactive material and the catheter are removed. The patient is allowed off bed rest and is discharged from the hospital when stable. Late complications that may arise after irradiation of the uterus include fistulas (vesicovaginal, ureterovaginal), cystitis, phlebitis, haemorrhage and fibrosis. If fibrosis occurs, the vaginal wall becomes smaller in diameter and shorter. Dilation of the vagina through intercourse or the use of sequentially sized dilators may be indicated. The patient is urged to report any unusual symptoms or complaints to her doctor or nurse practitioner. (Brachytherapy and related nursing care are discussed in Ch 15.)
 NURSING MANAGEMENT: CANCERS OF THE FEMALE REPRODUCTIVE SYSTEM
NURSING MANAGEMENT: CANCERS OF THE FEMALE REPRODUCTIVE SYSTEM
 Nursing assessment
Nursing assessment
Malignant tumours of the female reproductive system can be found in the cervix, endometrium, ovaries, vagina and vulva. The patient with any of these malignant tumours may experience a variety of clinical manifestations, including leucorrhoea (thick, whitish vaginal discharge), irregular vaginal bleeding, increase in abdominal pain and pressure, bowel and bladder dysfunction, and vulvar itching and burning. Assessment for these signs and symptoms is an important nursing responsibility.
 Nursing diagnoses
Nursing diagnoses
Nursing diagnoses for the female patient with cancer of the reproductive system include, but are not limited to, the following:
• anxiety related to threat of a malignancy and lack of knowledge about the disease process and prognosis
• acute pain related to pressure secondary to an enlarging tumour
• disturbed body image related to loss of body part and loss of good health
• ineffective sexuality pattern related to physiological limitations and fatigue
• ineffective breathing pattern related to presence of ascites and effusions
 Planning
Planning
The overall goals are that the patient with cancer of the female reproductive system will: (1) actively participate in treatment decisions; (2) achieve satisfactory pain and symptom management; (3) recognise and report problems promptly; (4) maintain her preferred lifestyle as long as possible; and (5) continue to practise cancer detection strategies.
 Nursing implementation
Nursing implementation
 Health promotion
Health promotion
Through their contact with women in a variety of settings, nurses have the opportunity to teach women the importance of routine screening for cancers of the reproductive system. Cancer can be prevented when screening reveals precancerous conditions of the vulva, cervix, endometrium and, rarely, the ovaries. Also, routine screening increases the chance that a cancer will be found in an early stage. When cancer is identified early, treatment can be more conservative and the woman’s prognosis improves. A pelvic examination and Pap smear test every 2 years will allow the healthcare provider to detect lesions on the vulva or any uterine or ovarian irregularities and screen for cervical cancer. Nurses should assist women to view routine cancer screening as an important self-care activity and recommend vaccination against cervical cancer for those women at high risk.
Educating women about risk factors for cancers of the reproductive system is also important. Limiting sexual activity during adolescence, using condoms, having fewer sexual partners and not smoking reduce the risk of cervical cancer. A high-fat diet increases the risk for ovarian cancer. When high-risk behaviours are identified, patients should be assisted to modify their lifestyles to decrease risk.
 Acute intervention related to surgery
Acute intervention related to surgery
All patients experience a degree of anxiety when surgery is contemplated, but the prospect of major gynaecological surgery may heighten these concerns. Some women may fear a loss of femininity and worry about possible changes in their secondary sex characteristics. Others may experience feelings of guilt, anger or embarrassment. Still others may focus on the effect the surgery will have on their reproductive and sexual functions. Some women view the whole process as annoying, whereas others are relieved by the thought of no longer having menstrual periods or becoming pregnant. Each patient must be understood in the light of her fears and concerns and must be approached and evaluated individually. The nurse should exhibit interest and willingness to listen as it can provide considerable psychological support.
Preoperatively, the patient is prepared physically for surgery with the standard perineal or abdominal preparation. The bladder should be emptied before the patient is sent to the operating room. An indwelling catheter is commonly inserted preoperatively.
 Hysterectomy
Hysterectomy
Postoperatively, the patient who has had a hysterectomy will have an abdominal dressing (abdominal hysterectomy) or a sterile perineal pad (vaginal hysterectomy). (See NCP 53-1 for care of the patient after a total abdominal hysterectomy.) The dressing should be observed frequently for any sign of bleeding during the first 8 hours after surgery. A moderate amount of serosanguineous drainage on the perineal pad is expected following a vaginal hysterectomy.
The patient may experience urinary retention postoperatively because of temporary bladder atony resulting from oedema or nerve trauma. This problem is more acute when a radical hysterectomy has been performed. At times an indwelling catheter is used for 1–2 days postoperatively to maintain constant drainage of the bladder and prevent strain on the suture line. If an indwelling catheter is not used, catheterisation may be necessary if the patient has not urinated for 8 hours postoperatively. If residual urine is suspected after the removal of an indwelling catheter, catheterisation is done to prevent bladder infection caused by pooling of urine. Accidental ligation of a ureter is a serious surgical complication. Any complaint of backache or decreased urine output should be reported to the surgeon.
