Cancer of unknown primary site (CUPS) is defined as follows: biopsy-proven malignancy; primary site unapparent after history, physical exam, chest x-ray, abdominal and pelvic CT, complete blood count, chemistry survey, mammography (women), β-human chorionic gonadotropin (hCG) levels (men), α-fetoprotein (AFP) levels (men), and prostate-specific antigen (PSA) levels (men); and histologic evaluation not consistent with a primary tumor at the biopsy site. CUPS incidence is declining, probably because of better pathology diagnostic criteria; it accounts for about 3% of all cancers today, down from 10–15% 15 years ago. Most pts are over age 60. The tumors are often aneuploid. Cell lines derived from such tumors frequently have abnormalities in chromosome 1.
Pts may present with fatigue, weight loss, pain, bleeding, abdominal swelling, subcutaneous masses, and lymphadenopathy. Once metastatic malignancy is confirmed, diagnostic efforts should be confined to evaluating the presence of potentially curable tumors, such as lymphoma, Hodgkin’s disease, germ cell tumor, ovarian cancer, head and neck cancer, and primitive neuroectodermal tumor, or tumors for which therapy may be of significant palliative value such as breast cancer or prostate cancer. In general, efforts to evaluate the presence of these tumor types depend more on the pathologist than on expensive clinical diagnostic testing. Localizing symptoms, a history of carcinogen exposure, or a history of fulguration of skin lesion may direct some clinical testing; however, the careful light microscopic, ultrastructural, immunologic, karyotypic, and molecular biologic examination of adequate volumes of tumor tissue is the most important feature of the diagnostic workup in the absence of suspicious findings on history and physical exam (Table 82-1).
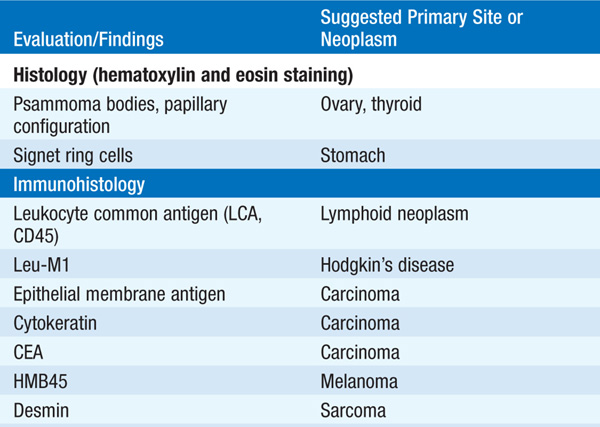
TABLE 82-1 POSSIBLE PATHOLOGIC EVALUATION OF BIOPSY SPECIMENS FROM PATIENTS WITH METASTATIC CANCER OF UNKNOWN PRIMARY SITE
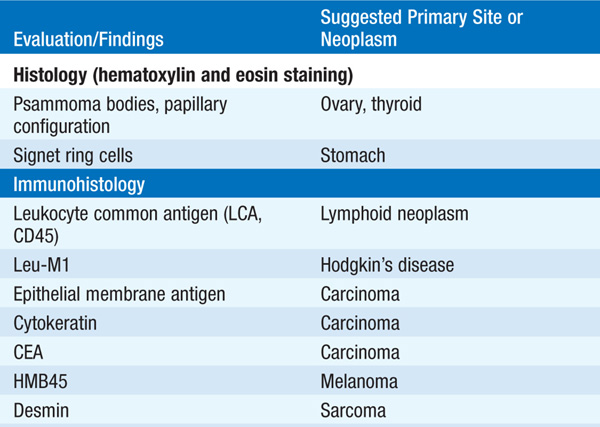
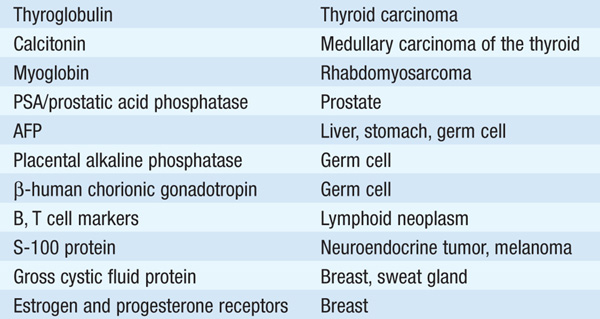
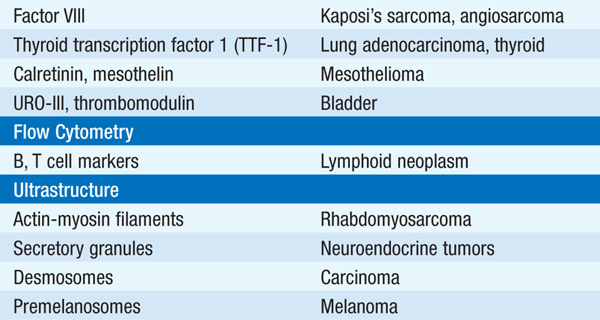
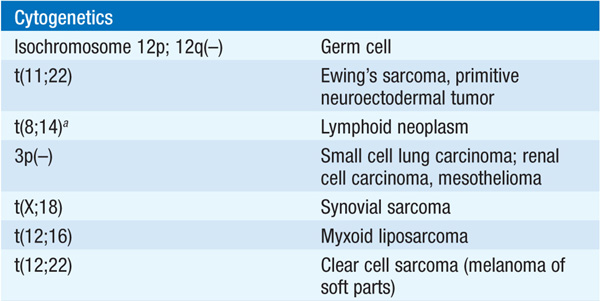
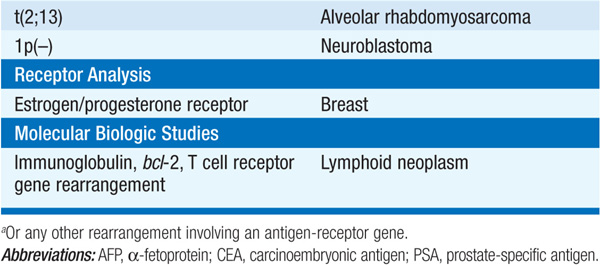
About 60% of CUPS tumors are adenocarcinomas, 5% are squamous cell carcinomas, and 30% are poorly differentiated neoplasms not further classified on light microscopy. Expression of cytokeratin subtypes may narrow the range of possible diagnoses (Fig. 82-1).
FIGURE 82-1 Approach to cytokeratin (CK7 and CK20) markers used in CUP.
