CHAPTER 28
Ventilators
Introduction
A mechanical ventilator is a fundamental component of modern anesthetic practice. The ventilator performs two critical functions for an anesthetized patient: oxygenation and ventilation. Oxygenation supplies the lungs (and thus, red blood cells) with oxygen. Oxygen is essential for the metabolic function and life of every cell. Supplying oxygen is the essential function of the lungs; its delivery, along with nutrients, is the primary function of the heart and blood vessels. (See Chapter 4, Cardiovascular Anatomy and Physiology.) Some tissues, particularly the brain, consume oxygen very rapidly and without it will soon die. Ventilation, which we more commonly call “breathing,” is the exchange of gas in and out of the lungs. It not only supplies oxygen but also removes waste gases such as carbon dioxide from the lungs, allowing the body to maintain a physiologic acid-base balance. Removal of waste is also essential but is not as time sensitive or life critical as oxygenation. Ventilation by the anesthesia machine is also used to administer and remove inhaled anesthetics.
While awake, patients maintain spontaneous ventilation by regularly generating negative intrathoracic pressures with contractions of the diaphragm, causing air to flow into the lungs (see Chapter 7, Respiratory Anatomy and Physiology). After induction of general anesthesia, respirations are often depressed or absent, depending on the choice of anesthetics and muscle relaxants (i.e., neuromuscular junction–blocking agents). Ventilation and oxygenation are then accomplished by administering positive pressure to the patient’s airway, leading to the flow of oxygen and anesthetic gases into and out of the lungs. At this point, the airway is often secured with an endotracheal tube (see Chapter 18, Principles of Airway Management).
When the mechanical ventilator is not engaged, positive pressure can be manually delivered to the breathing circuit by squeezing the breathing reservoir bag with the adjustable pressure-limiting (APL or “pop-off”) valve partially closed (see Chapter 24, The Anesthesia Machine). Alternatively, the breathing circuit can be placed in continuity with the ventilator, which delivers positive pressure breaths at a desired frequency. When the positive pressure is released, the patient passively exhales gases, including waste carbon dioxide, back into the breathing circuit.
Although both manual and mechanical ventilation are capable of providing oxygen, delivering anesthetic gases, and removing carbon dioxide, mechanical ventilation has several distinct advantages. First, it frees the anesthesia provider from having to perform continuous manual ventilation throughout the case. Second, it allows the anesthesia provider to set specific pressures and/or volumes for each breath, allowing for more precise control of ventilation than is possible manually. This fine control is critical when small changes in ventilatory parameters are required to optimize a complex patient’s respiratory function. Third, modern ventilators can deliver positive pressure waveforms that are difficult to achieve with manual ventilation, such as pressure control ventilation or end-inspiratory pauses (“holds”). Fourth, modern ventilators are linked to pressure monitoring systems that give important information about lung compliance. Thus, they are able to instantly release positive pressure if a threshold (maximum) pressure is reached, providing an additional measure of safety (for instance, when a patient coughs or strains against the ventilator). Finally, in certain modes, mechanical ventilators can even assist a patient’s spontaneous breathing by detecting a patient’s respiratory efforts and synchronously delivering positive pressure at the appropriate times.
Ventilator Modes
Modern ventilators operate in specific modes that define the overall pattern of positive pressure delivery. The anesthesia provider independently programs parameters specific to each patient/procedure. Basic ventilator modes are distinguished based on two important characteristics: whether the ventilator delivers a fixed tidal volume or a specific inspiratory pressure, and whether the ventilator is triggered by an internal timer or by the patient’s own respiratory efforts.
Volume control ventilation delivers a set volume (also referred to as the tidal volume) with each positive pressure breath. These breaths are delivered at a provider-determined frequency, and thus, this mode provides a predictable minute ventilation (minute ventilation = ventilator rate × tidal volume). One major advantage of the volume control mode is the consistency of minute ventilation over prolonged periods of time, even during changes in lung expandability (known as lung compliance—see Chapter 7, Respiratory Anatomy and Physiology). For example, if a patient suddenly bears down and stiffens the chest muscles (decreasing chest compliance), the ventilator needs more pressure to expand the lungs than when the patient was completely relaxed. The ventilator will increase the inspiratory pressure accordingly and still deliver the same tidal volume as long as the inspiratory pressure limit (Pmax, often set to 40 cm H2O in adults) is not reached. However, once the pressure limit is reached, the ventilator will stop delivering positive pressure and an alarm will sound, warning the anesthesia provider of the high airway pressure. One disadvantage of this mode is that it often requires slightly higher absolute peak pressures than other modes to achieve the same minute ventilation (Fig. 28.1A). Also, the lungs spend less time at larger lung volumes compared to pressure control ventilation, which may decrease the time available for gas exchange in some portions of the lung.
