Haptoglobin
Indications
This test is used to identify the presence of intravascular hemolysis. This protein is decreased when significant hemolysis occurs. It is nonspecific for indicating the type of hemolytic anemia.
Test Explanation
The serum haptoglobin test is used to detect intravascular destruction (lysis) of red blood cells (RBCs). This is called hemolysis. Haptoglobins are glycoproteins produced by the liver. These haptoglobins are powerful, free hemoglobin–binding proteins. In hemolytic anemias associated with the hemolysis of RBCs, the released hemoglobin is quickly bound to haptoglobin and the new complex is rapidly catabolized. This results in a diminished amount of free haptoglobin in the serum; this decrease cannot be readily compensated for by normal liver production. As a result, the patient demonstrates a transient reduced level of haptoglobin in the serum. Megaloblastic anemias can reduce the haptoglobin level because of the increased destruction of megaloblastic RBC precursors in the bone marrow.
Haptoglobins are also decreased in patients with primary liver disease not associated with hemolytic anemias. This occurs because the diseased liver is unable to produce these glycoproteins. Hematoma can reduce haptoglobin levels by the absorption of hemoglobin into the blood and by binding hemoglobin with haptoglobin.
Elevated haptoglobin concentrations are found in many inflammatory diseases, and therefore haptoglobin can be used as a nonspecific acute-phase reactant protein in much the same way as the erythrocyte sedimentation rate (see p. 221). That is, levels of haptoglobin increase with severe infection, inflammation, tissue destruction, acute myocardial infarction (AMI), burns, and some cancers.
Interfering Factors
• A slight decrease in haptoglobin levels is noted in normal pregnancy.
• Ongoing infection can cause falsely elevated test results.
![]() Drugs that may cause increased haptoglobin levels include androgens and steroids.
Drugs that may cause increased haptoglobin levels include androgens and steroids.
![]() Drugs that may cause decreased levels include chlorpromazine, diphenhydramine, indomethacin, isoniazid, nitrofurantoin, oral contraceptives, quinidine, and streptomycin.
Drugs that may cause decreased levels include chlorpromazine, diphenhydramine, indomethacin, isoniazid, nitrofurantoin, oral contraceptives, quinidine, and streptomycin.
Test Results and Clinical Significance
 Increased Levels
Increased Levels
Infection (e.g., pyelonephritis, urinary tract infection [UTI], pneumonia),
Tissue destruction (e.g., myocardial infarction [MI]),
The above and many other diseases can cause an elevation of haptoglobin, an acute-phase reactant protein.
Biliary obstruction: Haptoglobin, after attaching to hemoglobin, is excreted by the liver in the bile. Obstruction will diminish that excretion.
 Decreased Levels
Decreased Levels
Hemolytic anemia (e.g., erythroblastosis fetalis, autoimmune hemolytic anemias, hemoglobinopathies [sickle cell], paroxysmal nocturnal hemoglobinuria, drug-induced hemolytic anemia, or uremia): Hemolysis occurs, freeing hemoglobin in the plasma. The free hemoglobin is tightly bound to haptoglobin. The complex is catabolized and excreted. Haptoglobin cannot be replaced fast enough and levels in the blood fall.
Transfusion reactions: ABO antibodies bind to ABO antigens on the RBC membrane and cause hemolysis. Hemoglobin is liberated from the RBC. The free hemoglobin is tightly bound to haptoglobin. The complex is catabolized and excreted. Haptoglobin cannot be replaced fast enough and levels in the blood fall.
Prosthetic heart valves: The mechanical trauma of the valve on the RBC causes hemolysis, and hemoglobin is liberated from the RBC. The free hemoglobin is tightly bound to haptoglobin. The complex is catabolized and excreted. Haptoglobin cannot be replaced fast enough and levels in the blood fall.
Primary liver disease: The diseased liver cannot make adequate amounts of haptoglobin. The liver is the sole source of haptoglobin.
Heinz Body Preparation
Indications
This test is used to detect Heinz bodies that occur as a result of oxidative denaturation of the hemoglobin molecule.
Test Explanation
Heinz bodies are water-insoluble precipitates of oxidated-denatured proteins or hemoglobin that form within red blood cells. They occur as a result of exposure to oxidative chemicals and drugs. Mutations of hemoglobin (particularly Hb Koln), thalassemias, and defects in the hemoglobin-reductive defense system against oxidation (G6PD deficiency or pyruvate kinase deficiency) lead to an enhanced tendency toward oxidative hemolysis. The diagnosis of these problems can be established by the detection of Heinz bodies in red blood cells (RBCs) by obtaining a Heinz body preparation.
Heinz bodies are often associated with hemolytic anemias and the presence of spherocytosis. The pathophysiology of these anemias starts with oxidative injury to hemoglobin. As a result, red cell inclusions (Heinz bodies) of variable size and usually eccentric location adhere to the red cell membrane. Smooth movement of the membrane over the cytosol is reduced. These RBCs are selectively blocked from leaving the splenic cords and entering the sinuses. Splenic macrophages attack these RBCs and cause hemolysis. This process can be severe enough to cause intravascular destruction as well, producing hemoglobinemia and hemoglobinuria. Most often the clinical picture includes a normocytic anemia associated with splenomegaly.
Agents that commonly induce oxidation of hemoglobin include: nitrofurantoin, sulfasalazine, p-aminosalicylic acid, acetaminophen, phenazopyridine, phenacetin, dapsone, and other sulfones. Diets high in pickled or smoked foods, nitrates, recreational drugs, mothballs, and industrial chemicals can also oxidize hemoglobin.
For Heinz body detection, fresh blood is incubated with a supravital stain (such as methyl violet or Nile blue) and examined by microscopy for presence of stained inclusions close to the red cell membrane (Heinz bodies). These RBC granules can be quantified by several different methods, but are most commonly counted microscopically. It is important not to confuse Heinz bodies with other RBC granules, such as Howell Jolly bodies.
Hematocrit (Hct, Packed Red Blood Cell Volume, Packed Cell Volume [PCV])
Normal Findings
Indications
The Hct is an indirect measurement of red blood cell (RBC) number and volume. It is used as a rapid measurement of RBC count. It is repeated serially in patients with ongoing bleeding or as a routine part of the complete blood cell count. It is an integral part of the evaluation of anemic patients.
Test Explanation
The Hct is a measure of the percentage of the total blood volume that is made up by the RBCs. The height of the RBC column is measured after centrifugation. It is compared to the height of the column of the total whole blood. The ratio of the height of the RBC column compared with the original total blood column is multiplied by 100%. This is the Hct value. It is routinely performed as part of a complete blood cell count. The Hct closely reflects the hemoglobin (Hgb) and RBC values. The Hct in percentage points usually is approximately three times the Hgb concentration in grams per deciliter when RBCs are of normal size and contain normal amounts of Hgb.
Normal values vary according to gender and age. Women tend to have lower values than men, and Hct values tend to decrease with age. Abnormal values indicate the same pathologic states as abnormal RBC counts and Hgb concentrations. Decreased levels indicate anemia (reduced number of RBCs). Increased levels can indicate erythrocytosis (Figure 2-18).

Figure 2-18 Tubes showing hematocrit levels of normal blood, blood with evidence of anemia, and blood with evidence of polycythemia. Note the buffy coat located between the packed red blood cells (RBCs) and the plasma. A, A normal percentage of RBCs. B, Anemia (low percentage of RBCs). C, Polycythemia (high percentage of RBCs).
Like other RBC values, the Hct can be altered by many factors other than RBC production. For instance, in dehydrated patients the total blood volume is contracted. The RBCs make up a greater proportion of the total blood volume, and the Hct measurement is therefore falsely high. Likewise, if the RBC is morphologically increased in size, the RBCs will make up a greater proportion of the total blood volume, and Hct will again be falsely high.
The Hct can be measured in a capillary tube (by skin puncture) by placing the blood in the tube, which is then spun in a microcentrifuge. The percentage of the RBC portion of the column to the whole column is the Hct. This value is most often calculated by automated cell counting machines.
Decisions concerning the need for blood transfusion are usually based on the Hgb or the Hct. In an otherwise healthy person, transfusion is not considered as long as the Hgb is above 8 g/dL or the Hct is above 24%. In younger people who can safely and significantly increase their cardiac output, a Hct of 18% may be acceptable. In an older individual with an already compromised oxygen-carrying capacity (caused by cardiopulmonary diseases), transfusion may be recommended when the Hct level is below 30%.
Interfering Factors
• Abnormalities in RBC size may alter Hct values. Larger RBCs are associated with higher Hct levels, because the larger RBCs take up a greater percentage of the total blood volume.
• Extremely elevated white blood cell (WBC) counts decrease Hct, which would falsely indicate anemia.
• Hemodilution and dehydration may affect the Hct level (see previous discussion).
• Pregnancy usually causes slightly decreased values because of chronic hemodilution.
• Living at high altitudes causes increased Hct values as a result of a physiologic response to the decreased oxygen available.
• Values may not be reliable immediately after hemorrhage because the percentage of total blood volume taken up by the RBC has not changed. Not until the total blood volume is replaced with fluids will the Hct decrease.
![]() Drugs that may cause decreased levels include chloramphenicol and penicillin.
Drugs that may cause decreased levels include chloramphenicol and penicillin.
Test Results and Clinical Significance
 Increased Levels
Increased Levels
Erythrocytosis: The number of RBCs is increased. This can result from illnesses or as a physiologic response to external situations.
Congenital heart disease: Cyanotic heart diseases cause chronically low Po2 levels. In response, the RBCs increase in number. Therefore the Hct increases.
Polycythemia vera: This is a result of the bone marrow inappropriately producing great numbers of RBCs, causing the Hct to increase.
Severe dehydration (e.g., severe diarrhea, burns): With depletion of extracellular fluid, the total blood volume decreases, but the number of RBCs stays the same. Therefore the percentage of total blood volume that is taken up by the RBCs increases and the Hct increases.
Severe chronic obstructive pulmonary disease (COPD): Chronic states of hypoxia cause stimulation of RBC production as a physiologic response to increased oxygen-carrying capacity. Therefore the Hct increases.
 Decreased Levels
Decreased Levels
Anemia: This is a term given to the state associated with reduced RBC numbers. Because the Hct is an indirect reflection of RBC numbers, the Hct will also be reduced. Many different types of diseases are associated with anemia.
Hemoglobinopathy: Patients with Hgb disorders or other blood dyscrasias have a reduced number and survival of RBCs. Therefore the Hct is decreased.
Cirrhosis: This is a chronic state of fluid overload. The RBCs are diluted and make up a smaller percentage of the total blood volume. Therefore the Hct decreases.
Hemolytic anemia (e.g., erythroblastosis fetalis, hemoglobinopathies, drug-induced hemolytic anemias, paroxysmal nocturnal hemoglobinuria): The RBC survival is diminished in hemolytic anemia. The number of RBCs decreases and therefore the Hct is decreased.
Hemorrhage: With active bleeding, the number of RBCs decreases and therefore the Hct is decreased. It takes time (several hours), however, for the Hct to fall. Only when the blood volume is replenished with fluid does the Hct diminish.
Dietary deficiency: With certain vitamin or mineral deficiencies (e.g., iron), the RBC number or size is decreased. Therefore the Hct is decreased.
Bone marrow failure: With reduced synthesis of the RBCs, the Hct will decrease.
Prosthetic valves: The prosthetic valve causes mechanical trauma to the RBCs. RBC survival is diminished, so RBC numbers diminish and Hct decreases.
Renal disease: Erythropoietin is made in the kidney and is a strong stimulant to RBC production. With a reduced level of erythropoietin, the RBC numbers diminish and the Hct is decreased.
Normal pregnancy: In pregnancy, normally there is increased blood volume because of a chronic state of overhydration. Combined with a relative “malnourished” state, the Hct is diminished by a decrease in the number of RBCs and the percentage of total blood volume they make up.
Rheumatoid/collagen-vascular diseases (e.g., rheumatoid arthritis, lupus): Chronic illnesses are associated with a reduced production of RBCs. Therefore the Hct is decreased.
Related Tests
Hemoglobin (p. 281). This is a measurement of the concentration of Hgb in the blood. It is closely associated with the RBC count and Hct value.
Red Blood Cell Count (p. 439). This is a measurement of the number of RBCs per cubic millimeter of blood. It is closely associated with the Hgb and Hct values.
Red Blood Cell Indices (p. 442). These provide data about the size and Hgb content of the RBC.
Hemoglobin (Hgb, Hb)
Normal Findings
Indications
This test is a measure of the total amount of Hgb in the blood. It is used as a rapid indirect measurement of the red blood cell (RBC) count. It is repeated serially in patients with ongoing bleeding or as a routine part of the complete blood cell count (CBC). It is an integral part of the evaluation of anemic patients.
Test Explanation
The Hgb concentration is a measure of the total amount of Hgb in the peripheral blood. The test is normally performed as part of a CBC. Hgb serves as a vehicle for oxygen and carbon dioxide transport. The oxygen-carrying capacity of the blood is determined by the Hgb concentration. Hgb also acts as an important acid-base buffer system.
As with the RBC count, normal values vary according to gender and age. Women tend to have lower values than men and Hgb values tend to decrease with age. The Hgb closely reflects the hematocrit (Hct) and RBC values. The Hct in percentage points usually is approximately three times the Hgb concentration in grams per deciliter when RBCs are of normal size and contain normal amounts of Hgb.
Abnormal values indicate the same pathologic states as abnormal RBC counts and Hct concentrations. Decreased levels indicate anemia (reduced number of RBCs). Increased levels can indicate erythrocytosis. In addition, however, changes in plasma volume are more accurately reflected by the Hgb concentration. Dilutional overhydration decreases the concentration, whereas dehydration tends to cause an artificially high value. Slight decreases in the values of Hgb and Hct during pregnancy reflect the expanded blood volume because of a chronic state of overhydration; the number of cells is actually increased during pregnancy. Hgb is usually measured by an automated cell counter. There is very little variability (2% to 3%) with most well-kept machines.
