60 | THE GENETICS OF ALZHEIMER’S DISEASE
RUDOLPH E. TANZI
Over the past three decades, considerable progress has been made in the identification of genetic risk factors for Alzheimer’s disease (AD). However, the challenges have been immense. First, although one of the key features of AD is familial aggregation and family history is the second greatest risk factor for AD, the genetics of AD are complex and heterogeneous (reviewed in Bertram et al., 2009; Bertram et al., 2010; Tanzi and Bertram, 2005). Second, a definitive diagnosis of AD requires a postmortem neuropathological examination of the brain. The quality of any genetic study depends on the validity and reliability of the phenotypes used. In considering “affection status” as a phenotype, it needs to be emphasized that any AD cohort consisting of living patients may be “contaminated” with non-AD cases of dementia (e.g., frontotemporal lobar dementia). A third challenge is that AD strikes late in life, usually after the age of 70 years. Thus, in family-based genetic studies, parental DNA is rarely if ever available. Moreover, family history, as related by family members may not be accurate. Despite these challenges, genetic discoveries in AD have provided the first and most vital clues regarding the causes of AD. For decades after Alois Alzheimer described the disease in the autopsied brain of a demented female patient in her 50s, our understanding of the etiology and pathogenesis was limited to what could be garnered from the pathological aftermath of the disease. The advent of the first AD genes in the 1980s and 1990s provided us with the first solid clues regarding the etiology and pathogenic events of AD along with strategies for treating and preventing this devastating disease.
EARLY-ONSET FAMILIAL ALZHEIMER’S DISEASE
Based on twin and family studies, approximately 80% of AD includes the inheritance of specific genetic factors as part of its etiology (Gatz et al., 2006). The existence of relatively large multigenerational early-onset familial Alzheimer’s disease (EO-FAD) families helped to make the EO-FAD genes the “low hanging fruit” in AD gene discovery. Roughly 5% of AD is EO-FAD, which can be caused by well over 200 rare, fully penetrant mutations in three different genes. In 1987, we and others isolated the gene encoding the amyloid β (A4) protein precursor (APP), (Goldgaber et al., 1987; Kang et al., 1987; Tanzi et al., 1987a; Tanzi et al., 1988a), and physically and genetically mapped it to chromosome 21 (Tanzi et al., 1987a). The cloning of APP was made possible by the publication of the amino acid sequence of the amyloid β-protein by Glenner and Wong (1984) and Masters et al (1985). In their paper, Glenner and Wong predicted that the gene responsible for making the “β-protein,” as they called it, would be on chromosome 21 and carry mutations causing AD. More importantly, Glenner first proposed that AD is a cerebral form of amyloidosis, in which the accumulation of cerebral amyloid β-protein drives all subsequent pathology. Glenner’s β-protein hypothesis was subsequently reinterpreted and reported eight years later as the “amyloid cascade hypothesis” of AD (Hardy and Higgins, 1992), and was further refined in later years (Hardy and Selkoe, 2002; Tanzi and Bertram, 2005).
When we and others used the Aβ amino acid sequence (Glenner’s β-protein and Masters’ A4) to clone the APP gene (Goldgaber et al., 1987; Kang et al., 1987, Tanzi et al., 1987a, Tanzi et al., 1988), the first AD candidate gene had been identified. Concurrent with the isolation of the APP gene, we also reported in that same issue of Science, evidence for genetic linkage of EO-FAD to genetic markers on chromosome 21 in the vicinity of APP (St George-Hyslop et al., 1987). From 1982 to 1987, Paul Watkins and I had been working in the laboratory of James Gusella at MGH to isolate the first single nucleotide polymorphisms (SNP) on chromosome 21, called restriction fragment length polymorphisms (RFLPs). These were used to build a complete genetic map of this chromosome (Tanzi et al., 1988b). At that same time, we had been collecting some of the largest, multi-generational EO-FAD families and started testing them for genetic linkage to chromosome 21 in 1983.