Pts with squamous cell carcinoma have a median survival of 9 months; those with adenocarcinoma or unclassifiable tumors have a median survival of 4–6 months. Pts in whom a primary site is identified usually have a better prognosis. Limited sites of involvement and neuroendocrine histology are favorable prognostic factors. Pts without a primary diagnosis should be treated palliatively with radiation therapy to symptomatic lesions. All-purpose chemotherapy regimens rarely produce responses but always produce toxicity. Certain clinical features may permit individualized therapy.
In pts <50 years with tumor involving midline structures, lung parenchyma, or lymph nodes and evidence of rapid tumor growth, germ cell tumor is a possible diagnosis. Serum tumor markers may or may not be elevated. Cisplatin, etoposide, and bleomycin (Chap. 79) chemotherapy may induce complete responses in ≥25%, and ~15% may be cured. A trial of such therapy should probably also be undertaken in pts whose tumors have abnormalities in chromosome 12.
Women who present with pelvic mass or pain and an adenocarcinoma diffusely throughout the peritoneal cavity, but without a clear site of origin, have primary peritoneal papillary serous carcinoma. The presence of psammoma bodies in the tumor or elevated CA-125 levels may favor ovarian origin. Such pts should undergo debulking surgery followed by paclitaxel plus cisplatin or carboplatin combination chemotherapy (Chap. 80). About 20% of pts will respond, and 10% will survive at least 2 years.
Such women should receive adjuvant breast cancer therapy appropriate for their menopausal status even in the absence of a breast mass on physical examination or mammography and undetermined or negative estrogen and progesterone receptors on the tumor (Chap. 77). Unless the ipsilateral breast is radiated, up to 50% of these pts will later develop a breast mass. Although this is a rare clinical situation, long-term survival similar to women with stage II breast cancer is possible.
The probability of prostate cancer is high; a trial of empirical hormonal therapy (leuprolide and flutamide) is warranted (Chap. 81).
Even if panendoscopy fails to reveal a head and neck primary, treatment of such pts with cisplatin and 5-fluorouracil chemotherapy may produce a response; some responses are long-lived (Chap. 75).
For a more detailed discussion, see Varadhachary GR, Abbruzzese JL: Carcinoma of Unknown Primary, Chap. 99, p. 821, in HPIM-18.