Chapter 68 NURSING MANAGEMENT: emergency care situations
1. Understand the principles of patient assessment in the emergency department, including triage, primary survey and secondary survey.
2. Differentiate between the various types and victims of violence: accidental versus abuse (domestic violence and children at risk).
3. Recognise the significance of ‘mechanism of injury’ and initial signs and symptoms for identifying actual or potential traumatic injury.
4. Describe the pathophysiology, assessment and multidisciplinary care of select environmental emergencies, including hyperthermia, hypothermia and submersion injury.
5. Identify a selection of Australia’s venomous creatures and discuss the principles of management for envenomation.
6. Explain the principles of care for select toxicology emergencies.
7. Explore the strategies of preparedness for the management of major incidents, emergency and/or disaster.
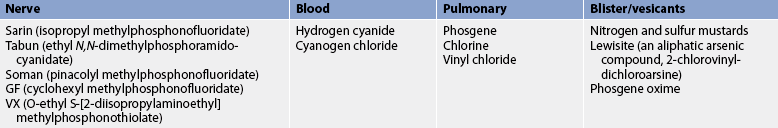
8. Describe the toxic agents and the principles of management for chemical, biological and radiation hazards.
Presentations to emergency departments (EDs) range across a wide spectrum of cases of all ages, encompassing medical, surgical, obstetric and psychological emergencies. These cases may present as immediate or potentially life-threatening cases, such as major trauma, acute cardiac and/or respiratory disease or acute psychological distress, or as less urgent cases, such as minor wounds or localised infections. Emergency nurses must be prepared to assess the range of cases and have sufficient clinical knowledge to determine the priorities of care. In ED, medical and nursing staff work collaboratively to ensure effective and efficient patient assessment and management. In many EDs nurses now assume advanced practice roles where they are responsible for advanced assessment and patient management strategies undertaking activities that, in the past, were considered solely the domain of medicine. This chapter examines both nursing care and multidisciplinary care.
In addition to the variety of presentations, EDs are faced with increasing numbers of presentations. The number of visits to the ED and the acuity of patient illnesses have increased significantly over the past decade. This is due to several reasons, which include:
• Population and social change. For example, Australia’s population grew from 16.9 million in 1989 to 22.2 million by 2010. This increase is predominantly the result of immigration rather than the birth rate; consequently, the population in general is ageing, which increases the burden on health services.1–3 In 2010, New Zealand’s population was approximately 4.4 million. New Zealand is facing a different problem to Australia due to a negative migration rate; however, this has also led to an ageing of the population.4
• Cost and access. EDs provide a 24-hour a day service, which is funded through the public taxation system. (Australia and New Zealand have reciprocal agreements for the provision of emergency services to citizens and permanent residents.) Since many general practitioners now charge fees on top of the government rebates, this increases the attractiveness of attending EDs, which are free at the point of service. Furthermore, ED services are supported by the entire services of the hospital and are therefore able to offer a wider range of health services than general practitioners. EDs in local hospitals may be the only after-hours services available in some rural and remote regions.
This chapter focuses on the initial assessment and management of the emergency patient and emergency conditions, including heat- and cold-related emergencies, submersion injuries, toxicology management, envenomation and a brief discussion about non-accidental injuries and major incidents and disaster preparedness. Table 68-1 provides a summary of where the management of various emergency situations can be found in this textbook.
| Title | Table |
|---|---|
| Abdominal trauma | 42-8 |
| Acute abdominal pain | 42-7 |
| Acute soft-tissue injury | 62-2 |
| Anaphylactic shock | 13-11 |
| Arrhythmias | 35-4 |
| Chemical burns | 24-2 |
| Chest pain | 33-14 |
| Chest trauma | 27-13 |
| Cocaine and amphetamine toxicity | 10-5 |
| Diabetic ketoacidosis | 48-11 |
| Electrical burns | 24-4 |
| Eye injury | 21-3 |
| Fractured extremity | 62-5 |
| Head injury | 56-6 |
| Hyperthermia | 68-6 |
| Hypothermia | 68-7 |
| Inhalation injury | 24-3 |
| Overdose of depressant drugs | 10-9 |
| Sexual assault | 53-8 |
| Shock | 66-6 |
| Spinal cord injury | 60-3 |
| Stroke | 57-2 |
| Submersion injuries | 68-8 |
| Surface skin wound | 23-6 |
| Thermal burns | 24-5 |
| Thoracic injuries | 27-14 |
| Tonic–clonic seizures | 58-4 |
Assessment of the emergency patient
The initial assessment of patients presenting to emergency begins with triage, a process of identifying the primary problem and prioritising the patients in an order to be seen. The word triage is of French origin meaning ‘to sort or choose’ and has been adopted into military, disaster and emergency management services to provide a systematic approach for the categorisation of patients, from the critically ill requiring immediate interventions to those who can wait.5,6
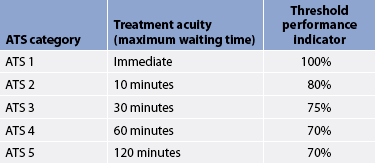
In Australia, triage category scales have evolved over the past 30 years. The Box Hill Triage Scale and the Ipswich Triage Scale were developed during the 1970s and the Australasian College of Emergency Medicine (ACEM) adapted these scales to develop the National Triage Scale during the early 1990s. During the late 1990s it was refined and renamed the Australasian Triage Scale (ATS). This triage system is used widely throughout New Zealand and Australia.5 Table 68-2 provides an overview of the ATS.
Triage is this first point of contact for patients presenting to the ED and is a rapid process beginning with the visual assessment. Visual assessment may be conducted from across the room, providing valuable information regarding the patient’s health status, including:
Visual assessment aids are used to determine who to see first when more than one person presents at the same time. In addition to visual assessment, the triage nurse must interview patients to identify the primary problem, assess their vital signs and determine the urgency of their complaint.
CONTINUING ASSESSMENT AND CARE OF THE EMERGENCY PATIENT
Following triage the patient undergoes a thorough assessment to determine the initial interventions, identify the underlying cause and plan the definitive management required.
The principles of patient assessment use all of the nurse’s senses except taste. Visual assessment provides valuable information, essentially determining whether the patient ‘looks good’ or ‘looks bad’ and the initial priority. Auditory assessment identifies the patient in distress, such as noisy respiration, pain or psychological distress, and enables the nurse to listen to the patient’s concerns. Auditory assessment also involves auscultation of the blood pressure, chest and abdomen. Touch provides information about the patient’s temperature, pulses and perfusion, as well as palpation of areas of pain or injury. Smell may identify odours such as ketosis (fruity smell to the breath), urine infection, melaena and infected or gangrenous wounds.
A systematic approach to patient assessment is called the primary and secondary survey. This approach was originally developed for the assessment of trauma patients but it can be applied for the assessment of any emergency patient. The primary and secondary survey extends beyond the A, B, Cs of basic and advanced life support to a method of complete patient assessment encompassing the letters A, B, C, D, E, F, G, H and I.7 There are some slight variations in the meaning of the letters E, F and G; however, the principles are consistent and provide a standardised, systematic approach that reduces the risk of missed injuries or associated signs and symptoms.
PRIMARY SURVEY
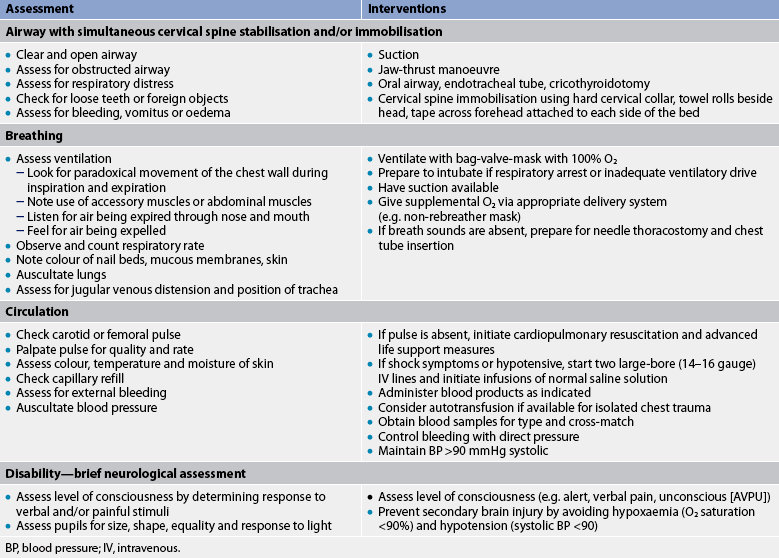
The primary survey (see Table 68-3) focuses on airway, breathing, circulation and disability, and serves to identify life-threatening conditions so that appropriate interventions can be initiated. Life-threatening conditions (see Box 68-1) must be managed prior to proceeding with any further assessment. If the patient presents following a traumatic incident, the assessment is conducted while maintaining cervical spine alignment.
BOX 68-1 Causes of life-threatening conditions identified during the primary survey*
*List is not all-inclusive.
A = airway with cervical spine stabilisation and/or immobilisation
The airway is always the initial focus. If the airway is not established and maintained, obstruction of airflow may occur, leading to hypoxia, anaerobic metabolism, acidosis and death. Airway obstruction may occur due to:
• the position of the patient occluding their airflow; patients at risk are those with an altered level of consciousness, such as secondary to stroke, head injury, intoxication, drug overdose, seizures, metabolic disorders, sepsis and hypoxia
• secretions, such as saliva, blood, vomitus
• laryngeal trauma, facial trauma or fractures
• oedema of the upper airway: burns, anaphylaxis, trauma
Primary signs and symptoms of a compromised airway include dyspnoea, coughing, hoarseness of the voice or an inability to vocalise, the presence of a foreign body in the airway, and trauma to the face or neck. Airway maintenance should progress rapidly from the least to the most invasive method. Treatment includes:
• positioning the patient to ensure that there are no anatomical obstructions of the airway (the neutral position maintaining cervical spine alignment)
• opening the airway using the jaw-thrust or chin-lift manoeuvre (avoiding hyperextension of the neck; see Fig 68-1)
• suctioning and/or removal of a foreign body
• insertion of a nasopharyngeal or oropharyngeal airway to maintain a patent airway (in cases of facial trauma and possible base of skull fractures nothing is passed into the patient’s nasopharyngeal region due to the risk of it passing through the base of the skull)
• endotracheal intubation to maintain an airway in a compromised patient. Patients should be ventilated with 100% oxygen using a bag-valve-mask (BVM) device before intubation. If intubation is difficult or unable to be achieved due to airway obstruction, an emergency cricothyroidotomy or tracheotomy should be performed (see Ch 26).
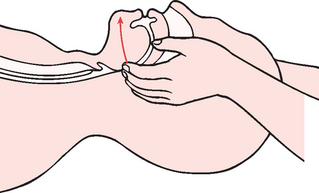
Figure 68-1 The jaw-thrust manoeuvre is the only widely recommended airway-opening procedure for use on an unconscious patient with possible neck or spinal injuries. The patient should be lying supine with the rescuer kneeling at the top of the head. The rescuer should carefully reach forwards and gently place one hand on each side of the patient’s chin at the lateral angles of the lower jaw. The patient’s head should be stabilised with the rescuer’s forearms, then the jaw pushed forwards while pressure is applied with the index fingers.
Rapid-sequence induction is the preferred procedure for intubation. It involves the use of sedating and short-acting paralysing agents to facilitate intubation while minimising the risk of aspiration.8 Common pharmacological preparations used include thiopentone (a rapid-onset, short-acting sedating agent) and suxamethonium (a short-acting depolarising neuromuscular blocking agent).9
Cervical spine precautions should be taken for any patient who has presented following traumatic injury until the cervical spine is cleared of injury. The cervical spine must be stabilised (head maintained in a neutral position) and/or immobilised during assessment of the airway. At the scene of the injury, the cervical spine is immobilised with a rigid cervical collar or a cervical immobilisation device (CID) (also known as ‘head blocks’). Application of a neck immobilisation device does not ensure complete spinal stabilisation. This, in combination with a spinal board with appropriate securing, is more effective. The rigid spinal board should be removed as soon as possible to reduce risk of pressure areas. This is usually done during the secondary survey when inspection and palpation of the spine are performed.10
B = breathing
Breathing is addressed immediately after establishing an airway. A patent upper airway allows for the passage of airflow; however, it does not ensure adequate ventilation. Inadequate respiration may again result in hypoxia and ultimately death. Conditions that may compromise respiration and gas exchange include:
• trauma: fractured ribs, pneumothorax, haemothorax, penetrating injury or pulmonary contusions
• respiratory disease/infections: chronic airways disease, asthma, pneumonia, bronchiolitis
• pulmonary oedema: cardiogenic, aspiration syndrome, such as in post-submersion injury
• altered level of consciousness leading to depressed respiratory effort and poor gas exchange.
Signs and symptoms of respiratory compromise include dyspnoea, tachypnoea or bradypnoea, cyanosis, tachycardia, anxiety, confusion, decreased level of consciousness, chest pain, paradoxical or asymmetrical chest wall movement (e.g. chest trauma, flail chest, pneumothorax), decreased or absent breath sounds on the affected side (e.g. pneumothorax, consolidation and atelectasis) and a visible wound to the chest wall (e.g. penetrating injury).
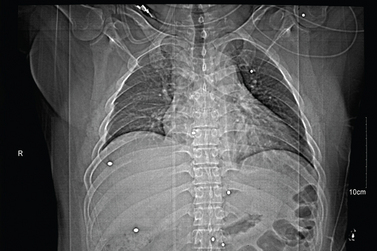
Patients who present with significant trauma or acute illness have an increased metabolic and oxygen demand and should have supplemental oxygen. Even patients with chronic respiratory disease, who have increased risk of carbon dioxide retention, require supplemental oxygen in acute stages of hypoxia. Patients with acute illness and significant trauma should be commenced on high-flow oxygen. A non-rebreather mask delivers oxygen concentrations close to 60–80%. The patient’s response should be monitored closely. Conditions such as a large pneumothorax or haemothorax and flail chest can severely compromise ventilation. Interventions in these situations include BVM ventilation with 100% oxygen, intercostal catheter insertion and possible intubation. If a tension pneumothorax is present, urgent decompression of the thorax is required. This requires the insertion of a 12–14-gauge needle in the second intercostal space and mid-clavicular line on the affected side, followed by chest drain insertion. An early chest X-ray is required for all patients displaying signs and symptoms of respiratory compromise. This will aid in the diagnosis of thoracic injuries and abnormalities of the heart, lungs and mediastinum.