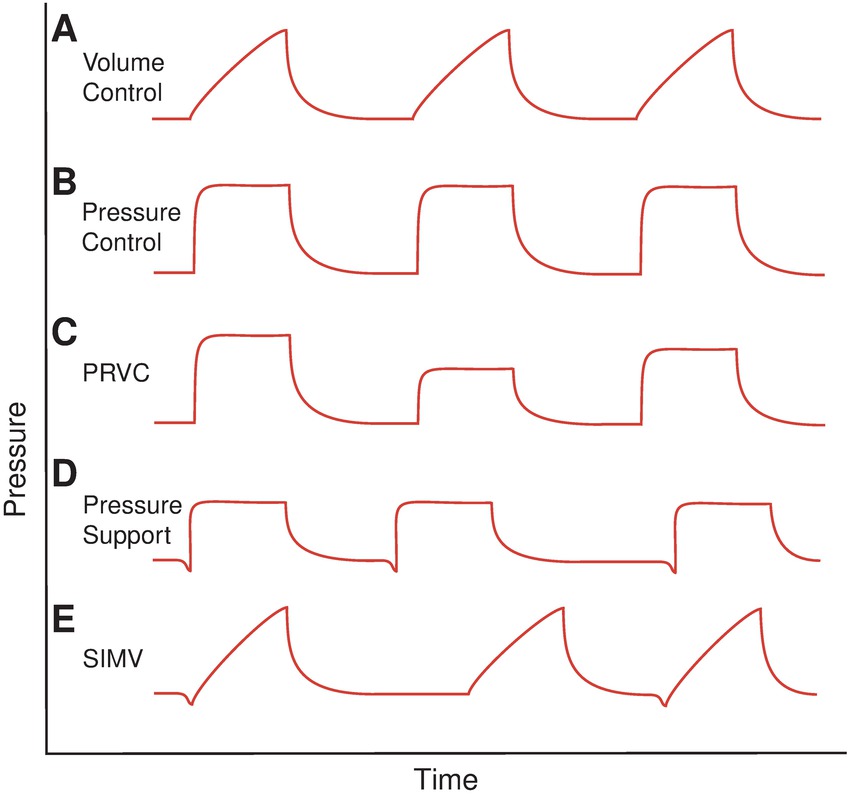
FIGURE 28.1. Pressure-time waveforms of different ventilation modes. A: In volume control ventilation, pressure steadily increases during inspiration, as gas (typically at a constant flow rate) fills the lungs. During expiration, pressure drops quickly as the chest and diaphragm passively recoil. Breaths are delivered at regular time intervals. B: In pressure control ventilation, the ventilator quickly reaches the plateau (control) pressure and maintains this throughout the breath. This requires an increased respiratory flow at the outset of the breath and a small delay for the ventilator to reach the target pressure. Expiratory flows are passive and follow the same waveform as in volume control. C: In pressure-regulated volume control (PRVC) ventilation, tidal volumes are kept constant and delivered at a set rate, using a flat plateau pressure waveform. Feedback control from each exhaled breath is used to adjust the inspiratory plateau pressure used for the subsequent breath, allowing the ventilator to maintain consistent tidal volumes as patient compliance changes. D: In pressure support ventilation, the patient initiates each pressure-controlled breath by generating negative pressure (note the downward deflections prior to the pressure support), and thus inspiratory timing is dependent on patient effort. E: In SIMV, a volume-controlled breath is delivered with each inspiratory effort. If the patient fails to initiate a breath after a set interval, the ventilator will deliver a volume-controlled breath regardless.
Pressure Control ventilation delivers a set plateau level of positive pressure with each inspiration (Fig. 28.1B). The actual tidal volume delivered depends on the patient’s lung compliance: more compliant lungs will expand more easily and thus receive a higher tidal volume at the same pressure control settings than less compliant (stiffer) lungs. One advantage of this mode is that for any given peak pressure, the patient will spend more time at larger lung volumes and have a larger tidal volume, than that reached during volume control ventilation. It may be particularly useful in patients with very stiff lungs, or those in whom it is otherwise difficult to sustain adequate ventilation without resorting to very high inspiratory pressures. A disadvantage of this ventilator mode is that minute ventilation can change substantially if the patient’s pulmonary compliance changes. However, this can be easily countered by programming the alarms on the ventilator to notify the provider when tidal volumes or minute ventilation fall outside of a predetermined range.
A newer ventilator mode known as Pressure Regulated Volume Control (PRVC; Fig. 28.1C) is increasingly becoming incorporated into anesthesia machine ventilators. PRVC combines some of the advantages of both pressure control and volume control ventilation. In PRVC, the anesthesia provider specifies a target tidal volume and respiratory rate, but the anesthesia machine delivers machine-timed breaths using a “pressure control”–type waveform of constant inspiratory pressure throughout the inspiratory phase of the cycle. The machine uses the spirometer in the expiratory loop of the circuit to determine the expired tidal volume and adjusts the inspiratory pressure upward or downward as needed after each breath to achieve the target tidal volume with the subsequent breath. The benefits of this mode are that lower inspiratory pressures are needed to achieve a given tidal volume (as in pressure control ventilation) and that the continuous adjustments allow the machine to maintain desired minute ventilation regardless of changes in the patient’s pulmonary compliance. In the case of a dramatic decrease in compliance (e.g., in the setting of bronchospasm, which would require much higher inspiratory pressures), the ventilator may be unable to achieve the desired tidal volume within the pressure limits set by the provider, in which case the machine should sound an audible alarm.
All of the aforementioned ventilator modes are designed to deliver a set number of breaths per minute (the respiratory rate) on a regularly timed basis. This is absolutely necessary when an anesthetized patient is paralyzed and unable to breathe spontaneously. However, many anesthetics do not require complete muscle paralysis, and these patients may continue to make respiratory efforts while fully anesthetized. Modern ventilators are able to assist these efforts by synchronizing positive pressure delivery with a patient’s own respiratory rate. This assistance helps to counter the respiratory depressant effects of many anesthetics and the increased work of breathing through the resistance of an endotracheal tube.
