 OHCM10 p. 26)
OHCM10 p. 26)Medicine
Surgery
Other specialties
Taking a thorough history is an essential skill as a junior doctor and something you will become extremely practised at.The basic features of a history, with details of how to perform a basic examination are described in this chapter. How to refine these approaches is further described for specific situations you may encounter.
Taking a history ( OHCM10 p. 26)
OHCM10 p. 26)
• Try to be in a setting that offers privacy and has a bed
• Establish the patient’s name and check their date of birth
Presenting complaint Why has the patient come to hospital? Let them tell their story. Write their main problem(s) in their own words along with duration of symptoms and who referred them; if the referral letter has a different presenting complaint then document this too.
History of presenting complaint(s) Ask questions aimed at differentiating the causes of the presenting complaint and assessing its severity. Try to exclude potentially life-threatening causes first. Ask specifically about previous episodes and investigations/treatments. Use the SOCRATES questions for pain (Site, Onset, Character, Radiation, Associations, Timing, Exacerbating/relieving factors, Severity). Ask about the effect on their activities of daily living (ADLs). If there are multiple problems, ask if they come on together or are related.
Risk factors Document recognized risk factors for important differentials.
Past medical history Ask about previous medical problems/operations and attempt to gauge the severity of each (eg hospital/ICU admissions, exercise tolerance (ET), treatment); use the drug history to prompt the patient’s memory. Consider documenting specifically about asthma, DM, angina, ↑ BP, MI, stroke, VTE, epilepsy, malignancy.
Drug history Document all drugs along with doses, times taken, and any recent changes. Always document drug allergies along with the reaction precipitated. Or no known drug allergies (NKDA). Remember to ask about OTC medications. Ask about compliance too.
Family history Ask about relevant illness in the family (eg heart problems, DM, cancer). What age were they at diagnosis? Are other family members well at the moment?
Social history This is essential: Home Ask about who they live with, the kind of house (eg bungalow, residential home), any home help, own ADLs (cooking, dressing, washing); Mobility Walking aids (stick/frame), exercise tolerance (how far can they walk on level ground? Can they climb stairs?); Lifestyle Occupation, alcohol (units/wk), smoking (cigarettes/d and pack-years), recreational drugs:
Systems review Relevant systems review will often be part of the HPC; a thorough systems review is only necessary if you are unsure what is relevant or are struggling to explain the symptoms. See Table 3.1 and  OHCM10 p. 28.
OHCM10 p. 28.
Table 3.1 Key symptoms to assess on systems review
| CVS | Chest pain, palpitations, SOB, ankle swelling, orthopnoea |
| Resp | Cough (?blood), sputum, wheeze, SOB |
| Abdo | Abdo pain, nausea/vomiting, bowel habit (?blood), stool colour and consistency, distension, dysuria, frequency, urgency, haematuria |
| Neuro | Headache, photophobia, neck stiffness, weakness, change in sensation, balance, fits, falls, speech, changes in vision/hearing |
| Systemic | Appetite, weight loss/gain, fever/night sweats, malaise, stiff/swollen joints, fatigue, rashes/itch, sleep pattern |
Summarizing Ask if there are any other problems that have not been discussed and repeat back a summary of the history to the patient to check that they agree (Box 3.1). It is a good idea to use the ICE questions (Ideas, Concerns, Expectations) at this point—ask the patient if they have any idea or suspicion of what might be wrong with them, if there’s anything in particular that they’re worried about (this may prompt them to admit specific concerns, eg having cancer), and what they expect will happen to them while they are in hospital. The art of ‘ICE’ is to ask naturally, so patients feel able to open up to you. Doing this while examining the patient can work well for some.
 Box 3.1 Should you take notes while clerking?
Box 3.1 Should you take notes while clerking?
There is no simple answer to this. Taking notes while the patient talks may allow you to record important details accurately or even to write up your clerking as you go. This can be extremely useful during busy on-calls. Alternatively, not taking notes allows you to give the patient your undivided attention and the opportunity to record the clerking having considered the whole picture. In the end it comes down to individual preference and workload.
Most patients have no idea about tests and investigations and find being admitted to hospital a frightening event; they often value the opportunity to talk about possible options and ask questions.
Always finish your history by asking specifically if the patient has any further questions or any other issues they would like to discuss, as frequently they will be too embarrassed/shy/reticent to ask.
By the end of taking the history you should have a reasonable idea of the differential diagnosis. Try to think of specific signs that would be present on examination to confirm or refute these differentials. A basic examination is described in the next topic ( p. 128).
p. 128).
It is good practice to perform a brief CVS, RS, abdo, and neuro exam on all patients but focus your examination according to their history. Check observations (temp, BP, HR, RR, O2 sats):
• Ask a nurse to chaperone you if necessary
• Get consent before touching the patient, ask where it hurts
• First assess briefly whether the patient looks well or ill.
Hands ( p. 154)
p. 154)
Inspection Of the hands for signs of disease.
Palpation Check the pulse for rate, rhythm, and character (eg ?collapsing pulse).
Inspection Central cyanosis, mucous membranes, stomatitis, beefy tongue (↓iron), candidiasis, ulcers, dental hygiene (risk factor for SBE).
Cardiovascular system ( pp. 130–131)
pp. 130–131)
Inspection JVP (very useful if visible), swollen ankles.
Palpation Temp of hands, capillary-refill, carotid pulse (volume and character), apex beat, heaves/thrills, hepatomegaly.
Auscultation Heart sounds, added sounds/murmurs (timing, volume, radiation), carotid bruits, basal crackles.
Respiratory system ( p. 132)
p. 132)
Inspection Asterixis (flap), stridor, JVP, RR and effort (accessory muscles, recession), chest wall movement, peripheral oedema.
Palpation Trachea, cervical lymphadenopathy, expansion.
Percussion Symmetrical, hyperresonant, dull, stony dull.
Auscultation Air entry, crackles, wheeze, bronchial breath sounds, rub.
Abdomen ( p. 133)
p. 133)
Inspection Jaundice, scars, distension, hernias, oedema.
Palpation Start away from pain and watch patient’s face: tenderness, peritonism (guarding, rebound, rigidity, percussion tenderness), masses, liver, spleen, kidneys and AAA (expansile mass), hernias, ± genitalia, PR (masses, stool, tenderness, prostate, blood/mucus/melaena).
Percussion Ascites (shifting dullness, fluid thrill), liver, spleen.
Auscultation Bowel sounds (absent, reduced, increased, tinkling).
Peripheral nerves ( pp. 136–138)
pp. 136–138)
Inspection Posture, movement of limbs.
Palpation Tone; power (5 normal, 4 weak, 3 against gravity only, 2 not even against gravity, 1 twitch, 0 none); reflexes (tendons, plantars); sensation.
Coordination Finger–nose, slide heel down opposite leg.
Cranial nerves ( p. 135)
p. 135)
Inspection GCS, mental state ( pp. 163–164), facial symmetry, scars, obvious gaze palsies, speech, posture.
pp. 163–164), facial symmetry, scars, obvious gaze palsies, speech, posture.
Eyes (II, III, IV, VI) Acuity, pupil reactivity, fields, movements, fundi.
Face (V, VII) Sensation and power.
Mouth (IX, X, XII) Tongue movements, uvula position, cough.
Other (VIII) Hearing, balance, gait (XI), shrug, head movements.
The initial clerking of a patient is one of the most important steps in their journey through the hospital. It will be reread by every team that looks after the patient and used as a benchmark for measuring the progress of the patient’s condition. A good clerking gives the patient the best opportunity to receive the correct investigations and treatment.
Heading Your name, position, location, date, time; state clearly why the patient is being clerked (eg referred from ED with chest pain).
Format Follow a logical order setting out each section under the headings shown in this topic. If a piece of information from a different section is really important then write it in the history of presenting complaint and/or under the social history.
Sources State where you got important information from (eg patient, relative (with name and relationship), notes, computer records). This makes it easy to check if the information is of critical importance.
Use the notes Don’t rely on a patient’s account of their previous medical history, especially for investigations and results. Try to find the official record of key investigations rather than relying on another doctor’s comments.
Be thorough These pages represent a basic clerking; you should record all of the information described on these pages at the very least. Use ‘NAD’ to record ‘nothing abnormal detected’ by all means, but do not be tempted to write it for a system you have not examined properly (‘not actually done’)—this is inaccurate and dishonest and even if the system seems unrelated to the presenting complaint, may lead to problems later if the patient subsequently develops an unexpected problem with that system causing colleagues to refer back to the admission clerking.
State the obvious What appears obvious now may not be to someone reading the notes or on the next shift, eg below-knee prosthetic leg, crying constantly.
Differential diagnosis What diseases are likely to explain the patient’s symptoms? What serious diseases need to be excluded? Make a list of these after the examination. Consider recording the most critical evidence for and against each diagnosis.
Management plan This should be a detailed list of the steps you will take to diagnose and treat the differential diagnosis. It should be written in order of priority. Alongside investigations and treatment consider nursing measures, frequency of observations, what to do in the event of deterioration, referrals, best location (eg respiratory ward, HDU). If you have referred the patient to another specialty, record the name, bleep, and time patient was accepted. Likewise if you have handed the patient over to a colleague at a shift change.
State what the patient was told This prevents confusion. If you are not telling the patient about a serious illness then state why.
 p. 76 for other tips about writing in the notes.
p. 76 for other tips about writing in the notes.
Symptoms Chest pain or heaviness, dyspnoea (exertional, orthopnoea, paroxysmal nocturnal) (see Table 3.2), ankle/limb swelling, palpitations, syncope or presyncope, limb pain (at rest or on exertion), fatigue, numbness, ulcers.
Past medical history IHD, MI, hypertension, palpitations, syncope, clotting problems, rheumatic fever, cardiac surgery, recent dental work, liver problems, renal problems, thyroid disease.
Table 3.2 Functional classification of heart failure (NYHA)
| Class I | Disease present but no symptoms during ordinary activity |
| Class II | Angina or dyspnoea during ordinary activity (eg walking to shops) |
| Class III | Angina or dyspnoea during minimal activity (eg making cup of tea) |
| Class IV | Angina or dyspnoea at rest |
Source: data from Dolgin M, et al. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels, 9th edition, Lippincott Williams and Wilkins (Boston: MA), 1994, and Criteria Committee, New York Heart Association, Inc. Diseases of the heart and blood vessels. Nomenclature and criteria for diagnosis, 6th edition, Little, Brown and Co. (Boston: MA), 1964.
Drug history Cardiac medications (and compliance), allergies (and reaction).
Social history Tobacco, alcohol, and caffeine consumption, illicit drug use (?IV, cocaine), occupation, exercise tolerance on flat and stairs.
Family history IHD, ↑lipids, cardiomyopathy, congenital heart disease, sudden cardiac death.
Coronary artery disease risk factors Previous IHD, smoking, ↑ BP, ↑lipids, family history of IHD, DM, obesity and physical inactivity, male sex.