Hgb is made up of heme (iron surrounded by protoporphyrin) and globin consisting of an alpha- and a beta-polypeptide chain. Abnormalities in the globin structure are called hemoglobinopathies (e.g., sickle cell disease, hemoglobin C disease). Some diseases are caused by abnormalities in globin chain synthesis (such as thalassemia). In these diseases the RBC counts can be low, the RBC survival can be diminished, and the RBC-carrying capacity can be reduced.
Too little Hgb puts a strain on the cardiopulmonary system to maintain good oxygen-carrying capacity. With critically low hemoglobin levels, patients are at great risk for angina, heart attack, congestive heart failure, and stroke. When Hgb levels are too high because of increased numbers of RBCs, intravascular sludging occurs, leading to stroke and other organ infarction. Decisions concerning the need for blood transfusion are usually based on the Hgb or the Hct. In an otherwise healthy person, transfusion is not considered as long as the Hgb is above 8 g/dL or the Hct is above 24%. In younger people who can safely and significantly increase their cardiac output, an Hgb level of 6 g/dL may be acceptable. In an older individual with an already compromised oxygen-carrying capacity (cardiopulmonary diseases), transfusion may be recommended when the Hgb level is below 10.
Interfering Factors
• Slight Hgb decreases normally occur during pregnancy because of the dilution effect of the expanded blood volume.
• There is a slight diurnal variation in Hgb levels.
• Hgb levels are highest around 8 AM and are lowest around 8 PM. This may vary as much as 1 g/dL.
• Heavy smokers have higher Hgb levels than nonsmokers.
• Living in high altitudes causes increased Hgb values as a result of a physiologic response to the decreased oxygen available at these high altitudes.
![]() Drugs that may cause increased levels include gentamicin and methyldopa (Aldomet).
Drugs that may cause increased levels include gentamicin and methyldopa (Aldomet).
![]() Drugs that may cause decreased levels include antibiotics, antineoplastic drugs, aspirin, indomethacin (Indocin), rifampin, and sulfonamides.
Drugs that may cause decreased levels include antibiotics, antineoplastic drugs, aspirin, indomethacin (Indocin), rifampin, and sulfonamides.
Test Results and Clinical Significance
 Increased Levels
Increased Levels
Erythrocytosis: The number of RBCs is increased as a result of illnesses or as a physiologic response to external situations (e.g., high altitude).
Congenital heart disease: Cyanotic heart diseases cause chronically low Po2 levels. In response, the RBCs increase in number. Therefore the Hgb increases.
Severe chronic obstructive pulmonary disease: Chronic states of hypoxia cause stimulation of RBC production as a physiologic response to increased oxygen-carrying capacity. Therefore the Hgb increases.
Polycythemia vera: This is a result of the bone marrow inappropriately producing great numbers of RBCs. Therefore the Hgb increases.
Severe dehydration (e.g., severe diarrhea, burns): With depletion of extracellular fluid, the total blood volume decreases, but the number of RBCs stays the same. Therefore the percentage of total blood volume that is taken up by the RBCs increases and Hgb increases.
 Decreased Levels
Decreased Levels
Anemia: This is a term given to the state associated with reduced RBC numbers. Because the Hgb is an indirect reflection of RBC numbers, the Hgb will also be reduced. Many different types of diseases are associated with anemia.
Hemoglobinopathy: Patients with Hgb disorders or other blood dyscrasias have reduced RBC number and RBC survival. Therefore the Hgb is decreased.
Cirrhosis: This is a chronic state of fluid overload. The RBCs are diluted and make up a smaller percentage of the total blood volume. Therefore the Hgb decreases.
Hemolytic anemia (e.g., erythroblastosis fetalis, hemoglobinopathies, drug-induced hemolytic anemias, transfusion reactions, or paroxysmal nocturnal hemoglobinuria): The RBC survival is diminished in hemolytic anemia. The number of RBCs decreases and the Hgb decreases.
Hemorrhage: With active bleeding, the number of RBCs decreases and the Hgb decreases. It takes time (several hours), however, for the Hgb to fall. Only if the blood volume is replenished with fluid does the Hgb diminish.
Dietary deficiency: With certain vitamin or mineral deficiencies (e.g., iron), the RBC number or size is decreased. Therefore the Hgb is decreased.
Bone marrow failure: With reduced synthesis of the RBCs, the Hgb will decrease.
Prosthetic valves: The prosthetic valve causes mechanical trauma to the RBCs. RBC survival is diminished. RBC numbers diminish and Hgb decreases.
Renal disease: Erythropoietin is made in the kidney and is a strong stimulant to RBC production. With a reduced level of erythropoietin, the RBC numbers diminish and the Hgb is decreased.
Normal pregnancy: In pregnancy, normally there is increased blood volume because of a chronic state of overhydration. Combined with a relative “malnourished” state, the Hgb is diminished by a decrease in the number of RBCs and the percentage of total blood volume they make up.
Rheumatoid/collagen-vascular diseases (e.g., rheumatoid arthritis [RA], lupus, sarcoidosis): Chronic illnesses are associated with a reduced production of RBCs. Therefore the Hgb is decreased.
Hematologic cancers are often associated with bone marrow failure of RBC production. The number of RBCs diminishes and the Hgb decreases.
Splenomegaly: With an enlarged functioning spleen, RBCs are sequestered and eliminated from the functioning vascular system.
Related Tests
Hematocrit (p. 277). This is a measurement of the percentage of the total blood volume taken up by the RBCs. It is closely associated with Hgb values and RBC count.
Red Blood Cell Count (p. 439). This is a measurement of the number of RBCs per cubic millimeter of blood. It is closely associated with Hgb and Hct values
Red Blood Cell Indices (p. 442). These provide data about the size and Hgb content of the RBC.
Hemoglobin Electrophoresis (Hgb Electrophoresis)
Indications
Hgb electrophoresis is a test that enables abnormal forms of Hgb (hemoglobinopathies) to be detected and quantified. This test is used to diagnose sickle cell anemia, thalassemia, and other hemoglobinopathies.
Test Explanation
Although many different Hgb variations have been described, the more common types are A1, A2, F, S, E, and C. Each major Hgb type is electrically charged to varying degrees. When the Hgb from lysed red blood cells (RBCs) is placed on electrophoresis paper in an electromagnetic field, the Hgb variants migrate at different rates and therefore spread apart from each other. The migration of the various forms of Hgb makes up a series of bands on the paper. The bands therefore correspond to the various forms of Hgb present. The pattern of bands is compared to normal and to well-known abnormal patterns. A diagnosis can then be made. Each band can be quantitated as a percentage of the total Hgb, indicating the severity of any recognized abnormality.
The form Hgb A1 constitutes the major component of Hgb in the normal RBC. Hgb A2 is only a minor component (2% to 3%) of the normal Hgb total. Hgb F is the major Hgb component in the fetus but usually exists in only minimal quantities in the normal adult. Levels of Hgb F greater than 2% in patients over 3 years of age are considered abnormal. Hgb F is able to transport oxygen when only small amounts of oxygen are available (as in fetal life). In patients requiring compensation for prolonged chronic hypoxia (as in congenital cardiac abnormalities), Hgb F may be found in increased levels to assist in the transport of the available oxygen.
Hgb S and Hgb C are abnormal forms of Hgb that occur predominantly in American blacks. Hemoglobin E occurs predominantly in Southeast Asians. Hgb S is associated with sickle cell anemia. Hgb S is a relatively insoluble variant. When little oxygen is available, it assumes a crescent (sickle) shape that greatly distorts the RBC morphology. Vascular sludging is a consequence of the localized sickling and may lead to organ infarction. The duration of survival of the sickled RBC is diminished, and these patients also have anemia. RBCs containing Hgb C have a decreased life span and are more readily lysed than normal RBCs. Mild to severe hemolytic anemia may result. The Hgb contents of some common disorders affecting hemoglobin, as determined by electrophoresis, are indicated in Table 2-27.
Hgb E is produced less efficiently by RBC precursors; if there is an increased Hgb E content in the RBCs, those cells will have a low mean corpuscular volume (MCV, p. 442).
Quantifying abnormal hemoglobins is helpful in determining the zygosity of a familial hemoglobinopathy. Furthermore quantification of abnormal hemoglobin proteins provides a method of monitoring treatments designed to increase more effective hemoglobin variants and decrease abnormal variants. Hemoglobin quantification can be performed by high-performance liquid chromatography (HPLC) and polymerase chain reaction (PCR) analysis.
Related Test
Hemoglobin (p. 281). This is a direct measurement of the Hgb that exists in the “average” RBC.
Hepatitis Virus Studies (Hepatitis-Associated Antigen [HAA], Australian Antigen)
Indications
This group of tests is used to diagnose and to identify the serologic type and current status of hepatitis. It is important to diagnose and identify the type of hepatitis as soon as possible so that the patient can be immediately treated and appropriately isolated.
Test Explanation
Hepatitis is an inflammation of the liver caused by viruses, alcohol ingestion, drugs, toxins, or overwhelming bacterial sepsis. The three common viruses now recognized to cause disease are hepatitis A, hepatitis B, and hepatitis C (also called non-A/non-B) viruses. Hepatitis D and E viruses are much less common in the United States. Hepatitis D can infect the liver only by entering into a hepatitis B virus, which it uses as a carrying vehicle. Therefore hepatitis D cannot cause disease unless patients have hepatitis B virus in their bloodstream in the active, chronic, or carrier forms. The various types of hepatitis cannot be differentiated on the basis of their clinical presentation. The clinical presentations are similar in that they all include low-grade fever, malaise, anorexia, and fatigue. Most often they are all associated with elevations of hepatocellular enzymes such as aspartate aminotransferase (AST), alanine aminotransferase (ALT), and lactic dehydrogenase (LDH).
Hepatitis A virus (HAV) was originally called infectious hepatitis. It has a short incubation period of 2 to 6 weeks and is highly contagious. During active infection, HAV is excreted in the stool and transmitted via oral-fecal contamination of food and drink. Most infections are not associated with symptoms severe enough to warrant medical evaluation. Immune globulin (IgG) and IgM antibodies to HAV are routinely used when HAV infection is suspected.
The first HAV antibody to appear is the IgM antibody (HAV-Ab/IgM) in approximately 3 to 4 weeks after exposure or just before hepatocellular enzyme elevations occur. These IgM levels usually return to normal in approximately 8 weeks. The next antibody to HAV to rise is IgG (HAV-Ab/IgG), which appears approximately 2 weeks after the IgM begins to increase and slowly returns to normal levels. The IgG antibody can remain detectable for more than 10 years after the infection. If the IgM antibody is elevated in the absence of the IgG antibody, acute hepatitis is suspected. If however IgG is elevated in the absence of IgM elevation, a convalescent or chronic stage of HAV viral infection is indicated.
These antibodies may not be positive soon after infection occurs, which can delay the investigation of the infectious outbreaks. The HAV virus can be detected directly by measuring HAV RNA in the sera of patients suspected of acute infection.
Hepatitis B virus (HBV) is commonly known as serum hepatitis. It has a long incubation period of 5 weeks to 6 months. HBV is most frequently transmitted by blood transfusion; however, it also can be contracted via exposure to other body fluids. HBV may cause a severe and unrelenting form of hepatitis culminating in liver failure and death. The incidence is increased among blood transfusion recipients, male homosexuals, dialysis patients, transplant patients, intravenous drug abusers, and patients with leukemia or lymphoma. Hospital personnel are also at increased risk for infection, mostly as a result of needle stick contamination.
HBV, also called the Dane particle, is made up of an inner core surrounded by an outer capsule. The outer capsule contains the hepatitis B surface antigen (HBsAg), formerly called Australian antigen. The inner core contains HBV core antigen (HBcAg). The hepatitis B e-antigen (HBeAg) is also found within the core. Antibodies to these antigens are called HBsAb, HBcAb, and HBeAb. The tests used to detect these antigens and antibodies include (Table 2-28):
TABLE 2-28
| Serologic Findings | Appearance/Disappearance | Application |
| HAV-Ab/IgM | 4-6 wk/3-4 mo | Acute HAV infection |
| HAV-Ab/IgG | 8-12 wk/10 yr | Previous HAV exposure/immunity |
| HBeAg | 1-3 wk/6-8 wk | Acute HBV infection |
| HBeAb | 4-6 wk/4-6 yr | Acute HBV infection ended |
| HBsAg | 4-12 wk/1-3 mo | Acute HBV infection |
| HBsAb total | 3-10 mo/6-10 yr | Previous HBV infection/immunity indicated |
| HBVc-Ab/IgM | 2-12 wk/3-6 mo | Acute HBV infection |
| HBVc-Ab total | 3-12 wk/life | Previous HBV infection/convalescent stage |
| HCV-Ab/IgG | 3-4 mo/2 yr | Previous HCV infection |
| HDV Ag | 1-3 days/3-5 days | Acute HDV infection |
| HDV-Ab/IgM | 10 days/1-3 mo | Acute HDV infection |
| HDV-Ab total | 2-3 mo/7-14 mo | Chronic HDV infection |
1. Hepatitis B surface antigen (HBsAg). This is the most frequently and easily performed test for hepatitis B, and it is the first test to become abnormal. HBsAg rises before the onset of clinical symptoms, peaks during the first week of symptoms, and returns to normal by the time jaundice subsides. HBsAg generally indicates active infection by HBV. If the level of this antigen persists in the blood, the patient is considered to be a carrier.
2. Hepatitis B surface antibody (HBsAb). This antibody appears approximately 4 weeks after the disappearance of the surface antigen and signifies the end of the acute infection phase. HBsAb also signifies immunity to subsequent infection. Concentrated forms of this agent constitute the hyperimmunoglobulin given to patients who have come in contact with HBV-infected patients (e.g., contact by an inadvertent needle prick from a needle previously used on a patient with HBV infection). HBsAb is the antibody that denotes immunity after administration of hepatitis B vaccine.