In pressure support ventilation, the ventilator senses a patient’s inspiratory effort as a drop in breathing circuit pressure and delivers a set level of positive pressure to augment the patient’s tidal volume (see Fig. 28.1D). In this mode, the patient is less likely to breathe in opposition to the ventilator and thus less likely to cough or strain. As this mode requires patient effort to initiate an inspiratory cycle, if the patient stops making ventilatory efforts (or these efforts are too weak to trigger the ventilator), he or she receives no ventilation. For this reason, pressure support modes often have a backup mode that automatically begins timed positive pressure ventilation after a specified time if no breaths are detected (often 30 seconds).
One last commonly employed ventilator mode, synchronized intermittent mandatory ventilation (SIMV), delivers a specified volume synchronously with a patient’s respiratory efforts (Fig. 28.1E). However, it is also programmed to deliver the same volume after a specified time even if the patient has not made any inspiratory efforts during this interval.
More advanced modern ventilators have additional modes, which combine several of the above characteristics. Additionally, more detailed settings such as the ratio of time the ventilator spends in inspiration vs expiration during each respiratory cycle (the I:E ratio) can be changed, which may be useful in managing clinical situations such as bronchospasm.
One commonly used, and clinically important, ventilator function is the ability to maintain positive pressure between breaths, called positive end expiratory pressure (PEEP). Without PEEP, the patient exhales gas back into the circuit until the airway pressure reaches atmospheric pressure. With PEEP engaged, expiratory flow is mechanically stopped when the desired expiratory pressure is reached, and thus, some positive pressure is maintained until the next inspiratory cycle. PEEP prevents lung alveoli from collapsing between breaths and can be of extreme utility in patients with pulmonary edema or obesity. In addition, PEEP is critical in the management of ventilation during many thoracic surgery procedures. However, if the respiratory rate is set so high that the patient does not have time to exhale completely between breaths, airway pressure may never fall back to the PEEP or atmospheric pressure, causing a phenomenon known as breath stacking and a gradual increase in pressures throughout the respiratory cycle.
Clinical Scenarios
Ventilator modes are selected by the anesthesia provider to maximize pulmonary function and gas exchange in different clinical scenarios, based primarily on the patient’s clinical condition and the specific needs of the procedure. It is useful for anesthesia technicians to have a familiarity with some of the common clinical scenarios encountered in the operating room (OR) in regard to how they impact mechanical ventilation.
- Neuromuscular blockade: Many operative procedures, such as open or laparoscopic abdominal surgery, are performed with (provider-induced) complete muscle paralysis, as these facilitate complete immobility and muscle relaxation necessary for optimal operative conditions. As this deep paralysis also prevents the diaphragm from contracting, the patient is unable to initiate a breath and thus absolutely needs a mechanical ventilator mode with timer-controlled breaths (such as volume control or PRVC) rather than a patient-initiated mode such as pressure support. If this timer malfunctions or the mechanical ventilator is disabled for any reason, the patient would need to be manually ventilated by the anesthesia provider; otherwise, they would die within minutes from hypoxia. This underscores why the mechanical ventilator must be watched with vigilance, and why in the setting of ventilator failure, the patient needs to be manually ventilated while the ventilator is fixed. Although it might be possible to continue manually ventilating patients for the remainder of the procedure, manual ventilation would likely require an additional dedicated provider, and if the gas delivery from the anesthesia machine was also compromised, it might also necessitate intravenous (rather than inhaled) anesthesia while the anesthesia technician works to repair or replace the malfunctioning machine.
- Nonparalyzed patients: Not all operative procedures require paralysis, and nonparalyzed patients often will continue to make respiratory efforts under general anesthesia, depending on the specific anesthetic agents and dosages used. Additionally, even after a long abdominal case with paralysis, this paralysis is reversed at the end of the case, so that the patient can breathe spontaneously. In these situations, providers will often choose a ventilator mode in which breaths can be initiated by the patient, such as pressure support or SIMV, so the patient is less likely to breathe in opposition to the ventilator, which could otherwise lead to coughing and straining (often termed “bucking” or “fighting” the ventilator). This can occur when the machine is trying to deliver inspiratory pressures to a patient that is trying to exhale (even under anesthesia), so that high pressures are generated leading to airway/lung irritation and coughing. In this situation, the provider may elect to pause mechanical ventilation and/or deepen the anesthetic to allow the patient to stop coughing.
- Patients with severe lung disease: Anesthesia machines offer many “modes” of ventilation, which providers can set to match patient needs: breaths can be delivered at any set rate or triggered by the patient; at any volume; the pressure delivered can be adjusted (or limited); pressure can be held at the end of breaths (PEEP); and more. As machines come onto the market, additional features are added all the time. These settings, like medications, are selected by the provider to meet patient specific needs.
As an anesthesia technician, you should be aware that intensive care ventilators are more sophisticated than anesthesia machines and offer additional modes of ventilation; they are not, however, capable of mixing in anesthesia gases. Rarely, an intensive care unit patient may have ventilator settings that the anesthesia machine is not capable of delivering and the anesthesia provider may use the intensive care ventilator throughout their anesthetic, in which case a total intravenous anesthetic must be used. Some patients with severe oxygenation problems may not tolerate manual ventilation for transport and the intensive care ventilator may be needed for transportation (see Chapter 51, Patient Transport). Normally, a respiratory therapist will manage the intensive care unit ventilator.