C = circulation
The purpose of the circulatory system, in brief, is to transport oxygen and nutrients to the cells and to transport the waste products of metabolism away from the cells for excretion. Therefore, circulation assessment comes immediately after the establishment of adequate ventilation. An effective circulatory system includes the heart, intact blood vessels, adequate blood volume and the constituents of blood (e.g. haemoglobin, platelets). An ineffective circulatory system may be secondary to pump failure (impaired cardiac function), abnormality of the blood vessels (inappropriate vasoconstriction or dilation, occlusion or damage to blood vessels) or reduced blood volume (acute dehydration or haemorrhage). Inadequate circulation places a person at risk of impaired perfusion, inadequate transport of oxygen and essential nutrients, and inadequate excretion of waste products, leading to hypoxia, acidosis, shock and death. (See Ch 66 for information relating to the different types of shock and their management.)
Conditions that may lead to inadequate circulation include:
• cardiac failure: cardiogenic shock, congestive cardiac failure, acute myocardial infarction, arrhythmia
• spinal injury: neurogenic shock
• major haemorrhage: trauma, gastrointestinal (GI) bleeding, antepartum or postpartum haemorrhage
Signs and symptoms of inadequate circulation include hypotension, bradycardia or tachycardia, thirst, altered level of consciousness, delayed capillary refill (peripherally and/or centrally), decreased urine output, pallor and poor skin turgor.
A central pulse (e.g. carotid or femoral) should be checked in an adult and a brachial pulse in a child, because peripheral pulses may be absent as a result of injury to the limb or vasoconstriction in response to stress or shock. If a pulse is palpated, the quality and rate of the pulse should be assessed. Skin should be assessed for colour, temperature and moisture. Delayed capillary refill (>2 seconds) and altered mental status are the most significant signs of shock. Care must be taken when evaluating capillary refill after exposure to cold environments because cold delays refill. Capillary refill may be assessed peripherally and centrally to aid in determining the patient’s perfusion status.
The patient with inadequate circulation requires intravenous (IV) access to allow for fluid resuscitation as well as pharmacological management of the underlying condition if needed. An IV cannula is best inserted into veins in the upper extremities unless contraindicated, such as a fracture or injury that affects limb circulation. In the event of major trauma or shock, two large-bore (14–16 gauge) cannulas are recommended.
External haemorrhage should be managed by direct pressure or stapling. Early stabilisation of long bone fractures reduces haemorrhage from the fracture site. It is essential to identify any bleeding, find out what is causing it and plan early intervention to stop haemorrhage. A focused abdominal sonography test (FAST) is performed to identify any occult intraabdominal blood.10 Internal haemorrhage often requires fluid resuscitation to maintain the patient’s blood pressure above 90 mmHg (systolic). Normal saline (crystalloid solution) is the first-line fluid for resuscitation in adults and children. Blood samples are obtained for typing to determine the ABO group and Rh factor. Type-specific packed red blood cells and clotting factors should be administered if needed. In an emergency (life-threatening) situation, uncross-matched blood may be given if immediate transfusion is warranted. Early surgical intervention is essential.
Inadequate perfusion secondary to cardiogenic causes, sepsis, spinal injury, acute allergy, endocrine disorder or toxicology effects requires early treatment of the underlying cause.
D = disability
A brief, rapid assessment for neurological or motor deficit is included in the primary survey as it provides significant information linked to airway, breathing and circulation. A decrease in the patient’s level of consciousness indicates possible risks to their airway, ability to adequately ventilate and possible compromise of cerebral circulation.
The degree of disability is measured by the patient’s level of consciousness. Determining the patient’s response to verbal and/or painful stimuli is one approach to assessing level of consciousness. A simple method to remember is AVPU:
The Glasgow Coma Scale (GCS) is also used to further assess the arousal aspect of the patient’s consciousness (see Ch 56). Pupils should be assessed for size, shape, equality and response to light. In addition to level of consciousness, a rapid visual assessment during the primary survey may identify motor deficits and/or deformity of limbs due to injury.
SECONDARY SURVEY
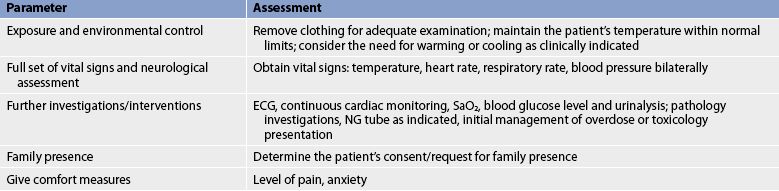
After each step of the primary survey has been addressed and any life-threatening conditions have been identified and interventions initiated, the secondary survey begins. The secondary survey is a brief, systematic process that is aimed at identifying all injuries and possible coexisting conditions (see Table 68-4).
E = exposure/environmental control
All trauma patients should have their clothes removed so that a thorough physical assessment can be performed. This applies to most patients presenting to the ED. Ensuring that the patient undresses allows for a thorough physical assessment. Once the patient is exposed, it is important to maintain privacy, limit heat loss and prevent hypothermia, especially in the compromised patient. Warming blankets, overhead warmers and warmed IV fluids may be required. Consideration must also be given to the hyperthermic patient who requires cooling measures.
F = full set of vital signs/further investigations/interventions/facilitate family presence
A complete set of vital signs—including blood pressure, heart rate, respiratory rate and temperature—should be obtained. Blood pressure should be obtained in both arms if the patient has sustained or is suspected of having sustained chest trauma or has a suspected aortic aneurysm. A difference in blood pressure in each arm may indicate major vessel injury.
At this point, it must be determined whether to proceed with the secondary survey or initiate additional interventions. The availability of other team members often influences this decision. Further investigations and/or interventions to consider include:
• an electrocardiogram (ECG) for heart rate, rhythm and function
• continued cardiac monitoring (depending on the patient’s acuity)
• pulse oximetry initiation and oxygen saturation monitoring
• urinalysis and possible indwelling catheter if indicated for the critically ill patient to monitor organ perfusion
• blood glucose level for patients with an altered level of consciousness and/or a history of diabetes
• pathology investigations (depends on presenting problem): haemoglobin, serum urea, creatinine, electrolytes, liver enzymes, cross-matching, coagulation factors, toxicology screening, β-human chorionic gonadotrophin (pregnancy), arterial blood gases and troponin for any suspected cardiac event
• radiology investigations: chest, films of specific injury
• management for overdose or toxicology exposure
• a nasogastric or orogastric tube may be indicated for the trauma patient or the patient requiring intubation.
Facilitating family presence completes this step of the secondary survey. Despite being contentious, some research has demonstrated positive benefits from the presence of family to patients, families and staff during resuscitation.11,12 Patients report that having family members present during invasive procedures comforts them, and enables family members to act as advocates as well as reminding the healthcare team of their personhood.10 Family presence during resuscitation can lead to increased patient comfort, family satisfaction and facilitation of information to staff and other family members.11,12 Should a family member request to be present during a procedure, it is essential that a dedicated member of the team explain the care being delivered and be available to answer questions. In addition, the adult patient must give consent for their presence.13
G = give comfort measures
Provision of comfort measures is of paramount importance when caring for patients in the ED. The incidence of patients presenting with pain to EDs is extremely high. The emotional or psychological effects of pain may outlast the physiological effects and may pose a risk to patients with underlying medical conditions. Pain management strategies should include both pharmacological preparations and the patient’s emotional needs.14 Emergency nurses play a pivotal role in pain management because of their frequent contact with patients. General comfort measures, such as verbal reassurance, listening, reducing stimuli (e.g. dimming lights) and developing a trusting relationship with the patient and family should be provided to all patients in the ED.
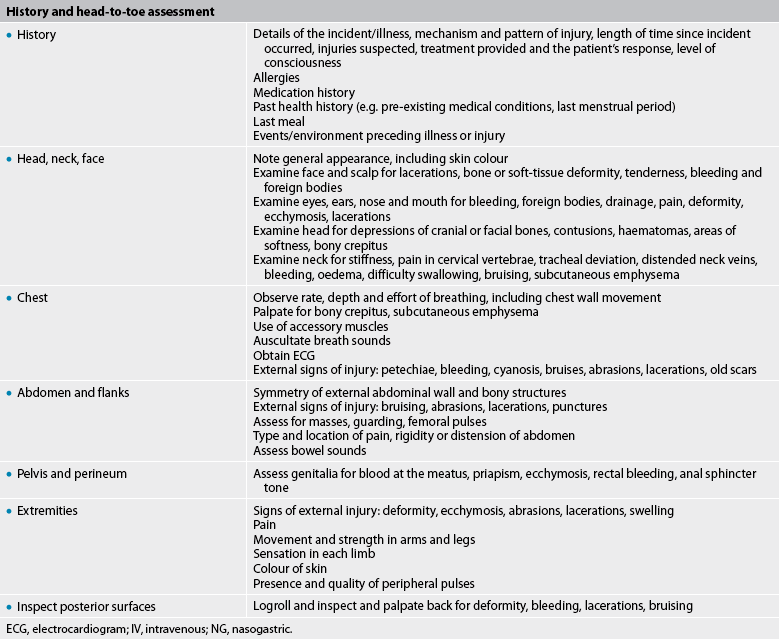
H = history and head-to-toe assessment
The history of the incident, injury or illness provides clues to the cause of the crisis and suggests specific assessment and intervention needs. The patient may be unable to give a history. However, family, friends, witnesses and pre-hospital personnel can frequently provide important information. Pre-hospital information should focus on the mechanism of injury (in the event of trauma), a history of events, vital signs, and treatment-initiated and patient responses.
Details of the incident are extremely important because for the trauma patient the mechanism of injury can predict specific injuries. For example, a front seat passenger with a seat belt may have a head injury from hitting the steering wheel; knee, femur or hip fractures or dislocation from striking the dashboard; and an abdominal injury from the seat belt.
Box 68-2 provides an overview of the factors that need to be considered at the scene of an accident when assessing the MIST criteria:
Mechanism of injury
Injury
• Penetrating injuries (except the limbs)
• Patients with a significant injury to a single region (e.g. head, neck, chest, abdomen, axilla, groin)
• Patients with lesser injuries involving two or more body regions
• Blunt trauma to two or more body regions
• Burns: airway and/or >20% body surface area (BSA) in an adult or >10% BSA in a child
The MIST criteria outline factors that should alert ED staff about the possibility of significant injury and the need for early focused trauma assessment and intervention.15
Pre-hospital personnel can often provide a detailed description of the patient’s general condition, level of consciousness and primary complaint or apparent injuries. An experienced ED team can complete a history within a few minutes of the patient’s arrival. If the patient is critically ill, a thorough history is obtained from family or friends after the patient is taken to the treatment area. The history should include the following questions:
1. What is the chief complaint? What caused the patient to seek attention?
2. What is the history of the presenting complaint?
3. What are the patient’s subjective complaints?
4. What is the patient’s description of pain (e.g. onset, location, duration, quality, character)?
5. How has this complaint affected the patient (i.e. reduced level of self-care, reduced mobility)?
6. What is the patient’s health history? The mnemonic AMPLE assists the nurse to obtain a complete history:
7. In the event of an injury, is this an accidental injury or is this patient a victim of assault?
This final question may identify a victim of a violent crime. In the case of adults, the person may wish to report the incident to police. Special cases of crimes that the emergency nurse must be aware of include:
• domestic violence, where the person presenting is exposed to a pattern of coercive behaviour in a relationship that involves fear, humiliation, intimidation, neglect and/or intentional physical, emotional, financial or sexual injury. (See Ch 53 for information about sexual assault.) Domestic violence is found in all professions, cultures, socioeconomic groups, ages and genders. Although men can be victims of domestic violence, most victims are women, children and the elderly.16
• child abuse (children at risk), where a child who is exposed to the abuse described above or who is witness to another family member being abused must be notified to the relevant department of community services. It is the responsibility of all healthcare workers to observe for the possible signs of child abuse. For any child who presents with an injury, the question must be asked ‘Does the injury match the mechanism of injury described?’
Any patient who is found to be a victim of abuse should be provided with appropriate interventions—this includes making referrals, providing emotional support and informing victims about their options (e.g. safe house, legal rights).16
Head, neck and face
The patient should be assessed for general appearance, skin colour and temperature. The eyes should be evaluated for extraocular movements. A disconjugate gaze is an indication of neurological damage. Bilateral haematoma to the eye region (raccoon eyes) or periorbital bruising is usually associated with a base of skull fracture (see Fig 56-13).10 The base of the skull lies behind the nasopharyngeal region. Fractures often result in cerebrospinal fluid (CSF) leaks, and anything passed via the nose in a person with a base of skull fracture may pass through the fracture into the cerebral space. The tympanic membranes and external canal should be checked for blood and CSF. Clear drainage from the ear or nose should be observed and monitored as a likely CSF leak. Packing of the nose and/or ears may stem the flow and reduce the risk of a portal of entry for infection into the brain.
The airway should be assessed for foreign bodies, bleeding, oedema and loose or missing teeth. It is also important to assess for difficulty swallowing, movement of the palate and ability to open the mouth. The neck should be examined for bruising, oedema, bleeding, distended neck veins and points of tenderness. The trachea should be palpated and visualised to determine whether it is in the midline. A deviated trachea may signal a life-threatening tension pneumothorax or massive haemothorax. Subcutaneous emphysema may result from a large pneumothorax or indicate laryngeal–tracheal trauma. A stiff or painful cervical spine may signify a fracture of a cervical vertebra. The cervical spine must be protected by using a rigid collar and maintaining the neutral position of the spine. Patients must be logrolled when movement is necessary.7
Chest
The chest should be examined for respiratory effort, use of accessory muscles and the possibility of paradoxical/asymmetrical chest movements and sucking chest wounds. The sternum, clavicles and ribs should be palpated for deformity and point tenderness. The chest should be assessed for pain on palpation, signs of respiratory distress, decreased breath sounds, noisy respiration such as crackles/rales or wheezes, signs of injury, distant heart sounds and distended neck veins. In addition to pneumothorax and open pneumothorax, the patient should be evaluated for rib fractures, pulmonary contusion, blunt cardiac injury and simple pneumothorax. A 12-lead ECG should be obtained, particularly on an older patient or a patient with suspected heart disease. The ECG should be done to detect arrhythmias and evidence of ischaemia or infarction. A chest X-ray will determine the presence of blood or air in the pleura, areas of disease and the size and shape of the thoracic structures.
