LEARNING OBJECTIVES
▪ Understanding the geographical aspects of health and health care provision
▪ Using GIS to map and analyse spatial health patterns and their socio-economic and geographic determinants
▪ Using GIS to identify health-related hot spots
▪ Geographical access to health care provision and location planning/spatial decision support
▪ Using GIS for the management and targeting of health resources
Health itself is difficult to define, but is generally considered as a state of well-being, with the World Health Organization (WHO) claiming that health is ‘a state of complete physical, mental and social well-being and not merely the absence of disease and infirmity’ (WHO, 1946). Although we often consider health (or more specifically ill-health) to be an individual factor, health and health care are important concepts from a geographical perspective. It is clear that both between countries and within countries there can be substantial health inequalities, whether those are differences in mortality rates or in access to primary care (doctors or GPs) or secondary care (hospitals). However, within the broader social sciences, there is an interesting debate around the relationship between health and place, and the causes of such health inequalities. Health is experienced at the individual level, but health issues are inherently geographical. Your own health is determined by pre-disposing genetic factors, but also by personal geographies including where you were brought up and where you live, work and socialise now, all of which affect your risk of ill-health, your access to health care and the quality of treatment you receive.
This fascinating debate is explored in more detail elsewhere (Kearns and Joseph, 1993; Curtis and Rees Jones, 1998; Curtis, 2010; Gatrell and Elliott, 2014). Although some researchers argue that processes operating at the level of the individual are far more important than the significance of different places, others argue that these processes that influence an individual’s health experience can operate differently in different places (Curtis and Rees Jones, 1998). Certainly, many health geographers would argue that health inequalities are a combination of the characteristics of individuals (age, gender, social class, ethnicity, etc.: often labelled compositional effects) and the place in which they live or were brought up (often labelled contextual effects). GIS allows policy makers to explore these health variations in more detail and perhaps try to ascertain, for each case study, whether compositional or contextual effects are more important. For certain, GIS allows more local interventions to be considered as policy options perhaps alongside national policy interventions that might impact on entire populations.
This chapter thus focuses on the use of GIS to evaluate health and health care from a geographical perspective. GIS has a major role to play in evaluating small-area health patterns, identifying where populations and health care need are located and in the targeting of resources. As we have seen with income, deprivation and geodemographics, GIS is most widely used as a visualisation tool to explore inequalities in small-area health patterns, but also as a more powerful tool for location planning/spatial decision support. Such uses include identification of optimal sites for health care facilities and evaluation of access to and provision of care. GIS is a fundamental tool for this purpose.
The chapter begins with a brief review of why geography is important in health care planning and analysis. Then we shall consider the use of GIS and spatial analysis to help manage health care provision, access and utilisation.
Geographical components of health and health care policy
Health care is increasingly focusing on small-area vari-ations in health in order to provide patient-centred health care services. There are ongoing academic debates about the origins of these small-area variations, but commonly they are considered to be driven by differences in individual composition and other contextual factors. Shaw et al. (1999, 2005) note that gender and wealth are key variables that affect individual health and there is a longstanding relationship between small-area deprivation and health outcomes, with more deprived areas being associated with higher mortality rates than relatively less deprived areas. In spite of this realisation, inequalities in health between relatively more deprived and affluent areas continue to increase in many countries.
In the UK, the 1980 Black Report presented the findings of a working group set up in 1977 to examine health inequalities (Black et al., 1980). The report suggested that the UK National Health Service (NHS), set up in 1948, had effectively failed in its drive towards equality and identified that major health inequalities by social class still exist. Similar findings were reported in the 1998 Acheson Report, an independent inquiry into health inequalities, which found that overall health outcomes had improved, but that the class gap had widened, thus suggesting inequality in health outcomes by social class at a local level. A 1999 publication titled The Widening Gap: Health Inequalities and Policy in Britain (Shaw et al., 1999) outlined some of the more extreme local-level health inequalities in Britain, and demonstrated the clear impacts of social class on life expectancy, rates of limiting long-term illness and infant mortality.
