The quintessential con artist of the nineteenth century was the snake oil peddler who sold sham elixirs to vulnerable patients—and it was the specter of his parasitical existence that ultimately spawned the Food and Drug Administration.1 The FDA's essential oversight of certain elements of the health-care industry was just the beginning of regulatory influence, however. The tentacles of governmental control now stretch throughout America's health-care system in a deep, tangled, and pervasive way—to the point that health care isn't private enterprise in the sense that automobiles, semiconductors, and strategy consulting are private. Indeed, much of the current public discourse on health-care reform focuses on whether private industry can be expected to fix the current system—or whether the government will have to become even more deeply involved. In many other economically advanced countries, of course, the government is the health-care system.
In this chapter we will catalog the ways in which government policies influence health care for good and ill, and we'll recommend regulatory changes that are essential to successfully disrupting the system. To do this, we have reviewed the history of government intervention in a range of industries whose products or services have been considered "public goods"—where the public interest has been broader than what market mechanisms might be expected to serve autonomously. These include education, ground and air transportation, financial services, telecommunications, and health care. All policies can't be lumped together and treated alike, of course. But it seems that in general terms, the intent of schemes to influence and regulate these industries in the public interest evolves through three stages:
1. Subsidizing the foundation of the industry
2. Stabilizing and strengthening the companies involved, ensuring fair and equal access to their products and services, and assuring that their products are safe and effective
3. Encouraging competition to reduce prices2
We've organized most of this chapter around these three stages, because government's interaction with the health-care industry can also be grouped into these categories. Much of its energies to date have been expended in the second of these stages. In discussing those regulations, we'll show how the pattern that typified other industries is now at work in health care: regulations whose initial purpose was to protect the patient ultimately get used to protect the provider. After modeling these, we'll draw on our studies to suggest how private-sector innovators can cause policy-makers to begin focusing on the third stage—and help them distinguish the types of regulatory reforms that can predictably lead to lower costs versus those that will predictably backfire.3 Finally, we'll close the chapter by assessing whether adopting a government-led single-payer system will help or hinder the sorts of reforms we need in our system—and we'll apply those insights to the situation in other nations, where national health ministries already provide most health care.
Governments sometimes conclude that a desirable industry can not emerge on its own—so they subsidize or in other ways facilitate the investments required to cause that industry to coalesce. For example, under the Morrill Act of 1862, the federal government gave land to states that agreed to create "land grant" colleges; and under separate legislation that same year, it began giving land and cash to railroads that were willing to lay track to span the continent.4 The 1925 Kelly Act initiated airmail service, which subsidized the establishment of the scheduled passenger airline industry. The Federal Home Loan Act of 1932, the creation of the Federal Housing Administration in 1934, and the Federal National Mortgage Association in 1936, were meant to help an affordable housing industry grow.5 In 1957 the government did the same for the trucking industry, by building the Interstate Highway System.
Often, government subsidies of the cost of launching industries take the form of research and development spending. By illustration, funding of military cargo jet aircraft by the Department of Defense essentially paid for the design of the first commercial jet airliner, the Boeing 707. The research that enabled the commercial nuclear power industry was funded through military budgets—as was development of the Internet. Indirectly, through its regulation of pricing, the government "taxed" AT&T's customers to fund Bell Laboratories, whose inventions in microelectronics and telecommunications proved to be an extraordinary blessing to mankind.6
The National Institutes of Health (NIH) have funded nearly all of the basic and much of the applied research that underpins modern medicine. Much of the knowledge that took many infectious diseases into precision medicine a generation earlier, and many of the insights in molecular medicine that are driving more diseases toward precision medicine today, have been developed in our leading research universities with NIH funding.
While everything can always be improved, we propose one enhancement to the methods used to allocate NIH grants. The NIH currently uses a single-blind referee system for evaluating grant proposals. When a researcher submits a proposal requesting that a project be funded by the NIH, the NIH sends the proposal to experts in the field in question. The reviewers evaluate the proposal's potential based upon their knowledge of the field, and will recommend that it be funded, that the project be reframed and resubmitted for further consideration, or that the grant simply not be made. The reviewers' names are typically not known to the researcher who submitted the proposal. The logic behind the single-blind method is that the reviewers need to know of researchers' track records in the field. But personal relationships and politics need to be kept from the decision-making process, ensuring that each decision is made purely on the merits of the science involved.
However, the inadvertent result of this system of sending proposals for review by the scientists with the deepest expertise in the specific topic is that it has "siloized" the structure of scientific work into ever narrower disciplines and subdisciplines—in our research universities and especially in our medical schools. The referees, as the experts in their particular subdiscipline, tend to view proposals positively if they extend knowledge in their known discipline even deeper. But if the proposal intends to push knowledge in a different direction—crossing the boundary into a different scientific domain—the proposal tends not to be viewed as positively. This is in part because most reviewers aren't comfortable vouching for the scientific potential of something beyond the boundaries of their own domain, and in part because it doesn't deepen knowledge in the direction in which their work and reputation are building.7
This shaping of the enterprise of science into ever more narrow fields generally facilitates the advancement of what the great historian of science, Thomas Kuhn, calls "normal science"—the incremental block-by-block construction of bodies of understanding upon the foundation of a paradigm.8 But this specialization of knowledge and perspective flies in the face of overwhelming evidence that breakthrough insights nearly always come at new, unconventional intersections of scientific or technical disciplines. Breakthroughs rarely emerge from within individual disciplines. Rather, we get new perspectives when researchers from other fields examine old problems from their different, and novel, points of view.9 Problems that have long vexed the experts are often resolved when someone in another field sees something that the first experts simply couldn't see or didn't think to look for.10
Typically, our instinct is to look to our own discipline as the credible source for solutions—and that is the right instinct when the issue is normal science. But it is the wrong instinct when breakthroughs are needed.11 This is also why we proposed in Chapter 10 that the breakthrough structures we need in medical student education might not emerge from within our medical schools, but from corporate medical schools that might be more willing and capable of adopting principles that have already been discovered at Toyota.
There is no doubt that we need breakthroughs in health care. This means the NIH needs to create different tracks for funding, and different methods for evaluating research projects that stand astride multiple disciplines or propose tackling problems in one field through methods that have been developed in another. Projects like these can be accurately assessed and prioritized, but only by different and appropriate means.
Once an industry has been launched, governments quite often then intervene in the name of the public good to stabilize it. The intent and effect of many of these "stabilizing" regulations is to limit competition in order to help companies become strong enough to endure. The purpose of other interventions is to ensure that everyone in the population that politicians believe ought to be served by that industry is in fact served. And many regulations, of course, are written to assure that the quality of products is adequate and won't harm consumers.
As an example, 44 years after the Bell Telephone Company was founded, the Willis-Graham Act of 1921 declared telephony to be a "natural monopoly." There wasn't anything "natural" about this monopoly at all: hundreds of local phone companies and equipment manufacturers populated the industry in the early 1900s.12 But getting their mutually incompatible systems to work together had been a hellacious technological task. Willis-Graham allowed AT&T to acquire its competitors and suppliers to become completely vertically integrated—to make and manage every element of its system, from soup to nuts. Given the technological interdependencies across various pieces of equipment at the time, this integration was needed to give the company the scale and scope to make telephony reliable on a national scale.
The regulation of the securities and banking industries during the Great Depression had a similar intent. By setting prices, defining disclosure rules, regulating balance sheet leverage, requiring approval for new banks and securities firms, and mandating deposit insurance, the government limited the potential for fraud and risk-taking behavior that could damage consumers. The Interstate Commerce Commission and the Civil Aeronautics Board regulated pricing and route-by-route entry into the trucking and airline industries to avoid ruinous competition, and to assure that rural and urban consumers alike could access these services at fair prices. The Federal Aviation Administration assures passenger safety. The National Highway Traffic Safety Administration regulations that govern the crashworthiness of automobiles are likewise intended to assure our protection.
The intent of most regulation to date in the health-care industry has likewise been to stabilize and assure. The avenues of influence that the government has used to stabilize the industry and assure the availability and quality of health-care services are not dissimilar to what the financial, trucking, and airline regulators did to stabilize and assure quality and availability in their industries. The government regulates prices, licenses and certifies the people and equipment that provide the services, and determines who can and cannot enter the industry and who they must serve. In the following pages we'll describe these avenues of influence.
We stated in Chapter 7 that the formulas and methods that the Centers for Medicare and Medicaid Services (CMS) use to set the prices of products and services constitute the most pervasive and potent regulatory controls in health care. The price at which CMS decides it will reimburse is an "anchor rate" of sorts, because most private insurers follow the lead of CMS in price-setting. This, then, determines the profitability of every product and service in health care—creating incentives for providers to sell more of what is most profitable and less of what isn't.
In a largely unintended way, the reimbursement policies of some large government payers even serve to prop price levels up by discouraging discounting in the rest of the health-care industry. For example, most states' Medicaid programs by statute pay drug companies a fixed percentage of the average wholesale price of each drug—a price that drug companies are free to set. Medicaid's reimbursement policies stipulate that at the end of each quarter, the prices paid for all of the products and services purchased must be rewritten to be as low or lower than the lowest prices offered to any other customers. This is accomplished through federally-controlled price ceilings and mandatory rebates from drug manufacturers.13
This seems like a smart deal for the government—it is the largest customer, and it ought to be guaranteed lowest prices. But consider, by illustration, its unintended, second-order effect. Suppose a chain pharmacy, which we'll call "MediQuik," negotiates a discount from a supplier of diabetes test strips, which we'll call "GluCorrect." Imagine that instead of paying GluCorrect 75 cents per strip (which would be marked up to a retail price of about a dollar per strip), MediQuik negotiates a 50-cent price, intending to pass those savings on to its customers in order to win more of the diabetes care business. But because government payers account for about 40 percent of the volume of this product, GluCorrect, in agreeing to this new discounted price, would have to cut its price to 50 cents not just for the volume it sells through MediQuik, but essentially and retrospectively cut the price to the same level on all of its government-paid business for that product—which amounts to at least 40 percent of its entire sales of those products that year. At the end of the quarter, MediQuik would be required to send to the government a check to refund the excess price that it originally charged—25 cents per strip, multiplied by the total number of strips sold to it that year.14
While this policy on the surface seems to benefit the government—assuring it of the best prices in the market—the effect is to make any discounting by the providers of drugs, devices, and services extremely expensive. Executives in every industry wish that their counterparts in competing companies had the "discipline" to act independently to maintain prices at profitable levels. The policies of Medicaid and other payers actually instill this pricing discipline in the health-care industry.15
Another class of policies for stabilization and assurance defines who does and does not have access to particular types of care. In the United States, for example, medical expenses are the leading cause of personal bankruptcy.16 Yet hospitals cannot deny life-saving treatment to the uninsured or those who cannot pay for care. America, as a result, actually already has universal health insurance, in a sense—though the present system forces people to wait until they have no other recourse but to seek care in an extraordinarily expensive hospital emergency department. Not surprisingly, many of the bills for these services go unpaid; as a result, the regulation of guaranteed access to lifesaving services imposes a much heavier burden on hospitals in lower income areas, such as rural communities and inner cities, than on those in more affluent communities.17
The bad debt that accumulates from uncompensated care isn't relieved by the Internal Revenue System, however, but through a hidden tax collected through private insurance companies from their clients. Charges to those who are insured or who can pay must be high enough to cover the cost of uncompensated care. Ultimately, the impact of this regulation that funnels the neediest and sickest into our costliest solution shops is to significantly increase costs (and human suffering) through its inadvertent second-order effects. It's ironic. America's system, which popular opinion holds excludes the uninsured and the poor from health care, actually guarantees access—albeit access that is costly to the system. In contrast, government systems that are widely viewed as granting universal access often are good at providing access to primary care and other basic services but quite stringently ration more expensive care in an exclusionary way.