Abdominal distension may develop from the sudden release of pressure on the intestines when a large tumour is removed or from paralytic ileus secondary to anaesthesia and pressure on the bowel. Food and fluids may be restricted if the patient is nauseated. A rectal tube may be prescribed to relieve abdominal flatus, and ambulation is encouraged.
Special care must be taken to prevent the development of deep vein thrombosis (DVT). Frequent changes of position, avoidance of the high Fowler position and avoidance of pressure under the knees minimise stasis and pooling of blood. Special attention must be given to patients with varicosities. The nurse should encourage leg exercises to promote circulation.
The loss of the uterus may bring about grief responses similar to any great personal loss. The ability to bear children is central to society’s image of being a woman. Although not experienced by all women, grief over this loss is normal. The nurse should elicit the patient’s feelings and concerns about her surgery to provide the necessary information to give understanding care. When surgery removes the ovaries as well, women experience surgical menopause. Oestrogen is no longer available from the ovaries, so symptoms of oestrogen deficiency will arise. To counter this, HRT may be initiated in the early postoperative period.
The patient should be prepared for what to expect following surgery (e.g. she will not menstruate) with discharge teaching. Instructions should include specific activity restrictions. Intercourse should be avoided until the wound is healed (about 4–6 weeks), but intercourse is not contraindicated once healing is complete. If a vaginal hysterectomy is performed, the nurse should inform the patient that there may be a temporary loss of vaginal sensation but the sensation will return in several months.
Physical activities are limited for a short time. Heavy lifting should be avoided for 2 months. Activities that may increase pelvic congestion, such as dancing and walking swiftly, should be avoided for several months, whereas activities such as swimming may be both physically and mentally helpful. Wearing a girdle is allowed and may provide comfort. The patient should be assured that once healing is complete, all previous activity can be resumed.
 Salpingectomy and oophorectomy
Salpingectomy and oophorectomy
Postoperative care of the patient who has undergone removal of a fallopian tube (salpingectomy) or an ovary (oophorectomy) is similar to that for any patient having abdominal surgery. However, if a large ovarian cyst was removed, there may be abdominal distension caused by the sudden release of pressure in the intestines. An abdominal binder may provide relief until the distension subsides.
When both ovaries are removed (bilateral oophorectomy), surgical menopause results. The symptoms are similar to those of regular menopause but may be more severe because of the sudden withdrawal of hormones. Attempts may be made to leave at least a portion of an ovary.
 Vulvectomy
Vulvectomy
Although cancer of the vulva is relatively uncommon, it is important to recognise the extent of the vulvectomy and the significant effect it is likely to have on the patient’s life. Having an honest, open attitude with the patient and her partner preoperatively can be most helpful in the postoperative period.
After a vulvectomy (see Table 53-7), the patient will return to the unit with a wound in the perineal area extending to the groin. The wound may be covered or left exposed and frequently has drains attached to portable suction (e.g. Haemovac, Jackson-Pratt). A heavy-pressure dressing is often in place for the first 24–48 hours. The wound is cleaned with normal saline solution or an antiseptic twice daily. Solutions can be applied with an aseptic bulb syringe or a Water Pik machine and a heat lamp or a hair dryer can be used to dry the area. Wound care must be meticulous to prevent infection, which results in delayed healing.
Special attention to bowel and bladder care is needed. A low-residue diet and stool softeners prevent straining and wound contamination. An indwelling catheter is used to provide urinary drainage. The nurse should be careful not to dislodge the catheter because extensive oedema makes its reinsertion difficult. Heavy, taut sutures are often used to close the wound, resulting in severe discomfort for the patient. In other instances the wound may be allowed to heal by granulation. Analgesics may be required frequently to control pain. The patient should be positioned carefully using strategically placed pillows to provide comfort. Ambulation is usually begun on the second postoperative day, but this varies with the preference of the surgeon. Anticoagulant therapy to prevent DVT is common.
Because the surgery causes mutilation of the perineal area and the healing process is slow, the patient is likely to become discouraged. The nurse should provide opportunities for the patient to express her feelings and concerns about the operation. The patient should be taught specific instructions in self-care before discharge and instructed to report any unusual odour, fresh bleeding, breakdown of incision or perineal pain. Home care nursing can benefit the patient during her adjustment period. Sexual function is often retained. Whether clitoral sensation is retained may be critical to some women, particularly if it was a primary source of orgasmic satisfaction. Discussing alternative methods of achieving sexual satisfaction may also be indicated.