3. Hepatitis B core antigen (HBcAg). No tests are currently available to detect this antigen.
4. Hepatitis B core antibody (HBcAb). This antibody appears approximately 1 month after infection with HBsAg and declines (although it remains elevated) over several years. HBcAb is also present in patients with chronic hepatitis. The HBcAb level is elevated during the time lag between the disappearance of HBsAg and the appearance of HBsAb. This interval is called the “core window.” During the core window, HBcAb is the only detectable marker of a recent hepatitis infection.
5. Hepatitis B e-antigen (HBeAg). This antigen generally is not used for diagnostic purposes but rather as an index of infectivity. The presence of HBeAg correlates with early and active disease, as well as with high infectivity in acute HBV infection. The persistent presence of HBeAg in the blood predicts the development of chronic HBV infection.
6. Hepatitis B e-antibody (HBeAb). This antibody indicates that an acute phase of HBV infection is over, or almost over, and that the chance of infectivity is greatly reduced.
Hepatitis B DNA can be quantified and is a direct measurement of the HBV viral load. A one- or two-log decrease in viral load in a hepatitis B–infected patient means antiviral therapy is working. A one- or two-log increase in a similar patient means an antiviral has stopped working and that viral resistance may have developed. High levels of HBV-DNA, ranging from 100,000 to more than 1 billion viral copies per milliliter, indicate a high rate of HBV replication. Low or undetectable levels, about 300 copies per milliliter or less, indicate an “inactive” infection. The World Health Organization established the international unit or copies per milliliter (mL), written as international units/mL or copies/mL, to measure HBV DNA. Detection of HBV DNA serves as an important supplementary test to serology in a number of clinical settings. It is helpful in the early detection of HBV infection, monitoring of disease, and determining low levels of viremia in patients with nonreplicative HBV disease and chronic hepatitis. Because the intent of treatment is to eliminate HBV, accurate measurement of low viral load is very important.
Hepatitis C virus (HCV) (non-A/non-B [NANB] hepatitis) is transmitted in a manner similar to HBV. Most cases of hepatitis are caused by blood transfusion. HCV is found in as many as 8% of blood donors worldwide. The incubation period is 2 to 12 weeks after exposure. The clinical manifestations of the illness parallel those of HBV. However, unlike with HBV, HCV infection is chronic in more than 60% of infected persons. Although the disease course is variable, it is slowly progressive. Twenty percent of HCV patients develop cirrhosis and hepatocellular cancers associated with this chronic infection.
The screening test for detecting HCV infection is the detection of anti-HCV antibodies to HCV recombinant core antigen, NS3 gene, NS4 antigen, and NS5 antigen. The antibodies can be detected within 4 weeks of infection. With HCV-RNA testing, the HCV virion can be directly detected and quantified (viral load). Real-time PCR is used for HBV DNA testing. HCV RNA viral load is quantitated by using RT-PCR methods and is usually expressed as units per milliliter or copies per milliliter. Although a higher viral load may not necessarily be a sign of more severe or more advanced disease, it does correlate with likelihood to respond to treatment. HCV RNA tests can also be used to monitor response to hepatitis C treatment.
Hepatitis D virus (HDV) is known to cause delta hepatitis. As stated earlier, the HDV must enter the HBV to gain access to the liver and be infective. The patient must have HBV in the blood from a past or synchronously occurring infection. In the United States this is most commonly transmitted through tainted blood. The HDV antigen can be detected by immunoassay within a few days after infection. The IgM and total antibodies to HDV are also detected early in the disease. A persistent elevation of these antibodies indicates a chronic or carrier state.
Hepatitis E virus (HEV) was initially included in the non-A/non-B virus group but was isolated several years ago as an etiologic virus of short incubation. No antigen or antibody tests are currently widely available and accurate for the serologic identification of this infecting agent.
Procedure and Patient Care
After
• Apply pressure or a pressure dressing to the venipuncture site.
• Assess the venipuncture site for bleeding.
• Handle the specimen as if it were capable of transmitting hepatitis.
• Immediately discard the needle in the appropriate receptacle.
• Send the specimen to the laboratory promptly.
![]() Advise patients with suspected hepatitis that they should refrain from intimate contact with another person. Until the serology indicates otherwise, the person should be considered infective.
Advise patients with suspected hepatitis that they should refrain from intimate contact with another person. Until the serology indicates otherwise, the person should be considered infective.
Hexosaminidase (Hexosaminidase A, Hex A, Total Hexosaminidase, Hexosaminidase A and B)
Indications
Hex A is used to identify patients affected by Tay-Sachs disease and unaffected persons who may be carriers of this deadly genetic defect.
Test Explanation
Tay-Sachs disease (TSD) is a lysosomal storage disease (GM2 gangliosidoses) first characterized by loss of motor skills in infancy and early childhood. Death usually occurs by age 4 to 8 years. TSD is a result of a mutation in an autosomal recessive gene carried on chromosome 15. An affected person must inherit a defective gene from each parent to have TSD. One out of 25 Ashkenazi (Eastern European) Jews is a carrier for this genetic mutation. There are 80 different genetic mutations that inhibit the function of this important gene (p. 1097). This gene encodes the synthesis of an enzyme called hexosaminidase. Without this enzyme, lysosomes of GM2 accumulate, particularly in the central nervous system.
Two clinically important isoenzymes of hexosaminidase have been detected in the serum: hexosaminidase A (made up of one alpha subunit and one beta subunit) and hexosaminidase B (made up of two beta subunits). Any genetic mutation that affects the alpha unit will cause a deficiency of hexosaminidase A, resulting in TSD. A mutation that affects the beta unit will cause a deficiency in hexosaminidase A and B. Sandhoff disease, an uncommon variant of Tay-Sachs, occurs with deficiency of both of these enzymes. Other genetic mutations of this same gene can cause chronic GM2-gangliosidosis, a disease similar to TSD that becomes apparent later in life (adolescence).
Because TSD is uniformly untreatable and fatal, a significant effort has gone into the development of biochemical testing to identify carriers of the genetic mutation (persons who carry one of the recessive genetic defective genes). Hex A has been found to be abnormally low in carriers, whereas hex B is high. Therefore testing for total hexosaminidase is not useful. A carrier has a 25% chance of having a child with TSD if the other biologic parent is also a carrier. Pregnancy should occur only with thorough genetic counseling. In communities in which the Ashkenazi Jewish population is high, hex A screening has been very effective for identifying carriers. Further, hex A is used to diagnose TSD in infants, young children, and adults. Genetic testing (p. 1093) is useful to corroborate the identification of an affected person or a carrier.
If a couple at risk for producing offspring with TSD chooses to proceed with pregnancy, amniocentesis (p. 632) can be performed. The amniotic fluid and or cells obtained by chorionic villus sampling can be tested for hex A. Cells obtained during amniocentesis can also be tested for the precise genetic mutation.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient. Emphasize the importance of this test to Jewish couples of Eastern European ancestry who plan to have children. Explain that both must carry the defective gene to transmit TSD to their offspring.
Explain the procedure to the patient. Emphasize the importance of this test to Jewish couples of Eastern European ancestry who plan to have children. Explain that both must carry the defective gene to transmit TSD to their offspring.
![]() Professional genetic counseling should be provided to every person considering undergoing this test.
Professional genetic counseling should be provided to every person considering undergoing this test.
![]() Patients should be made aware of the possible effects on their lives if hex A levels are found to be reduced.
Patients should be made aware of the possible effects on their lives if hex A levels are found to be reduced.
• Check with the laboratory regarding withholding contraceptives.
Related Tests
Genetic Testing (p. 1093). By testing for a mutation at the site of the gene known to be involved in TSD, more definitive corroborative evidence of disease state and carrier status can be obtained.
Amniocentesis (p. 632). Through this technique, fetal cells and fluid can be obtained and tested for hex A.
HIV Drug Resistance Testing (HIV Genotype, HIV Tropism)
Indications
This test is used for the identification of key HIV genotypic mutations that are associated with resistance to highly active antiretroviral therapy (HAART).
Test Explanation
There are several factors that affect the success of HIV antiviral medications. These include patient compliance, access to adequate care, optimal dosing, and drug pharmacology issues, including absorption, elimination, and drug interactions. Another significant factor that determines a patient's response to anti-viral HIV drugs is the percentage of a HIV viral population that is resistant to the nucleotide reverse-transcriptase inhibitors, non-nucleotide reverse-transcriptase inhibitors, and protease inhibitors that may be administered to destroy the HIV virus. HIV resistance to therapy develops in 78% of patients. In these patients, genotypic mutations arising in the drug-targeted HIV viral gene loci occur because of evolutionary pressure from antiviral therapy and results in antiviral resistance that may compromise HAART in HIV-infected patients receiving HAART. This information can be identified based on HIV genotyping or the identification of HIV tropism. When combination therapy fails, detection and analysis of HIV genotypic mutations or tropism can guide necessary changes to antiretroviral therapy and decrease HIV viral load, thereby improving patient outcome.
HIV tropism is laboratory methodology that sets up a vector construct that when the patient's nucleic acid is inserted, the ability of the HIV virus to infect the cell is determined. This is a phenotype assay that is biologically driven. This assay is sensitive and correlates well to clinical outcomes. Unfortunately, this testing is expensive and labor intensive. HIV genotyping is an alternative to HIV tropism.
HIV genotyping is able to detect changes in the viral genome that are associated with drug resistance. By amplification and analysis of drug-targeted HIV gene sequence, identification of changes in nucleotide bases and associated amino acid codons that may cause antiviral drug resistance can be identified. Such genotypic changes are deemed as mutations by comparing the sequence data of the patient's HIV strain to those of a “wild-type” HIV strain. The significance of these genotypic mutations in relation to antiviral resistance is then determined by a set of interpretive rules.
Results of any genotypic mutation found would include:
• “Susceptible” result indicates no reduced susceptibility.
• “Possible resistance” result indicates that the mutation(s) detected has or have been associated with diminished virologic response in some but not all patients.
• “Resistant” result indicates that the mutation(s) detected has or have been associated with a maximum reduction in susceptibility of the virus.
• “Insufficient evidence” result indicates that current scientific data are insufficient to determine if the mutation(s) detected is or are associated with decreased susceptibility of the virus to the specific antiviral drug.
• “Unable to genotype” result indicates that the sequence data obtained are of poor quality to determine the presence or absence of genotypic resistant mutations in the patient's HIV strain. One possible cause of such poor sequence data is low HIV viral load (i.e., <1000 copies/mL).
HIV genotyping is particularly useful when failure to the most active antiviral therapy is suspected by decreasing CD4 counts (p. 147). HIV genotyping can also be performed in conjunction with HIV drug sensitivity testing. HIV sensitivity testing estimates the ability of a cloned copy of the patient's virus to replicate in a cell culture in the presence of a particular antiviral drug. This same testing can help determine the amount of drug needed to inhibit viral replication. It is generally reported as the concentration of drug required to inhibit (inhibiting concentration, IC) viral replication by 50%, or the IC50. This is particularly helpful when considering the use of expensive drugs or when frequent hypersensitivity to a particular drug is possible.
Procedure and Patient Care
During
• Observe universal body and blood precautions. Wear gloves when handling blood products from all patients.
• Obtain venous blood in lavender (EDTA) or pink (K2EDTA) tube.
• Never recap needles. Dispose of needles and syringes required for obtaining the blood specimen in a puncture-proof container designed for this purpose.
Related Tests
HIV Serologic and Virologic Testing (p. 297). These tests are used to detect HIV infection.
HIV RNA Quantification (see following test). This is a measure of the HIV viral load in an HIV-infected patient.
HIV RNA Quantification (HIV Viral Load)
Indications
This test is used to determine the amount of human immunodeficiency virus (HIV) viral load in the blood of an infected patient. This test is an accurate marker for prognosis, disease progression, response to antiviral treatment, and indication for antiretroviral prophylactic treatment.
Test Explanation
Quantitation of HIV RNA in the blood of patients infected with HIV can be used as a confirmatory or supplementary test after serologic tests (p. 297) are positive. Quantification is also helpful when confirmatory tests are indeterminate or cannot be accurately interpreted. Virologic testing is helpful in differentiating newborn HIV infection from passive transmission of HIV antibodies from a HIV infective mother. Finally HIV RNA quantification testing determines HIV “viral load.” Determining viral load is used:
• To determine a baseline viral level before initiating anti–HIV-1 drug therapy
• To identify HIV-1 drug resistance while on anti-HIV therapy
• To identify noncompliance with anti–HIV-1 drug therapy
• To monitor HIV-1 disease progression while on or off anti–HIV-1 drug therapy
• To recommend the initiation of antiretroviral treatment (Table 2-29). To determine the course of the disease because it is more accurate than any other test, including CD4 T-cell counts (p. 147).
• To determine patient survival (Table 2-30).
HIV viral load is determined by quantifying the amount of genetic material of the virus in the blood. There are several different laboratory methods of measuring HIV viral load. It is important that the same method be used in monitoring the course of the disease. Because results vary according to the testing methods, it is important to know which method is used when considering whether to initiate treatment. A common method uses a reverse-transcriptase polymerase chain reaction (RT-PCR) using gene amplification. This method can quantify HIV-1 or -2 RNA to ranges of less than 50 copies/mL.