Abdomen and flanks
The abdomen and flanks are more difficult to assess. Frequent evaluation for subtle changes in the abdominal examination is essential. Blunt trauma to the abdomen may result from assault, falls from a significant height or a motor vehicle accident, all of which have the potential for major vessel or organ trauma. Penetrating trauma tends to injure specific organs. Decreased bowel sounds may indicate a temporary paralytic ileus or bowel obstruction. Bowel sounds in the chest may indicate a diaphragmatic rupture. The abdomen should be inspected for distension, scars and other abnormalities, auscultated for bowel sounds, percussed for distension (e.g. tympany [excessive air], dullness [excessive fluid]) and palpated for pain, tenderness, rigidity, guarding and masses.10
If an acute abdomen is suspected, further investigations may include computed tomography (CT) scan, ultrasound or diagnostic peritoneal lavage (DPL, for trauma cases with suspected intraabdominal haemorrhage) to identify the need for urgent surgical intervention.
Pelvis and perineum
If the patient has fallen or suffered trauma, the pelvis should be palpated gently. If pain is elicited, it may indicate a pelvic fracture. The genitalia should be inspected for bleeding and obvious injuries. Blood at the urethral meatus is indicative of a urethral injury. A rectal examination should check for blood, a high-riding prostate gland and loss of sphincter tone (loss of anal sphincter tone may indicate spinal injury). It is also important to assess for bladder distension, haematuria, dysuria or the inability to void.
Extremities
The upper and lower extremities should be observed for colour and perfusion, deformity and swelling, and palpated for point tenderness, crepitus sensation and pulses. Injured extremities should be elevated, while maintaining spinal alignment, and ice packs applied. Injured extremities are splinted above and below the injury to decrease further soft-tissue injury and pain. Grossly deformed extremities should be realigned and splinted. Pulses should be checked before and after movement or splinting of an extremity. A pulseless extremity represents a time-critical vascular or orthopaedic emergency. Prophylactic antibiotics and tetanus prophylaxis are administered for open fractures.10 Patients with fractures should receive intravenous analgesia due to the acuteness and severity of the pain.14
I = inspect the posterior surfaces
The trauma patient should always be turned (using spinal precautions) to inspect the posterior surfaces. The back should be inspected for bruising, abrasions, puncture wounds, cuts and obvious deformities. The entire spine should be palpated for misalignment, deformity and pain.10
EVALUATION AND DOCUMENTATION OF FINDINGS
The primary and secondary surveys provide information for the continued prioritisation of the patient’s need for intervention and further investigation, including life support measures, analgesia, hydration and electrolyte maintenance, antibiotics, vaccines (e.g. tetanus prophylaxis; see Table 68-5), correction of metabolic disturbances such as control of diabetes, and arrhythmia management. All assessment findings and the management instigated require documentation. Concise accurate documentation provides an ongoing record of the patient’s health status and the healthcare team’s responses.
TABLE 68-5 Therapeutic guidelines for tetanus
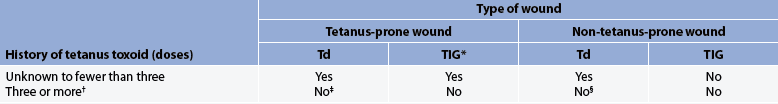
Td, tetanus-diphtheria toxoid absorbed (for adult use); TIG, tetanus immune globulin (human).
* When TIG and TD are administered concurrently, separate sites and syringes must be used.
† If only three doses of fluid toxoid have been received, a fourth dose of toxoid, preferably absorbed toxoid, should be given.
‡ Yes, if more than 5 years since last dose. More frequent boosters are not needed and can accentuate side effects.
Regardless of the patient’s chief complaint, ongoing patient monitoring and evaluation of the interventions are critical in an emergency situation. The nurse is responsible for providing appropriate interventions and assessing the patient’s response. The evaluation of airway patency and the effectiveness of breathing and circulation will always assume highest priority. The nurse should monitor oxygenation and cardiovascular status to help determine the patient’s progress in these areas. Level of consciousness, vital signs, quality of peripheral pulses, urine output and skin temperature, colour and moisture provide key information about circulation and perfusion and are also monitored.
Depending on the patient’s injuries and/or illness, the patient may be: (1) transported for diagnostic tests such as a CT scan, X-ray or magnetic resonance imaging (MRI); (2) admitted to a ward or an intensive care unit; or (3) transferred to another facility. The emergency nurse is responsible for monitoring the patient up to the time of transfer and, in some cases, during the transfer process. Nurses accompanying critically ill patients on intrahospital or interhospital transfers must be competent in advanced life support measures.
DEATH IN THE EMERGENCY DEPARTMENT
Unfortunately, a number of emergency patients are not able to benefit from the skill, expertise and technology available in the ED and may die on their way to hospital or soon after arrival in the ED. It is important for emergency nurses to be able to deal with their feelings about sudden death so that they can help families and significant others begin the grieving process.
The emergency nurse should recognise the importance of legal requirements for deaths in hospital, in particular preserving evidence in a Coroner’s case, and for specific cultural needs in caring for the body after death and preparing the bereaved to grieve. The Coroner’s Act outlines the legal requirements surrounding deaths in hospitals. The emergency nurse may be involved in collecting the belongings of the deceased and passing them on to relatives or to police if required for evidence (appropriate documentation of belongings must occur), viewing the body and preparing the family for the possibility of organ donation. The nurse plays a significant role in providing comfort to the surviving loved ones.
Many patients who die in the ED could potentially be candidates for organ donation. Tissues and organs such as corneas, heart valves, bone, kidneys and skin can be harvested from patients after death. Approaching families about donation after an unexpected death is distressing to both the staff and the family. Nevertheless, for many families the act of donation may be the first positive step in the grieving process.17 Many hospitals have on-site organ donation staff, who may assist with the process of screening potential donors, counselling donor families, supporting medical and nursing staff, and obtaining informed consent for organ donation. Early referral to a social worker may be helpful.
ENVIRONMENTAL EMERGENCIES
Increased interest in outdoor activities, such as running, hiking, cycling, skiing, sailing and swimming, has increased the number of environmental emergencies seen in the ED. Illness or injury may be caused by the activity, exposure to weather, or attack from various animals or humans. Specific environmental emergencies discussed in this section include heat-related emergencies, cold-related emergencies, submersion injuries, bites, stings and envenomation.
Emergency care: paediatric and gerontological considerations
Both ends of the age spectrum presenting to the ED warrant special consideration and a lower threshold for allocating a higher triage category code. Risks associated with the extremes of age include the following.
Children have lower blood volume and higher body water content and therefore do not tolerate blood loss well. They are rapidly dehydrated, especially when they have high temperatures and low oral intake.
The very elderly have a lower total body water content and therefore decreased reserves to cope with decreased fluid intake.
Children have a relatively large body surface area, a small body mass and an immature hypothalamus, which places them at greater risk of hypothermia if left exposed to cold and of hyperthermia if left exposed to heat.
The very elderly, due to the general decline in metabolic processes and decreased muscle and fat deposits, are at an increased risk of both hypothermia and hyperthermia.
• Decreased response/reserves to cope with stress
Children have immature myocardial compliance and immature reserves in their response to stress.
The very elderly also have decreased myocardial compliance, a decreased immune response and decreased reserves to cope with stress.
Children’s bones are more malleable than adults’ bones. This poses the risk of greenstick fractures and underlying soft-tissue injury, or spinal injury without bony deformity.
The very elderly have a greater risk of fractures due to a decline in essential mineral deposits, leading to a decreased bone density.
Children’s needs are different from adults, and nurses need to be aware of the stages in a child’s development so that they can respond appropriately to children’s needs and so reduce anxiety and provide a safe environment.
The very elderly are at an increased risk of confusion and/or dementia and this can pose challenges in the approach to their management to reduce anxiety and provide a safe environment.
Which colloid solutions are safest for intravascular volume replacement?
EVIDENCE-BASED PRACTICE
Clinical question
For critically ill patients requiring volume replacement (P), do some types of colloid solutions administered (I) increase adverse reactions or mortality (O)?
Conclusion
• Although significant differences may exist among colloids, there is no evidence that one colloid is more effective or safe than another when replacing intravascular fluid.
• Larger trials of fluid therapy are needed if clinically significant differences in mortality rate are to be detected or excluded.
Heat-related emergencies
Humans need to maintain a core body temperature within a relatively narrow range (36–37.3°C) to allow for normal cellular function. The hypothalamus is the primary centre for body temperature regulation and responds to environmental changes by producing physiological and powerful behavioural responses to either conserve and produce heat or reduce body temperature. Exposure to heat or cold for prolonged periods may overwhelm the body’s normal responses to maintain a normal core temperature, leading to hyperthermic or hypothermic states.
Physiological and behavioural responses to maintain body temperature include:
• increased activity to produce heat, decreased activity to reduce heat
• donning more clothing to conserve heat, removing clothing to reduce heat
• eating or drinking warm fluids to produce heat, drinking cool drinks to reduce heat
• shivering/piloerection to produce heat, perspiration to reduce heat
• increased respirations to reduce heat
• vasoconstriction to conserve heat centrally, vasodilation to reduce central heat.18
Factors that contribute to hyperthermia or hypothermia include:
• prolonged exposure to extremes in temperature
• inappropriate clothing—excessive in hot climates, inadequate clothing and/or wet clothing in cold temperatures
• wind chill factor—exposure to wind increases the loss of heat from the body via convection
• poorly ventilated areas/enclosed spaces (e.g. locked cars left in the sun—temperatures within cars left exposed to the summer sun may be fatal, particularly for young children or the elderly)
• body fat—aids in conserving the core body temperature: persons who are significantly underweight are at risk of hyperthermia or hypothermia; obesity increases the risk of hyperthermia
• circulating blood volume—adequate circulation aids in maintaining body temperature
• restrictive circulation (restrictive clothing may increase the risk of hypothermia), arterial disease and hypertension may interfere with the body’s normal responses to maintain body temperature
• excessive activity in the heat—this may lead to dehydration and hyperthermic states
• fatigue, smoking, poor nutrition—may all reduce people’s ability to maintain their core body temperature
• age—the elderly and the very young have reduced reserves to maintain core body temperature.19,20
Environmental hyperthermia
Environmental hyperthermia is said to exist when there is a rise in the body temperature as a result of exposure to heat. Brief exposure to intense heat or prolonged exposure to less intense heat leads to heat stress when thermoregulatory mechanisms, such as sweating, vasodilation and increased respirations, cannot compensate for the exposure to increased ambient temperatures.18 Strenuous activities in hot or humid environments and clothing that interferes with perspiration can all lead to environmental hyperthermia (see Box 68-3).20 Effects can be mild (heat rash) with mild dehydration, or severe (heat exhaustion and heat stroke) associated with severe dehydration. The management of heat-related emergencies is summarised in Table 68-6.
BOX 68-3 Risk factors for heat-related emergencies
Source: Adapted from Howard PK, Steinmann RA, eds. Sheehy’s emergency nursing. 6th edn. St Louis: Mosby; 2010.
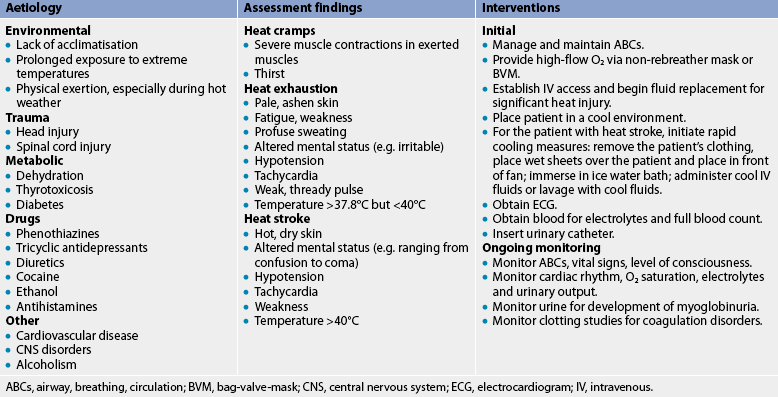
ABCs, airway, breathing, circulation; BVM, bag-valve-mask; CNS, central nervous system; ECG, electrocardiogram; IV, intravenous.
Heat rash is a fine, red, papular rash that occurs on the torso, neck and skinfolds. The rash occurs when sweat ducts are obstructed and become inflamed so that sweat excretion is inhibited. The rash usually occurs in warm weather but has also been reported in cold weather as a result of clothing.
Heat syncope is associated with prolonged standing and heat exposure. Manifestations include dizziness, orthostatic hypotension and syncope. (Syncope is discussed in Ch 36.) The elderly are at greater risk due to changes to vasomotor tone associated with ageing.
Heat oedema is characterised by swelling of the hands, feet and ankles, usually in non-acclimatised individuals, as a result of prolonged standing or sitting. Swelling usually resolves in days with rest, elevation and support stockings. Diuretics are not recommended as this condition is self-limiting and requires no additional treatment.
HEAT CRAMPS
Heat cramps are severe cramps in large muscle groups, commonly the abdomen, arms and legs, after strenuous activity. They are generally as a result of decreased body water content and loss of salt through sweat. Other associated symptoms include nausea, pallor, weakness (heart rate may be normal or slightly raised) and diaphoresis. The condition is seen most often in healthy, acclimatised athletes with inadequate fluid intake. Management is to rest and allow the body to cool. Cramps generally resolve rapidly with rest and oral or parenteral replacement of water and sodium. Elevation, gentle massage and analgesia may assist with pain associated with heat cramps. The patient should avoid strenuous activity for at least 12 hours after the development of heat cramps. Commercially prepared electrolyte solutions (e.g. sports drinks) are recommended.18
HEAT EXHAUSTION
Prolonged exposure to heat over hours or days leads to heat exhaustion, a clinical syndrome characterised by fatigue, light-headedness, nausea, vomiting, diarrhoea and feelings of impending doom (see Table 68-6). Tachypnoea, hypotension, tachycardia, elevated body temperature, dilated pupils, mild confusion, ashen colour and profuse diaphoresis are also present. Hypotension and mild-to-severe temperature elevation (37.5–40°C) are due to dehydration.21 Heat exhaustion usually occurs in individuals engaged in strenuous activity in hot, humid weather, but it also occurs in sedentary individuals.18
Treatment begins by placing the patient in a cool area and removing constrictive clothing. The patient is monitored for airway, breathing and circulation (ABCs), including cardiac arrhythmias (due to electrolyte imbalances). Oral fluid and electrolyte replacement is initiated unless the patient is nauseated. Salt tablets are not recommended because of potential gastric irritation and hypernatraemia. A 0.9% saline solution is initiated intravenously when oral solutions are not tolerated. An initial fluid bolus may be used to correct hypotension. However, fluid replacement should be correlated to clinical and laboratory parameters. Cooling measures include cold packs to the axilla and groin region. Hospital admission is considered for the elderly, the chronically ill or those who do not improve within 3–4 hours.