Ventilator Operation
Most mechanical ventilators used in OR environments today can be categorized by the mechanism (the external force) used to compress the gas for each breath: bellows, piston, or turbine. In each of these designs, the gas reservoir is in continuity with the breathing circuit and delivers whatever gas mix is in the circuit to the patient. During inspiration, the external force mechanism compresses the reservoir, pushing the gas into the patient. At the beginning of expiration, the force is released, depressurizing the circuit. As the circuit pressure falls, gas moves out of the patient, driven by the patient’s elastic chest recoil. The ventilator’s gas reservoir refills with a combination of fresh gas from the anesthesia machine and expired gas returning from the patient (which at some point passes through the carbon dioxide absorption canister). Depending on the mode of ventilation, an inspiratory cycle may be based upon achieving a certain desired pressure or delivering a particular volume over a specified amount of time.
Each ventilator model employs different designs to accomplish similar goals. However, all modern anesthesia machine ventilators share certain characteristics:
- A manual/mechanical control switch, which converts between manual and mechanical ventilation. This can be either a manual toggle or a digitally controlled servo. Thus, either the ventilator or the reservoir bag is able to ventilate the patient, but not both simultaneously. When the mechanical ventilator is engaged, the APL valve is bypassed, and compression of the bag does not cause gas to flow into the patient.
- Check valves integrated into the inspiratory and expiratory limbs of the patient breathing circuit (see Chapter 29, Preventing and Solving Anesthesia Machine Problems) to ensure unidirectional gas flow in all spontaneous, manual, and mechanical ventilatory modes. Although not part of the mechanical ventilator per se, properly functioning valves are critical to the function of anesthesia ventilators.
- Excess gas scavenging. Fresh gas from the anesthesia machine is often supplied in excess of what is required for ventilation, so ventilators must have a mechanism to shunt excess gas (particularly at high gas flows) from the ventilatory circuit into the scavenging system (see Chapter 24, The Anesthesia Machine). Additionally, ventilators must contain a valve that isolates the positive ventilator pressures from the scavenging system during inspiration, in order to allow the ventilator to deliver the positive pressure to the patient.
- A PEEP valve, which is either a manual (rotary) valve or a digitally controlled expiratory valve that is able to stop gas return from the patient when a particular circuit pressure has been reached. In some older machines, PEEP is accomplished by attaching a mechanical ball valve to the expiratory limb of the circuit.
- Pressure sensors that measure pressure on the patient side of the circuit. At the very least, circuit pressure can be measured by the analog pressure gauge in line with the circuit, but newer machines often display a digital pressure measurement as well. This digital manometer is often located within the anesthesia machine, and is often used by computer-controlled ventilators to provide feedback control of inspiratory pressures and to manage PEEP.
- Flow sensors that measure gas flow, which are used by the anesthesia machine to determine expiratory flow rates and to calculate tidal volumes. Currently, most anesthesia machines use one flow sensor on the expiratory limb of the circuit. Many newer flow sensors use what is called a “dual hot-wire design,” which uses heated platinum wires to detect variations in temperature gradients due to gas flow through the sensor. As gas flows across the flow sensor, it cools the first wire. This results in an increase in the amount of electrical current needed to maintain the wire’s constant temperature, which is proportional to the gas flow rate. A second platinum wire in the measuring tube is used to compensate for interference from different gases present in the respiratory gas mixture, as different gases (e.g., N2O vs O2) present in the respiratory gas have various thermal conductivities. Some newer machines now measure the flow both going to and coming from the patient, to assist with leak detection within the patient circuit and to detect patients’ spontaneous inspiratory efforts for synchronized breaths.
- Pressure alarms and mechanical pressure-release valves to alert the provider of changes in lung compliance and to prevent pressure-related lung damage (barotrauma).
Gas Delivery Mechanisms
A bellows-type ventilator uses pressurized gas to compress the bellows and thus deliver anesthetic gases to the patient. The bellows are simply a collapsible reservoir in which to store the mixed anesthesia gas. Older bellows ventilators do not require electricity but use manual controls and timers to regulate the flow of pressurized gas into a sealed chamber surrounding the bellows. As the pressure in this chamber increases, the bellows are compressed and anesthetic gas inside the bellows flows into the breathing circuit. At the end of the inspiratory cycle, the pressure in the chamber is released, allowing the bellows to refill with gases from the patient and from the anesthesia machine. This functional bellows design has been in practice for many decades as a mechanical/pneumatic system and has since been enhanced through the addition of electromagnetic valves, which increase precision in gas flow delivery and pressure control.
A diagram of a bellows-type ventilator is presented in Figure 28.2. Note that bellows-type ventilators necessitate an exhaust valve to separate the breathing circuit from the scavenging/overflow system during inspiration. A typical bellows ventilator uses the increased drive gas pressure in the bellows chamber to close the exhaust valve, thus directly uncoupling the ventilator from the scavenging system during inspiration. In the event of a power failure, older bellows ventilators do not require power to generate ventilator pressure. However, because they require pressurized oxygen, they will fail in the absence of pressurized gas and cause a backup tank to run out more quickly in the event of wall oxygen supply failure. Newer bellows ventilators are computer controlled and thus require electrical power in addition to pressurized gas for operation (from wall outlets or a machine’s internal backup battery system).
