Emphysema and Overinflation
Steven R. Boas, Glenna B. Winnie
Pulmonary emphysema consists of distention of air spaces with irreversible disruption of the alveolar septa. It can involve part or all of a lung. Overinflation is distention with or without alveolar rupture and is often reversible. Compensatory overinflation can be acute or chronic and occurs in normally functioning pulmonary tissue when, for any reason, a sizable portion of the lung is removed or becomes partially or completely airless, which can occur with pneumonia, atelectasis, empyema, and pneumothorax. Obstructive overinflation results from partial obstruction of a bronchus or bronchiole, when it becomes more difficult for air to leave the alveoli than to enter. Air gradually accumulates distal to the obstruction, the so-called bypass, ball-valve, or check-valve type of obstruction.
Localized Obstructive Overinflation
When a ball-valve type of obstruction partially occludes the main stem bronchus, the entire lung becomes overinflated; individual lobes are affected when the obstruction is in lobar bronchi. Segments or subsegments are affected when their individual bronchi are blocked. When most or all of a lobe is involved, the percussion note is hyperresonant over the area and the breath sounds are decreased in intensity. The distended lung can extend across the mediastinum into the opposite hemithorax. Under fluoroscopic scrutiny during exhalation, the overinflated area does not decrease and the heart and the mediastinum shift to the opposite side because the unobstructed lung empties normally.
Unilateral Hyperlucent Lung
The differential diagnosis for this resultant unilateral hyperlucent lung is quite broad and can involve the lung parenchyma, airways, pulmonary vasculature, chest wall (see Chapter 445 ), and mediastinum. Localized obstructions that can be responsible for overinflation include airway foreign bodies and the inflammatory reaction to them (see Chapter 414 ), abnormally thick mucus (cystic fibrosis, Chapter 432 ), endobronchial tuberculosis or tuberculosis of the tracheobronchial lymph nodes (see Chapter 242 ), and endobronchial or mediastinal tumors.
Patients with unilateral hyperlucent lung can present with clinical manifestations of pneumonia, but in some patients the condition is discovered only when a chest radiograph is obtained for an unrelated reason. A few patients have hemoptysis. Physical findings can include hyperresonance and a small lung with the mediastinum shifted toward the more abnormal lung.
Swyer-James or Macleod Syndrome
The condition is thought to result from an insult to the lower respiratory tract following most commonly adenovirus (see Chapter 289 ) or respiratory syncytial virus (see Chapter 287 ), Mycoplasma pneumoniae (see Chapter 250 ), or measles (see Chapter 273 ). The infection can cause pulmonary vascular hypoplasia with resultant hypoperfusion leading to unilateral hyperlucent lung (underdevelopment). Clinically, children with this condition often have chronic cough, recurrent pneumonia, hemoptysis, and wheezing, although some are asymptomatic. Some patients show a classic mediastinal shift away from the lesion with exhalation. CT scanning or bronchography can often demonstrate bronchiectasis. Thorascopic evaluation may be useful. The triad of unilateral hyperlucent lung, diffusely decreased ventilation, and matching decreased perfusion of the affected lung supports the diagnosis. In some patients, previous chest radiographs have been normal or have shown only an acute pneumonia, suggesting that a hyperlucent lung is an acquired lesion. For those with recurrent infection or severe lung destruction, treatment may include immunization with influenza and pneumococcal vaccines, as well as surgical resection. However, without treatment, some individuals may become less symptomatic with time.
Congenital Lobar Emphysema (Congenital Large Hyperlucent Lobe)
Congenital lobar emphysema (CLE) can result in severe respiratory distress in early infancy and can be caused by localized obstruction. Familial occurrence has been reported. In 50% of cases, a cause of CLE can be identified. Congenital deficiency of the bronchial cartilage, external compression by aberrant vessels, bronchial stenosis, redundant bronchial mucosal flaps, and kinking of the bronchus caused by herniation into the mediastinum have been described as leading to bronchial obstruction and subsequent CLE and commonly affect the left upper lobe.