There is also substantial evidence that we've framed the problem of access incorrectly. It is the marked inconvenience of finding affordable basic care that makes it inaccessible to the uninsured poor, not simply its cost. Care is often free for those who can't afford it, but only accessible to those who have the patience and fortitude to endure the indignity and inconvenience of finding it. As an illustration, MassHealth, the Medicaid program in Massachusetts, provides comprehensive health coverage for those in need. In March 2002, under pressure to reduce spending, MassHealth reduced the amount it would reimburse dentists for a range of basic dental services—and the already small pool of dentists willing to accept MassHealth patients declined even further by 15 percent. Additional free care was still available in community health centers funded by the state through a different pool of funds, but these were much less convenient to access for many of the poor. Within three years of the reimbursement cuts, 100,000 fewer MassHealth patients received dental services that were reimbursed by MassHealth.18
One option that addresses this issue is to eliminate the unfunded obligation to provide free care. This is not to say that the sick and needy should be turned away—far from it. Rather, our system of charity care needs to ensure they have equal right to convenient, quality care that doesn't threaten them with bankruptcy or force them to wait until they're much sicker before they are allowed succor. One solution is to obligate the uninsured poor to purchase high-deductible insurance on a subsidized basis. They must also be equipped with health savings accounts that can be subsidized, when necessary. But this isn't enough. Regulators must promote—and pay for, when necessary—retail clinics staffed with nurse practitioners and dental technicians, in order to stabilize and assure that a system of convenient care is available and accessible to the uninsured poor, not just to the wealthy and insured. If we uphold our moral and societal obligations to cover the cost of health care for the uninsured poor but do not simultaneously make it affordable and accessible, we have in fact provided "coverage without care."19
In addition to its power to set prices and control who has access to the goods and services of these industries, the government uses a third avenue to bring stability and assurance to health care—by approving, certifying, and licensing, and thereby determining which people and institutions can and cannot compete to provide different types of care.
The most visible form of permitting and certification is the authority of the Food and Drug Administration to approve the sale of drugs and devices. As we noted in Chapter 8, clinical trials for new drugs have traditionally been designed as a "final examination" of sorts, to see whether a drug adequately helped a sufficient portion of patients while harming them a minimal amount. If the result of a trial was that an inadequate minority of patients responded to the drug, then the drug often was not approved. The new perspective that molecular biology has given us is that when only a portion of patients respond to a therapy, it should be taken as a signal that those patients in the trial must have at least two different diseases and/or there is a genetic variation between subgroups that causes them to respond differently to the therapy. Clinical trials in the future therefore need to be managed not as one-off tests, but as research trials whose purpose is to assist the researchers in defining and diagnosing diseases more precisely.
In addition, clinical trials historically have been organized around diseases that were defined and diagnosed by observable physical symptoms in particular organs or locations in the body. As we explained in Chapter 2, it turns out that these categorizations sometimes run orthogonally to the true nature of the diseases being treated. The organization of clinical trials needs to adapt to changing and increasingly precise definitions of disease, so it is the efficacy of the drug in treating the underlying cause that is being tested, and not simply the extent to which the drug ameliorates a symptom that happens to be correlated.
In our opinion, the FDA has made significant progress already in designing new "fast track" processes for evaluating drugs, such as its Critical Path Initiative. These newer research programs and trials tend to incorporate biomarkers as end points, pursue drug-diagnostic codevelopment, enrich patient populations by first diagnosing them as precisely as possible, utilize bioinformatics, and retain specimens for future testing and analysis should the understanding of disease change.20 There remains, of course, much to do.
The FAA doesn't just certify new aircraft as being safe to fly after they've been designed and built. They certify pilots as having been thoroughly trained to operate them, and they certify facilities as being equipped to handle aircraft of various types. In the same way, governments don't just certify drugs and devices. They also certify people and places.
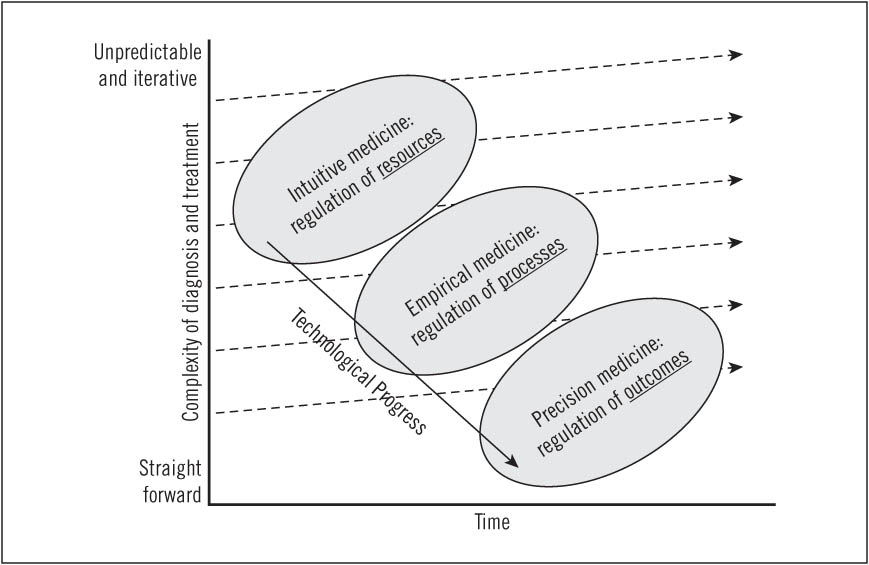
Because the nature of the technology available affects the skill required to use it, the fact that scientific progress pushes care from intuitive toward precision medicine demands different regulatory emphases over time, as illustrated in Figure 11.1. When a disease can only be treated through intuitive medicine, the inputs or resources used in the caregiving process are the critical points of assurance control. In this situation it is primarily the training and qualifications of the physicians that must be assured.
Over time, however, greater understanding and predictability arise from the cycles of qualified physicians repeatedly working together to deliver outcomes in solution shops. Processes coalesce that embody the best of what has been learned about how to approach various diseases. A lot of know-how gets embodied in equipment and drugs. These mechanisms draw treatment into empirical medicine—where we can't guarantee the result, but can assert the probability of achieving a desired outcome if a particular therapeutic process is followed, using particular drugs or devices. When this happens, the emphasis of regulation needs to shift from a focus on the inputs and resources used, to a focus on the process used—to ensure that the best demonstrated practices are employed. This is what happens when an association of medical specialists or a hospital system proclaims new guidelines and standards of care for a certain condition, or an insurer declares that it will only reimburse if a specific procedure is followed. These are all regulations that govern process.
FIGURE 11.1 Matching regulations with the changing nature of medical practice
Often, the training of the professionals who provide care within these processes does not need to be as extensive as was formerly required in the regime of intuitive medicine. As regulators shift focus to process, therefore, they must simultaneously revisit their regulation of resources—because often caregivers with less training can do the job perfectly well.
When improved understanding has further shifted care into precision medicine, the focus of regulation needs to evolve again, toward a focus on outcomes, rather than on resources or processes. And because outcomes are predictable at this stage, regulators should focus on ensuring transparency and reporting relevant data from all providers. Regulating adherence to previously established standards for inputs and processes becomes less relevant, because competitive success typically compels adherence to these standards.
Many who have written about health-care reform urge in an undifferentiated way for transparency—for disclosure of outcomes data for individual hospitals and physicians. We have concluded that a key reason why such transparency hasn't emerged is that what these reformers have urged is not just overly simplistic: it is an impossible apples and oranges problem. For care of diseases in the realm of intuitive medicine that is provided in solution shops, the outcome is a diagnosis. But when care is provided in value-adding process clinics for diseases in precision medicine, the outcome is a cure. It is the latter in which outcomes data must be transparent and comparable. It comes as no surprise to us then that many physicians oppose the idea of pay-for-performance initiatives, often stating that their incentives are tied to processes and decisions beyond their control. This opposition arises not because they are opposed to quality care, but because a pay-for-performance system that attempts to encourage specific outcomes can only be effective for care that is fully in the realm of precision medicine.21
Regulatory insistence on compliance to inputs and process standards eventually can become a hindrance to further innovation if a pioneering company could potentially figure out a way to deliver superior outcomes by deviating from convention. A great example of an appropriate response to changing technology of this sort is in the FAA regulation that there must be an FAA-certified pilot and copilot in the cockpit for each commercial flight. The avionics on these aircraft and in control centers are now so sophisticated and comprehensive that much of the navigation, ground-air-ground communication, and piloting work is performed by computers, not pilots.22 These advances are sophisticated and reliable enough that just a single pilot is needed at the controls. In the new microjets produced by Eclipse Aviation, Spectrum Aeronautical, and others for the emerging air taxi industry, the FAA no longer requires a copilot. There isn't even room for one.
Those who resist regulatory reforms such as these in health care have frequently told us, "Yeah, but it's lives that are at stake in health care." To which we reply, "You're right, and it is lives that are at stake on these planes too." Indeed, as the aviation regulations have shifted in emphasis to equipment, processes, and outcomes, the safety record of the technology is proving better than that of pilots.23
We are not calling for wholesale deregulation of the health-care industry. Indeed, history has shown that when competitive markets can't create an industry that functions for the public good, regulation for stability and assurance has always been critical at a particular stage.
The dark side of this necessity for regulation, however, is that rules survive long after the public need for stability and assurance have been satisfied by technological progress. While the original intent of permitting and certification is a genuine concern for the patient, almost always the rules then come to be used to protect the economic interests of the providers—still invoked, of course, in the name of the patient, or of the passenger, or of the "public good." If regulators do not evolve the focus of their rules as science and technology progress, they will trap care in high-cost business models whose outcomes are less predictable, and are actually not as good as those that might otherwise be developed by innovators. Regulators must keep their vigil and adapt the focus and nature of the regulations to evolutions in medical practices, processes, and technology—but they rarely do.