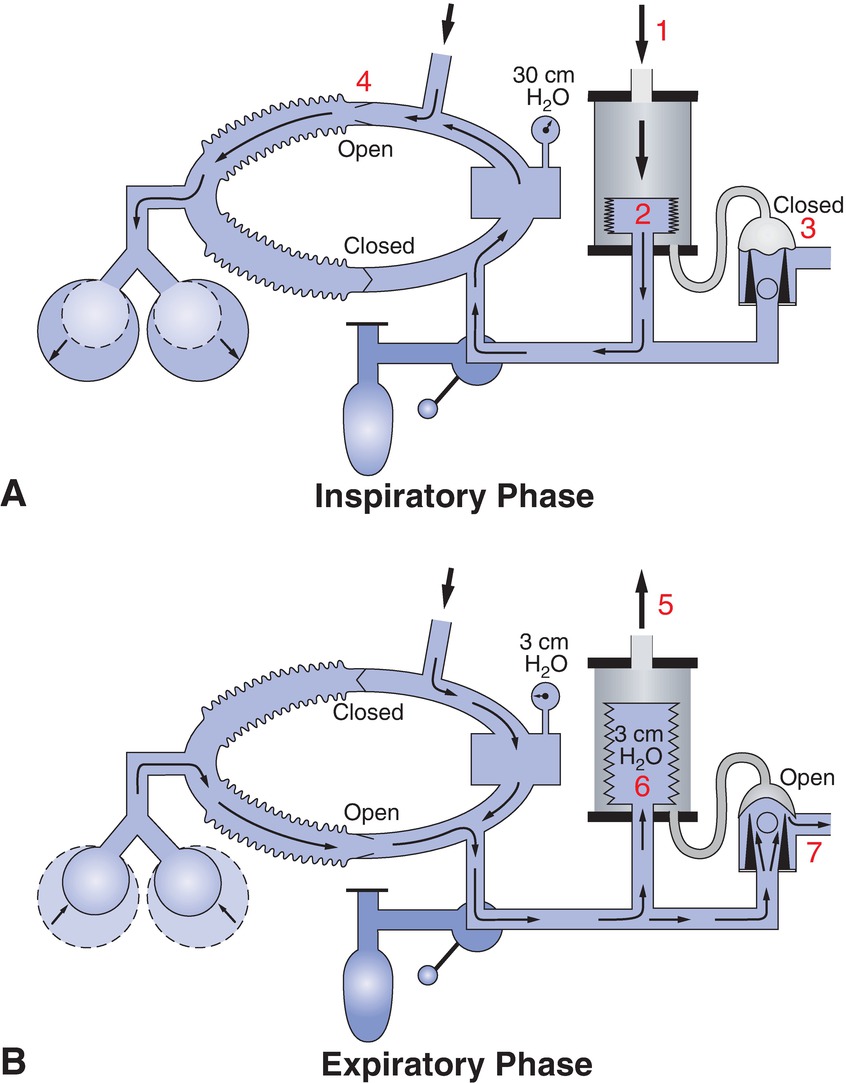
FIGURE 28.2. Bellows ventilator function: Inspiration and expiration. A:1. During inspiration, bellows ventilators inject pressurized gas into the bellows’ housing chamber. 2. The bellows are compressed, forcing anesthetic gases inside the bellows into the breathing circuit, through the CO2 absorber, and into the patient. 3. Simultaneously, the ventilator drive pressure closes the overflow valve to the scavenging system, preventing gas from leaving the circuit. 4. Thus, during inspiration, all gas, including fresh gas from the machine, enters the patient. B: 5,6. During expiration, ventilator drive pressure is released, allowing gas to return and refill the bellows reservoir. 7. Release of bellows driving pressure also opens the scavenging valve, such that any additional anesthetic gases can exit the system once the ventilator bellows has filled.
Piston ventilators use a motorized drive to compress a piston chamber, thus compressing the gas in the circuit. Newer piston-driven ventilators provide more precise volume delivery, as the linear displacement of the piston allows the actual volume delivered to the circuit to be exactly determined. Additionally, piston ventilators are typically able to deliver higher peak pressures than many bellows ventilators, which may be of value in patients with lung disease but which also increase the potential for lung damage from the higher pressures. These ventilators do not need a gas source to power the ventilator but absolutely require electricity to run, from either a wall source or a battery backup. A typical piston ventilator design is detailed in Figure 28.3, which also shows how computer-controlled valves isolate the ventilator from the scavenging circuit as well as maintain PEEP.