 Box 3.2 Palpation of central and peripheral pulses
Box 3.2 Palpation of central and peripheral pulses
Central
• Carotid Two fingers, medial to the sternocleidomastoid muscle and lateral to the thyroid cartilage (do not palpate both sides together)
• Abdominal aorta Fingertips of both hands, applied halfway between umbilicus and xiphisternum.
Arms
• Radial Two fingers pressed on the radial aspect of the inner wrist
• Ulnar Two fingers pressed on the ulnar aspect of the inner wrist
• Brachial Two fingers pressed into the antecubital fossa, just medial to the biceps tendon (ask patient to flex arm against resistance to find the tendon).
Legs
• Femoral Two fingers pressed firmly into the middle of the crease in the groin, halfway between the symphysis pubis and the anterior superior iliac spine
• Popliteal Ask patient to flex their knee, put both your thumbs either side of the patella and press firmly with your fingertips into the popliteal fossa
• Posterior tibial Two fingers pressed 1cm posterior to the medial malleolus
• Dorsalis pedis Two fingers pressed between the 1st and 2nd metatarsals.
General inspection Dyspnoea at rest, cyanosis, pallor, facial flushing, Marfan’s, Turner’s, Down’s syndromes, rheumatological disorders, acromegaly.
Hands Radial pulses (right and left, collapsing pulse) (see Box 3.2), clubbing, splinter haemorrhages, Osler’s nodes, peripheral cyanosis, xanthomata.
Face Eyes (pallor, jaundice, xanthelasma), malar flush, mouth (cyanosis, high-arched palate, dentition).
Neck JVP, carotids (pulse character) (see Box 3.2).
Precordium Inspection (scars, deformity, apex beat), palpate (apex beat, thrills, heave (Table 3.3)), auscultate (heart sounds (Table 3.4), murmurs—also auscultate with the patient in both left lateral and sitting forward positions).
Back Scars, sacral oedema, pleural effusions, pulmonary oedema.
Abdomen Palpate liver, spleen, aorta, ballot kidneys, percuss for ascites, femoral and renal artery bruits, radiofemoral delay.
Legs Peripheral pulses (see Box 3.2), temperature, ulceration, oedema, calf tenderness, venous guttering, thin shiny skin, loss of hair, gangrene, varicose veins, eczema, haemosiderin pigmentation of the skin (particularly above the medial malleolus), lipodermatosclerosis (‘inverted champagne bottle leg’).
Blood pressure Lying and standing, consider also left and right arms separately.
Other Urine analysis, fundoscopy, temperature chart.
Table 3.3 Characteristics of valve defects
| Mitral stenosis | Mid-diastolic rumbling murmur, loud 1st HS, opening snap, malar flush, AF, tapping apex, left parasternal heave |
| Mitral regurgitation | Pansystolic murmur radiating to the axilla, soft 1st HS, 3rd HS present, thrusting apex, left parastenal heave |
| Aortic stenosis | Ejection systolic murmur radiating to the neck, 4th HS, reversed HS splitting, slow rising pulse, systolic thrill |
| Aortic regurgitation | Early diastolic murmur (best heard in expiration), collapsing pulse, wide BP, pistol-shot femoral pulse, Corrigan’s sign, Quincke’s sign, de Musset’s sign |
Table 3.4 Heart sounds
| 1st (S1) | Physiological; blocking of blood flow after closing of the mitral (M1) and tricuspid (T1) valves |
| 2nd (S2) | Physiological; blocking of blood flow after closing of the aortic (A2) and pulmonary (P2) valves; aortic precedes pulmonary and splitting can be heard during inspiration |
| 3rd (S3) | Sometimes pathological; caused by blood rushing into the ventricles after S2; suggests increased volume of blood in athletes, pregnancy or heart failure |
| 4th (S4) | Pathological; blood pushing open a stiff ventricle before S1; suggests LVF, aortic stenosis, cardiomyopathy |
Symptoms Cough, sputum, shortness of breath, wheeze, chest pain, fevers and sweats, weight loss, hoarseness, snoring, day sleepiness (obstructive sleep apnoea).
Past medical history Chest infections/pneumonias (as child or adult), tuberculosis, HIV status and risk factors, allergy, rheumatoid disease.
Drug history Respiratory drugs (inhalers, steroids, etc), vaccination history (especially BCG, Hib, pneumococcus), drugs known to cause respiratory problems (bleomycin, methotrexate, amiodarone, etc), allergies.
Social history Tobacco use (expressed in pack-years—ie 20 cigarettes/d for 1yr = 1pack-year) and social exposure to tobacco smoke if non-smoker, pets, exposure to other family members with respiratory problems (TB etc), illicit drug use (crack cocaine, cannabis).
Occupational history Past and present jobs, asking specifically about dust exposure, asbestos, animal dander.
Family history Asthma/atopy, cystic fibrosis, emphysema.
General inspection O2 requirements, cough, audible wheeze or stridor, rate and depth of respiration, use of accessory muscles, body habitus.
Hands Clubbing, peripheral cyanosis, tar staining, wasting/weakness of intrinsic muscles, HR, fine tremor of β-agonists, flapping tremor of CO2 retention.
Face Eyes (Horner’s syndrome, anaemia), mouth (central cyanosis), voice.
Neck Trachea position (± scars), JVP.
Chest anteriorly Inspect (shape, scars, radiotherapy marks), palpate (supraclavicular nodes, axillary nodes, expansion, vocal fremitus, apex beat, parasternal heave), percuss, auscultate.
Chest posteriorly Inspect, palpate (including cervical nodes), percuss, auscultate.
Other Peripheral oedema, calf erythema/tenderness, temperature chart, breast examination (if suspect malignancy), abdominal examination, PEFR (see Box 3.3), sputum pot.
 Box 3.3 Recording PEFR
Box 3.3 Recording PEFR
Ensure the meter is set to zero and fit a new disposable mouthpiece. Stand the patient up (or sit up if unable to stand) and give them clear instructions. They should take as deep a breath as possible, before placing the meter in their mouth and closing their lips around the mouthpiece. Encourage them to blow out as hard and as fast as possible. Record the reading obtained, then document the best of 3 efforts.
Symptoms Abdo pain, association with eating, vomiting, or opening bowels, weight loss, appetite, bruising, bleeding, nausea, vomiting (appearance), dysphagia, odynophagia. dysuria, urinary frequency and urgency, possibility of pregnancy. Stool Change in bowel habit, frequency, consistency, colour, pain on passing, recurrent urge, blood (bowl or paper), offensive smell, mucus.
Past medical history GI bleeds, GORD, varices, gallstones, liver problems, jaundice, IBD, haemorrhoids, polyps, blood transfusions.
Drug history NSAIDs, anticoagulants, hepatotoxic drugs ( p. 174), opioids, laxatives, recent antibiotics (Clostridium difficile).
p. 174), opioids, laxatives, recent antibiotics (Clostridium difficile).
Social history Foreign travel, illicit drug use (?IV), sexual history.
Alcohol Intake per day (in units,  p. 126), CAGE questions (
p. 126), CAGE questions ( p. 372).
p. 372).
Family history IBD, liver disease, cancer.
General inspection Oedema, wasting, jaundice, anaemia, lymphadenopathy, breath odour, mouth ulcers, gynaecomastia, spider naevi, bruises.
Hands Clubbing, nail colour, palm colour, flap, Dupuytren’s.
Abdomen Distension (fat, faeces, flatus, fluid, foetus), prominent veins, tenderness (guarding, rebound), masses, organomegaly (see Tables 3.5 and 3.6), ascites, hernial orifices (inguinal, femoral, incisional), bowel sounds.
PR Visible haemorrhoids, fissures and skin tags, anal tone, prostate, rectal masses, appearance of faeces ± blood.
Table 3.5 Common abdominal masses—if in doubt, check with USS
| Liver | RUQ, extends to RLQ, unable to get above, dull to percussion |
| Spleen | LUQ extends to RLQ, unable to get above, notch |
| Kidney | RUQ and/or LUQ, ballotable, able to get above it, smooth outline |
| Faeces | Indentable mass away from umbilicus |
Table 3.6 Common causes of enlarged liver and spleen
| Hepatomegaly | Alcohol, hepatitis, EBV, CMV, thin patient, autoimmune hepatitis, toxins, liver metastases, lymphoma, leukaemia, haemochromatosis, amyloidosis, hyperexpanded chest, eg COPD, heart failure |
| Splenomegaly | Chronic liver disease, autoimmune disease, thrombocytopenia, EBV, CMV, hepatitis, HIV, haemolytic anaemia, leukaemia, lymphoma, endocarditis, thalassaemia, sickle cell, myelofibrosis, sarcoid, amyloidosis, malaria, leishmaniasis |
| Hepatosplenomegaly | Hepatitis, EBV, CMV, chronic liver disease, leukaemia, lymphoma, myelofibrosis, amyloidosis |
Presenting complaint Onset, duration, course (improving, worsening, relapsing–remitting), aggravating or alleviating factors, change with time of day, trauma.
Symptoms Headache, pain, numbness, tingling, weakness, tremor, twitching, abnormal movements, loss of consciousness, seizures, abnormal smells, vision (loss, diplopia, flashing lights), hearing, swallowing, speech, balance, vertigo, nausea, vomiting, coordination, urinary incontinence or retention, impotence, faecal incontinence, constipation, personality, memory, language, visuospatial skills, change in intellect.
Collateral history In many neurological conditions the patient may not be able to describe all the symptoms, eg seizure; try to get a history from a witness or family member.
Past medical history Similar episodes, meningitis, migraines, strokes, seizures, heart problems, hypertension, DM, psychiatric problems.
Drug history Neurological drugs (eg antiepileptics, Parkinson’s medications), psychiatric drugs (eg antipsychotics, antidepressants), all others (especially cardiac and hypoglycaemic drugs).
Family history Draw a family tree with all four grandparents and all their children and grandchildren, ask specifically about learning difficulties, disability, epilepsy, dementia, CVAs, psychiatric problems.
Social history Alcohol, smoking, illicit drugs, occupation, travel abroad, dominant hand.
Obs GCS, BP (lying and standing), HR, RR, glucose.
General appearance Posture, neglect, nutrition, mobility aids.
Cognition Tested using the Mini-Mental State Exam ( p. 377) or 10-point Abbreviated Mental State Exam (
p. 377) or 10-point Abbreviated Mental State Exam ( p. 375).
p. 375).
Meningism Photophobia, neck stiffness, Brudzinski’s sign (involuntary flexion of hips and knees when neck flexed due to neck stiffness), Kernig’s sign (unable to straighten leg when hip fully flexed in supine patient), straight leg raise (hamstring spasm on passively flexing the hip).
Skin Birthmarks, vitiligo, café-au-lait spots, ash leaf macules, lumps, tufts of hair/dimples at the base of the spine.
See Table 3.7 for cranial nerve examination, and Fig. 3.1.