 Pelvic exenteration
Pelvic exenteration
When other forms of therapy fail to control the spread of cancer and no metastases have been found outside of the pelvis, pelvic exenteration may be performed. Although different types are done, this radical surgery usually involves removal of the uterus, ovaries, fallopian tubes, vagina, bladder, urethra and pelvic lymph nodes (see Fig 53-12). In some situations, the descending colon, rectum and anal canal may also be removed. Candidates for this procedure are selected on the basis of their likelihood of surviving the surgery and their ability to adjust to and accept the resulting limitations.

Figure 53-12 Total exenteration is removal of all pelvic organs with the creation of an ileal conduit and a colostomy.
Postoperative care is similar to that for the patient who has had a radical hysterectomy, an abdominal perineal resection and an ileostomy or a colostomy. The physical, emotional and social adjustments to life on the part of the patient and her family are great. The patient will have urinary or faecal diversions in the abdominal wall, a reconstructed vagina and the onset of menopausal symptoms.
The patient’s rehabilitative process should keep pace with her acceptance of the situation. Much understanding and support are needed from the nursing staff during the long recovery period. The patient needs to be gently encouraged to regain her independence. She needs to verbalise her feelings about her altered body structure. Including the family in the plan of care is important.
The patient will need to return to her treating doctor at specified intervals. Early recurrence of the cancer may be identified and treated. At this time the patient’s physical and emotional adjustment to the changes in body image produced by the surgery and her ability to carry out any treatment measures should be assessed. Additional teaching and counselling can then be provided.
 Acute intervention with radiation therapy
Acute intervention with radiation therapy
Nursing management of the patient receiving brachytherapy requires special considerations. Nurses should not stay in the immediate area any longer than is necessary to give proper care and attention. No individual nurse should attend the patient for more than 30 minutes per day. The nurse should stay at the foot of the bed or at the entrance to the room to minimise radiation exposure. Visitors should be instructed to stay 2 metres away from the bed and to limit visits to less than 3 hours a day. Efficient organisation of nursing care is essential so that nursing staff do not stay in the immediate area of the patient any longer than is necessary. The reasons for these precautions must be explained fully to the patient and her visitors. (A more detailed discussion of nursing care of the patient receiving brachytherapy is given in Ch 15.)
The patient who is to receive external radiation should be instructed to urinate immediately before the treatment to minimise radiation exposure to the bladder. She should also be advised about radiation side effects, including enteritis and cystitis. These are natural reactions to radiation therapy and do not indicate an overdose. The patient should be fully informed of the possible side effects and measures that can be used to reduce their impact.
 Evaluation
Evaluation
The expected outcomes are that the patient with cancer of the female reproductive system will: (1) actively participate in treatment decisions; (2) achieve satisfactory pain and symptom management; (3) recognise and report problems promptly; (4) maintain her preferred lifestyle as long as possible; and (5) continue to practise cancer detection strategies.
PROBLEMS WITH PELVIC SUPPORT
The most commonly occurring problems with pelvic support are uterine prolapse, cystocele and rectocele. Although vaginal birth increases the risk for these problems, these conditions can occur in women who have never experienced childbirth. Obesity, chronic coughing and straining during bowel movements can increase the likelihood of these problems. The decreased oestrogen that normally accompanies the perimenopause also reduces some connective tissue support.
Uterine prolapse
Uterine prolapse is the downward displacement of the uterus into the vaginal canal (see Fig 53-13).48 Prolapse is rated by degrees. In first-degree prolapse, the cervix rests in the lower part of the vagina. Second-degree prolapse means the cervix is at the vaginal opening. A third-degree prolapse means the uterus protrudes through the introitus. Symptoms vary with the degree of prolapse. The patient may describe a feeling of ‘something coming down’. She may have dyspareunia, a dragging or heavy feeling in the pelvis, backache and bowel or bladder problems if cystocele or rectocele is also present. Stress incontinence is a common and troubling problem. When third-degree uterine prolapse occurs, the protruding cervix and vaginal walls are subjected to constant irritation, and tissue changes may occur.

Figure 53-13 Uterine prolapse. A, First-degree prolapse. B, Second-degree prolapse. C, Third-degree prolapse.
Therapy depends on the degree of prolapse and how much the woman’s daily activities have been affected. Pelvic muscle strengthening exercises (Kegel exercises) may be effective for some women (see Ch 45). If not, a pessary may be used. A pessary is a device that is placed in the vagina to help support the uterus.49 A wide variety of shapes exist, including rings, arches and balls. Most are made of plastic or wire coated with plastic. When a woman first receives a pessary, she needs instructions for its cleaning and follow-up. Pessaries that are left in place for long periods are associated with erosion, fistulas and an increased incidence of vaginal carcinoma. If more conservative measures are not successful, surgery is indicated. Surgery generally involves a vaginal hysterectomy with anterior and posterior repair of the vagina and underlying fascia.