HEAT STROKE
Heat stroke, the most serious form of heat stress, results from failure of the central thermoregulatory mechanisms and is considered a medical emergency. Box 68-3 lists risk factors for heat-related emergencies, especially heat stroke. Increased sweating, vasodilation and increased respiratory rate (the body’s attempt to lower temperature) deplete fluids and electrolytes. Eventually, sweat glands stop functioning, so the core temperature increases rapidly. The patient has a core temperature greater than 40°C, altered mentation, absence of perspiration and circulatory collapse. The skin is hot, dry and ashen. The brain is extremely sensitive to thermal injuries; therefore, a range of neurological symptoms occur, such as hallucinations, loss of muscle coordination and combativeness. Cerebral oedema and haemorrhage may occur as a result of direct thermal injury to the brain and decreased cerebral blood flow.18
The development of heat stroke is directly related to the amount of time that the patient’s body temperature remains elevated.18 Prognosis is related to age, baseline health status and length of exposure. Older adults and individuals with diabetes mellitus, chronic renal disease, cardiovascular disease, pulmonary disease or other physiological compromise are particularly vulnerable.
Multidisciplinary care
Treatment of heat stroke focuses on stabilising the patient’s ABCs and rapidly reducing the core temperature.20 Administration of 100% oxygen compensates for the patient’s hypermetabolic state. Ventilation with a BVM or intubation and mechanical ventilation may be required. Fluid and electrolyte imbalances are corrected, and continuous cardiac monitoring for arrhythmia is initiated.
Various cooling methods are available, such as removing clothing; applying cold packs to the neck, axilla and groin region; placing the patient in front of a fan (evaporative cooling); administering cool fluids or lavaging with cool fluids.22 Wet sheets may be used to assist with cooling; however, this may lead to shivering.20 Whatever method is selected, the nurse is responsible for closely monitoring the patient’s temperature and controlling shivering. Shivering will increase core temperature due to the associated heat generated by muscle activity and complicates cooling efforts. A rectal probe is generally used to monitor temperature, yet there is a thermal lag with this measurement site and oesophageal or nasopharyngeal measurements produce more accurate responses. Careful fluid administration and fluid balance are required as the patient is at risk of cerebral oedema.
The patient is also monitored for signs of rhabdomyolysis (a potentially fatal disease characterised by breakdown of skeletal muscle). The muscle breakdown releases myoglobin and potassium, leading to myoglobinuria, which places the kidneys at risk of acute failure. Therefore, urine should be carefully monitored for colour, amount, pH and myoglobin. Finally, clotting studies are performed to monitor the patient for signs of disseminated intravascular coagulation (DIC; see Ch 30).
Patient and family teaching focuses on how to avoid future problems. Essential information regarding proper hydration during hot weather and physical exercise is imperative. Patients should also be instructed on the early signs of, and interventions for, heat-related stress.
Environmental hypothermia
Hypothermia, classified as a core temperature below 35°C, occurs when the body’s heat production mechanisms cannot compensate for heat loss. The major issues related to hypothermia are a reduction in metabolic function leading to organ dysfunction and cardiac arrhythmias. Approximately 55–60% of all body heat is lost as radiant energy, with the greatest loss from the head, thorax and lungs (with each exhalation).22 Wet clothing increases evaporative heat loss five times greater than normal; immersion in cold water increases heat loss by a factor of 25. Environmental exposure to freezing temperatures, cold winds and wet, damp conditions in the presence of physical exhaustion, inadequate clothing and/or inexperience predisposes individuals to hypothermia.22 Near-drowning and water immersion are also associated with hypothermia.
The elderly are more prone to hypothermia as a result of decreased body fat, diminished energy reserves, decreased basal metabolic rate, decreased shivering response, decreased sensory perception, chronic medical conditions and medications that alter body defences. In addition, certain drugs, alcohol and diabetes are considered risk factors for hypothermia.20
Hypothermia can present as cerebral or metabolic disturbances causing ataxia, confusion and withdrawal, so the patient may be misdiagnosed. Peripheral vasoconstriction occurs in an attempt to conserve heat. This shunts blood centrally and reduces the interaction of blood with the cooler extremities. As cold temperatures persist, shivering and movement produce body heat, yet the capacity to maintain normal body temperatures is limited. Death usually occurs when the core temperature falls below 28°C.
Symptoms of hypothermia include:
• 35°C: cold, pale skin, poor muscle coordination, shivering, tachypnoea, piloerection, tachycardia
• 35–32°C: no shivering, cold waxy skin, confusion, bradypnoea
• 32–30°C: muscle rigidity, poor reflexes, dilated pupils, hypotension, bradycardia, coma
• 30–28°C: flaccid muscles, fixed dilated pupils, arrhythmias, cardiac arrest.
As core temperature drops, the basal metabolic rate decreases two or three times. The cold myocardium is extremely irritable, so any movement can precipitate ventricular fibrillation. Decreased renal blood flow decreases the glomerular filtration rate, which impairs water reabsorption and leads to dehydration. The haematocrit increases as intravascular volume decreases. Cold blood becomes thick and acts as a thrombus, placing the patient at risk of stroke, myocardial infarction, pulmonary emboli, acute tubular necrosis and renal failure. Decreased blood flow leads to lactic acid accumulation from anaerobic metabolism and subsequent metabolic acidosis.
Profound hypothermia (<30.6°C) makes the person appear dead. Metabolic rate, heart rate and respirations are so slow that they may be difficult to detect. Reflexes are absent and the pupils fixed and dilated. Profound bradycardia, asystole or ventricular fibrillation may be present. Every effort is made to warm the patient to at least 32.2°C before the person is pronounced dead. The cause of death is usually refractory ventricular fibrillation.
Multidisciplinary care
Treatment of hypothermia focuses on managing and maintaining ABCs, rewarming the patient, correcting dehydration and acidosis, and treating cardiac arrhythmias (see Table 68-7). Passive or active external rewarming is used for mild hypothermia. Passive external rewarming involves moving the patient to a warm, dry place, removing damp clothing and placing warm blankets on the patient.20,22 Gentle handling is essential to prevent stimulation of the cold myocardium. Active external rewarming involves body-to-body contact, fluid- or air-filled warming blankets or radiant heat lamps. The patient should be closely monitored for marked vasodilation and hypotension during rewarming.
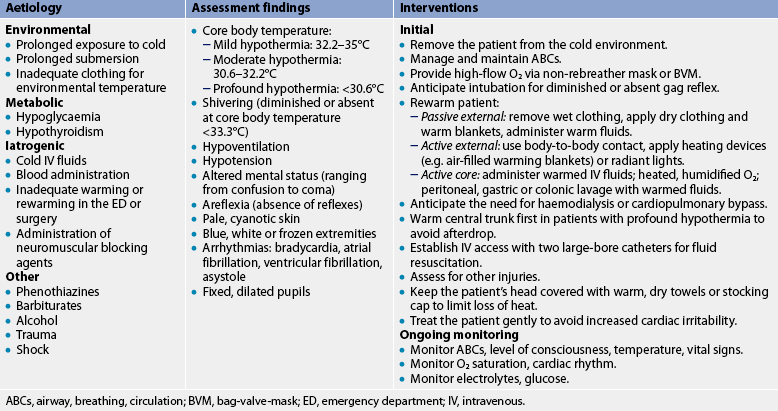
ABCs, airway, breathing, circulation; BVM, bag-valve-mask; ED, emergency department; IV, intravenous.
Active core rewarming is used for moderate-to-profound hypothermia and refers to heat applied directly to the core. Techniques include heated (40.6–46.1°C) humidified oxygen, warmed IV fluids and peritoneal or gastric lavage with warmed fluids. Haemodialysis or cardiopulmonary bypass may also be considered in profound hypothermia.20
Core temperature should be monitored carefully during rewarming procedures. Warming places the patient at risk of afterdrop, a further drop in core temperature, which occurs when cold peripheral blood returns to the central circulation. Afterdrop can produce hypotension and arrhythmias that negatively affect the rewarming efforts. Thus, patients with moderate-to-profound hypothermia should have the core warmed before the extremities.22
Patient teaching should focus on how to avoid future cold-related problems. Essential information includes dressing in layers for cold weather, covering the head, carrying high-carbohydrate foods for extra energy and developing a plan for survival should an injury occur.
Localised cold injury
FROSTBITE
Frostbite occurs more frequently in New Zealand than in Australia. Prolonged exposure in cold climates, particularly in the snow, without adequate clothing, increases a person’s risk of frostbite. Frostbite can be described as ‘true tissue freezing’, which results in the formation of ice crystals in the tissues and cells. Peripheral vasoconstriction is the initial response to cold stress and results in a decrease in blood flow and vascular stasis. As cellular temperature decreases and ice crystals form in intracellular spaces, intracellular sodium and chloride increase, the cell membrane is destroyed and organelles are damaged. These alterations result in oedema. The depth of frostbite is the result of ambient temperature, length of exposure, type and condition (wet or dry) of clothing, and contact with metal surfaces. Other factors that affect severity include skin colour (darker-skinned people are more prone to frostbite), lack of acclimatisation, previous episodes, exhaustion and poor peripheral vascular status.
Superficial frostbite involves skin and subcutaneous tissue, usually the ears, nose, fingers and toes. The skin appearance will range from pale to blue to mottled and the skin will feel crunchy and frozen. The patient may complain of tingling, numbness or a burning sensation. Injured tissue is easily damaged, so the area should be handled carefully and never squeezed, massaged or scrubbed. Clothing and jewellery should be removed because they may constrict the extremity and decrease circulation. The affected area should be immersed in a water bath (38.9–42.2°C).20 Warm soaks may be used for the face. The patient often experiences a warm, stinging sensation as tissue thaws. Blisters form within a few hours (see Fig 68-2). The blisters should be debrided and a sterile dressing applied. Heavy blankets and clothing should be avoided as friction and weight can lead to sloughing of damaged tissue. Rewarming is extremely painful. Residual pain may last weeks or even years. Analgesia should be administered and tetanus prophylaxis should be given as appropriate (see Table 68-5). The patient should be evaluated for systemic hypothermia.22

Figure 68-2 Oedema and blister formation 24 hours after frostbite injury occurring in an area covered by a tightly fitted boot.
Deep frostbite involves muscle, bone and tendon. The skin is white, hard and insensitive to touch. The area has the appearance of deep thermal injury with mottling gradually progressing to gangrene (see Fig 68-3). The affected extremity is submersed in a circulating water bath (38.9–42.2°C) until distal flush occurs. After rewarming, the extremity should be elevated to lessen oedema.22 Significant oedema may begin within 3 hours, with blistering in 6 hours to days. IV analgesia is always required in severe frostbite because of the pain associated with tissue thawing. Tetanus prophylaxis should be given (see Table 68-5), and the patient should be evaluated for systemic hypothermia. Amputation may be required if the injured area is untreated or treatment is unsuccessful. The patient may be admitted to the hospital for observation over 24–48 hours with bed rest, elevation of the injured part and prophylactic antibiotics if the wound is at risk of infection.
Submersion injuries
Submersion injury results when a person becomes hypoxic due to submersion in a substance, usually water. In 2009/2010, there were 314 drownings in Australia and approximately 800 hospitalisations as a result of drowning. In Australia, males are more likely to drown than females.23 In New Zealand, drowning is the third leading cause of death from unintentional injury, surpassed only by motor vehicle collisions and falls; on average, approximately 100 deaths occur annually as a result of drowning.24 Although the number of deaths by drowning has halved in New Zealand during the past 20 years, New Zealanders drown at twice the rate of Australians on a per capita basis.23,24
At the 2002 World Congress on Drowning, a group of experts suggested a consensus definition for drowning in order to decrease the confusion over the number of terms and definitions that had been previously used in the literature. The group believed that a uniform definition would allow more accurate analysis and comparison of data and studies and improve the accuracy of surveillance and prevention activities. The definition states that drowning ‘is a process resulting in primary respiratory impairment from submersion in a liquid medium’25,26 and the terms wet drowning, dry drowning, active or passive drowning, near-drowning, secondary drowning and silent drowning are no longer used. This internationally-accepted definition allows for the inclusion of fatal and non-fatal drowning. Immersion syndrome occurs with immersion in cold water; this leads to stimulation of the vagus nerve and potentially fatal arrhythmias (e.g. bradycardia).27
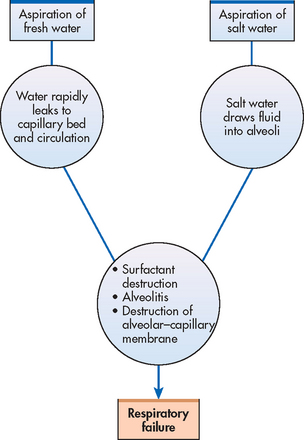
Death from a submersion injury is caused by hypoxia secondary to aspiration and swallowing of fluid, usually water. Swallowed water may cause vomiting and additional aspiration. The majority of all drowning victims aspirate water into the pulmonary tree and develop pulmonary oedema.27 Victims who do not aspirate fluid develop intense bronchospasm and airway obstruction (formerly known as dry drowning). Regardless of what fluid is aspirated into the pulmonary tree, the ultimate result is pulmonary oedema. The osmotic gradient caused by aspirated fluid causes fluid imbalances in the body. Hypotonic fresh water is rapidly absorbed into the circulatory system through the alveoli. Figure 68-4 shows the pulmonary effects of saltwater and freshwater aspiration.
The body attempts to compensate for hypoxia by shunting blood to the lungs. This results in increased pulmonary pressures and deteriorating respiratory status. Larger volumes of blood are shunted through the alveoli. However, the blood is not adequately oxygenated, so hypoxaemia worsens. Anaerobic metabolism predominates, leading to lactic acidosis and death.