For example, the Civil Aeronautics Board effectively "stabilized" the airline industry from the 1930s through 1977 by limiting the number and type of airlines that could fly on any given route, and by setting the fares they could charge. The Securities and Exchange Commission similarly "stabilized" the Wall Street brokerage firms as they emerged from the chaos of the Great Depression, by allowing the New York Stock Exchange to set at a profitable level the fees its member firms would charge to execute a trade. When Southwest Airlines and Charles Schwab sought approval in the 1970s to compete with the established firms in their respective industries through discount pricing, the lawyers for the established firms mounted eloquent arguments for why, in the name of the public good, the discounters should not be allowed to enter the market. Fortunately, they were allowed.
In a similar way, health-care providers regularly fall back on stability and assurance regulations to block competition. For example, in 2003, at the urging of the hospital industry, Congress imposed a nationwide moratorium on the construction of specialty hospitals such as heart and orthopedic hospitals. The argument was that in the event that a patient undergoing a cardiac bypass procedure suffered a stroke, for example, you needed to have within the hospital the ability to treat stroke, not just to repair hearts or replace hips. For the good of the patient, they claimed, all care needed to be delivered in general hospitals. It is interesting that the general hospitals have never militated to ban specialty psychiatric hospitals, even though, surely, patients in psychiatric hospitals on occasion have heart attacks, strokes, and hypoglycemia. Certainly, for the good of the patients, those with mental disorders also should be cared for in general hospitals. The reason for general hospitals' schizophrenic concern about heart and orthopedic hospitals but not psychiatric ones, of course, is that the procedures siphoned off by the former two are highly profitable, and psychiatric patients typically are far less profitable (and usually unprofitable). The actual reason for the 2003 ban was that these specialty hospitals could perform some of the general hospitals' most profitable procedures, but at much lower cost.24
As another example, out of concern for patient safety, many states still prohibit nurse practitioners from writing prescriptions without the direct supervision of a doctor, even for precisely diagnosable, rules-based disorders like strep throat. This effectively prevents retail clinics from competing against physicians' practices in those states—even though in the other states the patients are doing just fine, at less than half the cost. Worse still, patients who may not be able to afford the rates of physicians' practices or who do not have access to a primary care physician but might be able to afford a visit to MinuteClinic get shut out altogether—in the name of patient safety.25
Because assurance-oriented regulations initially limit rights of practice to those with the required expertise, a paternalistic culture often emerges in regulated industries that is built around the belief—validated at the outset—that people can't be expected to care for their own needs. This was the defense raised against discount and on-line brokerage firms. It is the fabric of the regulatory culture in legal services that to date has stymied disruption of that industry. And it pervades the defenses of the status quo in health care as well. In the realms of empirical and precision medicine people can actually competently assume responsibility for a growing portion of their care. This is a key reason for our call in Chapter 5 that patients with diseases in the "Chronic Quadrangle" be financially affected by their adherence to therapy. This is a critical change that regulators must allow. These diseases are decidedly in an empirical, rather than intuitive mode. We are no longer in the realm where paternalism is appropriate.
Many of the activities of certification, licensing, and permitting in health care are actually administered by trade or professional associations in the private sector, as well as by universities and various nonprofit organizations. The actions of these entities are given teeth when the ability to get paid for something—by Medicare or by private insurers—is tied to being credentialed. Among the best known and most influential agencies are the Joint Commission on Accreditation of Hospitals, which certifies hospitals for compliance with federal regulations and whose accreditation is required for Medicare reimbursement; the National Board of Medical Examiners, which tests the capabilities of medical school graduates and whose assessment is required for medical licensure; and the members of the American Board of Medical Specialties, which evaluates physicians in areas of specialty care and whose certification is necessary for physicians to be hired or credentialed by most hospital systems.
When Medicare or insurance companies follow a policy of paying only for services provided by licensed professionals, they can block disruptive innovations. There are many examples where technology has progressed to the point that procedures can be performed in clinics instead of hospitals, or by nurse practitioners instead of doctors, resulting in outcomes that are as good or better. Yet the rule of reimbursing only for services provided by certified caregivers makes it impossible or unprofitable to hand off care to lower-cost disruptive providers, because changes in certification typically lag many years behind changes in technology.
When governments are democratic rather than autocratic, the entities that profit from the status quo typically have many more means of influencing elected and appointed officials to preserve the present system, compared to the more meager resources of disruptive entrants who petition to shift the focus of obsolete regulations away from resources like professionals and institutions and toward processes and outcomes instead. The $450 million the health-care industry spent in lobbying efforts with the government in 2007, in fact, exceeded spending to influence government policy by the finance, insurance and real estate, telecommunications and electronics, and energy and natural resources industries.26
The result of this massive imbalance of resources on the side of those resisting reform, based upon our studies, is that the reformers almost always lose head-on battles to deregulate what is regulated. Would-be disruptors who have directly petitioned the authorities to change regulation are left waiting on the sidelines for the regulation to one day change by fiat, or have simply abandoned their disruptive ideas. On the other hand, those disruptors that successfully dismantled the regulations that stood in their way succeeded by circumventing the regulation—by innovating in a disruptive market that was beyond the regulators' reach or was peripheral to their vision. Regulations ultimately change in reaction to the innovators' success in those markets—they rarely change to enable disruptive success.
For example, until 1980 Regulation Q profoundly shaped the structure and nature of competition in the consumer banking industry. It dictated that banks could not pay interest on checking accounts and capped the interest rates commercial banks and savings and loan associations could pay on savings deposits at 5.25 and 5.5 percent, respectively.27 These regulations were broken when Merrill Lynch offered a cash management account that allowed customers to write checks against a "money market fund," and whose assets were short-term government securities that yielded more attractive interest rates. Fidelity quickly joined Merrill Lynch in offering interest-bearing checking accounts. Because they weren't banks and operated only on the periphery of bank regulators' vision, Merrill Lynch and Fidelity didn't attract the scrutiny that banks drew when they sought permission to pay interest on checking accounts. The disruptive Merrill Lynch and Fidelity products drew such enormous volumes of assets out of the conventional banks that ultimately the Federal Reserve had to change its regulations in response. Aggressive banks and consumer groups had lobbied for years to change these regulations from within the dominant value network, and they failed. It was the creation of a new disruptive value network, and the pulling of customers into it, that brought regulatory change.
As another example, until 1978 the Civil Aeronautics Board regulated the routes that airlines could fly and the prices they could charge. In 1971, Southwest Airlines began flying short routes within the state of Texas at very low prices, competing as a new-market disruptor to the major airlines by serving people who previously couldn't afford to travel by airplane. Because Southwest did not offer interstate travel, its routes and fares could not be regulated by the CAB. Furthermore, Southwest steered clear of the main DFW airport in Dallas, electing instead to fly in and out of the smaller, older, Love Field—where there were no established competitors. Southwest gradually started a few cross-border flights to adjacent states, but it minimized the opposition of established carriers by shuttling between smaller airports that weren't the bread and butter of the major airlines. By 1978 it became clear that the safety of discount airlines was just as good as—and the pricing for consumers significantly better than—what major airlines had been offering. So the CAB deregulated the airline industry. But once again, deregulation did not come from a direct appeal to the regulators.28
Note that in the earlier example of the virtual copilot in the minijets of Spectrum Aeronautical and Eclipse Aviation, even though similar avionics had long ago automated control on major aircraft, the mainstream pilots' union would have fought elimination of a required copilot to the death. But by going where they aren't—where the alternative is no pilots flying at all—the pilots and their passengers are delighted to see the regulation changed. Little by little, as Eclipse and Spectrum move up-market into bigger planes and grow from selling hundreds to thousands every year, the need for a copilot will be obviated.
And we see the same pattern in those few instances where the focus of health-care regulation has changed: you have to start where they aren't.
Consider this illustration. Despite the fact that it is preventable, tooth decay, the chronic disease that leads to most tooth loss, is present in over a quarter of all children between ages two and five, over half of all children between ages 12 and 15, and 90 percent of all adults over age 40.29 Tooth decay plagues 5 billion people worldwide, disproportionately affecting low-income households. It accounts for 10 percent of all health costs in industrialized nations.30 There must be an opportunity for disruptive innovation to address this global public health concern.
There is. But for the good of the patients, it's having a hard time getting to those who need it. Consider what's happening in Massachusetts as an illustration of how, when attacked directly, regulations get morphed to defend the professionals, not the patients.
Dental hygienists have been promoting legislation to allow specially trained hygienists to clean teeth and apply fluoride without direct supervision by a dentist.31 The Massachusetts Dental Society has vociferously opposed this, citing concerns for public safety. But the MDS has proposed an alternative—the creation of a different class of specially trained dental assistants who could clean teeth and even place fillings under direct supervision by a dentist.32 The Massachusetts Dental Hygienists' Association (MDHA) then voiced its opposition, concerned about how the introduction of dental assistants might "squeeze out more qualified registered dental hygienists."33 All evidence points to a long battle in Massachusetts over these direct disruptive attacks. Organizations and professions will predictably fight to protect their livelihood.
Yet where fewer people are looking, dentistry is being disrupted. In 2000, to address the lack of dental services in rural areas,34 the Alaska Native Tribal Health Consortium (ANTHC) persuaded the state to create a new type of dental provider called a dental health aide therapist (DHAT).35 The model had been implemented in New Zealand over 90 years ago with demonstrable success, and similar programs existed in 42 other countries, including Canada and the United Kingdom.36 In fact, the first Alaskan students to train in dental therapy went to the School of Dentistry at the University of Otago in New Zealand, since no such program was available in the United States. DHATs train for two years, instead of the minimum of four that dentists train, and at $60,000 per year, they make about one-third the salary of a typical dentist.