Table 3.7 Cranial nerve examination
| Nerve | Function | Tests | |
| Olfactory | I | Smell | Rarely tested |
| Optic (Fig. 3.1) | II | Vision | Visual acuity, visual fields, pupil reflexes, fundoscopy |
| Oculomotor | III | Eye movements, lift the eyelid, pupil constriction | Eye movements, pupil reflexes |
| Trochlear | IV | Superior oblique | Move eye down and out |
| Trigeminal | V | Sensation to face, movement of jaw muscles | Facial sensation, jaw power, corneal reflex |
| Abducens | VI | Lateral rectus muscle | Move eye laterally |
| Facial | VII | Facial muscle movement, taste (anterior ⅔), salivary and lacrimal glands, stapedius muscle | Facial power |
| Vestibulo-cochlear | VIII | Hearing and balance | Whispering numbers, Weber’s (forehead), Rinne’s (behind ear) |
| Glosso-pharyngeal | IX | Taste (posterior ⅓), parotid gland, sensation of pharynx, nasopharynx, middle ear | Saying ‘Ahh’, swallow, gag reflex |
| Vagus | X | Sensation of pharynx and larynx, movement of palate, pharynx, larynx | Saying ‘Ahh’ (uvula deviates away from defect), cough, swallow, speech, gag reflex |
| Accessory | XI | Movement of sternomastoid and trapezius | Shrug shoulders, turn head |
| Hypoglossal | XII | Movement of tongue | Stick Tongue out (deviates Towards defect), speech |
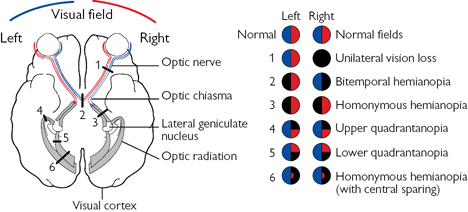
Fig. 3.1 Optic pathways and effect of a lesion on the visual fields at various locations.
Appearance Posture, tremor, muscle wasting, fasciculation, abnormal movements, facial expression and symmetry, neglect.
Hold out hands With palms up and eyes closed; look for drift (pyramidal defect), tremor, or involuntary finger movement (loss of position sense).
Tone Tone at wrist, elbow, knee, and ankle (increased, decreased, clasp knife, cog-wheeling), clonus at the ankle (≥5 beats is abnormal).
Power Isolate each joint with one hand so that only the muscle group you are testing can be used for the movement; compare each side (Table 3.8).
See Table 3.9 for root levels of main limb movements.
Table 3.8 Medical Research Council (MRC) grading of muscle power
| Grade 0 | No movement |
| Grade 1 | Flicker of movement |
| Grade 2 | Movement but not against gravity |
| Grade 3 | Weakness but movement against gravity |
| Grade 4 | Weakness but movement against resistance |
| Grade 5 | Normal power |
© Crown Copyright. The Aids to the Examination of the Peripheral Nervous System (Memorandum No. 45) is licensed under the Open Government Licence 3.0. Used with the permission of the Medical Research Council.
Table 3.9 Root levels of main limb movements
| Joint | Movement | Root | Joint | Movement | Root | |
| Shoulder | Abduction | C5 | Hip | Flexion | L1–2 | |
| Adduction | C5–7 | Adduction | L2–3 | |||
| Elbow | Flexion | C5–6 | Extension | L5–S1 | ||
| Extension | C7 | Knee | Flexion | L5–S1 | ||
| Wrist | Flexion | C7–8 | Extension | L3–4 | ||
| Extension | C7 | Ankle | Dorsiflexion | L4 | ||
| Fingers |
Flexion Extension Abduction |
C8 C7 T1 |
Plantarflexion | S1–2 | ||
| Big toe | Extension | L5 |
Reflexes Deep tendon reflexes comparing each side (Table 3.10)—if absent ask the patient to clench their teeth (reinforcement); plantar reflexes.
Table 3.10 Tendon reflexes
| Grading of tendon reflexes | Root levels of tendon reflexes | ||||
| 0 | Absent | Reflex | Root | Reflex | Root |
| ± | Present with reinforcement | Bicep | C5–6 | Knee | L3–4 |
| + | Reduced | Supinator | C5–6 | Ankle | S1–2 |
| ++ | Normal | Tricep | C7–8 | ||
| +++ | Increased | ||||
| ++++ | Increased with clonus | ||||
Coordination Finger–nose, dysdiadochokinesia, tapping, heel–shin.
Romberg’s This is tested with patient standing with eyes open then closed, positive if more unbalanced with eyes closed; suggests sensory ataxia.
Sensation Pinprick, light touch, vibration, joint position; the spinal dermatomes of the front and back are shown in Fig. 3.2. For spinal tract anatomy and function, see Table 3.11 and Fig. 3.3.
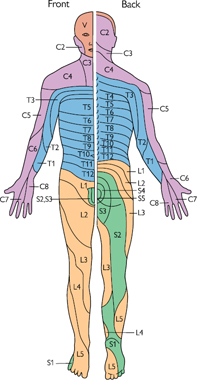
Fig. 3.2 Dermatomes of the front (L) and back (R).
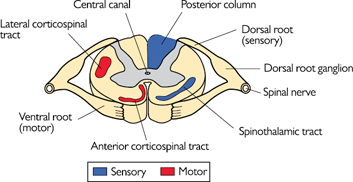
Fig. 3.3 Cross-section of the spinal cord showing spinal tracts.
Table 3.11 Spinal tracts and anatomy
| Tract | Modality | Crosses (decussates) at |
| Lateral corticospinal (pyramidal) | Motor | Medulla |
| Anterior corticospinal | Motor | Level of exit of the cord |
| Posterior columns (dorsal) | Light touch, vibration, position | Medulla |
| Spinothalamic | Hard touch, pain, temperature | Level of entry to the cord |
Nerves of the hand See Table 3.12 and Fig. 3.4.
Table 3.12 Innervation of hand movements
| Movement | Nerve |
| Finger abduction and adduction | Ulnar |
| Thumb opposition and abduction | Median |
| Finger extension | Radial |

Fig. 3.4 Sensation of the hand.
Gait This forms an essentially and highly informative part of the examination of both the central and peripheral nervous systems; see Table 3.13.
Table 3.13 Gait examination
| Gait | Description | Cause |
| Antalgic | Painful gait, limping, short weight-bearing on painful side | Mechanical injury, sciatica |
| Apraxic | Unable to lift legs despite normal power, magnetic steps/stuck to floor | Hydrocephalus, frontal lesions |
| Ataxic | Uncoordinated, wide based, unsteady (as if drunk), worse with eyes shut if sensory | Cerebellar, sensory |
| Festinating | A shuffling gait with accelerating steps | Parkinson’s |
| Hemiparetic | Knee extended, hip circumducts and drags leg; elbow may be flexed up | Hemiplegia, eg CVA |
| Myopathic | Waddling, leaning back, abdomen sticking out | Proximal myopathy |
| Shuffling | Short, shuffled steps, stooped, no arm swing | Parkinson’s |
| Spastic | Restricted knee and hip movements, slow, shuffling, ‘wading through water’ | Pyramidal tract lesion, eg MS |
| Steppage | High steps with foot slapping, ‘foot drop’ | Peripheral neuropathy |
Symptoms Weight loss, weight gain, appetite, sweating, heat/cold intolerance, tremor, weakness, tiredness, dizziness, hirsutism, joint pain/swelling, change in appearance (skin, hair, nails, face, eyes), change in clothes/shoe/hat size, altered sensation, ulcers, visual problems.
Cardiorespiratory features Chest pain, breathlessness, palpitations, sleep apnoea.
GI/urinary features Diarrhoea, constipation, nausea, vomiting, abdominal pain, thirst, polyuria.
Reproductive features Menstrual irregularities, infertility, gynaecomastia, galactorrhoea, impotence.
Psychiatric features Anxiety, mood changes, memory problems.
Eye features Blurred vision, visual field defects, bulging eyes.
Past medical history Hypercholesterolaemia (thyroid function affects lipid levels), thyroid surgery, stroke, heart failure, liver failure, renal artery stenosis, renal failure, adrenal surgery, brain surgery.
Drug history Steroids, diuretics, OCP, HRT, levothyroxine, insulin.
Family history DM, thyroid disease, pituitary tumours.
General inspection Body habitus, ‘buffalo hump’, facial appearance (‘moon face’), striae, bruising, muscle wasting, hyperpigmentation, coarse skin, prominent jaw and brow ridge, goitre, gynaecomastia, hirsutism, acanthosis nigricans, vitiligo, acne, necrobiosis lipoidica, pre-tibial myxoedema.
Hands Temperature, sweating, size, tremor.
Eyes Lid lag, proptosis, exophthalmos, bitemporal hemianopia, cranial nerve III, IV, or VI palsy, fundoscopy.
Neck Goitre, thyroid lumps.
Cardiorespiratory ↑↓ HR, ↑↓ BP, postural hypotension, irregular pulse, peripheral oedema, bibasal crackles (LVF).
Neurological Cranial nerve III/IV/VI palsy, peripheral neuropathy, slow relaxing reflexes, weakness (myopathy).
Other Joints, skin, genitalia, fundoscopy, urine analysis, U+E, early morning cortisol, TFTs, short Synacthen® test ( p. 585), GTT—more specialist tests on advice from an endocrinologist.
p. 585), GTT—more specialist tests on advice from an endocrinologist.
Presenting skin complaint Timing How long present for, sudden or gradual onset, getting better or worse; Location Original site and subsequent sites affected;Symptoms Itch (localized or generalized), pain, burning, bleeding, weeping; Exacerbating factors Dietary components, drugs, sunlight (seasonal variability), pet dander, night-time, water; Relieving factors Emollient cream, topical/systemic steroids.
Current health Anorexia, diarrhoea, fever, headache, fatigue, weight loss, depression, sore throat, joint pain.
Past medical history Previous skin disease, DM, IBD, asthma/atopy, varicose veins, peripheral arterial disease, cardiac problems, endocrine disease, coeliac disease, neurological problems, ulcers, trauma, sarcoid, porphyria, SLE, malignancy, sensitivity of skin to sun exposure, lifelong history of sun exposure or use of sun beds.
Drug history Dermatological agents being used at present and their effects, previous drugs used and their effects, oral and topical steroids, other drugs being taken, immunosuppressants, drug allergies.
Allergy Hayfever, pet dander, dust mite, etc.
Occupational history Current and previous jobs and effect of work upon skin, exposure to chemicals; hobbies and recreational activities.
Family history Anyone else in the family affected; need to differentiate inherited pathology versus infectious pathology.
Travel history Recent foreign travel and relationship of any travel to skin disease—vaccinations/prophylaxis taken for foreign travel.
Function Restricted actions, effect on life, mobility, occupation, dominant hand, hobbies/sports, smoking, social support.
The whole body should be examined in good natural light; patients complaining of a rash on their arm may well have other tell-tale signs elsewhere on the body. Ask patients to fully undress to enable a full skin inspection. Remember the importance of gaining consent and having a chaperone present.
Distribution Solitary lesion, flexor aspects of limbs/trunk, extensor aspects of limbs/trunk, scalp/eyebrows/gutters of nose, sun-exposed sites, tip of nose, helix of ear, webspaces of hands or feet, periumbilical.