In general, it is recommended to determine the baseline viral load by obtaining two measurements 2 to 4 weeks apart after HIV infection. Monitoring may continue with testing every 3 to 4 months in conjunction with CD4 counts. Both tests provide data used to determine when to start antiviral treatment. The viral load test can be repeated every 4 to 6 weeks after starting or changing antiviral therapy. Usually antiviral treatment is continued until the HIV viral load is less than 500 copies/mL. It is important to recognize that a nondetectable result does not mean no virus is left in the blood after treatment; it means that the viral load has fallen below the limit of detection by the test. However the clinical implications of a viral load below 50 copies/mL remain unclear. Possible causes of such a result include very low plasma HIV-1 viral load present (e.g., in the range of 1 to 19 copies/mL), very early HIV-1 infection (i.e., less than 3 weeks from time of infection), or absence of HIV-1 infection (i.e., false-positive). A significant (greater than threefold) rise of viral load should warrant consideration of alteration of therapy.
In general, this test is not recommended as a screening/confirmatory test for suspected HIV infection. However, clinicians may recommend the quantification of viral load (DNA or RNA) for screening of infants born to HIV-infected mothers.
Procedure and Patient Care
During
• Observe universal body and blood precautions. Wear gloves when handling blood products from all patients.
• Collect a blood sample in a lavender-top (EDTA) tube. If the test is sent out, the plasma is separated out and at least 2.5 mL is frozen and sent.
• Never recap needles. Dispose of needles and syringes required for obtaining the blood specimen in a puncture-proof container designed for this purpose.
After
• Immediately transport the specimen to the laboratory.
• Specimens are often sent to a central laboratory.
• Apply pressure to the venipuncture site.
![]() Instruct the patient to observe the venipuncture site for infection. Patients with AIDS are immunocompromised and susceptible to infection.
Instruct the patient to observe the venipuncture site for infection. Patients with AIDS are immunocompromised and susceptible to infection.
![]() Do not give results over the telephone. Increasing viral load may have devastating consequences.
Do not give results over the telephone. Increasing viral load may have devastating consequences.
![]() Encourage the patient to discuss his or her concerns regarding the prognostic information that may be obtained by these results.
Encourage the patient to discuss his or her concerns regarding the prognostic information that may be obtained by these results.
Related Tests
HIV Serology (p. 297). This test is used to diagnose HIV infection.
Lymphocyte Immunophenotyping (p. 147). This test is used to measure CD4 lymphocyte counts. This is another marker for disease prognosis, response to treatment, and also an indicator for starting prophylactic antiretroviral treatment.
HIV Drug Resistance Testing (p. 292). HIV drug sensitivity testing estimates the ability of a cloned copy of the patient's virus to replicate in a cell culture in the presence of a particular antiviral drug. It can help determine the amount of drug needed to inhibit viral replication.
HIV Serologic and Virologic Testing (AIDS Serology, Acquired Immunodeficiency Serology, AIDS Screen, Human Immunodeficiency Virus [HIV] Antibody Test, Western Blot Test, p24 Direct Antigen, HIV-RNA Viral Test)
Test Explanation
There are two active types of human immunodeficiency viruses, types 1 and 2. HIV 1 is most prevalent type within the United States and Western Europe, whereas HIV 2 is mostly limited to Western African nations. Serologic testing identifies antibodies developed as a result of HIV 1 or 2 infections. Virologic tests identify RNA (or DNA) specific to HIV. Virologic tests can identify HIV infection in the first 11 days after infection. Serologic tests can identify HIV infection only after about 3 weeks. This 3-week time period is called the “seroconversion window.” Serologic testing for HIV is divided into “screening tests” and “confirmatory” tests (Box 2-11).
In the past serologic screening of patients suspected of having HIV-1 or -2 infection usually began with a HIV antibody “screening test” using a qualitative chemiluminescent immunoassay. If positive, a confirmatory test was required to make the diagnosis of HIV infection. HIV serologic qualitative screening tests (for HIV-1 and -2) were used to screen high- and low-risk individuals or for donor blood products (Table 2-31 and Box 2-12). Because these rapid screening qualitative antibody immunoassays do not detect viral antigens, they could not detect infection in its earliest stage (before antibodies are formed). Because some persons who undergo HIV testing do not return to learn their test results, there has been a strong push toward the “point of service” rapid HIV antibody serologic screening testing in which results can be available in less than 1 hour. This is particularly helpful in urgent or emergent care points of service in which HIV transmission could occur from blood or body fluid contamination. Furthermore, rapid antibody testing is helpful during labor in women whose HIV status is unknown.
TABLE 2-31
Centers for Disease Control HIV Screening Recommendations
| Who | How Often |
| All adults ages 18-64 | Once in a lifetime |
| All adults with known risk factors | Yearly |
| All pregnant women | Once |
| Pregnant women at risk for HIV | Second test in third trimester |
| Newborns if mother is HIV+ or HIV status is unknown | Frequent repeated testing through first 6 months of life |
Point-of-care home kits are available that provide anonymous registration and pretest counseling via a toll-free call. Sample collection in the privacy of one's home, laboratory processing, and post-test counseling are components of this home-testing process. The procedure involves pricking a finger with a special device, placing drops of blood on a specially treated card, and then mailing the card to a licensed laboratory to be tested. Test results are available to the client within 3 business days for the Express Kit and 7 days for the Standard Kit after shipment of the sample to the laboratory.
Confirmatory tests for HIV-1 and -2 antibodies include the Western blot assay and the indirect immunofluorescence assay (IFA). The Western blot assay can recognize either HIV-1 or -2 antibodies. The Western blot is associated with lower sensitivity during the time of seroconversion. However, when positive, the Western blot is very accurate. IFA assay can also discriminate between HIV-1 and -2 antibodies. It is more sensitive than the Western blot assay. These are often done as multi-spot or immunoblot testing.
The p24 direct serologic antigen assay detects the viral protein p24 in the peripheral blood of HIV-infected individuals, in which it exists either as a free (core) antigen or complexed to anti-p24 antibodies. The p24 antigen may be detectable as early as 16 days after infection. The p24 antigen test can be used to assess the antiviral activity of anti-HIV therapies. The p24 antigen test can also be used to differentiate active neonatal HIV infection from passive HIV antibody present from the mother's blood. It is also used to detect HIV infection before antibody seroconversion, detect HIV in donor blood, and monitor therapy.
The use of oral fluids for serologic HIV testing is as an alternative to serum testing. These new HIV-1 antibody tests use oral mucosal transudate (OMT), a serum-derived fluid that enters saliva from the gingival crevice and across oral mucosal surfaces. Another noninvasive alternative to blood testing is urine testing for HIV. Only a spot urine collection is required. Testing urine for HIV antibodies is valuable, especially when venipuncture is inconvenient, difficult, or unacceptable. Insurance companies also commonly use it. It is important to note that all urine HIV tests are detecting antibodies and not the HIV particles. Urine does not contain the virus and is not a body fluid capable of infecting others.
HIV antigen/antibody (Ag/Ab) combination assays are now available that can detect HIV infection on average 5 to 7 days earlier than assays that only detect antibodies. Reducing the seroconversion window has always been an important goal in HIV diagnostics because individuals with acute HIV infection have high viral loads and are highly infectious. As discussed, in the past, the two-step immunoassay (IA)/rapid test screen followed by the Western blot confirmation approach had been the gold standard for HIV diagnosis. With the development of the newer Ag/Ab combination test, the CDC has proposed another algorithm for HIV testing (Figure 2-19).

Figure 2-19 CDC proposed HIV testing algorithm. (Reprinted with permission from the Association of Public Health Laboratories [APHL] 2011.)
The serologic tests described in the preceding detect HIV infection based on demonstration of antibodies to HIV or to HIV viral antigen protein (p. 297). HIV viral RNA particles can be detected (by qualitative testing for HIV RNA) and quantified (by HIV RNA quantification-viral load, see p. 294) using Nucleic Acid Amplification Tests (NAATs) methods. Although too expensive to use as screening tests, NAAT testing can identify HIV 11 days after infection. HIV-RNA tests can be used as confirmatory or discriminatory tests, especially when other confirmatory tests are indeterminate or cannot be accurately interpreted. NAAT testing is helpful in differentiating newborn HIV infection from passive transmission of HIV antibodies from an HIV-infective mother.
A person with positive HIV test results does not have AIDS until he or she develops the clinical features of diminished immune ability. Positive confirmatory HIV antibody test results are required under laws in many states to be reported to the departments of health of the respective states in which the patients reside.
Interfering Factors
• False-positive results can occur in patients who have autoimmune disease, lymphoproliferative disease, leukemia, lymphoma, syphilis, or alcoholism.
• False-positives can occur in noninfected pregnant women.
• HIV-2 infection can cause a positive HIV-1 and -2 screening antibody test and an indeterminate WB HIV-1 confirmatory test.
• False-negative results can occur in the early incubation stage or end stage of AIDS.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient.
Explain the procedure to the patient.
• Obtain an informed consent as required by law.
![]() Tell the patient that no fasting or preparation is required.
Tell the patient that no fasting or preparation is required.
• Maintain a nonjudgmental attitude toward the patient's sexual practices and allow the patient ample time to express his or her concerns regarding the results.
During
• Observe universal blood and body precautions. Wear gloves when handling blood products from all patients.
• For routine HIV testing, collect a venous blood sample in a red-top tube. The blood is often sent to an outside laboratory for testing, although testing kits are becoming increasingly available in hospital laboratories and even in homes.
• If the patient wishes to remain anonymous, use a number with the patient's name; be sure to record it accurately.
• Note that if the serologic test is reactive (i.e., test is positive twice consecutively), the Western blot test is performed on the same blood sample.
After
• Apply pressure or a pressure dressing to the venipuncture site.
• Assess the site for bleeding.
![]() Instruct the patient to observe the venipuncture site for infection. Patients with AIDS are immunocompromised and susceptible to infection.
Instruct the patient to observe the venipuncture site for infection. Patients with AIDS are immunocompromised and susceptible to infection.
• Follow the institution's policy regarding test result reporting.
• Do not give results over the telephone. Remember that positive results may have devastating consequences.
![]() Explain to the patient that a positive Western blot test merely implies exposure to and presence of the AIDS virus within the body. It does not mean that the patient has clinical AIDS. Not all patients with positive results on an antibody test will acquire the disease.
Explain to the patient that a positive Western blot test merely implies exposure to and presence of the AIDS virus within the body. It does not mean that the patient has clinical AIDS. Not all patients with positive results on an antibody test will acquire the disease.
![]() Encourage patients testing positive to identify their sexual contacts so that they can be informed and tested.
Encourage patients testing positive to identify their sexual contacts so that they can be informed and tested.
![]() Inform the patient that subsequent sexual contact will put new partners at high risk for contracting AIDS.
Inform the patient that subsequent sexual contact will put new partners at high risk for contracting AIDS.
Related Tests
Cell Surface Immunophenotyping (p. 147). This test quantifies the number of CD4 and CD8 lymphocytes in an HIV-positive patient. These tests are predictive of the disease course and prognosis.
HIV Viral Load (p. 294). This test is used to determine the amount of HIV viral load in the blood of an infected patient and is an accurate marker for prognosis and disease progression.
Homocysteine (HCY)
Indications
Homocysteine is an important predictor of coronary, cerebral, and peripheral vascular disease. When a strong familial predisposition or early-onset vascular disease is noted, homocysteine testing should be performed to determine if genetic or acquired homocysteine excess exists. Because elevated homocysteine levels are associated with vitamin B12 or folate deficiency, this is a reasonable test to use for the detection and surveillance of malnutrition.
Test Explanation
Homocysteine is an intermediate amino acid formed during the metabolism of methionine. Increasing evidence suggests that elevated blood levels of homocysteine may act as an independent risk factor for ischemic heart disease, cerebrovascular disease, and peripheral arterial disease. Homocysteine appears to promote the progression of atherosclerosis by causing endothelial damage, promoting low-density lipoprotein (LDL) deposition, and promoting vascular smooth muscle growth. Screening for hyperhomocysteinemia (levels >15 μmol/L) should be considered in individuals with progressive and unexplained atherosclerosis despite normal lipoproteins and in the absence of other risk factors. It is also recommended in patients with an unusual family history of atherosclerosis, especially at a young age. A person with an elevated homocysteine level is also at a five-times increased risk for stroke, dementia, and Alzheimer disease. Elevated levels also appear to be a risk factor for osteoporotic fractures in older men and women.
Dietary deficiency of vitamins B6, B12, or folate is the most common nongenetic cause of elevated homocysteine. These vitamins are essential cofactors involved in the metabolism of homocysteine to methionine. Because of the relationship of homocysteine to these vitamins, homocysteine blood levels are helpful in the diagnosis of deficiency syndromes associated with these vitamins. In patients with megaloblastic anemia, homocysteine levels may be elevated before results of the more traditional tests become abnormal. Therefore using homocysteine as an indicator may result in earlier treatment and thus improvement of symptoms in patients with these vitamin deficiencies. Some practitioners recommend homocysteine testing in patients with known poor nutritional status (alcoholics, drug abusers) and the elderly. Homocysteine is elevated in children with inborn errors of methionine metabolism.
Some researchers believe that elevated levels of homocysteine can be treated by administration of vitamins B6 and B12, and folate. Several research reports recommend this vitamin therapy for homocysteine levels greater than 14 μmol/L.
Genetic defects encoding the synthesis of the enzymes responsible for the metabolism of homocysteine to cysteine or the remethylation of homocysteine to methionine are the most common familial cause of hyperhomocysteinemia. Afflicted children suffer from homocystinuria and experience very premature and accelerated atherosclerosis during childhood.
Both fasting and post–methionine loading levels of homocysteine can be measured. In most laboratories, total homocysteine concentrations are measured. A major disadvantage in homocysteine testing is that methods are not standardized. With the more recent development of enzyme immunoassay (EIA), results will be more standardized. However, newer testing kits simplifying high-performance liquid chromatography with fluorescence detection are simple and accurate. In general, homocysteine levels lower than 12 are considered optimal, levels from 12 to 15 are borderline, and levels greater than 15 are associated with high risk for vascular disease. When blood levels are elevated, urine levels of homocysteine are also increased.