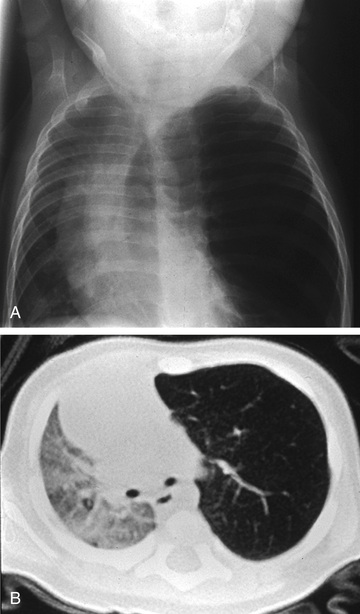
Clinical manifestations usually become apparent in the neonatal period but are delayed for as long as 5-6 yr in 5% of patients. Many cases are diagnosed by antenatal ultrasonography. Infants with prenatally diagnosed cases are not always symptomatic at birth. In some patients, CLE remains undiagnosed until school age or beyond. Clinical signs range from mild tachypnea and wheeze to severe dyspnea with cyanosis. CLE can affect one or more lobes; it affects the upper and middle lobes, and the left upper lobe is the most common site. The affected lobe is essentially nonfunctional because of the overdistention, and atelectasis of the ipsilateral normal lung can ensue. With further distention, the mediastinum is shifted to the contralateral side, with impaired function seen as well (Fig. 420.1 ). A radiolucent lobe and a mediastinal shift are often revealed by radiographic examination. A CT scan can demonstrate the aberrant anatomy of the lesion, and MRI or MR angiography can demonstrate any vascular lesions, which might be causing extraluminal compression. Nuclear imaging studies are useful to demonstrate perfusion defects in the affected lobe. Fig. 420.2 outlines evaluation of an infant presenting with suspected CLE. The differential diagnosis includes pneumonia with or without an effusion, pneumothorax, and cystic adenomatoid malformation.

Treatment by immediate surgery and excision of the lobe may be lifesaving when cyanosis and severe respiratory distress are present, but some patients respond to medical treatment. Selective intubation of the unaffected lung may be of value. Some children with apparent CLE have reversible overinflation, without the classic alveolar septal rupture implied in the term emphysema. Bronchoscopy can reveal an endobronchial lesion.
Pulmonary Vascular Abnormalities
Unilateral hyperlucency may result from unilateral pulmonary agenesis (see Chapter 423 ) that typically presents in the neonatal period. Volume loss of the affected lung results in a mediastinal shift with hyperinflation of the contralateral lung. An anomalous origin of the left pulmonary artery (see Chapter 459 ), also known as a pulmonary artery sling , can impinge the right mainstem bronchus with resultant right-sided hyperinflation or atelectasis producing hyperlucency on either the ipsilateral or contralateral side. Pulmonary venolobar syndrome (see Chapter 453 ), also known as scimitar syndrome , can also result in a hyperlucent contralateral lung dependent on the extent of hypoplasia of the right lung.
Generalized Obstructive Overinflation
Acute generalized overinflation of the lung results from widespread involvement of the bronchioles and is usually reversible. It occurs more commonly in infants than in children and may be secondary to a number of clinical conditions including asthma, cystic fibrosis, acute bronchiolitis, interstitial pneumonitis, atypical forms of acute laryngotracheobronchitis, aspiration of zinc stearate powder, chronic passive congestion secondary to a congenital cardiac lesion, and miliary tuberculosis.
Pathology
In chronic overinflation, many of the alveoli are ruptured and communicate with one another, producing distended saccules. Air can also enter the interstitial tissue (i.e., interstitial emphysema), resulting in pneumothorax and pneumomediastinum (see Chapters 439 and 440 ).