The assessment findings of a patient with a submersion injury are listed in Table 68-8. Aggressive resuscitation efforts and the mammalian diving reflex improve survival of drowning victims even after submersion in cold water for long periods of time.28 Cold water lowers the body’s metabolic rate and oxygen demand. The mammalian diving reflex causes apnoea, bradycardia and peripheral vasoconstriction, and further decreases metabolic rate. Blood flow is redistributed to the most vital organs (i.e. heart, lungs, brain). This may protect the brain from the effects of decreased oxygen. Resuscitation should continue until the core temperature is greater than 30°C.28
TABLE 68-8 Submersion injuries
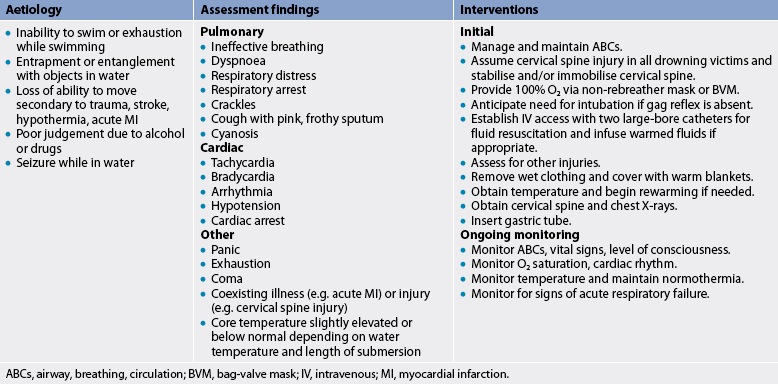
ABCs, airway, breathing, circulation; BVM, bag-valve mask; IV, intravenous; MI, myocardial infarction.
MULTIDISCIPLINARY CARE
Treatment of submersion injuries focuses on correcting hypoxia, acid–base imbalances and fluid imbalances, supporting basic physiological functions and rewarming when hypothermia is present. Initial evaluation involves assessment of the airway, cervical spine, breathing and circulation. Cervical spine precautions are necessary as the near drowning episode may be as a result of trauma (e.g. diving accident, surf injury). Other interventions are listed in Table 68-8.
Mechanical ventilation with positive end-expiratory pressure or continuous positive airway pressure may be used to improve gas exchange across the alveolar–capillary membrane when significant pulmonary oedema is present. Ventilation and oxygenation are the primary techniques used to treat acidosis. Mannitol or frusemide may be given to decrease free water and treat cerebral oedema. Hypothermia may be present and make circulatory assessment difficult.
Deterioration in neurological status suggests cerebral oedema, increased hypoxia or profound acidosis. Drowning victims may also have head injuries that cause prolonged alterations in level of consciousness. All victims of drowning should be observed in hospital for a minimum of 4–6 hours. Delayed pulmonary oedema (previously known as secondary drowning), pneumonia and cerebral oedema have been reported in patients who were essentially free of symptoms immediately after the drowning episode but later developed problems.
Teaching should focus on water safety and minimising the risks of drowning. Swimming pool gates should be locked, life jackets should be used on all watercraft, including inner tubes and rafts, and water survival skills (i.e. swimming lessons) should be a priority. The dangers of combining alcohol and drugs with swimming and other water sports should be emphasised.23
Bites and stings
The most common bite injuries seen in emergency are attributed to dogs, cats or humans. Other animal bites may be from other pets, such as horses, or native animals. In addition to the relatively minor animal bites, northern Australia also poses the risk of crocodile attack, and ocean sports/activities may lead to risk of shark attack. Crocodile and/or shark attacks can be very severe and are managed in the same way as a significant traumatic injury.
Dog bites usually occur on the extremities; however, facial bites are common in small children. Most victims know the dogs that bite them either through being the owner or a friend of the owner. Dog bites may involve significant tissue damage, with fatalities reported, usually in children or the elderly. Skull fractures with intracranial injury and death may occur in children under 2 years old. Disfiguring wounds of the face should be evaluated by a plastic surgeon. Dog bites have the potential for causing infection due to the bacterial flora within the dog’s mouth.
Cat bites cause deep puncture wounds that can involve tendons and joint capsules. Cat bites may result in infection because of the organism, Pasteurella, which is carried in the mouths of most healthy cats.21 Septic arthritis, osteomyelitis and tenosynovitis have been reported following cat bites.
Human bites also cause puncture wounds or lacerations and carry a high risk of infection from oral bacterial flora, most commonly Staphylococcus aureus, streptococci and hepatitis virus. Hands, fingers, ears, nose, vagina and penis are the most common sites of human bites and are frequently a result of violence or sexual activity. The human jaw has great crushing ability, causing laceration, puncture, crush injury, soft-tissue tearing and even amputation. More than 40 potential pathogens found in the human mouth account for an infection rate of approximately 50% in cases where victims do not seek medical intervention within 24 hours of injury. Boxer’s fracture, which is a fracture of the fifth metacarpal, is often associated with an open wound when the knuckles strike teeth.
MULTIDISCIPLINARY CARE
Initial treatment for animal and human bites includes cleaning with copious irrigation, debridement, tetanus prophylaxis and analgesia as needed. Prophylactic antibiotics are used for animal and human bites at risk of infection, such as wounds over joints, those more than 6–12 hours old, puncture wounds and bites of the hand or foot. Individuals at greatest risk of infection are infants, older adults, immunosuppressed patients, alcoholics, diabetics and people taking corticosteroids.
Puncture wounds are left open, whereas lacerations are loosely sutured if necessary. Wounds over joints are splinted. However, initial closure is reserved only for facial wounds. The patient requires IV antibiotic therapy when an infection is present. There is an increased incidence of cellulitis, osteomyelitis and septic arthritis in these patients.
Envenomation
Australia has numerous venomous creatures, which include snakes, arachnids, insects, marine animals and some mammals. Australian toxicologists have identified 38 species of terrestrial snakes, 23 sea snakes, 22 species of spiders, insects (e.g. ants, bees, wasps, scorpions and caterpillars), blue-ringed octopi, jellyfish, cone shells, stonefish, stingrays, starfish, anemones, frogs and toads, the platypus and echidna, all of which are equipped with venom.29 New Zealand, by comparison, has far fewer venomous creatures. There are insects such as bees and wasps, marine animals such as stingrays and cone shells, and spiders. New Zealand is essentially free from snakes; however, there have been incidents of snakes found in port areas transported inadvertently from Australia.30
Emergency presentations related to envenomation are predominantly spider bites, bee stings, wasp stings or snakebite. While accurate data on the incidence of snake and spider bites are difficult to find, snake and spider bites result in more than 5000 calls annually to Poison Information Centres in New Zealand and Australia.29–31 Although in many cases simple wound care and symptomatic management is all that is required, observation for symptoms of envenomation must be made, especially when identification of the snake or spider is uncertain. Even though antivenom exists for many of the more dangerous spider and snake species, its use is often restricted to those patients who present with systemic effects.31
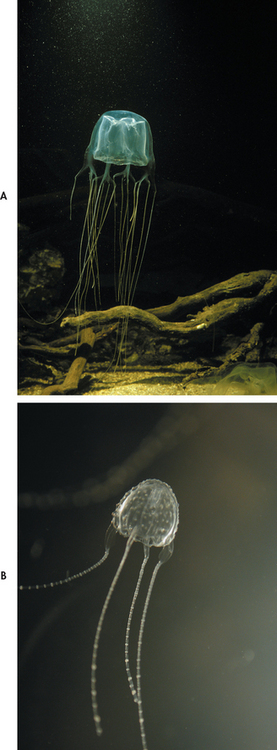
Envenomation by other species may also pose significant health risks. Bites from flying insects such as mosquitoes, bees and wasps are associated with both local and systemic effects. Deaths secondary to insect bites are more commonly associated with anaphylaxis rather than the toxicity of the venom.31,32 Marine animals frequently cause significant clinical effects requiring hospital treatment and/or admission. Most importantly, the sting of the box jellyfish, Chironex fleckeri, is known to cause severe systemic effects, including cardiorespiratory arrest.33,34
Many types of venom have multiple components (neurotoxins, myotoxins, haematological toxins, nephrotoxins and local toxins), which may present a complex clinical picture. Management is aimed at preventing the venom from reaching the systemic circulation, neutralising the venom, correcting venom-induced abnormalities and maintaining vital life functions.
ARACHNID ENVENOMATION
Of the thousands of species of spiders in Australia and New Zealand, three species in Australia are known to have caused death in humans. They are the Sydney funnel-web spider, the redback spider and the Australian bush tick.31 However, this does not mean that other spiders are not potentially lethal, and all spider bites should be treated with caution—for example, other spiders in Australia may produce local symptoms such as ulceration. New Zealand has only two spiders known to be poisonous: the redback and the Katipo spider.30,35
Spider bite classification has been simplified into three groups: big black spiders, redback spiders and all other spiders.36 Big black spiders include any large black-looking spider and bites from such spiders are treated as potential funnel-web spider bites for 4 hours after envenomation.36 Redback spider bites do not cause life-threatening effects but may cause systemic effects and significant pain at the injury site. Spiders in the ‘all other spiders’ group cause only minor effects. Therefore, if there is no evidence of big black spider or redback spider envenomation, treatment is not necessary.36
The funnel-web spider
The funnel-web spider, found throughout south-eastern Australia, is one of the most venomous spiders in the world. Hospital presentations are most common in New South Wales and more recently in south-east Queensland, and occasionally in Tasmania, the Australian Capital Territory, the Northern Territory and Victoria.32,37
There are approximately 35–40 species of the funnel-web spider with two genera: Atrax and Hadronyche. The Sydney funnel-web (Atrax robustus) is the only one to have definitely caused death. The male spiders are the main culprits as they roam in search of a mate (see Fig 68-5, A). The lethal component is believed to be confined to one component of the robustotoxin (atraxotoxin), which causes spontaneous release of neurotransmitters and inhibits neurologically mediated release.31,37,38
The funnel-web spider produces a painful bite; death has occurred within 15 minutes and up to 3 days. The first stage of envenomation by a funnel-web spider often presents as generalised piloerection, widespread muscle fasciculation (often starting at the face, tongue and intercostal muscles), tachycardia and severe hypertension leading to raised intracranial pressure. Within 30 minutes of envenomation the patient may present with severe muscle writhing, diaphoresis, salivation and coma. Several hours after the envenomation the patient may be found to be normotensive, as the muscle twitching, perspiration and salivation subside. However, in cases of severe envenomation, progressive hypotension, episodes of apnoea and pulmonary oedema may follow.
Management of funnel-web spider bite involves application of a pressure-immobilisation bandage (bandage over the bite site then up the entire limb with enough pressure to restrict lymph flow not blood flow). Bites to the face or torso are associated with a higher mortality rate due to the inability to apply a pressure-immobilising bandage and the close proximity to the central circulation. Funnel-web venom has been shown to inactivate with prolonged pressure immobilisation.31,37,38
Funnel-web antivenom is developed from rabbit serum and was first released in 1980. The antivenom works in bites by the Atrax and Hadronyche species.36 To treat these bites, 2 vials of antivenom are given and repeated every 15–30 minutes until symptoms have settled. There is the potential for allergic reaction and treatment with antihistamine may be required. Patients with funnel-web spider bites or unidentified big black spider bites without symptoms should always be treated as patients with funnel-web envemonation. They require a pressure immobilisation bandage and, ideally, 4 hours of observation. The bandage should be removed only if funnel-web antivenom is available.36
The redback spider
Latrodectus hasseltii is found in all states of Australia, is believed to have been introduced during colonisation and has since been introduced to New Zealand. It is a member of the widow family and as such enjoys a fearsome reputation, due mainly to the number of suspected bites reported annually. The venom contains a neurotoxin called α-latrotoxin, which causes depletion of either acetylcholine or catecholamines. The mechanism of death is uncertain but may be as a result of paralysis of the respiratory muscles. No deaths have occurred since 1955, although the antivenom was not developed until 1956. It is estimated that the redback is responsible for up to10,000 bites annually in Australia.39 While there are no precise statistics on envenomation, it is estimated that approximately 300 patients with bites require antivenom annually.31
Common features of envenomation are pain at the bite site, which increases with pressure to the site and eases with ice, and perspiration at the bite site, which may progress over the entire limb. Headache, nausea, vomiting, joint pain and abdominal pain are indicative of systemic envenomation.31
Management consists of administration of antivenom.36 The antivenom is developed from horse serum and may pose a risk of allergic reaction; however, there is a low incidence of reactions to redback antivenom. A single ampoule of antivenom is administered intramuscularly. Further doses may be required if symptoms persist; in some cases symptoms have re-presented weeks after the bite.40 Ice applied to the bite site can be helpful, although not always. It is important to note that pressure bandaging is not recommended for redback spider bites.36
Katipo spider
The Katipo spider (Latrodectus katipo) is native to New Zealand and is closely related to the redback spider (see Fig 68-5, B). Venom actions are similar in producing pain at the site, headache, malaise, abdominal cramps and fever. This spider is particularly rare and, therefore, bites are rare as well.35
Management includes application of ice to ease the pain. Antivenom is available and is indicated for symptomatic envenomation.30
The Australian bush tick
Ixodes holocyclus is found in dense bushland and rainforest regions of Australia. The toxin is a presynaptic neurotoxin, which is believed to be released in the saliva of the tick as it feeds. Initially, the person may complain of local skin irritation. If the tick is not removed within 4–6 days the person may then experience progressive ascending paralysis presenting as an ataxic gait followed by malaise and developing weakness, then dysarthria, dysphagia, respiratory failure and death.31,41 Paralysis tick envenomation resulting in severe muscle paralysis requires antivenom therapy.
Management is by removal of the tick, ensuring that the head of the tick is removed from the site. Tick removal does not always result in symptom resolution. Severe symptoms may persist for up to 48 hours after the tick(s) have been removed.
Antivenom is available if symptoms do not abate. The antivenom is made from dog serum. One ampoule is administered via slow IV infusion. Each vial contains 1000 units derived from canine immunoglobulin I (IgI). The crystalline powder must be reconstituted with 6.3 mL of sterile water prior to dilution (1:10) and given via IV infusion over 15–30 minutes. As with all antivenom administration, anaphylaxis may develop; therefore, emergency resuscitation equipment, including adrenaline, should be readily available.41
SNAKEBITE
Australia has 21 of the 23 most venomous snakes in the world (see Fig 68-6). New Zealand does not have any indigenous snakes; however, due to its close proximity to Australia and imports from Australia, snakes have been found there. New Zealand’s Ministry for Agriculture and Forestry provides a reporting service for snakes found in the country and this reporting service also requests notification of redback spider sightings.29,30

Figure 68-6 Three poisonous Australian snakes. A, King brown or mulga snake (Pseudechis australis). B, Common or eastern brown snake (Pseudonaja textilis). C, Death adder (Acanthophis antarcticus).