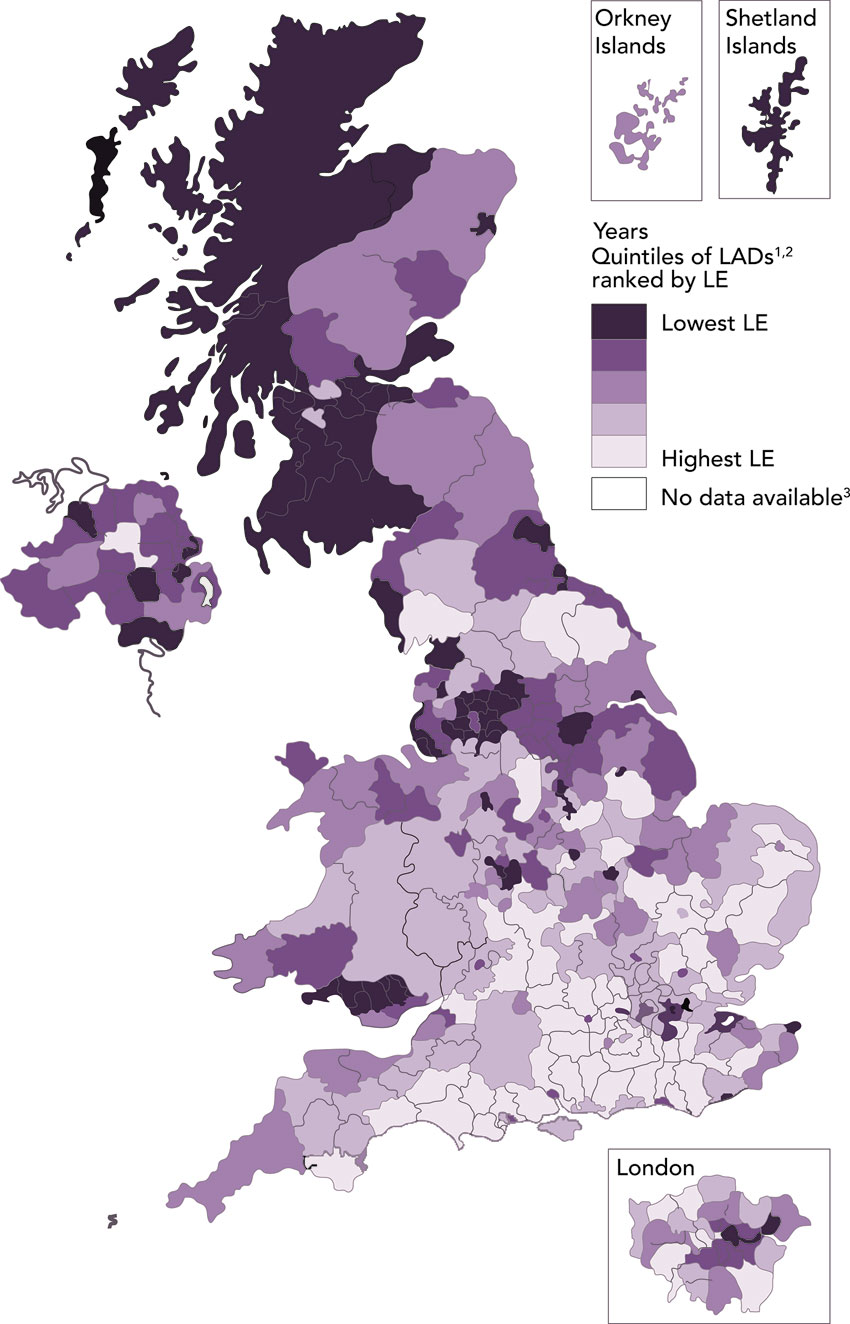
Figure 9.1 Variations in life expectancy (LE) for males at birth by local authority district, UK, 2010–12
Source: ONS (2014)
Shaw et al. (2005) and Dorling (2013) provide excellent overviews of health inequalities in Britain (especially since the 2000s) exploring the link with deprivation and poverty. Figure 9.1 shows more recent UK data and clearly highlights a high degree of spatial clustering of low life expectancy around locations such as Scotland, South Wales and northern England, and a broader distribution of long life expectancy across much of the south-east of England. Even within deprived areas there are pronounced variations in mortality rates. Tunstall et al. (2011) outline that broader socio-demographic factors, including ethnicity, have a pronounced impact on small-area health variations. Since there is a tendency for many of these groups to cluster, especially within urban areas, there are clear issues here for health care planning.
Figure 9.2 shows similar spatial variations for predicted heart disease (CVD) in the US between 2014 and 2024 (Yang et al., 2015). In this case, the east–west variations are as striking as the north–south variations in the UK (showing a clear link again with US variations in poverty which show a similar pattern), although the deep south also shows high risk.
There are also likely to be substantial spatial variations in health within a city or part of a city. Figure 9.3 shows an example of a recent London atlas produced by the geographer James Cheshire. Using the London underground map is a novel way of showing how (in this case) infant mortality rates vary across London, in comparison to child poverty rates mapped as an overlay. Similarly, Figure 9.4 shows a map of Michigan in the US, by county, displaying four levels of coronary heart disease age-adjusted five-year hospitalisation rates, by patients’ county of residence. The map clearly shows higher rates of heart disease in the downtown, less affluent area of the city.
Figure 9.2 Variations in likely future patterns of male heart disease in the US
Source: Yang et al. (2015)
Figure 9.3 Spatial variations in life expectancy in London plotted against child poverty
Source: Cheshire (2012)
Figure 9.4 Variations in hospitalisation rates for heart disease across Michigan, US
Source: CDC (undated), www.cdc.gov/dhdsp/maps/gisx/mapgallery/maps/pdf/mi-chd-hosprates.pdf
In Chapters 7 and 8 we noted the use of GIS to create hot spot maps. There are many examples of these in the GIS literature in relation to health care. Figure 9.5 shows a hot spot map for colorectal cancer between 1998 and 2003 across Iowa, US (Beyer and Rushton, 2009). The proportion of cases has been standardised by age and sex and smoothed using adaptive filter density estimation. Each rate is based on the closest 50 expected cases on a three-mile grid. Red areas indicate higher rates than expected and blue rates lower than expected (given the statewide rate). Many of these hot spots are in areas of lower income.