Clinical Manifestations
Generalized obstructive overinflation is characterized by dyspnea, with difficulty in exhaling. The lungs become increasingly overdistended, and the chest remains expanded during exhalation. An increased respiratory rate and decreased respiratory excursion result from the overdistention of the alveoli and their inability to be emptied normally through the narrowed bronchioles. Air hunger is responsible for forced respiratory movements. Overaction of the accessory muscles of respiration results in retractions at the suprasternal notch, the supraclavicular spaces, the lower margin of the thorax, and the intercostal spaces. Unlike the flattened chest during inspiration and exhalation in cases of laryngeal obstruction, minimal reduction in the size of the overdistended chest during exhalation is observed. The percussion note is hyperresonant. On auscultation, the inspiratory phase is usually less prominent than the expiratory phase, which is prolonged and roughened. Fine or medium crackles may be heard. Cyanosis is more common in the severe cases.
Diagnosis
Radiographic and fluoroscopic examinations of the chest assist in establishing the diagnosis. Both leaves of the diaphragm are low and flattened, the ribs are farther apart than usual, and the lung fields are less dense. The movement of the diaphragm during exhalation is decreased, and the excursion of the low, flattened diaphragm in severe cases is barely discernible. The anteroposterior diameter of the chest is increased, and the sternum may be bowed outward.
Bullous Emphysema
Bullous emphysematous blebs or cysts (pneumatoceles) result from overdistention and rupture of alveoli during birth or shortly thereafter, or they may be sequelae of pneumonia and other infections. They have been observed in tuberculosis lesions during specific antibacterial therapy and in end stage cystic fibrosis lung disease. These emphysematous areas presumably result from rupture of distended alveoli, forming a single or multiloculated cavity. The cysts can become large and might contain some fluid; an air-fluid level may be demonstrated on the radiograph (Fig. 420.3 ). The cysts should be differentiated from pulmonary abscesses. In most cases, treatment is not required as the cysts disappear spontaneously within a few months, although they can persist for a yr or more. Aspiration or surgery is not indicated except in cases of severe respiratory and cardiac compromise.

Subcutaneous Emphysema
Subcutaneous emphysema results from any process that allows free air to enter into the subcutaneous tissue (Fig. 420.4 ). The most common causes include pneumothorax or pneumomediastinum (see Chapters 439 and 440 ). In addition, it can be a complication of fracture of the orbit, which permits free air to escape from the nasal sinuses. In the neck and thorax, subcutaneous emphysema can follow tracheotomy, deep ulceration in the pharyngeal region, esophageal wounds, or any perforating lesion of the larynx or trachea. It is occasionally a complication of thoracentesis, asthma, or abdominal surgery. Rarely, air is formed in the subcutaneous tissues by gas-producing bacteria.
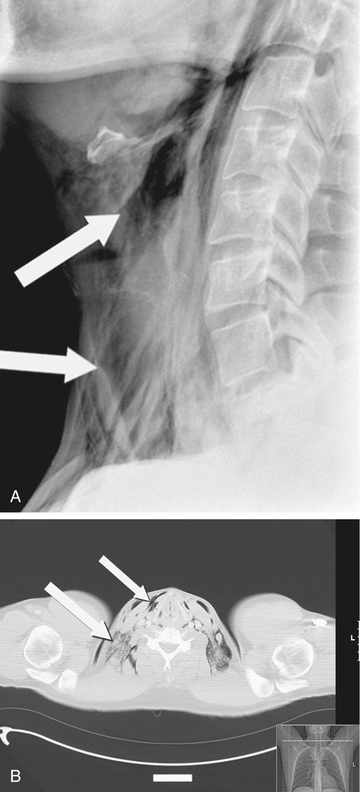
Tenderness over the site of emphysema and a crepitant quality on palpation of the skin are classic manifestations. Subcutaneous emphysema is usually a self-limited process and requires no specific treatment. Minimization of activities that can increase airway pressure (cough, performance of high-pressure pulmonary function testing maneuvers) is recommended. Resolution occurs by resorption of subcutaneous air after elimination of its source. Rarely, dangerous compression of the trachea by air in the surrounding soft tissue requires surgical intervention.