Cystocele and rectocele
Cystocele occurs when support between the vagina and bladder is weakened (see Fig 53-14). Similarly, rectocele results from weakening between the vagina and rectum (see Fig 53-15). These problems are common and asymptomatic in many women. With large cystoceles, complete emptying of the bladder can be difficult, predisposing women to bladder infections. A woman with a large rectocele may not be able to completely empty her rectum when defecating unless she helps push the stool out by putting her fingers in her vagina.
As with uterine prolapse, Kegel exercises (see Ch 45) may be used to strengthen the weakened perineal muscles if the cystocele or rectocele is not too problematic. A pessary may be helpful for cystoceles. Surgery designed to tighten the vaginal wall is generally the method of treatment. Cystocele is corrected with a procedure called an anterior colporrhaphy, whereas a posterior colporrhaphy is used for rectocele. If further surgery is needed to relieve stress incontinence, procedures to support the urethra and restore the proper angle between the urethra and the posterior bladder wall are used.
 NURSING MANAGEMENT: PROBLEMS WITH PELVIC SUPPORT
NURSING MANAGEMENT: PROBLEMS WITH PELVIC SUPPORT
Patients should be assisted to avoid or decrease problems with pelvic support by learning how to do Kegel exercises. Women of all ages may benefit from these exercises. Kegel exercises are especially important following childbirth or whenever women begin to have incontinence. To instruct a patient in this exercise, she should be told to pull in or contract her muscles as if she were trying to stop the flow of urine. She should hold the contraction for several seconds and then relax. Sets of 5–10 contractions each should be done several times daily.
If vaginal surgery is necessary, the preoperative preparation usually includes a cleansing douche the morning of surgery. A cathartic enema and a cleansing enema are usually given when a rectocele repair is scheduled. A perineal shave may be done.
In the postoperative period, the goals of care are to prevent wound infection and pressure on the vaginal suture line. This necessitates perineal care at least twice a day and after each urination or defecation. An ice pack can be applied locally to help relieve the initial perineal discomfort and swelling—a disposable glove filled with ice and covered with a cloth works well in these instances. Later, sitz baths may be used.
After an anterior colporrhaphy, an indwelling catheter is usually left in the bladder for 4 days to allow the local oedema to subside. The catheter keeps the bladder empty, preventing strain on the sutures. Twice-daily catheter care with an antiseptic is generally required. After posterior colporrhaphy, straining at stool is avoided by means of a low-residue diet and the prevention of constipation. A stool softener is usually given each night.
The nurse should review discharge instructions before the patient leaves the hospital. These include the use of douches or a mild laxative as needed; restriction of heavy lifting and prolonged standing, walking or sitting; and avoidance of intercourse until the doctor gives permission. There may be a loss of vaginal sensation, which can last for several months, but the patient should be reassured that this situation is temporary.
Fistula
A fistula is an abnormal opening between internal organs or between an organ and the exterior of the body (see Fig 53-16). Gynaecological procedures cause most urinary tract fistulas. Other causes include injury during childbirth and disease processes, such as carcinoma. Fistulas may develop between the vagina and the bladder, urethra, ureter or rectum. When vesicovaginal fistulas (between the bladder and the vagina) develop, some urine leaks into the vagina, whereas with rectovaginal fistulas (between the rectum and the vagina), flatus and faeces escape into the vagina. In both instances, excoriation and irritation of the vaginal and vulvar tissues occur and may lead to severe infections. In addition to wetness, offensive odours may develop, causing embarrassment and severely limiting socialisation.
Because small fistulas may heal spontaneously within a matter of months, treatment may not be needed.50 If the fistula does not heal, surgical excision is required. Inflammation and tissue oedema must be eliminated before surgery is attempted. This may involve a wait of up to 6 months for the surgery. The fistulectomy may result in the patient having an ileal conduit or temporary colostomy.
 NURSING MANAGEMENT: FISTULAS
NURSING MANAGEMENT: FISTULAS
Perineal hygiene is of great importance both preoperatively and postoperatively. The perineum should be cleansed at least every 4 hours, warm sitz baths should be taken three times daily if possible and perineal pads should be changed frequently. The patient should be encouraged to maintain an adequate fluid intake. Encouragement and reassurance are needed in helping the patient to cope with her problems.
Postoperatively, nursing care emphasises the avoidance of stress on the repaired areas and the prevention of infection. The nurse should take care so that the indwelling catheter, usually in place for 7–10 days, is draining at all times. The patient should be urged to take oral fluids to provide for internal catheter irrigation. Minimal pressure and strict asepsis are used if catheter irrigation becomes necessary. The first stool after bowel surgery may be purposely delayed to prevent contamination of the wound. Later, stool softeners or mild laxatives can be given. (See Ch 45 for care of the patient with an ileal conduit and Ch 42 for care of the patient with a colostomy.) Surgical repair of fistulas is not always effective, even in the best conditions. Therefore, supportive nursing care for the patient and her significant others is especially important.