Residents of lower income areas might also have poorer lifestyles in terms of higher propensities to smoke and consume alcohol and lower propensities to consume fresh fruit and vegetables (and generally have a poorer diet than more affluent persons). Morris et al. (2017) profiled women consumers in a large UK survey by geodemographics (see Chapter 5 for a review of geodemographics). They used data-driven dietary patterns in order to show how these varied by geodemographic group nationally. Then they mapped estimated dietary patterns across Leeds, UK, based on local geodemographics. The better quality ‘Higher Diversity Traditional Omnivore’ and ‘Health Conscious’ dietary patterns were seen to be most likely to be present in North Leeds (in the higher income areas) while ‘Traditional Meat, Chips and Pudding Eaters’ and ‘Monotonous Omnivores’ were seen to be more likely in the deprived inner suburbs to the south and east of the city centre (Figure 9.6).
Poor diet has been linked in many studies to higher rates of obesity. GIS has also been used in recent years to explore spatial variations in patterns of obesity. Drewnowski et al. (2007, 2014) have rare access to obesity data for Seattle in the US and have mapped those distributions with interesting results. Figure 9.7 shows an example of this, with higher rates of obesity seen in the southern districts of Seattle, generally in poorer areas, non-white locations with lower property values (which they have shown to be an important predictor of obesity patterns in Seattle).
But obesity is not simply associated with poor diet and low-income areas. Edwards and Clarke (2009) undertook a geodemographic profile of children in Leeds who were categorised as overweight or obese. They showed that there was a broad correlation with deprivation (the usual correlation found in the literature as noted above) but that some more affluent areas did have obese children (perhaps to do with more sedentary lifestyles). Based on this analysis they then ranked schools as hot or cold spots for obesity based on what we might expect rates to be given the socio-demographics of the catchments of each school. Thus, schools in high-income areas with high obesity rates were hot spots, while schools in low-income areas with low obesity rates were cold spots.
Figure 9.5 Hot and cold spot mapping of late-stage colorectal cancer in Iowa, US, 1998–2003
Source: Beyer and Rushton (2009)
Figure 9.6 Locating the geography of poorer diets, Leeds, UK: estimated ‘Traditional Meat, Chips and Pudding Eater’ dietary pattern in Leeds at the OA level
Source: Morris et al. (2017)
In addition to low income and poverty, such hot spots could be caused by the physical environments in which people live, work and socialise. By its very nature, exposure to environmental factors tends to be spatially clustered, but behavioural or environmental factors are also inherently linked to small geographic areas, such as neighbourhoods, since individuals exhibiting these behaviours tend to spatially cluster. In Chapter 1 we showed the famous map in spatial epidemiology of cholera patients in Soho London in the 19th century. John Snow was the GP who located the source of a cholera outbreak in Soho by mapping the locations of patients with cholera. By focusing on the centre of the distribution map he created, the contaminated drinking tap was able to be identified as the most likely source of the outbreak. Since then many other spatial mapping exercises have been undertaken. Figure 9.8 shows the work of Stan Openshaw and colleagues in 1988, mapping each incidence of childhood leukaemia in the North of England and then plotting the hot spots (or blobs as he called them). The research had anticipated finding greater numbers of childhood leukaemia around Sellafield nuclear power station (Cluster b to the west of the map). However, Openshaw et al. were able to find equally alarming clusters in other locations not predicted in advance. Cluster a was, for example, the largest. Subsequent investigation suggested that a waste incinerator plant in Gateshead (near Newcastle) was the most likely source of the contamination.
Figure 9.7 Obesity in Seattle, Washington, US
Source: Drewnowski et al. (2007)
Figure 9.8 Plotting hot spots of childhood leukaemia in the North of England
Source: Openshaw et al. (1988)
Figure 9.9 shows another example of potential small-area variations in environmental contamination, this time in New York. Corburn et al. (2006) plotted asthma hospitalisation rates by small area across Belmont, Bronx, Harlem and Brooklyn. They showed the higher rates of hospital cases around the poorest neighbourhoods, a mixture of contamination from poor housing, high inner-city traffic counts and pollution from inner-city noxious industries.
Figure 9.9 Variations in hospitalisation rates for asthma in New York, 1996–2000
Source: Corburn et al. (2006)
Using GIS to analyse health care provision
We have established that demand for health services is spread unevenly across space, broadly in line with population distribution, but also driven by a complex range of individualised and area-based factors. Health services, however, have to be provided at discrete locations, such as hospitals, GP surgeries, pharmacies and walk-in centres. Due to this, it is inevitable that there will always be inequalities in the provision of health care, as it is impossible to provide a universal coverage of services at the point of demand.
There is a hierarchy of health care provision, with pharmacies and GP surgeries being widely distributed at a neighbourhood level, while more specialised services such as hospitals tend to be more centralised. Access to primary care is important as a ‘gateway’ to the whole health system. One major issue for health care planners is the need for specialisation. Expensive facilities and specialised staff cannot be deployed uniformly and must be centralised at key hospital sites to achieve the economies of scale and high patient volumes required to make provision viable. For patients, this is likely to result in higher travel cost and time and therefore it is important to consider notions of access to health care. GIS is a fundamental tool here, and has been used widely to consider the physical separation of supply and demand – taking account of distance and travel times to appropriate health services.