Interfering Factors
• Levels may increase with age.
• Patients with renal impairment have elevated levels of homocysteine because of poor excretion of the protein.
• Men usually have higher levels of homocysteine than women do. This is most likely because of higher creatinine values and greater muscle mass.
• Patients with a low intake of B vitamins have higher levels of homocysteine. The B vitamins help to break down and recycle homocysteine.
• Smoking is associated with increased homocysteine levels.
![]() Drugs that may cause increased levels include azaribine, carbamazepine, methotrexate, nitrous oxide, theophylline, and phenytoin.
Drugs that may cause increased levels include azaribine, carbamazepine, methotrexate, nitrous oxide, theophylline, and phenytoin.
![]() Drugs that are associated with decreased levels include folic acid, oral contraceptives, and tamoxifen.
Drugs that are associated with decreased levels include folic acid, oral contraceptives, and tamoxifen.
Procedure and Patient Care
During
• Obtain the fasting blood sample in a collection tube that contains EDTA, heparin, or sodium citrate (blue-top or lavender-top tube).
• For methionine loading, the patient ingests approximately 100 mg/kg of methionine after fasting for 10 to 12 hours. A blood sample is obtained. Repeat blood samples are collected at 2, 4, 8, 12, and 24 hours to compare levels of B vitamins and amino acids in the plasma.
Test Results and Clinical Significance
 Increased Levels
Increased Levels
As a direct effect of homocysteine on the vascular wall, intimal injury and plaque formation occurs. Accentuated smooth muscle vascular constriction serves to further diminish the vessel lumen, thereby compounding the vascular occlusive results. Ischemic events in the cerebral, coronary, and peripheral tissues occur earlier, more severely, and more frequently.
Deficient quantity of metabolic enzymes or metabolic cofactors (vitamin B12 or folate) diminishes metabolism of homocysteine. Blood levels and subsequently urine levels increase.
Malnutrition: Malnourished patients have low vitamin B12 and folate intake. Because these vitamins are essential to the metabolism of homocysteine, blood levels increase.
Related Tests
Vitamin B12 (p. 518) and Folate (p. 242). Blood levels of these substances are easily determined. The results have an impact on levels of homocysteine.
Lipoproteins (p. 342). Lipoproteins are also important predictors of cardiac atherosclerotic risks.
Cholesterol (p. 154) and Triglycerides (p. 504). These, too, are important predictors of cardiac atherosclerotic risks.
Apolipoproteins (p. 106). This test is used to measure apolipoprotein levels. This may be a better indicator of atherogenic risks than total high-density lipoprotein (HDL) or total LDL.
Human Chorionic Gonadotropin (hCG, Pregnancy Tests, hCG Beta Subunit)
Indications
That test is used to diagnose pregnancy. It is also helpful in monitoring high-risk pregnancies. It can be used as a tumor marker for hCG-producing cancers.
Test Explanation
All pregnancy tests are based on the detection of human chorionic gonadotropin (hCG), which is secreted by the placental trophoblast after the ovum is fertilized. hCG appears in the blood and urine of pregnant women as early as 10 days after conception. In the first few weeks of pregnancy, hCG rises markedly, and serum levels are higher than urine levels. After about 1 month, hCG is about the same in either specimen.
hCG is made up of alpha and beta subunits. The alpha subunit is the same for many other glycoprotein hormones, including TSH, FSH, and LH. The beta subunit is specific for hCG. Immunologic tests are performed by using commercially prepared antibodies against the hCG and its subunits (particularly the beta subunit). Most of these laboratory methods use sandwich type immunoassay. In this technique, a monoclonal antibody directed to the alpha and beta subunit of hCG is applied to a bound solid phase substrate. The specimen (urine or serum) is applied to the bound solid phase substrate. Simultaneously or sequentially, a labeled monoclonal antibody directed to the beta subunit is bound to that same surface. The free antibody is washed away and the residual bound beta subunit identified by its particular label represents the quantity of the beta subunit of hCG that exists within the patient's specimen.
With the development of hCG sandwich-type immunoassay, very small levels of hCG can be detected, and pregnancy can be determined 3 to 7 days after conception. Furthermore, this method of EIA eliminates any crossover reactivity with other non-hCG glycoprotein hormones and thereby increases accuracy and specificity. The diagnostic cutoff for pregnancy is >25 IU/L. Values between 5 and 25 IU/L are indeterminate for pregnancy. Results can be confirmed with a repeat test in 72 hours. Values in pregnancy should double every 3 days for the first 6 weeks. When an embryo is first large enough to be visible on transvaginal ultrasound (p. 887), the patient generally will have hCG concentrations between 1000 and 2000 IU/L. If the hCG value is high and gestational contents are not visible in the uterus, ectopic pregnancy is suggested.
There are qualitative serum and urine hCG assays and quantitative serum hCG assays (Table 2-32). All assays use the same sandwich immunoassays. There are different point-of-care testing devices for hospital/laboratory use and for use by the general public. In the tests for the public, the patient's urine is tested. The urine is applied to a testing apparatus and the color change is compared to a standard. If the color matches that standard, pregnancy is present. Other tests kits use the development of a line or plus symbol that may appear indicating pregnancy. These tests take only a few minutes to perform and obtain results. They are best if performed a few days after all missed menses. However, they can be positive on the day of an expected menses.
TABLE 2-32
Recommended Uses for hCG Testing
| Test Name | Recommended Use |
| Qualitative beta hCG | Rapid pregnancy test |
| Quantitative hCG | More accurate pregnancy test Used to monitor high-risk pregnancy |
| Quantitative hCG (tumor marker) | Monitor patients with hCG secreting tumors |
hCG is synthesized in the placenta and maintains the corpus luteum, and, hence, progesterone production, during the first trimester. Thereafter the placenta produces steroid hormones, diminishing the role of hCG. Concentrations of hCG fall, leveling off around week 20, significantly above pre-pregnancy levels. After delivery, miscarriage, or pregnancy termination, hCG falls until prepregnancy levels are reached. Increased total hCG levels in the first and second trimester are associated with Down syndrome, whereas decreased levels may occur in trisomy 18.
Normally hCG is not present in nonpregnant women. In a very small number of women (less than 5%), hCG exists in minute levels. The presence of hCG does not necessarily indicate a normal pregnancy. Ectopic pregnancy, hydatidiform mole of the uterus, recent abortion, and choriocarcinoma of the uterus can all produce hCG. However, hCG levels in ectopic pregnancy fail to double appropriately, and decreased levels eventually result relative to the values expected in normal pregnancies of similar gestational age.
Outside of pregnancy, hCG may be secreted by seminomatous and non-seminomatous testicular tumors, ovarian germ cell tumors, gestational trophoblastic disease (e.g., hydatidiform mole), and benign or malignant nontesticular teratomas. Rarely other tumors including hepatic, neuroendocrine, breast, ovarian, pancreatic, cervical, and gastric cancers may secrete hCG. In tumors, hCG is a valuable marker that can be used to identify and monitor tumor activity. Serial measurement of hCG following treatment is used to monitor therapeutic response in these tumors and will detect persistent or recurrent neoplastic disease.
Interfering Factors
• Tests performed too early in the pregnancy, before there is a significant hCG level, may give false-negative results.
• Hematuria and proteinuria in the urine may cause false-positive results.
• Hemolysis of blood may interfere with test results.
• Urine pregnancy tests can vary according to the dilution of the urine. hCG levels may be undetectable in a dilute urine specimen but may be detectable in a concentrated urine specimen.
![]() Drugs that may cause false-negative urine results include diuretics (by causing dilute urine) and promethazine.
Drugs that may cause false-negative urine results include diuretics (by causing dilute urine) and promethazine.
![]() Drugs that may cause false-positive results include anticonvulsants, antiparkinsonian drugs, hypnotics, and tranquilizers (especially promazine and its derivatives).
Drugs that may cause false-positive results include anticonvulsants, antiparkinsonian drugs, hypnotics, and tranquilizers (especially promazine and its derivatives).
Test Results and Clinical Significance
 Increased Levels
Increased Levels
Highest beta hCG levels (>30,000 milli-international units/mL) are recorded in pregnancy. Lowest amounts are generally seen in ectopic pregnancy.
Germ cell (choriocarcinoma, teratomas, embryonal cell) tumors of testes or ovaries,
Other tumors (poorly differentiated tumors, such as hepatoma and lymphoma):
Human Lymphocyte Antigen (HLA Antigen, HLA-B27 Antigen, Human Leukocyte A Antigen, White Blood Cell Antigens, Histocompatibility Leukocyte A Antigen)
Indications
HLA testing is used in histocompatibility testing for organ or other tissue transplantation. These antigens are present with certain diseases, so the test is used to support their diagnosis. These antigens can identify patients who are allergic to certain medications. Finally HLA testing is used in paternity investigations.
Test Explanation
The HLA antigens exist on the surface of white blood cells (WBCs) and on the surface of all nucleated cells in other tissues. These antigens can be detected most easily on the cell surface of lymphocytes. The presence or absence of these antigens is determined by the genes on chromosome 6. There are four genes at this locus. Each gene controls the presence or absence of HLA A, B, C, and D. There is probably a fifth genetic locus that is closely related to D and is called DR.
The HLA system of antigens (particularly D) has been used to indicate tissue compatibility with tissue transplantation. If the HLA antigens of the donor are not compatible with the recipient, the recipient will make antibodies to those antigens, accelerating rejection. Survival of the transplanted tissue is increased if HLA matching is good. Prior HLA sensitization causes antibodies to form in the blood of a transplant recipient and shortens the survival of red blood cells (RBCs) or platelets when transfused.
The HLA system has also been used to assist in the diagnosis of certain other diseases. For example, HLA B27 is present in 80% of patients with Reiter syndrome. When a patient presents with recurrent and multiple arthritic complaints, the presence of HLA-B27 supports the diagnosis of Reiter syndrome. HLA-B27 is found in 5% to 7% of normal patients. Other HLA-disease associations are listed in Table 2-33.
TABLE 2-33
| HLA Antigen | Disease |
| B27 | Reiter syndrome |
| Ankylosing spondylitis | |
| Yersinia enterocolitica arthritis | |
| Anterior uveitis | |
| Graves disease | |
| B8 | Celiac disease |
| Chronic active hepatitis | |
| Multiple sclerosis | |
| Myasthenia gravis | |
| Dermatitis herpetiformis | |
| B17 | Psoriasis |
| Bw15 + B8 | Juvenile diabetes |
| DR3 or DR4 | Diabetes associated with beta cell autoantibodies |
| A3 | Hemochromatosis |
| DR4 | Rheumatoid arthritis |
| DR7, DRw3, B8 | Gluten enteropathy |
The HLA-B 1502 allele is associated with hypersensitivity to carbamazepine, phenytoin, and fosphenytoin used to treat epilepsy, manic/bipolar disorders, and neuropathic pain. Hypersensitivity to carbamazepine is a leading cause of Stevens-Johnson syndrome and toxic epidermal necrolysis (SJS/TEN).
Because HLA antigens are genetically determined, they are useful in paternity investigations. This is particularly helpful if the reputed father or child has an unusual HLA genotype. A common HLA genotype in either the father or child increases the likelihood that there are many potential fathers of that child.
Although this test has been performed using serologic methods, PCR using other laboratory methods such as Luminexx technology are primarily utilized. It is important when requesting HLA testing, that the order indicates the specific HLA antigen test to be performed.
Human Placental Lactogen ([hPL], Human Chorionic Somatomammotropin [HCS])
Test Explanation
The human placenta produces several hormones that are homologous to hormones of the anterior pituitary. Human placental lactogen (hPL), whose task is to maintain the pregnancy, is structurally similar to both human prolactin and growth hormone. Not surprisingly, hPL demonstrates both lactogenic and growth-stimulating activity.
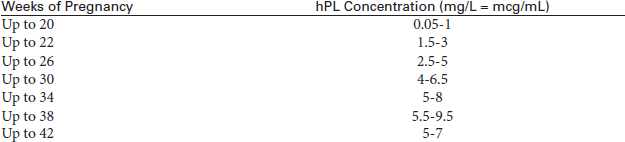
Serum levels of hPL rise very early in normal pregnancy and continue to increase until a plateau is reached at approximately the 35th week postconception. As such, assays for maternal serum levels of hPL are useful in monitoring placental function. Measurements of hPL are also used in pregnancies complicated by hypertension, proteinuria, edema, postmaturity, placental insufficiency, or possible miscarriage.
A decreasing serum concentration of hPL is pathognomonic for a malfunction of the placenta that may cause intrauterine growth restriction, an intrauterine death of the fetus, or an imminent miscarriage. Pregnant women experiencing hypertonia also show low serum concentrations of hPL. Because of the short biologic half-life of hPL in serum, the determination of hPL always gives a very accurate picture of the present situation.
Increased serum concentrations of hPL are found in women suffering from diabetes mellitus (DM) and, because of the higher placental mass, in multiple pregnancies. In contrast to estriol, the hPL concentration only depends on the placental mass and not on the fetal function. The simultaneous determination of hPL and estriol can be helpful in the differential evaluation of the placental function.
No single endocrine test has proved to be effective in all cases. Of the current endocrine factors, serum unconjugated estriol (p. 226) would appear to be the best predictor of fetal distress or well-being. However, estriol interpretation is limited because values experience short-term and daily fluctuations. When following high-risk pregnancies, the delivery decision should not be based on a single factor. Rather, the decision to deliver should be based on the estriol values, hPL, and monitoring of the fetal heart rate in response to contractions or stress (p. 566).
Quantitative (and qualitative) analysis is performed by radial immunodiffusion (RID). ELISA test kits are available and are accurate.
Related Tests
Estrogen Fractions (p. 226). Estrogen fractions are an accurate predictor of the status of the placenta and fetus.
Fetal Contraction Stress Test (p. 566) and Fetal Nonstress Test (p. 569). These are tests of the adequacy of the fetal-placental unit.