Morphology Noting or describing the appearance of the rash using the terms defined in Boxes 3.4–3.7 refines the list of differential diagnoses.
Hair Alopecia (hair loss) may be generalized or localized and scarring/non scarring. Hirsutism (hair in the typical male distribution), hypertrichosis (excessive hair growth).
Nails Clubbing, pitting, ridging, onycholysis, nail loss, thinning of nail plate, discolouration.
 Box 3.4 Non-palpable skin lesions
Box 3.4 Non-palpable skin lesions
Ecchymosis Bruising; discolouration from blood leaking into the skin.
Macule Flat, well-defined area of altered skin pigmentation.
Petechia Non-blanching, pinpoint-sized purple macule.
Purpura Purple lesion resulting from free red blood cells in the skin, non-blanching.
Telangiectasia Abnormal visible dilatation of blood vessels (spider naevi).
 Box 3.5 Palpable skin lesions
Box 3.5 Palpable skin lesions
Nodule Solid, mostly subcutaneous lesion (>0.5cm diameter).
Papule Raised, well-defined lesion (<0.5cm diameter).
Plaque Raised, flat-topped lesion, usually >2cm diameter.
Weal Transient, raised lesion with pink margin.
Urticaria Weals with pale centres and well-defined pink margins.
 Box 3.6 Blisters
Box 3.6 Blisters
Abscess Fluctuant swelling containing pus beneath the epidermis.
Bulla Fluid-filled blister larger than a vesicle (>0.5cm diameter).
Pustule Well-defined pus-filled lesion.
Vesicle Fluid-filled blister (<0.5cm diameter).
 Box 3.7 Skin defects
Box 3.7 Skin defects
Abrasion Scraping off superficial layers of the skin (a graze).
Atrophy Thinning and loss of skin substance.
Crust Dried brownish/yellow exudates.
Erosion Superficial break in the continuity of the epidermis.
Excoriation Linear break in the skin surface (a scratch).
Fissure Crack, often through keratin.
Incisional wound Break to the skin by sharp object.
Laceration Break to the skin caused by blunt trauma/tearing injury.
Lichenification Skin thickening with exaggerated skin markings.
Scale Fragment of dry skin.
Ulcer Loss of epidermis and dermis resulting in scar.
Symptoms Weight loss, anorexia, weakness, lethargy, fatigue, cough, haemoptysis, shortness of breath, postural dizziness, nausea, vomiting, diarrhoea, constipation, PR bleeding, lumps, swelling, pain, fractures, bone pain, polyuria, prostatism, bruising, recurrent epistaxis, haemarthrosis, heavy menstrual loss, recurrent miscarriage, recurrent VTE, fevers, infections, focal neurology.
Past medical history DM, asthma, ↑ BP, IHD, liver disease, jaundice, thyroid problems, anaemia, malignancy (and radiotherapy), epilepsy, gastric or small bowel surgery, malabsorption, chronic disease (eg RA), blood transfusions, splenectomy.
Drug history Chemotherapy (regimen, date of last dose, response, side effects), iron, vitamin B12/folate, aspirin, anticoagulants, vaccinations post-splenectomy, long-term antibiotics, OCP, allergies.
Social history Smoking, alcohol, family support, living circumstances, home help, occupation, previous exposure to dyes/asbestos/coal tar, racial origin, diet (vegan, vegetarian), recreational drug use.
Family history Malignancy, thalassaemia, sickle-cell anaemia, haemophilia, von Willebrand’s disease, pernicious anaemia, spherocytosis, thrombophilia.
General inspection Bruising, pigmentation, rashes and nodules, ulceration, cyanosis, plethora, jaundice, excoriations, racial origin (haemoglobinopathies and thalassaemias).
Hands Nails (koilonychias, pallor, clubbing), palmar crease pallor, arthropathy.
Face Eyes (jaundice, pallor), mouth (gum hypertrophy or bleeding, ulceration, candida, atrophic glossitis, angular stomatitis, gingivitis).
Lymph nodes Cervical, axillary, epitrochlear (elbow), inguinal.
Bones Bony pain in sternum, spine, clavicles, scapulae.
Abdomen Hepatomegaly, splenomegaly, para-aortic nodes, ascites.
Legs Vasculitis, bruising, pigmentation, ulceration, neurological signs.
Other Fundi (haemorrhages, engorged veins, papilloedema), temperature chart, urinalysis.
Lump Size, duration, mobility, pain, nipple discharge/bleeding/inversion, skin changes, previous breast lumps.
Past obs/gynae history Number of pregnancies, age of first pregnancy, breastfeeding, menarche, menopause.
Past medical history DM, asthma, ↑ BP, IHD, clotting problems, liver disease, anaemia, previous malignancy, epilepsy.
FH Breast cancer (male/female), gynae cancer—age of relative at their diagnosis.
DH HRT, COC use.
Ensure a chaperone is present and document their details in the notes (name, job title).
Examine both breasts (normal side first):
Inspection Asymmetry, scars, skin changes, nipple discharge/inversion, skin tethering, erythema, oedema. Ask the patient to tense pectoral wall by putting their hands on hips and tensing. Ask the patient to lean forward. Look for any skin tethering.
Palpation Ask the patient to show you where the lump is, palpate all four quadrants (see Fig. 3.5) and axillary tail, assess any palpable masses.
Lymphadenopathy Axilla, cervical, supraclavicular. The patient must be fully relaxed for you to adequately palpate the axillary nodes. Take the weight of their arm in yours as you palpate.
Other Liver, spine.
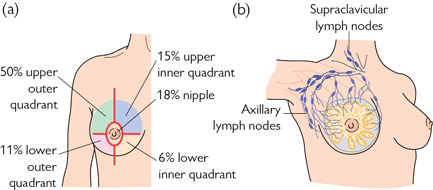
Fig. 3.5 Anatomy of the breast. (a) Quadrants of the breast showing proportion of breast cancer by location. (b) Glands and lymphatics of the right breast.
Symptoms Reduced/impaired vision or visual loss, red eye, discomfort (gritty or FB sensation), pain of the eye or soft tissues around the eye, dry eyes or excessive watering, itch, swelling, photophobia or haloes around lights, floaters or flashing lights, diplopia, discharge.
Past ophthalmic history Glaucoma, myopia, cataracts, previous surgery, glasses/contact lens prescription and last optometry check-up.
Past medical history Numerous systemic diseases can affect the eye, including DM, ↑ BP, vascular disease, RA, SLE, thyroid disease, MS.
Drug history Ophthalmic medications, steroids, anticholinergics, medications for coexisting disease; allergies.
Family history Glaucoma, retinoblastoma.
Social history Ability to self-care, impact eye disease has upon ADLs and home support received/needed.
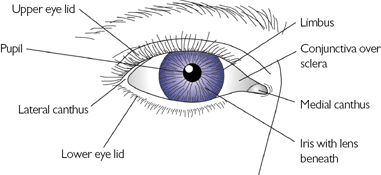
Fig. 3.6 Surface anatomy of the right eye.
Inspection Exophthalmos, proptosis, jaundice, pallor, xanthelasma, eyelids (cysts, inflammation), red eye, corneal arcus, periorbital cellulitis (Fig. 3.6).
Visual acuity This must be tested in all patients:
• Use a Snellen chart at 6m to test visual acuity
• Make sure the patient is using the correct glasses for the test (reading vs distance); if in doubt, use a pin-hole in a piece of card
• If visual acuity is very bad, assess ability to count fingers, awareness of movement (waving hand), or perception of light (pen torch).
Pupillary response and reflexes Check the pupils are equal, reacting to light and accommodation (PERLA) and for a relative afferent papillary defect. Look for the red reflex (absent in dense cataracts). An absent red reflex at the 6wk baby check is a red flag (treat this as a same-day urgent referral).
Visual fields Confrontation testing to identify any visual field loss and to establish if the defect is unilateral or bilateral ( p. 135).
p. 135).
Ocular movements Look for diplopia, loss of conjugate gaze or nystagmus.
• With the ophthalmoscope set on +10 the cornea and anterior chambers can be examined. 1 or 2 drops of fluorescein highlights corneal ulcers, abrasions, and foreign bodies, especially under the blue light
• With the ophthalmoscope set on 0 the user can visualize the retina. It is important to dilate the pupil with 1 or 2 drops of a weak mydriatic (Box 3.8) (eg 0.5% or 1% tropicamide) to allow full visualization of the retina. The risk of causing acute glaucoma with mydriatics is small.
 Box 3.8 Descriptive terms in ophthalmology
Box 3.8 Descriptive terms in ophthalmology
Accommodation Alteration in lens and pupil to focus on near/far objects.
Acuity Ability of the eye to discriminate fine detail.
Anterior chamber Between cornea and iris, containing aqueous.
Aqueous Fluid-like jelly in the anterior chamber of the eye.
Blepharitis Inflammation/infection of eyelids.
Canthus Medial or lateral junction of the upper and lower eyelids.
Chemosis Conjunctival oedema.
Choroid Layer sandwiched between retina and sclera.
Conjunctiva Mucous membrane covering sclera and cornea anteriorly.
Cycloplegia Ciliary muscle paralysis preventing accommodation.
Dacryocystitis Inflammation of the lacrimal sac.
Ectropion Eyelids evert outwards (away from the cornea).
Entropion Eyelids invert towards the cornea (lashes irritate cornea).
Fovea Highly cone-rich area of the macula (yellow-spot).
Fundus Area of the retina visible with the ophthalmoscope.
Hyphaema Blood in the anterior chamber seen as a red fluid level.
Hypopyon Pus in the anterior chamber seen as a white fluid level.
Limbus Border between cornea and sclera.
Macula Rim around the fovea, rich in cone cells.
Miotic Agent resulting in pupillary constriction (eg pilocarpine).
Mydriatic Agent resulting in pupillary dilatation (eg tropicamide).
Optic cup Depression in the centre of the optic disc.
Optic disc Optic nerve head seen as white opacity on fundoscopy.
Posterior chamber Chamber between the iris and lens.
Presbyopia Age-related reduction in near acuity (long-sightedness).
Ptosis Drooping eyelid(s).
Sclera The visible white fibrous layer of the eye.
Scotoma Defect resulting in loss of a specific area of vision.
Strabismus Squint, loss of conjugate gaze.
Tonometer Apparatus for indirectly measuring intraocular pressure.
Vitreous Jelly-like matter which occupies the globe behind the lens.
As well as a good general history, specific symptoms to note include:
Ears Pain, blocked ears, wax, discharge, tinnitus, deafness, unilateral/bilateral features, vertigo, trauma, itching, FBs, noise exposure, occupation.
Nose Blocked nose, watery discharge, sneezing, itching, coughing, change in voice, altered sensation of smell/taste, external deformity/recent trauma, epistaxis, sinusitis; ask about daytime variation in symptom severity, pattern of obstruction, effects on speech and sleep. Are symptoms uni/bilateral?
Throat Dysphagia, pain on swallowing, hoarseness, difficulty opening jaw (trismus), stridor, sleep apnoea/snoring; ask about neck lumps, vomiting, heartburn, waterbrash (acid regurgitation or filling of mouth with saliva).