In one such example, Haynes et al. (1999) calculated access to hospitals and GP surgeries using straight-line distance from UK census ward centres (to hospitals), or census enumeration districts (to GPs). In this case, small-area population distribution was used as a proxy for demand for services, taking account of underlying conditions such as deprivation. They found that many inner-city deprived communities, where health needs might be greater, enjoy good access to health care facilities, which are often located nearby. However, many of the examples that follow identify that straight-line distance is a very crude measure of access, with factors such as cost, time and inconvenience being important considerations, alongside more practical measures of access which include availability of public transport, opening hours, availability of appointments, etc.
Martin et al. (2002) used GIS-based analysis to investigate access measures between general district hospitals and the underlying distribution and health needs of the population in Cornwall, UK. Cornwall is a rural area in south-west England, characterised by poor geographic access. They incorporated drive time data to measure access to district hospitals, using rates of limiting long-term illness as a proxy for small-area health need. A digital road network was used to create a series of raster-based population layers and travel time ‘cost’ surfaces – these are continuous surfaces made up of a series of cells, such that from any given point, the estimated travel time to the nearest hospital can be calculated, taking account of the underlying road network and road speeds (Figure 9.10). They demonstrate the improvements in evaluating health care access that can be achieved by using road travel time in place of straight-line distance.
Lovett et al. (2002) carried out a similar investigation in East Anglia, another rural area in the UK characterised by poor access. They specifically considered travel times to GP practices. With access to patient registers, they were able to calculate sophisticated cost surface access measures based on both road travel time and public transport (public bus and other community transport services). Figure 9.11 provides an example of the travel time surfaces they produced. They identified that while only 10% of residents faced a car journey of over ten minutes to reach a GP practice, for those without access to private transport, 13% were not able to reach a GP surgery by bus after taking account of timetables and the availability of a return journey. They found that those residents with higher health needs tended to be located in remote rural areas, where low personal mobility and lack of any form of public transport made access to primary care almost impossible.
This form of analysis reveals important concerns regarding access to primary care (with implications for referrals to secondary care), and implies the existence of an ‘inverse care law’, whereby those most in need of care (in this case elderly or more deprived rural residents with poor health) lack effective health care provision that is accessible to their needs. Lovett et al. (2002) also demonstrated that measures of access need to take account of public transport, since many of the groups with low personal mobility and lacking access to private transport have greater health needs. In addressing this need, Martin et al. (2008) present a software tool created to analyse public transport timetable data in order to analyse bus travel times. They explored bus travel times to Derriford Hospital in Devon, England, taking account of the underlying demographic and socio-economic characteristics of the population and, in common with Lovett et al. (2002), identified high concentrations of less mobile elderly populations and those with self-reported limiting long-term illness suffering poor access to health care services.
Figure 9.10 Stages in the creation of a road travel time cost surface for hospital accessibility
Source: Martin et al. (2002)
Figure 9.11 Estimated travel time by car to nearest GP surgery
Source: Lovett et al. (2002)å
Figure 9.12 Access to adult specialist inpatient hospices in England and Wales based on travel time
Source: Gatrell and Wood (2012)
There is also increasing concern surrounding access to palliative or end-of-life care for patients that are close to death and who would prefer to die at home or within a specialist hospice, rather than within a hospital or other health facility. Gatrell and Wood (2012) examine variations in small-area geographic access to specialist hospices relative to estimated need. In this case, need (or demand) is determined by cancer mortality rates, as a major cause of premature death in the UK. Gatrell and Wood (2012) measure access relative to demand using travel time at the LSOA level, each containing around 1,500 residents. They also account for the size/capacity of each facility, and consider their accessibility scores relative to area-based deprivation. Figure 9.12 shows an extract from their findings and suggests that pronounced geographic variations in access to these services exist.
Estimates of accessibility often go hand in hand with more sophisticated measures of access. Spatial interaction models are a well-established technique for calculating accessibility or provision indicators based on how far people travel (or would have to travel) to reach facilities (the size or quality of which can also be taken into account). Good examples appear in Clarke and Wilson (1994) and Clarke et al. (2002). Morrissey et al. (2010, 2015) first estimated the number of persons with depression in Ireland using spatial microsimulation (see again Chapter 6 and good overviews provided by Tanton and Edwards (2012) and O’Donoghue et al. (2013)). Figure 9.13a shows the spatial pattern of depression as estimated. Greater concentrations can be seen in the more rural but less affluent census tracts to the north and west of Ireland. Figure 9.13b then shows an accessibility score based on spatial interaction models. There is clearly a very worrying mismatch here – areas with high rates of estimated depression have the lowest access to mental health care facilities (so many of which are centralised around the capital of Dublin).