Sexual assault
Sexual assault is the forcible perpetration of a sexual act on a person without his or her consent. It can include any of the following actions: sodomy (anal or oral copulation with a person of the same or opposite sex), forced vaginal intercourse, assault with a foreign object and serial battery. Sexual assault can dramatically disrupt the roles normally performed by the adult woman.
CLINICAL MANIFESTATIONS
Physical
Of the women who seek help immediately after an assault, between half and two-thirds do not have any evidence of physical trauma. Such evidence may be limited because women do not resist for fear of physical danger and injury. When present, physical injuries may include bruising and lacerations to the perineum, hymen, vulva, vagina, cervix and anus. Fractures, subdural haematomas, cerebral concussions and intraabdominal injuries have resulted in the need for hospitalisation. Sexual assault also places women at risk for STIs and pregnancy.
Psychological
Immediately after the assault, women may show shock, numbness, denial or withdrawal. Some women may seem unnaturally calm; others may cry or express anger. Feelings of humiliation, degradation, embarrassment, anger, self-blame and fear of another assault are commonly expressed. These symptoms usually decrease after 2 weeks, and victims may appear to have adjusted. Yet any time from 2–3 weeks to months to years after the assault, symptoms may return and become more severe. The rape-trauma syndrome is a classification of posttraumatic stress disorder. Flashbacks, intrusive recall, sleep disturbances, GI symptoms and numbing of feelings are common initial symptoms. Women will feel embarrassment, self-blame and powerlessness. Later symptoms include mood swings, irritability and anger. Feelings of despair, shame and hopelessness are often the cause of the anger. These feelings may be internalised and expressed as depression. Suicidal ideation may also occur.
MULTIDISCIPLINARY CARE
In the acute care of an assault survivor, ensuring the woman’s emotional and physical safety has the highest priority. Table 53-8 outlines the emergency management of the patient who has been sexually assaulted. Most emergency departments (EDs) have identified health team members who have received special training to provide care to victims of sexual assault, while ensuring evidence is safeguarded. Special procedures are followed in taking the history and conducting the examination in order to preserve all evidence in case of future prosecution.
When the survivor of an assault is admitted to the ED or clinic, a specific chain of events occurs (see Box 53-7). A signed informed consent is obtained from the woman before any data are collected. All materials gathered are well documented, labelled and given to the appropriate person, such as the pathologist or a police officer. The materials are handled by as few people as possible, and signatures of all responsible for keeping and handling the data are obtained. Many items can be used as evidence if the victim chooses to file a complaint. Consequently, the integrity of the material must be maintained. The nurse’s involvement in the medicolegal process depends on the policies of the individual institution and state law.
BOX 53-7 Evaluation of alleged sexual assault
5. Laboratory samples
• Vaginal vault content sampling
• Vaginal smears—microscope evaluation for trichomonads and semen
• Oral or rectal swabs and smears, if indicated
• Blood samples—VDRL serology, pregnancy test; serological testing for HIV and hepatitis B infection
• Freeze serum sample for later testing
• Cultures—cervix and other areas (if indicated) for gonorrhoea and Chlamydia
6. Treatment
• Care of injuries and emotional trauma
• Prophylaxis for STIs, tetanus and hepatitis B (see appropriate chapters)
• Follow-up for pregnancy test in 2–3 weeks (if appropriate)
• Testing for HIV, syphilis and hepatitis B may be done at 6–8 weeks
• Recommendation of continued follow-up and services of rape crisis centre
HIV, human immunodeficiency virus; STIs, sexually transmitted infections; VDRL, Venereal Disease Research Laboratory.
A gynaecological and sexual history and an account of the assault (who, what, when and where), as well as a general physical and pelvic examination, add further information about the rape incident. Laboratory tests are done primarily to determine the presence of sperm in the vagina and to identify any existing STIs or pregnancy.
Follow-up physical and psychological care is essential. Women should return weekly for the first month following the assault. This includes the time period when a woman’s psychological reactions may be the most severe. Providers should have the telephone numbers and names of contacts for local resources for sexual assault survivors, including rape crisis centres, legal and law enforcement authorities, and human services.
 NURSING MANAGEMENT: SEXUAL ASSAULT
NURSING MANAGEMENT: SEXUAL ASSAULT
Nurses should assist all women to become aware of sexual assault prevention tactics (see Box 53-8). Women should also be encouraged to learn some basic techniques of self-defence. Self-defence classes in which formal instruction is given are available in many communities. Practising the various techniques with a friend strengthens a woman’s confidence in her ability to fight back. Learning self-defence can make a woman less vulnerable and more self-reliant.
BOX 53-8 Sexual assault prevention tactics
PATIENT TEACHING GUIDE
The following instructions should be given when teaching women measures to prevent sexual assault:
1. Place and maintain lights at all entrances to your home.
2. Keep your doors locked and do not open them to a stranger; ask for identification if a service person comes to the door.
3. Do not advertise that you live alone; list only your initials with your last name in the telephone directory or on the mailbox; never reveal to a caller that you are home alone.