Progesterone (p. 416). Progesterone can be used to monitor the status of the placenta.
Human T-Cell Lymphotrophic Virus ([HTLV] I/II Antibody)
Test Explanation
Several forms of HTLV, a human retrovirus, affect humans. HTLV-I is associated with adult T-cell leukemia/lymphoma. HTLV-II is associated with adult hairy-cell leukemia and neurologic disorders such as tropical spastic paraparesis. Humans can be infected with these viruses, however, and not develop any malignancy or diseases.
The human immunodeficiency viruses (HIVs), which are known to be the cause of acquired immunodeficiency syndrome (AIDS), are also retroviruses; however, HTLV infection is not associated with AIDS. HTLV transmission is similar, though, to HIV transmission (e.g., body fluid contamination, intravenous drug use, sexual contact, breastfeeding).
Infection by these viruses results in the appearance of specific antibodies against the viruses that can be detected by serologic tests. Blood and organ donors are routinely tested for the presence of anti-HTLV-I/II antibodies by enzyme immunoassays (EIA), which are highly sensitive but lack specificity. For accurate diagnosis of HTLV-I/II infection, all initially EIA-positive results should be verified by a confirmatory test, such as Western blot or line immunoassay. HTLV-I and -II can also be directly detected by real-time amplification of the specific HTLV genomic DNA sequences from the blood of infected patients.
21-Hydroxylase Antibodies
Test Explanation
Chronic primary adrenal insufficiency (Addison’s disease) is most commonly caused by the insidious autoimmune destruction of the adrenal cortex and is characterized by the presence of adrenal cortex autoantibodies in the serum. It can occur sporadically or in combination with other autoimmune endocrine diseases. This antibody may precipitate this disease. Measurement of this antibody is used in the investigation of causes of adrenal insufficiency.
Immunoglobulin Quantification
Indications
Serum protein quantification is used to detect and monitor the course of hypersensitivity diseases, immune deficiencies, autoimmune diseases, chronic infections, malignancies, and intrauterine fetal infections.
Test Explanation
Proteins within the blood are made up of albumin and globulin. Several types of globulin exist, one of which is gamma globulin. Antibodies are made up of gamma globulin protein and are called immunoglobulins. There are many classes of immunoglobulins (antibodies). Immunoglobulin G (IgG) constitutes approximately 75% of the serum immunoglobulins; therefore it constitutes the majority of circulating blood antibodies. IgA constitutes approximately 15% of the immunoglobulins within the body and is present primarily in secretions of the respiratory and gastrointestinal tracts, saliva, colostrum, and tears. IgA is also present to a smaller degree in the blood. IgM is an immunoglobulin primarily responsible for ABO blood grouping and rheumatoid factor; it is also involved in the immunologic reaction to many infections. IgM does not cross the placenta, therefore an elevation of IgM in a newborn indicates in utero infection such as rubella, cytomegalovirus (CMV), or sexually transmitted disease (STD). IgE often mediates an allergic response and is measured to detect allergic diseases. IgD, which constitutes the smallest part of the immunoglobulins, is rarely evaluated or detected.
Laboratory methods to identify specific light chain monoclonal proteins associated with specific neoplastic and non-neoplastic diseases are increasingly becoming available. Although electrophoresis is usually required to interpret an elevated immunoglobulin class as polyclonal versus monoclonal, immunofixation is usually required to characterize a monoclonal protein. If there is a discrete M-peak, the monoclonal protein can be monitored with quantitative immunoglobulins (in the blood or urine with immunonephelometry).
Increased serum immunoglobulin concentrations occur because of polyclonal or oligoclonal immunoglobulin proliferation in hepatic disease (hepatitis, liver cirrhosis), connective tissue diseases, and both acute and chronic infections. Elevation of immunoglobulins may occur in monoclonal gammopathies such as multiple myeloma, primary systemic amyloidosis, monoclonal gammopathies of undetermined significance, and related disorders. Decreased immunoglobulin levels are found in patients with acquired or congenital immune deficiencies. Specific immunologic testing can indicate the etiologic agents of infection or allergy. It can be used to monitor therapy and recurrence. Testing can determine the type of connective tissue disease, its severity, clinical course, and response to therapy.
Test Results and Clinical Significance
 Decreased IgA Levels
Decreased IgA Levels
 Increased IgG Levels
Increased IgG Levels
Chronic granulomatous infections (e.g., tuberculosis, Wegener granulomatosis, sarcoidosis),
Multiple myeloma (monoclonal IgG type),
Autoimmune diseases (e.g., rheumatoid arthritis, Sjögren disease, systemic lupus erythematosus [SLE]):
All the above conditions stimulate IgG synthesis. The pathophysiology of this observation is not known.
Intrauterine devices: These devices work by creating a subclinical localized inflammatory reaction that is harmful to the sperm. Part of that reaction is the synthesis of IgG.
 Decreased IgG Levels
Decreased IgG Levels
These diseases are a result of a genetic deficiency that results in inadequate synthesis of IgG and other immunoglobulins.
Acquired immunodeficiency syndrome (AIDS): This creates a deficiency throughout the entire immune system. IgG and other immunoglobulins are diminished.
Hypoproteinemia (e.g., nephrotic syndrome, protein-losing enteropathies): The hypoproteinemia that results from these diseases causes the IgG deficiency.
Drug immunosuppression (steroids, dextran): The production of IgG is diminished.
 Increased IgM Levels
Increased IgM Levels
Waldenström macroglobulinemia: This is a malignancy similar to myeloma in which IgM is secreted at high levels by the malignant lymphoplasma cells. It is very similar diagnostically to IgM myeloma.
Chronic infections (e.g., hepatitis, mononucleosis, sarcoidosis): These infections stimulate the humoral response and many of the immunoglobulins, including IgM.
Autoimmune diseases (e.g., SLE, rheumatoid arthritis): The pathophysiology is not well known. It is assumed that these antibodies somehow contribute to the disease process.
Acute infections: IgM is the first immunoglobulin to respond to an infectious agent (viral, bacterial, parasitic).
Chronic liver disorders (e.g., biliary cirrhosis): The pathophysiology is not well defined.
 Decreased IgM Levels
Decreased IgM Levels
Agammaglobulinemia: This disease is a result of a genetic deficiency in which the synthesis of IgM and other immunoglobulins is inadequate.
AIDS: This creates a deficiency throughout the entire immune system. IgM and other immunoglobulins are diminished.
Hypoproteinemia (e.g., nephrotic syndrome, protein-losing enteropathies): The hypoproteinemia that results from these diseases causes the IgM deficiency.
Drug immunosuppression (steroids, dextran): The production of IgM is diminished.
Related Tests
Protein (p. 424). This is a quantification of all the components that make up the serum proteins, including albumin, alpha 1 and 2, beta 1 and 2, and gamma globulins. This test can also detect abnormal proteins created by neoplasms and infections.
Prealbumin (p. 412). This is a quantification of prealbumin, which is a component of proteins. This test is used to assess a person's nutritional status. It is also used to indicate the status of liver function.
Insulin Assay
Indications
This test is used to diagnose insulinoma (tumor of the islets of Langerhans) and to evaluate abnormal lipid and carbohydrate metabolism. It is used in the evaluation of patients with fasting hypoglycemia.
Test Explanation
Insulin regulates blood glucose levels by facilitating the movement of glucose out of the bloodstream and into the cells. Insulin secretion is primarily reactive to the blood glucose level. Normally, as the blood glucose level increases, the insulin level also increases; as the glucose level decreases, insulin release stops.
Some investigators believe that measuring the ratio of the blood sugar and insulin on the same specimen obtained during the oral glucose tolerance (GT) test is more reliable than measuring insulin levels alone. Combined with the oral GT test, the insulin assay can show characteristic curves. For example, patients with juvenile diabetes have low fasting insulin levels and display flat GT insulin curves, because there is little or no increase in insulin levels. Patients who are mildly diabetic have normal fasting insulin levels and display GT curves with a delayed rise.
Type 2 diabetes (adult onset) is characterized by an excess of insulin production in response to GT testing. This hyperresponse of insulin may precede hyperglycemia by many years, allowing the patient time and opportunity to take action to reduce the incidence of outright diabetes through diet management and lifestyle changes.
When combined with a fasting blood sugar, insulin assay is very accurate in detecting insulinoma. After the patient fasts for 12 to 14 hours, the insulin/glucose ratio should be less than 0.3. Patients with insulinoma have ratios greater than this. To increase the sensitivity and specificity of these combined tests for insulinoma, Turner and others have proposed the “amended” insulin/glucose ratios using variable mathematic “fudge” factors:
A Turner amended ratio greater than 50 suggests insulinoma.
Insulin is quantified utilizing immunoassay laboratory methodology such as quantitative electrochemiluminescent immunoassay. Results will vary considerably according to the technique used.
Interfering Factors
• Most patients treated with insulin for diabetes develop insulin antibodies within a few months. These antibodies can interfere with insulin radioimmune assay (RIA) results by competing with the insulin antibodies used in the insulin assay.
• Food intake and obesity may cause increased insulin levels.
![]() Recent administration of radioisotopes may affect test results by interfering with the RIA method to detect insulin.
Recent administration of radioisotopes may affect test results by interfering with the RIA method to detect insulin.
![]() Drugs that may cause increased insulin levels include corticosteroids, levodopa, and oral contraceptives.
Drugs that may cause increased insulin levels include corticosteroids, levodopa, and oral contraceptives.
Procedure and Patient Care
Test Results and Clinical Significance
 Increased Levels
Increased Levels
Insulinoma: This is a tumor of the beta cells in the islets of Langerhans of the pancreas. This is diagnosed in patients who have hyperinsulinemia despite hypoglycemia. These patients have persistently high C-peptide levels despite glucose levels of below 30 mg/dL. The amended Turner insulin/glucose ratio exceeds 50.
Cushing syndrome: The elevated glucose caused by the cortisol overproduction in patients with this syndrome acts as a constant stimulant to insulin.
Acromegaly: The elevated glucose level caused by growth hormone overproduction in the patient with acromegaly acts as a constant stimulant to insulin.
Obesity: These patients have a persistently high insulin level.
Fructose or galactose intolerance: These complex sugars cannot be metabolized normally and, like glucose, stimulate insulin production.
Related Tests
Glucose Tolerance (p. 261). This is a test of a patient's capability to handle a glucose load.
Glucose, Postprandial (p. 257). This is a timed glucose measurement after a carbohydrate meal.
C-Peptide (p. 182). This test is used to evaluate diabetic patients. It is also used to identify patients who secretly self-administer insulin.
Insulin Antibody (p. 206). This test is used in the evaluation of insulin resistance. It is also used to identify type 1 diabetes. It is used when allergy to insulin is suspected.
Insulin-like Growth Factor (IGF-1, Somatomedin C, Insulin-like Growth Factor Binding Proteins [IGF BP])
Indications
This is a screening test to identify patients with growth hormone (GH) deficiency, pituitary insufficiency, and acromegaly. These levels depend on the levels of GH.
Test Explanation
Growth hormone (GH) exerts its effects on many tissues through a group of peptides called somatomedins. The most commonly tested somatomedin is insulin-like growth factor (IGF-1).
Great variation in GH secretion occurs during the day. A random GH assay result may significantly overlap between normal and abnormal values. To diminish the common variations in GH secretion, screening for IFG-1 provides a more accurate reflection of the mean plasma concentration of GH. Somatomedins are not affected (as GH is) by the time of day, food intake, or exercise because they circulate bound to proteins that are durable or long-lasting. As a result there is no overlap of results of IGF-1 between normal and abnormal values. Normally there is a large increase during the pubertal growth spurt.
Levels of IGF-1 depend on levels of GH. As a result, IGF-1 levels are low when GH levels are deficient. (See GH [p. 269] for a discussion of causes of and diseases associated with GH deficiency.) Nonpituitary causes of reduced IGF-1 levels include malnutrition, severe chronic illnesses, severe liver disease, hypothyroidism, renal failure, inflammatory bowel disease, and Laron dwarfism. Abnormally low test results require an abnormally reduced or absent GH during a GH-stimulation test (p. 272) to make the diagnosis of GH deficiency.
Pediatricians commonly use insulin-like growth factor binding proteins (IGF BPs) to even further diminish the impact of the variables affecting GH and somatomedin levels. Specifically IGF BP 2 and IGF BP 3 are the most commonly measured. However, if GH deficiency is strongly suspected yet documentation using GH or somatomedins is questionable, IGF BP determinations are helpful. IGF BP 3 is less age dependent and is the most accurate (97% sensitivity and specificity). These proteins help to evaluate GH deficiencies and GH-resistant syndromes (e.g., Laron dwarfism). Finally these binding proteins are very useful in predicting responses to therapeutic exogenous GH administration.
The causes of short stature and the initial tests for patients with short stature are listed in Box 2-13 and Table 2-34, respectively.
TABLE 2-34
Initial Tests for Patients With Short Stature
| Test | Reason for Test |
| Thyroxine | Rule out hypothyroidism |
| Somatomedin C | Rule out GH deficiency |
| GH | Rule out GH deficiency |
| GH stimulation | Rule out GH deficiency |
| X-ray films of wrists | Document growth retardation |
| Calcium (serum levels) | Rule out pseudohypoparathyroidism |
| Phosphate (serum levels) | Rule out rickets |
| Bicarbonate (serum levels) | Rule out renal tubular acidosis |
| Blood urea nitrogen (BUN) | Rule out renal failure |
| Complete blood cell count | Rule out anemia or nutritional or chronic disorders |
| Sedimentation rate | Rule out inflammatory bowel diseases |
| Chromosomal karyotype | Rule out chromosomal abnormalities (gonadal dysgenesis) |
Test Results and Clinical Significance
 Decreased Levels
Decreased Levels
GH deficiency: Somatomedin C is dependent on GH levels.