Figure 9.13 Measuring both small-area variations in depression in Ireland and access to mental health care facilities
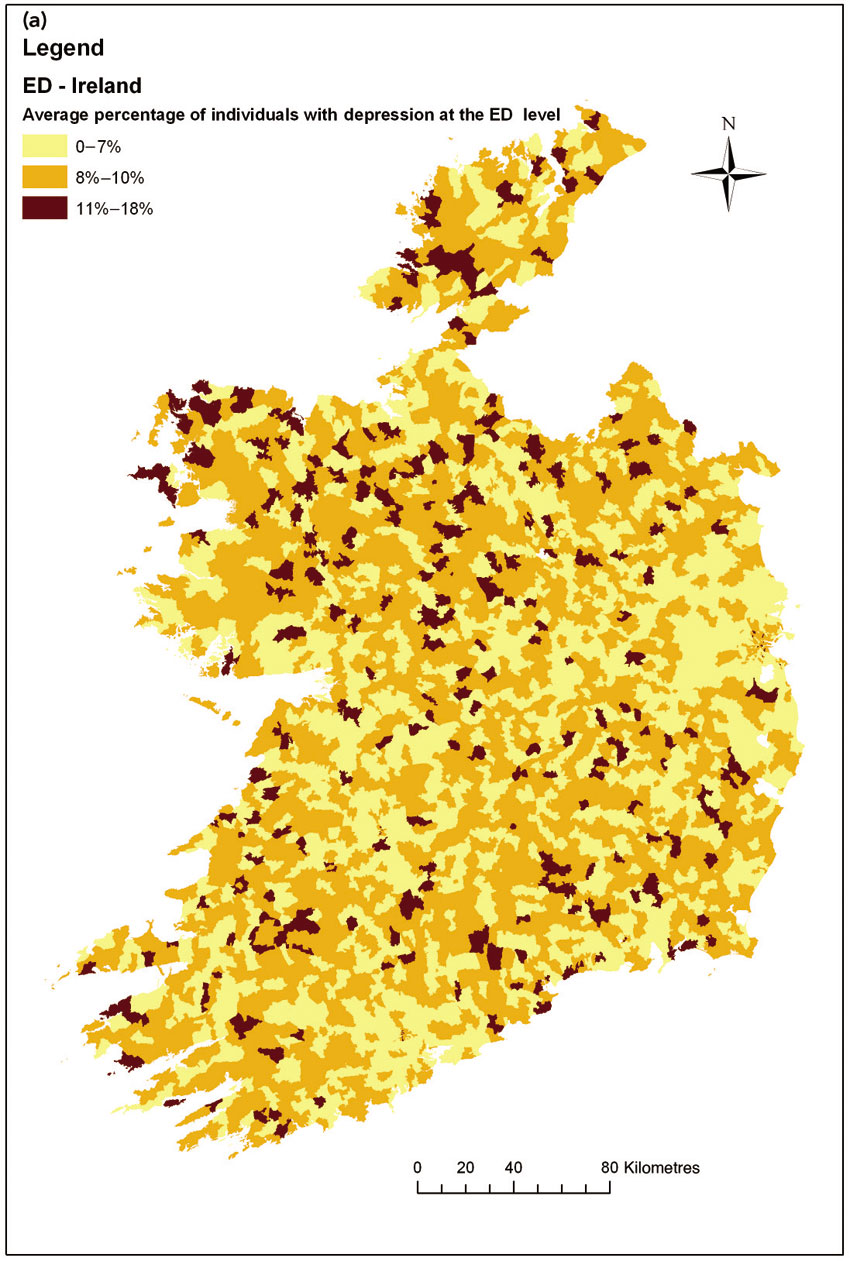
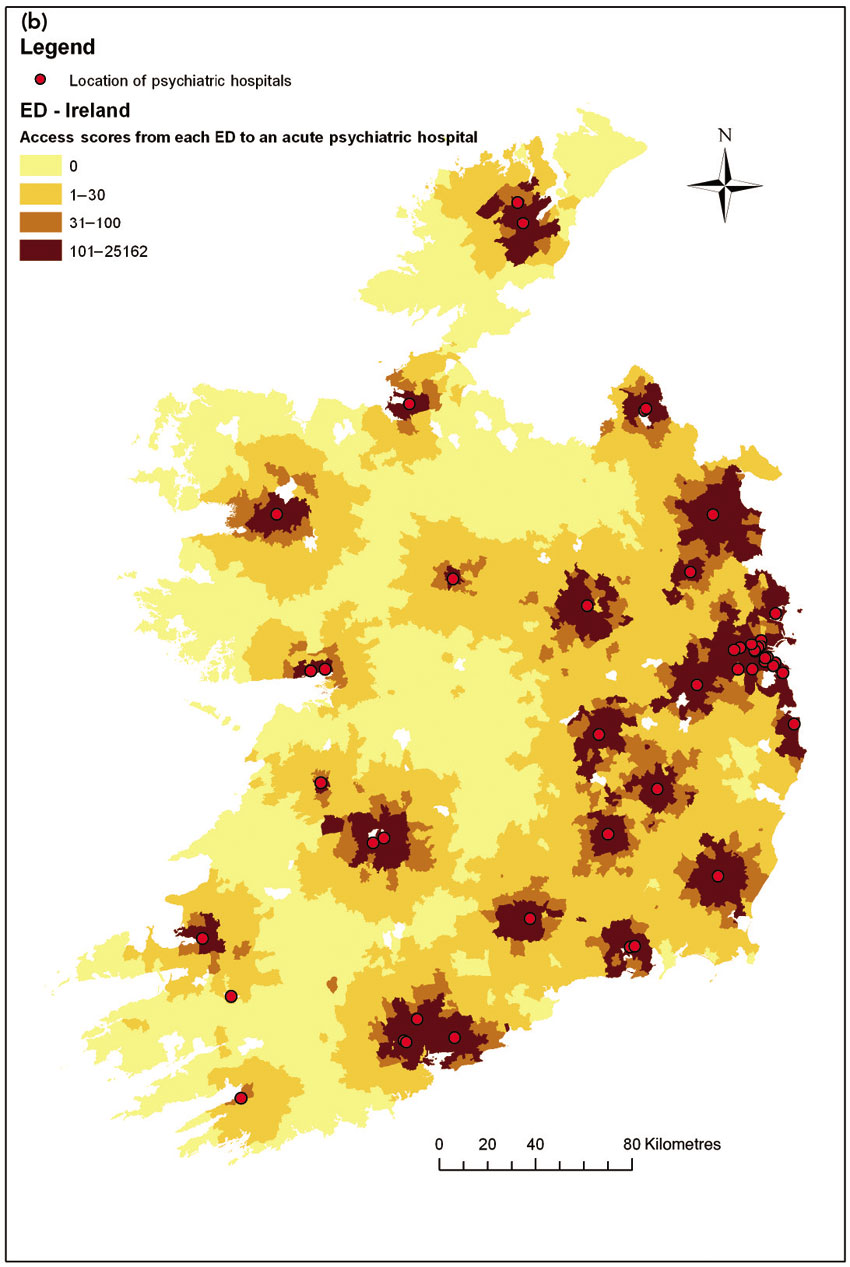
Source: Morrissey et al. (2010)
Health care access has improved at a local level in a number of countries with the introduction of walk-in centres and smaller GP practices. These provide dispersed, localised provision of services (although this might be at the expense of facilities, staffing levels and opening hours). Tomintz et al. (2008) investigate the demand for and distribution of one form of localised health care provision, neighbourhood-level stop smoking clinics in Leeds, UK. Stop smoking services tend to be colocated with other health facilities, but might offer restricted service hours or appointment times. For example, Tomintz et al. (2008) note that there were a total of 51 smoking cessation service points in Leeds, but that only nine offer services on a Friday. Consequently, provision of (and access to) these services varies on different days of the week, and more complex modelling is required. You will be able to consider the provision of these services in Leeds in the associated practical activity.
Tomintz et al. (2008) also used a spatial microsimulation approach to estimate the distribution of smokers across Leeds, and then used location-allocation modelling (introduced in Chapter 4) to investigate the extent to which the current provision of these services matches the optimum spatial distribution and locations for these services based on the inferred demand, at any given time. Figures 9.14 and 9.15 show extracts from the paper, and identify that access to these services for the target population varies considerably by day of the week, with service provision and access being worse on a Friday and Saturday, when fewer clinics are open. Using location-allocation modelling, they identify that a re-distribution of service locations, while maintaining the overall daily levels of provision, could result in considerable improvements in overall patient access (even though some individuals may have to travel further), especially on a Friday.