In Australia, approximately 3000 snakebites are seen each year, with 200–500 requiring antivenom. The severity of the envenomation is dependent on the amount of venom injected and the relative toxicity of the venom (dry bites may occur where no venom is injected). Only about 2 deaths per year are reported following snake bite. The majority of bites occur in the rural areas of Queensland, Western Australia, New South Wales and Victoria.29,42
The multiple components of snake venoms often lead to a complex clinical picture, including:
• neurological signs—ptosis, blurred vision, facial and pharyngeal paralysis, widespread voluntary muscle weakness and progressive paralysis
• haematological effects—coagulopathy, haematuria, prolonged bleeding from the bite site and from the venepuncture site, cerebral haemorrhage
• renal effects—myotoxins and/or nephrotoxins may result in renal failure.
Australian snakebites are often painless and the bite site may not be visible or may vary between a linear laceration, a pair of fang marks and multiple puncture wounds. Continued bleeding from the bite site may indicate envenomation; tender or painful lymph nodes are also an indication of envenomation as the venom is transported via the lymphatic system. Systemic symptoms include headache, nausea, vomiting, abdominal pain and often transient hypotension.43
Initial management is to apply a pressure-immobilising bandage to the bite site and to the entire limb to limit the volume of venom reaching the systemic circulation. The bite site should not be washed as it may be swabbed to identify the presence of venom and the species of snake.43,44 Snake identification should be performed by a herpetologist. Expert advice is available from the Poison Information Centres in Australia and New Zealand.
Medical management of snakebite depends on the severity of the envenomation. Although first aid measures remain a priority, in the event of a patient presenting with symptoms of envenomation, the first priority in the ED is stabilisation. The nurse should ensure that the airway is patent, respiration is adequate and cardiovascular collapse is prevented. Oxygen should be administered as necessary. If respiratory muscle paralysis is present, endotracheal intubation and mechanical ventilation may be required. If shock is evident the nurse should gain intravenous access and commence fluid resuscitation. Blood samples should be collected and sent for analysis of renal and liver function, coagulation and cross-match.
Where there are signs of systemic envenomation and if venom is detected at the bite site, antivenom should be administered via slow IV infusion. Several antivenoms are available; polyvalent antivenom provides enough antivenom to neutralise the average yield of venom for all of Australia’s dangerous snakes. This is a large dose and poses a significant risk of allergic or anaphylactic reaction. Monovalent antivenom specific to the snake species is a smaller volume dose than polyvalent antivenom. The minimum dose of antivenom is 1 vial, although this is higher for some antivenoms. Multiple bites or severe envenomation mandate higher doses of antivenom with the dose increasing by 1–3 vials.45 If an acute allergic response occurs or anaphylaxis develops, the nurse should administer intramuscular (IM) adrenaline (adults 0.5 mg, children 0.01 mg/kg), high-flow oxygen and IV fluids, and consider corticosteroids and antihistamines in severe cases.42 Venom detection kits identify 5 different snake groups and the appropriate monovalent antivenom to administer.
HYMENOPTERAN STINGS
Hymenopteran insects have a stinger attached to a sac of venom. The stinger is forced through the skin and the venom is injected. Bee and wasp stings are the most common presentations to hospital within this group. Most often, the local reaction is minor, albeit uncomfortable and self-limiting. Urticaria, wheals and erythema are common initial signs. Pain may be intense initially but generally quickly subsides. Occasionally bullous or haemorrhagic lesions appear in children or immunocompromised patients. Multiple stings or single stings to patients who have been previously sensitised may result in systemic reactions and allergy. IgE hypersensitivity has been reported following stings from ants; however, it has been more commonly related to wasps and bees and, over the years, bees have caused higher mortality than any other venomous creature in Australia or New Zealand.31,46
Initial management includes wound cleansing with soap and water. Ice packs are useful to relieve local pain and swelling. Symptoms of anaphylaxis include severe swelling in the pharynx and around the face (especially the lips and eyes), bronchospasm and hypotension. Emergency management includes maintenance of the airway, breathing and cardiac output. Supplemental oxygen is recommended. Nebulised β-adrenergic agonists, such as salbutamol, may be necessary to reverse bronchospasm. IV access should be obtained for fluid resuscitation and blood samples.
Adrenaline is the physiological antagonist to histamine and is the drug of choice. Adults should receive 0.3–0.5 mg IM and children 0.01 mg/kg. Antihistamines and corticosteroids may also be useful. Patients who have a history of anaphylaxis to insect bites should be educated about the risks of exposure and should carry appropriate emergency drugs, normally IM adrenaline and oral antihistamines. (See Ch 13 for a discussion about anaphylaxis.)
MARINE ANIMALS
Most marine animal envenomations do not result in hospital presentations. Bluebottle, jellyfish and sea anemone envenomations are usually managed by first aid measures. Stingray barbs generally result in traumatic injury as opposed to envenomation complications. The box jellyfish (Chironex fleckeri) and the Irukandji jellyfish (Carukia barnesi) (see Fig 68-7) pose more serious complications of envenomation.34
Bluebottle jellyfish
The bluebottle jellyfish (Physalia physalis) is a medium-sized creature often seen in swarms about the northern and eastern coasts of Australia. Skin contact with the nematocysts produces immediate pain and erythema around the contact area. Semicircular blanched wheals are common with surrounding erythema. Nematocysts are likely to adhere to the skin but can be removed by application of water or vinegar. Systemic toxicity is extremely unlikely, but intermittent, sometimes severe, muscle pain may be experienced. No antivenom is available or required.
Box jellyfish
The Australian box jellyfish (Chironex fleckeri) has been implicated in more than 70 fatal envenomations. Commonly found in tropical waters, this jellyfish is multi-tentacled with a head or bell up to 30–40 cm in diameter. These creatures are most often encountered close to shore in water less than 1 m deep. They are more common on the incoming tide when a mild breeze is present. Most stings occur during the late afternoon to early evening between October and June (stinger season). The majority of reported deaths are in children.33
The exact mechanism of action of box jellyfish venom remains unknown. Animal studies have found that sodium and calcium channels are disrupted due to alterations in membrane permeability affecting ion transport. Cardiac conduction and cardiac and skeletal muscles may be adversely affected. Hypertension may occur initially, followed by hypotension, cardiac arrhythmias and coronary hypoperfusion. Death can occur within minutes, which is thought to be secondary to direct cardiac toxicity.39,47
Symptoms may initially include only immediate pain in the area of nematocyst contact lasting up to 8 hours. Ice applied to the affected area quickly controls this pain. Large amounts of vinegar (acetic acid) applied to visible sting sites will inactivate undischarged sting cells.39 Few patients require systemic analgesia. If symptoms are severe or persistent, then a single dose of magnesium sulfate up to 10 mmol should be given as a slow IV injection. Antivenom may also be useful.
Initial management in life-threatening cases should include airway, breathing and circulation assessment. Oxygen should be administered for respiratory compromise. Deactivation and removal of the nematocysts is essential to stop further envenomation, and for this vinegar is the recommended treatment.47
If symptoms of severe envenomation (cardiopulmonary arrest or severe compromise) are present, then 20,000 units (1 vial) of antivenom should be administered intravenously. If symptoms persist, up to three doses may be given consecutively. In addition, magnesium sulfate (0.2 mmol/kg up to 10 mmol) should be given as an IV infusion over 5–15 minutes. Repeat doses of antivenom (three further vials) and magnesium sulfate may be considered if persistent cardiac arrest is present.
Irukandji jellyfish
The Irukandji jellyfish is smaller than the box jellyfish; however, its tentacles may reaCh 1 m in length. Typical signs and symptoms of Irukandji envenomation include abdominal pain, back pain, nausea, vomiting, chest tightness and leg cramps. Tachycardia and hypotension are prominent features and severe envenomation has led to pulmonary oedema.46,47 There is currently no antivenom available and management is based on inactivating the nematocysts and removing them. Vinegar may be applied to achieve this. Treatment of symptoms, particularly the control of hypertension and pain, is crucial.
Poisonings/toxicology
Toxicological emergencies may result from exposure to a poisonous substance via ingestion, inhalation or topical absorption. Toxic or poisonous substances range from illicit/recreational drugs to prescribed or over-the-counter therapeutic drugs, plants, food substances, chemicals, biological agents and radiological agents.
Toxicology exposure may be via accidental or intentional poisoning, but both require specific psychological support following the initial emergency management phase. Deliberate poisoning and accidental overdose/exposure pose significant challenges for ED staff because, in addition to the variety of clinical manifestations, the impact of the toxic substance may not be limited to the patient presenting. Consideration must also be given to the potential contamination of staff and/or other patients from the substance. It is therefore essential that ED staff are aware of the types of toxic substances and the methods of absorption.
Poisoning may occur across the spectrum of the population. In Australia, the most recent data indicate that there were 6813 hospital admissions caused by poisoning, including both pharmaceutical and other substances, in one year.48 These statistics do not include the numerous drug and alcohol-related presentations in EDs, so the actual number of poisoning presentations is considerably higher. The most common poisoning presentation in Australia is alcohol intoxication, followed by overdoses of benzodiazapines, antidepressants and paracetamol.39
Accidental overdose may occur due to a lack of information about the substance, ingesting the incorrect dosage or ingesting substances that interact adversely with other substances. Patients in the early stages of dementia may take larger doses than prescribed. Prescribed medications, which have an ideal therapeutic range, pose risks if not monitored carefully. Regular medications such as digoxin, lithium and warfarin may lead to a toxicology presentation.
Children generally present with accidental exposure through either receiving an incorrect dose or being inquisitive; however, in the adolescent age group deliberate overdoses are becoming more common.49 Approximately 50 Australian children present each week with toxicology-related presentations: 7 out of 10 of these relate to ingestion of unprescribed medications. In New Zealand, more than 500 hospital admissions each year are caused by poisoning in the 0–14-year-old age group (approximately 10 per week); these included both prescription and non-prescription medications.50 It is estimated that more than 60 per cent of poisonings occur in males.
The severity of a poisoning depends on the type, concentration and route of exposure to the toxin.51 Toxins can affect every tissue of the body, so symptoms may be wide-ranging and occur across any body system. Common poisons and their manifestations are reviewed in Table 68-9. Other poisonings related to the use of illegal drugs, such as amphetamines, narcotics and hallucinogens, are discussed in Chapter 10. Poisoning may also be due to toxic plants or contaminated foods. (Food poisoning is discussed in Ch 41.)
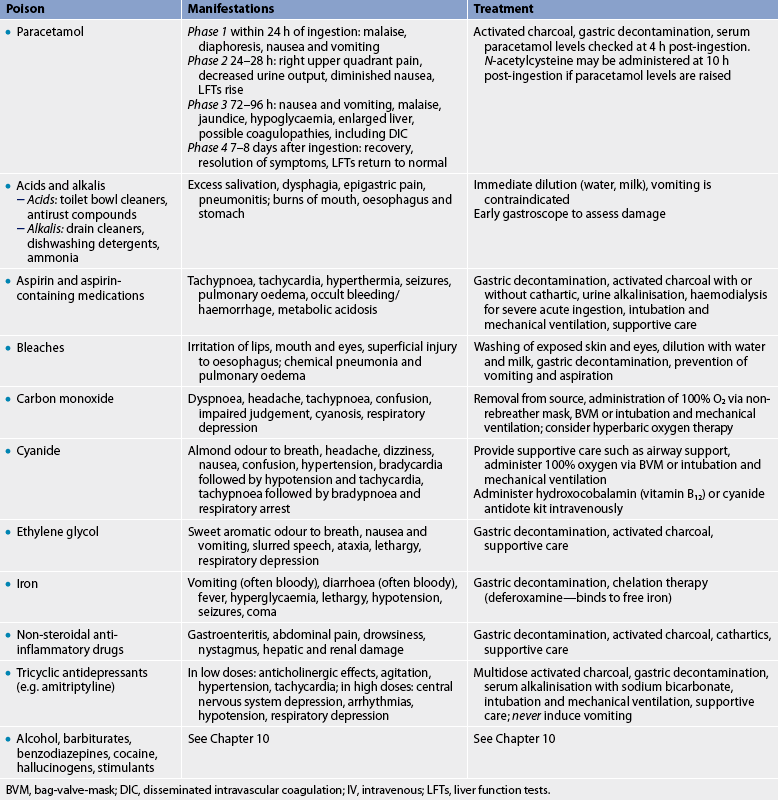
BVM, bag-valve-mask; DIC, disseminated intravascular coagulation; IV, intravenous; LFTs, liver function tests.
ASSESSMENT
Assessment of the patient must include monitoring of all body systems. Details for the assessment of specific body systems can be found in the relevant chapters. To ensure a comprehensive assessment is ongoing, the following should be assessed in all patients with poisoning:
• risk assessment: this is a priority when managing the poisoned patient—it aids in determining the likely course and potential clinical complications associated with poisoning and can be determined by using the ABCDE mnemonic:
• regular assessment of vital signs: the time interval is determined by the severity of the presentation and the potential risks posed by the toxic substance
• cardiac monitoring, until it is established that there is no further risk of cardiac complications; an electrocardiogram should be performed to determine any cardiac conduction abnormalities
• haemodynamic monitoring, including fluid input and urine output
• general physical assessment for signs such as diaphoresis, rashes or injuries associated with exposure to a substance, such as burns
• psychological assessment to determine the ongoing risk of self-harm or risks that may develop for psychotropic toxins.
INVESTIGATIONS
The basis for clinical investigation of a person presenting with a poisoning is to:
• identify the toxic substance (including the paracetamol level, where relevant)39
• where possible and relevant, elicit the blood plasma level of the toxic substance
• determine, if any, the effects of the toxic substance through clinical assessment and pathology investigations
• determine the need for antidote administration where there is an antidote available
MANAGEMENT
The specific management of poisoning involves decreasing absorption of the toxic substance, enhancing its elimination, administrating a toxin antidote if available and treating the specific signs and symptoms as they present. The Australian Poisons Information Network has various centres in Australia and the New Zealand National Poisons Centre is located in Dunedin. Both networks are available 24 hours a day and should be consulted for the most current treatment protocols for specific poisons (see the Resources on p 1978).