Pituitary insufficiency: GH is produced in the pituitary. Diseases, tumors, ischemia, or trauma to the pituitary or hypothalamus causes GH deficiency. Somatomedin C is dependent on GH levels.
Dwarfism: This is a result of GH and somatomedin C deficiency in children.
Laron type dwarfism: This syndrome is associated with GH receptor resistance. Somatomedin C secretion does not occur.
Hyperglycemia: Elevated glucose levels inhibit GH and somatomedin C secretion.
Failure to thrive: This is a result of GH and somatomedin C deficiency in infants.
Delayed sexual maturity: This is a result of GH and somatomedin C deficiency in adolescents.
These diseases lead to hypoproteinemia. Because somatomedin C is a protein, levels will be reduced with hypoproteinemia.
Severe liver disease: Somatomedin C is made in the liver. With severe liver disease, somatomedin levels fall.
Hypothyroidism: Somatomedin C levels fall in hypothyroid patients.
Intrinsic Factor Antibody (IF ab)
Indications
The intrinsic factor antibody is used to diagnose pernicious anemia (PA). It is particularly helpful when the hematologic picture is not fully developed.
Test Explanation
Pernicious anemia is one of the major causes of vitamin B12 deficiency and megaloblastic anemia. It is a disease of the stomach in which secretion of intrinsic factor is severely reduced or absent, resulting in malabsorption of B12. In view of its association with a variety of antibodies, including parietal cell antibody (see p. 92) and at least two types of anti–intrinsic factor antibody, pernicious anemia appears to be an autoimmune process. Antibodies to intrinsic factor are found in very high percentage of children with juvenile pernicious anemia (PA).
Approximately 50% to 75% of adult patients have intrinsic factor antibodies. There are two types of this antibody. Type I, blocking antibody, the more common, prevents the binding of vitamin B12 and intrinsic factor. Type II antibody, binding antibody, is less specific for PA and affects the binding of intrinsic factor in the ileum. The blocking antibody is extremely specific for PA and is more sensitive than binding antibody. In the context of a low or borderline B12 result, where other clinical and hematologic findings are compatible with a diagnosis of B12 deficiency, the presence of intrinsic factor blocking antibody can be taken as confirmation of this diagnosis and, at the same time, as an indication of its cause. A negative result, on the other hand, cannot rule out the possibility of pernicious anemia because blocking antibody is not demonstrable in nearly 50% of all patients with this disorder.
The diagnosis of PA rarely requires vitamin B12 absorption testing (Schilling Test). Testing for antiparietal cell antibodies and intrinsic factor antibodies is easier, quicker, and in most cases more accurate. Rapid testing can be performed easily with radioimmunoassay methods.
Related Tests
Schilling Test. With the use of this test, the ability to absorb vitamin B12 is evaluated. This test is also used in the evaluation of patients with pernicious anemia. This test is no longer a major part of the diagnosis of PA.
Anti–Parietal Cell Antibody (p. 92). This test is used to diagnose PA serologically.
Vitamin B12 (p. 518). This test is a direct measurement of B12 serum levels, known to be reduced in PA.
Iron Level (Fe), Total Iron-Binding Capacity (TIBC), Transferrin, Transferrin Saturation
Indications
These tests are used to evaluate iron metabolism in patients when iron deficiency, overload, or poisoning is suspected.
Test Explanation
Serum Iron
Abnormal levels of iron are characteristic of many diseases, including iron-deficiency anemia and hemochromatosis. As much as 70% of the iron in the body is found in the hemoglobin of the red blood cells (RBCs). The other 30% is stored in the form of ferritin (see p. 234) and hemosiderin. Iron is supplied by the diet. About 10% of the ingested iron is absorbed in the small intestine and transported to the plasma. There the iron is bound to a globulin protein called transferrin and carried to the bone marrow for incorporation into hemoglobin. Transferrin exists in relationship to the need for iron. When iron stores are low, transferrin levels increase, whereas transferrin is low when there is too much iron. Usually about one third of the transferrin is being used to transport iron. Because of this, the blood serum has considerable extra iron-binding capacity, which is the Unsaturated Iron Binding Capacity (UIBC). The TIBC equals UIBC plus the serum iron measurement. Some laboratories measure UIBC, some measure TIBC, and some measure transferrin. The serum iron determination is a measurement of the quantity of iron bound to transferrin.
Iron-deficiency anemia is a result of reduced stored iron. It has many causes, including (1) insufficient iron intake, (2) inadequate gut absorption, (3) increased requirements (as in growing children and late pregnancy), and (4) loss of blood (as in menstruation, bleeding peptic ulcer, colon neoplasm). Iron deficiency results in a decreased production of hemoglobin, which in turn results in a small, pale (microcytic, hypochromic) RBC. A decrease in the mean corpuscular volume and mean corpuscular hemoglobin concentration (see p. 442) is also seen. A decreased serum iron level, elevated total iron-binding capacity (TIBC), and low transferrin saturation value are characteristic of iron-deficiency anemia.
Acute iron poisoning due to accidental or intentional overdose is characterized by a serum iron level that exceeds the total iron binding capacity (TIBC). Chronic iron overload or poisoning is called hemochromatosis or hemosiderosis. Excess iron is usually deposited in the brain, liver, and heart and causes severe dysfunction of these organs. Massive blood transfusions also may cause elevated serum iron levels, although only transiently. Transfusions should be avoided before serum iron level determinations.
Because serum iron levels may vary significantly during the day, the blood specimen should be drawn in the morning, especially when the results are used to monitor iron replacement therapy. The patient should refrain from eating for approximately 12 hours to avoid artificially high iron measurements caused by eating food with a high iron content.
TIBC and Transferrin
TIBC is a measurement of all proteins available for binding mobile iron. Transferrin represents the largest quantity of iron-binding proteins. Therefore TIBC is an indirect yet accurate measurement of transferrin. Ferritin is not included in TIBC, because it binds only stored iron. During iron overload, transferrin levels stay about the same or decrease, whereas the other less common iron-carrying proteins increase in number. In this situation, TIBC is less reflective of true transferrin levels. TIBC is increased in 70% of patients with iron deficiency.
Transferrin is a negative acute-phase reactant protein. That is, in various acute inflammatory reactions, transferrin levels diminish. Transferrin also is diminished in patients with chronic illnesses such as malignancy, collagen-vascular diseases, or liver diseases. Hypoproteinemia is also associated with reduced transferrin levels. Pregnancy and estrogen therapy are associated with increased transferrin levels.
TIBC is usually measured by adding excess iron to the patient's serum. This saturates all the transferrin. Excess iron is removed. The iron that is left is a direct measurement of TIBC and an indirect measurement of transferrin. Many laboratories do not perform TIBC measurements; in this case, transferrin is measured directly.
TIBC varies minimally with iron intake. TIBC is more a reflection of liver function (transferrin is produced by the liver) and nutrition than of iron metabolism. TIBC values often are used to monitor the course of patients receiving hyperalimentation.
TIBC and Transferrin Saturation
The percentage of transferrin and other mobile iron-binding proteins saturated with iron is calculated by dividing the serum iron level by the TIBC.
The normal value for transferrin saturation is 20% to 50%. Calculation of transferrin saturation is helpful in determining the cause of abnormal iron and TIBC levels. Transferrin saturation is decreased to below 15% in patients with iron deficiency anemia. It is increased in patients with hemolytic, sideroblastic, or megaloblastic anemias and also in patients with iron overload or iron poisoning. Increased intake or absorption of iron (as in hemochromatosis) leads to elevated iron levels. In such cases the TIBC is unchanged; as a result, the percentage of transferrin saturation is very high. Unsaturated iron binding capacity (UIBC) has been proposed as an inexpensive alternative to transferrin saturation.
Chronic illness (e.g., infections, neoplasia, cirrhosis) is characterized by a low serum iron level, decreased TIBC, and normal transferrin saturation. Pregnancy is marked by high levels of protein, including transferrin. Because iron requirements are high, it is not unusual to find low serum iron levels, high TIBC, and a low percentage of transferrin saturation in late pregnancy.
Interfering Factors
• Recent blood transfusions may increase serum iron.
• Recent ingestion of a meal containing high iron content may increase serum iron.
• Hemolytic diseases may be associated with an artificially high iron content.
![]() Drugs that may cause increased iron levels include chloramphenicol, dextran, estrogens, ethanol, iron preparations, methyldopa, and oral contraceptives.
Drugs that may cause increased iron levels include chloramphenicol, dextran, estrogens, ethanol, iron preparations, methyldopa, and oral contraceptives.
![]() Drugs that may cause decreased iron levels include adrenocorticotropic hormone (ACTH), cholestyramine, chloramphenicol, colchicine, deferoxamine, methicillin, and testosterone.
Drugs that may cause decreased iron levels include adrenocorticotropic hormone (ACTH), cholestyramine, chloramphenicol, colchicine, deferoxamine, methicillin, and testosterone.
![]() Drugs that may cause increased TIBC levels include fluorides and oral contraceptives.
Drugs that may cause increased TIBC levels include fluorides and oral contraceptives.
![]() Drugs that may cause decreased TIBC levels include ACTH and chloramphenicol.
Drugs that may cause decreased TIBC levels include ACTH and chloramphenicol.
Test Results and Clinical Significance
 Increased Serum Iron Levels
Increased Serum Iron Levels
Hemosiderosis or hemochromatosis: These two forms of iron deposits are created by serum iron excesses. They can be acquired or result from a genetic defect in iron metabolism.
Iron poisoning: Increased iron intake increases serum iron levels.
Hemolytic anemia: The iron in the hemoglobin of the hemolyzed RBCs leaks out into the bloodstream.
Massive blood transfusions: There is about 1 mg of iron in each milliliter of packed RBCs.
Hepatitis or hepatic necrosis: The pathophysiology of this observation is not well established.
Lead toxicity: The lead overload may displace the iron stores.
 Decreased Serum Iron Levels
Decreased Serum Iron Levels
Insufficient dietary iron: Because all body iron is from dietary intake, a persistently reduced intake will lead to reduced serum levels.
Chronic blood loss (irregular menses, uterine cancer, GI cancer, inflammatory bowel disease, diverticulosis, urologic tract [hematuria] cancer, hemangioma, arteriovenous malformation): Chronic blood loss depletes the iron because most of the iron in the body exists in the hemoglobin of the RBCs.
Inadequate intestinal absorption of iron (e.g., malabsorption, short-bowel syndrome): Because all body iron is from dietary intake, a persistently reduced intake will lead to reduced serum levels.
Pregnancy (late): Fetal requirements deplete the mother's body store of iron.
Iron-deficiency anemia: This anemia results when iron and iron stores become depleted.
Neoplasia: Iron levels are depleted in these patients for several reasons.
 Decreased TIBC or Transferrin Levels
Decreased TIBC or Transferrin Levels
Related Test
Ferritin (p. 234). This is a measure of iron stores and is the most accurate indicator of iron deficiency.
Ischemia-Modified Albumin (IMA)
Indications
This test is performed on patients with chest pain to determine if the pain is caused by cardiac ischemia.
Test Explanation
When albumin is exposed to an ischemic environment its N terminal is altered causing an alteration of the albumin called ischemia-modified albumin (IMA). This has become particularly helpful in identifying cardiac ischemia. When combined with troponins (p. 508), myoglobin (p. 365), and ECG, the diagnosis of an ischemic cardiac event can be corroborated or ruled out. IMA is produced continually during the period of ischemia. Blood levels will rise within 10 minutes of the initiation of the ischemic event and stay elevated for 6 hours after ischemia has resolved.
Normally, the N terminal of albumin can easily bind heavy metals, such as cobalt. In contrast, IMA cannot bind cobalt. This reality forms the basis for IMA testing. In the Cobalt Binding Test, cobalt is added to the patient's serum. Unbound cobalt levels are measured. Higher levels of unbound cobalt indicate greater concentrations of IMA, which in turn indicates cardiac ischemia.
IMA may also be elevated in patients with pulmonary embolus or acute stroke. False positives can occur in other clinical circumstances such as advance cancers, acute infections, and endstage renal or liver disease.
Procedure and Patient Care
During
• Collect a venous blood sample in a yellow-top (serum separator) tube. This is usually done after the initial onset of chest pain, then 12 hours later, and then daily testing for 3 to 5 days.
• Rotate the venipuncture sites.
• Record the exact time and date of venipuncture on each laboratory slip. This aids in the interpretation of the temporal pattern of blood level elevations.
Related Tests
Creatine Phosphokinase MB (p. 186). Elevation of CPK-MB on this blood test is closely linked to myocardial muscle. It is elevated early in myocardial injury. Its usefulness is limited in patients who have had chest pain for more than 24 hours.
Myoglobin (p. 365). This protein is a nonspecific indicator of cardiac disease. However, it is also elevated with skeletal muscle disease or trauma.
Electrocardiogram (ECG) (p. 544). This is the electrodiagnostic test most commonly used to detect myocardial injury and infarction.
Troponins (p. 508). This test is a specific indicator of cardiac muscle injury. It is also helpful in predicting the possibility of future cardiac events.
Lactic Acid (Lactate)
Indications
Measurement of lactic acid is helpful to document and quantify the degree of tissue hypoxemia associated with shock or localized vascular occlusion. It is also a measurement of the degree of success associated with treatment of those conditions.