The type of analysis presented by Tomintz et al. (2008) assists health care planners in identifying hypothetically ideal locations for services such as smoking cessation, but it must be acknowledged that due to long-term investment in resources and infrastructure in particular locations, health service provision cannot constantly shift locations and service delivery points in order to meet the ever-changing distribution of demand. Nonetheless, increasingly, colocation of services such as stop smoking clinics within other facilities such as supermarkets could enable short-term provision of services in an area where existing infrastructure does not exist but a need has been identified.
Figure 9.14 Location-allocation results for smoking cessation services in Leeds, UK, on selected days of the week
Source: Tomintz et al. (2008)
Figure 9.15 Actual smoking cessation centres compared with optimal centres for Leeds, UK, on a typical Friday
Source: Tomintz et al. (2008)
Tomintz et al. (2008) used a location-allocation model for finding optimal locations. Other forms of optimisation models are increasingly seen in the literature to provide similar solutions. Figure 9.16 shows an example based on the optimal location of ambulance centres in Hong Kong (Sasaki et al., 2010).
They used a different form of optimisation model, a genetic algorithm, to optimally locate ambulance stations within a GIS environment. Figure 9.16a shows the existing distribution of emergency cases. Figure 9.16b shows the current location of 27 ambulance stations serving Hong Kong, while Figure 9.16c shows the optimal location of 27 ambulance stations based on emergency cases in 2007. Finally, Figure 9.16d shows the optimal location of 27 ambulance stations based on predicted emergency cases for 2030. The solid circles show optimal locations that are the same as current locations, while the ringed circles show new locations; hollow circles with a cross show current sites not selected during optimisation. The modified GGA was run to select 27 ambulance site locations evaluated on the network distance between each census centroid, weighted by the count of emergency cases. For each census area, the nearest site location was also calculated to indicate the catchment or service area for each ambulance location. Of the 27 locations, 23 were existing stations but four were not, indicating that some improvement in ambulance accessibility could be achieved with some re-allocation of resources (see also Comber et al. (2011) for another example of finding optimal locations for ambulance stations).