Ears Inspect The pinna, auditory meatus, tenderness over pinna or mastoid; Otoscopy Examine all four quadrants of the eardrum (see Fig. 3.7) (colour, bulging/retraction, perforation, exudate); Test hearing See following ‘Hearing tests’ text.
Nose Look for Obvious scars, deviations/deformities, tilt the head back and look down each nostril (Fig. 3.8); Rhinoscopy (Administer lidocaine spray first), look for polyps, inflamed turbinates, pus.
Throat Inspect The lips, around and inside the mouth; Examine The tongue and tonsils using a torch and tongue depressor, check palate movements by asking the patient to say ‘ah’ (Fig. 3.9).
Neck Look for Swellings, asymmetry, scars; Ask The patient to swallow, protrude the tongue; Palpate The neck from behind and ask the patient to take a sip of water; Feel for Tracheal deviation, lymphadenopathy, tenderness; Auscultate For a bruit; Examine Any lumps ( pp. 472–473).
pp. 472–473).
Hearing tests ( OHCS10 p. 540)
OHCS10 p. 540)
Whisper Whisper a different number into each ear, standing 30cm away while blocking the other ear. Ask the patient to repeat it in turn.
Rinne’s test Place the tuning fork on the patient’s mastoid bone until it is no longer heard; then place the fork near the external auditory meatus where it is still heard in a normal ear, but not in an ear with conductive deafness. Normally air conduction >bone conduction. Confusingly, a normal result is called Rinne positive.
Weber’s test Place the tuning fork in the middle of the forehead and ask which side the sound is loudest; in sensorineural deafness the sound is loudest in the normal ear, in conductive deafness the sound is loudest in the abnormal ear.
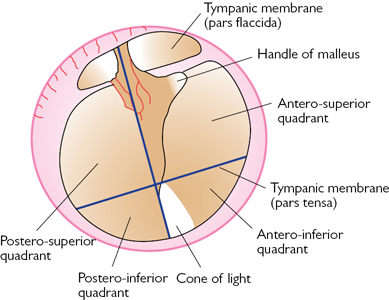
Fig. 3.7 Structures and quadrants of the right tympanic membrane (eardrum) as seen on otoscopy.
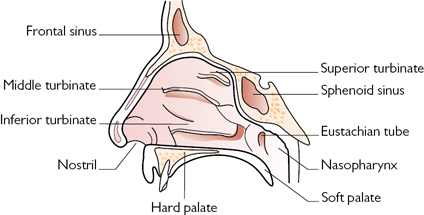
Fig. 3.8 Anatomy of the nose.
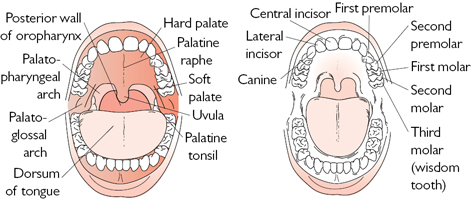
Fig. 3.9 Anatomy of the mouth and oropharynx.
Symptoms Joint pain, swelling, deformity, morning stiffness, instability, sensory changes, back pain, limb pain, muscle/soft tissue aches, cold fingers and toes, dry eyes and mouth, red eyes, systemic symptoms (fatigue, weight loss, tight skin, fever, rash, diarrhoea), injury/trauma (mechanism, timing, change in symptoms since), bleeding tendency.
Past medical history Previous trauma/surgery, recent infections (streptococcal, gonorrhoeal, TB, etc), insect/tick bites, IBD, skin disease (psoriasis), childhood arthritis, haemophilia.
Drug history Previous antiarthritic agents (NSAIDs, steroids (oral/intra-articular), DMARDs) with beneficial/side effects, long-standing steroids, Ca2+ supplements, vitamin D analogues, bisphosphonates, other concurrent medications (antihypertensives etc), allergies.
Activities of daily living Ability to: bathe, dress (and undress), eat, transfer from bed to chair and back, use of the toilet; ?change with symptoms.
Social history Domestic arrangements (who else is at home, location of bathroom in relation to bed), smoking history, drug and alcohol use.
Family history Rheumatoid, gout, osteoarthritis, haemochromatosis, IBD, haemophilia.
Each joint has a specific examination routine, though the underlying principles for each are very similar. Always examine the joint above and below too.
General inspection Overall appearance of the patient and their gait.
Look Close inspection of the joint, comparing left to right if possible.
Feel Assessment of warmth, tenderness, crepitus, effusions, etc.
Move Active (patient moving the joint) and passive (examiner moving joint) movements; stressing joint where appropriate.
Measure Range of movements (in degrees) and degree of joint laxity.
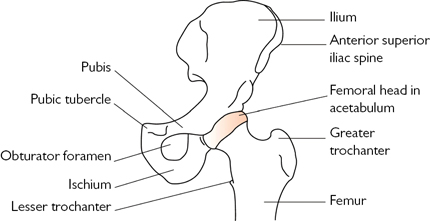
Fig. 3.10 Anatomy of the left hip joint.
Hip (See Fig. 3.10;  OHCS10 p. 682)
OHCS10 p. 682)
Inspection Leg shortening, internal rotation (hip dislocation), external rotation (fractured neck of femur), scars, sinuses, cellulitis, bruising.
Palpation Check bony landmarks (greater trochanter, anterior superior iliac crest) are symmetrical, warmth, crepitus and clicks on movement.
Supine Active and passive range of movement; flexion (straight leg flexion 0–90°, flexion with knee bent 0–135°), abduction (0–50°), adduction, internal (0–45°) and external (0–45°) rotation, fixed flexion deformity (with hand in lumbar lordosis, check the popliteal fossa can touch the couch).
Prone Active and passive range of movement; extension (0–20°).
Gait Trendelenburg gait ( p. 138), walking aids.
p. 138), walking aids.
Other joints Knee (Fig. 3.11) and lower spine/sacroiliac ( p. 151).
p. 151).
Inspection Swelling, erythema, resting position, varus (bow-legs) or valgus (knock-knees) deformity, scars, sinuses, cellulitis, muscle wasting of thigh muscles compared to the other side (especially vastus medialis).
Palpation Temperature, bony landmarks (head of fibula, medial and lateral joint lines, patella), effusion (if large infra-patella sulci will be bulging outwards with a positive patella tap, if small try milking fluid down from thigh and stroking fluid from one side to the other), crepitus, clunks or clicks on movement, patella position, tenderness, and mobility.
Supine Active and passive movement; flexion (0–135°), extension (0°).
Prone Popliteal fossa cysts or aneurysms.
Stressing Cruciates Flex knee to 90°, immobilize the patient’s foot by sitting on it and check the integrity of the anterior and posterior cruciate ligaments by pulling and pushing the lower leg, respectively; Collaterals Flex knee to 30°, fix the thigh with your left hand and test medial collateral (pull lower leg laterally) and then lateral collateral (push lower leg medially).
Gait Limp, walking aids.
Other joints Hip (see previous section) and ankle ( p. 150).
p. 150).
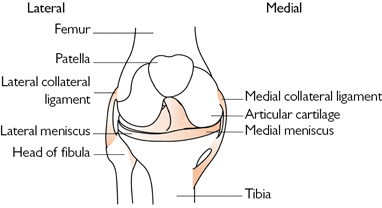
Fig. 3.11 Anatomy of the right knee joint.
Ankle (See Fig. 3.12;  OHCS10 p. 694)
OHCS10 p. 694)
Inspection Swelling, erythema, resting position (consider fracture–dislocation and get immediate senior help if there is marked deviation of the foot following trauma ( pp. 448–451).
pp. 448–451).
Palpation Temperature, bony landmarks (medial and lateral malleolus, tibiotalar joint), crepitus, pain, swelling, effusion, crepitus.
After trauma Palpate proximal fibula head to exclude its fracture, check foot pulses ( p. 130), distal sensation and cap-refill.
p. 130), distal sensation and cap-refill.
Movement Active and passive movement; plantarflexion (0–50°), dorsiflexion (0–15°), inversion (0–30°), eversion (0–15°).
Gait Limp, walking aids, ability to walk 2 paces unaided.
Other joints Knee ( pp. 149–150) and foot (
pp. 149–150) and foot ( p. 150).
p. 150).
 Ottawa ankle rules Ankle X-ray only required in adults and children>6 if any pain in malleolar area and bony tenderness over any of: distal 6cm of posterior edge of tibia or fibula, or tip of medial or lateral malleolus or if unable to bear weight both immediately and in the ED for 4 steps.
Ottawa ankle rules Ankle X-ray only required in adults and children>6 if any pain in malleolar area and bony tenderness over any of: distal 6cm of posterior edge of tibia or fibula, or tip of medial or lateral malleolus or if unable to bear weight both immediately and in the ED for 4 steps.
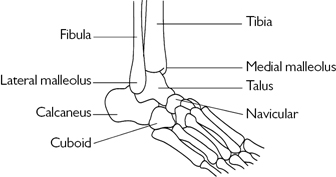
Fig. 3.12 Anatomy of the right ankle joint.
Foot (See Fig. 3.13)
Inspection Swelling, erythema, resting position, high arch, bunions.
Palpation Temperature, pain or crepitus along each metatarsal and phalanx, forefoot bones (navicular, cuboid and medial, intermediate and lateral cuneiform), foot pulses ( p. 130), distal sensation, and cap-refill.
p. 130), distal sensation, and cap-refill.
Movement As for ankle examination but also adduction and abduction across the talonavicular and calcaneocuboid joints.
Gait Limp, walking aids, ability to walk 2 paces unaided.
Other joints Ankle ( p. 150).
p. 150).
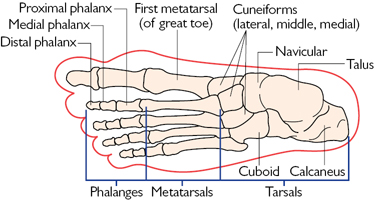
Fig. 3.13 Anatomy of the left foot.
Back (See Fig. 3.14;  OHCS10 p. 672)
OHCS10 p. 672)
Inspection Deformity, loss or exaggeration of thoracic kyphosis or lumbar lordosis, lateral deviation from the midline (scoliosis).
Palpation With patient standing in front, palpate each vertebra for pain; with patient prone palpate each side of pelvis for sacroiliac tenderness.
Movement Active Flexion (touch toes with knees together and legs straight; most people can touch their shins), extension (leaning backwards), lateral bending (lateral flexion) and rotation (best assessed with patient seated so pelvis is fixed); Passive With patient supine, perform straight leg raise by elevating each leg in turn (0–85°).
Measure Schober’s test for lumbar flexion (mark the level of the posterior iliac spine in the midline; make a further two marks, one 5cm below this and one 10cm above this; the distance between these two new marks measured when the patient is standing and then in full flexion—an increase of <5cm suggests limited lumbar flexion) (eg ankylosing spondylitis).
Other joints Hip ( p. 149) and knee (
p. 149) and knee ( p. 149).
p. 149).