Test Explanation
Under conditions of normal oxygen availability to tissues, glucose is metabolized to CO2 and H2O for energy. When oxygen to the tissues is diminished, anaerobic metabolism of glucose occurs, and lactate (lactic acid) is formed instead of CO2 and H2O. To compound the problem of lactic acid buildup, when the liver is hypoxic, it fails to clear the lactic acid. Lactic acid accumulates, causing lactic acidosis (LA). Therefore blood lactate is a fairly sensitive and reliable indicator of tissue hypoxia. The hypoxia may be caused by local tissue hypoxia (e.g., mesenteric ischemia, extremity ischemia) or generalized tissue hypoxia such as exists in shock. Lactic acid blood levels are used to document the presence of tissue hypoxia, determine the degree of hypoxia, and monitor the effect of therapy. Type I LA is caused by diseases that increase lactate but are not hypoxia related, such as glycogen storage diseases or liver diseases, or by drugs. LA caused by hypoxia is classified as type II. Shock, convulsions, and extremity ischemia are the most common causes of type II LA. Type III LA is idiopathic and is most commonly seen in nonketotic patients with diabetes. The pathophysiology of lactic acid accumulation in type III LA is not known.
Test Results and Clinical Significance
 Increased Levels
Increased Levels
Anaerobic metabolism occurs in hypoxemic organs and tissues. As a result, lactic acid is formed, causing increased blood levels.
Carbon monoxide poisoning: Carbon monoxide binds hemoglobin more tightly than oxygen. Therefore no oxygen is available to the tissues for normal aerobic metabolism. Anaerobic metabolism occurs and lactic acid is formed, resulting in increased blood levels.
Acquired and genetic diseases associated with inefficient aerobic glucose metabolism causes increased amounts of lactic acid to be synthesized. Therefore blood levels rise.
Diabetes mellitus (nonketotic): Lactic acid levels rise in patients with poorly controlled diabetes most likely because of inefficient aerobic glucose metabolism, causing increased production of this product.
Related Test
Arterial Blood Gases (p. 109). This is a measure of acid-base balance of the blood. An increased level of lactic acid is associated with metabolic acidosis.
Lactic Dehydrogenase (LDH, Lactate Dehydrogenase)
Indications
This is an intracellular enzyme used to support the diagnosis of injury or disease involving the heart, liver, red blood cells (RBCs), kidneys, skeletal muscle, brain, and lungs.
Test Explanation
The enzyme LDH is found in the cells of many body tissues, especially the heart, liver, RBCs, kidneys, skeletal muscle, brain, and lungs. Because LDH is widely distributed through the body, the total LDH level is not a specific indicator of any one disease or indicative of injury to any one organ. When disease or injury affects the cells containing LDH, the cells lyse and LDH is spilled into the bloodstream where it is identified in higher than normal levels. The LDH is a measure of total LDH. Actually five separate fractions (isoenzymes) make up the total LDH. Each tissue contains a predominance of one or more LDH enzymes (Table 2-35).
In general, isoenzyme LDH-1 comes mainly from the heart; LDH-2 comes primarily from the reticuloendothelial system; LDH-3 comes from the lungs and other tissues; LDH-4 comes from the kidney, placenta, and pancreas; and LDH-5 comes mainly from the liver and striated muscle. In normal persons, LDH-2 makes up the greatest percentage of total LDH.
Specific patterns of LDH isoenzymes are considered classic for certain diseases. For example:
• Isolated elevation of LDH-1 (above LDH-2) indicates myocardial injury.
• Isolated elevation of LDH-5 indicates hepatocellular injury or disease.
• Elevation of LDH-2 and LDH-3 indicates pulmonary injury or disease.
• Elevation of all LDH isoenzymes indicates multiorgan injury (e.g., myocardial infarction [MI] with congestive heart failure [CHF] causing pulmonary and hepatic congestion along with decreased renal perfusion). Advanced malignancy and diffuse autoimmune inflammatory diseases such as lupus can also cause this pattern.
With myocardial injury, the serum LDH level rises within 24 to 48 hours after an MI, peaks in 2 to 3 days, and returns to normal in approximately 5 to 10 days. This makes the serum LDH level especially useful for a delayed diagnosis of MI (e.g., when the patient reports having had severe chest pain 4 days earlier). The LDH-1 is generally not as useful as troponin (p. 508) or creatine kinase-MB (p. 186) for the detection of MI, unless the MI occurred 24 hours or more prior to the assay.
It is important to note that two diseases causing elevated LDH may coexist and that one may obscure the other. For example, a patient who has one disease (e.g., pulmonary infarction or congestive heart failure) may also be having an acute MI. The elevation in LDH-1 may be obscured by the elevation of LDH-2 or LDH-3.
LDH is also measured in other body fluids. Elevated urine levels of total LDH indicate neoplasm or injury to the urologic system. When the LDH in an effusion (pleural, cardiac, peritoneal) is greater than 60% of the serum total LDH (i.e., effusion LDH/serum LDH ratio >0.6), the effusion is said to be an exudate and not a transudate.
Interfering Factors
• Hemolysis of blood will cause false-positive LDH levels because LDH exists in the RBCs. Lysis of these cells causes the LDH to pour out into the specimen blood and falsely elevate the LDH level.
• Strenuous exercise may cause elevation of total LDH and specifically LDH-1, LDH-2, and LDH-5.
![]() Drugs that may cause increased LDH levels include alcohol, anesthetics, aspirin, clofibrate, fluorides, mithramycin, narcotics, and procainamide.
Drugs that may cause increased LDH levels include alcohol, anesthetics, aspirin, clofibrate, fluorides, mithramycin, narcotics, and procainamide.
![]() Drugs that may cause decreased levels include ascorbic acid.
Drugs that may cause decreased levels include ascorbic acid.
Test Results and Clinical Significance
 Increased Levels
Increased Levels
MI: These patients classically have significant elevations in LDH-1 and, to a lesser degree, LDH-2.
Pulmonary disease (e.g., embolism, infarction, pneumonia, CHF): These patients classically have significant elevations in LDH-2 and LDH-3.
Hepatic disease (e.g., hepatitis, active cirrhosis, neoplasm): These patients classically have significant elevations in LDH-5.
RBC disease (e.g., hemolytic or megaloblastic anemia, RBC destruction from prosthetic heart valves): These patients classically have significant elevations in LDH-1.
Skeletal muscle disease and injury (e.g., muscular dystrophy, recent strenuous exercises, muscular trauma): These patients classically have significant elevations in LDH-5.
Renal parenchymal disease (e.g., infarction, glomerulonephritis, acute tubular necrosis, kidney transplantation rejection): These patients classically have significant elevations in LDH-1.
Intestinal ischemia and infarction: These patients classically have significant elevations in LDH-5.
Testicular tumors (seminoma, dysgerminomas):
Lymphoma and other reticuloendothelial system (RES) tumors: These patients classically have significant elevations in LDH-3 and LDH-2.
Advanced solid tumor malignancies: These patients classically have significant elevations in all LDH isoenzymes.
Pancreatitis: These patients classically have significant elevations in LDH-4.
Diffuse disease or injury (e.g., heat stroke, collagen disease, shock, hypotension): These patients classically have significant elevations in all LDH isoenzymes.
Related Tests
Aspartate Aminotransferase (AST) (p. 119). This is another enzyme existing predominantly in the liver.
Gamma-Glutamyl Transpeptidase (GGTP) (p. 246). This is another enzyme existing predominantly in the liver.
Alkaline Phosphatase (p. 47). This is another enzyme existing predominantly in the liver.
5'-Nucleotidase (p. 376). This is another enzyme existing predominantly in the liver.
Creatine Phosphokinase (CPK) (p. 186). This enzyme is used predominantly to evaluate heart and skeletal muscle.
Alanine Aminotransferase (ALT) (p. 39). This enzyme is used similarly to aspartate aminotransferase and exists predominantly in the liver.
Leucine Aminopeptidase (LAP) (p. 337). This enzyme is specific to the hepatobiliary system. Diseases affecting that system will cause elevation of this enzyme.
Lactose Tolerance
Indications
This test is used to identify patients who have lactose intolerance caused by lactase insufficiency, intestinal malabsorption, maldigestion, or bacterial overgrowth in the small intestine. This test is performed on adults who complain of diarrhea and in infants who have failure to thrive, persistent diarrhea, or vomiting.
Test Explanation
This test is performed to detect lactose intolerance. Lactose is a disaccharide typically found in dairy products; during digestion, lactose is broken down into glucose and galactose by the intestinal enzyme lactase. Because lactose-intolerant patients have an absence of lactase, lactose digestion will not occur. Likewise, patients with other causes of malabsorption or maldigestion also will not absorb lactose. Glucose plasma will not rise after the ingestion and the small bowel is flooded with a high lactose load. Bacterial catabolism of the lactose occurs within the intestine. This creates excess hydrogen ions and methane (flatus). It also has a strong cathartic effect. Symptoms of lactose intolerance include flatulence, abdominal cramping, abdominal bloating, diarrhea, and failure to thrive in infants. Although all adults have some degree of lactase reduction, severe lactose intolerance can occur in patients with inflammatory bowel disease, short-gut syndrome, and other malabsorption syndromes. Lactase deficiency can be congenital and become apparent in the newborn.
The incidence of primary lactose deficiency is greater than 50% in several ethnic groups, such as Mediterranean, black African, and Asian. Northern European and North American Caucasians are the only population groups able to maintain small-intestinal lactase activity throughout life.
In this test a lactose load is given. If lactase is not present in sufficient quantities, lactose is not metabolized to glucose and galactose. Plasma levels of glucose do not rise as expected. Therefore lower-than-expected serum glucose levels suggest no absorption. Patients who have malabsorption without lactase deficiency will also fail to elevate the blood glucose levels, not because the lactose was not broken down but because the glucose could not be absorbed. These patients can be evaluated by following the lactose tolerance test with a glucose tolerance test. That is, after a positive lactose tolerance test, the patient returns and is given 25 g of a glucose/galactose preparation. A normal increase in glucose indicates that the patient can absorb glucose and that the problem is, indeed, lactase insufficiency.
There is also a breath test portion to this test in which the exhaled air is analyzed for hydrogen content. This is called the lactose breath test (or hydrogen breath test). The bacteria in the colon produce hydrogen when exposed to unabsorbed food, particularly the lactose load that was not absorbed in the small intestine. Large amounts of hydrogen may also be produced when the colonic bacteria move back into the small intestine, a condition called bacterial overgrowth of the small bowel. In this instance, the bacteria are exposed to the lactose load, which has not had a chance to completely traverse the small intestine to be fully digested and absorbed. Large amounts of the hydrogen produced by the bacteria are absorbed into the blood flowing through the wall of the small intestine and colon. This hydrogen-containing blood travels to the lungs, where the hydrogen is released and exhaled in the breath in measurable quantities.
Prior to lactose hydrogen breath testing, individuals must fast for at least 12 hours. At the start of the test, the individual blows into a hydrogen analyzer. The individual then ingests a small amount of the test sugar (lactose, sucrose, sorbitol, fructose, lactulose, etc., depending on the purpose of the test). Additional samples of breath are collected and analyzed for hydrogen every 15 minutes for 1 to 5 hours. When rapid intestinal transit is present, the test dose of nondigestible lactulose reaches the colon more quickly than normal, and therefore hydrogen is produced by the colonic bacteria soon after the sugar is ingested. When bacterial overgrowth of the small bowel is present, ingestion of lactulose results in two separate periods during the test in which hydrogen is produced, an earlier period caused by the bacteria in the small intestine and a later one caused by the bacteria in the colon.
Interfering Factors
• Enterogenous steatorrhea (i.e., malabsorption) will diminish absorption of glucose from the gut even if the lactose is broken down by normal levels of lactase.
• Strenuous exercise will reduce the glucose levels and possibly give a false-positive result.
• Diabetics may have a rise in glucose levels that exceed 20 mg/dL despite lactase insufficiency.
• Smoking may increase blood glucose levels and cause false-positive results.
• Ethnicity has a major impact on primary lactose deficiency.
![]() Antibiotics can decrease the bacteria in the intestine and may cause false-negative breath tests. They should not be taken for 1 month before testing.
Antibiotics can decrease the bacteria in the intestine and may cause false-negative breath tests. They should not be taken for 1 month before testing.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient. Inform the patient that four blood samples will be needed.
Explain the procedure to the patient. Inform the patient that four blood samples will be needed.
![]() Instruct the patient to fast for 8 hours before testing.
Instruct the patient to fast for 8 hours before testing.
![]() Instruct the patient to avoid strenuous exercise for 8 hours before testing because it may factitiously affect the blood glucose level.
Instruct the patient to avoid strenuous exercise for 8 hours before testing because it may factitiously affect the blood glucose level.
![]() Inform the patient that smoking is prohibited before testing. This may falsely increase the blood glucose level.
Inform the patient that smoking is prohibited before testing. This may falsely increase the blood glucose level.
During
• Obtain a venous blood sample in a gray-top tube from the fasting patient.
• Provide a specified dose of lactose for the patient. Usually 100 g of lactose is diluted with 200 mL of water for ingestion in adults.
• Note that pediatric doses of lactose are based on weight.
• Collect three more blood samples at 30, 60, and 120 minutes after the ingestion of lactose.
![]() Tell the patient that the only discomfort is the venipuncture; however, patients with lactase deficiency may have symptoms such as cramps and diarrhea.
Tell the patient that the only discomfort is the venipuncture; however, patients with lactase deficiency may have symptoms such as cramps and diarrhea.
• If the breath test is being done, the exhaled air is evaluated for hydrogen content before ingestion of lactose and every 15 minutes thereafter. Hydrogen levels are recorded for 2 hours.
Test Results and Clinical Significance
 Decreased Levels
Decreased Levels
Lactase insufficiency: Lactase quantities are insufficient to break down the lactose load. Glucose is not absorbed, and serum glucose levels do not rise.
Enterogenous diarrhea: Despite normal breakdown of lactose, the glucose is not absorbed because of malabsorption disease of the gut. Serum glucose levels do not rise.
Related Test
Glucose Tolerance (p. 261). This test is used to assist in the diagnosis of diabetes mellitus (DM). It is also used in the evaluation of patients with hypoglycemia. Because it differentiates the lactase-deficient patient from the patient with enterogenous malabsorption diarrhea, this test is helpful in the evaluation of patients suspected of having lactose intolerance.