Figure 9.16 Emergency cases and current and optimal ambulance locations with their catchment areas in Hong Kong
Source: Sasaki et al. (2010)
Access to health care has also been increased through the introduction of non-geographic services such as NHS direct – a nurse-led advice line and web-based service where health advice can be sought at any location and time with no need for direct doctor contact. These services have an important role in providing patient reassurance in the out-of-hours period and might appeal to certain sectors of the community, such as young males, who might be less likely to visit their GP for face-to-face consultations. Turnbull et al. (2011) investigate the use of telephone-based advice from primary care centres (PCCs) to manage out-of-hours calls to GPs. Much of the out-of-hours services are managed by telephone, with some patients being asked to travel to the PCC or receiving a follow-up home visit. These services should improve health access for those unable to reach the PCC. Turnbull et al. (2011) identify that geography – and specifically distance – play an important role in determining the advice given, with patients living further than six kilometres from the primary care centre more likely to be given telephone advice only, and less likely to be seen face-to-face. Consequently, in spite of efforts to improve access through the use of telephone-based services; it appears that geographical inequalities in terms of equity access exist.
Inequalities in service provision might not always result from poor access or availability. Even where access and the availability of services offered are considered to be good, there might be inequalities between different areas in terms of the quality of services provided, or the resulting health outcomes. For example, after receiving primary care, small-area variations may exist in referral or admission rates, or in expenditure on certain health conditions. In order to improve patient outcomes and make effective use of the health care resources provided, the UK NHS is taking steps to identify and reduce these variations. Visualisation and spatial data analysis are essential tools in identifying variations in activity rates (e.g. referral), expenditure, quality and outcomes.
This chapter has identified that health and the management of health care provision and service delivery are inherently geographical concepts. Individual health is driven by personal geographies which can affect risk of ill-health, access to health care and health outcomes. In particular, there is a clear relationship between small-area deprivation and health needs, although health policy seeks to reduce these inequalities and variations in health, striving for a consistent level of care relative to need.
We have identified that GIS is an important tool for visualising health inequalities, identifying small-area health needs and evaluating access to health care facilities. We have explored a range of examples in which GIS and spatial data analysis have been applied in order to evaluate the need for and provision of care to meet the needs of small-area populations. Tools to identify area-based health, driven by underlying demographic and socio-economic indicators have been identified, and a series of studies have been presented which apply increasingly sophisticated measures of health access. We have seen how modelling techniques (techniques such as microsimulation and location-allocation models), when coupled with GIS, can be applied to evaluate the provision of services, and we have explored indicators of health outcomes.
|
The accompanying practical (Practical 5: Health care analysis) explores the interrelationships between health needs and service provision. You consider access to smoking cessation clinics in the UK city of Leeds, drawing on the discussion above. You briefly visualise estimated ‘need’ for smoking cessation services and use buffer and overlay techniques to consider provision of smoking cessation clinics. We introduce a new and powerful technique – location-allocation modelling – in order to optimise the provision of these services.
All website URLs accessed 30 May 2017.
Beyer, K. M. M., & Rushton, G. (2009) Mapping cancer for community engagement. Preventing Chronic Disease, 6(1), A03.
Black, D., Morris, J., Smith, C., & Townsend, P. (1980) Inequalities in Health: Report of a Research Working Group, Department of Health and Social Security, London.
Centers for Disease Control and Prevention (CDC) (undated) Michigan hospitalisation rates for coronary heart disease by county. Centers for Disease Control and Prevention, Atlanta, GA. Available from: www.cdc.gov/dhdsp/maps/gisx/mapgallery/mi_chd_hosprates.html.
Cheshire, J. (2012) Lives on the line: life expectancy and child poverty as a Tube map. Available from: http://spatial.ly/2012/07/lives-on-the-line/.
Clarke, G. P., & Wilson, A. G. (1994) A new geography of performance indicators for urban planning, in C. S. Bertuglia, G. P. Clarke, & A. G. Wilson (eds) Modelling the City, Routledge, London, 55–81.
Clarke, G. P., Eyre, H., & Guy, C. (2002) Deriving indicators of access to food retail provision in British cities: studies of Leeds, Bradford and Cardiff. Urban Studies, 11, 2041–2060.
Comber, A. J., Sasaki, S., Suzuki, H., & Brunsdon, C. (2011) A modified grouping genetic algorithm to select ambulance site locations. International Journal of Geographical Information Science, 25(5), 807–823.
Corburn, J., Osleeb, J., & Porter, M. (2006) Urban asthma and the neighbourhood environment in New York City. Health & Place, 12(2), 167–179.
Curtis, S. (2010) Space, Place and Mental Health, Ashgate Publishing Ltd, London.
Curtis, S., & Rees Jones, I. (1998) Is there a place for geography in the analysis of health inequality? Sociology of Health and Illness, 20(5), 645–672.
Dorling, D. (2013) Unequal Health: The Scandal of Our Times, Policy Press, Bristol.