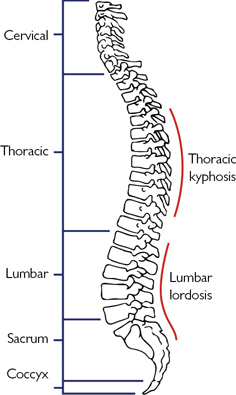
Fig. 3.14 Anatomy of the spine.
The joints in the pelvis are fixed, however the sacroiliac joint can be palpated for tenderness from behind; in a trauma emergency, a senior member of the trauma team may test the pelvis for instability. See Fig. 3.15.
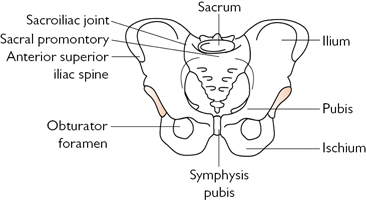
Fig. 3.15 Anatomy of the pelvis.
Shoulder (See Fig. 3.16;  OHCS10 p. 664)
OHCS10 p. 664)
Inspection Swelling, erythema, deformity, resting position, (check from the front, side and back), scars, sinuses, cellulitis, swelling, muscle wasting (deltoid, supraspinatus, infraspinatus).
Palpation Temperature, bony landmarks (acromion, clavicle, spine of scapula, cervical and upper thoracic vertebrae), crepitus, clicks.
Movement Active and passive movement; abduction (0–90° with elbow flexed, 0–180° with elbow extended), adduction, internal (0–90°) and external (0–65°) rotation, flexion (0–180°) and extension (0–65°), passive abduction should be undertaken carefully if painful.
Stressing Impingement test Arm held at 90° abduction and internally rotated, if pain detected it is a positive test; Scarf test Patient’s left hand placed over their right shoulder and vice versa, if pain detected it is a positive test (acromioclavicular joint pathology).
Other joints Elbow ( p. 153) and back (
p. 153) and back ( p. 151).
p. 151).
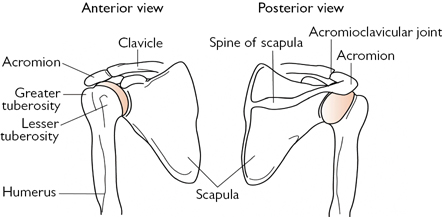
Fig. 3.16 Anatomy of the right shoulder joint.
Elbow (See Fig. 3.17;  OHCS10 p. 668)
OHCS10 p. 668)
Inspection Swelling, erythema, inflamed bursae, rheumatoid nodules or psoriatic plaques over the olecranon, scars.
Palpation Temperature, bony landmarks (medial and lateral epicondyles, olecranon), crepitus, clicks, instability.
Movement Active and passive movement; flexion (0–150°) and extension (0°); pronation, supination.
Other joints Shoulder (Fig. 3.16) and wrist (Fig. 3.18).
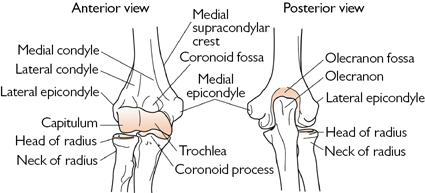
Fig. 3.17 Anatomy of the right elbow.
Wrist (See Fig. 3.18;  OHCS10 p. 670)
OHCS10 p. 670)
Inspection Swelling, erythema, deformity (eg Colles’ fracture), features of rheumatoid disease ( p. 468), scars.
p. 468), scars.
Palpation Temperature, bony landmarks (styloid process of radius, head and styloid process of ulna), scaphoid (base of the anatomical snuff-box).
Movement Active and passive movement; flexion (0–75°), extension (0–75°), radial (0–20°), ulnar deviation (0–20°), pronation, supination.
Other joints Elbow ( p. 153) and hand (
p. 153) and hand ( p. 154).
p. 154).
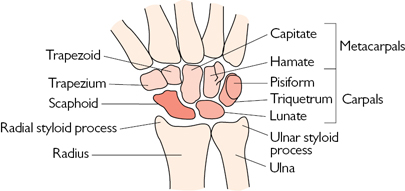
Fig. 3.18 Anatomy of the wrist and hand.
Hand (See Fig. 3.19;  OHCS10 p. 670)
OHCS10 p. 670)
Inspection Erythema, swelling, breaks to the skin, features of rheumatoid disease ( p. 468) or osteoarthritis (
p. 468) or osteoarthritis ( p. 468), deformity, dislocation, muscle wasting, nail pitting.
p. 468), deformity, dislocation, muscle wasting, nail pitting.
Palpation Temperature, palpate each metacarpal and phalanx for pain or crepitus, distal cap-refill and sensation.
Movement Active and passive movement; flexion and extension of every MTPJ, PIPJ, and DIPJ, abduction and adduction of every MTPJ, opposition and circumduction of the thumb MTPJ; ask the patient to: hold a pencil and write, pick up a mug, undo a button, oppose their thumb and little finger (check strength of this against your own); check strength of extension and flexion following penetrating or lacerating trauma to identify tendon injury.
Stressing Collateral ligaments of the digits following trauma or dislocation by attempting to deviate the phalanges medially or laterally.
Other joints Wrist ( p. 153) and inspect the elbow.
p. 153) and inspect the elbow.
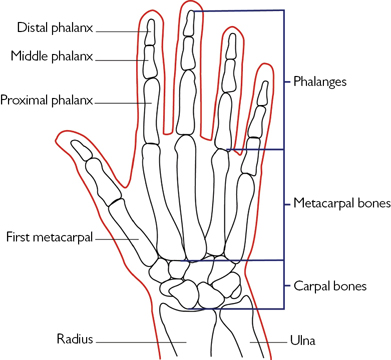
Fig. 3.19 Anatomy of the hand, thumb and fingers.
Symptoms Polyuria, anuria, prostatism (urgency, hesitancy, poor stream, terminal dribble, nocturia, straining), haematuria, dysuria, oedema, renal colic, incontinence, malaise, lethargy, N+V, anorexia, weight loss, itching, passing stones in the urine, incontinence, impotence, infertility, bone pain, genital discharge, genital/perineal lesion, scrotal pain, dyspareunia (pain on intercourse), FB (vaginal, urethral, anal), anal/perianal problems.
Past medical history DM, ↑ BP, recurrent UTIs, renal/ureteric stones, myeloma, known renal impairment/failure, previous vesicoureteric reflux, gout, immunosuppression (steroids, HIV), neurological disease, long-term urinary catheter, STIs, spinal cord pathology; Male Tight foreskin, recurrent balanitis, testicular pain/swelling; Female Number of children, mode of delivery and any complications, last cervical smear and result.
Drug history Nephrotoxics (including NSAIDs, ACEi, aminoglycosides), bladder neck relaxants, infertility or impotence drugs, antiandrogens; allergies.
Social history Foreign travel, ability to cope with ADLs, sex abroad, illicit drug use (smoke, oral, IV).
• Last sexual intercourse (LSI)—date, gender, type of intercourse (vaginal, anal, oral), protected, relationship of partner (casual, long term), problems or symptoms in partner, high-risk area, sex worker
• Repeat the above for all partners in the last 3mth
• All men should also be asked if they have ever had sex with another man in the past as this affects risk and types of STI to consider.
Occupational history Past and present jobs, exposure to dyes.
Family history Polycystic kidney disease, DM, ↑ BP.
Examination (lying flat, supine) (See Fig. 3.20)
General inspection Mental state, RR (?Kussmaul breathing of metabolic acidosis), hiccups, pallor, hydration (dehydrated: sunken eyes, dry lips/tongue; fluid-overload: peripheral oedema, pulmonary oedema).
Hands Leuconychia, brown nails, pale nail beds.
Arms Bruising (purpura), pigmentation, scratch marks, fistula, BP (lying and standing).
Face Eyes (anaemia, jaundice), mouth (dehydration, ulcers, fetor), rash.
Neck JVP.
Abdomen Inspect (distended bladder, scars, transplanted kidney, dialysis port), palpate (ballot kidneys, bladder, liver, spleen, lymph nodes), percuss (enlarged bladder, ascites), auscultate (renal artery bruits), PR for prostate.
Rectum Size, surface, consistency and symmetry of prostate in men, faecal impaction (will worsen urinary retention).
Back Oedema, loin tenderness on percussion.
Chest CVS and RS examination (pericarditis, heart failure, fluid overload).
Legs Oedema, bruising, pigmentation, scratch marks, neuropathy, proximal weakness (myopathy), altered reflexes, muscle wasting.
Urinalysis Glucose, blood, protein, nitrites, leucocytes.
Other Fundoscopy (DM and ↑ BP changes), blood glucose, weight.
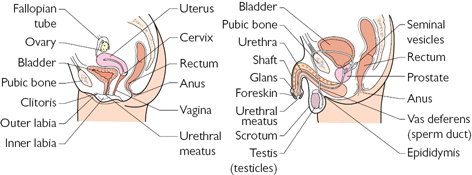
Fig. 3.20 Anatomy of the female (L) and male (R) urogenital systems.
Inspection Look for any ulceration (including retracting foreskin and checking the glans), warts, scars, or sinuses, urethral discharge, tight foreskin (phimosis) or retracted foreskin which is stuck leaving the glans exposed (paraphimosis). Inspect the scrotum for skin changes or oedema and, while the patient is standing, the lie of the testes (the left testis usually hangs lower than the right and both testes lie longitudinally—a high testis with a transverse lie may indicate torsion, though a torted testis may also appear normal).
Palpate each testis in turn between the fingers and the thumb feeling for texture, tenderness, nodules, and to compare left to right. An absent testis may be maldescended and trapped in the inguinal canal. Examine epididymis and follow it up superiorly to the spermatic cord and up into the inguinal ring. Palpate inguinal lymph nodes or maldescended testis.
Examination of female genitalia See  pp. 158–159.
pp. 158–159.
Menstrual history Date of last period, length of menstrual cycle (regular or irregular), length of period, associated pain/symptoms (Box 3.9), age when periods started/stopped; bleeding/discharge severity of periods (number of pads/tampons, clots, flooding), bleeding between periods, after intercourse (vaginal, anal, oral), or after menopause, rectal/urinary bleeding, effect on lifestyle, other vaginal discharge (colour, consistency and smell).
Sexual history Pain on superficial or deep penetration (dyspareunia), type of intercourse (vaginal, anal, oral), use of contraception, intercourse in foreign countries, previous sexually transmitted infections; contraception current and previous types, problems/benefits.
Cervical smear Date of last test and result, previous results and any treatment (repeat smears, colposcopy clinic, laser ablation).
Past gynae history Previous problems and/or operations (where and name of surgeon), breast or thyroid problems, use of HRT, prolapse.
Past obstetric history Number of pregnancies, number of births, type of delivery, complications, subfertility ( p. 160 for obstetric history).
p. 160 for obstetric history).
Past medical history Clotting problems, thyroid problems, anaemia, malignancy.
Urinary problems Incontinence (on laughing/coughing/exercising or spontaneous), dysuria, urgency, frequency, haematuria, if symptomatic ask about fluid intake, leg weakness, faecal incontinence, back pain and previous spinal problems/surgery, effect on lifestyle.