After testing the first two EO-FAD families (of Canadian and Italian descent), no genetic linkage of AD was observed for the SNPs on our genetic linkage map of chromosome 21. Later, two more EO-FAD families (of German and Russian descent) were added to the study, and Peter St George-Hyslop and Jonathan Haines had taken over the project as I turned my own efforts to cloning the first AD candidate gene, APP. At the same time that we and others had reported the identification and characterization of the APP gene, St George-Hyslop and Haines claimed to find linkage to chromosome 21 in the vicinity of the APP gene near marker D21S1 (St George-Hyslop et al., 1987). Disappointingly, soon after, we showed that the same four large EO-FAD families apparently linked to markers on chromosome 21 near APP exhibited absolutely no genetic linkage to APP (Tanzi et al., 1987b). Van Broeckhoven et al. also reported lack of linkage of EO-FAD to APP in other EO-FAD families (Van Broeckhoven et al., 1987). Importantly, in both of papers, APP was ruled from linkage in the specific EO-FAD families tested, however, we did not rule out APP as a candidate gene for other cases of AD. Later the four EO-FAD families reported to be linked to chromosome 21 were shown to actually be linked to an EO-FAD locus on chromosome 14q24 and were ultimately demonstrated to carry mutations in the presenilin 1 (PSEN1) gene (Sherrington et al., 1995).
So, although the original genetic linkage of EO-FAD to chromosome 21 (St George-Hyslop et al., 1987) was spurious, ironically, it prompted other groups, including that of John Hardy, to test other EO-FAD families for genetic linkage of EO-FAD to our DNA markers (RFLPs) on chromosome 21. And some of those families exhibited genuine linkage to our chromosome 21 map RFLP markers that we had shared with John Hardy. In 1991, the first EO-FAD mutation was found in APP by re-sequencing those independent chromosome 21-linked EO-FAD families (Goate et al., 1991). However, this was not the first disease mutation reported in APP. Prior to the Goate et al. (1991) paper, Frangione et al. had already reported the first pathogenic mutation in APP (Levy et al., 1990). Levy et al. (1990) sequenced exons 16 and 17 of APP, which encode the Aβ domain, and uncovered the first pathogenic mutation in APP, which was responsible for Dutch hereditary cerebral hemorrhage with amyloidosis, sometimes referred to as a vascular form of AD. Goate et al. (1991) took a similar approach on their chromosome 21-linked families by resequencing the same two APP exons, to find the first EO-FAD mutation (London mutation; V717I) in APP.
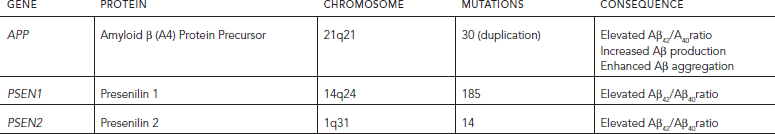
Less than a year after the elucidation of the first APP mutations, it became clear that mutations in APP accounted for a very tiny proportion of EO-FAD (Tanzi et al., 1992). In 1995, several EO-FAD mutations were found in PSEN1 (Sherrington et al., 1995) on chromosome 14. Shortly afterward, we reported a homolog of PSEN1 called presenilin (PSEN2) (Levy-Lahad et al., 1995) on chromosome 1 and showed that it contained the N141I mutation in Volga-German EO-FAD families. This was subsequently confirmed by Rogaev et al. (1995). To date, 30 mutations (plus duplications) have been reported for APP, 185 for PSEN1, and 14 for PSEN2 (Alzheimer’s Disease & Frontotemporal Dementia Mutation Database; http://www.molgen.ua.ac.be/ADMutations). Generally, the EO-FAD mutations in APP, PSEN1, and PSEN2 and duplication of APP are fully penetrant for causing AD (Table 60.1). However, we recently reported the first case of non-penetrant APP duplication (Hooli et al., 2012).
The vast majority of the more than 200 EO-FAD mutations in APP, PSEN1, and PSEN2 lead to increase in the ratio of Aβ42:Aβ40 (Scheuner et al., 1996; Tanzi and Bertram, 2005). The increase in relative levels of Aβ42 then promotes the aggregation of the peptide into β-amyloid (Jarrett et al., 1993). Three years after the discovery of the presenilins in 1995, they were shown to act as aspartyl proteases that carry out γ-secretase cleavage of APP in it transmembrane domain to produce Aβ (reviewed in Tanzi and Bertram, 2005). Based on these collective findings, we have been collaborating with Steve Wagner (UCSD) to develop a class of highly promising AD drugs known as γ-secretase modulators, which are aimed at reversing this ratio. (Kounnas et al, 2010).