Drewnowski, A., Rehm, C. D., & Solet, D. (2007) Disparities in obesity rates: analysis by ZIP code area. Social Science & Medicine, 65(12), 2458–2463.
Drewnowski, A., Moudon, A. V., Jiao, J., Aggarwal, A., Charreire, H., & Chaix, B. (2014) Food environment and socioeconomic status influence obesity rates in Seattle and in Paris. International Journal of Obesity, 38(2), 306–314.
Edwards, K. L., & Clarke, G. P. (2009) The design and validation of a spatial microsimulation model of obesogenic environments for children in Leeds: SimObesity. Social Science and Medicine, 69(7), 1127–1134.
Gatrell, A. C., & Elliott, S. J. (2014) Geographies of Health: An Introduction, Wiley, Chichester.
Gatrell, A. C., & Wood, D. J. (2012) Variation in geographic access to specialist inpatient hospices in England and Wales. Health & Place, 18(4), 832–840.
Haynes, R., Bentham, G., Lovett, A., & Gale, S. (1999) Effects of distances to hospital and GP surgery on hospital inpatient episodes, controlling for needs and provision. Social Science and Medicine, 49, 425–433.
Kearns, R. A., & Joseph, A. E. (1993) Space in its place: developing the link in medical geography. Social Science & Medicine, 37(6), 711–717.
Lovett, A., Haynes, R., Sunnenberg, G., & Gale, S. (2002) Car travel time and accessibility by bus to general practitioner services: a study using patient registers and GIS. Social Science and Medicine, 55, 97–111.
Martin, D., Wrigley, H., Barnett, S., & Roderick, P. (2002) Increasing the sophistication of access measurement in a rural healthcare study. Health & Place, 8, 3–13.
Martin, D., Jordan, H., & Roderick, P. (2008) Taking the bus: incorporating public transport timetable data into health care accessibility modelling. Environment and Planning A, 40, 2510–2525.
Morris, M., Clarke, G. P., Edwards, K. L., Hulme, C., & Cade, J. E. (2017) Exploring small area geographies of obesity in the UK: evidence from the UK Women’s Cohort Study, in J. Lombard, G. P. Clarke, & E. Stern (eds) Applied Spatial Modelling and Planning. Routledge, London, 280–299.
Morrissey, K., Clarke, G. P., Hynes, S., & O’Donoghue, C. (2010) Examining the factors associated with depression at the small area level in Ireland using spatial microsimulation techniques. Irish Geography, 43(1), 1–22.
Morrissey, K., Clarke, G. P., Williamson, P., Daly, A., & O’Donoghue, C. (2015) Mental illness in Ireland: simulating its geographical prevalence and the role of access to services. Environment and Planning B: Planning and Design, 42, 338–353.
O’Donoghue, C., Ballas, D., Clarke, G. P., Hynes, S., & Morrissey, K. (2013) Spatial Microsimulation for Rural Policy Analysis, Springer, Berlin.
Office for National Statistics (ONS) (2014) Life Expectancy at Birth and at Age 65 by Local Areas in the United Kingdom: 2006–08 to 2010–12, ONS, London.
Openshaw, S., Charlton, M., Craft, A. W., & Birch, J. M. (1988). Investigation of leukaemia clusters by use of a geographical analysis machine. The Lancet, 331(8580), 272–273.
Sasaki, S., Comber, A. J., Suzuki, H., & Brunsdon, C. (2010) Using genetic algorithms to optimise current and future health planning – the example of ambulance locations. International Journal of Health Geographics, 9(4).
Shaw, M., Dorling, D., Gordon, D., & Davey Smith, G. (1999) The Widening Gap: Health Inequalities and Policy in Britain, Policy Press, Bristol.
Shaw, M., Davey Smith, G., & Dorling, D. (2005) Health inequalities and New Labour: how the promises compare with real progress. British Medical Journal, 330, 1016–1021.
Tanton, R., & Edwards, K. (eds) (2012) Spatial Microsimulation: A Reference Guide for Users (Vol. 6). Springer Science & Business Media, Berlin.
Tomintz, M., Clarke, G., & Rigby, J. (2008) The geography of smoking in Leeds: estimating individual smoking rates and the implications for the location of stop smoking services. Area, 40(3), 341–353.
Tunstall, H., Mitchell, R., Gibbs, J., Platt, S., & Dorling, D. (2011) Socio-demographic diversity and unexplained variation in death rates among the most deprived parliamentary constituencies in Britain. Journal of Public Health, 34(2), 296–304.
Turnbull, J., Pope, C., Martin, D., & Lattimer, V. (2011) Management of out-of-hours calls by a general practice cooperative: a geographical analysis of telephone access and consultation. Family Practice, 28(6), 677–682.
World Health Organization (WHO) (1946) Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference. International Health Conference, New York, 19–22 June.
Yang, Q., Zhong, Y., Ritchey, M., Loustalot, F., Hong, Y., Merritt, R., & Bowman, B. A. (2015) Predicted 10-year risk of developing cardiovascular disease at the state level in the US. American Journal of Preventive Medicine, 48(1), 58–69.