Since 2003, DHATs in rural Alaska have been providing services such as cleaning, drilling, filling, and extraction with only indirect supervision via periodic case reviews. Today, 10 DHATs serve 20 villages in Alaska—places that previously received dental care only one or two weeks each year from a visiting dentist. In 2005 a quality assessment by a professor of dentistry from the University of Washington School of Dentistry reported:
During my four-day site visit to the dental clinics at Bethel, Buckland, and Shungnak, I evaluated the clinical performance of the four dental therapists who have been providing primary care for Alaska Natives since the beginning of 2005. In every respect their performance met the standard of care I had established. Their basic training and subsequent preceptorships have produced competent providers. Each is equipped not only to provide essential preventive services but simple treatments involving irreversible dental procedures such as fillings and extractions. Their patient management skills surpass the standard of care. They know the limits of their scope of practice and at no time demonstrated any willingness to exceed them. On multiple occasions they demonstrated their ability to recognize and avoid clinical situations that might pose a threat to patient safety. My firsthand observations convince me that statements by dentists and dental societies suggesting that dental therapists cannot be trained to provide competent and safe primary care for Alaska Natives are overstated.37
The American Dental Association and Alaska Dental Society have predictably opposed allowing DHATs to provide unsupervised dental services, requesting an injunction from the Alaska Superior Court in 2006 to block their encroachment.38 The judge ruled in favor of the ANTHC, stating that "a significant number of the enumerated health objectives . . . would continue to go unmet if the Alaska State Board of Examiners were placed in charge of dental health for Alaska Natives located in rural areas."39 We expect that DHATs will soon be allowed in rural areas in the lower 48 states of America, where the population is not being well served by dentists. Eventually, the disruption will arrive in Massachusetts. But the shortest distance between two points is not a straight line.40
Over the past decade, there has been significant growth in the use of teleradiology, beginning with off-hours, or "nighthawk," radiology services, which allow hospitals to transmit digital images to anywhere in the world for interpretation. Even if the patient arrives in the dead of night, the radiographs can be interpreted within minutes by a radiologist at another center in the United States, or even in Australia, India, or France. This implementation of teleradiology has enabled hospitals to maintain reliable and efficient services around-the-clock and to meet the exploding demand for CT scans (growing at 14 percent annually) and other imaging studies, despite much slower growth in the number of radiologists.41 The largest of these off-hours radiology providers, Idaho-based NightHawk Radiology Services, serves 26 percent of all U.S. hospitals.42
Teleradiology services began by targeting nonconsumption—radiologists gladly allowed the new services to manage their less desirable time slots on nights and weekends. However, once they began to offer daytime services, there was predictable opposition from radiologists. Leaders of the American College of Radiology raised concerns about ensuring the quality, accuracy, and accountability of personnel based in another state or country.43 There were also concerns about communication problems when the radiologist and referring physician were so far apart. In 2002 an attempt by Massachusetts General Hospital to partner with a nonprofit company in India to shift some of its radiology work to Indian doctors resulted in hate mail and ultimate failure for the venture.44 Legislators got involved, claiming that patient privacy was at risk, and placed restrictions on transferring patient data abroad.
In response to this reinforcement of the intuition-era regulatory focus on the doctor's qualifications, most teleradiology services, even if located abroad, have been compelled to employ only U.S.-trained and -licensed radiologists, who must also be credentialed at the hospitals for which they perform services.45 Furthermore, their interpretations are often considered only preliminary until reviewed, or "overread" by a U.S.-based radiologist. The Joint Commission on Accreditation of Health Care Organizations also weighed in to require teleradiology services to meet licensing and accreditation standards that have long been in place for hospital-based solution shops of radiologists.46 The result: a typical NightHawk radiologist has licenses in 38 states and is credentialed at over 400 hospitals. The company employs 35 to 40 people simply to manage all of this administrative overhead—and yet can still provide these services at lower cost than most of its customers can when they choose to perform them in-house.47
However, a funny thing is happening at the edge of this stalemate. A growing segment of work is no longer dependent on a radiologist's expert eye and clinical experience to interpret shadowy anatomical structures and link them to patients' clinical histories and physical symptoms.48 "Functional" radiology, involving dynamic in-motion studies and molecular tracers rather than still pictures, and "quantitative" radiology—a related discipline based on measurements and scoring algorithms—have significantly enhanced the ability of nonradiologist physicians to elucidate physiologic abnormalities.49 Starting with basic technologies like ultrasound and fluoroscopy, these machines automate image acquisition and analysis, embedding into algorithms some of the diagnostic skill that used to reside only in the intuition of radiologists. These machines also require less space, shielding, and power, so they can be integrated into the offices of cardiologists and orthopedic surgeons working in value-adding process clinics.50
The door was opened, in typical disruptive fashion, to nonradiologist physicians to begin performing and interpreting some of the simpler studies for themselves, and they are referring fewer and fewer patients to the radiology solution shops of the local hospital. So while radiologists were trying to figure out how to prevent the loss of work overseas, other physicians were beginning to perform some of that work for themselves within their very same offices and communities.
An important insight from this end run around regulation is that the cardiologists and orthopedic surgeons didn't need to seek regulatory approval. Radiologists make their money on a fee-for-service basis by interpreting images ordered by other physicians. Teleradiologists have been attempting a low-end disruption into this business—using a lower-cost business model to capture segments of the market—but still on a fee-for-service basis. The cardiologists and orthopedists working in capitation or fee-for-outcome models didn't need to worry about regulatory approval because they don't make their money interpreting images—they make it by repairing hearts and bones. Radiology simply helps them repair more hearts and joints better and faster.51
We suspect that after a few years of cardiologists, orthopedic surgeons, and others using these computer-assisted imaging technologies with results comparable to those of radiologists, regulations will eventually change to focus on processes and outcomes, rather than on the credentials of the physicians. Already, in fact, the initial fears about the safety of outsourcing radiology services to off-hours providers now seem unfounded.52 The time will even come when point-of-care doctors won't need a radiologist as a copilot.53
Lao-Tzu framed the deregulation strategy of "Starting where they aren't" better than we have when he wrote, "Water is fluid, soft, and yielding. But water will wear away rock, which is rigid and cannot yield. As a rule, whatever is fluid, soft, and yielding will overcome whatever is rigid and hard. This is another paradox: What is soft is strong."54
When stability and quality have become assured, governments often then shift their focus toward the third stage of government influence—to regulations that improve the affordability and convenience of the products and services in question. This can be achieved by deregulation, or the unwinding of restrictions on price-cutting and entry, that had been put in place when stabilization and assurance were paramount concerns. Antitrust action is another weapon used in the pursuit of competitiveness and efficiency.
Economists and economists-turned-deregulators have habitually employed a standard and simplistic formula for cost-reduction: ↑ competition = ↓ prices. Their simple creed is that in the absence of competition, companies will charge monopolists' prices. If you intensify competition it will drive prices down. It turns out that the hoped-for good news of this gospel often doesn't materialize. When deregulation or antitrust action pits new entrants against the established industry leaders from the regulated era in sustaining competition, it typically results in an enormous waste of resources and little impact on prices, because the entrants fail. It is disruptive competition that yields dramatic reduction in price and improved accessibility. The implication is that deregulators need to focus not simply on enabling competition—but on facilitating disruptive competition.55 When regulators don't get this formula right, history has shown time and again that the results can be catastrophic. Let's look at three such cases, the scenarios of which are summarized at the end of the following section, in Figure 11.2.
In the 1960s, IBM dominated the market for mainframe computers. It enjoyed a 70 percent market share, but captured about 95 percent of the industry's profit. This near-monopoly of course bothered the United States Department of Justice, and so in 1968 the DOJ sued to break up IBM into a set of smaller companies in the belief that more intense competition amongst mainframe computer makers would reduce the cost of computing. For 13 years the government spent hundreds of millions of dollars prosecuting this lawsuit, and IBM spent hundreds of millions defending itself.
While the lawyers were working on this problem, the disruptive minicomputer and personal computer value networks were emerging. As these ecosystems grew, they pulled more and more customers and applications from the mainframe value network in the back plane of the disruption diagram into the disruptive networks in the front. One day one of the lawyers noticed, "Hey! There aren't many customers back here using these mainframes! They're out there computing on those microprocessor-based machines!" So they closed their briefcases and went home. IBM's mainframe monopoly indeed had been broken—but not by the Justice Department. It was broken through disruption.
We invite our readers to pause at this point, boot up their notebook computers, and reflect on two historical possibilities. What impact would breaking up IBM's mainframe monopoly—in order to create more competition among mainframe providers—have had on the cost, availability, and quality of computing? How does that compare with the impact that disruption has had on these three variables? It's a great way to visualize how important it is for regulators and the economists who advise them to differentiate between sustaining and disruptive competition.
By the late 1990s an even more dominant near-monopolist named Microsoft had emerged in the personal computer operating system business. Its market share exceeded 90 percent, and the company was making extraordinary profits. This of course bothered the United States Department of Justice deeply, and so in May 1998 it sued to break up Microsoft in the belief that more intense competition among operating system and Internet browser vendors would reduce the cost of computing. The government spent hundreds of millions of dollars prosecuting this lawsuit, and Microsoft spent comparable sums defending itself. A decree in 2001 signaled that Microsoft had survived the first attack of the Justice Department.
While the DOJ's Antitrust Division is figuring out its next steps, a new disruptive value network is emerging in a new plane of competition. While it has many names, we'll call it Internet-centric computing. It is disrupting the enterprise-centric computer networks within which most of us have been computing during the last decade. Linux has become the operating system of choice in Web servers, and firms like Google, Yahoo, and Amazon have built their systems upon Linux. As these Internet-centric services are becoming faster, more convenient, secure, and reliable, more and more applications are being drawn out of the enterprise network in the back plane of the disruption diagram, into the Internet-centric value network in the front—customer by customer, application by application, from searching for documents on our hard drives to searching for them on the Internet.
One day soon some antitrust lawyer will notice that the government's latest legal briefs had been composed on GoogleDocs, not Microsoft Word, and will send out the message, "Hey! There aren't many customers left here using these enterprise networks! They're all out there computing on those Web servers!" They will then close their briefcases and go home. Microsoft's monopoly will indeed have been broken—but not by the Justice Department. It will have been broken through disruption.
In the Telecommunications Deregulation Act of 1996, the United States government again attempted to enhance affordability and accessibility with the same naive theory—that competition per se will drive costs down. To promote competition, the act required that the independent local exchange carriers—also known as ILECs, comprising US West, Pacific Bell, Bell South, Ameritech, Southwestern Bell, and Bell Atlantic—share their networks with new entrants at discounted, regulated rates. These entrants, called competitive local exchange carriers (CLECs), were invited to create competition over the "last mile" to customers' homes and offices, and then "plug in" to the established ILECs' local networks that interfaced with long-distance networks. The hope was that a large barrier to entry—the creation of the physical "local loop" of communications lines and switches—could be circumvented by utilizing existing networks, thereby promoting competition in local telephone service that would hopefully result in lower rates for consumers.
Close to 300 CLECs garnered more than $300 billion in funding from venture capitalists and Wall Street, entering the markets of over 100 cities. By 2002 only 70 CLECs remained, and by 2007 nearly all of them were gone. High fliers like WinStar, Covad, NorthPoint, Rhythms, and Teligent all went bankrupt.56 The sector became a poster child for the dot-com bubble burst. Indeed, rather than spurring more competition and lowering prices, a wave of industry consolidation occurred, and pricing for local telephone service remained high.
What happened? By enticing new entrants to use the prevailing business model, based on the existing local communications infrastructure, the regulators essentially pitted the start-up CLECs into head-on, sustaining-innovation competition against the ILECs on their home turf. Again, our research on innovation has shown overwhelmingly that when entrant companies attack incumbent leaders with a sustaining innovation, using a similar business model in the leaders' existing markets, the leaders invariably triumph. And they did.