TABLE 60.1. Early-onset familial Alzheimer’s disease genes
GENETICS OF LATE-ONSET ALZHEIMER’S DISEASE
The most common form of the disease is defined by onset after 65 years and is referred to as LOAD. Unlike EO-FAD, which is characterized by classic Mendelian inheritance most often in an autosomal dominant manner, LOAD exhibits a genetically complex pattern of inheritance. Risk for most cases of LOAD involve the influence of both genetic and life exposure factors. The most highly confirmed risk factor for LOAD is the ε4 variant of the apolipoprotein E gene (APOE) (Strittmatter et al, 1993) on chromosome 19. The three major variants of APOE are based on combinations of amino acids 112 and 158 (ε2: Cys112/Cys158; ε3: Cys112/Arg158; ε4: Arg112/Arg158). A single copy of the ε4-allele increases AD risk by about four-fold, whereas two copies increase risk by greater than 10-fold. In contrast, the ε2-allele of APOE is protective (Corder et al., 1994). Functionally, APOE is believed to play a role in the clearance of Aβ from the brain (reviewed in Kim et al., 2009).
For a decade or more after the report of association of LOAD with APOE, hundreds of genes were tested for association with AD leading to endless series of replications and refutations. Lars Bertram, colleagues, and I started an online database called AlzGene.org (http://www.alzgene.org) (Bertram and Tanzi, 2008; Bertram et al., 2007) to summarize and display these findings in a systematic and objective manner. In addition, AlzGene.org presents metaanalysis results for AD candidate genes that have been tested in at least four independent case-control samples. The strongest association with LOAD on AlzGene is obtained with APOE. Roses et al. (2010) recently proposed that additional genes near APOE might also influence risk for AD. One of these is a poly-T variant in the gene for the translocase of outer mitochondrial membrane 40 homolog (TOMM40), which is in strong linkage disequilibrium with APOE, mapping only ~2,000 basepairs away. The “long” poly-T repeats were reported to be associated with earlier onset of AD. This creates a conundrum because it is highly unlikely that both APOE and TOMM40, sitting right next door to each other, both contribute to AD risk. Given the choice of whether the real AD gene there is APOE or TOMM40, functional studies strongly support APOE as the actual AD gene in this region based on its ability to affect cerebral Aβ clearance (reviewed in Kim et al., 2009). Moreover, in our own family-based studies of AD, the statistical signal strength of the association of APOE with AD is 15 orders of magnitude higher than that observed for any of other genes in the APOE region, including TOMM40 (unpublished data).
Although most studies searching for novel AD genes after the report of the association with APOE employed candidate gene searches, more genome-wide association studies (GWAS) have become more common. In GWAS, up to one million SNPs (along with single copy probes to detect copy number variants) are tested for genetic association with disease risk and phenotypes including age-of-onset, biomarkers, imaging results, and neuropathological endpoints. The first genome-wide significant GWAS finding of a gene associated with LOAD was with the gene encoding GRB2-associated binding protein 2 (GAB2; Reiman et al., 2007). However, the association was only deemed “genome-wide significant” following post hoc stratification by APOE. The association was followed by a series of replications and refutations. Functionally, GAB2 has been proposed to affect both tau phosphorylation (Reiman et al., 2007) and Aβ production (Nizzari et al., 2007).
A year after the GAB2, we reported the first genes to exhibit genome-wide significant association with AD without stratification on APOE. To achieve this, we employed family-based GWAS (Bertram et Koob and Le Moal, 2008) and reported three AD genes candidates containing SNPs that exhibited genome-wide significance for association AD. These included ATXN1 (ataxin 1), CD33 (siglec 3), and an uncharacterized locus on chromosome 14 (GWA_14q31.2). ATXN1 can carry an expanded poly-glutamine repeat that causes spinocerebellar ataxia type 1. ATXN1 also affects Aβ levels by regulating levels of β-secretase, the rate-limiting enzyme for Aβ production (Zhang et al., 2010). CD33 is a sialic acid-binding, immunoglobulin-like lectin that regulates the innate immune system (Crocker et al., 2007), including inflammation. We recently showed that Aβ has the microbiological properties of an antimicrobial peptide, used in the brain’s innate immune system (Soscia et al., 2010). Thus, control of the brain’s innate immune system by molecules like CD33, might also regulate Aβ levels via clearance by microglial cells.