4. Avoid walking alone in deserted areas; walk to the car park with a friend; be sure you see each other leave.
5. Have your keys ready as you approach your car or home.
6. Say what you mean in social situations; be sure your voice and body language reflect your response.
7. Proceed with caution in online correspondence.
8. Carry a loud whistle and use it when you think you are in danger.
9. Yell ‘Fire!’ if you are attacked and run towards a lighted area.
When a sexual assault survivor is brought to the clinic or ED, a quiet, private area should be used for the initial assessment and the examinations that follow. The patient should not be left alone. Whenever possible, the same nurse should remain with the patient throughout her stay and provide needed emotional support. The patient’s actions and words as she describes the incident may be inconsistent and confused and may seem inappropriate. It is important to maintain a non-judgemental attitude.
The patient usually has many feelings and thoughts about the assault and generally wants to talk about them to an interested listener. Talking may help the patient to feel better and gain understanding of her reactions to the incident. When the nurse listens carefully, the patient feels that she is not alone and is better able to gain control over the situation.
The nurse should assess the patient’s stress level before preparing her for the various procedures that will follow. The nurse also needs to support the patient’s coping mechanisms. The patient needs to know what to expect and what is expected of her, as well as why the particular procedures must be done. Because the pelvic examination may trigger a flashback of the attack, the nurse should answer all related questions before the examination and be a supportive presence during the examination.
Following the examinations, the patient’s physical comfort needs should be considered. She will need a change of clothing, because her original garments may be torn or soiled, or kept as evidence. Most women who have been sexually assaulted feel dirty and need a place to wash, as well as to use a mouthwash, especially if oral sex was involved. Food and drink may also provide comfort to the victim. The possibility of pregnancy should be discussed and the patient can be offered the morning-after pill as an emergency contraceptive.
When the patient is discharged, the nurse should make certain that the patient has transportation home. If friends or family members are not available, the hospital or clinic should make arrangements with an appropriate community resource. The patient should not be sent home alone. The victim’s partner and family have tremendous potential as both a negative and a positive influence.
Many communities today have crisis centres. These public service organisations have trained professional and non-professional volunteers who provide an emotional support system on request. Their programs provide advocacy to ensure dignified treatment throughout the medical and police procedures, short-term counselling for the woman and her family, and court assistance and public education on rape-related issues.
The patient with uterine prolapse and vaginal hysterectomy
CASE STUDY
Patient profile
Kelly Lee is a 62-year-old non-Indigenous woman who has developed lower pelvic discomfort and stress incontinence. She has type 2 diabetes mellitus and hypertension. She is the mother of four children. A second-degree uterine prolapse is diagnosed. She was treated conservatively with a pessary, but her symptoms did not improve. She comes to the hospital for a vaginal hysterectomy and anterior/posterior repair.
CRITICAL THINKING QUESTIONS
1. What are the common causes of uterine prolapse?
2. This patient asks you about the effect of the surgery on her sexuality. How would you respond?
3. What are priorities of care for this patient?
4. What possible complications (including their basis for development) can arise after vaginal hysterectomy?
5. What should this patient be taught about managing her condition once she gets home?
6. Based on the assessment data presented, write one or more appropriate nursing diagnoses. Are there any collaborative problems?
1. In telling a patient with infertility what she and her partner can expect, the nurse explains that:
2. A patient with a spontaneous abortion is more likely than a patient with an induced abortion to have:
3. An appropriate question to ask the patient with painful menstruation to differentiate primary from secondary dysmenorrhoea is:
4. In caring for a patient after an ectopic pregnancy was surgically removed, the nurse advises the patient that:
5. To prevent or decrease age-related changes that occur after menopause in a patient who chooses not to take hormone replacement therapy, the nurse teaches the patient that the most important self-care measure is:
6. The patient’s history indicating thick, white and curd-like vaginal discharge and vulvar pruritus is most consistent with:
7. The nurse caring for a patient with pelvic inflammatory disease places her in the semi-Fowler position. The rationale for this measure is to:
8. In planning care for the patient receiving medical management of endometriosis, the nurse includes teaching regarding the side effect of:
9. A 31-year-old woman who wishes to have children is diagnosed with leiomyoma. The nurse plans care for the patient based on the knowledge that:
10. A 53-year-old woman who has not had a menstrual period for 24 months tells the nurse that she has recently had some period-like bleeding. The nurse advises the patient that:
11. The nurse plans early and frequent ambulation for the patient who has undergone an abdominal hysterectomy in order to:
12. Nursing responsibilities related to the patient receiving internal radiation for endometrial cancer include:
13. The first nursing intervention for the patient who has been sexually assaulted is to:
1 National Institute for Clinical Excellence. Clinical guideline 11. Fertility: assessment and treatment for people with fertility problems. Available at www.nice.org.uk/nicemedia/live/10936/29267/29267.pdf, Updated March 2010. accessed February 2011.