While the regulators and their lawyers and economists have been using head-on sustaining competition as their tool for making telecommunications services more affordable and pervasively accessible, disruptive business models already are booming in a new disruptive plane of competition—without the subsidy of government. Using Voice over Internet Protocol (VoIP), Skype, to name just one example, is now one of the largest telephony providers in the world, with more than 350 million users. Its premium service offers unlimited local and long-distance calling starting at $35.40 per year—and its customers take their telephone numbers with them wherever they go in the world.57 And we are only beginning to see the revolution in affordability and accessibility that will come with wireless VoIP and video over the Internet.58 Meanwhile, in the rearmost plane of competition in the disruption diagram, the network companies and cable companies are engaged in multi-billion-dollar competitive battles of sustaining innovation, each striving to bring higher-definition television and more reliable wire-line telephony at higher prices to their most attractive customers in "Triple Play" bundled pricing.
The importance of applying the model of disruptive innovation to the challenge of improving the cost and accessibility of health-care services is presaged by Supreme Court Justice Stephen Breyer's opinion after the 1996 Telecommunications Act was challenged by a number of telephone carriers. Breyer offered an apt postmortem of the entire debacle: "It is in the unshared, not in the shared, portions of the enterprise that meaningful competition would likely emerge. Rules that force firms to share every resource or element of a business would create, not competition, but pervasive regulation, for the regulators, not the marketplace, would set the relevant terms."59
FIGURE 11.2 Patterns in the impact of regulation versus disruption in making services affordable and accessible
We could recount in detail for deregulators how air travel, trucking, stock brokerage, and many more regulated products and services have become significantly more affordable not by introducing head-on sustaining competition, but through disruption. The topic deserves a book in itself. Suffice it to say that there is a pattern here. Regulators and deregulators have not once—not once—brought significantly lower costs and better access by demanding enhanced competition among the established practitioners of existing business models. When regulations that were put in place to stabilize and assure subsequently need to be relaxed and refocused, significant improvements in cost and access have only come from disruptive business model innovation. When we read simplistic, undifferentiated calls for more competition, we all ought to invoke Yogi Berra's immortal phrase: "It's déjà vu all over again."60
In the decade over which we conducted the research that we tried to distill into this book, we've noted a growing sense of despair among doctors and executives about the counterproductive roles that Medicare policies play in the overall American health-care industry. Medicare has become so massive, the refrain goes, that it simply cannot be changed. We believe that Medicare can be transformed into a neutral force in the industry—still able to fulfill its mission of providing care to the elderly, yet not inhibiting innovation that can help everyone. This can be done by following the same rules: We need to initiate change in portions of the industry that are beyond Medicare's reach, rather than trying to change Medicare directly. And we need to control the ballooning costs of Medicare through regulatory change that enables or facilitates disruptive business models.
How does one create a value network beyond the reach of Medicare pricing mechanisms that create such powerful distortions in U.S. health care? One way is to internalize the market within the major integrated provider systems described in Chapter 6, where members pay a fixed annual fee for the health services they receive.
If organizations like Kaiser Permanente, Intermountain Health-care, and Geisinger Health System create focused and disruptive business models appropriate for the different categories of disease, they can internally make decisions and direct patient care based upon efficacy and economics, not in response to distorting regulations on reimbursement.61 As these delivery systems prove their efficacy and cost advantage, then one by one, patients can be drawn from the original plane of competition—where independent suppliers apply for Medicare reimbursement on a fee-for-service basis—into a new disruptive one. Ultimately, Medicare would assist its covered population in the payment of annual fees associated with care in the integrated fixed-fee provider system. Importantly, the fixed annual fee would be the only price that Medicare would be concerned with—and it would be a negotiated price between the payer and provider. Other prices would be set between vendors of drugs, devices, and services, and the integrated entities that buy from them, on a competitive basis.
In many respects the United States, with its hybrid public-private system, has a leg up in health-care reform over those democratic countries without a substantial private system. When the government is everywhere, innovators can't go where the regulators aren't, in order to initiate disruption. Reformers in those nations must tackle the system head-on—which, as the final section below will show, is a fight we wouldn't wish for our worst enemies.
Our claim at the beginning of this chapter that "the tentacles of governmental influence and control stretch throughout America's health-care system in a deep, tangled, and pervasive way," actually might have been an understatement. CMS typically sets the anchor rates for medical reimbursement, which private insurers then follow. The NIH and FDA are essentially make-or-break supporters and gatekeepers for innovations in biomedical research and new technologies. Other institutions, including the Veterans Health Administration, Indian Health Service, and an extensive network of federally funded and state-funded public health centers, deliver care.
Given the pervasive influence of all these agencies, one might reason whether the government itself might be the only entity with the power and scope to solve the health-care crisis. In fact, nearly every decade brings a renewed push for the United States to emulate the system used by most industrialized nations—a government-sponsored, single-payer nationalized system.
The critical challenge we actually face is not how to pay for health care. Nobel laureate Milton Friedman long ago assured us that there is no such thing as a free lunch. Whether the check is written by individuals, employers, or government-run health-care systems, in the end it comes from the pockets of the people.
A second question of some import is whether to pay for health care. Overwhelmingly, American employers have chosen to pay for it. A key reason why health care accounts for a smaller share of Gross Domestic Product in other developed nations is that their governments have chosen not to pay for it: Almost every government with nationalized health care has been forced to ration access to advanced care in one way or another. The straits in which Canada's public, paid-for system finds itself, for example, prompted Chief Justice Beverly McLachlin of the Supreme Court of Canada to opine in 2005 that "access to a waiting list is not access to health care."62 As a result, most countries with national health systems have had to develop alternative market-based channels for coverage as well—so people can choose for themselves whether to pay for certain services, rather than leaving that choice to bureaucrats.63
Government health systems in general do a better job not just of rationing, but also of controlling the salaries earned by doctors and nurses, because governments essentially are the only employers for most of those who pursue health-care careers—and monopsonistic purchasers have the power to dictate the prices they will pay.64 Because of governments' tight control on caregivers' salaries, in many nations the best physicians establish themselves in private practice, where they can earn higher incomes by serving the wealthy. This is another paradox of national health systems: while the intent is to assure universal access, often it is the elite who see the elite, while the rest see the rest.65
Hence we come to the focus of this book: how to make health care affordable. We hope our readers are convinced by now that it is the business model within which the professionals work that is the major driver of cost, not just in health care, but in every industry. National health systems have not done a better job than America's system of making health-care costs affordable through disruptive business model innovation. Both, to date, have done poorly.
We believe that despite all the roadblocks we expect disruptive innovators to encounter in America, however, a decade from now disruptive reformers within America's system will prove to have been much more successful at making care more affordable and accessible than will those in most nationalized health systems. We therefore urge America's political leaders not to view further government control as a vehicle for solving our problems. Rather, it is time for America's government to foster disruption.
Most government health ministries are comprised of decentralized fiefdoms. Hospitals are administered independently of the physicians' organizations, which are administered independently of the drug pricing and distribution system, and so on. Though the administrators are civil servants and the doctors are employed by the ministry of health, these systems are not different in their basic administrative structure from the non-integrated system that characterizes most of the United States health-care industry. Those few public health ministries with a high degree of centralized, coordinative control, such as in Singapore and the United Kingdom, resemble in their structure the integrated providers like Kaiser Permanente, which we discussed earlier. In other words, the centralization of the power to orchestrate change is what is critical—and that power can be vested in either a government ministry or a private provider.66 Most government health ministries are actually quite powerless to implement significant changes, because the political process of convincing the separate entities to fall in line in the new disruptive direction would stymie all semblance of reform.
To explain why the power to orchestrate is so critical, we'll draw on a final model from our research on innovation, which we call the "Tools of Cooperation." The essence of this model is that having the right vision for where your company (or a ministry of health) needs to go is just the start. Once you know the necessary future direction, you then need to convince all the other people and entities whose resources and energies are required to succeed in that journey to cooperatively work together to get there.
The effectiveness of the various tools that might be wielded to elicit this cooperation depends upon the extent of preexisting agreement along two dimensions. The first is the extent to which the people involved agree on what they want—the results they seek, what their priorities are, and which trade-offs they're willing to make to achieve those results. The second is the extent to which they agree with each other on which actions will yield the desired result.
For those who must manage change, there is no "best" position along these two dimensions of preexisting agreement. The key is recognizing the extent of agreement and then selecting the tools of cooperation that will work most effectively in that situation. We believe this simple model applies to units as small as families, to business units and corporations, to school districts, and even to nations.
Figure 11.3 maps these dimensions of agreement in a matrix, and describes the types of tools managers can wield in different situations, in order to elicit cooperation among the stakeholders to work in concert in achieving the needed change. The boundaries delineating the domains in which the various tools can work are not rigid, but the broad labels can give leaders a sense of which tools are likely to be more or less effective in various situations.
FIGURE 11.3 Four types of cooperation tools
When there are sharp disagreements among the concerned parties about what they want and how to get it, the only tools that will elicit cooperation in pursuit of a new course are "power tools" such as fiat, force, coercion, and threats. This is how Marshal Tito brought peace to the Balkan Peninsula, for example. After World War II, he herded the disparate and antagonistic ethnic groups in that region into a more or less artificial nation and said, in essence, "I don't care if you agree with me or with each other on what you want out of life or how to get it. I just want you to look down the barrel of this gun and cooperate with me and each other." It worked.
Tools such as negotiation, strategic planning, and financial incentives don't work well in situations of minimal agreement. As depicted in Figure 11.3, these will work only when there is a modicum of agreement on both dimensions of the matrix. In environments of antagonistic disagreement—whether in the Middle East or in the infamous clashes between the management of Eastern Airlines and its machinist union—negotiation does not work. A leader might use strategic planning to figure out where the organization ought to go next, but lacking some agreement on both dimensions, the strategic plan itself will not elicit the cooperative behavior required to get there. And financial incentives—essentially paying others to want what you want—typically backfire in a low-consensus environment. People will react indifferently, because they do not agree with the incentives' goals.
Only power tools are reliably effective in low-agreement situations. The key is having the authority to use them. In democracies, many of these mechanisms are outlawed. This hamstrings public-sector executives who face a mandate for change with little power to do what needs to be done. We will return to this point later.
The tools that elicit cooperation in the lower-right region of the agreement matrix of Figure 11.3 are coordinative and process-oriented in nature. We call these "Management Tools," and they include training, standard operating procedures, and measurement systems. For such tools to work, group members need not agree on what they want from their participation in the enterprise, but they must agree on cause and effect.
For instance, in many companies, unionized manufacturing workers come to work for different reasons from those of senior marketing managers. But if both groups agree that following new manufacturing procedures will result in better levels of quality and cost, they will cooperate. If there is no consensus among the people concerned that following the new methods or metrics leads to the desired outcomes any more effectively than the old ones, however, they are unlikely to behave differently after being trained in the use of the new routines. The effectiveness of training is more dependent on the level of agreement about how the world works than on the quality of the training itself.