In 2009, two of the largest case-control GWAS carried out to date (Harold et al., 2009; Lambert et al., 2009) led to three novel AD genes: CLU (clusterin; apolipoprotein J), CR1 (complement component [3b/4b] receptor 1), and PICALM (phosphatidylinositol binding clathrin assembly protein). However, the effect sizes of the AD-associated SNPs in these genes are tiny (i.e. increasing or decreasing risk by ~1.15-fold). In contrast, APOE-ε4 increases risk for AD by ~4-fold and 15-fold, for one or two alleles, respectively. Functionally, CLU is likely involved in importing Aβ from plasma back into the brain (DeMattos et al., 2004; Nuutinen et al., 2009). In contrast, APOE exports the peptide out of the brain into the plasma. PICALM is involved in clathrin-mediated endocytosis (Tebar et al., 1999; Treusch et al., 2011), and CR1, like CD33, plays a role in the innate immune system (Khera and Das, 2009). In 2010, another case-control GWAS (Seshadri et al., 2010) reported association with the gene for bridging integrator 1 (BIN1), which had actually been reported to be associated with AD in an earlier study (Lambert et al., 2009). The AD-associated SNP in BIN1 also has a very small effect size on AD risk with an allelic odds ratio of ~1.15. BIN1 is expressed in the CNS and like PICALM, plays a role in receptor-mediated endocytosis (Pant et al., 2009).
In 2011, two more case-control GWAS reported four more AD candidate genes including CD2AP, MS4A6A/MS4A4E, EPHA1, and ABCA7 (Hollingworth et al., 2011; Naj et al., 2011). These studies also identified a second AD-associated SNP in CD33 providing strong support for our previously reported genome-wide significant association of CD33 with AD three years earlier (Bertram et al., 2008). Thus, in addition to the four original AD genes, APP, PSEN1, PSEN2, and APOE, 11 more AD genes (CD33, GWA_14q31.2, ATXN1, CLU, PICALM, CR1, BIN1, ABCA7, MS4A6E/MS4A4E, CD2AP, and EPHA1) harbor SNPs that exhibit genome-wide significance for association with LOAD (Table 60.2).
The predicted and known functions of the AD genes fall into four basic categories: Aβ metabolism, lipid metabolism, innate immunity, and cellular signaling. With the identification of the original 4 and 11 novel confirmed AD genes, we hope to answer some key remaining questions regarding the etiology and pathogenesis of AD. First, which genes besides APP, PSEN1 and PSEN2 affect the production of Aβ? Based on our own data these would minimally include ATXN1 (Zhang et al., 2010). Second, which genes besides APOE affect the clearance of Aβ in the brain? These would likely include CLU and according to our own unpublished preliminary data, CD33, based on its ability to activate microglial degradation of Aβ. Other AD candidate genes that activate microglia to clear Aβ may also be involved (e.g. CR1).
The excessive accumulation of Aβ in the brain is believed to trigger tauopathy and tangles, followed by neurodegeneration and inflammation. The ability of excess accumulation of cerebral Aβ to trigger tauopathy likely involves aberrant signaling and could therefore involve PICALM, BIN1, CD2AP (Treusch et al., 2011). Neurodegeneration accompanied by tauopathy and excess Aβ accumulation must also induce inflammatory pathways to complete the course of neuronal cell death and synapse loss initially triggered by excessive Aβ accumulation in the brain. It is likely that AD genes involved in the innate immune system (e.g. CD33, CLU, MS4A6E/MS4A4E, and EPHA1) play a role here. Thus, so far, the known AD genes and newly confirmed AD gene candidates from GWAS fit fairly nearly into an overall pathogenic pathway in which excessive accumulation of Aβ leads to tauopathy and neurodegeneration followed by inflammation ultimately resulting in catastrophic loss of neurons and synapses leading to dementia (Tanzi and Bertram, 2005).