2 Wang Y, Chambers G, Sullivan A. Assisted reproductive technologies in Australia and New Zealand. Available at www.aihw.gov.au/publications/per/49/11525.pdf, 2010. accessed 17 December 2010.
3 Kendall J. Women’s health: female infertility 2: treatments. Prac Nurs. 2008;19:10.
4 Gerber-Epstein P, Leichtentritt RD, Benyamini Y. The experience of miscarriage in first pregnancy: women’s voices. Death Studies. 2009;33:1.
5 Nurse practitioners’ prescribing reference, 2008–2009. New York: Haymarket Media, 2008.
6 Davidson MR, London ML, Ladewig PA. Maternal-newborn nursing and women’s health across the lifespan, 8th edn. Upper Saddle River, NJ: Pearson, 2008.
7 Brown J, O’Brien PMS, Marjoribanks J, et al. Selective serotonin reuptake inhibitors for premenstrual syndrome. Cochrane Library. 2, 2009. CD001396
8 Rapkin AJ, Gambone JC. Pelvic pain. In Hacker NF, Gambone JC, Hobel CJ, eds.: Hacker and Moore’s essentials of obstetrics and gynecology, 5th edn., Philadelphia: Saunders, 2010.
9 Smith RP, ed. Netter’s obstetrics and gynecology, 2nd edn., Philadelphia: Saunders, 2008.
10 Ayers D, Montgomery M. Putting a stop to dysfunctional bleeding. Nursing. 2009;39:44.
11 Centers for Disease Control and Prevention. Toxic shock syndrome. Available at www.cdc.gov/ncidod/dbmd/diseaseinfo/toxicshock_t.htm. accessed 16 December 2010.
12 Casanova BC, Sammel MD, Chittams J, et al. Prediction of outcome in women with symptomatic first-trimester pregnancy: focus on intrauterine rather than ectopic gestation. J Women’s Health. 2009;18:2.
13 Shamonki M, Nelson AL, Gambone JC. Ectopic pregnancy. In Hacker NF, Gambone JC, Hobel CJ, eds.: Hacker and Moore’s essentials of obstetrics and gynecology, 5th edn., Philadelphia: Saunders, 2010.
14 Lund K. Menopause and the menopausal transition. Med Clin North Am. 2008;92:1253.
15 Cooper M. How modern women can manage the menopause. Prim Health Care. 2009;19:10.
16 Alraek T, Malterud K. Acupuncture for menopausal hot flashes: a qualitative study about patient experiences. J Alternative Compl Med. 2009;15:153.
17 Accortt EE, Freeman MP, Allen JB. Women and major depressive disorder: clinical perspectives on causal pathways. J Women’s Health. 2008;17:1583.
18 Currie H. Prescribing HRT. Prac Nur. 2008;25:4.
19 Women’s Health Initiative (WHI) Study. Findings from the WHI post-menopausal hormone therapy trials. Department of Health and Human Services. Available at www.nhlbi.nih.gov/whi. accessed 16 December 2010.
20 North American Menopause Society. Position statement: oestrogen and progesterone use in menopausal women, July 2008, Menopause. 2008;15:4. Available at www.menopause.org.au/consumers/position-statements/531 accessed 21 December 2010.
21 Birkhauser MH, Panay N, Archer DF, et al. Updated practical recommendations for hormone replacement therapy in the peri- and postmenopause. Climacteric. 2008;11:108.
22 Rani S. The psychosexual implications of menopause. Br J Nurs. 2009;18:6.
23 Brocki J. Physiology and effects of the menopause. Nurse Prescribing. 2008;6:5.
24 Ramos-Valdivielso M, Bueno C, Hernanz JM. Significant improvement in extensive lichen sclerosis with tacrolimus ointment and PUVA. Am J Clin Derm. 2008;9(3):175–179.
25 Cottrell Hansen B, Close FT. Vaginal douching among university women in the southeastern United States. J Am College Health. 2008;56:4.
26 Australian Institute of Health &Welfare (AIHW). Australia’s health. Available at www.aihw.gov.au/publications/aus/ah08/ah08-c05.pdf, 2008. accessed 16 October 2010.
27 Haggarty CL, Gottlieb S, Taylor BD, Low N, Xu F, Ness RB. Risk of sequelae after Chlamydia trachomatis genital infection in women, J Infect Dis. 2010;201(suppl 2):S134–S155. Available at www.cdc.gov/std/stats09/womenandinf.htm accessed 22 December 2010.
28 Ortiz D. Chronic pelvic pain in women. Am Acad Fam Phys. 2008;77:1535.
29 Rogers P, D’Hooge T, Fazleabas A, Gargett C, Giudice L, Montgomery G, et al. Priorities for endometriosis research: recommendations from an international consensus workshop. Reproductive Sciences. 2009;16:4.