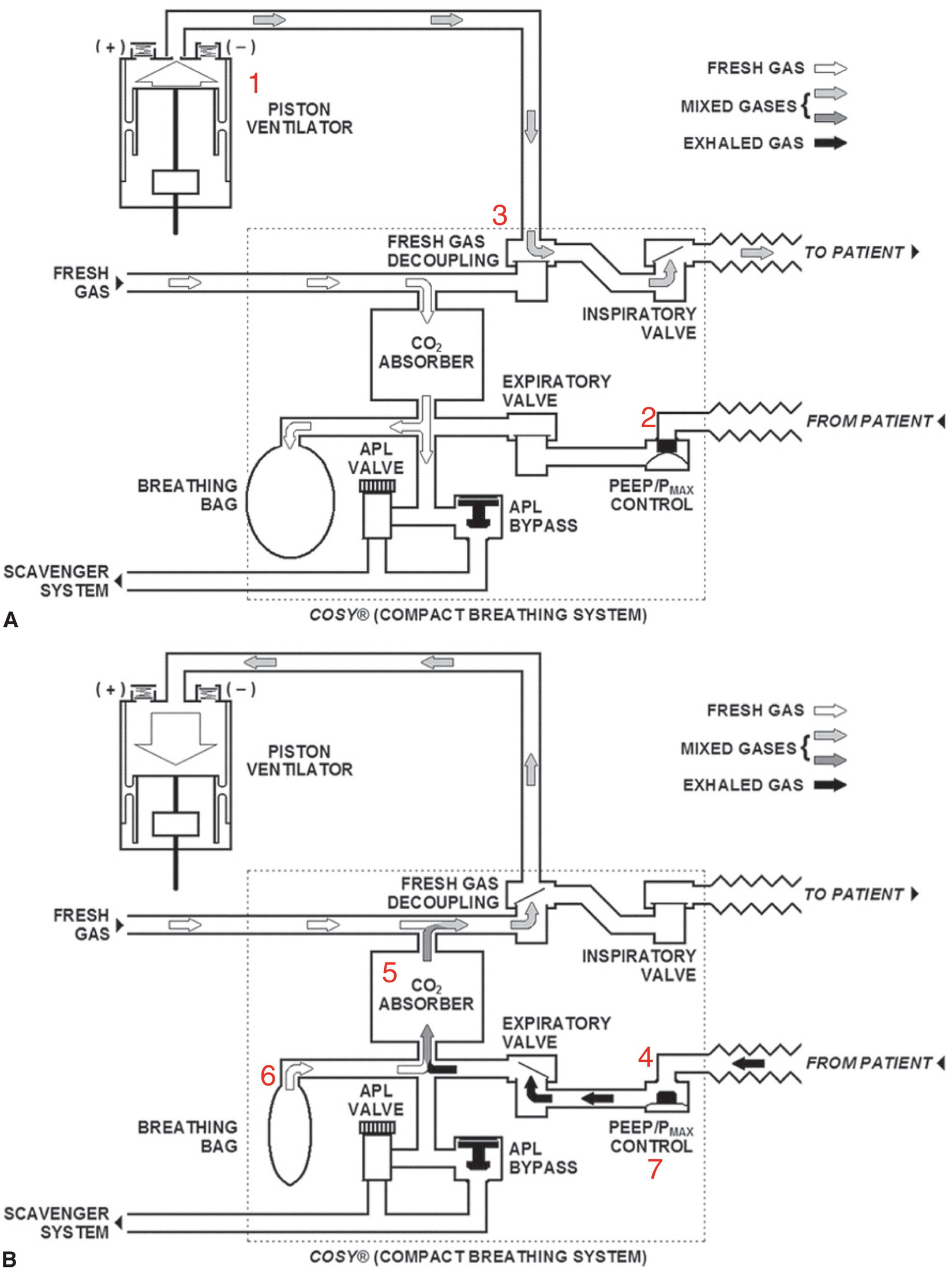
FIGURE 28.3. Piston ventilator circuit example. A: 1. In this example of a piston-driven ventilator (Dräger Fabius GS), piston movement compresses circuit gases during the inspiratory phase of the cycle. 2. A computer-controlled valve (PEEP/Pmax control) closes during this phase, allowing pressure to increase in the circuit and expand the patient’s lungs. 3. A separate one-way (fresh gas decoupling) valve isolates the inspiratory flows to the patient from the fresh gas arriving from the anesthesia machine. B: 4. At the end of inspiration, the PEEP/Pmax valve opens, allowing expiration. 5. Gas returning from the patient passes through the CO2 absorber and returns to the piston reservoir. 6. In this particular model, the breathing bag actually stores anesthetic gases that can be used to refill the piston chamber during expiration, while in bellows design, the breathing bag is entirely removed from the circuit when the mechanical ventilator is engaged. 7. If PEEP is desired, the PEEP/Pmax valve closes when the circuit pressure reaches the desired PEEP pressure, thus maintaining this pressure until the next inspiratory cycle.
Some newer anesthesia machine mechanical ventilators incorporate turbines to deliver positive pressure. These jet-driven ventilators use computer-controlled turbines to drive the anesthetic gas mixture into the patient. During inspiration, the turbine conveys gas from the breathing bag through the absorber and inspiratory valve into the patient’s lungs. The inspiratory pressure is adjusted with the jet and PEEP valve. When expiration begins, the PEEP valve will open and will allow gas to flow out of the patient’s lung through the expiratory valve. Some of the benefits to this new form of ventilation include rapid response to changes in gas composition due to smaller circuit volumes, high accuracy, autoclavability, and easy replacement.
Many modern ventilators have additional features that improve ease of use, safety, and accuracy. Commonly available features include the following:
- Digital display/controls: Most modern ventilators incorporate a computerized control interface, which allows digital control of ventilator modes, pressures, volumes, PEEP, and alarm settings (see Fig. 28.4). Despite the fact that many modern ventilators include digital readouts of tidal volumes and pressures, bellows and pistons can often still be seen moving through a clear window, which serves as an important visual cue to confirm ventilator function. Some electronic machines, however, now provide a graphical display representation of a bellows and a sound representation of its operation.
- Compliance compensation: Because the disposable breathing circuit tubing expands during inspiration, some of the measured tidal volume stays in the expanded tubing and never reaches the patient. Newer ventilators are able to measure circuit compliance (during machine checkout) and compensate for the volume lost in expanding the circuit by increasing the delivered tidal volume.
- Fresh gas decoupling excludes fresh gas from the breathing circuit during inspiration. In older ventilator designs, fresh gas entering the circuit during inspiration was added to gas being delivered from the bellows, significantly (and potentially dangerously) increasing tidal volume when respiratory rates were slow or flow rates were high (Fig. 28.2).
- Feedback compensation: Newer ventilators are able to dynamically regulate the delivered tidal volume in order to compensate for leaks in the circuit or the airway. These ventilators compare the tidal volumes returned from the patient with the programmed values and increase the volumes delivered in order to maintain the provider-specified volumes.