TABLE 60.2. Late-onset Alzheimer’s disease genes
| GWAS | DESIGN |
GENES EXHIBITING GENOME-WIDE SIGNIFICANT ASSOCIATION WITH LOAD |
| Reiman, 2007 | Case-control | APOE, GAB2 |
| Bertram, 2008 | Family-based | APOE, ATXN1, CD33, GWA_14q31 |
| Lambert, 2009 | Case-control | APOE, CLU, CR1 |
| Harold, 2009 | Case-control | APOE, CLU, PICALM |
| Seshadri, 2010 | Case-control | APOE, BIN1 |
| Naj, 2011 | Case-control | MS4A6A/MS4A4E, EPHA1,CD33, CD2AP |
| Hollingworth, 2011 | Case-control | ABCA7, MS4A6A/MS4A4E, EPHA1, CD33, CD2AP |
ADAM10: FIRST LOAD GENE WITH RARE PATHOGENIC MISSENSE MUTATIONS
Late-onset AD has been associated with common genetic variants, which, with the exception of APOE, exert small effects on risk. However, our laboratory recently reported two rare, highly penetrant mutations for LOAD (Kim et al., 2008), located in the ADAM10 gene. ADAM10 encodes the major α-secretase in the brain, which cleaves within the Aβ domain of APP to preclude β-amyloid formation We reported two rare (7 of 1000 LOAD families) LOAD mutations in ADAM10: Q170H and R181G. Both are located in the prodomain region and lead to AD at roughly 70 years old. Both mutations severely impair ADAM10’s ability to cleave at the α-secretase site of APP in vitro (Kim et al., 2008) and these effects have now been confirmed in vivo (unpublished observations). To date, these are the first and only highly penetrant, rare mutations reported for LOAD. These findings underscore the critical need for whole genome or whole exome sequencing to identify other rare functional DNA variants causing LOAD, perhaps with high penetrance as we have observed for the novel LOAD mutations in ADAM10.
CONCLUSIONS
Over the past three decades, the identification and characterization of the AD genes have elucidated the etiology and pathogenesis of AD. Studies of these genes have also provided valuable clues regarding treatment and prevention of AD (reviewed in Bertram and Tanzi, 2010; Tanzi and Bertram, 2005). Following the initial discovery of the first four established AD genes, APP, PSEN1, PSEN2, and APOE, AD GWAS aimed at identifying additional AD genes (reviewed in Bertram et al., 2009, 2010) have introduced a new era of AD genetics. However, the new LOAD genes coming out of GWAS carry SNPs that generally have only small effect sizes. It is almost certain that in most, if not all cases, these SNPs are not the functional variants affecting risk for AD. Fortunately, the development of powerful sequencing technologies such as whole genome sequencing should allow us to identify the actual functional variants in the novel AD genes emerging from GWAS, as well as in the original AD genes. The eventual elucidation of the actual functional variants in these genes (as we have found in ADAM10) will allow for more meaningful biological and translational studies as well as novel animal models for AD. In this way, genetic studies of AD will continue to inform and guide new treatment strategies for preventing and treating this terrible disease.
DISCLOSURES
Dr. Tanzi serves as a consultant to Prana Biotechnology. Eisai, Genomind, Probio Drug, Abide, and EcoEos. He also has a financial interest in Prana Biotechnology, Neurogenetic Pharmaceuticals, Evolutionary Genomics, Neuroptix, Abide, and Genomind.
REFERENCES
Bertram, L., and Tanzi, R.E. (2005). The genetic epidemiology of neurodegenerative disease. J. Clin. Invest. 115(6):1449–1457.
Bertram, L., and Tanzi, R.E. (2008). Thirty years of Alzheimer’s disease genetics: systematic meta-analyses herald a new era. Nat. Rev. Neurosci. 9:768–778.
Bertram, L., and Tanzi, R.E. (2009). Genome-wide association studies in Alzheimer’s disease. Hum. Mol. Genet. 18(R2):R137–R145.
Bertram, L., Lange, C., et al. (2008). Genome-wide association analysis reveals putative Alzheimer’s disease susceptibility loci in addition to APOE. Am. J. Hum. Genet. 83(5):623–632.
Bertram, L., Lill, C.M., et al. (2010). The genetics of Alzheimer disease: back to the future. Neuron 68(2):270–281.
Bertram, L., McQueen, M.B., et al. (2007). Systematic meta-analyses of Alzheimer disease genetic association studies: the AlzGene database. Nat. Genet. 39(1):17–23.
Corder, E.H., Saunders, A.M., et al. (1994). Protective effect of apolipoprotein E type 2 allele for late onset Alzheimer disease. Nat. Genet. 7:180–184.