30 Farquhar C. Do uterine fibroids cause infertility and should they be removed to increase fertility? BMJ 2009; 338:b126. Available at www.bmj.com/content/338/bmj.b126.ful. accessed 16 October 2010.
31 Radosh L. Drug treatments for polycystic ovary syndrome. Am Fam Physician. 2009;79:671.
32 Australian Institute of Health & Welfare (AIHW). Australia’s health. Available at www.aihw.gov.au/publications/aus/ah10/ah10.pdf, 2010. accessed 16 December 2010.
33 National Screening Unit. Cervical cancer in New Zealand. Available at www.nsu.govt.nz/current-nsu-programmes/1228.asp. accessed 17 December 2010.
34 Australian Cancer Council. Look after number one: a cancer prevention plan for women. Available at www.cancer.org.au//Healthprofessionals/patientfactsheets/Lifestyle/Get_checked_women.htm. accessed 16 October 2010.
35 Sankaranarayanan R, Nene BM, Shastri SS, et al. HPV screening for cervical cancer in rural India. N Engl J Med. 2009;360:1385.
36 US Preventive Services Task Force. Screening for cervical cancer: recommendations and rationale. Agency for Healthcare Research and Quality. Available at www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm. accessed 16 December 2010.
37 Ashton K, Proietto A, Otton G, Symonds I, McEvoy M, et al. Oestrogen receptor polymorphisms and the risk of endometrial cancer, Br J Obst & Gynaecol. 2009;116:8. Available at http://onlinelibrary.wiley.com/doi/10.1111/j.1471-0528.2009.02185.x/ful accessed 16 October 2010.
38 Australian National Endometrial Cancer Study. What is endometrial cancer? Available at www.anecs.org.au/html/Whatis.html. accessed 17 December 2010.
39 New Zealand Gynaecological Cancer Foundation. Gynaecological cancers (includes endometrial cancer). Available at www.silverribbon.co.nz/index.cfm/pageid/31/ViewPage/Uterine+Cancer. accessed 17 December 2010.
40 Permuth-Wey J, Sellars T. Epidemiology of ovarian cancer. Methods Molec Biol. 2009;472(II):413–437.
41 Australian Institute of Health & Welfare (AIHW). Ovarian cancer in Australia. Available at www.aihw.gov.au/publication-detail/?id=6442468331, 2010. accessed 30 March 2011.
42 New Zealand Gynaecological Cancer Foundation. Ovarian cancer in New Zealand. Available at www.silverribbon.co.nz/index.cfm/pageid/11/ViewPage/Ovarian+Cancer+in+New+Zealand. accessed 17 December 2010.
43 American Cancer Society. Cancer facts and figures. Available at www.cancer.org/Cancer/BreastCancer/DetailedGuide/breast-cancer-what-causes, 2009. accessed 16 December 2010.
44 Visintin I, Feng Z, Longton G, et al. Diagnostic markers for early detection of ovarian cancer. Clin Cancer Res. 2008;14:1065.
45 Anderson N, Hacker E. Fatigue in women receiving intraperitoneal chemotherapy for ovarian cancer. Clin J Oncol Nurs. 2008;12:445.
46 Grulich A, Fenji J, Conway L, Stein A, Hocking J. Cancers attributable to human papilloma virus infection. Sexual Health. 2010;7:244–252.
47 Candiani M, Izzo S, Bulfoni A, et al. Laparoscopic vs vaginal hysterectomy for benign pathology. Am J Obstet Gynecol. 2009;200:368.
48 Uterine prolapse. In: Ferri’s clinical advisor, 2009: instant diagnosis and treatment. Philadelphia: Mosby; 2009.
49 Herbruck L. Urinary incontinence in the childbearing woman. Urol Nurs. 2008;28:163.
50 McGee M, Delaney C. Stomas and fistulas. In: Walsh D, Caraceni A, Fainsinger R, et al, eds. Palliative medicine. Philadelphia: Saunders, 2008.
ACCESS—Australia’s National Infertility Network. www.access.org.au
Australasian Chapter of Sexual Health Medicine. www.racp.edu.au/page/australasian-chapter-of-sexual-health-medicine/
Australasian Menopause Society. www.menopause.org.au
Cancer Council Australia. www.cancer.org.au
Cancer Society of New Zealand. www.cancernz.org.nz
Fertility NZ. www.fertilitynz.org.nz
HealthInsite: pelvic inflammatory disease. www.healthinsite.gov.au/topics/pelvic_inflammatory_disease
National Breast and Ovarian Cancer Centre. www.nbocc.org.au
National Cervical Screening Program. www.cervicalscreen.health.gov.au
New Zealand Guidelines Group. www.nzgg.org.nz
New Zealand Health Information. www.everybody.co.nz
Ovarian Cancer Australia. www.ovariancancer.net.au
Women’s Health Action Trust. www.womens-health.org.nz

