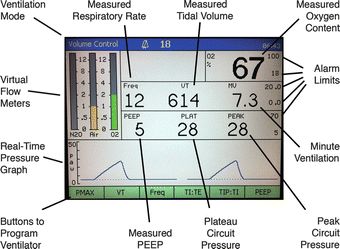
FIGURE 28.4. A typical ventilator control screen. This image demonstrates features found on many computer-controlled ventilator interface screens. These include displays of the actual measured tidal volume, respiratory rate, and minute ventilation, and buttons (left to right on bottom) to set the peak inspiratory pressure limit (Pmax), tidal volume, rate, I:E ratio, an inspiratory pause, and PEEP. Also shown is a continuously charted graph of airway pressure vs time, with numerical readouts of the peak, plateau, and PEEP pressures. This ventilator is functioning in a volume control mode. The oxygen concentration measured from the oxygen sensor is displayed in the upper right corner.
Ventilator Maintenance
The maintenance for both types of ventilators is the same: periodic replacement of parts on a maintenance schedule prescribed by the original equipment manufacturer (OEM), as well as regular functional performance verification of delivered flows, concentrations, and other monitored diagnostic values. Manufacturer-trained, in house Biomedical Equipment Support Specialists (BESS), or manufacturer-provided Field Service Engineers (FSE), will perform this scheduled maintenance. Obviously, any ventilator malfunction should be thoroughly diagnosed and repaired prior to clinical use if at all possible.
In the absence of malfunction, ventilators (either piston driven or a regular bellows) should have the rubber components of the gas reservoirs replaced regularly, often every 6 months, or as recommended by the manufacturer. There may also be some O-rings/seals that are replaced in conjunction with the bellows. If any lubrication of piston rubber O-rings/seals/hoses is needed, it should be done by trained service professionals. They have special instruments for the job and will use lubricants that are manufacturer approved for the oxygen-rich environment. The discs that serve as the inspiratory and expiratory check valves are replaced on a periodic basis, although often less frequently than the bellows.
Frequent problems with ventilators include holes in the rubber material, collapsed bellows that fail to compress gas, bellows that catch/hang on one side, thus preventing accurate gas delivery, or pistons that lose their calibration. Piston-driven vents typically have an electronic eye that looks for a sensor to be in a certain light path when in the start position. If this finely tuned measurement is compromised, the piston-driven ventilator will not know what location it is in and will display errors on the display screen.
Ventilator Failure
During an anesthetic, the mechanical ventilator may gradually or suddenly read very high inspiratory pressures during volume control ventilation. If this pressure is above the predetermined Pmax, the ventilator will stop delivering positive pressure and sound an alarm. In this situation, the compliance of the circuit has markedly changed. Because this is an immediate problem with the patient’s ventilation, it can be a true emergency, and one in which you as the anesthesia technician may be essential. Patients may have suddenly high peak pressures for a number of reasons; some are related to a change in patient condition (such as bronchospasm), tube malposition, partial or complete tube occlusion; the cause can also be ventilator failure. The resolution of this situation is dependent on prompt identification of the cause of the compliance decrease and often involves manual ventilation of the patient (sometimes with an Ambu bag or Jackson-Rees circuit), while the provider determines whether the increase is due to something on the patient side of the circuit or something within the machine or circuit itself. Anesthesia technicians can help troubleshoot the ventilator while the provider works to stabilize and resolve any issues with the patient. (See also Chapter 29, Preventing and Solving Anesthesia Machine Problems.) If the problem is determined to be an intraoperative ventilator failure, a patient can be manually ventilated with the breathing bag, while the anesthesia technician participates in troubleshooting the ventilator and perhaps assists with an intraoperative machine switch, in which case a separate Ambu-Bag or Jackson-Rees circuit will be needed for ventilation as well as a total intravenous anesthetic.
Summary
Because many patients under general anesthesia cannot breathe for themselves, ventilation is essential to the practice of anesthesia. Anesthesia technicians play a key role in assisting patient care by understanding the modes in which mechanical ventilation is delivered and how different ventilator designs accomplish this task. Although different ventilator models will vary slightly from the designs shown in this chapter, an understanding of the functional components of a standard ventilator will make it straightforward to contextualize these differences. With any particular model, a review of technical and functional specifications particular to that ventilator (provided by the manufacturer) will allow you to inspect, maintain, and ensure the safe and proper functioning of each machine and to assist providers during anesthetics if problems occur.
Review Questions
1. Which of the following ventilator modes requires patients to initiate a respiratory cycle?
A) Volume control
B) Pressure support
C) Pressure control
D) PEEP mode
E) None of the above
Answer: B
With pressure support ventilation, the ventilator senses a drop in circuit pressure initiated by a patient’s breath and then delivers a set pressure to augment the patient’s breath. This mode is often used to synchronize the ventilator with the patient’s respiratory efforts. Volume control delivers a fixed volume breath at a given rate regardless of patient effort. Pressure control delivers a fixed pressure breath at a given rate regardless of patient effort. PEEP is not really a ventilator “mode” but rather a setting for the ventilator to maintain a small amount of fixed pressure during expiration.
2. Which of the following is TRUE regarding piston-driven ventilators?
A) Pressurized gas drives movement of the piston.
B) They are unable to work in pressure support mode.
C) They require wall outlet electricity to be functional at all times.
D) They require a servo-controlled valve that prevents the circuit pressure from exiting to the scavenging system during inspiration.
E) None of the above.