In the upper-left region of Figure 11.3, results-oriented tools, as opposed to process-oriented ones, are more effective because there is a high existing consensus about what employees want from their participation in the organization. Charismatic leaders who command respect, for example, often do not address how to get things done; instead they motivate people to just do what needs to be done. The same actions that employees view as inspiring and visionary when they're in the upper-left corner of the agreement matrix are often regarded with indifference or disdain when the people are in the lower quadrants. For example, when people agree on what they want to achieve, vision statements can be energizing. But if people do not agree among themselves about what they want, vision statements typically induce a lot of eye rolling.
People located in the matrix's upper-right region will cooperate almost automatically to continue in the same direction. This is the essence of a strong culture. Their common view of what they want and of how the world works means that little debate is necessary about where to go and how to get there.67 But this very strength can make such organizations highly resistant to change. The tools of cooperation that are available in the realm of strong culture—including ritual, folklore, and democracy—facilitate cooperation only to preserve the status quo; they begrudgingly yield to change. When executives in this circumstance see big changes in the future and realize that the organization's momentum is propelling it in the wrong direction, the culture often fires the manager. Just ask former CEOs John Sculley (Apple), Durk Jager (Procter & Gamble), Carly Fiorina (Hewlett-Packard), and George Fisher (Kodak).
Where are health-care systems positioned in the agreement matrix? For the most part, they are in the lower-left corner of the diagram. Patients, doctors, regulators, IT professionals, hospital administrators, insurance companies, executives in pharmaceutical and medical device companies, small businesses, large businesses, and politicians all have divergent priorities and disagree strongly about how to achieve them.
The fact that health care is in the lower-left world of disagreement helps explain why certain remedies that reformers tried to introduce in the past have not worked. For example, reformers who advocate evidence-based medicine bewail the fact that many doctors continue to follow their own instincts rather than best demonstrated practices. But if those recalcitrant doctors don't agree that doing it a certain way brings the desired results, they won't follow the rules. Similarly, the reason why metrics of performance and value have been almost impossible to create is that the conflation of solution shops and value-adding process businesses within hospitals puts us in the lower-left portion of the matrix. Metrics of performance only work if there is strong agreement on cause and effect, and a modicum of agreement on what various parties want from their participation in the enterprise.
The scary thing about this situation is that democracy—the primary tool in most societies where health-care reform is at issue—is effective only in the upper-right circumstance, when there already is broad, preexisting consensus on what is wanted and how the world works.68 And what's worse, like all the tools in the culture quadrant of the matrix, democracy is not an effective tool for radical change—it is a tool best used for maintaining the status quo.
So is it possible that changing our health-care systems is impossible? No, it can be done—if we use a fifth tool—that of separation.
There are instances in which disagreement among the parties that need to cooperate is so fundamental that it's simply impossible to reach consensus on a course of action—and yet no one has amassed the power to coerce cooperation. When all other tools have failed, there is a trump card to play, and it does not reside within the agreement matrix. We call it "separation"—dividing the conflicted parties into separate groups so they can each be in strong agreement with others inside their own group, yet don't need to agree with those in other groups. In the post-Tito Balkans, by illustration, no one could again successfully amass and wield the requisite power to maintain peace, as Tito had. So we tried the charisma of President Bill Clinton and sales skills of Prime Minister Tony Blair. We tried democracy and negotiation. We used economic sanctions and incentives. Nothing worked—except separation. Peace came to the Balkans when the need for cooperation across antagonistic ethnic divides was obviated by dividing the peninsula into nations and regions for each ethnic group.
In our studies of disruptive innovation, we have seen the same thing. The only instances in which an industry's leading company also became the leader in the following disruptive wave occurred when the corporate leaders wielded the separation tool. These companies survived disruption by establishing an independent business unit under the corporate umbrella and giving it unfettered freedom to pursue the disruptive opportunity with a unique business model, essentially placing it in competition with the parent company.
If employees responsible for sustaining the core business must work in the same business unit as those responsible for disruptive products, they are forever conflicted about whether new or existing customers are most important; whether moving up- or down-market offers more growth; and so on. Separation in these instances is the only viable course of action. In addition, it takes the power of the CEO suite to wield the tool of separation. As a result, only a few companies have ever successfully disrupted themselves.69
It is this model that provides the theoretical foundation for our recommendation of "Starting where they aren't" when pursuing deregulation. Situations requiring regulatory reform, by definition, are in the lower-left corner of the agreement matrix. Cramming deregulation down the throats of those who don't want it requires extraordinary power—and in a democracy, nobody possesses such power. In a health system such as America's, private entrepreneurs can find interstitial spaces in which to establish a disruptive foothold—out of the eyesight and earshot of regulators and influential competitors in the existing market. If America's government were to bring health care into a single-payer system, by definition it would make it impossible to incubate reforms in fringe areas "where they aren't." And it would strip from executives in the industry the ability to wield the tools of power that are critical to making things happen in situations where disruptive innovations will be unpopular to the established interests.
This is why we urge our readers, our lawmakers, and our fellow American citizens not to look to a government-controlled single-payer system as a solution to our health-care crisis. It is a route that is relatively easy to get onto, but it is in fact a one-way street heading in the wrong direction. And there is no exit.
The sections above highlight eight regulations or other mechanisms of influence that need to be changed in order to facilitate the transformation we call for in this book. We'll list these changes here, in summary.
1. The NIH needs to create a different methodology for evaluating research proposals that draw upon multiple disciplines. Otherwise, the peer review process will continue to push medical science into increasingly narrow silos of knowledge, and we will fail to capture the novel approaches and discoveries that only come from the intersection of different points of view.
2. The formulas by which CMS and private insurers determine the prices they will pay for services need to be replaced. Prices that reflect true value and actual cost must be allowed to emerge, as pure solution shops, value-adding process clinics, and facilitated networks contract for business directly with employers and patients. Built into these prices are accountability of provider organizations and transparency of information for consumers—not equations of relative value administered by bureaucrats with false precision.
3. Reimbursement policies that unintentionally encourage disciplined price maintenance among competitors by rewriting prices based upon lowest-in-market rates each year must be discontinued. If health plans independently negotiate prices with suppliers and focused providers as we recommend employers do, overall pricing in the market will fall, not rise.
4. Because inconvenience and cost make health care inaccessible to the uninsured poor, the obligation of providers to provide uncompensated care should be eliminated. In its place, governments should mandate, with subsidies when necessary, the purchase of high-deductible health insurance and the use of health savings accounts by those who are now classed as poor and uninsured. At the same time, governments must foster not just a financial safety net, but expand the safety net of providers to include conveniently located retail clinics staffed by adequately trained nurse practitioners and dental technicians that are convenient, affordable, and accessible to everyone.
5. FDA clinical trials processes need to be redefined, when necessary, as research trials. At the same time, drugmakers should be encouraged to define the scope of clinical trials according to the molecular definition of the disease, and not necessarily by organ system or, in our parlance, symptom of disease.
6. The focus of regulations such as licensure and certification needs to keep pace with technological change and scientific progress. When care is in the realm of intuitive medicine, the focus should be on accrediting people. As care moves through empirical medicine toward precision medicine, the focus should shift to accrediting processes, and ultimately to guaranteeing outcomes.
7. The economists who advise deregulators need to abandon the simple, century-old, one-dimensional axis that pictures competition on one end and monopoly on the other. Rather, it is a particular type of competition—disruptive innovation—that will predictably bring significantly lower costs to health care. As soon as technological progress enables it, regulators must facilitate disruption. This is what will make health care affordable and accessible.
8. Employers need to be allowed to create financial incentives for healthy behavior. By illustration, they should be allowed to shift their contributions between high-deductible insurance and health savings accounts for individual employees as data on healthy or unhealthy behavior indicate that the long-term costs of insuring an employee are changing.
1. The Food and Drug Administration's origins can be traced back to the Division of Chemistry in the U.S. Department of Agriculture, which began publishing its research on misrepresented food and drugs in the late nineteenth century. Regulatory powers were granted to the agency by President Roosevelt with the 1906 Food and Drugs Act, which authorized seizure of intentionally misbranded or adulterated food and drugs. The organization was renamed the Food and Drug Administration in 1930.
2. A significant group of Clayton Christensen's MBA students have written course papers and independent research project papers on this subject. In chronological order, these include Scott Anthony, Erik Roth, Dan Svoboda, Peter Šararík, Sara Dawes, and Privahini Bradoo. Each of these built upon the research of the prior students, culminating in many of the insights summarized in this chapter. We are deeply grateful for their hard work and very thoughtful contributions to our understanding of a portion of this extremely complicated field.
3. In his review of the manuscript of this chapter, Charlie Baker, CEO of the Boston-based Harvard-Pilgrim Health Plan, commented, "We need the government to do these things to permit disruptive innovation to flourish. Private enterprise alone, without decent, intelligent federal policy support, cannot find a way out."
4. The mechanism for doing this was the Pacific Railroad Act of 1862. It called for two railroad companies to complete the transcontinental line. The railroad would be a "land-grant railroad," meaning the government would give each company 6,400 acres of land and up to $48,000 for every mile of track it built.
5. The government's track record in creating new industries through subsidies and setasides is mixed. There is strong reason to expect, for example, that the present subsidies of the ethanol, hydrogen, and solar and wind energy industries will ultimately be multi-billion-dollar debacles and disasters. First, because consumption is so pervasive in economically developed countries, these nascent technologies cannot be commercialized in a disruptive way (targeted at nonconsumers). They can only compete head-on as sustaining innovations against well-established, mature, efficient, and reliable competing products and companies. For many reasons chronicled in our research on disruption, entrants almost always fail when pitted in head-on sustaining innovation against incumbents. In contrast, in the developing world where there are many areas of nonconsumption of electric power, we can expect solar and wind energy to thrive commercially. The second reason why we can expect these massive subsidies to fail is technological interdependence. Ethanol and hydrogen are not "plug compatible" with the existing infrastructure for distribution and use. These technologies will require building completely independent infrastructures—a proposition whose cost is extraordinary. However, a developing nation with no significant existing infrastructure will weigh its options differently and often choose the "leapfrog" technology—so called because it bypasses an entire generation of infrastructure requirements that had been necessary in the past.