Other Vaginal lumps, weight loss, other concerns.
Always have a chaperone who can reassure the patient and also guard the door. Document name and role in notes. Ask friends and family members to leave, unless the patient wants them to stay (this also provides an opportunity to ask questions which the patient may not have answered fully with others present). As with any examination it is essential to keep the patient informed about what you are going to do. Start with the patient lying flat on her back with arms by her sides. It is important the patient is relaxed and that you have a good examination lamp. See Fig. 3.21.
Abdominal Assess for scars, striae, hernias, body hair distribution, everted umbilicus, distension, tenderness including loins (± guarding, rebound), masses, organomegaly, percuss (masses, shifting dullness).
Ask the patient to move her feet apart, bend her knees, and let her legs flop outwards. Have a strong light source directed at the vulva and gloves on both hands.
Vulval Look for rashes, ulcers, warts, lumps or other lesions; spread the labia majora using your non-dominant thumb and index finger and look for lesions, lumps, discharge (urethral/vaginal), bleeding; ask the patient to push down (look for prolapse) and cough.
Vaginal Insert a well-lubricated index and middle finger (dominant hand) into the vagina and feel for the cervix, noting the size, shape, consistency, and whether it is mobile or tender. Feel above, below, and to the sides (adnexae) for masses or tenderness. Finally, palpate the uterus by placing your other hand above the pubic symphysis and press down with the fingers at the cervix; pressing up feel for uterine position (anteverted/retroverted), size, shape, consistency, mobility, and tenderness. Inspect the finger afterwards for blood or discharge.
Cusco’s speculum While the patient is in the same position insert a well lubricated and warmed speculum into the vagina. Look at the cervix. If you are unable to visualize the cervix, ask the patient to tilt her pelvis forward by placing her fists under her bottom. Look for ulceration, bleeding, cysts or other lesions and the cervical os. If required take swabs and/or a cervical smear.
Consider Sims’ speculum (for examining prolapses), rectal examination.
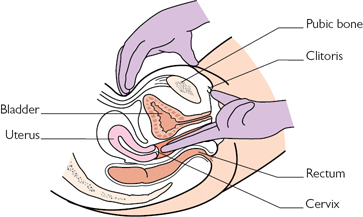
Fig. 3.21 Examination of the female reproductive system.
 Box 3.9 Descriptive terms in gynaecology
Box 3.9 Descriptive terms in gynaecology
Anatomy Adnexae The areas lateral to the cervix where the ovaries are located.
Introitus The entrance to the vagina.
Abnormal bleeding
Climacteric Phase of irregular periods and associated symptoms prior to menopause.
Intermenstrual Bleeding between periods.
Menopause The end of a woman’s menstrual cycles.
Menorrhagia Excessive blood loss during menstruation (>80mL/cycle).
Oligomenorrhoea Infrequent menstruation, >42d menstrual cycle.
Postcoital Bleeding after sexual intercourse.
Postmenopausal Bleeding >6mth after the menopause.
Primary amenorrhoea Failure to start menstruating by 16yr.
Secondary amenorrhoea Absence of menstruation for >6mth after menstruation has started and not due to pregnancy.
Pain
Dysmenorrhoea Pain associated with menstruation.
Dyspareunia Pain associated with sexual intercourse, can be superficial (eg vulval or entrance to vagina) or deep (only on deep penetration).
Current pregnancy Estimated due date (EDD), gestation, last menstrual period (LMP), method of conception, scan results, site of placenta, rhesus status, concerns, attitude to pregnancy. Current symptoms Bleeding, other vaginal discharge, headache, visual disturbance, dysuria, urinary frequency or urgency, constipation, vomiting, GORD.
Previous pregnancies Number of pregnancies (gravidity), number of deliveries ≥24/40wk (parity), miscarriages, terminations (reason, gestation, method), stillbirths, complications: vomiting, anaemia, bleeding, group B strep, BP, proteinuria, gestational DM, poor foetal growth, admission.
Delivery history Method of delivery and reason (vaginal, ventouse, forceps, elective/emergency Caesarean), gestation, birthweight, sex, complications (fever, prolonged rupture of membranes, CTG trace), postnatal baby problems (feeding, infection, jaundice), admission to SCBU/NNU, outcome (how is the child now), postnatal maternal problems (pain, fever, bleeding, depression).
Past gynae history Previous problems, operations, STIs.
Past medical history DVT, PE, DM, admissions, psychiatric problems.
Family history DM, ↑ BP, pre-eclampsia, congenital abnormalities, DVT, PE, multiple pregnancies.
Social history Support from family/partner, type of housing, employment, financial problems, smoking, alcohol, substance abuse.
Table 3.14 Antenatal care (uncomplicated pregnancies)
| Gestation (wk) | Standard antenatal care: purpose of each visit* |
| Booking | FBC, G+S, red cell antibodies, rubella, syphilis, hepatitis B, HIV serology, sickle-cell disease, thalassaemia, BMI, BP, urine dipstick and culture |
| 11–14 | USS for gestational assessment and nuchal screening (combined test) |
| 16 | Urine, BP, serum screening (for Down’s and neural tube defects; triple/quadruple test) |
| 20 | USS for foetal anomalies and growth and placental position |
| 28 | Fundal height, BP, urine, FBC, red cell antibodies, anti-D if rhesus –ve. Offer pertussis vaccine |
| 25†, 31† | Fundal height, BP, urine |
| 34 | Fundal height, BP, urine, anti-D if rhesus –ve |
| 36, 38, 40† | Foetal position, fundal height, BP, urine, offer ECV if breech at 36/40 |
| 41 | Discuss induction, foetal position, fundal height, BP, urine, offer membrane sweep |
*For further information, see  www.nice.org.uk/guidance/cg62
www.nice.org.uk/guidance/cg62
†For the first pregnancy only.
Foetal heart Audible from 12wk using a Doppler ultrasound and 24wk using a Pinard stethoscope; it is faster than the mother’s (110–160bpm).
Weight Plot mother’s weight and BMI ( p. 618) at the booking visit (Table 3.14).
p. 618) at the booking visit (Table 3.14).
Inspection Striae, linea nigra (line of pigmentation from the pubic symphysis to the navel that darkens during the 1st trimester), venous distension, scars, oedema.
Fundal height The fundus (top of the uterus) is palpable from about 12wk gestation; it should be measured from the top of the pubic symphysis to the top of the fundus with a tape measure. Between 16 and 36wk the fundal height in centimetres should be the same as the gestation ±2cm, eg 23–27cm at 25wk. Fundal height is unreliable after 36wk. See Fig. 3.22.
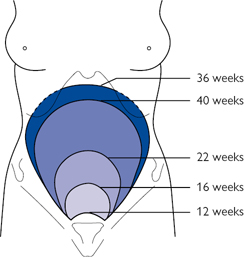
Fig. 3.22 Location of the fundus as pregnancy progresses.
Foetal lie After 32wk it is possible to assess the position of the foetus by palpating across the abdomen for the foetal head:
Presentation Palpation after 32wk can also assess the presentation though this is liable to change until about 36wk. By palpating both ends of the foetus the position of the head can be determined:
Engagement This is assessed by palpating the base of the uterus above the pubic symphysis between two hands to assess how much of the presenting part is palpable. If only the top 1/5th of the presenting part is palpable the foetus has ‘engaged’.
Blood pressure This must be monitored regularly to assess for pregnancy-induced ↑BP; consider urine dipstick and fundoscopy too.
Urine dipstick For protein (pre-eclampsia) and glucose (DM).
USS Lie, presentation, and engagement can be confirmed on USS.
Are you safe? Sit so the patient is not between you and the door, remove all potential weapons, be familiar with the panic alarm, check notes/ask staff about previous violence, have a low threshold for a chaperone.
Set the scene Make sure you are both comfortable, ensure privacy and that you will not be disturbed, eg give the bleep to someone else, have tissues available, emphasize confidentiality.
Basics Full name, age, marital status, occupation, who were they referred by, current status under Mental Health Act.
Past psychiatric history Previous psychiatric diagnoses, in-patient/day patient/out-patient care, do they have a community psychiatric nurse (CPN), previous deliberate self-harm (DSH), previous treatments and effects, ever been admitted under the Mental Health Act.
Medication history Current and previous medications, effects, did they/do they take it, allergies/reactions, alternative/herbal remedies.
• Childhood Pregnancy, birth, development ( p. 166), associated memories, names of schools attended, reason if changed schools, types of school (mainstream/specialist), age of leaving school, qualifications
p. 166), associated memories, names of schools attended, reason if changed schools, types of school (mainstream/specialist), age of leaving school, qualifications
• Employment loss of jobs, which did they enjoy, why did they change, ask about unemployment and why
• Relationships Current relationship(s) and sexual orientation, list of major relationships and reasons for ending, any children and who they live with and relationship to patient.
Forensic Contact with police, convictions or charges, sentences, outstanding charges.
Personality How would they describe their personality now and before the illness? How would others describe it?
Social history Occupation and duration of employment/unemployment, where they live, concerns over money, friends and relationships, hobbies.
Drug and alcohol Smoking, alcohol, illicit drugs.
Family history Family tree with parents and siblings, ages, occupations, relationships, illnesses.
Psychiatrists examine the mind through talking to the patient (Boxes 3.10 and 3.11). Much of the information is gleaned while taking the history and should be organized under the following headings. This is called the Mental State Examination (MSE).
Appearance Racial origin, age, dress, make-up, hairstyle, jewellery, tattoos, cleanliness, neglect, physical condition.
Behaviour Appropriateness, posture, movement (excessive, slow, exaggerated), gestures, tics, facial expression, eye contact, anxiety, suspiciousness, rapport, abnormal movements, aggression, distraction, concentration.
Mood The patient’s subjective assessment of their mood.
Affect Interviewer’s objective assessment of mood and appropriateness of patient’s response, eg flat, reactive, blunted.
Speech form Accent, volume, rate, tone, quantity, hesitations, stuttering; Content Associations (derailment, changing between subjects), puns.
Thought form Rate, flow (eg blocked), connection (eg flight of ideas, derailment); Content Beliefs about self, beliefs about others, thought insertion/withdrawal/control/broadcast, beliefs about the world/future, delusions, overvalued ideas, obsessions, compulsions, ruminations, rituals, phobias.
Perception Illusions, hallucinations (visual, auditory, tactile, olfactory), unusual experiences, depersonalization, derealization.
Cognition This can be tested formally using the Mini-Mental State Examination (MMSE) on  p. 377; often the Abbreviated Mental Test Score (AMTS) is used instead (
p. 377; often the Abbreviated Mental Test Score (AMTS) is used instead ( p. 375).
p. 375).
Risk Thoughts of deliberate self-harm, suicide, harming others, plans, acquiring equipment, writing notes, previous suicide attempts. Can ‘protective factors’ be identified? Document these if so. Consider risk both to self and to others.
Insight Awareness of illness and need for treatment.