Answer: D
Piston control ventilators use a motorized drive to move the piston and deliver the breath. Bellows control ventilators, not piston control, use pressurized gas to collapse the bellows and deliver a breath. Piston control ventilators require electricity to drive the piston, but this can come from either a wall outlet or the internal battery. All anesthesia machine ventilators must have a mechanism to prevent a positive-pressure breath from escaping into the scavenging system instead of being delivered to the patient. Piston control ventilators have a servo-controlled valve that is triggered at the same time the piston is triggered, and which shuts off flow to the scavenging system.
3. Why is fresh gas decoupling important?
A) It prevents wall oxygen from mixing with the anesthesia gases.
B) It allows patients to breathe spontaneously while the ventilator is active.
C) It allows delivered tidal volumes to be independent of gas flow rate through the machine.
D) It allows fresh volatile anesthetics to be separated from those exhaled from the patient.
E) It allows ventilators to deliver positive pressure during both expiration and inspiration.
Answer: C
In many older ventilators, the fresh gas flow continues to flow into the circuit while the ventilator is delivering a breath. This means that the fresh gas flow during inspiration will be added to the flow from the ventilator. At high fresh gas flows, this can significantly increase a delivered tidal volume if the ventilator is set to volume control. Fresh gas decoupling excludes fresh gas from flowing into the circuit during an inspiration from the ventilator.
4. What is the function of PEEP?
A) It can improve patient oxygenation by preventing alveolar collapse.
B) It prevents backward flow of ventilator gases through the vaporizer.
C) It pushes breathing circuit gases through the CO2 absorber.
D) High PEEP allows more comfortable breathing for lightly anesthetized patients.
E) It accelerates the flow of gases at the beginning of the next inspiratory cycle.
Answer: A
With PEEP, the breathing circuit is pressurized with a small amount of positive pressure (usually 5-10 cm H2O, controlled by the PEEP setting) during exhalation, to prevent alveoli from collapsing. This can improve oxygenation in some patients.
5. Which of the following is NOT an advantage of mechanical ventilation?
A) It allows precise control of tidal volumes.
B) It allows precise control of minute ventilation.
C) It allows the anesthesia provider to perform other tasks without manually ventilating.
D) It prevents patients from trying to initiate spontaneous breathing.
E) It allows fine adjustment of inspiratory and expiratory pressures.
Answer: D
Mechanical ventilation can allow the anesthesia provider to control tidal volumes, respiratory rate, minute ventilation (rate × tidal volume), inspiratory pressure, and expiratory pressure. It also does not require the anesthesia provider to squeeze the bag for each breath and can free her or him up to perform other tasks. However, just because a patient is anesthetized or on a mechanical ventilator does not mean that the patient cannot attempt to breathe on his or her own: respiratory efforts are not blocked by some anesthetics. Patients can also “overbreathe” the ventilator as they attempt to take breaths during mechanical ventilation, which might prompt the anesthesia provider to change the mode to pressure support ventilation to augment the patient’s breathing efforts.
6. During volume control ventilation, the mechanical ventilator reads a high inspiratory pressure that is above the predetermined P-max, causing the ventilator to stop delivering positive pressure and sound an alarm. Which of the following should be done?
A) The ventilator should be set to deliver a lower fixed tidal volume.
B) The ventilator should be switched to a PRVC mode.
C) PEEP should be turned on; if it is already on, the respiratory rate should be lowered.
D) The provider should momentarily pause mechanical ventilation.
E) The provider should switch to manual ventilation while the anesthesia technician troubleshoots the ventilator.
Answer: D
If the inspiratory pressure is above the predetermined P-max during volume control ventilation, the provider should switch to manual ventilation of the patient while the anesthesia technician troubleshoots the ventilator. In this situation, the compliance of the circuit has markedly changed, indicating a dramatic change in patient condition, tube malposition, partial or complete tube occlusion, or ventilator failure. Although the anesthesia provider may momentarily pause the mechanical ventilator for nonparalyzed patients who are coughing or straining, doing so to address the very high inspiratory pressure would not be appropriate.
7. A patient is undergoing laparoscopic abdominal surgery with deep paralysis. Which of these ventilator modes should be selected, and why?
A) Patient Regulated Volume Control—the patient may continue to make respiratory efforts and would otherwise “fight” against the ventilator.
B) Pressure Support—the patient may continue to make respiratory efforts and would otherwise “fight” against the ventilator.
C) Patient Regulated Volume Control—the patient’s diaphragm is unable to contract, leaving the patient unable to assist with ventilation.
D) Pressure Support—the patient’s diaphragm is unable to contract, leaving the patient unable to assist with ventilation.
E) None of the above correctly explain what would be chosen and why.
Answer: C
During deep paralysis, the patient is completely paralyzed, making them unable to contract their diaphragm and assist in ventilation efforts. Therefore, it is absolutely vital that a ventilation mode with timed ventilation is selected.
SUGGESTED READINGS
Dorsch JA, Dorsch SE, eds. Anesthesia ventilators. In: Understanding Anesthesia Equipment. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008:310-372.
Grasso S, Mascia L, Ranieri VM. Respiratory care. In: Miller RD, Eriksson LI, Fleisher LA, et al., eds. Miller’s Anesthesia. 8th ed. Philadelphia, PA: Saunders; 2015:3063-3083.
Riutort KT, Eisenkraft JB. The anesthesia workstation and delivery systems for inhaled anesthetics. In: Barash PG, Cullen BF, Stoelting RK, et al., eds. Clinical Anesthesia. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2017:644-705.