The overall goal in the management of a poisoned patient is supportive care to maintain vital functions while the poison is being metabolised or eliminated.39,51 Decontamination is the process of enhancing the elimination of poison through the use of dilution/washing, gastric decontamination (activated charcoal or whole bowel irrigation), haemodialysis, haemoperfusion, urine alkalinisation, chelating agents or antidotes. The method of decontamination is dependent on the method of exposure, the type of substance and the time of exposure.
The current recommendations for the decontamination of poisonings are as follows:
1. Skin irrigation—for topical exposure to a substance. Skin decontamination involves removal of toxins from the skin using copious amounts of water or saline. With the exception of mustard gas (water mixes with mustard gas and releases chlorine gas), most toxins can be safely removed with water or saline. As a general rule, dry substances should be brushed from the skin and clothing before water is used. Powdered lime should not be removed with water; it should just be brushed off. Radioactive material present on clothing or skin should be washed with water. Personal protective equipment (e.g. gloves, gowns, goggles and masks) should be worn for decontamination to prevent secondary exposure. Respirators are required for suspected nerve agents. Those specially trained in hazardous material decontamination may undertake decontamination procedures for incidences of major chemical or biological contamination. If the decontamination process is performed at the hospital, consideration should be given for the wastewater run-off during the procedure, and local policies regarding containment and disposal of contaminated clothing and wastewater must be adhered to. Decontamination takes priority over all interventions except basic life support.53
2. Eye irrigation—for ocular decontamination. This uses the principle of flushing and diluting the contaminant with saline (0.9%) or Hartmann’s solution. The eye should be reviewed after 1 L of solution has been applied: the nurse should wait 5 minutes and then check pH. The acceptable pH range is 6.5–8.5.54
3. Gastric decontamination—for ingested substances. Gastric decontamination is one of the most effective interventions for the management of ingested poisonings. Generally, substances ingested more than 1 hour prior to presentation will have passed out of the stomach and will render many methods of gastric decontamination of little value. Therefore, gastrointestinal decontamination is reserved for patients where risk assessment suggests severe toxicity and where antidote or supportive care will not ensure a satisfactory patient outcome.39 The two main types of gastric contamination are:
Activated charcoal
Activated charcoal is manufactured by the pyrolysis (thermochemical decomposition) of wood pulp followed by oxidation at 600–900°C. Activated charcoal is prepared in a way that dramatically increases its surface area by the production of an extensive network of internal pores. The surface area of charcoal products varies between 900 and 1200 m2/g. Administration of activated charcoal is either orally or via a gastric tube. Toxins adhere to the charcoal and are excreted through the GI tract rather than absorbed into the portal circulation. The dose of 50 g for adults or 1 g/kg for children is given as a single dose.39
Activated charcoal can absorb a number of poisons from the GI tract but it does not absorb ethanol, alkalis, iron, boric acid, lithium, methanol or cyanide. For some toxins (e.g. phenobarbitone) repeated doses of charcoal may be required. Contraindications to the administration of charcoal include decreased level of consciousness, incomplete ingestion of a substance poorly absorbed by charcoal and ingestion of a subtoxic dose of drug.39 Charcoal is not recommended for a number of drugs and chemicals because adsorption does not occur, is minimal or is contraindicated due to the risk of aspiration. These substances include alcohol, corrosive substances, hydrocarbons, and metals and their salts (e.g. lead, iron, potassium). In addition to these contraindications, the ability of charcoal to absorb a substance is dependent on the time of ingestion. The effectiveness of charcoal is decreased significantly after 1 hour post-ingestion due to gastric emptying.
Activated charcoal may be dispensed in a powdered form to be mixed with water or in a pre-packed preparation of charcoal and water or charcoal and sorbitol. Sorbitol is an osmotic cathartic that acts by increasing the amount of fluid present in the gut. Sorbitol does not increase the efficacy of charcoal, but it does increase the risk of vomiting and consequent aspiration. Aspiration of sorbitol precipitates a similar fluid movement in the lungs, with potentially serious consequences. The addition of a cathartic does not offer any additional benefit and therefore is not recommended.
Adult patients are generally able to drink charcoal from a cup, and it is more palatable when the bag containing the charcoal is warmed in hot water, making the ‘gritty’ feeling often complained about less noticeable and its consistency less thick. Children may pose some challenges for the oral administration of charcoal as the appearance and gritty texture may upset some, despite the absence of any taste. Experience drawn from EDs suggests that a number of strategies can minimise the psychological trauma to a child and enable easier administration. Children respond to a confident and calm approach. The charcoal can be placed in an opaque cup or glass with a lid on it; a straw is also useful. Young children enjoy discovery and are quickly able to take the initiative to discover what they can do for themselves. Fantasy and make-believe are an integral part of a child’s daily activities, which may contribute to the overwhelming interest in everything that looks edible. This aspect of growth and development can be harnessed to the nurse’s benefit. Allowing the child to choose the colour of their cup and straw often adds an element of play to the task, while asking them to assist in preparing the charcoal may increase the likelihood of cooperation and successful administration.
In patients with a compromised airway, central nervous system depression or potential seizure, endotracheal intubation is the most effective intervention for maintaining a secure airway prior to the administration of charcoal.
Whole bowel irrigation
Whole bowel irrigation is controversial and involves administration of large volumes of a non-absorbable bowel evacuant solution. The solution is administered every 4–6 hours until stools are clear. This process can be effective for swallowed objects such as cocaine-filled balloons or condoms or substances such as iron tablets that are not absorbed by charcoal. Complications include nausea, vomiting and abdominal bloating, metabolic acidosis and pulmonary aspiration. There is a high risk of electrolyte imbalance due to fluid and electrolyte losses with this procedure.39 Intravenous maintenance of fluids may be required to support hydration. The process is time-consuming and requires a nurse to stay with the patient.
Haemodialysis and haemoperfusion
Haemodialysis and haemoperfusion are invasive techniques that simply remove the toxic substance and metabolites from the circulation and correct electrolyte disturbances. They are effective in cases of severe toxicity secondary to intoxication from alcohol, lithium and phenobarbitone.39 Patients undergoing these procedures often require intensive care monitoring. Haemoperfusion is a similar process to haemodialysis but utilises the adsorptive properties of charcoal to bind drugs or toxins as the patient’s blood is passed through a charcoal membrane or filter; it is more effective than simple dialysis.
Antidote administration
A limited number of true antidotes are available, and many of these agents are themselves toxic.39 In addition, their use in cases of acute-on-chronic overdose requires caution. Patients who have developed dependence on drugs such as opiates or benzodiazepines are much more likely to develop significant withdrawal with the administration of an antidote. The administration of either flumazenil or naloxone (as appropriate) should be limited to the dose required to maintain respiration and not to fully reversing the effects of the respective drug.
The role of, choice of method of and indications for gastric decontamination remain controversial, although there are patients who are likely to benefit from this form of treatment. Innovations for the treatment of poisonings, such as digoxin-Fab fragments, currently used for the treatment of digoxin poisoning, must be available at the appropriate time to be effective.55 It is important, however, to remember that antidotes themselves are drugs and frequently cause adverse effects. Administration is based on risk–benefit analysis. It is recommended that antidotes be used only under strict clinical supervision, in the correct dose, with the correct route and with appropriate monitoring.39,56
PSYCHOLOGICAL SUPPORT
Education and support to avoid any subsequent toxic emergencies focuses on how the poisoning occurred and safety. A mental health professional should assess patients whose poisoning is the result of a suicide attempt. Patients who have a history of substance abuse may be referred for alcohol or drug detoxification if they consent. Patients who have suffered accidental poisoning of prescribed medications require pharmacological education and, in some cases, may benefit from the introduction of pre-packaged medication to reduce the risk of confusion with medication doses.
Major incident and disaster preparedness
A major incident is an incident that involves or has the potential to involve a large number of casualties and can be adequately managed by available resources, but requires a significant coordinated response. The most recognised recent global disasters include the destruction of the World Trade Center by hijacked aeroplanes on 11 September 2001, the 2004 Boxing Day tsunami and the devastating tsunami in Japan in March 2011. Disasters have also occurred closer to home: Australia experienced the Victorian bushfires in February 2009 and the Queensland and Victorian floods in January 2011, while New Zealand faced two earthquakes in Christchurch and the Pike River Mine disaster in 2010. New Zealand was also heavily involved in the response to the Samoan tsunami in 2009.
As a result of the first Bali bombing in 2002, which tested the coordination of the disaster response in Australia and New Zealand, emergency response and management in both countries have been refined. In New Zealand, the management of major incidents and disasters is coordinated via the New Zealand Civil Defence Emergency Management (CDEM) Strategy. The National Crisis Management Centre (NCMC) facilitates crisis management arrangements, links the various agencies and ensures that there are sufficient resources to deal with any type of event or crisis. The CDEM Strategy contains four goals: (1) increasing community awareness, understanding, preparedness and participation in civil defence emergency management; (2) reducing the risks from hazards to New Zealand; (3) enhancing New Zealand’s capability to manage civil defence emergencies; and (4) enhancing New Zealand’s capability to recover from civil defence emergencies.57 Disaster management is governed by the Civil Defence Emergency Management Act 2002.
In Australia, major incidents and disasters are managed under the National Health Emergency Management (NHEM) Plan. Both the Commonwealth and state agencies are responsible for coordinating responses to major incidents, emergencies and/or disasters. These agencies include Emergency Management Australia (EMA), state emergency management committees, emergency services (e.g. police, fire brigade, ambulance), State Emergency Services (SES), the Red Cross and Defence authorities. The roles and responsibilities for these agencies are legislated by the Commonwealth and the states. The EMA is Australia’s leading agency in the coordination of disaster management and is responsible for the development of several Australian government disaster response plans assisting with disaster response both nationally and abroad.58
The terms emergency and disaster may be used interchangeably depending on the country and local terminology. Disaster, as defined in the Community Welfare Act 1987 (Australia), is an occurrence, whether or not due to natural causes, that causes loss of life, injury, distress or danger to people, or loss of, or damage to, property. An emergency/disaster is an event that is actual or imminent (e.g. fire, flood, storm, earthquake, explosion, accident, epidemic or war-like action) that:
• endangers, or threatens to endanger, the safety or health of people in the state or territory, or
• destroys or damages, or threatens to destroy or damage, any property in the state, being an emergency that requires a significant and coordinated response.
In New Zealand, where both disasters and emergencies are referred to as civil defence emergencies, an emergency/disaster is defined as a situation that:
(a) is the result of any happening, whether natural or otherwise, including, without limitation, any explosion, earthquake, eruption, tsunami, land movement, flood, storm, tornado, cyclone, serious fire, leakage or spillage of any dangerous gas or substance, technological failure, infestation, plague, epidemic, failure of or disruption to an emergency service or a lifeline utility, or actual or imminent attack or warlike act; and
(b) causes or may cause loss of life or injury or illness or distress or in any way endangers the safety of the public or property in New Zealand or any part of New Zealand; and
(c) cannot be dealt with by emergency services, or otherwise requires a significant and coordinated response under the Act. [CDEM Act 2002 section 4]57
EMERGENCY SERVICES
Staff in the ED need to be prepared to deal with unexpected and severe injuries occurring as a result of disasters and terrorist attacks. Their own communities may have been affected and staff themselves have to confront uncertainty and fear while providing care for those who have been injured. For example, in New Zealand the severity of the Christchurch earthquake meant that staff working in EDs were looking after victims while at the same time being unsure whether their own families and homes were safe (see Figs 68-8 and 68-9). Similarly, in Australia the devastation of the Victorian fires meant that ED staff were caring for injured members of their own communities while trying to deal with the personal effects of the catastrophe. Although Australia and New Zealand have so far avoided a terrorist attack within their borders, the Bali terrorist attacks in 2002 and 2004 affected many local hospitals when victims were flown back to Australia for treatment.

Figure 68-9 Severe crush injuries may result from the damage caused by an earthquake, such as the recent Christchurch earthquake.
Source: Photolibrary.
Staff in EDs, in common with the rest of the community, suffer from shock and disbelief when disasters such as these occur but, because they are on the front line of clinical management, it is important that they still practise the fundamental principles of assessment and management. Staff efforts are often focused on the management of complex patient injuries following such incidents (see Fig 68-10). Triaging of patients based on the seriousness and extent of injuries is crucial (see Fig 68-11). Injuries of patients involved in disasters are varied but may involve extensive penetrating injuries when bomb blasts occur (see Fig 68-12). Materials used in homemade bombs present unusual injuries requiring inventive and sometimes unusual treatment. For instance, ball bearings used in terrorist bomb attacks scatter widely and cause extensive, serious injuries (see Fig 68-13).

Figure 68-10 Emergency management of victims from the Bali terrorist attack.
Source: Used with permission. Royal Darwin Hospital, Clinical Photo Library.

Figure 68-11 Patient injuries from the Bali terrorist attack. Note triage assessment.
Source: Used with permission. Royal Darwin Hospital, Clinical Photo Library.
Chemical, biological and radiation hazards
Chemical, biological and radiation (CBR) hazards may result from industrial accidents, epidemics or agricultural pesticide exposure. In addition to accidental exposure, the world currently faces the threat of terrorism. Terrorism involves overt actions, such as the dispensing of disease pathogens or other agents (e.g. chemical, biological and/or radiological) as weapons for the express purpose of causing harm. Prompt recognition and identification of potential health hazards is essential in the preparedness of healthcare professionals.53
Chemicals agents that pose major health risks are categorised according to their target organ or effect (see Table 68-10). Agents include:
• nerve agents (e.g. organophosphates)
• blister agents (e.g. mustard gas, lewisite and phosgene oxime)
Even though these chemicals may be used industrially, they also have the potential to be used in terrorist acts.