6. The government's hits have been offset by a lot of misses, of course, and this topic deserves a Ph.D. dissertation, not just a footnote. But as a general rule, government funding of infrastructure upon which an industry can grow—highways, railroads, airports, etc.—results in successful economic growth. For similar reasons, government funding to develop scientific techniques—such as gene splicing techniques or synthetic biology techniques—typically creates more growth than funding to develop specific technologies. Anticipating which technologies will be commercially valuable is a much harder question to answer correctly, whereas subsidizing the creation of tools to enable companies to develop technologies seems to work better. When government funding of specific technologies seems imperative, those that are disruptive (such as the Internet and the transistor) also are often successful, because those technologies compete against nonconsumption—they find a much more ready market. However, when the government has funded technologies that can only be implemented in sustaining ways, in head-on competition with the conventional technology in common use, with just a few exceptions it results in a vast waste of financial and natural resources. This is because the steady, incremental advance of existing technologies in the value networks within which they function is persistent. and the new technologies are rarely plug-compatible in existing systems. Hence, the massive oil shale investments in the 1970s were a dramatic waste. We predict that today's investments in biofuels will similarly result in a waste of resources, a distortion of markets, and will have little beneficial impact on oil consumption or cost. It is a sustaining technology pitted into head-on competition against an established technology.
7. We thank Professor Emeritus H. Kent Bowen of Harvard Business School for his insights on these issues. He has pointed out that the funding of America's research universities by the National Science Foundation has had a similar "siloization" on institutions like the Massachusetts Institute of Technology.
8. Kuhn, Thomas, The Structure of Scientific Revolutions (Chicago: University of Chicago Press, 1962).
9. For readers with a deeper interest in this principle of intersections, we recommend Johansson, Frans, The Medici Effect (Boston, Massachusetts: Harvard Business School Press, 2004). This is a fascinating history of the technological intersections that led to many of the world's great scientific breakthroughs. And two case studies by Professor H. Kent Bowen, "The Langer Lab: Commercializing Science" (Harvard Business School case # 9-605-017) and "The Whitesides Lab" (Harvard Business School case # 9-605-017), chronicle how two of the most productive biotechnology laboratories in the world (at MIT and Harvard, respectively) are structured to deliberately force a multidisciplinary perspective into each research project.
10. Consider, as an example of productivity at an unconventional intersection, the persistence of malaria in vast areas of the world, long the bane of infectious disease researchers and public health workers. Drawing upon the science of immunology to develop vaccines hasn't worked because the Plasmodium parasite that female anopheles mosquitoes inject into the human bloodstream, causing malaria, simply evolves too quickly; we can't keep up with it. One promising approach on the horizon for the prevention and treatment of malaria has been developed by a company in Havre de Grace, Maryland, General Resonance LLC. Its science comes from the study of nanotechnology and particle physics, not immunology or infectious diseases. Its founders have observed that a long-known property of materials called "resonance," whose effects are dampened or canceled in crystalline structures, actually become powerful among nanoscale particles of a material. They found that while human cells seem inert to the resonance generated by these materials, their resonance can be lethal to a very broad spectrum of these parasites. Whether this will prove to be the solution to eradicating this pernicious disease remains to be seen, of course. But it is an illustration of the principle that breakthrough insights almost always come at the intersections of disciplines, rather than from within one of them.
11. One of Thomas Kuhn's most prominent conclusions was that when a new paradigm is emerging from the work of scientists in other fields, the experts in the old paradigm remain convinced, even to their dying day, that the new paradigm cannot possibly be true. The reason is that the old paradigm has so powerfully shaped their beliefs about how the world works, and what is and is not possible, that their minds literally cannot see the phenomena that led to the articulation of the new paradigm. We would expect, as a result, that many leaders of our most prominent medical schools will discount the possibility of the reforms we have advocated, for reasons that are perfectly rational to them.
12. A useful summary of this early history, told through the language of disruptive innovation, can be found in Christensen, Clayton; Scott D. Anthony; and Erik A. Roth, Seeing What's Next (Boston, Massachusetts: Harvard Business School Press, 2004).
13. Under the Veterans Health Care Act of 1992, the Veterans Health Administration is also guaranteed discounts based on the non-federal average manufacturers price. However, in part because it is a closed system, the VA has also been able to establish other methods of discounting, including aggressive formulary management and national standardization contracts that encourage competitive bids. Medicare Part B previously had a similar "we get the lowest price" policy, but this was modified by the Medicare Modernization Act of 2003. Prices are now set at 106% of the average sales price, which is a statutorily defined price based on actual sales transactions, rather than a fixed discount of the average wholesale price. That same legislation also created Medicare Part D to expand prescription drug coverage, but included a "noninterference" provision that forbids the Department of Health and Human Services from negotiating drug pricing on behalf of Medicare beneficiaries. Instead, Part D encourages market competition by encouraging individual health plans to negotiate prices and discounts on behalf of their members, and offers no specific guidance on pricing. This "noninterference" clause is under threat of repeal. See Jacobson, G., Panangala, S., and Hearne, J., "Pharmaceutical Costs: A Comparison of Department of Veterans Affairs (VA), Medicaid, and Medicare Policies," Congressional Research Service Report for Congress, Domestic Social Policy Division, April 13, 2007; and "Medicaid Drug Price Comparison: Average Sales Price to Average Wholesale Price," Department of Health and Human Services, Office of Inspector General, OEI-03-05-0020, June 2005.
14. We do not know the specific portion of blood glucose test strips purchased through government payers; but we've chosen to apply a simple assumption for ease of illustration.
15. The numbers in this example are very round and approximate ones, and not the result of a purposeful study on this topic. We have chosen this example for a purpose, however. Knowledgeable friends have informed us that while diabetes test strips indeed retail at prices near a dollar apiece, the cost to manufacture these strips is less than 10 cents. Of course there are fixed costs that must be covered from the gross margins on these strips, but situations like this are exactly where one typically sees price discounting as competitors vie for major contracts. And yet the competitors in this industry have maintained extraordinary discipline in raising and maintaining prices. We are not suggesting, nor has anyone else charged, that there has been collusion to set prices high in this industry. We're simply suggesting that a core reason why prices have risen and are maintained at such heights might be that Medicaid and similar systems of reimbrusement have made discounting to anyone very expensive. Executives in industries like airlines, where rogue competitors routinely discount prices, can only dream of what it's like to compete against suppliers to the health-care industry, where pricing discipline is so pervasive.
16. Interestingly, according to a Health Affairs survey in 2005, medical bankruptcy affected roughly 2 million Americans (including dependents), and 75.7 percent of them had insurance when they first became ill. See Himmelstein, David, U., et al., "MarketWatch: Illness and Injury as Contributors to Bankruptcy," Health Affairs. Accessed at http://content.healthaffairs.org/cgi/content/full/hlthaff.w5.63/DC1. This is evidence that underinsurance is also a significant problem contributing to medical bankruptcy.
17. Public hospitals in the 100 largest metropolitan areas, considered key safety-net hospitals, comprise only 2% of all hospitals, but provide over 20% of all uncompensated care (Report of the Council on Medical Service, American Medical Association, December 2001). The burden of uncompensated care tends to fall on only a small number of hospitals, typically those that are: government-sponsored teaching institutions, rural nonprofit hospitals, or serving areas with a disproportionately high number of uninsured patients ("Nonprofit, For-Profit, and Government Hospitals: Uncompensated Care and Other Community Benefits." U.S. Government Accountability Office, GAO-05-743T, May 26, 2005.
18. In the end, costs were merely shifted from one area to another, and any estimated savings to the state, at best $16.5 million out of a $3 billion MassHealth budget, came at the expense of increased suffering of patients due to untreated, and often preventable, dental disease. Dental coverage was reinstated in 2007, but reimbursement rates remain much lower than other dental insurance plans. See Pryor, C., and M. Monopoli, "Eliminating Adult Dental Coverage in Medicaid: An Analysis of the Massachusetts Experience," Kaiser Family Foundation, Kaiser Commission on Medicaid and the Uninsured, September 2005.
19. This is the phrase that Dr. Marcia Angell, former executive editor of the New England Journal of Medicine, used to describe the impact of the law in Massachusetts that mandates health insurance for everyone, without taking any initiative to reduce the cost of providing that care. Source: Kuttner, Robert, "A Health Law with Holes," Boston Globe, Jan. 28, 2008 (editorial page).
20. For more about the FDA's Critical Path Initiative, we refer readers to http://www.fda.gov/oc/initiatives/criticalpath/initiative.html.
21. Astute readers will also recognize that once care reaches the stage of precision medicine, the intuition of physicians is no longer needed. At this point, rather than have insurers try to implement pay-for-performance for physicians, it would make more sense in many cases simply to have patients purchase their services directly from value-adding process clinics. If such a retail environment were to develop, market pricing could obviate the need for any pay-for-performance program imposed by a third party.
22. Unmanned Aerial Vehicles (UAVs) already in regular use by the military can fly and land automatically. They have become increasingly capable—even in combat situations that previously had required a pilot.
23. See Public Broadcasting System, "How Risky Is Flying? Commercial Aircraft Fatalities, 1982–2005," sourced at http://www.pbs.org/wgbh/nova/planecrash/risky.html. It shows how much safer flight has become in recent years. We know this book is about health care and not aviation, but check out this description of what the "virtual copilot" on these Eclipse jets does (taken from the company's Web site in August 2008): "Avio NG, Eclipse's exclusive Total Aircraft Integration system, incorporates technology never before available in general aviation. Avio NG centrally controls aircraft systems including avionics, engine operation, fuel system, flaps, landing gear, cabin pressure, and temperature. Beyond that, it acts as a virtual copilot, providing checklists and advanced navigation and avionics information, improving safety and dramatically reducing pilot workload—especially during single-pilot operation. Twin PW610F turbofan engines have an Automatic Power Reserve to boost power to one engine by 10 percent if the other should fail. Both engines are protected by Eclipse Aviation's exclusive PhostrEx next-generation fire suppression system. The Eclipse 500 features pneumatic de-ice boots, heated engine inlets, electrically heated windshields, and data ports that enable flight into known icing conditions. Reliability and redundancy are built into every system, from the four independent power sources to the electric trim motors and servos. So the pilot is never overwhelmed, and the passengers can relax and enjoy the ride."
24. Note that the general hospitals also have not militated against rehabilitation, cancer, senior care, women's, children's, and community hospitals either—even though an intellectually consistent approach ought to have raised some of the same concerns for patient safety against these institutions as well.
25. A 2008 RAND study revealed that only 38.7 percent of retail clinic patients reported having a primary care physician, compared to 80.7 percent of patients nationwide. See Mehrotra, A., et al., "Retail Clinics, Primary Care Physicians, and Emergency Departments: A Comparison of Patients' Visits," Health Affairs, vol. 27(5):1272–82.
26. Center for Responsive Politics, accessed from http://opensecrets.org.
27. The level of these rates could be changed, but they always were set by the Federal Reserve, and commercial banks always could pay one-quarter percent below what savings banks and savings and loan associations paid.
28. In fact, the famous Wright amendment, enacted in 1979 to protect the home base of American and Braniff at DFW Airport, essentially banned Southwest from DFW until 1996, when it finally was revoked.
29. "Oral Health: Preventing Cavities, Gum Disease, and Tooth Loss 2008," U.S. Department of Health and Human Services, Centers for Disease Control and Prevention," Coordinating Center for Health Promotion, February 2008, accessed from http://www.cdc.gov/nccdphp/publications/AAG/doh.htm on Aug. 5, 2008.