 Box 3.10 Defining ‘mental illness’
Box 3.10 Defining ‘mental illness’
What constitutes abnormal behaviour to the extent of constituting a mental illness can be a controversial and difficult area, subject to allegations of cultural and political bias and even suggestions of undue pharmaceutical industry influence. Two main classification systems are accepted:
• The Diagnostic and Statistical Manual of Mental Disorders, produced by the American Psychiatric Association; the 5th edition (2013) is currently in use: DSM-5
• The International Classification of Diseases, published by the World Health Organization (covers all of medicine); 10th edition (1992) is currently in use: ICD-10. ICD-11 is due to be published (2018).
Each classification carries a slightly different emphasis and diagnostic criteria; in rare instances, this results in an abnormal condition recognized in one, but not the other.
 Box 3.11 Common terms in psychiatry
Box 3.11 Common terms in psychiatry
Affect Pattern of observable behaviours which reflects emotions experienced.
Anxiety Feeling of apprehension caused by anticipation of perceived danger.
Approved clinician A doctor entitled to recommend compulsory admission for treatment under the 2007 Mental Health Act.
Cognition The process of thinking, reasoning, and remembering.
Compulsion Repetitive behaviours in response to obsessions; often to relieve the distress caused by them, eg washing hands.
Delirium Acute onset of disordered cognition with attentional deficits; typically involves changes in arousal and may be associated with hallucinations.
Delusion A fixed, false belief that goes against available evidence and is not explained by the person’s religious or cultural background.
Dementia Global organic deterioration of cognition with preserved consciousness.
Depersonalization Altered sense of self as if detached or outside the body.
Derealization Altered sense of reality as if detached from surroundings.
Emotion A complex state of feeling that results in physical and psychological changes that influence thought and behaviour.
Euphoria Pathologically exaggerated feeling of well-being.
Flight of ideas Rapid switching of topics where the thread of connection can be determined (eg sound, content).
Formal admission Admission under a section of the Mental Health Act.
Hallucination A false sensory perception in absence of a real stimulus, eg hearing voices; feature of psychosis if the subject lacks recognition of the false nature.
Illusion False interpretation of a real external stimulus, eg seeing a shadow and thinking it is a person.
Informal admission Voluntary admission as a psychiatric in-patient.
Insight The ability of a person to recognize their mental illness.
Mania Abnormal elevation of mood with grandiose ideas, increased energy and agitation, pressure of speech, distractibility, and pleasure seeking.
Mood Emotional state that colours the person’s perception of the world.
Obsession Recurrent unwanted thoughts or images, eg my hands are dirty.
Passivity Delusional belief in external control of a person’s actions or thoughts.
Personality disorder Enduring and inflexible behavioural patterns that markedly differ to societal norms.
Phobia Persistent, irrational fear of an activity, object, or situation, leading to the desire to avoid the feared stimulus; beyond voluntary control.
Psychosis Disordered thinking and perception without insight, often accompanied by delusions or hallucinations.
Ruminations A compulsion to consider an idea or phrase.
Stereotype Repeated pattern of movement or speech without any goal.
Thought insertion Delusional belief by a person that an external agency is putting thoughts into his/her mind (a passivity phenomenon).
The baby check is a key component of life in paediatrics. All neonates should be examined within 72h of birth with the aim of:
Preparation Prior to the examination you should check the maternal notes for: significant maternal illness, gestation at birth, birthweight, type of delivery, problems at delivery (meconium, premature rupture of membranes (PROM), group B strep, low APGAR scores: appearance, pulse, grimace, activity, respiration).
Introduction Introduce yourself to the mother/parents, offer congratulations and explanation. Has the baby passed faeces and urine? Feeding well? Any parental concerns? Ask them to undress the baby to the nappy.
 Settled baby Consider doing the following first as they are difficult if the baby is crying: listening to the heart and feeling the apex beat, count RR, feeling the femoral pulse, and looking in the eyes.
Settled baby Consider doing the following first as they are difficult if the baby is crying: listening to the heart and feeling the apex beat, count RR, feeling the femoral pulse, and looking in the eyes.
 Crying baby Try getting the baby to suck (pacifier, breast, bottle, parent’s little finger, your little finger); if this fails, swaddle the baby and ask the parents to give the baby a feed then return in 30min.
Crying baby Try getting the baby to suck (pacifier, breast, bottle, parent’s little finger, your little finger); if this fails, swaddle the baby and ask the parents to give the baby a feed then return in 30min.
Overall Take a few moments just to look; is the baby: jaundiced, blue, dysmorphic, moving normally, breathing normally?
Neuro Tone (Degree of head support, spontaneous symmetrical limb movements), Moro reflex is not routinely performed.
Head Anterior and posterior fontanelle (bulging, sunken), head circumference, eyes red reflex (red flag if absent), face (dysmorphic?), ear shape and position (tags, pits, top of insertion of pinna should be at the level of the eyes), palate (with your little finger), suck reflex.
Hands/arms Fingers (number, shape, colour), palms (single crease in 60% of Down’s and 1% of non-Down’s), symmetrical arm movement.
Chest Respiratory rate (RR >60 is abnormal), listen to the heart, apex beat, gently feel the clavicles for fractures.
Abdo Palpate (to exclude hepatomegaly, splenomegaly, masses), descended testes, patent anus, enlarged clitoris, femoral pulses.
Hips/feet Anterior hip creases (symmetrical?), Barlow test (flex hip to 90°, press posteriorly, feel for a click/clunk if the hip dislocates), Ortolani test (after Barlow’s abduct the hips one at a time while pressing on the greater trochanter with your middle finger, feel for a click/clunk as the hip relocates), note repetition of these tests can cause hip instability, ankles (talipes, correctable or not), toes (number, shape, colour).
Turn baby over Spine (straight), sacrum (lumps, dimples, hair tufts, skin defects), buttocks (blue spots—make a note), posterior hip creases.
Plot In the red book: weight, head circumference, examination.
Basics Age in days (until 1mth), weeks (until 2mth), months (until 2yr), or years, gender, who gave the history, who was present.
Current state Feeding and drinking, weight gain, wetting nappies/passing urine, fever, bowels, crying, runny nose, cough, breathing problems, pulling ears, drawing up legs, rash.
Birth Pregnancy problems and medications, gestation at birth (37–42/40 is normal), type of delivery (NVD, induced, ventouse, forceps, if LSCS ask why), resuscitation, special care, birthweight, PROM, group B strep (GBS), meconium, maternal pyrexia during labour, vitamin K (IM or oral), feeding (breast, bottle, type of milk).
Immunizations Check the child is up to date with vaccinations (Table 3.15); jabs will be postponed if the child is unwell or febrile beforehand and children often get a slight fever for <24h afterwards.
Table 3.15 UK vaccination schedule (from August 2017)
| Birth | May get tuberculosis (BCG) and/or hepatitis B if at risk |
| 2mth | Diphtheria, tetanus, pertussis, polio and Haemophilus influenzae type b (DTaP/IPV/Hib), hepatitis B, pneumococcal disease (PCV), Rotavirus, meningococcal group B (MenB) |
| 3mth | Diphtheria, tetanus, pertussis, polio and Haemophilus influenzae type b (DTaP/IPV/Hib), hepatitis B, and rotavirus |
| 4mth | Diphtheria, tetanus, pertussis, polio and Haemophilus influenzae type b (DTaP/IPV/Hib), hepatitis B, pneumococcal disease (PCV) and MenB |
| 12–13mth | Measles, mumps, rubella (MMR), Haemophilus influenzae type B (Hib), pneumococcal (PCV), meningococcal group C disease (MenC), MenB |
| 2yr to 8yr | Influenza |
| 3yr4mth–5yr | Diphtheria, tetanus, pertussis and polio (DTaP/IPV), MMR |
| 12–13yr | Human papilloma virus (girls only) |
| 14yr | Tetanus, diphtheria, and polio (Td/IPV) and meningococcal groups A, C, W, and Y disease |
Source: data from  https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/633693/Complete_imm_schedule_2017.pdf. Contains public sector information licensed under the Open Government Licence v3.0.
https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/633693/Complete_imm_schedule_2017.pdf. Contains public sector information licensed under the Open Government Licence v3.0.
Development See Table 3.16 and ask about school performance.
Social history Who the child lives with, parental responsibility, parental jobs, smoking, nursery/school attendance, type of school (mainstream, special needs), academic ability, sporting ability, friends, enjoyment of school, foreign travel.
Family history Family tree with parents and siblings, consanguinity if relevant, illnesses in the family, how are their parents and siblings at the moment, asthma, eczema, hayfever, DM, epilepsy, other diseases specific to presenting complaint.
Much of the examination can be performed by simply observing the child; this usually has the advantage of limiting tears. Approach younger children gently while they are sitting on a parent’s knee and feeling secure. Examination is much the same as for adult patients, but include the following:
► If unwell ABC and resuscitate,  pp. 238–240. Always records obs—for normal ranges by age, see Box 6.11 (
pp. 238–240. Always records obs—for normal ranges by age, see Box 6.11 ( p. 240).
p. 240).
Chaperone Ask a nurse to accompany you if a child of either sex is over 10yr, if there is a child protection issue, or whenever you feel it is necessary.
Hydration Fontanelle, capillary-refill (≤2s), warm peripheries, mucous membranes, tears if crying, skin turgor, sunken eyes, tachycardia, lethargy.
Respiratory Grunting, head bobbing, nasal flaring, tracheal tug, cervical lymphadenopathy, recession (sternal, subcostal, intercostal).
Cardiovascular Cyanosis (check mouth), clubbing, mottled skin, murmurs may radiate to the back, femoral pulses (coarctation), radiofemoral delay, dextrocardia, hepatomegaly (heart failure).
Abdominal Check the external genitalia if young, relevant, or boys with abdominal pain (torsion); never do a PR (though seniors might).
Neurological AVPU (Alert, responds to Voice, responds to Pain, Unresponsive), fontanelles, tone, reflexes (including Moro and grasp reflex if young), head circumference (growth chart), development (Table 3.16).
Table 3.16 Key stages in childhood development
| Age | Gross motor | Fine motor | Speech | Social |
| 6wk | Holds head in line | Eyes follow 90° | Startles to sound | Smiles |
| 3mth | Lifts head up | Eyes follow 180° | Coos | Laughs |
| 6mth | Sits unsupported | Transfers objects | Babbles | Objects to mouth |
| 9mth | Pulls to stand | Finger–thumb grip | ‘Mama, dada’ | Waves goodbye |
| 12mth | Walks unsupported | Points | First words | Finger foods |
| 18mth | Running | Scribbles | Asks for ‘wants’ | Feeds alone |
| 2yr | Lumps | Copies line | 2–3-word sentences | Uses fork |
| 3yr | Uses tricycle | Copies circle | Name and age | Dry by day |
| 4yr | Hops | Copies cross | Counts to 10 | Dry by night |
ENT Always check the ears and throat if there is a suspicion of infection; describe the colour, appearance, and if an effusion or pus is present.
Weight, height These should be plotted on a sex-specific growth chart.
Head circumference This is especially important in infants and those with neurological disease; the measurement should be plotted on a sex-specific chart.