Radiation exposure may occur through occupational exposure, diagnostic procedures such as X-ray and CT scans or nuclear medicine, treatments such as those used in radiation oncology or via radioactive materials used in war or terrorist actions. Exposure to radiation may or may not include skin contamination with radioactive material. If external radioactive contaminants are present, decontamination procedures must be initiated. Acute radiation syndrome develops after a substantial exposure to radiation and follows a predictable pattern (see Table 68-11).53
TABLE 68-11 Terrorism with ionising radiation: general guidance pocket guide
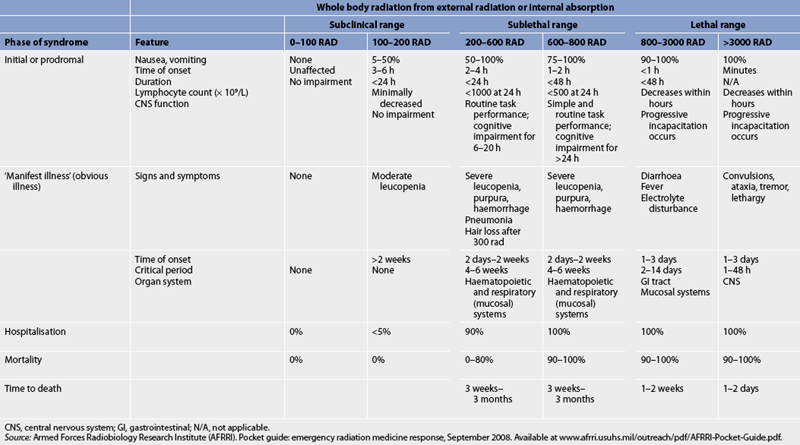
CNS, central nervous system; Gl, gastrointestinal; N/A, not applicable.
Source: Armed Forces Radiobiology Research Institute (AFRRI). Pocket guide: emergency radiation medicine response, September 2008. Available at www.afrri.usuhs.mil/outreach/pdf/AFRRI-Pocket-Guide.pdf.
Exposure to CBR agents requires specific decontamination to avoid the risk of secondary contamination of staff and/or other patients within the ED and hospital. Planning for the response and recovery from a CBR incident is considered a major focus in emergency management planning, not only due to the threat of terrorist acts but also due to the risks of exposure in general industry and within hospitals.
CASE STUDY
Patient profile
A 20-year-old female trauma patient is brought to the emergency department in an ambulance. She was the driver in a motor vehicle collision and was not wearing a seat belt. Two children in the car were pronounced dead at the scene. The paramedics stated that there was significant damage to the car on the driver’s side.
Objective data
CRITICAL THINKING QUESTIONS
1. What life-threatening injury does this patient probably have?
2. What is the priority of care?
3. What interventions are needed immediately?
4. What other interventions should the nurse consider?
5. Several family members have arrived in the emergency department, including a woman who states her child was in the car (one of the children who died). The second child who died was the patient’s child. How should the nurse approach the family?
6. Based on assessment data presented, write one or more nursing diagnoses. Are there any collaborative problems?
1. An elderly man arrives at the emergency department. He is tachypnoeic and disoriented, and his skin is hot and dry. The priority for treatment at this point is to:
2. A patient has presented with a core temperature of 32.2°C. The most appropriate rewarming technique would be:
3. The recommended management for reducing the absorption of many ingested poisons is:
4. What is the recommended immediate management for a funnel-web spider bite?
5. In the absence of significant clinical signs and symptoms, what information would lead nursing and medical staff to suspect the potential for underlying injury and the need for trauma team management?
6. A chemical spill has occurred in a nearby industrial site. The first responders report that approximately 20 victims need to be transported to the emergency department after decontamination at the site. This is an example of:
7. Which of the following biological agents has no effective treatment?
1 Australian Bureau of Statistics (ABS). Australian demographic trends, 2010. Canberra: ABS; 2010. Available at www.abs.gov.au/ausstats/abs@.nsf/mf/3101.0 accessed 22 October 2010.
2 Trewin D. Australian social trends, 2006. Canberra: ABS, 2006.
3 Australian Bureau of Statistics (ABS). Australian migration statistics, 2008–2009. Canberra: ABS, 2010.
4 Department of Foreign Affairs and Trade. New Zealand country brief. Available at www.dfat.gov.au/geo/new_zealand/nz_country_brief.html, February 2007. accessed December 2010.
5 Australasian College of Emergency Medicine. Guidelines on the implementation of the Australasian Triage Scale in emergency departments, 2000. Still current. Available at www.acem.org.au/media/policies_and_guidelines/G24_Implementation_ATS.pdf. accessed December 2010.
6 The National Education Framework for Emergency Triage Working Party. Department of Health and Ageing: emergency department triage education kit. Canberra: Commonwealth Government, 2009.
7 Jacobs B, Hoyt KS, eds. Trauma nursing core course: provider manual, 6th edn., Des Plaines, IL: Emergency Nurses Association, 2007.
8 Ollerton JE. Adult trauma clinical practice guidelines, emergency airway management in the trauma patient. Sydney: Institute of Trauma and Injury Management, 2007.
9 Armstrong B, Reid C, Heath P, Howard S, Kitching J, et al. Rapid sequence induction anaesthesia: a guide for nurses in the emergency department. Int Emerg Nurs. 2009;17:161–168.
10 American College of Surgeons Committee in Trauma. Advanced trauma life support for doctors: ATLC student course manual, 8th edn. Chicago: American College of Surgeons, 2008.
11 Holzhauser K, Finucane J, De Vries SM. Family presence during resuscitation: a randomised controlled trial of the impact of family presence. Australas Emerg Nurs J. 2006;8(4):139–147.
12 Holzhauser K, Finucane J. Part B: a survey of staff attitudes immediately post-resuscitation to family presence during resuscitation. Australas Emerg Nurs J. 2008;11:114–122.
13 Hodge AN, Marshall AP. Family presence during resuscitation and invasive procedures. Collegian. 2009;16:101–118.
14 Macintyre PE, Schug SA, Scott DA, Visser EJ, Walker SM. APM:SE Working Group of the Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine. Acute pain management: scientific evidence, 3rd edn. Melbourne: ANZCA, 2010.
15 Victorian State Trauma System. Metropolitan and regional paediatric and adult major trauma triage guidelines. Available at www.health.vic.gov.au/trauma/publications/triageguidelines.pdf, Updated October 2010. accessed December 2010.
16 Fraser K. Domestic violence and women’s physical health. Sydney: Australian Domestic and Family Violence Clearinghouse; 2003. Available at www.austdvclearinghouse.unsw.edu.au/PDFfiles/physical_health.pdf accessed December 2010.
17 Rodrigue JR, Cornell DL, Howard RJ. Organ donation decision: comparison of donor and nondonor families. Am J Transplant. 2006;6:190–198.
18 Hermstad E, Adams B. Traumatic brain injury complicated by environmental hyperthermia. J Emerg Trauma Shock. 2010;3(1):66–69.
19 Auerback PS. Wilderness medicine, 5th edn. Philadelphia: Elsevier, 2007.
20 Winkenwerder W, Sawka M. Disorders due to heat and cold. In Goldman C, Ausiello D, eds.: Cecil medicine, 23rd edn., Philadelphia: Elsevier, 2008.
21 Ferri FF. Practical guide to the care of the medical patient, 8th edn. St Louis: Mosby, 2010.
22 Edelstein JA, Li J, Silverberg MA, Decker W. Hypothermia: treatment & medication. eMedicine from WedMD. Available at http://emedicine.medscape.com/article/770542-treatment, Updated October 2010. accessed 26 January 2011.
23 Royal Life Saving Society. The national drowning report. Available at www.royallifesaving.com.au//resources/documents/2010_Drowning_Report.pdf, 2010. accessed December 2010.
24 Water Safety New Zealand. Provisional drowning report. Available at www.watersafety.org.nz/assets/pdfs/Drowning-Report-2009.pdf, 2009. accessed December 2010.
25 Final Recommendations of the World Congress on Drowning: Amsterdam. Available at www.cslsa.org/events/ArchiveAttachments/Spr03Minutes/AttachmentG2.pdf, 26–28 June 2002. accessed December 2010.
26 Australian Resuscitation Council. Guideline 8.7: resuscitation of the drowning victim. Melbourne: Australian Resuscitation Council, 2005. Still current. Available at www.resus.org.au/policy/guidelines/section_8/8_7_feb05.pdf accessed December 2010.
27 Verive MJ. Near drowning. eMedicine from WedMD. Available at hhtp://emedicine.medscape.com/article/908677-overview, Updated April 2009. accessed January 2011.
28 Headdon WG, Wilson PW, Dalton HR. Case report: the management of accidental hypothermia. Br Med J. 2009;338:2085.
29 Thompson C, Loadsman J. Envenomation in Australia. Available at www.anaes.med.usyd.edu.au/venom/envenomation.html. accessed December 2010.
30 Slaughter RJ, Michael D, Beasley G, Lambie BS, Schep LJ. New Zealand’s venomous creatures. J NZ Med Assoc. 2009;122:1290.
31 Thompson C, Loadsman J. Australian spider and insect bites. Available at www.anaes.med.usyd.edu.au/venom/spiders.html. accessed December 2010.
32 Isbister GK, White J. Clinical consequences of spider bites: recent advances in our understanding. Toxicon. 2004;43:477–492. (Seminal work)
33 Isbister GK. Managing injuries by venomous sea creatures in Australia. Aust Prescriber. 2007;30(5):117–121.
34 Currie BJ, Jacups SP. Prospective study of Chironex fleckeri and other box jellyfish stings in the Top End of Australia’s Northern Territory. Med J Aust. 2005;183:631–636. (Seminal work)
35 Adams S. Bites and stings: spiders. J Accident Med Pract Assoc. 2006;3:1–7.
36 Isbister GK. Spider bite: a current approach to management. Aust Prescriber. 2006;29:156–158.
37 Isbister G, Gray MR, Balit CR, et al. Funnel-web spider bite: a systemic review of recorded clinical cases. Med J Aust. 2005;182:407–411.
38 Brown SGA. Spider envenomations, funnel web. Available at www.emedicine.com/emerg/topic548.htm. accessed December 2010.
39 Murray L, Daly F, Little M, Cadogan M. Toxicology handbook. Sydney: Elsevier, 2011.
40 Commonwealth Serum Laboratory. CSL antivenom handbook. Red back spider antivenom. Available at www.wch.sa.gov.au/paedm/clintox/cslavh_antivenom_redback.html. accessed December 2010.
41 Commonwealth Serum Laboratory. CSL antivenom handbook. Paralysis tick antivenom. Available at www.toxinology.com/generic_static_files/cslavh_antivenom_tick.html. accessed December 2010.
42 Better Health Victoria. Bites and stings first aid. Available at www.betterhealth.vic.gov.au/bhcv2/bhcarticles.nsf/pages/Bites_and_stings_first_aid, Updated November 2009. accessed January 2011.
43 Thompson C, Loadsman J. Australian snake bites. Available at www.usyd.edu.au/anaes/venom/snakebite.html. accessed December 2010.
44 Australian Resuscitation Council (ARC). Envenomation: pressure immobilisation technique. Revised policy statement no. 8.9.1. Melbourne: ARC, 2005.
45 NSW Health Statewide Services Branch. Snakebite and spiderbite clinical management guidelines, 2007. North Sydney: NSW Department of Health, 2007.
46 Tiballs J. Australian venomous jellyfish envenomation syndromes, toxins and therapy. Toxicon. 2006;48:830–859.
47 Thompson C, Loadsman J. Australian marine envenomations. Available at www.usyd.edu.au/anaes/venom/marine_enven.html. accessed December 2010.
48 Australian Institute of Health & Welfare (AIHW). Australia’s health, 2010. Australia’s Health Series no. 12. Canberra: AIHW, 2010.
49 Kendrick D, Smith S, Sutton A, Watson MC, Coupland C, Mulvaney C, Mason-Jones A. The effect of education and safety equipment on poisoning prevention practices and poisoning: systematic review, meta-analysis and meta-regression. Arch Dis Children. 2008;93:599–608.
50 Alatini M. Analysis of unintentional child injury data in New Zealand: mortality 2001–2005 and morbidity 2003–2007. Auckland: Safekids New Zealand; 2009. Available at www.safekids.org.nz/Downloads/Research/Safekids%20Analysis%20VLR_2.pdf accessed January 20011.
51 Gavaghan C. Overdose and poisoning. Available at http://216.55.99.51/clinical/emergency/overdose.html. accessed December 2010.
52 Murray L. General principles in the management of drug overdoses. In Cameron P, Jelinek G, Kelly A, et al, eds.: Textbook of adult emergency medicine, 2nd edn., Edinburgh: Churchill Livingstone, 2004.
53 Koop D, Ward M. Major incident preparedness management. In: Curtis K, Ramsden C, Friendship J, eds. Emergency and trauma nursing. Sydney: Elsevier, 2007.
54 Sehu W, Higgons R. Eye emergency manual: an illustrated guide, 2nd edn. North Sydney: NSW Department of Health, 2009.
55 Dart RC, Borrow SW, Caravati EM, et al. Expert consensus guidelines for stocking of antidotes in hospitals that provide emergency care. Ann Emerg Med. 2009;54:386–394.
56 Cooper GM, Le Couteur DG, Richardson D, Buckley NA. A randomised clinical trial of activated charcoal for the routine management of oral drug overdose. QJ Med. 2005;98:655–660.
57 Ministry of Civil Defence and Emergency Management. National Civil Defence and Emergency Management Strategy, 2007. Wellington: Department of Internal Affairs; 2008. Available at www.civildefence.govt.nz accessed January 2011.
58 Smith E. National disaster preparedness in Australia: before and after 9/11, J Emerg Prim Health Care. 2006;4:3. Available at www.jephc.com/uploads/990195.pdf accessed January 2011.
Australasian College for Emergency Medicine. www.acem.org.au
Australian College of Critical Care Nurses. www.acccn.com.au
College of Emergency Nursing Australasia. www.cena.org.au
College of Emergency Nurses, New Zealand. www.cennz.co.nz
Donate West (Western Australia). www.donatewest.health.wa.gov.au
Emergency Management Australia. www.ema.gov.au
Ministry of Civil Defence and Emergency (New Zealand). www.civildefence.govt.nz
New Zealand National Poisons Centre. poisons.co.nz
NSW Poisons Information Centre. www.chw.edu.au/poisons/
Organ Donor Register (Australia). http://australia.gov.au/service/organ-donor-register
Organ Donation New Zealand. www.donor.co.nz/donor/about/odnz.php
Queensland Poisons Information Centre. www.health.qld.gov.au/PoisonsInformationCentre/
Victorian Poisons Information Centre. www.austin.org.au/poisons
Western Australian Poisons Information Centre. www.scgh.health.wa.gov.au/Clinicians/Services/PoisonInformationCentre.html