Crocker, P.R., Paulson, J.C., et al. (2007). Siglecs and their roles in the immune system. Nat. Rev. Immunol. 7(4):255–266.
DeMattos, R.B., Cirrito, J.R., et al. (2004). ApoE and clusterin cooperatively suppress Abeta levels and deposition: evidence that ApoE regulates extracellular Abeta metabolism in vivo. Neuron 41:193–202.
Gatz, M., Reynolds, C.A., et al. (2006). Role of genes and environments for explaining Alzheimer disease. Arch. Gen. Psychiat. 63:168–174.
Glenner, G.G., and Wong, C.W. (1984). Alzheimer’s disease and Down’s syndrome: sharing of a unique cerebrovascular amyloid fibril protein. Biochem Biophys. Res. Comm. 122:1131–1135.
Goate, A., Chartier-Harlin, M.C., et al. (1991). Segregation of a missense mutation in the amyloid precursor protein gene with familial Alzheimer’s disease. Nature 349(6311):704–706.
Goldgaber, D., Lerman, M.I., et al. (1987). Characterization and chromosomal localization of a cDNA encoding brain amyloid of Alzheimer’s disease. Science 235:877–880.
Hardy, J.A., and Higgins, G.A. (1992). Alzheimer’s disease: the amyloid cascade hypothesis. Science 256:184–185.
Hardy, J., and Selkoe, D.J. (2002). The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science 297:353–356.
Harold, D., Abraham, R., et al. (2009). Genome-wide association study identifies variants at CLU and PICALM associated with Alzheimer’s disease. Nat. Genet. 41(10):1088–1093.
Hollingworth, P., Harold, D., et al. (2011). Common variants at ABCA7, MS4A6A/MS4A4E, EPHA1, CD33 and CD2AP are associated with Alzheimer’s disease. Nat. Genet. 43(5):429–435.
Hooli, B.V., Mohapatra, G., et al. (2012). Role of common and rare APP DNA sequence variants in Alzheimer disease. Neurology 78(16):1250–1257.
Jarrett, J.T., Berger, E.P., et al. (1993). The carboxy terminus of the beta amyloid protein is critical for the seeding of amyloid formation: implications for the pathogenesis of Alzheimer’s disease. Biochemistry 32:4693–4697.
Kang, J., Lemaire, H.G., et al. (1987). The precursor of Alzheimer’s disease amyloid A4 protein resembles a cell-surface receptor. Nature 325:733–736.
Kim, J., Castellano, J.M., et al. (2009). Overexpression of low-density lipoprotein receptor in the brain markedly inhibits amyloid deposition and increases extracellular A beta clearance. Neuron 64(5):632–644.
Kim, M., Suh, J., et al. (2009). Potential late-onset Alzheimer’s disease-associated mutations in the ADAM10 gene attenuate α-secretase activity. Hum Mol Genet. 18(20):3987–3996.
Kounnas, M.Z., Danks, A.M., et al. (2010). Modulation of γ-secretase reduces β-amyloid deposition in a transgenic mouse model of Alzheimer’s disease. Neuron 67(5):769–780.
Lambert, J., Heath, S., et al. (2009). Genome-wide association study identifies variants at CLU and CR1 associated with Alzheimer’s disease. Nat. Genet. 41(10):1094–1099.
Levy, E., Carman, M.D., et al. (1990). Mutation of the Alzheimer’s disease amyloid gene in hereditary cerebral hemorrhage, Dutch type. Science 248:1124–1126.
Levy-Lahad, E., Wasco, W., et al. (1995). Candidate gene for the chromosome 1 familial Alzheimer’s disease locus. Science 269(5226):973–977.
Masters, C.L., Simms, G., et al. (1985). Amyloid plaque core protein in Alzheimer disease and Down syndrome. Proc. Natl. Acad. Sci. USA 82:4245–4249.
Naj, A.C., Jun, G., et al. (2011). Common variants at MS4A4/MS4A6E, CD2AP, CD33 and EPHA1 are associated with late-onset Alzheimer’s disease. Nat. Genet. 43(5):436–441.
Nizzari, M., Venezia, V., et al. (2007). Amyloid precursor protein and Presenilin1 interact with the adaptor GRB2 and modulate ERK 1,2 signaling. J. Biol. Chem. 282(18):13833–13844.