30. "Billions Suffer from Tooth Decay," BBC News, Feb. 25, 2004, accessed from http://news.bbc.co.uk/1/hi/health/3485940.stm on Aug. 5, 2008.
31. S.2203 and H.2221: An Act Authorizing Dental Hygienists to Practice in Public Health Settings, filed by the Massachusetts Dental Hygienists' Association (MDHA). Our readers will of course note the similarities to the fight to allow nurse practitioners to examine patients and write prescriptions without physician supervision.
32. S.1216: An Act Relative to Dental Auxiliaries, filed by the Massachusetts Dental Society, would create new dental assistant classifications (registered dental assistants and expanded function dental assistants) and a new dental hygienist classification (expanded function dental hygienists), all of whom would be considered Dental Assistants with Advanced Training, accessed from http://www.mass.gov/legis/bills/senate/185/st01/st01216.htm on Aug. 5, 2008.
33. Massachusetts Dental Hygienists' Association Web site, accessed from http://www.massdha.org/news-events/legislative-updates.asp on Aug. 5, 2008.
34. According to the Agency for Health-care Research and Quality, accessed from http://www.innovations.ahrq.gov/content.aspx?id=1840, on Aug. 6, 2008, Alaska Native children and adults suffer much higher rates of oral disease than other Americans. Alaskan children between ages two and four have a rate of dental decay five times the national average. In addition, 85,000 Alaska Natives are dispersed throughout small villages of less than 400 people that are relatively inaccessible. There are also fewer dentists available per capita, making access even more difficult.
35. Alaska Dental Health Aide Therapist Initiative, Alaska Native Tribal Health Consortium, 2000, accessed from http://www.anthc.org/cs/chs/dhs/index.cfm, on Aug. 6, 2008.
36. Nash, David A., and Ron J. Nagel, "Confronting Oral Health Disparities Among American Indian/Alaska Native Children: The Pediatric Oral Health Therapist," American Journal of Public Health, 2005; 95(8):1325–29.
37. Fiset, Louis, "A Report on Quality Assessment of Primary Care Provided by Dental Therapists to Alaska Natives," Alaska Native Tribal Health Consortium, Sept. 30, 2005. A second report in 2007 from a professor of dentistry from Texas A&M University found that care provided by DHATs were within the scope of their training and met the standard of care in dentistry. The study found no difference in the rate of complications resulting from care delivered by DHATs and dentists. See Bolin, Kenneth A., "Quality Assessment of Dental Treatment Provided by Dental Health Aide Therapists in Alaska," paper presented at the National Oral Health Conference, May 1, 2007.
38. Alaska Dental Society et al. v. State of Alaska et al. Complaint for Declaratory and Injunctive Relief. 3AN-06-04797 CI (Alaska Super. Ct., Jan. 31, 2006).
39. "Superior Court Judge Rules in ANTHC Favor June 27," Mukluk Telegraph, August/Sept. 2007, vol. 10, Issue 2, page 7; and "Judge Dismisses Case Against Dental Therapists," accessed from http://www.ktuu.com/global/story.asp?s=6720173, on Aug. 6, 2008. Although still opposed to the initiative, the ADA and ADS have since agreed to work with DHATs to promote dental care in Alaska's rural communities.
40. Our thanks to Dr. Keith Batchelder and Peter Miller of Genomic Health-care Strategies for bringing our attention to this example.
41. Mullaney, T., "The Sensible Side of Telemedicine," BusinessWeek OnlineExtra, June 26, 2006, accessed from http://www.businessweek.com/magazine/content/06_26/b3990079.htm, on July 29, 2008.
42. NightHawk Radiology Services Web site and press release, accessed from http://www.nighthawkrad.net/ and http://biz.yahoo.com/prnews/080717/aqth080.html?.v=54, on July 29, 2008.
43. It's funny how the challenge of accurately interpreting images at night and on weekends was so simple that it could be done remotely without concern for patient safety, whereas the images that needed to be interpreted during weekdays were so complex that an on-site radiologist would be required.
44. Pollack, Andrew, "Who's Reading Your X-Ray?" New York Times, Nov. 16, 2003, accessed from http://www.nytimes.com/2003/11/16/business/yourmoney/16hosp.html, on July 29, 2008.
45. Mishra, Raja, "Radiology Work Shifts to Overnight, Overseas," Boston Globe, June 29, 2005.
46. Johnson, Douglas E., "NightHawk Teleradiology Services: A Template for Pathology?" Archives of Pathology and Laboratory Medicine, vol. 132, no. 5, 745–57.
47. Steinbrook, Robert, "The Age of Teleradiology," New England Journal of Medicine, vol. 357:5–7, July 5, 2007.
48. Our thanks to Dr. Keith Batchelder and Peter Miller of Genomic Health-care Strategies for suggesting these technological enablers of disruption in radiology.
49. Prior to functional brain imaging, for example, even for a brain-dead patient images might often indicate a normal brain.
50. Our thanks to Joseph Camaratta of Siemens for his generous comments regarding this case study.
51. This is one of the inherent advantages of a value-adding process business model, which can be evaluated based on its outcomes rather than its component resources.
52. Wong, Wilson S., et al., "Outsourced Teleradiology Imaging Services: An Analysis of Discordant Interpretation in 124,870 Cases," Journal of the American College of Radiology, 2005; 2:478-84.
53. Radiologists, it should be noted, have not sat still, as forays into interventional radiology have enabled them to disrupt the low end of general surgery. Telemedicine services are similarly challenging the fields of pathology and intensive care, with others certain to follow.
54. Lau-Tzu, Tao Te Ching, circa 600 BC.
55. Our assertion here is that significant cost reductions typically do not occur within a business model. They occur when a new, disruptive business model is created to displace the old. A frequent reaction of those with whom we've discussed this assertion has been to cite significant price declines of products as they move from introduction to volume production. Intel, for example, frequently will drop the price of its microprocessors from an introductory height of $600 to a floor of $200 or so, as costs drop with increasing volumes. This is a different phenomenon than the one we are discussing in this chapter. As Intel moves from one generation of processors to the next, the introductory prices of the new-generation products tend to be as high as the prior ones; and the floors to which they drop tend to be similar to prior floors. The technology (and the corresponding business models in which it is embedded) that threatens Intel's hegemony in logic circuitry is the digital signal processor, or DSP chip, which is made by companies like Texas Instruments and is used in handheld devices like the RIM BlackBerry and wireless telephone handsets.
56. For more information on this history, see Doherty, Jacqueline, "Telecom Tightrope," Barron's, Jan. 8, 2001, 17-18; Darby, Larry F.; Jeffrey A. Eisenach; and Joseph S. Kraemer, "The CLEC Experiment: Anatomy of a Meltdown," Progress on Point 9.23, Progress & Freedom Foundation, Sept. 2002; and Christensen, Clayton, Scott Anthony, and Eric Roth, Seeing What's Next. (Boston, Massachusetts: Harvard Business School Press, 2004). Note that some companies predated the 1996 Act.
57. Skype's SkypeOut service started in 2006 at $29.95 per year for worldwide calls. Currently it costs $35.40 per year for unlimited calls within the United States and Canada. Skype's unlimited global plan is $119.40 per year as of August 2008.
58. If we went further back into the history of the industry, we could tell the same story. The cost of long-distance was made significantly lower by a disruptor, Microwave Communications Inc., or MCI.
59. AT&T Corp. v. Iowa Utilities Bd., Supreme Court of the United States, Jan. 25, 1999. Accessed at http://www.law.cornell.edu/supct/html/97-826.ZX2.html.
60. We have sought a reliable source for this phrase that so frequently has been attributed to the venerable former catcher for the New York Yankees, but have not succeeded. Professors Michael Porter and Elizabeth Teisberg recently published a treatise, Redefining Health Care (Harvard Business School Press, 2006), in which they argue for enabling the better measurement of value and for enhancing competition among providers that will reward those that provide the best value. We hope that our research can bring more specificity to their findings, by contributing the notion that we should expect fundamentally different outcomes from sustaining and disruptive competition.
61. In his speech at a Health Affairs press briefing on Sept. 10, 2008, Glenn Steele, president and CEO of Geisinger Health System, described this perspective of integrated delivery systems in a comment about recent innovations at his organization: "It didn't matter who won financially. That's key. If the insurance company wins, or if the doctor group wins, which is rare, or if the hospital wins, it doesn't matter as long as the patient wins. Because we can do the internal transfer pricing. We can basically redistribute the financial benefits." See http://www.kaisernetwork.org/health_cast/hcast_index.cfm?display=detail&hc=2965.
62. "Unsocialized Medicine," Wall Street Journal, June 13 2005, A12.
63. Canada is the only country other than Cuba and North Korea where it is still illegal to purchase health care privately.
64. In the parlance of economists, monopolists are entities that are the sole suppliers of a product or service in a market. Monopsonists are the sole purchasers of a product or service in a market.
65. For example, see Anderson, Gerard F. and Peter Hussey, "Special Issues with Single-Payer Health Insurance Systems." Health, Nutrition and Population department of the World Bank Human Development Network. Discussion Paper. September 2004. In analyzing Sweden's health care system, the authors state, "Although most physicians are paid publicly, the share in private practice has increased, and public physicians can see private patients in their spare time. This may diminish access to care in the public system for poor patients if physicians spend more time with private-paying patients."
66. For example, see Zamiska, Nicholas, "China Thinks Small in Prescription for Health Care: Primary-Care Clinics to Become First Stop in Revitalizing System." Wall Street Journal, March 11, 2008, A10.
67. Schein, Edgar, Organizational Culture and Leadership (San Francisco: Jossey-Bass, 1987).
68. A moment's reflection supports this assertion. Whenever America has swooped into a country where there wasn't broad consensus on what everyone wanted or how to get it, and has tried to impose democracy—whether in Haiti or Nigeria, in Iraq or Afghanistan—the result has been a widespread breakdown in social order. The nations where fundamental regulatory changes have been implemented to enable rapid economic development in the last 50 years—including South Korea, Taiwan, Singapore, and Chile—were all governed by relatively honest dictators who could wield the tools of power to do what needed to be done. As those countries prospered, consensus on the two axes increased, and democracy gradually became feasible.
69. A good example is at General Motors. Its executives spun Saturn off in 1985 as an independent company under the GM corporate umbrella. Initially billed as, "A different kind of company, a different kind of car," little by little the organization's cultural power has pulled Saturn back into the General Motors cultural orbit. The corporate executives just haven't had or been able to wield enough power to keep it as separate as originally intended. Chapter 10 in Christensen, Clayton, and Michael Raynor, The Innovator's Solution (Harvard Business School Press, 2003), provides a listing of the few companies that have managed to disrupt themselves.