Nuutinen, T., Suuronen, T., et al. (2009). Clusterin: a forgotten player in Alzheimer’s disease. Brain. Res. Rev. 61(2):89–104.
Pant, S., Sharma, M., et al. (2009). AMPH-1/Amphiphysin/Bin1 functions with RME-1/Ehd1 in endocytic recycling. Nat. Cell Biol. 11(12):1399–1410.
Reiman, E.M., Webster, J.A., et al. (2007). GAB2 alleles modify Alzheimer’s risk in APOE epsilon4 carriers. Neuron 54(5):713–720.
Rogaev, E.I., Sherrington, R., et al. (1995). Familial Alzheimer’s disease in kindreds with missense mutations in a gene on chromosome 1 related to the Alzheimer’s disease type 3 gene. Nature 376(6543):775–778.
Roses, A.D., Lutz, M.W., et al. (2010). A TOMM40 variable-length polymorphism predicts the age of late-onset Alzheimer’s disease. Pharmacogenomics J. 10:375–384.
Scheuner, D., Eckman, C., et al. (1996). Secreted amyloid beta-protein similar to that in the senile plaques of Alzheimer’s disease is increased in vivo by the presenilin 1 and 2 and APP mutations linked to familial Alzheimer’s disease. Nat. Med. 2:864–870.
Seshadri, S., Fitzpatrick, A.L., et al. (2010). Genome-wide analysis of genetic loci associated with Alzheimer disease. JAMA 303(18):1832–1840.
Sherrington, R., Rogaev, E.I., et al. (1995). Cloning of a gene bearing missense mutations in early-onset familial Alzheimer’s disease. Nature 375(6534):754–760.
Soscia, S.J., Kirby, J.E., et al. (2010). The Alzheimer’s disease-associated amyloid beta-protein is an antimicrobial peptide. PLoS ONE 5(3):e9505.
St George-Hyslop, P.H., Tanzi, R.E., et al. (1987). The genetic defect causing familial Alzheimer’s disease maps on Chromosome 21. Science 235:885–890.
Strittmatter, W.J., Saunders, A.M., et al. (1993). Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. Proc. Natl. Acad. Sci. USA 90(5):1977–1981.
Tanzi, R.E., Gusella, J.F., et al. (1987a). Amyloid beta protein gene: cDNA, mRNA distribution, and genetic linkage near the Alzheimer locus. Science 235(4791):880–884.
Tanzi, R.E., St George-Hyslop, P.H., et al. (1987b). The genetic defect in familial Alzheimer’s disease is not tightly linked to the amyloid beta protein gene. Nature 329:156–157.
Tanzi, R.E., Haines, J.L., et al. (1988a). Genetic linkage map of human chromosome 21. Genomics 3:129–136.
Tanzi, R.E., McClatchey, A.I., et al. (1988b). Protease inhibitor domain encoded by an amyloid protein precursor mRNA associated with Alzheimer’s disease. Nature 331:528–530.
Tanzi, R.E., Vaula, G., et al. (1992). Assessment of β-amyloid protein precursor gene mutations in a large set of familial and sporadic Alzheimer disease cases. Am. J. Hum. Genet. 51:273–282.
Tanzi, R.E., and Bertram, L. (2005). Twenty years of the Alzheimer’s disease amyloid hypothesis: a genetic perspective. Cell 120(4):545–555.
Tebar, F., Bohlander, S.K., et al. (1999). Clathrin assembly lymphoid myeloid leukemia (CALM) protein: localization in endocytic-coated pits, interactions with clathrin, and the impact of overexpression on clathrin-mediated traffic. Mol. Biol. Cell 10(8):2687–2702.
Treusch, S., Hamamichi, S., et al. (2011). Functional links between Aβ toxicity, endocytic trafficking, and Alzheimer’s disease risk factors in yeast. Science 334(6060):1241–1245.
Van Broeckhoven, C., Genthe, A.M., et al. (1987). Failure of familial Alzheimer’s disease to segregate with the A4-amyloid gene in several European families. Nature 329:153–155.
Zhang, C., Browne, A., et al. (2010). Loss of function of ATXN1 increases amyloid beta-protein levels by potentiating beta-secretase processing of beta-amyloid precursor protein. J. Biol. Chem. 285(12):8515–8526.